Abstract
Background
Sleep difficulties are often reported in practice, and are part of the diagnostic criteria for depression and bipolar disorder.
Aims
To inform the understanding of the relationship between sleep and both depression and bipolar disorder.
Method
We conducted a narrative literature review of affective disorders and sleep difficulties in children and young people.
Results
Specific sleep disorders, such as parasomnias, narcolepsy and sleep-related movement disorders, are associated with depression, whereas insomnia, obstructive sleep apnoea and circadian rhythm disorders are associated with both depression and bipolar disorder in children and young people. Conversely, children and young people with depression can present with a number of sleep difficulties, and these are associated with higher depression severity and greater fatigue, suicidal ideation, physical complaints, pain and decreased concentration. Sleep disturbances among adolescents with bipolar disorder can affect the severity of depressive and manic symptoms, are a poor prognostic indicator and have been associated with social and academic impairment. Antidepressants and antipsychotics can directly affect sleep architecture, which clinicians need to be aware of. Non-pharmacological interventions for sleep problems could prevent and/or minimise the risk of relapse in affective disorders.
Conclusions
Sleep difficulties can occur before, during and after an episode of depression or bipolar disorder, and have a higher prevalence in affective disorders compared with the general population. A multi-modal approach would include the treatment of both the affective and specific sleep disorder. Further research is needed in this field to understand the impact of combined interventions on clinical outcomes.
Keywords: Bipolar affective disorders, sleep disorders, depressive disorders, cognitive–behavioural therapies, comorbidity
Introduction
Sleep is a biological necessity, essential for infant, child and adolescent growth; metabolism and immune system regulation; and normal memory and affect.1,2 This narrative review aims to serve as a clinician's guide, and will describe the following in children and young people: normal sleep, sleep disorders, the effect of affective disorders on sleep, the effect of disturbed sleep on mood and the role of targeted sleep therapy, particularly with respect to mood. Awareness of this complex relationship among healthcare professionals working with children and young people could lead to better care and improved long-term outcomes. This review does not discuss the relationship between sleep and affective disorders in children and young people with a neurodevelopmental disorder, such as hyperkinetic disorders, autism spectrum disorder and/or intellectual disabilities.
Normal sleep
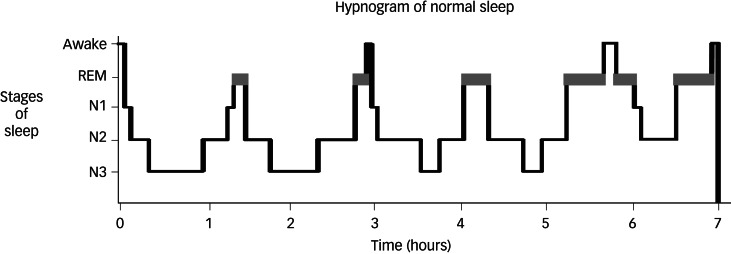
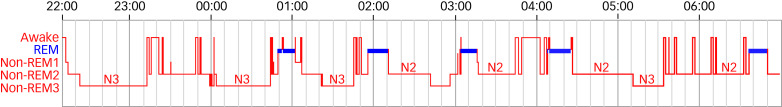
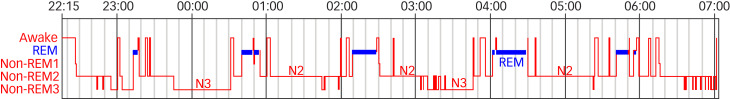
Sleep is composed of two phases: rapid eye movement (REM) and non-rapid eye movement (NREM).3,4 NREM sleep is further divided into stages N1, N2 and N3, with stage N3 known as slow-wave sleep (SWS). REM sleep is associated with inhibition of peripheral muscle tone, along with active cortical function and increased blood pressure, heart and respiration rates.1 The switches that result in the cycling between REM and NREM are facilitated by monoaminergic and cholinergic neurons within the brain-stem (see Figs 1–3).5 Sleep is essential in the development of neurosensory, memory and motor systems in the foetus and neonate, and in the maintenance of brain plasticity over the lifetime.2 The overall regulation of sleep depends on two major processes: the sleep–wake homeostatic process and the circadian timing system. The homeostatic process ensures that the longer a person stays awake, the more pressure there is to fall asleep.6
Fig. 1.
Hypnogram showing normal sleep in an adult. Non-rapid eye movement sleep is split into stages N1–N3. Courtesy of Dr Kirstie N. Anderson. REM, rapid eye movement.
Fig. 2.
Hypnogram of a 9-year-old boy with a short sleep onset latency and shorter sleep cycle duration. Non-rapid eye movement sleep is split into stages N1–N3. Courtesy of Dr Elizabeth A. Hill, Royal Hospital for Sick Children, Edinburgh.
Fig. 3.
Hypnogram of a 14-year-old male. Longer (more adult-like) sleep cycle duration (some sleep fragmentation). Non-rapid eye movement sleep is split into stages N1–N3. Courtesy of Dr Elizabeth A. Hill, Royal Hospital for Sick Children, Edinburgh. REM, rapid eye movement.
Sleep during childhood and adolescence
The duration of sleep, the duration of sleep cycles and the circadian rhythm differ between individuals, and vary during a person's lifetime. Newborns sleep most of the day and toddlers sleep for up to 12 h during the night, as well as having one or two naps during the day.7 REM and NREM cycles occur every 50–60 min in children under the age of 8 years, and these cycles gradually change to every 90 min as the child develops. Night waking is normal for all children, but is typically very brief, with rapid return to sleep. The proportion of stage N3 SWS is higher and the amplitude of the delta waves is far larger in children compared with adults; this proportion continuously reduces throughout adolescence and into adulthood (see Figs 2 and 3).1 During the final stages of puberty, there is a biological change in the circadian system whereby children fall asleep later and increase their total sleep time. This often coincides with a desire to stay up late at night to engage in more adult social activities. This delay in circadian phase leads to a delay in sleep onset,8 and may cause a lack of synchronicity between adolescent circadian rhythm and that of the parents and of societal structures (such as school timetables). These changes can lead to insufficient sleep, family discord and subsequent emotional difficulties.9 Sleep deprivation, particularly REM deprivation, in neonates and infants may have a permanent negative effect on development of neural circuitry of the primary sensory system, and of emotion, social learning and memory.2
Affective disorders in adolescents
Major depressive disorder (MDD) in adolescence is characterised by a pervasive and persistent low or irritable mood10 and/or anhedonia, which can also be accompanied by low self-esteem.11 Adolescents with depression may report certain symptoms more often than adults, such as loss of energy, weight and appetite changes, and sleep difficulties, whereas adults report more anhedonia and concentration difficulties.12 Early and accurate detection and management of MDD is important because early onset can be a potent predictor of lifelong recurrent depression.13
Bipolar disorder is a chronic, typically relapsing condition, characterised by episodes of (hypo)mania and depression with a negative effect on overall functioning. In the DSM-IV14 and DSM-5,10 it has been separated into type 1, type 2, cyclothymia and not otherwise specified.10,14,15 A number of specifiers have been used for bipolar disorder when it occurs in young people, including prepubescent, juvenile, childhood or adolescent bipolar disorder.10 Bipolar disorder in adolescence is more likely to exhibit rapid cycling and mixed states, and the symptoms are more likely to have a fluctuating intensity and duration, thereby reducing the likelihood of accurate diagnosis compared with adults.10
Adolescent-onset MDD and bipolar disorder often have a chronic, episodic course, and can be accompanied by long-term functional impairment.16 Those affected have higher rates of substance misuse, poor academic attainment, interpersonal difficulties, poor sleep patterns and higher risk of suicide compared with healthy adolescents. These difficulties can negatively affect physical, emotional, cognitive and social development.16–18
Sleep disorders
The International Classification of Sleep Disorders, Third Edition (ICSD-3)19 defines more than 70 sleep disorders classified into seven major categories, one of which is insomnia.19 The DSM-510 describes ten sleep–wake disorders, and the ICD-1011 groups nonorganic sleep disorders into dyssomnias, parasomnias and nonpsychogenic disorders (see Table 1). When considering disordered sleep, it is worth noting that subjectively reported sleep correlates poorly with objective findings.20,21 For further information on specific sleep disorders, please refer to Table 2.
Table 1.
Diagnostic entities in ICSD-3, DSM-5 and ICD-10
| ICSD-3 | DSM-5 | ICD-10 | |
|---|---|---|---|
| Over 70 disorders classified in seven categories19 | Ten disorders for adult, geriatric and paediatric patients10 | Two categories of nonorganic sleep disorders in adults and children and one category of nonpsychogenic disorders11 | |
| Category: sleep–wake disorders | Category: dyssomnias | ||
|
|
|
|
| Category: parasomnias | |||
|
|||
| Category: nonpsychogenic disorders | |||
|
ICSD-3, International Classification of Sleep Disorders, Third Edition; NREM, non-rapid eye movement; REM, rapid eye movement.
Table 2.
Sleep disorders
| Name | Diagnostic criteria | Considerations | Treatment |
|---|---|---|---|
| Insomnia | DSM-510
|
Paediatric insomnia Reports from young people and parents or carers need to be taken into consideration when assessing for insomnia23 |
Psychoeducation Behavioural management Pharmacotherapy |
| CRDs | Delayed sleep phase disorder
|
People with CRDs are unable to sleep and wake at the times required for normal work, school or social needs11 | Sleep–wake scheduling Timed light exposure Melatonin |
| Sleep-related breathing disorders | OSA
|
|
Adenotonsillectomy is the primary treatment of this condition in those aged <8 years25 Continuous positive airway pressure therapy for older children25 |
| Parasomnias | NREM parasomnias
Nightmares |
NREM parasomnias
|
Psychoeducation Behavioural management Treatment of comorbidities |
REM-related parasomnias
| |||
| Narcolepsy and hypersomnia | Narcolepsy
|
Narcolepsy
|
Psychoeducation Behavioural management Pharmacotherapy (stimulants) |
Primary hypersomnia in children
|
Primary hypersomnia in children |
ICSD-3, International Classification of Sleep Disorders, Third Edition; CRD, circadian rhythm disorder; OSA, obstructive sleep apnoea; NREM, non-rapid eye movement; REM, rapid eye movement.
Insomnia
The diagnostic criteria for insomnia in adults and young people are the same; however, in the younger population, the problems around initiating and maintaining sleep can also be reported by the carers. These difficulties are typically associated with bedtime resistance and behavioural change.23
Circadian rhythm disorders
The social zeitgeber theory posits that changes to the circadian rhythm can be linked to disruptions of bedtime, wake time or meal times.31 Circadian rhythm sleep disorders (CRDs) are caused by desynchronisation between the internal sleep–wake rhythms and the light–dark cycle, or a misalignment between the body clock and the person's external environment.
Sleep-related breathing disorders
Among the sleep-related breathing disorders, obstructive sleep apnoea (OSA) is the most common and is primarily caused by enlarged tonsils and adenoids.
Parasomnias and nightmare disorders
Parasomnias are divided into two categories: REM and NREM. They affect up to 50% of children27 and are a risk factor for the subsequent development of MDD in adulthood.32 REM-related parasomnias, such as sleep paralysis or nightmare disorder, are frequently encountered in childhood and, like NREM parasomnias, they often resolve spontaneously in adolescence.1,27,28
Narcolepsy and hypersomnia
Narcolepsy is a rare sleep disorder caused by the loss of a specific population of hypocretinergic neurons. This condition has been associated with depression both in adults32 and the paediatric population.33–35 Primary hypersomnia may be transient or may represent a slight delay in normal development,30 and has not been associated with affective psychiatric disorders in adulthood. Bouts of episodic hypersomnia, along with cognitive and behavioural changes, are part of the very rare condition of Kleine–Levin syndrome.
Sleep-related movement disorders
Sleep-related movement disorders, such as restless legs syndrome (RLS), periodic limb movement disorder (PLMD) or the far less common condition of rhythmic movement disorder, are conditions that cause movement during or before sleep.
Sleep disorders and their relationship with mood
Behavioural pattern insomnia occurs more often in children and has been associated with symptoms of depression in preschoolers.29 It is important to be mindful of the parent–child interaction around bedtime, and a thorough assessment often helps to identify the aetiology of the sleep problem. Children can become habituated into needing a bedtime story or other event as the associated condition to fall asleep. This can create sleep difficulties, such as when children wake through the night and are unable or unwilling to self-settle in its absence. Sleep difficulties can occur when parents struggle to implement boundaries or routines around bedtime in older children. Additionally, certain parental expectations that are not in line with the developmental stage36 and children's sleep needs might lead to their erroneous identification of disordered sleep, in particular the natural later bedtimes through puberty and teenage years.
Data from school-aged children37 and adult research have shown an association between OSA and depression.32,38 OSA is more prevalent in people with bipolar disorder, both in adults39 and adolescents,40 but research in this field remains sparse.
Significant, intrusive and distressing parasomnia has been associated with suicidal thinking41 and, in younger children (aged 12 years), with psychotic phenomena, albeit rarely.42 Adults with MDD and bipolar disorder are more likely to have experienced parasomnias, such as confusional arousal disorder, night terrors and sleepwalking, than the general population, but the nature of this association remains unclear given how common these symptoms are in children and are mostly benign, infrequent and self-limiting.43
When frequent and intrusive, nightmares can occasionally result in daytime impairment and reduced quality of life, and are associated with psychological distress and symptoms of anxiety and depression.44,45 Sheaves et al found that high nightmare frequency followed by subsequent distress was positively associated with higher scores in difficulties, such as depression, among students.46
Narcolepsy has been associated with depression in adults32 and in the paediatric population.33–35 Additionally, there are no biomarkers for Kleine–Levin syndrome, its aetiology is debated, there is spontaneous remission and one study suggested that young people with a history of Kleine–Levin syndrome may experience depression later in life.47
CRDs have a higher prevalence in adults with bipolar disorder than the general population,48,49 with a significant association with a younger onset of bipolar disorder.50 CRDs are also risk factors for developing MDD in adults,32 and have been associated with depressive symptoms in adolescents.51
RLS and PLMD have been associated with depression in adults when severe and sleep disruptive.32 In children and young people, RLS has a prevalence of 2–4%52 and has been associated with depression, although to a lesser extent, and usually the condition is milder in younger adults.53 Adolescents with PLMD also appear to display more depressive symptoms.54
Mood disorders and their relationship with sleep
Disturbed sleep is a core feature of a depressive episode,55 may occur in the prodromal period56,57 and/or be a residual symptom of depression.55 Conversely, mood disturbance is listed as one of the functional impairment criteria for insomnia disorder.
In the general teenage population, insomnia is associated with mental health difficulties later in life.58 Disturbed sleep confers an increased risk of subsequent bipolar.59–63 Wakefulness in bed56 and a shorter duration of sleep57 can be regarded as aetiological factors for depression.64–67 Sleep difficulties can precede affective episodes59,61–63,68,69 and other mental health difficulties58 by several years in young people. Aspects of the sleep architecture of insomnia, such as reductions in SWS, low spindle activity or changes in REM, are also associated with internalising behaviours.70
In young people who are currently depressed, disturbed sleep incorporating sleep continuity problems,17 wakefulness in bed and increased sleep-onset latency is common. Decreased sleep efficiency, short sleep duration, daytime sleepiness, non-restorative sleep, hypersomnia and irregular sleep–wake rhythm are also common.12,17,20,29,56,57,71–75 Sleep difficulties are associated with higher depression severity and recurrence;76 greater fatigue, suicidal ideation, physical complaints and pain;17 and decreased concentration.73,77 There is evidence that sleep quality, total sleep time and sleep microarchitecture can predict new onset and recurrence of depression.78
Robust adult data and preliminary data in young people suggests that sleep problems can be encountered in all phases of bipolar disorder,79 can be associated with psychosocial impairment and can play a role in predicting mania and depression.80–82 Sleep disturbances among adolescents with bipolar disorder can have an effect on the severity of depressive80,81 and manic symptoms, are associated with academic and social impairment during recovery,80 and can be a poor prognostic indicator. Young people with bipolar disorder show a range of sleep difficulties, including delayed sleep onset, insomnia, hypersomnia and difficulties waking up in the morning. They can also present with difficulties maintaining a regular rhythm, longer naps during the day, more night-time wakings, a greater total time awake during the night and nightmare disorder.80,83–86 Nightmares appear to augment the risk of suicide, and insufficient sleep duration has been associated with self-injurious behaviours.84 Mania has been associated with decreased need for sleep in young people;87 however, in adolescents, mania also appears to be linked to a broader sleep disturbance,59 including variable sleep duration and unstable morning routines.80 Sleep disturbance does not appear to differentiate between types of bipolar disorders, being as common, for instance, in bipolar disorder not otherwise specified as in bipolar disorder type 1.88 Disturbed sleep is seen more often in the children of parents with bipolar disorder than in healthy controls.61,89 One study of children whose parents were diagnosed with bipolar disorder showed shorter time to onset of sleep and longer duration on actigraphy, with opposite subjectively reported experiences.90 This is in accordance with a second study showing that people deemed to be at high risk of developing bipolar disorder, either through family history of bipolar disorder or personal history of severe depression and subthreshold mania symptoms, have shown a longer duration for sleep onset, but also higher levels of sleep specific worries.85 Depressed youth with bipolar disorder are significantly more likely to be affected by daytime sleepiness and hypersomnia than young people with unipolar depression.86
Mechanism of the association between mood disorders and sleep
Maladaptive thinking processes, such as cognitive inflexibility, attention bias by selectively focusing on negative information, misperception of sleep deficit, rumination and worry, may underlie insomnia, depression and bipolar disorder in adolescence.70 These processes may trigger autonomic arousal and the reinforcement of negative cognitions. Similarly, abnormalities of circadian rhythm, perhaps mediated by genetic vulnerability via polymorphisms of serotonin, dopamine and circadian clock genes60,91 or dysfunction in the white matter integrity, could also play a role in the aetiology of these conditions.92 Disruption of the corticolimbic circuitry70 may be a consequence of insomnia, and may impair affective reactivity and regulation.93 Dysregulation of reward/approach related brain function,70,94 hypothalamic-pituitary-adrenal axis dysregulation and elevated inflammatory cytokines may also contribute to both psychopathology and sleep disturbance.70 Disruptions to the circadian rhythm have been postulated to contribute to the pathophysiology of bipolar disorder.95 Genetic commonality between sleep and impulsivity and anger/frustration has also been described.96 Antidepressants, particularly those with noradrenergic or dopaminergic mechanisms, may induce or aggravate insomnia. Electronic media use among adolescents, particularly at night-time, may be related to sleep disturbance and higher levels of depressive symptoms,97 in which a sleep debt developed over school days is paid back at the weekend.98
Interventions for mood disorders and sleep problems
Non-pharmacological interventions for depression and sleep problems
Psychoeducation, consistent sleep–wake schedules and tailored interventions for addressing sleep problems should play an important role in the prevention and treatment of mental health difficulties, at any age. Concomitantly addressing sleep problems can lead to an increased remission rate of depression.67,99
Cognitive–behavioural therapy for insomnia (CBT-I) has a strong evidence base for decreasing insomnia severity.70,100 There have been a number of studies of CBT-I in young people with comorbidities (e.g. Moore et al101); two randomised controlled trials in young people not selected on the basis of comorbidity have shown a persistent benefit in sleep onset, latency, efficiency and anxiety, but not in total sleep time.102,103 Internet-delivered CBT-I has also been examined. Recent large, randomised controlled trials, one of which targeted university students,104 have shown a benefit in sleep and a number of mental health problems, such as depression, anxiety and psychotic phenomena.104,105
Transdiagnostic sleep and circadian intervention collates established sleep management strategies,106 and has been shown to exert a sustained beneficial effect on eveningness circadian preference in adolescents.107 Post hoc analysis revealed that the initial broader health benefits were not maintained (compared with psychoeducation) at 6 months.107,108
Pharmacological intervention for depression and sleep problems
Many patients with depression enter REM stage quicker and have less NREM sleep in the first sleep cycle. Antidepressants typically alter sleep in the opposite direction.109 Selective serotonin reuptake inhibitors (SSRIs) are the antidepressants of choice in children and young people. It is important that sleep effects are considered in the discussion of positives, negatives and gaps in knowledge that are required to allow an informed decision of whether and when to use medication alongside psychosocial interventions for treating depression. SSRIs are known to increase REM latency and SWS, reduce REM sleep and sleep continuity, and may also induce nightmares, cause enhanced dreaming and lead to changes in dream content.65,109–114 Upon stopping the treatment, rebound REM sleep is known to occur.110 SSRIs can increase the risk of aggravating RLS, or induce RLS or PLMD symptoms.115
Melatonin
Melatonin is often used for children with sleep-onset insomnia or delayed sleep phase syndrome and neurodevelopmental disorders. High doses of melatonin are rarely needed for managing insomnia. Behavioural strategies should be used as a first-line treatment.116–118 Adults with affective disorders have been found to have abnormalities in the timing and amplitude of biological rhythms, including abnormal patterns of melatonin secretion.119 Differences in the level of melatonin and in the pattern of its production have been described in adults with bipolar disorder across mood states.120 A recent study suggested that melatonin levels are related to social and occupational functioning in young people with affective disorders. The putative role of melatonin in the treatment of depression in young people is an exciting prospect.121
Non-pharmacological interventions for bipolar disorder and sleep
Regulating sleep and maintaining consistent sleep–wake schedules in young people with bipolar disorder improves outcomes, and potential affective relapses can be prevented and/or minimised. This may be enacted via psychoeducation, the development of consistent sleep and wake times and routines, relaxation procedures, and reinforcement of good sleep habits,122 chronotherapy123 or CBT-I.124
Pharmacological interventions for bipolar disorder and sleep
The use of psychotropic medication in children and young people is only advisable when a clear diagnosis of bipolar disorder has been made, and should not be used solely for addressing sleep. Improved sleep is associated with pharmacologically mediated improvement in mood symptoms in adolescents,84 but it is worth considering whether the effect of bipolar psychotropics on sleep mediates some of these changes. Olanzapine and quetiapine have a significant impact on sleep duration in younger people with bipolar disorder.85 Antipsychotics, including olanzapine, quetiapine and ziprasidone, have been shown in the adult population to increase the duration of sleep continuity, increase total sleep time and sleep efficiency, increase REM latency and SWS, decrease stage 2 sleep spindle density and reduce the amount of REM sleep.125
The increased risk of metabolic syndrome in bipolar disorder also increases the risk of OSA in adolescents.40 Another study suggested a possible relationship between the use of medication and enuresis,88 which could further affect the sleep.
Research direction
There are a number of challenges in the field of sleep research in MDD and bipolar disorder. First, most studies are cross-sectional, with an unclear timeline between the onset of the affective disorder, that of sleep difficulties and the short- and long-term complications.83 There is still limited objective sleep assessment with polysomnography, and many studies report subjective sleep via self-/parent report or actigraphy without, for example, screening for specific sleep disorders or using polysomnography. The parent–child agreement for psychiatric disorders is low and, wherever possible, the children and young people should be consulted about their sleep directly; depression and bipolar disorder are no exception.84,126 Terms such as sleep disorders and sleep difficulties are used interchangeably, and there is a need for greater precision with the use of, for example, insomnia disorder or CRD. Additionally, there seems to be a very high reliance on assessment questionnaires for diagnosing sleep problems and sometimes even affective disorders. Over the years, there have been inconsistent findings in the studies for depression in children and young people,127 as study designs vary a great deal.
The number of patients included in trials for bipolar disorder tends to be relatively low, which might be linked to the relatively low prevalence in children and adolescents and the subsequent recruitment challenge. Some studies seem to focus on one type of bipolar disorder and do not include the full spectrum of disorders, which might leave out important information.88 Findings vary across studies because of differences not only in the sleep measurement, but also sampling; some studies focus on children who have been diagnosed with bipolar disorder, whereas others include children whose parents have an affective disorder.81 There is also a high variability of the age range, as there is no consensus on the age of onset of paediatric bipolar disorder; some papers have included participants of 5 years of age,88 whereas others have focused on prepubescents128 or adolescents.80 One has to consider the importance of brain maturation and expected sleep changes that occur in these stages of life, as well as the beliefs around sleep within the family.
An important direction for future research would be developing a robust study design that allows a longer-term evaluation of the symptoms of a bigger cohort, objective and subjective standardised measures of sleep and mood, screening for comorbid sleep disorders, collecting collateral information and focusing on behavioural interventions for sleep, such as CBT-I.
Conclusions
The relationship between sleep difficulties and mood in children and young people is complex. Sleep problems are reported long before the onset, during and sometimes after, an episode of unipolar depression or bipolar disorder, and can play an important role in their presentation. The prevalence of sleep disorders, such as insomnia, CRDs and sleep apnoea, in depression and bipolar disorder is higher than in the general population, but often these diagnoses are missed and specific treatment not offered. A multi-modal approach would include the treatment of both the affective and specific sleep disorder. ‘Sleep disturbance’ is not a diagnosis. There is a need for further longitudinal studies with subjective and objective sleep measures to improve therapy and the nature of the relationship between mood and sleep. Of most importance is the impact of specific treatment for sleep disorders on the long-term outcome of affective disorders. Clinicians need to know if better nights reliably lead to better days.
Acknowledgements
The authors wish to thank Dr Elizabeth A. Hill (Royal Hospital for Sick Children, Edinburgh) for assistance with hypnograms.
Author contributions
All authors have made substantial contributions to the conception of the work, have revised it critically for important intellectual content, have offered the final approval of the version to be published and are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. In addition, M.C., K.N.A. and S.W. made substantial contributions to the design of the work and drafted the paper. Furthermore, M.C. also acquired and interpreted the data.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Data availability
Data availability is not applicable to this article as no new data were created or analysed in this study.
Declaration of interest
None.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1192/bjo.2021.1076.
click here to view supplementary material
References
- 1.Mindell JA, Owens JA, Carskadon MA. Developmental features of sleep. Child Adolesc Psychiatr Clin N Am 1999; 8(4): 695–725. [PubMed] [Google Scholar]
- 2.Penn AA, Shatz CJ. Brain waves and brain wiring: the role of endogenous and sensory-driven neural activity in development. Pediatr Res 1999; 45(4): 447–58. [DOI] [PubMed] [Google Scholar]
- 3.Gelder MG. New Oxford Textbook of Psychiatry. Oxford University Press, 2012. [Google Scholar]
- 4.Carley DW, Farabi SS. Physiology of sleep. Diabetes Spectr 2016; 29(1): 5–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hobson JA, McCarley RW, Wyzinski PW. Sleep cycle oscillation: reciprocal discharge by two brainstem neuronal groups. Science 1975; 189(4196): 55–8. [DOI] [PubMed] [Google Scholar]
- 6.Czeisler CA, Duffy JF, Shanahan TL, Brown EN, Mitchell JF, Rimmer DW, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science 1999; 284(5423): 2177–81. [DOI] [PubMed] [Google Scholar]
- 7.Bathory E, Tomopoulos S. Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children. Curr Probl Pediatr Adolesc Health Care 2017; 47(2): 29–42. [DOI] [PubMed] [Google Scholar]
- 8.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health 2002; 31(suppl 6): 175–84. [DOI] [PubMed] [Google Scholar]
- 9.Carskadon MA. Sleep in adolescents: the perfect storm. Pediatr Clin 2011; 58(3): 637–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association, 2013. [Google Scholar]
- 11.World Health Organization (WHO). The ICD-10 Classification of Mental and Behavioural Disorders. WHO, 1993. [Google Scholar]
- 12.Rice F, Riglin L, Lomax T, Souter E, Potter R, Smith DJ, et al. Adolescent and adult differences in major depression symptom profiles. J Affect Disord 2019; 243: 175–81. [DOI] [PubMed] [Google Scholar]
- 13.Carballo JJ, Muñoz-Lorenzo L, Blasco-Fontecilla H, Lopez-Castroman J, García-Nieto R, Dervic K, et al. Continuity of depressive disorders from childhood and adolescence to adulthood: a naturalistic study in community mental health centers. Prim Care Companion CNS Disord 2011; 13(5): PCC.11m01150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). American Psychiatric Association, 1994. [Google Scholar]
- 15.Nottelmann E. National Institute of Mental Health Research roundtable on prepubertal bipolar disorder. J Am Acad Child Adolesc Psychiatry 2001; 40(8): 871–8. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez-Mendoza J, Calhoun SL, Vgontzas AN, Li Y, Gaines J, Liao D, et al. Insomnia phenotypes based on objective sleep duration in adolescents: depression risk and differential behavioral profiles. Brain Sci 2016; 6(4): 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murray CB, Murphy LK, Palermo TM, Clarke GM. Pain and sleep-wake disturbances in adolescents with depressive disorders. J Clin Child Adolesc Psychol 2012; 41(4): 482–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts RE, Roberts CR, Duong HT. Chronic Insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health 2008; 42(3): 294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Academy of Sleep Medicine. International Classification of Sleep Disorders – Third Edition (ICSD-3). American Academy of Sleep Medicine, 2014. [Google Scholar]
- 20.Bertocci MA, Dahl RE, Williamson DE, Iosif AM, Birmaher B, Axelson D, et al. Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry 2005; 44(11): 1158–66. [DOI] [PubMed] [Google Scholar]
- 21.Chen MC, Burley HW, Gotlib IH. Reduced sleep quality in healthy girls at risk for depression. J Sleep Res 2012; 21(1): 68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zucconi M, Ferri R. Assessment of sleep disorders and diagnostic procedures. Eur Sleep Res Soc 2014; 23: 95–110. [Google Scholar]
- 23.Bruni O, Novelli L. Sleep disorders in children. BMJ Clin Evid 2010; 2010: 2304. [PMC free article] [PubMed] [Google Scholar]
- 24.Marcus CL, Brooks LJ, Ward SD, Draper KA, Gozal D, Halbower AC, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012; 130(3): e714–e55. [DOI] [PubMed] [Google Scholar]
- 25.Chinnadurai S, Jordan AK, Sathe NA, Fonnesbeck C, McPheeters ML, Francis DO. Tonsillectomy for obstructive sleep-disordered breathing: a meta-analysis. Pediatrics 2017; 139(2): e20163491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masand P, Popli A, Weilburg J. Sleepwalking. Am Fam Physician 1995; 51(3): 649–54. [PubMed] [Google Scholar]
- 27.Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician 2014; 89(5): 368–77. [PubMed] [Google Scholar]
- 28.Kazaglis L, Bornemann MAC. Classification of parasomnias. Curr Sleep Med Rep 2016; 2(2): 45–52. [Google Scholar]
- 29.Steinsbekk S, Berg-Nielsen TS, Wichstrom L. Sleep disorders in preschoolers: prevalence and comorbidity with psychiatric symptoms. J Dev Behav Pediatr 2013; 34(9): 633–41. [DOI] [PubMed] [Google Scholar]
- 30.Steinsbekk S, Wichstrom L. Stability of sleep disorders from preschool to first grade and their bidirectional relationship with psychiatric symptoms. J Dev Behav Pediatr 2015; 36(4): 243–51. [DOI] [PubMed] [Google Scholar]
- 31.Grandin LD, Alloy LB, Abramson LY. The social zeitgeber theory, circadian rhythms, and mood disorders: review and evaluation. Clin Psychol Rev 2006; 26(6): 679–94. [DOI] [PubMed] [Google Scholar]
- 32.Byrne EM, Timmerman A, Wray NR, Agerbo E. Sleep disorders and risk of incident depression: a population case-control study. Twin Res Hum Genet 2019; 22(3): 140–6. [DOI] [PubMed] [Google Scholar]
- 33.Ohayon MM. Narcolepsy is complicated by high medical and psychiatric comorbidities: a comparison with the general population. Sleep Med 2013; 14(6): 488–92. [DOI] [PubMed] [Google Scholar]
- 34.Inocente CO, Gustin MP, Lavault S, Guignard-Perret A, Raoux A, Christol N, et al. Depressive feelings in children with narcolepsy. Sleep Med 2014; 15(3): 309–14. [DOI] [PubMed] [Google Scholar]
- 35.Plazzi G, Clawges HM, Owens JA. Clinical characteristics and burden of illness in pediatric patients with narcolepsy. Pediatr Neurol 2018; 85: 21–32. [DOI] [PubMed] [Google Scholar]
- 36.Werner H, Jenni OG. Do parental expectations play a role in children's sleep and mothers’ distress? An exploration of the goodness of fit concept in 54 mother-child dyads. Sleep Disord 2011; 2011: 104832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hodges E, Marcus CL, Kim JY, Xanthopoulos M, Shults J, Giordani B, et al. Depressive symptomatology in school-aged children with obstructive sleep apnea syndrome: incidence, demographic factors, and changes following a randomized controlled trial of adenotonsillectomy. Sleep 2018; 41(12): zsy180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garbarino S, Bardwell WA, Guglielmi O, Chiorri C, Bonanni E, Magnavita N. Association of anxiety and depression in obstructive sleep apnea patients: a systematic review and meta-analysis. Behav Sleep Med 2020; 18(1): 35–57. [DOI] [PubMed] [Google Scholar]
- 39.Kelly T, Douglas L, Denmark L, Brasuell G, Lieberman DZ. The high prevalence of obstructive sleep apnea among patients with bipolar disorders. J Affect Disord 2013; 151(1): 54–8. [DOI] [PubMed] [Google Scholar]
- 40.Mieczkowski BP, Oduguwa A, Kowatch RA, Splaingard M. Risk factors for sleep apnea in children with bipolar disorder. J Affect Disord 2014; 167: 20–4. [DOI] [PubMed] [Google Scholar]
- 41.Gau S-F, Suen Soong W-T. Psychiatric comorbidity of adolescents with sleep terrors or sleepwalking: a case-control study. Aust N Z J Psychiatry 1999; 33(5): 734–9. [DOI] [PubMed] [Google Scholar]
- 42.Fisher HL, Lereya ST, Thompson A, Lewis G, Zammit S, Wolke D. Childhood parasomnias and psychotic experiences at age 12 years in a United Kingdom birth cohort. Sleep 2014; 37(3): 475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry 1999; 60(4): 268–76. [DOI] [PubMed] [Google Scholar]
- 44.Levin R, Fireman G. Nightmare prevalence, nightmare distress, and self-reported psychological disturbance. Sleep 2002; 25(2): 205–12. [PubMed] [Google Scholar]
- 45.Krakow B. Nightmare complaints in treatment-seeking patients in clinical sleep medicine settings: diagnostic and treatment implications. Sleep 2006; 29(10): 1313–9. [DOI] [PubMed] [Google Scholar]
- 46.Sheaves B, Porcheret K, Tsanas A, Espie CA, Foster RG, Freeman D, et al. Insomnia, nightmares, and chronotype as markers of risk for severe mental illness: results from a student population. Sleep 2016; 39(1): 173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Groos E, Chaumereuil C, Flamand M, Brion A, Bourdin H, Slimani V, et al. Emerging psychiatric disorders in Kleine-Levin syndrome. J Sleep Res 2018; 27(5): e12690. [DOI] [PubMed] [Google Scholar]
- 48.Melo MCA, Abreu RLC, Linhares Neto VB, de Bruin PFC, de Bruin VMS. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev 2017; 34: 46–58. [DOI] [PubMed] [Google Scholar]
- 49.Talih F, Gebara NY, Andary FS, Mondello S, Kobeissy F, Ferri R. Delayed sleep phase syndrome and bipolar disorder: pathogenesis and available common biomarkers. Sleep Med Rev 2018; 41: 133–40. [DOI] [PubMed] [Google Scholar]
- 50.Takaesu Y, Inoue Y, Murakoshi A, Komada Y, Otsuka A, Futenma K, et al. Prevalence of circadian rhythm sleep-wake disorders and associated factors in euthymic patients with bipolar disorder. PLoS One 2016; 11(7): e0159578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saxvig IW, Pallesen S, Wilhelmsen-Langeland A, Molde H, Bjorvatn B. Prevalence and correlates of delayed sleep phase in high school students. Sleep Med 2012; 13(2): 193–9. [DOI] [PubMed] [Google Scholar]
- 52.Xue R, Liu G, Ma S, Yang J, Li L. An epidemiologic study of restless legs syndrome among Chinese children and adolescents. Neurol Sci 2015; 36(6): 971–6. [DOI] [PubMed] [Google Scholar]
- 53.Angriman M, Cortese S, Bruni O. Somatic and neuropsychiatric comorbidities in pediatric restless legs syndrome: a systematic review of the literature. Sleep Med Rev 2017; 34: 34–45. [DOI] [PubMed] [Google Scholar]
- 54.Frye S, Fernandez-Mendoza J, Calhoun SL, Vgontzas AN, Liao D, Bixler EO. 0933 Role of periodic limb movements during sleep in adolescents with attention deficit hyperactivity disorder: differential association with internalizing vs. externalizing behaviors. J Sleep Disord Res 2017; 40(suppl 1): A347. [Google Scholar]
- 55.Skapinakis P, Rai D, Anagnostopoulos F, Harrison S, Araya R, Lewis G. Sleep disturbances and depressive symptoms: an investigation of their longitudinal association in a representative sample of the UK general population. Psychol Med 2013; 43(2): 329–39. [DOI] [PubMed] [Google Scholar]
- 56.Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev 2014; 18(6): 521–9. [DOI] [PubMed] [Google Scholar]
- 57.Sivertsen B, Harvey AG, Lundervold AJ, Hysing M. Sleep problems and depression in adolescence: results from a large population-based study of Norwegian adolescents aged 16–18 years. Eur Child Adolesc Psychiatry 2014; 23(8): 681–9. [DOI] [PubMed] [Google Scholar]
- 58.Gregory AM, Caspi A, Eley TC, Moffitt TE, O'Connor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol 2005; 33(2): 157–63. [DOI] [PubMed] [Google Scholar]
- 59.Faedda GL, Baldessarini RJ, Glovinsky IP, Austin NB. Pediatric bipolar disorder: phenomenology and course of illness. Bipolar Disord 2004; 6(4): 305–13. [DOI] [PubMed] [Google Scholar]
- 60.Ankers D, Jones SH. Objective assessment of circadian activity and sleep patterns in individuals at behavioural risk of hypomania. J Clin Psychol 2009; 65(10): 1071–86. [DOI] [PubMed] [Google Scholar]
- 61.Ritter PS, Höfler M, Wittchen H-U, Lieb R, Bauer M, Pfennig A, et al. Disturbed sleep as risk factor for the subsequent onset of bipolar disorder–data from a 10-year prospective-longitudinal study among adolescents and young adults. J Psychiatr Res 2015; 68: 76–82. [DOI] [PubMed] [Google Scholar]
- 62.Hernandez M, Marangoni C, Grant MC, Estrada J, Faedda GL. Parental reports of prodromal psychopathology in pediatric bipolar disorder. Curr Neuropharmacol 2017; 15(3): 380–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ritter PS, Marx C, Bauer M, Lepold K, Pfennig A. The role of disturbed sleep in the early recognition of bipolar disorder: a systematic review. Bipolar Disord 2011; 13(3): 227–37. [DOI] [PubMed] [Google Scholar]
- 64.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep 2008; 31(4): 473–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Anderson KN, Bradley AJ. Sleep disturbance in mental health problems and neurodegenerative disease. Nat Sci Sleep 2013; 5: 61–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. J Affect Disord 2013; 148(1): 66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McGlinchey EL, Reyes-Portillo JA, Turner JB, Mufson L. Innovations in practice: the relationship between sleep disturbances, depression, and interpersonal functioning in treatment for adolescent depression. Child Adolesc Ment Health 2017; 22(2): 96–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011; 135(1–3): 10–9. [DOI] [PubMed] [Google Scholar]
- 69.Pancheri C, Verdolini N, Pacchiarotti I, Samalin L, Delle Chiaie R, Biondi M, et al. A systematic review on sleep alterations anticipating the onset of bipolar disorder. Eur Psychiatry 2019; 58: 45–53. [DOI] [PubMed] [Google Scholar]
- 70.Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin Psychol Rev 2018; 63: 25–40. [DOI] [PubMed] [Google Scholar]
- 71.Liu X, Buysse DJ, Gentzler AL, Kiss E, Mayer L, Kapornai K, et al. Insomnia and hypersomnia associated with depressive phenomenology and comorbidity in childhood depression. Sleep 2007; 30(1): 83–90. [DOI] [PubMed] [Google Scholar]
- 72.Glozier N, O'Dea B, McGorry PD, Pantelis C, Amminger GP, Hermens DF, et al. Delayed sleep onset in depressed young people. BMC Psychiatry 2014; 14: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Urrila AS, Karlsson L, Kiviruusu O, Pelkonen M, Strandholm T, Marttunen M. Sleep complaints among adolescent outpatients with major depressive disorder. Sleep Med 2012; 13(7): 816–23. [DOI] [PubMed] [Google Scholar]
- 74.Murru A, Guiso G, Barbuti M, Anmella G, Verdolini N, Samalin L, et al. The implications of hypersomnia in the context of major depression: results from a large, international, observational study. Eur Neuropsychopharmacol 2019; 29(4): 471–81. [DOI] [PubMed] [Google Scholar]
- 75.Orchard F, Gregory AM, Gradisar M, Reynolds S. Self-reported sleep patterns and quality amongst adolescents: cross-sectional and prospective associations with anxiety and depression. J Child Psychol Psychiatry 2020; 61(10): 1126–37. [DOI] [PubMed] [Google Scholar]
- 76.Emslie G J, Armitage R, Weinberg WA, Rush AJ, Mayes TL, Hoffmann RF. Sleep polysomnography as a predictor of recurrence in children and adolescents with major depressive disorder. Int J Neuropsychopharmacol 2001; 4(2): 159–68. [DOI] [PubMed] [Google Scholar]
- 77.Emslie GJ, Kennard BD, Mayes TL, Nakonezny PA, Zhu L, Tao R, et al. Insomnia moderates outcome of serotonin-selective reuptake inhibitor treatment in depressed youth. J Child Adolesc Psychopharmacol 2012; 22(1): 21–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Armitage R, Hoffmann RF, Emslie GJ, Weinberg WA, Mayes TL, Rush AJ. Sleep microarchitecture as a predictor of recurrence in children and adolescents with depression. Int J Neuropsychopharmacol 2002; 5(3): 217–28. [DOI] [PubMed] [Google Scholar]
- 79.Salvatore P, Ghidini S, Zita G, Panfilis CD, Lambertino S, Maggini C, et al. Circadian activity rhythm abnormalities in ill and recovered bipolar I disorder patients. Bipolar Disord 2008; 10(2): 256–65. [DOI] [PubMed] [Google Scholar]
- 80.Lunsford-Avery JR, Judd CM, Axelson DA, Miklowitz DJ. Sleep impairment, mood symptoms, and psychosocial functioning in adolescent bipolar disorder. Psychiatry Res 2012; 200(2–3): 265–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gershon A, Singh MK. Sleep in adolescents with bipolar I disorder: stability and relation to symptom change. J Clin Child Adolesc Psychol 2017; 46(2): 247–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lewis KS, Gordon-Smith K, Forty L, Di Florio A, Craddock N, Jones L, et al. Sleep loss as a trigger of mood episodes in bipolar disorder: individual differences based on diagnostic subtype and gender. Br J Psychiatry 2017; 211(3): 169–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stanley IH, Hom MA, Luby JL, Joshi PT, Wagner KD, Emslie GJ, et al. Comorbid sleep disorders and suicide risk among children and adolescents with bipolar disorder. J Psychiatr Res 2017; 95: 54–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roybal DJ, Chang KD, Chen MC, Howe ME, Gotlib IH, Singh MK. Characterization and factors associated with sleep quality in adolescents with bipolar I disorder. Child Psychiatry Hum Dev 2011; 42(6): 724–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ritter PS, Marx C, Lewtschenko N, Pfeiffer S, Leopold K, Bauer M, et al. The characteristics of sleep in patients with manifest bipolar disorder, subjects at high risk of developing the disease and healthy controls. J Neural Transm 2012; 119(10): 1173–84. [DOI] [PubMed] [Google Scholar]
- 86.Diler RS, Goldstein TR, Hafeman D, Merranko J, Liao F, Goldstein BI, et al. Distinguishing bipolar depression from unipolar depression in youth: preliminary findings. J Child Adolesc Psychopharmacol 2017; 27(4): 310–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Harvey AG, Talbot LS, Gershon A. Sleep disturbance in bipolar disorder across the lifespan. Clin Psychol 2009; 16(2): 256–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baroni A, Hernandez M, Grant M, Faedda G. Sleep disturbances in pediatric bipolar disorder: a comparison between bipolar I and bipolar NOS. Front Psychiatry 2012; 3: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sebela A, Novak T, Kemlink D, Goetz M. Sleep characteristics in child and adolescent offspring of parents with bipolar disorder: a case control study. BMC Psychiatry 2017; 17: 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jones SH, Tai S, Evershed K, Knowles R, Bentall R. Early detection of bipolar disorder: a pilot familial high-risk study of parents with bipolar disorder and their adolescent children. Bipolar Disord 2006; 8(4): 362–72. [DOI] [PubMed] [Google Scholar]
- 91.Mansour HA, Monk TH, Nimgaonkar VL. Circadian genes and bipolar disorder. Ann Med 2005; 37(3): 196–205. [DOI] [PubMed] [Google Scholar]
- 92.Bollettini I, Melloni EMT, Aggio V, Poletti S, Lorenzi C, Pirovano A, et al. Clock genes associate with white matter integrity in depressed bipolar patients. Chronobiol Int 2017; 34(2): 212–24. [DOI] [PubMed] [Google Scholar]
- 93.Dahl RE. The regulation of sleep and arousal: development and psychopathology. Dev Psychopathol 1996; 8(1): 3–27. [Google Scholar]
- 94.Casement MD, Keenan KE, Hipwell AE, Guyer AE, Forbes EE. Neural reward processing mediates the relationship between Insomnia symptoms and depression in adolescence. Sleep 2016; 39(2): 439–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bradley AJ, Webb-Mitchell R, Hazu A, Slater N, Middleton B, Gallagher P, et al. Sleep and circadian rhythm disturbance in bipolar disorder. Psychol Med 2017; 47(9): 1678–89. [DOI] [PubMed] [Google Scholar]
- 96.Miadich SA, Shrewsbury AM, Doane LD, Davis MC, Clifford S, Lemery-Chalfant K. Children's sleep, impulsivity, and anger: shared genetic etiology and implications for developmental psychopathology. J Child Psychol Psychiatry 2020; 61(10): 1070–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. J Youth Adolesc 2015; 44(2): 405–18. [DOI] [PubMed] [Google Scholar]
- 98.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int 2006; 23(1–2): 497–509. [DOI] [PubMed] [Google Scholar]
- 99.Clarke G, Harvey AG. The complex role of sleep in adolescent depression. Child Adolesc Psychiatr Clin 2012; 21(2): 385–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Clarke G, McGlinchey EL, Hein K, Gullion CM, Dickerson JF, Leo MC, et al. Cognitive-behavioral treatment of insomnia and depression in adolescents: a pilot randomized trial. Behav Res Ther 2015; 69: 111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Moore T, Phillips N, Palermo T, Lah S. Acceptability, feasibility, and usability of a manualized cognitive behavioural programme for treatment of insomnia in children who sustained traumatic brain injury: a service providers’ perspective. Neuropsychol Rehabil 2021; 31(4): 583–600. [DOI] [PubMed] [Google Scholar]
- 102.Paine S, Gradisar M. A randomised controlled trial of cognitive-behaviour therapy for behavioural insomnia of childhood in school-aged children. Behav Res Ther 2011; 49(6): 379–88. [DOI] [PubMed] [Google Scholar]
- 103.Schlarb AA, Bihlmaier I, Velten-Schurian K, Poets CF, Hautzinger M. Short- and long-term effects of CBT-I in groups for school-age children suffering from chronic insomnia: the KiSS-program. Behav Sleep Med 2018; 16(4): 380–97. [DOI] [PubMed] [Google Scholar]
- 104.Freeman D, Sheaves B, Goodwin GM, Yu L-M, Nickless A, Harrison PJ, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry 2017; 4(10): 749–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Christensen H, Batterham PJ, Gosling JA, Ritterband LM, Griffiths KM, Thorndike FP, et al. Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight study): a randomised controlled trial. Lancet Psychiatry 2016; 3(4): 333–41. [DOI] [PubMed] [Google Scholar]
- 106.Harvey AG. A transdiagnostic intervention for youth sleep and circadian problems. Cogn Behav Pract 2016; 23(3): 341–55. [Google Scholar]
- 107.Dong L, Dolsen MR, Martinez AJ, Notsu H, Harvey AG. A transdiagnostic sleep and circadian intervention for adolescents: six-month follow-up of a randomized controlled trial. J Child Psychol Psychiatry 2020; 61(6): 653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Dong L, Gumport NB, Martinez AJ, Harvey AG. Is improving sleep and circadian problems in adolescence a pathway to improved health? A mediation analysis. J Consult Clin Psychol 2019; 87(9): 757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wichniak A, Wierzbicka A, Walęcka M, Jernajczyk W. Effects of antidepressants on sleep. Curr Psychiatry Rep 2017; 19(9): 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wilson S, Argyropoulos S. Antidepressants and sleep. Drugs 2005; 65(7): 927–47. [DOI] [PubMed] [Google Scholar]
- 111.Pagel J, Helfter P. Drug induced nightmares—an etiology based review. Hum Psychopharmacol 2003; 18(1): 59–67. [DOI] [PubMed] [Google Scholar]
- 112.Lepkifker E, Dannon P, Iancu I, Ziv R, Kotler M. Nightmares related to fluoxetine treatment. Clin Neuropharmacol 1995; 18(1): 90–4. [DOI] [PubMed] [Google Scholar]
- 113.Kirschner NT. Medication and dreams: changes in dream content after drug treatment. Dreaming 1999; 9(2–3): 195–200. [Google Scholar]
- 114.Sharpley AL, Cowen PJ. Effect of pharmacologic treatments on the sleep of depressed patients. Biol Psychiatry 1995; 37(2): 85–98. [DOI] [PubMed] [Google Scholar]
- 115.Kolla BP, Mansukhani MP, Bostwick JM. The influence of antidepressants on restless legs syndrome and periodic limb movements: a systematic review. Sleep Med Rev 2018; 38: 131–40. [DOI] [PubMed] [Google Scholar]
- 116.Gringras P, Nir T, Breddy J, Frydman-Marom A, Findling RL. Efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2017; 56(11): 948–57. [DOI] [PubMed] [Google Scholar]
- 117.Smits MG, van der Heijden K, Meijer AM, Coenen AM, Kerkhof GA. Melatonin improves health status and sleep in children with idiopathic chronic sleep-onset insomnia: a randomized placebo-controlled trial. J Am Acad Child Adolesc Psychiatry 2003; 42(11): 1286–93. [DOI] [PubMed] [Google Scholar]
- 118.Wilson S, Anderson K, Baldwin D, Dijk D-J, Espie A, Espie C, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders: an update. J Psychopharmacol 2019; 33(8): 923–47. [DOI] [PubMed] [Google Scholar]
- 119.Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol 2008; 23(7): 571–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Nurnberger JI J, Adkins S, Lahiri DK, Mayeda A, Hu K, Lewy A, et al. Melatonin suppression by light in euthymic bipolar and unipolar patients. Arch Gen Psychiatry 2000; 57(6): 572–9. [DOI] [PubMed] [Google Scholar]
- 121.Carpenter JS, Abelmann AC, Hatton SN, Robillard R, Hermens DF, Bennett MR, et al. Pineal volume and evening melatonin in young people with affective disorders. Brain Imaging Behav 2017; 11(6): 1741–50. [DOI] [PubMed] [Google Scholar]
- 122.Schwartz LA, Feeny NC. The nature of and behavioral treatment of sleep problems in youth with bipolar disorder. Int J Behav Consult Ther 2007; 3(1): 88. [Google Scholar]
- 123.Robillard R, Naismith SL, Rogers NL, Ip TK, Hermens DF, Scott EM, et al. Delayed sleep phase in young people with unipolar or bipolar affective disorders. J Affect Disord 2013; 145(2): 260–3. [DOI] [PubMed] [Google Scholar]
- 124.Harvey AG, Mullin BC, Hinshaw SP. Sleep and circadian rhythms in children and adolescents with bipolar disorder. Dev Psychopathol 2006; 18(4): 1147–68. [DOI] [PubMed] [Google Scholar]
- 125.Göder R, Fritzer G, Gottwald B, Lippmann B, Seeck-Hirschner M, Serafin I, et al. Effects of olanzapine on slow wave sleep, sleep spindles and sleep-related memory consolidation in schizophrenia. Pharmacopsychiatry 2008; 41(3): 92–9. [DOI] [PubMed] [Google Scholar]
- 126.Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull 1987; 101(2): 213. [PubMed] [Google Scholar]
- 127.Ivanenko A, Crabtree VM, Gozal D. Sleep and depression in children and adolescents. Sleep Med Rev 2005; 9(2): 115–29. [DOI] [PubMed] [Google Scholar]
- 128.Lofthouse N, Fristad M, Splaingard M, Kelleher K. Parent and child reports of sleep problems associated with early-onset bipolar spectrum disorders. J Fam Psychol 2007; 21(1): 114–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1192/bjo.2021.1076.
click here to view supplementary material
Data Availability Statement
Data availability is not applicable to this article as no new data were created or analysed in this study.