Abstract
Alzheimer’s disease (AD) is a progressive, neurodegenerative disorder that currently has reached epidemic proportions among elderly populations around the world. In China, available traditional Chinese medicines (TCMs) that organically combine functional foods with medicinal values are named “Medicine Food Homology (MFH)”. In this review, we focused on MFH varieties for their traditional functional features, substance bases, clinical uses, and mechanisms of action (MOAs) for AD prevention and treatment. We consider the antiAD active constituents from MFH species, their effects on in vitro/in vivo AD models, and their drug targets and signal pathways by summing up the literature via a systematic electronic search (SciFinder, PubMed, and Web of Science). In this paper, several MFH plant sources are discussed in detail from in vitro/in vivo models and methods, to MOAs. We found that most of the MFH varieties exert neuroprotective effects and ameliorate cognitive impairments by inhibiting neuropathological signs (Aβ-induced toxicity, amyloid precursor protein, and phosphorylated Tau immunoreactivity), including anti-inflammation, antioxidative stress, antiautophagy, and antiapoptosis, etc. Indeed, some MFH substances and their related phytochemicals have a broad spectrum of activities, so they are superior to simple single-target drugs in treating chronic diseases. This review can provide significant guidance for people’s healthy lifestyles and drug development for AD prevention and treatment.
Keywords: Alzheimer’s disease, traditional Chinese medicines, medicine food homology, broad-spectrum activities, drug development
1. Introduction
Alzheimer’s disease (AD) is a specific onset and process of cognitive and functional decline with particular neurological characteristics, especially in people over 65 years of age with high morbidity and mortality [1,2]. Prince M et al. estimated that 65.7 million people in 2030 and 115.4 million people in 2050 will live with dementia worldwide, which implies an extremely serious burden to global public health and social welfare [3]. Deficits in the ability to encode and store new memories characterize the initial stages of the disease. Subsequent progressive changes in cognition and behavior accompany the later stages. Due to the complexity of the etiology of AD, its pathological and physiological mechanisms have been controversial. To date, the core pathological hallmarks recognized by researchers are amyloid plaques, neurofibrillary tangles, synapses, and/or neuronal loss [4,5].
At present, the main licensed pharmacologic therapy of patients is cholinesterase inhibitors (donepezil, rivastigmine, and galantamine) and noncompetitive N-methyl-D-aspartate receptor (NMDA) antagonists (memantine). Cholinesterase inhibitors are licensed therapy for patients with mild-to-moderate Alzheimer’s disease, and NMDA antagonists are licensed therapy for patients with moderate-to-severe AD [6]. Other treatments include immunotherapy (bapineuzumab), amyloid aggregators (tramiprosate), tau aggregation inhibitors (methylthioninium chloride), glycogen synthase kinase 3 (GSK3) inhibitors (lithium), and natural products and vitamins (ginkgo biloba, omega 3 fatty acids, docosahexaenoic acid, and vitamin E) [6,7].
In recent years, with the improvement of public health awareness, people have paid increasing attention to the prevention and treatment of chronic diseases through diet, such as a “low-, fermentable oligo-, and di-, monosaccharides and polyols” diet, Mediterranean diet, a low-lactose diet, and medicinal food herb diet [8,9,10,11]. The concept of medicine food homology (MFH) originally came from the (Huangdi’s) Internal Classic in ancient China, which means that Chinese medicine and food are of the same origin, and, thus, they can be used as food and administered to patients as medication to regulate the human body’s metabolic disturbances or imbalances [11,12].
In China, many traditional Chinese medicines (TCMs) are functional foods and dietary supplements, such as Panax ginseng C.A. Mey., Crocus sativus L., and Angelica acutiloba (Siebold & Zucc.) Kitag. For cultural reasons, herbal remedies are called alternative therapies in North America and other countries [8]. MFH substances with abundant resources have exhibited pharmacological effects at preventing and treating a variety of diseases, including cancers, diabetes, cardiovascular diseases, Alzheimer’s disease, Parkinson’s disease, viruses, influenza, and, in particular, chronic diseases [13]. To ensure the safety of functional foods from TCM, the National Health Commission of the People’s Republic of China released specific provisions on MFH items, which considered 109 TCMs as functional foods for alleviating or curing various chronic diseases through the diet as of 2019 [8].
For this paper, the literature review covers the period between 2001 and 2021 relating to MFH items with antiAD effects. The literature was collected from the SciFinder, EMBASE, Mendeley, Google Scholar, PubMed, and Web of Science databases. The keywords used for the literature search were as follows: “Medicine-food Herb and Alzheimer’s disease”, “Medicine-food Herb and chemical components or phytoconstituents or natural products”, and “Medicine-food Herb and clinical evidence and Alzheimer’s disease”. Then, we tried to classify all data pertaining to the pharmacological effects of MFH functional foods on memory in different animal models, methods, mechanisms, etc. The summarized results comprised a total of 28 plant species, 35 phytochemicals, and 9 TCM formulations of MFH resources with antiAD activities exhibited in various preclinical and five clinical studies (Table 1, Table 2, Table 3, Table 4 and Table 5). The main MFH items that will be introduced are those, which are often used, such as “Monarch medicine” and clinical evidence, including Angelica acutiloba (Siebold & Zucc.) Kitag., Panax ginseng C.A. Mey., and Poriacocos (Schw.) Wolf. This review will provide further support for the basic and clinical research on MFH and the use of functional foods in a healthy lifestyle in the future.
Table 1.
The clinical evidence of prevention and treatment of Alzheimer’s disease using MFH.
| No. | Registration No | Number of Subjects | Trial Period | Intervention Model | Intervention Group | Controlled Group | Findings/Mechanism | References |
|---|---|---|---|---|---|---|---|---|
| 1 | NCT00391833 | 77 patients | 12 weeks | An open-label study | Panax ginseng C.A. Mey. | Panax ginseng is clinically effective in the cognitive performance of AD patients. | [14] | |
| 2 | 61 patients | 12-week | An open-label trial | Korean red Panax ginseng C.A. Mey. | Either donepezil, galantamine, memantine or rivastigmine | Korean red ginseng showed good efficacy for the treatment of Alzheimer’s disease | [15] | |
| 3 | 91 patients | 24-week | A 24-week randomized open-label study | The effect of KRG on cognitive functions was sustained for 2-year follow-up, indicating feasible efficacies of long-term follow-up for Alzheimer’s disease. | [16] | |||
| 4 | IRCT138711051556N1 | 91 patients | 22 weeks | A multicenter, randomized, double-blind controlled trial | Crocus sativus L. | Donepezil | This phase II study provides preliminary evidence of a possible therapeutic effect of saffron extract in the treatment of patients with mild-to-moderate Alzheimer’s disease. | [17] |
| 5 | 56 patients | 16 weeks | A randomized and placebo-controlled trial | Placebo | Saffron is both safe and effective in mild to moderate AD. | [18] | ||
| 6 | 17 patients on crocus and 18 on a waiting list | 12 months | 1-year single-blind randomized, with parallel groups, clinical trial | Crocus is a good choice for management of aMCImd | [19] | |||
| 7 | 24 participants | Cistanche afghanica Gilli | Donepezil | Cistanches Herba could improve cognitive and independent living ability of moderate AD patients, slow down volume changes of hippocampus, and reduce the levels of T-tau, TNF-α, and IL-1β. | [20] |
Table 2.
MFH varieties and their functional features [21].
| Names | Parts to Be Consumed | Therapeutic Class | Features | |
|---|---|---|---|---|
| Chinese Name | English Name | |||
| Ren shen | Panax ginseng C.A. Mey. | Root | Qi-reinforcing medicinal | To reinforce the vital energy, to remedy collapse and restore the normal pulse, to benefit the spleen and lung, to promote the production of body fluid, and to calm the nerves. |
| Xi hong hua | Crocus sativus L. | Stigma | Blood-activating stasis removing medicinal | To activate blood circulation and eliminate blood stasis, to remove heat from blood and counteract toxicity, and to calm the nerves. |
| Rou cong rong | Cistanche afghanica Gilli | Fleshy stem | Yang-reinforcing medicinal | To reinforce the kidney, replenish vital essence and blood, and induce taxation. |
| Dang gui | Angelica acutiloba (Siebold & Zucc.) Kitag. | Root | Blood-tonifying medicinal | To enrich blood, activate blood circulation, regulate menstruation, relieve pain, and relax bowels. |
| Huang qi | Astragalus aaronii (Eig) Zohary | Root | Qi-reinforcing medicinal | To reinforce qi and invigorate the function of the spleen. |
| Fu ling | Poriacocos (Schw.) Wolf | Sclerotium | Diuretic dampness excreting medicinal | To cause diuresis, to invigorate the spleen function, and to calm the mind. |
| Yi zhi ren | Alpinia oxyphylla Miq. | Fruit | Astringent medicinal | To warm spleen, check diarrhea, warm kidney, reduce urine, and secure essence. |
| Sheng jiang | Zingiber officinale Roscoe | Fresh rhizome | Pungent-warm exterior-releasing medicinal | To induce perspiration and dispel cold, to warm the stomach and arrest vomiting, and to resolve phlegm and relieve cough. |
| Yu zhu | Polygonatumodoratum (Mill.) Druce | Rhizome | Yin-tonifying Medicinal | To nourish yin, promote the production of body fluid, and relieve dryness syndromes. |
| Gao liang jiang | Alpinia officinarum Hance | Rhizome | Interior-warming medicinal | To warm the stomach and relieve vomiting, dispel cold, and relieve pain. |
| Xiang ru | Mosla chinensis Maxim. | Aerial parts | Pungent-warm exterior-releasing medicinal | To promote diaphoresis and release to the exterior, to resolve dampness and harmonize the spleen and stomach, to promote water metabolism and release edema |
| Hei hu jiao | Piper nigrum L. | Fruit | Interior-warming medicinal | To dispel cold from the stomach and to eliminate phlegm. |
| Ling zhi | Ganoderma lucidum (Leyss.ex Fr.) Karst. | Dried sporocarp | Qi-reinforcing medicinal | To invigorate qi and calm the nerves and relieve cough and asthma. |
| Sang shen | Morus alba L. | Ear of fruit | Yin-tonifying medicinal | To promote the production of body fluid. |
| Jiang huang | Curcuma longa L. | Tuberoid | Blood-activating and stasis-dispelling medicinal | To eliminate blood stasis, promote the flow of qi, stimulate the release of menstruation, and relieve pain. |
| Ge gen | Puerarialobata (Willd.) Ohwi | Tuberoid | Pungent-warm exterior-releasing medicinal | To relieve fever, to promote the production of body fluid, to facilitate eruption, and to arrest diarrhea. |
| Suan zao ren | Ziziphi Spinosae Semen | Seed | Heart-nourishing tranquillizing medicinal | To replenish the liver, to cause tranquilizations, to arrest excessive perspiration, and to promote the production of body fluid. |
| Gan cao | Glycyrrhiza uralensis Fisch. | Root, rhizome | Qi-reinforcing drugs | To reinforce the function of the spleen and replenish qi, to remove heat and counteract toxicity, to dispel phlegm and relieve cough, to alleviate spasmodic pain, and to moderate drug actions. |
| Lai fu zi | Raphanus sativus L. | Seed | Digestants | To promote digestion and relieve abdominal distension and to relieve cough and resolve phlegm. |
| Rou gui | Cinnamomum cassia (L.) J.Presl | Bark | Interior-warming medicinal | To supplement body fire, to reinforce yang, and to lead the fire back to the kidney, to dispel cold and relieve pain, and to activate blood circulation and stimulate menstrual discharge. |
| Tian ma | Gastrodia elata Blume | Stem and tuber | Liver-pacifying and wind-extinguishing medicinal | To extinguish wind and check tetany, to calm liver and subdue yang, to dispel wind, and to free network vessels. |
| Gou qi zi | Lycium barbarum L | Fruit | Yin-tonifying medicinal | To benefit the liver and the kidney, to replenish vital essence, and to improve eyesight. |
| Yu xing cao | Houttuynia cordata thunb. | Aerial parts | Heat-clearing and detoxicating medicinal | To remove toxic heat, to promote the drainage of pus, and to relieve dysuria. |
| Jue ming zi | Cassia obtusifolia L. | Ripe seed | Fire-purging medicinal | To remove heat from the liver, to improve eyesight, and to relax bowels. |
| Shan zhu yu | Cornus officinalis Siebold & Zucc. | Fruit | Astringent medicinal | To replenish the liver and kidney, to restrain seminal discharge, and to relieve collapse. |
| Da zao | Ziziphus jujuba Mill. | Ripe fruit | Qi-reinforcing medicinal | To tonify the spleen and replenish qi, to nourish blood, and to ease the mind. |
| Shi hu | Dendrobium nobile Lindl. | Fresh or dried stems | Yin-tonifying medicinal | Treatment of thirst due to impairment to yin or deficiency of body fluid, loss of appetite with nausea, fever in deficiency conditions after a severe disease, and impaired vision. |
| Bi bo | Piper longum L. | Ear of fruit | Interior-warming medicinal | To warm the interior and expel internal cold |
Table 3.
The mechanism of “Jun medicine” of MFH in TCM formulae against Alzheimer’s disease.
| No. | “Jun Medicine” of MFH | TCH Formulae | Dose Range | Controls | Experimental Models | Mechanism | References | |||
|---|---|---|---|---|---|---|---|---|---|---|
| In Vitro | In Vivo | Positive | Negative | In Vitro | In Vivo | |||||
| 1 | Panax ginseng C.A. Mey. | Shenma Yizhi Decoction (SMYZD) | 2.97, 11.88 g/kg | Wistar rats | ↑NG2, ↑Ang1, ↑PDGFR-β | [22] | ||||
| Yizhi Qingxin Formula (YZQXF) | 0.3, 0.6 mg/kg | Donepezil hydrochloride | Distilled water | Wistar rats | ↑IL-10, ↓amyloid-β peptide, ↓TNFα, ↓IL2, ↓IL-6, ↑BDNF, ↑TrkB, ↑BDNF/TrkB pathway, ↑Erk and Akt signaling | [23] | ||||
| 2.6, 5.2, 10.4 g·kg−1 | Distilled water | APP/PS1 mice | ↑LC3II/LC3I, ↑Beclin1, ↓mTOR, ↑4EBP1, ↓p62, ↑cathepsin D, ↑V-ATPase, ↓Aβ | [24] | ||||||
| Jangwonhwan | 50, 75, 100, 150 µg/mL | 400 mg/kg | SH-SY5Y cells | APPswe/PS1De9 mice | ↓Abeta (1-42), ↓Abeta (1-40) | [25] | ||||
| 2 | Angelica acutiloba (Siebold & Zucc.) Kitag. | Danggui Buxue Tang (DGBXT) | 25, 50, 75, 100 µM | Cortical neurons | ↑Bcl2/Bax, ↓cleaved-caspase 3/9, ↓PARP | [26] | ||||
| Danggui-Shaoyao-San (DGSYS) | 1.6, 3.2, 4.8 g/kg | SAMR1 and SAMP8 mice | ↑E2, ↑NO, ↑glycine | [27] | ||||||
| 1.6, 3.2, 6.4 g/kg | Aricept | Saline | APP/PS1 mice | ↓PEG2, ↓TXB2, ↓LTB4, ↓cPLA2, ↓COX-1, ↓COX-2 | [28] | |||||
| Fo Shou San (FSS) | 1.6, 3.2, 6.4 g/kg | Donepezil | Ultrapure water | APP/PS1 mice | ↓LPS, ↑AP, ↓MDA | [29] | ||||
| 3 | Astragalus aaronii (Eig) Zohary | Tiaoxin Recipe | 0.057 g/d | APPswe/PS1De9 mice | ↓amyloid plaque, ↓Aβ1-42 | [30] | ||||
| Fuzheng Quxie Decoction (FZQXD) | 1.3, 2.6 g/kg | SAMP8 mice | ↓HIF1α | [31] | ||||||
| 4 | Poriacocos (Schw.) Wolf | Lingui Zhugan Decoction (LGZGD) | 4.8, 2.4 or 1.2 g/kg | Donepezil | Saline | Sprague–Dawley rats | ↓TNF-α, ↓IL-1β, ↓Aβ1-42, ↓p-Erk1/2, ↓p-p38, ↓p-NF-κB, ↓p-IκBα, ↓MAPK signaling, ↓NF-κB signaling | [32] | ||
Table 4.
Extract from MFH on the role and mechanism of Alzheimer’s disease.
| No. | Extract of MFH | Dose Range | Controls | Experimental Models | Mechanism | References | |||
|---|---|---|---|---|---|---|---|---|---|
| In Vitro | In Vivo | Positive | Negative | In Vitro | In Vivo | ||||
| 1 | Red Panax ginseng C.A. Mey. | 1, 10, 100, 500, and 1000 μg/mL | 100 mg/kg | HT22 cells | 5XFAD mice | ↓Mitochondrial Dysfunction; ↓Aβ Deposits; ↓Neuroinflammation; ↓Neuronal Death | [33] | ||
| Fermented Panax ginseng C.A. Mey. | 200 or 400 μg/mL | 400 and 800 mg/kg | Saline | HeLa cells | ICR mice; APP/PS1 mice | ↓Aβ42 | [34] | ||
| White Panax ginseng C.A. Mey. extract | 100 and 500 mg/kg | Saline | ICR mice | ↓cell death; ↓AβO1–42-induced microglial activation; ↑synaptophysin-positive areas; ↑optical density of ChAT immunoreactivity | [35] | ||||
| Korean white ginseng, red ginseng extract, and black ginseng | 0.5, 2, 4, 6, 8 mg/mL | 2 mg/kg | 0.9% saline | Spectrophotometric method | ICR mice | ↓AChE; ↓BuChE | [16] | ||
| 2 | Crocus Sativus L. | 1, 10 μM | PC-12 cells | ↓caspase-3, ↓Bcl-XL mRNA | [36] | ||||
| 3 | Poriacocos (Schw.) Wolf | 1.2 g kg−1/day | APP/PS1 mice | ↓Aβ | [37] | ||||
| 100, 300, 900 mg/kg | Fluoxetine | 0.5% carboxymethyl cellulose | Sprague–Dawley rats | ↓p38, ↓NF-κB, ↓TNF-α | [38] | ||||
| 4 | Alpinia oxyphylla Miq. | 80, 120, 160, 200, 240 μg/mL | Cerebral cortices of BALB/c mouse | ↓glutamate-induced apoptosis | [39] | ||||
| 20, 40, 60, 80, 100, 150, 200 μg/mL | 30, 60, 100, 150, 200 mg/mL | RSC96 Schwann cells | Sprague–Dawley rats | ↑uPA, ↑tPA, ↑MMP-9, ↑MAPKs, ↑Pas, ↑MMP9 signaling, ↑MEK1/2, ↑ERK1/2, ↑JNK1/2, ↑p38, ↑MMP-2, ↓TIMP-1, ↓TIMP-2 | [40] | ||||
| 360 mg/kg | Donepezil | Saline | ICR mice | ↓IBA-1, ↓IL-1β, ↓Aβ1–42, ↓p-tau | [41] | ||||
| 180, 360 mg/kg | Donepezil | Saline | ICR mice | ↑GSH-px, ↓MDA, ↓Aβ1–42 | [42] | ||||
| 5 | Zingiber officinale Roscoe | 1, 2, 4 g/kg | Saline | Sprague–Dawley rats | ↓MDA, ↑SOD, ↑CAT, ↓NF-Κb, ↓IL-1β | [43] | |||
| 50, 100, 200 mg/kg | Carboxymethyl cellulose | Wistar rats | ↓IL-1β, ↓GFAP | [44] | |||||
| 0.13, 0.19, 0.25, 0.31 mg/mL | Rat brain | ↓AChE, ↓MDA | [45] | ||||||
| 0.02, 0.1, 0.2 mg in 2 Μl of DMSO | Rat hippocampal | ↓Abeta oligomers | [46] | ||||||
| 6 | Polygonatumodoratum (Mill.) Druce | 3% lyophilized 70% ethanol extracts | Hippocampal Slices of Sprague–Dawley rats | Insulin signaling, energy↑, glucose metabolism↑, tau protein↓ | [47] | ||||
| 7 | Piper nigrum L. | 187.5 or 93.75 mg/kg | Aluminum chloride | Rats | ↑Ach, ↑TAC, ↑SOD, ↓AchE, ↓MDA, ↓NO | [48] | |||
| 50 mg/kg, 100 mg/kg | Diazepam | Wistar rats | ↓SOD, ↓GPX, ↓CAT, ↓GSH, ↓MDA | [49] | |||||
| 8 | Morus alba L. | 0.1, 1, 10 μg/mL | 20 mg/kg, 100 mg/kg, and 500 mg/kg | Donepezil | Saline | Hippocampus of Sprague–Dawley rats | Sprague–Dawley rats | ↑GSK-3β, PI3k/Akt pathway, ↓tau hyperphosphorylation, ↑Bcl-2/Bax, ↓depolarization of the mitochondrial membrane, ↓cytochrome C release into the cytosol, ↓caspase-3 | [50] |
| 2, 10, 50 mg/kg | Donepezil | Wistar rats | ↓AChE, ↑Bcl-2-immunopositive neurons density, ↑GSH-Px | [51] | |||||
| 50, 100, 500 mg/kg | SAMR1 and SAMP8 mice | ↓lipid oxidation, ↑antioxidant defense, ↓p38, ↓JNK, ↑ERK1/2, ↑Nrf2, ↓Aβ | [52] | ||||||
| 200 μg/mL | PC12 cells | ↓Apaf1, ↓Bace2, ↓Plcb4 | [53] | ||||||
| 9 | Puerarialobata (Willd.) Ohwi | 340 mg/kg | Saline | C57BL/6J mice | ↓4HNE, ↑pS9-GSK3β, ↓Aß, ↑IDE, ↓pTau, ↑PSD95, ↑synaptophysin | [54] | |||
| 10 | Ziziphi Spinosae Semen | 3, 30 μg/mL | Hippocampal of 5XFAD mice | ↑plasmin | [55] | ||||
| 10, 30, 100 μg/mL | Hippocampal Slices of CD-1 mice | ↑BDNF, BDNF/TrkB signaling, ↑plasmin | [56] | ||||||
| 20, 50, 100, 200, 400 µg/mL | PC12 cells | Caenorhabditis elegans | ↓Aβ-induced toxicity, ↓ROS | [57] | |||||
| 11 | Cinnamomum cassia (L.) J. Presl | 0.75 mg/mL | 100 µg/mL | Water | 5XFAD mice | ↓Aβ species formation | [58] | ||
| 500 μm | 100 mg/kg | BV-2 cells | 5XFAD mice | ↓ROS, ↓p21rac, ↑GSH, ↓GFAP, ↓Iba-1protein, ↓cleaved caspase 3, ↓tau phosphorylation, ↓Aβ | [59] | ||||
| 50 mg/kg | Saline | Sprague–Dawley rat | ↓AChE, ↑GSK3β, ↓cholinesterase | [60] | |||||
| 12 | Gastrodia elata Blume | 0.01, 0.05, 0.5, 1, 5, 10, 20 and 30 mg/mL | 50, 250, 500 mg/kg | Scopolamine | PC12 cells | Sprague–Dawley rats | ↓Neuronal cell death | [61] | |
| 500, 1000 mg/kg | 0.5% cellulose | Rats | ↓Acetylcholinesterase | [62] | |||||
| 13 | Lycium barbarum L | 10−4, 10−3, 10−2, 10−1, 1, 10, 102 μg/mL | Neurons of Sprague–Dawley rats | ↓caspase-3, ↓phospho-JNK-1, ↓phospho-c-Jun-I, ↓phospho-c-Jun-II | [63] | ||||
| 14 | Houttuynia cordata thunb. | 400 mg/kg | Donepezil | Cortical neurons | Male ICR mice | ↓AChE | [64] | ||
| 15 | Cassia obtusifolia L. | 12.5, 25, 50, 100 mg/kg | ICR mice | ↓acetylcholinesterase | [65] | ||||
| 1, 10 μg/mL | 50 mg/kg | Hippocampal | CD-1 mice | ↑GSK-3β, Akt signaling, ↓iNOS, ↓COX | [66] | ||||
| 16 | Ziziphus jujuba Mill. | 0.75, 1.5, 3 mg/mL | Astrocytes from postnatal SD rat | ↑NQO1, ↑GCLC, ↑GCLM, ↑GST | [67] | ||||
| 0.75, 1.5, and 3.0 mg/mL | PC12 cells | PKA signaling, ↑CREB phosphorylation | [68] | ||||||
| 0.375, 0.75, 1.5, and 3.0 mg/mL | RAW 264.7 macrophages | ↓IL-1β, ↓IL-6, ↓pNF-κB-Luc | [69] | ||||||
| 17 | Dendrobium nobile Lindl. | 40 mg/kg | Distilled water | Kunming mice | ↑BDNF, ↑GDNF, ↑CNTF | [70] | |||
| 0.025, 0.25, 2.5 mg/L | Primary neuronal cultures | ↑PSD-95 mRNA, ↑SYP | [71] | ||||||
| 3.5, 35, 350 ng/mL | Hippocampus tissues | ↓Aβ23-35 peptide cytotoxicity, | [72] | ||||||
| 18 | Piper longum L. | 10 μL/g | 0.5% carboxymethyl cellulose | C57BL/6J mice | ↑NR2B, ↑ERK1/2, ↑CaMKIIα | [73] | |||
| 0.5, 1.0, 2.5 μM | 1.5, 3 mg/kg | DMSO + PBS | BV-2 cells | ICR mice | ↓APP, ↓BACE1, ↓COX-2, ↓iNOS, ↓translocation of NF-κB proteins (p50 and p65) to the nucleus, ↓IκB, ↓GFAP, ↓ IBA-1 | [74] | |||
Table 5.
Active ingredients from MFH on the role and mechanism of Alzheimer’s disease.
| No. | Ingredients of MFH | Category | Source | Dose Range | Controls | Experimental Models | Mechanism | References | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| In Vitro | In Vivo | Positive | Negative | In Vitro | In Vivo | ||||||
| 1 | GinsenosideRg1 | Saponin | Panax ginseng C.A. Mey. | 20 mg/kg·d | Saline | SD rats | ↑SOX-2, ↓Aeg-1, ↑GSH-Px, ↑SOD, ↓IL-1β, ↓IL-6, ↓TNF-α, p53, ↓p21Cip1/Waf1, ↓p19Arf | [75] | |||
| 2 | Ginsenoside Rh2 | Saponin | 1.5, 2.5, 3.5 μM | 10 mg/kg | Saline | Cortex neurons | tg2576 mice | ↓Abeta 1-40, ↓Abeta 1-42 | [76] | ||
| 3 | Ginsenoside Rd | Saponin | 2.5 or 5 μmol/L | 10mg/kg | Saline | Cortical neurons | Sprague–Dawley rats | ↓tau hyperphosphorylation, ↑PP-2A | [77] | ||
| 4 | Gintonin | Lysophosphatidic Acids-Protein Complexes | 0.1, 0.3, 1.0, 3.0, 10 μg/mL | B103 cells | transient Ca2+ mobilization, Gproteins/PLC/IP3 receptor/Ca2+ pathways | [78] | |||||
| 5 | Ginsenoside compound K | Saponin | 50, 20, 10, 1 and 0 μM | Primary astrocytes | ↓Aβ, ↓mTOR signal pathway | [79] | |||||
| 6 | Trans-Crocin 4/trans-Crocetin | Crocus sativus L. | 0.1, 1, 10, 100, 1000 μM | SH-SY5Y cells; PC12 cells | ↓BACE1, ↓γ-secretases (PSEN1 and PSEN2 complexes), ↓tau, ↓GSK3β, ↓ERK2, ↓pERK1, ↓pERK2 | [80] | |||||
| 7 | Tubuloside B | Phenylethanoid | Cistanche afghanica Gilli | 1, 10, or 100 mg/L | SH-SY5Ycells | ↓ROS, ↓caspase-3, ↓Ca2+ | [81] | ||||
| 8 | Echinacoside | Phenylethanoid | 60 mg/kg | C57BL/6 mice | ↓HMGB1 | [82] | |||||
| 9 | Vanillic acid | Aromatic acid | Angelica acutiloba (Siebold & Zucc.) Kitag. | 25, 50, and 100 mg/kg | Swiss albinomice | ↓AChE, ↓corticosterone, ↓TNF-α | [83] | ||||
| 10 | Decursinol | 2, 4, and 8 mg | ICR mice | ↓Aβ (1-40) induced memory impairment | [84] | ||||||
| 0.01, 0.1, 1.0, 10 μM | PC12 cells | ↓ROS, ↑Bcl-2/Bax, ↑MMP, ↓cytochrome c, ↓Caspase-3 | [85] | ||||||||
| 11 | Z-ligustilide | Aromatic ester | 40 mg/kg | Saline | SPF Wistar rats | ↓Aβ, ↓APP, ↓p-Tau, ↓NF-κB | [86] | ||||
| 0.01, 1, 3, 10, 30 μM | SH-SY5Y cells; PC12 cells | p38/ PI3-K/Akt pathways | [87] | ||||||||
| 12 | Astragaloside IV | Saponin | Astragalus aaronii (Eig) Zohary | 25, 50, 100 μM | HT22 cells | ↑PPARγ/BDNF signaling pathway | [88] | ||||
| 10.0 mg/kg | Saline | APP/PS1 mice | ↑PPARγ, ↓BACE1 | [89] | |||||||
| 10, 25, 50 µM | SK-N-SH cells | ↓Bax, ↓caspase-3, ↑Bcl-2, ↓mPTP, ↓ROS | [90] | ||||||||
| 13 | 5-Hydroxymethylfurfural | Furfural | Alpinia oxyphylla Miq. | 15, 150 μg/kg | Kunming mice | ↓β-secretase, ↓MDA, ↑GPx, ↑SOD | [91] | ||||
| 14 | Tectochrysin | Flavonoid | 14 µg/kg | Donepezil | Kunming mice | ↑SOD, ↑GSH-px, ↓MDA | [92] | ||||
| 15 | 6-gingerol | Olefinic alcohol | Zingiber officinale Roscoe | 40, 80, 120, 200, 300 μM | PC12 Cells | ↓ROS, ↓NO, ↓LDH, ↑SOD, ↓MDA, ↑p-Akt, ↑p-GSK-3β | [93] | ||||
| 6 mg/kg | DMSO | C57BL/6N mice | ↑emotional memory deficit | [94] | |||||||
| 10 mg/kg | Donepezil | Saline | ICR mice | ↑NGF, ↑PSD-95, ↑synaptophysin | [95] | ||||||
| 16 | Narirutin | Flavonoid | Polygonatumodoratum (Mill.) Druce | 50, 100 mg/kg | APPswe/PS1dE9 mice | ↑CaMKII | [96] | ||||
| 17 | Hesperidin | Flavonoid | 100 mg/kg | Saline | Wistar rats | ↓TBARS, ↑GSH, ↑SOD, ↑catalase, ↑GPx, ↓Bax, ↑Bcl-2 | [97] | ||||
| 1, 3 and 9 μg/mL | 100 mg/kg | 1% CMC | RAW 264.7 cells | APP/PS1 mice | ↓Aβ plaques, ↓iNOS, ↓TNF-α, ↓IL-1β | [98] | |||||
| 20, 40, 80 mg/kg | APP/PS1 mice | ↓TNF-α, ↓C-reactive protein ↓MCP-1, ↓NF-κB, ↑Akt, ↑GSK-3β (Ser 9), ↑Nrf2, ↑HO-1, ↓RAGE, ↓IκBα, ↓NF-κB/p65, ↑Akt/Nrf2 signaling, ↓RAGE/NF-κB signaling | [99] | ||||||||
| 18 | Limonene (+) | Terpene | 50 μg/mL | Fly Strains | ↓Aβ42, ↓NO | [100] | |||||
| 19 | Apigenin | Flavonoid | Mosla chinensis Maxim./Alpinia officinarum Hance | 40 mg/kg | 5% CMC-Na | APP/PS1 Mice | ↓Aβ, ↓BACE1, ERK1/2/CREB/BDNF pathway | [101] | |||
| 0.1, 1.0, 10.0 μM | SH-SY5Y cells | ↓AβPP, ↓ROS, ↑GSH, ↑SOD, ↑GSH-Px, ↓p38 MAPK signal pathway, ↓SAPK/JNK pathway | [102] | ||||||||
| 1, 5 and 10 μM | BV-2 cells | ↓NO, ↓PGE2, ↓JNK, ↓p38 MAPK | [103] | ||||||||
| Neuron/Glial Cells | ↓CD68, ↓OX42, ↓IL-6, ↓gp130, ↑BDNF | [104] | |||||||||
| 20 | Galangin | Flavonoid | Alpinia officinarum Hance | 6.25–400 μM | Rat adult brains | ↓AChE | [105] | ||||
| 21 | β-Caryophyllene | Sesquiterpene | Piper nigrum L. | 16, 48, 144 mg/kg | APP/PS1 mice | ↓COX-2, ↓TNF-α, ↓IL-1β | [106] | ||||
| 22 | Piperine | Alkaloid | 2.5, 5, 10, 25µM | Donepezil | SH-SY5Y cells | ↓AChE | [107] | ||||
| 5 mg/kg | Donepezil | Saline | Wistar rats | ↓MDA, ↓NO | [108] | ||||||
| 5, 10 and 20 mg/kg | Donepezil hydrochloride | Wistar rats | ↓lipid peroxidation, ↓acetylcholinesterase | [109] | |||||||
| 23 | Curcumin | Polyphenol | Curcuma longa L. | 150 mg/kg | APP/PS1 mice | ↓NF-κB pathway, ↑PPAR-γ | [110] | ||||
| 50 mg/kg | PBS | 5xFAD mouse | ↓Aβ, ↓GFAP-IR, ↓Iba-1-IR | [111] | |||||||
| 24 | Aromatic-turmerone | Flavonoid | 5, 10 and 20 μM | HT-22 cells | ↓MMP-9, ↓iNOS, ↓COX-2, ↓TNF-α, ↓IL-1β, ↓IL-6, ↓MCP-1, ↓ROS, ↓IκB-α, ↓JNK, ↓p38 MAPK. | [112] | |||||
| 5, 10 and 20 μM | 50, 100 mg/kg | PBS | BV2 cells | C57 mice | ↓TNF-α, ↓IL-1β, ↓Myd88, ↓MAPK, ↓NF-κB | [113] | |||||
| 50 µg/mL | Cerebellar granule neuron | ↓cleaved caspase-3 | [114] | ||||||||
| 25 | Puerarin | Isoflavone | Puerarialobata (Willd.) Ohwi | 80 mg/kg | Saline | Sprague–Dawley rats | ↓tau hyperphosphorylation, ↓GSK-3β, ↓FGF-2 | [115] | |||
| 30 mg/kg | APP/PS1 transgenic mice | ↑HO-1, GSK-3β/Akt signaling pathways | [116] | ||||||||
| 100 μM | PC12 cells | ↑Bcl-2, ↑p-Bad, ↓caspase-3, ↑Akt | [117] | ||||||||
| 26 | Spinosin | C-glycoside flavonoid | Ziziphi Spinosae Semen | 1.25, 2.5, 5 and 10 mg/kg | 0.5% CMC | ICR mice | ↑ERK–CREB–BDNF signaling | [118] | |||
| 6.25, 12.5, 25 μM | Neuro-2a cells | ↓APP, ↓BACE1, ↑ADAM10, ↓ROS, ↑Nrf2, ↑HO-1, Nrf2/HO-1 signaling pathway | [119] | ||||||||
| 10 and 100 µg/kg | Kunming mice | ↓MDA, ↓Aβ1–42, ↑BDNF, ↑Bcl-2, ↓IL-6 | [120] | ||||||||
| 30 μM | Donepezil | 5XFAD hippocampus | ↑LTP, ↑plasmin | [121] | |||||||
| 0.1, 1, and 10 μg/mL | 4, 20, 100 and 500 μg/mL | Donepezil | Hippocampus | ICR mice | ↑choline acetyltransferase | [122] | |||||
| 27 | Liquiritin | Flavonoids | Glycyrrhiza uralensis Fisch. | 25, 50, 100 mg/kg | Donepezil (3 mg/kg) | SD rats | ↑GSH-Px, ↑SOD, ↓8-OHdG, ↓MDA | [123] | |||
| 28 | Glabridin | Flavonoid | 1, 2 and 4 mg kg–1 | Scopolamine (0.5 mg kg–1) | 0.3 % carboxymethyl cellulose suspension | Kunming mice | ↓cholinesterase | [124] | |||
| 29 | Liquiritigenin | Flavonoid | 2.5, 5, 10, 20, 50, and 100 μM | 30 mg/kg | 0.1% sodium carboxymethyl cellulose | N2A cells; BV2 cells | APP/PS1 double transgenic mice | ↓NLRP3, ↓cleaved caspase-1, ↓caspase-3, ↓IL-1β, ↓TNF-α, ↑IL-4, ↑IL-13, ↓BAX, ↑Bcl-2, ↓Aβ, ↑NEP, ↑IDE | [125] | ||
| 30 | Sulforaphene | Isothiocyanates | Raphanus sativus L. | 0.5, 1, 2, 4, 8, 16, and 32 μM | 25, 50 mg/kg | Donepezil (5 mg/kg) | ddH2O | BV-2 cells | SD rats | ↓TNF-α; IL-6; ↑IL-10, ↑p-Akt (Ser473)/Akt, ↑p-GSK-3β (Ser9)/GSK-3β, ↓NO, ↓NF-κB | [126] |
| 31 | Gastrodin | Phenolic Glycosides | Gastrodia elata Blume | 60 mg/kg | Saline | Sprague–Dawley rats | ↓Aβ1-40/42, ↓APP, ↓β-site APP-cleaving, ↓Beclin-1, ↓LC3-II, ↓p62, ↓Bax, ↑Bcl-2, P38 MAPK signaling pathway | [127] | |||
| 32 | P-coumaric acid | Phenylacrylic acid | Cornus officinalis Siebold & Zucc. | 5, 25, 50 µM | PC12 cells | ↓BACE1, ↓iNOS, ↓p65, ↓ERK1/2, ↓JNK | [128] | ||||
| 33 | Ursolic acid | Pentacyclic triterpenoids | 1,10, 20 µM | PC12 cells | ↓iNOS, ↓COX-2, ↓p65, ↓p-38, ↓JNK, ↓ERK | [128] | |||||
2. Medicine and Food Herb Extract and Its Ingredients against Alzheimer’s Disease
2.1. Panax Ginseng C.A. Mey
2.1.1. Traditional Functional Features
Panax ginseng, an herb from the Araliaceae family, is a qi-tonifying medicinal substance with the effects of tranquilizing the mind and replenishing wisdom [129]. Its supposed health benefits are such that it is used in many countries. Ginseng is “generally recognized as safe” (GRAS) for consumption by adults by the U.S. Food and Drug Administration [130].
2.1.2. MOAs of the Extract
Korean white ginseng, red ginseng extract, and black ginseng are the main processed products of ginseng. Lee et al. reported that their extracts can inhibit AChE and BuChE in a concentration-dependent manner in scopolamine (SCOP)-induced amnesic mice. The IC50 values are 1.72 mg/mL, 5.89 mg/mL, and 6.30 mg/mL [16]. Simultaneously, the processed products of ginseng showed their antiAD mechanisms. Specifically, in vitro and in vivo findings indicated that red ginseng significantly ameliorated AD-related pathologies, such as Aβ deposition, gliosis, and neuronal loss [33]. Fermented ginseng extract enhanced behavioral memory function in an effort to reduce Aβ levels in ICR mice and TG mice and in HeLa cells [34]. Furthermore, white ginseng extract (100 and 500 mg/kg/day) could improve memory impairment by attenuating neuronal damage and neuroinflammation caused by AβO in intrahippocampal AβO (10 μM)-injected mice [35] (Figure 1).
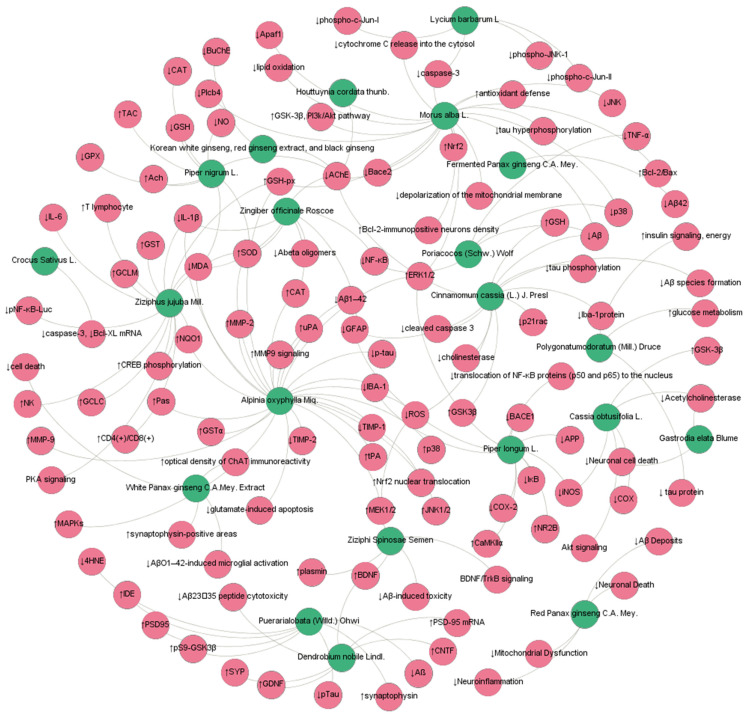
Figure 1.
MFH antiAD network mechanism diagram. (Blue nodes represent MFH, and red nodes represent targets/pathways).
In addition, in vivo and in vitro pharmacological studies have shown that ginseng plays a key role in antiAD as a “Jun medicine” in TCM prescriptions, such as Shenmayizhi decoction (SMYZD), Yizhi Qingxin formula (YZQXF), and Jangwonhwan.
Evidence has revealed that YZQXF alleviates cognitive deficits by increasing the levels of LC3II/LC3I and Beclin1, remarkably activating 4EBP1 and inhibiting the phosphorylation of mammalian target of rapamycin (mTOR) at Ser2448 in early-onset AD mice [24]. Researchers also showed that YZQXF ameliorated cognitive decline by decreasing BDNF, TrkB, TNFα, IL-2, and IL-6 levels and upregulating acetylcholine and IL-10, thus promoting the activation of Erk and Akt signaling in APP/PS1 mice [23]. In an in vivo model of AD, SMYZD at concentrations of 11.88 g/kg/d can significantly improve memory abilities associated with an increase in the levels of NG2 and Ang1 protein expression levels in Wistar rats [22]. An in vitro study showed that Jangwonhwan at 400 mg/kg/day notably reduced Abeta (1–42) levels and beta-amyloid deposition and partially suppressed oxidative stress accumulation in SH-SY5Y neuroblastoma cells [25].
2.1.3. MOAs of Ingredients
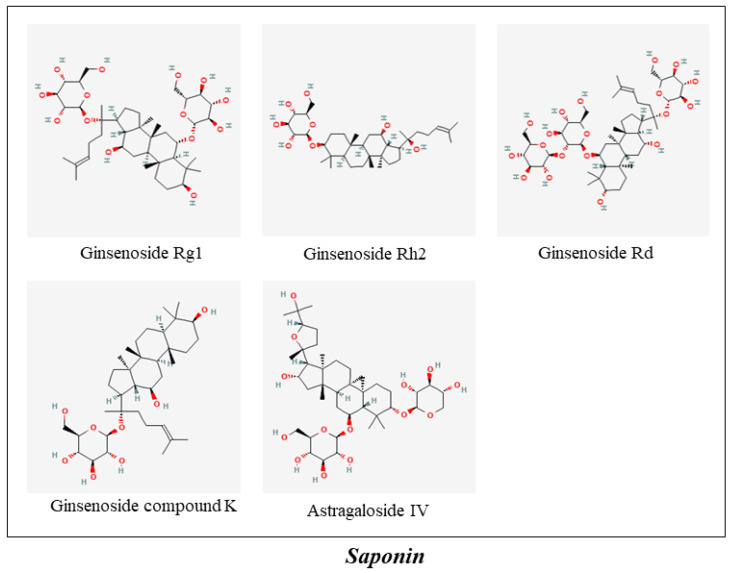
Ginsenoside Rg1, ginsenoside Rh2, and ginsenoside Rd are the main saponins of Panax ginseng. Evidence has indicated that ginsenoside Rg1 can improve cognitive ability, protect NSCs/NPCs, and promote neurogenesis by enhancing antioxidant (GSH-Px, SOD) and anti-inflammatory (IL-1β, IL-6, and TNF-α) capacities in the hippocampus [75]. Ginsenoside Rh2, another saponin component of ginseng, was reported to improve learning and memory function by inhibiting cholesterol and lipid raft concentrations, thus reducing amyloid-beta secretion and APP endocytosis in tg2576 mice [76]. Additionally, ginsenoside Rd (10 mg/kg for 7 days) prevented okadaic acid-induced neurotoxicity through the upregulation of PP-2A in cultured cortical neurons (2.5 or 5 μmol/L for 12 h) [77] (Figure 2).
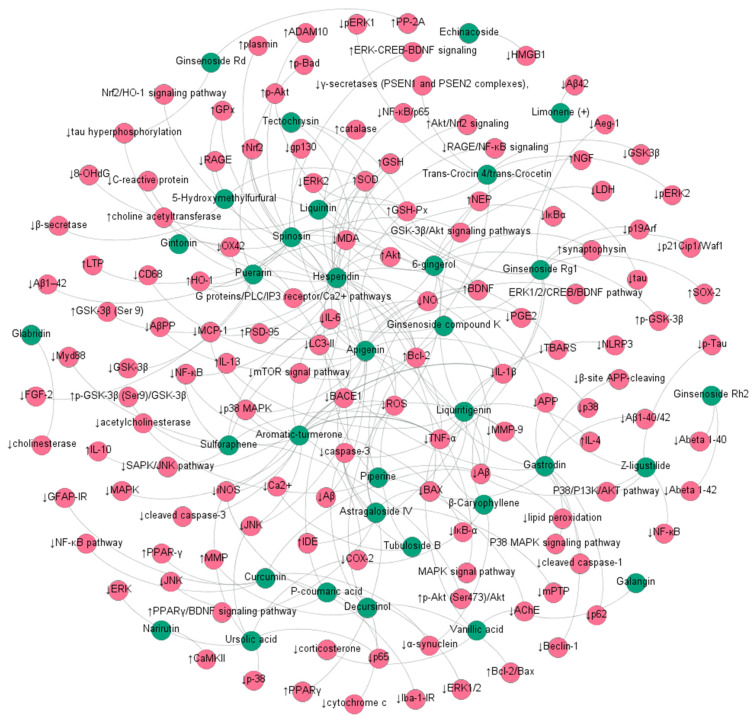
Figure 2.
The ingredients of MFH antiAD network mechanism diagram. (Blue nodes represent ingredient, and red nodes represent targets/pathways).
Notably, gintonin, a novel lysophosphatidic acid–protein complex in ginseng, can exert nervous system protection through the LPA receptor-Gαq/11 protein-phospholipase C-IP3 receptor-[Ca2+] I transient pathway [78,131]. In addition, ginsenoside Compound K is a metabolite of panaxadiol generated by the metabolic actions of intestinal flora in humans. A study demonstrated that Compound K promoted the clearance of Aβ by enhancing autophagy via the mTOR signaling pathway in primary astrocytes [79].
2.1.4. Clinical Evidence
In an open-label study, the Mini-Mental State Examination (MMSE) and AD Assessment Scale (ADAS) began to show improvements and continued up to 12 weeks (p = 0.029 and p = 0.009 vs. baseline, respectively) during 12 weeks of ginseng treatment. The results indicated that Panax ginseng is clinically effective in the treatment of AD. Simultaneously, three randomized open-label studies have shown that Korean Red Ginseng extract is clinically effective and gradually improves cognitive function in AD patients [14,15,16].
2.2. Crocus sativus L.
2.2.1. Traditional Functional Features
Crocus sativus L., a stemless herb that belongs to the Iridaceae family, has blood-activating and menstruation-regulating properties and has been considered an edible food since ancient times. It is mainly used in activating blood circulation and eliminating blood stasis, removing heat from blood and counteracting toxicity, and calming the nerves [132].
2.2.2. MOAs of the Extract
In recent years, researchers have found that Crocus sativus L. has various useful pharmacological properties, such as anticonvulsant, antidepressant, anti-inflammatory, antitumor, and learning and memory-improving effects [133]. A review by Hatziagapiou K et al. summarized the anti-AD mechanism of Crocus sativus L., including the following: antioxidative stress, inhibitory effects of Aβ fibrillogenesis, inhibitory effects of tau aggregation, reduction of glutamatergic synaptic transmission, restoration of cellular antioxidant defenses, and inhibition of cellular apoptosis or death [134]. For example, Soeda et al. designed an experiment to investigate the neuroprotection mechanisms of Crocus sativus L. by inhibiting cellular apoptosis/death. It was found that Crocus sativus L. prevented ethanol-induced impairment of learning and memory with a marked reduction in the caspase-3 and TNF-alpha-induced release of cytochrome c from the mitochondria in PC-12 cells [36] (Figure 1).
2.2.3. MOAs of Ingredients
The in vitro and in vivo research of Ochiai T et al. showed that crocin, a constituent of Crocus sativus L., effectively promoted mRNA expression of gamma-glutamylcysteinyl synthase, contributing to GSH synthesis in mice and, thus, inhibiting neutral sphingomyelinase activity and ceramide formation [135]. Another study indicated that Crocus sativus compounds (trans-Crocin 4 and trans-Crocetin) suppressed the levels of GSK3β and ERK1/2 kinases and significantly reduced total tau and tau phosphorylation, which may be promising candidates in the prevention and treatment of AD [80] (Figure 2).
2.2.4. Clinical Evidence
In a double-blind and randomized study on patients with mild-to-moderate AD, 54 Persian-speaking adults were randomly assigned to receive a capsule of saffron at 30 mg/day (15 mg twice per day) or donepezil at 10 mg/day (5 mg twice per day). This phase II study (Clinical Trials Registry: IRCT138711051556N1) provides preliminary evidence that saffron extract may be used as a potential TCM for mild-to-moderate AD patients [17]. A 16-week, randomized and placebo-controlled study on patients randomly assigned to receive 30 mg/day of saffron capsule or placebo capsule (two capsules/day) demonstrated comparable results with the placebo capsule, and saffron was both safe and effective in mild-to-moderate AD in the short-term [18]. Another single-blind randomized clinical trial by the Tsolaki M et al. group also showed that Crocus is efficacious and safe for the management of amnesic and multidomain MCI [19].
2.3. Cistanche afghanica Gilli
2.3.1. Traditional Functional Features
As a tonic herb, Herba Cistanches has earned the honor of “Ginseng in the deserts” with its function of reinforcing the kidney, replenishing vital essence and blood, and inducing taxation [136].
2.3.2. MOAs of the Extract
Herba Cistanches, a yang-tonifying medicine in China, possesses broad medicinal functions in immunomodulation, endocrine regulation, hepatoprotection, and antiaging, antibacterial, antiviral, and antitumor [137]. In recent years, several excellent reviews have described that Herba Cistanches have great potential in the treatment of age-related diseases. On the one hand, the mechanisms were mainly involved in blocking Aβ 1–42 amyloid deposition, decreasing P-tau phosphorylation, inhibiting the formation of NO, affecting the signaling pathway between ROS, and the opening of Ca2+ channels. On the other hand, Herba Cistanches could induce neuroprotection by inducing cell cycle arrest and apoptosis, increasing the expression of the antiapoptotic proteins, stimulating intestinal epithelial cell proliferation, upregulating TGF-β and CRMP-2 expression levels, and improving antioxidant enzymes [138,139,140].
2.3.3. MOAs of Ingredients
It was also found that phenylethanoid glycosides from Cistanches salsa (10, 50 mg/kg) were able to protect dopaminergic neurons against dopamine neurotoxicity induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine in C57 mice [141]. Another interesting finding indicated that echinacoside, a phenylethanoid from the stems of Cistanche salsa, showed both antiapoptotic and anti-inflammatory properties. Pretreatment with echinacoside also significantly inhibited inflammatory mediators, such as TNF-α, IL-1β, and IL-6 [82] (Figure 2).
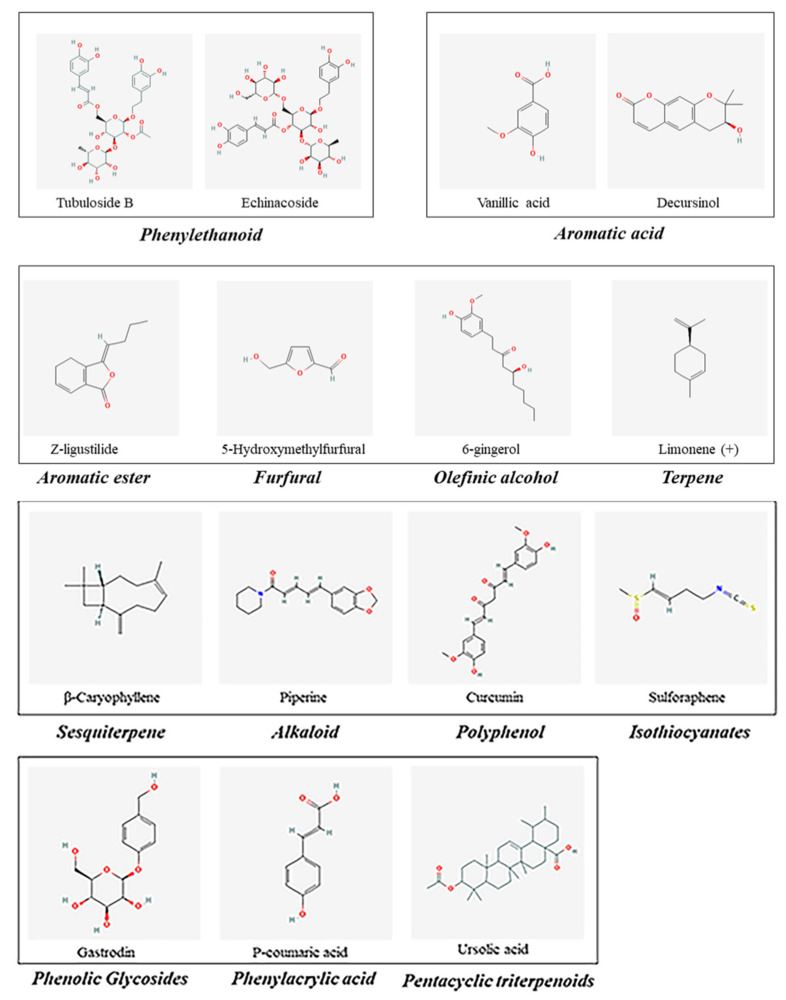
In addition, tubuloside B, a phenylethanoid of the stems of Cistanche salsa, has neuroprotective effects, such as antioxidative stress and antiapoptotic actions (Figure 3). Deng et al. then revealed that tubuloside B (1, 10, or 100 mg/L) attenuated TNF-a-induced apoptosis and the accumulation of intracellular ROS and [Ca2+]I in SH-SY5Y neuronal cells [81].
Figure 3.
Other active ingredients in MFH.
2.3.4. Clinical Evidence
Li N, et al. evaluated the neuroprotective effects of Cistanches Herba on patients with moderate AD. Conclusions were obtained in their studies that Cistanches Herba had potential neuroprotective effects for moderate AD by reducing the levels of T-tau, TNF-α, and IL-1β [20].
2.4. Angelica acutiloba (Siebold & Zucc.) Kitag.
2.4.1. Traditional Functional Features
Angelica acutiloba (Siebold & Zucc.) Kitag. (RAK), an ancient Chinese herb, can be found in Divine Farmers Materia Medica (Han Dynasty, A.D. 25–220). It is a blood-tonifying medicine that can activate blood circulation, regulate menstruation, relieve pain and feminine hernias, and is also called “female ginseng” [142].
2.4.2. MOAs of the Extract
RAK (Danggui), as a main medicine, plays a major role in many TCM tonic blood prescriptions, such as Danggui Buxue Tang (DGBXT), Danggui-Shaoyao-San (DGSYS), and Fo Shou San (FSS).
DGBXT, a historical Chinese herbal decoction, contains just two MFH materials: Astragali Radix and Radix Astragali. An in vitro assay demonstrated that DGBXT protected β-amyloid-induced cell death by altering the expression ratio of Bcl2 to Bax and markedly suppressed the Aβ-induced expression of apoptotic markers (cleaved-caspase 3/9 and PARP) in cultured cortical neurons [26]. Emerging evidence also showed that DGSYS could increase E2, NO, and glycine in SAMP8 mice, contributing to cognitive improvement [27]. Another study showed that DGSYS ameliorated oxidative stress and inflammation by decreasing the levels of PEG2, TXB2, and LTB4 and inhibiting the expression of cPLA2, COX-1, and COX-2, thus ameliorating cognitive deficits in APP/PS1 mice [28]. The FSS formula was reported to ameliorate the symptoms of AD by regulating the gut–liver–brain axis, oxidative stress (MDA), and gastrointestinal tract barrier in APP/PS1 mice [29].
2.4.3. MOAs of Ingredients
RAK and Astragalus aaronii (Eig) Zohary are both important MFH substancess, and many of their active ingredients have been tested in vivo and in vitro to prove their therapeutic effect on AD, such as decursinol, vanillic acid, and ligustilide [143,144]. Pretreatment of mice with decursinol significantly attenuated the Abeta (1–42)-induced impairment in passive avoidance performance in ICR mice [84]. Additionally, decursinol exerted a neuroprotective effect against Aβ25–35-induced neurotoxicity in PC12 cells by suppressing the mitochondrial pathway of cellular apoptosis [85]. In addition, a study showed that vanillic acid reduced AChE, TNF-α, and corticosterone, thus improving antioxidants to contribute to neuroprotection in Swiss albino mice [83].
Importantly, Z-ligustilide (40 mg/kg) significantly ameliorated both AD-related neuropathological signs (Abeta, amyloid precursor protein, and phosphorylated Tau immunoreactivity) and proinflammatory mediators (TNF-alpha and NF-kappaB) in the hippocampus of Wistar rats [86]. In addition, Z-ligustilide can resist the neurotoxicity induced by β -amyloid by simultaneously regulating p38 and PI3-K/Akt pathways in SH-SY5Y cells and PC12 cells [87]. It is worth noting that ligustilide has been demonstrated to permeate the blood–brain barrier in freely moving rat brains, suggesting that ligustilide may be a promising compound for the treatment of AD [145] (Figure 3).
2.5. Astragalus aaronii (Eig) Zohary
2.5.1. Traditional Functional Features
Astragalus aaronii (Eig) Zohary, derived from the roots of Astragalus membranaceus and A. membranaceus var. mongholicus, is a qi-tonifying herb that is widely used in China and shows potent cardiovascular protective effects [146].
2.5.2. MOAs of the Extract
Astragalus aaronii (Eig) Zohary plays a powerful role in the Tiaoxin Recipe and Fuzheng Quxie Decoction (FZQXD). Compared with the normal control group, treatment with the Tiaoxin Recipe decreased the content of serum Aβ1–42 accumulation in APP/PS1 mouse serum. Studies have also shown that microRNA-34a (miR-34a) expression can significantly lead to neuronal apoptosis [147]. The administration of a Tiaoxin Recipe significantly decreased miR-34a expression in APP/PS1 mice [30]. In vivo experiments confirmed that FZQXD could exert a neuroprotective effect on AD via VEGF and VEGF-receptor signaling [31].
2.5.3. MOAs of Ingredients
Astragaloside IV (AS-IV) is a small molecular weight (MW = 784 Da) saponin purified from Astragalus membranaceus that has shown multiple beneficial effects in the prevention and treatment of neurodegenerative disorders [148] (Figure 4). The literature has demonstrated that AS-IV prevents AβO-induced memory impairment by promoting the PPARγ/BDNF signaling pathway [88]. An in vivo study showed that AS-IV treatment increased PPARγ and BACE1 expression and reduced neuritic plaque formation and Aβ levels in the brains of APP/PS1 mice and ultimately attenuated the generation of Aβ [89]. In addition, pretreatment with AS-IV prevented Aβ1–42-induced SK-N-SH cell apoptosis by inhibiting the mPTP opening and ROS generation for the prevention and treatment of neurodegenerative disorders such as AD [90].
Figure 4.
The ingredients of Saponin in MFH.
2.6. Poriacocos (Schw.) Wolf
2.6.1. Traditional Functional Features
Poriacocos (Schw.) Wolf, an edible mushroom, grows underground on the roots of pine trees. It is a water-draining and swelling-dispersing herb for the treatment of edema, nephrosis, gastric atony, acute gastroenteric catarrh, dizziness, and nausea. Poria cocos is often commercially available and is popularly used in Asia [149].
2.6.2. MOAs of the Extract
Extracts from Poriacocos (Schw.) Wolf have various pharmacological properties, including anti-inflammatory, immunomodulatory, anticancer, and antihyperglycemic effects [150]. Huang et al. found that P. cocos water extract significantly attenuated the UCMS-induced turnover rate of DA and 5-HT and inhibited the UCMS-induced activated inflammatory response (p38, NF-κB, and TNF-α) in the frontal cortex by using an SD rat model [38]. Sun Y et al. applied the APP/PS1 mouse model to study the effects of learning and memory and the mechanisms of the aerial part of Poria cocos. The results showed that this medicinal plant, which is also a functional food, might ameliorate cognitive function by reducing the formation of Aβ, increasing its clearance and reversing gut microbiota dysbiosis [37] (Figure 1).
In addition, Poriacocos (Schw.) Wolf is the most important herb of Lingui Zhugan decoction (LGZGD) with neuroprotective effects. LGZGD, a notable prescription for the treatment of AD, significantly improved learning and memory ability by regulating Aβ transportation and inhibiting RAGE/MAPK and NF-κB signaling [32].
2.7. Alpinia oxyphylla Miq.
2.7.1. Traditional Functional Features
Alpinia oxyphylla Miq. (AOM), derived from the mature and dried fruits of the Zingiberaceae plant Alpinia oxyphylla Miq., has good effects as a medicine and food in China. AOM is an astringent herb that arrests discharge due to insecure healthy qi and decreases visceral functions, such as excessive sweating, chronic diarrhea, and enuresis [151].
2.7.2. MOAs of the Extract
Recently, a systematic overview of progress on the anti-AD mechanism of AOM was reported. Research has demonstrated that AOF exerts great therapeutic potential in the treatment of AD by inhibiting the formation of Aβ and phosphorylation of tau, increasing antioxidant capacity, anti-inflammatory and anti-apoptosis effects, and inhibiting the activity of acetylcholinesterase [41,152].
Wang et al. found that AOM extracts attenuated LPS-induced learning and memory impairment due to their inhibitory effect on neuroinflammation, amyloid -β (Aβ) deposition, and p-tau [40]. Chang et al. also confirmed in vivo and in vitro that AOM increased the expression of uPA, tPA, MMP-9, and MAPKs and induced ERK1/2, JNK, and p38 phosphorylation to exert nerve regeneration [39]. In addition, a study also showed that treating neurons with AOM extract (80–200 μg/mL) significantly increased cell viability and reduced the number of apoptotic cells, thus exerting neuroprotection [42]. 81Moreover, the butanol extract of AOM (180 mg/kg, 360 mg/kg) was reported to be efficacious in preventing neuronal damage by inhibiting β-secretase and the level of Aβ (1–42) in ICR mice [92] (Figure 1).
2.7.3. MOAs of Ingredients
5-Hydroxymethylfurfural (5-HMF) and tetochrysin (TEC) are the main effective compounds of AOF ethanol extract and exert neuroprotective activities against AD (Figure 2 and Figure 3). For example, both 5-HMF and TEC significantly decreased the content of Aβ 1–42 and increased the activities of antioxidative enzymes, including SOD and GPx [91,153].
2.8. Zingiber officinale Roscoe
2.8.1. Traditional Functional Features
Zingiber officinale Roscoe (ZOR) is the fresh rhizome of Zingiber officinale Roscoe traced from Shen Nong Ben Cao Jing. In the Chinese Pharmacopoeia, ZOR has the function of inducing perspiration and dispelling cold, warming the stomach, stopping vomiting, resolving phlegm, and relieving coughs [154].
2.8.2. MOAs of the Extract
ZOR is a traditional pungent-cool exterior-releasing medicine and is widely used as an antioxidant, anti-inflammatory, antidiabetic, antinausea, neuroprotective, and cardiovascular protective agent [155].
Accumulated investigations have demonstrated that ginger positively affects memory function by anti-inflammatory effects in the treatment of AD. The results from the SD rat model revealed that the operation + high dose (4 g/kg) groups of ginger root extract had lower levels of the nuclear factor-κB (NF-κB) and interleukin-1β (IL-1β) expression than the operation + moderate dose (2 g/kg) and operation + low dose groups (1 g/kg) [43]. Further experiments in the hippocampus of Wistar rats revealed that ZOR extracts at a dose of 200 mg/kg significantly suppressed the inflammatory response of GFAP and IL-1β expression [44].
Mathew M et al. evaluated the antioxidant activity and cholinesterase inhibition properties of a methanolic extract of dry ginger (GE). The extract of total phenolic content and dry material contained 18 ± 0.6 mg/g gallic acid equivalents and 4.18 ± 0.69 mg quercetin equivalents/g, respectively. They found that GE expressed high antioxidant activity with an IC50 value of 70 ± 0.304 microg/mL in the DPPH assay and 845.4 ± 56.62 microM Fe (II) equivalents/g dry weight in the FRAP assay. They also found that GE had IC50 values of 41 ± 1.2 microg/mL and 52 ± 2 microg/mL for the inhibition of acetylcholinesterase and butyrylcholinesterase, respectively, in Ellman’s assay [46]. Another study found that water-extractable red and white ginger inhibited acetylcholinesterase (AChE) activities in a dose-dependent manner, and white ginger had higher acetylcholinesterase inhibitory activity than red ginger. Both extracts significantly decreased the MDA content induced by sodium nitroprusside and quinolinic acid in a dose-dependent manner [45] (Figure 1).
2.8.3. MOAs of Ingredients
6-Gingerol, a phenolic compound, is the major pharmacologically active component in ginger rhizomes with diverse pharmacological activities, such as antitumor, anti-inflammatory, and antioxidant effects, etc. [156]. At present, there have been sufficient in vivo and in vitro experiments to prove that 6-gingerol has potential neuroprotective effects.
An in vitro experiment resulted in 6-gingerol exhibiting neuroprotective effects, and pretreatment with 6-gingerol significantly increased cell viability and reduced cell apoptosis in Aβ1–42-treated PC12 cells. Additionally, 6-gingerol pretreatment markedly reduced the levels of intracellular ROS, MDA, NO, and lactate dehydrogenase (LDH) leakage and increased SOD activity compared with the Aβ1–42 treatment group. Moreover, pretreatment with 6-gingerol (80, 120 μM) also markedly enhanced the protein levels of p-Akt and p-GSK-3β caused by Aβ1–42 [93].
In vivo, in a rat C57BL/6N mouse model induced by a high-fat, high-sugar Western diet (HFSD), 6-shogaol dose-dependently ameliorated obesity and emotional memory deficits [94]. In another study with an ICR mouse model, administration of 6-shogaol at a concentration of 10 mg/kg significantly elevated the expression levels of NGF, PSD-95, and synaptophysin in hippocampal tissues, compared with the vehicle-treated group [95].
2.9. Polygonatumodoratum (Mill.) Druce
2.9.1. Traditional Functional Features
Polygonatumodoratum (Mill.) Druce (PMD), a kind of native citrus germplasm with yin-tonifying medicine that tonifies and nourishes yin fluid, is used to strengthen the body’s resistance to TCM in Southwest China [157].
2.9.2. MOAs of the Extract
PMD extract is rich in flavonoids and phenolics that might ameliorate cognitive dysfunction in β- amyloid-induced rats. Research proved that oral consumption of a flavonoid-rich yuzu extract normalized insulin signaling and improved energy and glucose metabolism in the hippocampus of β-amyloid-infused rats [47].
2.9.3. MOAs of Ingredients
Research indicated that the total phenolic compound content of PMD was 47.8 ± 0.45 mg/100 g, including rutin (4.9 ± 0.7), rutin hydrate (4.2 ± 0.1), narirutin (29.2 ± 3.1), naringin (13.1 ± 1.5), apigen-7-glucoside (17.8 ± 1.5), hesperidin (38.1 ± 2.7), quercetin (1.9 ± 0.2), tangeretin (0.6 ± 0.1), and other ingredients [158,159,160].
Rutin, as a multifunctional biological molecule, can treat and prevent Alzheimer’s disease by regulating various pharmacological mechanisms, such as antioxidant mechanisms, mechanisms related to metal chelation, anti-inflammatory mechanisms, Aβ mechanisms, formation of Aβ, Aβ aggregation and toxicity, and acetyl cholinesterase (AChE) mechanisms [158].
In vitro bioassays have revealed that narirutin is a high-affinity BACE1 inhibitor and extends its applicability as a functional food in AD management [161]. Studies have shown that treatment with naringin (100 mg/kg) enhanced the autophosphorylation of CaMKII and the phosphorylation of the α-amino-3-hydroxy-5-methyl-4-isoxazole propionic (AMPA) receptor in the APPswe/PS1dE9 transgenic mouse model of AD [96].
In addition, hesperidin improved cognitive function and attenuated oxidative stress and apoptosis in an AlCl3-induced rat model [97]. It also showed significantly attenuated β-amyloid deposition and TGF-β immunoreactivity, activated Akt/Nrf2 signaling, and inhibited RAGE/NF-κB signaling in the brains of APP/PS1 mice [98,99,162].
Furthermore, Zaplatic E et al. suggested that quercetin has a potential protective effect against neurodegenerative diseases, including AD. On the one hand, the molecular mechanisms of quercetin in attenuating AD are antioxidant activities, mainly involving the nuclear factor (erythroid-derived 2)-like 2 pathway, paraoxonase-2 pathway, JNK-mediated pathways, PKC pathway, MAPK signaling cascades, and PI3K/Akt pathway. On the other hand, the neuroprotective properties of quercetin were able to inhibit Aβ aggregation, NFT formation, amyloid precursor protein (APP) cleaving enzyme (BACE1), and acetylcholinesterase (AChE) [163].
Moreover, limonene (+) from PMD essential oil has a neuroprotective function against the neurotoxicity of Aβ42 [100].
2.10. Piper nigrum L.
2.10.1. Traditional Functional Features
Piper nigrum L., is widely distributed in tropical regions, and its fruits are used for spices and seasonings as a functional food. P. nigrum, an interior-warming medicine in TCM, can dispel cold from the stomach and eliminate phlegm [164].
2.10.2. MOAs of the Extract
Modern pharmacological research has been founded on broad biological activities, including antioxidant, antimicrobial, and insecticidal activities [165,166]. Mahdy K et al. revealed that the total plant extracts of P. nigrum reduced oxidative stress and ameliorated neurodegeneration characteristics by significantly increasing Ach and serum total antioxidant capacity (TAC) and SOD and significantly decreasing AchE, MDA, and NO in AD-induced rats [48]. The methanolic extract of P. nigrum (50 and 100 mg/kg) restored the activities of SOD and Catalase (CAT) and increased GPX activity in the hippocampus of Aβ (1–42)-treated rats. Simultaneously, as an antioxidant agent, both doses of the methanolic extract (50 and 100 mg/kg) decreased the protein carbonyl and MDA levels and increased GSH in hippocampal homogenates [49].
2.10.3. MOAs of Ingredients
GC-MS and LC-ESI-MS analyses revealed that β-caryophyllene (51.12%) is the dominant component of P. nigrum essential oil (EO) [167].
Liu et al. demonstrated that β-caryophyllene can alleviate the Alzheimer-like phenotype by inhibiting inflammation and reducing the β-amyloid burden. Their research showed that β-caryophyllene prevented cognitive impairment in APP/PS1 mice by reducing the β-amyloid burden in both the hippocampus and the cerebral cortex. In addition, β-caryophyllene reduced the protein levels of COX-2 and the mRNA levels of the proinflammatory cytokines TNF-α and IL-1β in the cerebral cortex. This study also explored the possibility that in an in vivo experiment, β-caryophyllene ameliorates memory impairment through CB2 receptor activation and the PPARγ pathway in APP/PS1 mice for the treatment of AD [106]. It is well known that α -synuclein forms amyloid aggregates in vitro in the presence of some metal ions or alcohol. A large number of experiments show that the mixture of curcumin and β-caryophyllene can not only inhibit the aggregation of α-synuclein, but also almost completely decompose the preformed aggregates at a relatively low concentration [168].
In addition, piperine, an alkaloid present in black pepper (Piper nigrum), has been shown to have anti-inflammatory, antioxidation, cholinergic neuronal transmission, antidepressant, and antipyretic effects [169].
Nazifi M et al. showed that piperine significantly ameliorated cognitive deficits by attenuating oxidative status compared to AD- or AD-Tween-treated groups [108]. Piperine at various doses of 5, 10, and 20 mg/kg significantly improved memory impairment and neurodegeneration in the hippocampus, partly associated with the decrease in lipid peroxidation and the acetylcholinesterase enzyme [109]. In vitro AChE inhibition demonstrated that piperine showed greater AChE inhibition with an IC50 of 76.6 ± 0.08 μg/mL in the SH-SY5Y cell model. Research also found that combined curcumin and piperine inhibited and disaggregated fibril formation and Aβ-induced oxidative damage compared to the Aβ group [107] (Figure 2).
2.11. Ganoderma lucidum (Leyss.ex Fr.) Karst.
2.11.1. Traditional Functional Features
Ganoderma lucidum (Leyss.ex Fr.) Karst. is also known as “the mushroom of immortality”, a basidiomycete white rot microfungus used extensively in China for 2000 years. In fact, during ancient times, G. lucidum was a qi-tonifying medicine that tonifies health for treating qi deficiency [170].
2.11.2. MOAs of the Extract
It should be mentioned that Ganoderma lucidum displays numerous pharmacological effects, mainly including antibacterial, antiaging, antiviral, antiangiogenic, antifibrotic, antioxidative, anti-inflammatory, and analgesic properties [171,172].
Alleviate nerve injury and neurotoxicity: Ganoderma lucidum can improve behavior disorders associated with a decrease in the levels of the Aβ-40 protein and an increase in the levels of ApoA1, ApoE, and Syt1 [173]. Further studies elucidated that the aqueous extract of G. lucidum attenuated the phosphorylation of c-Jun, N-terminal kinase, c-Jun, and p38 MAP kinase, thus blocking Abeta-induced synaptoxicity [174].
Anti-inflammatory effects: Ganoderma lucidum ethanol extract (EGL) in the treatment of neurodegenerative diseases inhibited the NF-κB and TLR signaling pathways, thereby reducing the inflammatory response in activated microglia. And an in vitro study showed that EGL exhibited a potential neuroprotective effect by blocking IκB degradation and inhibiting TLR4 and MyD88 expression, which exerted its anti-inflammatory effects in LPS-stimulated BV2 cells [175].
Antioxidative effects: A study by Lee et al. revealed that EGL augmented the cellular antioxidant defense capacity by increasing the expression and phosphorylation of Nrf2 and HO-1 in a C2C12 myoblast cell line [118] (Figure 1).
2.11.3. MOAs of Ingredients
Mechanistic studies clarified that Ganoderma lucidum polysaccharide promotes cognitive function and neural progenitor proliferation by activating FGFR1 and inhibiting ERK and AKT cascades [176]. Compared to normal mice, Ganoderma lucidum triterpenoids reduced the hippocampus of APP/PS1 mouse brain damage by inhibiting apoptosis (Bax, Bcl2, and caspase 3/cleaved caspase 3), relieving oxidative damage (Nrf2, NQO1, and HO1), and inactivating the increase in ROCK1 and ROCK2 [177]. Lu SY et al. showed that aromatic constituents from Ganoderma lucidum exerted remarkable anti-inflammatory activity with IC50 values ranging from 4.68 to 15.49 μM in RAW264.7 macrophages [176] (Figure 2).
2.12. Puerarialobata (Willd.) Ohwi
2.12.1. Traditional Functional Features
Puerarialobata (Willd.) Ohwi is a pungent-cool exterior-releasing medicine in Shennong Bencao Jing common during the Western Han Dynasty (206 BC–8 AD). In the traditional sense, the main effect of Pueraria is to release flesh, clear heat, engender fluid, and outthrust rashes [178].
2.12.2. MOAs of the Extract
Existing pharmacological experiments show that Puerariae Radix offers neuroprotective effects, cardiovascular protection, and osteonecrosis prevention, etc. [116]. To clarify the mechanism of Puerariae Radix for neuroprotective effects, Huang HJ et al. designed C57BL/6J mice that received a direct infusion of soluble oligomeric A to evaluate the extract of Puerariae Radix alleviation of Aβ deposition in the rat hippocampus. Experimentally, it was observed that Puerariae Radix aqueous extract decreased Aβ deposition, tau protein phosphorylation, inflammation, and loss of noradrenergic and serotonergic neurons, while increasing synaptophysin- and insulin-degrading enzymes against the toxicity of oligomeric Aβ [54].
2.12.3. MOAs of Ingredients
Puerarin, isolated from Puerariae Radix, has the potential to cure angiocardiopathy and cerebrovascular diseases [179]. The effect of puerarin in the prevention of Aβ-induced neurotoxicity through the inhibition of neuronal apoptosis was also examined. Experiments revealed that treatment of PC12 cells with puerarin dose-dependently ameliorated Bax expression and cytochrome c release and increased P-Akt, Bcl-2, and p-Bad expression [117].
Additionally, in an in vivo experiment, puerarin may improve cognitive performance by activating the Akt/GSK-3β signaling pathway associated with a decrease in the levels of GSK-3β and an increase in the levels of Akt in the hippocampus of APP/PS1 mice [179]. Moreover, in vivo evidence indicates that puerarin can serve as a treatment for age-related neurodegenerative disorders by attenuating tau hyperphosphorylation in D-galactose rats [115].
2.13. Ziziphi Spinosae Semen
2.13.1. Traditional Functional Features
Ziziphus jujuba Mill. (SJM) mainly grows in the inland areas of northern China, which has a saying that “thorns are everywhere” in ancient China. SJM, a famous heart-nourishing medicine in China, nourishes the yin blood of the heart to calm the mind in TCM [180].
2.13.2. MOAs of the Extract
SJM is a promising MFH item with various pharmacological actions, including anti-inflammatory, anticomplementary activity, hematopoiesis, antioxidant stress, and anticancer properties [181]. In modern pharmacology research experiments, SJM is widely used to alleviate AD-like symptoms. There is evidence that administering SJM orally to 5XFAD mice ameliorated memory impairments by elevating plasmin levels and activity in hippocampal slices from 5XFAD mice [55]. Other studies have demonstrated that SZS ameliorates Aβ-induced LTP deficits through BDNF/TrkB signaling and stimulates plasmin activity in the hippocampus of CD-1 mice [56]. Recent studies suggest that the flavonoid extract of SJM can reduce Aβ-induced toxicity in Caenorhabditis elegans [57].
2.13.3. MOAs of Ingredients
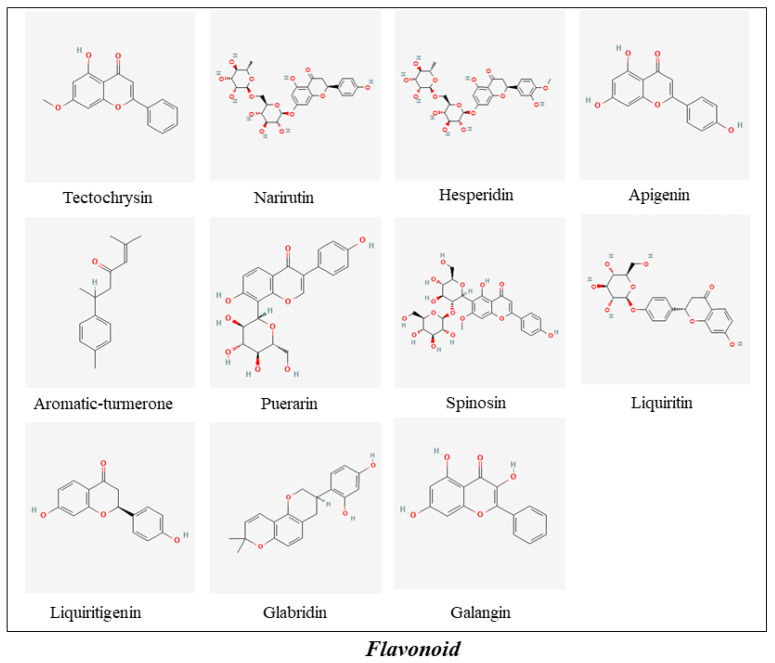
Spinosin is a C-glycoside flavonoid derived from the seeds of SJM that has pharmacological activities, such as anxiolytic and hypnotic effects, and ameliorates memory impairment [182] (Figure 5). Subchronic disease treatment with spinosin (5 mg/kg) activated the ERK-CREB-BDNF signaling pathway to treat cognitive dysfunction in the hippocampus [174]. Another in vitro study using Neuro-2a cells (N2a/WT) and N2a/APP695 cells showed that spinosyn markedly reduced Aβ1–42 production by activating the Nrf2/HO-1 pathway [119]. In addition, spinosin might be beneficial to treat learning and memory deficits through the regulation of oxidative stress, inflammatory processes, apoptotic programs, and plasmin activity [120,121,122].
Figure 5.
The ingredients of Flavonoid in MFH.
2.14. Gastrodia elata Blume
2.14.1. Traditional Functional Features
Gastrodia elata Blume, commonly called Chijian or Ming tian ma in Chinese, is considered a liver-pacifying and wind-extinguishing medicine from the tuber of Gastrodia elata Blume (Orchidaceae) [183].
2.14.2. MOAs of the Extract
Studies in vivo demonstrated that Gastrodia elata significantly reduced the number of amyloid deposits, increased choline acetyltransferase expression, and decreased the activity of acetylcholinesterase [62]. There is further evidence that Gastrodia elata extract (50, 250, and 500 mg/kg) may potentially ameliorate cognitive impairments caused by neuronal cell death in amyloid-β peptide (Aβ)-treated PC12 cells [61].
2.14.3. MOAs of Ingredients
Gastrodin (GAS) is an active constituent extracted from Gastrodia elata (Figure 4). Liu Y and other review articles found that GAS has potential therapeutic effects on a variety of central nervous system diseases, including AD, PD, affective disorders, cerebral ischemia/reperfusion, and epilepsy. Its extensive pharmacological activities and principal mechanisms include regulating mitochondrial cascades, antioxidant and anti-inflammatory functions, modulating neurotransmitters, suppressing microglial activation, and upregulating neurotrophins [184].
A molecular analysis showed that GAS could effectively treat BCCAO-induced vascular dementia (BCK) by targeting the formation of Aβ-related proteins (Aβ1–40/42, APP, and β-site APP-cleaving enzyme 1) and inhibiting autophagy (Beclin-1, LC3-II, and p62) and apoptosis (Bax/Bcl-2 and P38 MAPK) in hippocampal neurons [127]. More importantly, GAS promoted Sirt3 upregulation and NOX-2 downregulation, acting on activated microglia in neuroprotection [185].
2.15. Lycium barbarum L.
2.15.1. Traditional Functional Features
Lycium barbarum L. (a “berry-type” fruit of the plant Lycium barbarum), a yin-tonifying medicine belonging to the Solanaceae family, is recorded in Shennong Ben Cao Jing (ca 100 AD) [186].
2.15.2. MOAs of the Extract
In recent years, Fructus lycii and its phytochemical components have been increasingly reported as promising anti-AD drugs with key pathological events, such as oxidative stress, anti-immune, antiapoptosis, and antinecrosis effects [187].
Extracts from Fructus lycii mitigated neuronal loss and behavioral impairments against the toxicity of fibrillar Abeta (1–42) and Abeta (25–35) fragments. An in vitro study revealed that extracts of Fructus lycii (100 μg/mL) ameliorated caspase-3 activity up to 11.8% compared with the Aβ peptide-treated group. In addition, pretreatment with extract isolated from Fructus lycii at 100 μg/mL markedly downregulated the protein levels of JNK, c-Jun, and β-actin, while the protein levels of total JNK, total c-Jun, and β-actin were unchanged after treatment with LBA [63] (Figure 1).
2.15.3. MOAs of Ingredients
Gao Y et al. showed that there are many antiaging active ingredients in Fructus lycii, such as Fructus lycii polysaccharides, β-sitosterol, caffeic acid, and zeaxanthin [188]. Studies have shown that the ability of organisms to respond to oxidative stress is intricately related to their aging and longevity [189]. Fructus lycii polysaccharides are a good antioxidant [190]. A systematic review and meta-analysis indicated that dietary zeaxanthin may be protective against age-related macular degeneration [191]. Habtemariam S. et al.’s mini review revealed that the antiAD therapeutic potential of caffeic acid is associated with antioxidant effects, specific anti-inflammatory mechanisms in the brain, and the various processes of β-amyloid formation [192].
2.16. Alpinia officinarum Hance/Mosla chinensis Maxim
2.16.1. Traditional Functional Features
Alpinia officinarum Hance (AOH), an interior-warming medicine native to China that can warm the stomach and relieve vomiting, dispel cold, and relieve pain is also known as lesser galangal. AOH, which belongs to the Zingiberaceae family, is indigenous to Southeast China (Guangdong, Guangxi, Hainan) [193].
Mosla chinensis Maxim. (MCM), a pungent-warm exterior-releasing medicine, can promote diaphoresis and release to the exterior and resolve dampness, thus harmonizing the spleen and stomach and promoting water metabolism [21].
2.16.2. MOAs of Ingredients
AOH is a dietary product with medicinal applications and also possesses a wide range of pharmacological effects, including angiogenesis, antimicrobial, anticancer, anti-inflammatory, vasorelaxation, and antioxidant activities [194]. Diarylheptanoids are considered as principal phytochemical constituents from the rhizome of A. officinarum, including apigenin and galangin [192]. Apigenin, a pharmacologically active agent, is also widely distributed in herbs (Elsholtzia rugulosa) [195].
Previous studies have proven that apigenin resists Aβ-induced toxicity, has anti-inflammatory and antioxidant effects, alleviates learning and memory deficits, and depresses neuronal apoptosis [196,197].
Inhibiting the apoptosis of neurons: Studies have shown that apigenin protects neuronal cells from injury by suppressing the phosphorylation of inducible nitric oxide synthase, cyclooxygenase-2 protein, p38 mitogen-activated protein kinase (MAPK), and c-Jun N-terminal kinase (JNK) in primary microglial cells [103]. Another study showed that apigenin could exert neuroprotection against Aβ-induced toxicity in the presence of copper mainly through inhibiting the p38 MAPK signaling pathway and SAPK/JNK pathway and depressing neuronal apoptosis in vitro [101].
Neuro-immunomodulatory: Dourado NS et al. evaluated the neuroimmunomodulatory and neuroprotective effects of apigenin on glial cells and neurons of Wistar rats. Treatment with apigenin preserves neuron and astrocyte morphology by reducing the expression of OX42, IL-6, and gp130. In addition, apigenin alone and after an inflammatory stimulus with IL-1β also increased the expression of BDNF to exert anti-inflammatory and neuroprotective effects [104]. In addition, apigenin also downregulated BACE1 and β-CTF levels, affecting APP processing and preventing the Aβ burden. Moreover, apigenin restored the neurotrophic ERK/CREB/BDNF pathway in the cerebral cortex for the prevention and/or therapy of AD [102].
Improving cholinergic neuronal transmission: Acetylcholinesterase (AChE) inhibitors are an important class of drugs for the treatment of AD, such as rivastigmine, galantamine, and huperzine. Galangin is a major flavonoid found in Rhizoma Alpiniae Officinarum with the strongest inhibitory effect on AChE activity (56.53 ± 0.03) [105] (Figure 5).
2.17. Curcuma longa L.
2.17.1. Traditional Functional Features
Curcuma longa L., a blood-activating analgesic medicine extensively cultivated in India and China, has been widely used as a spice in foods. It can eliminate blood stasis, promote the flow of qi, stimulate menstrual discharge, and relieve pain [198].
2.17.2. MOAs of Ingredients
Curcuma longa L. inhibits anti-inflammatory, antihuman immunodeficiency virus, antibacterial, and antioxidant effects [199,200].
Curcumin (Cur), a potent antiamyloid natural polyphenol, is derived from the root of RCL (Figure 3). Studies have shown that Cur can effectively modify AD pathology by preventing the formation and accumulation of Aβ, tau inhibition, copper-binding and cholesterol-lowering abilities, anti-inflammatory activity and modulation of microglia, acetylcholinesterase inhibition, regulation of the insulin signaling pathway, and antioxidant activity [201,202]. For example, Cur directly bound to PPARγ increased the transcriptional activity and protein levels of PPARγ and inhibited the nuclear factor kappa B (NF-κB) signaling pathway, indicating that the beneficial effects of Cur on AD are attributable to the suppression of neuroinflammation in APP/PS1 mice [110].
Da Costa et al., in a systematic review, indicated that Cur supplementation, a promising approach in AD, reversed neurotoxic and behavioral damage in both in vivo (Sprague–Dawley rats, APPswe/PS1dE9 and 5xFAD transgenic mice) and in vitro (PC12 cells, SK-N-SH cells, and neonate rat cells) models of AD [203]. For instance, Cur (50 mg/kg) also provided antiamyloid and neuroprotective outcomes in 5xFAD mice [111].
Aromatic-turmerone is an analog of curcumin and is rich in Curcuma longa. Accumulating evidence has demonstrated that aromatic-turmerone impairs the Aβ-induced inflammatory response of microglial cells by inhibiting the NF-κB, JNK, and p38 MAPK signaling pathways in hippocampal HT-22 cells [112]. Moreover, aromatic-turmerone significantly limited brain damage by inhibiting TLR4 and lowered the release of inflammatory mediators [113]. Further evidence was provided that aromatic- turmerone prevented cleaved caspase-3, while neither the level of ROS nor the mitochondrial membrane potential was affected in cerebellar granule neurons [114].
3. Other MFH with Potential AntiAD Activity
In addition to the abovementioned more comprehensive and systematic preclinical and clinical studies on MFH, there are other studies that show positive effects on AD. Among them, some MFH substancess, such as Alpinia officinarum Hance [103], Mosla chinensis Maxim. [101,104], Curcuma longa L. [110,111], Glycyrrhiza uralensis Fisch. [123,124,125], Raphanus sativus L. [126], and Cornus officinalis Siebold & Zucc. [128], focus only on the pharmacological effects of their active ingredients against AD, as shown in Table 4. However, other MFH items have only conducted in vivo/in vitro pharmacological experimental studies on their crude extracts against AD, including Morus alba L. [50,51,52,53], Cinnamomum cassia (L.) J. Presl [58,59,60], Houttuynia cordata thunb. [64], Cassia obtusifolia L. [65,66],, Ziziphus jujuba Mill. [67,68,69], Dendrobium nobile Lindl. [70,71,72], and Piper longum L. [73,74] (Figure 1 and Figure 2). It is worth developing a better experimental design and conducting clinical research in the future.
4. Discussion and Conclusions
Historically, Chinese ancestors developed many kinds of TCM through long-term practice and summarized their application in treating disease [204]. They also realized that many of these TCMs could be eaten as functional foods (TCM nutrition) in their daily lives, which reflects the theory of MFH [8,13,205].
Since the 20th century, chronic diseases have become the main cause of global morbidity and mortality. A very important reason for this is the imbalance of nutrition and suboptimal lifestyle behaviors, leading to such diseases as AD [206,207]. In recent years, limited by the complexity of AD pathology, new drugs targeting amyloid-β peptide (Aβ) or tau proteins have failed to show significant clinical benefits, such as ClinicalTrials.gov identifier: CAD106 (NCT01097096), ACC-001 (NCT01284387), and AFFITOPE AD02 (NCT01117818 CAD106) [208,209]. Consequently, the development of new drugs and new treatment methods have encountered considerable obstacles and bottlenecks. Interestingly, some TCMs are used as functional foods with brain targets, nutritional benefits, and long-term applications, adjusting diet nutrition to prevent the occurrence of AD, such as Salvia miltiorrhiza Bunge, Cinnamomum cassia (L.) J.Presl, Zingiber officinale Roscoe, and Panax ginseng C.A. Mey. [210,211] (Figure 1 and Figure 2). Taking MFH substances as the primary functional foods can ensure the safety and therapeutic effect of functional food. At the same time, good social and economic benefits can also be obtained by using the cost and technical advantages of TCM, coupled with the progress of the modern food industry [212]. Therefore, MFH foods are used as a dietary intervention to provide higher specialist guidance for AD.
However, although pharmacological research and clinical research have been devoted to proving the safety and effectiveness of MFH items in treating AD, the MOAs of MFH and their active components against AD are still unclear [211,213]. Fortunately, TCM transcriptomics, metabonomics, and protein omics, as well as TCM systematic pharmacology, are in full swing. Future research can combine multiomics and systems pharmacology to explore the pharmacokinetics of the multiple ingredients in these MFH substances [214,215]. In addition, most studies on the mechanism and efficacy of MFH are still at the animal and cellular levels; therefore, clinical research is scarce. Future clinical research should be performed to discover novel antiAD agents of MFH foods. Moreover, given the diversity of AD pathology, MFH antiAD research should also focus on its multicomponent and multitarget mechanisms in a holistic way.
MFH originated in China, but is now favored by people worldwide in the daily diet to prevent the occurrence and development of AD. The rapid development of modern science and technology should provide an advanced theory and a wider field of vision for explaining the advantages of traditional MFH theory in AD. Particularly in recent years, overcoming chronic diseases requires more basic and clinical research to develop new drugs. As a renewable and promising resource, MFH should be a resource to take ongoing effective measures to develop and produce new antiAD drugs or health care products.
Author Contributions
P.G. designed and implemented the research, carried out the analysis, and wrote the original draft; B.Z., J.Z., C.W. and Z.W. conducted check and calibration; A.L. and G.D. conceived the research idea, supervised the project, and revised the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the Drug Innovation Major Project, grants numbers 2018ZX09711001-003-002; 2018ZX09711001-012; by CAMS Initiative for Innovative Medicine, grants numbers CAMS-IZM; 2016-IZM-3-007, and by the Beijing National Science Foundation, grants numbers 7192134.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Soria Lopez J.A., González H.M., Léger G.C. Alzheimer’s disease. Handb. Clin. Neurol. 2019;167:231–255. doi: 10.1016/B978-0-12-804766-8.00013-3. [DOI] [PubMed] [Google Scholar]
- 2.Ferrari C., Sorbi S. The complexity of Alzheimer’s disease: An evolving puzzle. Physiol. Rev. 2021;101:1047–1081. doi: 10.1152/physrev.00015.2020. [DOI] [PubMed] [Google Scholar]
- 3.Prince M., Bryce R., Albanese E., Wimo A., Ribeiro W., Ferri C.P. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimer’s Dement. 2013;9:63–75. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 4.DeTure M.A., Dickson D.W. The neuropathological diagnosis of Alzheimer’s disease. Mol. Neurodegener. 2019;14:32. doi: 10.1186/s13024-019-0333-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lashley T., Schott J.M., Weston P., Murray C.E., Wellington H., Keshavan A., Zetterberg H. Molecular biomarkers of Alzheimer’s disease: Progress and prospects. Dis. Model Mech. 2018;8:11. doi: 10.1242/dmm.031781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oboudiyat C., Glazer H., Seifan A., Greer C., Isaacson R.S. Alzheimer’s disease. Semin. Neurol. 2013;33:313–329. doi: 10.1055/s-0033-1359319. [DOI] [PubMed] [Google Scholar]
- 7.Chu L.W. Alzheimer’s disease: Early diagnosis and treatment. Hong Kong Med. J. 2012;18:228–237. [PubMed] [Google Scholar]
- 8.Hou Y., Jiang J.-G. Origin and concept of medicine food homology and its application in modern functional foods. Food Funct. 2013;4:1727–1741. doi: 10.1039/c3fo60295h. [DOI] [PubMed] [Google Scholar]
- 9.Owen L., Corfe B. The role of diet and nutrition on mental health and wellbeing. Proc. Nutr. Soc. 2017;76:425–426. doi: 10.1017/S0029665117001057. [DOI] [PubMed] [Google Scholar]
- 10.Popa S.L., Pop C., Dumitrascu D.L. Diet Advice for Crohn’s Disease: FODMAP and Beyond. Nutrients. 2020;12:3751. doi: 10.3390/nu12123751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang X., Wang X., Xue Z., Zhan G., Ito Y., Guo Z. Prevention properties on cerebral ischemia reperfusion of medicine food homologous Dioscorea yam-derived diosgenin based on mediation of potential targets. Food Chem. 2021;345:128672. doi: 10.1016/j.foodchem.2020.128672. [DOI] [PubMed] [Google Scholar]
- 12.Gong X., Ji M., Xu J., Zhang C., Li M. Hypoglycemic effects of bioactive ingredients from medicine food homology and medicinal health food species used in China. Crit. Rev. Food Sci. Nutr. 2019;60:2303–2326. doi: 10.1080/10408398.2019.1634517. [DOI] [PubMed] [Google Scholar]
- 13.Song D.X., Jiang J.G. Hypolipidemic Components from Medicine Food Homology Species Used in China: Pharmacological and Health Effects. Arch. Med. Res. 2017;48:569–581. doi: 10.1016/j.arcmed.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Lee S.-T., Chu K., Sim J.-Y., Heo J.-H., Kim M. Panax Ginseng Enhances Cognitive Performance in Alzheimer Disease. Alzheimer Dis. Assoc. Disord. 2008;22:222–226. doi: 10.1097/WAD.0b013e31816c92e6. [DOI] [PubMed] [Google Scholar]
- 15.Heo J.H., Lee S.T., Chu K., Oh M.J., Park H.J., Shim J.Y., Kim M. An open-label trial of Korean red ginseng as an adjuvant treatment for cognitive impairment in patients with Alzheimer’s disease. Eur. J. Neurol. 2008;15:865–868. doi: 10.1111/j.1468-1331.2008.02157.x. [DOI] [PubMed] [Google Scholar]
- 16.Heo J.H., Lee S.T., Oh M.J., Park H.J., Shim J.Y., Chu K., Kim M. Improvement of cognitive deficit in Alzheimer’s disease patients by long term treatment with Korean red ginseng. J. Ginseng. Res. 2011;35:457–461. doi: 10.5142/jgr.2011.35.4.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akhondzadeh S., Shafiee Sabet M., Harirchian M.H., Togha M., Cheraghmakani H., Razeghi S., Vossoughi A. A 22-week, multicenter, randomized, double-blind controlled trial of Crocus sativus in the treatment of mild-to-moderate Alzheimer’s disease. Psychopharmacology. 2010;207:637–643. doi: 10.1007/s00213-009-1706-1. [DOI] [PubMed] [Google Scholar]
- 18.Akhondzadeh S., Sabet M.S., Harirchian M.H., Togha M., Cheraghmakani H., Razeghi S., Moradi A. Saffron in the treatment of patients with mild to moderate Alzheimer’s disease: A 16-week, randomized and placebo-controlled trial. J. Clin. Pharm. 2010;35:581–588. doi: 10.1111/j.1365-2710.2009.01133.x. [DOI] [PubMed] [Google Scholar]
- 19.Tsolaki M., Karathanasi E., Lazarou I., Dovas K., Verykouki E., Karakostas A., Georgiadis K., Tsolaki A., Adam K., Kompatsiaris I., et al. Efficacy and Safety of Crocus sativus L. in Patients with Mild Cognitive Impairment: One Year Single-Blind Randomized, with Parallel Groups, Clinical Trial. J. Alzheimer’s Dis. 2016;54:129–133. doi: 10.3233/JAD-160304. [DOI] [PubMed] [Google Scholar]
- 20.Li N., Wang J., Ma J., Gu Z., Jiang C., Yu L., Fu X. Neuroprotective Effects of Cistanches Herba Therapy on Patients with Moderate Alzheimer’s Disease. Evid. Based Complement. Altern. Med. 2015;2015:103985. doi: 10.1155/2015/103985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fang S., Dong L., Liu L., Guo J., Zhao L., Zhang J., Zhao Y. HERB: A high-throughput experiment-and refer-ence-guided database of traditional Chinese medicine. Nucleic Acids Res. 2021;49:D1197–D1206. doi: 10.1093/nar/gkaa1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun C., Liu J., Li N., Liu M., Luo Z., Li H. Traditional Chinese Medicine Shenmayizhi Decoction Ameliorates Memory and Cognitive Impairment Induced by Multiple Cerebral Infarctions. Evid. Based Complement. Altern. Med. 2021;2021:6648455. doi: 10.1155/2021/6648455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma L., Cao Y., Wang F., Li Z., Wang Z., Yang Y., Pei H., Li H. Yizhi Qingxin Formula Extract Ameliorates Cognitive Decline in Aged Rats via the Brain-Derived Neurotrophic Factor/Tropomyosin Receptor Kinase B Pathway. Front. Pharmacol. 2020;11:510. doi: 10.3389/fphar.2020.00510. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Yang Y., Wang Z., Cao Y., Liu J., Li P., Li H., Liu M. Yizhiqingxin Formula Alleviates Cognitive Deficits and Enhances Autophagy via mTOR Signaling Pathway Modulation in Early Onset Alzheimer’s Disease Mice. Front. Pharmacol. 2019;10:1041. doi: 10.3389/fphar.2019.01041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seo J.S., Yun J.H., Baek I.S., Leem Y.H., Kang H.W., Cho H.K., Han P.L. Oriental medicine Jangwonhwan reduces Abeta(1–42) level and beta-amyloid deposition in the brain of Tg-APPswe/PS1dE9 mouse model of Alzheimer disease. J. Ethnopharmacol. 2010;128:206–212. doi: 10.1016/j.jep.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 26.Gong G., Qi B., Liang Y.T., Dong T.T.X., Wang H.Y., Tsim K.W.K., Zheng Y. Danggui Buxue Tang, an ancient Chinese herbal decoction, protects β-amyloid-induced cell death in cultured cortical neurons. BMC Complement. Altern. Med. 2019;19:9. doi: 10.1186/s12906-018-2411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang Y., Hu Z.-Y., Yuan H., Shu L., Liu G., Qiao S.-Y., Sun L., Zhou W.-X., Zhang Y.-X. Danggui-Shaoyao-San Improves Learning and Memory in Female SAMP8 via Modulation of Estradiol. Evid. Based Complement. Altern. Med. 2014;2014:327294. doi: 10.1155/2014/327294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang J., Wang X., Xie L., Wu M., Zhao W., Zhang Y., Wang Q., Yao L., Li W. Extract of Danggui-Shaoyao-San ameliorates cognition deficits by regulating DHA metabolism in APP/PS1 mice. J. Ethnopharmacol. 2020;253:112673. doi: 10.1016/j.jep.2020.112673. [DOI] [PubMed] [Google Scholar]
- 29.Lu J., Guo P., Liu X., Zhang Y., Guo X., Gao X., Chen Y. Herbal Formula Fo Shou San Attenuates Alzheimer’s Dis-ease-Related Pathologies via the Gut-Liver-Brain Axis in APP/PS1 Mouse Model of Alzheimer’s Disease. Evid. Based Complement. Altern. Med. 2019;2019:8302950. doi: 10.1155/2019/8302950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu Y.R., Xing S.L., Chen C., Shen D.Z., Chen J.L. Tiaoxin Recipe, a Chinese herbal formula, inhibits microRNA-34a expression in the APPswe/PS1ΔE9 mouse model of Alzheimer’s disease. J. Integr. Med. 2019;17:404–409. doi: 10.1016/j.joim.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Wang F., Feng J., Yang Y., Liu J., Liu M., Wang Z., Pei H., Wei Y., Li H. The Chinese herbal formula Fuzheng Quxie Decoction attenuates cognitive impairment and protects cerebrovascular function in SAMP8 mice. Neuropsychiatr. Dis. Treat. 2018;14:3037–3051. doi: 10.2147/NDT.S175484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu Q., Yu B., Chen Q., Wang Y., Ling Y., Sun S., Zhou C. Effect of Linguizhugan decoction on neuroinflammation and expression disorder of the amyloid β-related transporters RAGE and LRP-1 in a rat model of Alzheimer’s disease. Mol. Med. Rep. 2018;17:827–834. doi: 10.3892/mmr.2017.7983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shin S.J., Jeon S.G., Kim J.I., Jeong Y.O., Kim S., Park Y.H., Moon M. Red Ginseng Attenuates Aβ-Induced Mitochondrial Dysfunction and Aβ-mediated Pathology in an Animal Model of Alzheimer’s Disease. Int. J. Mol. Sci. 2019;20:3030. doi: 10.3390/ijms20123030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim J., Kim S.H., Lee D.S., Lee D.J., Kim S.H., Chung S., Yang H.O. Effects of fermented ginseng on memory impairment and β-amyloid reduction in Alzheimer’s disease experimental models. J. Ginseng. Res. 2013;37:100–107. doi: 10.5142/jgr.2013.37.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Choi J.G., Kim N., Huh E., Lee H., Oh M.H., Park J.D., Pyo M.K., Oh M.S. White Ginseng Protects Mouse Hippocampal Cells Against Amyloid-Beta Oligomer Toxicity. Phytother. Res. 2017;31:497–506. doi: 10.1002/ptr.5776. [DOI] [PubMed] [Google Scholar]
- 36.Soeda S., Ochiai T., Paopong L., Tanaka H., Shoyama Y., Shimeno H. Crocin suppresses tumor necrosis fac-tor-alpha-induced cell death of neuronally differentiated PC-12 cells. Life Sci. 2001;69:2887–2898. doi: 10.1016/S0024-3205(01)01357-1. [DOI] [PubMed] [Google Scholar]
- 37.Sun Y., Liu Z., Pi Z., Song F., Wu J., Liu S. Poria cocos could ameliorate cognitive dysfunction in APP / PS1 mice by restoring imbalance of Aβ production and clearance and gut microbiota dysbiosis. Phytother. Res. 2021;35:2678–2690. doi: 10.1002/ptr.7014. [DOI] [PubMed] [Google Scholar]
- 38.Huang Y.-J., Hsu N.-Y., Lu K.-H., Lin Y.-E., Lin S.-H., Lu Y.-S., Liu W.-T., Chen M.-H., Sheen L.-Y. Poria cocos water extract ameliorates the behavioral deficits induced by unpredictable chronic mild stress in rats by down-regulating inflammation. J. Ethnopharmacol. 2020;258:112566. doi: 10.1016/j.jep.2020.112566. [DOI] [PubMed] [Google Scholar]
- 39.Chang Y.M., Ye C.X., Ho T.J., Tsai T.N., Chiu P.L., Tsai C.C., Huang C.Y. Alpinia oxyphylla Miquel fruit extract activates MAPK-mediated signaling of PAs and MMP2/9 to induce Schwann cell migration and nerve regeneration. Int. J. Artif. Organs. 2014;37:402–413. doi: 10.5301/ijao.5000313. [DOI] [PubMed] [Google Scholar]
- 40.Wang Y., Wang M., Fan K., Li T., Yan T., Wu B., Jia Y. Protective effects of Alpinia oxyphylla Fructus extracts on lipopolysaccharide-induced animal model of Alzheimer’s disease. J. Ethnopharmacol. 2018;217:98–106. doi: 10.1016/j.jep.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 41.Yu S.H., Kim H.J., Jeon S.Y., Kim M.R., Lee B.S., Lee J.J., Kim D.S., Lee Y.C. Anti-inflammatory and anti-nociceptive activities of Alpinia oxyphylla Miquel extracts in animal models. J Ethnopharmacol. 2020;260:112985. doi: 10.1016/j.jep.2020.112985. [DOI] [PubMed] [Google Scholar]
- 42.Yu X., An L., Wang Y., Zhao H., Gao C. Neuroprotective effect of Alpinia oxyphylla Miq. fruits against gluta-mate-induced apoptosis in cortical neurons. Toxicol. Lett. 2003;144:205–212. doi: 10.1016/S0378-4274(03)00219-4. [DOI] [PubMed] [Google Scholar]
- 43.Zeng G.-F., Zhang Z.-Y., Lu L., Xiao D.-Q., Zong S.-H., He J.-M. Protective Effects of Ginger Root Extract on Alzheimer Disease-Induced Behavioral Dysfunction in Rats. Rejuvenation Res. 2013;16:124–133. doi: 10.1089/rej.2012.1389. [DOI] [PubMed] [Google Scholar]
- 44.Kongsui R., Sriraksa N., Thongrong S. The Neuroprotective Effect of Zingiber cassumunar Roxb. Extract on LPS-Induced Neuronal Cell Loss and Astroglial Activation within the Hippocampus. BioMed Res. Int. 2020;2020:4259316. doi: 10.1155/2020/4259316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oboh G., Ademiluyi A.O., Akinyemi A. Inhibition of acetylcholinesterase activities and some pro-oxidant induced lipid peroxidation in rat brain by two varieties of ginger (Zingiber officinale) Exp. Toxicol. Pathol. 2012;64:315–319. doi: 10.1016/j.etp.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 46.Mathew M., Subramanian S. In vitro evaluation of anti-Alzheimer effects of dry ginger (Zingiber officinale Roscoe) extract. Indian J. Exp. Boil. 2014;52:606–612. [PubMed] [Google Scholar]
- 47.Yang H.J., Hwang J.T., Kwon D.Y., Kim M.J., Kang S., Moon N.R., Park S. Yuzu Extract Prevents Cognitive Decline and Impaired Glucose Homeostasis in β-Amyloid–Infused Rats. J. Nutr. 2013;143:1093–1099. doi: 10.3945/jn.112.173401. [DOI] [PubMed] [Google Scholar]
- 48.Mahdy K., Shaker O., Wafay H., Nassar Y., Hassan H., Hussein A. Effect of some medicinal plant extracts on the oxidative stress status in Alzheimer’s disease induced in rats. Eur. Rev. Med. Pharm. Sci. 2012;16:31–42. [PubMed] [Google Scholar]
- 49.Hritcu L., Noumedem A.J., Cioanca O., Hancianu M., Postu P., Mihasan M. Anxiolytic and antidepressant profile of the methanolic extract of Piper nigrum fruits in beta-amyloid (1–42) rat model of Alzheimer’s disease. Behav. Brain Funct. 2015;11:1–13. doi: 10.1186/s12993-015-0059-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim H.G., Park G., Lim S., Park H., Choi J.G., Jeong H.U., Kang M.S., Lee M.K., Oh M.S. Mori Fructus improves cognitive and neuronal dysfunction induced by beta-amyloid toxicity through the GSK-3β pathway in vitro and in vivo. J. Ethnopharmacol. 2015;171:196–204. doi: 10.1016/j.jep.2015.05.054. [DOI] [PubMed] [Google Scholar]
- 51.Kaewkaen P., Tong-Un T., Wattanathorn J., Muchimapura S., Kaewrueng W., Wongcharoenwanakit S. Mulberry Fruit Extract Protects against Memory Impairment and Hippocampal Damage in Animal Model of Vascular Dementia. Evid. Based Complement. Altern. Med. 2012;2012:263520. doi: 10.1155/2012/263520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shih P.H., Chan Y.C., Liao J.W., Wang M.F., Yen G.C. Antioxidant and cognitive promotion effects of anthocyanin-rich mulberry (Morus atropurpurea L.) on senescence-accelerated mice and prevention of Alzheimer’s disease. J. Nutr. Biochem. 2010;21:598–605. doi: 10.1016/j.jnutbio.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 53.Song N., Yang H., Pang W., Qie Z., Lu H., Tan L., Li H., Sun S., Lian F., Qin C., et al. Mulberry extracts alleviate aβ 25-35-induced injury and change the gene expression profile in PC12 cells. Evid. Based Complement. Altern. Med. 2014;2014:150617. doi: 10.1155/2014/150617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huang H.-J., Huang C.-Y., Lee M., Lin J.-Y., Hsieh-Li H.M. Puerariae Radix Prevents Anxiety and Cognitive Deficits in Mice Under Oligomeric Aβ-Induced Stress. Am. J. Chin. Med. 2019;47:1459–1481. doi: 10.1142/S0192415X19500757. [DOI] [PubMed] [Google Scholar]
- 55.Park H.J., Jung I.H., Kwon H., Yu J., Jo E., Kim H., Ryu J.H. The ethanol extract of Zizyphus jujuba var. spinosa seeds ameliorates the memory deficits in Alzheimer’s disease model mice. J. Ethnopharmacol. 2019;233:73–79. doi: 10.1016/j.jep.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 56.Kwon H., Jung I.H., Yi J.H., Kim J.H., Park J.H., Lee S., Kim D.H. The Seed of Zizyphus jujuba var. spinosa Attenuates Alzheimer’s Disease-Associated Hippocampal Synaptic Deficits through BDNF/TrkB Signaling. Biol. Pharm. Bull. 2017;40:2096–2104. doi: 10.1248/bpb.b17-00378. [DOI] [PubMed] [Google Scholar]
- 57.Yang T., Fang L., Lin T., Li J., Zhang Y., Zhou A., Xie J. Ultrasonicated sour Jujube seed flavonoids extract exerts ameliorative antioxidant capacity and reduces Aβ-induced toxicity in Caenorhabditis elegans. J. Ethnopharmacol. 2019;239:111886. doi: 10.1016/j.jep.2019.111886. [DOI] [PubMed] [Google Scholar]
- 58.Frydman-Marom A., Levin A., Farfara D., Benromano T., Scherzer-Attali R., Peled S., Vassar R., Segal D., Gazit E., Frenkel D., et al. Orally administrated cinnamon extract reduces β-amyloid oligomerization and corrects cognitive impairment in Alzheimer’s disease animal models. PLoS ONE. 2011;6:e16564. doi: 10.1371/journal.pone.0016564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Modi K.K., Roy A., Brahmachari S., Rangasamy S.B., Pahan K. Cinnamon and Its Metabolite Sodium Benzoate Attenuate the Activation of p21rac and Protect Memory and Learning in an Animal Model of Alzheimer’s Disease. PLoS ONE. 2015;10:e0130398. doi: 10.1371/journal.pone.0130398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Madhavadas S., Subramanian S. Cognition enhancing effect of the aqueous extract of Cinnamomum zeylanicum on non-transgenic Alzheimer’s disease rat model: Biochemical, histological, and behavioural studies. Nutr. Neurosci. 2017;20:526–537. doi: 10.1080/1028415X.2016.1194593. [DOI] [PubMed] [Google Scholar]
- 61.Park Y.M., Lee B.G., Park S.H., Oh H.G., Kang Y.G., Kim O.J., Lee H.Y. Prolonged oral administration of Gastrodia elata extract improves spatial learning and memory of scopolamine-treated rats. Lab. Anim. Res. 2015;31:69–77. doi: 10.5625/lar.2015.31.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang G.B., Zhao T., Muna S.S., Jin H.M., Park J.I., Jo K.S., Chung Y.C. Therapeutic potential of Gastrodia elata Blume for the treatment of Alzheimer’s disease. Neural Regen. Res. 2013;8:1061–1070. doi: 10.3969/j.issn.1673-5374.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yu M.S., Leung S.K., Lai S.W., Che C.M., Zee S.Y., So K.F., Chang R.C. Neuroprotective effects of anti-aging oriental medicine Lycium barbarum against beta-amyloid peptide neurotoxicity. Exp. Gerontol. 2005;40:716–727. doi: 10.1016/j.exger.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 64.Huh E., Kim H.G., Park H., Kang M.S., Lee B., Oh M.S. Houttuynia cordata Improves Cognitive Deficits in Cholinergic Dysfunction Alzheimer’s Disease-Like Models. Biomol. Ther. 2014;22:176–183. doi: 10.4062/biomolther.2014.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim D.H., Yoon B.H., Kim Y.W., Lee S., Shin B.Y., Jung J.W., Kim H.J., Lee Y.S., Choi J.S., Kim S.Y., et al. The seed extract of Cassia obtusifolia ameliorates learning and memory impairments induced by scopolamine or transient cerebral hypoperfusion in mice. J. Pharmacol. Sci. 2007;105:82–93. doi: 10.1254/jphs.FP0061565. [DOI] [PubMed] [Google Scholar]
- 66.Yi J.H., Park H.J., Lee S., Jung J.W., Kim B.C., Lee Y.C., Ryu J.H., Kim D.H. Cassia obtusifolia seed ameliorates amyloid β-induced synaptic dysfunction through anti-inflammatory and Akt/GSK-3β pathways. J. Ethnopharmacol. 2016;178:50–57. doi: 10.1016/j.jep.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 67.Chen J., Maiwulanjiang M., Lam K.Y., Zhang W.L., Zhan J.Y., Lam C.T., Xu S.L., Zhu K.Y., Yao P., Lau D.T., et al. A standardized extract of the fruit of Ziziphus jujuba (Jujube) induces neuronal differentiation of cultured PC12 cells: A signaling mediated by protein kinase A. J. Agric. Food Chem. 2014;62:1890–1897. doi: 10.1021/jf405093f. [DOI] [PubMed] [Google Scholar]
- 68.Chen J., Yan A.L., Lam K.Y., Lam C.T., Li N., Yao P., Xiong A., Dong T.T., Tsim K.W. A chemically standardized extract of Ziziphus jujuba fruit (Jujube) stimulates expressions of neurotrophic factors and anti-oxidant enzymes in cultured astrocytes. Phytother. Res. 2014;28:1727–1730. doi: 10.1002/ptr.5202. [DOI] [PubMed] [Google Scholar]
- 69.Chen J., Du C.Y., Lam K.Y., Zhang W.L., Lam C.T., Yan A.L., Yao P., Lau D.T., Dong T.T., Tsim K.W. The standardized extract of Ziziphus jujuba fruit (jujube) regulates pro-inflammatory cytokine expression in cultured murine macrophages: Suppression of lipopolysaccharide-stimulated NF-κB activity. Phytother. Res. 2014;28:1527–1532. doi: 10.1002/ptr.5160. [DOI] [PubMed] [Google Scholar]
- 70.Nie J., Tian Y., Zhang Y., Lu Y.L., Li L.S., Shi J.S. Dendrobium alkaloids prevent Aβ(25-35)-induced neuronal and synaptic loss via promoting neurotrophic factors expression in mice. PeerJ. 2016;4:e2739. doi: 10.7717/peerj.2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang W., Wu Q., Lu Y.L., Gong Q.H., Zhang F., Shi J.S. Protective effects of Dendrobium nobile Lindl. alkaloids on amyloid beta (25-35)-induced neuronal injury. Neural Regen Res. 2017;12:1131–1136. doi: 10.4103/1673-5374.211193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li L.S., Lu Y.L., Nie J., Xu Y.Y., Zhang W., Yang W.J., Gong Q.H., Lu Y.F., Lu Y., Shi J.S. Dendrobium nobile Lindl alkaloid, a novel autophagy inducer, protects against axonal degeneration induced by Aβ(25-35) in hippocampus neurons in vitro. CNS Neurosci. Ther. 2017;23:329–340. doi: 10.1111/cns.12678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Go J., Park T.S., Han G.H., Park H.Y., Ryu Y.K., Kim Y.H., Hwang J.H., Choi D.H., Noh J.R., Hwang D.Y., et al. Piperlongumine decreases cognitive impairment and improves hippocampal function in aged mice. Int. J. Mol. Med. 2018;42:1875–1884. doi: 10.3892/ijmm.2018.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gu S.M., Lee H.P., Ham Y.W., Son D.J., Kim H.Y., Oh K.W., Han S.B., Yun J., Hong J.T. Piperlongumine Improves Lipopolysaccharide-Induced Amyloidogenesis by Suppressing NF-KappaB Pathway. Neuromol. Med. 2018;20:312–327. doi: 10.1007/s12017-018-8495-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhu J., Mu X., Zeng J., Xu C., Liu J., Zhang M., Li C., Chen J., Li T., Wang Y. Ginsenoside Rg1 Prevents Cognitive Impairment and Hippocampus Senescence in a Rat Model of D-Galactose-Induced Aging. PLoS ONE. 2014;9:e101291. doi: 10.1371/journal.pone.0101291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Qiu J., Li W., Feng S.H., Wang M., He Z.Y. Ginsenoside Rh2 promotes nonamyloidgenic cleavage of amyloid pre-cursor protein via a cholesterol-dependent pathway. Genet. Mol. Res. 2014;13:3586–3598. doi: 10.4238/2014.May.9.2. [DOI] [PubMed] [Google Scholar]
- 77.Li L., Liu J., Yan X., Qin K., Shi M., Lin T., Zhu Y., Kang T., Zhao G. Protective effects of ginsenoside Rd against okadaic acid-induced neurotoxicity in vivo and in vitro. J. Ethnopharmacol. 2011;138:135–141. doi: 10.1016/j.jep.2011.08.068. [DOI] [PubMed] [Google Scholar]
- 78.Hwang S.H., Shin T.-J., Choi S.-H., Cho H.-J., Lee B.-H., Pyo M.K., Lee J.-H., Kang J., Kim H.-J., Park C.-W., et al. Gintonin, newly identified compounds from ginseng, is novel lysophosphatidic acids-protein complexes and activates G protein-coupled lysophosphatidic acid receptors with high affinity. Mol. Cells. 2012;33:151–162. doi: 10.1007/s10059-012-2216-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Guo J., Chang L., Zhang X., Pei S., Yu M., Gao J. Ginsenoside compound K promotes β-amyloid peptide clearance in primary astrocytes via autophagy enhancement. Exp. Ther. Med. 2014;8:1271–1274. doi: 10.3892/etm.2014.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chalatsa I., Arvanitis D.A., Koulakiotis N.S., Giagini A., Skaltsounis A.L., Papadopoulou-Daifoti Z., Tsarbopoulos A., Sanoudou D. The Crocus sativus Compounds trans-Crocin 4 and trans-Crocetin Modulate the Amyloidogenic Pathway and Tau Misprocessing in Alzheimer Disease Neuronal Cell Culture Models. Front. Neurosci. 2019;13:249. doi: 10.3389/fnins.2019.00249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Deng M., Zhao J.Y., Ju X.D., Tu P.F., Jiang Y., Li Z.B. Protective effect of tubuloside B on TNFalpha-induced apoptosis in neuronal cells. Acta Pharm. Sin. 2004;25:1276–1284. [PubMed] [Google Scholar]
- 82.Li X., Gou C., Yang H., Qiu J., Gu T., Wen T. Echinacoside ameliorates D-galactosamine plus lipopolysaccha-ride-induced acute liver injury in mice via inhibition of apoptosis and inflammation. Scand. J. Gastroenterol. 2014;49:993–1000. doi: 10.3109/00365521.2014.913190. [DOI] [PubMed] [Google Scholar]
- 83.Singh J.C.H., Kakalij R.M., Kshirsagar R.P., Kumar B.H., Komakula S.S.B., Diwan P. Cognitive effects of vanillic acid against streptozotocin-induced neurodegeneration in mice. Pharm. Biol. 2014;53:630–636. doi: 10.3109/13880209.2014.935866. [DOI] [PubMed] [Google Scholar]
- 84.Yan J.J., Kim D.H., Moon Y.S., Jung J.S., Ahn E.M., Baek N.I., Song D.K. Protection against beta-amyloid pep-tide-induced memory impairment with long-term administration of extract of Angelica gigas or decursinol in mice. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2004;28:25–30. doi: 10.1016/S0278-5846(03)00168-4. [DOI] [PubMed] [Google Scholar]
- 85.Li L., Du J., Zou L., Xia H., Wu T., Kim Y., Lee Y. The Neuroprotective Effects of Decursin Isolated from Angelica gigas Nakai Against Amyloid β-Protein-Induced Apoptosis in PC 12 Cells via a Mitochondria-Related Caspase Pathway. Neurochem. Res. 2015;40:1555–1562. doi: 10.1007/s11064-015-1623-0. [DOI] [PubMed] [Google Scholar]
- 86.Kuang X., Du J.R., Chen Y.S., Wang J., Wang Y.N. Protective effect of Z-ligustilide against amyloid beta-induced neurotoxicity is associated with decreased pro-inflammatory markers in rat brains. Pharm. Biochem. Behav. 2009;92:635–641. doi: 10.1016/j.pbb.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 87.Xu W., Yang L., Li J. Protection against β-amyloid-induced neurotoxicity by naturally occurring Z-ligustilide through the concurrent regulation of p38 and PI3-K/Akt pathways. Neurochem. Int. 2016;100:44–51. doi: 10.1016/j.neuint.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 88.Wang X., Xu W., Chen H., Li W., Li W., Zhu G. Astragaloside IV prevents Aβ1-42 oligomers-induced memory impairment and hippocampal cell apoptosis by promoting PPARγ/BDNF signaling pathway. Brain Res. 2020;1747:147041. doi: 10.1016/j.brainres.2020.147041. [DOI] [PubMed] [Google Scholar]
- 89.Wang X., Wang Y., Hu J.P., Yu S., Li B.K., Cui Y., Zhang L.D. Astragaloside IV, a Natural PPARγ Agonist, Reduces Aβ Production in Alzheimer’s Disease Through Inhibition of BACE1. Mol. Neurobiol. 2017;54:2939–2949. doi: 10.1007/s12035-016-9874-6. [DOI] [PubMed] [Google Scholar]
- 90.Sun Q., Jia N., Wang W., Jin H., Xu J., Hu H. Protective effects of astragaloside IV against amyloid beta1-42 neuro-toxicity by inhibiting the mitochondrial permeability transition pore opening. PLoS ONE. 2014;9:e98866. doi: 10.1371/journal.pone.0098866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu A., Zhao X., Li H., Liu Z., Liu B., Mao X., Jia Y. 5-Hydroxymethylfurfural, an antioxidant agent from Alpinia oxyphylla Miq. improves cognitive impairment in Aβ 1-42 mouse model of Alzheimer’s disease. Int. Immunopharmacol. 2014;23:719–725. doi: 10.1016/j.intimp.2014.10.028. [DOI] [PubMed] [Google Scholar]
- 92.Shi S.-H., Zhao X., Liu A.-J., Liu B., Li H., Wu B., Bi K.-S., Jia Y. Protective effect of n-butanol extract from Alpinia oxyphylla on learning and memory impairments. Physiol. Behav. 2014;139:13–20. doi: 10.1016/j.physbeh.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 93.Zeng G.-F., Zong S.-H., Zhang Z.-Y., Fu S.-W., Li K.-K., Fang Y., Lu L., Xiao D.-Q. The Role of 6-Gingerol on Inhibiting Amyloid β Protein-Induced Apoptosis in PC12 Cells. Rejuvenation Res. 2015;18:413–421. doi: 10.1089/rej.2014.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gabriel M.O., Nikou M., Akinola O.B., Pollak D.D., Sideromenos S. Western diet-induced fear memory impairment is attenuated by 6-shogaol in C57BL/6N mice. Behav. Brain Res. 2019;380:112419. doi: 10.1016/j.bbr.2019.112419. [DOI] [PubMed] [Google Scholar]
- 95.Moon M., Kim H.G., Choi J.G., Oh H., Lee P.K., Ha S.K., Kim S.Y., Park Y., Huh Y., Oh M.S. 6-Shogaol, an active constituent of ginger, attenuates neuroinflammation and cognitive deficits in animal models of dementia. Biochem. Biophys. Res. Commun. 2014;449:8–13. doi: 10.1016/j.bbrc.2014.04.121. [DOI] [PubMed] [Google Scholar]
- 96.Wang D.M., Yang Y.J., Zhang L., Zhang X., Guan F.F., Zhang L.F. Naringin Enhances CaMKII Activity and Improves Long-Term Memory in a Mouse Model of Alzheimer’s Disease. Int. J. Mol. Sci. 2013;14:5576–5586. doi: 10.3390/ijms14035576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Justin Thenmozhi A., William Raja T.R., Manivasagam T., Janakiraman U., Essa M.M. Hesperidin ameliorates cognitive dysfunction, oxidative stress and apoptosis against aluminium chloride induced rat model of Alzheimer’s disease. Nutr. Neurosci. 2017;20:360–368. doi: 10.1080/1028415X.2016.1144846. [DOI] [PubMed] [Google Scholar]
- 98.Li C., Zug C., Qu H., Schluesener H., Zhang Z. Hesperidin ameliorates behavioral impairments and neuropathology of transgenic APP/PS1 mice. Behav. Brain Res. 2015;281:32–42. doi: 10.1016/j.bbr.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 99.Hong Y., An Z. Hesperidin attenuates learning and memory deficits in APP/PS1 mice through activation of Akt/Nrf2 signaling and inhibition of RAGE/NF-κB signaling. Arch. Pharm. Res. 2018;41:655–663. doi: 10.1007/s12272-015-0662-z. [DOI] [PubMed] [Google Scholar]
- 100.Shin M., Liu Q.F., Choi B., Shin C., Lee B., Yuan C., Song Y.J., Yun H.S., Lee I.-S., Koo B.-S., et al. Neuroprotective Effects of Limonene (+) against Aβ42-Induced Neurotoxicity in a Drosophila Model of Alzheimer’s Disease. Biol. Pharm. Bull. 2020;43:409–417. doi: 10.1248/bpb.b19-00495. [DOI] [PubMed] [Google Scholar]
- 101.Zhao L., Wang J.L., Liu R., Li X.X., Li J.F., Zhang L. Neuroprotective, anti-amyloidogenic and neurotrophic effects of apigenin in an Alzheimer’s disease mouse model. Molecules. 2013;18:9949–9965. doi: 10.3390/molecules18089949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhao L., Wang J.L., Wang Y.R., Fa X.Z. Apigenin attenuates copper-mediated β-amyloid neurotoxicity through antioxidation, mitochondrion protection and MAPK signal inactivation in an AD cell model. Brain Res. 2013;1492:33–45. doi: 10.1016/j.brainres.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 103.Ha S.K., Lee P., Park J.A., Oh H.R., Lee S.Y., Park J.-H., Lee E.H., Ryu J.H., Lee K.R., Kim S.Y. Apigenin inhibits the production of NO and PGE2 in microglia and inhibits neuronal cell death in a middle cerebral artery occlusion-induced focal ischemia mice model. Neurochem. Int. 2008;52:878–886. doi: 10.1016/j.neuint.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 104.Dourado N.S., Souza C., De Almeida M.M.A., Da Silva A.B., dos Santos B.L., Silva V.D.A., De Assis A.M., Da Silva J.S., Souza D.O., Costa M.D.F.D., et al. Neuroimmunomodulatory and Neuroprotective Effects of the Flavonoid Apigenin in in vitro Models of Neuroinflammation Associated with Alzheimer’s Disease. Front. Aging Neurosci. 2020;12:119. doi: 10.3389/fnagi.2020.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Guo A.J., Xie H.Q., Choi R.C., Zheng K.Y., Bi C.W., Xu S.L., Dong T.T., Tsim K. Galangin, a flavonol derived from Rhizoma Alpiniae Officinarum, inhibits acetylcholinesterase activity in vitro. Chem. Interactions. 2010;187:246–248. doi: 10.1016/j.cbi.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 106.Cheng Y., Dong Z., Liu S. β-Caryophyllene Ameliorates the Alzheimer-Like Phenotype in APP/PS1 Mice through CB2 Receptor Activation and the PPARγ Pathway. Pharmacology. 2014;94:1–12. doi: 10.1159/000362689. [DOI] [PubMed] [Google Scholar]
- 107.Abdul Manap A.S., Wei Tan A.C., Leong W.H., Yin Chia A.Y. Synergistic Effects of Curcumin and Piperine as Potent Acetylcholine and Amyloidogenic Inhibitors With Significant Neuroprotective Activity in SH-SY5Y Cells via Computational Molecular Modeling and in vitro Assay. Front. Aging Neurosci. 2019;11:206. doi: 10.3389/fnagi.2019.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nazifi M., Oryan S., Esfahani D.E., Ashrafpoor M. The functional effects of piperine and piperine plus donepezil on hippocampal synaptic plasticity impairment in rat model of Alzheimer’s disease. Life Sci. 2021;265:118802. doi: 10.1016/j.lfs.2020.118802. [DOI] [PubMed] [Google Scholar]
- 109.Chonpathompikunlert P., Wattanathorn J., Muchimapura S. Piperine, the main alkaloid of Thai black pepper, protects against neurodegeneration and cognitive impairment in animal model of cognitive deficit like condition of Alzheimer’s disease. Food Chem. Toxicol. 2010;48:798–802. doi: 10.1016/j.fct.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 110.Liu Z.J., Li Z.H., Liu L., Tang W.X., Wang Y., Dong M.R., Xiao C. Curcumin Attenuates Beta-Amyloid-Induced Neuroinflammation via Activation of Peroxisome Proliferator-Activated Receptor-Gamma Function in a Rat Model of Alzheimer’s Disease. Front. Pharm. 2016;7:261. doi: 10.3389/fphar.2016.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Maiti P., Paladugu L., Dunbar G.L. Solid lipid curcumin particles provide greater anti-amyloid, anti-inflammatory and neuroprotective effects than curcumin in the 5xFAD mouse model of Alzheimer’s disease. BMC Neurosci. 2018;19:7. doi: 10.1186/s12868-018-0406-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 112.Park S.Y., Jin M.L., Kim Y.H., Kim Y., Lee S.J. Anti-inflammatory effects of aromatic-turmerone through blocking of NF-κB, JNK, and p38 MAPK signaling pathways in amyloid β-stimulated microglia. Int. Immunopharmacol. 2012;14:13–20. doi: 10.1016/j.intimp.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 113.Chen M., Chang Y.Y., Huang S., Xiao L.H., Zhou W., Zhang L.Y., Zhang K. Aromatic-Turmerone Attenuates LPS-Induced Neuroinflammation and Consequent Memory Impairment by Targeting TLR4-Dependent Signaling Path-way. Mol. Nutr. Food Res. 2018;62:1700281. doi: 10.1002/mnfr.201700281. [DOI] [PubMed] [Google Scholar]
- 114.Saga Y., Hatakenaka Y., Matsumoto M., Yoshioka Y., Matsumura S., Zaima N., Konishi Y. Neuroprotective effects of aromatic turmerone on activity deprivation-induced apoptosis in cerebellar granule neurons. NeuroReport. 2020;31:1302–1307. doi: 10.1097/WNR.0000000000001551. [DOI] [PubMed] [Google Scholar]
- 115.Hong X.-P., Chen T., Yin N.-N., Han Y.-M., Yuan F., Duan Y.-J., Shen F., Zhang Y.-H., Chen Z.-B. Puerarin Ameliorates D-Galactose Induced Enhanced Hippocampal Neurogenesis and Tau Hyperphosphorylation in Rat Brain. J. Alzheimer’s Dis. 2016;51:605–617. doi: 10.3233/JAD-150566. [DOI] [PubMed] [Google Scholar]
- 116.Zhou Y.-X., Zhang H., Peng C. Puerarin: A Review of Pharmacological Effects. Phytother. Res. 2013;28:961–975. doi: 10.1002/ptr.5083. [DOI] [PubMed] [Google Scholar]
- 117.Xing G., Dong M., Li X., Zou Y., Fan L., Wang X., Niu Y. Neuroprotective effects of puerarin against be-ta-amyloid-induced neurotoxicity in PC12 cells via a PI3K-dependent signaling pathway. Brain Res. Bull. 2011;85:212–218. doi: 10.1016/j.brainresbull.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 118.Lee Y.H., Kim J.H., Song C.H., Jang K.J., Kim C.H., Kang J.S., Choi Y.H., Yoon H.M. Ethanol Extract of Ganoderma lucidum Augments Cellular Anti-oxidant Defense through Activation of Nrf2/HO-1. J Pharmacopuncture. 2016;19:59–69. doi: 10.3831/kpi.2016.19.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhang X., Wang J., Gong G., Ma R., Xu F., Yan T., Jia Y. Spinosin Inhibits Aβ(1-42) Production and Aggregation via Activating Nrf2/HO-1 Pathway. Biomol. Ther. 2020;28:259–266. doi: 10.4062/biomolther.2019.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Xu F., He B., Xiao F., Yan T., Bi K., Jia Y., Wang Z. Neuroprotective Effects of Spinosin on Recovery of Learning and Memory in a Mouse Model of Alzheimer’s Disease. Biomol. Ther. 2019;27:71–77. doi: 10.4062/biomolther.2018.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cai M., Jung I., Kwon H., Cho E., Jeon J., Yun J., Lee Y.C., Kim D.H., Ryu J.H. Spinosin Attenuates Alzheimer’s Disease-Associated Synaptic Dysfunction via Regulation of Plasmin Activity. Biomol. Ther. 2020;28:131–136. doi: 10.4062/biomolther.2019.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ko S.Y., Lee H.E., Park S.J., Jeon S.J., Kim B., Gao Q., Jang D.S., Ryu J.H. Spinosin, a C-Glucosylflavone, from Zizyphus jujuba var. spinosa Ameliorates Aβ1-42 Oligomer-Induced Memory Impairment in Mice. Biomol. Ther. 2015;23:156–164. doi: 10.4062/biomolther.2014.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jia S.L., Wu X.L., Li X.X., Dai X.L., Gao Z.L., Lu Z., Zheng Q.S., Sun Y.X. Neuroprotective effects of liquiritin on cognitive deficits induced by soluble amyloid-β(1-42) oligomers injected into the hippocampus. J. Asian Nat. Prod. Res. 2016;18:1186–1199. doi: 10.1080/10286020.2016.1201811. [DOI] [PubMed] [Google Scholar]
- 124.Cui Y.M., Ao M.Z., Li W., Yu L.J. Effect of glabridin from Glycyrrhiza glabra on learning and memory in mice. Planta Med. 2008;74:377–380. doi: 10.1055/s-2008-1034319. [DOI] [PubMed] [Google Scholar]
- 125.Du Y., Luo M., Du Y., Xu M., Yao Q., Wang K., He G. Liquiritigenin Decreases Aβ Levels and Ameliorates Cognitive Decline by Regulating Microglia M1/M2 Transformation in AD Mice. Neurotox Res. 2021;39:349–358. doi: 10.1007/s12640-020-00284-z. [DOI] [PubMed] [Google Scholar]
- 126.Yang W., Liu Y., Xu Q.Q., Xian Y.F., Lin Z.X. Sulforaphene Ameliorates Neuroinflammation and Hyperphosphorylated Tau Protein via Regulating the PI3K/Akt/GSK-3β Pathway in Experimental Models of Alzheimer’s Disease. Oxid. Med. Cell Longev. 2020;2020:4754195. doi: 10.1155/2020/4754195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Liu B., Gao J.M., Li F., Gong Q.H., Shi J.S. Gastrodin Attenuates Bilateral Common Carotid Artery Occlu-sion-Induced Cognitive Deficits via Regulating Aβ-Related Proteins and Reducing Autophagy and Apoptosis in Rats. Front. Pharm. 2018;9:405. doi: 10.3389/fphar.2018.00405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yoon J.H., Youn K., Ho C.T., Karwe M.V., Jeong W.S., Jun M. p-Coumaric acid and ursolic acid from Corni fructus attenuated β-amyloid(25-35)-induced toxicity through regulation of the NF-κB signaling pathway in PC12 cells. J. Agric. Food Chem. 2014;62:4911–4916. doi: 10.1021/jf501314g. [DOI] [PubMed] [Google Scholar]
- 129.Kiefer D., Pantuso T. Panax ginseng. Am. Fam. Physician. 2003;68:1539–1542. [PubMed] [Google Scholar]
- 130.Ginseng . Drugs and Lactation Database (LactMed) National Library of Medicine; Bethesda, MD, USA: 2006. [(accessed on 27 November 2021)]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK501814/ [Google Scholar]
- 131.Choi S.-H., Hong M.-K., Kim H.-J., Ryoo N., Rhim H., Nah S.-Y., Kang L.-W. Structure of ginseng major latex-like protein 151 and its proposed lysophosphatidic acid-binding mechanism. Acta Crystallogr. Sect. D Biol. Crystallogr. 2015;71:1039–1050. doi: 10.1107/S139900471500259X. [DOI] [PubMed] [Google Scholar]
- 132.Fernández-Albarral J.A., de Hoz R., Ramírez A.I., López-Cuenca I., Salobrar-García E., Pinazo-Durán M.D., Salazar J.J. Beneficial effects of saffron (Crocus sativus L.) in ocular pathologies, particularly neurodegenerative retinal diseases. Neural. Regen. Res. 2020;15:1408–1416. doi: 10.4103/1673-5374.274325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Moshiri M., Vahabzadeh M., Hosseinzadeh H. Clinical Applications of Saffron (Crocus sativus) and its Constituents: A Review. Drug Res. 2014;65:287–295. doi: 10.1055/s-0034-1375681. [DOI] [PubMed] [Google Scholar]
- 134.Hatziagapiou K., Kakouri E., Lambrou G.I., Bethanis K., Tarantilis P.A. Antioxidant Properties of Crocus sativus L. and Its Constituents and Relevance to Neurodegenerative Diseases; Focus on Alzheimer’s and Parkinson’s Disease. Curr. Neuropharmacol. 2019;17:377–402. doi: 10.2174/1570159X16666180321095705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ochiai T., Shimeno H., Mishima K.-I., Iwasaki K., Fujiwara M., Tanaka H., Shoyama Y., Toda A., Eyanagi R., Soeda S. Protective effects of carotenoids from saffron on neuronal injury in vitro and in vivo. Biochim. Biophys. Acta Gen. Subj. 2007;1770:578–584. doi: 10.1016/j.bbagen.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 136.Song Y., Zeng K., Jiang Y., Tu P. Cistanches Herba, from an endangered species to a big brand of Chinese medicine. Med. Res. Rev. 2021;41:1539–1577. doi: 10.1002/med.21768. [DOI] [PubMed] [Google Scholar]
- 137.Lei H., Wang X., Zhang Y., Cheng T., Mi R., Xu X., Zu X., Zhang W. Herba Cistanche (Rou Cong Rong): A Review of Its Phytochemistry and Pharmacology. Chem. Pharm. Bull. 2020;68:694–712. doi: 10.1248/cpb.c20-00057. [DOI] [PubMed] [Google Scholar]
- 138.Fu Z., Fan X., Wang X., Gao X. Cistanches Herba: An overview of its chemistry, pharmacology, and pharmacokinetics property. J. Ethnopharmacol. 2018;219:233–247. doi: 10.1016/j.jep.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 139.Gu C., Yang X., Huang L. Cistanches Herba: A Neuropharmacology Review. Front. Pharmacol. 2016;7:289. doi: 10.3389/fphar.2016.00289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wang N., Ji S., Zhang H., Mei S., Qiao L., Jin X. Herba Cistanches: Anti-aging. Aging Dis. 2017;8:740–759. doi: 10.14336/AD.2017.0720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Geng X., Song L., Pu X., Tu P. Neuroprotective effects of phenylethanoid glycosides from Cistanches salsa against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced dopaminergic toxicity in C57 mice. Biol. Pharm. Bull. 2004;27:797–801. doi: 10.1248/bpb.27.797. [DOI] [PubMed] [Google Scholar]
- 142.Yi L., Liang Y., Wu H., Yuan D. The analysis of Radix Angelicae Sinensis (Danggui) J. Chromatogr. A. 2009;1216:1991–2001. doi: 10.1016/j.chroma.2008.07.033. [DOI] [PubMed] [Google Scholar]
- 143.Gong G., Li N., Lau K.-M., Lee P.S.-C., Yan L., Xu M., Lam C.T.-W., Kong A.Y.-Y., Lin H.-Q., Dong T.T.-X., et al. Calycosin orchestrates the functions of Danggui Buxue Tang, a Chinese herbal decoction composing of Astragali Radix and Angelica Sinensis Radix: An evaluation by using calycosin-knock out herbal extract. J. Ethnopharmacol. 2015;168:150–157. doi: 10.1016/j.jep.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 144.Singh Y.P., Rai H., Singh G., Singh G.K., Mishra S., Kumar S., Srikrishna S., Modi G. A review on ferulic acid and analogs-based scaffolds for the management of Alzheimer’s disease. Eur. J. Med. Chem. 2021;215:113278. doi: 10.1016/j.ejmech.2021.113278. [DOI] [PubMed] [Google Scholar]
- 145.Guo J., Shang E.-X., Duan J.-A., Tang Y., Qian D. Determination of ligustilide in the brains of freely moving rats using microdialysis coupled with ultra-performance liquid chromatography/mass spectrometry. Fitoterapia. 2011;82:441–445. doi: 10.1016/j.fitote.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 146.Su H., Shaker S., Kuang Y., Zhang M., Ye M., Qiao X. Phytochemistry and cardiovascular protective effects of Huang-Qi (Astragali Radix) Med. Res. Rev. 2021;41:1999–2038. doi: 10.1002/med.21785. [DOI] [PubMed] [Google Scholar]
- 147.Baker J.R., Vuppusetty C., Colley T., Papaioannou A.I., Fenwick P., Donnelly L., Ito K., Barnes P.J. Oxidative stress dependent microRNA-34a activation via PI3Kα reduces the expression of sirtuin-1 and sirtuin-6 in epithelial cells. Sci. Rep. 2016;6:35871. doi: 10.1038/srep35871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Wang X., Gao F., Xu W., Cao Y., Wang J., Zhu G. Depichering the Effects of Astragaloside IV on AD-Like Phenotypes: A Systematic and Experimental Investigation. Oxid. Med. Cell. Longev. 2021;2021:1020614. doi: 10.1155/2021/1020614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sun Y. Biological activities and potential health benefits of polysaccharides from Poria cocos and their derivatives. Int. J. Biol. Macromol. 2014;68:131–134. doi: 10.1016/j.ijbiomac.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 150.Ríos J.-L. Chemical Constituents and Pharmacological Properties of Poria cocos. Planta Med. 2011;77:681–691. doi: 10.1055/s-0030-1270823. [DOI] [PubMed] [Google Scholar]
- 151.Zhang Q., Zheng Y., Hu X., Hu X., Lv W., Lv D., Chen J., Wu M., Song Q., Shentu J. Ethnopharmacological uses, phytochemistry, biological activities, and therapeutic applications of Alpinia oxyphylla Miquel: A review. J. Ethnopharmacol. 2018;224:149–168. doi: 10.1016/j.jep.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 152.Li J., Du Q., Li N., Du S., Sun Z. Alpiniae oxyphyllae Fructus and Alzheimer’s disease: An update and current per-spective on this traditional Chinese medicine. Biomed. Pharm. 2021;135:111167. doi: 10.1016/j.biopha.2020.111167. [DOI] [PubMed] [Google Scholar]
- 153.He B., Xu F., Yan T., Xiao F., Wu B., Wang Y., Jia Y. Tectochrysin from Alpinia oxyphylla Miq. alleviates Aβ(1-42) induced learning and memory impairments in mice. Eur. J. Pharm. 2019;842:365–372. doi: 10.1016/j.ejphar.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 154.Ginger . Drugs and Lactation Database (LactMed) National Library of Medicine; Bethesda, MD, USA: 2006. [(accessed on 27 November 2021)]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK501786/ [Google Scholar]
- 155.Mao Q.-Q., Xu X.-Y., Cao S.-Y., Gan R.-Y., Corke H., Beta T., Li H.-B. Bioactive Compounds and Bioactivities of Ginger (Zingiber officinale Roscoe) Foods. 2019;8:185. doi: 10.3390/foods8060185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kou X., Wang X., Ji R., Liu L., Qiao Y., Lou Z., Ma C., Li S., Wang H., Ho C.-T. Occurrence, biological activity, and metabolism of 6-shogaol. Food Funct. 2018;9:1310–1327. doi: 10.1039/C7FO01354J. [DOI] [PubMed] [Google Scholar]
- 157.Jiang J., Hou R., Yang N., Li L., Deng J., Qin G., Ding D. Physiological and TMT-labeled proteomic analyses reveal important roles of sugar and secondary metabolism in Citrus junos under cold stress. J. Proteom. 2021;237:104145. doi: 10.1016/j.jprot.2021.104145. [DOI] [PubMed] [Google Scholar]
- 158.Habtemariam S. Rutin as a Natural Therapy for Alzheimer’s Disease: Insights into its Mechanisms of Action. Curr. Med. Chem. 2016;23:860–873. doi: 10.2174/0929867323666160217124333. [DOI] [PubMed] [Google Scholar]
- 159.Aliaga K.L.J., Bermejo-Bescós P., Benedi J., Martín-Aragón S. Quercetin and rutin exhibit antiamyloidogenic and fibril-disaggregating effects in vitro and potent antioxidant activity in APPswe cells. Life Sci. 2011;89:939–945. doi: 10.1016/j.lfs.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 160.Yu X.L., Li Y.N., Zhang H., Su Y.J., Zhou W.W., Zhang Z.P., Liu R.T. Rutin inhibits amylin-induced neurocy-totoxicity and oxidative stress. Food Funct. 2015;6:3296–3306. doi: 10.1039/C5FO00500K. [DOI] [PubMed] [Google Scholar]
- 161.Chakraborty S., Basu S. Multi-functional activities of citrus flavonoid narirutin in Alzheimer’s disease therapeutics: An integrated screening approach and in vitro validation. Int. J. Biol. Macromol. 2017;103:733–743. doi: 10.1016/j.ijbiomac.2017.05.110. [DOI] [PubMed] [Google Scholar]
- 162.Viswanatha G.L., Shylaja H., Sandeep Rao K.S., Santhosh Kumar V.R., Jagadeesh M. Hesperidin ameliorates im-mobilization-stress-induced behavioral and biochemical alterations and mitochondrial dysfunction in mice by modulating nitrergic pathway. ISRN Pharm. 2012;2012:479570. doi: 10.5402/2012/479570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zaplatic E., Bule M., Shah S.Z.A., Uddin M.S., Niaz K. Molecular mechanisms underlying protective role of quercetin in attenuating Alzheimer’s disease. Life Sci. 2019;224:109–119. doi: 10.1016/j.lfs.2019.03.055. [DOI] [PubMed] [Google Scholar]
- 164.Meghwal M., Goswami T.K. Piper nigrum and Piperine: An Update. Phytother. Res. 2013;27:1121–1130. doi: 10.1002/ptr.4972. [DOI] [PubMed] [Google Scholar]
- 165.Salehi B., Venditti A., Sharifi-Rad M., Kręgiel D., Sharifi-Rad J., Durazzo A., Lucarini M., Santini A., Souto E.B., Novellino E., et al. The Therapeutic Potential of Apigenin. Int. J. Mol. Sci. 2019;20:1305. doi: 10.3390/ijms20061305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Vinturelle R., Mattos C., Meloni J., Nogueira J., Nunes M.J., Vaz I.S., Rocha L., Lione V., Castro H.C., Das Chagas E.F. In Vitro Evaluation of Essential Oils Derived from Piper nigrum (Piperaceae) and Citrus limonum (Rutaceae) against the Tick Rhipicephalus (Boophilus) microplus (Acari: Ixodidae) Biochem. Res. Int. 2017;2017:5342947. doi: 10.1155/2017/5342947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Andriana Y., Xuan T.D., Quy T.N., Tran H.-D., Le Q.-T. Biological Activities and Chemical Constituents of Essential Oils from Piper cubeba Bojer and Piper nigrum L. Molecules. 2019;24:1876. doi: 10.3390/molecules24101876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Gautam S., Karmakar S., Bose A., Chowdhury P.K. β-cyclodextrin and curcumin, a potent cocktail for disaggregating and/or inhibiting amyloids: A case study with α-synuclein. Biochemistry. 2014;53:4081–4083. doi: 10.1021/bi500642f. [DOI] [PubMed] [Google Scholar]
- 169.Derosa G., Maffioli P., Sahebkar A. Piperine and Its Role in Chronic Diseases. Adv. Exp. Med. Biol. 2016;928:173–184. doi: 10.1007/978-3-319-41334-1_8. [DOI] [PubMed] [Google Scholar]
- 170.Wang J., Cao B., Zhao H., Feng J. Emerging Roles of Ganoderma Lucidum in Anti-Aging. Aging Dis. 2017;8:691–707. doi: 10.14336/AD.2017.0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ahmad M.F. Ganoderma lucidum: Persuasive biologically active constituents and their health endorsement. Biomed Pharm. 2018;107:507–519. doi: 10.1016/j.biopha.2018.08.036. [DOI] [PubMed] [Google Scholar]
- 172.Sanodiya B.S., Thakur G.S., Baghel R.K., Prasad G.B.K.S., Bisen P.S. Ganoderma lucidum: A Potent Pharmacological Macrofungus. Curr. Pharm. Biotechnol. 2009;10:717–742. doi: 10.2174/138920109789978757. [DOI] [PubMed] [Google Scholar]
- 173.Qin C., Wu S., Chen B., Wu X., Qu K., Liu J., Lu Y. Effect of Ganoderma Lucidum Preparation on the Behav-ior, Biochemistry, and Autoimmune Parameters of Mouse Models of APP/PS1 Double Transgenic Alzheimer’s Disease. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2017;39:330–335. doi: 10.3881/j.issn.1000-503X.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 174.Lai C.S., Yu M.S., Yuen W.H., So K.F., Zee S.Y., Chang R.C. Antagonizing beta-amyloid peptide neurotoxicity of the anti-aging fungus Ganoderma lucidum. Brain Res. 2008;1190:215–224. doi: 10.1016/j.brainres.2007.10.103. [DOI] [PubMed] [Google Scholar]
- 175.Yoon H.M., Jang K.J., Han M.S., Jeong J.W., Kim G.Y., Lee J.H., Choi Y.H. Ganoderma lucidum ethanol extract inhibits the inflammatory response by suppressing the NF-κB and toll-like receptor pathways in lipopolysaccha-ride-stimulated BV2 microglial cells. Exp. Med. 2013;5:957–963. doi: 10.3892/etm.2013.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lu S.-Y., Peng X.-R., Dong J.-R., Yan H., Kong Q.-H., Shi Q.-Q., Li D.-S., Zhou L., Li Z.-R., Qiu M.-H. Aromatic constituents from Ganoderma lucidum and their neuroprotective and anti-inflammatory activities. Fitoterapia. 2019;134:58–64. doi: 10.1016/j.fitote.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 177.Yu N., Huang Y., Jiang Y., Zou L., Liu X., Liu S., Zhu Y. Ganoderma lucidum Triterpenoids (GLTs) Reduce Neuronal Apoptosis via Inhibition of ROCK Signal Pathway in APP/PS1 Transgenic Alzheimer’s Disease Mice. Oxid. Med. Cell Longev. 2020;2020:9894037. doi: 10.1155/2020/9894037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zhang Z., Lam T.N., Zuo Z. Radix Puerariae: An overview of its chemistry, pharmacology, pharmacokinetics, and clinical use. J. Clin. Pharm. 2013;53:787–811. doi: 10.1002/jcph.96. [DOI] [PubMed] [Google Scholar]
- 179.Zhou Y., Xie N., Li L., Zou Y., Zhang X., Dong M. Puerarin alleviates cognitive impairment and oxidative stress in APP/PS1 transgenic mice. Int. J. Neuropsychopharmacol. 2013;17:635–644. doi: 10.1017/S146114571300148X. [DOI] [PubMed] [Google Scholar]
- 180.He S.-R., Zhao C.-B., Zhang J.-X., Wang J., Wu B., Wu C.-J. Botanical and Traditional Uses and Phytochemical, Pharmacological, Pharmacokinetic, and Toxicological Characteristics of Ziziphi Spinosae Semen: A Review. Evid. Based Complement. Altern. Med. 2020;2020:5861821. doi: 10.1155/2020/5861821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Villanueva J.R., Villanueva L.R. Experimental and Clinical Pharmacology of Ziziphus jujuba Mills. Phytother. Res. 2017;31:347–365. doi: 10.1002/ptr.5759. [DOI] [PubMed] [Google Scholar]
- 182.Wang L.E., Cui X.Y., Cui S.Y., Cao J.X., Zhang J., Zhang Y.H., Zhao Y.Y. Potentiating effect of spinosin, a C-glycoside flavonoid of Semen Ziziphi spinosae, on pentobarbital-induced sleep may be related to postsynaptic 5-HT(1A) receptors. Phytomedicine. 2010;17:404–409. doi: 10.1016/j.phymed.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 183.Zhan H.-D., Zhou H.-Y., Sui Y.-P., Du X.-L., Wang W.-H., Dai L., Sui F., Huo H.-R., Jiang T.-L. The rhizome of Gastrodia elata Blume—An ethnopharmacological review. J. Ethnopharmacol. 2016;189:361–385. doi: 10.1016/j.jep.2016.06.057. [DOI] [PubMed] [Google Scholar]
- 184.Liu Y., Gao J., Peng M., Meng H., Ma H., Cai P., Xu Y., Zhao Q., Si G. A Review on Central Nervous System Effects of Gastrodin. Front. Pharmacol. 2018;9:24. doi: 10.3389/fphar.2018.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Li J.-J., Liu S.-J., Liu X.-Y., Ling E.-A. Herbal Compounds with Special Reference to Gastrodin as Potential Therapeutic Agents for Microglia Mediated Neuroinflammation. Curr. Med. Chem. 2019;25:5958–5974. doi: 10.2174/0929867325666180214123929. [DOI] [PubMed] [Google Scholar]
- 186.Neelam K., Dey S., Sim R., Lee J., Eong K.-G.A. Fructus lycii: A Natural Dietary Supplement for Amelioration of Retinal Diseases. Nutrients. 2021;13:246. doi: 10.3390/nu13010246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Xing X., Liu F., Xiao J., So K.F. Neuro-protective Mechanisms of Lycium barbarum. Neuromol. Med. 2016;18:253–263. doi: 10.1007/s12017-016-8393-y. [DOI] [PubMed] [Google Scholar]
- 188.Gao Y., Wei Y., Wang Y., Gao F., Chen Z. Lycium barbarum: A Traditional Chinese Herb and A Promising Anti-Aging Agent. Aging Dis. 2017;8:778–791. doi: 10.14336/AD.2017.0725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Finkel T., Holbrook N.J. Oxidants, oxidative stress and the biology of ageing. Nature. 2000;408:239–247. doi: 10.1038/35041687. [DOI] [PubMed] [Google Scholar]
- 190.He M., Pan H., Chang R.C., So K.F., Brecha N.C., Pu M. Activation of the Nrf2/HO-1 antioxidant pathway con-tributes to the protective effects of Lycium barbarum polysaccharides in the rodent retina after ischemia-reperfusion-induced damage. PLoS ONE. 2014;9:e84800. doi: 10.1371/journal.pone.0084800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ma L., Dou H.-L., Wu Y., Huang Y.-M., Huang Y.-B., Xu X.-R., Zou Z., Lin X.-M. Lutein and zeaxanthin intake and the risk of age-related macular degeneration: A systematic review and meta-analysis. Br. J. Nutr. 2011;107:350–359. doi: 10.1017/S0007114511004260. [DOI] [PubMed] [Google Scholar]
- 192.Habtemariam S. Protective Effects of Caffeic Acid, and the Alzheimer’s Brain: An Update. Mini Rev. Med. Chem. 2017;17:667–674. doi: 10.2174/1389557516666161130100947. [DOI] [PubMed] [Google Scholar]
- 193.Basri A.M., Taha H., Ahmad N. A Review on the Pharmacological Activities and Phytochemicals of Alpinia officinarum (Galangal) Extracts Derived from Bioassay-Guided Fractionation and Isolation. Pharm. Rev. 2017;11:43–56. doi: 10.4103/phrev.phrev_55_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Abubakar I.B., Malami I., Yahaya Y., Sule S.M. A review on the ethnomedicinal uses, phytochemistry and pharmacology of Alpinia officinarum Hance. J. Ethnopharmacol. 2018;224:45–62. doi: 10.1016/j.jep.2018.05.027. [DOI] [PubMed] [Google Scholar]
- 195.Tao L., Wang Z.-T., Zhu E.-Y., Lu Y.-H., Wei D.-Z. HPLC analysis of bioactive flavonoids from the rhizome of Alpinia officinarum. S. Afr. J. Bot. 2006;72:163–166. doi: 10.1016/j.sajb.2005.06.007. [DOI] [Google Scholar]
- 196.Liu R., Zhang T., Yang H., Lan X., Ying J., Du G. The flavonoid apigenin protects brain neurovascular coupling against amyloid-β25–35-induced toxicity in mice. J. Alzheimers Dis. 2011;24:85–100. doi: 10.3233/JAD-2010-101593. [DOI] [PubMed] [Google Scholar]
- 197.Zhao L., Hou L., Sun H., Yan X., Sun X., Li J., Bian Y., Chu Y., Liu Q. Apigenin Isolated from the Medicinal Plant Elsholtzia rugulosa Prevents β-Amyloid 25–35-Induces Toxicity in Rat Cerebral Microvascular Endothelial Cells. Molecules. 2011;16:4005–4019. doi: 10.3390/molecules16054005. [DOI] [Google Scholar]
- 198.Soleimani V., Sahebkar A., Hosseinzadeh H. Turmeric (Curcuma longa) and its major constituent (curcumin) as nontoxic and safe substances: Review. Phytother. Res. 2018;32:985–995. doi: 10.1002/ptr.6054. [DOI] [PubMed] [Google Scholar]
- 199.Araújo C., Leon L. Biological activities of Curcuma longa L. Mem. Do Inst. Oswaldo Cruz. 2001;96:723–728. doi: 10.1590/S0074-02762001000500026. [DOI] [PubMed] [Google Scholar]
- 200.Dosoky N.S., Setzer W.N. Chemical Composition and Biological Activities of Essential Oils of Curcuma Species. Nutrients. 2018;10:1196. doi: 10.3390/nu10091196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Tang M., Taghibiglou C. The Mechanisms of Action of Curcumin in Alzheimer’s Disease. J. Alzheimer’s Dis. 2017;58:1003–1016. doi: 10.3233/JAD-170188. [DOI] [PubMed] [Google Scholar]
- 202.Singh P.K., Kotia V., Ghosh D., Mohite G.M., Kumar A., Maji S.K. Curcumin Modulates α-Synuclein Aggregation and Toxicity. ACS Chem. Neurosci. 2012;4:393–407. doi: 10.1021/cn3001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Da Costa I.M., Freire M., Cavalcanti J.R.L.D.P., De Araújo D.P., Norrara B., Rosa I.M.M.M., De Azevedo E.P., Rêgo A.C.M.D., Filho I.A., Guzen F.P. Supplementation with Curcuma longa Reverses Neurotoxic and Behavioral Damage in Models of Alzheimer’s Disease: A Systematic Review. Curr. Neuropharmacol. 2019;17:406–421. doi: 10.2174/0929867325666180117112610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Liu S.-H., Chuang W.-C., Lam W., Jiang Z., Cheng Y.-C. Safety Surveillance of Traditional Chinese Medicine: Current and Future. Drug Saf. 2015;38:117–128. doi: 10.1007/s40264-014-0250-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Ji M.-Y., Bo A., Yang M., Xu J.-F., Jiang L.-L., Zhou B.-C., Li M.-H. The Pharmacological Effects and Health Benefits of Platycodon grandiflorus—A Medicine Food Homology Species. Foods. 2020;9:142. doi: 10.3390/foods9020142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Chapel J.M., Ritchey M.D., Zhang D., Wang G. Prevalence and Medical Costs of Chronic Diseases Among Adult Medicaid Beneficiaries. Am. J. Prev. Med. 2017;53:S143–S154. doi: 10.1016/j.amepre.2017.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Cockerham W.C., Hamby B.W., Oates G.R. The Social Determinants of Chronic Disease. Am. J. Prev. Med. 2017;52:S5–S12. doi: 10.1016/j.amepre.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ising C., Stanley M., Holtzman D.M. Current thinking on the mechanistic basis of Alzheimer’s and implications for drug development. Clin. Pharm. 2015;98:469–471. doi: 10.1002/cpt.200. [DOI] [PubMed] [Google Scholar]
- 209.Liu E., Wang D., Sperling R., Salloway S., Fox N.C., Blennow K., Scheltens P., Schmidt M.E., Streffer J., Novak G., et al. Biomarker pattern of ARIA-E participants in phase 3 randomized clinical trials with bapineuzumab. Neurology. 2018;90:e877–e886. doi: 10.1212/WNL.0000000000005060. [DOI] [PubMed] [Google Scholar]
- 210.Hügel H.M. Brain Food for Alzheimer-Free Ageing: Focus on Herbal Medicines. Nat. Compd. Ther. Agents Amyloidogenic Dis. 2015;863:95–116. doi: 10.1007/978-3-319-18365-7_5. [DOI] [PubMed] [Google Scholar]
- 211.Pei H., Ma L., Cao Y., Wang F., Li Z., Liu N., Liu M., Wei Y., Li H. Traditional Chinese Medicine for Alzheimer’s Disease and Other Cognitive Impairment: A Review. Am. J. Chin. Med. 2020;48:487–511. doi: 10.1142/S0192415X20500251. [DOI] [PubMed] [Google Scholar]
- 212.Graziose R., Lila M.A., Raskin I. Merging Traditional Chinese Medicine with Modern Drug Discovery Technologies to Find Novel Drugs and Functional Foods. Curr. Drug Discov. Technol. 2010;7:2–12. doi: 10.2174/157016310791162767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Xu Q.-Q., Shan C.-S., Wang Y., Shi Y.-H., Zhang Q.-H., Zheng G.-Q. Chinese Herbal Medicine for Vascular Dementia: A Systematic Review and Meta-Analysis of High-Quality Randomized Controlled Trials. J. Alzheimer’s Dis. 2018;62:429–456. doi: 10.3233/JAD-170856. [DOI] [PubMed] [Google Scholar]
- 214.Sancesario G.M., Bernardini S. Alzheimer’s disease in the omics era. Clin. Biochem. 2018;59:9–16. doi: 10.1016/j.clinbiochem.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 215.Wilkins J.M., Trushina E. Application of Metabolomics in Alzheimer’s Disease. Front. Neurol. 2017;8:719. doi: 10.3389/fneur.2017.00719. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.