Abstract
Background and Objectives
Nursing homes (NHs) care for 70% of Americans dying with dementia. Many consider deaths in NHs rather than hospitals as preferable for most of these residents. NH characteristics such as staff teamwork, communication, and other components of patient safety culture (PSC), together with state minimum NH nurse staffing requirements, may influence location of death. We examined associations between these variables and place of death (NH/hospital) among residents with dementia.
Research Design and Methods
Cross-sectional study of 11,957 long-stay NH residents with dementia, age 65+, who died in NHs or hospitals shortly following discharge from one of 800 U.S. NHs in 2017. Multivariable logistic regression systematically estimated effects of PSC on odds of in-hospital death among residents with dementia, controlling for resident, NH, county, and state characteristics. Logistic regressions also determined moderating effects of state minimum NH nurse staffing requirements on relationships between key PSC domains and location of death.
Results
Residents with dementia in NHs with higher PSC scores in communication openness had lower odds of in-hospital death. This effect was stronger in NHs located in states with higher minimum NH nurse staffing requirements.
Discussion and Implications
Promoting communication openness in NHs across nursing disciplines may help avoid unnecessary hospitalization at the end of life, and merits particular attention as NHs address nursing staff mix while adhering to state staffing requirements. Future research to better understand unintended consequences of staffing requirements is needed to improve end-of-life care in NHs.
Keywords: Communication, End-of-life care, State nursing home nurse staffing requirements
Background and Objectives
Nursing homes (NHs) are final care settings for 70% of Americans dying with dementia (Li et al., 2013). While components of “good deaths” are debatable, that the majority of persons with dementia die in NHs emphasizes the necessity of ensuring NHs address the complex needs of this population (Flory et al., 2004).
Place of death is an important marker of end-of-life (EOL) care quality to patients, families, and NHs caring for residents with dementia (Mitchell et al., 2005). The NH is “home” for NH residents, and most individuals prefer to die at home (Institute of Medicine, 1997). Many dying residents with dementia experience burdensome hospitalizations and aggressive treatments (Gozalo et al., 2011), although comfort is often the main care goal at the EOL (Institute of Medicine, 1997).
Improving the quality of NH care by promoting patient safety and patient safety culture (PSC) is gaining attention from consumers, NHs, and policy makers alike (Brauner et al., 2018). PSC is a subdomain of care quality (Brauner et al., 2018) and emphasizes the importance of organizational context, focusing on system-level modifiable care processes such as how well people work together (i.e., teamwork), how well information about patients is passed from one shift to another (i.e., handoffs), or the extent that staff are able to voice opinions, suggestions, and problems in the NH and how often ideas are valued (i.e., communication openness). Therefore, PSC may improve EOL practice patterns and outcomes (Sorra et al., 2018; Stone et al., 2005; Temkin-Greener et al., 2016). The Agency for Health Care Research and Quality (AHRQ) developed a Survey on PSC for NHs (Agency for Healthcare Research and Quality, 2012) consisting of a number of domains including management support for resident safety (i.e., management actively engages with staff to promote resident safety), organizational learning (i.e., informed changes are made to improve resident safety), and compliance with procedures (i.e., staff follow procedures to keep residents safe), among others. NH staff generally perceive PSC to be inadequate (Bonner et al., 2008; Castle et al., 2010), which is unfortunate because better NH PSC is associated with fewer resident falls and pressure ulcers, less restraint use, broad safety and quality of care, and reduced staff turnover (Banaszak-Holl et al., 2017; Castle et al., 2010; Li et al., 2019; Temkin-Greener et al., 2020; Thomas et al., 2012).
Studies have indirectly examined aspects of PSC in relation to EOL care and residents with dementia. One Canadian study examined organizational context (i.e., leadership, formal and informal team interaction) and EOL care, comparing symptom burden among dying NH residents with and without dementia; it found that resident behavioral expressions and delirium were more prevalent in facilities with better team leadership and interactions, while pain, dyspnea, and urinary tract infections were lower (Estabrooks et al., 2015). Focusing on EOL care in U.S. NHs, one study found significant associations between better certified nurse assistant (CNA) staff communication and better EOL care processes (e.g., EOL assessment, care delivery) (Zheng & Temkin-Greener, 2010), but not specifically for residents with dementia. Overall, little is known whether PSC in general and/or certain domains are associated with where residents with dementia die. Given that some consider location of death a key indicator of EOL care quality (Li et al., 2013), such information is particularly useful to guide practice and policy.
Implementing a culture of PSC in NHs depends on organizational structure and staffing arrangements, which may vary by state requirements. For example, minimum nurse staffing requirements prompt NHs to alter staffing arrangements to meet requirements within budget constraints. As licensed staff earn roughly twice the hourly wage as CNAs, studies have documented substitution effects in NHs in states with higher staffing requirements (e.g., fewer registered nurses [RNs] and ancillary staff, more CNAs), with variation depending on NH Medicaid payments and local competition for NH beds (Bowblis, 2011; Bowblis & Hyer, 2013; Chen & Grabowski, 2015). However, increased Medicaid reimbursement is not consistently associated with optimal staffing ratios (Bowblis & Applebaum, 2017; Feng et al., 2008). Improved NH quality (e.g., reductions in deficiency citations, contractures, potentially avoidable hospitalizations, pressure ulcers) was found in NHs with higher staffing requirements, but only up to certain thresholds (Centers for Medicare and Medicaid Services, 2001; Chen & Grabowski, 2015). Additionally, impacts of minimum nurse staffing requirements on outcomes are stronger in nonprofit and low-staff facilities (Park & Stearns, 2009). Collectively, minimum NH nurse staffing requirements are important to care quality (Castle et al., 2011), as higher-staffed NHs provide better care (Harrington et al., 2016; Schnelle et al., 2004).
While NH PSC and staffing requirements appear to influence NH quality of care overall, how these may work together and whether EOL care specifically for residents with dementia is impacted remains unclear. To fill these knowledge gaps, our objectives were to (a) examine associations between PSC domains and place of death among residents with dementia and (b) evaluate the extent to which state minimum NH nurse staffing requirements moderate these effects. If such associations exist, NH and state-level policy initiatives can be guided to target meaningful interventions for improving EOL care among residents with dementia.
Conceptual Framework
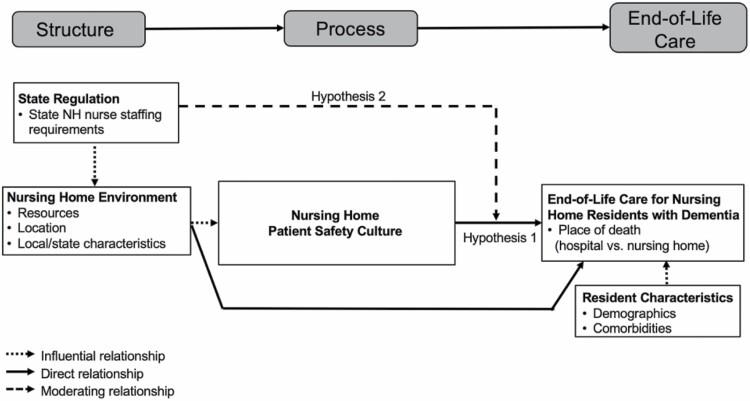
We adopted Donabedian’s commonly used Structure, Process, Outcome model to assess care quality (Donabedian, 1988), which was previously used to examine associations between NH PSC and safe resident care (Thomas et al., 2012). The model (Figure 1) suggests that NH environments are likely directly related to EOL care for residents with dementia. Previous studies have examined elements of NH environments such as ownership, location, resident composition, and state-level NH policies and found associations with NH care quality (Grabowski et al., 2010; Gruneir et al., 2007; Joyce et al., 2018; Konetzka et al., 2008; Miller et al., 2011; Mitchell et al., 2003; Schnelle et al., 2004; Temkin-Greener et al., 2009; Xing et al., 2013; Zimmerman et al., 2002). These same NH characteristics and state regulations may also influence care processes measured by PSC (e.g., teamwork, training and skills, nonpunitive response to mistakes, handoffs), which are hypothesized to directly affect EOL care for residents with dementia, after accounting for influences of resident characteristics (e.g., demographics, comorbidities, functional status).
Figure 1.
Conceptual model. Expected relationships between measures of nursing home structure, process, and end-of-life care for residents with dementia.
Furthermore, state regulations such as minimum NH nurse staffing requirements are associated with NH care quality and may moderate associations between PSC and EOL care. Depending on the stringency of these requirements, NHs may alter staffing arrangements, likely influencing PSC and perhaps affecting EOL care. For example, prior research has shown that perceptions of compliance with procedures, nonpunitive response to mistakes, and handoffs were higher in NHs with lower RN turnover, while perceptions of staffing and training and skills were higher in NHs with lower CNA turnover (Temkin-Greener et al., 2020). That PSC is differentially related to the mix of NH nursing staff is important, but how staffing requirements may work together with PSC to affect EOL care remains unclear.
Because a priori it is unclear if overall PSC or select domains are related to EOL care for residents with dementia, we assessed each domain independently, in addition to the overall score, examining the following hypotheses: (a) In NHs with better PSC (higher scores), residents with dementia are more likely to die in NHs (compared to hospitals), controlling for resident, NH, county, and state characteristics; (b) The relationship between PSC and place of death among residents with dementia will be stronger in NHs located in states with higher minimum NH nurse staffing requirements, controlling for resident, NH, county, and state characteristics.
Research Design and Methods
Data Sources and Sample
We used 2017 survey data based on a national random sample of NH administrators, directors of nursing, and unit leaders completing AHRQ’s Survey on PSC for NHs; the response rate was 37% (Li et al., 2019; Temkin-Greener et al., 2020). NHs in 46 states and the District of Columbia participated in the survey (excluding 18 [0.12%] NHs in Alaska, 80 [0.51%] NHs in Idaho, 36 [0.23%] NHs in Vermont, and 38 [0.24%] NHs in Wyoming where no survey was returned). The average number of NHs participating in the survey per state was 17 (SD = 14.3), ranging from 1 to 60; the average number of decedents with dementia per NH was 14.9 (SD = 10.6), ranging from a minimum of 1 to a maximum of 84.
Responding NHs were merged with 2016–2017 national data from the Centers for Medicare & Medicaid (CMS) Medicare Provider Analysis and Review File (ResDAC, 2016c), Master Beneficiary Summary File (MBSF) (ResDAC, 2016b), and Minimum Data Set (MDS) (ResDAC, 2016a). NH-, county-, and state-level covariates were obtained from CMS’ NH Compare File (Centers for Medicare and Medicaid Services, 2018), LTCfocus (Brown School of Public Health, 2018), Area Health Resources File (Health Resources & Services Administration, 2018), MACPAC (Medicaid and CHIP Payment Access Commission, 2019), state NH Medicaid pay rates for 2016 (American Health Care Association, 2016), and state NH staffing requirements for 2017 (Harrington, 2010). NH Medicaid pay rates and state NH staffing requirements were obtained using previous approaches (e.g., review of state statutes, regulations, and state websites) (Bowblis, 2011).
Quarterly and annual MDS assessments in 2017 were used to identify long-stay residents. Dementia diagnosis was determined using residents’ last assessment before death, specifically, items for Alzheimer’s Disease or Dementia and ICD-10 diagnosis codes for dementia (F00/dementia in Alzheimer disease; F01/vascular dementia; F02/dementia in other diseases; F03/unspecified dementia; and G30/Alzheimer dementia).
Residents were included in analyses if they had dementia, were at least 65 years old upon death (determined by validated death dates in the MBSF), not comatose, died in NHs or hospitals within 8 days post-NH discharge, and resided in survey responding NHs. Decedent residents with dementia from 16 NHs could not be matched with the sample and 2 NHs did not have decedents with dementia. After these exclusions, the analytical sample included 11,957 decedents with dementia from 800 NHs.
This study protocol was reviewed and approved by University of Rochester’s institutional review board.
Variables
Outcome
We used MDS discharge assessments to determine whether residents died in NHs or were discharged to hospitals and died there within 8 days. An 8-day cutoff captured more than 85% of in-hospital deaths among our sample and avoids inclusion of long hospitalizations potentially outside the control of NHs. This time frame was also used by others (Mukamel et al., 2012).
Patient safety culture
Our key independent variables were derived from the PSC survey, which has been verified for psychometric validity and internal consistency and used previously (Li et al., 2019; Temkin-Greener et al., 2020). The survey included 42 questions covering 12 domains: teamwork, staffing, compliance with procedures, training and skills, nonpunitive response to mistakes, handoffs, feedback and communication about incidents, communication openness, supervisor expectations and actions promoting resident safety, overall perceptions of resident safety, management support for resident safety, and organizational learning. Responses to each item were based on 5-point Likert scales ranging from 1 (strongly disagree) to 5 (strongly agree). We followed the conventional approach to operationalize each domain by calculating the percent positive responses and averaging across responders in each NH. Scores ranged from 0 to 100, with higher scores representing better NH PSC, and were expressed in terms of 10-percentage point increases (i.e., percentage point × 10) in analyses for ease of interpretation.
State minimum NH nurse staffing requirements
We combined state NH requirements for licensed staff and CNAs, obtaining requirements for total staffing, and expressed in terms of hours per resident day (HPRD).
Other covariates
We included resident sociodemographics, behavior and functioning, and medical information commonly used as risk adjusters for place of death (Mukamel et al., 2012, 2016). Sociodemographic characteristics included age, race (White/non-White), dual eligibility for Medicare/Medicaid, enrollment in Medicare advantage plans in the month of death, marital status (married/not married), and gender. Residents with dementia were classified into three levels of cognitive impairment using the Cognitive Function Scale (CFS): intact/mild (CFS = 0–1), moderate (CFS = 2), and severe (CFS = 3) (Thomas et al., 2017). Impairments in activities of daily living (ADL) determined functional status based on a scale of 0–28; higher scores indicate greater impairment (Morris et al., 1999). Moderate/severe aggressive behavior was determined using the Aggressive Behavior Scale (score of 3–12 vs none/mild [0–2]) (Perlman & Hirdes, 2008). Medical information was captured through number of diagnoses and presence/absence of conditions related to heart/circulation; musculoskeletal; diabetes; chronic obstructive pulmonary disease; depression; anxiety; stroke; pneumonia; pressure ulcer in the last 90 days of life; urinary and bowl incontinence; urinary tract infection; swallowing problem; feeding tube; indwelling catheter; oxygen therapy; and use of pain and antipsychotic, antianxiety, and antidepressant medications.
Factors at NH, county, and state levels were based on prior studies identifying associations with NH care quality (Bowblis, 2011; Cai et al., 2018; Chen & Grabowski, 2015; Grabowski et al., 2010; Gruneir et al., 2007; Joyce et al., 2018; Konetzka et al., 2008; Miller et al., 2011; Schnelle et al., 2004; Temkin-Greener et al., 2009; Walsh et al., 2010; Xing et al., 2013; Zimmerman et al., 2002). NH-level factors included volume of NH hospice days in the last 90 days of life, prevalence of NH-level dementia, proportion of NH potentially avoidable hospitalization in the last 90 days of life, ownership (for-profit vs government-owned/nonprofit), chain affiliation, total staffing HPRD (sum of RNs, licensed practical nurses, and CNAs), RN/total staffing HPRD, occupancy rate, number of beds, presence of Alzheimer’s unit, and percent Medicare and Medicaid residents.
County-level characteristics included number of hospice providers in the county, number of hospital beds per 1,000 persons 65+, whether NHs were located in urban (vs rural) counties, and competition for NH beds measured by the Herfindahl–Hirschman Index (0–1; higher values = greater competition). At the state level, we included payment type for NH Medicaid reimbursement (cost-based, hybrid, price-based), NH Medicaid payment rates, and presence/absence of bed-hold policy and monetary adjustment for behavioral problems or mental health/cognitive impairment.
Statistical Analyses
We first examined associations between independent variables and place of death using chi-squared tests and analyses of variance. We then used multivariable logistic regression to systematically estimate associations of each PSC domain and overall score on odds of in-hospital death among residents with dementia, controlling for resident, NH, county, and state characteristics, and with NH random effects to account for clustering of residents within NHs. We used a series of models, beginning with unadjusted models and sequentially adding resident, NH, county, and state covariate groupings; Wald tests determined the significance of additional groupings. Further logistic regressions were employed using fully adjusted models to determine influences of interactions between key domains and state minimum NH nurse staffing requirements on likelihoods of in-hospital death.
Analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC) and STATA version 12.1 (StataCorp, LLC, College Station, TX).
Results
Sample Characteristics
Among our sample, 9.1% died in hospital. Most associations across residents with dementia dying in hospital vs NHs were significant. Residents with dementia who died in hospital were less likely to be severely cognitively impaired (18.6% vs 31.9%), female (61.5% vs 69.4%), and White (73.7% vs 86.8%) compared to residents dying in NHs (Table 1). These decedents were also less functionally impaired (ADL score 19.6 vs 21.3) and less likely to have had cancer (5.5% vs 8.0%), among other significant differences.
Table 1.
Descriptive Characteristics of NH Decedents With Dementia Who Died in 2017 in the NH or Hospital From One of 800 NHs Responding to the NH Patient Safety Culture Survey (N = 11,957)
| Variable | In-hospital death, N = 1,092 | NH death, N = 10,865 |
p-valuea (χ 2 or ANOVA) |
|---|---|---|---|
| Mean ± SD or % | Mean ± SD or % | ||
| Patient safety culture (% positive) | |||
| Overall (domains 1–12) | 80.1 ± 17.2 | 82.0 ± 13.8 | .009 |
| Domain | |||
| 1: Teamwork | 85.6 ± 24.0 | 86.4 ± 22.6 | .269 |
| 2: Staffing | 64.0 ± 29.6 | 64.9 ± 27.9 | .319 |
| 3: Compliance with procedures | 64.6 ± 27.0 | 64.1 ± 25.2 | .599 |
| 4: Training and skills | 75.7 ± 29.0 | 75.3 ± 27.6 | .634 |
| 5: Nonpunitive response to mistakes | 71.2 ± 25.8 | 73.8 ± 24.4 | .001 |
| 6: Handoffs | 69.6 ± 28.5 | 70.8 ± 26.8 | .156 |
| 7: Feedback and communication about incidents | 95.7 ± 14.9 | 96.7 ± 11.7 | .013 |
| 8: Communication openness | 85.3 ± 24.9 | 88.0 ± 20.2 | <.001 |
| 9: Supervisor expectations and actions promoting resident safety | 91.2 ± 20.9 | 92.4 ± 18.5 | .037 |
| 10: Overall perceptions of resident safety | 94.2 ± 19.3 | 96.0 ± 13.8 | <.001 |
| 11: Management support for resident safety | 90.7 ± 20.9 | 92.2 ± 17.0 | .005 |
| 12: Organizational learning | 82.8 ± 23.3 | 84.0 ± 20.5 | .067 |
| State minimum total nurse staffing level (hours per resident day) | 2.15 ± 1.42 | 2.13 ± 1.39 | .605 |
| Resident-level covariates | |||
| Sociodemographic characteristics | |||
| Age | 85.2±7.6 | 87.5±7.8 | <.001 |
| Female | 61.5% | 69.4% | <.001 |
| White | 73.7% | 86.8% | <.001 |
| Married | 23.2% | 21.8% | .206 |
| Medicare advantage plan | 21.9% | 26.7% | .001 |
| Dually eligible for Medicare/Medicaid | 82.8% | 76.3% | <.001 |
| Behavior and functioning characteristics | |||
| Moderate/severe aggressive behavior | 6.0% | 7.5% | .113 |
| Cognitive Function Scale: | <.001 | ||
| Mild | 33.6% | 18.5% | |
| Moderate | 47.6% | 49.4% | |
| Severe | 18.6% | 31.9% | |
| Anxiety | 31.0% | 36.4% | <.001 |
| Depression | 43.1% | 47.5% | .006 |
| Activities of daily living score | 19.6 ± 5.7 | 21.3 ± 4.3 | <.001 |
| Number of diagnoses | 6.0 ± 3.6 | 5.8 ± 3.5 | .133 |
| Medical information | |||
| Pneumonia | 4.3% | 4.6% | .634 |
| Diabetes mellitus | 37.6% | 30.1% | <.001 |
| Heart/circulation | 94.2% | 92.0% | .008 |
| Musculoskeletal | 39.6% | 43.1% | .026 |
| Cancer | 5.5% | 8.0% | .003 |
| Stroke | 8.5% | 9.2% | .464 |
| Chronic obstructive pulmonary disease | 31.0% | 24.6% | <.001 |
| Urinary tract infection | 5.8% | 5.1% | .326 |
| Urinary incontinent | 78.1% | 86.1% | <.001 |
| Bowel incontinent | 75.7% | 85.3% | <.001 |
| Swallowing problem | 3.2% | 7.7% | <.001 |
| Feeding tube | 9.6% | 3.9% | <.001 |
| Oxygen therapy | 16.6% | 19.2% | .038 |
| Indwelling catheter | 8.4% | 8.6% | .888 |
| Pain medication | 54.7% | 63.3% | <.001 |
| Antipsychotic, antianxiety, antidepressant medication | 64.5% | 66.1% | .278 |
| Pressure ulcer in last 90 days of life | 11.7% | 11.5% | .852 |
| NH-level covariates | |||
| For-profit | 72.9% | 61.1% | <.001 |
| Chain membership | 49.7% | 51.2% | .412 |
| Total staffing hours per day | 3.8 ± 0.6 | 3.8 ± 0.6 | .026 |
| Registered nurse/total staffing hours per day | 0.2 ± 0.1 | 0.2 ± 0.1 | <.001 |
| Number of beds | 146.4 ± 80.7 | 138.9 ± 70.4 | .001 |
| Occupancy rate | 84.2 ± 11.9 | 84.2 ± 12.3 | .898 |
| % Medicare residents | 14.2 ± 10.5 | 13.4 ± 10.1 | .016 |
| % Medicaid residents | 62.1 ± 18.9 | 59.6 ± 18.9 | <.001 |
| Alzheimer’s unit | 21.6% | 28.9% | <.001 |
| Proportion of NH dementia | 73.0 ± 13.2 | 72.8 ± 12.9 | .516 |
| Volume of NH hospice days in last 90 days of life | 5.3 ± 3.8 | 6.1 ± 4.2 | <.001 |
| Proportion of NH potentially avoidable hospitalizations in last 90 days of life | 12.3 ± 10.1 | 9.4 ± 8.1 | <.001 |
| County-level covariates | |||
| Number of hospice providers in county | 19.7 ± 80.1 | 9.0 ± 40.7 | <.001 |
| Number of hospital beds per 1,000 persons 65+ | 18.2 ± 10.8 | 18.0 ± 13.1 | .509 |
| County NH bed competition (1-Herfindahl Hirschman Index) | 0.8 ± 0.3 | 0.8 ± 0.2 | .238 |
| Urban NH | 73.0% | 73.4% | .939 |
| State-level covariates | |||
| Payment type for NH Medicaid reimbursement: | <.001 | ||
| Cost-based | 49.4% | 41.7% | |
| Hybrid | 20.6% | 29.2% | |
| Price-based | 30.0% | 29.1% | |
| Adjustment for behavioral problems, or mental health/cognitive impairment | 38.7% | 40.2% | .361 |
| Bed-hold policy | 88.4% | 87.3% | .301 |
| Medicaid pay rate | $195.12 ± $34.19 | $195.08 ± $33.86 | .974 |
Notes: NH = nursing home.
a p-values test associations between residents who died in the hospital or NH.
Residents with dementia who died in hospital were more likely to have resided in NHs that were for-profit (72.9% vs 61.1%), larger (146 vs 139 beds), and with lower prevalence of Alzheimer’s units (21.6% vs 28.9%) and higher proportions of NH-level potentially avoidable hospitalizations in the last 90 days of life (12.3% vs 9.4%). They were also more likely to have resided in states using cost-based reimbursement methods for Medicaid payments (49.4% vs 41.7%), among other differences.
Compared to residents dying in NHs, those dying in hospital more likely resided in NHs with lower PSC scores for overall score (80.1% vs 82.0%), nonpunitive response to mistakes (71.2% vs 73.8%), feedback and communication about incidents (95.7% vs 96.7%), communication openness (85.3% vs 88.0%), supervisor expectations and actions promoting resident safety (91.2% vs 92.4%), overall perceptions of resident safety (94.2% vs 96.0%), and management support for resident safety (90.7% vs 92.2%).
PSC (Hypothesis 1)
In our sample, responding NHs were more likely than NHs nationally to be nonprofit (33.0% vs 26.0%) and have higher overall five-star ratings (30.5% vs 26.4%), but there were no statistically significant differences regarding staffing, number of beds, occupancy, and state-level policies (Supplementary Table 1). The average overall PSC score among our sample was 81.9% (SD 14.1%), and average PSC domains ranged from a minimum of 64.2% (SD 25.4%) for compliance with procedures to a maximum of 96.6% (SD 12.0%) for feedback and communication about incidents (data not shown).
In unadjusted models, 10-percentage point increases in nonpunitive response to mistakes, communication openness, and overall perceptions of resident safety were associated with 4.0%–7.0% decreased odds of in-hospital death (Table 2, unadjusted model). For nonpunitive response to mistakes and overall perceptions of resident safety, these associations were attenuated and became insignificant after controlling for resident, NH, county, and state-level characteristics (Table 2, fully adjusted model; Supplementary Table 3, Models 2–5). In NHs reporting higher communication openness scores, however, decedents with dementia had 5.0% lower odds of in-hospital death across models adjusting for resident, NH, and county characteristics. (Complete model results of the fully adjusted model for communication openness are given in Supplementary Table 2.) In contrast, associations between teamwork and in-hospital death became significant when adding resident-, NH-, and county-level covariates. Across all domains, adding county- and state-level characteristics did not significantly improve model fit.
Table 2.
Multivariable Results for Patient Safety Culture Domains From Logistic Regression Models of In-Hospital Death Among NH Decedents With Dementia Who Died in 2017 in the NH or Hospital From NHs Responding to the NH Patient Safety Culture Survey
| Patient safety culture | Unadjusted modela | Fully adjusted modelb | Interaction |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | p-valuec | |
| [p-value] | [p-value] | ||
| Overall (domains 1–12) | 0.95 (0.88, 1.01) [.105] | 0.97 (0.90, 1.04) [.356] | .089 |
| Domain | |||
| 1: Teamwork | 0.99 (0.95, 1.02) [.422] | 0.97 (0.93, 1.00) [.077] | .356 |
| 2: Staffing | 0.99 (0.96, 1.02) [.493] | 0.99 (0.96, 1.03) [.730] | .615 |
| 3: Compliance with procedures | 1.01 (0.97, 1.04) [.715] | 0.99 (0.96, 1.03) [.692] | .155 |
| 4: Training and skills | 1.01 (0.97, 1.04) [.742] | 1.01 (0.98, 1.05) [.505] | .823 |
| 5: Nonpunitive response to mistakes | 0.96 (0.93, 0.99) [.011] | 0.98 (0.95, 1.02) [.377] | .160 |
| 6: Handoffs | 0.98 (0.95, 1.02) [.330] | 1.00 (0.96, 1.03) [.749] | .810 |
| 7: Feedback and communication about incidents | 0.95 (0.88, 1.01) [.113] | 0.99 (0.91, 1.08) [.867] | .913 |
| 8: Communication openness | 0.94 (0.91, 0.98) [.005] | 0.96 (0.92, 1.00) [.062] | .011 |
| 9: Supervisor expectations and actions promoting resident safety | 0.97 (0.93, 1.01) [.128] | 0.99 (0.95, 1.04) [.792] | .078 |
| 10: Overall perceptions of resident safety | 0.93 (0.88, 0.98) [.005] | 0.96 (0.89, 1.04) [.293] | .001 |
| 11: Management support for resident safety | 0.95 (0.90, 1.01) [.082] | 0.97 (0.91, 1.03) [.311] | .196 |
| 12: Organizational learning | 0.97 (0.93, 1.02) [.255] | 0.98 (0.93, 1.03) [.502] | .149 |
Notes: CI = confidence interval; NH = nursing home; OR = odds ratio.
aPatient safety culture domains are expressed in terms of 10-percentage point increases in each domain. Each patient safety culture domain was included individually in 13 separate models, and covariate groupings were sequentially added to the unadjusted models. b Models adjusted for resident, NH, county, and state characteristics. Wald p-values >.05, testing the statistical significance of additional covariate groupings from the unadjusted models. c The p-value is for the interaction term between each patient safety culture domain and state minimum NH nurse staffing requirements for the fully adjusted models.
State Minimum NH Nurse Staffing Requirements (Hypothesis 2)
In 2017, all states had requirements for licensed staff and 17 states did not have requirements for CNAs; 8 states had updated CNA requirements since 2010. The majority of NHs (82.9%) met or exceeded state staffing requirements for total staffing HPRD among our sample. The average difference between total staffing HPRD and state staffing requirements across states was 1.81, ranging from −0.71 (Illinois) to 4.14 (North Dakota).
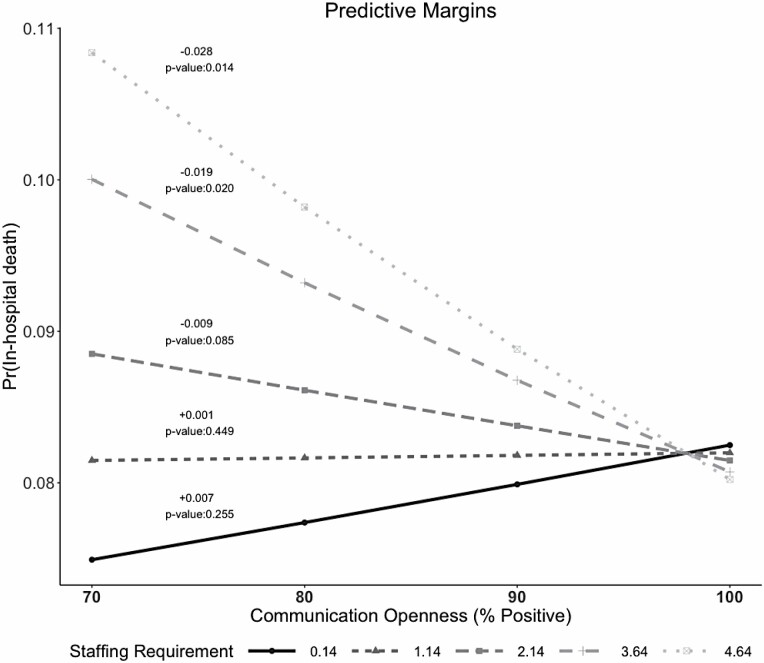
The interaction between communication openness and state minimum NH nurse staffing requirements in the fully adjusted model was significant (p-value = .011) (Table 2; Supplementary Tables 2 and 3), suggesting that such requirements moderate effects on place of death. The interaction with overall perceptions of resident safety was also significant, but not explored further as the main effect was overall insignificant across models in Hypothesis 1.
Further examining the interaction between communication openness and minimum staffing requirements in relation to the probability of in-hospital death among NH residents with dementia, Figure 2 demonstrates a stronger relationship with in-hospital death in NHs located in states with higher (above 2.14 HPRD [average]) minimum NH nurse staffing requirements. In these states, increasing communication openness from 70% to 100% (1 SD around the mean score of 87.8%) was associated with 1.9%–2.8% absolute reductions in probabilities of in-hospital death (19.3%–26.0% relative reductions).
Figure 2.
Predictive margins for the probability of in-hospital death. Differences in probabilities of in-hospital death when increasing communication openness from 70% to 100% for different levels of state staffing requirements are shown.
Discussion and Implications
This national study is the first to examine potential influences of NH PSC and state minimum NH nurse staffing requirements on place of death for residents with dementia. Findings show increased communication openness was associated with lower probability of in-hospital deaths among residents with dementia (Hypothesis 1), and state minimum NH nurse staffing requirements moderate this relationship (Hypothesis 2). Overall, these suggest that interventions promoting open communication in NHs may have potential to improve EOL care among this population. However, fostering communication openness in NHs across nursing disciplines merits particular attention especially as NHs struggle to maintain optimal mixes of nursing staff while adhering to state staffing requirements (Bowblis & Hyer, 2013; Chen & Grabowski, 2015).
The fact that communication openness emerged of importance is consistent with a 2010 study of communication among CNAs in a sample of New York NHs (Zheng & Temkin-Greener, 2010). The authors defined communication as “the degree to which communication between CNAs and their supervisors and co-workers is uninhibited, accurate, timely and effective” and found better communication was associated with better EOL care processes including EOL assessment and care delivery. The PSC survey measures communication openness based on the extent that staff are able to voice opinions, suggestions, and problems in the NH and how often ideas are valued. While the measurement of communication and samples differ between these studies, the message is similar: encouraging open communication across staff may improve NH EOL care, including for residents with dementia.
Communication among NH staff is often hierarchical (e.g., between physicians and licensed staff; between licensed staff and CNAs). In NHs located in states with higher staffing requirements, larger CNA presence is probable and communication openness across nursing disciplines may be suppressed. This finding may have important implications for EOL care. CNAs are often the first to notice changes in a resident’s health and care needs. If communication between CNAs and licensed staff is poor (e.g., CNAs do not feel their ideas and suggestions are valued), stifling their input regarding residents’ changing health status may affect the likelihood of treating residents onsite and avoiding unnecessary hospitalization. Supporting this assumption, other work has also concluded that improved communication may reduce hospitalizations (Zimmerman et al., 2016).
Null findings in our study are also important. Nonpunitive response to mistakes and overall perceptions of resident safety were significant in unadjusted models only, suggesting that resident and NH characteristics (e.g., ownership, volume of NH hospice days in the last 90 days of life, proportion of NH PAHs in the last 90 days of life) are more important predictors of in-hospital death than these PSC domains among our sample. That the addition of county- and state-level characteristics did not significantly improve model fit for communication openness emphasizes the importance of communication in improving EOL care practices among this population.
Regarding state minimum NH nurse staffing requirements, our findings support prior studies demonstrating improved resident outcomes and quality with higher requirements (Bowblis, 2011; Harrington et al., 2016; Zhang & Grabowski, 2004). However, the relationship is far from clear, given that incremental quality improvements have been found only up to identified thresholds (ranging from 0.55 to 2.8 HPRD) (Centers for Medicare and Medicaid Services, 2001) and in some cases small effects have occurred only in NHs with initially low staffing levels (Park & Stearns, 2009). Our study found a moderating effect of nurse staffing requirements regarding communication openness, with effects on reducing probabilities of in-hospital death only significant for NHs in states with higher staffing requirements.
Several limitations in our study should be noted. First, there is a concern of potential omitted variable bias, but this is somewhat diminished through inclusion of an extensive set of covariates at individual, NH, and market levels. Second, our sample is limited to residents in the 37% of NHs responding to the voluntary survey; it is not possible to know if bias affected the detected associations, and so results of this study are not suggested to be generalizable to all NHs. Third, we were unable to detect causal relationships in this cross-sectional study. Fourth, state minimum NH nurse staffing requirements are not specific to dementia or EOL care. However, based on prior studies (Bowblis & Hyer, 2013; Chen & Grabowski, 2015), we assume that nurse staffing requirements alter NH staff composition, and expect these requirements affect all types of nursing care. Finally, we were not able to account for staff turnover, which has been associated with differing perceptions of PSC (Temkin-Greener et al., 2020); however, this is not likely to affect our findings as our study focuses on relationships between PSC and place of death. Staff turnover would likely only strengthen the effect of this relationship but not alter the direction.
Our findings suggest promotion of communication openness among NH staff may reduce EOL hospitalization for residents with dementia, especially in states with higher nurse staffing requirements. The CMS NH Compare metrics, commonly used to assess NH quality, do not include measures of EOL care among residents with dementia (Mukamel et al., 2012) or direct measures of patient safety (Brauner et al., 2018) and PSC is not mandated in state regulations; our results could serve as preliminary benchmarking data for public reporting of EOL care for residents with dementia. This effort would not only inform stakeholders about NH quality of EOL care, but could also have potential to improve transparency, quality of care, and outcomes for this population (Campanella et al., 2016; Castle et al., 2007).
Just as recent growth in the NH culture change movement has been identified as especially important for patients at the EOL (Schwartz et al., 2019), our findings similarly present the importance of promoting elements of PSC, especially communication openness, when caring for dying residents with dementia. As the population of persons with dementia grows and NHs increasingly become the final care setting for this population, our study has implications for a wide audience including persons with dementia and their families, NH staff, and policy makers seeking to improve the quality of NH care persons with dementia receive at the EOL. Future research to better understand complex relationships between communication, nurse staffing requirements, and EOL care is warranted to identify possible mechanisms promoting improved EOL care among residents with dementia. Additionally, our findings suggest that communication openness and nurse staffing requirements may be relevant to EOL care for all NH residents regardless of the level of cognition, but further study is required to confirm this hypothesis.
Supplementary Material
Contributor Information
Jessica Orth, Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, New York, USA.
Yue Li, Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, New York, USA.
Adam Simning, Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, New York, USA; Department of Psychiatry, University of Rochester School of Medicine and Dentistry, New York, USA.
Sheryl Zimmerman, The Cecil G. Sheps Center for Health Services Research and The Schools of Social Work and Public Health, University of North Carolina at Chapel Hill, USA.
Helena Temkin-Greener, Department of Public Health Sciences, University of Rochester School of Medicine and Dentistry, New York, USA.
Funding
This work was supported by the Agency for Healthcare Research and Quality [grant number R01HS024923].
Conflict of Interest
None declared.
References
- Agency for Healthcare Research and Quality . (2012). Nursing home survey on patient safety culture. Retrieved from http://www.ahrq.gov/sops/surveys/nursing-home/index.html [DOI] [PubMed]
- American Health Care Association, E. L., Hansen Hunter & Company PC . (2012, December). A report on shortfalls in Medicaid funding for nursing center care. https://www.ahcancal.org/Data-and-Research/Pages/default.aspx
- Banaszak-Holl, J., Reichert, H., Todd Greene, M., Mody, L., Wald, H. L., Crnich, C., McNamara, S. E., & Meddings, J. (2017). Do safety culture scores in nursing homes depend on job role and ownership? Results from a national survey. Journal of the American Geriatrics Society, 65(10), 2244–2250. doi: 10.1111/jgs.15030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonner, A. F., Castle, N. G., Perera, S., & Handler, S. M. (2008). Patient safety culture: A review of the nursing home literature and recommendations for practice. The Annals of Long-Term Care, 16 (3), 18–22. [PMC free article] [PubMed] [Google Scholar]
- Bowblis, J. R. (2011). Staffing ratios and quality: An analysis of minimum direct care staffing requirements for nursing homes. Health Services Research, 46 (5), 1495–1516. doi: 10.1111/j.1475-6773.2011.01274.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowblis, J. R., & Applebaum, R. (2017). How does Medicaid reimbursement impact nursing home quality? The effects of small anticipatory changes. Health Services Research, 52 (5), 1729–1748. doi: 10.1111/1475-6773.12553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowblis, J. R., & Hyer, K. (2013). Nursing home staffing requirements and input substitution: Effects on housekeeping, food service, and activities staff. Health Services Research, 48 (4), 1539–1550. doi: 10.1111/1475-6773.12046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauner, D., Werner, R. M., Shippee, T. P., Cursio, J., Sharma, H., & Konetzka, R. T. (2018). Does nursing home compare reflect patient safety in nursing homes? Health Affairs (Project Hope), 37 (11), 1770–1778. doi: 10.1377/hlthaff.2018.0721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown School of Public Health . (2018). Long-term care: Facts on care in the US. http://ltcfocus.org/1/about-us
- Cai, S., Miller, S. C., & Gozalo, P. L. (2018). Nursing home-hospice collaboration and end-of-life hospitalizations among dying nursing home residents. Journal of the American Medical Directors Association, 19 (5), 439–443. doi: 10.1016/j.jamda.2017.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campanella, P., Vukovic, V., Parente, P., Sulejmani, A., Ricciardi, W., & Specchia, M. L. (2016). The impact of public reporting on clinical outcomes: A systematic review and meta-analysis. BMC Health Services Research, 16, 296. doi: 10.1186/s12913-016-1543-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle, N. G., Engberg, J., & Liu, D. (2007). Have nursing home compare quality measure scores changed over time in response to competition? Quality & Safety in Health Care, 16 (3), 185–191. doi: 10.1136/qshc.2005.016923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle, N. G., Wagner, L. M., Ferguson, J. C., & Handler, S. M. (2011). Nursing home deficiency citations for safety. Journal of Aging & Social Policy, 23 (1), 34–57. doi: 10.1080/08959420.2011.532011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castle, N. G., Wagner, L. M., Perera, S., Ferguson, J. C., & Handler, S. M. (2010). Assessing resident safety culture in nursing homes: Using the nursing home survey on resident safety. Journal of Patient Safety, 6 (2), 59–67. doi: 10.1097/PTS.0b013e3181bc05fc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services . (2001). Appropriateness of minimum nurse staffing ratios in nursing homes: Report to Congress: Phase II final volume 1. Abt Associates Inc. [Google Scholar]
- Centers for Medicare and Medicaid Services . (2018). Nursing Home Compare Data Archive: 2017 data. https://data.medicare.gov/data/archives/nursing-home-compare
- Chen, M. M., & Grabowski, D. C. (2015). Intended and unintended consequences of minimum staffing standards for nursing homes. Health Economics, 24 (7), 822–839. doi: 10.1002/hec.3063 [DOI] [PubMed] [Google Scholar]
- Donabedian, A. (1988). The quality of care. How can it be assessed? Journal of the American Medical Association, 260 (12), 1743–1748. doi: 10.1001/jama.260.12.1743 [DOI] [PubMed] [Google Scholar]
- Estabrooks, C. A., Hoben, M., Poss, J. W., Chamberlain, S. A., Thompson, G. N., Silvius, J. L., & Norton, P. G. (2015). Dying in a nursing home: Treatable symptom burden and its link to modifiable features of work context. Journal of the American Medical Directors Association, 16 (6), 515–520. 10.1016/j.jamda.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Feng, Z., Grabowski, D. C., Intrator, O., Zinn, J., & Mor, V. (2008). Medicaid payment rates, case-mix reimbursement, and nursing home staffing—1996–2004. Medical Care, 46 (1), 33–40. doi: 10.1097/MLR.0b013e3181484197 [DOI] [PubMed] [Google Scholar]
- Flory, J., Yinong, Y. X., Gurol, I., Levinsky, N., Ash, A., & Emanuel, E. (2004). Place of death: U.S. trends since 1980. Health Affairs (Project Hope), 23(3), 194–200. doi: 10.1377/hlthaff.23.3.194 [DOI] [PubMed] [Google Scholar]
- Gozalo, P., Teno, J. M., Mitchell, S. L., Skinner, J., Bynum, J., Tyler, D., & Mor, V. (2011). End-of-life transitions among nursing home residents with cognitive issues. The New England Journal of Medicine, 365 (13), 1212–1221. doi: 10.1056/NEJMsa1100347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski, D. C., Feng, Z., Intrator, O., & Mor, V. (2010). Medicaid bed-hold policy and Medicare skilled nursing facility rehospitalizations. Health Services Research, 45(6 Pt 2), 1963–1980. doi: 10.1111/j.1475-6773.2010.01104.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruneir, A., Lapane, K. L., Miller, S. C., & Mor, V. (2007). Long-term care market competition and nursing home dementia special care units. Medical Care, 45(8), 739–745. doi: 10.1097/MLR.0b013e3180616c7e [DOI] [PubMed] [Google Scholar]
- Harrington, C. (2010). Nursing home staffing standards in state statutes and regulations. University of California. http://www.pascenter.org [Google Scholar]
- Harrington, C., Schnelle, J. F., McGregor, M., & Simmons, S. F. (2016). The need for higher minimum staffing standards in U.S. nursing homes. Health Services Insights, 9, 13–19. doi: 10.4137/HSI.S38994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources & Services Administration . (2018). Area health resources files. https://data.hrsa.gov/data/download
- Institute of Medicine . (1997). Approaching death: Improving care at the end of life. The National Academies Press. [PubMed] [Google Scholar]
- Joyce, N. R., McGuire, T. G., Bartels, S. J., Mitchell, S. L., & Grabowski, D. C. (2018). The impact of dementia special care units on quality of care: An instrumental variables analysis. Health Services Research, 53(5), 3657–3679. doi: 10.1111/1475-6773.12867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka, R. T., Stearns, S. C., & Park, J. (2008). The staffing-outcomes relationship in nursing homes. Health Services Research, 43(3), 1025–1042. doi: 10.1111/j.1475-6773.2007.00803.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Q., Zheng, N. T., & Temkin-Greener, H. (2013). Quality of end-of-life care of long-term nursing home residents with and without dementia. Journal of the American Geriatrics Society, 61(7), 1066–1073. doi: 10.1111/jgs.12330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y., Cen, X., Cai, X., & Temkin-Greener, H. (2019). Perceived patient safety culture in nursing homes associated with “nursing home compare” performance indicators. Medical Care, 57 (8), 641–647. doi: 10.1097/mlr.0000000000001142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicaid and CHIP Payment Access Commission . (2019). States’ Medicaid fee-for-service nursing facility payment policies. https://www.macpac.gov/publication/nursing-facilty-payment-policies/
- Miller, S. C., Gozalo, P., Lima, J. C., & Mor, V. (2011). The effect of Medicaid nursing home reimbursement policy on Medicare hospice use in nursing homes. Medical Care, 49(9), 797–802. doi: 10.1097/MLR.0b013e318223c0ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell, S. L., Teno, J. M., Miller, S. C., & Mor, V. (2005). A national study of the location of death for older persons with dementia. Journal of the American Geriatrics Society, 53(2), 299–305. doi: 10.1111/j.1532-5415.2005.53118.x [DOI] [PubMed] [Google Scholar]
- Mitchell, S. L., Teno, J. M., Roy, J., Kabumoto, G., & Mor, V. (2003). Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. Journal of the American Medical Association, 290(1), 73–80. doi: 10.1001/jama.290.1.73 [DOI] [PubMed] [Google Scholar]
- Morris, J. N., Fries, B. E., & Morris, S. A. (1999). Scaling ADLs within the MDS. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 54(11), M546–M553. doi: 10.1093/gerona/54.11.m546 [DOI] [PubMed] [Google Scholar]
- Mukamel, D. B., Caprio, T., Ahn, R., Zheng, N. T., Norton, S., Quill, T., & Temkin-Greener, H. (2012). End-of-life quality-of-care measures for nursing homes: Place of death and hospice. Journal of Palliative Medicine, 15(4), 438–446. doi: 10.1089/jpm.2011.0345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel, D. B., Ladd, H., Caprio, T., & Temkin-Greener, H. (2016). Prototype end-of-life quality measures based on MDS 3 data. Medical Care, 54(11), 1024–1032. doi: 10.1097/MLR.0000000000000576 [DOI] [PubMed] [Google Scholar]
- Park, J., & Stearns, S. C. (2009). Effects of state minimum staffing standards on nursing home staffing and quality of care. Health Services Research, 44(1), 56–78. doi: 10.1111/j.1475-6773.2008.00906.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman, C. M., & Hirdes, J. P. (2008). The aggressive behavior scale: A new scale to measure aggression based on the minimum data set. Journal of the American Geriatrics Society, 56(12), 2298–2303. doi: 10.1111/j.1532-5415.2008.02048.x [DOI] [PubMed] [Google Scholar]
- ResDAC . (2016a). Long term care Minimum Data Set (MDS) 3.0. https://www.resdac.org/cms-data/files/mds-3.0
- ResDAC . (2016b). Master Beneficiary Summary File (MBSF) base. https://www.resdac.org/cms-data/files/mbsf-base
- ResDAC . (2016c). MedPAR. https://www.resdac.org/cms-data/files/medpar
- Schnelle, J. F., Simmons, S. F., Harrington, C., Cadogan, M., Garcia, E., & M Bates-Jensen, B. (2004). Relationship of nursing home staffing to quality of care. Health Services Research, 39(2), 225–250. doi: 10.1111/j.1475-6773.2004.00225.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz, M. L., Lima, J. C., Clark, M. A., & Miller, S. C. (2019). End-of-life culture change practices in U.S. nursing homes in 2016/2017. Journal of Pain and Symptom Management, 57(3), 525–534. doi: 10.1016/j.jpainsymman.2018.12.330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorra, J., Gray, L., Streagle, S., Famolaro, T., Yount, N., & Behm, J. (2018). AHRQ Nursing Home Survey on Patient Safety Culture. Agency for Healthcare Research and Quality. Prepared by Westat under Contract No HHSA290201300003C. AHRQ Publication No. 18-0038-EF (Replaces 08(09)-0060, 15(16)-0052-EF); July 2018. [Google Scholar]
- Stone, P. W., Harrison, M. I., Feldman, P., Linzer, M., Peng, T., Roblin, D.,…Williams, E. S. (2005). Organizational climate of staff working conditions and safety—An integrative model. In Henriksen K.et al. (Eds.), Advances in patient safety: From research to implementation (volume 2: concepts and methodology). Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- Temkin-Greener, H., Cen, X., & Li, Y. (2020). Nursing home staff turnover and perceived patient safety culture: Results from a national survey. The Gerontologist, 60(7), 1303–1311. doi: 10.1093/geront/gnaa015 [DOI] [PubMed] [Google Scholar]
- Temkin-Greener, H., Li, Q., Li, Y., Segelman, M., & Mukamel, D. B. (2016). End-of-life care in nursing homes: From care processes to quality. Journal of Palliative Medicine, 19(12), 1304–1311. doi: 10.1089/jpm.2016.0093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temkin-Greener, H., Zheng, N. T., Norton, S. A., Quill, T., Ladwig, S., & Veazie, P. (2009). Measuring end-of-life care processes in nursing homes. The Gerontologist, 49(6), 803–815. doi: 10.1093/geront/gnp092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, K. S., Dosa, D., Wysocki, A., & Mor, V. (2017). The Minimum Data Set 3.0 Cognitive Function Scale. Medical Care, 55(9), e68–e72. doi: 10.1097/MLR.0000000000000334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, K. S., Hyer, K., Castle, N. G., Branch, L. G., Andel, R., & Weech-Maldonado, R. (2012). Patient safety culture and the association with safe resident care in nursing homes. The Gerontologist, 52(6), 802–811. doi: 10.1093/geront/gns007 [DOI] [PubMed] [Google Scholar]
- Walsh, E. G., Freiman, M., Haber, S., Bragg, A., Ouslander, J., & Wiener, J. M. (2010). Cost drivers for dually eligible beneficiaries: Potentially avoidable hospitalizations from nursing facility, skilled nursing facility, and home and community-based services waiver programs. U.S. Centers for Medicare and Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/downloads/costdriverstask2.pdf [Google Scholar]
- Xing, J., Mukamel, D. B., & Temkin-Greener, H. (2013). Hospitalizations of nursing home residents in the last year of life: Nursing home characteristics and variation in potentially avoidable hospitalizations. Journal of the American Geriatrics Society, 61(11), 1900–1908. doi: 10.1111/jgs.12517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X., & Grabowski, D. C. (2004). Nursing home staffing and quality under the nursing home reform act. The Gerontologist, 44(1), 13–23. doi: 10.1093/geront/44.1.13 [DOI] [PubMed] [Google Scholar]
- Zheng, N. T., & Temkin-Greener, H. (2010). End-of-life care in nursing homes: The importance of CNA staff communication. Journal of the American Medical Directors Association, 11(7), 494–499. doi: 10.1016/j.jamda.2010.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman, S., Bowers, B. J., Cohen, L. W., Grabowski, D. C., Horn, S. D., & Kemper, P., for the THRIVE Research Collaborative . (2016). New evidence on the Green House model of nursing home care: Synthesis of findings and implications for policy, practice, and research. Health Serivces Research, 51(Suppl. 1), 475–496. doi: 10.1111/1475-6773.12430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman, S., Gruber-Baldini, A. L., Hebel, J. R., Sloane, P. D., & Magaziner, J. (2002). Nursing home facility risk factors for infection and hospitalization: Importance of registered nurse turnover, administration, and social factors. Journal of the American Geriatrics Society, 50 (12), 1987–1995. doi: 10.1046/j.1532-5415.2002.50610.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.