Abstract
Background and aim:
The anxiolytic effects of music have been studied during the past twenty years in different medical therapies. The aim of this study is to evaluate the effect of music therapy on patients’ dental anxiety, salivary cortisol, heart rate, blood pressure and body temperature during dental treatment.
Methods:
In this randomized control study, 46 patients were randomly selected from the Urgent Care dental clinic who needed urgent endodontic treatment (endodontic access and pulp extirpation). Participants were divided into two groups: intervention group (N=23) which was exposed to slow rhythm melody music and had no lyrics throughout the entire procedure and a control group (N=23) who undergoes the same dental procedure without being exposed to music. Participants’ blood pressure, heart rate, body temperature and salivary cortisol were measured before and after the treatment for both groups.
Results:
Patients in the intervention group showed lower salivary cortisol, blood pressure, heart rate and body temperature compared to those in the control group, however, the differences did not reach to statistical significance.
Conclusion:
Despite the change in the dental anxiety and stress during treatment with music, the findings of this study could not establish evidence of the effect of music in reducing dental anxiety and lowering physiological stressors. Therefore, further studies with larger sample size may be needed. (www.actabiomedica.it)
Keywords: Music therapy, dental anxiety, salivary cortisol, heart rate, blood pressure, dental treatment, body temperature, ELISA
Introduction
The use of music therapy is a very old tradition, dating back to the classical world and the Middle Ages (1). In fact, Pythagoras, the sixth-century Greek philosopher and the founder of music therapy; believed that music has an overall positive influence on body as well as on psyche creating unique harmony between them. Nilsson further elaborated on Pythagoras’s concept and specified music criteria needed to obtain optimal results. He also highlighted that clinicians often have to prioritize physical care over the patient’s emotional, spiritual, and psychological needs (1, 2). However, clinically music can support such needs by creating an environment that stimulates and maintains relaxation, wellbeing, and comfort (3).
The importance of the sense of hearing is confirmed by the fact that it is developed before the sense of sight in embryonic stage and is the first functional sense in human life (4). Furthermore, the anxiolytic effects of music have been studied for the last 20 years during different medical treatments (surgical, cardiac, oncologic and other patients), which is a logical explanation of why music therapy is being excessively integrated in the medical and dental fields nowadays, as well as in the treatment of alcohol, tobacco and drug addictions (5). Music therapy is also used to improve self-acceptance; treat anxiety and depression in patients with multiple sclerosis (HH6). In addition, it has the ability to distract and block attention away from stressful stimuli including stressful background noise; it also diverts attention towards a pleasurable emotional state (7, 8, 9, 10, 11, 12). Furthermore, it can be used to reduce procedure time and the amount of sedation needed in patients undergoing colonoscopy (13).
The effect of music is not limited to certain procedures or gender; a systematic review of randomized controlled trials proved that music intervention reduced anxiety in female patients undergoing colposcopy, which usually causes high levels of anxiety and negative emotional responses in all female patients (14, 15). Dental anxiety in patients undergoing dental procedures remains one of the most frustrating challenges dentists face worldwide, with an estimated prevalence of 6–15% of the world’s adult population and a range of 5.7% and 19.5% in children (16). Numerous studies have been conducted to measure, analyze and understand this phenomenon more clearly (17, 18, 19).
Current anxiety theories, describes anxiety as an emotion which helps organisms defend against a variety of threats (20). In other terms, anxiety arises from a dysregulation of the body’s normal defensive response. Previous research on dental anxiety highlighted a number of factors that contribute to this phenomenon; with traumatic past dental experience, being at the top of a long list. Other factors include fear of feeling pain, fear of suffocation because of the altered management of salivation and swallowing, blood, wounds and finally, the use of sharp instruments (20). All of these problems highlighted the need for managing dental anxiety in clinical practice. Current methods include distraction techniques, psycho-therapeutic or pharmacological interventions, and cognitive therapy (21). Hence, the aim of this study is to evaluate the effect of music therapy on patients’ dental anxiety, salivary cortisol, heart rate, blood pressure, and body temperature during dental treatment as a destruction technique.
Material and Methods
In this randomized controlled study, forty-six patients were selected from the Urgent Care Dental Department at University of Sharjah Dental Hospital, Sharjah, United Arab Emirates. The patients were diagnosed and referred for urgent endodontic treatment and were randomly divided into two groups, one group was exposed to the music therapy (intervention group) throughout the entire endodontic procedure (N=23) and a control group that was not exposed to music therapy during the same dental procedure (N=23). Participants’ blood pressure, heart rate, and body temperature were measured for both groups. Saliva samples were taken in order to measure salivary cortisol levels before and after the dental treatment.
Patients’ inclusion criteria
Eligible participants were above 18 years of age and medically fit patients with no mental or physical disability. We excluded patients who were diabetic, hypertensive, pregnant, xerostomic or suffering from other systemic, chronic or endocrine diseases. Patients under permanent drug treatments such as antihistamines, antidepressants and anticholinergics were excluded as well. All patients gave their written consent for their participation in this study and for obtaining their saliva samples, blood pressure and body temperature before and after treatment and completion of a dental anxiety questionnaire. Ethical approval was obtained from the Research Ethics Committee at the University of Sharjah (REC-17-11-17-01-S).
Anxiety scoring
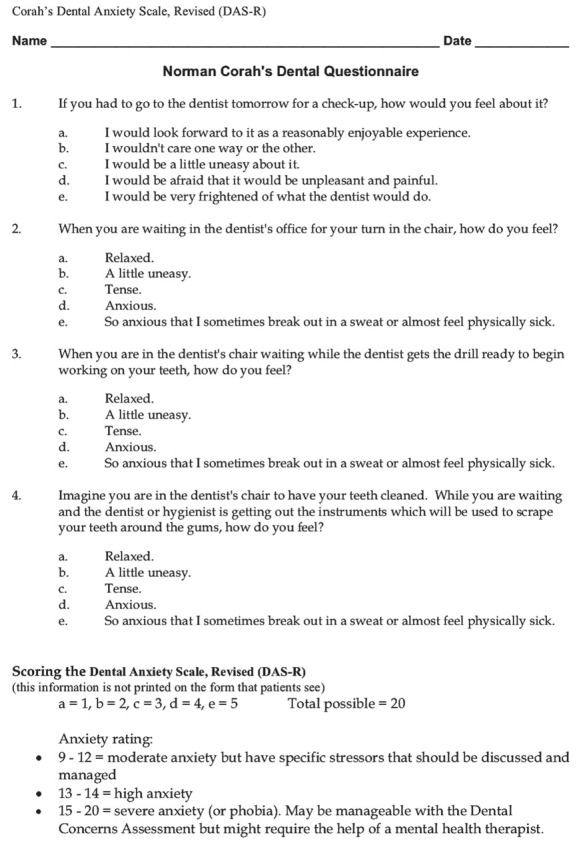
Prior to the experiment, participants of both groups were asked to fill Corah’s Dental Anxiety Scale (DAS) (Appendix 1), which is a reliable, valid, and useful scale for measuring dental anxiety, and available in two languages (English and Arabic) to assess their baseline measures of anxiety (17). The scale consists of a four simple question survey, with five possible answers. Questions can be completed in less than three minutes and focus on the patient’s subjective reactions about going to the dentist, waiting in the dentist’s office, and anticipation of drilling and scaling. In addition, the anxiety score is easily calculated according to the patient’s answers. The answers vary on a scale of “1” (not anxious) to “5” (extremely anxious) then the four scores are summed, with higher scores indicating higher levels of anxiety, with “4” being the lowest and “20” being the highest score for the total scale. A score between “9” and “12” indicates moderate anxiety, “13” and “14” indicates high anxiety and “15” to “20” indicates severe anxiety or phobia (18).
Demographic data and vital signs
Demographic data was collected from the patient about gender, age, education, occupation, native language and number of previous dental appointments at the University Hospital. All vital signs were recorded such as blood pressure, heart rate and body temperature in order to measure the anxiety before and after treatment for both groups by using Rossmax AX356 Automatic Blood Pressure Monitor and Rossmax RA600 Infrared Ear thermometer.
Saliva collection and storage
All patients were asked to provide unstimulated salivary samples of at least 5 ml before and after dental treatment in order to measure their salivary cortisol levels. Salivary cortisol is an expression of free plasma cortisol concentrations which freely expands in the saliva and remains steady compared to plasma cortisol (19).
To ensure accurate testing, participants did not have any food for at least 60 minutes before sample collection. Saliva samples were collected then placed in an ice container while being transferred to the freezer where they were stored in -20 degrees.
At the time of cortisol quantification, the saliva samples were centrifuged at 3000 rpm for 5 min. The concentration of cortisol was then quantified using a direct competitive enzyme-linked immunosorbent assay (ELISA) kit properly validated by (Salimetrics TM State College, USA).
Music specifications
Recruited participants were divided into two groups randomly via a random number generator. The control group continued their treatment regularly without any musical intervention. The intervention group was exposed throughout the entire procedure to slow rhythm and free of words music that produces physical and emotional relaxation. Disposable earphones were used for each patient and then discarded in the hospital general waste after every use.
Music used for this research was a regular soft music track, further analysis was done on the music track using an audio spectrum analyzer (academo.org) (Fig. 1A) to find out the frequency of the music in Khz. Furthermore, the frequency of our track was compared to the frequency of the sounds normally heard by the patient in the Urgent Care Clinic (Fig. 1B). We also tested the track using a virtual oscilloscope (academo.org) which revealed that the music track consisted of regular, equal and harmonious sound waves (Fig. 2) and has 136 Beats per minute (BPM).
Figure 1.
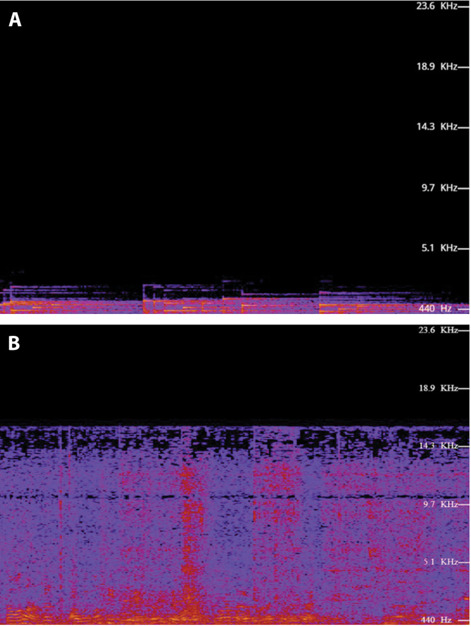
Sound frequency. A–Graph showing the frequency of the music track used in this research. The frequency of the track was between 440 Hz–5.1 KHz. B–Graph showing the frequency of the background sounds regularly heard in the Urgent Care department by a patient not wearing headphones. Frequency without of the background noise exceeded 143 KHz and ranged from 143–189 KHz.
Figure 2.
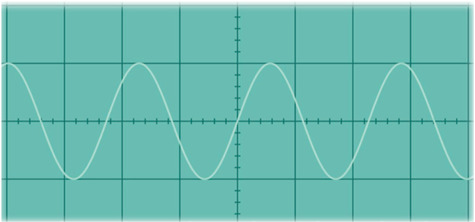
virtual oscilloscope of the music track used in this research showing regular, equal and harmonious sound waves.
Statistical Analysis
The data was analyzed by IBM SPSS version 25 (Statistical Package for the Social Sciences Inc., Chicago IL, USA). Categorical variables were expressed as frequencies and percentages and continuous variables were expressed as median (Interquartile range). Non-parametric Wilcoxon Test was used to compare the medians of related variables before and after intervention. The association of the anxiety levels with the sociodemographic parameters in the intervention and control group using Chi-square tests. Statistical significance levels were set at p < 0.05.
Results
The study included 46 participants divided into control (N=23) and intervention group (N=23). The sociodemographic characteristics of the participants was summarized in Table 1. The median age of these participants was 30 years, and the majority of them (82.6%) were males and Arabs (43.5%). When divided based on the education level, it showed that the majority of the participants completed only primary-high school (54.3%) and only (39.1%) completed their university degree, whilst a minority had no school education (6.5%).
Table 1.
Sociodemographic characteristics of the participants
| Variables | N (%) |
|---|---|
| Age (years) | 30 (13)* |
| Gender | |
| Males | 38 (82.6) |
| Females | 8 (17.4) |
| Education | |
| None | 3 (6.5) |
| Prim-High School | 25 (54.3) |
| University | 18 (39.1) |
| Visits to the dentists | |
| First time | 21 (45.7) |
| Previous visits | 25 (54.3) |
| Nationality | |
| Arab | 20 (43.5) |
| Non-Arab | 26 (56.5) |
| Consumption of caffeine, alcohol and NSAIDS | |
| Yes | 16 (34.8) |
| No | 30 (65.8) |
| Salivary cortisol collection time | |
| Am | 20 (43.5) |
| Pm | 26 (56.5) |
* Median (Interquartile range)
With regards to previous dental visits, more than half of the participants (54.3%) had previously visited the dentist whilst (45.7%) of them had their first dental visit during this study. Moreover, patients were asked about their consumption of caffeine, alcohol, nicotine and NSAID’S 12 hours prior to testing and (65.8%) did not consume any of the mentioned substances, whereas (34.8%) had consumed. More than half (56.6%) of the participants had salivary collection performed in the afternoon and (43.5%) in the morning.
All the measured physiological parameters; namely systolic and diastolic blood pressure, heart rate, body temperature and salivary cortisol, were less in intervention group, however, both control and intervention group did not show statistical difference before and after intervention Table 2. The association of the anxiety levels with the sociodemographic parameters in the intervention and control groups was demonstrated in Table 3. Almost four fifth (19/23; 82.6%) of the control group had mild anxiety compared to three fourth (17/23; 73.9%) of the intervention group, while 17.4% and 26.1% of the control and intervention group respectively, had moderate to severe anxiety and the level of anxiety is independent on the intervention (p>0.05). In both groups there was no statistically significant association between all tested variables and the anxiety level (p>0.05).
Table 2.
Comparison of different physiological parameters before and after intervention
| Physiological parameters | Control group (N=23) | Intervention group (N=23) | ||||
|---|---|---|---|---|---|---|
| Before | After | p value | Before | After | p value | |
| Systolic blood pressure | 130(28) | 132(24) | 0.66 | 129(18) | 126(28) | 0.25 |
| Diastolic blood pressure | 78(15) | 84(16) | 0.06 | 80(18) | 83(10) | 0.82 |
| Heart rate | 76(15) | 76(13) | 0.93 | 75(15) | 75(11) | 0.74 |
| Body temperature | 35.5(0.8) | 35.2(1.5) | 0.40 | 35.3(1.7) | 35.3(1.2) | 0.89 |
| Salivary cortisol | 0.345(0.47) | 0.269(0.35) | 0.19 | 0.393(0.27) | 0.290(0.39) | 0.19 |
*Median(IQR)
Table 3.
The association of the anxiety levels with the sociodemographic parameters in the intervention group using Chi-square tests
| Intervention Group | |||
|---|---|---|---|
| Anxiety level | |||
| Mild N=17 N(%) |
Moderate-Severe N=6 N(%) |
p value | |
| Gender | |||
| Male | 13(76.5) | 5 (83.3) | 0.72 |
| Female | 4 (23.5) | 1 (16.7) | |
| Education | |||
| Illiterate | 1(5.9) | 0(0) | 0.15 |
| Primary to Highschool | 12(70.6) | 2(33.3) | |
| University | 4(23.5) | 4(66.7) | |
| Nationality | |||
| Arab | 6(35.3) | 3(50) | 0.52 |
| Non – Arab | 11(64.7) | 3(50) | |
| Consumption of caffeine or painkillers | |||
| No | 6(35.3) | 1(16.7) | 0.39 |
| Yes | 11(64.7) | 5(83.3) | |
| Salivary cortisol collection time | |||
| AM | 7(41.2) | 2(33.3) | 0.73 |
| PM | 10(58.8) | 4(66.7) | |
Table 3B.
The association of the anxiety levels with the sociodemographic parameters in the control group using Chi-square tests
| Control Group | |||
|---|---|---|---|
| Anxiety level | |||
| Mild N= 19 N(%) |
Moderate –Severe N= 4 N(%) |
P value | |
| Gender | |||
| Male | 16(84.2) | 4(100) | 0.39 |
| Female | 3(15.8) | 0(0) | |
| Education | |||
| Illiterate | 2(10.5) | 0(0) | 0.35 |
| Primary to Highschool | 10(52.6) | 1(25) | |
| University | 7(36.8) | 3(75) | |
| Nationality | |||
| Arab | 10(52.6) | 1(25) | 0.31 |
| Non-Arab | 9(47.4) | 3(75) | |
| Consumption of caffeine or pain-killers | |||
| No | 9(47.4) | 0(0) | 0.07 |
| Yes | 10(52.6) | 4(100) | |
| Salivary cortisol collection time | |||
| AM | 9(47.4) | 2(50) | 0.92 |
| PM | 10(52.6) | 2(50) | |
Discussion
The aim of this study was to establish whether listening to calm, relaxing and lyric free music reduces dental anxiety among patients undergoing emergency endodontic treatment (endodontic access and pulp extirpation). Dental anxiety identified as a significant problem that interferes with dentists’ work and performance. More importantly, dental anxiety also plays a central role in the cycle of dental avoidance where anxious patients avoid dental care and therefore allow their oral health problems to deteriorate (22, 23, 24). Previous researches from various countries have focused on adult dental anxiety (25, 26, 27, 28, 29). Specifically, dental anxiety was found to be higher among patients in emergency clinics compared to others (30), which supports our choice of the urgent care department at the University Dental Hospital by using used Corah’s Dental anxiety scale. Woodmansey et al. assessed the anxiety level of patients using Corah Dental Anxiety Scale and reported that the majority of patients attending a university dental clinic had low to medium anxiety (31). While another study measured patient anxiety using (Modified Dental Anxiety Scale) from four different clinics; including a university dental school, private and public hospital clinics; their study reported high anxiety in only 13.6% of their sample (32). .
The majority of literature supports the hypothesis that music can positively affect patients’ feelings and physiological responses of anxiety (33, 34). Despite having several studies on music effect in medical/ surgical treatments, few studies exist that test music effect on dental treatments (34). No study examined the effect of music therapy in reducing dental anxiety in patients seeking urgent endodontic treatment/pulp extirpation (35).
We particularly chose music as it has been suggested to have positive effect on body and psyche by stimulating emotions, motivating, renewing memories and soothing tension (36). Furthermore, it is a painless, noninvasive procedure that has calming and anxiolytic effects. When compared to pharmacological and other treatments, music therapy does not require great investments in training or equipment which renders it being cost effective. Also, the fact that sound is not limited by time and space allowing music to reach the nervous system easily and influence brain waves thus changing physiological and psychological condition of an individual (37).
The timing of the music intervention is an important factor; if listening to music started prior to the onset of dental treatment, it may help prevent anxiety from building as the patient is awaiting the start of treatment (38). This was implemented in this study, since patients started listening to music prior to the placement of rubber dam and initiation of the treatment. Moreover, it is recommended that patients are instructed to actively focus on the music rather than merely listen to the music (38). Music therapy was effective in reducing self-reported anxiety but did not reduce self-reported stress or mood (39). Furthermore, some researches allowed participants to choose their own music believing that this will effectively aid in reducing anxiety, however our research used standardized music (39).
To understand how music can reduce anxiety, we need to understand how anxiety affects the body physiologically. Dental anxiety was reported to increase the sympathetic and parasympathetic nervous system activities (40). Overstimulation of sympathetic nerves will then be followed by an increase in noradrenaline secretion causing an increase in blood pressure, heart rate, and muscle contractility. Activation of the autonomic nervous system (ANS) causes the release of epinephrine and norepinephrine from the adrenal medulla. Upon activation of the hypothalamic-pituitary- adrenal axis, cortisol gets secreted to all body fluids, including saliva. It was demonstrated that cortisol levels in the saliva have been shown to be higher in patients undergoing wisdom teeth extractions and prior to urgent dental care (41). Moreover, Saliva samples were collected a few minutes after the stressful dental stimulus because cortisol enters the saliva by passive diffusion, and the time lag between changes in plasma and salivary cortisol levels is very short, 1–2 minutes (19). No salivary stimulant was used, since it was evident that obtaining salivary cortisol levels does not depend on salivary flow rate (35).
Blocking the external environment is important, since stressful background noise is often part of dentists’ working environment. Specifically, certain stimuli have been directly linked to increased apprehension resulting in dental anxiety. This includes: metallic sound of instruments and drill noises, sharp instruments, rubber dam and conversations of staff members, which can all lead to exaggerated responses and anxiety (44).
All the measured physiological parameters; in both control and intervention group, did not show statistical difference (p>0.05) before and after intervention. This does not coincide with Gupta et al. who reported gradual decrease in heart rate throughout minor oral surgery procedures. Furthermore, Gupta et al. took several readings of heart rate at several intervals (45). However, we took two readings only which is before initiation of the treatment and at the end of the treatment. On the other hand, Kim et al. reported that there were no significant differences between groups in blood pressure; however, the music-treated group showed a significantly smaller change in heart rate than the control group (46).
Body temperature can be affected by stress and those with dental anxiety may be oversensitive to heat or cold environment which may contribute to further agitation and anxiety making any temperature changes noticeable. This study took place in a relatively cold environment (dental hospital) and our results revealed no statistically significant difference between music and body temperature, (P>0.05).
Although cortisol is a useful indicator of long-term stress, heart rate is a far more useful indicator of immediate fear, anxiety and stress (42, 43). Previous studies linked changes in cortisol levels to many variables such as the education level. Educated people were expected to experience less anxiety, since educated patients would expect what they are going to go through while uneducated patients will have no expectation thus resulting in increased fear and anxiety (1). However, we found no significant difference between educated and uneducated patients regarding anxiety.
Previous studies reported that smoking increases the salivary cortisol levels (47, 48). No differences were observed in our study between smokers and nonsmokers. Caffeine is another substance that can increase the cortisol production in the human body (49). According to our results, no significant difference was seen between those who recently consumed caffeine and those who did not. Women in general were found to have significantly higher levels of morning cortisol than men (50), however we did not have enough female participants in order to accurately document this relationship. Since one of the origins of dental anxiety is the fear of the unknown (51), we compared between those who experienced dental treatment and those who did not, and our results showed no significant differences between them. Also, the number of previous appointments in the same environment did not reduce dental anxiety.
Conclusion
Results from this study showed that music therapy may help in reducing salivary cortisol, blood pressure, heart rate and body temperature among patients in the intervention group who exposed to slow rhythm music compared to control group treated without exposing to music, however, this reduction was not statistically significant. This study also showed no relationship between gender, education, consumption of painkillers and caffeine, number of previous appointments and anxiety. More studies are required with larger sample groups to further investigate the effect of musical therapy on reducing dental anxiety and stress.
Acknowledgments:
The authors would like to thank Dr. Farah Al-Marzooq and Dr. Mohamed El-Kishawi for their help and support during this study.
Appendix: The Corah’s Dental anxiety scale
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Nilsson U. The anxiety-and pain-reducing effects of music interventions: a systematic review. AORN journal. 2008;87(4):780–807. doi: 10.1016/j.aorn.2007.09.013. [DOI] [PubMed] [Google Scholar]
- Packyanathan JS, Lakshmanan R, Jayashri P. Effect of music therapy on anxiety levels on patients undergoing dental extractions. J Family Med Prim Care. 2019;8:3854–60. doi: 10.4103/jfmpc.jfmpc_789_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamioka H, Tsutani K, Yamada M, et al. Effectiveness of music therapy: a summary of systematic reviews based on randomized controlled trials of music interventions. Patient preference and adherence. 2014;8:727–54. doi: 10.2147/PPA.S61340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gfeller K. Music therapy in the treatment of medical conditions. In: Davis WB, Gfeller KE, Thaut MH, editors. An Introduction to Music Therapy and Practice. Dubuque, IA: WC Brown; 1992. pp. 234–50. [Google Scholar]
- Petot T, Bouscaren N, Maillard O, Huiart L, Boukerrou M, Reynaud D. Comparing the effects of self-selected music versus predetermined music on patient anxiety prior to gynaecological surgery: a study protocol for a randomised controlled trial. PMC - trials. 2019;20(20) doi: 10.1186/s13063-018-3093-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostermann T, Schmid W. Music therapy in the treatment of multiple sclerosis: a comprehensive literature review. Expert Rev Neurother. 2006;6(4):469–477. doi: 10.1586/14737175.6.4.469. [DOI] [PubMed] [Google Scholar]
- Facco E, Zanette G. The Odyssey of Dental Anxiety: From Prehistory to the Present. A Narrative Review. Front Psychol. 2017;8:1155. doi: 10.3389/fpsyg.2017.01155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulina T, et al. The Effect of Music Intervention on Dental Anxiety During Dental Extraction Procedure. Open Dent J. 2017;11:565–572. doi: 10.2174/1874210601711010565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dionne R. A, et al. Assessing the need for anesthesia and sedation in the general population. J Am Dent Assoc. 1998;129(2):167–173. doi: 10.14219/jada.archive.1998.0173. [DOI] [PubMed] [Google Scholar]
- Klingberg G, Broberg A. G. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007;17(6):391–406. doi: 10.1111/j.1365-263X.2007.00872.x. [DOI] [PubMed] [Google Scholar]
- Carr C, et al. A systematic review of music therapy practice and outcomes with acute adult psychiatric in-patients. PLoS One. 2013;8(8):e70252. doi: 10.1371/journal.pone.0070252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moola S, et al. Effectiveness of music interventions on dental anxiety in paediatric and adult patients: a systematic review. JBI Libr Syst Rev. 2011;9(18):588–630. doi: 10.11124/01938924-201109180-00001. [DOI] [PubMed] [Google Scholar]
- Tam W. W, et al. Effect of music on procedure time and sedation during colonoscopy: a meta-analysis. World J Gastroenterol. 2008;14(34):5336–5343. doi: 10.3748/wjg.14.5336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galaal K, et al. Interventions for reducing anxiety in women undergoing colposcopy. Cochrane Database Syst Rev. 2011;12:Cd006013. doi: 10.1002/14651858.CD006013.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell M. Patient anxiety and modern elective surgery: a literature review. J Clin Nurse. 2003;12(6):806–815. doi: 10.1046/j.1365-2702.2003.00812.x. [DOI] [PubMed] [Google Scholar]
- Maggirias, John & Locker, David. Fiver-Year inicidence of dental anxiety in an adult population. Community dental health. 2002;19:173–9. [PubMed] [Google Scholar]
- Corah N. L. Development of a dental anxiety scale. J Dent Res. 1969;48(4):596. doi: 10.1177/00220345690480041801. [DOI] [PubMed] [Google Scholar]
- Corah N. L, Gale E. N, Illig S. J. Assessment of a dental anxiety scale. The Journal of the American Dental Association. 1978;97(5):816–819. doi: 10.14219/jada.archive.1978.0394. [DOI] [PubMed] [Google Scholar]
- Mejía-Rubalcava C, et al. Changes induced by music therapy to physiologic parameters in patients with dental anxiety. Complement Ther Clin Practice. 2015;21(4):282–286. doi: 10.1016/j.ctcp.2015.10.005. [DOI] [PubMed] [Google Scholar]
- Marks I. F, Nesse R.M. Fear and fitness: An evolutionary analysis of anxiety disorders. Ethology and Sociobiology. 1994;15(5):247–261. [Google Scholar]
- Appukuttan D. P. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clinical, cosmetic and investigational dentistry. 2016;8:35–50. doi: 10.2147/CCIDE.S63626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armfield JM, Spencer AJ, Stewart JF. Dental fear in Australia: who's afraid of the dentist? Aust Dent J. 2006;51(1):78–85. doi: 10.1111/j.1834-7819.2006.tb00405.x. [DOI] [PubMed] [Google Scholar]
- Thomson WM, Stewart JF, Carter KD, Spencer AJ. Dental anxiety among Australians. Int Dent J. 1996;46(4):320–4. [PubMed] [Google Scholar]
- Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007;7:1. doi: 10.1186/1472-6831-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson WM, Locker D, Poulton R. Incidence of dental anxiety in young adults in relation to dental treatment experience. Community Dent Oral Epidemiol. 2000;28:289–94. doi: 10.1034/j.1600-0528.2000.280407.x. [DOI] [PubMed] [Google Scholar]
- McGrath C, Bedi R. The association between dental anxiety and oral health-related quality of life in Britain. Community Dent Oral Epidemiol. 2004;32:67–72. doi: 10.1111/j.1600-0528.2004.00119.x. [DOI] [PubMed] [Google Scholar]
- Hofer D, Thoma MV, Schmidlin PR, Attin T, Ehlert U, Nater UM. Pre-treatment anxiety in a dental hygiene recall population: a cross-sectional pilot study. BMC Oral Health. 2016;16:43–7. doi: 10.1186/s12903-016-0198-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagglin C, Hakeberg M, Ahlqwist M, Sullivan M, Berggren U. Factors associated with dental anxiety and attendance in middle-aged and elderly women. Community Dent Oral Epidemiol. 2000;28:451–60. doi: 10.1034/j.1600-0528.2000.028006451.x. [DOI] [PubMed] [Google Scholar]
- Saatchi M, Abtahi M, Mohammadi G, Mirdamadi M, Sadaat Binandeh E. The prevalence of dental anxiety and fear in patients referred to Isfahan dental school, Iran. Dental Research Journal. 2015;2(3):248–53. [PMC free article] [PubMed] [Google Scholar]
- Kaakko T, Getz T, Martin MD. Dental anxiety among new patients attending a dental school emergency clinic. J Dent Educ. 1999;63(10):748–52. [PubMed] [Google Scholar]
- Woodmansey KF. The prevalence of dental anxiety in patients of a university dental clinic. J Am College Health. 2005;54(1):59–61. doi: 10.3200/JACH.54.1.59-61. [DOI] [PubMed] [Google Scholar]
- Ofori MA, Adu-Ababio F, Nyako EA, Ndanu TA. Prevalence of dental fear and anxiety amongst patients in selected dental clinics in Ghana. Health Educ J. 2009;68(2):130–9. [Google Scholar]
- Singh D, Samadi F. Stress reduction through audio distraction in anxious paediatric dental patients: an adjunctive clinical study. Int J Clin Pediatr Dent. 2014;7:149–152. doi: 10.5005/jp-journals-10005-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Standley J M. Music research in medical/dental treatment: Meta-analysis and clinical applications. J Music Ther. 1986;23:56–122. doi: 10.1093/jmt/23.2.56. [DOI] [PubMed] [Google Scholar]
- Corah N L, Gale E N. Comparative study. Relaxation and Musical programming as a means of reducing psychological stress during dental procedures. J Am Dent Assoc. 1981;103:232–234. doi: 10.14219/jada.archive.1981.0245. [DOI] [PubMed] [Google Scholar]
- Nater U. M, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology. 2009;34(4):486–496. doi: 10.1016/j.psyneuen.2009.01.014. [DOI] [PubMed] [Google Scholar]
- Guzzetta C. Music therapy: nursing the music of the soul. In: Campbell D, editor. Music Physician for Times to Come. Wheaton, IL: Quest Books; 1991. pp. 146–66. [Google Scholar]
- Ogba F. N, Ede MO, Onyishi CN, et al. Effectiveness of music therapy with relaxation technique on stress management as measured by perceived stress scale. Medicine (Baltimore) 2019;98(15):e15107. doi: 10.1097/MD.0000000000015107. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Raghav K, Van Wijk AJ, Abdullah F, Islam MN, Bernatchez M, De Jongh A. Efficacy of virtual reality exposure therapy for treatment of dental phobia: a randomized control trial. BMC Oral Health. 2016;16:25. doi: 10.1186/s12903-016-0186-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadock BJ, Sadock VA, Williams L, Ott CA. Book Review: Kaplan & Sadock's Pocket Handbook of Clinical Psychiatry. 2010;44(10):1684. [Google Scholar]
- Miller CS, Dembo JB, Falace DA, Kaplan AL. Salivary cortisol response to dental treatment of varying stress. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79(4):436–441. doi: 10.1016/s1079-2104(05)80123-4. [DOI] [PubMed] [Google Scholar]
- Nater UM, Rohleder N, Gaab J, Berger S, Jud A, Kirschbaum C, et al. Human salivary alpha-amylase reactivity in a psychosocial stress paradigm. Int J Psychophysiol. 2005;55(3):333–342. doi: 10.1016/j.ijpsycho.2004.09.009. [DOI] [PubMed] [Google Scholar]
- AlMaummar M, AlThabit HO, Pani S. The impact of dental treatment and age on salivary cortisol and alpha-amylase levels of patients with varying degrees of dental anxiety. BMC Oral Health. 2019;19(1):211. doi: 10.1186/s12903-019-0901-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggirias J, Locker D. Psychological factors and perceptions of pain associated with dental treatment. Community Dent Oral Epidemiol. 2002;30:151–9. doi: 10.1034/j.1600-0528.2002.300209.x. [DOI] [PubMed] [Google Scholar]
- Gupta A, Ahmed B. Experience of listening to music on patient anxiety during minor oral surgery procedures: a pilot study. Br Dent J. 2020;228:89–92. doi: 10.1038/s41415-019-1162-1. [DOI] [PubMed] [Google Scholar]
- Kim S M, Kim Y K, Myoung H. Musical intervention reduces patients' anxiety in surgical extraction of an impacted mandibular third molar. J Oral Maxillofac Surg. 2011;69:1036–1045. doi: 10.1016/j.joms.2010.02.045. [DOI] [PubMed] [Google Scholar]
- Wong JA, Pickworth WB, Waters AJ, al'Absi M, Leventhal AM. Cortisol levels decrease after acute tobacco abstinence in regular smokers. Hum Psychopharmacol. 2014;29(2):152–162. doi: 10.1002/hup.2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kankaanpää R, Auvinen J, Rantavuori K, Jokelainen J, Karppinen J, Lahti S. Pressure pain sensitivity is associated with dental fear in adults in middle age: Findings from the Northern Finland 1966 birth cohort study. Community dentistry and oral epidemiology. 2019;47(3):193–200. doi: 10.1111/cdoe.12443. [DOI] [PubMed] [Google Scholar]
- Ping J, Lei Y, Liu L, Wang T, Feng H, Wang H. Inheritable stimulatory effects of caffeine on steroidogenic acute regulatory protein expression and cortisol production in human adrenocortical cells. Chemico-biological interactions. 2012;195(1):68–75. doi: 10.1016/j.cbi.2011.11.001. [DOI] [PubMed] [Google Scholar]
- Larsson CA, Gullberg B, Råstam L, Lindblad U. Salivary cortisol differs with age and sex and shows inverse associations with WHR in Swedish women: a cross-sectional study. BMC Endocr Disord. 2009;9:16. doi: 10.1186/1472-6823-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorka S. M, Lieberman L, Shankman S. A, Phan K. L. Startle potentiation to uncertain threat as a psychophysiological indicator of fear-based psychopathology: An examination across multiple internalizing disorders. Journal of abnormal psychology. 2017;126(1):8–18. doi: 10.1037/abn0000233. [DOI] [PMC free article] [PubMed] [Google Scholar]


