Abstract
Objective:
Research from the early months of the COIVD-19 pandemic identifies many COVID-related stressors, including fears of infection, disruptions to work/learning and daily self-care routines, and lack of access to reliable information and resources. Measuring the complex, ongoing nature of the stressors related to COVID-19 is of great practical utility, as is investigating how people may differently respond to stressors. The objective of the present study was to identify the possible profiles of COVID-19-related stressors using a recently developed measure, the COVID-19 Stressors Scale.
Method:
The present study sampled individuals from MTurk (n = 1,530) and examined the COVID-19 Stressors Scale with latent profile analysis.
Results:
Using a latent profile analysis, three profiles of COVID-19-related stressors were identified, Moderate Disruption Distress, High Disruption Distress, and Identity and Role Strain.
Conclusions:
Based on the results of the study, the authors encourage researchers to differentiate types of stressors profiles of individual experiences COVID-19 or future pandemics.
Keywords: COVID-19, latent profile analysis, stress scale, measurement
Introduction
COVID-19 (SARS-Cov-2) arrived in the United States in January 2020. By March, the spread of the disease altered daily routines nationwide and was classified as a global pandemic by the World Health Organization (WHO, 2020); new cases would first peak in the US on April 10th, 2020 before declining for the month May into early June (Johns Hopkins University Center for Systems Science and Engineering, 2021). COVID-19 is a preventable, highly communicable, novel coronavirus with a mortality rate estimated to potentially exceed rates seen during other flu and SARS epidemics (CDC COVID Response Team, 2020; Layne et al., 2020). Research from other epidemics and the early months of the COVID-19 epidemic identifies COVID-related stressors that include fears of infection, disruptions to work/learning and daily self-care routines, and lack of access to reliable information and resources (Brooks et al., 2020; Main et al., 2011; Qiu et al., 2020). The mental health sequalae of disasters are extensive and widespread (Baral & Bhagawati, 2019; North, 2016; Park et al., 2012) and include a variety of mental health symptoms, some of which stem from the steps taken to slow the spread of the disease. In particular, social distancing measures including quarantines may be crucial for infectious disease prevention but are also associated with lasting mental health impacts (McGuire et al., 2018; Solomon, 2020). The COVID-19 pandemic can be considered an instance of traumatic stress, likely worsening existing mental health difficulties for some and creating new pathogenic conditions for others (Horesh & Brown, 2020). Important research considerations arise concerning potential interindividual differences in mental health sequalae that may be experienced over time, as not all individuals will experience the COVID-19 pandemic as a trauma. Attending to the experiences of those who do and identifying the potential profiles for vulnerable individuals is warranted.
Community-wide crises, including natural disasters (Bolt et al., 2018; Fussell & Lowe, 2014; Seto et al., 2019; Sprague et al., 2015) and acts of terror (Jose et al., 2019) can have long-term impacts on mental health, including posttraumatic stress, anxiety, and coping difficulties (Labarada et al., 2003; North & Pfefferbaum, 2013). In the case of the enduring COVID-19 pandemic, the pathogenic effects of stress over time may be amplified, because the stressful conditions of the community-wide crisis (e.g., the threat of infection and the impacts of social distancing/quarantine and related financial consequences) are projected to be sustained over months. By late summer, 2020, rates of COVID-19 infections reached new highs and established a second peak in the U.S. (Johns Hopkins University Center for Systems Science and Engineering, 2021).
One early study of mental health outcomes of COVID-19 in China indicates one-third of a national sample reported elevated depression, anxiety, or stress (Qiu et al., 2020). It is likely that these early experiences of deleterious mental health impacts foreshadow long-term impacts (Galea et al., 2020; McGuire et al., 2018; North, & Pfefferbaum, 2013). Questions remain about possible patterns in these impacts, given known variability in stress sensitivity (Henchken et al., 2016; Kim et al., 2019), and whether discernable profiles for groups exist regarding who experiences particularly severe distress during the COVID-19 pandemic. For example, Alderidge and Roesch (2008) note unique patterns in stress and coping responses among cultural and ethnic minority groups, who encounter distinct stressors compared to white majority groups (e.g., poor education, limited access to health care, higher poverty rates and the cumulative disadvantages associated with these like higher crime and violence rates), including the salient stressful experience of racism. Several studies have described different distress groupings (trajectories) following community-wide traumas such as 9/11 (e.g., Bonnano et al., 2006), the 2010 Indian Ocean tsunami (e.g., Johannesson et al., 2015), and Hurricane Katrina (e.g., Rossellini et al., 2014); these studies tend to focus primarily on PTSD and occasionally include other indicators of stress. Understanding and measuring the complex, ongoing nature of the stressors related to COVID-19 is of great practical utility in articulated needed responses as the pandemic is projected to stretch through 2021.
An important determinant of mental health outcomes is total exposure to the event (e.g., proximity to the disaster in geographically restricted disasters, pervasiveness of impacts, or number of negative consequences). Despite the importance of exposure, relatively few studies have attempted to quantify it (e.g., Garfin et al., 2014; Verger et al., 2003). Exposure, and the associated feelings of distress, are significant predictors of long-term mental health outcomes. Exposure to aspects of the pandemic, including those prompted by personal role, employment, or social location, and the distress associated with that exposure, are important determinants of long-term mental health outcomes. It is critical to quantify them for measurement purposes.
Individuals may differ on the impact disasters have on their appraisals of stress and the event itself (Drapeau et al., 2012). Measures of stress often assume homogeneity of the experiences of individuals in disasters and have not tested potential heterogeneity. There may be specific profiles of people on how their respond to stressors and what concerns them during a disaster. These possible profiles may be due to demographic factors and personal resources that individuals possess (Fernandez et al., 2020). A recent study identified that during COVID-19, the overall quarantine experience of stress was more related to severity of symptoms than types of symptomology and individuals could be split into different profiles of symptoms severity (Fernandez et al., 2020). However, this research did not specifically test for different profiles of responses of stressors. Studies cited above based on a resilience framework (e.g., Bonanno et al., 2006; Rossellini et al., 2014) focus solely on distress rather than modeling groups with different exposure and stress appraisals. Identifying and describing patterns in stress response for specific groups carries tremendous considerable value for the development of intervention supports and the outreach efforts to deliver them to the most vulnerable segments of the population. The current paper explores the evidence for discernable profiles through latent profile analysis (LPA) using a recently validated measure of COVID-19 related stress, the COVID-19 Stressors Scale (Park et al., 2021).
A latent profile analysis allows researchers to identify classes or clusters of participants (the latent profiles) based on their responses to continuous manifest variables (Ferguson et al., 2019). This type of analysis relies on probability to estimate the likelihood that each participant belongs to a particular profile. It is a person-centered approach used to identify the underlying and unknown categorical variable that separates the sample into profiles. Without identifying this variable, a variable-centered approach such as a confirmatory factor analysis assumes the participants in the sample all belong to the same group without differentiating the latent subgroups within the sample (Ferguson et al., 2019). By ignoring likely differences within a given group, researchers may miss patterns of variation between and within the sample causing model misfit or concluding that all participants’ experiences are the same. There may be qualitatively different profiles of stressfulness, and the understanding of the patterns in individual responses is meaningful. Said another way, it is useful to know what types of stressors are most impactful to individuals during a crisis like the COVID-19 pandemic (i.e., are distressing stressors more likely to be work-related, or infection-related?) and if there are different groups of people who experience different stressors being most salient to them. For example, in a LPA, one profile may demonstrate higher than average distress around work-related stressors while low distress for family-related stressors, while another profile could have the reverse (Spurk et al., 2020). A latent profile analysis approach enables the examination of person-centered differences, rather than differences in total scores, means, or distributions. Examining parameter estimates like the numeric means of different profiles would quantitatively derive the same score, but qualitatively may contain different factors. Thus, the LPA approach allows researchers to identify homogeneous profiles of people within a larger heterogeneous sample and identify possible crucial differences in what stresses individuals during a global pandemic.
Current Study
The present study examined person-level data from the COVID-19 Stressors Scale, a novel stress exposure scale developed during the first few weeks of the widespread US quarantine and shelter-in-place orders in response to the spread of COVID-19. We used latent profile analysis to examine potential heterogeneity among COVID-19 stressors experiences. We sought to identify A) the number and shape of profiles for COVID-19 stressors and B) the prevalence of the identified profiles. Our aim with this work is to advance the dialog concerning crisis-generated linkages between stressful event exposure and distress and how people may experience stressors differently.
Methods
Participants
Data were obtained from a national sample of individuals who participated in a larger (Park et al., 2021) study of COVID-19 pandemic impacts between April 7–14, 2020, at the first peak rate of 7-day averages for new COVID-19 diagnoses in the US (Johns Hopkins University Center for Systems Science and Engineering, 2021). Participants 18 years or older living in the U.S. and English-speaking were solicited to participate through Amazon’s Mechanical Turk (MTurk). MTurk is a global online worker platform through which eligible participants complete tasks described through online job postings, called Human Intelligence Tasks, or HITs (Sheehan, 2018). The HIT in this study sought workers who met the inclusion criteria for the research (i.e., were over 18 and resided in the US) to complete an anonymous 30-minute survey with the option to complete subsequent study surveys over the next six months. Each participant was compensated with a $2 incentive for participation at baseline, and $3 for each follow-up survey. MTurk has increased in popularity as a sampling mechanism in behavioral and public health fields, as MTurk workers are fairly representative of larger populations (Bartneck et al., 2015; Sheehan, & Pittman, 2016), and research has found this recruitment method replicates the relationships found in the population, and is therefore, an effective sampling strategy in health research (Mortensen & Hughes, 2018).
The protocol for the study was reviewed and approved by the University of Connecticut IRB. The researchers posted the baseline HIT on MTurk April 7, 2020 and closed out data collection 2 weeks later. The larger study’s follow-up HITS were posted for this baseline cohort subsequently; only data from the baseline assessment point are included for the present analysis. Interested MTurk workers reviewed a brief explanation of the research protocol and followed a hyperlink to the assent page and survey materials for the study. No constraints were placed on the eligibility of MTurk workers (e.g., minimum worker approval ratings), apart from meeting the study’s inclusion criteria and successfully passing a captcha attention screener at the outset of each survey.
Measures1
COVID-19 Stressors Scale
The COVID-19 Stressors Scale (Park et al., 2021) is a disaster-specific measure of stressor exposure and appraisal, developed to quantify overall stress associated with the COVID-19 pandemic. The measure was developed to include items tapping all the dominant themes identified in studies of previous SARS outbreaks and the early months of the COVID-19 pandemic in China (e.g., financial stressors, fear of infection; Brooks et al., 2020; Main et al., 2011; Qiu et al., 2020), including infection-related stressors, daily routine disruption stressors, and resource-related stressors. Where published, reliable survey items were adapted for use in line with the COVID-19 Stressor Scale format described below; where salient items were discussed – based on thematic analysis of qualitative data, for example – new items were drafted for inclusion. This measure assesses past-week stressfulness with binary (yes/no) exposure to 23 stressors, paired with a continuous rating of stressfulness. For each item participants indicate “yes”, a subsequent linked question assessed the event’s stressfulness using a Likert rating scale from 1 to 5 (“not at all stressful” to “extremely stressful”). Thus, the scale yields count of stressor exposures (Park et al., 2021) and a composite distress/impact score (Tambling et al., 2021). Preliminary measurement testing of psychometric properties indicates the measure is internally consistent (α = .96; Tambling et al., 2021) and has a unidimensional structure with all items loading on the single factor above 0.6 (Tambling et al., 2021).
For the present study, the composite variable method of scale scoring (Tambling et al., 2021) was used. A variable was computed for each stressor indicator such that binary ratings were coded as 0/1 and multiplied by appraisal scores (1–5). The resulting variable ranged from 0 (indicating the respondent did not experience the event and thus reported no stress) to 5 (indicating that the respondent had the experience, and that it was appraised as highly stressful). To account for zero inflation when analyzing the variance-covariance structures of the data the scale was shifted by one point, by adding one to each score, resulting in a range of 1–6. This lends greater confidence in the researchers identifying a construct(s) that were not artifacts of near zeros in the results.
Data Analysis
Latent Profile Analysis
A series of LPAs were conducted using Mplus 8.4 (Muthen & Muthen, 2020), using maximum likelihood estimation, to identify latent profiles of subpopulations taking the COVID-19 Stressors Scale. Latent profile analysis is a model testing process, fitting multiple models with different number of profiles. Each model is compared with previous models in an iterative process comparing model fit between models. A total of six LPA models were run in an iterative process, starting with one profile, and the process concluded when there was little or no improvement in fit with the addition of more profiles.
The researchers used common model fit indices (Ferguson et al., 2019) for model selection decisions. These indices were the Akaike’s Information Criterion (AIC), Bayesian information criterion (BIC), and the Sample-Adjusted BIC (SABIC). For these fit criteria smaller values indicate the preferred model. In addition, the researchers used the bootstrap likelihood ratio test (BLRT), which compares one model with k classes with a model with k-1 classes on their model fit, and the Lo-Mendell-Rubin (LMR) test, which functions similarly to a χ2 to compare models using the likelihood ratio. A p-value that is not significant for these tests indicates that the k-1 model is preferred for the BLRT and a significant LMR result indicates that the model with fewer profiles represents the data worse than the model with more profiles.
Results
Screening Participants
Participants were obtained through a task on the MTurk platform, an online worker tool. Guidelines for online survey data management recommend eliminating cases in which substandard completion of the survey is suspected, by either pattern of response or time to completion (Kees, Berry, Burton, & Sheehan, 2017; Sheehan, 2018). To determine appropriate response time for inclusion, average response time in seconds was calculated based on preliminary piloting of the survey (approximately 1,290 seconds). Any completed entry from the baseline assessment point (n = 1,648) that fell below 50% of this average was eliminated (n = 118), resulting in a final study sample of 1,530 adults, 42.6% of whom were male (n = 653); average age = 35.96 years old (range = 18 – 88 years old). Respondents were racially diverse and were able to endorse more than one racial group. The majority of individuals reported being white 79.1% (n = 1,212). Other respondents reported Black racial identity (13.2%; n = 203) and endorsed identity aligned with a variety of other racial groups (201 Asian, 88 Pacific Islanders, and 118 Native Americans). Additional demographic characteristics are presented in Table 1. Due to the nature of MTurk completion guidelines, missing data were found for fewer than 1% of items, and at very low rates (missing for no more than .5% of the sample). Given a lack of interpretable pattern in the very low rates of missingness, these are assumed to be missing completely at random.
Table 1.
Sample demographics
| μ (SD) | |
|---|---|
|
| |
| Age | 35.96 (XX) |
| N (%) | |
|
| |
| Gender | |
| Male | 653 (43.6%) |
| Female | 832 (55.6%) |
| Transgender | 12 (0.7%) |
| Non-binary | 11 (0.6%) |
| Prefer not say | 22 (l.4%) |
| Race | |
| Black/African American | 203 (13.6%) |
| Asian/Asian American | 201 (13.4%) |
| Native Hawaiian/Other Pacific Islander | 88 (5.9%) |
| American Indian/Alaska Native | 118 (7.8%) |
| White | 1,212 (80.1%) |
| Ethnicity | |
| LatinX | 147 (9.8%) |
| Non-LatinX | 1352 (90.2%) |
| Geographic US Census region | |
| West | 333 (22.0%) |
| Midwest | 292 (19.5%) |
| South | 306 (20.4%) |
| Northeast | 306 (20.4%) |
| Current employment | |
| No | 466 (31.1%) |
| Yes, part-time | 297 (19.8%) |
| Yes, full-time | 736 (49.1%) |
| Finances adequate to meet needs | |
| Not at all | 127 (8.5) |
| A little | 313 (20.9) |
| Moderately | 336 (22.4) |
| Mostly | 397 (26.5) |
| Completely | 326 (21.7) |
Note: Respondents could select multiple races; responses to demographic items were not required, thus there is some item missingness, particularly for geographic state
Preliminary Analysis
The first step in better understanding the measure, and its assessment of distress related to the pandemic, was to examine the distribution of scores on the measure. Prior to conducting the LPA, the researchers gathered general information about the respondents. Table 2 presents the means and standard deviations for each item as well as the median and modal scores.
Table 2.
Means, standard deviations, and modal scores of COVID Stressor Scale Items
| Item | Mean | SD | Median | Mode |
|---|---|---|---|---|
|
| ||||
| 1 | 3.37 | 2.18 | 4.00 | 1.00 |
| 2 | 2.62 | 1.92 | 1.00 | 1.00 |
| 3 | 3.88 | 2.41 | 5.00 | 1.00 |
| 4 | 2.10 | 1.96 | 1.00 | 1.00 |
| 5 | 4.97 | 1.33 | 5.00 | 5.00 |
| 6 | 1.38 | 1.27 | 1.00 | 1.00 |
| 7 | 1.74 | 1.53 | 1.00 | 1.00 |
| 8 | 4.87 | 1.71 | 5.00 | 5.00 |
| 9 | 4.08 | 1.81 | 4.00 | 5.00 |
| 10 | 3.89 | 2.35 | 5.00 | 1.00 |
| 11 | 2.14 | 1.98 | 1.00 | 1.00 |
| 12 | 4.35 | 1.79 | 5.00 | 5.00 |
| 13 | 1.96 | 1.85 | 1.00 | 1.00 |
| 14 | 3.84 | 2.07 | 4.00 | 1.00 |
| 15 | 2.03 | 1.86 | 1.00 | 1.00 |
| 16 | 3.33 | 2.16 | 4.00 | 1.00 |
| 17 | 2.66 | 2.01 | 1.00 | 1.00 |
| 18 | 2.79 | 1.93 | 3.00 | 1.00 |
| 19 | 2.88 | 2.52 | 1.00 | 1.00 |
| 20 | 1.69 | 1.71 | 1.00 | 1.00 |
| 21 | 3.87 | 2.32 | 5.00 | 1.00 |
| 22 | 3.17 | 2.32 | 1.00 | 1.00 |
| 23 | 1.87 | 1.83 | 1.00 | 1.00 |
Preliminary analysis of the data found that the items of the COVID Stressor Scale were consistent with one another, α = .84. This internal consistency was lower than the .934 of the measure development sample (Tambling et al., 2021), but still displayed good internal consistency. Analysis of the data suggested that some items were more likely than others to be rated by respondents as stressful/distressing. For example, the modal scores for items 5, 8, 9, and 12 are five, while the other items have a modal score of 1. Further exploration of the measures of central tendency suggests that there might be broad differences in respondents’ reports. For example, item 10 (which indicates stress related to changes in daily work routine) has a median of 5.0, mode of 1.0, and mean of 3.89 (SD 2.35) in this sample. Analysis of the distribution of scores on the measure indicated a potential bimodal distribution. The response pattern was as follows: 1, n = 545 (36%); 2, n = 0; 3, n = 48 (3%); 4, n = 170 (11%); 5, n = 266 (17%); 6, n = 248 (16%); 7, n = 253 (16%). This distribution suggests that nearly as many people found item 10 not stressful as did very stressful. Other items with similar distributions were found, suggesting that some items were either particularly stressful or were not at all. Some items, for example, item 6 (which indicates stress related to stigma, shame, and discrimination related to quarantine or working in a high-risk area), were not at all stressful for most people. Nearly the entire sample (n = 1400; 91%) scored a 1 on this item, indicating that it was not distressing for the majority of individuals.
Latent Profile Analysis
Six latent profile analyses were conducted, and fit information is presented in Table 3. The AIC, BIC, and SABIC never reached a minimum value. In addition, the p-values of the LMR and BLRT continued to be significant, supporting greater number of profiles. Because the LMR and BLRT may never become nonsignificant (Ferguson et al., 2019) due to additional profiles increasing the representation of the data, and there was little conceptual reason for there to be seven profiles, the researchers plotted the log likelihood values and examined the plot for the “elbow”, determining that a three profile model was the result that improved the model without hampering parsimony (Masyn, 2013).
Table 3.
Fit Information for the COVID Stressor Scale
| Log-likelihood | AIC | BIC | SABIC | P LMRT | P BLRT | |
|---|---|---|---|---|---|---|
|
| ||||||
| 1 Profile Model | −72885.614 | 145863.229 | 146108.548 | 145962.417 | ||
| 2 Profile Model | −70808.980 | 141757.959 | 142131.271 | 141908.899 | .000 | .000 |
| 3 Profile Model | −68878.450 | 137944.900 | 138146.204 | 138147.590 | .000 | .000 |
| 4 Profile Model | −68436.356 | 137108.712 | 137738.009 | 137363.153 | .000 | .000 |
| 5 Profile Model | −68080.675 | 136445.349 | 137202.638 | 136751.540 | .033 | .000 |
| 6 Profile Model | −66942.292 | 134216.584 | 135101.866 | 134574.526 | .001 | .000 |
| 7 Profile Model | −66483.973 | 133347.946 | 134361.220 | 133757.638 | .000 | .000 |
Note. n =1506; The LMR test and the BLRT compare the current model to a model with k - 1 profiles. LPA = latent profile analysis; AIC = Akaike’s Information Criterion; BIC = Bayesian Information Criterion; SABIC = Sample-Adjusted BIC; LMR = Lo-Mendell Ruben; BLRT = bootstrap likelihood ratio test.
As table 4 and figure 1 show, the latent class profiles were similar and were defined by the severity of their stressors. The profile labeled Class 1 (Moderate Disruption Distress; 55.6% of the sample) had the lowest overall scores and showed participants in this profile were overall moderately distressed and did not have same upward scoring trend on questions 17 and 18 that the other two profiles did. These items were related to stressors of having increased contact with loved ones (item 17) and pressure to find a silver lining (item 18).
Table 4.
Three-Profile Model Results. Means (Standard Deviations)
| Variable | Profile 1 Moderate Disruption Distress (n = 851) |
Profile 2 High Disruption Distress (n = 550) |
Profile 3 Identity and Role Strain (n = 129) |
|---|---|---|---|
|
| |||
| Item 1 | 2.579 (1.991) | 4.324 (1.992) | 4.543 (1.992) |
| Item 2 | 2.019 (1.792) | 3.257 (1.292) | 3.829 (1.792) |
| Item 3 | 3.077 (4.982) | 4.914 (2.232) | 4.760 (2.232) |
| Item 4 | 1.573 (1.851) | 2.583 (1.851) | 3.566 (1.851) |
| Item 5 | 4.481 (0.274) | 5.622 (1.216) | 5.403 (1.216) |
| Item 6 | 1.002 (1.403) | 1.000 (0.273) | 5.465 (0.274) |
| Item 7 | 1.268 (1.493) | 2.116 (1.403) | 3.264 (1.403) |
| Item 8 | 4.136 (1.495) | 5.874 (1.493) | 5.403 (1.493) |
| Item 9 | 3.216 (1.528) | 5.196 (1.528) | 4.969 (1.528) |
| Item 10 | 2.820 (2.022) | 5.276 (2.022) | 5.085 (2.022) |
| Item 11 | 1.527 (1.850) | 2.815 (1.850) | 3.287 (1.850) |
| Item 12 | 3.599 (1.578) | 5.276 (1.578) | 4.845 (1.578) |
| Item 13 | 1.565 (1.765) | 2.289 (1.779) | 3.202 (1.779) |
| Item 14 | 2.984 (1.829) | 4.987 (1.829) | 4.612 (1.829) |
| Item 15 | 1.642 (1.799) | 2.404 (1.799) | 3.000 (1.938) |
| Item 16 | 2.572 (1.938) | 4.255 (1.938) | 4.364 (1.938) |
| Item 17 | 2.055 (1.892) | 3.463 (1.892) | 3.225 (1.892) |
| Item 18 | 1.980 (1.706) | 3.841 (1.706) | 3.674 (1.706) |
| Item 19 | 2.050 (2.342) | 3.949 (2.343) | 3.760 (2.343) |
| Item 20 | 1.185 (1.597) | 2.153 (1.597) | 3.093 (1.597) |
| Item 21 | 3.179 (2.191) | 4.771 (2.191) | 4.535 (2.191) |
| Item 22 | 2.564 (2.220) | 3.894 (2.221) | 4.093 (2.221) |
| Item 23 | 1.425 (1.745) | 2.258 (1.745) | 3.155 (1.745) |
Note. Values representing highest response are given in boldface.
Figure 1:
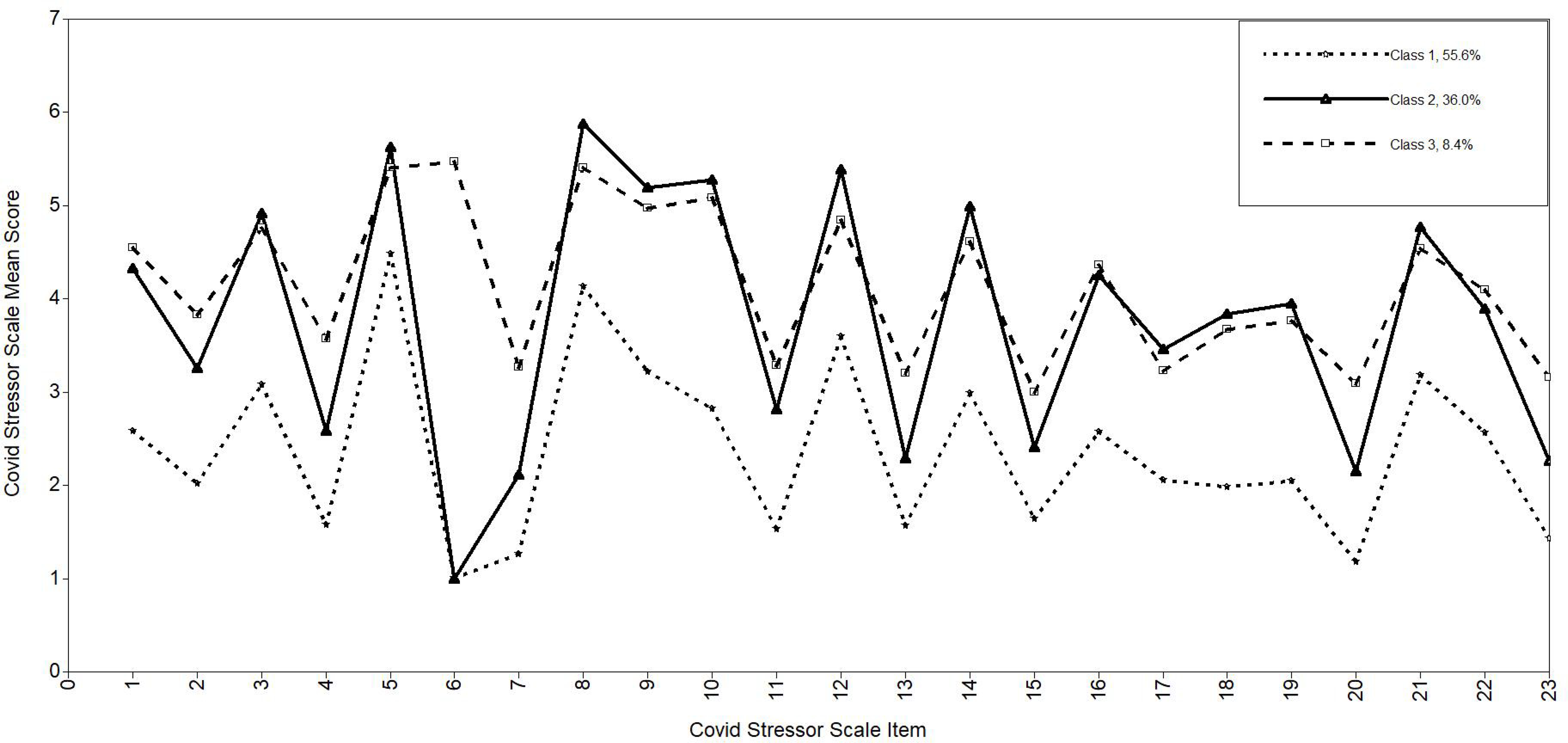
Line Graph Comparing Profiles on Items of the COVID Stressor Scale
The profile labeled Class 2 (High Disruption Distress; 36.0% of the sample) answered the highest overall on scores. This profile followed the same overall trend of the three profiles. This trend highlighted the greatest stressors and concerns were participants’ lives being disrupted in daily activities, financial disruption, and the risk of being infected.
The profile labeled Class 3 (Identity and Role Strain; 8.4% of the sample) also had high overall scores related to disruption, but scored much higher on items 6 and 7 compared to profiles one and two. Items 6 and 7 are unique to the rest of the assessment because these items ask about stigma, shame, or discrimination related to working in a high-risk area or profession (item 6) or a certain age group (item 7). Participants in profile 3 were not only highly stressed about COVID-related stressors, but were also uniquely of the three profiles, also stressed about their job or their age and worried about facing stigma or discrimination about these two factors.
Covariate analysis
Based on recent research that suggests that gender as a factor influencing distress during the pandemic (Horesh et al., 2020) and issues such as intimate partner violence increasing (Moreira & Pinto da Costa, 2020), we conducted a post hoc multinomial logistic regression analysis to identify if gender predicted profile membership, using profile 1 as the reference. Forty-five participants were excluded because of their gender identifications were insufficiently powered, transgender (n = 12), non-binary (n = 11), or did not disclose (n = 22). The results of the regression analysis suggests that there are differences in the probability of group membership by gender. Relative to profile 1, female participants had a higher probability of fitting profile 2 (OR = 1.926, 95% CI 1.50–2.48) than males. In addition, relative to profile 1, female participants had a higher probability of fitting profile 3 (OR = 1.528. 95% CI 1.02–2.29) than males.
Discussion
This report documents the results of an examination of the latent profiles identified in scores on the COVID-19 Stressors Scale. Three unique profiles were found and showed differences regarding how individuals responded to the stressors of COVID-19. The lowest overall scores comprised the most common profile, Moderate Disruption Distress. Individuals with this profile had moderate distress about the disruptions caused by COVID-19 and quarantine, but overall were less stressed about COVID-19 than those in the other two profiles. Those with the second most common profile, High Disruption Distress, had the highest distress related to COVID-19 of the three profiles. The least common profile, Identity and Role Strain, had high scores as well, indicating distress, but unique to the three profiles, had high concern about stigma and shame related to either working in a high-risk area or being associated with a particular group. In addition, participants in this profile also had the highest scores regarding stressors related to becoming infected (item 1), monitoring for symptoms (item 2), and unintentionally infecting others (item 4), which further corroborates that participants in this profile likely had higher risk of exposure to the virus. The presence of the profile of Identity and Role Strain also suggests that some items have more utility regarding differentiating between profiles. If a participant has high scores on either or both items 6 and 7, it is likely that the individual would fit the Identity and Role Strain profile, a highly distressed profile. It is clear that members of this profile have a unique experience of the pandemic related to their role/job stressors that members of the other two profiles do not. Further research specific to this profile is needed to better understand how to help members cope with higher risk of exposure and stigma related to their age, job, or social location. Intervention may also be necessary with this group, as they are highly distressed, and may experience poor mental health outcomes as a result.
The results of the covariate analysis found that female participants were more likely to be in profiles 2 (High Disruption Distress) and 3 (Identity and Role Strain) than male participants. These results are unsurprising given that previous research has found gender to influence distress during the pandemic (Horesh et al., 2020). There are a several possible reasons for this. During the pandemic, females may be even more strained to complete the “second shift” of childcare and household work than before the pandemic (Power, 2020) and they may also experience a larger reduction in work hours and employment compared to men (Bick & Blandin, 2021). In addition, women are more likely to be employed in jobs and occupations that require high contact and proximity to others (Albanesi et al., 2020), possibly explaining the Role and Identity Strain profile. Finally, intimate partner violence has increased during the pandemic which disproportionately affects women compared to men (Moreira & Pinto da Costa, 2020).
All three profiles identified showed that participants were at least moderately distressed by the disruption caused by the COVID-19 pandemic and the ensuing quarantine. All participants reported concern about the risk of themselves or others becoming infected and the disruption caused by pandemic and quarantine. Identifying profiles of how people respond and to what stressor they respond to during a pandemic has clinical implications, as does the likelihood of membership of these profiles for men and women. Practitioners and researchers can have a better understanding of client and patient stressors based on their profiles and give a more targeted treatment. In terms of intervention, all profiles may benefit from information that would help ease fears of infection, including messaging about social distancing, healthy hygiene, and quarantining. Future research that examines differences in scores across groups, perhaps those who have sought clinical help, or those in “frontline” professions (a response highlighted by item 6), would also be useful. Specific to profile 3, practitioners can identify the specific stigma and distress caused by working in high-risk areas or specific age groups and target identification of resources specific to this group. Based on profiles 2 and 3, prevention researchers and interventionist can also target eliminating the disparities between women and men in carrying larger burdens in terms of childcare and household tasks, employment, and domestic violence.
As of this writing in February 2021, rates of COVID-19 diagnoses are declining from a recent surge across the US, during which rates exceeded those of the disease’s early peak on April 10, 2020 (Johns Hopkins University Center for Systems Science and Engineering, 2021) and mortality rates have surpassed 400,000. Clearly the virus will continue to pose significant public health risks for some time to come, even as vaccines are delivered, but who is most impacted and in what domains remains to be seen. Surges in diagnosis rates vary, perhaps associated with state and local policies for relaxing early shelter-in-place restrictions (Bosman & Smith, 2020), such that some states are able to maintain relative stability, whereas others are contending with new record high rates of disease transmission, hospitalizations, and death. This suggests that investigating the profiles of different geographic locations may be salient for future studies.
It is also possible that as we look at subsequent waves of COVID-19 and the advent of new strains of the virus, the nature and salience of the three profiles may shift. For example, early in the pandemic in the US, the stress of disruption may have been more acutely felt than the stress of disease risk. As people confronted the risk of infection more directly at later phases, the risk profile related to infection distress may have elevated. However, as COVID-19 vaccinations increase, the stressors related to risk infection may decrease. Future studies could conduct analyses of subsequent waves to investigate how profiles change over time.
There are limitations to the study. Recruitment through the MTurk platform may limit the sample’s generalizability as all respondents were MTurk workers with some shared characteristics that may not be representative of the public at large (access to a computer with internet access, specifically). Researchers in future studies might consider using the filters MTurk provides to access only workers with high worker approval ratings to strengthen confidence in the reliability of data from this recruitment platform. Further, while the national sample has representation of each US Census region, the sample is not representative of the US population.
Additional care should be taken to sample vulnerable groups in particular (e.g., Black, Indigenous and people of color and other under-represented groups) and attend to the potential for any internalized stigma they may experience anchored in the context of a given crisis. For example, given the likely origins of the disease and the resulting stigma and racism, further work should be conducted specifically with the Asian American population in the United States to examine the specific stressors this population may experience. While this study does not specifically address the stigma that people of Asian-descent may experience, COVID-related stigma may be a meaningful stress experience during COVID-19 that warrants a future adaptation of the measure with an additional set of targeted items (or, at a minimum, concurrent but separate measurement thereof). Furthermore, racial/ethnic minorities may also have increased burdens related to employment, healthcare inequalities, the type of jobs they have, and household responsibilities (Alderidge & Roesch, 2008; El-Khatib et al., 2020). Sufficiently sampling racial/ethnic minorities and examining their data with an LPA may find that not only are they more likely to have membership in profiles 2 and 3, but there may be additional profiles that only fit their stressor experiences.
Despite these limitations, the present study provides valuable information about the possible profiles of stressors that people experience during the pandemic using the COVID-Stressors Scale. Participants were at a minimum moderately distressed by the disruptions that the pandemic caused and were concerned about the possibility of infection. However, the profile also demonstrated that some are more highly distressed, which disproportionately were female participants, and that shame and stigma related to age and/or job only impacted some participants, again disproportionately female participants. These results provide further evidence of the differences in stressors between males and females and the possibility of greater burden borne by females during a pandemic.
The results also indicate a subset of items that are most distressing, or which differentiate between profiles who are highly distressed and those who are not. Knowing this may help healthcare professionals in determining what interventions are most needed for clients based on their profiles, and which stressors may be less salient to focus on. Furthermore, the results of the LPA suggest that for greater ease of use, the COVID-19 Stressors Scale could be reduced to only the salient stressor items. With a time-sensitive need to evaluate the variation of COVID-19 experiences and their impacts on mental health across diverse regions and populations (Park et al., 2021, Russell et al., 2020; Tambling et al., 2021), this scale provides an important common data element that researchers can employ to make valid comparisons across samples, identifying the profiles that may need specific interventions.
Supplementary Material
Clinical Impact Statement:
This paper looked at a new assessment of COVID-19-related stressors, the COVID-19 Stressors scale. The paper found that individuals respond to stressors in different ways and specific stressors may be more significant for different people.
Acknowledgements:
This research was supported by grants from the University of Connecticut Institute for Collaboration on Health, Intervention and Policy (InCHIP) and by a grant from the National Institute on Alcoholism and Alcohol Abuse (1R34AA027455–01A1)
Footnotes
During data collection, participants also completed the Generalized Anxiety Disorder scale (Spitzer et al., 2006), the Perceived Stress Scale (Cohen et al., 1983), the Difficulties in Emotion Scale (Victor & Klonsky, 2016), and the Depression Anxiety Stress Scales (S. Lovibond & P. Lovibond, 1995).
References
- Albanesi S, Gihleb R, Huo J, & Kim J (2020). Household insurance and the macroeconomic impact of the novel coronavirus. Unpublished Manuscript, University of Pittsburgh. [Google Scholar]
- Aldridge AA, & Roesch SC (2008). Developing coping typologies of minority adolescents: A latent profile analysis. Journal of Adolescence, 31(4), 499–517. 10.1016/j.adolescence.2007.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral IA, & Bhagawati KC (2019). Post traumatic stress disorder and coping strategies among adult survivors of earthquake, Nepal. BMC Psychiatry, 19(1), 118. 10.1186/s12888-019-2090-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartneck C, Duenser A, Moltchanova E, Zawieska K, & Voracek M (2015). Comparing the similarity of responses received from studies in Amazon’s Mechanical Turk to studies conducted online and with direct recruitment. Plos One, 10(4), 1–23. 10.1371/journal.pone.0121595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CJ, Boden JM, Horwood LJ, & Mulder RT (2017). The role of peri-traumatic stress and disruption distress in predicting symptoms of major depression following exposure to a natural disaster. Australian & New Zealand Journal of Psychiatry, 51, 711–718. 10.1177/0004867417691852. [DOI] [PubMed] [Google Scholar]
- Bick A, & Blandin A (2021). Real-time labor market estimates during the 2020 coronavirus outbreak. Social Science Research Network. 10.2139/ssrn.3692425 [DOI] [Google Scholar]
- Bolt MA, Helming LM, & Tintle NL (2018). The associations between self-reported exposure to the Chernobyl nuclear disaster zone and mental health disorders in Ukraine. Front Psychiatry. 9. 10.3389/fpsyt.2018.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA, Galea S, Bucciarelli A, & Vlahov D (2006). Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychological Science, 17(3), 181–186. 10.1111/j.1467-9280.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Bosman J & Smith M (2020, June 14). Coronavirus cases spike across sun belt as economy lurches into motion. New York Times. https://www.nytimes.com/2020/06/14/us/coronavirus-united-states.html?auth=login-google
- Brackbill RM, Alper HE, Frazier P, Gargano LM, Jacobson MH, & Solomon A (2019). An assessment of long-term physical and emotional quality of life of persons injured on 9/11/2001. International Journal of Environmental Research and Public Health, 16, 1054. 10.3390/ijerph16061054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395, 912–920. 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control (2020) Coronavirus (COVID 19): How to protect yourself and others. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html.
- Cohen S, & Janicki-Deverts D (2012). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006 and 2009. Journal of Applied Social Psychology, 42(6), 1320–1334. 10.1111/j.1559-1816.2012.00900.x. [DOI] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- COVID-19 Forecasts. (2020, May 14). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/covid-data/forecasting-us.html
- Drapeau A, Marchand A, & Beaulieu-Prevost D (2012). Epidemiology of psychological distress. In L’Abate L (Ed.), Mental illnesses – Understanding prediction and control (pp. 105–134). InTech. [Google Scholar]
- El-Khatib Z, Jacobs GB, Ikomey GM, & Neogi U, (2020). The disproportionate effect of COVID-19 mortality on ethnic minorities: genetics or health inequalities? EClinicalMedicine, 23(100430), 1–2. 10.1016/j.eclinm.2020.100430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson SL, Moore EWG, Hull DM (2019). Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. International Journal of Behavioral Development, 44(5), 1–11. 10.1177/0165025419881721. [DOI] [Google Scholar]
- Fernandez RS, Crivelli L, Guimet NM, Allegri RF, & Pedreira ME (2020). Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. Journal of Affective Disorders, 277, 75–84. 10.1016/j.jad.2020.07.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fussell E, & Lowe SR (2014). The impact of housing displacement on the mental health of low-income parents after hurricane Katrina. Social Science & Medicine, 113, 137–144. 10.1016/j.socscimed.2014.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Merchant R, M., & Lurie N (2020). The mental health consequences of Covid-19 and physical distancing the need for prevention and early intervention. JAMA Internal Medicine, 180(6), 817. 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Garfin DR, Silver RC, Gil-Rivas V, Guzmán J, Murphy JM, Cova F, et al. (2014). Children’s reactions to the 2010 Chilean earthquake: The role of trauma exposure, family context, and school-based mental health programming. Psychological Trauma: Theory, Research, Practice, and Policy, 6(5), 563–573. 10.1037/a0036584. [DOI] [Google Scholar]
- Henckens MJ, Klumpers F, Everaerd D, Kooijman SC, van Wingen GA, & Fernández G (2016). Interindividual differences in stress sensitivity: Basal and stress-induced cortisol levels differentially predict neural vigilance processing under stress. Social Cognitive and Affective Neuroscience, 11(4), 663–673. 10.1093/scan/nsv149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D, & Brown AD (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12, 331–335. 10.1037/tra0000592. [DOI] [PubMed] [Google Scholar]
- Horesh D, Lev-Ari RK, & Hasson-Ohayon I (2020). Risk factors for psychological distress during the COVID-19 pandemic in Israel: Loneliness, age, gender, and health status play an important role. British Journal of Health Psychology, 25, 925–933. 10.1111/bjhp.12455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johannesson KB, Arinell H, & Arnberg FK (2015). Six years after the wave. Trajectories of posttraumatic stress following a natural disaster. Journal of Anxiety Disorders, 36, 15–24. 10.1016/j.janxdis.2015.07.007. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University Center for Systems Science and Engineering (2021, February 18). COVID-19 dashboard. https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
- Jose R, Holman EA, & Silver RC (2019). Community organizations and mental health after the 2013 Boston Marathon bombings. Social Science & Medicine, 222, 367–376. 10.1016/j.socscimed.2018.08.019. [DOI] [PubMed] [Google Scholar]
- Kees J, Berry C, Burton S, & Sheehan K (2017). An analysis of data quality: Professional panels, student subject pools, and Amazon’s Mechanical Turk. Journal of Advertising, 46, 141–155. 10.1080/00913367.2016.1269304. [DOI] [Google Scholar]
- Kim S, Jang H, Myung W, Kim K, Cha S, Lee H, Cho SK, Kim B,…Won H (2019). Heritability estimates of individual psychological distress symptoms from genetic variation. Journal of Affective Disorders, 252, 413–420. 10.1016/j.jad.2019.04.011. [DOI] [PubMed] [Google Scholar]
- Labarda CE, Jopson QDQ, Hui VK, & Chan CS (2020). Long-term displacement associated with health and stress among survivors of typhoon Haiyan. Psychological Trauma: Theory, Research, Practice, and Policy, 12(7), 765–773. 10.1037/tra0000573. [DOI] [PubMed] [Google Scholar]
- Layne SP, Hyman JM, Morens DM, & Taubenberger JK (2020). New coronavirus outbreak: Framing questions for pandemic prevention. Science Translational Medicine, 12(534), eabb1469. 10.1126/scitranslmed.abb1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond SH, & Lovibond PF (1995). Manual for the Depression Anxiety Stress Scales. Psychology Foundation. [Google Scholar]
- Main A, Zhou Q, Ma Y, Luecken LJ, & Liu X (2011). Relations of SARS-related stressors and coping to Chinese college students’ psychological adjustment during the 2003 Beijing SARS epidemic. Journal of Counseling Psychology, 58, 410–423. 10.1037/a0023632. [DOI] [PubMed] [Google Scholar]
- Masyn KE (2013). Latent class analysis and finite mixture modeling. In Little T (Eds.), The Oxford handbook of quantitative methods (pp. 551–611). Oxford University Press. [Google Scholar]
- McGuire AP, Gauthier JM, Anderson LM, Hollingsworth DW, Tracy M, Galea S, & Coffey SF (2018). Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: Effects for displaced and nondisplaced residents. Journal of Traumatic Stress, 31(2), 223–233. 10.1002/jts.22270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira DN, & Pinto da Costa M (2020). The impact of the COVID-19 pandemic in the precipitation of intimate partner violence. International Journal of Law and Psychiatry, 71, 101606. 10.1016/j.ijlp.2020.101606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen K, & Hughes TL (2018). Comparing Amazon’s Mechanical Turk platform to conventional data collection methods in the health and medical research literature. Journal of General Internal Medicine, 33, 533–538. 10.1007/s11606017-4246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen B, & Muthen L (2018). Mplus user’s guide. Muthen and Muthen. [Google Scholar]
- North CS, & Pfefferbaum B (2013). Mental health response to community disasters: A systematic review. JAMA, 310(5), 507–518. 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- Park CL, Finkelstein-Fox L, Russell BS, Fendrich M, Hutchison M, & Becker J (2021). Americans’ distress early in the COVID-19 pandemic: Protective resources and coping strategies. Psychological Trauma: Theory, Research, Practice, and Policy. Advance online publication. 10.1037/tra0000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Riley K & Snyder L (2012). Meaning making coping, making sense, & posttraumatic growth following the 9/11 terrorist attacks. The Journal of Positive Psychology, 7(3), 198–207. 10.1080/17439760.2012.671347. [DOI] [Google Scholar]
- Power K (2020). The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice, and Policy, 16(1), 67–83. 10.1080/15487733.2020.1776561. [DOI] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, & Xu Y (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33, 1–3. 10.1136/gpsych-2020100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosellini AJ, Coffey SF, Tracy M, & Galea S (2014). A person-centered analysis of posttraumatic stress disorder symptoms following a natural disaster: Predictors of latent class membership. Journal of Anxiety Disorders, 28(1), 16–24. 10.1016/j.janxdis.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell BS, Hutchison M, Tambling RR, Tomkunas AJ, & Horton AL (2020). Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent-child relationship. Child Psychiatry & Human Development, 51, 671–682. 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto M, Nemoto H, Kobayashi N, Kikuchi S, Honda N, Kim Y, Kelman I, & Tomita H (2019). Post-disaster mental health and psychosocial support in the areas affected by the great east Japan earthquake: A qualitative study. BMC Psychiatry 19(1), 261. 10.1186/s12888-019-2243-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan KB, & Pittman M (2016). Amazon’s Mechanical Turk for academics: The HIT handbook for social science research. Melvin & Leigh. [Google Scholar]
- Sheehan KB (2018). Crowdsourcing research: Data collection with Amazon’s Mechanical Turk . Communication Monographs: Special Issue: Advances in Methods and Statistics, 85, 140–156. 10.1080/03637751.2017.1342043. [DOI] [Google Scholar]
- Solomon HV (2020). COVID-19 checklist: Mask, gloves, and video chatting with grandpa. Psychiatry Research, 288, e112986. 10.1016/j.psychres.2020.112986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder the GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sprague CM, Kia-Keating M, Felix E, Aff T, Reyes G, & Aff W (2015). Youth psychosocial adjustment following wildfire: The role of family resilience, emotional support, and concrete support. Child Youth Care Forum, 44(3), 433–450. 10.1007/10566-014-9285-7. [DOI] [Google Scholar]
- Spurk D, Hirschi A, Wang M, Valero D, & Kauffeld S (2020). Latent profile analysis: A review and “how to” guide of its application within vocational behavior research. Journal of Vocational Behavior, 120, 103445. 10.1016/j.jvb.2020.103445. [DOI] [Google Scholar]
- Tambling RR, Russell BS, Park CL, Fendrich M, Hutchinson M, Horton AL, & Tomkunas AJ (2020). Measuring cumulative stressfulness: Psychometric properties of the COVID-19 Stressors Scale. Health Education and Behavior, 48(1), 20–28. 10.1177/1090198120979912. [DOI] [PubMed] [Google Scholar]
- United States Bureau of Labor (2020, July 31). Unemployment Rate. https://data.bls.gov/timeseries/LNS14000000
- Verger P, Rotily M, Brenot J, Baruffol E, & Bard D (2003). Assessment of exposure to a flood disaster in a mental health study. Journal of Exposure Analysis and Environmental Epidemiology, 13(6), 436–442. 10.1038/sj.jea.7500290. [DOI] [PubMed] [Google Scholar]
- Victor SE, & Klonsky ED (2016). Validation of a brief version of the difficulties in emotional regulation scale (DERS-18) in five samples. Journal of Psychopathology Behavior Assessment, 38, 582–589. 10.1007/s10862-016-9547-9. [DOI] [Google Scholar]
- World Health Organization (2020). Coronavirus disease (COVID-19) advice for the public: Advocacy. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/healthy-parenting
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


