Abstract
Home dialysis modalities remain significantly underused in the United States despite similar overall survival in the modalities, and recent incentives to expand these modalities. Although the absolute number of patients using home modalities has grown, the proportion compared to in-center hemodialysis (ICHD) continues to remain quite low. Well known barriers to home dialysis utilization exist, and an organized and team-based approach is required to overcome these barriers. Herein, we describe our efforts at growing our home dialysis program at a large academic medical center, with the proportion of home dialysis patients growing from 12% to 21% over the past 9 years. We prioritized individualized education for patients and better training for physicians, with the help of existing resources, aimed at better utilization of home modalities; an example includes dedicated dialysis education classes taught twice monthly by an experienced nurse practitioner, as well as the utilization of the dialysis educator from a dialysis provider for inpatient education of patients with CKD. The nephrology fellowship curriculum was restructured with emphasis on home modalities, and participation in annual home dialysis conferences has been encouraged. For timely placement and troubleshooting of access for dialysis, we followed a complementary team approach using surgeons and interventional radiologists and nephrologists, driven by a standardized protocol developed at UAB, and comanaged by our access coordinators. A team-based approach, with emphasis on staff engagement and leadership opportunities for dialysis nurses as well as collaborative efforts from a team of clinical nephrologists and the dialysis provider helped maintain efficiency, kindle growth, and provide consistently high-quality clinical care in the home program. Lastly, efforts at reducing burden of disease such as decreased number of monthly visits as well as using innovative strategies, such as telenephrology and assisted PD and HHD, were instrumental in reducing attrition.
Keywords: dialysis, barriers to home dialysis, home dialysis, home dialysis academy, home hemodialysis, modality education, peritoneal dialysis, telenephrology, urgent peritoneal dialysis
Introduction
The past year has been an exciting year for nephrology in the United States, with the Presidential Executive Order bringing home dialysis into the spotlight. The Advancing American Kidney Health Initiative (AAKHI) signed as a part of the Executive Order in July 2019 is a major step in improving access to home dialysis for patients with ESKD. This is an opportune time for the nephrology community to analyze areas of strengths and weaknesses in home modalities and to grow home modalities in an organized and sustainable fashion.
There have been regional and national efforts at improving utilization of home dialysis in the past decade, such as the Prospective Payment System and urgent peritoneal dialysis (PD) programs, although they have been met with limited success. The challenges to appropriately use home modalities have been multifold, including low start rates, high attrition rates, and inadequate infrastructure in all facets of medicine to care for the patient on home dialysis (nursing facilities, trained access operators, transition to home, etc.). We briefly describe some of these barriers (Supplemental Table 1). One of the main challenges is a lack of comfort and familiarity among patients and nephrologists, likely due to inadequate education. Other common issues include lack of trained and willing operators to place and troubleshoot dialysis access, as well as inadequate infrastructure to care for patients on home dialysis. The system is better organized at directing a patient toward in-center hemodialysis (ICHD), but multiple hurdles exist in educating and training a patient to perform home dialysis. We describe our efforts at a large academic medical center (University of Alabama at Birmingham, UAB) in identifying challenges, and how we have adopted strategies to overcome some of these limitations and expanded our home dialysis program; the percentage of patients on home dialysis at UAB has grown from 67 of the total 575 patients on dialysis (12%) in 2011 to 148 of the 701 total patients on dialysis (21%) in January 2020. These efforts include increased access to dialysis education, team-based approaches, strategies to improve access placement, urgent start PD, and innovations such as telehealth for home dialysis (Table 1).
Table 1.
University of Alabama at Birmingham home dialysis program growth: key strategies
| Key Strategies |
| Education |
| Emphasis on timely and repetitive patient-tailored education |
| Experienced and engaged nurse practitioner–led dialysis modality education |
| Using dialysis provider’s CKD educator for in-hospital dialysis education |
| Structured curriculum for trainees in home dialysis |
| Access |
| Use of existing access coordinators in the home dialysis program |
| Use interventional radiology and surgery for access placement |
| Protocols developed to triage patients for PD access in a timely fashion |
| Teamwork |
| Dedicated and experienced team of home dialysis nurses |
| Emphasis on staff engagement and leadership for nurses |
| Multipronged approach to dialysis modality education |
| Strong collaboration with dialysis provider |
| Dedicated effort from two nephrologists toward the home dialysis program |
| Other |
| Using innovative approaches like telenephrology and assisted PD |
| Easy availability of urgent start for PD and HHD |
| Decreasing attrition by reducing burden of treatment, and other strategies |
| Repurposing existing resources toward the home dialysis program such as access coordinators, APPs, and dialysis provider’s CKD educator |
APP, advanced practice providers; PD, peritoneal dialysis; HHD, home hemodialysis.
Education
Lack of timely and well planned predialysis education remains a major barrier to patients choosing home modalities (Supplemental Table 2). Studies reveal that over a third of patients perceive that they did not get education on home modalities (1,2); others feel they receive biased information, and are not able to play an important role in decision making for modality selection (1,3). The recent push to improve utilization of home modalities has led to enhanced efforts toward modality education, although as a nation we may be guilty of using a “one-style-fits-all” approach that needs to be modified. Many patients feel their individual preferences are not considered at the time of modality education (4); most dialysis education is designed to have a short description of in-center and home modalities, describing the advantages and disadvantages of both settings. This does not personalize the preferences and individual characteristics of the patient such as age, occupation, family support, and transportation, among other factors. For example, a young working patient would automatically be referred to a home program, but a 72-year-old patient with diabetes with a prosthetic limb may not even be offered home dialysis. An organized program that starts off with a group session and then personalizes education and training based on the patients’ preferences and understanding of the different modalities, with an individual session with an educator as well as guided dialysis unit visits, offers a more tailored approach.
The nephrologists’ suggestion often plays a critical role in patients’ choice of dialysis modality selection (5), which puts the responsibility of the education, even if as part of a larger CKD education program, back on the treating nephrologist; this can only be well executed if the nephrologist is engaged, competent, and well educated about home dialysis themselves. A study conducted in 2010 revealed that United States trainees have limited home dialysis exposure, lack of a continuity of care for patients on home dialysis, and lack of a home dialysis curriculum, among other educational gaps; the proportion of the recently graduated nephrologists who felt well trained and competent in home dialysis was alarming: 56% in PD and 16% in home hemodialysis (HHD) (6). It is evident that we need a dedicated and organized effort for improving the structure of our nephrology training programs with focus on home dialysis, including hands-on training (4). With the changing landscape of home dialysis over the past decade, it is conceivable that this may have changed; a follow-up study to understand our current home dialysis trainee education and its effects is warranted to determine best practices in home modality education.
At UAB, both patient and trainee education were reinvigorated by improving and individualizing patient education, and establishing a dedicated curriculum for the nephrology trainees. Patient education starts with an initial discussion in the nephrologists’ clinic, with a discussion of the different dialysis modality options (as well as renal transplant and “supportive care”) offered to the patient. A PD mannequin, with a PD catheter, as well as a PD machine prototype are available in the clinic for demonstration, which helps the patients understand the details of PD. In addition, twice monthly dialysis education classes taught by a seasoned nurse practitioner are offered to the patient, and scheduled via the access center and the nephrology office. These classes are held in a conference center in the outpatient clinic and last 45–90 minutes, with emphasis on discussion about the need for dialysis and the different dialysis modalities available; existing patients on in-center dialysis as well as home dialysis are often invited to attend and answer questions for patients considering dialysis. This is followed by an individual dialysis education session with a dialysis educator, which involves audiovisual aids, one-on-one discussion, as well as a tour of the dialysis units (home and in-center). Sit-down discussions are offered with home dialysis nurses, as well as existing patients on dialysis, based on patient preference and the educator’s assessment of their needs. Patients are given access to reading materials and videos on the different modality types which summarizes previous knowledge and adds experiences of other patients. A similar approach is followed for inpatients. A dialysis educator, an employee of the dialysis provider, is credentialed at our organization, with access to our electronic medical record. This educator makes daily rounds in the hospital and provides one-on-one sessions, lasting 30–45 minutes, to all patients with advanced CKD, in collaboration with the treating nephrologist, and documents in the electronic medical record. This also ensures two levels of follow-up for all such patients: the dialysis educator from the dialysis provider maintains follow-up with the patient, and so does the UAB team, with the responsibility of access placement assigned to the UAB team of nephrologist and access coordinators. There is ample data as well as focus on patient-centered approaches to care that support early patient involvement in decision making and adequate predialysis education (7–10). In our experience, using a combination of educational strategies in an organized, collaborative, and repetitive fashion, with individual attention to patient attributes, enables the patient to make the most informed decision regarding initiation of a dialysis modality.
For trainee education, we incorporated a curriculum-based approach, with dedicated rotations for home dialysis in fellowship supervised by the home dialysis faculty. The rotation includes extensive exposure to patients, with focus on dosing, access troubleshooting, and volume management, along with more practical aspects of home dialysis such as establishing and growing a program and decreasing attrition (Table 2). In addition, UAB hosts the Home Dialysis Academy, a 2.5-day course attended by 40–50 nephrology trainees annually. Home Dialysis Academy focuses on helping trainees gain confidence in initiating and maintaining patients on home modalities. It covers the basics of “why home dialysis?,” patient selection and education, pathophysiology, prescription management, and troubleshooting scenarios. Frequent, well-spaced, interactive groups sessions help clarify key concepts, solve clinically applicable scenarios, and answer individual questions. The last day entails small group sessions in the home dialysis unit, where trainees learn hands-on techniques like catheter dysfunction, transfer set changes, HHD machine setup, and using prescription algorithms to best meet the needs of their patients. The course has been met with immense enthusiasm from fellows from across the nation, and has been incorporated in the fellowship curriculum of other academic programs. The Home Dialysis University is another well organized program dedicated to home dialysis education.
Table 2.
University of Alabama at Birmingham Nephrology Fellowship home dialysis curriculum
| Home Dialysis Curriculum | |
| Objectives: First year of training | Objectives: Second year of training |
| Understand home dialysis prescription | Training patients on home dialysis |
| Introduction to urgent start PD | Independently prescribing PD and HHD |
| Manage PD patients undergoing abdominal surgery | Access evaluation in PD and HHD |
| Importance of residual renal function | Independently manage complications |
| Management of complications | Understand social aspects of home modalities |
| Peritonitis | Learn team-based approach |
| Catheter-related infections | Understand the role of medical director |
| Catheter dysfunction | |
| Structured learning | |
| 1–2 mo rotations in both years of fellowship | |
| Twice weekly clinics while on rotation; evaluate 6–8 patients a day | |
| Participate in a home visit with the nurse | |
| Coordinate patient care using access coordinators, dietician, social worker with dialysis attendings | |
| Annual Home Dialysis Academy, one-on-one teaching, and independent reading | |
| Active participation in monthly multidisciplinary quality meeting | |
| Competency milestones | |
| Patient care: independent assessment and management of home dialysis patients | |
| Medical knowledge: develop a knowledge base of HHD and PD pathophysiology and prescription management, and formulate treatment strategies in challenging situations | |
| Problem-based learning and improvement: integrate evidence-based medicine in evaluation and management of patient problems | |
| Interpersonal and communication skills: work as a part of the dialysis team, understand role of medical director, including quality and safety | |
| Problem-based practice: effectively use team-based resources to accomplish patient-centered care in an effective manner | |
PD, peritoneal dialysis; HHD, home hemodialysis.
Access
Access for PD, just like hemodialysis (HD), is a major obstacle in establishing and maintaining patients on the modality. In the ideal world, a good program requires timely and skilled catheter placement, along with continued and prompt support when an intervention such as revision or exchange is required. Furthermore, timely HD access placement needs to be sought if there is a possibility of the PD access not working or impending technique failure.
Several well described challenges limit the availability and enthusiasm of surgeons to place and troubleshoot PD catheters (Table 3). A coordinated effort to engage surgical colleagues is pivotal to systematically grow home modalities. Every program should assess their need, and planned growth, and invest in training their surgeon(s) in programs such as the PD University for Surgeons. As volumes increase, PD catheters may become a substantial part of a surgeon’s practice to allow for dedicated time and effort, which may then lead to improved training of surgical trainees and catheter outcomes. At UAB, we have collaborated with multiple surgeons from transplant surgery and gastrointestinal surgery; having more than one surgeon, from different subspecialties, allows availability for timely access placement and troubleshooting of catheters. This especially holds true in situations such as vacation time, national conferences, and conflicting responsibilities of emergency surgeries like deceased donor renal transplants and liver transplants, when coverage from another surgeon in a timely fashion can help prevent delays in care.
Table 3.
Challenges to surgeon availability for access placement
| Challenges |
| Limited expertise related to inadequate exposure and training (11) |
| Limited operating room time |
| Conflicting responsibilities |
| Administrative |
| Renal transplant or other surgical proceduresa |
| Vascular access placement |
| Recurrent catheter troubleshooting after initial PD catheter placement |
| Coverage issues secondary to small surgical team (11) |
| Reimbursement not lucrative for the time invested in PD catheter placement (12) |
| Low volume of procedures, and hence inability to make it a niche |
PD, peritoneal dialysis.
At University of Alabama at Birmingham, PD catheters are placed by renal transplant surgeons.
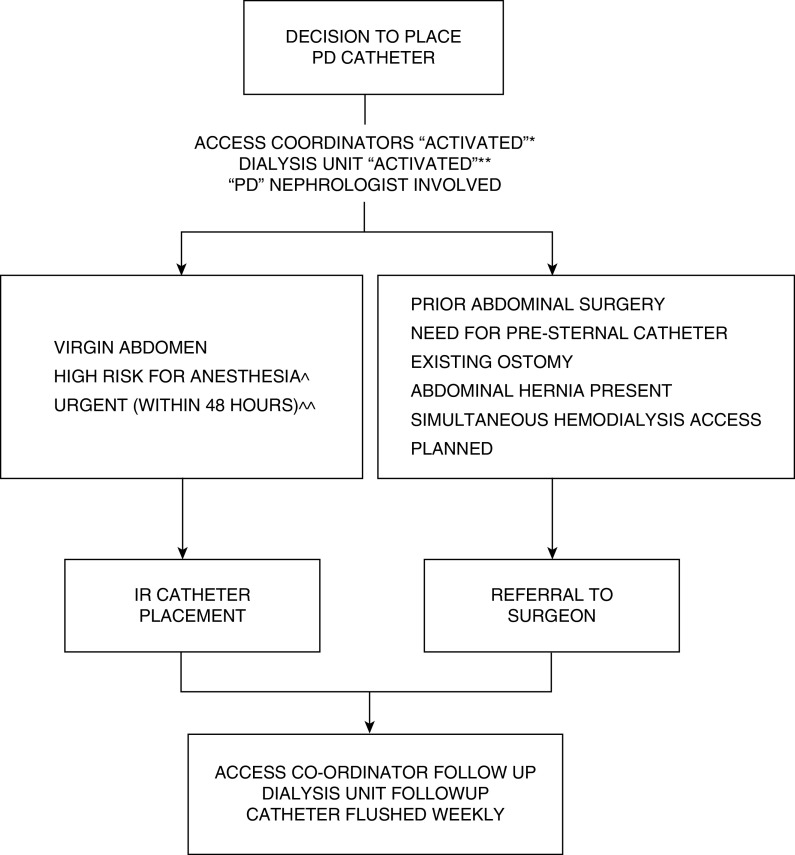
Evidence suggests similar outcomes, including catheter survival and complications, for catheters placed by surgeons versus interventional radiology (IR) and nephrology (13,14); also, using IR for PD catheter placement helps shorten time to catheter placement and enhances PD penetration in a program (14–20). This is encouraging and, if used in a team-based approach, can prevent interdisciplinary disputes, allow IR and surgery to complement each other, and improve the utilization of home modalities (21,22). Figure 1 describes our methodology for determining the most appropriate operator. Every organization needs to develop their own algorithm, based on availability of resources, expertise of the operators, and the clinical volume. UAB has five operators within IR who currently place PD catheters, two of whom are interventional nephrologists; in addition, we have three surgeons who place PD catheters. At UAB, patients with no prior abdominal surgeries are referred to IR for a PD catheter placement to best use resources in a timely manner. Patients who had multiple abdominal surgeries, have an ostomy, require a presternal catheter, or require a concomitant abdominal hernia repair are referred to a surgeon. This approach allows us to use the expertise of both IR and surgery, without overburdening either specialty, and provides us the ability to expedite catheter placement, with a goal of 48 hours from consult to placement when urgent.
Figure 1.
Methodology for determining most appropriate operator for peritoneal dialysis (PD) catheter placement. *Access coordinators ensure the patient has been educated, questions answered, and appropriate imaging and appointments are coordinated. **Dialysis unit starts paperwork for admission, and early involvement helps allay patient/family fears; also helps in a smooth transition into the dialysis unit once catheter ready for use. ***Virgin abdomen: No prior abdominal surgeries. ^High risk for anesthesia: needs a discussion between patient, nephrologist, surgeon and interventional radiology on a case by case basis. ^^Urgent catheter placement: if multiple prior abdominal surgeries, or need for surgical intervention anticipated, nephrologist communicates directly with surgeon.
PD catheter malfunction accounts for a large proportion of technique failure, especially in the first 6 months after starting PD (23,24). As such, timely interventions help ensure success of a PD program. A team of well trained nephrologists and nurses can manage most access-related complications in the dialysis clinic, allowing the surgeon to concentrate only on specific surgical interventions if needed, such as repositioning or resiting the catheter. We have developed protocols at UAB (Figure 2) that allow us to collaborate well with the surgeon, limiting their referrals to only those requiring a surgical intervention, and enables effective communication to avoid unnecessary transition to HD and the postoperative resumption of PD.
Figure 2.
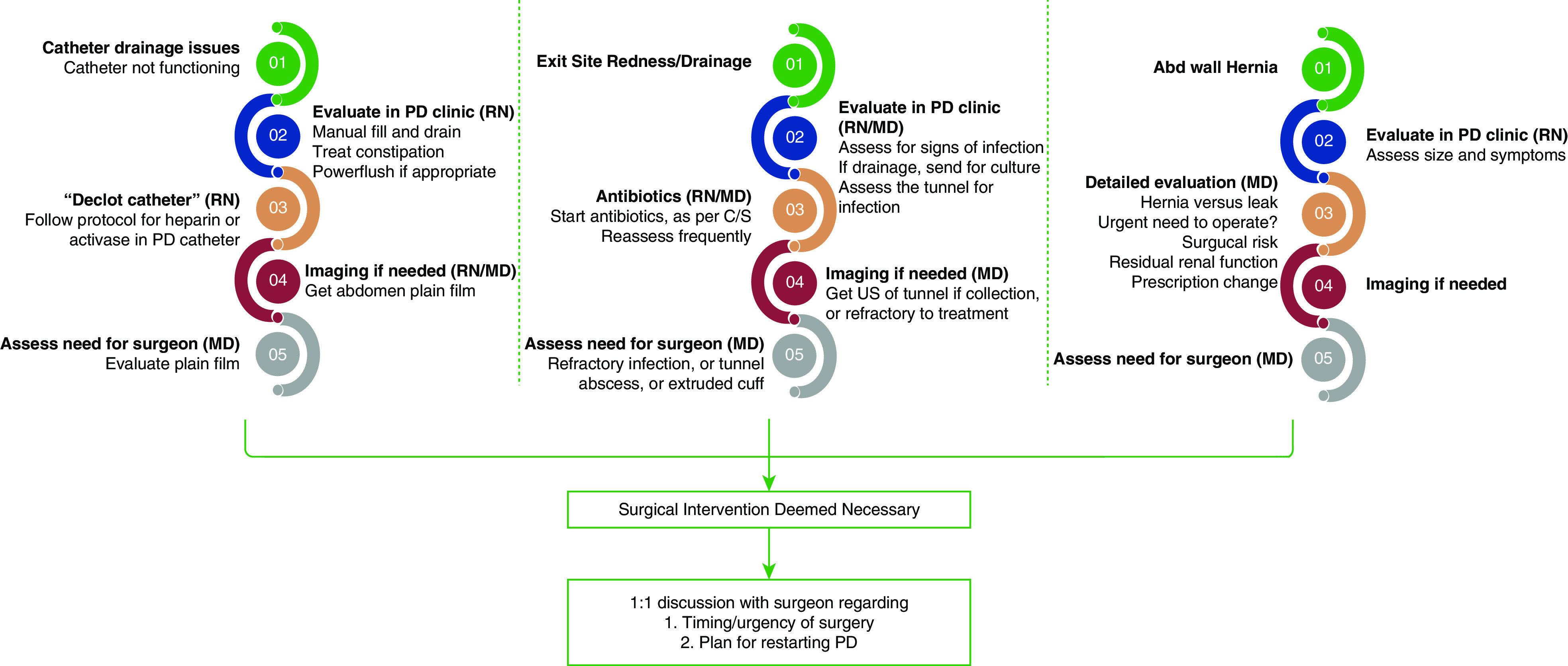
Catheter troubleshooting protocols developed at University of Alabama at Birmingham. Abd, abdominal; C/S, culture and sensitivity; MD, medical doctor; RN, registered nurse; US, ultrasound.
Self-cannulation of permanent vascular access is a well established patient-perceived barrier to the uptake of HHD; some home programs are reluctant to offer HHD to patients with indwelling catheters in view of the existing evidence that suggests worse outcomes in patients on HHD with vascular catheters compared with permanent arteriovenous access (25). These facts, taken together, should not be misinterpreted to make a case for starting patients on ICHD in place of HHD if they have a vascular catheter; instead, for the appropriate patient who is interested in HHD, this should encourage us to establish permanent access as soon as possible, and transition from catheter to permanent access while on HHD. We have followed this pathway for many years, and have been able to transition most patients successfully to permanent arteriovenous access. With the national emphasis on home modalities, incentives to operators regarding placement and revisions of PD catheters are necessary to ensure adequate numbers of operators who are willing to place and revise catheters. The recent introduction of an outcomes-based program for nephrologists and health systems is a perfect setting to consider a similar structured program for surgeons (12).
Team-Based Approach
A team-based, dynamic approach is critical to the success of a home dialysis program. UAB home program’s clinical growth, while maintaining high-quality care, has been made possible by a team-based approach, led by the nephrologist but executed by the dialysis team of nursing staff, access coordinators, nutritionists, social workers, IR, and surgeons, with support from the dialysis provider (Figure 3).
Figure 3.
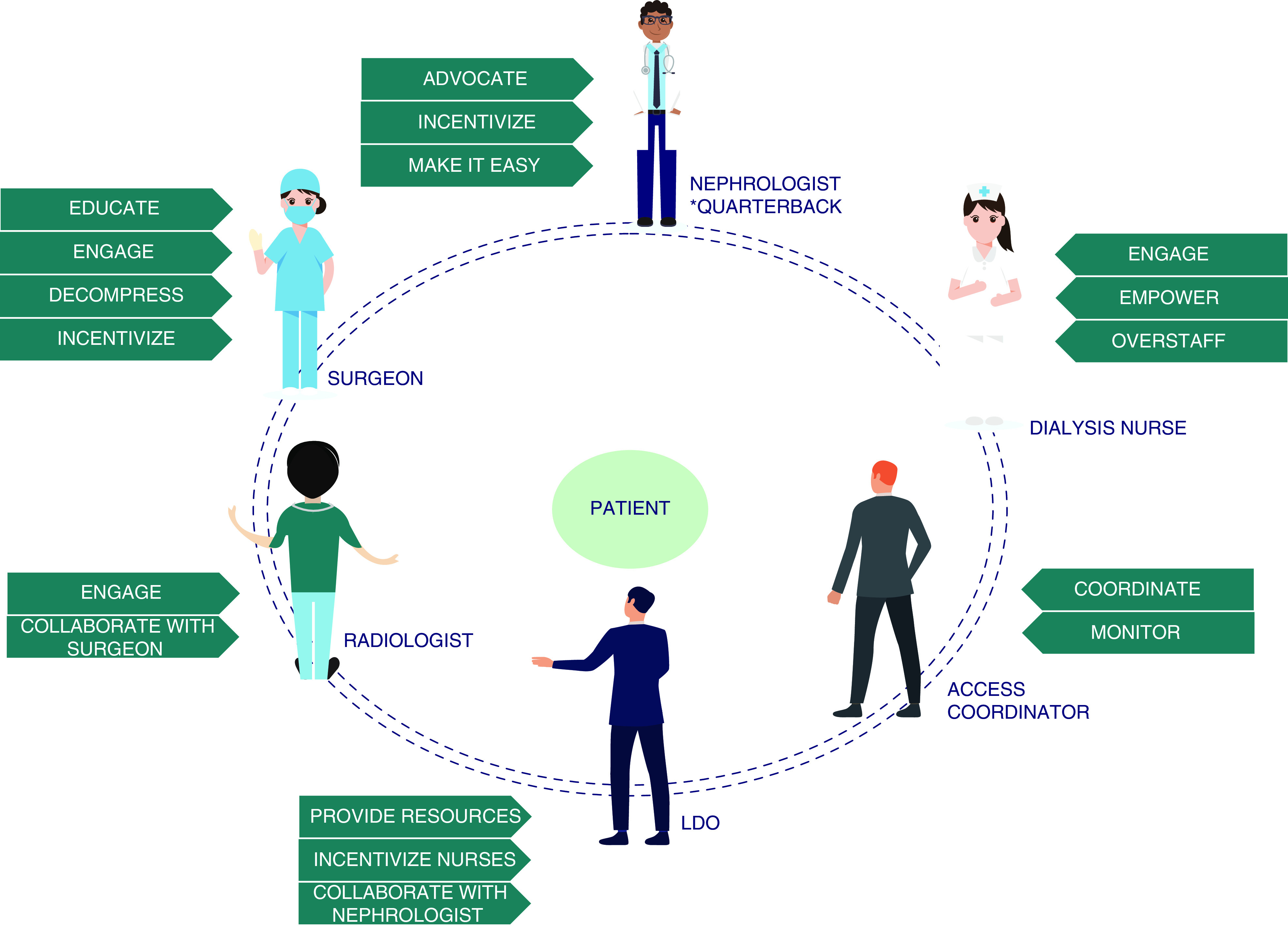
A team-based dynamic approach for home dialysis programs. LDO, large dialysis organization.
Dialysis nurses play a pivotal role in the success of any home dialysis program, and have been at the forefront of our program’s growth. The home dialysis nurses are able to form deep bonds with the patient, considering the continuity of care and the long period of training as well as home visits. In addition, the patients have access 24/7 to their home dialysis team through a call phone, compared to the patients on ICHD who often have to reach the physician office after hours or on the weekends. The nurses individualize their education, training, and care to each home patient, while following an underlying set of care standards as set by the team. They often know which patient would balk at the idea of a 10-hour overnight treatment, or the one who would prefer a midday exchange instead of increasing their last fill volume, or whose wife is developing worsening dementia and may need respite care. Nurses must be involved in key decision making for the patients because the combined knowledge of the physician and the nursing team, assisted by patient input, leads to solutions that work best for patients. Furthermore, nutritionists and social workers are vital to support patient care, improve outcomes, and ensure adequate access to care and the services needed to care for patients with ESKD.
Home dialysis offers some inherent scheduling advantages to dialysis nurses, in addition to other potential benefits compared to in-center nurses (Table 4); despite this, the training and retention of nurses remains a challenge. The high disease burden in patients on dialysis, expectations for a high patient/nurse ratio, 24-hour call coverage for patient-related issues, and competing offers from other dialysis provider organizations all play a role in nursing retention difficulties. We describe strategies that have been successful in retaining our home dialysis nurses in Table 4. The registered nurse/patient ratio at UAB is 1:20 for PD and 1:12 for HHD; our current team consists of ten PD nurses and two HHD nurses, and two nurses who are cross-trained on PD and HHD. The nurses are allowed a flexible schedule to train their patients and to accommodate clinic visits and the urgent-start patients. They perform a home visit at the time of evaluation, after finishing training and then annually; in addition, if a change in the home situation occurs (death of a spouse, moving homes, frequent episodes of peritonitis, etc.), a home visit is performed. Experienced nurses play leadership roles in clinical outcomes, infection prevention, training younger nurses, and are allowed a lower patient workload.
Table 4.
Strategies to improve nurse engagement in home dialysis programs
| Home Dialysis Nurses | |
| Advantages | Disadvantages |
| Schedule of 8 am to 5 pm | Less opportunities for growth into leadership, considering smaller market share of patients on home dialysis |
| No scheduled work on holidays or weekends | Call responsibilities for after-hours issues |
| 1:1 care of patient, starting with evaluation, training, and then care at home | Lack of moonlighting opportunities |
| Role in education and training | |
| Nurse to patient ratio (1:20 at UAB) may appear high, but ability to see patients at your own pace | |
| Measures that helped our program in high retention of staff | |
| Offer a 4-day work week | |
| Offer flexibility in work and call schedule | |
| Dedicated steps toward staff engagement, including team building efforts and quality incentives | |
| Ongoing discussions, with success, with LDO to adjust nurse/patient ratios (overstaffing) to | |
| Accommodate for training and growth | |
| Achieve quality and safety measures | |
| Train new hires | |
| Cross-training of nurses in home hemodialysis and peritoneal dialysis | |
| Proposals for a national level policy change | |
| Consider incentives for nursing staff engaged in home modalities | |
| Dedicated effort to offer leadership and growth opportunities to home dialysis nurses | |
UAB, University of Alabama at Birmingham; LDO, large dialysis organization.
At UAB, dedicated access coordinators play a major role in coordinating access placement, troubleshooting, and follow-up. Examples include monitoring the progress of patients after access placement, reminding the dialysis unit to recheck cultures a week after finishing antibiotics for peritonitis, or coordinating catheter flushes on a weekly basis as requested by surgeon. An often under-recognized element in the care of the patient with kidney disease is the “non-nephrology” physician. The primary care physicians often have a long-standing relationship with the patient and help them make critical decisions, including the choice of dialysis modality (26). We realized this was just as important in the care of patients with solid organ transplants, who often sought the opinion of their transplant physician in making a dialysis modality decision. We have consciously involved the primary care physicians, and other specialties across UAB Medicine, in both education about home modalities and dispelling myths related to home modalities. This leads to a more unified approach to advanced kidney disease management, and allays the fears of the patient deciding on a modality. Lastly, it is important to understand the role of the dialysis provider in providing care to patients on dialysis and to work as a team, encouraging them to provide high-quality innovative care, while also guiding them with the expertise of medical decision making. UAB’s collaboration with our partnering dialysis provider has been successful and has allowed for prompt and expert nursing support and partnership in innovative ideas, in addition to the resources required to expand home dialysis.
Effective utilization of resources, with patient-centered care, as well as staff engagement are some of the underlying principles of modern-day medicine. We were fortunate to have existing resources that we repurposed in an innovative manner. The dialysis access coordinators were existing employees (two registered nurses, with a 40-hour work week) within the Division of Nephrology at UAB, handling predominantly vascular access; we used their role in helping triage patients for PD catheter placement and follow-up PD catheters in an effective manner. An existing, experienced nurse practitioner, with a special interest in CKD education, offered to spearhead dialysis modality education; she spends 2 hours every 2 weeks in providing dialysis education in the outpatient setting, and many payers allow billing for this dialysis education. The ability to have dedicated time built into the clinical effort of two clinical nephrologists helps them take care of existing patients, educate, train, and assume the care of patients who choose home dialysis, as well as develop strategies to sustain growth and high-quality care. All new starts on home dialysis transfer their dialysis care to the home unit nephrologists, which allows for a streamlined care pathway. We were also able to use existing resources offered by the LDO (large dialysis organization), and modify them; this enabled us to use the educator employed by the LDO to provide the in-hospital education to our advanced CKD and unplanned dialysis start patients. Similarly, we requested our home dialysis nurses to play a bigger role in educating patients when they visit the home unit, as well as train the younger nurses in imparting education; the LDO in return allowed the senior nurses to have a lesser number of patients considering their leadership and administrative roles.
Unplanned Dialysis
Unplanned dialysis or “urgent start” initiation is unfortunately very common and a majority of these patients are started on ICHD (27–29). Many of these patients wish for a more extensive discussion of their dialysis modality choices before dialysis initiation (28,30). Unplanned start on PD is considered a safe and efficient alternative to unplanned HD, even in the elderly (29,31–33), and decreases the need for temporary tunneled dialysis catheter for HD, without increasing hospital stays (13,34).
The UAB urgent PD program was started in 2013 and has been successful in providing choice of modalities to all patients, including unplanned starts, and has been an integral part of the growth of our home dialysis program (Supplemental Table 3). The key to making this work is prompt education of the patient, easy and quick access placement, and a smooth transition to home without prolonging the hospital length of stay. An unexpected benefit of initiating an urgent PD program was the culture change at our organization to always give patients a choice in modalities (Figure 4). One reason for this culture change was that initiating a patient on PD became as efficient for the nephrologist as initiating someone on ICHD, thus removing a significant barrier for initiating of home therapy (Table 5).
Figure 4.
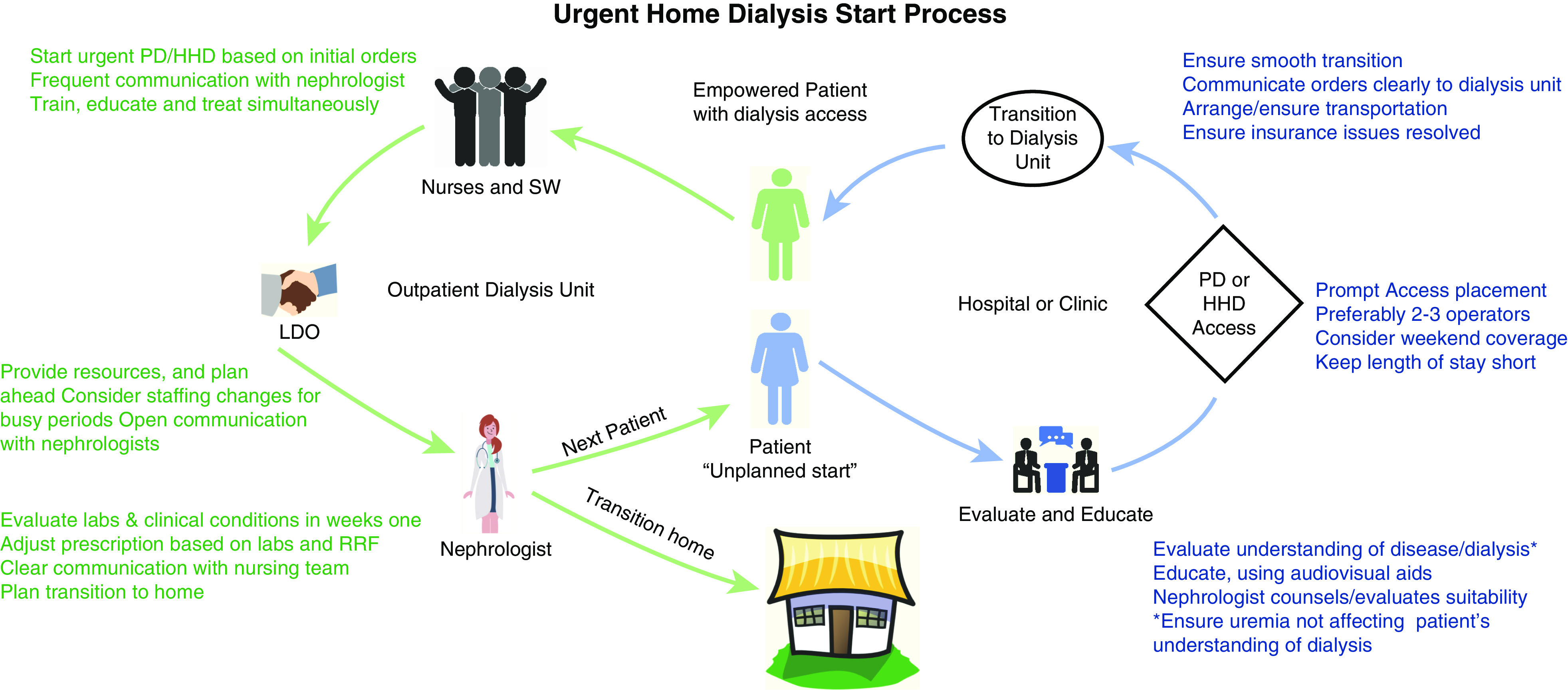
Urgent home dialysis: the process from initiation to transition home. HHD, home hemodialysis; SW, social worker.
Table 5.
Culture change at UAB Medicine with the urgent start PD program
| Nephrologists |
| Improved access to PD, inpatient and outpatient |
| Prompt PD catheter placement avoids need for temporary hemodialysis access |
| Urgent PD protocols “make it easy” |
| Smooth transition into dialysis unit prevent prolonged length of stay at the hospital |
| Interventional Radiology/Nephrology |
| Enthusiastic support in catheter placement |
| Innovative measures in patients with critical illness such as refractory heart failure |
| Routine calls to PD team about patients with challenging vascular access to consider PD as an option |
| Trainees |
| Choices of modality for unplanned dialysis starts, even in the hospital |
| Urgent PD led to increasing interest in PD |
| Multiple calls from trainees to consider patients for urgent start dialysis, either home hemodialysis or peritoneal dialysis |
| Access/Transplant Surgeons |
| Tangible increase in surgeons suggesting home modalities to patients, even when evaluating for hemodialysis access |
| Patients with failing renal allografts, especially sudden onset, referred for urgent home start |
UAB, University of Alabama at Birmingham; PD, peritoneal dialysis.
For HHD, we offer programs such as “urgent start HHD” (similar to urgent PD, and we allow initiation of HHD with tunneled dialysis catheters); “experience the difference,” where patients can experience HHD at the time of discharge, and make a more deliberate decision about modality choice while on HHD; as well as “transitional care units,” where patients are allocated to a dedicated ICHD unit with the aim of providing education on modality and access twice weekly, with the goal of transitioning to home dialysis based on patient choice.
Decreasing Attrition
Home dialysis remains plagued by high attrition rates, often to ICHD (24,35,36). Efforts aimed at reducing technique failure are key to the growth of any home program. We discuss some measures implemented at UAB that are well described in literature, although not commonly practiced.
There is increasing interest in laparoscopic procedures in patients on PD, with early resumption of PD in uncomplicated surgeries such as cholecystectomy, appendectomy, abdominal wall hernia repairs, and gastric sleeve surgery; in patients who undergo complicated surgeries such as hemicolectomy, with adequate surgical expertise, and perioperative antibiotic prophylaxis, removal of the PD catheter can be prevented, with resumption of PD in 3–4 weeks (37,38). Similarly, there is evidence to suggest good outcomes in patients who continue PD in the perioperative period when undergoing cardiothoracic surgery; unnecessary transition to HD and placement of an HD catheter and the associated risk of infection can be avoided with early involvement of the nephrologist in many such patients (39). The UAB PD nephrologist plays the role of the quarterback in these situations, adjusting prescription before surgery and resuming PD after surgery, with modifications to prescription based on multiple factors, including kind of surgery, risk for complications, and residual renal function.
Many patients with ESKD need rehabilitation after their hospital stay considering the high disease burden. Although there are many facilities that accept patients on HD, with provision for either HD within the facility or transportation to a dialysis facility, placement of patients on PD in these facilities remains a challenge. Patients on PD in need of these services are forced with the choice of forgoing the service or changing modalities. UAB has partnered with a local rehabilitation facility that accepts patients on PD, and the nurses at the facility perform PD. A partnership with UAB provides adequate initial and ongoing training to nurses on staff; in addition, the teamwork of the PD nephrologist and the medical director of the nursing facility helps ensure a holistic approach to the care of patients on PD in these facilities.
For patients with impending transition from PD, our cross-trained home nurses initiate the conversation about HHD early on, to encourage HD access placement, education, and assurance about HHD; this often leads to a smooth transition and enables us to keep the patient at home. Another less commonly discussed strategy that can safely keep patients on PD is simultaneous catheter exchange. Considering the potential role of a biofilm in the lumen of the PD catheter in patients presenting with a relapsing or early repeat peritonitis (within 3 months), simultaneous catheter exchange is a superior option to administration of thrombolytics (40). In this subset of patients, after treatment with antibiotics for 3 weeks, if cultures are negative, symptoms have resolved, and peritoneal cell counts are zero, a simultaneous catheter exchange is performed at UAB. PD is resumed within 2 days after the exchange and antibiotics are continued for 1 week postexchange.
Reducing the burden of disease on patients on home dialysis is very important to reducing technique failure. One strategy we follow at UAB to reduce burden of disease includes incremental PD which allows patients to have reduced number of days, fill volume, or exchanges as long as the total PD clearance remains adequate. Incremental PD may preserve residual renal function and improve quality of life for patients, without any effect on mortality or technique failure (41,42). In addition, to keep the burden of clinic visits and transportation low, we offer patients the ability to make only one clinic visit per month for their laboratory draws and the physician visit; they are called a week later with their test results by one of the team members, and abnormal laboratory results and interventions are discussed on the phone.
Innovation
The strength of any program lies in the ability to recognize challenging scenarios, adapt, and provide innovative solutions. At UAB, we work closely with many teams to provide care for complicated patients with a high disease burden, sometimes because they are unable to be accepted into in-center dialysis units. We have collaborated with our Advanced Heart Failure team to initiate patients with inotrope-dependent heart failure and severe hypotension on urgent PD, with a transition to home dialysis. Urgent PD enabled many of these patients to be weaned off the inotropes and be considered for advanced therapies for heart failure. Similarly, we were able to provide long-term HHD to a patient dependent on a left ventricular assist device, who was not accepted in any in-center dialysis unit as his BP required sonographic measurement during treatment. UAB has been a pioneer in the use of telemedicine to allow for patients to reduce physical trips to the home dialysis unit while not compromising on quality of care (43). Digital advances such as remote patient monitoring have been shown to reduce hospitalizations in the home dialysis population, and UAB has implemented remote patient monitoring of its home dialysis patients (44). Assisted PD and HHD have also been used at UAB, although these were provided for by the patients’ families; growth of these interventions, with some support from the payers, is essential to grow home modalities to the degree desired by the AAKHI.
Conclusion
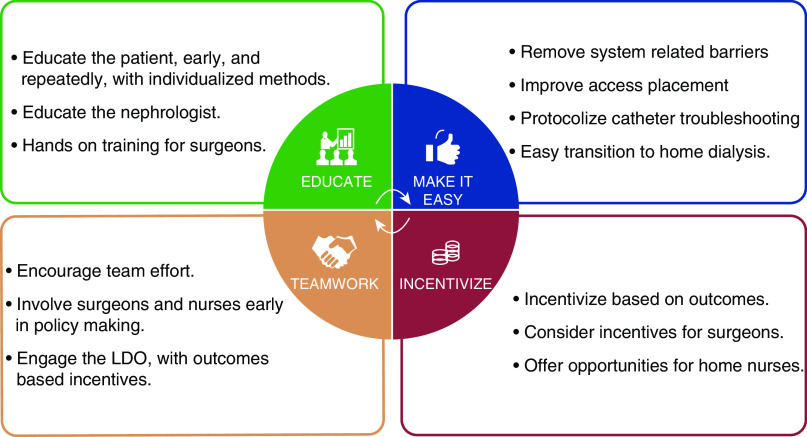
There is a sense of urgency and reignited interest from the authorities in increasing the use of home dialysis modalities. Our goal should be to design an infrastructure where PD and HHD are as easily available to patients as is ICHD: starting from raising awareness and individualized education of patients, seamless and prompt access placement and troubleshooting, adequate and engaged nursing support, and dialysis providers accommodating them at the outpatient unit within 24 hours of access placement. As a nation, we have mastered the ability to place patients ICHD within 24–48 hours; it is time to do the same for home dialysis. Dedicated efforts at curriculum development for nephrologists, along with hands-on training sessions for surgeons and nursing staff, are necessary to provide a good supporting network for this infrastructure. Careful thought has led to incentive models for the nephrologists and dialysis providers, and this should lead the path to a similar consideration for surgeons and radiologists. The collaboration efforts with payers and dialysis providers cannot be overstated, and if the incentives are outcomes based, it is a win-win situation for the patient and dialysis provider (Figure 5). Increased penetration of home modalities will improve patient choice and we owe it to our patients to give them a choice (45).
Figure 5.
Key components to grow a home program.
Disclosures
G. Jain and E. Wallace serve as medical directors at Davita dialysis units. E. Wallace is a consultant for Medtronics, and has received honorariums from Baxter Heathcare, Davita, and Nxstage (educational grant). All remaining authors have nothing to disclose.
Funding
None.
Supplemental Material
This article contains supplemental material online at http://kidney360.asnjournals.org/lookup/suppl/doi:10.34067/KID.0000662019/-/DCSupplemental.
Barriers to home dialysis. Download Supplemental Table 1, PDF file, 90 KB (89.8KB, pdf)
Caveats in pre-dialysis education. Download Supplemental Table 2, PDF file, 90 KB (89.8KB, pdf)
UAB urgent PD protocol. Download Supplemental Table 3, PDF file, 90 KB (89.8KB, pdf)
Acknowledgments
We thank Riya Jain, a high school student at Tara Anglican School in Sydney, Australia for the illustrations and technical assisitance in the manuscript. We would also like to thank our teammates at our home dialysis unit and our access coordinators for helping us take care of patients every day: Chloe Harkins, Natalie Harris, Pamela Myers, Veronica McGee, Ashley Ashe, Shannon Smith, Alicia Dean, Annetris Bates, Mykia Strown, John Wheelock, Carolyn Gancy, Amanda Hunt Jones, Jessie Holmes, Matlie Garner, Erin Estrada, Angela Suggs, and Vicki Brooks. Jane S. Davis is a nurse practitioner in the Division of Nephrology at UAB, and has been leading our dialysis modality education for >10 years.
Author Contributions
M. Ahmad and G. Jain wrote the original draft; G. Jain was responsible for supervision and visualization; and G. Jain and E. Wallace reviewed and edited the manuscript.
References
- 1.Fadem SZ, Walker DR, Abbott G, Friedman AL, Goldman R, Sexton S, Buettner K, Robinson K, Peters TG: Satisfaction with renal replacement therapy and education: The American Association of Kidney Patients survey. Clin J Am Soc Nephrol 6: 605–612, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Biesen W, van der Veer SN, Murphey M, Loblova O, Davies S: Patients’ perceptions of information and education for renal replacement therapy: An independent survey by the European Kidney Patients’ Federation on information and support on renal replacement therapy. PLoS One 9: e103914, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A: Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int 68: 378–390, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Mehrotra R: Peritoneal dialysis education: Challenges and innovation. Semin Dial 31: 107–110, 2018 [DOI] [PubMed] [Google Scholar]
- 5.Valson AT, Asad RA, Radhakrishnan RC, Sinha S, Jacob S, Varughese S, Tamilarasi V: “Why I chose hemodialysis over peritoneal dialysis”: An opinion survey among in-center hemodialysis patients. Perit Dial Int 38: 305–308, 2018 [DOI] [PubMed] [Google Scholar]
- 6.Berns JS: A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol 5: 490–496, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ribitsch W, Haditsch B, Otto R, Schilcher G, Quehenberger F, Roob JM, Rosenkranz AR: Effects of a pre-dialysis patient education program on the relative frequencies of dialysis modalities. Perit Dial Int 33: 367–371, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deber RB, Kraetschmer N, Urowitz S, Sharpe N: Do people want to be autonomous patients? Preferred roles in treatment decision-making in several patient populations. Health Expect 10: 248–258, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goovaerts T, Jadoul M, Goffin E: Influence of a predialysis education program on the choice of renal replacement therapy. Am J Kidney Dis 60: 499–500, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Lacson E Jr., Wang W, DeVries C, Leste K, Hakim RM, Lazarus M, Pulliam J: Effects of a nationwide predialysis educational program on modality choice, vascular access, and patient outcomes. Am J Kidney Dis 58: 235–242, 2011 [DOI] [PubMed] [Google Scholar]
- 11.Wong LP, Liebman SE, Wakefield KA, Messing S: Training of surgeons in peritoneal dialysis catheter placement in the United States: a national survey. Clin J Am Soc Nephrol 5: 1439–1446, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crabtree JH: Who should place peritoneal dialysis catheters? Perit Dial Int 30: 142–150, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Artunc F, Rueb S, Thiel K, Thiel C, Linder K, Baumann D, Bunz H, Muehlbacher T, Mahling M, Sayer M, Petsch M, Guthoff M, Heyne N: Implementation of urgent start peritoneal dialysis reduces hemodialysis catheter use and hospital stay in patients with unplanned dialysis start. Kidney Blood Press Res 44: 1383–1391, 2019 [DOI] [PubMed] [Google Scholar]
- 14.Perakis KE, Stylianou KG, Kyriazis JP, Mavroeidi VN, Katsipi IG, Vardaki EA, Petrakis IG, Stratigis S, Kroustalakis NG, Alegakis AK, Daphnis EK: Long-term complication rates and survival of peritoneal dialysis catheters: The role of percutaneous versus surgical placement. Semin Dial 22: 569–575, 2009 [DOI] [PubMed] [Google Scholar]
- 15.Asif A, Byers P, Gadalean F, Roth D: Peritoneal dialysis underutilization: The impact of an interventional nephrology peritoneal dialysis access program. Semin Dial 16: 266–271, 2003 [DOI] [PubMed] [Google Scholar]
- 16.Asif A, Pflederer TA, Vieira CF, Diego J, Roth D, Agarwal A: Does catheter insertion by nephrologists improve peritoneal dialysis utilization? A multicenter analysis. Semin Dial 18: 157–160, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Goh BL, Ganeshadeva YM, Chew SE, Dalimi MS: Does peritoneal dialysis catheter insertion by interventional nephrologists enhance peritoneal dialysis penetration? Semin Dial 21: 561–566, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Zaman F, Pervez A, Atray NK, Murphy S, Work J, Abreo KD: Fluoroscopy-assisted placement of peritoneal dialysis catheters by nephrologists. Semin Dial 18: 247–251, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Perl J, Pierratos A, Kandasamy G, McCormick BB, Quinn RR, Jain AK, Huang A, Paterson JM, Oliver MJ: Peritoneal dialysis catheter implantation by nephrologists is associated with higher rates of peritoneal dialysis utilization: A population-based study. Nephrol Dial Transplant 30: 301–309, 2015 [DOI] [PubMed] [Google Scholar]
- 20.Ng EK, Goh BL, Chew SE, Tan CC, Ching CH, Sha’ariah MY, Rozina MG: Multicenter analysis on the impact of nephrologist-initiated catheter insertion program on peritoneal dialysis penetration. Semin Dial 25: 569–573, 2012 [DOI] [PubMed] [Google Scholar]
- 21.Finkelstein FO, Ezekiel OO, Raducu R: Development of a peritoneal dialysis program. Blood Purif 31: 121–124, 2011 [DOI] [PubMed] [Google Scholar]
- 22.Yu X, Mehrotra R, Yang X: Components of a successful peritoneal dialysis program. Semin Nephrol 37: 10–16, 2017 [DOI] [PubMed] [Google Scholar]
- 23.Guo A, Mujais S: Patient and technique survival on peritoneal dialysis in the United States: evaluation in large incident cohorts. Kidney Int Suppl 64: S3–S12, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Kolesnyk I, Dekker FW, Boeschoten EW, Krediet RT: Time-dependent reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int 30: 170–177, 2010 [DOI] [PubMed] [Google Scholar]
- 25.Polkinghorne KR: Vascular access, mortality, and home hemodialysis: back to the future. Am J Kidney Dis 67: 176–178, 2016 [DOI] [PubMed] [Google Scholar]
- 26.Greer RC, Ameling JM, Cavanaugh KL, Jaar BG, Grubbs V, Andrews CE, Ephraim P, Powe NR, Lewis J, Umeukeje E, Gimenez L, James S, Boulware LE: Specialist and primary care physicians’ views on barriers to adequate preparation of patients for renal replacement therapy: a qualitative study. BMC Nephrol 16: 37, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arulkumaran N, Navaratnarajah A, Pillay C, Brown W, Duncan N, McLean A, Taube D, Brown EA: Causes and risk factors for acute dialysis initiation among patients with end-stage kidney disease-a large retrospective observational cohort study. Clin Kidney J 12: 550–558, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown PA, Akbari A, Molnar AO, Taran S, Bissonnette J, Sood M, Hiremath S: Factors associated with unplanned dialysis starts in patients followed by nephrologists: a retropective cohort study. PLoS One 10: e0130080, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ivarsen P, Povlsen JV: Can peritoneal dialysis be applied for unplanned initiation of chronic dialysis? Nephrol Dial Transplant 29: 2201–2206, 2014 [DOI] [PubMed] [Google Scholar]
- 30.Nilsson EL: Patients’ experiences of initiating unplanned haemodialysis. J Ren Care 45: 141–150, 2019 [DOI] [PubMed] [Google Scholar]
- 31.Jin H, Ni Z, Che X, Gu L, Zhu M, Yuan J, Huang J, Gu A, Jin Y, Yan H, Wang Q, Yu Z, Zhou W, Fang W: Peritoneal dialysis as an option for unplanned dialysis initiation in patients with end-stage renal disease and diabetes mellitus. Blood Purif 47: 52–57, 2019 [DOI] [PubMed] [Google Scholar]
- 32.Povlsen JV, Sørensen AB, Ivarsen P: Unplanned start on peritoneal dialysis right after PD catheter implantation for older people with end-stage renal disease. Perit Dial Int 35: 622–624, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chiang PC, Hou JJ, Jong IC, Hung PH, Hsiao CY, Ma TL, Hsu YH: Factors associated with the choice of peritoneal dialysis in patients with end-stage renal disease. BioMed Res Int 2016: 5314719, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jin H, Fang W, Zhu M, Yu Z, Fang Y, Yan H, Zhang M, Wang Q, Che X, Xie Y, Huang J, Hu C, Zhang H, Mou S, Ni Z: Urgent-start peritoneal dialysis and hemodialysis in ESRD patients: Complications and outcomes. PLoS One 11: e0166181, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pulliam J, Li NC, Maddux F, Hakim R, Finkelstein FO, Lacson E Jr.: First-year outcomes of incident peritoneal dialysis patients in the United States. Am J Kidney Dis 64: 761–769, 2014 [DOI] [PubMed] [Google Scholar]
- 36.Jaar BG, Plantinga LC, Crews DC, Fink NE, Hebah N, Coresh J, Kliger AS, Powe NR: Timing, causes, predictors and prognosis of switching from peritoneal dialysis to hemodialysis: A prospective study. BMC Nephrol 10: 3, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mari G, Scanziani R, Auricchio S, Crippa J, Maggioni D: Laparoscopic surgery in patients on peritoneal dialysis: A review of the literature. Surg Innov 24: 397–401, 2017 [DOI] [PubMed] [Google Scholar]
- 38.Lew SQ: Peritoneal dialysis immediately after abdominal surgery. Perit Dial Int 38: 5–8, 2018 [DOI] [PubMed] [Google Scholar]
- 39.Kumar VA, Ananthakrishnan S, Rasgon SA, Yan E, Burchette R, Dewar K: Comparing cardiac surgery in peritoneal dialysis and hemodialysis patients: Perioperative outcomes and two-year survival. Perit Dial Int 32: 137–141, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams AJ, Boletis I, Johnson BF, Raftery AT, Cohen GL, Moorhead PJ, el Nahas AM, Brown CB: Tenckhoff catheter replacement or intraperitoneal urokinase: A randomised trial in the management of recurrent continuous ambulatory peritoneal dialysis (CAPD) peritonitis. Perit Dial Int 9: 65–67, 1989 [PubMed] [Google Scholar]
- 41.Lee Y, Chung SW, Park S, Ryu H, Lee H, Kim DK, Joo KW, Ahn C, Lee J, Oh KH: Incremental peritoneal dialysis may be beneficial for preserving residual renal function compared to full-dose peritoneal dialysis. Sci Rep 9: 10105, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Golper TA, Mehrotra R: The intact nephron hypothesis in reverse: an argument to support incremental dialysis. Nephrol Dial Transplant 30: 1602–1604, 2015 [DOI] [PubMed] [Google Scholar]
- 43.Nayak KS, Ronco C, Karopadi AN, Rosner MH: Telemedicine and remote monitoring: supporting the patient on peritoneal dialysis. Perit Dial Int 36: 362–366, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sanabria M, Buitrago G, Lindholm B, Vesga J, Nilsson LG, Yang D, Bunch A, Rivera A: Remote patient monitoring program in automated peritoneal dialysis: impact on hospitalizations. Perit Dial Int 39: 472–478, 2019 [DOI] [PubMed] [Google Scholar]
- 45.Jung HY, Jeon Y, Park Y, Kim YS, Kang SW, Yang CW, Kim NH, Choi JY, Cho JH, Park SH, Kim CD, Kim YL: Better quality of life of peritoneal dialysis compared to hemodialysis over a two-year period after dialysis initiation. Sci Rep 9: 10266, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Barriers to home dialysis. Download Supplemental Table 1, PDF file, 90 KB (89.8KB, pdf)
Caveats in pre-dialysis education. Download Supplemental Table 2, PDF file, 90 KB (89.8KB, pdf)
UAB urgent PD protocol. Download Supplemental Table 3, PDF file, 90 KB (89.8KB, pdf)