Abstract
Background
Drug-related emergency department (ED) visits are escalating, especially for stimulant use (i.e., cocaine and psychostimulants such as methamphetamine). We sought to characterize rates, presentation, and management of ED visits related to cocaine and psychostimulant use, compared to opioid use, in the United States (US).
Methods
We used 2008–2018 National Hospital Ambulatory Medical Care Survey data to identify a nationally representative sample of ED visits related to cocaine and psychostimulant use, with opioids as the comparator. To make visits mutually exclusive for analysis, we excluded visits related to 2 or more of the three possible drug categories. We estimated annual rate trends using unadjusted Poisson regression; described demographics, presenting concerns, and management; and determined associations between drug-type and presenting concerns (categorized as psychiatric, neurologic, cardiopulmonary, and drug toxicity/withdrawal) using logistic regression, adjusting for age, sex, race/ethnicity, and homelessness.
Results
Cocaine-related ED visits did not significantly increase, while psychostimulant-related ED visits increased from 2008 to 2018 (2.2 visits per 10,000 population to 12.9 visits per 10,000 population; p < 0.001). Cocaine-related ED visits had higher usage of cardiac testing, while psychostimulant-related ED visits had higher usage of chemical restraints than opioid-related ED visits. Cocaine- and psychostimulant-related ED visits had greater odds of presenting with cardiopulmonary concerns (cocaine adjusted odds ratio [aOR] 2.95, 95% CI 1.70–5.13; psychostimulant aOR 2.46, 95% CI 1.42–4.26), while psychostimulant-related visits had greater odds of presenting with psychiatric concerns (aOR 2.69, 95% CI 1.83–3.95) and lower odds of presenting with drug toxicity/withdrawal concerns (aOR 0.47, 95%CI 0.30–0.73) compared to opioid-related ED visits.
Conclusion
Presentations for stimulant-related ED visits differ from opioid-related ED visits: compared to opioids, ED presentations related to cocaine and psychostimulants are less often identified as related to drug toxicity/withdrawal and more often require interventions to address acute cardiopulmonary and psychiatric complications.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12873-022-00573-0.
Keywords: Amphetamines, Cocaine, Stimulants, Emergency department, Opioids, Overdose
Introduction
Emergency department (ED) visits related to drug overdose are escalating, especially during the COVID-19 pandemic [1]. While national attention has focused on opioids in the escalating overdose crisis, EDs across the United States (US) are also facing an expanding burden of visits related to stimulant use [2–5]. Stimulant-related ED visits are largely attributed to the use of substances such as cocaine and psychostimulants (e.g., methamphetamine) [6–9]. Cocaine has contributed to stimulant-related harms since at least 2011 [9], though in recent years, the US has seen a surge in methamphetamine use and related complications [10]. In addition to stimulant-related ED visits increasing nationwide [5], stimulant-related overdose deaths have also rapidly increased since 2010 [11] and now outnumber deaths attributed to prescription opioids and heroin [8].
Prior studies have mostly focused on ED visits related to stimulant overdose [1, 4, 5]. However, acute stimulant toxicity is not always recognized as an overdose [12], and these studies do not address visits related to chronic complications of drug use. There is a need to broadly examine the characteristics, presentations, and clinical management of all stimulant-related ED visits, not only visits that are identified as related to overdose. Presentations from stimulant toxicity also show wide variability, affect multiple organ systems, and are not as readily attributed to substance use [4, 13–16]. Cocaine toxicity is strongly associated with cardiovascular complications [13, 17], while psychostimulant toxicity is also associated with cardiac complications, as well as acute psychosis and agitation [3, 4, 14]. Few studies elucidate the prevalence of presenting concerns for psychostimulant-related ED visits or how they may vary compared to opioid-related ED visits. A better understanding of how patients with stimulant-related concerns present to the ED is needed, as this information has significant implications on clinical management and ED resource utilization.
We sought to describe the annual trends and characteristics of cocaine- and psychostimulant-related ED visits, with opioids-related ED visits as the reference group, given epidemiology and presentations of opioid-related visits are well understood and elucidated. We also evaluated whether chief presenting concerns during ED visits differ between these groups of drug-related ED visits.
Methods
Study design and setting
We conducted a secondary analysis using 2008–2018 data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), a nationally representative dataset of ED visits collected annually by the Centers for Disease Control and Prevention National Center for Health Statistics (NCHS) [18]. Each year, trained staff abstract visit data from medical records using standardized recording forms, including demographics, reasons for visit (RFV), diagnostic testing, administered medications, diagnoses rendered, etc. NHAMCS uses a multi-stage probability design and applies survey weights to obtain a nationally representative sample of ED visits to non-federal, general, short-stay acute care US hospitals [18, 19].
For each ED visit in NHAMCS in 2008–2013, ≤ 3 associated diagnosis codes, ≤ 3 RFV codes, and ≤ 8 administered medications were available [20, 21]. For 2014–2018, ≤ 5 associated diagnosis codes, ≤ 5 RFV codes, and ≤ 30 administered medications were available [22]. For consistency, we used only the top three listed diagnosis codes, top three listed RFV codes as their chief presenting concerns, and top eight listed administered medications.
Selection of emergency department visits
The sample included ED visits made by adults (≥ 18 years old) with the visit related to cocaine use, psychostimulant use, or opioid use, based on listed International Classification of Diseases Clinical Modification (ICD-CM) visit diagnosis codes. We included any visit that had any ICD-9-CM/ICD-10-CM code related to drug dependence, abuse, or poisoning for either cocaine, psychostimulant, or opioid use in any of the top three listed diagnoses codes (see Additional file 1 for complete list of ICDcodes used) [23, 24]. We excluded “in remission” codes to capture visits related to active drug use. We adapted this approach from the Centers for Medicare and Medicaid Services and other studies [2, 4, 25]. To make groups mutually exclusive and allow for comparisons, we excluded visits involving two or more of the three drug-related diagnosis groups (cocaine, psychostimulant, or opioid), approximately 5% of unweighted eligible visits. We excluded visits identified by NHAMCS as follow up visits and visits where the patient was seen at the same hospital within the preceding 72 h to limit repeat visits for the same illness episode.
Measurements and outcomes
The primary exposure of interest was the type of drug associated with the ED visit, as defined above (cocaine, psychostimulant, or opioid). The primary outcomes of interest were the chief presenting concerns. We sought to determine if presentations of drug-related visits were more commonly identified as belonging to a specific organ system (e.g., psychiatric, neurologic, or cardiopulmonary), or related to the broader constructs of drug toxicity and withdrawal. We measured four separate outcomes of dichotomous variables if visit concerns were related to: (1) psychiatric; (2) neurologic; (3) cardiopulmonary; or (4) drug toxicity/withdrawal concerns. Visits could contribute to more than one category of presenting concerns. For chief presenting concerns, NHAMCS uses an RFV coding scheme, where RFV is defined as “the patient’s complaint(s), symptom(s), or other reasons for this visit.” [20] We adapted the RFV coding scheme to measure if any of the top three RFV codes were related to psychiatric, neurologic, cardiopulmonary, and drug toxicity/withdrawal categories [26]. For example, psychiatric presenting concerns included RFV codes such as “depression” and “suicide attempt.” Cardiopulmonary concerns included codes such as “chest pain,” “shortness of breath,” and “respiratory arrest.” Drug toxicity/withdrawal concerns included “drug detoxification,” “accidental poisoning,” and “adverse effects of drug use” such as unintentional overdose (see Additional file 2 for RFV code categorization).
For each category of drug-related visits (cocaine, psychostimulant, or opioid), we described patient characteristics including age, sex, race/ethnicity, primary payer, homelessness, and multimorbidity (defined as the presence of two or more comorbidities assessed by NHAMCS) [27]. We used the imputed measure of race/ethnicity provided by NHAMCS, which adjusts for 16–18% missingness of race/ethnicity data extracted from the medical chart [21, 22]. We assessed hospital-level factors including urban location, US census region, and safety-net status, defined per NCHS criteria as having either > 30% of visits with the primary payer being Medicaid or uninsured, or having > 40% of visits from combined Medicaid and uninsured [28].
To evaluate characteristics of clinical management, we assessed diagnostic testing, administered medications, and disposition. As above, we analyzed the top eight administered medications, using the drug classification scheme developed by NCHS [21, 29]. We reviewed drug codes available and included any drug codes that could be classified as “atypical antipsychotics,” “benzodiazepines,” “naloxone,” or “opioids.” As certain combinations of polysubstance use are common (e.g., cocaine and alcohol [30]), we additionally examined whether visits were concurrently associated with alcohol-related and other drug-related diagnoses, including cannabis, sedatives/hypnotics, etc. (Additional file 1).
Statistical analysis
We applied survey sample weights to yield an unbiased national estimate of ED visit percentages and characteristics [19]. We calculated annual ED visit rates by dividing the weighted number of visits each year by the US Census Bureau estimates of civilian, noninstitutionalized adults aged 18 and older [19]. We conducted a Poisson regression analysis using visit year as the ordinal predictor to test for significant trends in visits over time. We described characteristics of cocaine-, psychostimulant-, and opioid-related visits using bivariate Pearson chi-squared tests. We used multivariable logistic regression to evaluate whether type of drug-related visit was associated with specific categories of chief presenting concerns, using separate models for each category. We adjusted for age, sex, race/ethnicity, and homelessness, as these factors could be associated with increased morbidity. All reported estimates were robust, defined by NCHS as an unweighted count in each group of ≥ 30 visits and/or a relative standard error of ≤ 30% [18, 31]. We completed all analyses using svyroutine commands within Stata/MP, version 16.0 (StataCorp LLC) [19, 32]. All p-values were two-sided and a p-value < 0.05 was used to determine statistical significance. The University of California, San Francisco Institutional Review Board exempted this study from review.
Results
Annual rate trends of drug-related emergency department visits
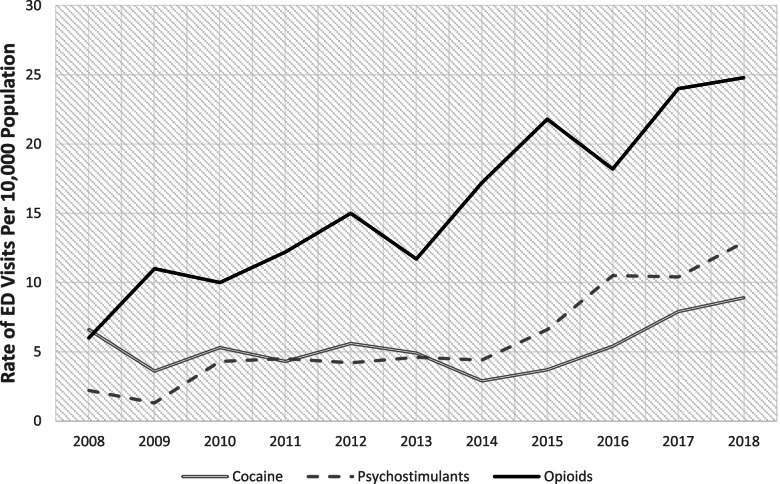
The study sample included 1,576,000 unweighted ED visits between 2008 to 2018, which was representative of 7,121,000 weighted ED visits. The rate of cocaine-related ED visits increased from 6.6 visits per 10,000 population (95%CI 3.9–9.3) in 2008 to 8.9 visits per 10,000 population (95%CI 4.7–13.1) in 2018, though this was not statistically significant (p = 0.23). Rates of psychostimulant-related ED visits increased from 2.2 visits per 10,000 population (95%CI 0.8–3.7) to 12.9 visits per 10,000 population (95%CI 7.3–18.4) (p < 0.001). The increase in ED visits was greatest for opioids, where rates of opioid-related ED visits increased from 6.0 visits per 10,000 population (95%CI 3.7–8.2) in 2014 to 24.8 visits per 10,000 population (95%CI 18.0–31.5) in2018 (p < 0.001) (Fig. 1).
Fig. 1.
Annual trends in rates of national emergency department visits related to cocaine, psychostimulant, or opioid use, 2008–2018. Emergency department visits categorized by drug-type if any of the top three ICD9-CM/ICD10-CM diagnoses codes were related to opioid, cocaine, or psychostimulant use. Visits were mutually exclusive for drug type, as visits associated with two or more drug-categories were excluded. Rates were calculated by dividing weighted number of visits in each year by US Census Bureau estimates of civilian, noninstitutionalized adults aged 18 and older for that year. All rates per 10,000 population.
Source: National Hospital Ambulatory Medical Care Survey
Characteristics of drug-related emergency department visits
In unadjusted analysis, psychostimulant- and opioid-related visits had comparable age and race/ethnicity distributions, whereas cocaine-related visits were more likely to be among those ≥ 40 years of age and identifying as Black (p < 0.001 for both characteristics) (Table 1). Patients with cocaine- and psychostimulant-related visits were more likely to be experiencing homelessness compared to patients with opioid-related visits (cocaine 10%, psychostimulant 12%, opioid 4%; p < 0.001). Cocaine-related visits were predominantly in the South (49%), while psychostimulant-related visits were more concentrated in the West (60%), and opioid-related visits were spread out throughout all regions. Cocaine and psychostimulant-related visits were slightly more concentrated at hospitals in urban areas than opioid-related visits (cocaine 96%, psychostimulant 91%, opioid 88%; p = 0.03).
Table 1.
Demographic characteristics of national emergency department visits related to cocaine, psychostimulant, opioid use, 2008–2018
| Weighted % (95% CI) | |||
|---|---|---|---|
|
Cocaine-related visits (n = 1,406,000) |
Psychostimulant-related visits (n = 1,590,000) |
Opioid-related visits (n = 4,125,000) |
|
| Age, years | |||
| 18–29 | 12 (9, 17) | 38 (31, 46) | 38 (33, 43) |
| 30–39 | 26 (19, 35) | 31 (24, 40) | 26 (22, 30) |
| 40–49 | 29 (23, 37) | 14 (10, 21) | 13 (10, 16) |
| ≥ 50 | 32 (25, 40) | 16 (10, 24) | 24 (20, 29) |
| Female | 39 (33, 46) | 39 (32, 47) | 47 (42, 51) |
| Race/ethnicity | |||
| Black | 54 (45, 62) | 10 (7, 15) | 11 (8, 15) |
| White | 28 (22, 36) | 64 (55, 72) | 78 (73, 82) |
| Other race/ethnicity | 18 (13, 25) | 26 (19, 35) | 11 (8, 15) |
| Primary Payer | |||
| Medicaid | 28 (22, 34) | 36 (27, 45) | 34 (29, 40) |
| Medicare | 13 (7, 23) | 5 (3, 8) | 13 (10, 17) |
| Private | 16 (11, 23) | 19 (13, 26) | 19 (15, 23) |
| Uninsured | 24 (19, 30) | 24 (17, 34) | 17 (14, 20) |
| Other | 19 (13, 27) | 16 (10, 26) | 17 (12, 23) |
| Homelessness | 10 (6, 17) | 12 (8, 17) | 4 (2, 6) |
| Urban region | 96 (92, 98) | 91 (83, 96) | 88 (82, 93) |
| US Region | |||
| Northeast | 16 (11, 23) | – | 22 (18, 26) |
| Midwest | 20 (14, 26) | – | 24 (20, 29) |
| South | 49 (40, 59) | 28 (22, 36) | 27 (23, 33) |
| West | 15 (10, 21) | 60 (51, 68) | 27 (21, 32) |
| Safety Net Hospital | 28 (22, 36) | 26 (19, 35) | 24 (20, 29) |
| Multimorbidity | 19 (13, 28) | – | 13 (10, 17) |
Source: National Hospital Ambulatory Medical Care Survey. Cell sizes with < 30 unweighted visits or > 30% relative standard error not included. Visits were mutually exclusive for drug type, as visits associated with two or more drug-categories were excluded. Multimorbidity as the presence of two or more comorbidities assessed by NHAMCS (including Alzheimer’s dementia, alcohol use disorder, asthma, cancer, cerebrovascular disease, chronic obstructive pulmonary disease, coronary artery disease, depression, diabetes, chronic kidney disease, end stage renal disease, venous thromboembolism, HIV/AIDS, hypertension, obesity, obstructive sleep apnea, osteoporosis, and substance use disorders)
Psychiatric concerns were more common in cocaine- and psychostimulant-related visits (cocaine 31%, psychostimulant 50%, opioid 25%; p < 0.001). Cardiopulmonary concerns were also more common in cocaine- and psychostimulant-related visits (cocaine 33%, psychostimulant 23%, opioid 12%; p < 0.001) concerns than opioid-related visits (Table 2). Drug-toxicity/withdrawal concerns were more common in opioid-related visits (cocaine 36%, psychostimulant 32%, opioid 49%; p < 0.001). Cocaine-related visits had a higher proportion of co-occurring alcohol-related diagnoses in the same ED visit (cocaine 19%, psychostimulant 6%, opioid 7%; p < 0.001).
Table 2.
Presenting concerns, clinical management, and disposition of national emergency department visits related to cocaine, psychostimulant, or opioid use, 2008–2018
| Weighted % (95% CI) | |||
|---|---|---|---|
|
Cocaine-related visits (n = 1,406,000) |
Psychostimulant-related visits (n = 1,590,000) |
Opioid-related visits (n = 4,125,000) |
|
| Chief presenting concern(s) | |||
| Psychiatric | 31 (24, 38) | 50 (42, 58) | 25 (21, 30) |
| Neurologic | 7 (4, 11) | 7 (4, 12) | 7 (4, 10) |
| Cardiopulmonary | 33 (26, 41) | 23 (17, 31) | 12 (10, 16) |
| Drug toxicity/withdrawal | 36 (30, 43) | 32 (25, 40) | 49 (43, 54) |
| Co-occurring Drug Related Diagnoses | |||
| Alcohol-related diagnosis | 19 (15, 25) | 6 (4, 10) | 7 (5, 9) |
| Other drug-related diagnosis | 9 (6, 13) | 9 (6, 14) | 9 (7, 12) |
| Diagnostic testing | |||
| Blood alcohol concentration | 20 (15, 27) | 20 (14, 29) | 16 (12, 19) |
| Cardiac monitoring | 24 (18, 32) | 13 (8, 20) | 12 (9, 16) |
| Cardiac biomarkers | 23 (16, 32) | 11 (7, 16) | 7 (5, 9) |
| Electrocardiogram | 51 (43, 59) | 34 (27, 41) | 29 (24, 33) |
| Urine toxicology | 56 (47, 64) | 42 (34, 51) | 35 (30, 41) |
| Any imaging | 54 (46, 61) | 35 (27, 44) | 35 (30, 41) |
| Any X-ray | 44 (37, 52) | 28 (21, 37) | 26 (20, 31) |
| Any CT Scan | 17 (12, 23) | 14 (8, 21) | 13 (10, 17) |
| Administered medications | |||
| Atypical antipsychotics | 6 (4, 11) | 13 (8, 20) | 2 (1, 3) |
| Benzodiazepines | 19 (14, 25) | 33 (26, 42) | 15 (12, 19) |
| Naloxone | – | – | 13 (10, 17) |
| Opioids | 17 (11, 24) | 9 (4, 17) | 14 (11, 18) |
| Disposition | |||
| Treat and release | 58 (51, 65) | 63 (55, 70) | 68 (63, 72) |
| Left before treatment complete | 3 (1, 5) | 2 (1, 6) | 3 (2, 6) |
| Transferred to psychiatric facility | 6 (3, 13) | 10 (6, 17) | 5 (3, 7) |
| Admitted | 16 (12, 22) | 9 (6, 13) | 16 (13, 20) |
Source: National Hospital Ambulatory Medical Care Survey. Cell sizes with < 30 unweighted visits or > 30% relative standard error not included. Visits were mutually exclusive for drug type, as visits associated with two or more drug-categories were excluded. Chief presenting concerns defined using top three “reason for visit” codes. Visits could contribute to more than one category of chief presenting concerns
The most common chief presenting concerns varied across groups. The most common chief presenting concern for opioid-related visits were “adverse effect of drug abuse” (27.9% of opioid-related visits), “drug detoxification” (6.0%), and “abnormal drug usage” (5.7%) (Additional file 3). The most common chief presenting concerns for cocaine-related visits were “chest pain” (27.2% of cocaine-related visits), “other problems relating to psychosis” (7.9%), and “abdominal pain” (5.7%). For psychostimulant-related visits, most common chief presenting concerns were “chest pain” (10.4% of psychostimulant-related visits), “abnormal drug usage” (9.3%), and “other symptoms related to psychosis” (8.7%).
Cocaine-related visits had the highest utilization of diagnostic testing, especially cardiovascular testing (e.g., cardiac biomarkers and monitoring). Psychostimulant-related visits had more administration of chemical restraint medications. Cocaine- and opioid-related visits more often resulted in admission (cocaine: 16%, psychostimulant 9%, opioid 16%; p < 0.001), while psychostimulant-related visits had more transfers to psychiatric facilities (cocaine 6%, psychostimulant 10%, opioid 5%; p < 0.001).
Multivariable analyses
Unadjusted odd ratios (OR) showing associations between drug type and presenting concerns are shown in Table 3. Adjusting for age, sex, race/ethnicity, and homelessness, psychostimulant-related visits had greater odds of presenting with a psychiatric chief concern compared to opioid-related visits (adjusted odds ratio [aOR] 2.69; 95% CI 1.83–3.95; Table 3). No differences were seen with neurologic chief concerns. Both cocaine- and psychostimulant-related visits had greater odds of presenting with cardiopulmonary chief concerns compared to opioid-related visits (cocaine aOR 2.95, 95% CI 1.70–5.13: psychostimulant aOR 2.46, 95% CI 1.42–4.27). In contrast, psychostimulant-related visits had lower odds of presenting with drug toxicity/withdrawal concerns (aOR 0.47, 95%CI 0.30–0.73).
Table 3.
Associations between drug type and chief presenting concerns among national emergency department visits related to cocaine, psychostimulant, or opioid use, 2008–2018
| Psychiatric chief concerns | Neurologic chief concerns | Cardiopulmonary chief concerns | Drug toxicity/ withdrawal chief concerns | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | OR | 95%CI | OR | 95%CI | |
| Unadjusted analyses | ||||||||
| Drug | ||||||||
| Cocaine | 1.32 | 0.85–2.21 | 0.99 | 0.51–1.95 | 3.52 | 2.34–5.31 | 0.60 | 0.42–0.87 |
| Psychostimulants | 2.99 | 2.04–4.39 | 1.03 | 0.49–2.17 | 2.12 | 1.26–3.58 | 0.49 | 0.32–0.76 |
| Opioid | Ref | Ref | Ref | Ref | ||||
| Adjusted analyses | ||||||||
| Drug | ||||||||
| Cocaine | 1.37 | 0.85–2.21 | 1.05 | 0.87–2.28 | 2.95 | 1.70–5.13 | 0.83 | 0.52–1.35 |
| Psychostimulants | 2.69 | 1.83–3.95 | 0.92 | 0.36–2.37 | 2.46 | 1.42–4.26 | 0.47 | 0.30–0.73 |
| Opioid | Ref | Ref | Ref | Ref | ||||
Source: National Hospital Ambulatory Medical Care Survey. Visits were mutually exclusive for drug type, as visits associated with two or more drug-categories were excluded. Chief presenting concerns defined using top three “reason for visit” codes. Visits could contribute to more than one category of chief presenting concerns. Adjusted analyses were adjusted for age, sex, race/ethnicity, and homelessness. OR Odds Ratio, CI confidence interval
Discussion
In this study using nationally representative ED visits, there were significant increases in psychostimulant-related ED visits, and presentations for both cocaine- and psychostimulant-related ED visits differed compared to opioid-related ED visits.
Psychostimulant-related ED visits increased from 2.2 to 12.9 visits per 10,000 population from 2008 to 2018. This is consistent with studies showing increasing national rates of ED visits, hospitalizations, and deaths from psychostimulant overdose [2, 4, 5, 33]. The increasing use of the ED and other acute care settings is likely linked to rising methamphetamine availability and use [34]. National Forensic Laboratory Information System data found methamphetamine case submissions increased from 2011 to 2019, with methamphetamine as the most frequently reported drug [35]. While psychostimulant-related ED visits were predominantly among Western regions in our study, recent data highlights the emergence of psychostimulant-related overdose deaths in the Midwest and Northeast, suggesting methamphetamine is already a nationwide concern [8, 36]. Increases in cocaine-related ED visits were not significant, potentially due to the exclusion of visits related to opioid and cocaine co-use. Polysubstance use is common in among individuals using cocaine [30], and other studies found rates of fatal overdoses and ED visits for overdose involving cocaine and opioid use are rising [5, 33].
We found stimulant-related ED visits were less likely to be identified as drug toxicity/withdrawal concerns, underscoring the differences in presentations between stimulant- and opioid-related visits. While the national surge in ED visits and deaths related to opioid overdose is linked to the rise in fentanyl in the drug supply [1, 33, 37], the main drivers of stimulant-related ED visits and overdoses are unclear. Possibilities include increased potency of fluctuating drug supplies [35], contamination or co-use with synthetic opioids like fentanyl [38], or the cumulative effects of chronic stimulant use over time [39]. Further, the term “overdose”, when applied to opioids commonly refers to an acute respiratory event from an episode of use, and this term is problematic when applied to stimulants, as it lacks specificity in capturing the diverse ways in which stimulant toxicity can present [16, 40]. Our data suggest that acute emergency presentations related to stimulant use are more likely due to the cumulative effect of stimulant use over time rather than from a single episode of use. Addressing acute stimulant toxicity may rely more on clinical management of various symptoms, rather than the development of a single reversal agent like naloxone for opioid overdose.
Cocaine-related ED visits were predominately made by individuals who were older, male, and Black. Potential reasons include differences in drug supply, disparities in comorbidities, socioeconomic disadvantage, and other factors related to structural racism that can affect health and healthcare access [41, 42]. Complications from cocaine use are disproportionately higher in Black communities, where rates of cocaine-related deaths are comparable to the rates of opioid-related deaths in white individuals [41]. Yet cocaine-related harms have been understudied in recent years. This is alarming given overdose deaths in Black individuals are rising faster compared to whites [43, 44], and in our study, cocaine-related visits were as likely to result in admission as opioid-related visits. As attention toward the rising epidemic of stimulant-related deaths increases, interventions addressing stimulant use must address racial equity and pay attention to both cocaine and psychostimulant use to avoid further exacerbating racial and economic disparities [45].
Both cocaine- and psychostimulant-related ED visits were associated with cardiopulmonary concerns, even after adjusting for cardiovascular risk factors. Both cocaine and psychostimulants are known cardiotoxins, and both acute and chronic use can lead to adverse events such as myocardial ischemia, stroke, and heart failure [17, 46, 47]. Simultaneous cocaine and alcohol use is also common and contributes to worse cardiovascular outcomes [48, 49]. Patients using stimulants who develop chronic cardiovascular conditions such as heart failure, despite being younger, face more severe in-hospital complications with higher rates of readmission compared to patients with non-stimulant-related heart failure [50, 51]. These findings suggest a need for targeted cardiopulmonary interventions for people who present to the ED with stimulant-related diagnoses.
Psychostimulant-related ED visits were strongly associated with psychiatric concerns, greater administration of chemical restraint medications, and more transfers to psychiatric facilities. Single center ED studies have drawn similar conclusions [14, 15], and our national study adds generalizability. Methamphetamine use not only precipitates psychotic symptoms but also exacerbates underlying psychiatric illness [14, 52]. Paired with high rates of homelessness seen in patients with stimulant-related ED visits, these findings are especially relevant for urban areas where addressing acute psychiatric presentations and homelessness are pressing concerns.
The ED has become a critical setting in responding to the overdose crisis and addressing the health needs of people who use drugs, particularly among low-income populations [53, 54]. EDs have taken up campaigns to distribute naloxone[55–57], initiate buprenorphine prescriptions for opioid use disorder treatment [54], and develop referral programs to increase linkages to treatment [58, 59]. Similarly, the ED can become a point of intervention for addressing acute and chronic complications of stimulant use disorders [60]. While no current Food and Drug Administration approved medications for stimulant use disorder exist, several medications show early promise [61–63]. Behavioral treatments such as contingency management and cognitive behavioral therapy are effective, though few can access these treatment modalities, especially for publicly-insured populations where reimbursement is limited [64–66]. EDs facing a high burden of stimulant-related visits could implement a navigator to facilitate linkages to existing treatment programs [58, 67], or offer harm reduction kits to reduce complications of drug use. As methamphetamine-related ED visits are associated with longer length of stays and higher costs [14], facilitating linkages to stimulant use treatment from the ED could help reduce costs and align with national policies focused on expanding access to treatment [68].
Several limitations should be considered. We excluded visits that included diagnoses related to both opioid and stimulant use. Rates of drug-related ED visits and calendar time trends in rates could differ from our findings when including visits related to polysubstance use. The transition from ICD-9-CM to ICD-10-CM starting in 2015 potentially affected trends, as increasing rates of drug-related visits during this period could be attributed to this transition [69]. However, the continued rise across all drug-related ED visits provides some reassurance of validity. Use of diagnostic coding may not have accurately captured all-drug related ED visits, as it often relies on the judgment of the treating physician and the clinical presentation without confirmatory urine drug testing, which may introduce misclassification. We are also unable to rule out polysubstance use involvement even with coding for specific drug-related illnesses. Moreover, the data do not allow us to readily distinguish acute toxicity from withdrawal presentations (e.g., opioid-related visits treated with benzodiazepines and opioids are likely related to withdrawal). However, these preliminary data are needed to set the stage for longitudinal prospective studies to validate findings. Finally, we assume that the majority of psychostimulant-related visits were due to methamphetamine use, as psychostimulant-related ICD codes have high positive predictive values for methamphetamine use in acute care settings [2, 6, 7, 70]. However, we could not distinguish between visits related to methamphetamine versus other psychostimulants.
Conclusions
Psychostimulant-related ED visits increased substantially from 2008 to 2018. Cocaine- and psychostimulant-related ED visits differ in presentation and management from opioid-related ED visits. They are less often identified as related to drug toxicity/withdrawal and require more interventions to address cardiopulmonary and psychiatric complications.
Supplementary Information
Acknowledgements
We thank Christopher Cairns and Loredana Santo at the Division of Health Care Statistics at the National Center for Health Statistics, and Dr. John Neuhaus at the UCSF Epidemiology & Biostatistics, for their assistance with the data. We would also like to thank the UCSF National Clinical Scholars Program for their support of this work.
Abbreviations
- ED
Emergency department
- ICD
International classification of diseases
- NCHS
National Center of Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- RFV
Reason for visit
Authors’ contributions
LWS and PC conceived the study and designed the study. LWS analyzed the data. TDM provided statistical advice on data analysis. All authors contributed to data interpretation. LWS and PC drafted the article, and all authors contributed substantially to its revision. All authors read and approved the final manuscript.
Funding
LWS was supported by the UCSF National Clinical Scholars Program and the San Francisco Veteran Affairs Medical Center. TDM has received training support from the National Institute on Drug Abuse (T32 DA007250). POC was supported by the National Institute on Drug Abuse (K24DA042720). The funding agencies had no role in study design, data collection, analysis, the decision to publish, or the preparation of the manuscript.
Availability of data and materials
All data is made publicly available through the National Center of Health Statistics and can be accessed through their website at https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm
Declarations
Ethics approval and consent to participate
As the study uses publicly available datasets, the University of California San Francisco Institutional Review Board exempted this study from review. All methods were performed in accordance with the relevant BMC Emergency Medicine guidelines and regulations.
Consent for publication
Not applicable
Competing interests
KTL has received research funding unrelated to this work from the California Department of Health Care Services, Public Health Institute, Sierra Health Foundation, and Substance Abuse and Mental Health Services Administration. POC serves on the Board of Scientific Counselors, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. All other authors have no competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Leslie W. Suen, Email: Leslie.suen@ucsf.edu
Thibaut Davy-Mendez, Email: tdavy@med.unc.edu.
Kathy T. LeSaint, Email: Kathy.LeSaint@ucsf.edu
Elise D. Riley, Email: Elise.Riley@ucsf.edu
Phillip O. Coffin, Email: Phillip.Coffin@sfdph.org
References
- 1.Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health overdose and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiat. 2021;8:372. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Winkelman TNA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open. 2018;1(6):e183758. doi: 10.1001/jamanetworkopen.2018.3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones CM, Olsen EO, O’Donnell J, Mustaquim D. Resurgent methamphetamine use at treatment admission in the United States, 2008–2017. Am J Public Health. 2020;110(4):509–516. doi: 10.2105/AJPH.2019.305527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vivolo-Kantor AM, Hoots BE, Seth P, Jones CM. Recent trends and associated factors of amphetamine-type stimulant overdoses in emergency departments. Drug Alcohol Depend. 2020;216:108323. doi: 10.1016/j.drugalcdep.2020.108323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoots B, Vivolo-Kantor A, Seth P. The rise in non-fatal and fatal overdoses involving stimulants with and without opioids in the United States. Addiction. 2020;115(5):946–958. doi: 10.1111/add.14878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crane EH. Highlights of the 2011 Drug Abuse Warning network (DAWN) findings on drug-related emergency department visits. Published online February 22, 2013. doi:10.1037/e515452011-001 [PubMed]
- 7.Substance abuse and mental health services administration. Drug abuse warning network, 2011: national estimates of drug-related emergency department visits. Substance Abuse and Mental Health Services Administration; 2013:100. https://www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf
- 8.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. doi: 10.15585/mmwr.mm7006a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011–2016. Natl Vital Stat Rep. 2018;67(9):1–14. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Health Alert Network (HAN) health advisory HAN00438. Centers for Disease Control and Prevention; 2020. Accessed February 8, 2021. https://emergency.cdc.gov/han/2020/han00438.asp
- 11.Black JC, Bau GE, Iwanicki JL, Dart RC. Association of medical stimulants with mortality in the US from 2010 to 2017. JAMA Intern Med. 2021;181:707. doi: 10.1001/jamainternmed.2020.7850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riley ED, Cohen J, Shumway M. Overdose fatality and surveillance as a method for understanding mortality trends in homeless populations. JAMA Intern Med. 2013;173(13):1264. doi: 10.1001/jamainternmed.2013.6838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Derlet RW, Albertson TE. Emergency department presentation of cocaine intoxication. Ann Emerg Med. 1989;18(2):182–186. doi: 10.1016/S0196-0644(89)80111-8. [DOI] [PubMed] [Google Scholar]
- 14.Murphy CE, Wang RC, Coralic Z, Lai AR, Raven M. Association between methamphetamine use and psychiatric hospitalization, chemical restraint, and emergency department length of stay. Acad Emerg Med. 2020;27(11):1116–1125. doi: 10.1111/acem.14094. [DOI] [PubMed] [Google Scholar]
- 15.Jones R, Woods C, Usher K. Rates and features of methamphetamine-related presentations to emergency departments: an integrative literature review. J Clin Nurs. 2018;27(13–14):2569–2582. doi: 10.1111/jocn.14493. [DOI] [PubMed] [Google Scholar]
- 16.Kaye S, Darke S. Non-fatal cocaine overdose among injecting and non-injecting cocaine users in Sydney Australia. Addiction. 2004;99(10):1315–1322. doi: 10.1111/j.1360-0443.2004.00875.x. [DOI] [PubMed] [Google Scholar]
- 17.Afonso L, Mohammad T, Thatai D. Crack whips the heart: a review of the cardiovascular toxicity of cocaine. Am J Cardiol. 2007;100(6):1040–1043. doi: 10.1016/j.amjcard.2007.04.049. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. NAMCS/NHAMCS - scope and sample design.; 2019. Accessed April 14, 2020. https://www.cdc.gov/nchs/ahcd/ahcd_scope.htm
- 19.Centers for Disease Control and Prevention. NAMCS/NHAMCS - estimation procedures.; 2019. Accessed April 14, 2020. https://www.cdc.gov/nchs/ahcd/ahcd_estimation_procedures.htm
- 20.National Center for Health Statistics. 2014 NHAMCS micro-data file documentation. National Center for Health Statistics; 2014. Accessed April 14, 2020. https://data.nber.org/nhamcs/docs/nhamcsed2014.pdf
- 21.Hsiao CJ. Understanding and using NAMCS and NHAMCS Data: data tools and basic programming techniques. Presented at: national conference for health statistics; August 16, 2010.
- 22.National Center for Health Statistics. 2015 NHAMCS micro-data file documentation.; 2015.
- 23.Centers for Disease Control Prevention. ICD - ICD-9-CM - International Classification of Diseases, ninth revision, clinical modification. Centers for Disease Control and Prevention. Published March 1, 2019. Accessed February 28, 2021. https://www.cdc.gov/nchs/icd/icd9cm.htm
- 24.Centers for Disease Control Prevention. ICD - ICD-10-CM - International Classification of Diseases, tenth revision, clinical modification. Centers for Disease Control and Prevention. Published January 26, 2021. Accessed February 28, 2021. https://www.cdc.gov/nchs/icd/icd10cm.htm
- 25.National Center for Health Statistics. Diagnosis master category list, 2016. Centers for Disease Control and Prevention; 2016.
- 26.Barnett ML, Song Z, Landon BE. Trends in physician referrals in the United States, 1999–2009. Arch Intern Med. 2012;172(2):163. doi: 10.1001/archinternmed.2011.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Navickas R, Petric VK, Feigl AB, Seychell M. Multimorbidity: what do we know? what should we do? J Comorb. 2016;6(1):4–11. doi: 10.15256/joc.2016.6.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burt C, Arispe I. Characteristics of emergency departments serving high volumes of safety-net patients: United States, 2000. National Center for Health Statistics; 2004. [PubMed]
- 29.Koch H, Campbell WH. The collection and processing of drug information: national ambulatory medical care survey. United States 1980. Vital Health Stat 2. 1982;90:1–90. [PubMed] [Google Scholar]
- 30.Liu Y, Williamson V, Setlow B, Cottler LB, Knackstedt LA. The importance of considering polysubstance use: lessons from cocaine research. Drug Alcohol Depend. 2018;192:16–28. doi: 10.1016/j.drugalcdep.2018.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCaig LF, Burt CW. Understanding and interpreting the national hospital ambulatory medical care survey: key questions and answers. Ann Emerg Med. 2012;60(6):716–721.e1. doi: 10.1016/j.annemergmed.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 32.StataCorp. Stata survey data reference manual: release 15. Published online 2017. Accessed April 15, 2021. https://www.stata.com/manuals/svysvy.pdf
- 33.Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2019. National Center for Health Statistics; 2020:8.
- 34.Lipari RN. Key Substance use and mental health indicators in the United States: results from the 2018 National survey on drug use and health. Published online 2018 82
- 35.Drug Enforcement Administration. National Forensic Laboratory Information System: NFLIS-drug mid year report 2019. US Department of Justice, Drug Enforcement Administration; 2020.
- 36.Howell BA, Bart G, Wang EA, Winkelman TNA. Service involvement across multiple sectors among people who use opioids, methamphetamine, or both, United States-2015-2018. Med Care. 2021;59(3):238–244. doi: 10.1097/MLR.0000000000001460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baldwin GT, Seth P, Noonan RK. Continued increases in overdose deaths related to synthetic opioids: implications for clinical practice. JAMA. 2021;325:1151. doi: 10.1001/jama.2021.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stephenson J. Drug overdose deaths head toward record number in 2020, CDC warns. JAMA Health Forum. 2020;1(10):e201318. doi: 10.1001/jamahealthforum.2020.1318. [DOI] [PubMed] [Google Scholar]
- 39.Turner C, Chandrakumar D, Rowe C, Santos GM, Riley ED, Coffin PO. Cross-sectional cause of death comparisons for stimulant and opioid mortality in San Francisco, 2005–2015. Drug Alcohol Depend. 2018;185:305–312. doi: 10.1016/j.drugalcdep.2017.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vasan S, Olango GJ. Amphetamine toxicity. StatPearls Publishing; 2020. Accessed May 7, 2021. https://www.ncbi.nlm.nih.gov/books/NBK470276/ [PubMed]
- 41.Shiels MS, Freedman ND, Thomas D, de BerringtonGonzalez A. Trends in U.S. drug overdose deaths in non-hispanic black hispanic and non-hispanic white persons, 2000–2015. Ann Intern Med. 2018;168(6):453. doi: 10.7326/M17-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cano M, Oh S, Salas-Wright CP, Vaughn MG. Cocaine use and overdose mortality in the United States: evidence from two national data sources, 2002–2018. Drug Alcohol Depend. 2020;214:108148. doi: 10.1016/j.drugalcdep.2020.108148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Drake J, Charles C, Bourgeois JW, Daniel ES, Kwende M. Exploring the impact of the opioid epidemic in black and hispanic communities in the United States. Drug Science, Policy and Law. 2020;6:2050324520940428. doi: 10.1177/2050324520940428. [DOI] [Google Scholar]
- 44.Khatri UG, Pizzicato LN, Viner K, et al. Racial/ethnic disparities in unintentional fatal and nonfatal emergency medical services-attended opioid overdoses during the COVID-19 pandemic in philadelphia. JAMA Netw Open. 2021;4(1):e2034878. doi: 10.1001/jamanetworkopen.2020.34878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nunes EV, Levin FR, Reilly MP, El-Bassel N. Medication treatment for opioid use disorder in the age of covid-19: can new regulations modify the opioid cascade? J Subs Abuse Treat. 2021;122:108196. doi: 10.1016/j.jsat.2020.108196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kevil CG, Goeders NE, Woolard MD, et al. Methamphetamine use and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2019;39(9):1739–1746. doi: 10.1161/ATVBAHA.119.312461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baumann BM, Perrone J, Hornig SE, Shofer FS, Hollander JE, Hollander DJ. Cardiac and hemodynamic assessment of patients with cocaine-associated chest pain syndromes. J Toxicol Clin Toxicol. 2000;38(3):283–290. doi: 10.1081/CLT-100100933. [DOI] [PubMed] [Google Scholar]
- 48.McCance-Katz EF, Kosten TR, Jatlow P. Concurrent use of cocaine and alcohol is more potent and potentially more toxic than use of either alone—a multiple-dose study. Biol Psychiat. 1998;44(4):250–259. doi: 10.1016/S0006-3223(97)00426-5. [DOI] [PubMed] [Google Scholar]
- 49.Farooq MU, Bhatt A, Patel MB. Neurotoxic and cardiotoxic effects of cocaine and ethanol. J Med Toxicol. 2009;5(3):134–138. doi: 10.1007/BF03161224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shetty S, Malik AH, Ali A, Yang YC, Briasoulis A, Alvarez P. Characteristics trends outcomes and costs of stimulant-related acute heart failure hospitalizations in the United States. Int J Cardiol. 2021;331:158–163. doi: 10.1016/j.ijcard.2021.01.060. [DOI] [PubMed] [Google Scholar]
- 51.Nishimura M, Ma J, Fox S, et al. Characteristics and outcomes of methamphetamine abuse among veterans with heart failure. Am J Cardiol. 2019;124(6):907–911. doi: 10.1016/j.amjcard.2019.05.068. [DOI] [PubMed] [Google Scholar]
- 52.Schultz BR, Lu BY, Onoye JM, Toohey TP. High resource utilization of psychiatric emergency services by methamphetamine users. Hawaii J Med Public Health. 2018;77(12):312–314. [PMC free article] [PubMed] [Google Scholar]
- 53.Hawk K, D’Onofrio G. Emergency department screening and interventions for substance use disorders. Addict Sci Clin Pract. 2018;13(1):18. doi: 10.1186/s13722-018-0117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence. JAMA. 2015;313(16):1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bukata WR, Bedard LA, Hoffman JR, Ranney ML, Whiteside LK, Hawk K. Naloxone prescriptions by emergency physicians. ACEP Resolution 39(14), 2014. Published online 2014. Accessed March 11, 2021. https://www.acep.org/what-we-believe/actions-on-council-resolutions/councilresolution/?rid=5AB946E9-9772-E911-A9AD-9BD2C184F805
- 56.Eswaran V, Allen KC, Bottari DC, et al. Take-home naloxone program implementation: lessons learned from seven chicago-area hospitals. Ann Emerg Med. 2020;76(3):318–327. doi: 10.1016/j.annemergmed.2020.02.013. [DOI] [PubMed] [Google Scholar]
- 57.Gunn AH, Smothers ZPW, Schramm-Sapyta N, Freiermuth CE, MacEachern M, Muzyk AJ. The emergency department as an opportunity for naloxone distribution. West J Emerg Med. 2018;19(6):1036–1042. doi: 10.5811/westjem.2018.8.38829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.D’Onofrio G, Chawarski MC, O’Connor PG, et al. Emergency department-initiated buprenorphine for opioid dependence with continuation in primary care: outcomes during and after intervention. J Gen Intern Med. 2017;32(6):660–666. doi: 10.1007/s11606-017-3993-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rapp RC, Otto AL, Lane DT, Redko C, McGatha S, Carlson RG. Improving linkage with substance abuse treatment using brief case management and motivational interviewing. Drug Alcohol Depend. 2008;94(1–3):172–182. doi: 10.1016/j.drugalcdep.2007.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Selby S, Wang D, Murray E, Lang E. Emergency departments as the health safety nets of society: a descriptive and multicenter analysis of social worker support in the emergency room. Cureus. 2018;10(9):e3247. doi: 10.7759/cureus.3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coffin PO, Santos GM, Hern J, et al. Effects of mirtazapine for methamphetamine use disorder among cisgender men and transgender women who have sex with men: a placebo-controlled randomized clinical trial. JAMA Psychiatry. Published online December 11, 2019. doi:10.1001/jamapsychiatry.2019.3655 [DOI] [PMC free article] [PubMed]
- 62.Trivedi MH, Walker R, Ling W, et al. Bupropion and naltrexone in methamphetamine use disorder. N Engl J Med. 2021;384(2):140–153. doi: 10.1056/NEJMoa2020214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.National Institute of Drug Abuse. What treatments are under development for methamphetamine use and addiction? National Institute on Drug Abuse. Published April 9, 2020. Accessed March 11, 2021. https://www.drugabuse.gov/publications/research-reports/methamphetamine/what-treatments-are-under-development-methamphetamine-use-addiction
- 64.Davis DR, Kurti AN, Skelly JM, Redner R, White TJ, Higgins ST. A review of the literature on contingency management in the treatment of substance use disorders, 2009–2014. Prev Med. 2016;92:36–46. doi: 10.1016/j.ypmed.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Petry NM. Contingency management: what it is and why psychiatrists should want to use it. Psychiatrist. 2011;35(5):161–163. doi: 10.1192/pb.bp.110.031831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rawson RA, McCann MJ, Flammino F, et al. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–274. doi: 10.1111/j.1360-0443.2006.01312.x. [DOI] [PubMed] [Google Scholar]
- 67.Herring A. California bridge program patient outcomes evaluationstudy protocol (main study). Public Health Institution; 2019. Accessed March 12, 2021. https://static1.squarespace.com/static/5c412ab755b02cec3b4ed998/t/5df2839b04b7db043c691f5d/1576174494551/CA+Bridge+Study+Protocol+-+Main+Study.pdf
- 68.Office of National Drug Control Policy. The Biden-harris administration’s statement of drug policy priorities for year one. Published online April 1, 2021.
- 69.Krive J, Patel M, Gehm L, et al. The complexity and challenges of the ICD-9-CM to ICD-10-CM transition in emergency departments. Am J Emerg Med. 2015;33(5):713–718. doi: 10.1016/j.ajem.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shearer RD, Shippee ND, Winkelman TNA. Characterizing trends in methamphetamine-related health care use when there is no ICD code for “methamphetamine use disorder”. J Subst Abuse Treat. 2021;127:108369. doi: 10.1016/j.jsat.2021.108369. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data is made publicly available through the National Center of Health Statistics and can be accessed through their website at https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm