Abstract
The global COVID-19 pandemic has affected the world’s population by causing changes in behavior, such as social distancing, masking, restricting people’s movement, and evaluating existing medication as potential therapies. Many pre-existing medications such as tocilizumab, ivermectin, colchicine, interferon, and steroids have been evaluated for being repurposed to use for the treatment of COVID-19. None of these agents have been effective except for steroids and, to a lesser degree, tocilizumab. Ivermectin has been one of the suggested repurposed medications which exhibit an in vitro inhibitory activity on SARS-CoV-2 replication. The most recommended dose of ivermectin for the treatment of COVID-19 is 150–200 µg/kg twice daily. As ivermectin adoption for COVID-19 increased, the Food and Drug Administration (FDA) issued a warning on its use during the pandemic. However, the drug remains of interest to clinicians and has shown some promise in observational studies. This narrative reviews the toxicological profile and some potential therapeutic effects of ivermectin. Based on the current dose recommendation, ivermectin appears to be safe with minimum side effects. However, serious questions remain about the effectiveness of this drug in the treatment of patients with COVID-19.
Keywords: Ivermectin, COVID-19, SARS-CoV-2, Coronavirus disease 2019
Introduction
In late 2019, the world faced a new life-threatening disease, the coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. The causative agent was first reported in Wuhan City, the capital of Hubei province in China. On 30 January, 2020, the World Health Organization (WHO) revealed COVID-19 as a public health emergency and an international issue [2, 3]. Surprisingly, a high number of new cases were detected worldwide in the first week of March, and COVID-19 established as a pandemic. As of 12 March, 2020, more than 125,000 confirmed cases and more than 4600 deaths were reported in 118 countries [2, 4]. The most common symptoms of this disease include cough, fever, fatigue, shortness of breath, pneumonia, and the common cold [5]. Also, some less frequent symptoms of SARS-CoV-2 infection are anosmia, dysgeusia, skin lesion, gastrointestinal symptoms, and headache [6–9].
Throughout the COVID-19 pandemic, many therapeutic agents have been repurposed and applied empirically and within clinical trials. Prophylactic medications for COVID-19 could have benefits. Furthermore, the efficacy of remdesivir, hydroxychloroquine, lopinavir/ritonavir, convalescent plasma, and monoclonal antibody therapy in decreasing mortality, when administered late in the course of the disease, is debated [10, 11]. Ivermectin is an exciting anti-parasitic medication that has received much attention recently [12].
In 2015, Japanese scientist, Satoshi Omura, was awarded the Nobel Prize in Physiology and Medicine for the discovery of ivermectin in 1974–1975 [13]. Ivermectin was first marketed as an anti-parasite drug by Merck Sharp and Dohme in 1981. It remains the world's leading anti-parasitic agent for livestock [14]. Some studies examined ivermectin's utility in COVID-19 patients. It has been reported that its administration reduced hospital stay and mortality of COVID-19 patients [15–17]. There is a need for compilation of the latest information on this drug from different corners of the world. Such data are likely to provide a better picture of the scope and limitations of ivermectin use in COVID-19. In this perspective review, ivermectin’s efficacy, and possible toxicity in the treatment of COVID-19 disease as a means to explore opportunities for expanded use of this drug are discussed.
Pharmacodynamics and pharmacokinetic of ivermectin
Ivermectin inhibits the transmission of chemicals at nerve synapses using glutamate-containing anion channels or γ-aminobutyric acid-containing chloride channels. It stimulates γ-aminobutyric acid (GABA) secretion from the presynaptic nerve end and increases binding to the postsynaptic receptors [18]. Also, ivermectin is believed to exhibit an effect that involves inhibition of viral protein translocation in a complex with importin (IMPα/β1) into the nucleus. The infected cells release interferon (IFN) that binds to the IFN receptors in neighboring cells, alerting them to a viral attack. The IFN-I and IFN-III receptors then further activate members of the JAK-STAT family. After entering the host cell, the COVID-19 virus acts in a way so as to interfere with the host cell’s natural anti-viral response through the effect of interferon. The proteins of SARSCoV-2 such as ORF3a, ORF6, and NSP1 suppress IFN-I signaling [19, 20]. As a result, cells around the virus-infected cells “fail” to receive “protective IFN signals”, allowing the SARS-CoV-2 virus to multiply and spread without hindrance [21]. It has been observed that ivermectin can enhance the expression of some IFN-related genes, such as IFIT1, IFIT2, IF144, IRF9, ISG20, and OASL [22]. The SARS-CoV-2 pathogenicity is possibly involved in inhibition of type I interferon (IFN-I) immune signaling, resulting in reduced Janus Kinase (JAK)-Signal Transducer and Activator of Transcription 1 (STAT1) signaling and anti-viral response. In the absence of a virus, phosphorylation activates STAT1 and can interact with IFN regulatory factor 9, which produces the IFN-stimulated gene factor 3 transcription complexes. This complex gets into the nucleus and binds to the IFN-stimulated response element, promoting host’s anti-viral response [23–27]. Ivermectin has the potential to target and inhibit SARS-CoV-2 replication by blocking viral entry into the nucleus. Hence, the Signal Transducer and Activator of Transcription 1 (STAT1) signaling is unaltered by the antagonistic activity of SARS-CoV-2, and the anti-viral response takes place. In vitro studies have demonstrated that the enzyme, CYP3A4, primarily metabolizes ivermectin. Depending on the in vitro method used enzymes, CYP2E1 and CYP2D6 were also involved in ivermectin’s metabolism, albeit to a much lesser extent than CYP3A4. The results of in vitro studies with human liver microsomes indicate that clinically relevant concentrations of ivermectin do not significantly inhibit the metabolic activities of CYP3A4, CYP2C9, CYP2E1, and CYP2E1 [28, 29].
Liver metabolisms convert ivermectin to at least ten metabolites, most of them being hydroxylated and demethylated derivatives of the drug. The drug is mainly eliminated in the feces, and fecal excretion accounts for 90% of the dose administered, with less than 2% of the dose excreted in the urine. Bile is the main route of excretion, and its elimination half-life is around a day [30].
Therapeutic use and dosage of ivermectin
Ivermectin is indicated for treating strongyloidiasis of the intestinal tract and onchocerciasis [31].
Onchocerciasis patients are generally treated as an annual oral dose (e.g., 150 or 200 µg/kg). Lymphatic filariasis is treated in endemic areas once a year (300–400 µg kg) or sometimes, twice a year (150–200 μg/kg) [31, 32]. Maximum doses of 2000 μg/kg are well tolerated in patients with parasitic infections [32, 33].
Analysis of data on severe adverse events (SAE) over 13 years in Africa revealed a cumulative incidence of 1 reported SAE per 800,000 reported treatments with ivermectin [34, 35]. No significant parasitic resistance to this drug has been observed in humans. Evidence suggests that ivermectin is a safe and effective anti-parasitic and anti-inflammatory agent that will continue to be used a main therapeutic course for parasitic infections for years to come [36]. It is believed that ivermectin has many cellular targets, and it has some anti-bacterial and anti-cancer activity [37]. It has also been observed through both in vitro and in vivo studies that ivermectin has some effects on several viruses. Several studies have shown that ivermectin might be helpful in treating COVID-19 patients at both mild–moderate and severe phases of the disease, and also as a potential prophylaxis [38–40].
The possibility of effectiveness against SARS-COV-2
Biological plausibility
It is proposed that ivermectin might have anti-viral and immunomodulatory properties [16, 39, 40]. There are several biologically plausible reasons for the activity of ivermectin against SARS-cov2 in the treatment of COVID-19:
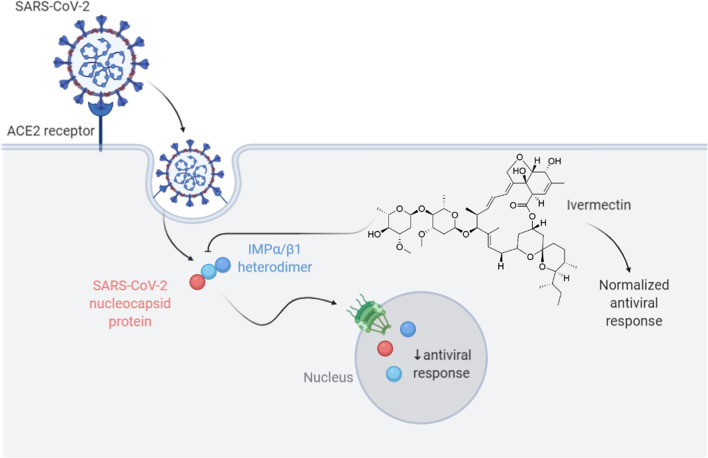
Ivermectin acts as a specific inhibitor of α/β-heterodimer in the nucleus of the cell, inhibiting replication of several RNA viruses [41–43]. It is presumed that ivermectin might inhibit SARS-CoV-2 using the same mechanism [44]. Additionally, Caly et al. have shown that the drug prevents SARS-CoV-2 replication and reproduction [44]. In their research, ivermectin was added to cells infected with SARS-CoV-2 RNA and they were analyzed by RT-PCR for observing the replication of the SARS-CoV-2 RNA at days 0–3. These cells were compared with the ones in the control group which did not receive ivermectin treatment. It was found that after 48 h, there was a ≈5000-fold reduction in viral RNA in the ivermectin treated cells compared to the control samples, and no toxicity was reported [44]. Spike protein on the viral envelope binds to the ACE-2 receptor and enters the cell through endocytosis, where importin (IMP) α/β1(IMPα/β1) binds to the viral nucleocapsid protein. The complex enters the nucleus through the nuclear pore complex (NPC) and separates, reducing the anti-viral reaction. In the presence of ivermectin, SARS-CoV-2 proteins are unable to bind to IMPα/ß1 heterodimers, as ivermectin destabilizes them (Fig. 1).
Ivermectin acts as a possible ionophore in infected cells disrupting biologic membrane in these cells [37].
Ivermectin has been reported to curb over-reacting innate and cellular immune responses during the inflammatory stage of COVID-19 [41, 45]. It has shown to have powerful anti-inflammatory properties through the inhibition of both production of cytokine and transcription of the most potent mediator of inflammation, the nuclear factor-κB (NF-κB) [46]. Therefore, theoretically, ivermectin might alleviate the symptoms of COVID-19 patients in the viral replication phase (in the first 7–10 days of infection) and later, in the hyper-inflammatory stage [41–44].
Interaction with ACE protein: Abdel-Mottaleb et al. demonstrated that ivermectin, hydroxychloroquine, and favipiravir are the most effective drugs that bind to ACE-2 and S protein in the human body [47]. A molecular modeling study by Dayer et al. also showed that ivermectin is one of the most effective agents that shields the host cells’ receptors from the SARS-CoV-2 spike protein [48]. Another study by Lehrer et al. showed that ivermectin docked leucine and histidine to the ACE-2 receptors [49]. In addition, Janabi et al., in computer-assisted molecular modeling, investigated the drug’s affinity for the active site of RNA-dependent RNA polymerase (RdRp). Five molecules, including ivermectin, were docked to the protein binding site using PyMol software, and the study reported a high binding affinity of ivermectin to RdRp [50].
Fig. 1.
Proposed ivermectin mechanism of action on SARS-CoV-2. S protein on the viral envelope binds to the ACE-2 receptor and enters the cell through endocytosis, where IMPα/β1 binds to the viral nucleocapsid protein. The complex enters the nucleus through the nuclear pore complex (NPC) and separates, reducing the anti-viral reaction. In the presence of ivermectin, SARS-CoV-2 proteins are unable to bind to IMPα/ß1 heterodimers, as ivermectin destabilizes them
Clinical studies
In a multi-center case–control study of 280 hospitalized patients, ivermectin was administered as a single dose of 150 µg/kg to patients with COVID-19. It significantly reduced in-hospital mortality (ivermectin: 1.4% vs. non-ivermectin: 8.5%; HR: 0.2, CI 95%: 0.11–0.37, p < 0.0001) [51]. The findings of a double-blind randomized clinical trial (RCT) in Colombia do not support the ivermectin use in the treatment of mild COVID-19. In this study, patients with mild SARS-CoV-2 infection received ivermectin (300 μg/kg/day for 5 days, n = 200) or placebo (n = 200). They found that a 5-day course of ivermectin did not significantly improve the time taken for symptom resolution compared with the placebo [52]. In another retrospective study by Camprubí et al., 13 patients admitted with severe COVID-19 received a standard dose of ivermectin (200 μg/kg). No differences were reported in the mobility, microbiological or clinical outcomes in this group of patients compared to a similar group of patients who did not receive ivermectin [53]. In another randomized double-blind clinical trial, three groups of patients were administered ivermectin 24 mg, ivermectin 12 mg, and a placebo, respectively. The negative RT-PCR at day 5 failed to show statistical significances (24 mg ivermectin: 47.5%: 12 mg ivermectin, 35.0%; and placebo: 31.1%; p: 0.3). The decrease in viral load on day 5 was similar in the three groups [54]. Chaccour et al. in a small, double-blind RCT in Spain randomized 24 patients to ivermectin and placebo groups. They found no differences in positive RT-PCR on day 7, but they reported statistically significant reduction in the viral load [55]. WHO recently commissioned a meta-analysis to evaluate the clinical efficacy of ivermectin using the ACC Accelerator Program. The meta-analysis consisted of 18 RCTs evaluating doses up to 0.6 mg/kg of ivermectin on a total of 2282 RT-PCR positive patients with mild-severe COVID-19. Six trials evaluated the efficacy of ivermectin on survival in 1255 patients using doses between 200 and 400 µg/kg in a 1–5 day treatment and found a 75% reduction in mortality (Relative Risk: 0.25, CI 95% 0.12–0.52, p < 0.0002) with ivermectin treatment. In addition, a reduction in the hospital stay was reported. Regarding viral clearance, the effect of ivermectin was greater in clinical trials evaluating its effects for up to five days [56]. Mohan-Padhy et al. performed another meta-analysis on four studies with a total of 629 COVID-19 patients, to evaluate the therapeutic effects of ivermectin at a standard dose of 200 µg/kg as an adjuvant therapy to the standard care. An overall odds ratio of 0.53 (95% CI 0.29–0.96) was found for the all-cause mortality that was statistically significant (p = 0.04) [57]. In a pre-print paper, Maurya et al. argue that ivermectin in combination with doxycycline may enhance the inhibition of viral entry, therefore, decreasing viral load and replication [58]. A propensity-matched cohort study was conducted in Florida by Rajter et al. on 280 patients, 173 of whom were treated with ivermectin and 107 without it. The ivermectin group had a significantly lower mortality rate (13.3% vs. 24.5%, OR 0.47, CI 0.22–0.99, p < 0.05) [15]. Rahman et al. conducted a prospective study in Bangladesh, enrolling patients with mild-to-moderate COVID-19 disease and comparing the effect of ivermectin plus doxycycline to hydroxychloroquine plus azithromycin. Two hundred patients received ivermectin (18 mg on the first day) and doxycycline (100 mg twice daily for 5 days), while the other 200 patients received hydroxychloroquine (800 mg on the first day and 400 mg daily for the next 10 days) and azithromycin (500 mg on the first day and 250 mg daily for 4 days after that). From this study, ivermectin plus doxycycline together were found to be safe and more effective in early viral clearance in patients with mild-to-moderate disease compared to hydroxychloroquine and azithromycin combination [59]. Another clinical trial was conducted on in-patients with mild-to-moderate COVID-19 infections. Sixteen patients received a single dose of ivermectin of 200 µg/kg, hydroxychloroquine (HCQ), and azithromycin (AZT) on admission day. They were compared with 71 controls of matching age, gender, clinical features, and comorbidities who received only HCQ and AZT. [16 (100%) vs. 69 (97.2%)]. Two patients died in the controls. The average hospital stay was significantly lower in the ivermectin group than in the control group (7.62 ± 2.75 vs. 13.22 ± 5.90 days, p = 0.00005, size of effect = 0.82), and no toxicity or adverse events were noted [16]. In a cross-sectional study by Malik et al., most healthcare professionals were treated with either azithromycin or doxycycline, with favorable outcomes observed [60]. A further study by Alam et al. in Bangladesh reported that the combination of ivermectin and doxycycline is efficient in SARS-CoV-2 clearance in patients with mild-to-moderate disease. They enrolled 100 patients with mild and moderate COVID-19 in their study. They treated them with a combination of ivermectin (200 µg/kg single dose) and doxycycline (100 mg daily for 10 days) in addition to supportive treatment. All patients' symptoms improved within 72 h, no side effects were observed, no other treatment was required, and there was no death in this study [61].
Another clinical trial in Iraq was conducted with 70 COVID-19 patients (48 mild–moderate, 11 severe, and 11 critical patients) who were treated with 200 µg/kg of oral ivermectin per day for 2–3 days along with 100 mg PO doxycycline twice per day for 5–10 days plus standard therapy. The control group of COVID-19 patients (48 mild–moderate and 22 severe and zero critical patients) was given standard treatment [45]. The time to recovery was seen to have significantly reduced in the ivermectin–doxycycline group compared to the control group; the mean recovery time in the ivermectin–doxycycline group was 10.61 ± 5.3 days versus mean recovery time in a control group, 17.9 ± 6.8 days (p < 0.05). The mortality rate was 0/48 (0%), 0/11 (0%) and 2/11 (18.2%) in moderate, severe and critical COVID-19 patients in the ivermectin–doxycycline group, respectively, compared to 0/48 (0%) and 6/22 (27.27%) in moderate and severe COVID-19 patients in the standard therapy group, thus, showing no significant difference (p = 0.052). A preprint observational analysis in Argentina by Carvallo et al. has reported only one mortality rate in 167 COVID-19 patients (135 mild, 32 moderate to severe) who received a combination of dexamethasone, aspirin, enoxaparin, and ivermectin protocol [40]. Chowdhury et al. also compared the combination of ivermectin and doxycycline with hydroxychloroquine and azithromycin in people with mild-to-moderate COVID-19 infections. Patients were categorized into two groups. The first group (n = 60) received ivermectin (200 µg/kg one dose) and doxycycline (100 mg twice daily for 10 days), and the second group (n = 56) received hydroxychloroquine (400 mg on the first day and 200 mg twice daily for the next 9 days) and azithromycin (500 mg daily for 5 days). According to this study, ivermectin and doxycycline were found to be superior to hydroxychloroquine and azithromycin in treating mild-to-moderate COVID-19 patients, but the time required for the patients to be symptom-free and achieve a negative COVID test was not statistically significant [62]. Shouman conducted a randomized clinical trial in Egypt, including 340 (228 treated, 112 controlled) patients who received ivermectin twice on the day of a positive COVID-19 test and thereafter, once at day 3 based on their body weight (40–60 kg: 15 mg, 60–80 kg: 18 mg, > 80 kg: 24 mg). After a 2-week follow-up, the case group showed a significant reduction in COVID-19 symptoms compared to the control group (7.4% vs. 58.4%, p < 0.001) [63].
The potential efficacy of ivermectin as prophylaxis for COVID-19
Héctor et al. conducted a prospective observational study in which they gave ivermectin and carrageenan daily to healthy volunteers for 28 days, comparing them to similarly healthy controls who did not take the drugs. Of the 229 study participants, 131 were treated with 0.2 mg ivermectin drops taken by mouth five times a day. After 28 days, none of the participants receiving ivermectin prophylaxis tested positive for SARS-COV-2, compared to 11.2% of the participants in the control group who tested positive [64]. In line with other prophylaxis reports, a recently published Preprint Matching Case–Control 374 study on medRxiv, which analyzed several drugs experimentally used as COVID-19 375 prophylaxis, showed a 73% reduction in COVID-19 infections in health care workers after two doses of ivermectin (OR 0.27; 95% CI 0.15–0.51) [65]. Remarkably, this study did not establish that a single dose of prophylaxis has a protective effect.
Probably the clearest evidence of the effectiveness of ivermectin as a prophylactic agent was recently published, comparing countries with presently active ivermectin mass drug delivery programs for the prevention of parasite infections. They found that COVID-19 case numbers were significantly lower in countries with such active programs [66]. What is evident is that both clinical and basic science studies are weak, and lack the preponderance of evidence in support of ivermectin for clinical use. However, ivermectin remains one of the drugs used for the treatment of COVID-19 and it has attracted our attention due to its safety profile.
Safety, side effects, and tolerated doses of ivermectin in humans
In cases of accidental poisoning with veterinary ivermectin formulations in humans, symptoms like rash, edema, headaches, dizziness, nausea, vomiting, diarrhea, and asthenia were often reported. Other adverse effects include seizures, dyspnea, paresthesia, urticaria, abdominal pain, and contact dermatitis [67]. In humans, the most common adverse effects of ivermectin in oral doses are fatigue (13%) and headache (9%), dizziness and drowsiness (10%), and itching (12%) and lightheadedness (9%) [68]. Muñoz et al. assessed the adverse effects of ivermectin in 54 voluntary participants and reported that the most frequent side effects were headache (6.02%), dysmenorrhea (5.54%), throat pain (1.80%) and diarrhea (1.80%). Of the 33 reported adverse effects, 10 were classified as mild and 23, as moderate [69].
Kamgno et al. evaluated and compared side effects of a standard dose and a high dose of ivermectin using a 3-year double-blind RCT. They reported that the common manifestations after ivermectin treatment were itching, edematous swellings, rash, and fever. Also, swellings seemed to be more associated with high-dose treatment as compared to standard dose treatment. In addition to these symptoms which have been reported classically in many literatures, the results showed that treatment with ivermectin was also related with a risk of ocular problems (blurred vision, change in color vision, etc.,) [70]. The pharmacokinetic properties and safety of ivermectin were studied in a multiple-dose clinical trial with healthy volunteers. Sixty-eight volunteers were assigned to four groups: 30 mg (three times a week) followed by a single dose after a 1-week washout, 60 mg (three times a week), 90 mg (single dose), and 120 mg (single dose). Safety assessments addressed both known ivermectin central nervous system (CNS) effects and general toxicity. The primary endpoint of safety was mydriasis, which was precisely quantified by pupillometry. Ivermectin was generally well tolerated, with no associated CNS toxicity at doses up to 10 times the FDA-approved maximum dose of 200 µg/kg. All doses had a mydriatic effect like a placebo. The adverse experiences between ivermectin and placebo were similar and did not increase with the ivermectin dose [32]. A recent meta-analysis showed that adverse events following a single dose treatment of up to 800 µg/kg of ivermectin do not occur with significant differences in frequency or intensity compared to currently approved doses [33]. Some studies reported an increased risk of deaths in elderly patients who were treated with an oral dose of ivermectin (150–200 µg/kg) for scabies. These findings were not replicated in other studies. Besides, long-term studies of ivermectin use in elderly populations found no excess deaths and no serious side effects [71].
The safety of higher doses of ivermectin was investigated in a phase III study that examined 200–400 μg/kg doses in patients with dengue fever and demonstrated that a daily dose of ivermectin treatment over three days is safe [72]. In another study by Guzzo et al., even higher doses (up to 10 times higher than approved doses) were investigated [32]. This study showed that ivermectin was well tolerated during fasting after a one-time dose of 120 mg (10 times higher than the approved dose) and 60 mg three times weekly (every 72 h). In their study, typical side effects of ivermectin treatment include nausea, dizziness, headaches, and rash. The frequency and nature of adverse events were relatively similar between ivermectin (24%) and placebo (35%) and did not increase with increase in the ivermectin dose. All dosages had mydriatic effects (the primary endpoint of safety from toxicology study results) similar to placebos [32]. Similarly, ivermectin was well tolerated at a single dose of 800 µg/kg, at 1600 µg/kg for 12 weeks, and at 1600 µg/kg for 13 days [73]. Also, an oral dose of ivermectin of up to 1400 µg/kg over a month is recommended by the US CDC as a treatment option for scabies [74]. Ocular side effects (temporary blurred vision, itching, pain in the eye, and dyschromatopsia) are important in onchocerciasis patients and require caution and further investigations when ivermectin is used in high doses for this indication. The adverse events reported in the reviewed studies were mostly mild or moderate, suggesting ivermectin’s safety [33].
Severe side effects of ivermectin
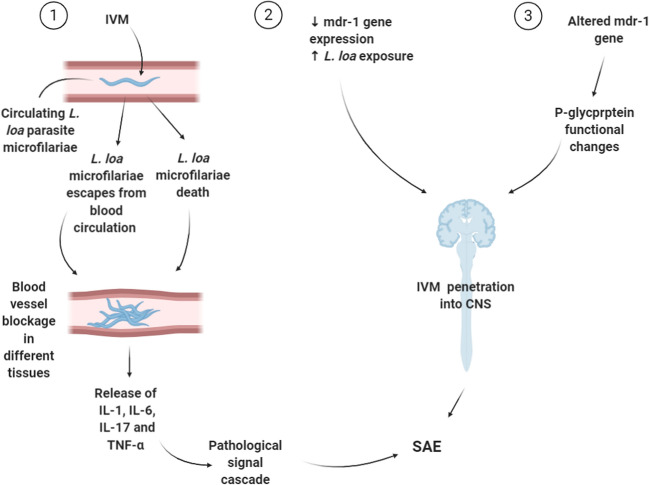
In terms of central nervous system-related events, ivermectin is considered safe theoretically, as its distribution to the brain is blocked by the blood–brain barrier (BBB). In particular, this is due to the size of the ivermectin molecule and the presence of efflux pumps. The primary efflux pump that transports ivermectin is the P-glycoprotein pump (P-gp) (ivermectin is both a substrate and a potent inducer of the P-gp). P-gp is involved in transporting ivermectin to the intestinal tract and preventing it from crossing the BBB. Therefore, ivermectin has generally been considered safe and free of potential neurologic adverse drug reactions, except in case of an overdose [75]. However, some neuralgic adverse effects have been reported. In 2018, Chandler et al. reported on the adverse effects from ivermectin and its safety. In their study, the common side effects of the drug were pruritus (25.3%), headache (13.9%), and dizziness (7.5%). They also reported some serious neurological side effects such as encephalopathy and coma [75]. These neurologic side effects were suspected to be due to a CNS infection with a high number of L. loa microfilariae and the p-glycoprotein drug pump’s failure as a result of lower expression of the mdr-1 gene [76]. Ivermectin causes the circulatory L. loa microfilariae death and their escape into other body fluids. These events result in a blood vessel blockage, which is followed by cytokine and tumor necrosis factor alpha release. The pathological signal cascade is associated with CNS adverse events, as also blocked blood vessels in various tissues cause tissue anoxia and death (Fig. 2). In a study, Twum-Danso et al. assessed all serious adverse events (SAE) that occurred in Africa from the introduction of mass treatment programs with ivermectin for onchocerciasis in 1989 until the end of the calendar year 2001. They reported 207 SAE cases in about 165 million reported treatments performed during the reporting period, resulting in a cumulative incidence of 1 reported SAE per 800,000 reported treatments. 97 cases were encephalopathic, two-thirds of these cases were ‘probable’ or ‘possible’ cases of Loa loa encephalopathy, temporally related to ivermectin treatment [77]. In Australia, between January, 1971 and December, 2013, 17 adverse events, including three reports of fatal adverse events from ivermectin treatment were reported to the Therapeutic Goods Administration (TGA), but no causal association with ivermectin could be detected [78]. Table 1 shows the descriptive analysis of adverse events of ivermectin in clinical trials.
Fig. 2.
Mechanism of adverse reactions caused by ivermectin in the presence of L. loa
Table 1.
Descriptive analysis of adverse events of ivermectin in clinical trials comparing standard (up to 400 µg/kg) vs. high dose (> 400 µg/kg) of ivermectin
| Condition under study | Ivermectin dosage (µg/kg) | Adverse effects rate (%) | Odds ratio or risk difference (95% CI) | |
|---|---|---|---|---|
| Kamgno et al. [70] | Onchocerciasis | 0.96 (0.64–1.44) | ||
| High dose | 800 | 14.8 | ||
| Standard dose | 150 | 15 | ||
| Munoz et al. [33] | Healthy volunteers | 0.907 (0.369–2.228) | ||
| High dose | 401–700 | 16 | ||
| Standard dose | 200–400 | 17 | ||
| Smit et al. [95] | Malaria | 6·9% (− 1·9 to 15·7) | ||
| High dose | 600 | 11 | ||
| Standard dose | 300 | 4 | ||
| Wimmersberger et al. [33] | Trichuriasis | 1.346 (0.532–3.405) | ||
| High dose | 600 | 27 | ||
| Standard dose | 100–400 | 22 | ||
Chandler et al. also reported two deaths attributed to ivermectin [75]. The first was the death of an 81-year-old woman who had received 12 mg of ivermectin on days 0 and 7 for the treatment of acarodermatitis. She died 5 days after the last dose from the events of a depressed level of consciousness and asphyxia. Also, she was receiving other medications like digoxin, rebamipide, crotamiton, and magnesium oxide. The second case was that of a 64-year-old man with a history of giant cellular arteritis treated with prednisone and who had developed sepsis after an aortic valve replacement surgery complicated by multi-system failure. Sputum culture revealed S. stercoralis presence. Strongyloides stercoralis and hyper-infection syndrome was diagnosed, and ivermectin 12 mg was administered every 48 h. He was given three oral doses of the drug, followed by two subcutaneous ones. Despite clinical and microbiological improvements, the patient remained in a vegetative state and died on day 25. The autopsy revealed elevated levels of ivermectin in the brain tissue 14 days after the last dose. Both cases did not meet the criteria of causality of death by ivermectin, but documented the presence of ivermectin in the brain tissue [79]. Sparsa et al. also reported severe side effects of ivermectin at a dose of 200 µg/kg. Most of the side effects observed with this medication were observed in the treatment of two elderly patients with scabies. The first was a 72-year-old man referred for scabies who was treated with benzyl benzoate (Ascabiol) and ivermectin (200 µg/kg) in a single dose. Two days later, the patient had abdominal pain and nausea, and elevated liver function parameters. Laboratory tests did not show cytolysis as a cause of hepatitis. Ivermectin-induced hepatitis was assumed and liver function returned to normal within 2 weeks. The second case was an 86-year-old woman hospitalized for scabies and treated with benzyl benzoate and a single ivermectin dose (200 µg/kg). Three days later, she developed sinus tachycardia and asthma. Ivermectin-induced cardiac toxicity was suspected [80]. Compared to the extensive post-marketing experience with ivermectin, SAEs are rare and have never met the causative criteria. However, clarifying individual risk factors such as advanced age, co-infection, and potential drug polymorphism with mdr-1 gene should be considered [75].
Discussion
In the light of the pandemic of SARS-COV-2 and the need for new or repurposed medication for the treatment of COVID-19, attention has been paid to three potential anti-viral chemicals. These include anti-malarial (hydroxychloroquine/chloroquine), anti-metabolites (colchicine), [81] and anti-parasitic (ivermectin) [82]. Although initially hydroxychloroquine/chloroquine were thought to be effective agents against SARS-COV-2, subsequent clinical trials have found these agents to be toxic and more harmful than ivermectin. Among these three proposed drugs, ivermectin shows the best safety profile, tolerated at high doses, and the least toxicity profile [33, 46]. Additionally, ivermectin's concurrent use with steroids, the proven effective drugs in the treatment of COVID-19 [83], might be beneficial beyond its potential anti-viral effect in its suppression of parasitic hyper-infection during anti-COVID therapy. Ivermectin targets glutamate-containing chloride channels in invertebrates. However, these agents show selectivity to parasites and do not enter the mammalian central nervous system to cause toxicity [84, 85].
In humans, healthy blood–brain barrier (BBB) and p-glycoproteins typically prevent ivermectin’s entry to the central nervous system and limit its toxicity. However, in patients with hyper-inflammatory diseases, drug–drug interactions can lead to an increase in the concentration of ivermectin, or in case of dysfunctions of the p-glycoprotein pump, ivermectin may penetrate the CNS, and increase the risk of toxicity [86]. Several serious neurological effects of ivermectin are attributed to drug interactions [75], including several cases of the simultaneous use of medicines such as statins, HIV protease inhibitors, calcium channel blockers, and benzodiazepines [75]. Ivermectin is considered to trigger several cytochrome P450 isoenzymes, including CYP1A, 2B, and 3A subfamilies [87], which can disrupt a large percentage of therapeutic agents. Drugs that are substrates of CYP3A4 enzymes are often also substrates of the P-glycoprotein transporter. Therefore, there is a risk of increased absorption beyond the blood–brain barrier when those drug are administered simultaneously with ivermectin [88]. Also, enhanced anti-virals, like lupinavir ritonavir and darunavir are potent cytochrome P450 3A4 inhibitors widely used against SARS-CoV-2. Concomitant use of these drugs with ivermectin may lead to increased systemic exposure to ivermectin and CNS toxicity. Additionally, ritonavir and its enhancers like cobicistat (used to increase the amount of atazanavir) can efficiently inhibit p-glycoprotein, one of the significant outlet pumps in the BBB, thereby causing more neurotoxicity [75]. A recent publication documents evidence of an in vitro interaction between ivermectin and a range of anti-retroviral agents [89]. Current labeling of ivermectin does not warn against its co-administration with CYP3A4 substrates [75]. Available evidence suggests that ivermectin levels with significant activity against SARS-CoV-2 may only be achieved with a considerable increase in its dose which could have toxic effects [84]. Although pharmacokinetic studies on healthy subjects have shown that single doses of up to 120 mg of ivermectin are safe and well-tolerated, the concentration achieved may be of an order of magnitude lower than the Cmax necessary for anti-SARS-COV-2 activity seen in vitro [32]. Some evidence from animal models shows ivermectin levels that are three times more abundant in lung tissue than in plasma, one week after the oral dose [90]. However, even with the high lung:plasma concentrations ratio, ivermectin is unlikely to reach the half-maximal inhibitory concentration (IC50) in the lungs after a single dose of 10 times higher than the approved US Food and Drug Administration (FDA) dose when administered orally [91, 92].
Conclusion
Based on the current data and the recommended dose of 150–200 µg/kg for COVID-19 treatment, ivermectin is probably safe; however, there is some serious doubt about its efficacy in treating COVID-19. Ivermectin has a better safety profile than other purposed and repurposed drugs such as hydroxychloroquine and colchicine [93] that lack efficacy and, in the case of hydroxychloroquine, has been shown to be harmful [33, 46, 82, 94]. Before initiating a patient on ivermectin therapy, clinicians need to be aware that ivermectin doses necessary to block SARS-COV-2, patients’ inflammatory status, other concurrent medications, and patients' potential genetic polymorphism for the p-glycoprotein mdr-1 gene may enhance ivermectin’s toxicity and serious side effects in humans.
Acknowledgements
Not applicable.
Abbreviations
- COVID-19
Coronavirus disease 2019
- SARS-CoV-2
Severe acute respiratory syndrome Coronavirus 2
- FDA
Food and Drug Administration
- GABA
γ-Aminobutyric acid
- IFN-I
Type I interferon
- JAK
Janus kinase
- STAT1
Signal transducer and activator of transcription 1
- SAE
Severe adverse events
- IMPα/β1
Importin α/β1
- NPC
Nuclear pore complex
- NF-κB
Nuclear factor-κB
- RdRp
RNA-dependent RNA polymerase
- HCQ
Hydroxychloroquine
- AZT
Azithromycin
- BBB
Blood–brain barrier
- TGA
Therapeutic Goods Administration
- IC50
Inhibitory concentration 50
Authors’ contributions
FMS, RM, SN, AN, SHGH, OM contributed to the conception, design, and preparation of the manuscript. FMS, RM, AN, OM conducted the data collection and contributed to acquisition and interpretation. FMS, RM, SN, AN, SHGH, OM made substantial contributions in drafting the manuscript and revising it critically for important intellectual content. All authors read and approved the final manuscript.
Funding
No funding was obtained for this study.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors take full responsibility for the contents of this article, and confirm that there are no conflicts of interests associated with this publication. The employment affiliations of all authors are presented on the cover page. This review article was not prepared on any request and has not been supported financially. The views and opinions expressed in the paper are those of the authors. The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ataei M, et al. A double-edged sword of using opioids and COVID-19: a toxicological view. Subst Abuse Treat Prev Policy. 2020;15(1):1–4. doi: 10.1186/s13011-020-00333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhagavathula AS, et al. Novel coronavirus (COVID-19) knowledge and perceptions: a survey on healthcare workers. medRxiv. 2020;6(2):e19160. doi: 10.2196/19160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eurosurveillance Editorial Team Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Eurosurveillance. 2020;25(5):200131e. doi: 10.2807/1560-7917.ES.2020.25.5.200131e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Novel coronavirus (COVID-19) situation. https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd. Accessed 13 Mar 2020.
- 5.Ahad MA. Coronavirus—a global emergency. Medicine Today. 2020;32(2):138–142. [Google Scholar]
- 6.Guarneri C, et al. Silent COVID-19: what your skin can reveal. Lancet Infect Dis. 2021;21(1):24–25. doi: 10.1016/S1473-3099(20)30402-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaira LA, et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: single-center experience on 72 cases. Head Neck. 2020;42(6):1252–1258. doi: 10.1002/hed.26204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geremia N, et al. A case of vasculitis-like skin eruption associated with COVID-19. Infect Dis Clin Pract. 2020;28(6):e30–e31. [Google Scholar]
- 9.Gonzalez-Martinez A, et al. Headache during SARS-CoV-2 infection as an early symptom associated with a more benign course of disease: a case–control study. Eur J Neurol. 2021;28(10):3426–3436. doi: 10.1111/ene.14718. [DOI] [PubMed] [Google Scholar]
- 10.Vijayvargiya P, et al. Treatment considerations for COVID-19: a critical review of the evidence (or lack thereof) Mayo Clin Proc. 2020;95(7):1454–1466. doi: 10.1016/j.mayocp.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yavuz S, Ünal S. Antiviral treatment of COVID-19. Turkish J Med Sci. 2020;50(SI-1):611–619. doi: 10.3906/sag-2004-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laing R, Gillan V, Devaney E. Ivermectin–old drug, new tricks? Trends Parasitol. 2017;33(6):463–472. doi: 10.1016/j.pt.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Õmura S, Crump A. The life and times of ivermectin—a success story. Nat Rev Microbiol. 2004;2(12):984–989. doi: 10.1038/nrmicro1048. [DOI] [PubMed] [Google Scholar]
- 14.Canga AG, et al. The pharmacokinetics and metabolism of ivermectin in domestic animal species. Vet J. 2009;179(1):25–37. doi: 10.1016/j.tvjl.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Rajter JC, et al. Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the Ivermectin in COVID nineteen study. Chest. 2021;159(1):85–92. doi: 10.1016/j.chest.2020.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorial FI, et al. Effectiveness of ivermectin as add-on therapy in COVID-19 management (pilot trial) medRxiv. 2020 doi: 10.1101/2020.07.07.20145979. [DOI] [Google Scholar]
- 17.Khan MSI, et al. Ivermectin treatment may improve the prognosis of patients with COVID-19. Arch Bronconeumol. 2020;56(12):828. doi: 10.1016/j.arbr.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dourmishev AL, Dourmishev LA, Schwartz RA. Ivermectin: pharmacology and application in dermatology. Int J Dermatol. 2005;44(12):981–988. doi: 10.1111/j.1365-4632.2004.02253.x. [DOI] [PubMed] [Google Scholar]
- 19.Konno Y, et al. SARS-CoV-2 ORF3b is a potent interferon antagonist whose activity is increased by a naturally occurring elongation variant. Cell Rep. 2020;32(12):108185. doi: 10.1016/j.celrep.2020.108185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang D, et al. Attenuated interferon and proinflammatory response in SARS-CoV-2–infected human dendritic cells is associated with viral antagonism of STAT1 phosphorylation. J Infect Dis. 2020;222(5):734–745. doi: 10.1093/infdis/jiaa356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuyama T, et al. An aberrant STAT pathway is central to COVID-19. Cell Death Differ. 2020;27(12):3209–3225. doi: 10.1038/s41418-020-00633-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zaidi AK, Dehgani-Mobaraki P. The mechanisms of action of Ivermectin against SARS-CoV-2: an evidence-based clinical review article. J Antibiot. 2021 doi: 10.1038/s41429-021-00430-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song Y, et al. COVID-19 treatment: close to a cure?—a rapid review of pharmacotherapies for the novel coronavirus. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.106080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chibber P, et al. Advances in the possible treatment of COVID-19: a review. Eur J Pharmacol. 2020;883:173372. doi: 10.1016/j.ejphar.2020.173372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mu J, et al. SARS-CoV-2 N protein antagonizes type I interferon signaling by suppressing phosphorylation and nuclear translocation of STAT1 and STAT2. Cell Discov. 2020;6(1):1–4. doi: 10.1038/s41421-020-00208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Worldometer. Coronavirus Update (Live): 113,124,037 Cases and 2,509,238 deaths from COVID-19 virus pandemic—worldometer. 2021. https://www.worldometers.info/coronavirus/. Accessed 25 Feb 2021.
- 27.World Health Organization. WHO Coronavirus Disease (COVID-19) dashboard. 2020. https://covid19.who.int. Accessed 16 Oct 2020.
- 28.Chaccour C, Hammann F, Rabinovich NR. Ivermectin to reduce malaria transmission I. Pharmacokinetic and pharmacodynamic considerations regarding efficacy and safety. Malaria J. 2017;16(1):1–16. doi: 10.1186/s12936-017-1801-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Malley PA. Ivermectin: 21st century “snake oil” or safe and effective for COVID-19? Clin Nurse Spec. 2022;36(1):16–19. doi: 10.1097/NUR.0000000000000640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canga AG, et al. The pharmacokinetics and interactions of ivermectin in humans—a mini-review. AAPS J. 2008;10(1):42–46. doi: 10.1208/s12248-007-9000-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henriquez-Camacho C, et al. Ivermectin versus albendazole or thiabendazole for Strongyloides stercoralis infection. Cochrane Database Syst Rev. 2016 doi: 10.1002/14651858.CD007745.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guzzo CA, et al. Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects. J Clin Pharmacol. 2002;42(10):1122–1133. doi: 10.1177/009127002401382731. [DOI] [PubMed] [Google Scholar]
- 33.Navarro M, et al. Safety of high-dose ivermectin: a systematic review and meta-analysis. J Antimicrob Chemother. 2020;75(4):827–834. doi: 10.1093/jac/dkz524. [DOI] [PubMed] [Google Scholar]
- 34.Twum-Danso NA, Meredith SE. Variation in incidence of serious adverse events after onchocerciasis treatment with ivermectin in areas of Cameroon co-endemic for loiasis. Tropical Med Int Health. 2003;8(9):820–831. doi: 10.1046/j.1365-3156.2003.01091.x. [DOI] [PubMed] [Google Scholar]
- 35.Ōmura S, Crump A. Ivermectin: panacea for resource-poor communities? Trends Parasitol. 2014;30(9):445–455. doi: 10.1016/j.pt.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Jans DA, Wagstaff KM. Ivermectin as a broad-spectrum host-directed antiviral: the real deal? Cells. 2020;9(9):2100. doi: 10.3390/cells9092100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rizzo E. Ivermectin, antiviral properties and COVID-19: a possible new mechanism of action. Naunyn Schmiedebergs Arch Pharmacol. 2020;393:1153–1156. doi: 10.1007/s00210-020-01902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vora A, et al. White paper on ivermectin as a potential therapy for COVID-19. Indian J Tuberc. 2020;67(3):448–451. doi: 10.1016/j.ijtb.2020.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mudatsir M, et al. Antiviral activity of ivermectin against SARS-CoV-2: an old-fashioned dog with a new trick—a literature review. Sci Pharm. 2020;88(3):36. [Google Scholar]
- 40.Carvallo HE, Hirsch RR, Farinella ME. Safety and Efficacy of the combined use of ivermectin, dexamethasone, enoxaparin and aspirin against COVID-19. medRxiv. 2020 doi: 10.1101/2020.09.10.20191619. [DOI] [Google Scholar]
- 41.Heidary F, Gharebaghi R. Ivermectin: a systematic review from antiviral effects to COVID-19 complementary regimen. J Antibiot. 2020;73(9):593–602. doi: 10.1038/s41429-020-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wagstaff KM, et al. Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem J. 2012;443(3):851–856. doi: 10.1042/BJ20120150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu T-L, et al. Antivirus effectiveness of ivermectin on dengue virus type 2 in Aedes albopictus. PLoS Negl Trop Dis. 2018;12(11):e0006934. doi: 10.1371/journal.pntd.0006934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caly L, et al. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antivir Res. 2020;178:104787. doi: 10.1016/j.antiviral.2020.104787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hashim HA, et al. Controlled randomized clinical trial on using ivermectin with doxycycline for treating COVID-19 patients in Baghdad, Iraq. MedRxiv. 2020 doi: 10.1101/2020.10.26.20219345. [DOI] [Google Scholar]
- 46.Kory P, et al. Review of the emerging evidence demonstrating the efficacy of ivermectin in the prophylaxis and treatment of COVID-19. Am J Ther. 2021;28(3):e299. doi: 10.1097/MJT.0000000000001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abdel-Mottaleb MS, Abdel-Mottaleb Y. In search for effective and safe drugs against SARS-CoV-2: part I simulated interactions between selected nutraceuticals, ACE2 enzyme and S protein simple peptide sequences. ChemRxiv. 2020 doi: 10.26434/chemrxiv.12155235.v1. [DOI] [Google Scholar]
- 48.Dayer MR. Coronavirus (2019-nCoV) deactivation via spike glycoprotein shielding by old drugs. Bioinform Study. 2020 doi: 10.20944/preprints202005.0020.v1. [DOI] [Google Scholar]
- 49.Lehrer S, Rheinstein PH. Ivermectin docks to the SARS-CoV-2 spike receptor-binding domain attached to ACE2. In Vivo. 2020;34(5):3023–3026. doi: 10.21873/invivo.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Janabi AHD. Effective anti-SARS-CoV-2 RNA dependent RNA polymerase drugs based on docking methods: the case of milbemycin, ivermectin, and baloxavir marboxil. Avicenna J Med Biotechnol. 2020;12(4):246. [PMC free article] [PubMed] [Google Scholar]
- 51.Cobos-Campos R, Apiñaniz A, Parraza N, Cordero J, García S, Orruño E. Potential use of ivermectin for the treatment and prophylaxis of SARS-CoV-2 infection. Curr Res Transl Med. 2021;69(4):103309. doi: 10.1016/j.retram.2021.103309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.López-Medina E, et al. Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial. JAMA. 2021;325(14):1426–1435. doi: 10.1001/jama.2021.3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Camprubí D, et al. Lack of efficacy of standard doses of ivermectin in severe COVID-19 patients. PLoS ONE. 2020;15(11):e0242184. doi: 10.1371/journal.pone.0242184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mohan A et al. Ivermectin in mild and moderate COVID-19 (RIVET-COV): a randomized, placebo-controlled trial. 2021. 10.21203/rs.3.rs-191648/v1. [DOI] [PMC free article] [PubMed]
- 55.Chaccour C, et al. The effect of early treatment with ivermectin on viral load, symptoms and humoral response in patients with non-severe COVID-19: A pilot, double-blind, placebo-controlled, randomized clinical trial. EClinicalMedicine. 2021;32:100720. doi: 10.1016/j.eclinm.2020.100720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hill A, et al. Meta-analysis of randomized trials of ivermectin to treat SARS-CoV-2 infection. Open Forum Infect Dis. 2021 doi: 10.21203/rs.3.rs-148845/v1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 57.Padhy BM, et al. Therapeutic potential of ivermectin as add on treatment in COVID 19: a systematic review and meta-analysis: ivermectin in COVID-19: a meta-analysis. J Pharm Pharm Sci. 2020;23:462–469. doi: 10.18433/jpps31457. [DOI] [PubMed] [Google Scholar]
- 58.Maurya DK. A combination of ivermectin and doxycycline possibly blocks the viral entry and modulate the innate immune response in COVID-19 patients. Biol Med Chem. 2020 doi: 10.26434/chemrxiv.12630539.v1. [DOI] [Google Scholar]
- 59.Rahman MA, et al. Comparison of viral clearance between ivermectin with doxycycline and hydroxychloroquine with azithromycin in COVID-19 patients. J Bangladesh Coll Phys Surg. 2020 doi: 10.3329/jbcps.v38i0.47514. [DOI] [Google Scholar]
- 60.Fazila-Tun-Nesa Malik MI, et al. Clinical presentation, management and in-hospital outcome of healthcare personnel with COVID-19 disease. Cureus. 2020 doi: 10.7759/cureus.10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alam MT, et al. A case series of 100 COVID-19 positive patients treated with combination of ivermectin and doxycycline. J Bangladesh Coll Phys Surg. 2020;12:10–15. [Google Scholar]
- 62.Chowdhury ATMM, et al. A Comparative study on ivermectin-doxycycline and hydroxychloroquine-azithromycin therapy on COVID-19 patients. EJMO. 2021 doi: 10.14744/ejmo.2021.16263. [DOI] [Google Scholar]
- 63.Shouman W. Use of ivermectin as a prophylactic option in asymptomatic family close contact for patient with COVID-19. Clinical trial registration NCT04422561. Aug. 2020. https://clinicaltrials.gov/ct2/show/NCT04422561. Accessed 26 Jan 2021.
- 64.Héctor C, et al. Study of the efficacy and safety of topical ivermectin+ iota-carrageenan in the prophylaxis against COVID-19 in health personnel. J Biomed Res Clin Investig. 2020 doi: 10.31546/2633-8653.1007. [DOI] [Google Scholar]
- 65.Behera P, et al. Role of ivermectin in the prevention of COVID-19 infection among healthcare workers in India: a matched case-control study. medRxiv. 2020 doi: 10.1101/2020.10.29.20222661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hellwig MD, Maia A. A COVID-19 prophylaxis? Lower incidence associated with prophylactic administration of ivermectin. Int J Antimicrob Agents. 2021;57(1):106248. doi: 10.1016/j.ijantimicag.2020.106248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Merck Sharp & Dohme BV. Tablets Stromectol®(Ivermectin). 2018. https://www.merck.com/product/usa/pi_circulars/s/stromectol/stromectol_pi.pdf. Accessed 2021.
- 68.Adenusi A, Oke A, Adenusi A. Comparison of ivermectin and thiabendazole in the treatment of uncomplicated human Strongyloides stercoralis infection. Afr J Biotech. 2003;2(11):465–469. [Google Scholar]
- 69.Muñoz J, et al. Safety and pharmacokinetic profile of fixed-dose ivermectin with an innovative 18mg tablet in healthy adult volunteers. PLoS Negl Trop Dis. 2018;12(1):e0006020. doi: 10.1371/journal.pntd.0006020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kamgno J, et al. Adverse systemic reactions to treatment of onchocerciasis with ivermectin at normal and high doses given annually or three-monthly. Trans R Soc Trop Med Hyg. 2004;98(8):496–504. doi: 10.1016/j.trstmh.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 71.Raffi J, Suresh R, Butler DC. Review of scabies in the elderly. Dermato The. 2019;9(4):623–630. doi: 10.1007/s13555-019-00325-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Avirutnan P. A phase II/III, Randomized, placebo controlled trial of efficacy and safety of ivermectin in children and adult patients with dengue infection. clinicaltrials.gov, Clinical trial registration NCT02045069. Oct 2015. Accessed 18 Jan 2021. https://clinicaltrials.gov/ct2/show/NCT02045069.
- 73.Abreu JL. Ivermectin and orthomolecular medicine combination therapy for COVID-19: successful clinical protocols and a case study. Daena Int J Good Consci. 2020;15(2):1–18. [Google Scholar]
- 74.Centers for Disease Control and Prevention. CDC—scabies—resources for health professionals—medications. 02 Oct 2019. https://www.cdc.gov/parasites/scabies/health_professionals/meds.html. Accessed 23 Jan 2021.
- 75.Chandler RE. Serious neurological adverse events after ivermectin—do they occur beyond the indication of onchocerciasis? Am J Trop Med Hyg. 2018;98(2):382. doi: 10.4269/ajtmh.17-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Boussinesq M, et al. Clinical picture, epidemiology and outcome of Loa-associated serious adverse events related to mass ivermectin treatment of onchocerciasis in Cameroon. Filaria J. 2003;2(1):1–13. doi: 10.1186/1475-2883-2-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Twum-Danso NA. Serious adverse events following treatment with ivermectin for onchocerciasis control: a review of reported cases. Filaria J. 2003;2(1):1–10. doi: 10.1186/1475-2883-2-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Database of Adverse Event Notifications (DAEN), Therapeutic Goods Administration (TGA). 30 Oct 2018. https://www.tga.gov.au/databaseadverse-event-notifications-daen. Accessed 25 Feb 2021.
- 79.van Westerloo DJ, et al. Persistent coma in Strongyloides hyperinfection syndrome associated with persistently increased ivermectin levels. Clin Infect Dis. 2014;58(1):143–144. doi: 10.1093/cid/cit656. [DOI] [PubMed] [Google Scholar]
- 80.Sparsa A, et al. Systemic adverse reactions with ivermectin treatment of scabies. Ann Dermatol Venereol. 2006 doi: 10.1016/s0151-9638(06)71044-4. [DOI] [PubMed] [Google Scholar]
- 81.Choudhary R, Sharma AK. Potential use of hydroxychloroquine, ivermectin and azithromycin drugs in fighting COVID-19: trends, scope and relevance. New Microbes New Infect. 2020 doi: 10.1016/j.nmni.2020.100684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gasmi A, et al. Chloroquine and hydroxychloroquine in the treatment of COVID-19: the never-ending story. Appl Microbiol Biotechnol. 2021 doi: 10.1007/s00253-021-11094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Group. R.C. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chaccour C, et al. Ivermectin and COVID-19: keeping rigor in times of urgency. Am J Trop Med Hyg. 2020;102(6):1156. doi: 10.4269/ajtmh.20-0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brunton LL, Hilal-Dandan R, Knollmann BC. “Chemotherapy of Helminth Infections” in Goodman & Gilman’s the pharmacological basis of therapeutics. 12. New York: McGraw-Hill Education; 2015. [Google Scholar]
- 86.Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1–12. doi: 10.1016/j.bbi.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 87.Skálová L, et al. Effect of ivermectin on activities of cytochrome P450 isoenzymes in mouflon (Ovis musimon) and fallow deer (Dama dama) Chem Biol Interact. 2001;137(2):155–167. doi: 10.1016/s0009-2797(01)00227-7. [DOI] [PubMed] [Google Scholar]
- 88.Benet L, Cummins C, Wu C. Unmasking the dynamic interplay between efflux transporters and metabolic enzymes. Int J Pharm. 2004;277(1–2):3–9. doi: 10.1016/j.ijpharm.2002.12.002. [DOI] [PubMed] [Google Scholar]
- 89.Kigen G, Edwards G. Drug-transporter mediated interactions between anthelminthic and antiretroviral drugs across the Caco-2 cell monolayers. BMC Pharmacol Toxicol. 2017;18(1):1–13. doi: 10.1186/s40360-017-0129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lespine A, et al. Influence of the route of administration on efficacy and tissue distribution of ivermectin in goat. Vet Parasitol. 2005;128(3–4):251–260. doi: 10.1016/j.vetpar.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 91.Schmith VD, Zhou J, Lohmer LR. The approved dose of ivermectin alone is not the ideal dose for the treatment of COVID-19. Clin Pharmacol Ther. 2020;108(4):762–765. doi: 10.1002/cpt.1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Momekov G, Momekova D. Ivermectin as a potential COVID-19 treatment from the pharmacokinetic point of view: antiviral levels are not likely attainable with known dosing regimens. Biotechnol Biotechnol Equip. 2020;34(1):469–474. [Google Scholar]
- 93.Northwestern Medicine, “Colchicine Drug Interactions”. 2020. https://asp.nm.org/uploads/9/0/7/8/90789983/colchicine_drug_interactions_-_pharmacists_letter_2020.pdf#:~:text=Colchicine%20is%20a%20very%20old%20drug%20that%20has,out%20of%20ten%20patients%20who%20take%20colchicine%20to. Accessed 2021.
- 94.Pastick K, et al. Review: hydroxychloroquine and chloroquine for treatment of SARS-CoV-2 (COVID-19) Open Forum Infect Dis. 2020 doi: 10.1093/ofid/ofaa130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Smit MR, et al. Safety and mosquitocidal efficacy of high-dose ivermectin when co-administered with dihydroartemisinin-piperaquine in Kenyan adults with uncomplicated malaria (IVERMAL): a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2018;18(6):615–626. doi: 10.1016/S1473-3099(18)30163-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.