Abstract
Objective
We sought to report on the demographics and epidemiology of knee cartilage injuries and preferred management in soccer players, across FIFA Medical Centers of Excellence (FMCE).
Design
A descriptive questionnaire focusing on characteristics of knee cartilage injuries and their management in soccer players during the 10-year period prior to the distribution of the questionnaire was sent to all FMCE around the world in September 2019 via an online platform. Voluntary responses from centers were processed and analyzed. Descriptive characteristics were reported using median and interquartile ranges (IQR) for continuous variables and frequencies and percentages (%) for discrete variables.
Results
A total of 15 centers from 5 continents responded to the questionnaire and reported on a total of 4526 soccer players. Among centers, the median age was 27 years (IQR: 23-38), the median rate of male players was 75% (IQR: 68-90), and the median rate of professional players was 10% (IQR: 5-23). The most common reported etiology for cartilage injury was traumatic (median 40%, IQR: 13-73). The most common nonoperative treatment utilized was physical therapy (median 90%, IQR: 51%-100%) and the most common operative treatment utilized was bone marrow stimulation/micro-fracture (median 40%, IQR: 19-54%). The utilization of other cartilage restoration procedures varied across centers.
Conclusions
Our findings highlight different tendencies in the management of these injuries across FMCE and emphasize the need for collaborative efforts focusing on establishing consensus guidelines for the optimal management of these challenging injuries in soccer players.
Keywords: articular cartilage, articular cartilage repair, soccer athlete, knee injections, physical therapy, osteochondral allograft, osteochondral autograft, bone marrow stimulation, osteochondral allograft transplantation, osteotomy
Introduction
Soccer players have an overall high prevalence of knee articular cartilage lesions (from 36% in asymptomatic players and up to 98% in symptomatic).1-4 This high prevalence, which includes different lesion grades and locations, is attributed to the high prevalence of anterior cruciate ligament (ACL) and meniscal injuries, as well as the inherent risks of the game.1,2,5 The symptomatic articular cartilage lesions may lead to reduced athletic performance, an early career ending, and also early onset of knee osteoarthritis.1,2,5-7
The management of symptomatic articular cartilage lesions is complex and multifactorial with numerous treatment options (both nonoperative and operative).8-10 Despite significant developments in recent years, optimal management of cartilage injuries in the athletic population remains highly challenging and controversial and has yet to be determined. In addition, there is limited evidence regarding the rate of return and timing of return to high-demand athletics following the various treatment options. A recent meta-analysis on return to sport after the surgical management of articular cartilage lesions in the knee 11 reported on an overall 76% return to sport at mid-term follow-up in athletes undergoing various procedures for symptomatic chondral defects; however, the included studies lacked studies investigating higher demand athletes (i.e., cutting/pivoting sports), such as soccer players.
FIFA Medical Centers of Excellence (FMCE) accreditation is provided to established centers around the world which have demonstrated their leadership in soccer medicine and routinely treat high-demand athletes. Considering the recognized interest in improving our understanding of cartilage injuries and their optimal management in soccer players and acknowledging the importance of active collaboration between centers of excellence around the world, the aim of this study was to report on the demographics and epidemiology of knee cartilage injury and the management of these injuries in soccer players, across FMCE. The rational for this study was that mapping current trends and tendencies in different locations around the world can add to the important base of knowledge needed for the development and promotion of innovative prevention and treatment strategies aiming to reduce the incidence of cartilage injury and risk of osteoarthritis in soccer players of all ages and skill levels.
Methods
The study was approved by our institutional review board and the FIFA Medical Committee. A descriptive questionnaire focusing on the demographics of symptomatic knee cartilage injuries and their management in soccer players (Appendix A available online) was sent via an online platform to all FMCE using the official FMCE email list during the period of September 2019. Centers were asked to base their answers on genuine collected data or provide an experience-based estimation wherever formal data was absent. Voluntary responses from centers were processed and analyzed. Our institutional cartilage registry was interrogated in order to provide the data required for patients treated at our institution who self-identified themselves as soccer players and diagnosed with cartilage injury.
Descriptive characteristics were reported using medians and interquartile ranges (IQR) for continuous variables and frequencies and percentages (%) for discrete variables. Our analysis was a center-based analysis, with measurements among centers and not among players.
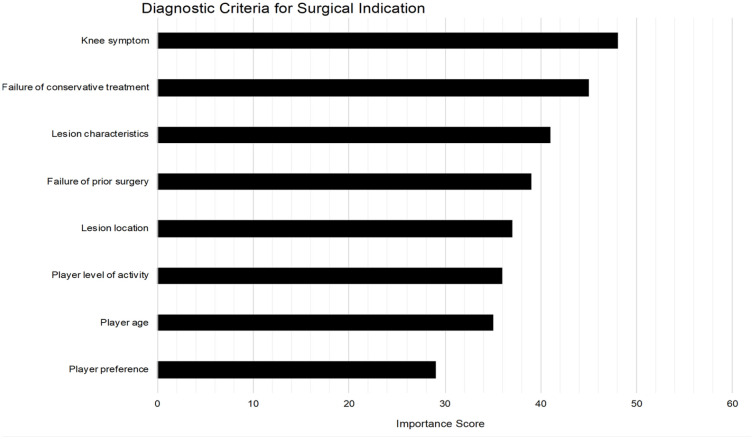
For calculation of the importance of diagnostic criteria used to indicate operative treatment (question number 50, Appendix A available online), the relevant responses for each criterion were converted to representative numbers in the following way: not important was converted to “0,” mildly important converted to “1,” moderately important was converted to “2,” very important was converted to “3,” and the most important was converted to “4.” Summation of the numbers for each criterion from all 15 relevant FMCE was referred to as the “importance score.”
For cartilage lesions etiology, the following definition were used: Traumatic, a traumatic cartilage lesion as a result of a clear traumatic injury; Congenital, an osteochondral lesion representing osteochondritis dissecans; Combined, symptoms followed a traumatic event with the symptomatic lesion diagnosed as osteochondritis dissecans; Overload, a lesion secondary to compartmental overload due to malalignment, meniscal damage, instability. Osteoarthritis, lesion/s secondary to degenerative compartment/joint changes.
For presentation of the data, the centers were anonymized, and each center was given a number by which it is represented throughout this study.
Results
A total of 15 centers from 5 continents responded to the questionnaire ( Table 1 ).
Table 1.
Responding FIFA Medical Centers of Excellence (N = 15).
| Continent | Country | City (State) |
|---|---|---|
| Africa | South Africa | Cape Town |
| North America | USA | Durham (North Carolina) |
| New York (New York) | ||
| South America | Mexico | Zapopan |
| Pachuca | ||
| Asia | Japan | Kobe |
| Tokyo | ||
| Thailand | Bangkok | |
| Europe | Austria | Innsbruck |
| Belgium | Liège | |
| France | Lyon | |
| Germany | Munich | |
| Spain | Madrid | |
| Sweden | Stockholm | |
| Turkey | Istanbul |
Demographics
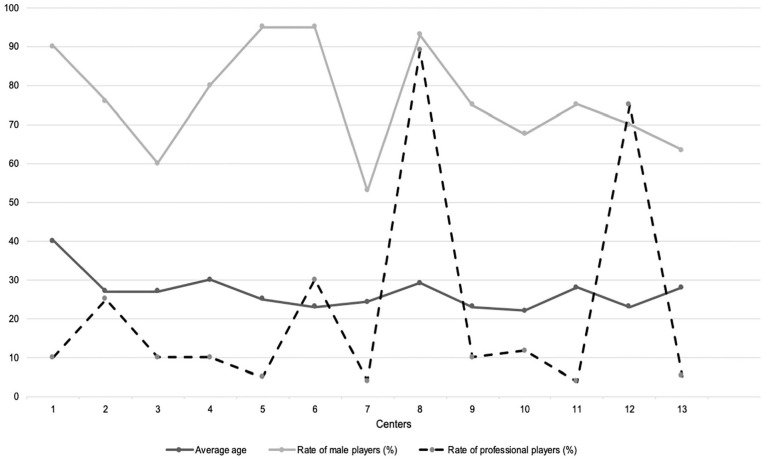
A total of 4526 soccer players treated in the past 10 years for a diagnosis of symptomatic cartilage injury were reported on by all centers combined (median: 95 players per center; IQR: 58-90). In the past 3 years, a median of 12 players per year (IQR: 10-18) were treated in each center. Across all centers, the median age was 27 years (IQR: 23-28), a median of 75% were male players (IQR: 68-90) and a median of 10% were professional players (IQR: 5-23). Figure 1 represents the distribution of data across centers, for average age and rate of male and professional players.
Figure 1.
Summary of the demographics of soccer players who were treated for a symptomatic cartilage injury in the various centers. Thirteen of 15 Centers provided full responses and are represented by numbers.
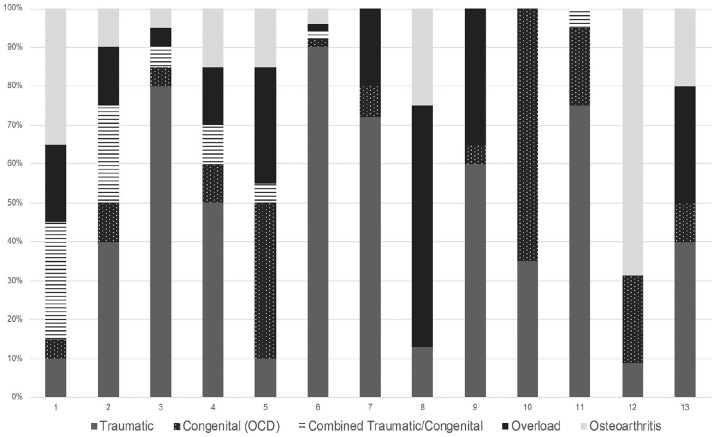
Cartilage Lesion Characteristics
The most common reported etiology for cartilage injury was traumatic (median 40%, IQR: 13-73) and the most common location was the medial femoral condyle (median 30%, IQR: 17-35). See Table 2 and Figure 2 for more lesion characteristics.
Table 2.
Cartilage Lesion Characteristics of Soccer Players Diagnosed with Symptomatic Cartilage Injury Based on Past 10 Years of Experience in FMCE Around the World. a
| Question | N | Median (IQR) | |
|---|---|---|---|
| Etiology (%) | Traumatic | 13 | 40 (13-73) |
| Congenital | 13 | 10 (5-20) | |
| Combined b | 13 | 2 (0-5) | |
| Overload | 13 | 15 (2-30) | |
| Osteoarthritis/degenerative | 13 | 10 (4-20) | |
| Lesion location (%) | LFC | 12 | 26 (18-32) |
| MFC | 12 | 30 (17-35) | |
| LTP | 12 | 5 (1-8) | |
| MTP | 12 | 6 (4-18) | |
| Patella | 12 | 16 (15-23) | |
| Trochlea | 12 | 15 (7-20) | |
| Bipolar lesions (%) | Medial compartment | 12 | 5 (0-23) |
| Lateral compartment | 12 | 11 (2-23) | |
| Patellofemoral compartment | 12 | 10 (4-35) | |
| Mean lesion area (cm2) | LFC | 12 | 2 (2-3.1) |
| MFC | 12 | 2 (1.6-2.5) | |
| LTP | 8 | 1.5 (1.3-2) | |
| MTP | 8 | 1.8 (1.5-2) | |
| Patella | 10 | 2 (1.6-2.5) | |
| Trochlea | 8 | 2 (1.8-2.5) | |
FMCE = FIFA Medical Centers of Excellence; IQR = interquartile range; LFC = lateral femoral condyle; MFC = medial femoral condyle; LTP = lateral tibial plateau; MTP = medial tibial plateau.
Data presented as the median of rates reported by FMCE for each category.
Congenial and traumatic.
Figure 2.
Cartilage lesions etiology in soccer players diagnosed with symptomatic cartilage injury, based on past 10 years of experience in FMCE around the world. Centers providing these data are presented as numbers. OCD, osteochondritis dissecans.
Treatment Strategies
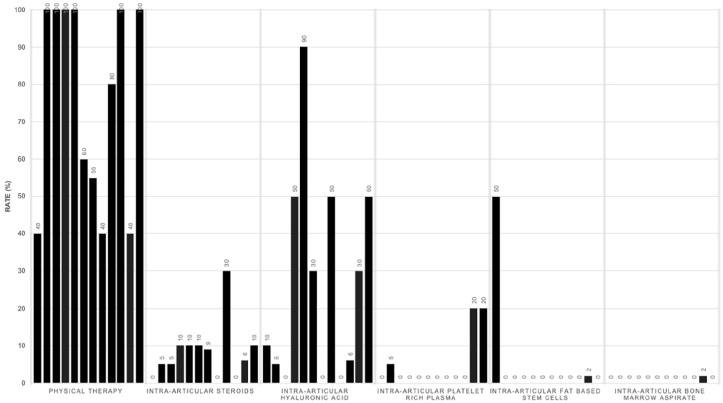
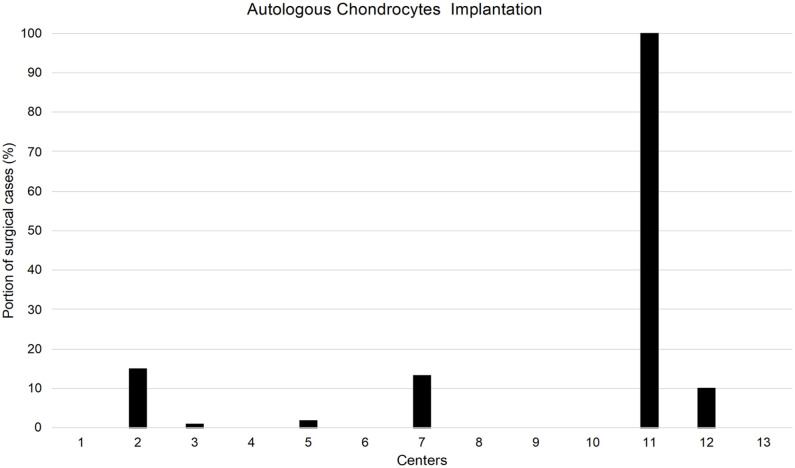
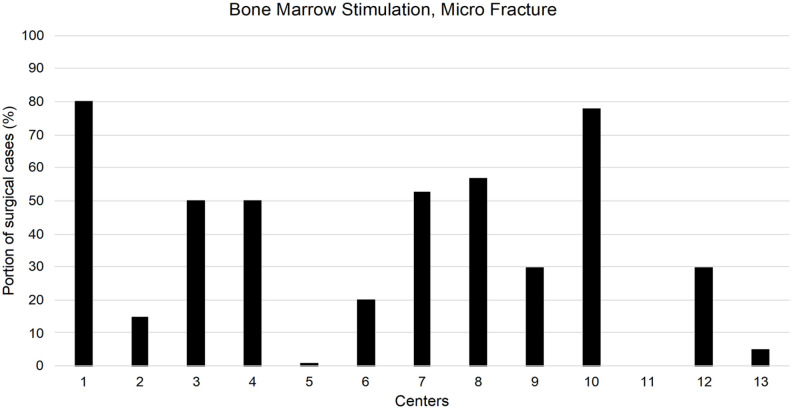
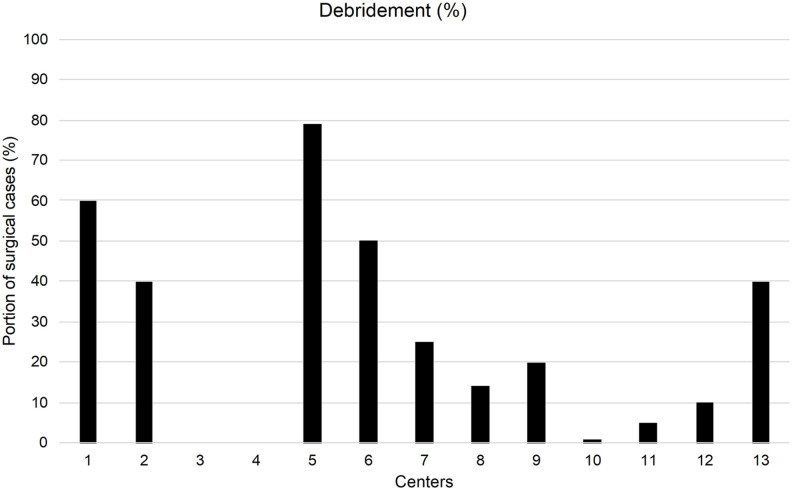
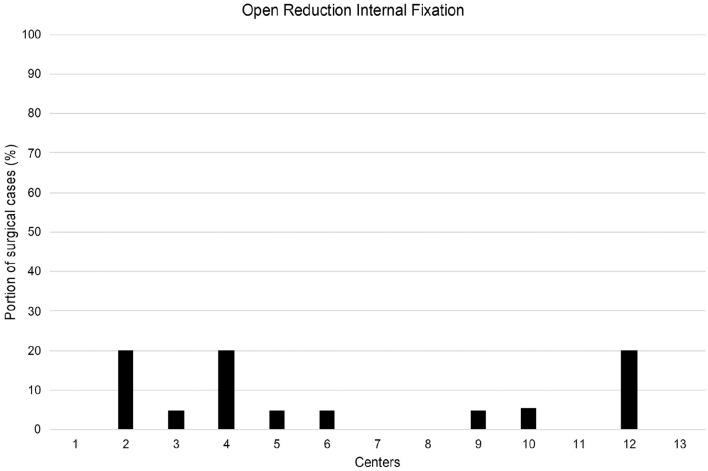
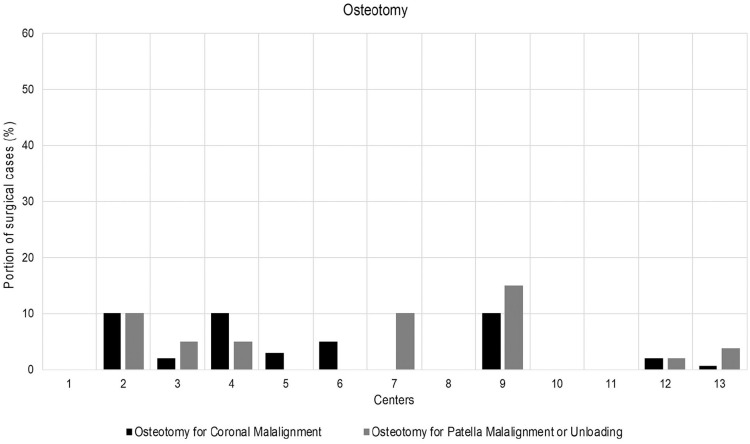
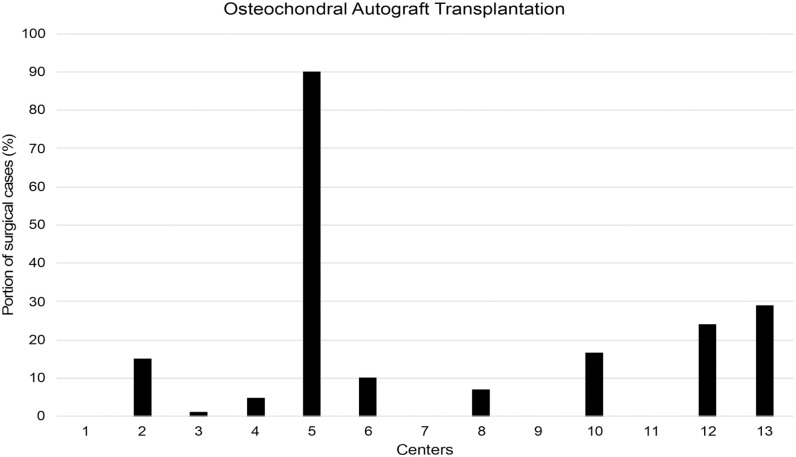
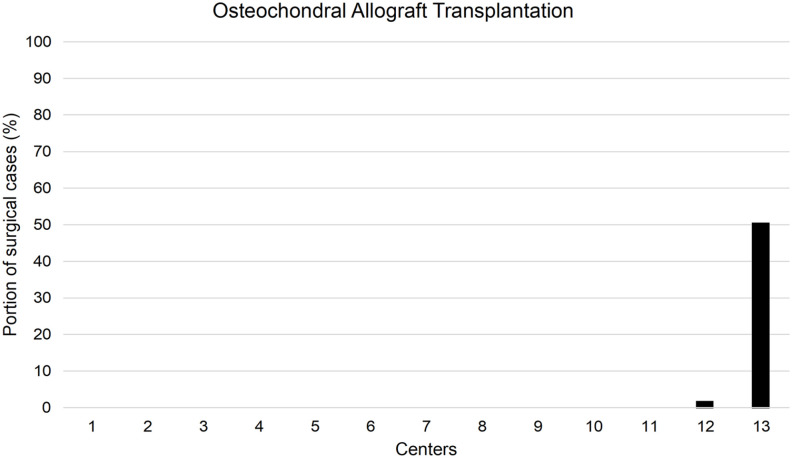
Across centers, a median of 50% (IQR: 25%-75%) of players were treated nonoperatively and a median of 50% (IQR: 25%-75%) were treated operatively. The most common nonoperative modality was physical therapy (median 90%, IQR: 51%-100%), followed by intra-articular hyaluronic acid injection (median 30%, range: 5%-50%). The most common operative treatment was bone marrow stimulation/microfracture (median 40%, IQR: 19%-54%). Two centers reported on augmentation of surgical procedures with biologic injections. One center reported iliac crest bone marrow aspirate injection in 26% of surgical cases and adipose tissue–derived cells (Lipogems, Lipogems International S.p.A, Milan, Italy) injection in 1.5% of surgical cases. Another center reported on adipose tissue derived cells (Lipogems) injection in 5% of surgical cases. Table 3 and Figures 3 to 10 show more treatment characteristic.
Table 3.
Treatment Strategies for Soccer Players Diagnosed with Cartilage Injury Based on Past 10 Years of Experience in Responding FMCE.
| Treatment | N | Median | IQR |
|---|---|---|---|
| Nonoperative (%) | 14 | 50 | 25-75 |
| Physical therapy | 12 | 90 | 51-100 |
| IA steroids | 10 | 10 | 5-10 |
| IA HA | 11 | 30 | 5-50 |
| IA PRP | 12 | 0 | 0-3 |
| IA stem cells (fat) | 11 | 0 | 0-1 |
| IA bone marrow | 11 | 0 | 0 |
| Operative (%) | 14 | 50 | 25-75 |
| Debridement | 12 | 23 | 9-43 |
| ORIF | 11 | 5 | 3-13 |
| Bone marrow stimulation | 14 | 40 | 19-54 |
| Osteochondral autograft | 12 | 9 | 1-15 |
| Osteochondral allograft | 11 | 0 | 0 |
| Autologous chondrocytes | 12 | 1 | 0-11 |
| Coronal osteotomy | 11 | 2 | 0-8 |
| TTO | 11 | 4 | 0-8 |
FMCE = FIFA Medical Centers of Excellence; IQR = interquartile range; IA = intra-articular; HA = hyaluronic acid; PRP = platelet-rich plasma; ORIF = open reduction internal fixation; TTO = tibial tuberosity osteotomy.
Figure 3.
Distribution of rates of the different non-operative treatments utilized across responding FMCE. For each treatment, responses from center’s numbered 1 to 10, 12, and 14 are presented in that order from left to right.
Figure 10.
Distribution of rates of surgical treatment with autologous chondrocytes implantation across responding FMCE.
Fifteen centers graded the criteria for surgical intervention. Knee symptoms was the diagnostic criterion receiving the highest importance score (48) for indicating surgery, followed by failure of conservative treatment (45) and cartilage lesion characteristics (41). The criterion receiving the lowest score was player’s preference (29) ( Fig. 11 ).
Figure 11.
Diagnostic criteria indicating surgical treatment and their importance in the decision-making process.
Return to Soccer
Return to soccer data are reported in Table 4 .
Table 4.
Return to Soccer of Players Diagnosed with Cartilage Injury Based on Past 10 Years of Experience in FMCE Around the World.
| Treatment | N | Median (IQR) |
|---|---|---|
| Nonoperative (%) | 12 | 80 (73-98) |
| Operative (%) | 13 | 75 (68-86) |
| Time to return to play a | ||
| Nonoperative (weeks) | 11 | 11 (7-15) |
| Operative (weeks) | 14 | 28 (18-30) |
FMCE = FIFA Medical Centers of Excellence; IQR = interquartile range.
Participation in games.
Discussion
Soccer players are a heterogeneous group of athletes characterized by a wide age range, different sex, different level of play, different positions played and more. In addition, different medical centers in the world are treating different portions of this population based on their location, the local soccer culture (e.g., a local soccer league for retired older people), the center’s expertise (e.g., a center being a referral center for cartilage injuries), the center’s coverage of local soccer teams and more. This heterogeneity is well represented in the results of this study ( Table 2 , Fig. 1 ) and should always be taken to consideration when evaluating injury patterns, their management, and outcomes in soccer players. Specifically, when analyzing and discussing this study’s results, it should be noted that this study did not aim to evaluate and compare a specific scenario-based treatment plan, but rather reporting on demographic and management trends across FMCE, acknowledging differences in population characteristic and injury patterns and their possible influence on the preferred treatment. Readers are encouraged to take this into consideration.
Focusing on symptomatic cartilage lesions characteristics in soccer players across all the responding FMCE, our results suggest that femoral condyles lesions are more common than lesions in other locations in the knee (medial more than lateral), followed by patella lesions. Similar findings were shown previously for professional soccer players undergoing osteochondral autograft transplantation surgery for symptomatic cartilage lesion. 12 Looking at the general athletic populations, Krych et al. 11 reported in their meta-analysis of athletes who underwent cartilage restoration procedures, on similar findings with majority of lesion in the medial femoral condyle (56%), followed by the lateral femoral condyle (23%).
Despite recent years advancements in treatment options for symptomatic cartilage injuries and the growing body of literature, this study shows there are still different approaches to the management of these injuries in soccer players. While all FMCE are recognized centers from around the world that have demonstrated their leadership in soccer medicine and routinely treat athletes of all levels, it is interesting to see that some centers reported they rarely indicate any active soccer player with symptomatic cartilage injury for surgical cartilage treatment, while other centers reported on doing it routinely. We approached a surgeon in one of the centers that reported on nonoperative treatments in most cases (90%) and he clarified they prefer nonoperative treatment even for players with larger full thickness cartilage lesions, with good return-to-soccer rates. He added they may consider surgery at the end of the player’s career or when he has no return to soccer expectations and in most cases, it would be a realignment surgery and not cartilage restoration procedures. On the other hand, some centers reported on surgical treatment for most symptomatic cartilage injuries they see in soccer players, with cartilage restoration procedures.
This lack of consensus is also true for the preferred surgical procedure. Various previously published studies suggested treatment protocols for symptomatic cartilage lesions based on characteristics of the patient and the lesion.13-18 In addition, previous studies focusing on soccer players showed good results with various cartilage repair techniques.1-3 In this study the most common surgical treatment across all FMCE in the past 10 years was bone marrow stimulation/microfracture, followed by debridement. Twelve centers (80%) from around the world reported on performing bone marrow stimulation/microfracture in 1% to 80% of their surgical cartilage cases. The other cartilage restoration procedures had a more skewed distribution across centers, with osteochondral autograft transplantation reported to be utilized in 9 centers, autologous chondrocytes implantation in 6 centers, and osteochondral allograft transplantation only in 2 centers. Interestingly, for each restoration technique, there was 1 center utilizing it for most of its surgical cases (different center for each technique, Figs. 3 - 9 ). Taking into consideration the limited availability of some of the techniques in certain parts of the world, the varied distribution of surgical treatments with some centers choosing almost exclusively one technique over the others may suggest a selective and biased treatment approach that is based on availability, local experience, and a preference to use familiar, reproducible, and reliable techniques in the hands of the surgeons and their staff.
Figure 4.
Distribution of rates of surgical treatment with bone marrow stimulation/microfracture across responding FMCE.
Figure 5.
Distribution of rates of surgical treatment with debridement across responding FMCE.
Figure 6.
Distribution of rates of surgical treatment with open reduction internal fixation across responding FMCE.
Figure 7.
Distribution of rates of surgical treatment with an osteotomy across responding FMCE.
Figure 8.
Distribution of rates of surgical treatment with osteochondral autograft transplantation across responding FMCE.
Figure 9.
Distribution of rates of surgical treatment with osteochondral allograft transplantation across responding FMCE.
Considering the fact that bone marrow stimulation/microfracture is the oldest described and utilized surgical treatment that allows the fastest return to soccer, it is not surprising that it was the most commonly used surgical treatment in the past 10 years across all responding FMCE; however, the concept of microfracture as an isolated procedure remaining the gold standard for articular cartilage repair is being challenged these days. This is based on growing body of literature that demonstrates less predictable long-term clinical outcomes mostly attributed to the problematic durability of fibrocartilage tissue.19,20A recent systematic review and meta-analysis, 21 which included only randomized controlled trials, 21 has shown inferior quality repair tissue, higher failure rates and lower return to activity rates for microfracture treatment when compared with cartilage repair technique such as osteochondral autograft transplantation and autologous chondrocytes implantation. Another meta-analysis 11 focusing on return to sport in the athletic population also found the lowest return to sport rates with microfracture treatment when compared with cartilage repair techniques. It remains to be seen if cartilage repair/restoration procedures 22 or an augmented microfracture procedure with biological adjuvants 19 will gradually replace the use of an isolated microfracture procedure and specifically in high-demand athletes, such as soccer players. At least 3 of the FMCE have already done so.
Looking at published protocols for the treatment of symptomatic cartilage lesions,13-18 it is clear that alignment of the limb plays an important role and should dictate the preferred management. It is well established that significant malalignment should be addressed in the treatment plan with either a realignment procedure as the primary procedure or as a secondary concomitant procedure in order to unload the effected compartment, when a cartilage restoration procedure is performed. While association between soccer players and genu varum has been previously suggested23,24 and is the clinical experience of many physicians and surgeons treating soccer players, 24 the low rates of coronal osteotomies across FMCE ( Table 4 , Fig. 7 ) can be explained by the fact it is still accepted that return to high-impact and strenuous activity like soccer, especially in the competitive and professional levels, is not a reasonable expectation after an osteotomy. Nevertheless, recent literature does report on high rates of return to low- and intermediate-impact sports after a realignment osteotomy.25-27 This emphasizes the unique management of soccer players injuries, owing to this sport-specific characteristics and demands.
Bekkers et al. 5 proposed a treatment protocol for symptomatic focal cartilage lesions in soccer players in 2012, based on critical evaluation of the available literature. The authors emphasized the lack of good-quality evidence on this topic and the need for better quality research including randomized controlled trials. A recently published meta-analysis 21 of randomized controlled trials on surgical techniques for cartilage repair reports on 5 such studies28-32 published after 2012, which include very limited number of surgical treatments with no study focusing on athletes in general or soccer players specifically. This lack of high-quality evidence combined with the differences in treatment approaches across FMCE found in this study stresses the need to form collaborative international initiatives focusing on developing consensus guidelines for the treatment of symptomatic cartilage injuries in soccer players. Part of this work should include mapping of knowledge gaps 33 in the evidence-based literature in this field and design new studies aiming to bridge these gaps and provide high quality evidence that can support an established treatment protocol.
When considering return to sport after surgery, a median rate of 75% return to soccer at a median time of 28 weeks was found across all responding FMCE and including all surgical procedures. This rate of return to sport is very similar to the 76% return-to-sport rate reported in a recent meta-analysis 11 evaluating return to sport after the surgical management of articular cartilage lesions in the knee; however, the mean time to return to sport in this meta-analysis was 36 weeks, which is a longer period of time. This meta-analysis also found the highest return-to-sport rate (93%) and quickest (20 weeks) return to sport was after osteochondral autograft transplantation, when comparing between surgical treatments. Our study’s results cannot provide any treatment-specific return-to-soccer data.
This study has some limitations. First, only 15 out of 49 FMCE participated in this study and responded to the questionnaire. We believe this is a result of many centers either not treating cartilage injuries routinely and/or centers not being able to provide with reliable data that is based on their real clinical experience. Second, FMCE responses represent their unique player’s population, injuries characteristics, surgical indications, and personal/institutional experience and preferences, all are inherently variable across centers. While the aim of this study was only to report on current demographics and preferred management across FMCE, this major limitation was taken to consideration when reporting the results. Third, since this is a questionnaire-based study, results can only be based on responses to the questions asked and verification of the data provided by centers cannot be conducted. Nonetheless, centers were reached out during the data processing phase in order to confirm their response, whenever there was a need. Fourth, this study did not include data on cartilage lesions grade, concomitant surgical procedures, and previous surgical procedures in the involved knee, as these data were not available. Fifth, this study only investigated known and commonly utilized techniques and procedures for cartilage restoration in the past 10 years and did not include emerging technologies/techniques. Sixth, considering the heterogeneity of data and its sources, all the statistical analysis in this study was center (FMCE) based, rather than player based.
In conclusion, this study provides an essential and first of its kind overview of the demographics and current trends and tendencies in the management of soccer players with symptomatic cartilage injuries, based on the experience of FMCE from around the world. This study’s findings highlight some significant differences in approaches and emphasize the need for collaborative efforts aiming to bridge the gap in knowledge and solve ongoing controversies in the management of these challenging injuries in soccer players. The data shown can guide future research focusing on one hand on prevention and on the other hand on developing well-accepted guidelines for the management and treatment of symptomatic cartilage lesions in soccer players, leading to optimal outcomes.
Supplemental Material
Supplemental material, sj-pdf-1-car-10.1177_19476035211018857 for Differences in the Demographics and Preferred Management of Knee Cartilage Injuries in Soccer Players Across FIFA Centers of Excellence by Niv Marom, Tyler Warner and Riley J. Williams in CARTILAGE
Footnotes
Acknowledgments and Funding: The authors wish to thank all participating FMCE in Bangkok, Cape Town, Durham, Innsbruck, Istanbul, Kobe, Liège, Lyon, Madrid, Munich, Pachuca, Stockholm, Tokyo, and Zapopan. The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the FIFA Medical Department.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: NM and TA have no disclosures. RJW receives royalties from Arthrex, receives research support from Histogenic Inc., and is a consultant for JRF Ortho.
Ethical Approval: The study was approved by our institutional review board and the FIFA Medical Committee.
Informed Consent: Not applicable.
Trial Registration: Not applicable.
ORCID iD: Niv Marom  https://orcid.org/0000-0001-5393-6134
https://orcid.org/0000-0001-5393-6134
Supplementary material for this article is available on the Cartilage website at http://cart.sagepub.com/supplemental.
References
- 1. Mandelbaum B, Mithoefer K, Peterson L, Saris D, Dvorak J. Cartilage issues in football (soccer): an executive summary of the Federation Internationale de Football Association (FIFA)/International Cartilage Repair Society (ICRS) initiative. Cartilage. 2012;3(1 Suppl):6S-10S. doi: 10.1177/1947603511428132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mithoefer K, Peterson L, Zenobi-Wong M, Mandelbaum BR. Cartilage issues in football-today’s problems and tomorrow’s solutions. Br J Sports Med. 2015;49(9):590-6. doi: 10.1136/bjsports-2015-094772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bezuglov EN, Lyubushkina AV, Khaitin VY, Tokareva AV, Goncharov EN, Gorinov AV, et al. Prevalence of asymptomatic intra-articular changes of the knee in adult professional soccer players. Orthop J Sports Med. 2019;7(11):2325967119885370. doi: 10.1177/2325967119885370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Everhart JS, Boggs Z, DiBartola AC, Wright B, Flanigan DC. Knee cartilage defect characteristics vary among symptomatic recreational and competitive scholastic athletes eligible for cartilage restoration surgery. Cartilage. 2021;12(2):146-54. doi: 10.1177/1947603519833144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bekkers JE, de Windt TS, Brittberg M, Saris DB. Cartilage repair in football (soccer) athletes: What evidence leads to which treatment? A critical review of the literature. Cartilage. 2012;3(1 Suppl):43S-9S. doi: 10.1177/1947603511416973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dvorak J. Osteoarthritis in football: FIFA/F-MARC approach. Br J Sports Med. 2011;45(8):673-6. doi: 10.1136/bjsm.2011.083584 [DOI] [PubMed] [Google Scholar]
- 7. Kirkendall DT, Garrett WE., Jr. Management of the retired athlete with osteoarthritis of the knee. Cartilage. 2012;3(1 Suppl):69S-76S. doi: 10.1177/1947603511408287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McAdams TR, Mithoefer K, Scopp JM, Mandelbaum BR. Articular cartilage injury in athletes. Cartilage. 2010;1(3):165-79. doi: 10.1177/1947603509360210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andrade R, Vasta S, Papalia R, Pereira H, Oliveira JM, Reis RL, et al. Prevalence of articular cartilage lesions and surgical clinical outcomes in football (soccer) players’ knees: a systematic review. Arthroscopy. 2016;32(7):1466-77. doi: 10.1016/j.arthro.2016.01.055 [DOI] [PubMed] [Google Scholar]
- 10. Briggs DT, Sadr KN, Pulido PA, Bugbee WD. The use of osteochondral allograft transplantation for primary treatment of cartilage lesions in the knee. Cartilage. 2015;6(4):203-7. doi: 10.1177/1947603515595072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Krych AJ, Pareek A, King AH, Johnson NR, Stuart MJ, Williams RJ, 3rd. Return to sport after the surgical management of articular cartilage lesions in the knee: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3186-96. doi: 10.1007/s00167-016-4262-3 [DOI] [PubMed] [Google Scholar]
- 12. Panics G, Hangody LR, Balo E, Vasarhelyi G, Gal T, Hangody L. Osteochondral autograft and mosaicplasty in the football (soccer) athlete. Cartilage. 2012;3(1 Suppl):25S-30S. doi: 10.1177/1947603511408286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Camp CL, Stuart MJ, Krych AJ. Current concepts of articular cartilage restoration techniques in the knee. Sports Health. 2014;6(3):265-73. doi: 10.1177/1941738113508917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cole BJ, Pascual-Garrido C, Grumet RC. Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am. 2009;91(7):1778-90. [PubMed] [Google Scholar]
- 15. Krych AJ, Gobbi A, Lattermann C, Nakamura N. Articular cartilage solutions for the knee: Present challenges and future direction. J Isakos. 2016;1(2):93-104. doi: 10.1136/jisakos-2015-000037 [DOI] [Google Scholar]
- 16. Richter DL, Schenck RC, Jr, Wascher DC, Treme G. Knee articular cartilage repair and restoration techniques: a review of the literature. Sports Health. 2016;8(2):153-60. doi: 10.1177/1941738115611350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gomoll AH, Farr J, Gillogly SD, Kercher J, Minas T. Surgical management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92(14):2470-90. [PubMed] [Google Scholar]
- 18. Hinckel BB, Thomas D, Vellios EE, Hancock KJ, Calcei JG, Sherman SL, et al. Algorithm for treatment of focal cartilage defects of the knee: classic and new procedures. Cartilage. Epub 2021 March 20. doi: 10.1177/1947603521993219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Arshi A, Fabricant PD, Go DE, Williams RJ, McAllister DR, Jones KJ. Can biologic augmentation improve clinical outcomes following microfracture for symptomatic cartilage defects of the knee? A systematic review. Cartilage. 2018;9(2):146-55. doi: 10.1177/1947603517746722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Erggelet C, Vavken P. Microfracture for the treatment of cartilage defects in the knee joint—a golden standard? J Clin Orthop Trauma. 2016;7(3):145-52. doi: 10.1016/j.jcot.2016.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zamborsky R, Danisovic L. Surgical techniques for knee cartilage repair: an updated large-scale systematic review and network meta-analysis of randomized controlled trials. Arthroscopy. 2020;36(3):845-58. [DOI] [PubMed] [Google Scholar]
- 22. Gowd AK, Cvetanovich GL, Liu JN, Christian DR, Cabarcas BC, Redondo ML, et al. Management of chondral lesions of the knee: analysis of trends and short-term complications using the national surgical quality improvement program database. Arthroscopy. 2019;35(1_suppl):138-46. [DOI] [PubMed] [Google Scholar]
- 23. Chantraine A. Knee joint in soccer players: osteoarthritis and axis deviation. Med Sci Sports Exerc. 1985;17(4):434-9. doi: 10.1249/00005768-198508000-00005 [DOI] [PubMed] [Google Scholar]
- 24. Witvrouw E, Danneels L, Thijs Y, Cambier D, Bellemans J. Does soccer participation lead to genu varum? Knee Surg Sports Traumatol Arthrosc. 2009;17(4):422-7. doi: 10.1007/s00167-008-0710-z [DOI] [PubMed] [Google Scholar]
- 25. Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E. Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc. 2013;21(1_suppl):64-73. doi: 10.1007/s00167-011-1461-9 [DOI] [PubMed] [Google Scholar]
- 26. Hoorntje A, Kuijer PPFM, van Ginneken BT, Koenraadt KLM, van Geenen RCI, Kerkhoffs GMMJ, et al. Prognostic factors for return to sport after high tibial osteotomy: a directed acyclic graph approach. Am J Sports Med. 2019;47(8):1854-62. doi: 10.1177/0363546519849476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kunze KN, Beletsky A, Hannon CP, LaPrade RF, Yanke AB, Cole BJ, et al. Return to work and sport after proximal tibial osteotomy and the effects of opening versus closing wedge techniques on adverse outcomes: a systematic review and meta-analysis. Am J Sports Med. 2020;48(9):2295-304. doi: 10.1177/0363546519881638 [DOI] [PubMed] [Google Scholar]
- 28. Stanish WD, McCormack R, Forriol F, et al. Novel scaffold-based BST-CarGel treatment results in superior cartilage repair compared with microfracture in a randomized controlled trial. J Bone Joint Surg Am. 2013;95(18):1640-50. doi: 10.2106/JBJS.L.01345 [DOI] [PubMed] [Google Scholar]
- 29. Volz M, Schaumburger J, Frick H, Grifka J, Anders S. A randomized controlled trial demonstrating sustained benefit of autologous matrix-induced chondrogenesis over microfracture at five years. Int Orthop. 2017;41(4):797-804. doi: 10.1007/s00264-016-3391-0 [DOI] [PubMed] [Google Scholar]
- 30. Shive MS, Stanish WD, McCormack R, Forriol F, Mohtadi N, Pelet S, et al. BST-CarGel® treatment maintains cartilage repair superiority over microfracture at 5 years in a multicenter randomized controlled trial. Cartilage. 2015;6(2):62-72. doi: 10.1177/1947603514562064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Knutsen G, Drogset JO, Engebretsen L, Grøntvedt T, Ludvigsen TC, Løken S, et al. A randomized multicenter trial comparing autologous chondrocyte implantation with microfracture: long-term follow-up at 14 to 15 years. J Bone Joint Surg Am. 2016;98(16):1332-9. doi: 10.2106/JBJS.15.01208 [DOI] [PubMed] [Google Scholar]
- 32. Brittberg M, Recker D, Ilgenfritz J, Saris DBF; SUMMIT Extension Study Group. Matrix-applied characterized autologous cultured chondrocytes versus microfracture: five-year follow-up of a prospective randomized trial. Am J Sports Med. 2018;46(6):1343-51. doi: 10.1177/0363546518756976 [DOI] [PubMed] [Google Scholar]
- 33. Cole BJ, Redondo ML, Cotter EJ. Articular cartilage injuries of the knee: patient health literacy, expectations for management, and clinical outcomes. Cartilage. 2021;12(2):139-45. doi: 10.1177/1947603518816429 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-car-10.1177_19476035211018857 for Differences in the Demographics and Preferred Management of Knee Cartilage Injuries in Soccer Players Across FIFA Centers of Excellence by Niv Marom, Tyler Warner and Riley J. Williams in CARTILAGE