Abstract
The COVID-19 outbreak has profoundly affected adolescents' life. Adolescents with pre-existing psychiatric disorders have been at particular risk of increased mental health problems and problematic media use. 178 patients, aged 12–18 years, referred before the COVID-19 outbreak to child and adolescent psychiatry, participated in an anonymous online survey on the impact of the lockdown on media use and mental well-being. The survey was conducted approximately one month after the first easing of restrictions following a six-week lockdown in Switzerland. Based on self-report, half of the patients had been diagnosed with internalizing disorders (ID; depression or anxiety disorder) and the other half with other disorders (non-ID, e.g. ADHD, autistic spectrum disorder). Patients with ID reported higher emotional distress during the lockdown, and a larger number of patients with ID indicated a deterioration of pre-existing symptoms compared to non-ID patients. Although more patients with ID than with non-ID indicated spending a large amount of time on social media, social media time per day in hours was not significantly higher in ID. Patients with ID indicated a higher impact of media use on well-being and mood in everyday life during the lockdown. Social media time was higher in worsened than in improved non-ID patients, while the opposite was found in ID patients, indicating a possible protective effect of media use at least for some ID patients. The results confirm positive as well as negative associations between mental health, emotional well-being and media use for adolescents with ID during the lockdown.
Keywords: Adolescent psychiatry, COVID-19, Internalizing disorder, Lockdown, Problematic use of the internet, Screen media
1. Introduction
The dynamic between the threat of the COVID-19 pandemic itself and its associated confinement measures such as lockdowns and physical distancing imposes greater challenges on the younger population than initially anticipated (Fegert et al., 2020; Green et al., 2021; Guessoum et al., 2020; Holmes et al., 2020; Lee, 2020; Liu et al., 2021; Ozamiz-Etxebarria et al., 2020; Palacio-Ortiz et al., 2020; Racine et al., 2020). Adolescents have been facing a period of insecurity, uncertainty, and anxiety (Buzzi et al., 2020; Duan et al., 2020; Jiao et al., 2020; Mohler-Kuo et al., 2021; Yeasmin et al., 2020; Zhou, 2020), higher levels of stress (Styck et al., 2021; see review by Marques de Miranda et al., 2020) and fears for the future with no definite end to the pandemic in sight (Ellis et al., 2020). Unsurprisingly, cross-sectional studies indicate that adolescents have shown high rates of new-onset internalizing disorders (ID) like depressive (Duan et al., 2020; Magson et al., 2021; Xie et al., 2020) and anxiety disorders (Chen et al., 2020; Duan et al., 2020; Lee, 2020; Torales et al., 2020). Moreover, adolescents with pre-existing psychiatric disorders may encounter greater difficulties in adapting to the present challenges and seem to be more susceptible to an exacerbation of their symptoms (Hawes et al., 2021; Colizzi et al., 2020; Palacio-Ortiz et al., 2020). However, not all pre-COVID psychopathologies are consistently associated with a symptom deterioration. According to the few existing studies in this area, the results are heterogeneous: While some children showed a deterioration of depression, irritability, obsession/ compulsions and hyperactivity others showed also an improvement in depression, anxiety and irritability under lockdown conditions (Bobo et al., 2020; Cost et al., 2021; Lavenne-Collot et al., 2021). The restrictions under lockdown may have provided potential relief, especially for adolescents with pre-existing social anxiety disorder, whereas individuals with other non-ID psychopathologies such as ADHD suffered from the loss of structure and were more likely to present with increased irritability, low mood or increased hyperactivity (Cost et al., 2021; Zhang et al., 2020; Mohler-Kuo et al., 2021). A further factor leading to symptom deterioration may lie in increased stress due to social isolation (Cost et al., 2021; Mohler-Kuo et al., 2021).
1.1. Internalizing disorders and media use
Pre-pandemic studies and meta-analyses revealed potential adverse effects of excessive or problematic internet use (e.g. Iannotti et al., 2009; Livingstone, 2014) associated with behavioral addiction (La Barbera et al., 2009), poor well-being (Richards et al., 2015) or ID (Keles et al., 2020; Maras et al., 2015; Marino et al., 2018; Restrepo et al., 2020). There appears to be a relationship between increased digital technology use and poorer psychiatric outcomes (“digital depression”; Ghaemi, 2020). Teenagers who increased their social media use, video gaming or TV watching, showed more depression and/ or anxiety problems (e.g. Barry et al., 2017; Fardouly et al., 2018; Ohannessian et al., 2021).
As could be expected, screen media time increased during the lockdown both in healthy adolescents (Drouin et al., 2020; López-Bueno et al., 2020; Magson et al., 2021) and in those with pre-existing psychiatric or other disorders (Pietrobelli et al., 2020; Werling et al., 2021), at least temporarily, and in some adolescents, unfavorable developments arose, e.g. excessive online gaming (Balhara et al., 2020; Magson et al., 2021), excessive social media use (Ammar et al., 2020; Burhamah et al., 2020.). During the pandemic, children and adolescents with higher anxiety symptoms increased their consumption of digital and social media to a greater degree than those with lower anxiety levels (Drouin et al., 2020). Reduced levels of depressive symptoms were associated with less internet time (Ellis et al., 2020), and increases of digital media time with higher depressive symptoms or anxiety (Burke et al., 2021). On the other hand, during the pandemic with its societal and recreational restrictions, media use has become an important tool, besides its role in education, for social connectedness, entertainment, distraction and information. The use of digital media may be beneficial to cope with feelings of loneliness, anxiety and stress in general (Hoge et al., 2017; Radovic et al., 2017) or during the pandemic in particular (Burke et al., 2021; Cauberghe et al., 2021; Jiao et al., 2020; Moore et al., 2020; Muzi et al., 2021; Werling et al. 2021; Xiang et al., 2020; Xiao et al., 2021). In adolescents aged 16 years or older, a positive association between anxiety and social media time has been found (Hossain et al., 2020), especially in girls (Hafstad et al., 2021).
The present study aims to investigate the impact of COVID-19 during the spring 2020 lockdown in Switzerland on media behavior and mental well-being in clinically referred adolescents with ID compared to adolescents with other pre-existing psychopathology (non-ID). The following research questions and hypotheses guided our research:
-
-
We intended to investigate whether adolescents with ID and non-ID differed with regard to the amount and impact of media use during the lockdown (self-rated retrospectively). We hypothesized that adolescents with ID would report higher social media time and a higher negative impact of media use on everyday life.
-
-
We hypothesized that the lockdown would have a stronger negative effect on pre-existing symptoms and cause greater emotional distress in adolescents with ID compared to adolescents with other psychopathologies. We expected a higher impact of the lockdown on behavioral problems in non-ID patients.
-
-
The third research question concerned the relation between media use and mental health. We hypothesized that elevated social media time would be associated with a deterioration of the main psychopathological problem. We further assumed that high emotional distress during the lockdown would be associated with a high impact of media use on everyday life and with elevated social media and gaming time.
2. Material and methods
2.1. Recruitment
Patients (aged 12–18 years) who had been treated in outpatient clinics of the Department of Child and Adolescent Psychiatry and Psychotherapy of the University of Zurich in the last two years, were invited via email to participate in the present anonymous online survey. Patients over the age of 14 years were addressed directly, and younger patients were addressed via their parents, who were asked to forward the link to their child. Responses from participants younger or older than the indicated age range or without information on gender, age, or main psychopathological problem were excluded. The study was conducted in accordance with the principles of the Declaration of Helsinki and in agreement with the local ethics committee.
2.2. Context
Data collection started on May 30th and was completed on 4th July 2020. In Switzerland, a complete lockdown with school closure – the only one so far – lasted from March 16th to the end of April 2020. From May 11th onwards, the first schools reopened. At the time of the survey, the majority of students had returned to class just now, albeit often with reduced onsite hours.
2.3. Instruments
Media-related items were based on a modified version of the Screening Questionnaire for Problematic Use of the Internet (PUI-SQ) for children and adolescents referred to child and adolescent psychiatry (Werling et al., 2021a, 2021b). The PUI-SQ comprises the following subscales/domains: 1. Self-evaluation of frequent media use (five items), 2. Leisure media time per day (six items), 3. Impact of media use on everyday life (five items), 4. Addictive tendencies (four items), 5. Risks and problem behaviors on the internet (six items). All items were rated on 4-point Likert scales, except for Leisure media time per day, which was rated on a 5-point Likert scale (no time at all, <1 hrs, 1–3 hrs, 4–6 hrs, >6 hrs). For further analyses, the mean of each time range was used as an estimate of mean media time (0 hrs, 0.5 hrs, 2 hrs, 5 hrs, 7 hrs). With the exception of the Risks and problem behaviors subscale, each item had to be rated in relation to three time points: retrospectively before the COVID-19 outbreak (January 2020), during the lockdown (March/ April 2020), and regarding the current situation (last two weeks).
To assess demographic characteristics, main psychopathology, emotional distress, behavioral problems, and worry, we used items from the European collaboration study on the impact of COVID-19 on children and adolescents with pre-existing mental health problems (CRISIS) of the ECNP group (Coghill et al., unpublished, Nikolaidis et al., 2021). Patients rated items relating to their mood, mental well-being and behavioral problems during the lockdown and the last two weeks on 5-point-Likert scales. An emotional distress subscale score was established using five items on sadness, exhaustion/fatigue, enjoyment of activities, anxiousness, and irritability. The behavioral problems subscale comprised four items: inattention/concentration, hyperactivity, physical aggressiveness, and overall behavioral problems. The classification of items into an emotional and behavioural score is based, with slight modifications, on the factor analysis of a large English sample (E. Simonoff, personal communication) and on a study recently published by Stevanovic and colleagues (Stevanovic et al., 2022). The psychopathological self-assessment was based on an item where patients had to indicate their main psychopathological problem by selecting one out of eight disorders or alternately by writing their main problem and possible comments into a text field. In the next item, patients were asked whether this problem had changed during the lockdown.
2.4. Statistics
On the item level, the ID and non-ID groups were compared using Chi2 tests. Repeated measures MANOVAs with group as between subject variable were used to compared subscale scores over two or three assessment times, with planned contrasts. Age as covariate was tentatively included but did not yield significant effects and was therefore dropped. ANOVA was used to calculate differences in social media time per day between subgroups with improved or deteriorated main psychopathology. Two multiple regression analyses were calculated separately for the ID and non-ID patient groups. All four PUI-SQ subscales and six media time per day scores (two activities, four devices) were entered into the analysis with a) the emotional distress score and b) the behavioral problems score as dependent variables.
3. Results
3.1. Sample description
Due to the low number of younger patients, which precluded the analysis of separate age groups as in our previous study (lockdown survey conducted with parents of patients; Werling et al., 2021b), we decided to eliminate patients under 12 and over 18 years from our sample of N = 226 patients in order to obtain a more homogeneous sample. Categorization into ID or non-ID was based on the category of the main problem selected by the patients; free text self-assessments were categorized by agreement between the first and last author. Female patients were largely overrepresented in the ID group. To achieve a better match, we also eliminated the six youngest male patients with non-ID, meaning that N = 89 non-ID patients and N = 89 ID patients were ultimately included in the analysis. In the final sample, a small age difference remained between ID and non-ID, but gender differences were not significant (Table 1 ). In the non-ID group, only one patient indicated “gaming” as main psychopathological problem (included in the category “other”, Table 1).
Table 1.
Description of the sample.
| Internalizing disorders (ID) | Other disorders (non-ID) | p | |
|---|---|---|---|
| Total N | 89 | 89 | |
| Age mean (years) (SD) | 15.7 (1.5) | 15.2 (1.7) | 0.024 |
| Age range (years) | 12–18 | 12–18 | |
| Gender ratio male/female/other | 14/69/6 | 23/56/10 | n.s. |
| Main psychopathology subgroups (N) % | Depression (59) 60% Anxiety disorder (30) 33% |
Autism spectrum disorder (22) 25% | |
| Eating disorder (15) 17% | |||
| ADHD (15) 17% | |||
| Gender conditions (10) 11% | |||
| Borderline (7) 8% | |||
| Other (20) 22% | |||
| Frequency of online home-schooling during the lockdown | Never/rarely 27% | Never/rarely 20% | n.s. |
| Sometimes 15% | Sometimes 19% | ||
| Often/always 58% | Often/always 61% |
3.2. Media use-related behaviors
3.2.1. Frequent leisure media use before, during and after lockdown
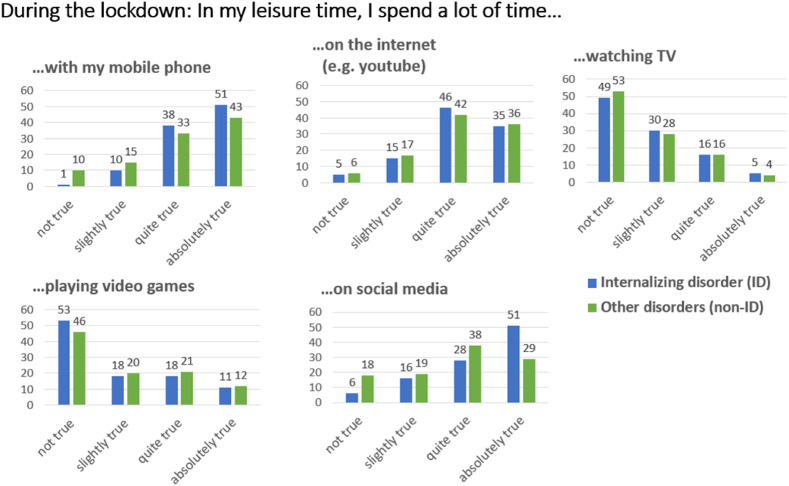
During the lockdown, more patients with ID than with non-ID disorders agreed with the statement that they spend a lot of time on their mobile phone and on social media. While in both groups, a large proportion of patients reported spending a lot of time on the internet (ID 35%, non-ID 36%), only a minority indicated frequent TV watching (ID 5%, non-ID 4%) or frequent video gaming (ID 11%, non-ID 12%) (Fig. 1 ). On item level, more ID than non-ID patients reported frequent social media use at all three time points before (Chi2 = 8.942; p < 0.030), during (Chi2 = 11.591; p < 0.009, and after the lockdown (Chi2 = 10.445; p < 0.015), while higher mobile use was only significant during the lockdown (Chi2 = 8.114; p < 0.24). On the subscale level, both groups of patients reported more frequent media use during the lockdown than before (Table 4). This increase appeared to be higher in the ID group but group differences were not statistically significant.
Fig. 1.
Frequent leisure media use during the lockdown related to different activities or devices in patients with ID and non-ID (percent of responses).
Table 4.
PUI-SQ subscales, emotional distress and behavioral problems scale scores before, during, and after lockdown.
| Before Lockdown |
Post hoc | Lockdown |
Post hoc | Last two weeks |
Post hoc | MANOVA, contrasts | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subscale scores | ID Mean (SD) |
Non-ID (mean SD) | ID Mean (SD) |
Non-ID (mean SD) | ID Mean (SD) |
Non-ID (mean SD) | ||||
| PUI-SQ | ||||||||||
| 1. Frequent media use | 10.98 (2.44) | 10.83 (2.94) | 13.40 (2.36) | 12.60 (3.15) | 11.97 (2.75) | 11.44 (3.07) | Time: F2/175 = 76.513*** Time by group: n.s. Group: n.s. T1<T2; T2>T3; T3>T1 |
|||
| 2. Impact on everyday life | 8.89 (2.62) | 8.10 (2.53) | p < 0.043 | 10.08 (2.99) | 9.07 (3.10) | p < 0.028 | 9.40 (2.79) | 8.46 (3.01) | p < 0.081 | Time: F 2/175 = 21.859*** Time by group: n.s. Group: F = 7752* T1<T2; T2>T3; T3>T1 |
| 3. Addictive tendencies | 6.62 (2.11) | 6.63 (2.34) | 7.12 (2.46) | 7.06 (2.52) | 6.48 (2.21) | 6.75 (2.52) | Time F 2/175 = 12.450*** Time by group: n.s. Group: n.s. T1<T2; T2>T3; T3 = T1 |
|||
| 4. Internet risk and problem behaviors | 5.70 (1.30) | 6.00 (1.69) | 5.75 (1.36) | 5.921 (1.62) | Time: n.s. Time by group: n.s. Group: n.s. |
|||||
| Emotion and behavior (based on CRISIS items) | ||||||||||
| Emotional distress | 16.53 (4.29) | 14.54 (5.41) | p < 0.003 | 16.48 (4,28) | 14.46 (4.28) | p < 0.001 | Time: n.s.; time by group: n.s. Group: F = 12.600*** |
|||
| Behavioral problems | 10.84 (2.85) | 9.92 (2.71) | p < 0.030 | 10.84 (2.97) | 10.17 (2.67) | n.s. | Time: n.s.; time by group: n.s.; Group: F = 4.412* |
|||
Note. PUI-SQ = Screening Questionnaire for Problematic Use of the Internet. ID = internalizing disorders; non-ID = non-internalizing disorders. T1 = before Lockdown, T2 = Lockdown; T3 = last 2 weeks. n.s. = non significant. *** = p < 0.001; * = p < 0.05.
3.2.2. Leisure time per day on screen media activities and devices
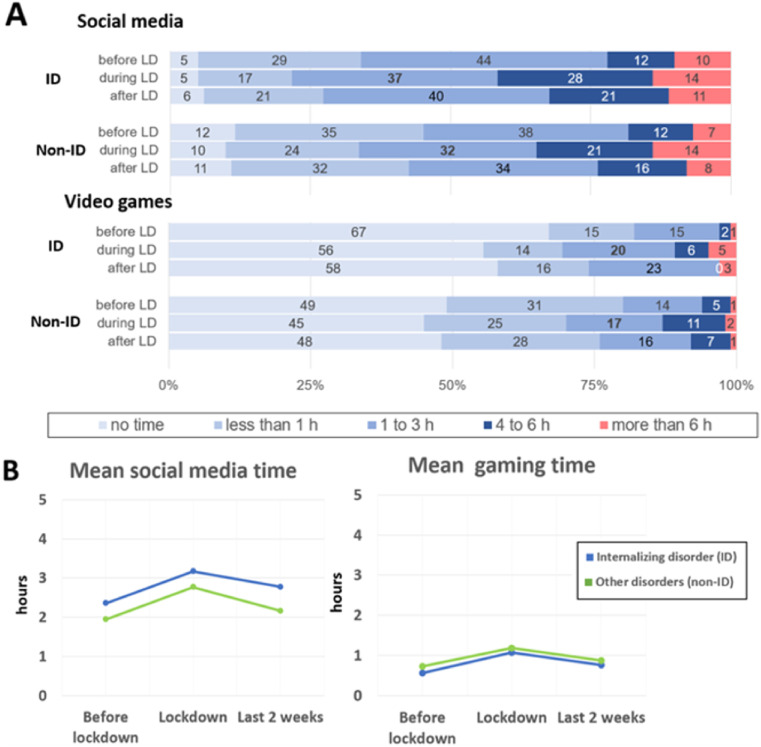
Patients with ID did not differ from non-ID patients in time per day spent on social media, either before, during or after the lockdown (Fig. 2 B). During the lockdown, 42% of ID patients and 35% of non-ID patients indicated having spent more than 4 h per day on social media, and 14% of each group reported more than 6 h (Fig. 2A). Across-time analysis of social media time per day revealed no significant group difference or group by time interaction. Mean social media time increased from pre-lockdown to lockdown and decreased thereafter but did not return to pre-COVID values (Fig. 2B). The majority of ID patients (67%) and about half of non-ID patients (49%) indicated that before the lockdown, they did not play video games on a daily basis, and this remained the case for 56% of ID patients and 46% of non-ID patients during the lockdown. On the item level, time spent on video gaming did not significantly differ between the two groups (Fig. 2 A). Across-time analyses of mean time scores did not reveal significant group differences or time by group interactions (Fig. 2B).
Fig. 2.
A) Time per day (percent of responses) and B) mean time per day spent on social media and video games before, during and after the lockdown in patients with internalizing disorders (ID) and other psychiatric disorders (non-ID). Note. A) None of the group comparisons on item level was significant. B) MANOVA social media mean time per day: time effects F2/175 = 22.321***; group by time: n.s.; group effects: n.s., time contrasts: T1 < T2, T2 >T3, T1<T3. MANOVA gaming mean time per day: time effect F2/175 = 17.169***; time by group n.s.; group effects n.s.; time contrasts T1<T2; T2>T3, T3>T1. T1 = before Lockdown, T2 = Lockdown; T3 = last 2 weeks. LD = Lockdown, n.s. = non significant, *** = p < 0.001.
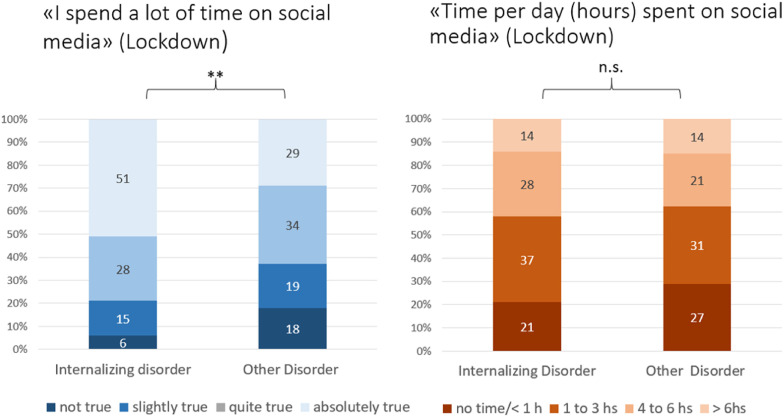
Interestingly, the higher social media use indicated by ID patients when the item was formulated in general terms, was not reflected in the reported social media time per day during the lockdown (Fig. 3 ). What is meant by spending “a lot of time” on social media seems to be interpreted somewhat differently in the two groups.
Fig. 3.
Media time general statement vs. indication of media hours per day spent on social media in patients with internalizing disorder (ID) and other disorders (non-ID).
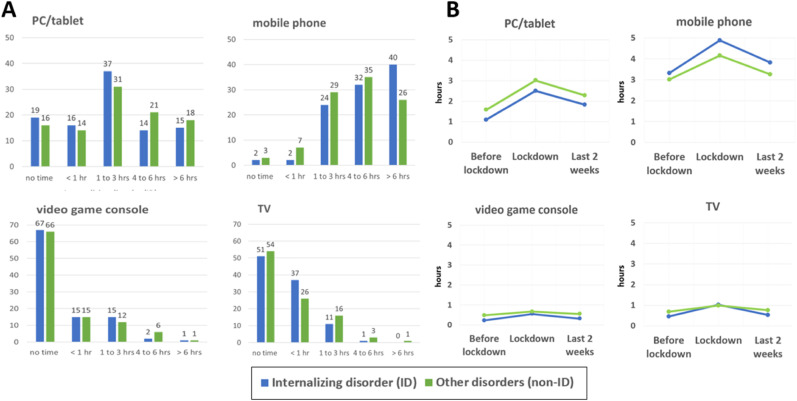
With regard to different media devices, the mobile phone proved to be the most frequently used device by both groups, followed by PC/tablet, TV and video game console. Even during the lockdown, the latter two were only used by the minority of participants and only to a very small extent (Fig. 4 A). Analyses of items or mean time of use showed neither group differences nor interaction effects. Mobile usage time did not differ between ID and non-ID during the lockdown on the item level (Chi2 = 5.749; p < 0.219, Fig. 4A) but repeated measures analyses revealed a trend for group differences (p < 0.059), with an overall longer mean time of use in ID. For all devices, mean media time significantly increased from pre-COVID to lockdown, and decreased from lockdown to the last two weeks. PC/tablet use after the lockdown remained higher than before the pandemic (p < 0.001) (Fig. 4B).
Fig. 4.
Media time per day (hours) on different devices in patients with internalizing disorders (ID) and other disorders (non-ID) (A) during the lockdown and (B) mean time of use per day (hours) before COVID-1), during the lockdown and in the last 2 weeks. Note. A) None of the group comparisons on item level was significant. B) MANOVA PC/tablet: time F2/175 = 46.870***; time by group n.s.; group effect n.s.; time contrasts T1<T2, T2>T3, T1<T3. MANOVA mobile phone: time F2/175 = 43.001***; time by group effect n.s.; group effect F = 3.605, p < 0.059°; time contrasts: T1<T2; T2>T3; T1<T3. MANOVA video game console: time F2/175 = 6.887***; time by group effect n.s.; group effect n.s.; time contrasts: T1<T2, T2>T3, T1 = T3. MANOVA TV: time F 2/175 = 14.318***; time by group n.s.; group effect n.s.; time contrasts: T1<T2; T2>T3; T1 = T3. T1 = before Lockdown, T2 = Lockdown; T3 = last 2 weeks. n.s. = non significant, *** = p < 0.001, ° = p < 0.10.
3.2.3. Impact of media use on everyday life
A significant difference between groups emerged on the item level regarding the impact of media on mood and well-being during the lockdown, and a trend emerged regarding the impact on friendships, with a higher impact in ID patients (Table 2 ). On the subscale level, ID patients scored higher compared to non-ID (Table 4). On the item level, we found one significant difference between ID and non-ID on the Addictive tendencies subscale, namely on the item referring to unsuccessful attempts to reduce media time (Table 2). However, the Addictive tendencies subscale scores did not significantly differ between the two groups. In general, Addictive tendencies subscale scores were low (Table 4).
Table 2.
Impact on everyday life subscale and Addictive tendencies subscale during the lockdown in patients with internalizing disorders (ID) and other disorders (non-ID) (percent of responses).
| Not true | Slightly true | Quite true | Absolutely true | Chi2 | p | ||
|---|---|---|---|---|---|---|---|
| Impact on everyday life | |||||||
| My media use … | |||||||
| … leads to problems and arguments with my parents | ID | 56% | 23% | 17% | 2% | 2.175 | 0.537 |
| Non-ID | 54% | 26% | 19% | 1% | |||
| ..does not leave enough time for homework and affects academic achievements | ID | 48% | 21% | 21% | 9% | 3.856 | 0.277 |
| Non-ID | 52% | 28% | 11% | 8% | |||
| … negatively affects friendships and real life activities | ID | 72% | 8% | 13% | 7% | 7.312 | 0.063 |
| Non-ID | 68% | 20% | 7% | 5% | |||
| …. affects my mood and mental well-being (e. g. can make me feel happy, stressed, aggressive or sad) | ID | 13% | 28% | 37% | 21% | 12.218 | 0.007 |
| Non-ID | 24% | 44% | 19% | 13% | |||
| … affects my physical health and well-being (e.g. sleep, feeling tense) | ID | 26% | 35% | 25% | 15% | 4.551 | 0.208 |
| Non-ID | 39% | 34% | 17% | 10% | |||
| Addictive tendencies | |||||||
| I have become very angry/aggressive when media use was constricted (e.g. by my parents) | ID | 48% | 32% | 8% | 12% | 0.721 | 0.868 |
| Non-ID | 52% | 28% | 10% | 10% | |||
| I tried to reduce the time spent on gaming, the internet or my mobile, but did not succeed. | ID | 48% | 31% | 16% | 5% | 9.004 | 0.029 |
| Non-ID | 43% | 44% | 4% | 9% | |||
| I felt stressed without access to my mobile (or gaming/or internet) and could not think of anything else. | ID | 48% | 32% | 12% | 8% | 5.169 | 0.169 |
| Non-ID | 64% | 25% | 8% | 3% | |||
| I have secretly spent more time with media than agreed upon. | ID | 55% | 25% | 14% | 7% | 4.846 | 0.183 |
| Non-ID | 47% | 26% | 10% | 17% | |||
Risks and problem behaviors were very rarely reported by both patients with ID and non-ID. No significant differences were found between patient groups on the item level (Table 3). Approximately 10% more non-ID patients frequented problematic chat groups compared to non-ID patients, but this difference was not significant. There was also no significant difference between the patient groups on the subscale score level or across time.
Table 3.
Results for the subscale Risks and problem behaviors on the internet during the lockdown in patients with ID and non-ID (percent of responses).
| I have … | Not true | Slightly true | Quite true | Absolutely true | ||
|---|---|---|---|---|---|---|
| …. been a victim of cyberbullying | ID | 89% | 9% | 2% | 0% | n.s. |
| Non-ID | 92% | 7% | 1% | 0% | ||
| … been a cyberbullying offender | ID | 98% | 1% | 1% | 0% | n.s. |
| non-ID | 95% | 5% | 0% | 0% | ||
| … uploaded private data on the internet (e.g. personnel data, pictures of me scantily dressed) | ID | 89% | 7% | 1% | 3% | n.s. |
| non-ID | 87% | 10% | 1% | 2% | ||
| … played video games with harmful content or not allowed for my age (e.g. glorifying violence) | ID | 86% | 6% | 6% | 2% | n.s. |
| non-ID | 77% | 9% | 6% | 8% | ||
| … visited problematic chatrooms/chat groups my parents should not know about | ID | 88% | 10% | 0% | 1% | p < 0.080 |
| non-ID | 80% | 10% | 7% | 3% | ||
| … illegally downloaded or downloaded or distributed prohibited content | ID | 83% | 10% | 5% | 2% | n.s. |
| non-ID | 82% | 11% | 6% | 1% |
3.3. Pre-existing symptoms, emotional distress and behavioral problems
3.3.1. Improvement or deterioration of psychopathological condition
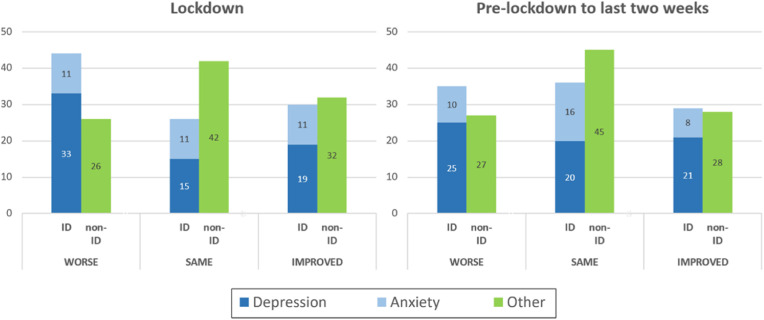
Of the ID patients, 44% reported a deterioration of the main psychopathological problem and 30% an improvement; of the non-ID group 26% reported a deterioration and 32% an improvement (based on the CRISIS item on changes of the main psychopathological problem). These group differences were significant (Chi2 = 7.408; p < 0.025). Thus, in contrast to non-ID patients, the majority of ID patients showed a deterioration of problems, which was evidently due to a higher number of depressed patients with worsened symptoms, while in patients with anxiety disorder, improvement and deterioration were equally distributed (Fig. 5 ). After lockdown, group differences were no longer significant (Chi2 = 2.252, p < 0.324).
Fig. 5.
Changed severity of the main psychopathological problem during the lockdown and from pre-COVID to the last two weeks (percent of responses) in patients with internalizing disorders (ID) and other disorders (non-ID).
3.3.2. Emotional distress and behavioral problems
More patients with ID compared to non-ID indicated greater emotional distress on items related to sadness (Chi2 = 11.234, p < 0.023) and irritability (Chi2 = 10.850, p < 0.0028) during the lockdown. On items related to behavioral problems, more ID patients reported problems concerning concentration/attention (Chi2 = 9.437, p < 0.051) and overall behavioral problems (Chi2 = 12.521, p < 0.014) during the lockdown. On the subscale level, patients with ID scored higher on the emotional distress as well as on the behavioral problems subscale during the lockdown and on the emotional distress subscale in the last 2 weeks. Across time comparison revealed no significant changes (Table 4).
3.3.3. General worry and fear of infection
Three items from the CRISIS questionnaire were related to general worry and to fear that oneself or family and friends might become infected. None of these items differentiated between ID and non-ID. Most adolescents reported mild to moderate worry under lockdown. About 25% indicated major general concern, 35% were quite or very worried that family or friends might be infected, and only 11% strongly worried about themselves.
3.4. Relation between media use and mental health under lockdown
When we investigated the relation between social media time per day and changes in severity of the main psychopathological problem in ID and non-ID, a significant interaction (F = 3.638, p < 0.028) was detected. While in non-ID patients, a deterioration of problems was associated with high social media time (mean 4.14 h, SD 2.37), the opposite was observed in ID: The highest mean social media time, almost 4 h per day (mean 3.83 h, SD 2.43), was found in the ID subgroup with an improvement of psychopathology (Fig. 6 ).
Fig. 6.
Social media time per day (hrs) during the lockdown in subgroups of patients with ID and other disorders (non-ID) with improvement, no change or deterioration of the main psychopathological problem. Note. Unequal group sizes: worse: ID n = 39, non-ID n = 23; same: ID n = 23, non-ID n = 38; better: ID n = 27, non-ID n = 28.
In ID patients, multiple regression analyses revealed significant associations between emotional distress and the Everyday life impact score, and an inverse relation between emotional distress and mean gaming time and Addictive tendencies. The behavioral problems score was related to Everyday life impact and inversely related to mobile time per day (Table 5 ; A, B). In non-ID patients, the emotional distress score was related to the Everyday life impact score, to the Risks and problems score and to TV time per day. Moreover, the behavioral problems score was related to the Everyday life impact score and to the Risks and problem behaviors score (Table 5; C, D).
Table 5.
Multiple regression analyses among variables influencing A) the emotional distress score, and B) behavioral problems score under lockdown in patients with internalizing disorders and C) emotional distress score and D) behavioral problems score in patients with other disorders (non-ID).
| Internalizing Disorders (N = 89) | ||||||
| A. Emotional distress | ||||||
| Independent variable | SE | Beta | T | P | ||
| Everyday life impact | 0.152 | 0.553 | 5.213 | <0.001 | F = 13.690*** R2 = 0.326 Adjusted R2 = 0.302 |
|
| Mean gaming time | 0.210 | -0.310 | −3.465 | <0.001 | ||
| Addictive tendencies | 0.185 | -0.226 | −2.129 | 0.36 | ||
| B. Behavioral problems | ||||||
| Independent variable | SE | Beta | T | P | ||
| Everyday life impact | 0.092 | 0.493 | 5.100 | <0.001 | F = 13.461*** | |
| Mean mobile time | 0.126 | -0.200 | −2.074 | 0.041 | R2 = 0.238 | |
| Adjusted R2 = 0.221 | ||||||
| Other Disorders (non-internalizing) (N = 89) | ||||||
| C. Emotional distress | ||||||
| Independent variable | SE | Beta | T | P | ||
| Everyday life impact | 0.128 | 0.405 | 4.605 | <0.001 | F = 16.170*** | |
| Internet risks and problems | 0.244 | 0.262 | 2.974 | 0.004 | R2 = 0.363 | |
| Mean TV time | 0.258 | 0.244 | 2.776 | 0.007 | Adjusted R2 = 0.341 | |
| D. Behavioral problems | ||||||
| Independent variable | SE | Beta | T | P | ||
| Everyday life impact | 0.082 | 0.453 | 4.740 | <0.001 | F = 18.881*** R2 = 0.305 Adjusted R2 = 0.289 |
|
| Internet risks and problems | 0.148 | 0.351 | 3.515 | <0.001 | ||
Note. Only variables remaining in the models are listed.
4. Discussion
The analysis of the responses from adolescent patients with ID compared to patients with other psychiatric disorders revealed several significant and clinically relevant differences. As expected, female patients were largely overrepresented, in line with data on higher prevalence of girls among adolescent patients with depression (Salk et al., 2017) or anxiety disorder (Essau et al., 2018). Patients with ID reported high social media consumption more frequently compared to non-ID patients when the question was formulated as a general statement. However, when asked to indicate social media time in hours, the group differences were not significant. In addition, patients with ID indicated a high usage of their mobile phone more often than those with non-ID. In this regard, at least a trend regarding the time per day spent on mobile phones was found, with higher means in ID patients. Nevertheless, this remained the only difference between groups in terms of media hours per day during the lockdown. Thus, one main difference between the groups may be seen in a differing evaluation of their media use. The importance of the subjective component is also reflected in a further group difference: Compared to non-ID patients, adolescents with ID reported a higher negative impact of their media use on everyday life, with the groups predominantly differing above all in their assessment of the influence of media on their mood and mental well-being. Addictive tendencies did not differentiate between the groups on the subscale level, while on the item level, ID patients more often reported unsuccessful attempts to reduce their media time. Risks and problem behaviors related to the internet were reported by a very small proportion of ID as well as non-ID patients and did not differentiate between the groups. Media-related subscale scores generally increased from pre-COVID to the lockdown, and subsequently decreased from lockdown to the last two weeks, but often did not return to pre-COVID-values. One might be tempted to interpret this as a sign of a permanent increase due to habituation, but it should also be kept in mind that at this time, “normal life” had not yet resumed.
As expected, more patients with ID compared to non-ID indicated a self-estimated deterioration of the main psychopathological problem during the lockdown. This confirms earlier reports of a particular burden of the lockdown on patients with depression and anxiety (Hawes et al., 2021). After the easing of measures, the two groups seem to have converged again in terms of symptom severity. Patients with ID indicated stronger emotional distress under lockdown, but as the two groups did not differ in terms of general worry or fear of being infected, this difference appears to be related rather to a greater vulnerability and differences in the ability to cope with confinement. Patients with ID scored higher on items related to emotions such as sadness and irritability, and on behavioral items related to concentration or general behavioral problems (comprising attentional problems, hyperactivity, etc.). Thus, upon closer inspection of the item content, the unexpected stronger behavioral problems on items that were originally aimed at externalizing disorders may equally be seen as characteristic effects of depression or anxiety.
Finally, we found interesting and in part differential interactions between media-related behavior, changes in the severity of psychopathological problems and emotional distress during the lockdown. While in non-ID patients, the highest social media time was associated with a worsening of symptoms, in patients with ID, the highest social media time was found in the subgroup with improved symptoms. One possible interpretation of these findings is that the use of social media seems to have rather beneficial effects on some ID patients, but rarely on non-ID patients. This complements earlier literature suggesting that social media use fulfils an important coping function in some patients, but has a detrimental effect on others (Liu et al., 2016; Riehm et al., 2019; Twenge et al., 2018). In ID and non-ID patients, the impact of media use on everyday life strongly predicted emotional distress and behavioral problems. Those patients who indicated a strong effect of media on their family life, school, and physical or mental well-being also indicated higher emotional distress and behavioral problems. In patients with ID, emotional distress was additionally inversely related to gaming time and addictive tendencies. Possibly, in times with unlimited access to media, patients with pre-existing PUI addictive tendencies benefitted from the opportunity to game at will, which is reflected by higher gaming time and lower emotional distress. Behavioral problems were inversely related to mean mobile time which supports the above interpretation that higher media time in ID is related to stress relief and lower emotional distress. One has, however, to keep in mind that all data are self-assessed and that the relation between media time and emotional distress may be assessed completely differently from the parents' point of view.
In non-ID patients we found an association between emotional distress, internet related risks and problem behaviors and TV consumption. Compared to other media, TV is non-interactive, and those who watched more TV were possibly more solitary or bored or unable to engage in a more social activity. A higher degree of internet risks or problem behaviors would have been expected in a patient group that also includes externalizing disorders. However, the only differential trend among items of this subscale was related to harmful chat groups, which one would rather associate with, for example, eating disorders (Mento et al., 2021). All items from the internet related risks or problems subscale may have contributed in differential ways to enhanced emotional distress and behavioral problems in this heterogeneous clinical group and in consequence no clear pattern emerged.
5. Limitations
The first limitation, linked to the anonymous data collection, is that all diagnoses are based on self-reports. Also, possible comorbidity and severity of disorders were not taken into account. Moreover, data relating to pre-COVID and lockdown states were gathered retrospectively and may thus be subject to bias. To a certain degree, the data reflect patients' perspective on events, behaviors and feelings considered at a very specific point in time of the pandemic, namely one month after experiencing a complete lockdown of six weeks. The sample is rather small compared to other pandemic-related surveys, at least too small to allow for meaningful comparison between subgroups with depression and anxiety, and the non-ID group was heterogeneous. Also, the non-ID group corresponds to a clinical control but cannot be considered as representative for clinically referred non-ID disorders, as the willingness and ability to participate in an anonymous online survey may differ between disorders and according to age and gender.
6. Conclusion
The present findings revealed that the lockdown had stronger adverse effects on both mental well-being and pre-existing psychopathology in patients with ID compared to other psychiatric disorders. Patients with ID reported a higher subjective importance of media use for their mental well-being, and high social media time evidently had a protective function at least for some ID patients. We conclude that in patients with ID, high media use does not always correspond to worsening of symptoms and that not only the duration but also the function of media use should be considered in a differentiated way for each individual case. While these results relate to the effects of the lockdown experience in spring 2020, the ongoing pandemic and social containment measures still threaten to exacerbate symptoms in adolescents with pre-existing psychiatric disorders and may increase media use as a functional or dysfunctional coping mechanism (Király et al., 2020). Further investigations are needed to assess the long-term impact and to compare with other sources, such as informant-reported data.
Authors' contributions
All authors contributed substantially to the conception and design of the study. AW und RD were involved in the acquisition and analysis of the data. AW, SW, EG, MG and RD participated in the interpretation of the data. AW, MG and RD drafted the paper. All authors critically revised the manuscript and gave final approval for the submission.
Declaration of competing interest
SW has received in the last 5 years royalties from Thieme Hogrefe, Kohlhammer, Springer, Beltz. Her work was supported in the last 5 years by the Swiss National Science Foundation (SNF), diff. EU FP7s, Bfarm Germany, ZInEP, Hartmann Müller Stiftung, Olga Mayenfisch, Gertrud Thalmann, Vontobel, Unicentia, Erika Schwarz Fonds. Outside professional activities and interests are declared under the link of the University of Zurich www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/. RD has received royalties from Hogrefe and her work has been supported by the SNF in the last 5 years. The other authors declare no conflict of interest.
Acknowledgments
The authors thank all adolescents and their families for their participation, and the support and collaboration of the colleagues from the outpatient and special units of the Department of Child and Adolescent Psychiatry and Psychotherapy, Zurich. Additionally, the authors appreciate the support and collaboration of the European Network for Problematic Usage of the Internet of the COST Action CA16207 (European Cooperation in Science and Technology) and the COVID research group of the ECNP Child and Adolescent Psychopharmacology Network.
References
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., Müller P., Müller N., Aloui A., Hammouda O., Paineiras-Domingos L.L., Braakman-Jansen A., Wrede C., Bastoni S., Pernambuco C.S., Mataruna L., Taheri M., Irandoust K., Khacharem A., Bragazzi N.L., Chamari K., Glenn J.M., Bott N.T., Gargouri F., Chaari L., Batatia H., Ali G.M., Abdelkarim O., Jarraya M., El Abed K., Souissi N., Van Gemert-Pijnen L., Riemann B.L., Riemann L., Moalla W., Gómez-Raja J., Epstein M., Sanderman R., Schulz S.V.W., Jerg A., Al-Horani R., Mansi T., Jmail M., Barbosa F., Ferreira-Santos F., Šimunič B., Pišot R., Gaggioli A., Bailey S.J., Steinacker J.M., Driss T., Hoekelmann A. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12 doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balhara Y.P.S., Kattula D., Singh S., Chukkali S., Bhargava R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J. Publ. Health. 2020;64:S172–S176. doi: 10.4103/ijph.IJPH_465_20. [DOI] [PubMed] [Google Scholar]
- La Barbera D., La Paglia F., Valsavoia R. Studies in Health Technology and Informatics. IOS Press; 2009. Social network and addiction; pp. 33–36. [DOI] [PubMed] [Google Scholar]
- Barry C.T., Sidoti C.L., Briggs S.M., Reiter S.R., Lindsey R.A. Adolescent social media use and mental health from adolescent and parent perspectives. J. Adolesc. 2017;61:1–11. doi: 10.1016/j.adolescence.2017.08.005. [DOI] [PubMed] [Google Scholar]
- Bobo E., Lin L., Acquaviva E., Caci H., Franc N., Gamon L., Picot M.C., Pupier F., Speranza M., Falissard B., Purper-Ouakil D. How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale. 2020;46:S85. doi: 10.1016/j.encep.2020.05.011. –S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhamah W., AlKhayyat A., Oroszlányová M., AlKenane A., Almansouri A., Behbehani M., Karimi N., Jafar H., AlSuwaidan M. The psychological burden of the COVID-19 pandemic and associated lockdown measures: experience from 4000 participants. J. Affect. Disord. 2020;277:977–985. doi: 10.1016/j.jad.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke T.A., Kutok E.R., Dunsiger S., Nugent N.R., Patena J.V., Riese A., Ranney M.L. A national snapshot of U.S. adolescents' mental health and changing technology use during COVID-19. Gen. Hosp. Psychiatr. 2021 doi: 10.1016/j.genhosppsych.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzzi C., Tucci M., Ciprandi R., Brambilla I., Caimmi S., Ciprandi G., Marseglia G.L. The psycho-social effects of COVID-19 on Italian adolescents' attitudes and behaviors. Ital. J. Pediatr. 2020;46 doi: 10.1186/s13052-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauberghe V., Van Wesenbeeck I., De Jans S., Hudders L., Ponnet K. How adolescents use social media to cope with feelings of loneliness and anxiety during COVID-19 lockdown. Cyberpsychol., Behav. Soc. Netw. 2021;24:250–257. doi: 10.1089/cyber.2020.0478. [DOI] [PubMed] [Google Scholar]
- Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. 2020. Depression and Anxiety Among Adolescents during COVID-19: A Cross-Sectional Study. Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coghill, D.R., unpublished. The European COVID-19vIruS Health Impact Survey 3.2 (CRISIS).
- Cost K.T., Crosbie J., Anagnostou E., Birken C.S., Charach A., Monga S., Kelley E., Nicolson R., Maguire J.L., Burton C.L., Schachar R.J., Arnold P.D., Korczak D.J. 2021. Mostly Worse, Occasionally Better: Impact of COVID-19 Pandemic on the Mental Health of Canadian Children and Adolescents. European Child and Adolescent Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drouin M., McDaniel B.T., Pater J., Toscos T. How parents and their children used social media and technology at the beginning of the COVID-19 pandemic and associations with anxiety. Cyberpsychol., Behav. Soc. Netw. 2020;23:727–736. doi: 10.1089/cyber.2020.0284. [DOI] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. 2020;52:177–187. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- Essau C.A., Lewinsohn P.M., Lim J.X., Ho M., ho R., Rohde P. Incidence, recurrence and comorbidity of anxiety disorders in four major developmental stages. J. Affect. Disord. 2018;228:248–253. doi: 10.1016/j.jad.2017.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fardouly J., Magson N.R., Johnco C.J., Oar E.L., Rapee R.M. Parental control of the time preadolescents spend on social media: links with preadolescents' social media appearance comparisons and mental health. J. Youth Adolesc. 2018;47:1456–1468. doi: 10.1007/s10964-018-0870-1. [DOI] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. 2020. Challenges and Burden of the Coronavirus 2019 (COVID-19) Pandemic for Child and Adolescent Mental Health: A Narrative Review to Highlight Clinical and Research Needs in the Acute Phase and the Long Return to Normality. Child and Adolescent Psychiatry and Mental Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaemi S.N. Digital depression: a new disease of the millennium? Acta Psychiatr. Scand. 2020;141:356–361. doi: 10.1111/acps.13151. [DOI] [PubMed] [Google Scholar]
- Green K.H., van de Groep S., Sweijen S.W., Becht A.I., Buijzen M., de Leeuw R.N.H., Remmerswaal D., van der Zanden R., Engels R.C.M.E., Crone E.A. Mood and emotional reactivity of adolescents during the COVID-19 pandemic: short-term and long-term effects and the impact of social and socioeconomic stressors. Sci. Rep. 2021;11 doi: 10.1038/s41598-021-90851-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatr. Res. 2020 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafstad G.S., Sætren S.S., Wentzel-Larsen T., Augusti E.-M. Adolescents' symptoms of anxiety and depression before and during the Covid-19 outbreak – a prospective population-based study of teenagers in Norway. Lancet Reg. Health - Europe. 2021;5:100093. doi: 10.1016/j.lanepe.2021.100093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes M.T., Szenczy A.K., Klein D.N., Hajcak G., Nelson B.D. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2021 doi: 10.1017/S0033291720005358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge E., Bickham D., Cantor J. Digital media, anxiety, and depression in children. Pediatrics. 2017;140:S76–S80. doi: 10.1542/peds.2016-1758G. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain T., Ahammed B., Chanda S.K., Jahan N., Ela M.Z., Islam N. Social and electronic media exposure and generalized anxiety disorder among people during COVID-19 outbreak in Bangladesh: a preliminary observation. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannotti R.J., Kogan M.D., Janssen I., Boyce W.F. Patterns of adolescent physical activity, screen-based media use, and positive and negative health indicators in the U.S. And Canada. J. Adolesc. Health. 2009;44:493–499. doi: 10.1016/j.jadohealth.2008.10.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020 doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keles B., McCrae N., Grealish A. A systematic review: the influence of social media on depression, anxiety and psychological distress in adolescents. Int. J. Adolesc. Youth. 2020 doi: 10.1080/02673843.2019.1590851. [DOI] [Google Scholar]
- Király O., Potenza M.N., Stein D.J., King D.L., Hodgins D.C., Saunders J.B., Griffiths M.D., Gjoneska B., Billieux J., Brand M., Abbott M.W., Chamberlain S.R., Corazza O., Burkauskas J., Sales C.M.D., Montag C., Lochner C., Grünblatt E., Wegmann E., Martinotti G., Lee H.K., Rumpf H.J., Castro-Calvo J., Rahimi-Movaghar A., Higuchi S., Menchon J.M., Zohar J., Pellegrini L., Walitza S., Fineberg N.A., Demetrovics Z. Preventing problematic internet use during the COVID-19 pandemic: Consensus guidance. Compr. Psychiatr. 2020;100:152180. doi: 10.1016/j.comppsych.2020.152180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavenne-Collot N., Ailliot P., Badic S., Favé A., François G., Saint-André S., Thierry A., Bronsard G. Did child-psychiatry patients really experience the dreaded clinical degradation during the COVID-19 pandemic lockdown? Neuropsychiatrie Enfance Adolescence. 2021;69:121–131. doi: 10.1016/j.neurenf.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M., Wu L., Yao S. Dose–response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br. J. Sports Med. 2016;50(20):1252–1258. doi: 10.1136/bjsports-2015-095084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Yue S., Hu X., Zhu J., Wu Z., Wang J.L., Wu Y. Associations between feelings/behaviors during COVID-19 pandemic lockdown and depression/anxiety after lockdown in a sample of Chinese children and adolescents. J. Affect. Disord. 2021;284:98–103. doi: 10.1016/j.jad.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingstone S. Developing social media literacy: how children learn to interpret risky opportunities on social network sites. Communications. 2014;39:283–303. doi: 10.1515/commun-2014-0113. [DOI] [Google Scholar]
- López-Bueno R., López-Sánchez G.F., Casajús J.A., Calatayud J., Gil-Salmerón A., Grabovac I., Tully M.A., Smith L. Health-related behaviors among school-aged children and adolescents during the Spanish Covid-19 confinement. Front. Pediatr. 2020;8 doi: 10.3389/fped.2020.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N.R., Freeman J.Y.A., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2021;50:44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maras D., Flament M.F., Murray M., Buchholz A., Henderson K.A., Obeid N., Goldfield G.S. Screen time is associated with depression and anxiety in Canadian youth. Prev. Med. 2015;73:133–138. doi: 10.1016/j.ypmed.2015.01.029. [DOI] [PubMed] [Google Scholar]
- Marino C., Gini G., Vieno A., Spada M.M. The associations between problematic Facebook use, psychological distress and well-being among adolescents and young adults: a systematic review and meta-analysis. J. Affect. Disord. 2018 doi: 10.1016/j.jad.2017.10.007. [DOI] [PubMed] [Google Scholar]
- Marques de Miranda D., da Silva Athanasio B., Sena Oliveira A.C., Simoes-e-Silva A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduc. 2020 doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mento C., Silvestri M.C., Muscatello M.R.A., Rizzo A., Celebre L., Praticò M., Zoccali R.A., Bruno A. Psychological impact of pro-anorexia and pro-eating disorder websites on adolescent females: a systematic review. Int. J. Environ. Res. Publ. Health. 2021 doi: 10.3390/ijerph18042186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohler-Kuo M., Dzemaili S., Foster S., Werlen L., Walitza S. Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. Int. J. Environ. Res. Publ. Health. 2021;18(9):4668. doi: 10.3390/ijerph18094668. PMID: 33925743. PMCID: PMC8124779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore S.A., Faulkner G., Rhodes R.E., Brussoni M., Chulak-Bozzer T., Ferguson L.J., Mitra R., O'Reilly N., Spence J.C., Vanderloo L.M., Tremblay M.S. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int. J. Behav. Nutr. Phys. Activ. 2020;17 doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzi S., Sansò A., Pace C.S. What's happened to Italian adolescents during the COVID-19 pandemic? A preliminary study on symptoms, problematic social media usage, and attachment: relationships and differences with pre-pandemic peers. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.590543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaidis A., Paksarian D., Alexander L., Derosa J., Dunn J., Nielson D.M., Droney I., Kang M., Douka I., Bromet E., Milham M., Stringaris A., Merikangas K.R. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci. Rep. 2021;11(1):8139. doi: 10.1038/s41598-021-87270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohannessian C.M.C., Fagle T., Salafia C. Social media use and internalizing symptoms during early adolescence: the role of co-rumination. J. Affect. Disord. 2021;280:85–88. doi: 10.1016/j.jad.2020.10.079. [DOI] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saúde Pública. 2020;36 doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- Palacio-Ortiz J.D., Londoño-Herrera J.P., Nanclares-Márquez A., Robledo-Rengifo P., Quintero-Cadavid C.P. 2020. Psychiatric disorders in children and adolescents during the COVID-19 pandemic. Revista Colombiana de Psiquiatria. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., Antoniazzi F., Piacentini G., Fearnbach S.N., Heymsfield S.B. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity. 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N., Korczak D.J., Madigan S. 2020. Evidence Suggests Children Are Being Left behind in COVID-19 Mental Health Research. European Child and Adolescent Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radovic A., Gmelin T.A., Venkatakrishnan K., Miller E. SOVA: acceptability and usability of a social media website for adolescents with depression or anxiety. J. Adolesc. Health. 2017;60:S93. doi: 10.1016/j.jadohealth.2016.10.364. [DOI] [Google Scholar]
- Restrepo A., Scheininger T., Clucas J., Alexander L., Salum G.A., Georgiades K., Paksarian D., Merikangas K.R., Milham M.P. Problematic internet use in children and adolescents: associations with psychiatric disorders and impairment. BMC Psychiatr. 2020;20 doi: 10.1186/s12888-020-02640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards D., Caldwell P.H.Y., Go H. Impact of social media on the health of children and young people. J. Paediatr. Child Health. 2015 doi: 10.1111/jpc.13023. [DOI] [PubMed] [Google Scholar]
- Riehm K.E., Feder K.A., Tormohlen K.N., Crum R.M., Young A.S., Green K.M., Pacek L.R., La Flair L.N., Mojtabai R. Associations between time spent using social media and internalizing and externalizing problems among US youth. JAMA Psychiatr. 2019;76:1266–1273. doi: 10.1001/jamapsychiatry.2019.2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk R.H., Hyde J.S., Abramson L.Y. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017;143(8):783–822. doi: 10.1037/bul0000102. PMID: 28447828. PMCID: PMC5532074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevanovic D., Basay B.K., Basay O., Leskauskas D., Nussbaum L., Zirakashvili M. COVID-19 pandemic-related aspects and predictors of emotional and behavioural symptoms in youth with pre-existing mental health conditions: results from Georgia, Lithuania, Romania, Serbia, and Turkey. Nord. J. Psychiatr. 2022 doi: 10.1080/08039488.2021.2013531. [DOI] [PubMed] [Google Scholar]
- Styck K.M., Malecki C.K., Ogg J., Demaray M.K. Measuring COVID-19-related stress among 4th through 12th grade students. Sch. Psychol. Rev. 2021:1–16. doi: 10.1080/2372966X.2020.1857658. [DOI] [Google Scholar]
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E., Rogers M.L., Martin G.N. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. Adolescents after 2010 and links to increased new media screen time. Clin. Psychol. Sci. 2018;6:3–17. doi: 10.1177/2167702617723376. [DOI] [Google Scholar]
- Werling A.M., Walitza S., Grünblatt E., Drechsler R. Media use before, during and after COVID-19 lockdown in a clinically referred sample in child and adolescent psychiatry: results of an online survey in Switzerland. Compr. Psychiatr. 2021 doi: 10.1016/j.comppsych.2021.152260. https://doi: 10.1016/j.comppsych.2021.152260 [DOI] [PubMed] [Google Scholar]
- Werling A.M., Walitza S., Drechsler R. Impact of the COVID-19 lockdown on screen media use in patients referred for ADHD to child and adolescent psychiatry: an introduction to problematic use of the internet in ADHD and results of a survey. J. Neural. Transm. 2021 doi: 10.1007/s00702-021-02332-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang M., Zhang Z., Kuwahara K. 2020. Impact of COVID-19 Pandemic on Children and Adolescents' Lifestyle Behavior Larger than Expected. Progress in Cardiovascular Diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao S., Yan Z., Zhao L. Physical activity, screen time, and mood disturbance among Chinese adolescents during COVID-19. J. Psychosoc. Nurs. Ment. Health Serv. 2021;59:14–20. doi: 10.3928/02793695-20201104-04. [DOI] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeasmin S., Banik R., Hossain S., Hossain M.N., Mahumud R., Salma N., Hossain M.M. Impact of COVID-19 pandemic on the mental health of children in Bangladesh: a cross-sectional study. Child. Youth Serv. Rev. 2020;117 doi: 10.1016/j.childyouth.2020.105277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Shuai L., Yu H., Wang Z., Qiu M., Lu L., Cao X., Xia W., Wang Y., Chen R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X. Psychological Trauma: Theory, Research, Practice, and Policy. Vol. 12. 2020. Managing psychological distress in children and adolescents following the COVID-19 epidemic: a cooperative approach. [DOI] [PubMed] [Google Scholar]