Abstract
The role of environmental factors in influencing health status is well documented. Heavy metals, polycyclic aromatic hydrocarbons (PAHs), polychlorinated biphenyls, dioxins, pesticides, ultrafine particles, produced by human activities put a strain on the body’s entire defense system. Therefore, together with public health measures, evidence-based individual resilience measures are necessary to mitigate cancer risk under environmental stress and to prevent reproductive dysfunction and non-communicable diseases; this is especially relevant for workers occupationally exposed to pollutants and/or populations residing in highly polluted areas. The Mediterranean diet is characterized by a high intake of fruits and vegetables rich in flavonoids, that can promote the elimination of pollutants in tissues and fluids and/or mitigate their effects through different mechanisms. In this review, we collected evidence from pre-clinical and clinical studies showing that the impairment of male fertility and gonadal development, as well as cancers of reproductive system, due to the exposure of organic and inorganic pollutants, may be counteracted by flavonoids.
Keywords: pollution, flavonoids, cancer, male infertility, Mediterranean diet, heavy metals, bisphenols, polycyclic aromatic hydrocarbons, dioxins, phthalates
1. Introduction
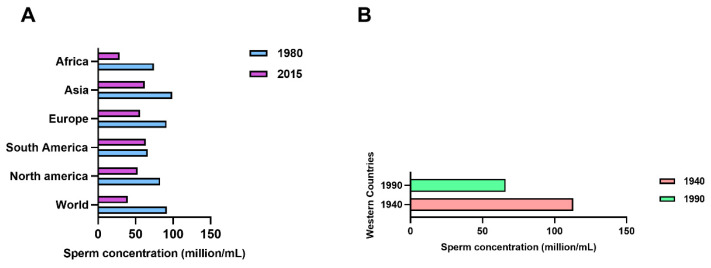
In recent decades, the role of environmental factors in influencing population health has become increasingly evident, so that chemical and physical pollutants are now considered the most important public health threat, whose effects, including transgenerational ones, come to be well reported in the scientific literature [1]. The World Health Organization (WHO) estimates that around a quarter of diseases are due to prolonged exposure to environmental pollutants [2] and air pollution is among the first risk factors for cardiovascular, chronic degenerative diseases, premature deaths and reproductive dysfunctions [3,4]. Noticeably, many outdoor and indoor pollutants carry out their action as endocrine disruptors [5] altering inter-cellular signaling and also inducing oxidative stress [6]. Excess of radical oxygen species (ROS) not balanced by the presence of reductive activity represents a central molecular mechanism of damage for various macromolecules (DNA, proteins, lipids) which, if not properly repaired, can cause inflammatory processes up to neoplastic transformation [7]. Indeed, the imbalance of antioxidant defenses and detoxification processes provides a logical explanation for the occurrence of oxidative stress-related diseases in humans [8]; including the increased susceptibility to pollutants [9]. The reproductive system appears to be particularly sensitive to environmental stresses and an increasing amount of in vitro and in vivo toxicological studies are performed on this system. In fact, besides its obvious functional importance, the reproductive system can also represent a sentinel to environmental stresses; the epidemiological and clinical data available today, in particular, on male infertility, seem to confirm this sensitivity [10,11]. A strong trend of decline, already described for sperm concentration from 113 × 106/mL in 1940 to 66 × 106/mL in 1990 [12], is observed for testosterone levels [13]. Sperm decline has been also reported in Africa, China, India, Brasil from 1980 to 2015 [14,15] (Figure 1).
Figure 1.
Decrease rates of sperm concentration worldwide. Sperm concentration declines in several areas of the world from 1980 to 2015 (A), and from 1940 to 1990 (B).
The incidence of male infertility has increased steadily in many countries [16,17]. The changes in sperm production correspond precisely to the increased introduction of chemicals in the living environment, especially after 1940, and were initially thought to be due solely to maternal exposure to environmental estrogens [18]; based on the current knowledge, especially from experimental data, these effects appear to be due to different types of endocrine disrupting chemicals (EDCs) [18]. EDCs can act through several mechanisms, targeting either nuclear receptors for steroid hormones (i.e., estrogen and androgen receptors), other nuclear receptors (i.e., peroxisome proliferator-activated receptors), steroidogenic enzymatic cascades, FSH/LH balance and at central and/or peripheric levels. Noticeably, the developmental phase is most sensitive: EDC exposure is involved the “testicular dysgenesis syndrome” with poor semen quality and increased risk of congenital anomalies such as hypospadias and cryptorchidism as well as of testicular cancer. Adult exposure to EDC (e.g., in highly polluted environments) may also affect spermatogenesis and male fertility. Also, EDC exposure might synergize with other conditions inducing impaired sperm production, including systemic diseases and genetic factors such as karyotype anomalies and Y chromosome microdeletions [18,19,20]. Indeed, the extensive use of EDCs appears to be involved not only in the fall in sperm count but also in the increased incidence of hypospadias, cryptorchidism and testicular malignancies [20]. The incidence of primary testicular tumors (TC), especially testicular seminomas has increased worldwide and the percentage over the past decades has risen approximately 1.2% per year [21,22,23]. TC generally affects young and middle-aged men; indeed, it is the most common type of cancer among males aged 15–44 years in developed countries [24]. Noticeably, over the past four decades, the incidence of this type of cancer has increased especially in wealthy, industrialized countries [25,26,27] and has started to grow in countries moving toward higher levels of development [27]. The increasing trend of TC has raised attention towards its epidemiological features and the genetic and non-genetic factors involved in the etiopathogenesis [28,29,30,31,32]. The causes of increased incidence of this type of cancer include cryptorchidism, occurring in 2–9% of boys born at term and considered to be linked to an almost 9-fold increased risk of TC, along with hypospadias; indeed, TC, cryptorchidism, and hypospadias are hallmark components of the “testicular dysgenesis syndrome” [20,33,34]. The first event in TC occurs prenatally as the presence of foci of poorly differentiated gonocytes in seminiferous tubules. Postnatally, TC development and progression is associated with allele polymorphisms of a number of transcription factors (i.e., GATA4 and GATA1), genes (i.e., PRDM14, DMRT1, SALL4, TEX14 WDR73, PMF1, CENPE, and PCNT) and receptors (i.e., CAG/GGC androgen receptor polymorphism), which are implicated in the maturation specification and differentiation of the postnatal testis [35,36,37,38]. Even though, compared to tumors in other districts, testicular cancer is still more treatable [39], both the cancer and its treatment are associated with several complications, particularly sexual dysfunction and infertility [40,41]. These, together with the expected growth in the coming decades, highlight the public health and socio-economic impacts of testicular cancers [42,43]. Nonetheless, environmental factors including heavy metals, polycyclic aromatic hydrocarbons (PAHs), polychlorinated biphenyls (PCBs), dioxins, pesticides, ultrafine particles, produced by human activities put a strain on the body’s entire defense system which struggles to metabolize and eliminate toxic compounds. Together with public health measures, evidence-based individual resilience measures are therefore necessary to mitigate health risks under conditions of environmental stress and to prevent noncommunicable diseases (NCDs); this holds true especially for workers occupationally exposed to pollutants and/or population residing in highly polluted areas. Mediterranean diet is a foremost model for nutritionally rich and balanced diets [44]. It is characterized by high intake of fruits and vegetables, rich in detoxifying and antioxidant substances, hence it is particularly rich of flavonoids. Flavonoids promote the elimination of pollutants in tissues and fluids and/or mitigate their effects through different mechanisms. In this review, the properties of flavonoids will be explored in the context of the Mediterranean diet model highlighting their role in mitigating the long-term effects of pollutants on human health with particular attention to reproductive system cancer and male infertility.
2. Mediterranean Diet
It is well-known, that diet can significantly influence the population’s risk profile, both at primary and secondary level of prevention. Several types of diets have been brought to public attention, but the one that has gained the most interest is no doubt the Mediterranean diet. The concept of Mediterranean diet originates from 60’s, when Ancel Keys first coined this term based on the results of an epidemiological study which showed that the populations (Italy and Greece) that faced the Mediterranean Sea presented a lower incidence of cardiovascular diseases and cancer than other populations [44]. After this famous study, other researches have corroborated these results, and the Mediterranean diet with its specific foods has been diffused all over the world as a model of a potential healthy diet. At present, the global scientific milieu highlights the Mediterranean-like diet pattern as the ideal dietary profile to maintain the health status and to reduce cancer mortality and in general the incidence of the major NCDs [45,46,47].
The Mediterranean diet is characterized by low consumption of meat, intake of vegetable oils instead of animal fats as sources of lipids, moderate amounts of red wine and significant amounts of fresh fruits and vegetables. Plant polyphenols have attracted considerable interest in the scientific communities in recent times for their health-promoting properties. In fact, many clinical studies have indicated health benefits attributable to the presence of significant quantities of these molecules, even though, in some cases, contradictory results have been reported, which highlights the need for further investigations. Therefore, recent research has sought to provide insights into the mechanisms of action of these compounds to help decipher the complex relationships between plant polyphenols and cellular homeostatic systems, including metabolic and redox balance, proteostasis, and the inflammatory response, establishing an increasingly strong molecular basis for the beneficial effects of these molecules. The underlying biochemical and molecular events include anti-inflammatory, antioxidant and anti-atherosclerotic mechanisms, as well as the epigenetic and gut-microbiota modulations pointed out by more recent studies [48]. Overall, the currently available data are providing a rationale for the possible use of natural polyphenols as nutraceuticals to counteract aging and combat many associated diseases [49]. In fact, various phytochemical compounds found in plant foods can prevent or counteract the harmful effects of environmental pollutants, through a number of mechanisms including reactive oxygen species (ROS) scavenging, chelation of toxic metals, anti-inflammation, epigenetic up-regulation of detoxifying genes or enzymes, and other [50,51,52,53,54,55,56]. Some systematic reviews found that diets rich in fish, shellfish and seafood, poultry, cereals, vegetables and fruits, low-fat dairy and skim milk were positively associated with sperm quality parameters [57,58].
A substantial body of research evidence from observational studies worldwide suggests that the diets’ models consistent with those promoted for the prevention of heart disease and other chronic conditions can be advantageous for male fertility as well [59]. Meanwhile, the evidence on the association between dietary patterns and male fertility is far from complete; nevertheless, several indications have emerged. The increased intake of omega-3 fatty acids, both as supplements or from foods (whether from nuts or fish) seems to positively affect spermatogenesis. Integration with antioxidants and nutrients implicated in the mono-carbon metabolism pathway (folate, vitamin B12, zinc) also seems a beneficial. In addition, a study conducted by Salas-Huetos et al., 2018 showed that supplementation of a conventional “Western” diet with walnuts, hazelnuts and almonds, present also in Mediterranean diet, improves key sperm quality parameters among healthy men of reproductive age, potentially by a reduction in sperm DNA fragmentation. These results support the potential benefits of some nutrients contained in nuts for sperm quality [60]. In a 24-week study on adult rats, Dominguez-Vias et al. [61] showed that a diet enriched with virgin olive oil, a major element of Mediterranean diet, increased the activity of dipeptidyl peptidase IV, an enzyme involved in glucose metabolism regulation as well as detoxification processes; in the testicular r tissue compared to a butter-enriched diet; this latter, contrary to olive oil enrichment, elicited a number of markers of saturated fat intake [61]. Bioactive substances in vegetable foods also deserve attention. Resveratrol (RES), abundant in grape, is a well-known cytoprotective substance with beneficial effects on diverse cell types thanks to its anti-inflammatory, anti-oxidant and anti-cancer properties. In vitro, it increased total and progressive sperm motility, restored chromatin compactness and decreased sperm lipoperoxidation, along with mitochondrial superoxide anion levels in benzopyrene-exposed spermatozoa. These biological activities deserve to be further investigated in vivo, for possible benefits in people with impaired fertility due to environmental factors [62]. A recent randomized clinical trial on healthy young males in highly polluted area of Italy has demonstrated positive effects of the Mediterranean diet and regular physical activity, on semen quality [63].
Although several studies indicate a favorable effect of the adherence to Mediterranean diet on semen parameters, few data evaluating the influence of diet on couple’s fertility are reported, including in couples attempting conception with assisted reproductive technology (ART). Thus, the impact of Mediterranean on couple fertility and ART success is a topic for further studies [64,65,66,67].
In addition, “organic” (i.e., cultivated based on agroecological criteria) foods, due to a higher content in bioactive compounds in comparison to conventional ones, has been suggested as an additional safeguard for counteracting the effects of environmental pollutants [68]. In this direction, the typical foods of the Mediterranean diet, when they are organically cultivated, should have a significantly reduced content of pesticides [69,70], whereas they are expected to contain higher concentrations of their natural occurring beneficial phytochemicals including polyphenols [71], flavonoids [72], carotenoids [73] and macro- and micro-nutrients such as vitamin C, iron, magnesium, phosphorus and omega-3 fatty acid [74]. Therefore, the environmentally friendly cultivation procedures endorsed by agroecology can maintain a higher content of bioactive compounds, compared to conventional foods. Indeed, several studies report that the consumption of organic foods may improve fertility, in addition to reducing other reproductive (pre-eclampsia, obesity in pregnancy) and other non-reproductive health disorders (overweight, eczema in children, some cancers, diabetes etc.). Therefore, rather than a specific effect, improved reproductive health may reflect a better health status associated with a healthier dietary style, higher intakes of nutrients, antioxidants and other bioactive compounds, as well as lower intakes of undesirable substances (i.e., nitrates and cadmium from fertilizers, pesticides, fertilizers, pollutants and their metabolites) [68,71,75,76,77,78,79,80,81]. Therefore, cultivation methods influence the potential of foods to counteract the oxidative stress and epigenetic alterations induced by environmental contaminants [51,52,53,54,55,56,57,82,83,84,85,86].
Communities living in polluted areas are recognized to experience a higher incidence of cancer, NCDs and male infertility. Therefore, in parallel to regulatory actions, evidence-based lifestyle intervention models should be designed in order to mitigate the impact of environmental pollutants on human health [63,87,88,89,90,91].
Spermatozoa are very sensitive to oxidative stress induced by environmental toxins so that the richness of antioxidants of Mediterranean diet nutrients has protective role especially on morphology, motility and sperm DNA [57,92,93,94]. Semen quality is also a potential susceptibility indicator to SARS-CoV-2 insults in polluted areas [14], and very recently it has been demonstrated that air pollution and COVID-19 could represent a possible dangerous synergy for male fertility [95].
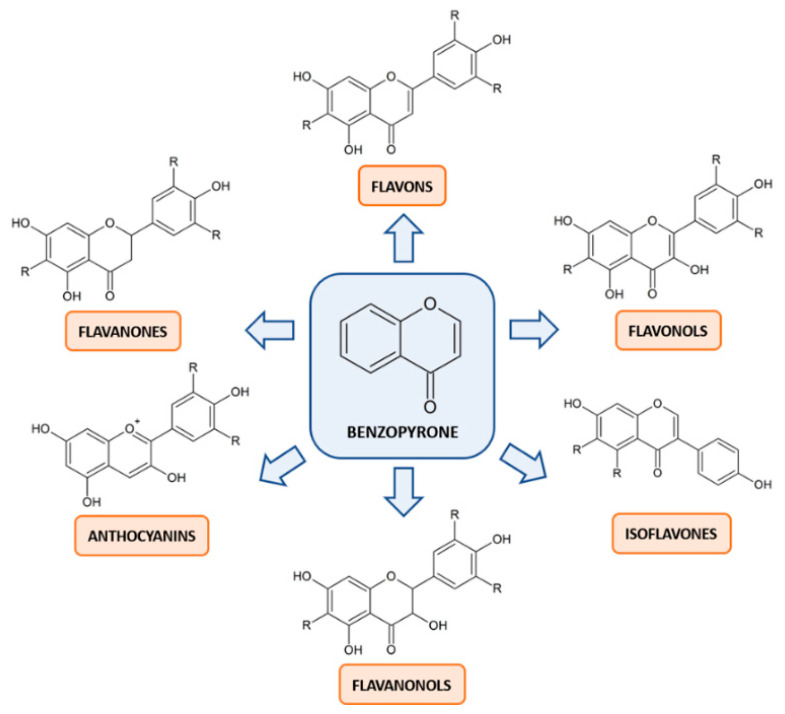
3. Flavonoids: Mechanisms of Action in Cancer
Flavonoids are the most prevalent and well-studied polyphenols in human diet. The common scaffold within this class of compounds is the benzo-pyrone moiety, which can be variously substituted. Based on the degree of oxidation or unsaturation, flavonoids can be classified into six major subclasses: flavonols, flavones, flavanones, flavanonols, anthocyanins and isoflavones (Figure 2). They are more frequently found as glycosides, although it is likely to find them as aglycone.
Figure 2.
Basic structures of the six classes of flavonoids. The lead compound benzopyrone can be variously substituted to form the derivative structures of flavonols, flavones, flavanones, flavanonols, anthocyanins and isoflavones. The hydroxyl groups can be linked to monosaccharides, in case of glycosides, or methoxylated. The radicals, expressed as R, can be either methyl or methoxy groups, depending on the structure.
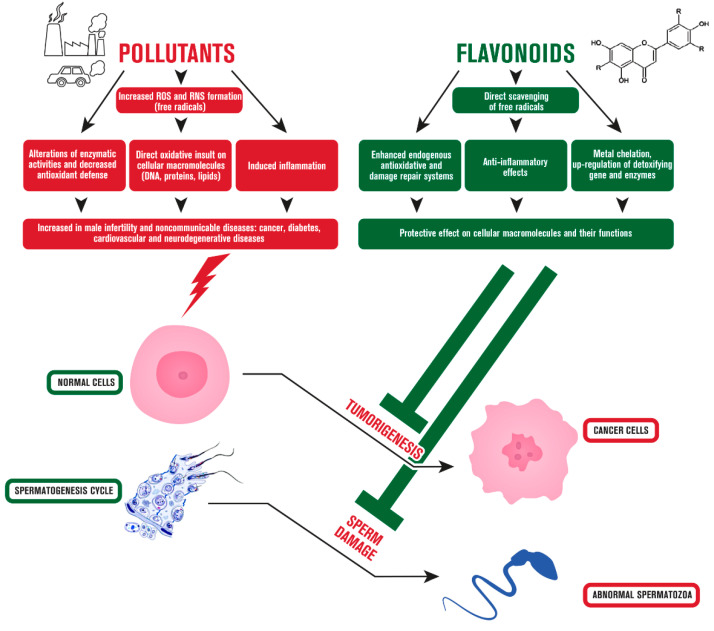
Citrus fruits, tea, and red wine are among their primary nutritional sources. Numerous studies have revealed that eating polyphenol-rich foods on a daily basis may benefit a wide range of human pathologies, including those characterized by an abnormal inflammatory and oxidant status, such as infections, autoimmune and neurodegenerative diseases, along with cancer [96,97,98,99,100,101,102]. These interesting properties are also exploited in clinical settings, mainly in the aromatherapy [103,104]. Regarding cancer, which is characterized by an uncontrolled cell proliferation and a disrupted cell cycle, leading to aberrant cells that infiltrate and metastasize to other regions of the body, flavonoid act by a wide plethora of mechanisms [105,106,107,108]. Moreover, it was documented that these compounds are able to counteract not only genetic causes of cancer development [109], but also external causes, such as pollution, smoking or radiation [110]. In particular, the ability of flavonoids to inhibit tumorigenesis was attributed primarily to their undoubted antioxidant activity, which is capable of preventing and scavenging the formation of ROS and reactive nitrogen species (RNS), known players in the toxicity of many pollutants [111]. Flavonoids also act as free radical scavengers mainly via chelating metallic ions, that consequently catalyze the generation of ROS and RNS [112,113,114]. These are the leading causes of many other conditions other than cancer, such as inflammation [115,116,117], and flavonoids target different receptors to modulate intracellular signaling pathways involved also in this process like SIRT1, nuclear factor kappa B (NF-κB), mitogen activated protein kinases (MAPKs) and cyclooxygenase-2 (COX-2) [118,119,120,121]. Flavonoids were shown to act also via immune cell regulation, suppressing chemokines and cytokines [122,123], which are known to be implied in cancer progression as well as in its spreading [124]. In this regard, flavonoids were shown to actively inhibit factors implied in metastasization of cancer via altering adhesion molecules such as metalloproteinases and other epithelial-mesenchymal transition markers [125,126,127]. Angiogenesis is another relevant process involved in cancer progression and migration, since it is crucial for the proper nourishment of the tumor microenvironment, hence the acknowledged role of flavonoid of inhibiting pivotal factors of this process, such as VEGF or EGFR expression, is one of the paths followed by these compounds to counteract cancer formation [128,129]. Among the numerous processes involved in tumorigenesis, the escape from apoptosis, which is a type of controlled cell death that is generally triggered by a number of signal transduction pathways and pro-apoptotic proteins, is acknowledged to represent one of the first characteristics acquired by cells undergoing promotion [130]. Flavonoids are able to interfere with the apoptotic machinery via hampering the activity of caspases and Bcl-2 family members [131,132]. Parallelly, flavonoids can restore also impaired autophagy in tumor cells due to the activation of beclin-1 and LC3, marker of early and late stages of autophagosome formation, respectively [133]. Moreover, the altered progression through cell cycle is another crucial element characterizing tumor development, and flavonoid were widely investigated in this field, finding their ability to modulate expression of several isoforms of cyclins, involved in each phase of cell cycle [134]. Finally, the intake of flavonoids through a varied and balanced diet, such as the Mediterranean diet, does not lead to any appreciable risk of undesirable effects, contrary to high intakes through supplements, where potential endocrine effects justify caution [135]. The effects of flavonoids against cancer development are summarized in Figure 3.
Figure 3.
Effects of flavonoids against environmental pollutant-induced carcinogenesis and male infertility. Physiological processes of normal cells can be altered by pollutants leading to cancer and sperm cell damage. Flavonoids can protect cellular functions from environmental insults via targeting a wide plethora of mechanisms.
4. Flavonoids: Mechanisms of Action in Male Infertility
Flavonoids have been extensively explored for the treatment of male reproductive dysfunctions. The observed favorable effects can be ascribable to a combination of biological mechanisms, for example their antioxidant, anti-inflammatory, immunostimulant, anti-apoptotic, anticarcinogenic activities [136]. Moreover, flavonoids are amphipathic molecules that can penetrate the lipid bilayer of membranes, thus providing possible protection for the entire spermatozoa and acrosome membrane. In this way, flavonoids prevent oxidative damage and guarantee the acrosome reaction of spermatozoa necessary for fertilization [137,138].
Rutin and quercetin, along with epigallocatechin, were shown to improve motility, plasma and acrosomal membrane integrity, mitochondrial activity, anti-oxidase activities, and lower intracellular ROS concentration of frozen sperm [139,140,141,142]. Among these, rutin was shown to improve the kinematic parameters of post-thawing sperm, as well as its fertilizing characteristics, prompting an increase in cleavage rates and blastocyst rate [142]. Instead, the main intercellular target of quercetin appears to be the mitochondria. Studies have demonstrated its protective and regulatory action of crucial mitochondrial processes, including electron transport chain and oxidative phosphorylation, which may affect the metabolism and performance of male gametes [140].
In male rats, quercetin reduces the endocrine and testicular alterations induced by the heavy metal cadmium [143,144]. Quercetin, apigenin, EGCG, and luteolin are also capable of increasing gene expressions of steroidogenic acute regulatory protein (StAR), cytochrome P450 11A (CYP11A), CYP17A, 17-beta-hydroxy steroid dehydrogenase (17-β-HSD) and 3-beta-hydroxy steroid dehydrogenase (3-β-HSD), useful for restoring Leydig cell function and testosterone secretion [145].
Oxidative stress is indicated as an essential contributor to apoptosis, DNA damage, lipid peroxidation, and decreased sperm motility [146]. Rutin and quercetin are able to attenuate ROS accumulation and malondialdehyde (MDA) production by improving antioxidant enzyme activity [142,147]. Moreover, quercetin eliminates the toxic effects of hydrogen peroxide (H2O2) on motility, amount of MDA and nitric oxide (NO), along with increasing viability and total antioxidant capacity (TAC) [148]. Effects of flavonoids on apoptosis have also been shown. In particular, rutin can inhibit cell apoptosis in H2O2-induced Leydig cells [149], while hesperetin lowers the number of TUNEL-positive germ cells in the testis [150]. In addition, rutin, hesperetin, and morin were noted to decrease apoptosis in testis by significantly increasing protein levels of Bcl-2 (B-cell leukemia/lymphoma 2), and decreased protein levels of BCL2-associated X (Bax) and cysteine aspartic acid-specific protease 3 (caspase 3) [149,150]. A relationship between Sertoli cells (Sc), blood-testis barrier (BTB), and flavonoids also exits. In this context, luteolin protects SCs and BTB integrity by up-regulating the expression of several antioxidant genes and ameliorating the protein expression of ZO-1, occludin, claudin-11, and Cx43 [151]. In addition, it was shown that icariin may affect spermatogenesis via regulating the claudin-11 mRNA expression in SCs [152]. Finally, investigations have established the important role that 3′,5′-cyclic adenosine monophosphate (cAMP)/ cAMP-dependent protein kinase-A (PKA) signaling pathway plays in the regulation of testosterone secretion. In this regard, another effect of quercetin, apigenin and luteolin is to inhibit cyclooxygenase-2 (COX-2)-dependent signal transduction, which has been found to enhance cAMP/PKA-dependent StAR gene expression and steroidogenesis in Leydig cells [145,153]. Overall, flavonoids show a number of biological mechanisms relevant to the protection of male fertility in in vitro and in vivo studies. The available evidence supports the design of studies on humans in areas polluted with EDC and other reproductive toxicants, in order to investigate the efficacy and safety of increasing flavonoid intake within a balanced and nutritionally rich dietary pattern, such as the Mediterranean diet.
Figure 3 summarizes the main effects of flavonoids that may counteract the pollutants affecting male.
5. Heavy Metals
Heavy metals are a naturally occurring part of the Earth’s crust, but anthropogenic and industrial activities have caused drastic environmental pollutions in distinct areas. The non-biodegradability of heavy metals causes them to persist in the environment. Thus, they can enter the food chain through cultivated plants, and eventually can accumulate in the human body through biomagnification. Given the toxicity of heavy metals, human health and ecosystems are threatened by their contamination. Heavy metals, however, are of utility in industrial areas such as alloying, smelting, and commercial product manufacturing. Of course, this contributes to increased exposure to heavy metals as waste from industrial processes represents a significant source of environmental contamination and subsequent accumulation in the human body.
Almost all heavy metals are severely toxic as carcinogens. For example, arsenic, cadmium, chromium, and nickel are classified as Group 1 carcinogens by the International Agency for Research on Cancer, and are used commercially [154]. Living organisms easily come into contact with various heavy metals such as cadmium, cobalt, methylmercury, manganese, and arsenic, and it has been shown in many research studies that a strong link exists between the environmental contaminants and human health. In addition, several metals also have negative effects on the reproductive health of organisms [155,156,157,158,159,160,161,162]. Heavy metals such as lead (Pb), mercury (Hg) and cadmium (Cd) can influence the endocrine system, disrupting embryonal programming and gonadal development in utero [163]. Chromium (Cr), Cd, iron (Fe), nickel (Ni), Pb, and copper can enhance ROS [164], which can impair DNA in the male germ line and increase health risk in offspring. Some studies have shown that the risk of hypospadias and cryptorchidism is significantly increased by paternal exposure to heavy metals [165]. This study, and also another [166], proposed that the risk of hypospadias may be elevated following maternal exposure to heavy metals. In addition, a recent study provides little evidence for the association of parental exposures to heavy metals and testicular germ cell cancer in progeny except in cases of high paternal chromium exposure [164].
The reported results of many research suggest that increased consumption of fruits and vegetables or certain dietary supplements can substantially enhance the protection against many heavy metals. Over the past decade, dietary factors have proven to reduce the toxicity of environmental pollutants and effect prevention against adverse chronic degenerative diseases and cancer in humans, and a growing scientific body of evidence has suggested that flavonoids, thanks to their antioxidant and metal chelating properties, are involved in preventing or decreasing the damage caused by heavy metals.
5.1. Cadmium (Cd)
The best documented explanation for the toxicity related to Cd is oxidative stress. Cd also acts as an endocrine disruptor, particularly of the reproductive hormones [163,167]. Cd mimics the chemical state of divalent Zn; therefore, it has the potential to interfere with the site of Zn binding to DNA. Furthermore, this metal mimicking endogenous estrogen, produces an increased risk of ovarian and breast cancer and also disrupts the ovarian steroidogenic pathway, progesterone and testosterone production [168,169]. Several studies reveal that testis is a susceptible target of toxicity from cadmium. In fact, cadmium exposure can cause germ cell apoptosis and decreased daily sperm production, which may account for the decline in male fertility [170].
Regarding Cd, Xia Li et al. highlighted how flavonoids can alleviate Cd toxicity [171]. Anthocyanins have been widely applied to nutritional intervention of Cd toxicity. Flavonoids having similar structure demonstrate analogous mechanisms of action in protecting the body against Cd poisoning. These mechanisms in Cd-induced diseases mainly include elimination of ROS, reduction of lipid peroxide production, increased activity of enzymes related to oxidative stress, reduction of free Cd2+ content, reduction of DNA damage and cell apoptosis, inhibition of inflammation and fibrosis, and influence of metal ions in vivo. In addition, experimental studies have shown that fenugreek seed powder attenuates cadmium-induced testicular damage and hepatotoxicity in male rats [172,173]. These authors, in fact, showed that flavonoids restored the depletion of antioxidants as they antagonized the effect of Cd on antioxidant enzyme activity or increased GSH content, improving the antioxidant capacity of the body. In parallel, a flavonoid rich-extract of bergamot juice counteracted both testicular and kidney damage induced by Cd exposure in rats [174,175]. Another research asserts that flavonoids reduced the chromosomal aberration regarding to structure and number of spermatocytes due to their detoxification action that protect protein and DNA from free radicals, and hence from cancer [173]. In a similar manner, catechin hydrate exhibited protective antigenotoxic and anti-immunotoxic roles via decreasing the fragmentation of DNA and by suppressing the expression of the genes related to apoptosis [176]. Quercetin is among the most important flavonoid found in vegetables and fruits; it shows anti-inflammatory, anti-hypertensive, vasodilator, anti-obesity, anti-hypercholesterolemic, and anti-atherosclerotic effects [177], as well as for its protective against testicular carcinogenesis [178]. The protective effects of quercetin can be explained by its ability to chelate metal ions and form stable complexes given its three potential bidentate binding sites (α-hydroxycarbonyl, β-hydroxycarbonyl or catechol) [179], along with its inhibitory effects on apoptosis, cell migration, differentiation and proliferation, oxidative balance, and inflammation [180].
As regards Cd-induced-pro-oxidant action, the protective effect of dietary quercetin in testicular germ cells was documented by several research [181]. In male mice, Cd significantly decreased testicular antioxidant system, including decreases in the level of GSH, SOD and GSH-Px activity. In addition, Cd exposure resulted in increased H2O2 production and lipid peroxidation in the testes and caused germ cell apoptosis by increasing the expression of the proapoptotic proteins Bax and caspase-3 and decreased the expression of the antiapoptotic protein Bcl-XL. Notably, the administration of quercetin significantly attenuated these effects [182]. In another work, it was showed that Cd accumulated in testes, leading to oxidative stress and autophagy and that quercetin decreased cadmium toxicity by reducing oxidative stress and inhibiting autophagy [183]. In a similar way, quercetin effectively inhibited apoptosis in chicken granulosa cells exposed to Cd by regulating the inhibition of antiapoptotic protein Bcl-2 and X-linked inhibitor of apoptosis protein (XIAP) and activated caspase-3 [184]. Quercetin is highly present in onions, beans and fruits, such as apples, apricots, cherries and grapes [185]; the studies on Cd and quercetin support that a rich, varied and predominantly plant-based diet, such as the Mediterranean diet, can provide bioactive substance mitigating the effects of environmental exposures.
5.2. Mercury (Hg)
Plant polyphenols, which have well recognized antioxidant properties, represent very effective agents counteracting oxidative environmental stressors, including Hg. The exposure to the organic Hg form, as methylmercury (MeHg), results in the generation of reactive species that can lead to oxidative damage of macromolecules, especially DNA. Furthermore, MeHg associates with endogenous biomolecules containing thiol groups, such as glutathione. The growing occurrence of food-borne Hg is a matter of concern, given the numerous serious adverse downstream effects, ranging from kidney, cardiovascular disease and reproductive problems, whereas MeHg specifically features as a developmental neurotoxic. In addition, infertile individuals exhibited higher Hg levels in blood, hair and urine in comparison with fertile subjects. Hg exposure prompted sperm DNA damage and abnormal sperm morphology and motility. Moreover, Hg levels were correlated with a greater incidence of menstrual and hormonal dysfunction and enhanced cases of adverse reproductive outcomes [186]. Several papers report the biochemical bases for pharmacological utilization of Fejioa sellowiana polyphenol-rich functional food in the prevention and suppression of Hg-related health disorders [187,188]. Moreover, diverse studies have also reported the possibility of reducing mercury toxicity with flavonoid intake. Among the variety of dietary flavonoids, the beneficial role of chrysin (CR), which is found mainly in passion fruit, honey, and propolis in preventing Hg-induced alterations in both human erythrocytes and neuroblastoma cells has been investigated [189]. Finally, a number of investigations have revealed the role of olive oil polyphenols in preventing Hg toxicity [190].
5.3. Inorganic Arsenic (iAs)
The toxic effects of iAs on gonadal glands have been long studied through animal models, showing that iAs can be accumulated in gonadal glands and induce an inhibitory effect on gonadal development [191]. In addition, iAs affects one or more sex hormones and induces inhibition of ovarian steroidogenesis, reproductive disorders, testicular steroidogenic function, and spermatogenesis [192]. Similar toxic effects have been observed in humans. In fact, iAs has been seen to cause a variety of reproductive problems through disruption of the gonadal endocrine system. Specifically, iAs has been shown to have a detrimental effect on reproduction and development in human reducing the quantity and quality of human sperm [193]. Moreover, iAs has been linked to the onset of various forms of cancer in human, including that affecting the breast, which is the most relevant [194]. To date, no report on the direct effects of flavonoids against iAs-induced tumorigenesis is present, although it has been claimed that flavan-3-ols, flavone, flavonol, flavanone, and anthocyanidin are positively associated with urinary dimethylarsinic acid excretion in a clinical trial performed on 1037 Mexican women living in a highly polluted area [195]. This supports the hypothesis that flavonoids may hamper iAs-toxicity and hence tumorigenesis, by increasing its excretion.
6. Bisphenols
Endocrine disrupting chemicals (EDCs) are hormone-like agents found in the environment that induce adverse health effects by altering the endocrine system of vertebrate animals, including humans. Specifically, xenoestrogens are believed to be involved in development, reproduction, and malignant diseases by mimicking the natural hormone 17β-estradiol (E2) and interfering with endogenous endocrine regulation at specific times, such as during fetal growth. Several organochlorine pesticides-polychlorinated biphenyls (PCBs), phthalates, and bisphenol A (BPA)-used in the chemical industry have been identified as estrogenic EDCs. BPA is currently severely restricted as an EDC in the European Union, but this compound has been used from the 1950s in industrial materials, food packaging, dental sealants, and personal care products. All persons have exposure to BPA via skin, inhalation, and through the digestive system. Exposure to substances with potential for endocrine disruptive effects are continually increasing and, in recent decades, are considered the primary factor in the rising incidence of testicular cancer. Because of its metabolic and endocrine interference and its link to various human diseases including cancer, diabetes, obesity, reproductive problems, BPA is subject of intense research [196]. BPA is known to disrupt the endocrine pathways since it is a partial estrogen agonist [197] and has anti-androgenic and anti-thyroid activities [198]. For several decades, the impact of low doses of bisphenols on male reproduction has been controversial. While some investigations have reported that the low dose administration of bisphenols does not affect the vital alteration of reproductive qualities, other studies have revealed varying degrees of damage they trigger on male fertility. However, equal exposure to the same disruptor is not uniquely associated with the same phenotype of testicular dysgenesis syndrome, and this highlights the role of genetic background in establishing susceptibility to genito-urinary disorders, in general, and testicular cancer in particular [198]. Furthermore, fetal and perinatal exposure to BPA in rodents has been reported to affect the brain, mammary gland, and reproductive tract, including hormone-dependent cancer [199,200]. In addition, BPA is also capable of triggering a non-genomic action in pancreatic islets, endothelial and pituitary cells, and mammary cancer cells starting fast responses at low doses [201,202]. Flavonoids have been explored for their role against BPA toxicity. In particular, a very recent study investigated if flavonoids from Cuscuta chinensis (CCF) could be used as dietary supplements to reverse BPA-induced epigenetic disturbances by analyzing the molecular mechanisms linked to impairment of testicular development by BPA. The results displayed that in comparison with BPA group, CCFs were able to markedly increase the serum content of testosterone (T), estradiol (E2), the transcript levels of DNA methyltransferase 3A (Dnmt3A), Dnmt3B and that of estrogen receptor alpha (ERα). These findings suggested that CCFs could lower the levels of ERα and H19/Igf2 gene methylation by suppressing DNA methyltransferase (DNMT) expression, thus decreasing reproductive hormone and receptor levels in adult males, and thus mitigating the adverse effect of BPA on testicular development in male mice [203]. Several flavonoids, including daidzein, genistein, luteolin, chrysin, flavone, and naringenin, have been shown to exhibit anti-estrogenic activity, preventing BPA from proliferating in MCF-7 breast cancer cells and causing malignant consequences [204]. In breast cancer cell lines, ER has been found to be antagonized by naringenin, inhibiting their proliferation and supporting the role of flavonoids in preventing BPA carcinogenesis and reproductive system damage.
Pharmacological inhibition of ERK1/2 could be considered as a target to mitigate the effects of bisphenols in testicular cells. A recent review has provided an overview to understand how oxidative stress induction may contribute to the harmful reproductive impacts induced by BPA exposure [205]. The several studies reviewed show that reproductive organs in males are more vulnerable to BPA exposure than those in females. Males may be more susceptible for several reasons. First, because there are gender differences in glutathione levels, considering its importance to the detoxification process (lower availability of glutathione in males). Also, there is greater capacity for sulfate-based detoxification in females. In addition, there is a greater inflammatory response in male reproductive organs to consider. Finally, reduced vulnerability to oxidative stress in female organs has been reported. Growing evidence shows that a wide variety of BPA doses (in vivo and in vitro or human exposure) promotes ROS generation and redox balance alteration, by leading to mitochondrial dysfunction and cell signaling pathway modulation related to oxidative stress. In addition, it should also be kept in mind that oxidative stress induced by BPA may operate in a dependent or independent manner from its endocrine and metabolic deregulatory properties and that all this may produce marked reproductive effects in prenatal, perinatal and postnatal exposure or in adulthood. Finally, the effect of BPA can be most severe when exposure is combined with other risk factors, such as a poor diet, metabolic impairments, and comorbidities [205]. The great antioxidant potential of flavonoids may also function in the body’s defense against BPA damage, including cancer.
7. Polycyclic Aromatic Hydrocarbons
Air pollution is known to contain various toxic substances, gases, particulates, polycyclic aromatic hydrocarbons (PAHs), toxic metals, etc. Some of them could affect the reproductive process and sperm quality by decreasing one or more sperm quality parameters i.e., sperm morphology, concentration, motility, sperm DNA damage, up to testicular cancer. The impact could be related to the concentration of pollutants and the duration of exposure [206]. PAHs, formed by pyrogenic, petrogenic and biogenic (biological) processes, are defined as persistent organic pollutants (POPs); two of them, 7, 12-dimethylbenzo[a]anthracene (DMBA) and benzo[a]pyrene (B[a]P), are among the most widely studied carcinogenic PAHs for their negative impact on the environment, human and animal health. In particular, the International Agency for Research on Cancer (IARC) defined PAHs as “probable” or “possible human carcinogens”, while benzo [a] pyrene has been reclassified in group 1 as a “human carcinogen” [207]. Scientific studies have shown that PAHs compounds undergo transformations through various metabolic reactions that occur in the body, before genuinely carcinogenic types of molecules are produced. It is precisely during these reactions that PAHs can transform into electrophilic intermediates capable of reacting with biological molecules, including DNA [6].
The toxicity of PAHs is related to their physical/chemical properties. PAHs are soluble in most organic solvents, are very lipophilic and have a high ability to adhere to organic material. Within 24 h, they then begin to degrade through a sequence of radical reactions, or undergo degradation by photolysis. The toxic effects occur through the formation of reactive intermediates and the activation of a particular aryl hydrocarbon receptor (AhR) [208] that regulates the expression of a series of genes. In addition to regulating the production of enzymes involved in metabolic processes, AhR also has a role in regulating the immune system, stem cells, cell differentiation and proliferation, apoptosis, carcinogenesis and drug metabolism [209]. Other evidence on infertile populations suggested a negative association between semen quality, testicular cancer, and PAH levels [210]. Moreover, male infertility can be induced by PAH by affecting sperm motility, chromatin integrity, and increased oxidative stress [211]. However, considering the human exposure at PAHs in the environment, the impact of these compounds on testicular cancer and the related mechanisms involved in toxicity could be further investigated.
As many environmental pollutants, PAHs promote the excessive production of both ROS and RNS [212]. Therefore, the maintenance of antioxidants is important in the prevention of the damage caused by environmental pollutants, such as PAHs.
Matzkin et al. [213], reported how anti-inflammatory and antioxidant compounds could exert a beneficial role in the improvement of physio-pathological state of the aged male gonad [214]. Similarly, a dimer of epicatechin from the endophytic fungus Curvularia australiensis reverted the tumorigenic effect of B[a]P exposure in female rats on induced cervical cancer by reducing oxidative stress markers and pro-inflammatory ones, thus ameliorating lesion histopathology [215]. Other authors [216] investigated the molecular mechanisms associated with the cytoprotective effect of quercetin and its metabolites against benzo[a]pyrene (B[a]P), suggesting the involvement of other mechanisms beyond the antioxidant activity. In particular, the reduction of B[a]P-induced cytotoxicity by quercetin and isorhamnetin occurs through a decrease of BPDE-DNA adducts and intracellular B[a]P and its metabolite, increasing the xenobiotic detoxification metabolism. Along the same line, an anthocyanin-rich pool from grape proved to enhance detoxification capacity of MCF-7 cells, blocking carcinogen-DNA adduct formation as well as ROS [217]. Moreover, eupatorin-5-methyl ether, a flavonoid present in several medicinal plants, hampered B[a]P stimulating effects in MCF-7 cancer cells, via inducing p21, JNK and p-JNK expression [218].
8. Dioxins
Dioxins are POPs that are largely produced by industrial combustion processes such as waste incineration, the manufacturing of chlorophenols and chlorophenoxy herbicides, metal processing, and free chlorine bleaching of paper pulp. Dioxins and similar compounds all act by interacting with AhR, albeit with different potency. The cumulative effects of dioxins are assessed using as parameter the AhR-binding potency of each congener relative to that of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD), the most known member of the dioxin-like class [219]. The role of dioxins on the onset of several types of cancer and the relative increase of mortality has been widely established by the numerous cohort and case-control studies [220]. Moreover, human exposure to dioxins has been linked to decreased semen quality, menorrhagia, and hampered male characteristic development more than female counterpart [221]. As already mentioned, these noxious effects are claimed to be ascribed to the interaction of TCDD to the AhR, protein which translocates into the nucleus to promote the transcription of several factors involved in survival, invasive and migrative potential of cancer cells [222]. Moreover, AhR is implied in reproductive function in both sexes, being widely spread in ovaries and testes. Indeed, it is known that testicular functions (i.e., spermatogenesis and sperm motility), and hence male fertility, are affected by activation of AHR induced by environmental toxicants [223]. Therefore, AhR has been studied as an interesting target of pollutant-induced cancers and, specifically, natural products, among which flavonoids, have seized the attention of the scientific community in these regards [224]. In particular, the isoflavone genistein from soy was showed to hamper TCDD-dependent downregulation and methylation of BRCA-1, whose alteration is known to play a pivotal role in the onset of breast cancer, along with decreasing levels of DNMT-1 and cyclin D1 in MCF-7 cells, proving the role of genistein in counteracting ER (estrogen receptor) α-positive breast cancer cells via antagonizing AhR [225]. These effects elicited by genistein were seen by the same group also in triple-negative breast cancer cells [226]. The flavanone hesperetin, mainly found in Citrus fruits, was proved to inhibit AhR translocation induced by TCDD exposure in MCF-7 cells, along with reducing gene expression of different cytochrome P450 isoforms and other xenobiotic metabolizing enzymes [227]. Kaempferol, a tetrahydroxyflavone present in many plant species, inhibited the TCDD-induced expression of both phase I and phase II drug-metabolizing enzymes (i.e., CYP1A1, NQO1, HO-1, GSTP1) in hepatocarcinoma HepG2 cells, targeting AhR and Nrf2 pathways, and its combination with luteolin proved to bring even stronger effects [228]. Kaempferol and luteolin, along with fisetin, apigenin and naringenin hampered the TCDD-induced up-regulation of CYP1A1 and UGT1A1 in colon carcinoma Caco2 cells, although other flavonoids, such as quercetin and morin, increased the effect of TCDD. These effects were explained by the different binding modes of these compounds to AhR, since specific residues interacted with antagonists (i.e., apigenin) and others with agonists (i.e., quercetin), while other residues were in common with both species [229]. These reports highlight the ability of dietary flavonoids to counteract AhR activation mediated by dioxin-like compounds like TCDD. Nevertheless, other members of this family proved to possess TCDD-like effects on AhR, thus caution and more evidence are required for a risk-to-benefit assessment of nutraceutical or pharmacological uses.
9. Phthalates
Phthalates, or phthalic acid diesters, are often employed to improve the flexibility, pliability, and elasticity of otherwise hard polymers. Given their chemo-physical characteristics, they are used in a wide range of industrial and consumer items, including toys, paints, adhesives, personal-care products, and a variety of medical equipment. However, due to their EDC properties, several phthalates in EUROPE are undergoing severe restrictions. In particular, the main phthalates with EDC properties present in food contact materials are di-butylphthalate (DBP), butyl-benzyl-phthalate (BBP), bis(2-ethylhexyl) phthalate (DEHP), di-isononylphthalate (DINP) [230]. DEHP and other phthalates with EDC properties have been linked to changes in puberty, development of testicular dysgenesis syndrome, cancer, and reproductive problems in both men and women. This because phthalates can influence the release of hypothalamic, pituitary, and peripheral hormones, along with interfere with nuclear and membrane receptors, intracellular signaling pathways, and affect gene expression involved with reproduction [231]. In particular, it has been shown that a chemokine secreted by immune cells, namely Chemokine (C-C motif) ligand 5 (CCL5) and also known as RANTES, is involved in the crosstalk to maintain the correct environment for optimal spermatogenesis [232]. Interestingly, the link between toxicity by environmental pollutants, such as dioxins, and impairment of male fertility has been ascribed also to a decrease of CCL5 expression, which experimentally induced a transitory decline in sperm reserves in the testes of TCDD-exposed rats [233]. In this field, a flavonoid present mainly in Citrus fruits, namely didymin, reverted the cancerous effects induced by several phthalate esters (i.e., BBP, DBP, DEHP) in an in vitro experimental model targeting the CCL5 pathway [234]. In particular, it was shown that MDA-MB-231 breast cancer cells co-cultured with monocyte-derived dendritic cells and exposed to phthalate esters displayed higher rates of progression, invasion and migration due to CCL5 release. Didymin was able to deplete its secretion, thus hampering the metastatic and proliferative activities of cancer cells and proving its role in cancer prevention via targeting CCL5 pathway, and possibly protect against phthalate-induced infertility. Notably, flavonoid consumption, specifically anthocyanidins and flavan-3-ols, has been also proved to be positively associated with reduced breast cancer-risk in a population-based case-control study (233 cases and 221 controls) performed in a highly polluted area of Mexico [235].
10. Conclusions
The unceasing development of anthropic activities brings consequently an ever-increasing level of air and soil pollutants, known to hamper human, animal and plant health. In order to increase one self’s defenses, secondary metabolites from edible plants may represent valuable allies, when assumed within a varied and well-balanced diet, such as the internationally recognized Mediterranean Diet model. In these regards, flavonoids are acknowledged for their beneficial effects on human health, including the mitigation of health risks from environmental pollutants. As here reviewed, the impairment of male fertility and gonadal development, as well as progression of cancers of reproductive systems of both sexes, due to the exposure of organic and inorganic pollutants, seemed to be counteracted by flavonoids in several pre-clinical and clinical studies. While the available evidence is promising, further studies are needed to definitively assert the role of flavonoids for the protection of both fertility and related cancers caused by the exposure to environmental pollutants. This will allow to design novel evidence-based dietary strategies to defend those subjects’ health who live or work in highly polluted areas.
Acknowledgments
A PON Industrial PhD fellowship from the Italian Minister of Instruction, University and Research (MIUR) to Alessandro Maugeri (code: DOT1314952; CUP: J98G18000040007) is gratefully acknowledged. This review was performed in the frame of the EcoFoodFertility Project.
Author Contributions
L.M. and M.P. conceived the study, performed the literature review and drafted the paper; A.M. (Alessandro Maugeri) and M.G.V. performed the literature review and drafted the article; A.M. (Alberto Mantovani), V.M. and S.M. critically revised the paper; M.N. designed the study and critically revised the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Morgan H.L., Watkins A.J. Transgenerational Impact of Environmental Change. Adv. Exp. Med. Biol. 2019;1200:71–89. doi: 10.1007/978-3-030-23633-5_4. [DOI] [PubMed] [Google Scholar]
- 2.Mortality G.B.D., Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ji W., Zhao B. Estimating mortality derived from indoor exposure to particles of outdoor origin. PLoS ONE. 2015;10:e0124238. doi: 10.1371/journal.pone.0124238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manisalidis I., Stavropoulou E., Stavropoulos A., Bezirtzoglou E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health. 2020;8:14. doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kabir E.R., Rahman M.S., Rahman I. A review on endocrine disruptors and their possible impacts on human health. Environ. Toxicol. Pharmacol. 2015;40:241–258. doi: 10.1016/j.etap.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Singh R., Kaur B., Kalina I., Popov T.A., Georgieva T., Garte S., Binkova B., Sram R.J., Taioli E., Farmer P.B. Effects of environmental air pollution on endogenous oxidative DNA damage in humans. Mutat. Res. 2007;620:71–82. doi: 10.1016/j.mrfmmm.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Kruk J., Aboul-Enein H.Y. Reactive Oxygen and Nitrogen Species in Carcinogenesis: Implications of Oxidative Stress on the Progression and Development of Several Cancer Types. Mini Rev. Med. Chem. 2017;17:904–919. doi: 10.2174/1389557517666170228115324. [DOI] [PubMed] [Google Scholar]
- 8.Hybertson B.M., Gao B., Bose S.K., McCord J.M. Oxidative stress in health and disease: The therapeutic potential of Nrf2 activation. Mol. Asp. Med. 2011;32:234–246. doi: 10.1016/j.mam.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Williams M.A., Rangasamy T., Bauer S.M., Killedar S., Karp M., Kensler T.W., Yamamoto M., Breysse P., Biswal S., Georas S.N. Disruption of the transcription factor Nrf2 promotes pro-oxidative dendritic cells that stimulate Th2-like immunoresponsiveness upon activation by ambient particulate matter. J. Immunol. 2008;181:4545–4559. doi: 10.4049/jimmunol.181.7.4545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montano L. Reproductive biomarkers as early indicators for assessing environmental health risk. In: Marfe G.D.S., editor. Toxic Waste Management and Health Risk. Bentham Science Publisher; Sharjah, United Arab Emirates: 2020. [DOI] [Google Scholar]
- 11.Montano L., Bergamo P., Andreassi M.G.L. The role of human semen as an early and reliable tool of environmental impact assessment on human health. In: Meccariello R., Chianese R., editors. Spermatozoa-Facts and Perspectives. InTechOpen; London, UK: 2017. [DOI] [Google Scholar]
- 12.Carlsen E., Giwercman A., Keiding N., Skakkebaek N.E. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992;305:609–613. doi: 10.1136/bmj.305.6854.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Travison T.G., Araujo A.B., O’Donnell A.B., Kupelian V., McKinlay J.B. A population-level decline in serum testosterone levels in American men. J. Clin. Endocrinol. Metab. 2007;92:196–202. doi: 10.1210/jc.2006-1375. [DOI] [PubMed] [Google Scholar]
- 14.Montano L., Donato F., Bianco P.M., Lettieri G., Guglielmino A., Motta O., Bonapace I.M., Piscopo M. Semen quality as a potential susceptibility indicator to SARS-CoV-2 insults in polluted areas. Environ. Sci. Pollut. Res. Int. 2021;28:37031–37040. doi: 10.1007/s11356-021-14579-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sengupta P., Dutta S., Krajewska-Kulak E. The Disappearing Sperms: Analysis of Reports Published Between 1980 and 2015. Am. J. Mens Health. 2017;11:1279–1304. doi: 10.1177/1557988316643383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agarwal A., Mulgund A., Hamada A., Chyatte M.R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 2015;13:37. doi: 10.1186/s12958-015-0032-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun H., Gong T.T., Jiang Y.T., Zhang S., Zhao Y.H., Wu Q.J. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990–2017: Results from a global burden of disease study, 2017. Aging (Albany NY) 2019;11:10952–10991. doi: 10.18632/aging.102497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharpe R.M. The ‘oestrogen hypothesis’—Where do we stand now? Int. J. Androl. 2003;26:2–15. doi: 10.1046/j.1365-2605.2003.00367.x. [DOI] [PubMed] [Google Scholar]
- 19.Krausz C. Male infertility: Pathogenesis and clinical diagnosis. Best Pract. Res. Clin. Endocrinol. Metab. 2011;25:271–285. doi: 10.1016/j.beem.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Lymperi S., Giwercman A. Endocrine disruptors and testicular function. Metabolism. 2018;86:79–90. doi: 10.1016/j.metabol.2018.03.022. [DOI] [PubMed] [Google Scholar]
- 21.Ghazarian A.A., Kelly S.P., Altekruse S.F., Rosenberg P.S., McGlynn K.A. Future of testicular germ cell tumor incidence in the United States: Forecast through 2026. Cancer. 2017;123:2320–2328. doi: 10.1002/cncr.30597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scott A.R., Stoltzfus K.C., Tchelebi L.T., Trifiletti D.M., Lehrer E.J., Rao P., Bleyer A., Zaorsky N.G. Trends in Cancer Incidence in US Adolescents and Young Adults, 1973–2015. JAMA Netw. Open. 2020;3:e2027738. doi: 10.1001/jamanetworkopen.2020.27738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2019. CA Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 24.Purdue M.P., Devesa S.S., Sigurdson A.J., McGlynn K.A. International patterns and trends in testis cancer incidence. Int. J. Cancer. 2005;115:822–827. doi: 10.1002/ijc.20931. [DOI] [PubMed] [Google Scholar]
- 25.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 26.Chia V.M., Quraishi S.M., Devesa S.S., Purdue M.P., Cook M.B., McGlynn K.A. International trends in the incidence of testicular cancer, 1973-2002. Cancer Epidemiol. Biomark. Prev. 2010;19:1151–1159. doi: 10.1158/1055-9965.EPI-10-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richiardi L., Bellocco R., Adami H.O., Torrang A., Barlow L., Hakulinen T., Rahu M., Stengrevics A., Storm H., Tretli S., et al. Testicular cancer incidence in eight northern European countries: Secular and recent trends. Cancer Epidemiol. Biomark. Prev. 2004;13:2157–2166. [PubMed] [Google Scholar]
- 28.Beiki O., Granath F., Allebeck P., Akre O., Moradi T. Subtype-specific risk of testicular tumors among immigrants and their descendants in Sweden, 1960 to 2007. Cancer Epidemiol. Biomark. Prev. 2010;19:1053–1065. doi: 10.1158/1055-9965.EPI-09-1190. [DOI] [PubMed] [Google Scholar]
- 29.Greene M.H., Kratz C.P., Mai P.L., Mueller C., Peters J.A., Bratslavsky G., Ling A., Choyke P.M., Premkumar A., Bracci J., et al. Familial testicular germ cell tumors in adults: 2010 summary of genetic risk factors and clinical phenotype. Endocr. Relat. Cancer. 2010;17:R109–R121. doi: 10.1677/ERC-09-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parkin D.M., Ferlay J., Curado M.P., Bray F., Edwards B., Shin H.R., Forman D. Fifty years of cancer incidence: CI5 I-IX. Int. J. Cancer. 2010;127:2918–2927. doi: 10.1002/ijc.25517. [DOI] [PubMed] [Google Scholar]
- 31.Rosen A., Jayram G., Drazer M., Eggener S.E. Global trends in testicular cancer incidence and mortality. Eur. Urol. 2011;60:374–379. doi: 10.1016/j.eururo.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 32.Turnbull C., Rahman N. Genome-wide association studies provide new insights into the genetic basis of testicular germ-cell tumour. Int. J. Androl. 2011;34:e86–e96. doi: 10.1111/j.1365-2605.2011.01162.x. [DOI] [PubMed] [Google Scholar]
- 33.Bray F., Richiardi L., Ekbom A., Pukkala E., Cuninkova M., Moller H. Trends in testicular cancer incidence and mortality in 22 European countries: Continuing increases in incidence and declines in mortality. Int. J. Cancer. 2006;118:3099–3111. doi: 10.1002/ijc.21747. [DOI] [PubMed] [Google Scholar]
- 34.Lorenzetti S., Marcoccia D., Mantovani A. Biomarkers of effect in endocrine disruption: How to link a functional assay to an adverse outcome pathway. Ann. Ist. Super. Sanita. 2015;51:167–171. doi: 10.4415/ANN_15_02_16. [DOI] [PubMed] [Google Scholar]
- 35.Rao C.V., Yamada H.Y., Yao Y., Dai W. Enhanced genomic instabilities caused by deregulated microtubule dynamics and chromosome segregation: A perspective from genetic studies in mice. Carcinogenesis. 2009;30:1469–1474. doi: 10.1093/carcin/bgp081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mondal G., Ohashi A., Yang L., Rowley M., Couch F.J. Tex14, a Plk1-regulated protein, is required for kinetochore-microtubule attachment and regulation of the spindle assembly checkpoint. Mol. Cell. 2012;45:680–695. doi: 10.1016/j.molcel.2012.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rao S., Zhen S., Roumiantsev S., McDonald L.T., Yuan G.C., Orkin S.H. Differential roles of Sall4 isoforms in embryonic stem cell pluripotency. Mol. Cell. Biol. 2010;30:5364–5380. doi: 10.1128/MCB.00419-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grassetti D., Giannandrea F., Paoli D., Masciandaro P., Figura V., Carlini T., Rizzo F., Lombardo F., Lenzi A., Gandini L. Androgen receptor polymorphisms and testicular cancer risk. Andrology. 2015;3:27–33. doi: 10.1111/j.2047-2927.2014.00252.x. [DOI] [PubMed] [Google Scholar]
- 39.Tandstad T., Dahl O., Cohn-Cedermark G., Cavallin-Stahl E., Stierner U., Solberg A., Langberg C., Bremnes R.M., Laurell A., Wijkstrom H., et al. Risk-adapted treatment in clinical stage I nonseminomatous germ cell testicular cancer: The SWENOTECA management program. J. Clin. Oncol. 2009;27:2122–2128. doi: 10.1200/JCO.2008.18.8953. [DOI] [PubMed] [Google Scholar]
- 40.Magelssen H., Brydoy M., Fossa S.D. The effects of cancer and cancer treatments on male reproductive function. Nat. Clin. Pract. Urol. 2006;3:312–322. doi: 10.1038/ncpuro0508. [DOI] [PubMed] [Google Scholar]
- 41.Kim C., McGlynn K.A., McCorkle R., Li Y., Erickson R.L., Ma S., Niebuhr D.W., Zhang G., Zhang Y., Bai Y., et al. Sexual functioning among testicular cancer survivors: A case-control study in the U.S. J. Psychosom. Res. 2012;73:68–73. doi: 10.1016/j.jpsychores.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Global Burden of Disease Cancer. Fitzmaurice C., Akinyemiju T.F., Al Lami F.H., Alam T., Alizadeh-Navaei R., Allen C., Alsharif U., Alvis-Guzman N., Amini E., et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2016: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2018;4:1553–1568. doi: 10.1001/jamaoncol.2018.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cai Q., Chen Y., Zhang D., Pan J., Xie Z., Xu C., Li S., Zhang X., Gao Y., Hou J., et al. Estimates of over-time trends in incidence and mortality of testicular cancer from 1990 to 2030. Transl. Androl. Urol. 2020;9:182–195. doi: 10.21037/tau.2020.02.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keys A., Menotti A., Karvonen M.J., Aravanis C., Blackburn H., Buzina R., Djordjevic B.S., Dontas A.S., Fidanza F., Keys M.H., et al. The diet and 15-year death rate in the seven countries study. Am. J. Epidemiol. 1986;124:903–915. doi: 10.1093/oxfordjournals.aje.a114480. [DOI] [PubMed] [Google Scholar]
- 45.Joint WHO/FAO Expert Consultation Diet, nutrition and the prevention of chronic diseases. World Health Organ. Tech. Rep. Ser. 2003;916:1–149. [PubMed] [Google Scholar]
- 46.American Heart Association Nutrition. Lichtenstein A.H., Appel L.J., Brands M., Carnethon M., Daniels S., Franch H.A., Franklin B., Kris-Etherton P., Harris W.S., et al. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 47.de Lorenzo A., Andreoli A., Sorge R.P., Iacopino L., Montagna S., Promenzio L., Serrano P. Modification of dietary habits (Mediterranean diet) and cancer mortality in a southern Italian village from 1960 to 1996. Ann. N. Y. Acad. Sci. 1999;889:224–229. doi: 10.1111/j.1749-6632.1999.tb08738.x. [DOI] [PubMed] [Google Scholar]
- 48.Tuttolomondo A., Simonetta I., Daidone M., Mogavero A., Ortello A., Pinto A. Metabolic and Vascular Effect of the Mediterranean Diet. Int. J. Mol. Sci. 2019;20:4716. doi: 10.3390/ijms20194716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leri M., Scuto M., Ontario M.L., Calabrese V., Calabrese E.J., Bucciantini M., Stefani M. Healthy Effects of Plant Polyphenols: Molecular Mechanisms. Int. J. Mol. Sci. 2020;21:1250. doi: 10.3390/ijms21041250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kelly F.J. Dietary antioxidants and environmental stress. Proc. Nutr. Soc. 2004;63:579–585. doi: 10.1079/PNS2004388. [DOI] [PubMed] [Google Scholar]
- 51.Jamalan M., Ghaffari M.A., Hoseinzadeh P., Hashemitabar M., Zeinali M. Human Sperm Quality and Metal Toxicants: Protective Effects of some Flavonoids on Male Reproductive Function. Int. J. Fertil. Steril. 2016;10:215–223. doi: 10.22074/ijfs.2016.4912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chung R.T. Detoxification effects of phytonutrients against environmental toxicants and sharing of clinical experience on practical applications. Environ. Sci. Pollut. Res. Int. 2017;24:8946–8956. doi: 10.1007/s11356-015-5263-3. [DOI] [PubMed] [Google Scholar]
- 53.Alegria-Torres J.A., Baccarelli A., Bollati V. Epigenetics and lifestyle. Epigenomics. 2011;3:267–277. doi: 10.2217/epi.11.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tedesco I., Russo M., Moccia S., Cervellera C., Spagnuolo C., Carbone V., Minasi P., Montano L., Verze P., Capece M. Protective effect of curcumin towards cadmium and polycyclic aromatic hydrocarbons toxicities: The EcoNutraPrevention Project. Nutr. Metab. Cardiovasc. Dis. 2020;30:540. doi: 10.1016/j.numecd.2019.12.036. [DOI] [Google Scholar]
- 55.Baldi F., Mantovani A. A new database for food safety: EDID (Endocrine disrupting chemicals—Diet Interaction Database) Ann. Ist. Super. Sanita. 2008;44:57–63. doi: 10.1016/j.reprotox.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 56.Mosbah R., Yousef M.I., Maranghi F., Mantovani A. Protective role of Nigella sativa oil against reproductive toxicity, hormonal alterations, and oxidative damage induced by chlorpyrifos in male rats. Toxicol. Ind. Health. 2016;32:1266–1277. doi: 10.1177/0748233714554675. [DOI] [PubMed] [Google Scholar]
- 57.Salas-Huetos A., Bullo M., Salas-Salvado J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: A systematic review of observational studies. Hum. Reprod. Update. 2017;23:371–389. doi: 10.1093/humupd/dmx006. [DOI] [PubMed] [Google Scholar]
- 58.Ricci E., Al-Beitawi S., Cipriani S., Alteri A., Chiaffarino F., Candiani M., Gerli S., Vigano P., Parazzini F. Dietary habits and semen parameters: A systematic narrative review. Andrology. 2018;6:104–116. doi: 10.1111/andr.12452. [DOI] [PubMed] [Google Scholar]
- 59.Alamo A., Condorelli R.A., Mongioi L.M., Cannarella R., Giacone F., Calabrese V., La Vignera S., Calogero A.E. Environment and Male Fertility: Effects of Benzo-alpha-Pyrene and Resveratrol on Human Sperm Function In Vitro. J. Clin. Med. 2019;8:561. doi: 10.3390/jcm8040561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Salas-Huetos A., Moraleda R., Giardina S., Anton E., Blanco J., Salas-Salvado J., Bullo M. Effect of nut consumption on semen quality and functionality in healthy men consuming a Western-style diet: A randomized controlled trial. Am. J. Clin. Nutr. 2018;108:953–962. doi: 10.1093/ajcn/nqy181. [DOI] [PubMed] [Google Scholar]
- 61.Dominguez-Vias G., Segarra A.B., Martinez-Canamero M., Ramirez-Sanchez M., Prieto I. Influence of a Virgin Olive Oil versus Butter Plus Cholesterol-Enriched Diet on Testicular Enzymatic Activities in Adult Male Rats. Int. J. Mol. Sci. 2017;18:1701. doi: 10.3390/ijms18081701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nassan F.L., Chavarro J.E., Tanrikut C. Diet and men’s fertility: Does diet affect sperm quality? Fertil. Steril. 2018;110:570–577. doi: 10.1016/j.fertnstert.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 63.Montano L., Ceretti E., Donato F., Bergamo P., Zani C., Viola G.C.V., Notari T., Pappalardo S., Zani D., Ubaldi S., et al. Effects of a Lifestyle Change Intervention on Semen Quality in Healthy Young Men Living in Highly Polluted Areas in Italy: The FASt Randomized Controlled Trial. Eur. Urol. Focus. 2021 doi: 10.1016/j.euf.2021.01.017. in press. [DOI] [PubMed] [Google Scholar]
- 64.Mitsunami M., Salas-Huetos A., Minguez-Alarcon L., Attaman J.A., Ford J.B., Kathrins M., Souter I., Chavarro J.E., Team E.S. Men’s dietary patterns in relation to infertility treatment outcomes among couples undergoing in vitro fertilization. J. Assist. Reprod. Genet. 2021;38:2307–2318. doi: 10.1007/s10815-021-02251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mitsunami M., Salas-Huetos A., Minguez-Alarcon L., Attaman J.A., Ford J.B., Kathrins M., Souter I., Chavarro J.E. A dietary score representing the overall relation of men’s diet with semen quality in relation to outcomes of infertility treatment with assisted reproduction. F&S Rep. 2021;2:396–404. doi: 10.1016/j.xfre.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Benatta M., Kettache R., Buchholz N., Trinchieri A. The impact of nutrition and lifestyle on male fertility. Arch. Ital. Urol. Androl. 2020;92 doi: 10.4081/aiua.2020.2.121. [DOI] [PubMed] [Google Scholar]
- 67.Karayiannis D., Kontogianni M.D., Mendorou C., Douka L., Mastrominas M., Yiannakouris N. Association between adherence to the Mediterranean diet and semen quality parameters in male partners of couples attempting fertility. Hum. Reprod. 2017;32:215–222. doi: 10.1093/humrep/dew288. [DOI] [PubMed] [Google Scholar]
- 68.Vigar V., Myers S., Oliver C., Arellano J., Robinson S., Leifert C. A Systematic Review of Organic Versus Conventional Food Consumption: Is There a Measurable Benefit on Human Health? Nutrients. 2019;12:7. doi: 10.3390/nu12010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim K.H., Kabir E., Jahan S.A. Exposure to pesticides and the associated human health effects. Sci. Total Environ. 2017;575:525–535. doi: 10.1016/j.scitotenv.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 70.Moshammer H., Poteser M., Hutter H.P. More pesticides-less children? Wien. Klin. Wochenschr. 2020;132:197–204. doi: 10.1007/s00508-019-01566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Baranski M., Srednicka-Tober D., Volakakis N., Seal C., Sanderson R., Stewart G.B., Benbrook C., Biavati B., Markellou E., Giotis C., et al. Higher antioxidant and lower cadmium concentrations and lower incidence of pesticide residues in organically grown crops: A systematic literature review and meta-analyses. Br. J. Nutr. 2014;112:794–811. doi: 10.1017/S0007114514001366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ribes-Moya A.M., Adalid A.M., Raigon M.D., Hellin P., Fita A., Rodriguez-Burruezo A. Variation in flavonoids in a collection of peppers (Capsicum sp.) under organic and conventional cultivation: Effect of the genotype, ripening stage, and growing system. J. Sci. Food Agric. 2020;100:2208–2223. doi: 10.1002/jsfa.10245. [DOI] [PubMed] [Google Scholar]
- 73.Hallmann E., Marszalek K., Lipowski J., Jasinska U., Kazimierczak R., Srednicka-Tober D., Rembialkowska E. Polyphenols and carotenoids in pickled bell pepper from organic and conventional production. Food Chem. 2019;278:254–260. doi: 10.1016/j.foodchem.2018.11.052. [DOI] [PubMed] [Google Scholar]
- 74.Srednicka-Tober D., Baranski M., Seal C.J., Sanderson R., Benbrook C., Steinshamn H., Gromadzka-Ostrowska J., Rembialkowska E., Skwarlo-Sonta K., Eyre M., et al. Higher PUFA and n-3 PUFA, conjugated linoleic acid, alpha-tocopherol and iron, but lower iodine and selenium concentrations in organic milk: A systematic literature review and meta- and redundancy analyses. Br. J. Nutr. 2016;115:1043–1060. doi: 10.1017/S0007114516000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hurtado-Barroso S., Tresserra-Rimbau A., Vallverdu-Queralt A., Lamuela-Raventos R.M. Organic food and the impact on human health. Crit. Rev. Food Sci. Nutr. 2019;59:704–714. doi: 10.1080/10408398.2017.1394815. [DOI] [PubMed] [Google Scholar]
- 76.Sun Y., Liu B., Du Y., Snetselaar L.G., Sun Q., Hu F.B., Bao W. Inverse Association between Organic Food Purchase and Diabetes Mellitus in US Adults. Nutrients. 2018;10:1877. doi: 10.3390/nu10121877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liang J., Liang X., Cao P., Wang X., Gao P., Ma N., Li N., Xu H. A Preliminary Investigation of Naturally Occurring Aluminum in Grains, Vegetables, and Fruits from Some Areas of China and Dietary Intake Assessment. J. Food Sci. 2019;84:701–710. doi: 10.1111/1750-3841.14459. [DOI] [PubMed] [Google Scholar]
- 78.Glibowski P. Organic food and health. Rocz. Panstw. Zakl. Hig. 2020;71:131–136. doi: 10.32394/rpzh.2020.0110. [DOI] [PubMed] [Google Scholar]
- 79.Crinnion W.J. Organic foods contain higher levels of certain nutrients, lower levels of pesticides, and may provide health benefits for the consumer. Altern. Med. Rev. 2010;15:4–12. [PubMed] [Google Scholar]
- 80.Chiu Y.H., Williams P.L., Gillman M.W., Gaskins A.J., Minguez-Alarcon L., Souter I., Toth T.L., Ford J.B., Hauser R., Chavarro J.E., et al. Association Between Pesticide Residue Intake From Consumption of Fruits and Vegetables and Pregnancy Outcomes Among Women Undergoing Infertility Treatment With Assisted Reproductive Technology. JAMA Intern. Med. 2018;178:17–26. doi: 10.1001/jamainternmed.2017.5038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Baudry J., Assmann K.E., Touvier M., Alles B., Seconda L., Latino-Martel P., Ezzedine K., Galan P., Hercberg S., Lairon D., et al. Association of Frequency of Organic Food Consumption With Cancer Risk: Findings From the NutriNet-Sante Prospective Cohort Study. JAMA Intern. Med. 2018;178:1597–1606. doi: 10.1001/jamainternmed.2018.4357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chang S.K., Alasalvar C., Shahidi F. Superfruits: Phytochemicals, antioxidant efficacies, and health effects—A comprehensive review. Crit. Rev. Food Sci. Nutr. 2019;59:1580–1604. doi: 10.1080/10408398.2017.1422111. [DOI] [PubMed] [Google Scholar]
- 83.Vanduchova A., Anzenbacher P., Anzenbacherova E. Isothiocyanate from Broccoli, Sulforaphane, and Its Properties. J. Med. Food. 2019;22:121–126. doi: 10.1089/jmf.2018.0024. [DOI] [PubMed] [Google Scholar]
- 84.Paolini M., Perocco P., Canistro D., Valgimigli L., Pedulli G.F., Iori R., Croce C.D., Cantelli-Forti G., Legator M.S., Abdel-Rahman S.Z. Induction of cytochrome P450, generation of oxidative stress and in vitro cell-transforming and DNA-damaging activities by glucoraphanin, the bioprecursor of the chemopreventive agent sulforaphane found in broccoli. Carcinogenesis. 2004;25:61–67. doi: 10.1093/carcin/bgg174. [DOI] [PubMed] [Google Scholar]
- 85.Ito S., Chen C., Satoh J., Yim S., Gonzalez F.J. Dietary phytochemicals regulate whole-body CYP1A1 expression through an arylhydrocarbon receptor nuclear translocator-dependent system in gut. J. Clin. Investig. 2007;117:1940–1950. doi: 10.1172/JCI31647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Abdull Razis A.F., Noor N.M. Cruciferous vegetables: Dietary phytochemicals for cancer prevention. Asian Pac. J. Cancer Prev. 2013;14:1565–1570. doi: 10.7314/APJCP.2013.14.3.1565. [DOI] [PubMed] [Google Scholar]
- 87.Zona A., Iavarone I., Buzzoni C., Conti S., Santoro M., Fazzo L., Pasetto R., Pirastu R., Bruno C., Ancona C., et al. SENTIERI: Epidemiological Study of Residents in National Priority Contaminated Sites. Fifth Report. Epidemiol. Prev. 2019;43:1–208. doi: 10.19191/EP19.2-3.S1.032. [DOI] [PubMed] [Google Scholar]
- 88.Maresca V., Fusaro L., Sorbo S., Siciliano A., Loppi S., Paoli L., Monaci F., Karam E.A., Piscopo M., Guida M., et al. Functional and structural biomarkers to monitor heavy metal pollution of one of the most contaminated freshwater sites in Southern Europe. Ecotoxicol. Environ. Saf. 2018;163:665–673. doi: 10.1016/j.ecoenv.2018.07.122. [DOI] [PubMed] [Google Scholar]
- 89.Basile A., Loppi S., Piscopo M., Paoli L., Vannini A., Monaci F., Sorbo S., Lentini M., Esposito S. The biological response chain to pollution: A case study from the “Italian Triangle of Death” assessed with the liverwort Lunularia cruciata. Environ. Sci. Pollut. Res. Int. 2017;24:26185–26193. doi: 10.1007/s11356-017-9304-y. [DOI] [PubMed] [Google Scholar]
- 90.Bergamo P., Volpe M.G., Lorenzetti S., Mantovani A., Notari T., Cocca E., Cerullo S., Di Stasio M., Cerino P., Montano L. Human semen as an early, sensitive biomarker of highly polluted living environment in healthy men: A pilot biomonitoring study on trace elements in blood and semen and their relationship with sperm quality and RedOx status. Reprod. Toxicol. 2016;66:1–9. doi: 10.1016/j.reprotox.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 91.Raimondo S., Gentile M., Esposito G., Gentile T., Ferrara I., Crescenzo C., Palmieri M., Cuomo F., De Filippo S., Lettieri G., et al. Could Kallikrein-Related Serine Peptidase 3 Be an Early Biomarker of Environmental Exposure in Young Women? Int. J. Environ. Res. Public Health. 2021;18:8833. doi: 10.3390/ijerph18168833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Montano L., Porciello G., Crispo A., Lorenzetti S., Salvatore R., Ubaldi S., Caputo M. The role of the Mediterranean diet on sperm morphology in healthy men living in polluted area (EcoFoodFertility project) Reprod. Toxicol. 2017;72:45. doi: 10.1016/j.reprotox.2017.06.170. [DOI] [Google Scholar]
- 93.Aitken R.J. Oxidative stress and the etiology of male infertility. J. Assist. Reprod. Genet. 2016;33:1691–1692. doi: 10.1007/s10815-016-0791-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aitken R.J., Gibb Z., Baker M.A., Drevet J., Gharagozloo P. Causes and consequences of oxidative stress in spermatozoa. Reprod. Fertil. Dev. 2016;28:1–10. doi: 10.1071/RD15325. [DOI] [PubMed] [Google Scholar]
- 95.Montano L., Donato F., Bianco P.M., Lettieri G., Guglielmino A., Motta O., Bonapace I.M., Piscopo M. Air Pollution and COVID-19: A Possible Dangerous Synergy for Male Fertility. Int. J. Environ. Res. Public Health. 2021;18:6846. doi: 10.3390/ijerph18136846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Musumeci L., Maugeri A., Cirmi S., Lombardo G.E., Russo C., Gangemi S., Calapai G., Navarra M. Citrus fruits and their flavonoids in inflammatory bowel disease: An overview. Nat. Prod. Res. 2020;34:122–136. doi: 10.1080/14786419.2019.1601196. [DOI] [PubMed] [Google Scholar]
- 97.Cirmi S., Navarra M., Woodside J.V., Cantwell M.M. Citrus fruits intake and oral cancer risk: A systematic review and meta-analysis. Pharmacol. Res. 2018;133:187–194. doi: 10.1016/j.phrs.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 98.Cirmi S., Bisignano C., Mandalari G., Navarra M. Anti-infective potential of Citrus bergamia Risso et Poiteau (bergamot) derivatives: A systematic review. Phytother. Res. 2016;30:1404–1411. doi: 10.1002/ptr.5646. [DOI] [PubMed] [Google Scholar]
- 99.Marino A., Paterniti I., Cordaro M., Morabito R., Campolo M., Navarra M., Esposito E., Cuzzocrea S. Role of natural antioxidants and potential use of bergamot in treating rheumatoid arthritis. PharmaNutrition. 2015;3:53–59. doi: 10.1016/j.phanu.2015.03.002. [DOI] [Google Scholar]
- 100.Mannucci C., Casciaro M., Sorbara E.E., Calapai F., Di Salvo E., Pioggia G., Navarra M., Calapai G., Gangemi S. Nutraceuticals against Oxidative Stress in Autoimmune Disorders. Antioxidants. 2021;10:261. doi: 10.3390/antiox10020261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Maugeri A., Cirmi S., Minciullo P.L., Gangemi S., Calapai G., Mollace V., Navarra M. Citrus fruits and inflammaging: A systematic review. Phytochem. Rev. 2019;18:1025–1049. doi: 10.1007/s11101-019-09613-3. [DOI] [Google Scholar]
- 102.Citraro R., Navarra M., Leo A., Donato Di Paola E., Santangelo E., Lippiello P., Aiello R., Russo E., De Sarro G. The Anticonvulsant Activity of a Flavonoid-Rich Extract from Orange Juice Involves both NMDA and GABA-Benzodiazepine Receptor Complexes. Molecules. 2016;21:1261. doi: 10.3390/molecules21091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mannucci C., Navarra M., Calapai F., Squeri R., Gangemi S., Calapai G. Clinical Pharmacology of Citrus bergamia: A Systematic Review. Phytother. Res. 2017;31:27–39. doi: 10.1002/ptr.5734. [DOI] [PubMed] [Google Scholar]
- 104.Mannucci C., Calapai F., Cardia L., Inferrera G., D’Arena G., Di Pietro M., Navarra M., Gangemi S., Ventura Spagnolo E., Calapai G. Clinical Pharmacology of Citrus aurantium and Citrus sinensis for the Treatment of Anxiety. Evid.-Based Complement. Alternat. Med. 2018;2018:3624094. doi: 10.1155/2018/3624094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Patra S., Pradhan B., Nayak R., Behera C., Das S., Patra S.K., Efferth T., Jena M., Bhutia S.K. Dietary polyphenols in chemoprevention and synergistic effect in cancer: Clinical evidences and molecular mechanisms of action. Phytomedicine. 2021;90:153554. doi: 10.1016/j.phymed.2021.153554. [DOI] [PubMed] [Google Scholar]
- 106.Cirmi S., Maugeri A., Ferlazzo N., Gangemi S., Calapai G., Schumacher U., Navarra M. Anticancer Potential of Citrus Juices and Their Extracts: A Systematic Review of Both Preclinical and Clinical Studies. Front. Pharmacol. 2017;8:420. doi: 10.3389/fphar.2017.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Adorisio S., Argentieri M., Avato P., Caderni G., Chioccioli S., Cirmi S., Delfino D., Greco G., Hrelia P., Iriti M. The molecular basis of the anticancer properties of quercetin. Pharmadvances. 2021;3:496–522. doi: 10.36118/pharmadvances.2021.10. [DOI] [Google Scholar]
- 108.Navarra M., Ursino M.R., Ferlazzo N., Russo M., Schumacher U., Valentiner U. Effect of Citrus bergamia juice on human neuroblastoma cells in vitro and in metastatic xenograft models. Fitoterapia. 2014;95:83–92. doi: 10.1016/j.fitote.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 109.Navarra M., Femia A.P., Romagnoli A., Tortora K., Luceri C., Cirmi S., Ferlazzo N., Caderni G. A flavonoid-rich extract from bergamot juice prevents carcinogenesis in a genetic model of colorectal cancer, the Pirc rat (F344/NTac-Apc(am1137)) Eur. J. Nutr. 2020;59:885–894. doi: 10.1007/s00394-019-01948-z. [DOI] [PubMed] [Google Scholar]
- 110.Clementino M., Shi X., Zhang Z. Prevention of Polyphenols against Carcinogenesis Induced by Environmental Carcinogens. J. Environ. Pathol. Toxicol. Oncol. 2017;36:87–98. doi: 10.1615/JEnvironPatholToxicolOncol.2017019057. [DOI] [PubMed] [Google Scholar]
- 111.Petriello M.C., Newsome B., Hennig B. Influence of nutrition in PCB-induced vascular inflammation. Environ. Sci. Pollut. Res. Int. 2014;21:6410–6418. doi: 10.1007/s11356-013-1549-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ferlazzo N., Visalli G., Cirmi S., Lombardo G.E., Lagana P., Di Pietro A., Navarra M. Natural iron chelators: Protective role in A549 cells of flavonoids-rich extracts of Citrus juices in Fe(3+)-induced oxidative stress. Environ. Toxicol. Pharmacol. 2016;43:248–256. doi: 10.1016/j.etap.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 113.Link A., Balaguer F., Goel A. Cancer chemoprevention by dietary polyphenols: Promising role for epigenetics. Biochem. Pharmacol. 2010;80:1771–1792. doi: 10.1016/j.bcp.2010.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Symonowicz M., Kolanek M. Flavonoids and Their Properties to Form Chelate Complexes. Lodz University of Technology Repository; Łódź, Poland: 2012. [Google Scholar]
- 115.Ferlazzo N., Cirmi S., Calapai G., Ventura-Spagnolo E., Gangemi S., Navarra M. Anti-Inflammatory Activity of Citrus bergamia Derivatives: Where Do We Stand? Molecules. 2016;21:1273. doi: 10.3390/molecules21101273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gugliandolo E., Fusco R., D’Amico R., Peditto M., Oteri G., Di Paola R., Cuzzocrea S., Navarra M. Treatment With a Flavonoid-Rich Fraction of Bergamot Juice Improved Lipopolysaccharide-Induced Periodontitis in Rats. Front. Pharmacol. 2018;9:1563. doi: 10.3389/fphar.2018.01563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Fusco R., Cirmi S., Gugliandolo E., Di Paola R., Cuzzocrea S., Navarra M. A flavonoid-rich extract of orange juice reduced oxidative stress in an experimental model of inflammatory bowel disease. J. Funct. Foods. 2017;30:168–178. doi: 10.1016/j.jff.2016.12.038. [DOI] [Google Scholar]
- 118.Maugeri A., Ferlazzo N., De Luca L., Gitto R., Navarra M. The link between the AMPK/SIRT1 axis and a flavonoid-rich extract of Citrus bergamia juice: A cell-free, in silico, and in vitro study. Phytother. Res. 2019;33:1805–1814. doi: 10.1002/ptr.6368. [DOI] [PubMed] [Google Scholar]
- 119.Curro M., Risitano R., Ferlazzo N., Cirmi S., Gangemi C., Caccamo D., Ientile R., Navarra M. Citrus bergamia Juice Extract Attenuates beta-Amyloid-Induced Pro-Inflammatory Activation of THP-1 Cells Through MAPK and AP-1 Pathways. Sci. Rep. 2016;6:20809. doi: 10.1038/srep20809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ferlazzo N., Cirmi S., Maugeri A., Russo C., Lombardo G.E., Gangemi S., Calapai G., Mollace V., Navarra M. Neuroprotective Effect of Bergamot Juice in 6-OHDA-Induced SH-SY5Y Cell Death, an In Vitro Model of Parkinson’s Disease. Pharmaceutics. 2020;12:326. doi: 10.3390/pharmaceutics12040326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cirmi S., Maugeri A., Lombardo G.E., Russo C., Musumeci L., Gangemi S., Calapai G., Barreca D., Navarra M. A Flavonoid-Rich Extract of Mandarin Juice Counteracts 6-OHDA-Induced Oxidative Stress in SH-SY5Y Cells and Modulates Parkinson-Related Genes. Antioxidants. 2021;10:539. doi: 10.3390/antiox10040539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yahfoufi N., Alsadi N., Jambi M., Matar C. The Immunomodulatory and Anti-Inflammatory Role of Polyphenols. Nutrients. 2018;10:1618. doi: 10.3390/nu10111618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Giacoppo S., Galuppo M., Lombardo G.E., Ulaszewska M.M., Mattivi F., Bramanti P., Mazzon E., Navarra M. Neuroprotective effects of a polyphenolic white grape juice extract in a mouse model of experimental autoimmune encephalomyelitis. Fitoterapia. 2015;103:171–186. doi: 10.1016/j.fitote.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 124.Cersosimo F., Lonardi S., Bernardini G., Telfer B., Mandelli G.E., Santucci A., Vermi W., Giurisato E. Tumor-Associated Macrophages in Osteosarcoma: From Mechanisms to Therapy. Int. J. Mol. Sci. 2020;21:5207. doi: 10.3390/ijms21155207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Qiu J., Zhang T., Zhu X., Yang C., Wang Y., Zhou N., Ju B., Zhou T., Deng G., Qiu C. Hyperoside Induces Breast Cancer Cells Apoptosis via ROS-Mediated NF-kappaB Signaling Pathway. Int. J. Mol. Sci. 2019;21:131. doi: 10.3390/ijms21010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Celano M., Maggisano V., De Rose R.F., Bulotta S., Maiuolo J., Navarra M., Russo D. Flavonoid Fraction of Citrus reticulata Juice Reduces Proliferation and Migration of Anaplastic Thyroid Carcinoma Cells. Nutr. Cancer. 2015;67:1183–1190. doi: 10.1080/01635581.2015.1073760. [DOI] [PubMed] [Google Scholar]
- 127.Seba V., Silva G., Santos M.B.D., Baek S.J., Franca S.C., Fachin A.L., Regasini L.O., Marins M. Chalcone Derivatives 4′-Amino-1-Naphthyl-Chalcone (D14) and 4′-Amino-4-Methyl-1-Naphthyl-Chalcone (D15) Suppress Migration and Invasion of Osteosarcoma Cells Mediated by p53 Regulating EMT-Related Genes. Int. J. Mol. Sci. 2018;19:2838. doi: 10.3390/ijms19092838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Liao Z.Y., Liang I.C., Li H.J., Wu C.C., Lo H.M., Chang D.C., Hung C.F. Chrysin Inhibits High Glucose-Induced Migration on Chorioretinal Endothelial Cells via VEGF and VEGFR Down-Regulation. Int. J. Mol. Sci. 2020;21:5541. doi: 10.3390/ijms21155541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Vemuri S.K., Banala R.R., Subbaiah G., Srivastava S.K., Reddy A.G., Malarvili T. Anti-cancer potential of a mix of natural extracts of turmeric, ginger and garlic: A cell-based study. Egypt. J. Basic Appl. Sci. 2017;4:332–344. doi: 10.1016/j.ejbas.2017.07.005. [DOI] [Google Scholar]
- 130.Vincent T.L., Gatenby R.A. An evolutionary model for initiation, promotion, and progression in carcinogenesis. Int. J. Oncol. 2008;32:729–737. [PubMed] [Google Scholar]
- 131.Abotaleb M., Samuel S.M., Varghese E., Varghese S., Kubatka P., Liskova A., Busselberg D. Flavonoids in Cancer and Apoptosis. Cancers. 2018;11:28. doi: 10.3390/cancers11010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Masuelli L., Benvenuto M., Di Stefano E., Mattera R., Fantini M., De Feudis G., De Smaele E., Tresoldi I., Giganti M.G., Modesti A., et al. Curcumin blocks autophagy and activates apoptosis of malignant mesothelioma cell lines and increases the survival of mice intraperitoneally transplanted with a malignant mesothelioma cell line. Oncotarget. 2017;8:34405–34422. doi: 10.18632/oncotarget.14907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Prieto-Dominguez N., Garcia-Mediavilla M.V., Sanchez-Campos S., Mauriz J.L., Gonzalez-Gallego J. Autophagy as a Molecular Target of Flavonoids Underlying their Protective Effects in Human Disease. Curr. Med. Chem. 2018;25:814–838. doi: 10.2174/0929867324666170918125155. [DOI] [PubMed] [Google Scholar]
- 134.Chae H.S., Xu R., Won J.Y., Chin Y.W., Yim H. Molecular Targets of Genistein and Its Related Flavonoids to Exert Anticancer Effects. Int. J. Mol. Sci. 2019;20:2420. doi: 10.3390/ijms20102420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cernelev O., Mantovani A. Natural substances in supplements and nutraceuticals as Endocrine Disruptors. In: Mantovani A., Fucic A., editors. Challenges in Endocrine Disruptor Toxicology and Risk Assessment. Royal Society of Chemistry; London, UK: 2020. pp. 356–376. [Google Scholar]
- 136.Ye R.J., Yang J.M., Hai D.M., Liu N., Ma L., Lan X.B., Niu J.G., Zheng P., Yu J.Q. Interplay between male reproductive system dysfunction and the therapeutic effect of flavonoids. Fitoterapia. 2020;147:104756. doi: 10.1016/j.fitote.2020.104756. [DOI] [PubMed] [Google Scholar]
- 137.Moretti E., Mazzi L., Terzuoli G., Bonechi C., Iacoponi F., Martini S., Rossi C., Collodel G. Effect of quercetin, rutin, naringenin and epicatechin on lipid peroxidation induced in human sperm. Reprod. Toxicol. 2012;34:651–657. doi: 10.1016/j.reprotox.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 138.Osawe S.O., Farombi E.O. Querce.etin and rutin ameliorates sulphasalazine-induced spermiotoxicity, alterations in reproductive hormones and steroidogenic enzyme imbalance in rats. Andrologia. 2018;50:e12981. doi: 10.1111/and.12981. [DOI] [PubMed] [Google Scholar]
- 139.Chen M., Liu W., Li Z., Xiao W. Effect of epigallocatechin-3-gallate (EGCG) on embryos inseminated with oxidative stress-induced DNA damage sperm. Syst. Biol. Reprod. Med. 2020;66:244–254. doi: 10.1080/19396368.2020.1756525. [DOI] [PubMed] [Google Scholar]
- 140.Duracka M., Lukac N., Kacaniova M., Kantor A., Hleba L., Ondruska L., Tvrda E. Antibiotics Versus Natural Biomolecules: The Case of In Vitro Induced Bacteriospermia by Enterococcus Faecalis in Rabbit Semen. Molecules. 2019;24:4329. doi: 10.3390/molecules24234329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pei Y., Yang L., Wu L., He H., Geng G., Xu D., Chen H., Li Q. Combined effect of apigenin and ferulic acid on frozen-thawed boar sperm quality. Anim. Sci. J. 2018;89:956–965. doi: 10.1111/asj.13009. [DOI] [PubMed] [Google Scholar]
- 142.Xu D., Wu L., Yang L., Liu D., Chen H., Geng G., Li Q. Rutin protects boar sperm from cryodamage via enhancing the antioxidative defense. Anim. Sci. J. 2020;91:e13328. doi: 10.1111/asj.13328. [DOI] [PubMed] [Google Scholar]
- 143.Prabu S.M., Shagirtha K., Renugadevi J. Amelioration of cadmium-induced oxidative stress, impairment in lipids and plasma lipoproteins by the combined treatment with quercetin and alpha-tocopherol in rats. J. Food Sci. 2010;75:T132–T140. doi: 10.1111/j.1750-3841.2010.01757.x. [DOI] [PubMed] [Google Scholar]
- 144.Farombi E.O., Adedara I.A., Akinrinde S.A., Ojo O.O., Eboh A.S. Protective effects of kolaviron and quercetin on cadmium-induced testicular damage and endocrine pathology in rats. Andrologia. 2012;44:273–284. doi: 10.1111/j.1439-0272.2012.01279.x. [DOI] [PubMed] [Google Scholar]
- 145.Couture R., Mora N., Al Bittar S., Najih M., Touaibia M., Martin L.J. Luteolin modulates gene expression related to steroidogenesis, apoptosis, and stress response in rat LC540 tumor Leydig cells. Cell Biol. Toxicol. 2020;36:31–49. doi: 10.1007/s10565-019-09481-9. [DOI] [PubMed] [Google Scholar]
- 146.Chen S.J., Allam J.P., Duan Y.G., Haidl G. Influence of reactive oxygen species on human sperm functions and fertilizing capacity including therapeutical approaches. Arch. Gynecol. Obstet. 2013;288:191–199. doi: 10.1007/s00404-013-2801-4. [DOI] [PubMed] [Google Scholar]
- 147.Appiah M.O., Li W., Zhao J., Liu H., Dong Y., Xiang J., Wang J., Lu W. Quercetin supplemented casein-based extender improves the post-thaw quality of rooster semen. Cryobiology. 2020;94:57–65. doi: 10.1016/j.cryobiol.2020.04.010. [DOI] [PubMed] [Google Scholar]
- 148.Ghaniei A., Eslami M., Zadeh Hashem E., Rezapour R., Talebi A. Quercetin attenuates H2O2-induced toxicity of rooster semen during liquid storage at 4 degrees C. J. Anim. Physiol. Anim. Nutr. 2019;103:713–722. doi: 10.1111/jpn.13056. [DOI] [PubMed] [Google Scholar]
- 149.Sun J., Wang H., Liu B., Shi W., Shi J., Zhang Z., Xing J. Rutin attenuates H2O2-induced oxidation damage and apoptosis in Leydig cells by activating PI3K/Akt signal pathways. Biomed. Pharmacother. 2017;88:500–506. doi: 10.1016/j.biopha.2017.01.066. [DOI] [PubMed] [Google Scholar]
- 150.Samie A., Sedaghat R., Baluchnejadmojarad T., Roghani M. Hesperetin, a citrus flavonoid, attenuates testicular damage in diabetic rats via inhibition of oxidative stress, inflammation, and apoptosis. Life Sci. 2018;210:132–139. doi: 10.1016/j.lfs.2018.08.074. [DOI] [PubMed] [Google Scholar]
- 151.Ma B., Zhang J., Zhu Z., Zhao A., Zhou Y., Ying H., Zhang Q. Luteolin Ameliorates Testis Injury and Blood-Testis Barrier Disruption through the Nrf2 Signaling Pathway and by Upregulating Cx43. Mol. Nutr. Food Res. 2019;63:e1800843. doi: 10.1002/mnfr.201800843. [DOI] [PubMed] [Google Scholar]
- 152.Chen M., Hao J., Yang Q., Li G. Effects of icariin on reproductive functions in male rats. Molecules. 2014;19:9502–9514. doi: 10.3390/molecules19079502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bharti S., Misro M.M., Rai U. Quercetin supplementation restores testicular function and augments germ cell survival in the estrogenized rats. Mol. Cell. Endocrinol. 2014;383:10–20. doi: 10.1016/j.mce.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 154.Kim H.S., Kim Y.J., Seo Y.R. An Overview of Carcinogenic Heavy Metal: Molecular Toxicity Mechanism and Prevention. J. Cancer Prev. 2015;20:232–240. doi: 10.15430/JCP.2015.20.4.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lettieri G., Notariale R., Carusone N., Giarra A., Trifuoggi M., Manna C., Piscopo M. New Insights into Alterations in PL Proteins Affecting Their Binding to DNA after Exposure of Mytilus galloprovincialis to Mercury-A Possible Risk to Sperm Chromatin Structure? Int. J. Mol. Sci. 2021;22:5893. doi: 10.3390/ijms22115893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lettieri G., Notariale R., Ambrosino A., Di Bonito A., Giarra A., Trifuoggi M., Manna C., Piscopo M. Spermatozoa Transcriptional Response and Alterations in PL Proteins Properties after Exposure of Mytilus galloprovincialis to Mercury. Int. J. Mol. Sci. 2021;22:1618. doi: 10.3390/ijms22041618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Piscopo M., Trifuoggi M., Notariale R., Labar S., Troisi J., Giarra A., Rabbito D., Puoti R., de Benedictis D., Brundo M.V., et al. Protamine-like proteins’ analysis as an emerging biotechnique for cadmium impact assessment on male mollusk Mytilus galloprovincialis (Lamarck 1819) Acta Biochim. Pol. 2018;65:259–267. doi: 10.18388/abp.2017_2533. [DOI] [PubMed] [Google Scholar]
- 158.Piscopo M., Notariale R., Rabbito D., Ausio J., Olanrewaju O.S., Guerriero G. Mytilus galloprovincialis (Lamarck, 1819) spermatozoa: hsp70 expression and protamine-like protein property studies. Environ. Sci. Pollut. Res. Int. 2018;25:12957–12966. doi: 10.1007/s11356-018-1570-9. [DOI] [PubMed] [Google Scholar]
- 159.De Guglielmo V., Puoti R., Notariale R., Maresca V., Ausio J., Troisi J., Verrillo M., Basile A., Febbraio F., Piscopo M. Alterations in the properties of sperm protamine-like II protein after exposure of Mytilus galloprovincialis (Lamarck 1819) to sub-toxic doses of cadmium. Ecotoxicol. Environ. Saf. 2019;169:600–606. doi: 10.1016/j.ecoenv.2018.11.069. [DOI] [PubMed] [Google Scholar]
- 160.Lettieri G., Mollo V., Ambrosino A., Caccavale F., Troisi J., Febbraio F., Piscopo M. Molecular effects of copper on the reproductive system of mytilus galloprovincialis. Mol. Reprod. Dev. 2019;86:1357–1368. doi: 10.1002/mrd.23114. [DOI] [PubMed] [Google Scholar]
- 161.Lettieri G., D’Agostino G., Mele E., Cardito C., Esposito R., Cimmino A., Giarra A., Trifuoggi M., Raimondo S., Notari T., et al. Discovery of the Involvement in DNA Oxidative Damage of Human Sperm Nuclear Basic Proteins of Healthy Young Men Living in Polluted Areas. Int. J. Mol. Sci. 2020;21:4198. doi: 10.3390/ijms21124198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lettieri G., Marra F., Moriello C., Prisco M., Notari T., Trifuoggi M., Giarra A., Bosco L., Montano L., Piscopo M. Molecular Alterations in Spermatozoa of a Family Case Living in the Land of Fires. A First Look at Possible Transgenerational Effects of Pollutants. Int. J. Mol. Sci. 2020;21:6710. doi: 10.3390/ijms21186710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Yang O., Kim H.L., Weon J.I., Seo Y.R. Endocrine-disrupting Chemicals: Review of Toxicological Mechanisms Using Molecular Pathway Analysis. J. Cancer Prev. 2015;20:12–24. doi: 10.15430/JCP.2015.20.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Togawa K., Le Cornet C., Feychting M., Tynes T., Pukkala E., Hansen J., Olsson A., Oksbjerg Dalton S., Nordby K.C., Uuksulainen S., et al. Parental Occupational Exposure to Heavy Metals and Welding Fumes and Risk of Testicular Germ Cell Tumors in Offspring: A Registry-Based Case-Control Study. Cancer Epidemiol. Biomark. Prev. 2016;25:1426–1434. doi: 10.1158/1055-9965.EPI-16-0328. [DOI] [PubMed] [Google Scholar]
- 165.Morales-Suarez-Varela M.M., Toft G.V., Jensen M.S., Ramlau-Hansen C., Kaerlev L., Thulstrup A.M., Llopis-Gonzalez A., Olsen J., Bonde J.P. Parental occupational exposure to endocrine disrupting chemicals and male genital malformations: A study in the Danish National Birth Cohort study. Environ. Health. 2011;10:3. doi: 10.1186/1476-069X-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Giordano F., Abballe A., De Felip E., di Domenico A., Ferro F., Grammatico P., Ingelido A.M., Marra V., Marrocco G., Vallasciani S., et al. Maternal exposures to endocrine disrupting chemicals and hypospadias in offspring. Birth Defects Res. A Clin. Mol. Teratol. 2010;88:241–250. doi: 10.1002/bdra.20657. [DOI] [PubMed] [Google Scholar]
- 167.Jahan S., Khan M., Ahmed S., Ullah H. Comparative analysis of antioxidants against cadmium induced reproductive toxicity in adult male rats. Syst. Biol. Reprod. Med. 2014;60:28–34. doi: 10.3109/19396368.2013.843039. [DOI] [PubMed] [Google Scholar]
- 168.Itoh H., Iwasaki M., Sawada N., Takachi R., Kasuga Y., Yokoyama S., Onuma H., Nishimura H., Kusama R., Yokoyama K., et al. Dietary cadmium intake and breast cancer risk in Japanese women: A case-control study. Int. J. Hyg. Environ. Health. 2014;217:70–77. doi: 10.1016/j.ijheh.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 169.Henson M.C., Chedrese P.J. Endocrine disruption by cadmium, a common environmental toxicant with paradoxical effects on reproduction. Exp. Biol. Med. (Maywood) 2004;229:383–392. doi: 10.1177/153537020422900506. [DOI] [PubMed] [Google Scholar]
- 170.Monsefi M., Alaee S., Moradshahi A., Rohani L. Cadmium-induced infertility in male mice. Environ. Toxicol. 2010;25:94–102. doi: 10.1002/tox.20468. [DOI] [PubMed] [Google Scholar]
- 171.Li X., Jiang X., Sun J., Zhu C., Li X., Tian L., Liu L., Bai W. Cytoprotective effects of dietary flavonoids against cadmium-induced toxicity. Ann. N. Y. Acad. Sci. 2017;1398:5–19. doi: 10.1111/nyas.13344. [DOI] [PubMed] [Google Scholar]
- 172.Arafa M.H., Mohammad N.S., Atteia H.H. Fenugreek seed powder mitigates cadmium-induced testicular damage and hepatotoxicity in male rats. Exp. Toxicol. Pathol. 2014;66:293–300. doi: 10.1016/j.etp.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 173.Abdel-Aziem S.H., El-Nekeety A.A., Barakat I.A., Mohamed M.I., Abdel-Wahhab M.A. Aquilegia vulgaris extract protects against the oxidative stress and the mutagenic effects of cadmium in Balb/c mice. Exp. Toxicol. Pathol. 2011;63:337–344. doi: 10.1016/j.etp.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 174.Cirmi S., Maugeri A., Micali A., Marini H.R., Puzzolo D., Santoro G., Freni J., Squadrito F., Irrera N., Pallio G., et al. Cadmium-Induced Kidney Injury in Mice Is Counteracted by a Flavonoid-Rich Extract of Bergamot Juice, Alone or in Association with Curcumin and Resveratrol, via the Enhancement of Different Defense Mechanisms. Biomedicines. 2021;9:1797. doi: 10.3390/biomedicines9121797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Ferlazzo N., Micali A., Marini H.R., Freni J., Santoro G., Puzzolo D., Squadrito F., Pallio G., Navarra M., Cirmi S., et al. A Flavonoid-Rich Extract from Bergamot Juice, Alone or in Association with Curcumin and Resveratrol, Shows Protective Effects in a Murine Model of Cadmium-Induced Testicular Injury. Pharmaceuticals. 2021;14:386. doi: 10.3390/ph14050386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Alshatwi A.A., Hasan T.N., Alqahtani A.M., Syed N.A., Shafi G., Al-Assaf A.H., Al-Khalifa A.S. Delineating the anti-cytotoxic and anti-genotoxic potentials of catechin hydrate against cadmium toxicity in human peripheral blood lymphocytes. Environ. Toxicol. Pharmacol. 2014;38:653–662. doi: 10.1016/j.etap.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 177.Barreca D., Trombetta D., Smeriglio A., Mandalari G., Romeo O., Felice M.R., Gattuso G., Nabavi S.M. Food flavonols: Nutraceuticals with complex health benefits and functionalities. Trends Food Sci. Technol. 2021;117:194–204. doi: 10.1016/j.tifs.2021.03.030. [DOI] [Google Scholar]
- 178.El-Diasty H.H., El-Sayyad H., Refaat S., El-Ghaweet H.A. Efficacy of Quercetin-Sensitized Cisplatin against N-Nitroso-NMethylurea Induced Testicular Carcinogenesis in Wistar Rats. Asian Pac. J. Cancer Prev. 2021;22:75–84. doi: 10.31557/APJCP.2021.22.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Psotova J., Lasovsky J., Vicar J. Metal-chelating properties, electrochemical behavior, scavenging and cytoprotective activities of six natural phenolics. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech. Repub. 2003;147:147–153. doi: 10.5507/bp.2003.020. [DOI] [PubMed] [Google Scholar]
- 180.Salehi B., Machin L., Monzote L., Sharifi-Rad J., Ezzat S.M., Salem M.A., Merghany R.M., El Mahdy N.M., Kilic C.S., Sytar O., et al. Therapeutic Potential of Quercetin: New Insights and Perspectives for Human Health. ACS Omega. 2020;5:11849–11872. doi: 10.1021/acsomega.0c01818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ola-Mudathir K.F., Suru S.M., Fafunso M.A., Obioha U.E., Faremi T.Y. Protective roles of onion and garlic extracts on cadmium-induced changes in sperm characteristics and testicular oxidative damage in rats. Food Chem. Toxicol. 2008;46:3604–3611. doi: 10.1016/j.fct.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 182.Bu T., Mi Y., Zeng W., Zhang C. Protective effect of quercetin on cadmium-induced oxidative toxicity on germ cells in male mice. Anat. Rec. (Hoboken) 2011;294:520–526. doi: 10.1002/ar.21317. [DOI] [PubMed] [Google Scholar]
- 183.Jia Y., Lin J., Mi Y., Zhang C. Quercetin attenuates cadmium-induced oxidative damage and apoptosis in granulosa cells from chicken ovarian follicles. Reprod. Toxicol. 2011;31:477–485. doi: 10.1016/j.reprotox.2010.12.057. [DOI] [PubMed] [Google Scholar]
- 184.Wang J., Zhu H., Wang K., Yang Z., Liu Z. Protective effect of quercetin on rat testes against cadmium toxicity by alleviating oxidative stress and autophagy. Environ. Sci. Pollut. Res. Int. 2020;27:25278–25286. doi: 10.1007/s11356-020-08947-2. [DOI] [PubMed] [Google Scholar]
- 185.Williamson G. The role of polyphenols in modern nutrition. Nutr. Bull. 2017;42:226–235. doi: 10.1111/nbu.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Henriques M.C., Loureiro S., Fardilha M., Herdeiro M.T. Exposure to mercury and human reproductive health: A systematic review. Reprod. Toxicol. 2019;85:93–103. doi: 10.1016/j.reprotox.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 187.Tortora F., Notariale R., Maresca V., Good K.V., Sorbo S., Basile A., Piscopo M., Manna C. Phenol-Rich Feijoa sellowiana (Pineapple Guava) Extracts Protect Human Red Blood Cells from Mercury-Induced Cellular Toxicity. Antioxidants. 2019;8:220. doi: 10.3390/antiox8070220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Piscopo M., Tenore G.C., Notariale R., Maresca V., Maisto M., de Ruberto F., Heydari M., Sorbo S., Basile A. Antimicrobial and antioxidant activity of proteins from Feijoa sellowiana Berg. fruit before and after in vitro gastrointestinal digestion. Nat. Prod. Res. 2020;34:2607–2611. doi: 10.1080/14786419.2018.1543686. [DOI] [PubMed] [Google Scholar]
- 189.Manzolli E.S., Serpeloni J.M., Grotto D., Bastos J.K., Antunes L.M., Barbosa Junior F., Barcelos G.R. Protective effects of the flavonoid chrysin against methylmercury-induced genotoxicity and alterations of antioxidant status, in vivo. Oxid. Med. Cell Longev. 2015;2015:602360. doi: 10.1155/2015/602360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Notariale R., Infantino R., Palazzo E., Manna C. Erythrocytes as a Model for Heavy Metal-Related Vascular Dysfunction: The Protective Effect of Dietary Components. Int. J. Mol. Sci. 2021;22:6604. doi: 10.3390/ijms22126604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Barbhuiya S.N., Barhoi D., Giri S. Impact of Arsenic on Reproductive Health. In: Otsuki T., editor. Environmental Health. IntechOpen; London, UK: 2021. [DOI] [Google Scholar]
- 192.Zadorozhnaja T.D., Little R.E., Miller R.K., Mendel N.A., Taylor R.J., Presley B.J., Gladen B.C. Concentrations of arsenic, cadmium, copper, lead, mercury, and zinc in human placentas from two cities in Ukraine. J. Toxicol. Environ. Health A. 2000;61:255–263. doi: 10.1080/00984100050136571. [DOI] [PubMed] [Google Scholar]
- 193.Shen S., Li X.F., Cullen W.R., Weinfeld M., Le X.C. Arsenic binding to proteins. Chem. Rev. 2013;113:7769–7792. doi: 10.1021/cr300015c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Pullella K., Kotsopoulos J. Arsenic Exposure and Breast Cancer Risk: A Re-Evaluation of the Literature. Nutrients. 2020;12:3305. doi: 10.3390/nu12113305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Quiller G., Merida-Ortega A., Rothenberg S.J., Cebrian M.E., Gandolfi A.J., Franco-Marina F., Lopez-Carrillo L. Dietary flavonoids improve urinary arsenic elimination among Mexican women. Nutr. Res. 2018;55:65–71. doi: 10.1016/j.nutres.2018.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Authority E.F.S. Bisphenol A: EFSA Draft Opinion Proposes Lowering the Tolerable Daily Intake. [(accessed on 15 December 2021)]. Available online: https://www.efsa.europa.eu/en/news/bisphenol-efsa-draft-opinion-proposes-lowering-tolerable-daily-intake.
- 197.De Toni L., Sabovic I., Cosci I., Ghezzi M., Foresta C., Garolla A. Testicular Cancer: Genes, Environment, Hormones. Front. Endocrinol. (Lausanne) 2019;10:408. doi: 10.3389/fendo.2019.00408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Matuszczak E., Komarowska M.D., Debek W., Hermanowicz A. The Impact of Bisphenol A on Fertility, Reproductive System, and Development: A Review of the Literature. Int. J. Endocrinol. 2019;2019:4068717. doi: 10.1155/2019/4068717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Maffini M.V., Rubin B.S., Sonnenschein C., Soto A.M. Endocrine disruptors and reproductive health: The case of bisphenol-A. Mol. Cell. Endocrinol. 2006;254–255:179–186. doi: 10.1016/j.mce.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 200.Markey C.M., Luque E.H., Munoz De Toro M., Sonnenschein C., Soto A.M. In utero exposure to bisphenol A alters the development and tissue organization of the mouse mammary gland. Biol. Reprod. 2001;65:1215–1223. doi: 10.1093/biolreprod/65.4.1215. [DOI] [PubMed] [Google Scholar]
- 201.Bulayeva N.N., Watson C.S. Xenoestrogen-induced ERK-1 and ERK-2 activation via multiple membrane-initiated signaling pathways. Environ. Health Perspect. 2004;112:1481–1487. doi: 10.1289/ehp.7175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Noguchi S., Nakatsuka M., Asagiri K., Habara T., Takata M., Konishi H., Kudo T. Bisphenol A stimulates NO synthesis through a non-genomic estrogen receptor-mediated mechanism in mouse endothelial cells. Toxicol. Lett. 2002;135:95–101. doi: 10.1016/S0378-4274(02)00252-7. [DOI] [PubMed] [Google Scholar]
- 203.Wei Y., Han C., Li S., Cui Y., Bao Y., Shi W. Cuscuta chinensis flavonoids down-regulate the DNA methylation of the H19/Igf2 imprinted control region and estrogen receptor alpha promoter of the testis in bisphenol A exposed mouse offspring. Food Funct. 2020;11:787–798. doi: 10.1039/C9FO02770J. [DOI] [PubMed] [Google Scholar]
- 204.Han D.H., Denison M.S., Tachibana H., Yamada K. Relationship between estrogen receptor-binding and estrogenic activities of environmental estrogens and suppression by flavonoids. Biosci. Biotechnol. Biochem. 2002;66:1479–1487. doi: 10.1271/bbb.66.1479. [DOI] [PubMed] [Google Scholar]
- 205.Meli R., Monnolo A., Annunziata C., Pirozzi C., Ferrante M.C. Oxidative Stress and BPA Toxicity: An Antioxidant Approach for Male and Female Reproductive Dysfunction. Antioxidants. 2020;9:405. doi: 10.3390/antiox9050405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Kumar S., Sharma A., Thaker R. Air pollutants and impairments of male reproductive health-an overview. Rev. Environ. Health. 2021;36:565–575. doi: 10.1515/reveh-2020-0136. [DOI] [PubMed] [Google Scholar]
- 207.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans Some non-heterocyclic polycyclic aromatic hydrocarbons and some related exposures. IARC Monogr. Eval. Carcinog. Risks Hum. 2010;92:1–853. [PMC free article] [PubMed] [Google Scholar]
- 208.Vogel C.F.A., Van Winkle L.S., Esser C., Haarmann-Stemmann T. The aryl hydrocarbon receptor as a target of environmental stressors—Implications for pollution mediated stress and inflammatory responses. Redox Biol. 2020;34:101530. doi: 10.1016/j.redox.2020.101530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gutierrez-Vazquez C., Quintana F.J. Regulation of the Immune Response by the Aryl Hydrocarbon Receptor. Immunity. 2018;48:19–33. doi: 10.1016/j.immuni.2017.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Xia W., Wong E.W., Mruk D.D., Cheng C.Y. TGF-beta3 and TNFalpha perturb blood-testis barrier (BTB) dynamics by accelerating the clathrin-mediated endocytosis of integral membrane proteins: A new concept of BTB regulation during spermatogenesis. Dev. Biol. 2009;327:48–61. doi: 10.1016/j.ydbio.2008.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Roychoudhury S., Chakraborty S., Choudhury A.P., Das A., Jha N.K., Slama P., Nath M., Massanyi P., Ruokolainen J., Kesari K.K. Environmental Factors-Induced Oxidative Stress: Hormonal and Molecular Pathway Disruptions in Hypogonadism and Erectile Dysfunction. Antioxidants. 2021;10:837. doi: 10.3390/antiox10060837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Poljsak B., Fink R. The protective role of antioxidants in the defence against ROS/RNS-mediated environmental pollution. Oxid. Med. Cell. Longev. 2014;2014:671539. doi: 10.1155/2014/671539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Matzkin M.E., Calandra R.S., Rossi S.P., Bartke A., Frungieri M.B. Hallmarks of Testicular Aging: The Challenge of Anti-Inflammatory and Antioxidant Therapies Using Natural and/or Pharmacological Compounds to Improve the Physiopathological Status of the Aged Male Gonad. Cells. 2021;10:3114. doi: 10.3390/cells10113114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Griffiths K., Aggarwal B.B., Singh R.B., Buttar H.S., Wilson D., De Meester F. Food Antioxidants and Their Anti-Inflammatory Properties: A Potential Role in Cardiovascular Diseases and Cancer Prevention. Diseases. 2016;4:28. doi: 10.3390/diseases4030028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Mani V.M., Soundari A., Balasubramanian B., Park S., Issara U., Preethi K., Liu W.C. Evaluation of Dimer of Epicatechin from an Endophytic Fungus Curvularia australiensis FC2AP on Acute Toxicity Levels, Anti-Inflammatory and Anti-Cervical Cancer Activity in Animal Models. Molecules. 2021;26:654. doi: 10.3390/molecules26030654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Kim M., Jee S.C., Kim K.S., Kim H.S., Yu K.N., Sung J.S. Quercetin and Isorhamnetin Attenuate Benzo[a]pyrene-Induced Toxicity by Modulating Detoxification Enzymes through the AhR and NRF2 Signaling Pathways. Antioxidants. 2021;10:787. doi: 10.3390/antiox10050787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Singletary K.W., Jung K.J., Giusti M. Anthocyanin-rich grape extract blocks breast cell DNA damage. J. Med. Food. 2007;10:244–251. doi: 10.1089/jmf.2006.258. [DOI] [PubMed] [Google Scholar]
- 218.Androutsopoulos V.P., Tsatsakis A.M. Benzo[a]pyrene sensitizes MCF7 breast cancer cells to induction of G1 arrest by the natural flavonoid eupatorin-5-methyl ether, via activation of cell signaling proteins and CYP1-mediated metabolism. Toxicol. Lett. 2014;230:304–313. doi: 10.1016/j.toxlet.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 219.EFSA Panel on Contaminants in the Food Chain (CONTAM) Knutsen H.K., Alexander J., Barregård L., Bignami M., Brüschweiler B., Ceccatelli S., Cottrill B., Dinovi M., Edler L., et al. Risk for animal and human health related to the presence of dioxins and dioxin-like PCBs in feed and food. EFSA J. 2018;16:e05333. doi: 10.2903/j.efsa.2018.5333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Xu J., Ye Y., Huang F., Chen H., Wu H., Huang J., Hu J., Xia D., Wu Y. Association between dioxin and cancer incidence and mortality: A meta-analysis. Sci. Rep. 2016;6:38012. doi: 10.1038/srep38012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Mocarelli P., Gerthoux P.M., Patterson D.G., Jr., Milani S., Limonta G., Bertona M., Signorini S., Tramacere P., Colombo L., Crespi C., et al. Dioxin exposure, from infancy through puberty, produces endocrine disruption and affects human semen quality. Environ. Health Perspect. 2008;116:70–77. doi: 10.1289/ehp.10399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Kolluri S.K., Jin U.H., Safe S. Role of the aryl hydrocarbon receptor in carcinogenesis and potential as an anti-cancer drug target. Arch. Toxicol. 2017;91:2497–2513. doi: 10.1007/s00204-017-1981-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Gu A., Ji G., Long Y., Zhou Y., Shi X., Song L., Wang X. Assessment of an association between an aryl hydrocarbon receptor gene (AHR) polymorphism and risk of male infertility. Toxicol. Sci. 2011;122:415–421. doi: 10.1093/toxsci/kfr137. [DOI] [PubMed] [Google Scholar]
- 224.Goya-Jorge E., Jorge Rodriguez M.E., Veitia M.S., Giner R.M. Plant Occurring Flavonoids as Modulators of the Aryl Hydrocarbon Receptor. Molecules. 2021;26:2315. doi: 10.3390/molecules26082315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Romagnolo D.F., Donovan M.G., Papoutsis A.J., Doetschman T.C., Selmin O.I. Genistein Prevents BRCA1 CpG Methylation and Proliferation in Human Breast Cancer Cells with Activated Aromatic Hydrocarbon Receptor. Curr. Dev. Nutr. 2017;1:e000562. doi: 10.3945/cdn.117.000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Donovan M.G., Selmin O.I., Doetschman T.C., Romagnolo D.F. Epigenetic Activation of BRCA1 by Genistein In Vivo and Triple Negative Breast Cancer Cells Linked to Antagonism toward Aryl Hydrocarbon Receptor. Nutrients. 2019;11:2559. doi: 10.3390/nu11112559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Tan Y.Q., Chiu-Leung L.C., Lin S.M., Leung L.K. The citrus flavonone hesperetin attenuates the nuclear translocation of aryl hydrocarbon receptor. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2018;210:57–64. doi: 10.1016/j.cbpc.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 228.Kitakaze T., Makiyama A., Nakai R., Kimura Y., Ashida H. Kaempferol modulates TCDD- and t-BHQ-induced drug-metabolizing enzymes and luteolin enhances this effect. Food Funct. 2020;11:3668–3680. doi: 10.1039/C9FO02951F. [DOI] [PubMed] [Google Scholar]
- 229.Jin U.H., Park H., Li X., Davidson L.A., Allred C., Patil B., Jayaprakasha G., Orr A.A., Mao L., Chapkin R.S., et al. Structure-Dependent Modulation of Aryl Hydrocarbon Receptor-Mediated Activities by Flavonoids. Toxicol. Sci. 2018;164:205–217. doi: 10.1093/toxsci/kfy075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.EFSA Panel on Food Contact Materials, Enzymes and Processing Aids (CEP) Aids P., Silano V., Barat Baviera J.M., Bolognesi C., Chesson A., Cocconcelli P.S., Crebelli R., Gott D.M., Grob K., et al. Update of the risk assessment of di-butylphthalate (DBP), butyl-benzyl-phthalate (BBP), bis(2-ethylhexyl)phthalate (DEHP), di-isononylphthalate (DINP) and di-isodecylphthalate (DIDP) for use in food contact materials. EFSA J. 2019;17:e05838. doi: 10.2903/j.efsa.2019.5838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Hlisnikova H., Petrovicova I., Kolena B., Sidlovska M., Sirotkin A. Effects and Mechanisms of Phthalates’ Action on Reproductive Processes and Reproductive Health: A Literature Review. Int. J. Environ. Res. Public Health. 2020;17:6811. doi: 10.3390/ijerph17186811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Feng X., Ma B.F., Liu B., Ding P., Wei J.H., Cheng P., Li S.Y., Chen D.X., Sun Z.J., Li Z. The Involvement of the Chemokine RANTES in Regulating Luminal Acidification in Rat Epididymis. Front. Immunol. 2020;11:583274. doi: 10.3389/fimmu.2020.583274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Rebourcet D., Odet F., Verot A., Combe E., Meugnier E., Pesenti S., Leduque P., Dechaud H., Magre S., Le Magueresse-Battistoni B. The effects of an in utero exposure to 2,3,7,8-tetrachloro-dibenzo-p-dioxin on male reproductive function: Identification of Ccl5 as a potential marker. Int. J. Androl. 2010;33:413–424. doi: 10.1111/j.1365-2605.2009.01020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hsu Y.L., Hsieh C.J., Tsai E.M., Hung J.Y., Chang W.A., Hou M.F., Kuo P.L. Didymin reverses phthalate ester-associated breast cancer aggravation in the breast cancer tumor microenvironment. Oncol. Lett. 2016;11:1035–1042. doi: 10.3892/ol.2015.4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Merida-Ortega A., Hernandez-Alcaraz C., Hernandez-Ramirez R.U., Garcia-Martinez A., Trejo-Valdivia B., Salinas-Rodriguez A., Svensson K., Cebrian M.E., Franco-Marina F., Lopez-Carrillo L. Phthalate exposure, flavonoid consumption and breast cancer risk among Mexican women. Environ. Int. 2016;96:167–172. doi: 10.1016/j.envint.2016.08.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.