Incidence and Prevalence of ESKD
According to the Korean ESKD registry (1), in 2018 there were 17,621 incident ESKD patients in Korea. The unadjusted incidence rate was 340.0 per million population (PMP) (Table 1). The number of patients with incident ESKD continued to increase until 2006, plateaued between 2007 and 2009, and rose again from 2010 (Figure 1A). This trend in rising ESKD incidence rate implies increasing burden of CKD, which is attributable to the aging Korean population and high rate of diabetes mellitus (DM) and hypertension.
Table 1.
Trends in annual number of patients with incident ESKD and incidence rates of ESKD in the Korean population, 2000–2018
| Hemodialysis | Peritoneal Dialysis | Transplant Recipients | All ESKD | |||||||||
| Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year |
| 2000 | 2736 | 57.0 | N/A | 1021 | 21.3 | N/A | 683 | 14.2 | N/A | 4440 | 92.5 | N/A |
| 2001 | 3373 | 69.9 | 22.6 | 1279 | 26.5 | 24.4 | 848 | 17.6 | 23.9 | 5500 | 113.9 | 23.1 |
| 2002 | 3878 | 79.9 | 14.3 | 1666 | 34.3 | 29.4 | 739 | 15.2 | −13.6 | 6283 | 129.5 | 13.7 |
| 2003 | 4769 | 97.7 | 22.2 | 1866 | 38.2 | 11.4 | 806 | 16.5 | 8.6 | 7441 | 152.4 | 17.7 |
| 2004 | 5279 | 107.6 | 10.1 | 2246 | 45.8 | 19.9 | 853 | 17.4 | 5.5 | 8378 | 170.8 | 12.1 |
| 2005 | 5400 | 109.6 | 1.9 | 2381 | 48.3 | 5.5 | 762 | 15.5 | −10.9 | 8543 | 173.4 | 1.5 |
| 2006 | 5694 | 114.7 | 4.7 | 2568 | 51.7 | 7.0 | 935 | 18.8 | 21.3 | 9197 | 185.3 | 6.9 |
| 2007 | 6193 | 123.8 | 7.9 | 2062 | 41.2 | −20.3 | 928 | 18.5 | −1.6 | 9183 | 183.5 | −1.0 |
| 2008 | 6415 | 127.3 | 2.8 | 1619 | 32.1 | −22.1 | 1145 | 22.7 | 22.7 | 9179 | 182.1 | −0.8 |
| 2009 | 6540 | 129.1 | 1.4 | 1125 | 22.2 | −30.8 | 1241 | 24.5 | 7.9 | 8906 | 175.8 | −3.5 |
| 2010 | 7204 | 140.1 | 8.5 | 867 | 16.9 | −23.9 | 1264 | 24.6 | 0.4 | 9335 | 181.5 | 3.2 |
| 2011 | 8057 | 155.8 | 11.2 | 920 | 17.8 | 5.3 | 1639 | 31.7 | 28.9 | 10,616 | 205.3 | 13.1 |
| 2012 | 8811 | 169.8 | 9.0 | 923 | 17.8 | 0.0 | 1738 | 33.5 | 5.7 | 11,472 | 221.1 | 7.7 |
| 2013 | 9543 | 183.3 | 8.0 | 884 | 17.0 | −4.5 | 1756 | 33.7 | 0.6 | 12,183 | 234.0 | 5.8 |
| 2014 | 10,594 | 206.4 | 12.6 | 867 | 16.9 | −0.6 | 1680 | 32.7 | −3.0 | 13,141 | 256.0 | 9.4 |
| 2015 | 12,011 | 233.1 | 12.9 | 854 | 16.6 | −1.8 | 1891 | 36.7 | 12.2 | 14,756 | 286.4 | 11.9 |
| 2016 | 13,049 | 252.4 | 8.3 | 786 | 15.2 | −8.4 | 2233 | 43.2 | 17.7 | 16,068 | 310.8 | 8.5 |
| 2017 | 13,754 | 265.6 | 5.2 | 742 | 14.3 | −5.9 | 2163 | 41.8 | −3.2 | 16,659 | 321.7 | 3.5 |
| 2018 | 14,779 | 285.2 | 7.4 | 735 | 14.2 | −0.7 | 2107 | 40.7 | −2.6 | 17,621 | 340.0 | 5.7 |
N/A, not applicable.
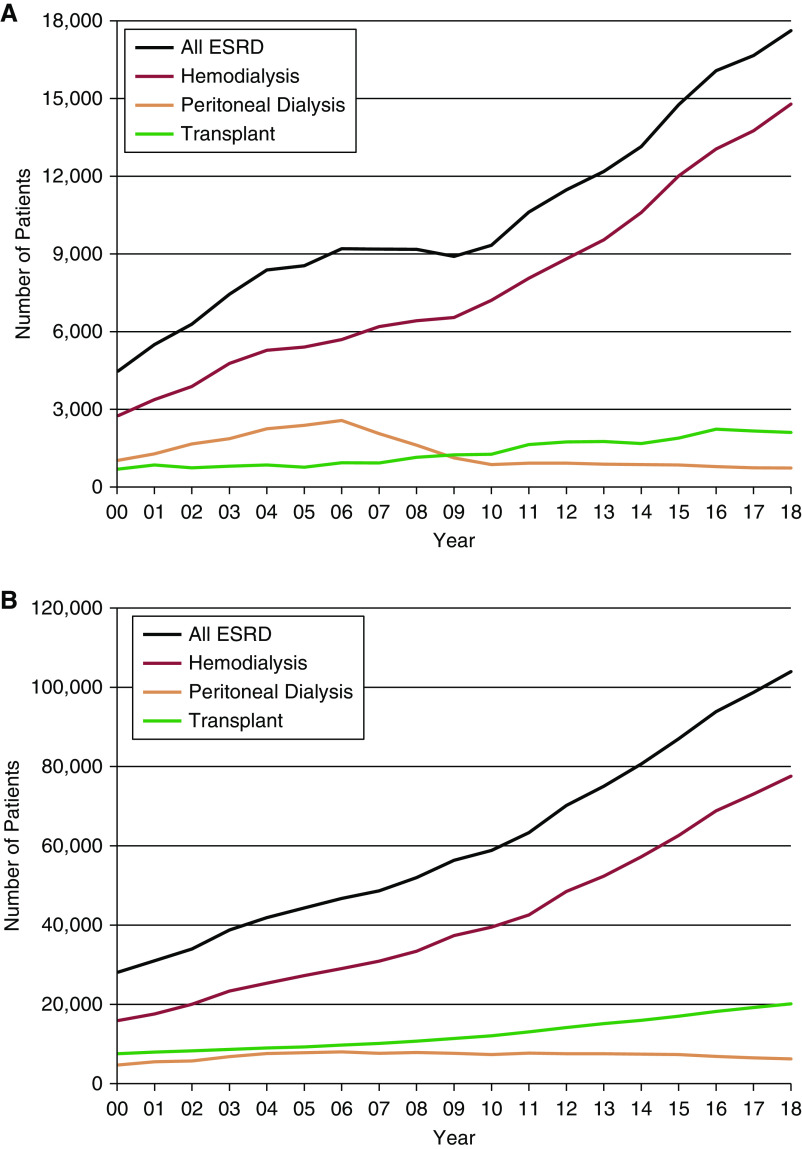
Figure 1.
Trends in the annual number of patients (A) with incident ESKD or (B) with prevalent ESKD by modality in the Korean population, 2000-2018. The number of patients with incident and prevalent HD has steadily increased. The number of patients with incident and prevalent PD continuously declined since 2006. The number of kidney transplants has gradually increased and plateaued since 2016.
On December 31, 2018, there were 103,984 patients with prevalent ESKD in Korea, representing a 271% increase since 2000. The unadjusted prevalence rate was 2006.4 PMP (Table 1), which ranked high globally (2). Prevalence rate of ESKD has steadily increased year after year (Figure 1B).
Treatment Modality
Hemodialysis (HD) was the predominant form of ESKD treatment modality in all years in both patients with incident and prevalent ESKD. The number of patients with incident peritoneal dialysis (PD) rapidly increased from the late 1990s and peaked in 2006 (n=2568), then declined every year until 2018 (n=735, a decrease of 71%) (Figure1A, Table 1). The ratio of HD to PD gradually changed from 68.9:31.1 in 2006 to 95.3:4.7 in 2018 in patients with incident ESKD, and from 78.4:21.6 in 2006 to 92.5:7.5 in 2018 in patients with prevalent ESKD (Figure 1B, Table 2). There are several potential reasons for the increasing HD use and decreasing PD use. First, the number of HD units increased continuously and rapidly since 2000 (n=304 in 2000, n=487 in 2005, n=631 in 2010, n=846 in 2015, and n=983 in 2018), probably because of higher dialysis facility revenues from HD than from PD. The high number of HD units provided patients on dialysis easy access to HD units in most areas. Second, because of low dialysis facility revenues, only university hospitals (10% of all dialysis units) and a few general hospitals offer PD facilities. Third, because the number of patients on PD decreased significantly, many nephrologists do not have sufficient knowledge, training, clinical experience, or confidence managing patients on PD, and so they prefer HD as a dialysis modality. Doctor’s preference may affect the patient’s decision about dialysis modality. Public policies need to be developed to reboot PD use (3,4). All patients on HD have received in-center HD because home HD is not available yet, due to lack of reimbursement and systematic support. The number of kidney transplants (KTs) rose from 2006, which was partly ascribed to an increase in deceased donor KT, and plateaued from 2016. An analysis of transplantation registry data revealed potential reasons for plateau of KT number since 2016. First, the number of transplantation centers has almost plateaued since 2016 (n=103 in 2016 and n=107 in 2018). Second, deceased donor KT has also plateaued since 2015 (n=263 in 2006, n=680 in 2011, n=901 in 2015, n=1059 in 2016, n=903 in 2017, and n=807 in 2018). There were 2107 KTs in 2018, which was a 208% increase since 2000. On December 31, 2018, 75% of patients with prevalent ESKD were receiving HD therapy, 6% were treated with PD, and 19% had a functioning KT (Table 2).
Table 2.
Trends in annual number of patients with prevalent ESKD and prevalence rates of ESKD in the Korean population, 2000–2018
| Hemodialysis | Peritoneal Dialysis | Functioning Kidney Transplant | All ESKD | |||||||||
| Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year | No. of Patients | Unadjusted Rate (per million population) | % Change from Previous Year |
| 2000 | 15,853 | 330.4 | N/A | 4671 | 97.4 | N/A | 7522 | 156.8 | N/A | 28,046 | 584.5 | N/A |
| 2001 | 17,568 | 363.8 | 10.1 | 5489 | 113.7 | 16.7 | 7957 | 164.8 | 5.1 | 31,014 | 642.3 | 9.9 |
| 2002 | 20,010 | 412.4 | 13.4 | 5712 | 117.7 | 3.5 | 8271 | 170.5 | 3.5 | 33,993 | 700.6 | 9.1 |
| 2003 | 23,348 | 478.2 | 16.0 | 6807 | 139.4 | 18.4 | 8635 | 176.9 | 3.8 | 38,790 | 794.5 | 13.4 |
| 2004 | 25,335 | 516.5 | 8.0 | 7569 | 154.3 | 10.7 | 8987 | 183.2 | 3.6 | 41,891 | 854.0 | 7.5 |
| 2005 | 27,246 | 553.0 | 7.1 | 7816 | 158.6 | 2.8 | 9271 | 188.2 | 2.7 | 44,333 | 899.8 | 5.4 |
| 2006 | 29,031 | 585.0 | 5.8 | 7990 | 161.0 | 1.5 | 9709 | 195.7 | 4.0 | 46,730 | 941.7 | 4.7 |
| 2007 | 30,907 | 617.7 | 5.6 | 7649 | 152.9 | −5.3 | 10,119 | 202.2 | 3.3 | 48,675 | 972.8 | 3.3 |
| 2008 | 33,427 | 663.3 | 7.4 | 7840 | 155.6 | 1.8 | 10,722 | 212.8 | 5.2 | 51,989 | 1031.6 | 6.0 |
| 2009 | 37,391 | 738.3 | 11.3 | 7618 | 150.4 | −3.3 | 11,387 | 224.8 | 5.6 | 56,396 | 1113.5 | 7.9 |
| 2010 | 39,509 | 768.1 | 4.0 | 7309 | 142.1 | −5.5 | 12,042 | 234.1 | 4.1 | 58,860 | 1144.4 | 2.8 |
| 2011 | 42,596 | 823.6 | 7.2 | 7694 | 148.8 | 4.7 | 13,051 | 252.4 | 7.8 | 63,341 | 1224.8 | 7.0 |
| 2012 | 48,531 | 935.4 | 13.6 | 7552 | 145.6 | −2.2 | 14,128 | 272.3 | 7.9 | 70,211 | 1353.3 | 10.5 |
| 2013 | 52,378 | 1006.1 | 7.6 | 7540 | 144.8 | −0.5 | 15,124 | 290.5 | 6.7 | 75,042 | 1441.5 | 6.5 |
| 2014 | 57,256 | 1115.3 | 10.9 | 7423 | 144.6 | −0.1 | 15,995 | 311.6 | 7.3 | 80,674 | 1571.5 | 9.0 |
| 2015 | 62,634 | 1215.5 | 9.0 | 7352 | 142.7 | −1.3 | 17,028 | 330.5 | 6.1 | 87,014 | 1688.6 | 7.5 |
| 2016 | 68,853 | 1331.9 | 9.6 | 6842 | 132.4 | −7.2 | 18,189 | 351.8 | 6.4 | 93,884 | 1816.1 | 7.6 |
| 2017 | 73,059 | 1411.0 | 5.9 | 6475 | 125.1 | −5.5 | 19,212 | 371.0 | 5.5 | 98,746 | 1907.1 | 5.0 |
| 2018 | 77,617 | 1497.6 | 6.1 | 6248 | 120.6 | −3.6 | 20,119 | 388.2 | 4.6 | 103,984 | 2006.4 | 5.2 |
N/A, not applicable.
Dialysis Units
On December 31, 2018, there were 983 dialysis units and 28,355 HD machines in Korea. The number of dialysis units and HD machines has increased by 223% and 444%, respectively, since 2000. The mean number of HD machine was 29 in a dialysis unit. All dialysis units are for-profit, 45% are freestanding, and 55% are hospital-based units including 10% university hospitals. Generally, patients receive HD treatment in a dialysis unit that is close to their home or work, because the quality of care and the dialysis cost are not different between freestanding and hospital-based units. However, university hospitals care for fragile patients who have more comorbidities and need specialized care from multiple departments. Patients on PD are treated only in university hospitals and a few general hospitals. A dialysis unit staff is simply composed of nephrologists and registered nurses. Technicians, nurse practitioners, or physicians’ assistants have not been established in Korea. All cannulation procedures are performed by nurses. The nurse-to-patient ratio is 1:8.3. A nephrologist who is in charge of the dialysis unit does rounds every day for patients on dialysis, and nephrology fellows in the university hospitals take care of patients under the supervision of the professors.
Causes of ESKD
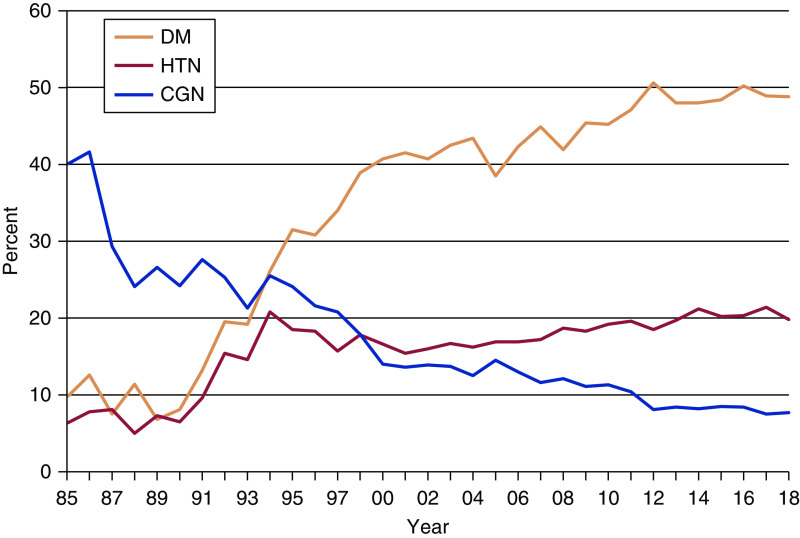
Primary causes of ESKD in incident patients in 2018 were DM (49%), hypertension (20%), chronic GN (8%; kidney biopsy-proven 3%, pathology unknown 4%), cystic kidney disease (2%), interstitial nephritis (0.5%), lupus nephritis (0.5%), hereditary nephropathy (0.3%), kidney tumor (0.3%), toxic nephropathy (0.2%), gouty nephropathy (0.2%), other (5%), and unknown (16%). The number of diabetic patients with ESKD rapidly increased from the early 1990s, became a leading primary cause of ESKD from 1994, and plateaued since 2012 (Figure 2). Korea is one of the countries for which DM is listed as the primary cause of ESKD (2).
Figure 2.
Trends in three leading causes of ESKD. CGN, chronic GN; DM, diabetes mellitus; HTN, hypertension.
Trends in Sex, Age, Duration of Dialysis Therapy, and Dialysis Therapy
In 2018, the male-to-female ratio was 60:40 in HD and 57:43 in PD. The ratio has remained same for the past 10 years. The mean age of patients on prevalent dialysis has continued to increase and was 62.3±14.4 years in 2018, which was 10 years older than the mean age of patients in 2000 (52.3±13.6 years). Elderly patients (≥65 years old) comprised 47% of all patients on dialysis. Patients on HD were older than those on PD (63.2±14.1 years versus 54.8±14.3 years) in 2018.
Duration of dialysis therapy has been prolonged in both HD and PD. In 2018, the proportion of the patients who have been maintained on dialysis for >5 years was 48% in HD and 53% in PD.
In 2018, 92% of patients on HD were receiving HD three times a week. Those who had a good amount of residual renal function or were being treated in combination with PD were receiving HD once or twice a week. In patients on PD, use of automated peritoneal dialysis has been increased since 2006, comprising 39% of patients on PD in 2018. The typical HD treatment time is 4 hours per session, and blood flow rate is 250–300 ml/min in most patients. Use of high-flux dialyzers is the standard care for HD. In 2019, high-flux dialyzers were used in 84% of all HD sessions.
Clinical Parameters
In December 2017, the majority (63%) of patients on HD had hemoglobin (Hgb) levels from 10 to <12 g/dl, 7% had Hgb ≥12 g/dl, 21% had Hgb from 9 to <10 g/dl, and 9% had Hgb <9 g/dl. The mean Hgb was 10.4 g/dl. In December 2017, the majority (53%) of patients on PD had Hgb levels from 10 to <12 g/dl, 8% had Hgb ≥12 g/dl, 24% had Hgb from 9 to <10 g/dl, and 15% had Hgb <9 g/dl. The mean Hgb was 10.3 g/dl. As of 2018, erythropoiesis-stimulating agents were prescribed to 86% of patients on HD and 84% of patients on PD.
Regarding dialysis adequacy in 2018, mean single-pool Kt/Vurea was 1.58±0.30 in patients on prevalent HD, and was higher in women (1.75±0.30) than in men (1.46±0.25). Mean urea reduction ratio was 73%±7% (women: 76%±6%, men: 70%±6%). Mean normalized protein catabolic rate was 0.98±0.28 g/kg per day (men: 0.94±0.26 g/kg per day, women: 1.05±0.30 g/kg per day).
In 2018, mean serum calcium levels were 8.76±0.94 mg/dl and 8.65±0.99 mg/dl in patients on HD and those on PD, respectively. Mean serum phosphorus levels were 4.99±1.66 mg/dl and 5.38±1.67 mg/dl in patients on HD and those on PD, respectively
The proportion of patients taking calcium-based phosphate binder decreased from 67% in 2012 to 43% in 2018, whereas the proportion of patients taking sevelamer or lanthanum increased from 12% in 2012 to 27% in 2018.
In 2018, 47% of patients on PD had a job (full time: 36%, part time: 11%), whereas 33% of patients on HD had a job (full time: 23%, part time: 10%). Patients on dialysis are considered severely disabled. The Ministry of Employment and Labor enacted a law providing for the employment of disabled persons. All workplaces having >100 staff are mandated to employ a certain number of disabled people (approximately 3% of all staff) according to the law. The government imposes a fine if they do not employ disabled people, and provides a financial incentive if they do. In addition, disabled people are financially and systematically supported by the law when they go into independent business. This law supports the high employment rate for patients on dialysis.
Insurance and Reimbursement
The National Health Insurance Service (NHIS) serves as the insurer, and makes the reimbursement policies. It is compulsory in Korea for an individual to take out medical insurance. Since January 2010, a patient on dialysis pays 10% of medical costs, including dialysis and interventional procedures for dialysis access, and the 90% remainder is borne by the NHIS. Some low-income patients (approximately 21% of all patients on dialysis) are exempt from the 10% payment of medical cost. The NHIS is a unique medical insurance system. All medical services including dialysis should be government funded, and a private medical insurance system is banned by law in Korea.
One session of HD costs approximately $135, arteriovenous fistula creation costs $658, arteriovenous graft creation costs $640, AVF or AVG angiography costs $345, percutaneous transluminal angioplasty costs $1050, mechanical thrombectomy costs $1141, and tunneled HD catheter insertion with fluoroscopy costs $152.
Vascular Access and Establishment of Interventional Nephrology
The type of HD vascular access has remained same for the past 5 years (in 2018: arteriovenous fistulas 77%, arteriovenous grafts 15%, central venous catheters 8%). PD catheter was mostly inserted surgically (67%), and swan neck straight-tip PD catheter was the most commonly used (48%). Vascular access has been created by surgeons (vascular surgeons approximately 60%). Tunneled central venous HD catheter insertion and endovascular intervention such as percutaneous transluminal angioplasty and thrombectomy have been mostly performed by radiologists (approximately 70%) (5).
Since 2010, nephrologists became interested in and trained in interventional nephrology, and began to play roles in vascular access management. Tunneled HD catheter insertion and endovascular intervention by nephrologists have slowly but consistently increased.
Recently, the number of central venous HD catheter insertion has decreased (303.8 catheters per 1000 patients on HD per year in 2010, 260.9 catheters per 1000 patients on HD per year in 2016), and tunneled HD catheter has been inserted more than nontunneled HD catheter, indicating that vascular access has been created timely and the vascular access team has been educated about and are following international guidelines (5).
Cause of Death
Cardiovascular disease accounted for 45% of known causes of death (cardiac 34%, vascular 12%) among patients on dialysis, followed by infectious disease (23%). Analysis of the mortality hazard ratio showed that low body mass index, low Hgb, low serum albumin, low phosphorus, and low URR were associated with a significantly increased mortality risk (6). Five-year survival rate was significantly lower in diabetic patients on HD compared with nondiabetic patients on HD (7).
Summary
The characteristics of dialysis therapy in Korea can be summarized as high incidence and prevalence rates of patients with ESKD, decreasing PD use, an increasing proportion of elderly patients, a high rate of diabetic patients, a sufficient number of HD units providing easy access, a unique insurance system enabling patients to pay low costs for dialysis, a high rate of adequate dialysis, and a high rate of arteriovenous fistula as HD vascular access (Table 3). Public policy to increase PD use will be a big challenge we have to rise to in the near future.
Table 3.
Characteristics of dialysis therapy in Korea
| No. of patients on dialysis | 83,865; 1618.2 per million population (December 31, 2018) |
| Percentage of patients on home dialysis | 7.5% (December 31, 2018) |
| Dialysis session covered by insurance | 90% of total cost, patient pays 10% of cost |
| Dialysis units: hospital-based versus freestanding | Hospital-based 54.9% versus freestanding 45.1% |
| Dialysis units: for-profit or nonprofit | For-profit |
| Reimbursement per dialysis session | $135 |
| Staff who deliver dialysis: nurses or technicians | Nurses |
| The nurse-to-patient ratio | 1:8.3 |
| Average length of a dialysis session | 4 h |
| Frequency that patients are seen by nephrologists | Every dialysis session |
| Type of vascular access | arteriovenous fistulas 77%, arteriovenous grafts 15%, central venous catheters 8% |
Disclosures
Y.-S. Kim and D.-C. Jin have nothing to disclose.
Author Contributions
Y.-S. Kim was responsible for data curation, formal analysis, and methodology, and wrote the original draft; and D.-C. Jin was responsible for formal analysis, investigation, methodology, and validation.
References
- 1.ESRD Registry Committee : Korean Society of Nephrology: Current Renal Replacement Therapy in Korea, 2018. Available at: http://www.ksn.or.kr/rang_board/list.html?code=sinchart_eng. Accessed September 23, 2019
- 2.U.S. Renal Data System : USRDS 2018 Annual Data Report: International Comparisons. 2018. Available at: https://www.usrds.org/2018/download/v2_c11_IntComp_18_usrds.pdf. Accessed September 23, 2019
- 3.Sloan CE, Coffman CJ, Sanders LL, Maciejewski ML, Lee SD, Hirth RA, Wang V: Trends in peritoneal dialysis use in the United States after Medicare payment reform [published online ahead of print November 21, 2019]. Clin J Am Soc Nephrol doi: 10.2215/CJN.05910519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young EW, Kapke A, Ding Z, Baker R, Pearson J, Cogan C, Mukhopadhyay P, Turenne MN: Peritoneal dialysis patient outcomes under the Medicare expanded dialysis prospective payment system. Clin J Am Soc Nephrol 14: 1466–1474, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim Y-S, Kim Y, Shin SJ, Lee HS, Kim SG, Cho S, Na KR, Kim JK, Kim SJ, Kim YO, Jin D-C: Current state of dialysis access management in Korea. J Vasc Access 20[Suppl]: 15–19, 2019 [DOI] [PubMed] [Google Scholar]
- 6.Jin DC: Analysis of mortality risk from Korean hemodialysis registry data 2017. Kidney Res Clin Pract 38: 169–175, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin DC, Yun SR, Lee SW, Han SW, Kim W, Park J, Kim YK: Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney Res Clin Pract 37: 20–29, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]