Abstract
Childhood obesity is a serious public health problem. Childhood obesity and overweight are associated with the appearance of coordination deficit disorder and can cause impaired motor performance. We searched online databases for all related articles using comprehensive international databases from the Medline PubMed Institute, Web of Science, ScienceDirect, SCOPUS, and PsycINFO up to December 20, 2020. Overall, 33 studies were included in this systematic review. The present review demonstrated that children with higher percentage of body fat had lower levels of moderate to vigorous physical activity, as well as decreased levels of gross motor coordination, as shown by tests for neuromuscular performance. These results corroborate the hypothesis that overweight and obesity in children and adolescents are associated, not only with insufficient performance during gross motor coordination activities, but also with a greater risk to physical health.
Systematic Review Registration
[https://www.crd.york.ac.uk/prospero/], identifier [CRD42020182935].
Keywords: obesity, metabolic syndrome, pediatric obesity, body mass index, motor skills
Introduction
Childhood overweight and obesity are one of the greatest public health challenges worldwide. The World Health Organization estimates that approximately 70 million children will be overweight or obese by 2025, as children below 5 years old have shown a rapid increase in the development of overweight and obesity in recent years (1). Childhood is a critical period for the development of overweight and obesity. Increased consumption of unhealthy sugar, sodium, and fats, in addition to ultra-processed foods, including sugar-sweetened beverages and high-energy, nutrient-poor packaged foods have been strongly associated with weight gain and several nutrition-related non-communicable diseases (2). The high rate of obesity is associated with an increase in the development of some disease conditions such as systemic arterial hypertension (3), insulin resistance (4), and stroke (5). In addition to these conditions, obesity can affect physical parameters such as motor performance and gross motor coordination, as they seem to be directly related to regular physical activity and body composition in children and adolescents (6).
Motor coordination corresponds to the congruous interactions between the nervous, skeletal, and sensory muscle systems, in order to produce precise motor actions, in addition to quick reactions to everyday situations, which involves proper development of muscle strength and the proper selection of muscles that control the performance of the movement (7). Notably, motor performance in childhood and adolescence may be related to the programming of physiological systems in adult life (8, 9).
Motor competence, on the other hand, is the ability to perform different motor actions, including coordination and gross motor skills (10). Gross motor competence is often defined as proficiency in a range of fundamental movement skills such as throwing, catching, and running, which are normally learned during preschool and early school years (11, 12). These provide a basis for children to develop more in specialized movement sequences, such those required in sports activities (13).
A growing body of studies have investigated the possible relationship between gross motor coordination and the level of adherence to participation in physical activity during adolescence. Most studies found a positive association between better performance in gross motor coordination and participation in physical activities (14, 15).
It is possible that children and adolescents with poor gross motor skills may not want to participate in physical activity, because it can be more challenging for. It is also plausible that among children with poor gross motor skills, sedentary activities (i.e., watching TV and computing games) may be more enjoyable options.
The muscle is characterized by plasticity and, therefore, is more likely to change its structure and function. In animals, accumulation of intramuscular fat caused stiffness in the muscle tissue, which caused less contractility and decreased strength in the gastrocnemius muscle (16). In humans, a longitudinal study carried out on growth and physical fitness related to health and motor competence in elementary school children showed that the pathways for the development of physical and motor fitness are related to the children’s body weight. Children who had a low or medium rate of development of physical fitness and motor competence were more likely to develop overweight or obesity at the end of primary school, regardless of sex and body mass index at baseline (17).
In this context, it is necessary to clarify how environmental factors can influence the appearance of overweight and obesity; in addition, it is necessary to understand the relationship between overweight and obesity and motor performance in childhood (18–20). Core motor tasks include bilateral and upper limb coordination, strength, balance, speed, and running agility.
Motor skills are acquired from the physiological maturation of the neuromuscular system and environmental factors (21) and correspond to a group of coordinated movements that children begin to learn during early childhood and involve locomotor skills and object control. Locomotor skills are used to move the body through space, such as running, galloping, and jumping. The object control task is the ability to manipulate and project objects such as throwing, catching, dribbling, kicking, hitting, and rolling (22).
Although the genetic and biological determinants of obesity can interact throughout life, the process that regulates the developmental trajectories of other potentially important behavioral factors linked to the status of body weight has not been investigated.
Another aspect to be noted is that few studies have explored the contribution of current body composition to motor performance of the research participants. Understanding the relationship between overweight and obesity and children’s physical activity can guide the development of interventions at different levels that may provide a better chance of increasing the levels of physical activity in the population. Therefore, the objectives of this study were to analyze the influence of overweight and/or obesity on motor performance and gross motor coordination in children and adolescents.
Methods and Materials
The protocol for this systematic review been published online (https://www.crd.york.ac.uk/prospero/) in PROSPERO (registration number CRD42020182935) and was reported as per Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) (12).
Search Strategy
This review was conducted in two phases, which included selection of studies followed by data extraction. Studies were selected from the search in the electronic databases Medline/PubMed (National Library of Medicine/Analysis of Medical Literature and Online Recovery System), Web of Science, ScienceDirect, SCOPUS, and PsycINFO, which was carried out in December 20, 2020. The following MeSH terms in Medline, PubMed, and DeCS in other databases were used as search filters: “obesity”; “pediatric obesity”; “metabolic syndrome”; “nutritional and metabolic diseases”; “body mass index”; and “motor skills”.
Selection of Studies
Selection of studies was performed independently by WB and RS, according to the following inclusion criteria: (a) original articles addressing metabolic changes related to motor skills; (b) studies assessing individuals aged between 5 years old and 14 years and 11 months old; (c) studies with control and experimental groups (overweight and/or obesity); and (d) articles with a sample size of less than 30 individuals. No language or period of publication was set. However, a search filter was activated for viewing studies performed only in humans. The following PICOS criteria were established: Population: children and adolescents; Intervention/exposure: motor training; Comparison: between sexes; Results: overweight/obesity, motor coordination; Study design: cross-sectional and longitudinal studies. Initially, the studies were pre-selected according to titles and abstracts. In the next stage of the study selection phase and after excluding duplicate articles, texts considered eligible were read in their entirety.
Data were collected from the selected studies based on the characteristics of the studies, the results, and the components used to assess the intervening factors were verified. For the qualitative synthesis of the data, the following characteristics of the studies were used: author’s name, year of publication, country, age variation, sex, nutritional status, total population, analyzed variables, body composition, and motor performance results.
Data Extraction
Selected abstracts were submitted to the second stage of analysis, in which two independent researchers reviewed the articles completely and, by consensus, excluded articles that did not meet the criteria. The following data from eligible articles were extracted: characteristics of the sample (mean age, distribution between sexes, and nutritional status), materials and methods (analyzed variables), and the main results found related to body composition and motor performance. The data extracted from the articles were collected using a standardized method among the authors. It was not possible to perform a meta-analysis in the present study, since there was substantial sample heterogeneity, in addition to the variability in the age range of the population of the studies, which could hinder the reliability of a meta-analysis.
Risk of Bias
The risk of bias was established through of a critical analysis of the studies selected using seven criteria for a methodological judgment supplied by the software Revman 5.3.0 program the Cochrane Handbook 23, developed for systematic reviews and available for free download (https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman/revman-5-download). Among the criteria that structure the bias assessment are (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other bias.
Results
Study Selection
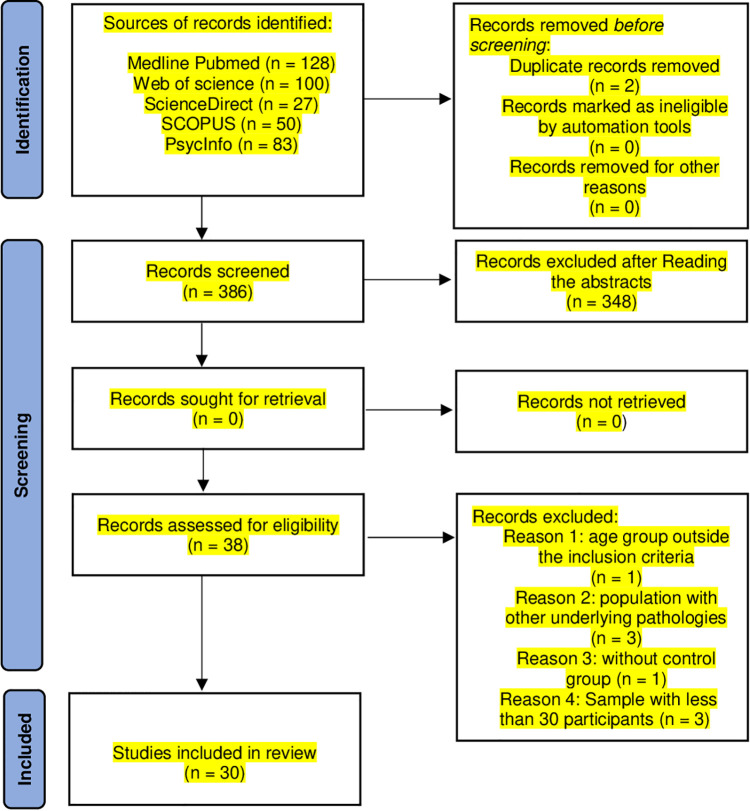
A total of 388 studies were identified in the literature search. Two duplicates were found. Of these 386 studies, 38 met the inclusion criteria based on the title and abstract. Finally, 33 studies ( Figure 1 ) were included in this review.
Figure 1.
A flow diagram of the selection strategy.
Description of Included Studies
Among the main findings of this review, 1 of the 30 selected articles included children aged between 5 and 7 years old (23), 15 assessed children with ages between 7 and 14 years old (20, 24–40), 6 articles included children between 6 and 10 years old (41–46), and 5 included children in other age groups (47–51). All studies were conducted with children of both sexes (20, 23–50, 52–55) ( Table 1 ).
Table 1.
Descriptions of the studies included in the systematic review: age, sex, and nutritional status.
| Author, year | Age range | Sex | Nutritional status | ||||
|---|---|---|---|---|---|---|---|
| Female | Male | Malnutrition | Eutrophic | Overweight | Obesity | ||
| (23) | 5 years | 324 | 370 | 59 (23 girls) moderate: 41 (22 girls) | 410 (200 girls) | 92 (45 girls) | 60 (17 girls) |
| (41) | 6.5–7.2 years | 369 | 412 | 8.1% (n = 63) | 75.9% (n = 593) | 8.8% (n = 69) | 7.2% (n = 56) |
| (42) | 6–10 years | 69 | 86 | – | – | 27.1% girls | 12.9% girls |
| 16.3% boys | 14.0% boys | ||||||
| (47) | Data performed at two different ages: 5 and 10 years | 307 | 361 | – | – | 5 years: 20.4% | 5 years: 21.7% |
| 10 years: 22.9% | 10years: 18.1% | ||||||
| (48) | 6–14 years | 2,787 | 2,351 | – | – | Subjects with high BMI: 1,526 | |
| (43) | 6–8 years | 204 | 200 | – | – | 14.7% girls | |
| 11% boys | |||||||
| (54) | 7–11 years | 155 | 178 | – | 205 | 72 | 54 |
| (24) | 8–11 years (Three years of intervention) | 108 (3rd year) | 123 (3rd year) | – | – | 3rd year: 23.4% girls and 23.5% boys | 3rd year:10.6% girls and 13.9% boys |
| 108 (5th year) | 126 (5th year) | 5th year: 21.4% girls and 28.9% boys | 5th year: 4.1% girls 3.9% boys | ||||
| (49) | 6–14 years | 657 (51.5%) | 619 (48.5%) | – | – | 20.70% girls | 5.02% girls |
| 17.69% boys | 7.47% boys | ||||||
| (26) | 9–12 years | Typical development:456 | 631 | – | 70.0% | 22.4% | 7.5% |
| Disorders of motor coordination and balance: 93 | 85 | – | 61.8% | 23.0% | 15.2% | ||
| Disorders of motor coordination and balance: 186 | 143 | – | 66.6% | 24.3% | 9.1% | ||
| (27) | 5–13 years (1st evaluation) | 1st evaluation: 1.188 | 1.329 | Longitudinal study: significant inverse associations within the follow-up subsample participants between z scores of BMI and KTK MQ at each point in time (i.e., baseline and follow-up) as well as over the 2-year course | |||
| 7–13 years (2nd evaluation) | 2nd evaluation: 371 | 383 | |||||
| (20) | 10 and 14 years (accompaniment) | 318 | 348 | – | 10 years: 507 | 116 | 43 |
| 14 years: 486 | 126 | 54 | |||||
| (28) | 10–13 years | 107 | 132 | – | 132 (56 girls) | – | 107 (51 girls) |
| (29) | 9–13 years | 268 | 322 | Children with coordination disorder: ↑ | |||
| BMI scores | |||||||
| (44) | 6–10 years | 48% | 52% | – | 50 | 42 | 8 |
| (30) | 7–10 years | 89 | 64 | – | – | 35 | 118 (65 girls) |
| (31) | 9–10 years | 951 | 1078 | – | 1,154 (577 girls) | 434 (230 girls) | 441 (144 girls) |
| (32) | 9–11 years | 1st wave: 1,120 | 1,158 | – | – | 30.1% | 9.7% |
| 2nd wave: 1,094 | 1,133 | 31.2% | 11.0% | ||||
| 3rd wave: 1,094 | 1,133 | 29.6% | 10.0% | ||||
| 4th wave: 1,032 | 1,054 | 32.1% | 10.5% | ||||
| 5th wave: 1,032 | 1,059 | 32.3% | 9.8% | ||||
| (33) | 11– 14 years | 120 | 140 | – | 103 (49 girls) | 86 (40 girls) | 71 (31 girls) |
| (34) | 8–10 years | 105 | 105 | – | 105 (52 girls) | 105 (53 girls) | – |
| (45) | Started: 6.8 ± 0,4 years | 301 | 314 | 7.5% | 77.8% | 8.1% | 6.6% |
| (50) | 5–12.8 years | 268 | 272 | – | 273 | 202 | 65 |
| (53) | 9–14 years | 268 | 322 | – | – | 90 (overweight/obese) | |
| (46) | 6.70 ± 0,42 years | 278 | 280 | 8.1% | 78.1% | 8.1% | 5.7% |
| (52) | 6–11 years | 335 | 341 | 04.28% (n = 29) | 68.77% (n = 465) | 11.24% (n = 76) | 12.28% (n = 83) |
| (36) | 10.4 ± 0.6 years | 42.7% | 57.3% | – | 177 | 36 (overweight/obese) | |
| (55) | 9–12 years | 281 | 315 | BMI only high than> 19.9 | |||
| (38) | 7–10 years | 343 | 313 | Children who eat breakfast almost every day have better functional motor skills and a lower BMI than children who do not regularly eat breakfast | |||
| (39) | 7–10 years | 198 | 182 | Thinness: 4 | 325 | 35 | Obesity: 10 |
| High thinness: 2 | Severe obesity: 4 | ||||||
| (40) | 7–14 years | 3,294 | 3,623 | – | – | 23.2% (overweight/obese) | |
Risk of Assessment
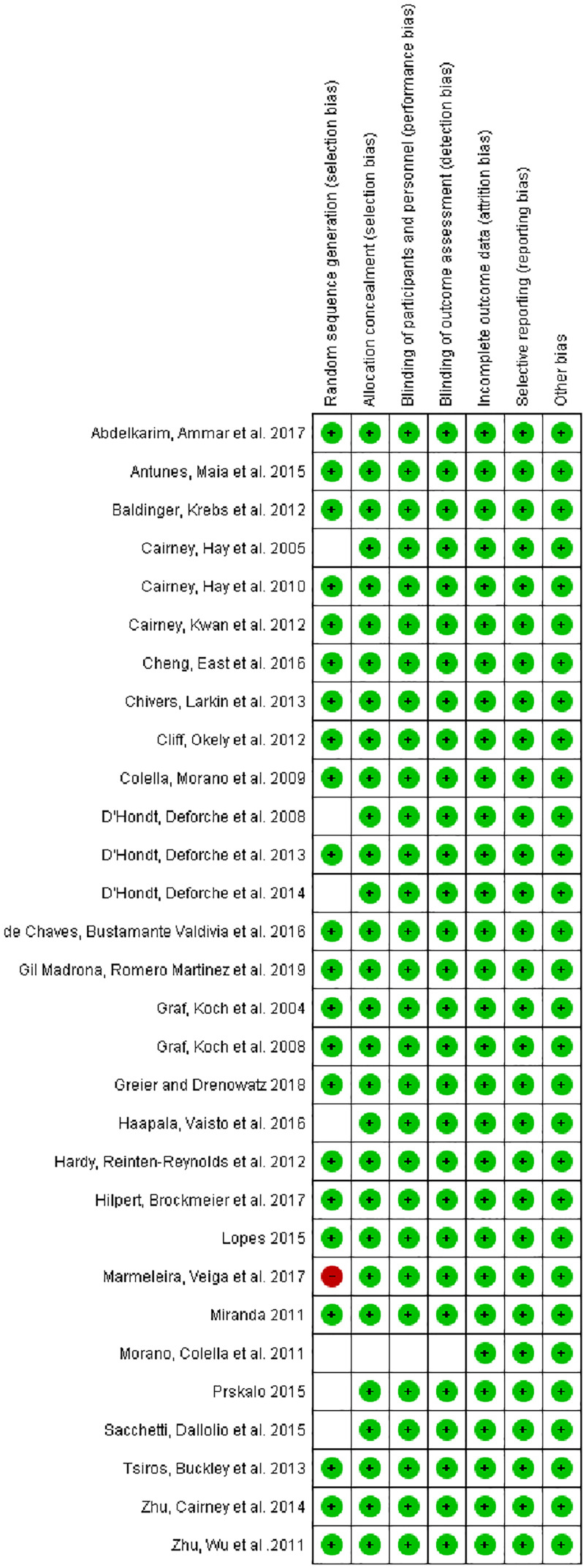
No studies with low risk of bias were excluded. The results are shown in Figures 2 and 3 .
Figure 2.
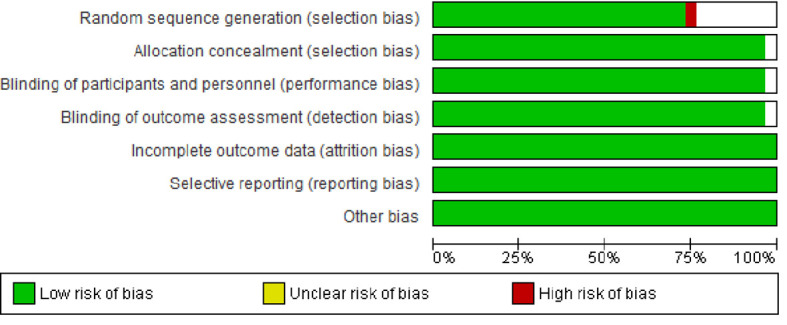
Risk of bias graph: review of authors’ judgements about each risk of bias item presented as percentages across all included studies.
Figure 3.
Risk of bias summary: review of authors’ judgements about each risk of bias item for each included study.
Nutritional Status and Age Group
The classification of the relationship between nutritional status and age group was heterogeneous among the selected articles. An article that included children between 5 and 7 years old found that most participants had normal nutritional status (23). In children between 7 and 14 years old, two articles reported an inverse association between BMI and motor coordination (27). In another article, children who ate breakfast almost every day had better functional motor skills and a lower BMI than children who did not eat breakfast regularly (38). Overweight was more prevalent in three articles (20, 24, 32), overweight and obesity in three articles (33, 35, 40), normal and overweight in one article (34), normal and obesity in one article (37), and obesity in one article (30), and in most studies, participants were classified as having normal weight (25, 26, 28, 31, 36, 39). In children between 6 and 10 years old, our analysis revealed a higher prevalence of normal weight (41, 44–46), while in two studies, children were classified as overweight and obesity (42, 43). Other articles had a different age range from those already presented. A study of children 5 and 10 years old found that 21.7% of children had obesity at 5 years, and at 10 years old, 22.9% were overweight (47). Another study with children 5–12.8 years old found that the majority of the population studied was eutrophic (50), whereas in another, the majority had overweight and obesity (47); in one study, 1,526 out of 5,138 children evaluated had high BMI (48).
This systematic review investigated the characteristics of body composition and motor performance in children, without orthopedic or neurological changes, notably related to gross motor coordination with or without exposure to physical activity. The results of analysis, specifically the main characteristics of the included studies, were organized according to the correlation between body composition and motor performance ( Table 1 ).
Body Composition Related to the Motor Performance of Children and Adolescents
Based on the theory of developmental plasticity, overweight and/or obesity in children and adolescents can interfere with motor performance, alter postural control, and, consequently, modify the state of motor coordination of these individuals. Taking this into account, six included studies assessed the research participants’ motor performance using running speed and agility tests such as the six-minute running test, TUDS (timed ascent and descent test), and other explosion tests (28, 34, 35, 37, 43, 54). In one of these studies, the authors found a relationship between an increase in the percentage of body fat and a decrease in the levels of moderate to vigorous physical activity (43).
Another study observed a decrease in the levels of static strength and explosive power in girls 7–11 years old with obesity, as well as in boys 10–11 years old with obesity (54). Balance and muscle strength power represent important components related to the ability of physical fitness that have to be sufficiently developed throughout life to perform sports and daily activities to decrease the risk of injuries and falls (56). Furthermore, Tsiros et al. (28) found a decrease in motor performance in children with obesity during the TUG (timed up and go), 6MWT (six-minute walk test), and TUDS tests. Other studies found that using explosion motor performance tests, overweight children had worse performance in the long jump and 10- and 20-m sprints; in addition, individuals with an increased percentage of body fat showed lower indexes in the long jump and repetition during sit-ups, in addition to a deficit in perceived physical capacity (34, 35).
Prevalence of overweight and obesity associated with the levels of physical fitness among primary school age children in Assiut city CPA (Checklist of Psychomotor Activities), KTK (Body coordination test for children: Koërper Koordination Test für Kinder), MABC (Movement Assessment Battery Test for Children), and BOTMP-SF (Bruininks–Oseretsky Test of Motor Proficiency—Short Form) was investigated. Three studies used MABC to assess global motor coordination and balance (26, 31, 50) in a population of 540, 2,029, and 2,057 children, respectively. Another four found a greater propensity to develop deficit of coordination in children with greater accumulation of body fat, BMI, and obesity, successively (32, 42, 47, 53). However, most studies used KTK to assess gross motor coordination.
In this review, worse performance of gross motor coordination in children with obesity was observed (27, 41, 44–46, 48, 49, 55). One study investigated only the participants’ balance and found a decrease in balance skills with increasing body mass (52). Furthermore, overweight was negatively associated with lower overall performance of movements (24), while children with obesity had mild motor difficulties (20); overweight and obesity were related to less perceived and real physical competence (33), in addition to lower performance in side jumping, standing long jump, 20-m speed back-and-forth running (38), and decreased motor skills (40). Notably, a study including 380 children revealed that the association between nutritional status and motor classification in boys and girls was not significant, which, according to the authors, neutralizes any influence of nutritional status on motor classification (39) ( Table 2 ).
Table 2.
Descriptions of the studies included in the systematic review.
| Author, Year | Country | Total population | Variables analyzed (Tests) | Results of body composition and motor performance |
|---|---|---|---|---|
| (23) | Spain | 694 children | BMI (body weight and stature); CPA | GIRLS: Laterality: ↓ Childhood with malnutrition; dynamic coordination: ↓ Obesity Childhood; ↑ BMI worse results in motor execution; tonic postural control: ↓ Childhood with overweight/obesity; balance: ↑ Childhood with low weight; ↑ BMI ↓ respiratory control; visual-motor coordination between normal weight and Obesity/overweight childhood: ↑ Childhood with normal weight; spatial orientation: ↑ Childhood with normal weight versus overweight. BOYS: ↑ BMI ↑ Laterality; respiratory control ↓ and visual-motor coordination ↑ in Obesity/overweight childhood. |
| (41) | Germany | 997 children | Height, body weight, BMI, SES, migratory background, motor skills: KTK and 6-min run, questionnaire on levels of daily and leisure activity, determination of sedentary activities | SES group ↓: ↑% obesity childhood, followed by the medium SES group and the high; obesity childhood group: ↑ migration history; overweight and obesity: ↓ gross motor development and resilience; how much ↑ SES, ↑ gross motor development; ↑ socioeconomic level, ↓ BMI and boys ↑ engine testing performance↑ computer/video game time: ↑ probability highest level of sports activity; history of migration: ↓ probability of participating in organized sports or being physically active at leisure |
| (42) | Portugal | 156 children | %GM e IMC (dobras cutâneas, peso e altura); teste Bruininks-Oseretsky de Proficiência Motora - Forma Curta | ↑ Cardiovascular disease risk: 27.5% girls and 24.4% boys excess body weight: 40% girls and 30.3% boys obesity childhood: ↓ gross motor skills and general motor proficiency; |
| (47) | Chile | 668 children | BMI (height and weight); Motor skills: BOTMP-SF test | 5 years: 20.4% overweight and 21.7% obesity; 10 years: 22.9% overweight and 18.1% obesity. Boys: ↑ total motor scores. Obesity childhood: ↓ gross and total motor skills (5 and 10 years) 5 obesity childhood years: ↓ performance in fine motor precision task (drawing lines). Childhood with obesity: ↓ motor skills from 5 to 10 years; ↓ motor proficiency at 5 years did not predict obesity or ↑ BMI. Overweight at 5 years was not enough to produce ↓ motor skills from 5 to 10 years; ↓ motor skill was associated with being overweight at 5 years |
| (48) | Peru | 5193 adolescents sea level, n = 1299 altitude, n = 1292 jungle, n = 2602 | BMI (height and weight); gross motor coordination: KTK; Physical fitness: Four EUROFIT battery tests (static and explosive muscle strength, flexibility, and speed/agility), abdominal muscle resistance of the Fitness gram battery and cardiorespiratory resistance of the American Alliance for Health, Physical Education, Recreation and Dance test battery; peak growth speed | Height, weight, and all motor performance test: ↑ with age except for sitting and reaching the boys outperform the girls in all tests. Girls: have 5 times + chances of ↓ gross motor coordination ↑ gross motor deficit with ↑ age; more mature girls and children: ↓ prone coordination deficits; ↑ BMI: ↑ prone to gross motor deficit. Children living at sea level or altitude: ↑ prone to gross motor deficit↑ flexible and ↑ strength: ↓ the probability of being diagnosed with deficit of gross motor coordination. |
| (43) | Finland | 512 children | Fat body mass,% body fat, and lean mass; weight and height; physical activity: heart rate and movement sensor, PANIC Physical Activity questionnaire; 50-m shuttle test: running speed and agility; 15-m running test; Martin vigorimeter: handgrip strength; test of standing distance jump: explosive strength of the lower limbs; abdominal test; modified flamingo balance test; box and block test: manual dexterity and speed of movement of the upper limb; sit and reach test: flexibility of the lumbar and hamstring muscles; pubertal status. | Boys: more active, ↓ fat mass and% body fat, ↓ 50-m run time and 15-m run test time, ↑ absolute handgrip power, ↑ jump test standing jump, ↑ test errors balance of the modified flamingo, ↓ cubes moved in the box and block test and ↓ distance achieved in the sit and reach test. Children ↑% body fat and levels ↓ moderate to vigorous physical activity: ↓ neuromuscular performance running and jumping tests. Children ↑ body fat content and ↑ MVPA levels: surpass overweight and ↓ children active in the 15-m sprint and the long jump test. Children ↑% of body fat and levels ↓ of physical activity: ↓ neuromuscular performance |
| (54) | Croatia | 333 children | Motor skills: polygon back - coordination, forward bending on a bench - flexibility, 15 ‘‘ manual touch - simple movement speed, long jump - explosive leg strength, flexed and static arm strength, abdominals - repetitive strength and high jump - MMII explosive force; % body fat (sum of subscapular skinfolds and triceps); body fat and fat-free mass; BMI (weight and height). | Obesity girls: between 9% and 13%. Obesity boys: range from 17% with age.7–9 years and 23% 10–11 years. Boys 7–9 years: N/S in motor skills when classified according to body weight. Boys 10–11 years old eutrophic: ↑ coordination, static, explosive and repetitive force. Girls 7–9 years old eutrophic: ↑ static strength and explosive power. Girls 10–11 years old eutrophic: ↑ static strength, explosive power, and coordination |
| (24) | Italy | 231 children | Anthropometric measurements (height, weight, BMI) and motor skills: Sit & Reach test, Forward Roll Test, Forward Throw 2 kg Medicine-ball test, long jump test, 20-m running speed test. | Beginning of the study: 35.8% of children ↑ weight (23.4% overweight childhood; 12.4% obesity childhood); after intervention: ↓ to 29.3% (25.3% overweight childhood; 4% obesity childhood). N/S in the various motor skills. There was an association between BMI and flexibility of the hips and lower back (Sit & Reach Test) or total dynamic body coordination (Advance Test). Overweight childhood: ↑ segmental movements (positive association with BMI), ↓ overall movement performance. |
| (49) | Portugal | 1,276 children | Gross motor coordination (MC): KTK; anthropometry: height and body mass; physical activity: Baecke’s questionnaire; and socioeconomic status (SES) | Overweight and obesity: 17.69% and 7.47%, respectively, for boys, and 20.70% and 5.02% for girls. Eutrophic children: overcome childhood with obesity in all tests of gross motor coordination. Gross scores when walking backwards and moving sideways: ↑ with age and performance boys ↑ when moving sideways |
| (26) | Taiwan | 2,057 children | MABC test; anthropometry: height, body weight, waist and hip circumference, BMI | Manual dexterity and ball skills in girls: scores ↑ mastery of manual dexterity; most anthropometric data (weight, waist circumference): ↑ group with developmental coordination disorder and balance deficits; children in the group with developmental coordination disorder and balance deficits: 2× ↑ probability of being obese |
| (27) | Belgium | 2,517 children initially n = 754 in the second evaluation | BMI, gross motor coordination: KTK, total physical activity: questionnaire | Performance ↓ in KTK at baseline predicted ↑ BMI z score; ↑ baseline BMI z score predicted ↓ KTK performance |
| (20) | Australia | 666 children and adolescents Evaluated at 10 and 14 years old | Anthropometric measurements: height, weight, BMI; engine performance: MAND | 14 years old eutrophic children group: ↑ general motor performance scores. 14 years: ↑ prevalence obesity childhood with mild motor difficulties. ↓ motor performance and BMI ratio; tasks + affected by BMI: those that involved a change in the center of mass; morphological restrictions of overweight and obesity affect the performance of motor tasks in tasks involving changes in the center of mass, but not static measures of strength |
| (28) | Australia | 239 children Obese n = 107 Normal weight n = 132 | Anthropometry: height, weight, BMI; body composition: dual-energy absorptiometry by x-rays; physical activity: uniaxial accelerometers; demographic/background information; activity capacity restrictions: TUDS; 6MWT, TUG; limitation of participation (performance): Multimedia Activity Recall for Children and Adolescents, QVRS | Obesity childhood: ↓ average accelerometry count, maternal education, and family income. Obesity childhood: ↑ mass, BMI, % fat and fat-free mass; obese group: restrictions on the ability to perform the TUG, the 6MWT and the TUDS; Obesity childhood: ↓ time in self-care activities and without physical difficulty in daily activities; obese: impaired quality of life |
| (29) | Canada | 590 children and adolescents | Height, weight (BMI), and % body fat by bioelectrical impedance analysis; BOTMP-SF; active game participation: participation questionnaire | Youth with Developmental Coordination Disorder: ↑% body fat. Boys with Developmental Coordination Disorder: ↑ BMI of all young people. Boys with Developmental Coordination Disorder: ↑ active play participation associated with ↑ BMI and% body fatBoys with Developmental Coordination Disorder: opposite relationship is observed |
| (44) | Belgium | 108 children | Anthropometry: body height, body weight, BMI, % body fat; level of gross motor coordination: KTK; FPAQ | Progression level of gross motor coordination over a period of 2 years was different, depending on the children’s weight status; eutrophic childhood group: ↑ progress; in addition to BMI (negative predictor), participation in sports organized within a sports club (positive predictor) determines the gross performance of motor coordination 2 years later |
| (30) | Australia | 175 children | Anthropometry: height, weight, BMI; fundamental movement skills: TGMD-2 age groups: 7–8 years and 9–10 years; all other SFM: 6 to 7 years and 8 to 10 years | 77% obesity childhood; boys: ↑ BMI and performance in object control skills; girls: ↑ proficiency in locomotor skills; all 12 skills in all age groups: domain prevalence was ↓ among overweight/Obesity childhood |
| (31) | Taiwan | 2,029 children | Height, weight, % body fat; coordination: MABC | Boys and girls with obesity: ↓ general motor coordination, mainly in static and dynamic balance; boys: ↑ developmental coordination disorder (DCD) in the obesity group |
| (32) | Canada | 2,278 children 1,979 performed the motor tests | Height, weight, BMI, waist circumference; identification of developmental coordination disorder: BOTMP-SF | Balance and total impairment score: ↑ obesity and overweight; girls: ↑ balance impairment score in obesity and overweight groups |
| (33) | Italy | 260 children | Anthropometry: height, weight, BMI; self-physical description questionnaire: perceived coordination, body fat and sports competence; drawings of Collins Children’s Figures: body image; Perceived Physical Capacity Scale: strength, speed and agility and tests involving standing long jump, 2 kg medicinal ball toss, 10 × 5 m shuttle race and 20- and 30-m sprints. | Overweight and obesity girls: ↓ perceived and real physical competence, ↑ perceived body fat and ↑ body dissatisfaction eutrophic children: ↑ standing long jump performance, 20-m shuttle run and 30-m run. Obesity childhood: ↑ pitch performance |
| (34) | Italy | 210 children Normal weight n = 105 Overweight n = 105 | Height, weight, BMI; motor performance tests: 3 explosion tests (standing long jump, medicine ball throw, basketball throw; 2 speed tests: 10- and 20-m sprint; body image: children’s drawings of Collins; scale of perception of physical ability for children | Scale of perception of physical ability for children: overweight childhood showed ↑ average body discrepancy; overweight childhood explosion tests: ↑ ball and basketball performance; long jump and 10- and 20-m sprint: eutrophic childhood ↑ performance |
| (45) | Germany | 615 children | Antropometria: altura, peso e IMC; testes motores: TC6; coordenação motora: KTK | Intervention schools: Overweight and Obesity childhood: ↓ motor test results on all tasks |
| (50) | Belgium | 540 children | Anthropometry: height, weight, and BMI; fine motor control: MABC in two postural conditions different: sitting and standing in a tandem position on a balance beam (BB) | Tandem position on balance beam: ↓ obese score in seated condition: N/S between overweight and eutrophic scores performance in placing obese pins: ↓ when seated. |
| (53) | Canada | 578 children | BOTMP-SF, % body fat, weight, height, and BMI | Children with coordination and balance deficit disorder: + prone to being overweight and obesity childhood (analyzing% body fat) |
| (46) | Germany | 668 children | Anthropometry; gross motor development: KTK; resistance: TC6; children’s leisure assessment questionnaires | Boys with coordination and balance deficit disorder: risk factor for overweight and obesity in childhood and early adolescence |
| (52) | Egypt | 676 children | Anthropometry: body height, body weight and BMI; physical fitness: DMT 6-18 | Overweight childhood: 11.24%; obese: 12.28% running and strength skills: negatively + affected by ↓ body weight balance skills affected by ↑ body mass; weight and endurance skills: affected by abnormal ↑ or ↓ body weight |
| (36) | Áustria | 213 classmates | Height, weight, and BMI; DMT 6–18: resistance, power, speed, coordination, and agility; 6MWT questionnaire participation in sports and use of media; migration status | Eutrophic childhood: 83% adolescents overweight/obesity participants: ↓ motor skills development Participants who lost weight or maintained normal weight: ↑ overall motor skill score over 4 years of follow-up + time using media eutrophic adolescents: ↑ performance in various tests of motor skills motor skills during the 4-year observation period: ↑ absolute performance more pronounced in eutrophic adolescents at baseline |
| (55) | Portugal | 596 children | Anthropometry: weight, % fat, height, waist circumference and BMI; motor coordination: KTK; 20-m shuttle-run test: assess cardiorespiratory fitness | Girls: ↓ CM and ↑% body fat BMI, waist circumference, % body fat and waist/height ratio: related to ↓ CM in both sexes, except for the waist/height ratio after adjustments for girls |
| (38) | Switzerland | 656 children | Coordinating and conditional skills: lateral jump, touch, standing jump, 20 m and shuttle run; weight, height, and BMI; nutritional research | Eutrophic childhood: ↑ running performance, side jump, long jump, and shuttle run. Low weight group: ↑ shuttle race performance. Obesity and overweight group: ↓ performance on 4 items of the motor functional tests (lateral jump, standing long jump, 20 m speed and shuttle run) |
| (39) | Brazil | 380 children | Motor performance: MABC-2—manual dexterity, throw receive skills and static and dynamic balance skills. Antrhropometry: weight, height, and BMI | Male: ↑ movement difficulty. Between ages: association N/S; age ranges by skill compared: significant difference between age range and static and dynamic balance skills (between ages 7 and 9 and between ages 7 and 10) motor classification and nutritional status by sex: N/S, which neutralizes any influence of nutritional status on motor classification |
| (40) | Australia | 6917 children | Demographic information: socioeconomic status (SES); fundamental movement skills: sprinting, vertical jumping side canter and jumping and object control skills (catching, throwing by the arm and kicking); cardiorespiratory endurance fitness: 20-m shuttle race test, parents reports of physical activities organized or not; validated physical activity recovery for adolescents questionnaire | Girls: ↑ low competence skills object control association with functional movement screen and inadequate cardiorespiratory fitness. There was no association between low competence and object control skills and overweight students/obesity. Motor skills: ↑ low overweight. Competence association/obesity; consistent associations for most individual motor skills |
BMI, body mass index; CPA, Checklist of Psychomotor Activities; SES, socioeconomic status; KTK, Body coordination test for children, Koërper Koordination Test für Kinder); N/S, not significant; BOTMP-SF, Bruininks–Oseretsky Test of Motor Proficiency—Short Form; MABC, Movement Assessment Battery Test for Children; MAND, McCarron Assessment of Neuromuscular Development; TUDS, timed ascent and descent test; 6MWT, six-minute walk test; TUG, timed up and go; HRQoL, related quality of life; FPAQ, Flemish Physical Activity Questionnaire; TGMD-2, gross motor development test 2; DMT 6–18, German engine test/Deutscher Motorik Test; MLG, Fat-free mass; SLJ, standing long jump; MVPA, moderate to vigorous physical activity; MT, Hand movement time.
Discussion
Overall, the results of this review confirmed the hypothesis that overweight and obesity can negatively affect motor performance and gross motor coordination in children and adolescents, although age, nutritional status, and the measures of motor performance analyzed were different among the investigated studies.
It is well recognized that motor performance in some tests is negatively affected by higher body weight (23, 53). In analyzing the magnitude of the relationships between gross motor coordination, physical activity, and physical conditioning, weight was strongly associated with age and sex in gross motor coordination tests (57, 58). A meta-analysis showed that age was positively associated with locomotion, object control, and stability skills. It is not surprising that the older children are, the better their skills, as long as they continue to participate in activities that develop these skills. Motor development in young children is influenced by biological maturation, and after this period, it depends more on practice and opportunity. Thus, it is conceivable that the relationship between age and gross motor competence may change over the developmental periods of early childhood, preschool, childhood, and adolescence. Notably, although primary evidence confirms age as a positive correlate in most aspects of motor competence, some studies (across all types of motor competence) have not found this relationship (59). One study that found age to be a negative correlate involved adolescents and suggested that the decline in girls’ motor competence was due to a reduction in the opportunity to be active (60). It then appears that gross motor coordination improves with age during middle childhood and adolescence, although there is a lack of consensus on sex-related differences between age groups and the gross motor coordination tests used.
In contrast to object control-related skills, which tend to be more static, locomotor activities involve changing or controlling a larger body mass that impedes functional movement and contributes to a higher rate of lower limb orthopedic changes, such as tibia rod and plantar pressure, among children with obesity (61). The negative association between gross motor activity and higher BMI may reflect the composition of assessments where the compound requires better motor coordination while moving and controlling the body, compared to object control skills. Sex, on the other hand, seems to relate differently to various aspects of gross motor competence. Male sex was considered a strong positive correlate of object control and motor coordination tasks, with pre-maturation biological differences being considered for boys and girls, especially in reference to skills such as throwing (62). Research has shown that, compared to girls, boys receive greater encouragement, support, and opportunities to engage in physical activity and sports at home and at school. Thus, girls’ opportunities to improve their gross motor skills may be limited (63, 64).
Biological and environmental factors can influence motor coordination, favoring both boys and girls. The activities performed by different sexes facilitate the performance in certain items of motor coordination; therefore, sex can be an intervening factor in motor performance. Regarding overweight and obesity, one of the hypotheses that can explain the interference in the performance related to gross motor coordination tasks is that during the tasks of supporting the body weight, there is a higher proportion of fat mass that must be supported or moved against the action of the force of gravity (65).
Another factor that can interfere with the performance in motor coordination is time, as can be seen in a longitudinal study that investigated the relationship between children’s weight and the level of gross motor coordination over time. Baseline measurements were collected from 2,517 children (5 to 13 years old, 52.8% boys). Measurements included the following: height and body weight for the calculation of BMI and gross motor coordination through KTK. After 2 years, 754 participants (7 to 13 years old, 50.8% boys) underwent anthropometric and KTK assessments again. There was a positive relationship between the worst motor performance at KTK at baseline and an increase in BMI. In addition, a higher baseline BMI score also predicted a decrease in KTK performance, suggesting that children’s weight negatively influences the level of gross motor coordination in the future and vice versa. Therefore, prevention and intervention initiatives through physical activity must consider this reciprocal causal relationship over the development time (50).
Furthermore, physical activity has a potential protective effect against the development of metabolic diseases during childhood and reduces the prevalence of cardiovascular diseases and diabetes, and morbidity and mortality of adult individuals prematurely (66). Thus, regular physical activity and adequate nutrition during the years of child growth and development increases the possibility of a healthy pattern of physical maturation consistent with a child’s genetic potential (67). Dudas et al. (2008) found that overweight children showed lower participation in sports clubs, while even more children with healthy weight were able to ride a bicycle.
In this perspective, this review demonstrated that children with a higher percentage of body fat had lower levels of moderate to vigorous physical activity, as shown by the neuromuscular performance in running and long jump tests (43). In addition, Tsiros et al. (28) performed a study on 239 children, of whom 107 had obesity and 132 had a healthy weight. They observed restrictions in the group with obesity regarding the ability to perform TUG, 6MWT, and TUDS. Morano et al. (33) evaluated 260 students between 11 and 14 years old through the questionnaire of physical self-description: perceived coordination, body fat, and sports competence; Collins Children’s Figures Drawings: body image; Perceived Physical Capacity Scale: strength, speed, and agility, and tests involving standing long jump, and 20- and 30-m sprints. Overweight and obese girls reported less perceived and real physical competence, a higher index of perceived body fat, and body dissatisfaction. Eutrophic childhood, on the other hand, showed better performance in standing long jump, shuttle run, and 20-m and 30-m run.
It is important to note that the mechanisms involving the neuroendocrine and musculoskeletal systems interact with each other and can explain the associations between weight and performance in gross motor coordination tests. Scientific literature demonstrates that stimuli from greater muscle activity are capable of promoting in their microenvironment the synthesis of chemical compounds called myokines. Among these, BDNF (brain-derived neurotrophic factor) and, recently, irisin stand out, because they are able to overcome the blood–brain barrier and can promote a positive outcome in both the cognitive and motor domains (68, 69).
For several years, muscles were considered targets for hormonal action; however, there is growing evidence that muscles, in a retrograde manner, exert unique forms of control over the CNS that affect motor behavior. Therefore, increasing evidence indicates that neural and muscular systems maintain some degree of plasticity throughout life, demonstrating that environmental factors influence the development of the musculoskeletal system and, as a consequence, motor performance.
Conclusion
Our results corroborate the hypothesis that overweight and, especially, obesity in children and adolescents are associated not only with insufficient performance during gross motor coordination activities, but also with an increased risk to physical health. It is, therefore, necessary to prevent childhood obesity and reduce the weight of affected children, and promote healthy eating and physical activities in daycare centers, schools, and homes. To be effective, in addition to the educational sector, all sectors of society must be mobilized so that the negative effect of commercial food products on children’s diets will be reduced.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author Contributions
WB and MSF contributed to research conception, data collection, interpretation of results, and critical review of the article. RS, KS, ASS, MS, and AS contributed to data analysis and interpretation, drafting, and critical review of the article. SS and VO contributed to data collection and critical review of the article. All authors contributed to the article and approved the submitted version.
Funding
The authors thank the “Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) – Edital PROPG n° 02/2021” and the “Conselho Nacional de Desenvolvimento Científico e Tecnológico” (CNPq) for their financial support. We would like to thank Editage (www.editage.com) for English language editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
References
- 1. WHO . Facts and Figures on Childhood Obesity (2020). Available at: http://www.who.int/end-childhood-obesity/facts/en/ (Accessed 28 Dec 2020).
- 2. Popkin BM, Barquera S, Corvalan C, Hofman KJ, Monteiro C, Ng SW, et al. Towards Unified and Impactful Policies to Reduce Ultra-Processed Food Consumption and Promote Healthier Eating. Lancet Diabetes Endocrinol (2021) 9:462–70. doi: 10.1016/S2213-8587(21)00078-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seravalle G, Grassi G. Obesity and Hypertension. Pharmacol Res (2017) 122:1–7. doi: 10.1016/j.phrs.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 4. Polsky S, Ellis SL. Obesity, Insulin Resistance, and Type 1 Diabetes Mellitus. Curr Opin Endocrinol Diabetes Obes (2015) 22:277–82. doi: 10.1097/MED.0000000000000170 [DOI] [PubMed] [Google Scholar]
- 5. Tang XN, Liebeskind DS, Towfighi A. The Role of Diabetes, Obesity, and Metabolic Syndrome in Stroke. Semin Neurol (2017) 37:267–73. doi: 10.1055/s-0037-1603753 [DOI] [PubMed] [Google Scholar]
- 6. Malina RM. Physical Growth and Biological Maturation of Young Athletes. Exercise Sport Sci Rev (1994) 22:389–433. doi: 10.1249/00003677-199401000-00012 [DOI] [PubMed] [Google Scholar]
- 7. Kiphard EJ, Schilling F. The Hamm-Marburg Body Control Test for Children. Monatsschrift Fur Kinderheilkunde (1970) 118:473–9. [PubMed] [Google Scholar]
- 8. Rizzo NS, Ruiz JR, Hurtig-Wennlof A, Ortega FB, Sjostrom M. Relationship of Physical Activity, Fitness, and Fatness With Clustered Metabolic Risk in Children and Adolescents: The European Youth Heart Study. J Pediatr (2007) 150:388–94. doi: 10.1016/j.jpeds.2006.12.039 [DOI] [PubMed] [Google Scholar]
- 9. Stabelini Neto A, Sasaki JE, Mascarenhas LP, Boguszewski MC, Bozza R, Ulbrich AZ, et al. Physical Activity, Cardiorespiratory Fitness, and Metabolic Syndrome in Adolescents: A Cross-Sectional Study. BMC Public Health (2011) 11:674. doi: 10.1186/1471-2458-11-674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Venetsanou F, Kambas A, Ellinoudis T, Fatouros I, Giannakidou D, Kourtessis T. Can the Movement Assessment Battery for Children-Test be the “Gold Standard” for the Motor Assessment of Children With Developmental Coordination Disorder? Res Dev Disabil (2011) 32:1–10. doi: 10.1016/j.ridd.2010.09.006 [DOI] [PubMed] [Google Scholar]
- 11. Branta C, Haubenstricker J, Seefeldt V. Age Changes in Motor Skills During Childhood and Adolescence. Exercise Sport Sci Rev (1984) 12:467–520. doi: 10.1249/00003677-198401000-00015 [DOI] [PubMed] [Google Scholar]
- 12. Gallahue D OJ. Understanding Motor Development: Infants, Children, Adolescents, Adults. Boston: McGrawHill; (2006). [Google Scholar]
- 13. Clarke JE MJ. The Mountain of Motor Development: A Metaphor. Natl Assoc Sport Phys Educ (2002) 45:163–90. [Google Scholar]
- 14. Lubans DR, Morgan PJ, Cliff DP, Barnett LM, Okely AD. Fundamental Movement Skills in Children and Adolescents: Review of Associated Health Benefits. Sports Med (2010) 40:1019–35. doi: 10.2165/11536850-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 15. Holfelder BS N. Relationship of Fundamental Movement Skills and Physical Activity in Children and Adolescents: A Systematic Review. Psychol Sport Exercise (2014) 15:382–91. doi: 10.1016/j.psychsport.2014.03.005 [DOI] [Google Scholar]
- 16. Rahemi H, Nigam N, Wakeling JM. The Effect of Intramuscular Fat on Skeletal Muscle Mechanics: Implications for the Elderly and Obese. J R Soc Interface (2015) 12:20150365. doi: 10.1098/rsif.2015.0365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rodrigues LP, Stodden DF, Lopes VP. Developmental Pathways of Change in Fitness and Motor Competence Are Related to Overweight and Obesity Status at the End of Primary School. J Sci Med Sport (2016) 19:87–92. doi: 10.1016/j.jsams.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 18. Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical Activity in US Youth: Effect of Race/Ethnicity, Age, Gender, and Weight Status. Med Sci Sports Exercise (2010) 42:2211–21. doi: 10.1249/MSS.0b013e3181e1fba9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malina RM, Beunen GP, Classens AL, Lefevre J, Vanden Eynde BV, Renson R, et al. Fatness and Physical Fitness of Girls 7 to 17 Years. Obes Res (1995) 3:221–31. doi: 10.1002/j.1550-8528.1995.tb00142.x [DOI] [PubMed] [Google Scholar]
- 20. Chivers P, Larkin D, Rose E, Beilin L, Hands B. Low Motor Performance Scores Among Overweight Children: Poor Coordination or Morphological Constraints? Hum Movement Sci (2013) 32:1127–37. doi: 10.1016/j.humov.2013.08.006 [DOI] [PubMed] [Google Scholar]
- 21. Catenassi FZM, Bastos CB, Basso L, Gerage AM. Relationship Between Body Mass Index and Gross Motor Skill in Four to Six Year-Old Children. Rev Bras Med Esport (2007) 13:203e–6e. doi: 10.1590/S1517-86922007000400003 [DOI] [Google Scholar]
- 22. Utley A, Astill SL. Developmental Sequences of Two-Handed Catching: How do Children With and Without Developmental Coordination Disorder Differ? Physiother Theory Pract (2007) 23:65–82. doi: 10.1080/09593980701211838 [DOI] [PubMed] [Google Scholar]
- 23. Gil Madrona P, Romero Martinez SJ, Saez-Gallego NM, Ordonez Camacho XG. Psychomotor Limitations of Overweight and Obese Five-Year-Old Children: Influence of Body Mass Indices on Motor, Perceptual, and Social-Emotional Skills. Int J Environ Res Public Health (2019) 16:427. doi: 10.3390/ijerph16030427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sacchetti R, Dallolio L, Musti MA, Guberti E, Garulli A, Beltrami P, et al. Effects of a School Based Intervention to Promote Healthy Habits in Children 8-11 Years Old, Living in the Lowland Area of Bologna Local Health Unit. Annali Di Igiene: Med Preventiva E Di Comunita (2015) 27:432–46. doi: 10.7416/ai.2015.2030 [DOI] [PubMed] [Google Scholar]
- 25. Boucher F, Handrigan GA, Mackrous I and Hue O. Childhood Obesity Affects Postural Control and Aiming Performance During an Upper Limb Movement. Gait Posture (2015) 42:116–21. doi: 10.1016/j.gaitpost.2015.04.016 [DOI] [PubMed] [Google Scholar]
- 26. Zhu YC, Cairney J, Li YC, Chen WY, Chen FC and Wu SK. High Risk for Obesity in Children With a Subtype of Developmental Coordination Disorder. Res Dev Disabil (2014) 35:1727–33. doi: 10.1016/j.ridd.2014.02.020 [DOI] [PubMed] [Google Scholar]
- 27. D’Hondt E, Deforche B, Gentier I, Verstuyf J, Vaeyens R, Bourdeaudhuij I, et al. A Longitudinal Study of Gross Motor Coordination and Weight Status in Children. Obes (Silver Spring) (2014) 22:1505–11. doi: 10.1002/oby.20723 [DOI] [PubMed] [Google Scholar]
- 28. Tsiros MD, Buckley JD, Howe PR, Olds T, Walkley J, Taylor L, et al. Day-To-Day Physical Functioning and Disability in Obese 10- to 13-Year-Olds. Pediatr Obes (2013) 8:31–41. doi: 10.1111/j.2047-6310.2012.00083.x [DOI] [PubMed] [Google Scholar]
- 29. Cairney J, Kwan MY, Hay JA, Faught BE. Developmental Coordination Disorder, Gender, and Body Weight: Examining the Impact of Participation in Active Play. Res Dev Disabil (2012) 33:1566–73. doi: 10.1016/j.ridd.2012.02.026 [DOI] [PubMed] [Google Scholar]
- 30. Cliff DP, Okely AD, Morgan PJ, Jones RA, Steele JR, Baur LA. Proficiency Deficiency: Mastery of Fundamental Movement Skills and Skill Components in Overweight and Obese Children. Obes (Silver Spring) (2012) 20:1024–33. doi: 10.1038/oby.2011.241 [DOI] [PubMed] [Google Scholar]
- 31. Zhu YC, Wu SK, Cairney J. Obesity and Motor Coordination Ability in Taiwanese Children With and Without Developmental Coordination Disorder. Res Dev Disabil (2011) 32:801–7. doi: 10.1016/j.ridd.2010.10.020 [DOI] [PubMed] [Google Scholar]
- 32. Cairney J, Hay J, Veldhuizen S, Missiuna C, Mahlberg N, Faught BE. Trajectories of Relative Weight and Waist Circumference Among Children With and Without Developmental Coordination Disorder. CMAJ: Can Med Assoc J J L’Association Med Can (2010) 182:1167–72. doi: 10.1503/cmaj.091454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Morano M, Colella D, Robazza C, Bortoli L, Capranica L. Physical Self-Perception and Motor Performance in Normal-Weight, Overweight and Obese Children. Scandinavian J Med Sci Sports (2011) 21:465–73. doi: 10.1111/j.1600-0838.2009.01068.x [DOI] [PubMed] [Google Scholar]
- 34. Colella D, Morano M, Robazza C, Bortoli L. Body Image, Perceived Physical Ability, and Motor Performance in Nonoverweight and Overweight Italian Children. Perceptual Motor Skills (2009) 108:209–18. doi: 10.2466/pms.108.1.209-218 [DOI] [PubMed] [Google Scholar]
- 35. Morano M, Rutigliano I, Rago A, Pettoello-Mantovani M, Campanozzi A. A Multicomponent, School-Initiated Obesity Intervention to Promote Healthy Lifestyles in Children. Nutrition (2016) 32:1075–80. doi: 10.1016/j.nut.2016.03.007 [DOI] [PubMed] [Google Scholar]
- 36. Greier K, Drenowatz C. Bidirectional Association Between Weight Status and Motor Skills in Adolescents: A 4-Year Longitudinal Study. Wiener Klinische Wochenschrift (2018) 130:314–20. doi: 10.1007/s00508-017-1311-y [DOI] [PubMed] [Google Scholar]
- 37. Elshemy S. Comparative Study: Parameters of Gait in Down Syndrome Versus Matched Obese and Healthy Children. Egyptian J Med Hum Genet (2013) 14:285–91. doi: 10.1016/j.ejmhg.2012.11.007 [DOI] [Google Scholar]
- 38. Baldinger N, Krebs A, Muller R, Aeberli I. Swiss Children Consuming Breakfast Regularly Have Better Motor Functional Skills and Are Less Overweight Than Breakfast Skippers. J Am Coll Nutr (2012) 31:87–93. doi: 10.1080/07315724.2012.10720013 [DOI] [PubMed] [Google Scholar]
- 39. Miranda T, Beltrame T, Cardoso F. Motor Performance and Nutritional Status of Schoolchildren With and Without Developmental Coordination Disorder. Rev Bras Cineantropometria E Desempenho Humano (2010) 13(1):59–6. doi: 10.5007/1980-0037.2011v13n1p59 [DOI] [Google Scholar]
- 40. Hardy LL, Reinten-Reynolds T, Espinel P, Zask A, Okely AD. Prevalence and Correlates of Low Fundamental Movement Skill Competency in Children. Pediatrics (2012) 130:e390–398. doi: 10.1542/peds.2012-0345 [DOI] [PubMed] [Google Scholar]
- 41. Hilpert M, Brockmeier K, Dordel S, Koch B, Weiß V, Ferrari N, et al. Sociocultural Influence on Obesity and Lifestyle in Children: A Study of Daily Activities, Leisure Time Behavior, Motor Skills, and Weight Status. Obes Facts (2017) 10:168–78. doi: 10.1159/000464105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Marmeleira J, Veiga G, Cansado H, Raimundo A. Relationship Between Motor Proficiency and Body Composition in 6- to 10-Year-Old Children. J Paediatrics Child Health (2017) 53:348–53. doi: 10.1111/jpc.13446 [DOI] [PubMed] [Google Scholar]
- 43. Haapala EA, Vaisto J, Lintu N, Tompuri T, Brage S, Westgate K, et al. Adiposity, Physical Activity and Neuromuscular Performance in Children. J Sports Sci (2016) 34:1699–706. doi: 10.1080/02640414.2015.1134805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. D’Hondt E, Deforche B, Gentier I, et al. A Longitudinal Analysis of Gross Motor Coordination in Overweight and Obese Children Versus Normal-Weight Peers. Int J Obes (Lond) (2013) 37:61–7. doi: 10.1038/ijo.2012.55 [DOI] [PubMed] [Google Scholar]
- 45. Graf C, Koch B, Falkowski G, et al. School-Based Prevention: Effects on Obesity and Physical Performance After 4 Years. J Sports Sci (2008) 26:987–94. doi: 10.1080/02640410801930176 [DOI] [PubMed] [Google Scholar]
- 46. Graf C, Koch B, Kretschmann-Kandel E, et al. Correlation Between BMI, Leisure Habits and Motor Abilities in Childhood (CHILT-Project). Int J Obes Related Metab Disorders: J Int Assoc Study Obes (2004) 28:22–6. doi: 10.1038/sj.ijo.0802428 [DOI] [PubMed] [Google Scholar]
- 47. Cheng J, East P, Blanco E, et al. Obesity Leads to Declines in Motor Skills Across Childhood. Child: Care Health Dev (2016) 42:343–50. doi: 10.1111/cch.12336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. de Chaves RN, Bustamante Valdivia A, Nevill A, et al. Developmental and Physical-Fitness Associations With Gross Motor Coordination Problems in Peruvian Children. Res Dev Disabil (2016) 53-54:107–14. doi: 10.1016/j.ridd.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 49. ntunes AM, Maia JA, Stasinopoulos MD, Gouveia ER, Thomis MA, Lefevre JA, et al. Gross Motor Coordination and Weight Status of Portuguese Children Aged 6-14 Years. Am J Hum Biol (2015) 27:681–9. doi: 10.1002/ajhb.22715 [DOI] [PubMed] [Google Scholar]
- 50. D’Hondt E, Deforche B, De Bourdeaudhuij I, Lenoir M. Childhood Obesity Affects Fine Motor Skill Performance Under Different Postural Constraints. Neurosci Lett (2008) 440:72–5. doi: 10.1016/j.neulet.2008.05.056 [DOI] [PubMed] [Google Scholar]
- 51. Abdelkarim O, Ammar A, Trabelsi K, Cthourou H, Jekauc D, Irandoust K, et al. Prevalence of Underweight and Overweight and Its Association With Physical Fitness in Egyptian Schoolchildren. Int J Environ Res Public Health (2019) 17(1):75. doi: 10.3390/ijerph17010075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Abdelkarim O, Ammar A, Soliman A, Hökelmann A. Prevalence of Overweight and Obesity Associated With the Levels of Physical Fitness Among Primary School Age Children in Assiut City. Egyptian Pediatr Assoc Gazette (2017) 65(2):43–8. doi: 10.1016/j.epag.2017.02.001 [DOI] [Google Scholar]
- 53. Cairney J, Hay JA, Faught BE, Hawes R. Developmental Coordination Disorder and Overweight and Obesity in Children Aged 9-14 Y. Int J Obes (Lond) (2005) 29:369–72. doi: 10.1038/sj.ijo.0802893 [DOI] [PubMed] [Google Scholar]
- 54. Prskalo I, Badric M, Kunjesic M. The Percentage of Body Fat in Children and the Level of Their Motor Skills. Collegium Antropologicum (2015) 39 Suppl 1:21–8. [PubMed] [Google Scholar]
- 55. Lopes L, Santos R, Moreira C, Pereira B, Lopes VP. Sensitivity and Specificity of Different Measures of Adiposity to Distinguish Between Low/High Motor Coordination. J Pediatria (2015) 91:44–51. doi: 10.1016/j.jped.2014.05.005 [DOI] [PubMed] [Google Scholar]
- 56. Caspersen CJ, Powell KE, Christenson GM. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep (1985) 100:126–31. [PMC free article] [PubMed] [Google Scholar]
- 57. Largo RH, Fischer JE, Rousson V. Neuromotor Development From Kindergarten Age to Adolescence: Developmental Course and Variability. Swiss Med Weekly (2003) 133:193–9. [DOI] [PubMed] [Google Scholar]
- 58. Vandorpe B, Vandendriessche J, Lefevre J, Pion J, Vaeyens R, Matthys S, et al. The KorperkoordinationsTest Fur Kinder: Reference Values and Suitability for 6-12-Year-Old Children in Flanders. Scandinavian J Med Sci Sports (2011) 21:378–88. doi: 10.1111/j.1600-0838.2009.01067.x [DOI] [PubMed] [Google Scholar]
- 59. Barnett LM, Lai SK, Veldman SLC, Hardy LL, Cliff DP, Morgan PJ, et al. Correlates of Gross Motor Competence in Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med (2016) 46:1663–88. doi: 10.1007/s40279-016-0495-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Jaakkola TWT. The Relationship Between Fundamental Movement Skills and Self-Reported Physical Activity During Finnish Junior High Schoo. Phys Educ Sport Pedagogy (2013) 18:492–505. doi: 10.1080/17408989.2012.690386 [DOI] [Google Scholar]
- 61. Hills AP, Hennig EM, Byrne NM, Steele JR. The Biomechanics of Adiposity–Structural and Functional Limitations of Obesity and Implications for Movement. Obes Rev (2002) 3:35–43. doi: 10.1046/j.1467-789X.2002.00054.x [DOI] [PubMed] [Google Scholar]
- 62. Butterfield SA, Angell RM, Mason CA. Age and Sex Differences in Object Control Skills by Children Ages 5 to 14. Perceptual Motor Skills (2012) 114:261–74. doi: 10.2466/10.11.25.PMS.114.1.261-274 [DOI] [PubMed] [Google Scholar]
- 63. Blatchford P BE, Pellegrini A. The Social Context of School Playground Games: Sex and Ethnic Differences, and Changes Over Time After Entry to Junior School. Br J Dev Psychol (2003) 21:481–505. doi: 10.1348/026151003322535183 [DOI] [Google Scholar]
- 64. Lee AM FK, Belcher D. Gender Differences in Children’s Conceptions of Competence and Motivation in Physical Education. Sport Educ Soc (1999) 4:161–74. doi: 10.1080/1357332990040204 [DOI] [Google Scholar]
- 65. Gentier I DHE, Shultz S, Deforche B, Augustijn M, Hoorne S, Verlaecke K DBI, et al. Fine and Gross Motor Skills Differ Between Healthy-Weight and Obese Children. Res Dev Disabil (2013) 34:4043–51. doi: 10.1016/j.ridd.2013.08.040 [DOI] [PubMed] [Google Scholar]
- 66. Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence Based Physical Activity for School-Age Youth. J Pediatr (2005) 146:732–7. doi: 10.1016/j.jpeds.2005.01.055 [DOI] [PubMed] [Google Scholar]
- 67. Hills AP, King NA, Armstrong TP. The Contribution of Physical Activity and Sedentary Behaviours to the Growth and Development of Children and Adolescents: Implications for Overweight and Obesity. Sports Med (2007) 37:533–45. doi: 10.2165/00007256-200737060-00006 [DOI] [PubMed] [Google Scholar]
- 68. Severinsen MCK, Pedersen BK. Muscle-Organ Crosstalk: The Emerging Roles of Myokines. Endocrine Rev (2020) 41(4):594–609. doi: 10.1210/endrev/bnaa016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Pedersen BK. Muscles and Their Myokines. J Exp Biol (2011) 214:337–46. doi: 10.1242/jeb.048074 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.