Abstract
Objectives
Patients with empty nose syndrome (ENS) suffer from paradoxical nasal obstruction with a patent objective nasal airway. ENS may result from the excessive surgical reduction of the turbinate tissue. ENS patients also experience significant psychological symptoms such as anxiety and depression. In this study, we aimed to evaluate the prevalence of suicidal thoughts in ENS patients and to characterize these patients for early identification.
Study Design
Prospective case series.
Methods
Patients with ENS were prospectively recruited for this study. The Sino‐Nasal Outcome Test‐25 (SNOT‐25), Empty Nose Syndrome 6‐item Questionnaire (ENS6Q), Beck Anxiety Inventory (BAI), and Beck Depression Inventory‐II (BDI‐II) were used to assess ENS patients before and 6 months after nasal reconstruction surgery.
Results
Sixty‐two patients with ENS were enrolled. Suicidal thoughts were identified in 23 ENS patients preoperatively and in four patients postoperatively. ENS patients with suicidal thoughts rated significantly higher in the SNOT‐25, ENS6Q, BDI‐II, and BAI total scores than those without suicidal thoughts (all P < .05). “Nose feels too open” was the item in ENS6Q that was significantly more severe in ENS patients with suicidal thoughts than those without suicidal thoughts (P < .001).
Conclusions
Suicidal thoughts are frequently identified in patients with ENS. ENS patients with suicidal thoughts experienced significantly more severe symptoms, impaired quality of life, and psychological burden than those without suicidal thoughts. Recognizing individuals who may carry suicidal thoughts and provide appropriate psychological interventions is critical to prevent tragedy.
Level of Evidence
4
Keywords: Beck Depression Inventory II, depression, Empty Nose Syndrome 6‐item Questionnaire, empty nose syndrome, suicidal thoughts
Suicidal thoughts are frequently identified in patients with empty nose syndrome (ENS). ENS patients with suicidal thoughts experienced significantly more severe symptoms, impaired quality of life, and psychological burden than those without suicidal thoughts. Recognizing individuals who may carry suicidal thoughts and provide appropriate psychological interventions is critical to prevent tragedy.
1. INTRODUCTION
Empty nose syndrome (ENS) was first described in 1994 by Dr. Eugene Kern. 1 He found that his patients committed suicide due to suffering from the ENS condition. ENS is a complicated condition that is not fully understood. Currently, it is considered to be caused by the excessive surgical removal of turbinate tissue. 1 , 2 The pathophysiology of ENS may be attributed to the abnormal mucosal recovery of neurosensory systems in healing process and changes in the airflow of nose after surgical intervention. 2 , 3 , 4 , 5 , 6 , 7 A lack of communication between breathing and the brain may be the key factor in the development of ENS.
Patients with ENS suffer from paradoxical nasal obstruction with patent objective nasal airways. 8 The other common symptoms encompass a spectrum of diversity and severity, including sensation of suffocation, dryness, burning, crusting, and lack of sense of airflow in the nasal cavity. 7 , 8 ENS patients usually experience psychiatric problems, including chronic fatigue, frustration, irritability, anger, anxiety, and depression. As a result, a significant negative impact on the quality of life and increased risk of mental health disorders are frequently reported. 9 , 10 , 11 , 12 , 13 Our previous studies demonstrated a high prevalence of anxiety and depression among ENS patients using the Sino‐Nasal Outcome Test‐25 (SNOT‐25), Beck Anxiety Inventory (BAI), and Beck Depression Inventory‐II (BDI‐II). 12 , 14 , 15 , 16 The high prevalence of mental health disorders in ENS patients is an alert to the risk of suicide in these patients. Thus, in this study, we aimed to evaluate the prevalence of suicidal thoughts in ENS patients and characterize these patients for early identification. These results would be beneficial for those with ENS who are at risk of suicide.
2. MATERIALS AND METHODS
2.1. Patients
Patients with ENS were prospectively recruited from the Department of Otolaryngology between 2016 and 2021. Demographic data and clinical characteristics of the patients were recorded. All patients provided informed consent for participation in the study. This study was approved by the Institutional Review Board of the Chang Gung Medical Foundation (IRB numbers: 201601703A3, 201802147A3, and 201902001A3).
ENS was diagnosed according to the symptoms of paradoxical nasal obstruction with an observation of a wide nasal airway on nasal endoscopy and/or computed tomography (Figure 1). Furthermore, diagnosis of ENS was confirmed by a cotton test as described in previous studies. 1 Briefly, a moistened cotton ball was placed in the nasal cavity of the participant, and the participant was asked to breathe through the nose. Improvement in nasal symptoms indicates a positive result in the cotton test. While, we excluded patients with (1) a craniofacial anomaly, or (2) other sinonasal diseases such as rhinosinusitis, or (3) psychiatric disorders who were previously diagnosed and has been treated by psychiatrists.
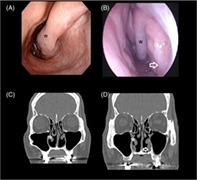
FIGURE 1.
Nasal endoscopy image in an empty nose syndrome (ENS) patient (A) before and (B) after surgical reconstruction by submucosal Medpor implantation. Nasal computed tomography in the ENS patient (C) before and (D) after surgical reconstruction by submucosal Medpor implantation. The SNOT‐25/ENS6Q scores before and after surgery were 76/22 and 47/10, respectively. Asterisk, remnant of inferior turbinate; arrow, submucosal Medpor implantation
The participants then received submucosal Medpor implantation under endoscopic assistance as described previously. 14 , 15 In brief, implantation of Medpor by pieces was done after creation of a submucosal pocket via an incision on the lateral wall of nose.
2.2. Questionnaire evaluations
Chinese versions of the Empty Nose Syndrome 6‐item Questionnaire (ENS6Q), SNOT‐25, BAI, and BDI‐II were used to evaluate the subjective symptoms and quality of life in patients with ENS before and 6 months after surgical reconstruction. 16 , 17 , 18 , 19 Participants rated each item from 0 to 5, with 0 indicating no symptoms and 5 representing the most severe symptoms in SNOT‐25 and ENS6Q evaluation. In addition, participants rated between 0 and 3 (symptom not present to strongly present) for each item in 21 items of the BDI‐II and BAI evaluation, respectively, which has a total score of 0–63. Suicidal thoughts were evaluated by the ninth item in the BDI‐II, and the participants selected between “I don't have any thoughts of killing myself (score 0),” “I have thoughts of killing myself, but I would not carry them out (score 1),” “would like to kill myself (score 2),” and “I would kill myself if I had the chance(score 3).” A total BDI‐II score of 0–13, 14–19, 20–28, and 29–63 indicates normal, mild, moderate, and severe depression, respectively. 18 , 20
2.3. Statistical analyses
The data were presented as the mean ± standard deviation (SD) and were statistically analyzed using GraphPad Prism 5 (GraphPad Prism Software, Inc.). Categorical variables were compared using the χ 2 test or Fisher's exact test, as appropriate. Continuous variables were analyzed using the Mann–Whitney U test or unpaired t‐test between participants with and without suicidal thoughts according to the results of the D'Agostino–Pearson omnibus normality test. To identify and characterize the specificity and sensitivity of the preoperative SNOT‐25, ENS6Q, BAI, and BDI‐II in the detection of suicidal thoughts in ENS patients, we generated receiver operating characteristic (ROC) curves of these metrics and calculated the area under the ROC curve (AUC). A P‐value of <.05 was considered statistically significant.
3. RESULTS
3.1. Clinical characteristics of the study population
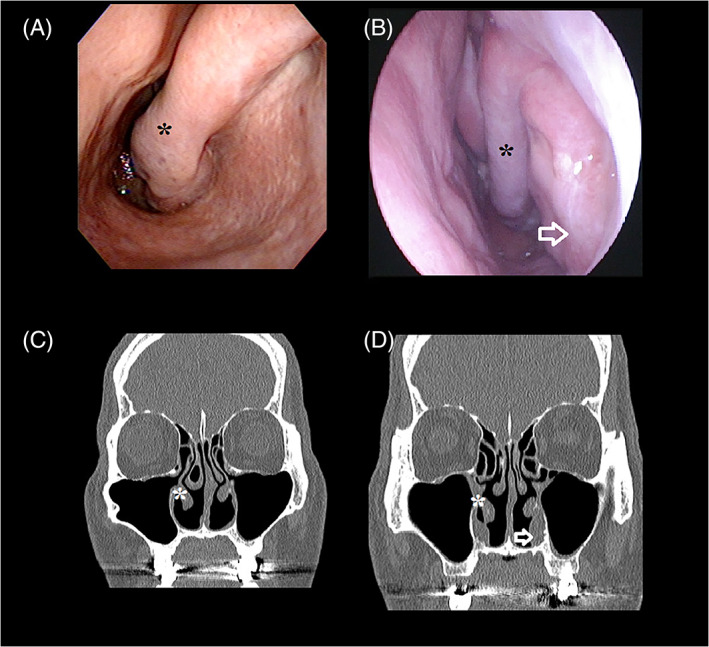
A total of 62 patients with ENS were enrolled during the study period. The general characteristics of the participants are summarized in Table 1. Suicidal thoughts were identified in 23 patients with ENS. Among them, 20 patients rated a score of 1, indicating “I have thoughts of killing myself, but I would not carry them out”; two patients rated a score of 2, indicating “I would like to kill myself”; and one patient rated a score of 3, indicating “I would kill myself if I had the chance” at baseline evaluation (Figure 2). After surgery, there were four patients who scored 1, and the other 58 patients scored 0, indicating “I don't have any thoughts of killing myself.” There was no difference between patients with and without suicidal thoughts in terms of age, male predominance, and serum total immunoglobulin (Ig) E, except for cigarette smoking. There were significantly more smokers in patients with suicidal thoughts than in those without suicidal thoughts.
TABLE 1.
Clinical characteristics of the study participants
| Total | Suicidal thoughts | P value a | ||
|---|---|---|---|---|
| No | Yes | |||
| Case number, n | 62 | 39 | 23 | |
| Age (year) | 49.8 ± 12.8 | 52.2 ± 12.0 | 45.8 ± 13.5 | .062 |
| Female: male, n | 15: 47 | 9: 30 | 6: 17 | .789 |
| Smoker, n (%) | 10 (16.1) | 3 (7.7) | 7 (30.4) | .018* |
| Serum IgE (IU/ml) | 186.2 ± 305.3 | 163.9 ± 212.6 | 225.7 ± 426.5 | 1.000 |
| Previous nasal surgery: | ||||
| Inferior turbinate surgery, n (%) | 62 | 39 | 23 | |
| Nasal septal surgery, n (%) | 39 | 24 | 15 | |
| Endoscopic sinus surgery, n (%) | 17 | 12 | 5 | |
| Caldwell–Luc operation, n (%) | 7 | 5 | 2 | |
| Pre‐op SNOT‐25 | 70.9 ± 23.1 | 66.9 ± 20.7 | 80.8 ± 20.2 | .041* |
| Pre‐op ENS6Q | 16.1 ± 5.5 | 15.3 ± 5.0 | 18.3 ± 4.9 | .018* |
| Pre‐op BDI‐II | 21.6 ± 15.1 | 14.7 ± 10.8 | 34.3 ± 13.0 | <.001** |
| Pre‐op BAI | 20.8 ± 13.2 | 15.7 ± 10.2 | 30.1 ± 12.3 | <.001** |
| Post‐op SNOT‐25 | 34.1 ± 25.0 | 33.9 ± 24.0 | 35.8 ± 26.7 | .776 |
| Post‐op ENS6Q | 6.8 ± 5.5 | 6.6 ± 5.2 | 7.3 ± 6.2 | .771 |
| Post‐op BDI‐II | 7.3 ± 9.1 | 7.5 ± 9.1 | 7.3 ± 9.3 | .392 |
| Post‐op BAI | 9.5 ± 10.0 | 9.7 ± 10.3 | 9.3 ± 9.7 | .878 |
Note: Data are represented as mean ± standard deviation (SD).
Abbreviations: BAI, Beck Anxiety Inventor; BDI‐II, Beck Depression Inventory II; ENS6Q, Empty Nose Syndrome 6‐item Questionnaire; Post‐op, 6 months postoperative; Pre‐op, pre‐operative; SNOT‐25, Sino‐Nasal Outcome Test‐25.
Analysis between patients with and without suicidal thoughts. *P < .05; **P < .001.
FIGURE 2.
Case number of patients with suicidal thoughts before (pre‐op) and after (post‐op) nasal reconstruction surgery. α: analysis of patient numbers with and without suicidal thoughts by χ 2 test
3.2. Questionnaire evaluations
The pre‐op BDI‐II scores comprised 22 (35.5%) patients without depression (scores of 0–13), 10 (16.1%) patients with mild depression (scores of 14–19), seven (11.3%) patients with moderate depression (scores of 20–28), and 23 (37.1%) patients with severe depression (scores of 29–63).
The pre‐op and 6‐month post‐op total scores of the SNOT‐25, ENS6Q, BAI, and BDI‐II are presented in Table 1. There was a significant difference in the total SNOT‐25, ENS6Q, BAI, and BDI‐II between the ENS patients with and without suicidal thoughts before surgery. However, there was no difference in the total score of these four questionnaires between ENS patients with and without suicidal thoughts 6 months after surgery.
In further comparison of each item in ENS6Q between patients with and without suicidal thoughts, “Nose feels too open” scored significantly higher in patients with suicidal thoughts (P < .001). The scores of the other items showed no difference between the two groups (Table 2).
TABLE 2.
The Empty Nose Syndrome 6‐item Questionnaire (ENS6Q) scores reported by participants before surgery
| Items | Total | Without suicidal thought | With suicidal thought | P value a |
|---|---|---|---|---|
| Dryness | 3.8 ± 1.3 | 3.6 ± 1.4 | 4.2 ± 1.0 | .114 |
| Sense of diminished nasal airflow | 3.8 ± 1.4 | 3.7 ± 1.4 | 3.9 ± 1.5 | .471 |
| Suffocation | 3.8 ± 1.5 | 3.8 ± 1.3 | 3.8 ± 1.7 | .522 |
| Nose feels too open | 2.0 ± 2.1 | 1.3 ± 1.7 | 3.2 ± 2.0 | <.001** |
| Nasal crusting | 1.5 ± 1.7 | 1.2 ± 1.5 | 2.0 ± 1.9 | .121 |
| Nasal burning | 1.7 ± 1.9 | 1.8 ± 2.0 | 1.5 ± 1.7 | .710 |
| Total score | 16.1 ± 5.5 | 15.3 ± 5.0 | 18.3 ± 4.9 | .018* |
Note: Data are represented as mean ± standard deviation (SD).
Analysis between patients with and without suicidal thoughts. *P < .05; **P < .001.
3.3. Using preoperative SNOT‐25, ENS6Q, BAI, BDI‐II, and “Nose feels too open” in ENS6Q metrics to predict having suicidal thoughts
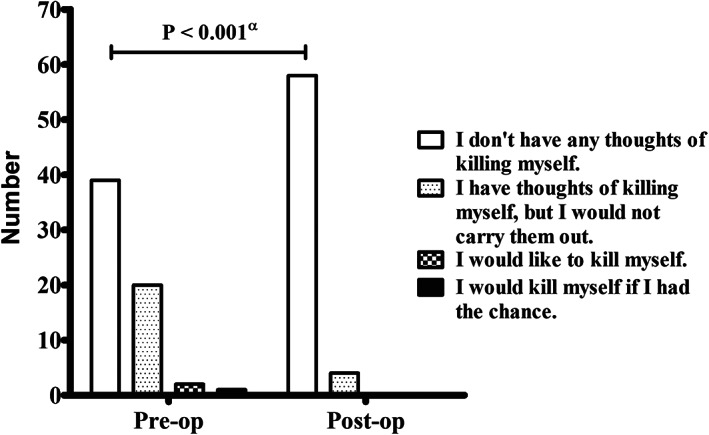
Given the concern that there was a significant difference in the baseline total score of SNOT‐25, ENS6Q, BAI, BDI‐II, and “Nose feels too open” in ENS6Q between the ENS patients with and without suicidal thoughts, ROC curves were generated, and the AUC was calculated to evaluate whether the preoperative SNOT‐25, ENS6Q, BAI, BDI‐II, and “Nose feels too open” in ENS6Q scores predicted suicidal thoughts in our participants (Figure 3). The preoperative SNOT‐25 (AUC = 0.657, P = .029), ENS6Q (AUC = 0.681, P = .009), BAI scores (AUC = 0.817, P < .001), BDI‐II scores (AUC = 0.884, P < .001), and “Nose feels too open” in ENS6Q (AUC = 0.745, P < .001) all had ROC curves with AUCs >0.5. The optimal cutoffs with maximal sum of sensitivity and specificity for these metrics were a SNOT‐25 score of >91 (sensitivity: 34.8%, specificity: 92.3%), an ENS6Q score of >15 (sensitivity: 69.6%, specificity: 69.2%), a BAI score of >25 (sensitivity: 69.6%, specificity: 82.1%), a BDI‐II score of >26 (sensitivity, 82.6%; specificity, 84.6%), and “Nose feels too open” >3 (sensitivity, 60.9%; specificity, 87.2%).
FIGURE 3.
Receiver operating characteristic curves to detect patients with suicidal thoughts using the variables of the preoperative (A) Sino‐Nasal Outcome Test‐25 (SNOT‐25), (B) Empty Nose Syndrome 6‐item Questionnaire (ENS6Q), (C) Beck Depression Inventory II (BDI‐II) scores, (D) Beck Anxiety Inventor (BAI) scores, and (E) “Nose feels too open” in ENS6Q. The optimal cutoffs for these metrics (maximizing the sum of sensitivity and specificity) are indicated
4. DISCUSSION
Patients with ENS carry a significant psychological burden including depression and anxiety. 9 , 11 , 12 , 16 , 21 In the present study, we investigated the suicidal thoughts in ENS patients using validated instruments, including SNOT‐25, ENS6Q, BAI, and BDI‐II. The results demonstrated a high prevalence of moderate‐to‐severe depression (BDI‐II ≥20, 48.4%) in ENS patients. Suicidal thoughts were identified in 23 of 62 (37.1%) ENS patients before surgery and in four patients after surgery. ENS patients with suicidal thoughts experienced significantly more severe symptoms, impaired quality of life, and psychological burden as evaluated by SNOT‐25, ENS6Q, BAI, and BDI‐II questionnaires as compared to those without suicidal thoughts. Thus, patients with severe ENS are at great risk of suicidal ideation and require exceptional attention. Health professionals must be aware of the vulnerability of these patients, identify potential risks, and offer assistance as necessary.
“Nose feels too open” was the item in ENS6Q that was significantly more severe in ENS patients with suicidal thoughts than those without. This symptom may be the most devastating, mentally, and psychologically to patients. Our previous study also revealed that the ENS symptom domain in the SNOT‐25 are associated with psychological burden and could be good predictors of moderate‐to‐severe depression. 12 , 16 The current study further demonstrated that the symptom of “Nose feels too open” may associate with suicidal thoughts. Our previous study 12 revealed sleep dysfunction and empty nose symptoms contribute to the psychological burden experienced by ENS patients. Sleep dysfunction domain score of >18, and empty nose symptoms domain score of >14 in SNOT25 evaluation were good predictors of moderate‐to‐severe depression. 12 In addition, there was a robust association between the sleep dysfunction and empty nose symptoms domains in ENS patients. Besides, there is a strong link between sleep and depression. 22 For example, people with insomnia have greater levels of depression and anxiety than do those who sleep normally. Sleep symptoms cause great distress, have a substantial impact on the quality of life and daily activities, and are a risk factor for suicidal ideation. 23 Taken together, “Nose feels too open” as one of the empty nose symptoms may interfere sleep and contribute to the psychological burden experienced by ENS patients. Thus, surgical reconstruction with Medpor reduced the symptom of “Nose feels too open” (from 2.0 ± 2.1 to 0.8 ± 1.2, P < .001), improved sleep quality, decreased the psychological burden, and diminished the suicidal thoughts.
Suicidal thoughts were associated with higher SNOT‐25, ENS6Q, BAI, and BDI‐II scores preoperatively. Thus, we next try to detect ENS patients with suicidal thoughts by ROC curve analysis with preoperative SNOT‐25, ENS6Q, BAI, and BDI‐II scores. The ROC curve analysis revealed that a SNOT‐25 score of >91, an ENS6Q score of >15, a BAI score of >25, and a BDI‐II score of >26 were predictors of preoperative suicidal thoughts. Recognizing individuals who may carry suicidal thoughts using appropriate instruments and providing appropriate psychological interventions are critical to prevent tragedy.
A functional magnetic resonance imaging study demonstrated a different cerebral processing of the feeling of nasal patency in the limbic system in ENS patients. Limbic activation may associate with unstable psychological condition in ENS patients. 24 Studies have also proposed successful managements by cognitive behavior therapy and a serotonin reuptake inhibitor in ENS patients with anxiety and depression. 25 , 26 Besides, a study also showed an association of hyperventilation syndrome and ENS, 10 while other studies suggested a multimodal approach that combined cognitive‐behavioral therapy (CBT) and surgical construction of tissues to address the psychological issue in ENS individuals carrying a significant psychological burden. 27 , 28 Current study further emphasized the importance of suicide thoughts identification in ENS patients, especially in cases of moderate‐to severe symptoms, including anxiety and depression. Screening for anxiety, depression and suicidal thoughts, collaboration with specialists in psychiatry and psychology, and planning care including both surgery and CBT by the patient's situation would be able to achieve optimal outcomes.
Several limitations in this study warrant consideration. First, this study evaluated ENS patients using four validated questionnaires; however, other potential factors that may contribute to the instability of these psychiatric symptoms and suicidal ideation were not comprehensively reviewed. Future studies collaborating with specialists in psychology and psychiatry are necessary to clarify our results. Second, patient‐reported measures are vulnerable to self‐reported biases such as variations in internal standards, priorities, or the interpretation of a given instrument. Third, there were only 62 patients with ENS including 23 patients with suicidal thoughts preoperatively, and the power calculated from the difference between the primary outcomes in the study groups was 73.7%. Besides, subgroup analysis such as the degree of depression was not allowed to stratify the ENS patients for a better understanding of the association between ENS, depression, and suicidal thoughts. Future large‐scale studies are necessary to validate our findings.
5. CONCLUSION
Suicidal thoughts are frequently identified in patients with ENS. ENS patients with suicidal thoughts experienced significantly more severe symptoms, impaired quality of life, and psychological burden. “Nose feels too open” was the item in ENS6Q that was significantly more severe in ENS patients with suicidal thoughts than those without. Recognizing individuals who may carry suicidal thoughts and provide appropriate psychological interventions is critical to prevent tragedy.
CONFLICT OF INTEREST
The authors declare no competing interests.
AUTHOR CONTRIBUTIONS
Ta‐Jen Lee and Chi‐Che Huang participated in the study design. Pei‐Wen Wu and Chien‐Chia Huang performed the data analysis and drafted the manuscript. Ta‐Jen Lee, Chi‐Che Huang, Cheng‐Chi Lee, and Po‐Hung Chang helped in the enrollment of participants and collection of clinical data. All authors participated in the scientific discussions and approved the final manuscript.
ACKNOWLEDGMENTS
The authors received research grants from the Ministry of Science and Technology (NMRPG3K0031 and NRRPG3L0101) and Chang Gung Memorial Hospital (CMRPG3K2321), Taiwan. The funding agency had no role in the study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Huang C‐C, Wu P‐W, Lee C‐C, Chang P‐H, Huang C‐C, Lee T‐J. Suicidal thoughts in patients with empty nose syndrome. Laryngoscope Investigative Otolaryngology. 2022;7(1):22‐28. doi: 10.1002/lio2.730
Chi‐Che Huang and Ta‐Jen Lee were contributed equally to this work.
Funding information Chang Gung Memorial Hospital, Grant/Award Number: CMRPG3K2321; Ministry of Science and Technology, Taiwan, Grant/Award Numbers: NMRPG3K0031, NRRPG3L0101
Contributor Information
Chi‐Che Huang, Email: hcc3110@cgmh.org.tw.
Ta‐Jen Lee, Email: entlee@cgmh.org.tw.
REFERENCES
- 1. Chhabra N, Houser SM. The diagnosis and management of empty nose syndrome. Otolaryngol Clin North Am. 2009;42:311‐330. [DOI] [PubMed] [Google Scholar]
- 2. Sozansky J, Houser SM. Pathophysiology of empty nose syndrome. Laryngoscope. 2015;125:70‐74. [DOI] [PubMed] [Google Scholar]
- 3. Zhao K, Blacker K, Luo Y, Bryant B, Jiang J. Perceiving nasal patency through mucosal cooling rather than air temperature or nasal resistance. PLoS One. 2011;6:e24618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Li C, Farag AA, Maza G, et al. Investigation of the abnormal nasal aerodynamics and trigeminal functions among empty nose syndrome patients. Int Forum Allergy Rhinol. 2018;8(3):444‐452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Konstantinidis I, Tsakiropoulou E, Chatziavramidis A, Ikonomidis C, Markou K. Intranasal trigeminal function in patients with empty nose syndrome. Laryngoscope. 2017;127(6):1263‐1267. [DOI] [PubMed] [Google Scholar]
- 6. Wu CL, Fu CH, Lee TJ. Distinct histopathology characteristics in empty nose syndrome. Laryngoscope. 2021;131(1):E14‐E18. [DOI] [PubMed] [Google Scholar]
- 7. Jiang C, Wong F, Chen K, Shi R. Assessment of surgical results in patients with empty nose syndrome using the 25‐item sino‐nasal outcome test evaluation. JAMA Otolaryngol Head Neck Surg. 2014;140:453‐458. [DOI] [PubMed] [Google Scholar]
- 8. Gill AS, Said M, Tollefson TT, Strong EB, Nayak JV, Steele TO. Patient‐reported outcome measures and provocative testing in the workup of empty nose syndrome‐advances in diagnosis: a systematic review. Am J Rhinol Allergy. 2020;34(1):134‐140. [DOI] [PubMed] [Google Scholar]
- 9. Manji J, Nayak JV, Thamboo A. The functional and psychological burden of empty nose syndrome. Int Forum Allergy Rhinol. 2018;8(6):707‐712. [DOI] [PubMed] [Google Scholar]
- 10. Mangin D, Bequignon E, Zerah‐Lancner F, et al. Investigating hyperventilation syndrome in patients suffering from empty nose syndrome. Laryngoscope. 2017;127(9):1983‐1988. [DOI] [PubMed] [Google Scholar]
- 11. Lee TJ, Fu CH, Wu CL, et al. Evaluation of depression and anxiety in empty nose syndrome after surgical treatment. Laryngoscope. 2016;126:1284‐1289. [DOI] [PubMed] [Google Scholar]
- 12. Huang CC, Wu PW, Fu CH, et al. What drives depression in empty nose syndrome? A Sinonasal Outcome Test‐25 subdomain analysis. Rhinology. 2019;57(6):469‐476. [DOI] [PubMed] [Google Scholar]
- 13. Kuan EC, Suh JD, Wang MB. Empty nose syndrome. Curr Allergy Asthma Rep. 2015;15(1):493. [DOI] [PubMed] [Google Scholar]
- 14. Lee TJ, Fu CH, Wu CL, et al. Surgical outcome for empty nose syndrome: impact of implantation site. Laryngoscope. 2018;128(3):554‐559. [DOI] [PubMed] [Google Scholar]
- 15. Tam YY, Lee TJ, Wu CC, et al. Clinical analysis of submucosal Medpor implantation for empty nose syndrome. Rhinology. 2014;52:35‐40. [DOI] [PubMed] [Google Scholar]
- 16. Huang CC, Wu PW, Fu CH, Huang CC, Chang PH, Lee TJ. Impact of psychologic burden on surgical outcome in empty nose syndrome. Laryngoscope. 2021;131(3):E694‐E701. [DOI] [PubMed] [Google Scholar]
- 17. Velasquez N, Thamboo A, Habib AR, Huang Z, Nayak JV. The Empty Nose Syndrome 6‐Item Questionnaire (ENS6Q): a validated 6‐item questionnaire as a diagnostic aid for empty nose syndrome patients. Int Forum Allergy Rhinol. 2017;7(1):64‐71. [DOI] [PubMed] [Google Scholar]
- 18. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory‐II. Psychological Corp; 1996. [Google Scholar]
- 19. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometirc properties. J Consult Clin Psychol. 1988;56:893‐897. [DOI] [PubMed] [Google Scholar]
- 20. Yeung A, Howarth S, Chan R, Sonawalla S, Nierenberg AA, Fava M. Use of the Chinese version of the Beck Depression Inventory for screening depression in primary care. J Nerv Ment Dis. 2002;190(2):94‐99. [DOI] [PubMed] [Google Scholar]
- 21. Kanjanawasee D, Campbell RG, Rimmer J, et al. Empty nose syndrome pathophysiology: a systematic review. Otolaryngol Head Neck Surg. 2021;19:1945998211052919. [DOI] [PubMed] [Google Scholar]
- 22. Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329‐336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thase ME. Depression and sleep: pathophysiology and treatment. Dialogues Clin Neurosci. 2006;8(2):217‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Freund W, Wunderlich AP, Stöcker T, Schmitz BL, Scheithauer MO. Empty nose syndrome: limbic system activation observed by functional magnetic resonance imaging. Laryngoscope. 2011;121:2019‐2025. [DOI] [PubMed] [Google Scholar]
- 25. Lemogne C, Consoli SM, Limosin F, Bonfils P. Treating empty nose syndrome as a somatic symptom disorder. Genl Hosp Psychiatry. 2015;37:273.e9‐273.e10. [DOI] [PubMed] [Google Scholar]
- 26. Leong SC. The clinical efficacy of surgical interventions for empty nose syndrome: a systematic review. Laryngoscope. 2015;125:1557‐1562. [DOI] [PubMed] [Google Scholar]
- 27. Gill AS, Said M, Tollefson TT, Steele TO. Update on empty nose syndrome: disease mechanisms, diagnostic tools, and treatment strategies. Curr Opin Otolaryngol Head Neck Surg. 2019;27(4):237‐242. [DOI] [PubMed] [Google Scholar]
- 28. Dholakia SS, Yang A, Kim D, et al. Long‐term outcomes of inferior meatus augmentation procedure to treat empty nose syndrome. Laryngoscope. 2021;131(11):E2736‐E2741. [DOI] [PubMed] [Google Scholar]


