Abstract
Background Non-contrast computed tomography (CT) scanning allows for reliable coronary calcium score (CCS) calculation at a low radiation dose and has been well established as marker to assess the future risk of coronary artery disease (CAD) events in asymptomatic individuals. However, the diagnostic and prognostic value in symptomatic patients remains a matter of debate. This narrative review focuses on the available evidence for CCS in patients with stable chest pain complaints.
Method PubMed, Embase, and Web of Science were searched for literature using search terms related to three overarching categories: CT, symptomatic chest pain patients, and coronary calcium. The search resulted in 42 articles fulfilling the inclusion and exclusion criteria: 27 articles (n = 38 137 patients) focused on diagnostic value and 23 articles (n = 44 683 patients) on prognostic value of CCS. Of these, 10 articles (n = 21 208 patients) focused on both the diagnostic and prognostic value of CCS.
Results Between 22 and 10 037 patients were included in the studies on the diagnostic and prognostic value of CCS, including 43 % and 51 % patients with CCS 0. The most evidence is available for patients with a low and intermediate pre-test probability (PTP) of CAD. Overall, the prevalence of obstructive CAD (OCAD, defined as a luminal stenosis of ≥ 50 % in any of the coronary arteries) as determined with CT coronary angiography in CCS 0 patients, was 4.4 % (n = 703/16 074) with a range of 0–26 % in individual studies. The event rate for major adverse cardiac events (MACE) ranged from 0 % to 2.1 % during a follow-up of 1.6 to 6.8 years, resulting in a high negative predictive value for MACE between 98 % and 100 % in CCS 0 patients. At increasing CCS, the OCAD probability and MACE risk increased. OCAD was present in 58.3 % (n = 617/1058) of CCS > 400 patients with percentages ranging from 20 % to 94 % and MACE occurred in 16.7 % (n = 175/1048) of these patients with percentages ranging from 6.9 % to 50 %.
Conclusion Accumulating evidence shows that OCAD is unlikely and the MACE risk is very low in symptomatic patients with CCS 0, especially in those with low and intermediate PTPs. This suggests a role of CCS as a gatekeeper for additional diagnostic testing. Increasing CCS is related to an increasing probability of OCAD and risk of cardiac events. Additional research is needed to assess the value of CCS in women and patient management in a primary healthcare setting.
Key Points:
A CCS of zero makes OCAD in patients at low-intermediate PTP unlikely
A CCS of zero is related to a very low risk of MACE
Categories of increasing CCS are related to increasing rates of OCAD and MACE
Future studies should focus on the diagnostic and prognostic value of CCS in symptomatic women and the role in primary care
Citation Format
Koopman MY, Willemsen RT, van der Harst P et al. The Diagnostic and Prognostic Value of Coronary Calcium Scoring in Stable Chest Pain Patients: A Narrative Review. Fortschr Röntgenstr 2022; 194: 257 – 265
Key words: computed tomography, chest pain, coronary calcium score, coronary artery disease, cardiovascular diseases
Zusammenfassung
Hintergrund Die kontrastfreie Computertomografie (CT) ermöglicht eine zuverlässige Berechnung des koronaren Kalziumscores (KKS) bei niedriger Strahlendosis und hat sich als Marker zur Beurteilung des Risikos für koronare Herzkrankheiten (KHK) bei asymptomatischen Personen bewährt. Der diagnostische und prognostische Wert bei symptomatischen Patienten bleibt jedoch umstritten. Die vorliegende Übersichtsarbeit befasst sich mit der verfügbaren Evidenz des KKS bei Patienten mit stabilen Brustschmerzbeschwerden.
Methode In PubMed, Embase und Web of Science wurde eine Literaturrecherche mit Suchbegriffen zu drei übergeordneten Kategorien durchgeführt: CT, Patienten mit symptomatischen Brustschmerzen und Koronarkalk. Die Suche ergab 42 Artikel, die die Ein- und Ausschlusskriterien erfüllten: 27 Artikel (n = 38 137 Patienten) konzentrierten sich auf den diagnostischen Wert und 23 Artikel (n = 44 683 Patienten) auf den prognostischen Wert des KKS. Davon befassten sich 10 Artikel (n = 21 208 Patienten) mit dem diagnostischen und dem prognostischen Wert des KKS.
Ergebnisse In die Studien zum diagnostischen und prognostischen Wert des KKS wurden zwischen 22 und 10 037 Patienten eingeschlossen, darunter 43 % bzw. 51 % Patienten mit KKS0. Die meisten Erkenntnisse liegen für Patienten mit einer niedrigen und mittleren Prätestwahrscheinlichkeit (PTP) für KHK vor. Insgesamt lag die Prävalenz der obstruktiven KHK (OKHK, definiert als luminale Stenose von ≥ 50 % in einer der Koronararterien), die mittels CT-Koronarangiografie bei KKS0-Patienten bestimmt wurde, bei 4,4 % (n = 703/16 074) mit einem Bereich von 0–26 % in einzelnen Studien. Die Ereignisrate für schwerwiegende unerwünschte kardiale Ereignisse („major adverse cardiac events“ MACE) reichte von 0 % bis 2,1 % während einer Nachbeobachtungszeit von 1,6 bis 6,8 Jahren, was bei KKS 0-Patienten zu einem hohen negativen Vorhersagewert für MACE zwischen 98 % und 100 % führte. Mit zunehmendem KKS stiegen die OKHK-Wahrscheinlichkeit und das MACE-Risiko. Bei 58,3 % (n = 617/1058) der Patienten mit einem KKS > 400 lag eine OKHK vor, wobei die Spanne von 20 % bis 94 % reichte. Bei 16,7 % (n = 175/1048) dieser Patienten trat ein MACE auf, mit einer Spanne von 6,9 % bis 50 %.
Schlussfolgerung Es gibt zunehmend mehr Hinweise darauf, dass bei symptomatischen Patienten mit KKS0 eine OKHK unwahrscheinlich und das MACE-Risiko sehr gering ist, insbesondere bei den Patienten mit niedriger und mittlerer PTP. Dies weist auf eine „Torwächter“-Rolle des KKS hinsichtlich zusätzlicher diagnostischer Tests hin. Mit zunehmendem KKS steigt sowohl die Wahrscheinlichkeit einer OKHK als das Risiko für kardiale Ereignisse. Weitere Forschungsarbeiten sind erforderlich, um den Wert des KKS bei Frauen und beim Patientenmanagement im Rahmen der medizinischen Grundversorgung zu bewerten.
1. Background
Coronary artery calcification can be quantified based on non-contrast computed tomography (CT) scanning and is quantified using a coronary calcium score (CCS) according to Agatston’s method 1 2 . Coronary calcium is a component of atherosclerosis and a marker for the presence of (subclinical) coronary artery disease (CAD). Multiple large-scale population-based studies with long-term follow-up have shown the strong predictive power of the CCS for major adverse cardiac events (MACE) 3 4 5 . Non-contrast CT scanning yields reliable CCS results at a low radiation dose (0.5–1 mSv) and low cost and is associated with low patient burden (e. g., no intravenous line needed, no exposure to contrast material, very short breath-hold, and short scan visit) 3 4 5 . However, in patients with stable chest pain, the diagnostic value of CCS for obstructive CAD (OCAD, defined as luminal stenosis of ≥ 50 % in any coronary artery) and the prognostic value of CCS for MACE remain unclear. The 2012 American Heart Association and American College of Cardiology (AHA/ACC) guidelines deemed CCS evaluation appropriate for patients with a low to intermediate pre-test probability (PTP) of OCAD (based on age, sex, and type of complaints). However, CCS was not included in the latest update in 2014 6 7 . The National Institute for Health and Care Excellence (NICE) guidelines (2010) also recommended CCS as a gatekeeper in low PTP patients, but it was not included in the latest version from 2016 8 9 . Recommendations in these guidelines were based on the latest data, suggesting that CCS 0 cannot fully exclude OCAD in patients with new onset of chest pain symptoms. However, new evidence with regard to CCS in chest pain patients has emerged since the publication of these guidelines. In the European Society of Cardiology guidelines of 2019, CCS is suggested to have a role as a PTP modifier in the very low PTP group 10 , showing that the role of the CCS in clinical decision making remains a matter of debate. This review describes the latest evidence on the diagnostic and prognostic value of CCS in stable chest pain patients.
2. Method
A search was performed in PubMed, Embase, and Web of Science with the latest update on April 20, 2021 using search terms related to three overarching categories: CT, symptomatic chest pain patients, and coronary calcium. An overview of the specific search terms and a summary of the search can be found in the Supplement. The flowchart ( Fig. 1 ) shows the result of the search and the inclusion and exclusion criteria. Eventually, 42 articles were included in this review. Of these, 19 articles described the diagnostic value, 13 articles described the prognostic value and 10 articles described both the diagnostic and prognostic value of the CCS.
Fig. 1.
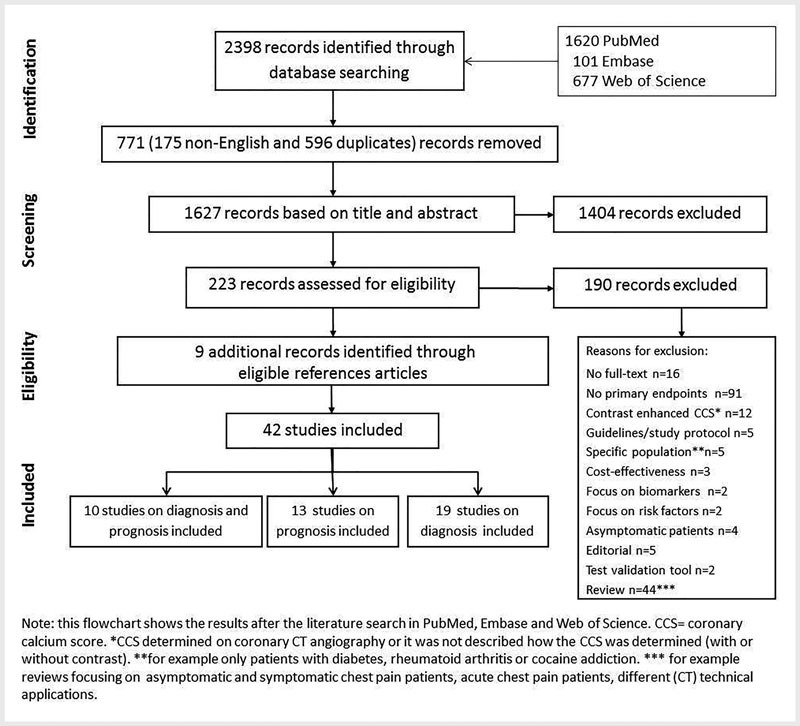
Flowchart of inclusion and exclusion of articles.
3. Diagnostic Value of Coronary Calcium Score
Supplementary Table 1, 2 describe articles assessing the diagnostic value of the CCS to determine OCAD in stable chest pain patients. In these studies, OCAD was based on coronary computed tomography angiography (cCTA, n = 25) or invasive coronary angiography (n = 2). All studies were performed in secondary care settings. The diagnostic value of CCS was determined in patients with stable chest pain. Per study the number of patients ranged from 22 to 10 037. 11 of the studies involved large cohorts of > 1000 patients 11 12 13 14 15 16 17 18 19 20 21 . In most studies (17/27, 64 %), the majority of included patients were men, with the mean age ranging from 53 ± 11 to 65 ± 11 years. The PTP estimation of patients for OCAD was described in 19 studies, five studies described the type of angina pectoris (AP) symptoms, and three studies did not describe PTP or AP symptoms ( Supplementary Table 1, 2 ). PTP is used to determine the probability of OCAD and is based on age, sex, and chest pain complaints. The estimations of OCAD probability were not consistently described in the included studies. In general, a low PTP indicates a probability of OCAD of 5–15 %, intermediate PTP indicates a probability of 15–65 %, and a high PTP indicates a probability of over 65 % 10 . To determine the CCS, different CT systems were used: electron beam CT (EBCT) was used in four studies, 64-slice multi-detector CT (MDCT) in 15 studies, and dual-source CT (DSCT) scanners in eight studies ( Supplementary Table 1, 2 ). Also, different CCS categories were used in the studies ( Supplementary Table 2 ). Below, to increase readability, we describe the diagnostic value of CCS 0 and CCS > 0 (evidence for the positive CCS categories combined).
3.1. Coronary calcium score of zero and OCAD
27 studies focused on the potential value of CCS 0 in the work-up of patients with stable chest pain, in particular to determine whether the absence of coronary calcium safely rules out the presence of OCAD. The percentage of patients with CCS 0 (n = 16 074/38 137, 42 %) ranged from 7.3 % to 89 % in individual studies. Overall, 4.4 % of CCS 0 patients had OCAD (n = 703/16 074). In individual studies the prevalence ranged from 0 % to 26 % 11 12 13 14 15 16 17 18 19 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 . Studies using EBCT and 64-MDCT (N = 18 studies, 14 554 patients) found OCAD in 1.9 % to 26 % of CCS 0 patients ( Supplementary Table 1 ) 11 12 13 14 15 16 18 23 24 25 26 28 29 30 31 35 . In studies using newer CT technologies (N = 9 studies, n = 4305) the OCAD prevalence was lower, and ranged from 0 % to 8.4 % (overall, 167/4861, 3.4 %) 17 18 19 27 32 33 34 36 .
In the majority of studies (64 %), less than 5 % of CCS 0 patients were diagnosed with OCAD 11 12 13 14 15 17 18 19 21 25 27 28 32 33 34 36 37 . Evidence is based on large cohort studies that included relatively high numbers of patients with CCS 0 (n = 92–5128). The other studies showed higher percentages (5.3 %) of OCAD in CCS 0 patients, but most of these studies consisted of relatively small cohorts that were scanned with older CT scanner generations 16 23 24 26 31 . Only one study with a higher OCAD prevalence (5.7 %) in CCS 0 patients consisted of a large cohort (n = 5515) 16 .
An important issue is whether the negative predictive value (NPV) of CCS for OCAD depends on the PTP and type of AP symptoms 10 . Four studies included a low PTP population, where OCAD percentages ranged from 1.5 % to 5.7 % in the CCS 0 subgroup ( Supplementary Table 1 ; Fig. 2 ). Overall, 215 of 5349 CCS 0 patients had OCAD (4.0 %) 12 16 18 36 . In the study with the most CCS 0 patients, 3.7 % of low PTP patients were diagnosed with OCAD (n = 90/2406) 12 . In seven studies a low and intermediate PTP population was included, and OCAD in CCS 0 patients ranged from 1.5 % to 5.8 % (412/9139 OCAD, 4.5 %). Five of these seven studies also described type of symptoms 13 14 17 19 21 28 31 . The largest cohort comprised n = 10 037 low and intermediate PTP patients including 13 % with typical symptoms. In this study, 5.1 % of CCS 0 patients (n = 244/5128) were diagnosed with OCAD 13 . In three small-scale intermediate PTP cohorts, the percentage of OCAD ranged from 0 % to 2 % in CCS 0 (total size CCS 0: n = 83, 121, 174) 15 27 32 . In the remaining four studies, with an intermediate and high PTP (n = 2) and with a high PTP (n = 2), OCAD prevalence in CCS 0 patients was higher, 3.6 % to 26 % (overall: 54/822 CCS 0 patients, 6.6 %) 23 29 30 34 . With regard to type of symptoms, in five studies ( Supplementary Table 1 ) consisting mostly of patients with either atypical or typical AP symptoms, OCAD was present in 0 % to 5.7 % of the CCS 0 patients 11 25 26 33 37 . In summary, OCAD is unlikely in CCS 0 patients, especially in patients with a low and intermediate PTP.
Fig. 2.
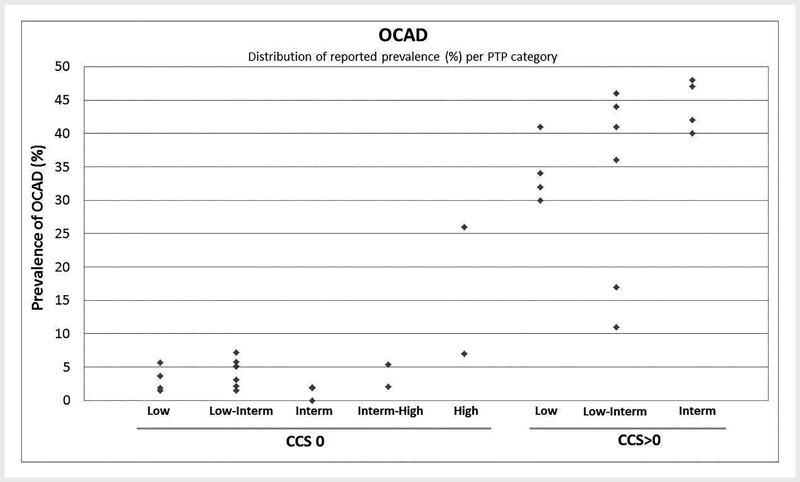
Prevalence of obstructive coronary artery disease (OCAD) per pre-test probability (PTP) category for coronary calcium score (CCS) 0 and CCS > 0; display of reported results in the studies with patient population in the indicated PTP category.
3.2. Coronary calcium score of zero and non-obstructive CAD
Two studies described the cCTA-based prevalence of non-calcified plaques in patients with CCS 0. Non-calcified plaques were found in 16 % (n = 24/147) and 6.6 % (n = 37/557) of CCS 0 patients ( Supplementary Table 1 ) 17 28 . In the largest study consisting of a low and intermediate PTP population, 37 of 557 CCS 0 patients (6.6 %) had non-calcified plaques, of whom 21 % (n = 8/37) were diagnosed with OCAD 17 . Ten studies reported non-OCAD as defined by luminal stenosis of < 50 % on cCTA in CCS 0 patients. In total, 14 % of patients had non-OCAD (n = 901/6702) with percentages ranging from 6.9 % to 74 % ( Supplementary Table 1 ) 13 15 18 21 22 24 26 28 29 35 . The two studies with high percentages of non-OCAD (25 % and 74 %) had outlier results due to the small number of patients in the CCS 0 category (n = 8, 61) 22 29 . In summary, non-OCAD can be present in CCS 0 patients.
3.3. Positive coronary calcium score and OCAD
Patients with CCS> 0 (n = 20 013/38 137, 52 %) were included in 27 studies. OCAD was diagnosed in 11–100 % of patients with CCS > 0 ( Supplementary Table 2 ) 11 14 15 16 17 18 22 23 26 . Studies including the CCS 1–100 category (n = 7) showed that 8–63 % of the patients had OCAD 12 24 25 27 28 32 33 35 . This increased to 8–76 % for the CCS 100–400 category (n = 7) 12 25 27 31 32 33 35 and to 20–94 % for the CCS > 400 category (n = 10) 12 25 27 28 31 32 33 35 36 37 .
In low PTP populations ( Supplementary Table 2 ; Fig. 2 ), 30–40 % of patients with a CCS > 0 were diagnosed with OCAD 12 16 18 36 . In seven studies comprising low and intermediate PTP populations ( Supplementary Table 2 ), the prevalence of OCAD increased to 40–92 % in the case of a CCS > 0 13 14 17 19 21 28 31 . In the largest study (n = 10 037), 44 % of CCS> 0 patients (n = 1825/4009) were diagnosed with OCAD 13 17 27 31 . In the four intermediate PTP studies, 40–48 % of CCS > 0 patients had OCAD 15 20 27 32 . Finally, the prevalence of OCAD in CCS > 0 patients with an intermediate and high PTP increased to 68 %–89 % 23 30 . Lastly, in the studies in which only type of symptoms was included ( Supplementary Table 2 ), comprising in particular atypical and typical AP patients, 15–71 % of CCS > 0 patients were diagnosed with OCAD 11 25 26 33 . In summary, CCS > 0 is related to a higher prevalence of OCAD than CCS 0. The probability of OCAD increases with a higher PTP and higher CCS, in particular in the case of CCS > 400.
4. Prognostic Value of Coronary Calcium Score
The prognostic value of the CCS in stable chest pain patients was studied in 23 articles, all performed in secondary care settings. Supplementary Table 3, 4 describe the number of patients diagnosed with MACE per CCS category and during which follow-up period. The number of patients ranged from 134 to 10 037 per study. 11 studies included large cohorts of > 1000 patients 12 13 14 15 18 19 21 38 39 40 41 . In most studies, the majority of the included patients were men (14/23, 61 %). The mean age ranged from 53 ± 11 to 65 ± 10 years. EBCT scanners were used in 2 studies, 64-slice MDCT scanners in 18 studies, and dual-source CT scanners in 3 studies. The PTP estimation of OCAD was described in 14 studies, while two studies only described the type of symptoms and the remaining studies (n = 7) did not describe PTP or type of symptoms ( Supplementary Table 3, 4 ). Different CCS categories were used in the studies. To increase readability, the prognostic value is described for CCS 0 and CCS > 0 (evidence of the CCS > 0 categories together).
4.1. Coronary calcium score of zero and MACE
MACE rates in stable chest pain patients with CCS 0 were reported in 19 studies ( Supplementary Table 3 ). CCS 0 was present in 27–100 % of the included cohorts 12 13 14 15 18 19 28 38 39 40 41 42 43 44 45 46 47 48 . Of the CCS 0 patients, 0–2.1 % suffered from MACE during a follow-up period from 1.6 to 6.8 years 12 13 14 15 18 19 28 38 39 40 41 42 43 45 46 48 . In low PTP populations, MACE in CCS 0 patients ranged from 0.1 % to 0.6 % during a follow-up of 2.2 years ( Supplementary Table 3 ; Fig. 3 ) 12 18 . Event rates increased slightly, up to 1.4 %, in low and intermediate PTP populations with CCS 0 (follow-up of 2.1–6–8 years) 13 14 19 21 28 40 42 46 . The study including the largest cohort within this PTP category (n = 10 037) reported an event rate of 0.9 % (n = 44/4738) in CCS 0 patients during a follow-up of 4.2 years 13 . In intermediate PTP populations, event rates in CCS 0 patients were 0–0.5 % during a follow-up of 1.9–2.4 years 15 43 45 . Within this category, the largest study (n = 1145) reported an event rate of 0.5 % in CCS 0 patients (n = 2/483) 15 . Finally, in the intermediate and high PTP study, the event rate was 1.4 % (n = 28/1978 patients) during a follow-up of 5.2 years 41 . In summary, MACE rates in CCS 0 patients are very low even in higher PTP patients, during short to intermediate duration follow-up. However, most evidence is derived from low and intermediate PTP populations.
Fig. 3.
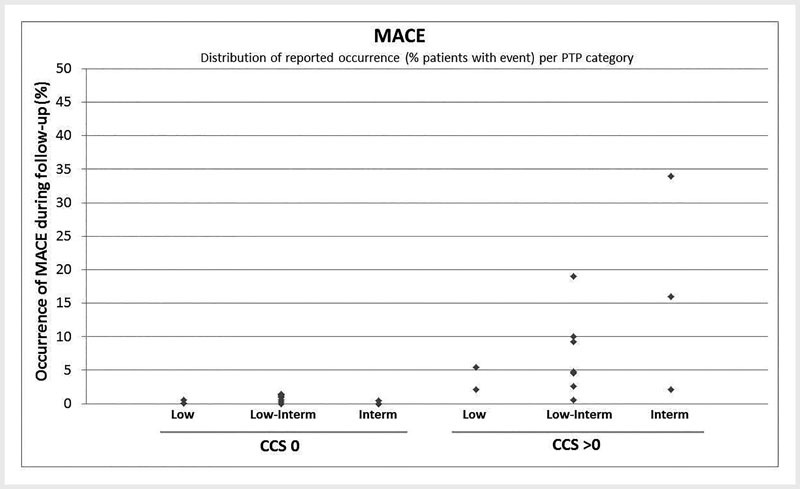
Occurrence of major adverse cardiac events (MACE) during follow-up (% patients with event) per pre-test probability (PTP) for coronary calcium score (CCS) 0 and CCS > 0; distribution based on results in the studies in the different PTP categories.
4.2. Positive coronary calcium score (CCS > 0) and MACE
21 studies reported the event rate of MACE in patients with CCS > 0 ( Supplementary Table 4 ) 12 13 14 15 18 19 28 38 39 40 41 42 43 44 45 46 47 . Event rates ranged from 0.6 % to 34 % during a follow-up of 1 to 6.8 years 12 13 14 15 18 19 21 28 37 38 39 40 42 43 45 46 . Studies including CCS 1–100 (n = 5) showed event rates from 1.4–13 % during a follow-up of 2–3 years 28 38 39 42 43 . Event rates increased to 3.7–34 % in the CCS 100–400 category (n = 7 studies, follow-up 1.7–3 years) 21 28 38 39 42 43 49 and to 6.9–50 % in the CCS > 400 category (n = 8 studies, follow-up 1.7–7 years) 21 28 37 38 39 42 43 46 .
In low PTP populations, 2.0–5.4 % of CCS > 0 patients suffered from MACE ( Supplementary Table 4 ; Fig. 3 ) 12 18 . In the low and intermediate PTP populations, event rates increased to 4.7–19 % 13 14 19 21 28 40 42 46 . The highest event rate of 19 % (n = 22/114) was reported in the smallest cohort (n = 155) with the longest follow-up (6.8 years) 46 . In comparison, the largest study (n = 10 037) reported a much lower event rate of 4.8 % in CCS > 0 patients (n = 19/4169 patients) during a follow-up of 4.1 years 13 . In intermediate PTP populations, the event rate in CCS > 0 patients ranged from 2.1 % to 34 % during a follow-up of 1.9–2.4 years 15 43 45 . In the largest intermediate PTP cohort (n = 1145), the MACE rate was 2.1 % (n = 14/622) during a follow-up of 2.4 years 15 . Finally, in an intermediate and high PTP cohort, the event rate of patients was 6.1 % (n = 119/1936) after a follow-up of 5.2 years 41 . In summary, patients with CCS > 0 experience a higher MACE rate compared to CCS 0 patients, and this risk increases with increasing CCS category. The highest MACE rates are seen in intermediate and high PTP populations, taking large cohorts (> 1000 patients) into account. However, these populations also had a higher distribution of CCS results. Lastly, there are few studies with a follow-up period of more than 5 years.
5. Value of coronary calcium scoring in stable chest pain
Current evidence shows that the large group of symptomatic patients with CCS 0 have a low prevalence rate of OCAD (overall: 4.5 %) and a very low risk of MACE (0–2.1 %). Evidence is mostly derived from low and intermediate PTP populations. Importantly, nearly half of the patients with stable chest pain, as included in the studies, have no coronary calcium. A trend was seen towards lower OCAD probability in CCS 0 patients in studies using newer CT technology (overall OCAD prevalence, 3 %), indicating higher sensitivity for coronary calcium detection. Thus, the possibility of the exclusion of coronary calcium and the clinical value are likely to become better with newer CT systems. For example, a first study using a photon-counting detector system has shown better calcium-soft tissue contrast in comparison with common energy-integrating detector CT systems, improving the diagnostic image quality of CCS, but research is still limited 50 . Thus, CCS 0 is a reassuring finding, in which OCAD is unlikely, and initial wait-and-see management may be considered, particularly since multiple prognostic studies show a very high NPV of CCS 0 for MACE. In contrast, patients with CCS > 0 often have OCAD and are at increased risk for MACE. Risk increases with increasing CCS, especially in patients with a CCS > 400. Despite substantial evidence supporting a role of CCS testing to make underlying OCAD unlikely, the most recent guidelines on the management of stable chest pain patients describe a limited role for the CCS. The AHA/ACC and NICE guidelines previously recommended CCS as a gatekeeper in low-intermediate PTP patients. However, this advice was not maintained in the latest versions of these guidelines, where CCS is not mentioned or not advised to be used as a standalone test 6 7 8 9 . Recommendations in these guidelines were based on data up to 2016. Additional reasoning was that CCS 0 alone cannot exclude OCAD and that cCTA is a more accurate standard that can directly assess the severity of the degree of stenosis, and thus should be used in those with new onset chest pain 6 7 8 9 . However, in certain cases, cCTA can cause an overestimation of the severity of CAD degree that may require additional functional testing for disease management 51 . According to the latest ECS guidelines (2019), the presence or absence of coronary calcium on non-contrast cardiac CT can be used as a decision aid in patients with a very low PTP, in order to establish the need for further diagnostic workup 10 . In addition, in the AHA/ACC guidelines (2019) on the management of cholesterol, CCS is recommended in intermediate risk, asymptomatic patients where the treatment decision based on risk-enhancing factors (e. g., diabetes, smoking, gender) is unclear. Patients with a CCS 0 can be classified in a lower risk category. In those with a CCS > 0, statin therapy is favored (CCS 1–99) or initiated (CCS > 100) 52 . Our systematic review results suggest that the negative predictive value of the CCS 0 for the occurrence of cardiovascular events in symptomatic patients is similar to the described, very high negative predictive value in asymptomatic populations (e. g., MESA cohort) 53 54 . The results of this review again confirm that CCS 0 is related to low OCAD probability and very low MACE rate, also in symptomatic patients. This supports a potential broader role as gatekeeper for additional testing and initial wait-and-see management in cases of CCS 0 in stable chest pain patients. The CRESCENT study compared CCS combined with cCTA to functional testing. This study incorporated a management strategy in which CCS 0 patients did not undergo cCTA 51 . As a result, cCTA could be withheld in 39 % (n = 98) of patients without comprising outcome (OCAD and MACE). This also reduced the mean radiation exposure from 4.1 mSv to 1.3 mSv 51 . Furthermore, studies that directly compared exercise electrocardiography to CCS determined that CCS is a more reliable test to exclude OCAD 34 37 51 . The CAD consortium (part of the European Network for the Assessment of Imaging in Medicine) established prediction models for accurate estimation of the PTP of OCAD in low prevalence populations. These models include age, gender, chest pain complaints, and cardiovascular risk factors 55 . Adding CCS to the PTP model was recommended to improve the risk estimation (c-statistic increased from 0.77–0.79 to 0.79–0.88) 55 . In conclusion, CCS 0, which is present in up to 50 % of stable chest pain patients, makes the presence of OCAD and the risk of MACE unlikely in low and intermediate PTP cohorts, and may be an efficient gatekeeper for additional testing, while categories of increasing CCS are directly proportional to OCAD probability and to MACE rate.
6. Recommendations for future research
To determine the diagnostic value of CCS 0 in high PTP patients, further research is needed, as potentially underlying non-OCAD can be a predictor of MACE 56 . Further studies should determine in which CCS 0 subgroups cCTA is indicated to evaluate the presence and severity of non-OCAD, thus enabling early treatment. One study in this review compared CCS 0 patients and an ultra-low CCS score group (CCS 0.1–0.9) and found a higher prevalence of OCAD in ultra-low CCS 19 . Downgrading of ultra-low CCS to the CCS 0 category could lead to possibly missed OCAD. More research is needed to assess the impact of downgrading ultra-low CCS in stable chest pain patients. So far, only three studies have addressed the long-term event rate based on CCS in stable chest pain. Even though the results are promising, more data based on longer-term outcomes are needed. Up to this point, only a minority of cohorts have been comprised of more than 50 % women. Future research should focus more on the diagnostic and prognostic value of CCS in women and investigate whether differential management is needed for symptomatic men and women . Finally, research to date has focused on the diagnostic stratification and prognostic value of CCS in secondary care settings. However, not one of the studies determined the diagnostic value of CCS in a primary care setting. Using CCS as a diagnostic test could be beneficial in primary health care. In the case of CCS 0, other causes for chest pain complaints can be explored, whereas patients with a positive CCS could benefit from (early) therapeutic intervention and/or referral to the cardiologist for additional diagnostic evaluation.
7. Conclusion
Accumulating evidence shows that OCAD is unlikely and MACE risk is very low in stable chest pain patients with a CCS of zero, especially in the case of low and intermediate PTP. This suggests a role of CCS as a gatekeeper for additional diagnostic testing. Increasing CCS is related to increasing probability of OCAD and risk of cardiac events. Additional research is needed to assess the value of CCS in women and in overall patient management in a primary healthcare setting.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Supplement
References
- 1.Mahmood T, Shapiro M D. Coronary artery calcium testing in low-intermediate risk symptomatic patients with suspected coronary artery disease: An effective gatekeeper to further testing? PLoS One. 2020;15:e0240539. doi: 10.1371/journal.pone.0240539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agatston A S, Janowitz W R, Hildner F J et al. Quantification of Coronary Artery Calcium Using Ultrafast Computed Tomography. J Am Coll Cardiol. 1990;15:827–834. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 3.Lo-Kioeng-Shioe M S, Rijlaarsdam-Hermsen D, van Domburg R T et al. Prognostic value of coronary artery calcium score in symptomatic individuals: A meta-analysis of 34000 subjects. Int J Cardiol. 2020;299:56–62. doi: 10.1016/j.ijcard.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Chaikriangkrai K, Palamaner Subash Shantha G, Jhun H Y et al. Prognostic Value of Coronary Artery Calcium Score in Acute Chest Pain Patients Without Known Coronary Artery Disease: Systematic Review and Meta-analysis. Ann Emerg Med. 2016;68:659–670. doi: 10.1016/j.annemergmed.2016.07.020. [DOI] [PubMed] [Google Scholar]
- 5.Nasir K, Clouse M. Role of Nonenhanced Multidetector CT Coronary Artery Calcium Testing in Asymptomatic and Symptomatic Individuals. Radiology. 2014;264:637–649. doi: 10.1148/radiol.12110810. [DOI] [PubMed] [Google Scholar]
- 6.Fihn S D, Gardin J M, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60:e44–e164. doi: 10.1016/j.jacc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Fihn S D, Blankenship J C, Alexander K P et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS Focused Update of the Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease. J Am Coll Cardiol. 2014;64:1929–1949. doi: 10.1016/j.jacc.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Smeeth L, Skinner J S, Ashcroft J et al. NICE clinical guideline: chest pain of recent onset. Br J Gen Pract. 2010;60:607–610. doi: 10.3399/bjgp10X515124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Excellence NIfHaC . Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. In, Clinical Guideline CG95. 2016. https://www.nice.org.uk/guidance/cg95:NICE. https://www.nice.org.uk/guidance/cg95:NICE [PubMed]
- 10.Knuuti J, Wijns W, Saraste A et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2019:1–71. doi: 10.1093/euroheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 11.Knez A, Becker A, Leber A et al. Relation of coronary calcium scores by electron beam tomography to obstructive disease in 2115 symptomatic patients. Am J Cardiol. 2004;93:1150–1152. doi: 10.1016/j.amjcard.2004.01.044. [DOI] [PubMed] [Google Scholar]
- 12.Kwon S W, Kim Y I, Shim J et al. Coronary Artery Calcium Scoring Does Not Add Prognostoc Value to Standard 64-Section CT Angiography Protocol in Low-Risk Patients Suspected of Having Coronary Artery Disease. Radiology. 2011;259:92–99. doi: 10.1148/radiol.10100886. [DOI] [PubMed] [Google Scholar]
- 13.Villines T C, Hulten E A, Shaw L J et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol. 2011;58:2533–2540. doi: 10.1016/j.jacc.2011.10.851. [DOI] [PubMed] [Google Scholar]
- 14.Kim Y J, Hur J, Lee H J et al. Meaning of zero coronary calcium score in symptomatic patients referred for coronary computed tomographic angiography. Eur Heart J Cardiovasc Imaging. 2012;13:776–785. doi: 10.1093/ehjci/jes060. [DOI] [PubMed] [Google Scholar]
- 15.Hulten E, Bittencourt M S, Ghoshhajra B et al. Incremental prognostic value of coronary artery calcium score versus CT angiography among symptomatic patients without known coronary artery disease. Atherosclerosis. 2014;233:190–195. doi: 10.1016/j.atherosclerosis.2013.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicoll R, Wiklund U, Zhao Y et al. The coronary calcium score is a more accurate predictor of significant coronary stenosis than conventional risk factors in symptomatic patients: Euro-CCAD study. Int J Cardiol. 2016;207:13–19. doi: 10.1016/j.ijcard.2016.01.056. [DOI] [PubMed] [Google Scholar]
- 17.van der Zant F M, Wondergem M, Lazarenko S V et al. Ruling out coronary artery disease in women with atypical chest pain: results of calcium score combined with coronary computed tomography angiography and associated radiation exposure. J Womens Health (Larchmt) 2015;24:550–556. doi: 10.1089/jwh.2014.4929. [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Le E PV, Rajani N K et al. A zero coronary artery calcium score in patients with stable chest pain is associated with a good prognosis, despite risk of non-calcified plaques. Open Heart. 2019;6:e000945. doi: 10.1136/openhrt-2018-000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Senoner T, Plank F, Beyer C et al. Does coronary calcium score zero reliably rule out coronary artery disease in low-to-intermediate risk patients? A coronary CTA study. J Cardiovasc Comput Tomogr. 2020;14:155–161. doi: 10.1016/j.jcct.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Kaczmarska E, Kepka C, Dzielinska Z et al. What is the optimal cut-off point for low coronary artery calcium score assessed by computed tomography? Multi-Detector Computed Tomography ANIN Registry. Postep Kardiol Interwencyjnej. 2013;9:9–15. doi: 10.5114/pwki.2013.34024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bom M J, Van der Zee P M, Van der Zant F M et al. Independent prognostic value of coronary artery calcium score and coronary computed tomography angiography in an outpatient cohort of low to intermediate risk chest pain patients. Neth Heart J. 2016;24:332–342. doi: 10.1007/s12471-016-0819-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feldman C, Vitola D, Schiavo N. Detection of coronary artery disease based on the calcification index obtained by helical computed tomography. Arq Bras Cardiol. 2000;75:471–480. doi: 10.1590/s0066-782x2000001200002. [DOI] [PubMed] [Google Scholar]
- 23.Lamont D H, Budoff M J, Shavelle D M et al. Coronary calcium scanning adds incremental value to patients with positive stress tests. Am Heart J. 2002;143:861–867. doi: 10.1067/mhj.2002.120972. [DOI] [PubMed] [Google Scholar]
- 24.Rubinshtein R, Gaspar T, Halon D A et al. Prevalence and extent of obstructive coronary artery disease in patients with zero or low calcium score undergoing 64-slice cardiac multidetector computed tomography for evaluation of a chest pain syndrome. Am J Cardiol. 2007;99:472–475. doi: 10.1016/j.amjcard.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 25.Ho J S, Fitzgerald S J, Stolfus L L et al. Relation of a coronary artery calcium score higher than 400 to coronary stenoses detected using multidetector computed tomography and to traditional cardiovascular risk factors. Am J Cardiol. 2008;101:1444–1447. doi: 10.1016/j.amjcard.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 26.Akram K, OʼDonnell R E, King S et al. Influence of symptomatic status on the prevalence of obstructive coronary artery disease in patients with zero calcium score. Atherosclerosis. 2009;203:533–537. doi: 10.1016/j.atherosclerosis.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 27.Nieman K, Galema T W, Neefjes L A et al. Comparison of the value of coronary calcium detection to computed tomographic angiography and exercise testing in patients with chest pain. Am J Cardiol. 2009;104:1499–1504. doi: 10.1016/j.amjcard.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 28.van Werkhoven J M, Schuijf J D, Gaemperli O et al. Incremental prognostic value of multi-slice computed tomography coronary angiography over coronary artery calcium scoring in patients with suspected coronary artery disease. Eur Heart J. 2009;30:2622–2629. doi: 10.1093/eurheartj/ehp272. [DOI] [PubMed] [Google Scholar]
- 29.Drosch T, Brodoefel H, Reimann A et al. Prevalence and clinical characteristics of symptomatic patients with obstructive coronary artery disease in the absence of coronary calcifications. Acad Radiol. 2010;17:1254–1258. doi: 10.1016/j.acra.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 30.Gottlieb I, Miller J M, Arbab-Zadeh A et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627–634. doi: 10.1016/j.jacc.2009.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Werkhoven J M, de Boer S M, Schuijf J D et al. Impact of clinical presentation and pretest likelihood on the relation between calcium score and computed tomographic coronary angiography. Am J Cardiol. 2010;106:1675–1679. doi: 10.1016/j.amjcard.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 32.Meyer M, Henzler T, Fink C et al. Impact of coronary calcium score on the prevalence of coronary artery stenosis on dual source CT coronary angiography in caucasian patients with an intermediate risk. Acad Radiol. 2012;19:1316–1323. doi: 10.1016/j.acra.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 33.Ueda H, Harimoto K, Tomoyama S et al. Relation of cardiovascular risk factors and angina status to obstructive coronary artery disease according to categorical coronary artery calcium score. Heart Vessels. 2012;27:128–134. doi: 10.1007/s00380-011-0128-2. [DOI] [PubMed] [Google Scholar]
- 34.Dedic A, Rossi A, Ten Kate G J et al. First-line evaluation of coronary artery disease with coronary calcium scanning or exercise electrocardiography. Int J Cardiol. 2013;163:190–195. doi: 10.1016/j.ijcard.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Liu Y C, Sun Z, Tsay P K et al. Significance of coronary calcification for prediction of coronary artery disease and cardiac events based on 64-slice coronary computed tomography angiography. Biomed Res Int. 2013;2013:472347. doi: 10.1155/2013/472347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yerramasu A, Lahiri A, Venuraju S et al. Diagnostic role of coronary calcium scoring in the rapid access chest pain clinic: prospective evaluation of NICE guidance. Eur Heart J Cardiovasc Imaging. 2014;15:886–892. doi: 10.1093/ehjci/jeu011. [DOI] [PubMed] [Google Scholar]
- 37.Geluk C A, Dikkers R, Perik P J et al. Measurement of coronary calcium scores by electron beam computed tomography or exercise testing as initial diagnostic tool in low-risk patients with suspected coronary artery disease. Eur Radiol. 2008;18:244–252. doi: 10.1007/s00330-007-0755-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hou Z H, Lu B, Gao Y et al. Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC Cardiovasc Imaging. 2012;5:990–999. doi: 10.1016/j.jcmg.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 39.Shah S, Bellam N, Leipsic J et al. Prognostic significance of calcified plaque among symptomatic patients with nonobstructive coronary artery disease. J Nucl Cardiol. 2014;21:453–466. doi: 10.1007/s12350-014-9865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Budoff M J, Mayrhofer T, Ferencik M et al. Prognostic Value of Coronary Artery Calcium in the PROMISE Study (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) Circulation. 2017;136:1993–2005. doi: 10.1161/circulationaha.117.030578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mittal T K, Pottle A, Nicol E et al. Prevalence of obstructive coronary artery disease and prognosis in patients with stable symptoms and a zero-coronary calcium score. Eur Heart J Cardiovasc Imaging. 2017;18:922–929. doi: 10.1093/ehjci/jex037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dedic A, Genders T S, Ferket B S et al. Stable angina pectoris: head-to-head comparison of prognostic value of cardiac CT and exercise testing. Radiology. 2011;261:428–436. doi: 10.1148/radiol.11110744. [DOI] [PubMed] [Google Scholar]
- 43.Petretta M, Daniele S, Acampa W et al. Prognostic value of coronary artery calcium score and coronary CT angiography in patients with intermediate risk of coronary artery disease. Int J Cardiovasc Imaging. 2012;28:1547–1556. doi: 10.1007/s10554-011-9948-5. [DOI] [PubMed] [Google Scholar]
- 44.Versteylen M O, Joosen I A, Winkens M H et al. Combined use of exercise electrocardiography, coronary calcium score and cardiac CT angiography for the prediction of major cardiovascular events in patients presenting with stable chest pain. Int J Cardiol. 2013;167:121–125. doi: 10.1016/j.ijcard.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 45.Parma Z, Parma R, Brzoska J et al. Prognostic value of coronary artery calcium score in patients with symptoms suggestive of coronary artery disease. Results from the Silesian Calcium Score (SILICAS) study. Pol Arch Med Wewn. 2016;126:395–401. doi: 10.20452/pamw.3443. [DOI] [PubMed] [Google Scholar]
- 46.Nappi C, Nicolai E, Daniele S et al. Long-term prognostic value of coronary artery calcium scanning, coronary computed tomographic angiography and stress myocardial perfusion imaging in patients with suspected coronary artery disease. J Nucl Cardiol. 2018;25:833–841. doi: 10.1007/s12350-016-0657-2. [DOI] [PubMed] [Google Scholar]
- 47.Shiga Y, Morii J, Idemoto Y et al. A Coronary Artery Calcium Score of Zero in Patients Who Have Undergone Coronary Computed Tomography Angiography Is Associated With Freedom From Major Adverse Cardiovascular Events. J Clin Med Res. 2020;12:662–667. doi: 10.14740/jocmr4335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rijlaarsdam-Hermsen D, Kuijpers D, van Dijkman P R. Diagnostic and prognostic value of absence of coronary artery calcification in patients with stable chest symptoms. Neth Heart J. 2011;19:223–228. doi: 10.1007/s12471-011-0097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schmermund A, Stang A, Möhlenkamp S et al. Prognostic value of electron-beam computed tomography-derived coronary calcium scores compared with clinical parameters in patients evaluated for coronary artery disease. Prognostic value of EBCT in symptomatic patients. Z Kardiol. 2004;93:696–705. doi: 10.1007/s00392-004-0120-2. [DOI] [PubMed] [Google Scholar]
- 50.Symons R, Sandfort V, Mallek M et al. Coronary artery calcium scoring with photon-counting CT: first in vivo human experience. Int J Cardiovasc Imaging. 2019;35:733–739. doi: 10.1007/s10554-018-1499-6. [DOI] [PubMed] [Google Scholar]
- 51.Lubbers M, Dedic A, Coenen A et al. Calcium imaging and selective computed tomography angiography in comparison to functional testing for suspected coronary artery disease: the multicentre, randomized CRESCENT trial. Eur Heart J. 2016;37:1232–1243. doi: 10.1093/eurheartj/ehv700. [DOI] [PubMed] [Google Scholar]
- 52.Grundy S M, Stone N J, Bailey A L et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 53.Dzaye O, Dardari Z A, Cainzos-Achirica M et al. Warranty Period of a Calcium Score of Zero: Comprehensive Analysis From MESA. J Am Coll Cardiol Img. 2021;12:990–1002. doi: 10.1016/j.jcmg.2020.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Valenti V, Hartaigh B, Heo R et al. A 15-Year Warranty Period for Asymptomatic Individuals Without Coronary Artery Calcium: A Prospective Follow-Up of 9715 Individuals. JACC Cardiovasc Imaging. 2015;8:900–909. doi: 10.1016/j.jcmg.2015.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Genders T S, Steyerberg E W, Hunink M G et al. Prediction model to estimate presence of coronary artery disease: retrospective pooled analysis of existing cohorts. Bmj. 2012;344:e3485. doi: 10.1136/bmj.e3485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Williams M C, Kwiecinski J, Doris M et al. Low-Attenuation Noncalcified Plaque on Coronary Computed Tomography Angiography Predicts Myocardial Infarction: Results From the Multicenter SCOT-HEART Trial (Scottish Computed Tomography of the HEART) Circulation. 2020;141:1452–1462. doi: 10.1161/circulationaha.119.044720. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


