Abstract
Objectives
The COVID-19 pandemic has impacted regular cardiovascular healthcare access and delivery. Service utilisation has declined, and excess cardiovascular mortality has been reported in several countries. We aim to estimate excess cardiovascular deaths in Chile during 2020.
Methods
We collected mortality data from the Chilean Department of Statistics and Health Information and refined them using the maps of Global Burden of Disease Studies in 2017 and 2010. We conducted a time series analysis using quasi-Poisson distribution to predict cardiovascular mortality in 2020 and compared it with observed numbers and calculated attributable fractions (AFs) with 95% uncertainty intervals, as a whole and by sex, age group and type of cardiovascular disease.
Results
During 2015–2020, 173 283 cardiovascular deaths were recorded, with 28 141 deaths in 2020. The observation in 2020 was lower than our projection in the overall data (−4.0% (−5.0% to −2.8%)) and in male (−11.7% (−13% to −10.3%)). However, positive AFs were noted among female (5.0% (3.2% to 6.8%)), people in age group 80–89 years (11.0% (8.6% to 13.5%)) and people who died from hypertensive heart diseases (18.9% (14.7% to 23.5%)).
Conclusions
Less overall cardiovascular deaths were observed in 2020 compared with our projection, possibly associated with competing risks from COVID-19 infection in men. Nonetheless, excess cardiovascular deaths were observed among women, people in the age group 80–89 years and people who died from hypertensive heart diseases suggesting possible negative cardiovascular impacts brought by the pandemic on these vulnerable groups.
Keywords: epidemiology, global burden of disease, COVID-19, global health, delivery of healthcare
Introduction
The COVID-19 pandemic has disrupted the usual healthcare delivery worldwide after its first outbreak in 2020.1 To minimise the possibility of transmission between people, a lockdown policy has been implemented in many cities with strict mobility restrictions. Additionally, the protocols of healthcare delivery were modified to meet the need of treating patients with COVID-19.2 Such measures have resulted in changes in cardiovascular epidemiology as observational reports from numerous countries have revealed lower numbers of admissions of acute cardiac events.3 4 Explanation to such a phenomenon varies. Some suggested that mentality among patients leads to avoidance towards medical assistance even when experiencing discomforts,5 while others attributed it to the overwhelmed medical personnel’s ignorance towards patients without COVID-19.6
Unlike most advanced economies, Chile is still in the process of renovating its health system to better fit its transitioning population, in which cardiovascular diseases show the highest increase recently.7 Containment interventions were implemented to slow the spread of COVID-19 since March 2020, including specific mobility restrictions for the elderly between April and June, night-time curfew, 90 days’ nationwide mandatory lockdown and the later implementation of the ‘Plan Paso a Paso’ (‘Step-by-step System’) in July 2020. The system, composed of four transition steps, is evaluated regularly and implemented locally at the county level. The most restrictive steps included restrictions of mobility and the ban of indoor and outdoor gatherings. Consequently, the COVID-19 health crisis has disrupted the usual healthcare service in Chile, with weekly utilisation of emergency services for cardiovascular diseases by senior citizens dropping 42% in the next week after the first mandatory lockdown in March 2020.8
Yet, to date, studies on the impact of the pandemic on the mortality of cardiovascular diseases have been limited, not only in Chile but around the world. In this research, we aim to calculate the excess of death from cardiovascular diseases in Chile during the COVID-19 pandemic in 2020, with emphasis on differences by sex, age and type of cardiovascular disease.
Methods
To study the excess number of cardiovascular deaths attributable to COVID-19, we predicted the monthly mortality for 2020, using a time series analysis on data from 2015 to 2019, and compared them with observed numbers.
Death records
Death records, including all cases between 2015 and 2020, were obtained from the Department of Statistics and Health Information, Chilean Ministry of Health. This database, open to the public, is the most up-to-date and comprehensive national database in Chile with a relevant level of accuracy and reliability. Data contained anonymous information with gender, age, date of death, place of death and cause of death, recorded in the International Classification of Diseases, 10th Revision (ICD-10). Data were stratified by sex, age group (40–59, 60–69, 70–79, 80–89 and 90+ years), and specific cardiovascular disease: ischaemic heart diseases (I20–I25.9), strokes (G45–G46.8, I60–I63.9, I64X, I65–I66.9, I67.0–I67.3, I67.5–I67.6, I67.8–167.9, I68.1–I68.2, I69.0–I69.4, I69.8), hypertensive heart diseases (I11–I11.9), miscellaneous (I34–I37.8, B33.2, I40–I41.9, I42.1–I42.8, I43–I43.9, I51.4, I48–I48.9, I71–I71.9, I70.2–I70.8, I73–I73.9, I33–I33.9 and I38–I39.9, including rheumatic heart diseases, non-rheumatic valvopathies, myocarditis, endocarditis, cardiomyopathies, aortic aneurysm and peripheral artery diseases), and other cardiovascular diseases (I01–I01.9, I02.0, I05–I09.9, I28–I28.8, I30–I31.1, I31.8–I32.8, I47–I47.9, I51.0–I51.3, I68.0, I72–I72.9, I77–I83.9, I86–I89.0, I89.9, I98 and K75.1). ICD-10 codes were extracted from the Global Burden of Disease (GBD) 2017 Cause-ICD Codes Map provided by the Institute for Health Metrics and Evaluation.9
Redistribution of garbage codes
Garbage codes are causes of death with little or ‘no public health value because they are too vague, are an immediate or intermediate cause of death or are impossible as an underlying cause of death’.10 These codes can account for an important fraction of the total causes of deaths, and they must be redistributed to improve the utility of death records.
We retrieved death records including garbage-coded ones, as defined by the ‘List of ICD codes mapped to the GBD cause list for causes of death’ in the GBD Study 2017 Data Resources. On these garbage-coded death records with clear redistribution proportion in the ‘List of garbage code redistribution over the GBD cause list for communicable diseases, non-communicable diseases and injuries’ in the online supplemental appendix of the GBD 2010,11 we redistributed accordingly. Garbage-coded death records without a specific redistribution guide, with more than 500 cases over the 6-year period and are cardiovascular related (ie, I678, I64X, I694, I698 and I679) were also redistributed. These garbage codes were reassigned to different types of cardiovascular disease using fractional redistribution according to sex and age group strata. All other death records were not included in our analyses.
heartjnl-2021-320082supp001.pdf (1.2MB, pdf)
Statistical analysis
A descriptive analysis of this refined database was obtained to characterise the targeted population. A projection of the mortality on all cardiovascular diseases was made using a quasi-Poisson regression model on the monthly cardiovascular mortality from 2015 to 2019. The quasi-Poisson model included three components: (1) secular trend, which used quadratic and cubic components; (2) within-year trend, which included each month as a categorical variable; and (3) interactions terms between the year and the month which allow considering the assumption that seasonality behaviour could change throughout the years of the study :
Number of deaths=B0intercept+B1month2+B2month3+B3Feb+B4Mar+B5Apr+B6May+B7Jun+B8Jul+B9Aug+B10Sep+B11Oct+B12Nov+B13Dec+B14year+B15Feb:year+ B17Mar:year+B17Apr:year+B18May:year+B19Jun:year+B20Jul:year+B21Aug:year+B22Sep:year+B23Oct:year+B24Nov:year+B25Dec:year
This model assumes that the trend of the factors influencing the number of cardiovascular deaths during 2015–2019, such as ageing and population size, remains constant during 2020. A backward process of selection was implemented to reduce the number of coefficients. Attributable fraction (AF), defined as 1 minus the fraction of the projected number of deaths over the observed number of deaths in 2020, was used to express the relative excess or deficit of deaths in 2020 compared with the predicted values for 2020 according to the general trend in 2015–2019. Analyses were also stratified by sex, age and specific cardiovascular disease.
Two sensitivity analyses were performed. In the first one, the secular trend of the quasi-Poisson model was restricted, allowing only a quadratic term. Also, interaction terms between months and the year were removed, and the backward selection procedure was not implemented. This alternative predicted more conservative values for 2020. In the second one, the redistribution of garbage codes was not performed (ie, excluding cases with garbage codes). This allowed us to examine the extent of impacts on the results by performing redistribution.
Analyses were performed using R (V.3.5.1). Uncertainty of AFs was obtained by simulating 10.000 number of expected deaths assuming a gamma distribution, using the predicted number and its SEs from regression models as inputs. These numbers were divided by the observed number of death and subtracted to 1. The percentiles 2.5% and 97.5% are presented as uncertainty intervals (95% UIs).
Patient and public involvement
Neither patients nor the public were involved in the design, conduct, reporting or dissemination plans of our research.
Results
During 2015–2020, 97 097 deaths were coded in cardiovascular condition. After redistribution of garbage codes (43.7% of overall cardiovascular deaths), this number increased to 173 283, among which 28 141 were observed in 2020. Compared with the data on cardiovascular deaths between 2015 and 2019, the ones collected in 2020 exhibited limited proportional differences in sex, age group and type of cardiovascular disease (table 1).
Table 1.
Distribution of deaths by cardiovascular diseases observed in period 2015–2019 and 2020, according to sex, age group and type of cardiovascular disease, Chile 2020
| n=145 143 | N=28 141 | |
| 2015–2019 | 2020 | |
| Female (%) | 48.9 | 49.0 |
| Age groups (%) | ||
| <40 | 1.7 | 1.8 |
| 40–59 | 10.4 | 10.4 |
| 60–69 | 13.8 | 13.9 |
| 70–79 | 23.2 | 22.3 |
| 80–89 | 32.5 | 31.3 |
| >89 | 18.3 | 20.4 |
| Types of cardiovascular disease (%) | ||
| Ischaemic heart diseases | 40.8 | 42.9 |
| Strokes | 36.7 | 34.5 |
| Hypertensive heart diseases | 11.0 | 11.4 |
| Miscellaneous | 8.0 | 7.2 |
| Other cardiovascular diseases | 3.4 | 4.0 |
All disease categories include fractions of garbage code redistribution.
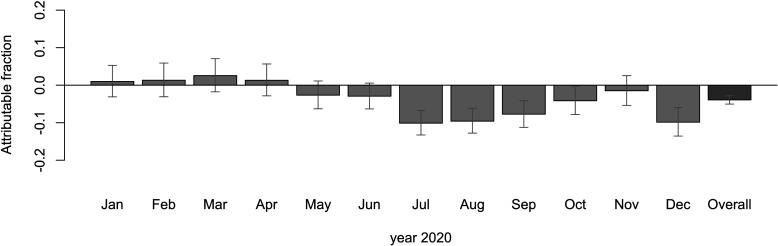
Overall, the AF (and accompanying 95% UI) of all cardiovascular deaths in 2020 was −4.0% (−5.0% to −2.8%), indicating that the observed number of cardiovascular deaths in 2020 was lower than our projection. Saved deaths were concentrated in July, August, September and December (figure 1).
Figure 1.
Monthly fraction of cardiovascular deaths in Chilean population attributable to 2020, according to projections using observed data from 2015 to 2019.
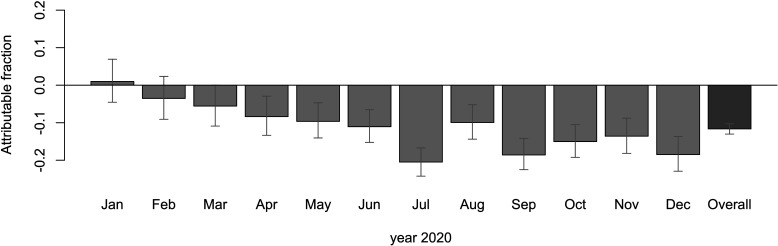
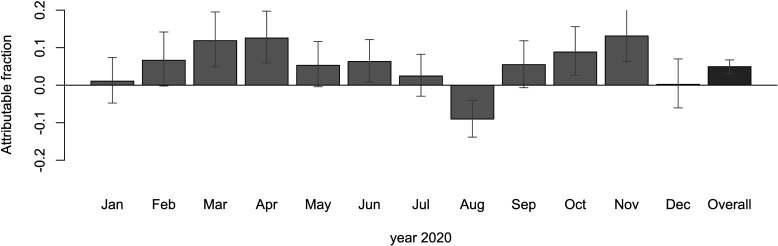
In the stratified analysis based on sex, we observed a steeper negative AF in men than in the general trend, reaching −11.7% (−13% to −10.3%). Saved deaths were significant from April to December with peaks in July, September and December (figure 2). An opposite pattern was observed in female cardiovascular deaths with an overall positive AF of 5.0% (3.2% to 6.8%). Peaks of deaths in excess were observed in March, April and November. Only 1 month (August) showed a reduced number of deaths (figure 3).
Figure 2.
Monthly fraction of cardiovascular deaths in Chilean men attributable to 2020, according to projections using observed data from 2015 to 2019.
Figure 3.
Monthly fraction of cardiovascular deaths in Chilean women attributable to 2020, according to projections using observed data from 2015 to 2019.
Disaggregated data based on age groups showed that those aged 60–69 years and 70–79 years showed negative AFs, like the overall trend. However, those aged 80 years or more showed a positive AF of 11.0% (8.6% to 13.5%) (table 2).
Table 2.
Estimated cardiovascular excess deaths (attributable fraction) according to sex, age group and type of cardiovascular disease, Chile 2020
| Median (%) | UI (%) 2.5%–97.5% |
|
| Overall | −4.0 | −5.0 to −2.8 |
| Sex | ||
| Male | −11.7 | −13 to −10.3 |
| Female | 5.0 | 3.2 to 6.8 |
| Age group | ||
| 40–59 | −1.4 | −4.9 to 2.2 |
| 60–69 | −22.6 | −24.7 to −20.4 |
| 70–79 | −15.4 | −17.3 to −13.5 |
| 80–89 | 11.0 | 8.6 to 13.5 |
| >89 | 2.4 | −0.3 to 5.1 |
| Type of cardiovascular disease | ||
| Ischaemic heart diseases | −3.7 | −5.4 to −2.0 |
| Strokes | −5.2 | −6.9 to −3.3 |
| Hypertensive heart diseases | 18.9 | 14.7 to 23.5 |
| Miscellaneous | −12.7 | −16.2 to −9.1 |
| Other cardiovascular diseases | −21.4 | −25.3 to −17.2 |
All disease categories include fractions of garbage code redistribution.
UI, uncertainty interval (quantiles 2.5–97.5).
All types of cardiovascular disease, except for hypertensive heart diseases, had negative AFs. There was a positive AF of 18.9% (14.7% to 23.5%) in hypertensive heart diseases (table 2).
Results are sensitive to model specification. In the sensitive analysis 1, excluding cubic terms and interaction terms, as well as using the same regression model for all estimates, overall, the obtained AFs were rather smaller than those from our main analysis (−0.2% (−1.3% to 1.0%)). However, the trend of AF deviation regarding zero in both male (−3.7% (−5.2% to −2.1%)) and female (3.7% (1.9% to 5.4%)), in age group 60–69 years (−9.9% (−12.5% to −7.1%)), 70–79 years (−2.9% (−5.2% to −0.6%)) and 80–89 years (4.5% (2.4% to 6.8%)) as well as in ischaemic heart diseases (−2.3% (−3.9% to −0.6%)) and hypertensive heart diseases (19.3% (14.8% to 23.9%)) is the same to our projection allowing cubic and interaction terms (online supplemental tables). In the sensitivity analysis 2, which is without the redistribution of garbage codes, the trend of results remains similar to our main analysis in overall cardiovascular deaths (−6.8% (−8.2% to −5.4%)), men (−11.9% (−13.6% to −10.1%)), age groups of 60–69 years (−24.5% (−27.0% to −21.9%)), 70–79 years (−8.5% (−11.3% to −5.6%)), and 80–89 years (9.7% (6.2% to 13.2%)), and in ischaemic heart diseases (−8.9 (−10.9% to −7.0%)), strokes (−14.1% (−16.8% to −11.2%)) and hypertensive heart diseases (22.4% (16.9% to 28.3%)). However, the AF deviations in women in sensitivity analysis 2 were less notable (0.3% (−2% to 2.7%)) (online supplemental tables).
Discussion
In 2020, we observed under the main analytical scenario fewer overall cardiovascular deaths than our projection, and this could be attributed to the effect of the COVID-19 pandemic. Despite an overall trend of decreased cases, the results differed interestingly by sex, age group and type of cardiovascular disease.
Decreased cardiovascular death could be explained by competitive mortality given by COVID-19. That means that several people who would have died by any cause in the second semester of 2020 died from COVID-19. Moreover, evidence showed that people with pre-existing cardiovascular diseases have a higher risk of dying when they are infected by SARS-CoV-2 than people without such pre-existing conditions.12 This could be the reason for the significantly negative deviated AF of overall cardiovascular deaths in July, August and September, which are the months after the peak of COVID-19 death in Chile. Other reasons have been proposed to explain fewer cardiovascular deaths. A drop in incidence could be caused by COVID-19 competitive mortality (especially in men) or by a drop in cardiovascular risks (or both). Environmental and lifestyle changes, including lessened noise13 and air pollution,14 and improved sleep deprivation,15 are factors that have received attention in some research. These environmental changes were observed in Chile16 and may contribute to the observed decrease in emergency room visits and hospital discharges during the first wave, without a parallel increase in cardiovascular mortality.8
The decrease of cardiovascular deaths during the pandemic, however, is not consistent worldwide. Reports have shown mixed results. In a UK study, Wu et al observed excess of non-COVID-19 cardiovascular mortality at 8% from March to June 2020. Deaths with the greatest excess were at home, care home and hospice, which constitute almost half of all cardiovascular deaths, with stroke and acute coronary syndrome being the most common. The study suggested that delay of medical care access could be the reason behind such phenomenon.17 Besides, a Brazilian study also observed an overall increase in cardiovascular deaths nationwide from mid-March to early June 2020, although a decrease in deaths in acute coronary syndrome and stroke was noted in most cities at the same time. In particular, there is a notable increase in unspecified deaths, with a strong correlation to deaths at home. Brant et al proposed that the excess cardiovascular mortality could be a result of collapsed healthcare systems and the decreased mortality in specific diseases could be due to misdiagnosis.18 Moreover, in a study on American cardiovascular mortality from mid-March to early June 2020, Wadhera et al revealed an increase in deaths by ischaemic heart disease and hypertensive diseases in parts of the USA, while deaths caused by heart failure, cerebrovascular disease or other diseases of the circulatory system did not change. The increased deaths of these specific diseases, however, are limited to some states and cities, not nationwide, and the authors suggested there may be indirect impacts on cardiovascular patients by the pandemic.19 While we do not share identical trends with the studies, our results echoed the findings on some types of cardiovascular diseases. Different from the studies, our study covered the whole of 2020, other than just a few months in early 2020 as most did. This is to take both the seasonal difference of cardiovascular mortality and the later arrival of the COVID-19 pandemic in Chile into account. Future studies over similar time frame will be better for further comparison between countries.
The decrease of cardiovascular death is, however, not consistent between sex. Men have a stable and significant negative deviation from our projection while women experienced increases in cardiovascular deaths over certain months during the pandemic. In a worldwide meta-analysis, Peckham et al demonstrated that male patients have a COVID-19 death OR of 1.39 (95% CI:1.31 to 1.47), despite a similar proportion of COVID-19 infection.20 The higher risk of men dying from COVID-19 could result in less mortality from causes of death other than COVID-19 among men.
However, the pandemic could expose women to more cardiovascular risks than before. As shown in our analysis, a significant excess of cardiovascular death is noted among women, especially from March to June 2020 in Chile’s big first wave. While there is no available causal information to explain such a phenomenon, the lack of awareness of cardiovascular diseases and gender-biased medical attention and treatment from cardiovascular units in healthcare facilities could be the major threat to female cardiovascular health. A recent study showed that women in Santiago, Chile have poor awareness of cardiovascular diseases as a prominent disease, which could delay their medical care.21 Chilean women have also been found to have higher risks of hospital mortality from acute myocardial infarction than men, suggesting a gap in treatment.22 These elements could be exacerbated during the pandemic, leaving women in a riskier situation. A possible solution to this issue could be rigorous public health campaigns through local media, which proved to be an effective way to promote awareness on the timely care of acute cardiovascular events during the pandemic in the USA and France.23 24
Other reasons for women’s vulnerability to cardiovascular disease during the pandemic have also been proposed, including the role as caregivers,25 increased rate of domestic violence26 as well as the sedentary lifestyle and dietary habits during quarantine periods.27 While these factors could impact all people, they are more prominent among women and therefore could contribute to the higher cardiovascular risk and mortality suffered by women. The long-ignored female cardiovascular health should be addressed in future policy to avoid ongoing excess of cardiovascular death both during the pandemic and in the post-pandemic era.
Higher excess of cardiovascular deaths observed in the age group 80–89 years seems counterintuitive since that group is the most vulnerable to die by COVID-19. However, they were protected from infection by the governmental isolation policy (ie, self-quarantine), which was specifically addressed to this age group at the beginning of the pandemic in Chile. The associated stress and worsening in mental health conditions could have increased the incidence of cardiovascular events. Additionally, the decreased medical access in ‘non-essential’ regular medical care on non-communicable diseases, including cardiovascular diseases, could have also increased case fatality.28 The higher vulnerability of the older population to cardiovascular events should be considered in the design of future policies.
Lastly, we also noted that there is a positive AF of deaths from hypertensive heart diseases in 2020, especially during the months when Chile was severely hit by COVID-19. While patients with hypertensive heart diseases usually require long-term care, the disruption of medical service during the pandemic creates barriers for continuous service access. Such disruption is worldwide as a WHO survey revealed that more than half of the 163 Ministries of Health reported disrupted service on hypertension management.29 Although innovative solutions such as home visits, home delivery of chronic medicines and telemedicine for higher risk populations have been implemented in Chilean public primary care services, the exact coverage of such a service has not been systematically evaluated.
This study has several limitations. First, we explored excess deaths by cardiovascular disease using the expected numbers of deaths according to the trend observed in the previous 5 years. Consequently, we cannot make direct attribution causation about the effect of the pandemic on the epidemiology of mortality by cardiovascular diseases, neither about the underlying mechanisms behind this causation. However, we implemented a flexible model that allows capturing the general trend, stationarity and particularities within each stationary cycle. Moreover, we performed a sensitivity analysis that explored some of the assumptions in the models, without substantial change in the direction of AF regarding zero. Second, since deaths are assigned only to one ICD-10 code, it is difficult to know if all deaths recorded are pure cardiovascular deaths without COVID-19 infection and vice versa. Chilean 202021 mortality database is still considered preliminary, so further validation may help reach definite conclusions. Third, our garbage code redistribution may not reflect the real cause of death. After redistribution, the newly added deaths account for 43.7% of all cardiovascular deaths in our database. However, in our sensitivity analysis without redistribution of garbage codes, we still observed negative AF deviation, despite different magnitudes (online supplemental table S2). Garbage codes mainly came from unspecified cardiovascular causes of death such as essential hypertension (code I10X), stroke, not specified as haemorrhage or infarction (code I64X), or heart failure, unspecified (code I509). Garbage codes are due to lack of access to accurate or complete medical records at the moment of death registration, inadequate training of physicians for completing death certifications and local misclassification practices.30 While we discussed the AF of each category, respectively, we recognised that these factors may be inter-related and have provided related tables in the online supplemental materials for reference (online supplemental table S3). Further research will be required to further explore the interplay between sex, age group and type of cardiovascular disease.
Conclusion
A decrease in overall cardiovascular deaths has been observed in Chile in 2020. Important differences by sex, age group and type of cardiovascular disease were found. Competing mortality of COVID-19 infection, changes in access or treatment offered by healthcare services, or the effect of preliminary death coding yet to be fully validated could explain some of these changes. Our findings suggest the need for further studies on the impacts brought by COVID-19 on cardiovascular health in Chile.
What is already known on this subject?
Previous studies on cardiovascular mortality in the UK, Brazil, Italy and France during the COVID-19 pandemic have shown an excess of non-COVID-19 cardiovascular deaths due to the lack of access to immediate medical services.
What might this study add?
We noted an overall decrease in cardiovascular deaths in Chile, compared with our projection using the data from 2015 to 2019. However, an excess of cardiovascular mortality was noted in women, people in the age group 80–89 years and people who died from hypertensive heart diseases, suggesting possible diverse impacts of the COVID-19 containment policy.
How might this impact on clinical practice?
While the competitive mortality of COVID-19 could lower cardiovascular deaths in high-risk populations like men, the containment policy could result in higher cardiovascular mortality in women and some vulnerable populations. Public health authorities should be aware of these possible collateral effects on cardiovascular health. Focused measures to maintain adequate access to cardiovascular care should be encouraged.
Acknowledgments
We would like to extend our sincere thanks to Dr Thomas J Bossert, who has provided invaluable insight into this work.
Footnotes
Contributors: S-WC, PZ, AP-S and PM were involved in planning the work. SW-C, PZ and ÁP-S processed the epidemiological data, performed the analysis, drafted the manuscript, and designed the tables and figures. PM aided in interpreting the results and worked on the manuscript. PM is the guarantor. All authors discussed the results and commented on the manuscript.
Funding: The publication of this study is sponsored by the Harvard Lown Scholar Programme.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository (reference 8). Data are available upon reasonable request. All data used are secondary and anonymous from an official governmental open-access source, following all the principles of the Helsinki Declaration.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study has been approved by the scientific ethical committee of the Pontificia Universidad Católica de Chile in Santiago, Chile.
References
- 1. Czeisler Mark É, Marynak K, Clarke KEN, et al. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1250–7. 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ganatra S, Dani SS, Shah S, et al. Management of cardiovascular disease during coronavirus disease (COVID-19) pandemic. Trends Cardiovasc Med 2020;30:315–25. 10.1016/j.tcm.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andersson C, Gerds T, Fosbøl E, et al. Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail 2020;13:e007274. 10.1161/CIRCHEARTFAILURE.120.007274 [DOI] [PubMed] [Google Scholar]
- 4. Kundi H, Balcı MM, Güngörer B, et al. Trends in acute myocardial infarction admissions during the COVID-19 pandemic in Ankara, Turkey. Anatol J Cardiol 2020;24:81. 10.14744/AnatolJCardiol.2020.70206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moroni F, Gramegna M, Ajello S, et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep 2020;2:1620–4. 10.1016/j.jaccas.2020.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gadella A, Sastre Miguel Ángel, Maicas C, et al. Infarto agudo de miocardio Con elevación del segmento ST en tiempos de COVID-19: ¿regreso al siglo pasado? Una llamada de atención. Revista Española de Cardiología 2020;73:582–3. 10.1016/j.recesp.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bossert TJ, Leisewitz T. Innovation and change in the Chilean health system. N Engl J Med 2016;374:1–5. 10.1056/NEJMp1514202 [DOI] [PubMed] [Google Scholar]
- 8. Ministerio de Salud de Chile, Departamento de Estadísticas e Información de Salud (DEIS). Datos abiertos. Available: https://deis.minsal.cl/#datosabiertos [Accessed 19 Apr 2021].
- 9. Network, G.B.o.D.C . Causes of death and nonfatal causes mapped to ICD codes, in global burden of disease study 2017 (GBD 2017). Seattle, USA: Institute for Health Metrics and Evaluation (IHME), 2018. [Google Scholar]
- 10. Naghavi M, Richards N, Chowdhury H, et al. Improving the quality of cause of death data for public health policy: are all ‘garbage’ codes equally problematic? BMC Med 2020;18:1–3. 10.1186/s12916-020-01525-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2095–128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–42. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 13. Münzel T, Sørensen M, Daiber A. Transportation noise pollution and cardiovascular disease. Nat Rev Cardiol 2021;18:619–36. 10.1038/s41569-021-00532-5 [DOI] [PubMed] [Google Scholar]
- 14. Yin P, Brauer M, Cohen AJ, et al. The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990-2017: an analysis for the global burden of disease study 2017. Lancet Planet Health 2020;4:e386–98. 10.1016/S2542-5196(20)30161-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Advani I, Gunge D, Banks S, et al. Is increased sleep responsible for reductions in myocardial infarction during the COVID-19 pandemic? Am J Cardiol 2020;131:128–30. 10.1016/j.amjcard.2020.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Toro A R, Catalán F, Urdanivia FR, et al. Air pollution and COVID-19 lockdown in a large South American City: Santiago metropolitan area, Chile. Urban Clim 2021;36:100803. 10.1016/j.uclim.2021.100803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wu J, Mamas MA, Mohamed MO, et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart 2021;107:113–9. 10.1136/heartjnl-2020-317912 [DOI] [PubMed] [Google Scholar]
- 18. Brant LCC, Nascimento BR, Teixeira RA, et al. Excess of cardiovascular deaths during the COVID-19 pandemic in Brazilian capital cities. Heart 2020;106:1898–905. 10.1136/heartjnl-2020-317663 [DOI] [PubMed] [Google Scholar]
- 19. Wadhera RK, Shen C, Gondi S, et al. Cardiovascular Deaths During the COVID-19 Pandemic in the United States. J Am Coll Cardiol 2021;77:159–69. 10.1016/j.jacc.2020.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 2020;11:1–10. 10.1038/s41467-020-19741-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Varleta P, Acevedo M, Casas-Cordero C, et al. Low cardiovascular disease awareness in Chilean women: insights from the ESCI project. Glob Heart 2020;15:55. 10.5334/gh.534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nazzal C, Alonso FT. Younger women have a higher risk of in-hospital mortality due to acute myocardial infarction in Chile. Rev Esp Cardiol 2013;66:104–9. 10.1016/j.rec.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 23. Garcia S, Stanberry L, Schmidt C, et al. Impact of COVID-19 pandemic on STEMI care: an expanded analysis from the United States. Catheter Cardiovasc Interv 2021;98:217–22. 10.1002/ccd.29154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Van Belle E, Manigold T, Piérache A, et al. Myocardial infarction incidence during national lockdown in two French provinces unevenly affected by COVID-19 outbreak: an observational study. Lancet Reg Health Eur 2021;2:100030. 10.1016/j.lanepe.2021.100030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stewart AL, Magnani JW, Barinas-Mitchell E, et al. Social role stress, reward, and the American heart association life's simple 7 in midlife women: the study of women's health across the nation. J Am Heart Assoc 2020;9:e017489. 10.1161/JAHA.120.017489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chandan JS, Thomas T, Bradbury-Jones C, et al. Risk of cardiometabolic disease and all-cause mortality in female survivors of domestic abuse. J Am Heart Assoc 2020;9:e014580. 10.1161/JAHA.119.014580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mattioli AV, Sciomer S, Maffei S, et al. Lifestyle and stress management in women during COVID-19 pandemic: impact on cardiovascular risk burden. Am J Lifestyle Med 2021;15:356–9. 10.1177/1559827620981014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Villalobos Dintrans P, Browne J, Madero-Cabib I. It is not just mortality: a call from Chile for comprehensive COVID-19 policy responses among older people. J Gerontol B Psychol Sci Soc Sci 2021;76:e275–80. 10.1093/geronb/gbaa092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization . Rapid assessment of service delivery for NCDS during the COVID-19 pandemic. Geneva: World Health Organization, 2020. [Google Scholar]
- 30. Johnson SC, Cunningham M, Dippenaar IN, et al. Public health utility of cause of death data: applying empirical algorithms to improve data quality. BMC Med Inform Decis Mak 2021;21:1–20. 10.1186/s12911-021-01501-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
heartjnl-2021-320082supp001.pdf (1.2MB, pdf)
Data Availability Statement
Data are available in a public, open access repository (reference 8). Data are available upon reasonable request. All data used are secondary and anonymous from an official governmental open-access source, following all the principles of the Helsinki Declaration.