Abstract
Ramadan fasting is observed by most of the 1.8 billion Muslims around the world. It lasts for 1 month per the lunar calendar year and is the abstention from any food and drink from dawn to sunset. While recommendations on ‘safe’ fasting exist for patients with some chronic conditions, such as diabetes mellitus, guidance for patients with cardiovascular disease is lacking. We reviewed the literature to help healthcare professionals educate, discuss and manage patients with cardiovascular conditions, who are considering fasting. Studies on the safety of Ramadan fasting in patients with cardiac disease are sparse, observational, of small sample size and have short follow-up. Using expert consensus and a recognised framework, we risk stratified patients into ‘low or moderate risk’, for example, stable angina or non-severe heart failure; ‘high risk’, for example, poorly controlled arrhythmias or recent myocardial infarction; and ‘very high risk’, for example, advanced heart failure. The ‘low-moderate risk’ group may fast, provided their medications and clinical conditions allow. The ‘high’ or ‘very high risk’ groups should not fast and may consider safe alternatives such as non-consecutive fasts or fasting shorter days, for example, during winter. All patients who are fasting should be educated before Ramadan on their risk and management (including the risk of dehydration, fluid overload and terminating the fast if they become unwell) and reviewed after Ramadan to reassess their risk status and condition. Further studies to clarify the benefits and risks of fasting on the cardiovascular system in patients with different cardiovascular conditions should help refine these recommendations.
Keywords: heart failure, coronary artery disease, hypertension, global health, education, medical
Introduction
There are approximately 1.8 billion Muslims in the world and 3.4 million Muslims in the UK, 93% of whom are likely to observe Ramadan fasting.1 With a significantly high and increasing prevalence of cardiovascular disease in Muslim communities, including the UK,2 healthcare professionals (HCPs) are likely to come across requests from patients asking for their suitability for Ramadan fasting.
Adult Muslims are obligated to fast during the month of Ramadan if it is safe to do so (see table 1 for fasting in major religions).3 Ramadan fasting is the abstinence of all food and drink from dawn until sunset. Taking medicines orally or intranasally is considered breaking one’s fast.4 5 Outside of the pre-dawn to sunset window, Muslims can eat, drink and take medications as normal. In a typical fast, Muslims have a pre-dawn meal (termed ‘suhoor’) and a meal at sunset to break their fast (termed ‘iftaar’). An Islamic lunar month can be 29 or 30 days and falls 11 days earlier each year compared with the Gregorian solar calendar.1 In temperate regions, when Ramadan falls in the winter, fasts are shorter. Conversely, summer fasts in some countries can be as long as 20 hours per day.3
Table 1.
Summary of the different fasting practices in major world religions* (reproduced based on10, with permission)
| Religion | Form of fasting |
| Islam | It is obligatory for Muslims to fast the month of Ramadan (30–31 days) which consists of no food or drink from dawn to sunset. Muslims also commonly fast the first 10 days of the Islamic lunar month Dhul-Hijjah and some Muslims commonly fast the Monday and Thursday of each week and/or the middle 3 days of each fast.49 |
| Christianity | Catholic Christians abstain from eating meat, but not fish, on Fridays in the 6-week period before Easter, called Lent. Many Catholics also only eat one full meal a day on the days of Ash Wednesday, the first day of Lent, and Good Friday.49
Some Protestants observe Lent by abstaining from certain favourite foods or habits such as smoking. A similar method of fasting is the ‘Daniel fast’ which lasts 21 days.49 The Eastern Orthodox church has different fasting periods exist including Lent as well as the Nativity fast, Apostles’ Fast and Dormition Fast. These are often several weeks long and entail fasting from specific food items such as red meat and poultry and sometimes fish, oil and wine. None of the major denominations in Christianity prohibit taking medications while fasting.49 |
| Judaism | There are several days of fasting in Judaism. These include Yom Kippur, Tisha B’Av, the Fast of Gedalia, the Tenth of Tevet, the Seventeenth of Tammuz and the Fast of Esther. These are single days of fasting from all forms of eating and drinking during this period—with the exception of Yom Kippur and Tisha B’Av where Jews abstained from all oral intake (including water) for 24 hours (from sunset to sunset). Historically, reform Jews only observed the Yom Kippur fast while Orthodox Jews the above-mentioned fasts. According to Jewish Law, important and/or regular medications can be taken with drink, and if necessary, with food as well but a patient’s medications should be reviewed by a healthcare professional to ensure the fast as compliant as possible.49 |
| Hinduism | Fasting takes many forms from abstaining from meat to only drinking water and milk. The most common fast in Hinduism is Ekadasi, which takes place twice a month and often consists of eating only fruits, vegetables and milk products (although a small minority abstain from all eating and drinking for 24 hours). Many Hindus also fast during the month of Shravan. Hindus are permitted to take medications while fasting.49 |
| Buddhism | Lay Buddhists fast by abstaining from meat and certain types of food such as processed foods, two or more times per month. Some Buddhists stop eating after midday every day and some monks go further by abstaining from food for 18 days, drinking only a small portion of water (Lee et al 2009). |
| Sikhism | Sikhism does not promote fasting except for medical reasons.49 |
| Baha’i | Fasting is observed from sunrise to sunset during the Baha’I month of ‘Ala with the complete abstention of food and drink. Patients are permitted to take medications while fasting.49 |
*Religious practice is heterogeneous. While certain fasting practices are mentioned, patients may not practise them or may practise them in a manner dissimilar to that described above.
Exemptions to Ramadan fasting exist for individuals whose health may come to significant harm from it.3 6 Groups such as the frail elderly and those with significant mental and/or physical health illness are exempt from fasting.7 8 Muslims are permitted to break their fast if they become unwell and can make up their fast if and when they fully recover.3 If Muslims are in doubt about their obligation to fast with respect to their medical condition, they are encouraged to consult with their HCPs and their local Islamic scholar. Many individuals who have been advised not to fast by their HCP may still choose to do so.9
Due to the absence of randomised controlled trials, guidelines or expert statements on the management of patients with cardiovascular disease who wish to undertake Ramadan fasting, we undertook a narrative review of the existing literature to underpin guidance for HCPs managing patients with cardiovascular conditions desiring to fast in Ramadan. Our work builds on a limited survey of the literature with brief recommendations by the authors of this manuscript, on behalf of the British Islamic Medical Association.10
Patients with cardiovascular disease frequently have comorbidities such as diabetes mellitus (DM) and chronic kidney disease (CKD). These conditions can interact with cardiovascular disease, such as iatrogenic hypoglycaemia triggering arrhythmias in a patient with DM.11 Therefore, it is essential to take a holistic approach when advising patients with cardiac disease undertaking Ramadan fasting. Guidance on managing patients with DM, epilepsy, adrenal insufficiency and CKD has recently been published.3 9 10 12–15
Methods
We identified publications in PubMed and Embase using the following predefined terms in various combinations: “intermittent fasting”, “fasting”, “Ramadan”, “restricted feeding”, “cardiovascular disease”, “atrial fibrillation”, “hypertension”, “channelopathies”, “cardiomyopathy” and “valvular heart disease”. We included studies that examined ‘intermittent fasting’ to broaden our evidence base, although we appreciate that some forms of intermittent fasting differ from Ramadan fasting, particularly with regard to water fasting.
We used any relevant studies, our clinical experience of managing Muslim patients fasting in Ramadan and the well-established International Diabetes Federation and the Diabetes and Ramadan International Alliance (IDF-DAR) risk stratification model16 to form a consensus statement and provide risk stratification and management recommendations for safe fasting. Although the more recently published IDF-DAR Ramadan guidelines14 introduce a scoring system, this has not been validated and is based on physician opinion derived from an online survey with a limited evidence base. As this is a very new introduction, even from a diabetes perspective, it is not known if it is better than the previous risk stratification.17 We therefore relied on their well-established risk stratification model, but as more evidence emerges in this area, a scoring system could be considered. Table 2 can therefore be used by HCPs to risk stratify patients with cardiovascular disease desiring to fast in Ramadan and provide appropriate advice.
Table 2.
Risk stratification for fasting in patients with cardiovascular conditions based on the IDF-DAR risk categories (reproduced based on10, with permission)
| Risk level | Moderate/low risk | High risk | Very high risk |
| Advice | May be able to fast - listen to medical advice | Should not fast | Must not fast |
|
|
|
|
| Patients with inherited cardiomyopathy, adult congenital heart disease, left ventricular assist device or heart transplantation should discuss fasting in Ramadan in their next routine appointment | |||
*Episodes of angina are not occurring at rest or increasing significantly in frequency or severity.
†A difficult concept to define but the ESC guidelines define stability as no or mild heart failure symptoms and signs that have not changed recently for at least 1 month according to Ponikowski et al (2016).
‡Diagnosed by a combination of symptoms, LVEF ≥45%–50%, Heart Failure Association score, natriuretic peptide levels±imaging (refer for specialist confirmation, if needed).
§Pulmonary artery systolic pressure >25 mm Hg without severe echocardiographic or right heart catheterisation features.
¶With significant left ventricular outflow tract obstruction (>50 mm Hg).
**On optimal medical therapy, LVEF ≤35%, with class III–IV NYHA symptoms, ≥1 hospitalisation in the last 6 months due to decompensated heart failure and severely impaired functional capacity (eg, 6 min walk distance <300 m).
††Defined as WHO/NYHA III–IV classification, right ventricular dysfunction and objective markers on right heart catheterisation, for example, SvO2 <60%.
ESC, European Society of Cardiology; HFpEF, heart failure with preserved ejection fraction; IDF-DAR, International Diabetes Federation and the Diabetes and Ramadan International Alliance; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
What therapies and factors need to be taken into consideration in patients with cardiovascular conditions
Fasting-associated dehydration may lead to electrolyte abnormalities which could be life-threatening in patients with unstable arrhythmias, inherited arrhythmia syndromes (eg, long QT or Brugada syndrome), or on medications such as class Ic antiarrhythmics, digoxin and renin–angiotensin–aldosterone antagonists.18 Many cardiac medications can induce hypotension, potentially precipitating syncope, particularly in elderly patients with impaired baroreflexes.19 20 This may be exacerbated by dehydration or a shortened interval between a bedtime and breakfast dose if medication dosing is altered by patients trying to facilitate fasting.
Aslam and Healy21 found 42% of the 81 Southeast Asian Muslim patients they surveyed were adherent to their usual treatment schedule in Ramadan, possibly because of a disruption in their routine as a result of fasting. In patients taking antiplatelets for coronary stent implantation or anticoagulation for stroke prevention in atrial fibrillation, medication non-compliance may be fatal.
Summary of the key studies examining fasting and cardiovascular disease
Hypertension
In a prospective observational study by Aslan et al 22 assessing the safety of diuretic therapy in patients with hypertension, Ramadan fasting appeared to significantly decrease systolic and diastolic blood pressures in individuals using diuretics, which was well tolerated without complication. Eldeeb et al 23 noted improved blood pressure control in patients with hypertension, irrespective of renal function, and improved arterial compliance in those without CKD, in patients undertaking Ramadan fasting.
Chronic coronary syndrome
In an observational study of patients with chronic coronary syndrome (CCS), as defined by the European Society of Cardiology (ESC),24 Khafaji et al 25 reported that Ramadan fasting was not associated with an increased cardiac mortality or morbidity, with 29% of patients reporting improved cardiac symptoms. Similar findings were seen by Mousavi et al 26 in patients with CCS and a normal left ventricular function.
Acute coronary syndrome
Temizhan et al 27 compared the incidence of acute coronary syndrome (ACS), as defined by the ESC, in 1655 patients at a single centre, in the month before, during and after Ramadan, over a 6-year period. They noted no significant differences in the incidence of ACS in Ramadan when compared with the preceding or following month. A multicentre study by Amin and Alaarag28 demonstrated that patients who undertook Ramadan fasting within 3 months of percutaneous coronary intervention had a higher incidence of significant cardiac events than those who did not undertake Ramadan fasting.
Heart failure
Abazid et al,29 in an observational study, demonstrated that 92% of patients with heart failure with a reduced ejection fraction (HFrEF) (left ventricular ejection fraction (LVEF) ≤40%) with ‘close monitoring’ did not experience worsening HF symptoms. Patients with a non-ischaemic cardiomyopathy and/or a history of non-compliance with fluid restrictions and/or medications were more likely to experience worsening HF symptoms. A retrospective review of more than 2000 patients hospitalised with HFrEF over a 10-year period found no increase in the number of HF hospitalisations in Ramadan when compared with other months in the year.30
An expert panel examined the safety of sodium–glucose cotransporter 2 inhibitors (SGLT2i) in patients observing Ramadan fasting and agreed on the following: SGLT2i should be initiated at low dose, in the evening and at least 1 month before Ramadan; fluid intake should be increased during non-fasting hours; hypoglycaemia should be avoided by reviewing any concomitant medications for type 2 DM and SGTL2i should be avoided in the elderly, patients with CKD or those receiving loop diuretics.31
Arrhythmias
Disrupted cellular metabolism and ion channel function can result in cardiac arrhythmias.32 Kahraman and Dogan33 report a asymptomatic high burden of premature ventricular complexes in a patient undertaking Ramadan fasting, with recurrences only in subsequent attempts at Ramadan fasting, on further monitoring. The ESC 2020 sports cardiology advises that patients with long QT syndrome should carefully avoid dehydration.34 American Heart Association guidelines state that sleep cycle and eating disturbances, common in Ramadan fasting, could lead to an increased incidence of atrial fibrillation.35 A multicentre cross-sectional study by Batarfi et al 36 surveyed a cohort of 809 patients undertaking Ramadan fasting and receiving oral anticoagulation: 68.4% of patients received warfarin, the remaining received direct oral anticoagulants (DOACs); of these 50% modified their anticoagulation regimen (intake time, skipped doses, drugs being taken at the same time two times per day) without prior consultation with their physician. Patients receiving two times per day DOACs were noted to be more likely to change their anticoagulation administration and more likely to be admitted to hospital with a consequence of their changes, for example, bleeding or stroke.
Other cardiovascular conditions
The 2014 ESC and 2020 American College of Cardiology guidelines for hypertrophic obstructive cardiomyopathy (HOCM) recommend that patients should remain well hydrated to reduce the occurrence of potentially life-threatening symptoms such as syncope.37 38 Likewise, the 2020 ESC guidelines for patients with adult congenital heart disease (ACHD) also recommend avoiding dehydration in patients with ACHD, particularly cyanotic ACHD.39 Dehydration is also noted as a risk factor for the recurrence of orthostatic intolerance syndromes, including neurogenic and non-neurogenic orthostatic hypotension and postural orthostatic tachycardia syndrome.40
Summary of the evidence
The available studies state that with ‘close monitoring’, fasting may be safely undertaken in patients with CCS or HFrEF. There are very few if no published data on Ramadan fasting in other forms of cardiovascular disease, including cardiomyopathies, arrhythmias or valvular heart disease. The published data on Ramadan fasting are weak, are observational, lack a large sample size with sufficient power, have prolonged follow-up beyond the month of Ramadan, do not clearly define what ‘close monitoring’ means or have detailed information about the diet of the patients outside of their fast (see our online supplemental index for a summary of the studies highlighted in our review). This point is echoed by Santos and Macedo41 in their narrative review of the published data on intermittent fasting on lipid profile.
heartjnl-2021-319273supp001.pdf (89.7KB, pdf)
General recommendations based on the available evidence
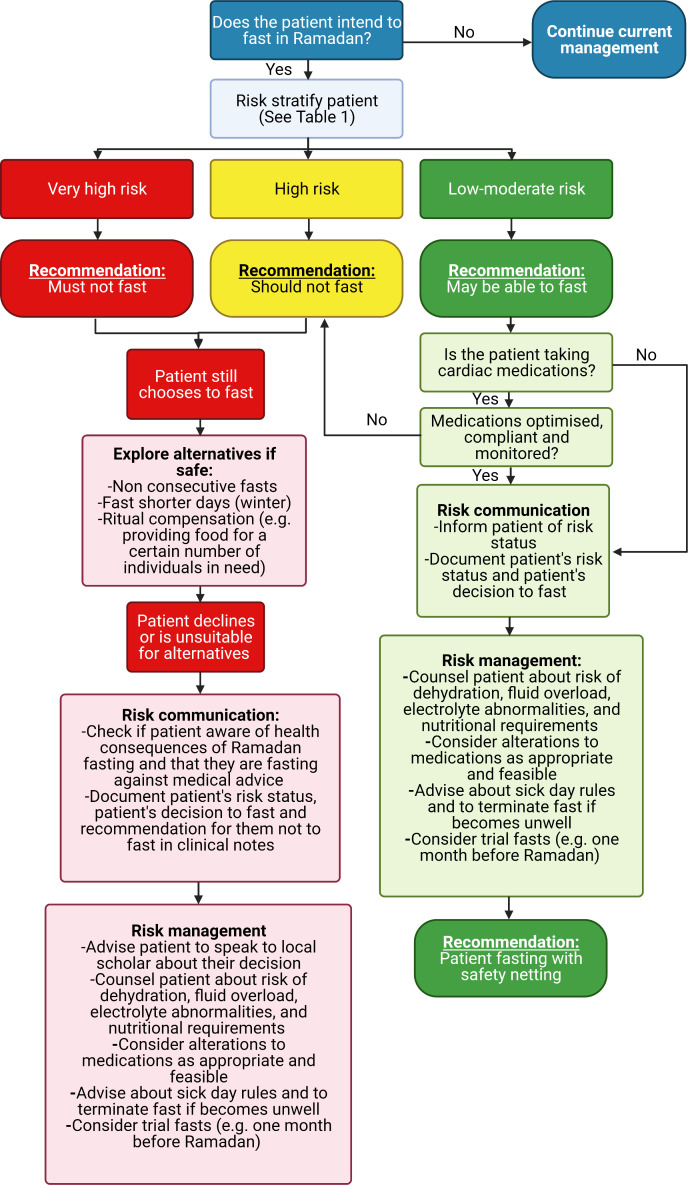
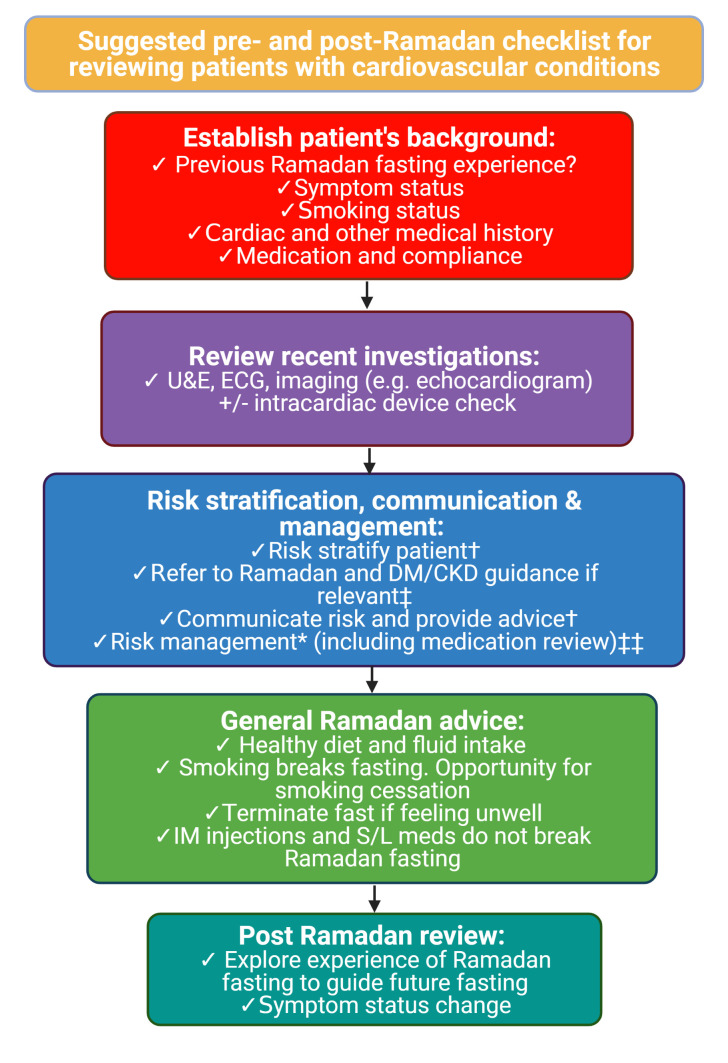
Patients with cardiac conditions desiring to fast in Ramadan should be assessed on an individual basis, by their HCP, during a routine consultation before Ramadan. In table 2, we risk stratify patients according to their cardiac conditions, although some patients deemed ‘low-moderate’ risk for fasting may be at higher risk in view of specific features of their conditions or their comorbidities. In figure 1, we provide a proposed pathway for HCPs managing a fasting patient with cardiac disease. At present, we are not able to provide guidance on the combination of low-moderate risk conditions, whether these are purely cardiovascular or combined with non-cardiac conditions as is frequently the case. Figure 2 provides a suggested consultation checklist for HCPs managing patients with cardiovascular disease desiring to fast in Ramadan.
Figure 1.
Proposed risk stratification and decision pathway for managing the fasting patient with cardiac disease (created with biorender.com).
Figure 2.
Suggested pre-Ramadan and post-Ramadan checklist for reviewing patients with cardiovascular conditions. CKD, chronic kidney disease; DM, diabetes mellitus; IM, intramuscular; S/L, sublingual; U&E, urea and electrolytes. †See figure 1. ‡Reference 3 9 11–14. ‡‡See table 3 (created with biorender.com).
Table 3 summarises the risks associated with different classes of cardiac medications and their use while fasting in Ramadan. In a review in the Canadian Pharmacists Journal, Grindrod and Alsabbagh4 suggested that if medication adjustments are made to facilitate fasting, strategies could include choosing once-daily medications or long-acting formulations where safe and appropriate to do so and without compromising the treatment offered. When initiating new medication in patients who may wish to fast, once a day dosing of medication should be considered, particularly where safety and efficacy is equivalent to medication with more frequent daily dosing. For patients on established therapies, we would suggest avoiding medication changes where possible.
Table 3.
Summary of the potential risks that could occur with different classes of cardiac medication used while fasting (reproduced based on10, with permission)
| Drug | Condition used in | Risk in fasting |
| ACE inhibitor (eg, ramipril) Aldosterone receptor blockers (eg, candesartan) Angiotensin receptor neprilysin inhibitor (ie, sacubitril/valsartan) |
Hypertension Heart failure |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness; may compound fasting-associated dehydration resulting in an acute kidney injury and/or life-threatening electrolyte abnormalities, for example, hyperkalaemia. Medication non-compliance may result in uncontrolled hypertension, decompensated heart failure. |
| Antiplatelet medications (eg, aspirin, clopidogrel, prasugrel, ticagrelor) |
Coronary artery disease/myocardial infarction | Medication non-compliance can increase risk of acute stent thrombosis, myocardial infarction and death if antiplatelets are not taken regularly—particularly in patients with recent coronary stent implantation (<6 months). Ticagrelor is taken two times per day and has a half-life of 7 hours (see above section on taking medications more than 12 hours apart and the effect it may have). |
| Antiarrhythmic drugs (AADs) (eg, amiodarone, flecainide, sotalol) | Atrial tachyarrhythmias Ventricular tachyarrhythmias |
Some may worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. Fasting-associated dehydration may result in significant electrolyte abnormalities that may increase risk of AAD toxicity. |
| Beta blockers (eg, bisoprolol) |
Coronary artery disease Heart failure Arrhythmias Hypertension |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. Medication non-compliance may result in worsening angina, decompensated heart failure, more frequent arrhythmias. |
| Calcium channel blockers (eg, amlodipine, diltiazem) |
Hypertension Arrhythmias Coronary artery disease |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. Medication non-compliance may result in worsening angina, more frequent arrhythmias, uncontrolled hypertension. |
| Cardiac glycosides (eg, digoxin) |
Arrhythmias Heart failure |
Digoxin toxicity may occur in potential case of fasting-related acute kidney injury. |
| Direct oral anticoagulants (DOACs) (eg, apixaban, rivaroxaban, edoxaban) | Atrial flutter/atrial fibrillation Deep venous thrombosis/pulmonary embolism |
Two times per day DOACs: The half-life of apixaban is 12 hours—if taken early morning, for example, 03:00 (suhoor) and then again at, for example, 20:00 (iftaar), there may be a period in between where the patient is not adequately anticoagulated. Medication non-compliance may result in stroke or death. |
| Immunosuppressant therapy (eg, tacrolimus) |
Heart transplant | May compound fasting-associated dehydration and result in an acute kidney injury and/or life-threatening electrolyte abnormalities, for example, hyperkalaemia. Medication non-compliance may result in organ rejection and death. Tacrolimus is taken two times per day and therefore care must be taken to avoid long periods in between. |
| Loop diuretics (eg, furosemide, bumetanide) Thiazide diuretics (eg, bendroflumethiazide) |
Hypertension Heart failure |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. May worsen fasting-associated dehydration resulting in an acute kidney injury and/or life-threatening electrolyte abnormalities, for example, hyperkalaemia. Medication non-compliance may result in uncontrolled hypertension, decompensated heart failure. |
| Mineralocorticoid receptor antagonists (eg, spironolactone) |
Hypertension Heart failure |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. May worsen fasting-associated dehydration resulting in an acute kidney injury and/or life-threatening electrolyte abnormalities, for example, hyperkalaemia. Medication non-compliance may result in uncontrolled hypertension, decompensated heart failure. |
| Phosphodiesterase type 5 inhibitors (eg, sildenafil) | Pulmonary hypertension | May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. May result in diarrhoea, worsening fasting-associated hypotension. |
| Prostanoids (eg, epoprostenol) | Idiopathic pulmonary arterial hypertension | May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. |
| Statins (eg, atorvastatin) |
Coronary artery disease/myocardial infarction | Fasting-associated dehydration may increase risk of acute kidney injury. This may compound a rare side effect of statins—rhabdomyolysis. |
| Sodium–glucose cotransporter 2 inhibitors (eg, dapaglifozin) |
Heart failure Diabetes mellitus |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. May worsen fasting-associated dehydration resulting in an acute kidney injury and/or life-threatening electrolyte abnormalities, for example, hyperkalaemia. Medication non-compliance may result in decompensated heart failure and cause/worsen hyperglycaemia in patients with diabetes mellitus. |
| Soluble guanylate cyclase inhibitors (eg, vericiguat) |
Heart failure | May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. |
| Vasodilators: Long-acting nitrates (eg, isosorbide mononitrate) Alpha blockers (eg, doxazocin, hydralazine) |
Hypertension Coronary artery disease Pulmonary hypertension |
May worsen fasting-associated hypotension, which may result in dizziness or loss of consciousness. |
Suhoor: pre-dawn meal before Muslims initiate fast; iftaar: meal at sunset that breaks fast.
Medication changes may not be possible due to (1) significantly reduced outpatient consultations with specialists and/or GPs due to COVID-19; (2) a specialist may deem alternate medications to be less beneficial for a patient. Medication changes should be planned well in advance of Ramadan and should be discussed in a patient’s next routine appointment with their specialist, GP and or pharmacist or if a patient is ever admitted to the hospital under the care of the cardiology team.
GP, general practitioner.
The following points should be considered when advising patients who wish to fast,10 although all recommendations should take into consideration the climate, country and season where the patient is fasting:
Hypertension
Blood pressure, kidney function and medications (particularly antihypertensives that have a diuretic component such as aldosterone antagonists or thiazide-like diuretics) should be reviewed by HCPs during a routine appointment to reduce the risk of hypotension and/or worsening kidney function. A home blood pressure monitor would be useful to observe a patient’s blood pressure response to antihypertensive treatment while fasting and provide clarity on any symptoms that could suggest a low blood pressure. Patients with well-controlled blood pressure, as defined by their HCP, would be deemed ‘low-moderate’ risk for fasting.
CCS and ACS
The few studies in patients with CCS, whom we deem as ‘low-moderate risk’, undertaking Ramadan fasting, indicate that it is safe for them to do so, provided patients are compliant with their medications. Patients within a 6-week period of an ACS, whom we deem to be at least high risk, or had cardiac surgery, are advised not to fast, particularly as they may not be able to undertake cardiac rehabilitation due to the risk of hypotension from fasting-associated dehydration.42
Heart failure
The few studies in patients with non-severe HFrEF, whom we would deem as ‘low-moderate’ risk undertaking Ramadan fasting suggest that is safe for them to do so, in line with guidance from the British Heart Foundation42 and the ESC.43 We deem patients with severe (LVEF ≤35%) HFrEF and advanced HF, as defined by the ESC,44 as high and very high risk for Ramadan fasting, respectively. There are no studies investigating patients with HF with preserved ejection fraction (HFpEF) undertaking Ramadan fasting. We propose that stable patients with HFpEF, as defined by the ESC,45 are ‘low-moderate’ risk; however, each patient should be reviewed as particulars about their condition and/or their comorbidities may increase the risk, especially since HFpEF is a heterogeneous group.
Intracardiac devices
There are no studies assessing patients with pacemakers undertaking Ramadan fasting. We deem them to be ‘low-moderate’ risk provided they have no electrolyte abnormalities and their device clinic feels their device parameters are stable. Patients with cardiac resynchronisation therapy or implantable cardioverter defibrillators would be deemed at least ‘high risk’ as they are only indicated in patients with severe HFrEF and/or patients at significant risk of ventricular arrhythmias. We advise patients with intracardiac devices to inform their device clinic in their next device check of their desire to fast in Ramadan. A remote or in-person device check just before Ramadan would be ideal to ensure there are no issues that may prevent a patient fasting.
Others
Published studies examining the risk of Ramadan fasting in patients with atrial fibrillation, inherited arrhythmic syndromes, valvular heart disease, pulmonary hypertension, heart transplantation or ACHD are lacking. Ramadan fasting in pregnant patients with cardiovascular conditions has been discussed elsewhere.10
In the absence of any studies assessing the above conditions in Ramadan fasting, we therefore advise that any disease where there may be a significant risk of dehydration or hypotension should be classed as at least ‘high risk’. This includes preload-dependent conditions such as severe aortic stenosis, HOCM with left ventricular outflow tract or mid-cavity obstruction at rest or with Valsalva manoeuvre (ie, peak gradient >50 mm Hg) as well as those with poorly controlled arrhythmias such as atrial fibrillation or at high risk of potentially fatal arrhythmias such as Brugada, long QT syndrome or arrhythmogenic cardiomyopathy.
Patients with severe pulmonary hypertension, as defined by the ESC (eg, New York Heart Association class III–IV breathlessness or right ventricular systolic impairment),46 would be considered very high risk for fasting, particularly those with presyncope and/or syncope.46
Patients with heart transplantation or ACHD should discuss Ramadan fasting with their specialist team during routine follow-up, although clearly patients with ACHD with cyanotic heart disease or features of other ‘high’ risk conditions such as severe valvular heart disease or poorly controlled arrhythmias would be classed as at least ‘high’ risk.
COVID-19-related cautions
If a patient is unwell with COVID-19, we advise against fasting. In a pandemic or in the post-pandemic phase, routine reviews by specialists or general practitioners, where patients could discuss their risk for Ramadan fasting, may not take place.
In these situations, we advise patients to adhere to professional advice or standard practice that they have received previously, provided there has not been a change in their clinical status that could increase their risk for fasting. Similarly, a bridge between taking an abstinence approach and not being able to access a clinician can be trial fasting in the weeks leading up to Ramadan.3 A patient’s previous experiences can also facilitate a clinician’s advice particularly if time is limited for a more thorough clinical assessment.3 It is worth noting however that many services, including blood test monitoring or community HF services, that may have facilitated fasting in Ramadan before, may not be available or available to a degree that allows patients to fast safely. Further discussion around fasting during COVID-19 is discussed elsewhere,47 48 but HCPs should bear these points in mind when risk stratifying their patient with cardiac disease for Ramadan fasting.
Conclusion
The literature on Ramadan fasting in patients with cardiovascular disease is limited. Our review highlights the important role HCPs play in risk assessment, providing advice and education, encouraging medication compliance and monitoring to enable patients, where safe to do so, to fulfil their religious obligation while minimising the potential for harm. As patients with cardiovascular disease often have non-cardiac comorbidities, our recommendations should be used in combination with those for Ramadan fasting in non-cardiac conditions such as CKD, DM and epilepsy. There is a strong need for patients, HCPs and religious/community leaders to engage with each other and discuss these contemporary medical issues. Further studies are needed to explore gaps in knowledge around fasting and to help refine current recommendations.
Acknowledgments
We would like to thank Professor John McMurray (Professor of Medical Cardiology, University of Glasgow), Dr Imran Zaman (General Practitioner, Broadway Health Centre, Birmingham), Shaykh Yunus Dhudwala (Imam and Head of Chaplaincy, Barts Health NHS Trust, London) and the British Islamic Medical Association (BIMA) for their review of the manuscript and valuable feedback.
Footnotes
Contributors: All the authors have been significantly involved in the conception and design of the narrative review, the acquisition and interpretation of data, drafting the work and revising it. Final approval of the version published has been given by all authors. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Ghani F. Most Muslims say they fast during Ramadan, 2013. Available: http://www.pewresearch.org/facttank/2013/07/09/global-median-of-93-of-muslims-say-they-fastduring-ramadan/ [Accessed 19 Jan 2020].
- 2. Jalal Z, Antoniou S, Taylor D, et al. South Asians living in the UK and adherence to coronary heart disease medication: a mixed- method study. Int J Clin Pharm 2019;41:122–30. 10.1007/s11096-018-0760-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ghouri N, Hussain S, Mohammed R. Diabetes, driving and fasting during Ramadan: the interplay between secular and religious law, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grindrod K, Alsabbagh W. Managing medications during Ramadan fasting. Can Pharm J 2017;150:146–9. 10.1177/1715163517700840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rasjid R. Part 1- what invalidates fasting related to the throat in light of modern medicine. al Balagh Academy publication papers, 2020. Available: https://www.academia.edu/43086999/PART_1_WHAT_INVALIDATES_FASTING_RELATED_TO_THE_THROAT_IN_LIGHT_OF_MODERN_MEDICINE_PART_1_WHAT_INVALIDATES_FASTING_RELATED_TO_THE_THROAT_IN_LIGHT_OF_MODERN_MEDICINE
- 6. Az-Zarqa MS. Sharh Al-Qawa‘id Al-Fiqhiyyah. 3rd edn. Damascus: Dar al-Qalam, 1993: 33–4. [Google Scholar]
- 7. Al-Shurunbulali A. Ascent to Felicity. 1st edn. London, UK: White Thread Press, 2010. [Google Scholar]
- 8. Hussain S, Hussain S, Mohammed R, et al. Fasting with adrenal insufficiency: practical guidance for healthcare professionals managing patients on steroids during Ramadan. Clin Endocrinol 2020;93:87–96. 10.1111/cen.14250 [DOI] [PubMed] [Google Scholar]
- 9. Babineaux SM, Toaima D, Boye KS, et al. Multi-country retrospective observational study of the management and outcomes of patients with type 2 diabetes during Ramadan in 2010 (CREED). Diabet Med 2015;32:819–28. 10.1111/dme.12685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. BIMA . British Islamic Medical association Ramadan rapid review, 2020. Available: https://britishima.org/wp-content/uploads/2020/05/Ramadan-Rapid-Review-Recommendations-v1.2.pdf [Accessed 9 Apr 2020].
- 11. International Hypoglycaemia Study Group . Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol 2019;7:e18:385–96. 10.1016/S2213-8587(18)30315-2 [DOI] [PubMed] [Google Scholar]
- 12. Mahmood A, Abbasi HN, Ghouri N, et al. Managing epilepsy in Ramadan: guidance for healthcare providers and patients. Epilepsy Behav 2020;111:107117–17. 10.1016/j.yebeh.2020.107117 [DOI] [PubMed] [Google Scholar]
- 13. Ahmed SH, Chowdhury TA, Hussain S, et al. Ramadan and diabetes: a narrative review and practice update. Diabetes Ther 2020;11:2477–520. 10.1007/s13300-020-00886-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. IDF-DAR . Diabetes and Ramadan: practical guidelines 2021, 2021. Available: https://www.daralliance.org/daralliance/idf-dar-practical-guidelines-2021/ [Accessed 23 Mar 2021].
- 15. Malik S, Bhanji A, Abuleiss H, et al. Effects of fasting on patients with chronic kidney disease during Ramadan and practical guidance for healthcare professionals. Clin Kidney J 2021;18:sfab032. 10.1093/ckj/sfab032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hassanein M, Al-Arouj M, Hamdy O, et al. Diabetes and Ramadan: practical guidelines. Diabetes Res Clin Pract 2017;126:303–16. 10.1016/j.diabres.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 17. Ghouri N, Hussain S, Ahmed SH, et al. Changing how we risk-categorise in Ramadan: does the IDF-DAR scoring system achieve the requirements for people with diabetes internationally? Diabetes Res Clin Pract 2021:108835. 10.1016/j.diabres.2021.108835 [DOI] [PubMed] [Google Scholar]
- 18. Bhatt D. Opie’s Cardiovascular Drugs: A Companion to Braunwald’s Heart Disease. 9th ed. Elsevier, 2021. [Google Scholar]
- 19. Ricci F, De Caterina R, Fedorowski A. Orthostatic hypotension: epidemiology, prognosis, and treatment. J Am Coll Cardiol 2015;66:848–60. 10.1016/j.jacc.2015.06.1084 [DOI] [PubMed] [Google Scholar]
- 20. Yasa E, Ricci F, Holm H, et al. Pacing therapy in the management of unexplained syncope: a tertiary care centre prospective study. Open Heart 2019;6:e001015. 10.1136/openhrt-2019-001015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Aslam M, Healy MA. Compliance and drug therapy in fasting Moslem patients. J Clin Hosp Pharm 1986;11:321–5. 10.1111/j.1365-2710.1986.tb00859.x [DOI] [PubMed] [Google Scholar]
- 22. Aslan S, Riza Demir A, Kahraman S, et al. The effect of Ramadan fasting on ambulatory blood pressure in treated hypertensive patients using diuretics. Blood Press Monit 2020;25:195–200. 10.1097/MBP.0000000000000451 [DOI] [PubMed] [Google Scholar]
- 23. Eldeeb AA, Mahmoud MA, Ibrahim AB, et al. Effect of Ramadan fasting on arterial stiffness parameters among Egyptian hypertensive patients with and without chronic kidney disease. Saudi J Kidney Dis Transpl 2020;31:582–8. 10.4103/1319-2442.289444 [DOI] [PubMed] [Google Scholar]
- 24. Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2020;29:ehaa575. 10.1093/eurheartj/ehaa575 [DOI] [PubMed] [Google Scholar]
- 25. Khafaji HARH, Bener A, Osman M, et al. The impact of diurnal fasting during Ramadan on the lipid profile, hs-CRP, and serum leptin in stable cardiac patients. Vasc Health Risk Manag 2012;8:7–14. 10.2147/VHRM.S22894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mousavi M, Mirkarimi SS, Rahmani G, et al. Ramadan fast in patients with coronary artery disease. Iran Red Crescent Med J 2014;16:e7887. 10.5812/ircmj.7887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Temizhan A, Dönderici O, Ouz D, et al. Is there any effect of Ramadan fasting on acute coronary heart disease events? Int J Cardiol 1999;70:pp149–53. 10.1016/s0167-5273(99)00082-0 [DOI] [PubMed] [Google Scholar]
- 28. Amin OA, Alaarag A. The safety of Ramadan fasting following percutaneous coronary intervention. BMC Cardiovasc Disord 2020;20:489. 10.1186/s12872-020-01784-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Abazid RM, Khalaf HH, Sakr HI, et al. Effects of Ramadan fasting on the symptoms of chronic heart failure. Saudi Med J 2018;39:p395–400. 10.15537/smj.2018.4.22011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Al Suwaidi J, Bener A, Hajar HA, et al. Does hospitalization for congestive heart failure occur more frequently in Ramadan: a population-based study (1991–2001). Int J Cardiol 2004;96:217–21. 10.1016/j.ijcard.2003.06.018 [DOI] [PubMed] [Google Scholar]
- 31. Hassanein M, Bashier A, Randeree H, et al. Use of SGLT2 inhibitors during Ramadan: an expert panel statement. Diabetes Res Clin Pract 2020;169:108465. 10.1016/j.diabres.2020.108465 [DOI] [PubMed] [Google Scholar]
- 32. Jeong E-M, Liu M, Sturdy M, et al. Metabolic stress, reactive oxygen species, and arrhythmia. J Mol Cell Cardiol 2012;52:454–63. 10.1016/j.yjmcc.2011.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kahraman S, Dogan A. Ventricular arrhythmia linked to long intermittent fasting. J Electrocardiol 2020;58:125–7. 10.1016/j.jelectrocard.2019.10.008 [DOI] [PubMed] [Google Scholar]
- 34. Pelliccia A, Sharma S, et al. , ESC Scientific Document Group, . 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease: the task force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of cardiology (ESC). Eur Heart J;42:17–96. 10.1093/eurheartj/ehaa605 [DOI] [PubMed] [Google Scholar]
- 35. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American heart association Task force on clinical practice guidelines and the heart rhythm society in collaboration with the Society of thoracic surgeons. Circulation 2019;140:e125–51. 10.1161/CIR.0000000000000665 [DOI] [PubMed] [Google Scholar]
- 36. Batarfi A, Alenezi H, Alshehri A, et al. Patient-guided modifications of oral anticoagulant drug intake during Ramadan fasting: a multicenter cross-sectional study. J Thromb Thrombolysis 2021;51:485–93. 10.1007/s11239-020-02218-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Elliott PM, Anastasakis A, Borger MA. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of cardiology (ESC). Eur Heart J 2014;35:2733–79. 10.1093/eurheartj/ehu284 [DOI] [PubMed] [Google Scholar]
- 38. Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: Executive summary: a report of the American College of Cardiology/American heart association joint Committee on clinical practice guidelines. Circulation 2020;142:e533–57. 10.1161/CIR.0000000000000938 [DOI] [PubMed] [Google Scholar]
- 39. Baumgartner H, De Backer J, Babu-Narayan SV, et al. 2020 ESC guidelines for the management of adult congenital heart disease. Eur Heart J 2021;42:563–645. 10.1093/eurheartj/ehaa554 [DOI] [PubMed] [Google Scholar]
- 40. Raj SR. Postural tachycardia syndrome (POTS). Circulation 2013;127:2336–42. 10.1161/CIRCULATIONAHA.112.144501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Santos HO, Macedo RCO. Impact of intermittent fasting on the lipid profile: assessment associated with diet and weight loss. Clin Nutr ESPEN 2018;24:14–21. 10.1016/j.clnesp.2018.01.002 [DOI] [PubMed] [Google Scholar]
- 42. British Heart Foundation . Can I fast during Ramadan? 2020. Available: https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/fasting-during-ramadan
- 43. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of cardiology (ESC). developed with the special contribution of the heart failure association (HFA) of the ESC. Eur J Heart Fail 2016;18:891–975. 10.1002/ejhf.592 [DOI] [PubMed] [Google Scholar]
- 44. AbouEzzeddine OF, Redfield MM. Who has advanced heart failure? definition and epidemiology. Congest Heart Fail 2011;17:160–8. 10.1111/j.1751-7133.2011.00246.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pieske B, Tschöpe C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the heart failure association (HFA) of the European Society of cardiology (ESC). Eur Heart J 2019;40:3297–317. 10.1093/eurheartj/ehz641 [DOI] [PubMed] [Google Scholar]
- 46. Rosenkranz S. Pulmonary hypertension: current diagnosis and treatment. Clinical Research in Cardiology 2007;96:527–41. 10.1007/s00392-007-0526-8 [DOI] [PubMed] [Google Scholar]
- 47. Waqar S, Ghouri N. Managing Ramadan queries in COVID-19. BJGP Open 2020;4. 10.3399/bjgpopen20X101097. [Epub ahead of print: 23 Jun 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kalin A, Mahmood A, Waqar S, et al. Is it safe for patients with COVID-19 to fast in Ramadan? the centre of evidence-based medicine (CEBM)., 2020. Available: https://www.cebm.net/covid-19/is-it-safe-for-patients-with-covid-19-to-fast-in-ramadan/ [Accessed 22 April 2020].
- 49. Morroco World News . How do the Religions of the world practice fasting? 2018. Available: https://www.moroccoworldnews.com/2018/06/247837/religions-world-practice-fasting/ [Accessed 4 Feb 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
heartjnl-2021-319273supp001.pdf (89.7KB, pdf)