Abstract
Improved wound healing of burnt skin and skin lesions, as well as medical implants and replacement products, requires the support of synthetical matrices. Yet, producing synthetic biocompatible matrices that exhibit specialized flexibility, stability, and biodegradability is challenging. Synthetic chitin/chitosan matrices may provide the desired advantages for producing specialized grafts but must be modified to improve their properties. Synthetic chitin/chitosan hydrogel and aerogel techniques provide the advantages for improvement with a bioinspired view adapted from the natural molecular toolbox. To this end, animal genetics provide deep knowledge into which molecular key factors decisively influence the properties of natural chitin matrices. The genetically identified proteins and enzymes control chitin matrix assembly, architecture, and degradation. Combining synthetic chitin matrices with critical biological factors may point to the future direction with engineering materials of specific properties for biomedical applications such as burned skin or skin blistering and extensive lesions due to genetic diseases.
Keywords: wound healing, materials, skin substitutes, aerogel, chitin, chitosan, insect, drosophila, proteins, obst-A
1. Introduction
Biopolymers are polymers of natural origin and can be found in wood, plants and animals. Chitin is the second-most abundant, non-toxic natural biopolymer containing N-acetylglucosamines (GlcNAc) linked by β-1,4 glycosidic bonds from which chitosan can be derived by N-deacetylation [1,2]. Polysaccharide-based chitin/chitosan materials are increasingly used for future human-made products [3,4]. The reasons for this are manifold, since chitin/chitosan matrices can be flexible and, at the same time, very robust and scratch-resistant [5,6]. In addition, they exhibit different properties in their permeability to molecules [7]. Furthermore, they offer incredible possibilities from transparency to multiple color arrangements [5,6]. Finally, chitosan possesses antimicrobial, antioxidant, anticarcinogenic, and anti-inflammatory properties [8,9].
Natural chitin polymer chains are helices in which each sugar unit is inverted with respect to its neighbors. This leads to high stability as the rigid ribbons are connected to hydrogen bonds [10]. Linear chitin polysaccharides occur naturally in three crystalline allomorphs known as α-, β-, and γ-chitin. They contain different orientations of the microfibrils [2,11,12,13,14,15,16,17,18,19]. The chitin sheets arrange in layers that show antiparallel orientation in α-, and γ-chitin and parallel orientation in β-chitin [20]. This arrangement has consequences on chitin properties. The α-chitin has the strongest inter-sheet and intra-sheet hydrogen bonding. In contrast, the β-chitin has weak hydrogen bonding by intra-sheets and is characterized by a weak intermolecular force [21,22]. Chitin/chitosan can be extracted from various natural sources, such as crabs, lobsters, shellfish, algae, and fungi. However, access to a high amount of natural chitin/chitosan is limited since the most abundant sources are part of a global sea food market [23,24,25,26,27,28,29].
Insects are a terrestrial source since their cuticles and wings contain chitin/chitosan [30]. However, this requires the cultivation of a high number of adult or pupal animals. Another alternative source could be microbes. The cell walls of fungi contain pools of chitin/chitosan, but chitin/chitosan production is not yet scaled up to an industrial level [31]. However, chemical extraction processes from such natural sources involve using aggressive chemicals at high temperatures for extended periods, which can alter the properties of chitin/chitosan [32]. Recent studies show a more ecofriendly extraction of chitin/chitosan from natural sources by fermentation using lactic acid bacteria [33]. Their main chitosan/chitin degradation products are oligosaccharide/chitooligosaccharide (COS), which also possess remarkable biological and biomedical properties. COS has a low molecular weight (Mw), high degree of deacetylation (DD), high degree of polymerization (DP), low viscosity, and complete water solubility [34]. The genetic engineering of bacteria plays an essential role in chitin bioconversion to COS products, servings as a primer for synthesizing complex carbohydrates [35].
Given the different options for obtaining chitin/chitosan or their degradation products, the challenge remains to produce chitin/chitosan-derived matrix materials for target-specific biomedical usage. The synthetic production of chitin/chitosan matrices could be one elegant alternative (Section 5). To further improve the properties of these synthesized matrices for biomedical applications (Section 2 and Section 3), the addition of bioactive molecules and proteins that control the matrix architecture provides an exciting option (Section 4, Section 5, Section 6 and Section 7).
2. Chitin/Chitosan Matrices Provide the Potential for Multiple Biomedical Applications
Due to their high biocompatibility, chitin and chitosan have shown great potential for various uses in the medical field [36]. The positive charge of a chitin/chitosan-based matrix due to the protonation of amino groups is an essential property [37]. This increases the solubility of chitosan and usually occurs in acidic environments [38]. Because of the positive charge, chitosan can form complexes with numerous negatively charged molecules, such as growth factors, nucleic acids, and cytokines [39,40,41]. Thus, chitin/chitosan matrices recruit bioactive factors from the environment, protect their degradation and increase local efficacy [36]. In addition, protonated chitosan can interact with extracellular matrix components such as glycosaminoglycans and proteoglycans [38,41]. Furthermore, the possibility of enzymatic degradation of chitosan plays a decisive role. Lysozyme (muramidase) is present in mucous membranes of the human intestine and other mucosal epithelial cells. This enzyme separates the bonds between acetylated units and thus cleaves chitin/chitosan into oligosaccharides [42,43,44,45,46,47]. Moreover, combining chitin/chitosan matrices with other polymer materials such as gelatin or collagen may improve their mechanical and biological properties [7,48,49,50]. Finally, synthetically engineered chitin/chitosan-produced materials show biocompatible, biodegradable, and non-toxic properties.
Biopolymers show multifunctionality as beads, microparticles, nanoparticles, micelles, hydrogels, tablets, and capsules. Chitin-based biopolymers can be formed into nanogels, namely hydrogels confined to the nanoscopic range. Chitin nanogels possess valuable attributes, such as the ability to load drugs, a large surface area for bio-conjunction, size tunability, controlled release, and an excellent ability to respond to environmental stimuli [51,52,53]. Chitosan gels show bioavailability for drugs, enzymes, and proteins [54]. In summary, films, beads, fibers, intragastric floating tablets, microspheres, and chitin/chitosan nanoparticles and their derivatives have been formulated for use in the pharmaceutical field. Recent findings even support their potential for gene therapy applications [7,40,55,56,57,58,59,60,61,62,63].
Studies over the past decade showed that the biomedical advantages of synthetic chitin/chitosan matrices are dependent on cell type, location and time of treatment, and limitations of the matrix itself [64]. The molecular weight (MW), which is affected by proteinization and degree of deacetylation (DD), can influence the properties of the chitin/chitosan matrix, e.g., solubility, viscosity, and biological activity [64]. The potential for gene delivery by chitosan/siRNA nanoparticles was supported by high MW and DD in human lung carcinoma cells [65]. In contrast, lower MW and DD showed a better hypocholesterolemic effect than high MW and DD in rats [66]. Moreover, these and other data, including the possibility of binding growth factors required for wound healing and bone regeneration, indicate the potential of chitosan-based grafts and nanoparticles for delivery of drugs and oligonucleotides (siRNA, etc.) for other biomedical applications [52,64,67,68,69,70].
The subject of current research is the improvement of synthetic chitin/chitosan matrices for various biomedical applications: for instance, chitosan displays biocompatibility during dental pulp regeneration of immature dog teeth [71]; chitin-nanocomposites showed improved blood clotting ability [72]; chitosan-gels induce angiogenesis in rabbit models [73]; application of chitosan hydrogels accelerates dermal wound healing in rats [74]; and chitosan–fiber scaffolds support attachment and differentiation of human monocytes, which is a central requirement for successful bone tissue engineering [75]. Chitosan-blended bacterial cellulose (cellulose synthesized by Acetobacter xylinum) composite films provide potential applications, such as wound dressing, arterial vascular grafting, and delivery systems of drugs and proteins [76]. Moreover, depending on its molecular weight, chitosan shows proinflammatory properties affecting the migration of leukocytes and macrophages, which is essential for wound healing and tissue regeneration [77,78,79,80]. However, proinflammatory properties could cause allergic reactions and restrict biomedical use [64]. For example, chitosan (Heppe Medical Chitosan) affects the integrity of the nasal epithelium by reducing transepithelial electrical resistance through the degradation of the tight junction protein occludin. This intranasal application facilitates transepithelial allergen passage in the mouse model [81]. In contrast, well-known allergies against seafood crustaceans are likely caused by the muscle protein tropomyosin and, are therefore, unrelated to their chitin/chitosan [82]. Moreover, crab shell has been clinically used for many years as natural chitin matrix wound dressing graft material in Japan, without reported allergic incidents [64]. Furthermore, chitin films showed no allergenicity upon dressing wounds in rats [83]. There is no apparent effect of chitosan in terms of allergy or severe inflammation [9]. Collectively, chitin/chitosan matrices and composites are promising materials for active pharmaceutical and other bioactive agents needed for orthopedic and periodontal applications as well as for tissue engineering and wound healing [53,55].
3. Natural and Synthetic Chitin/Chitosan Matrices Support Wound Closure
A closer look at the biological function reveals interesting analogies between the multilayered epidermis of vertebrate skin and layers of the epidermal epithelium, with its overlaying lamellar chitin matrix, in insects [84]. The chitin matrix forms the central barrier at the insect cuticles [85], similar to the suprabasal cell layers of the human epidermis [84,86]. Loss of the chitin matrix and defective skin epidermis compromises the critical barrier function against dehydration and harmful environments. This can have devastating consequences for animals and humans. Atopic dermatitis is a broad term for many defects of the epidermis, such as epidermolysis bullosa simplex (EBS) or junctional epidermolysis bullosa (JEB). Patients suffer from chronically swollen and cracked skin areas with fragile barriers and devastating inflammations [86,87]. Healing of such large areas of skin is often not possible, taking months or longer, and requires enormous medical efforts in rare genetic diseases, including even gene therapy interventions. [87].
Chitin and chitosan have been shown to be useful as wound dressing materials. For example, the used inner chitinous membrane of soft crab shell carapaces showed advantages in wound healing [88]. Cells show the capacity to spread, proliferate, elongate and adhere to the used chitinous membrane, and in the rabbit model, it promoted faster epidermal wound closure. Enhanced cell adhesion could be the underlying molecular reason due to specific matrix surface structures. In addition, increased numbers of neutrophils and macrophage immune cells infiltrate the epidermis, and after two weeks, the chitinous membrane fell off without showing any side effects in the rabbit model [88]. In the mouse model, chitosan dressing of grafts directly promoted skin wound healing by affecting growth factor expression [89]. Macroscopic and histological analysis demonstrated the role of chitosan hydrogel in the treatment of dermal burns through the induction of full-thickness transcutaneous dermal wounds in Wistar rats [74]. Moreover, chitin gauze and spray revealed satisfactory healing of various traumatic wounds in humans [90]. Chitin/chitosan in artificial grafts taping such wounds could be used to re-establish skin architecture [74]. Adding bioactive molecules, such as antimicrobial agents and growth factors promotes skin cell growth, regeneration, and anti-inflammatory effects [91]. Thus, clinical models show that gels based on chitin nanofibrils accelerate the healing of wounds in humans. Their biochemical activities lead to activation of polymorphonuclear cells, fibroblast activation, cytokine production, migration of giant cells, and stimulation of type IV collagen synthesis. In addition, it prevents hypertrophic scarring and keloid scars [92]. Techniques of 3D printing, electrospinning, and aerogels with chitin/chitosan will improve the properties of wound materials [7,50]. Production of a very powerful chitin/chitosan matrix could be even suitable in cases where it could act as a long-lasting graft-like tissue forcing wound closure while also protecting as a barrier.
Skin grafting is essential for reconstructive surgery in patients with burns, trauma, and non-healing or large wounds. Wound healing comprises many aspects, namely cleansing, granulation/vascularization, and re-epithelialization. These depend on an optimal microenvironment and cytotoxic factors [93,94]. However, the main phases of wound healing, namely inflammation, new tissue formation, and remodeling, are all affected by mechanical forces. Indeed, mechanotransduction is a potential target of excessive scar formation, a significant clinical and financial burden, and requires improved therapies to reduce scarring [95]. Thus, mechanical offloading can provide access to minimize scar formation and advance adult wound healing. To meet the specific and individual medical requirements, the production of a synthetic chitin matrix with defined mechanical properties will be a future challenge. Therefore, we focus on a concept combining chemical and molecular biology tools to develop a new perspective for generating improved materials.
4. Using the Natural Toolbox to Improve the Quality of Synthetic Chitin/Chitosan Matrices
Polysaccharide-based aerogels are porous materials with a net-like nanostructure. Aerogels exhibits high porosity, low density, thermal conductivity and large surface area. In addition, they are ultra-lightweight, have high water absorption capacity, excellent shock-absorbing properties, and are flame and moisture resistant. Overall, these multiple special properties make them suitable for numerous applications in the medical, pharmaceutical, and cosmetic sectors, among others [4,96]. The promising use of natural and synthetic aerogels for fluid management, healing, and regeneration of wounds led to the increasing trend of articles published in recent years [4,96,97,98]. Many promising examples provide evidence for the multiple usage of synthetic chitin/chitosan-based matrices, such as chitosan hydrogels, films, porous scaffolds, textile fibers, and others, and the capacity to optimize their functionality and bioactivity as biomedical materials [73,74,75,99,100,101]. The numerous synthetic chitosan-based scaffolds used to promote wound healing were recently summarized [7]. Chitin/chitosan-aerogels show advanced properties, such as inhibiting the Staphylococcus aureus growth, a widespread cutaneous pathogen responsible for the great majority of bacterial skin infections in humans [102,103]. Moreover, the aerogel technique provides powerful tools for technical modifications, such as blending, crosslinking, and modifying microstructural and physical properties to produce chitin/chitosan matrices (see Section 5).
Hou and colleagues state in their recent opinion that for the future’s advanced technologies, chitin will ultimately drive many innovations and alternatives using biomimicry in materials science [6]. Indeed, natural chitin/chitosan matrices form incredibly different properties, depending on the location and developmental timing at which animals need them [104,105]. For example, natural chitin/chitosan matrices form the outermost body barrier or cell wall, protecting organisms, shaping their organs, or even serving as tight claws or teeth [106,107]. They even cover soft wings or form the transparent layer of compound eyes of insects [108]. Moreover, thinking about the beauty of butterflies, chitin offers a unique color palette that is durable and responsive. The coherent scattering in the periodic arrays of multilayered chitin/chitosan matrix structures creates countless color combinations [6]. Recent investigations of different biological disciplines concluded that the high performance of natural chitin matrices relies on their specialized structures, the perfect packaging of the chitin/chitosan chains into long fibers that must assemble into complex architectures [109]. A key role lies in the molecular mechanisms, namely the genes coding for the key proteins and enzymes that establish natural chitin matrices, mature them, and degrade them without preventing newly formed matrices from keeping epithelial barriers [110,111,112].
In our view, the numerous variations of chitin matrix architecture in insects suggest a bioinspired view of the natural molecular toolbox (see Section 6). Synthetic chitin matrix scaffolds such as aerogels can be improved and adapted to the specific medical application of wound healing by adding proteins that determine the matrix architecture and thus reducing tensile stress, improving wetting and impermeability to pathogens and toxins. The improved materials could then enable more efficient wound healing with as little scarring as possible.
5. Production of Polysaccharide-Based Chitin/Chitosan Aerogel Matrices
5.1. Engineering Synthetic Chitin/Chitosan Matrices
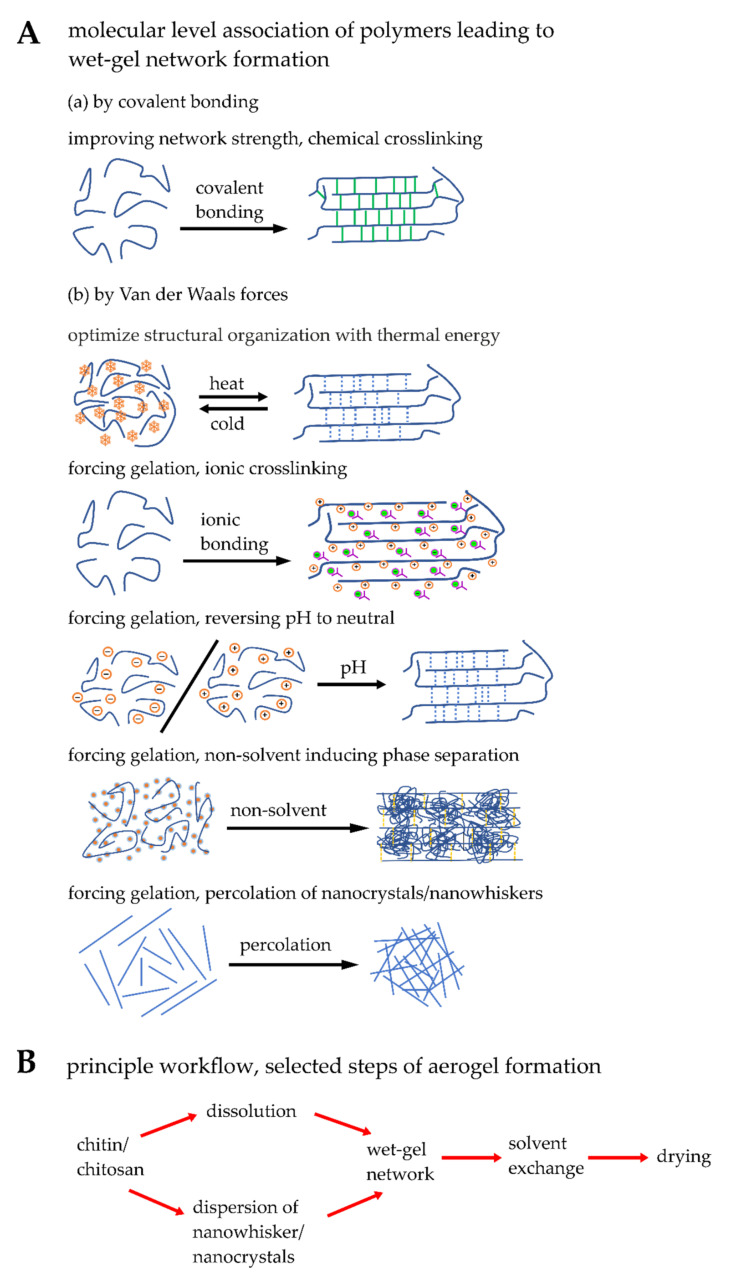
The optimization of synthetic matrices for biomedical applications is a demanding challenge. Nature’s highly hierarchical architecture of chitin matrices could be a significant obstacle for engineering synthetic materials. However, generating a synthetic material based on the inspiration of biological chitin/chitosan matrices with structural and functional properties is challenging. Therefore, as a prerequisite for developing future bioinspired materials with synergistic properties of the chitin/chitosan peptide matrix system, various materials still need to be explored. Various methods of wet-gel matrix formations are listed in Table 1.
Table 1.
Advantages and disadvantage of wet-gel network formation methods.
| Matrix Formation | Bonding | Advantage | Disadvantage |
|---|---|---|---|
| Chemical crosslinking | Covalent bonding | Improving network strength results in rigid matrix formation providing high mechanical strength | May become brittle |
| Thermal energy | Van der Waals force | Reversible in wet-gel matrix formation | Gel transition temperature may be very high (>40 °C) or it is controlled by additives |
| Ionic crosslinking | Van der Waals force | Strong interaction with biological medium; advantage of using the ionic matrix as carrier; buffering at biological medium | High volume shrinkage while supercritically dried aerogel formation |
| Reversing pH of medium | Van der Waals force | Most employed economic path and easy to handle; possible to functionalize with sensitive biological molecules in neutralized post wet-gel matrix | Inappropriate for functionalizing the chitin/chitosan molecules with sensitive biological molecules |
| Non-solvent induced phase separation | Van der Waals force | Macropore channels are formed | Non-aqueous medium was used as non-solvent |
| Percolation | Van der Waals force | Highly crystalline wet-gel matrix is generated | Precursors should be produced in situ; should be stored or transported with high care and caution; not forming wet-gel matrix |
Engineering randomly connected fiber matrices of chitin/chitosan into various dimensions can be achieved in laboratories by inducing either the self-assembly of the molecular chains or percolated network formation of nanowhiskers/nanofibrils. Van der Waals physical bonding or covalent binding between molecular chains is significant for forming matrices. There is a series of actions happening in the wet state-forming higher-order structures of chitin/chitosan matrices: (a) association of molecular chains in a fashion producing the smallest building blocks called nanofibers; (b) formation of a randomly interconnected three-dimensional network in a small domain; (c) finally the complete formation of pure matrices of chitin/chitosan filled with liquid. The following parameters are the actors controlling molecular chains from their solute state to the fibrillar network: temperature, pH, chemical crosslinking, and a non-solvent approach [113,114,115].
5.2. Blending, Physical and Chemical Crosslinking of Chitin/Chitosan Matrices
Recent reports show modifications of chitin/chitosan matrices with desired peptide/protein molecules [116,117]. Chitin/chitosan-bound peptide/protein matrices were developed by blending the molecular chains or inducing the physical (Van der Waals forces) or chemical crosslinking between the molecules. Compared with chitin, chitosan can be used for synthesizing bound chitosan-peptide/protein matrices because of abundant deacetylated amine functional groups. The amine functional groups of chitosan can be activated for blending or physical crosslinking by protonation. Physical crosslinking, such as through Van der Waals force interaction, occurs between chitin/chitosan and protein, forming polyelectrolyte complexes [72,118,119,120,121,122]. Cost-effective methods have been reported to produce polyelectrolyte complexes as dried membranes [119] or scaffold materials (by freeze-drying) [118] by blending chitosan with silk fibroin. In this case, dried membranes and scaffold materials of blended polyelectrolytes have not displayed nanofibrillated gel networks. However, the blended materials have exhibited efficient wound healing properties [119], enhanced biological activity, and suitability as supporting materials for tissue engineering [120].
Compared with physically bound gel matrices, chemical binding between chitosan and peptide/protein provides high stability and enhanced mechanical properties. In general, the chemical crosslinking reactions are carried out, forming covalent bonds between chitosan and peptide/protein molecule by either coupling with an anchoring spacer group/crosslinker between them or eliminating the water molecules by amidation [123,124,125,126,127,128,129]. In this case, a robust three-dimensional hydrogel network can be achieved, mimicking the extracellular matrix, promoting the adhesive property of cells and biological functions. As the crosslinkers do not play any vital role in the desired biological function, the crosslinker should be a non-toxic reagent. In recent reports, a nature-based crosslinking agent, genipin, was used to produce chitosan–protein hydrogel [124,130,131]. In the case of chitosan–collagen–hyaluronic acid, after increasing the crosslinking concentration by genipin, the cell spreading capacity was improved although the water uptake capacity of hydrogels was reduced [124].
No crosslinkers are necessary when chitosan can be directly bound with peptide/protein by amidation [126,132]. The most employed reagents for the amidation reaction are N-hydroxysuccinimide or derivatives of it (activating the amine groups of chitosan and carboxylate groups of peptide/proteins) and water-soluble carbodiimides (scavenging the water molecules turned to be urea derivatives). The covalent crosslinking of carboxymethyl chitosan with collagen peptides using water-soluble carbodiimide (1-(3-dimethylaminopropyl)-3-ethylcarbodiimide hydrochloride) and N-hyydroxysuccinimide was recently shown [132]. Further purification of hydrogels is essential to use the matrices for biological applications. The workflow and methods for preparing chitin/chitosan-aerogels are summarized in Figure 1
Figure 1.
Schematic drawing presenting selected steps of a workflow of chitin/chitosan-aerogel production. (A) Network formation methods at the molecular level either by covalent bonding or by Van der Waals forces, mainly hydrogen bonding. (B) A general principle workflow of aerogel synthesis includes several steps: network-formation, solvent exchange, and drying. For more details, see [54,114,133].
5.3. Modifying Microstructural and Physical Properties of Synthetic Matrices
The morphology and topography of the chitin/chitosan matrices receive close attention in designing the wound dressing materials. When ambient drying or vacuum-drying the wet-gel matrices of chitin/chitosan materials, the existing surface tension between solid, liquid, and gas can pull the nanostructures together. At the same time, the fluid becomes a gas, which destroys the natural structure [134]. Therefore, it results in more than 90% of volume shrinkage. These materials are named xerogels [135]. The complete collapse of pores can be confirmed by nitrogen adsorption-desorption analyses, mostly showing no considerable values if the solvent medium in the matrix is water or ethanol [135,136]. The methods for preserving pores employed in the laboratories are freeze-drying (sublimation of frozen water to gas) and supercritical drying (solvent exchange of solvent with supercritical gas [134,136]. They fabricate highly porous materials as the fluid in the wet-gel nanostructures of chitin/chitosan can be replaced with air [54].
In the freeze-drying technique, the natural gel nanostructures are destroyed due to Vander Waals interactions, promoting significant aggregation of nanofibers. As a result, the specific surface area becomes low (<110 m2/g) [136]. However, due to the frozen water molecules (ice crystals), the pores generated by sublimation can display the material as being highly porous. These foam-like materials are named cryogels [134,136]. In some reports, it was demonstrated that use of tert-butyl alcohol instead of water in the gel matrix could prevent structural damage [137]. Due to the low surface tension and high freezing point of tert-butyl alcohol compared to water, freeze-drying reduces the capillary forces between the solvent and the gel matrix and maintains the three-dimensional network structure [137].
Supercritical drying can be employed in which the fluid in the gel matrix is converted to gas in its supercritical state [134]. No existence of surface tension favors preserving the microstructure of the gel matrices. In supercritical drying, an environment-friendly supercritical gas such as carbon dioxide is employed. In this drying process, the fluid in the gel matrix is switched to a suitable solvent such as simple alcohol (e.g., ethanol), which has good miscibility with CO2. Then the alcohol in the gel matrix is saturated with CO2 under supercritical conditions (>31 °C and >73.8 bar) in an autoclave [134].
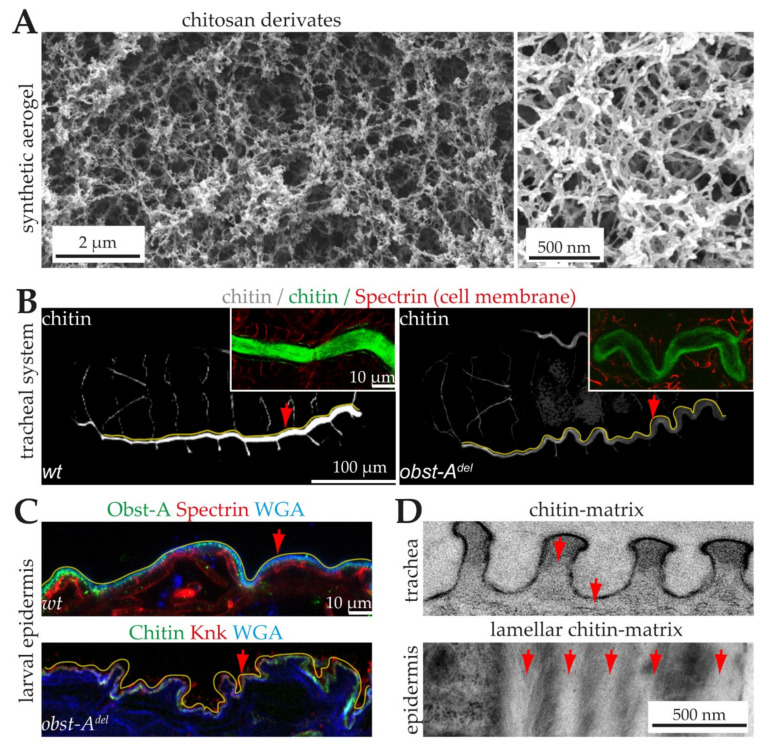
Finally, supercritical carbon dioxide gas is degassed at above 40 °C, and the matrix is filled with air [134]. Approximately 5–40% of volume shrinkage can be observed in this process depending upon the matrix’s mechanical strength and physical properties. For instance, examples of aerogel of chitosan derivate which was dried under supercritical conditions, are shown in Figure 2A [133]. As a result, an open porous structure of the chitin/chitosan matrix can be achieved with properties close to the reality in the hydrogel or wet-gel media [54].
Figure 2.
Synthetic and genetically controlled chitin matrices. (A) Scanning electron microscopy images of aerogel chitosan derivates [133]. Scale bars indicate 2 µm (left) and 0.5 µm (right). (B) 3D-projections of confocal Z-stacks of whole-mount immunostainings showing chitin (green) in late Drosophila embryos. Anterior is left, dorsal is up. An Alexa488-linked chitin-binding probe (green) detects chitin in the tracheal tube lumen. The main tracheal tube (marked by yellow lines) is straight and stable (arrow, left image) in wt but over-elongated and unstable with sinusoidal buckling (arrow, right image) in obstructor (obst)-A null mutants. Inlay, wt embryo shows a bright chitin staining (green) in the tracheal tubes, while the obst-A null mutant embryo contains only weak chitin staining (green), indicating unusual premature degradation of the matrix. The α-Spectrin antibody marks the tracheal cell membranes (red). Scale bars indicate 10 µm (inlay) or 100 µm. (C) Confocal images of ultrathin epidermal sections of larval immunostainings. The wt epidermis (upper image) contains a tight cuticle (indicated by the yellow line) that shapes the straight appearance of the epidermis (arrow) of the animal. In obst-A mutants (lower image), the epidermal chitin matrix (yellow line) lost its stability and integrity, resulting in a fragile, wrinkled epidermis (arrow) with partial lesions between cells and cuticle. The Obst-A and Knickkopf antibodies detect the chitin matrix. The Alexa633 conjugated wheat germ agglutinin (WGA, in blue) is a lectin that marks chitin and membranes. Scale bar indicates 10 µm. (D) Transmission electron microscopy images reveal the soft non-lamellar (upper image, arrows), tracheal and tight lamellar (lower image, arrows point to chitin-lamellae) epidermal chitin matrices. Images were provided by Dr. Dietmar Riedel (Electron Microscopy Group, Max-Planck-Institute for Biophysical Chemistry). Note the fine twisted plywood-like structure of lamellar chitin-protein planes in the epidermis. Red lines indicate epidermal cell surfaces. Scale bar indicates 0.5 µm.
There are huge morphological differences between ambient dried, freeze-dried, and supercritically dried materials [136]. Xerogels, cryogels, and aerogels do not show similar interactive properties with the wound surface. For instance, Guo et al. demonstrated in the recent report that the morphology of aerogels of chitin promoted the healing process, accelerated macrophage migration, enhanced fibroblast proliferation, induced collagen deposition, and promoted granulation and vascularization in comparison with cryogels. Moreover, after 11 days of the wound healing process, the scar area appeared reduced and was significantly smaller in the case of aerogels than cryogels. [138].
In the last decades, the dry membrane, scaffolds, fibers, and hydrogels of chitin/chitosan in wound healing applications have been explored, and their mechanisms have been analyzed in vitro and in vivo [55,80,139,140,141,142]. Nevertheless, the finely distributed nanostructures and open porous network of aerogels of chitin and chitosan will be a new class of porous materials for this field of application (examples are listed in Table 2). The aerogels of chitin/chitosan functionalized with protein/peptides are promising candidates for wound healing applications. The materials possess specific surface area, high sorption capacity, biocompatibility, antimicrobial property, interactive surface functionalities, and a structural similarity to the skin’s extracellular matrix [4,138].
Table 2.
Examples for non-protein/peptide-based chitin/chitosan aerogel matrices, reporting good biocompatibility after in vitro tests and high water absorption capacity.
| Aerogels | Crosslinked/Blended with Additives | Observed in Biomedicine Application |
|---|---|---|
| Chitosan | Crosslinked with diatom-biosilica by in situ polymerization of dopamine (Michael-type cycloaddition) [137] | Improved hemostatic performance. |
| No additives [143] | Improved hemostatic performance | |
| Blended with alginate producing polyelectrolyte complex [144] | Efficient antibacterial activity (Staphylococcus aureus and Klebsiella pneumoniae) and effective wound closure | |
| Crosslinked with itaconic acid using epichlorohydrin [145] | Efficient antibacterial activity (Corynebacterium glutamicum and Escherichia coli) | |
| Vancomycin, drug-loaded chitosan aerogel [97] | Efficient antibacterial activity (Staphylococcus aureus) and drug release kinetics | |
| Cellulose nanofibers dry-crosslinked in the chitosan matrix [146] | Shape recoverable foam material under wet conditions showing improved hemostatic performance | |
| Chitin | No additives, electrophoretic deposition of chitin nanoparticles [138] | Accelerate wound healing and reduce scar area in comparison with cryogels |
6. The Molecular Toolbox for Natural Chitin Matrix Production
The already nature-like aerogel matrix provides an optimal synthetic basis for implementing a bioinspired version. To go even further, the biological knowledge of how natural matrices can take on different structures and their associated properties will be very useful. Chitin-based matrices are the most prominent part of the arthropod cuticles [147,148]. The chitin matrix has two main functions: it forms an exoskeleton that shapes the organs/animals, and it protects the organs from various stresses, such as mechanical impact, invading pathogens, toxins, and desiccation at high temperatures [84,149,150,151]. Arthropod cuticles repeatedly molt during the transition of larval/nymph stages to fit their increasing body size, which is under systematic hormonal control [148,152,153,154,155,156].
6.1. The Architecture of Cuticular Chitin Matrices
In arthropod cuticles, including insects, antiparallel arranged α-chitin chains are most abundant [157]. About 18 to 25 chitin chains assemble into nanofibrils (~3 nm diameter; ~0.3 µm length) [158]. Chain assembly ultimately requires proteins to encase the nascent nanofibrils. At the next hierarchical level, the nanofibrils assemble into long chitin-protein fibers arranged in horizontal planes. Nanofiber stacks form a plywood structure, which is a prominent part of many cuticles [110,147,159]. The hierarchic arrangement, the stiffness, strength, fracture toughness, and the working fracture of insect chitin matrices have been discussed previously [110,160,161,162,163,164].
6.2. Natural Chitin Production
The common feature of epithelial cells is their apical-basal polarity, with the apical cell side facing outward (epidermis) or into the lumen of tubular organs. Located in the apical membrane, chitin synthases (CHS) synthesize the chitin chains [1,165]. The latter can form initial chitin fibrils in a self-assembly process [111]. Dynamic apical cell surface structures (microvilli) can determine the boundary conditions for chitin-fiber self-assembly [112]. However, the synthesis and initial self-assembly of chitin polymers are not enough to form chitin matrices with defined architecture and properties.
6.3. Proteins Control Proper Chitin Matrix Formation
Importantly, the volume fraction of the constituents of the chitin–protein fibers significantly influences the matrix performance [166]. For example, the epidermal chitinous-matrix is relatively stiff, very dense, and robust against diverse stresses [84,85,167]. This requires strong chitinization with a lamellar, multilayer chitin matrix arrangement (Figure 2B–D) [85,105,168]. In contrast, the chitin matrices of tubular organs are relatively soft and only single-layered [164]. Examples include the respiratory tracheal system and the digestive system [169,170,171,172,173,174,175,176]. The tracheal and foregut chitin matrix must seal tube lumina for specific transport processes while being flexible [177,178,179,180]. The peritrophic matrix surrounding the midgut food is a chitin matrix that needs to be selectively permeable for nutritional uptake [180]. In all cases, chitin chains are embedded in a protein matrix [147,159,180,181]. Those proteins control the formation of the above-described rigid/stiff and also flexible chitin matrices, and are therefore fundamental for controlling chitinous cuticle functions (Figure 2B,C) [180,182,183,184,185,186,187,188].
Insects possess a large number of cuticle proteins that contain chitin-binding domains and belong to different families [189,190,191,192,193]. Proteins with one or three chitin-binding domains (CBD) are members of the CPAP1 or CPAP3 family (Cuticle Proteins Analogous to Peritrophis) [194,195,196,197,198]. Those with a Rebers and Riddiford (R&R) chitin-binding sequence belong to the CPR family [192,193,195,196]. However, only a small number of the numerous chitin-binding proteins are critical for matrix formation (summarized in [111]). They mainly determine physiochemical properties such as the viscoelasticity and permeability of matrices. For example, loss of Tribolium CPR18 and CPR27 results in wrinkled elytra [199], and CPAP-1C, -H, -J knockdown showed fragile chitin matrix and structural integrity effects [194]. The CPAP-analogous Drosophila genes were identified as the obstructor (obst) gene family, consisting of 10 members, each with three chitin-binding domains [200]. Null mutant studies of three members, Obstructor (Obst)-A, Obst-C, and Obst-E, confirmed their vital and critical functions in assembling chitin matrices during insect development [198,201,202]. The mutant studies further prove that the chitin matrix assembly and packaging into higher-ordered structures are prerequisites for cuticle stability, tightness, protecting function, and insect survival [183,202].
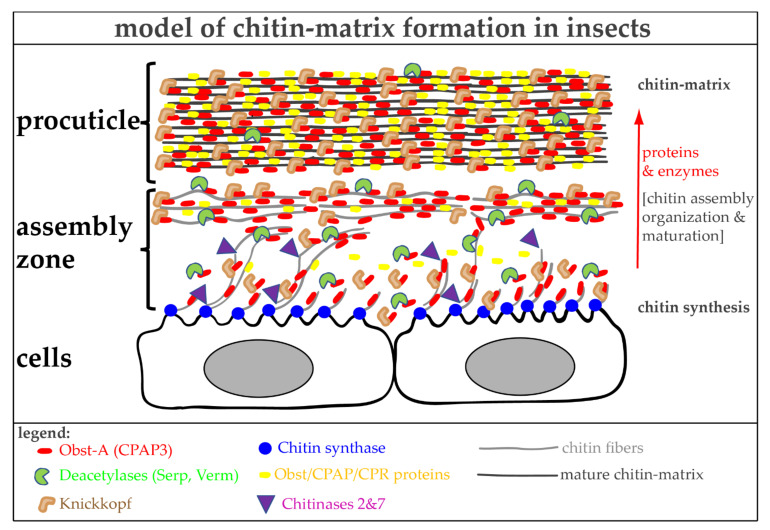
At the molecular level, Obst-A binds chitin and provides a scaffold that embeds chitin chains/fibrils. In addition, Obst-A localizes the chitin deacetylases Serpentine (Serp) and Vermiform (Verm) within the scaffold, enabling optimal chitin/chitosan matrix maturation. Chitin deacetylases catalyze the removal of acetyl groups from chitinous substrates and play critical roles in shaping the chitin matrices of cuticles in Drosophila [174,175,203] and other insects [204,205,206,207,208]. To further package and protect the chitin matrix, Obst-a recruits Knickkopf [183,202]. Knickkopf (German term for buckling head) protects newly synthesized chitin fibers from chitinases and organizes fibers into thicker and longer bundles that can stack into horizontal lamellae [182,209,210]. The Obst-A, Serp, Verm, and Knickkopf proteins represent a molecular core complex unit that acts as a hub for chitin matrix assembly, packaging, and protection (Figure 3). This protein complex mainly acts at the apical cell surface in the so-called cuticle assembly zone. Accordingly, proteins and enzymes enrich apically at the cell surface within the cuticle assembly zone. Therefore, these hub proteins offer an exciting starting point for improving synthetic chitin matrices to achieve modifications and setups of highly complex structures with defined properties.
Figure 3.
Genetic control of chitin matrix formation in Drosophila melanogaster. The chitin-binding protein Obst-A (CPAP3-A) operates as a hub for chitin matrix formation. Within the assembly zone, Obst-A recruits chitin to a scaffold where it places chitin deacetylases (Serp and Verm) and Knickkopf for chitin matrix assembly and maturation into nanofibrils and the subsequent accumulation into compact fibers of the chitinous procuticle. Obst/CPAP family members act synergistically in this process. The genes and their discussed products, the hub of chitin matrix formation, are evolutionarily conserved among arthropods, indicating their general necessity for cuticle biology.
Chitinases (Chts) belong to the large glycosylhydrolase family 18, widespread in the animal kingdom [211,212]. Usually, they are known to degrade chitin matrices by hydrolyzing chitin chains into smaller oligosaccharides. However, it remained unclear why insects possess numerous chitinase genes. Genetic studies uncovered a set of core chitinases (Cht2, Cht5, Cht7, Cht12) that degrade tight lamellar and soft non-lamellar chitin matrices. They contain various features, including (multiple) catalytical domains, transmembrane or chitin-binding domains that guarantee substrate specificity [85,164,213]. In contrast, Drosophila Cht2 and Tribolium Cht7 are also required for chitin matrix assembly [164,214,215]. Both influence chitin chain assembly into higher structures by potentially limiting the increasing lengths of nascent chains and resulting fibers (Figure 3). Whether Cht2 and Cht7 belong to the hub of chitin matrix formation remains elusive.
7. Advantages and Limitations of Chitin/Chitosan-Protein Materials
The development of biomedical materials is challenging. These materials require surfaces that enhance cell attachment and maturation [73]. Therefore, using chitin-binding proteins and enzymes, such as deacetylases, that control the surface architecture of natural chitin matrices could be an attractive new option to improve synthetic chitin/chitosan-based aerogel materials. However, despite all the confidence in coupling proteins to produce synthetic chitin/chitosan–protein matrices, some technical limitations must be considered. First, proteins are more than just large peptides and long chains of amino acids. Proteins are polymers that must fold into and retain their native three-dimensional structure to be bioactive during and, if desired, after production. Thus, and second, synthetic production or in vitro expression systems must allow the isolation of natively folded proteins. Third, the expression systems must modify proteins post-translationally, e.g., to carry out phosphorylation and glycosylation. These properties are achievable using the well-established insect cell expression systems and the baculoviral technique [216]. Fourth, exposure to harsh solvents must be avoided during engineering steps, as they could damage protein bioactivity. Fifth, the optimized ratio of proteins to each other and the chitin/chitosan molecules is uncertain and needs to be clarified.
When coupling high molecular weight protein with chitin/chitosan nanofibers, retaining protein physical and structural properties is critical for biological applications. It is possible to surpass it with small proteins or peptide molecules (oligo-/polypeptides), which enhance the interaction of biological molecules with artificial chitin/chitosan matrices. However, most cuticle proteins are not high-molecular-mass proteins (e.g., MW > 100 kDa) but are much smaller, as is the case for Obst-A (237 amino acids; 27 kDa), and are therefore likely to be easier to handle. Alternatively, instead of coupling the full-length Obst-A protein, its critical chitin-binding domains, which are evolutionarily well-conserved, could be used. Obst-A contains three short chitin-binding domains (57/59/67 amino acids), each of which binds in vivo and in vitro to colloidal chitin (unpublished results MB). The coupling of these domains, either as single or multiple domains, could alter the surface properties of porous chitin/chitosan materials. Concerning the material’s cleanliness, quality, physical and structural properties, the synthesis of artificial material will be limited to the aqueous medium.
The initial interactions are determined by the surface energy, chemical composition, stiffness, structure, and topography of the biomaterial surface in contact with the biological environment [73]. Hydrophobic or charged surfaces of the materials attract bioactive molecules. Such bioactive molecules are human extracellular matrix proteins, growth factors, short bioactive peptides, and synthetic chemicals, which specify the materials for the requested biomedical application. The addition of these bioactive molecules could further improve chitin/chitosan materials [73]. Additionally, it is possible to combine these techniques, but this requires many steps, which could be disadvantageous.
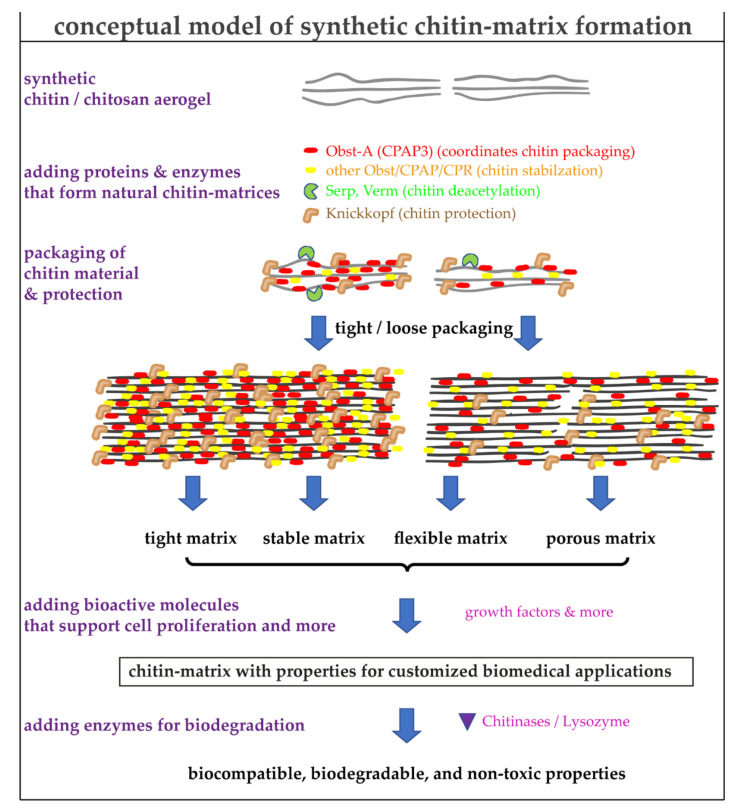
Importantly, aerogels are excellent materials to entrap, reinforce, or even interact with proteins, drugs, or bioactive material, making them a fascinating biomedical product [4,138]. Therefore, the potential of the interaction of chitin controlling proteins that modulate aerogels is one essential thesis of our final conceptual model (Figure 4).
Figure 4.
A conceptual model for the usage of critical proteins that control properties of synthetic chitin matrices. The known functions of the proteins are indicated. The combination of synthetic chitin-based aerogels with proteins controlling the chitin packaging and additional bioactive molecules (discussed in the text) will significantly improve and adjust the properties of the materials for customized biomedical applications. The eco-friendly biodegradability is an additional advantage of these new materials.
8. Conclusions
The skin is our largest organ and is vital for our survival. However, wound healing of large areas of skin is very problematic, takes very long periods, and requires enormous efforts, or even gene therapy interventions in rare genetic diseases. With the increasing knowledge of chitin/chitosan science regarding structural and functional designs for biological application, customized chitin/chitosan matrices could be generated. The molecular control of the architecture of chitin matrices is a key to specialized functions [110,217]. In insects, a small set of chitin matrix core complex unit proteins controls chitin matrix properties precisely [85,164,182,183,186,204,205,209,215,218]. Thus, we are pursuing a strategy of tailoring synthetic chitin/chitosan molecules at the molecular level with peptide/protein molecules that may be transferred to stable matrices through molecular assembly processes and the formation of nanofibrillar structures. Exploring individual matrix concepts such as bioinspired chitin/protein matrices will show us new ways to shift the paradigm from purely curative medicine to preventive medicine, from a one-size-fits-all approach to personalized therapies (Figure 4).
Acknowledgments
The authors thank Yanina-Yasmin Pesch, Christian Wolf, Dietmar Riedel, Lena Behr and members of our laboratories for critical reading. M.B. wants to thank Dietmar Riedel for sharing TEM images. The authors apologize to all colleagues whose contributions were not mentioned in this manuscript. We acknowledge support from Leipzig University for Open Access Publishing. M.B. appreciates the University Leipzig BioImaging Core facility (BCF equipment INST 268/230-1; INST 268/293-1; SFB-TR67; EFRE 100192650, 100195814, 100144684) for assistance.
Author Contributions
Conceptualization, M.B. and K.G.; writing—original draft preparation—review and editing, M.B. and K.G. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by Leipzig University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Merzendorfer H. The cellular basis of chitin synthesis in fungi and insects: Common principles and differences. Eur. J. Cell Biol. 2011;90:759–769. doi: 10.1016/j.ejcb.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 2.Lodhi G., Kim Y.-S., Hwang J.-W., Kim S.-K., Jeon Y.-J., Je J.-Y., Ahn C.-B., Moon S.-H., Jeon B.-T., Park P.-J. Chitooli-gosaccharide and its derivatives: Preparation and biological applications. BioMed Res. Int. 2014;2014:654913. doi: 10.1155/2014/654913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wegst U.G., Bai H., Saiz E., Tomsia A.P., Ritchie R.O. Bioinspired structural materials. Nat. Mater. 2015;14:23–36. doi: 10.1038/nmat4089. [DOI] [PubMed] [Google Scholar]
- 4.Bernardes B.G., Del Gaudio P., Alves P., Costa R., García-Gonzaléz C.A., Oliveira A.L. Bioaerogels: Promising nanostructured materials in fluid management, healing and regeneration of wounds. Molecules. 2021;26:3834. doi: 10.3390/molecules26133834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hong M.-S., Choi G.-M., Kim J., Jang J., Choi B., Kim J.-K., Jeong S., Leem S., Kwon H.-Y., Hwang H.-B., et al. Biomimetic chitin–silk hybrids: An optically transparent structural platform for wearable devices and advanced electronics. Adv. Funct. Mater. 2018;28:1705480. doi: 10.1002/adfm.201705480. [DOI] [Google Scholar]
- 6.Hou J., Aydemir B.E., Dumanli A.G. Understanding the structural diversity of chitins as a versatile biomaterial. Phil. Trans. R. Soc. A. 2021;379:20200331. doi: 10.1098/rsta.2020.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merzendorfer H., Cohen E. Chitin/Chitosan: Versatile Ecological, Industrial, and Biomedical Applications. In: Cohen E., Merzendorfer H., editors. Extracellular Sugar-Based Biopolymers Matrices. Springer International Publishing; Cham, Switzerland: 2019. pp. 541–624. [Google Scholar]
- 8.Matica M.A., Aachmann F.L., Tøndervik A., Sletta H., Ostafe V. Chitosan as a wound dressing starting material: Antimicrobial properties and mode of action. Int. J. Mol. Sci. 2019;20:5889. doi: 10.3390/ijms20235889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muzzarelli R.A.A. Chitins and chitosans as immunoadjuvants and non-allergenic drug carriers. Mar. Drugs. 2010;8:292–312. doi: 10.3390/md8020292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elieh-Ali-Komi D., Hamblin M.R. Chitin and Chitosan: Production and application of versatile biomedical nanomaterials. Int. J. Adv. Res. 2016;4:411–427. [PMC free article] [PubMed] [Google Scholar]
- 11.Rudall K.M. Advances in Insect Physiology. Elsevier; Amsterdam, The Netherlands: 1963. The Chitin/Protein complexes of insect cuticles; pp. 257–313. [Google Scholar]
- 12.Focher B., Naggi A., Torri G., Cosani A., Terbojevich M. Structural differences between chitin polymorphs and their pre-cipitates from solutions—Evidence from CP-MAS 13C-NMR, FT-IR and FT-Raman spectroscopy. Carbohydr. Polym. 1992;17:97–102. doi: 10.1016/0144-8617(92)90101-U. [DOI] [Google Scholar]
- 13.Kameda T., Miyazawa M., Ono H., Yoshida M. Hydrogen bonding structure and stability of alpha-chitin studied by 13C solid-state NMR. Macromol. Biosci. 2005;5:103–106. doi: 10.1002/mabi.200400142. [DOI] [PubMed] [Google Scholar]
- 14.Zhang M., Haga A., Sekiguchi H., Hirano S. Structure of insect chitin isolated from beetle larva cuticle and silkworm (Bombyx mori) pupa exuvia. Int. J. Biol. Macromol. 2000;27:99–105. doi: 10.1016/S0141-8130(99)00123-3. [DOI] [PubMed] [Google Scholar]
- 15.Minke R., Blackwell J. The structure of α-chitin. J. Mol. Biol. 1978;120:167–181. doi: 10.1016/0022-2836(78)90063-3. [DOI] [PubMed] [Google Scholar]
- 16.Kaya M., Mujtaba M., Ehrlich H., Salaberria A.M., Baran T., Amemiya C.T., Galli R., Akyuz L., Sargin I., Labidi J. On chemistry of γ-chitin. Carbohydr. Polym. 2017;176:177–186. doi: 10.1016/j.carbpol.2017.08.076. [DOI] [PubMed] [Google Scholar]
- 17.Carlström D. The crystal structure of alpha-chitin (poly-N-acetyl-D-glucosamine) J. Biophys. Biochem. Cytol. 1957;3:669–683. doi: 10.1083/jcb.3.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hackman R.H., Goldberg M. Studies on chitin. VI. The nature of alpha- and beta-chitins. Aust. J. Biol. Sci. 1965;18:935–946. doi: 10.1071/BI9650935. [DOI] [PubMed] [Google Scholar]
- 19.Blackwell J. Structure of beta-chitin or parallel chain systems of poly-beta-(1-4)-N-acetyl-D-glucosamine. Biopolymers. 1969;7:281–298. doi: 10.1002/bip.1969.360070302. [DOI] [PubMed] [Google Scholar]
- 20.Sugiyama J., Boisset C., Hashimoto M., Watanabe T. Molecular directionality of beta-chitin biosynthesis. J. Mol. Biol. 1999;286:247–255. doi: 10.1006/jmbi.1998.2458. [DOI] [PubMed] [Google Scholar]
- 21.Jang M.-K., Kong B.-G., Jeong Y.-I., Lee C.H., Nah J.-W. Physicochemical characterization of α-chitin, β-chitin, and γ-chitinseparated from natural resources. J. Polym. Sci. A Polym. Chem. 2004;42:3423–3432. doi: 10.1002/pola.20176. [DOI] [Google Scholar]
- 22.Rudall K.M., Kenchington W. The chitin system. Biol. Rev. 1973;48:597–633. doi: 10.1111/j.1469-185X.1973.tb01570.x. [DOI] [Google Scholar]
- 23.Jones M., Kujundzic M., John S., Bismarck A. Crab vs. mushroom: A review of crustacean and fungal chitin in wound treatment. Mar. Drugs. 2020;18:64. doi: 10.3390/md18010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kostag M., El Seoud O.A. Sustainable biomaterials based on cellulose, chitin and chitosan composites—A review. Carbohydr. Polym. Tech. Applic. 2021;2:100079. doi: 10.1016/j.carpta.2021.100079. [DOI] [Google Scholar]
- 25.Peter M.G. Chitin and Chitosan from Animal Sources. In: Steinbüchel A., editor. Biopolymers: Biology, Chemistry, Biotechnology, Applications. Wiley-VCH; Weinheim, Germany: 2001. [Google Scholar]
- 26.Gooday G.W. The Ecology of Chitin Degradation. In: Marshall K.C., editor. Advances in Microbial Ecology. Springer; Boston, MA, USA: 1990. pp. 387–430. [Google Scholar]
- 27.Peter M.G. Chitin and Chitosan in Fungi. In: Steinbüchel A., editor. Biopolymers: Biology, Chemistry, Biotechnology, Applications. Wiley-VCH; Weinheim, Germany: 2001. [Google Scholar]
- 28.Latgé J.-P. The cell wall: A carbohydrate armour for the fungal cell. Mol. Microbiol. 2007;66:279–290. doi: 10.1111/j.1365-2958.2007.05872.x. [DOI] [PubMed] [Google Scholar]
- 29.Rahman M.A., Halfar J. First evidence of chitin in calcified coralline algae: New insights into the calcification process of Clathromorphum compactum. Sci. Rep. 2014;4:6162. doi: 10.1038/srep06162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu S., Sun J., Yu L., Zhang C., Bi J., Zhu F., Qu M., Jiang C., Yang Q. Extraction and characterization of chitin from the beetle Holotrichia parallela Motschulsky. Molecules. 2012;17:4604–4611. doi: 10.3390/molecules17044604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dhillon G.S., Kaur S., Brar S.K., Verma M. Green synthesis approach: Extraction of chitosan from fungus mycelia. Crit. Rev. Biotechnol. 2013;33:379–403. doi: 10.3109/07388551.2012.717217. [DOI] [PubMed] [Google Scholar]
- 32.Joseph S.M., Krishnamoorthy S., Paranthaman R., Moses J.A., Anandharamakrishnan C. A review on source-specific chemistry, functionality, and applications of chitin and chitosan. Carbohydr. Polym. Technol. Appl. 2021;2:100036. doi: 10.1016/j.carpta.2021.100036. [DOI] [Google Scholar]
- 33.Castro R., Guerrero-Legarreta I., Bórquez R. Chitin extraction from Allopetrolisthes punctatus crab using lactic fermentation. Biotechnol. Rep. 2018;20:e00287. doi: 10.1016/j.btre.2018.e00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Naveed M., Phil L., Sohail M., Hasnat M., Baig M.M.F.A., Ihsan A.U., Shumzaid M., Kakar M.U., Mehmood Khan T., Akabar M.D., et al. Chitosan oligosaccharide (COS): An overview. Int. J. Biol. Macromol. 2019;129:827–843. doi: 10.1016/j.ijbiomac.2019.01.192. [DOI] [PubMed] [Google Scholar]
- 35.Cottaz S., Samain E. Genetic engineering of Escherichia coli for the production of NI, NII-diacetylchitobiose (chitinbiose) and its utilization as a primer for the synthesis of complex carbohydrates. Metab. Eng. 2005;7:311–317. doi: 10.1016/j.ymben.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 36.Yang T.-L. Chitin-based materials in tissue engineering: Applications in soft tissue and epithelial organ. Int. J. Mol. Sci. 2011;12:1936–1963. doi: 10.3390/ijms12031936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Q.Z., Chen X.G., Liu N., Wang S.X., Liu C.S., Meng X.H., Liu C.G. Protonation constants of chitosan with different molecular weight and degree of deacetylation. Carbohydr. Polym. 2006;65:194–201. doi: 10.1016/j.carbpol.2006.01.001. [DOI] [Google Scholar]
- 38.Madihally S.V., Flake A.W., Matthew H.W.T. Maintenance of CD34 expression during proliferation of CD34 & +; cord blood cells on glycosaminoglycan surfaces. Stem Cells. 1999;17:295–305. doi: 10.1002/stem.170295. [DOI] [PubMed] [Google Scholar]
- 39.Masuoka K., Ishihara M., Asazuma T., Hattori H., Matsui T., Takase B., Kanatani Y., Fujita M., Saito Y., Yura H., et al. The interaction of chitosan with fibroblast growth factor-2 and its protection from inactivation. Biomaterials. 2005;26:3277–3284. doi: 10.1016/j.biomaterials.2004.07.061. [DOI] [PubMed] [Google Scholar]
- 40.Rondon E.P., Benabdoun H.A., Vallières F., Segalla Petrônio M., Tiera M.J., Benderdour M., Fernandes J.C. Evidence supporting the safety of pegylated Diethylaminoethyl-Chitosan polymer as a nanovector for gene therapy applications. Int. J. Nanomed. 2020;15:6183–6200. doi: 10.2147/IJN.S252397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim I.-Y., Seo S.-J., Moon H.-S., Yoo M.-K., Park I.-Y., Kim B.-C., Cho C.-S. Chitosan and its derivatives for tissue engi-neering applications. Biotechnol. Adv. 2008;26:1–21. doi: 10.1016/j.biotechadv.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 42.Kim S., Cui Z.-K., Koo B., Zheng J., Aghaloo T., Lee M. Chitosan-Lysozyme conjugates for Enzyme-Triggered Hydrogel degradation in tissue engineering applications. ACS Appl. Mater. Interfaces. 2018;10:41138–41145. doi: 10.1021/acsami.8b15591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nordtveit R.J., Vårum K.M., Smidsrød O. Degradation of fully water-soluble, partially N-acetylated chitosans with lysozyme. Carbohydr. Polym. 1994;23:253–260. doi: 10.1016/0144-8617(94)90187-2. [DOI] [Google Scholar]
- 44.Roman D.L., Ostafe V., Isvoran A. Deeper inside the specificity of lysozyme when degrading chitosan. A structural bioinformatics study. J. Mol. Graph. Model. 2020;100:107676. doi: 10.1016/j.jmgm.2020.107676. [DOI] [PubMed] [Google Scholar]
- 45.Ren D., Yi H., Wang W., Ma X. The enzymatic degradation and swelling properties of chitosan matrices with different degrees of N-acetylation. Carbohydr. Res. 2005;340:2403–2410. doi: 10.1016/j.carres.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 46.Mason D.Y., Taylor C.R. The distribution of muramidase (lysozyme) in human tissues. J. Clin. Pathol. 1975;28:124–132. doi: 10.1136/jcp.28.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Geyer G. Lysozyme in Paneth cell secretions. Acta Histochem. 1973;45:126–132. [PubMed] [Google Scholar]
- 48.Saraiva S.M., Miguel S.P., Ribeiro M.P., Coutinho P., Correia I.J. Synthesis and characterization of a photocrosslinkable chitosan–gelatin hydrogel aimed for tissue regeneration. RSC Adv. 2015;5:63478–63488. doi: 10.1039/C5RA10638A. [DOI] [Google Scholar]
- 49.Islam M.M., Shahruzzaman M., Biswas S., Nurus Sakib M., Rashid T.U. Chitosan based bioactive materials in tissue engineering applications-A review. Bioact. Mater. 2020;5:164–183. doi: 10.1016/j.bioactmat.2020.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li S., Tian X., Fan J., Tong H., Ao Q., Wang X. Chitosans for tissue repair and organ three-dimensional (3D) bioprinting. Micromachines. 2019;10:765. doi: 10.3390/mi10110765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rejinold N.S., Chennazhi K.P., Tamura H., Nair S.V., Rangasamy J. Multifunctional chitin nanogels for simultaneous drug delivery, bioimaging, and biosensing. Acs Appl. Mater. Interfaces. 2011;3:3654–3665. doi: 10.1021/am200844m. [DOI] [PubMed] [Google Scholar]
- 52.Hanagata N., Zhang H., Chen S., Zhi C., Yamazaki T. Chitosan-coated boron nitride nanospheres enhance delivery of CpG oligodeoxynucleotides and induction of cytokines. Int. J. Nanomed. 2013;8:1783–1793. doi: 10.2147/IJN.S43251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parhi R. Drug delivery applications of chitin and chitosan: A review. Environ. Chem. Lett. 2020;18:577–594. doi: 10.1007/s10311-020-00963-5. [DOI] [Google Scholar]
- 54.Takeshita S., Zhao S., Malfait W.J., Koebel M.M. Chemistry of Chitosan Aerogels: Three-dimensional pore control for tailored applications. Angew. Chem. Int. Ed. 2021;60:9828–9851. doi: 10.1002/anie.202003053. [DOI] [PubMed] [Google Scholar]
- 55.Singh R., Shitiz K., Singh A. Chitin and chitosan: Biopolymers for wound management. Int. Wound J. 2017;14:1276–1289. doi: 10.1111/iwj.12797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Song X., Huang X., Li Z., Li Z., Wu K., Jiao Y., Zhou C. Construction of blood compatible chitin/graphene oxide composite aerogel beads for the adsorption of bilirubin. Carbohydr. Polym. 2019;207:704–712. doi: 10.1016/j.carbpol.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 57.Wu S., Duan B., Lu A., Wang Y., Ye Q., Zhang L. Biocompatible chitin/carbon nanotubes composite hydrogels as neuronal growth substrates. Carbohydr. Polym. 2017;174:830–840. doi: 10.1016/j.carbpol.2017.06.101. [DOI] [PubMed] [Google Scholar]
- 58.Ratanajiajaroen P., Ohshima M. Synthesis, release ability and bioactivity evaluation of chitin beads incorporated with curcumin for drug delivery applications. J. Microencapsul. 2012;29:549–558. doi: 10.3109/02652048.2012.668954. [DOI] [PubMed] [Google Scholar]
- 59.McCarthy P.C., Zhang Y., Abebe F. Recent applications of dual-stimuli responsive chitosan hydrogel nanocomposites as drug delivery tools. Molecules. 2021;26:4735. doi: 10.3390/molecules26164735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Narmani A., Jafari S.M. Chitosan-based nanodelivery systems for cancer therapy: Recent advances. Carbohydr. Polym. 2021;272:118464. doi: 10.1016/j.carbpol.2021.118464. [DOI] [PubMed] [Google Scholar]
- 61.Pathak K., Misra S.K., Sehgal A., Singh S., Bungau S., Najda A., Gruszecki R., Behl T. Biomedical Applications of Quaternized Chitosan. Polymers. 2021;13:2514. doi: 10.3390/polym13152514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Araujo V.H.S., de Souza M.P.C., Carvalho G.C., Duarte J.L., Chorilli M. Chitosan-based systems aimed at local application for vaginal infections. Carbohydr. Polym. 2021;261:117919. doi: 10.1016/j.carbpol.2021.117919. [DOI] [PubMed] [Google Scholar]
- 63.Boroumand H., Badie F., Mazaheri S., Seyedi Z.S., Nahand J.S., Nejati M., Baghi H.B., Abbasi-Kolli M., Badehnoosh B., Ghandali M., et al. Chitosan-based nanoparticles against viral infections. Front. Cell. Infect. Microbiol. 2021;11:643953. doi: 10.3389/fcimb.2021.643953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hayashi Y., Yamada S., Yanagi Guchi K., Koyama Z., Ikeda T. Chitosan and Fish Collagen as Biomaterials for Regenerative Medicine. In: Kim S.-K., editor. Marine Medicinal Foods: Implications and Applications—Animals and Microbes. Elsevier Academy Press; Amsterdam, The Netherlands: 2012. pp. 107–120. [DOI] [PubMed] [Google Scholar]
- 65.Liu X., Howard K.A., Dong M., Andersen M.Ø., Rahbek U.L., Johnsen M.G., Hansen O.C., Besenbacher F., Kjems J. The influence of polymeric properties on chitosan/siRNA nanoparticle formulation and gene silencing. Biomaterials. 2007;28:1280–1288. doi: 10.1016/j.biomaterials.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 66.Koide M., Osaki K., Konishi J., Oyamada K., Katakura T., Takahashi A., Yoshizato K. A new type of biomaterial for artificial skin: Dehydrothermally cross-linked composites of fibrillar and denatured collagens. J. Biomed. Mater. Res. 1993;27:79–87. doi: 10.1002/jbm.820270111. [DOI] [PubMed] [Google Scholar]
- 67.Aibibu D., Hild M., Wöltje M., Cherif C. Textile cell-free scaffolds for in situ tissue engineering applications. J. Mater. Sci. Mater. Med. 2016;27:63. doi: 10.1007/s10856-015-5656-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sadeghi A.M.M., Dorkoosh F.A., Avadi M.R., Saadat P., Rafiee-Tehrani M., Junginger H.E. Preparation, characterization and antibacterial activities of chitosan, N-trimethyl chitosan (TMC) and N-diethylmethyl chitosan (DEMC) nanoparticles loaded with insulin using both the ionotropic gelation and polyelectrolyte complexation methods. Int. J. Pharm. 2008;355:299–306. doi: 10.1016/j.ijpharm.2007.11.052. [DOI] [PubMed] [Google Scholar]
- 69.Shivakumar P., Gupta M.S., Jayakumar R., Gowda D.V. Prospection of chitosan and its derivatives in wound healing: Proof of patent analysis (2010–2020) Int. J. Biol. Macromol. 2021;184:701–712. doi: 10.1016/j.ijbiomac.2021.06.086. [DOI] [PubMed] [Google Scholar]
- 70.Xiao B., Ma P., Viennois E., Merlin D. Urocanic acid-modified chitosan nanoparticles can confer anti-inflammatory effect by delivering CD98 siRNA to macrophages. Colloids Surf. B. 2016;143:186–193. doi: 10.1016/j.colsurfb.2016.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Palma P.J., Ramos J.C., Martins J.B., Diogenes A., Figueiredo M.H., Ferreira P., Viegas C., Santos J.M. Histologic evaluation of regenerative endodontic procedures with the use of chitosan scaffolds in immature dog teeth with apical periodontitis. J. Endod. 2017;43:1279–1287. doi: 10.1016/j.joen.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 72.Mehrabani M.G., Karimian R., Rakhshaei R., Pakdel F., Eslami H., Fakhrzadeh V., Rahimi M., Salehi R., Kafil H.S. Chitin/silk fibroin/TiO2 bio-nanocomposite as a biocompatible wound dressing bandage with strong antimicrobial activity. Int. J. Biol. Macromol. 2018;116:966–976. doi: 10.1016/j.ijbiomac.2018.05.102. [DOI] [PubMed] [Google Scholar]
- 73.Tallawi M., Rosellini E., Barbani N., Cascone M.G., Rai R., Saint-Pierre G., Boccaccini A.R. Strategies for the chemical and biological functionalization of scaffolds for cardiac tissue engineering: A review. J. R. Soc. Interface. 2015;12:20150254. doi: 10.1098/rsif.2015.0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ribeiro M.P., Espiga A., Silva D., Baptista P., Henriques J., Ferreira C., Silva J.C., Borges J.P., Pires E., Chaves P., et al. Development of a new chitosan hydrogel for wound dressing. Wound Repair Regen. 2009;17:817–824. doi: 10.1111/j.1524-475X.2009.00538.x. [DOI] [PubMed] [Google Scholar]
- 75.Heinemann C., Heinemann S., Bernhardt A., Lode A., Worch H., Hanke T. In vitro osteoclastogenesis on textile chitosan scaffold. Eur. Cells Mater. 2010;19:96–106. doi: 10.22203/eCM.v019a10. [DOI] [PubMed] [Google Scholar]
- 76.Ostadhossein F., Mahmoudi N., Morales-Cid G., Tamjid E., Navas-Martos F.J., Soriano-Cuadrado B., Paniza J.M.L., Simchi A. Development of Chitosan/Bacterial cellulose composite films containing nanodiamonds as a potential flexible platform for wound dressing. Materials. 2015;8:6401–6418. doi: 10.3390/ma8095309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Negut I., Dorcioman G., Grumezescu V. Scaffolds for wound healing applications. Polymers. 2020;12:2010. doi: 10.3390/polym12092010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Peluso G., Petillo O., Ranieri M., Santin M., Ambrosic L., Calabró D., Avallone B., Balsamo G. Chitosan-mediated stimulation of macrophage function. Biomaterials. 1994;15:1215–1220. doi: 10.1016/0142-9612(94)90272-0. [DOI] [PubMed] [Google Scholar]
- 79.Shibata Y., Metzger W.J., Myrvik Q.N. Chitin particle-induced cell-mediated immunity is inhibited by soluble mannan: Mannose receptor-mediated phagocytosis initiates IL-12 production. J. Immunol. 1997;159:2462. [PubMed] [Google Scholar]
- 80.Jayakumar R., Prabaharan M., Sudheesh Kumar P.T., Nair S.V., Tamura H. Biomaterials based on chitin and chitosan in wound dressing applications. Biotechnol. Adv. 2011;29:322–337. doi: 10.1016/j.biotechadv.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 81.Kortekaas K.I., Seys S.F., Lund G., Jonckheere A.-C., Dierckx de Casterlé I., Ceuppens J.L., Steelant B., Hellings P.W. Nasal epithelial barrier dysfunction increases sensitization and mast cell degranulation in the absence of allergic inflammation. Allergy. 2020;75:1155–1164. doi: 10.1111/all.14132. [DOI] [PubMed] [Google Scholar]
- 82.Lopata A.L., Lehrer S.B. New insights into seafood allergy. Curr. Opin. Allergy Clin. Immunol. 2009;9:270–277. doi: 10.1097/ACI.0b013e32832b3e6f. [DOI] [PubMed] [Google Scholar]
- 83.Yusof N.L.B.M., Wee A., Lim L.Y., Khor E. Flexible chitin films as potential wound-dressing materials: Wound model studies. J. Biomed. Mater. Res. 2003;66:224–232. doi: 10.1002/jbm.a.10545. [DOI] [PubMed] [Google Scholar]
- 84.Moussian B., Uv A.E. An ancient control of epithelial barrier formation and wound healing. Bioessays. 2005;27:987–990. doi: 10.1002/bies.20308. [DOI] [PubMed] [Google Scholar]
- 85.Pesch Y.-Y., Riedel D., Patil K.R., Loch G., Behr M. Chitinases and imaginal disc growth factors organize the extracellular matrix formation at barrier tissues in insects. Sci. Rep. 2016;6:18340. doi: 10.1038/srep18340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kumar V., Behr M., Kiritsi D., Scheffschick A., Grahnert A., Homberg M., Schwieger-Briel A., Jakob T., Bruck-ner-Tuderman L., Magin T.M. Keratin-dependent thymic stromal lymphopoietin expression suggests a link between skin blistering and atopic disease. J. Allergy Clin. Immunol. 2016;133:1461–1464. doi: 10.1016/j.jaci.2016.04.046. [DOI] [PubMed] [Google Scholar]
- 87.Hirsch T., Rothoeft T., Teig N., Bauer J.W., Pellegrini G., De R.L., Scaglione D., Reichelt J., Klausegger A., Kneisz D., et al. Regeneration of the entire human epidermis using transgenic stem cells. Nature. 2017;551:327–332. doi: 10.1038/nature24487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ngoc-Hai V.C., Hong-My D.D., Bach P.T., Ngoc T.Q., van Vo T., Nguyen T.-H. Simple fabrication of a chitin wound healing membrane from Soft-Shell crab carapace. Mater. Lett. 2021;297:129995. doi: 10.1016/j.matlet.2021.129995. [DOI] [Google Scholar]
- 89.Baxter R.M., Dai T., Kimball J., Wang E., Hamblin M.R., Wiesmann W.P., McCarthy S.J., Baker S.M. Chitosan dressing promotes healing in third degree burns in mice: Gene expression analysis shows biphasic effects for rapid tissue regeneration and decreased fibrotic signaling. J. Biomed. Mater. Res. A. 2013;101:340–348. doi: 10.1002/jbm.a.34328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Muzzarelli R.A., Morganti P., Morganti G., Palombo P., Palombo M., Biagini G., Mattioli Belmonte M., Giantomassi F., Orlandi F., Muzzarelli C. Chitin nanofibrils/chitosan glycolate composites as wound medicaments. Carbohydr. Polym. 2007;70:274–284. doi: 10.1016/j.carbpol.2007.04.008. [DOI] [Google Scholar]
- 91.Miguel S.P., Figueira D.R., Simões D., Ribeiro M.P., Coutinho P., Ferreira P., Correia I.J. Electrospun polymeric nanofibres as wound dressings: A review. Colloids Surf. B. 2018;169:60–71. doi: 10.1016/j.colsurfb.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 92.Mezzana P. Clinical efficacy of a new chitin nanofibrils-based gel in wound healing. Acta Chir. Plast. 2008;50:81–84. [PubMed] [Google Scholar]
- 93.Paddle-Ledinek J.E., Nasa Z., Cleland H.J. Effect of different wound dressings on cell viability and proliferation. Plast. Reconstr. Surg. 2006;117:110S–118S. doi: 10.1097/01.prs.0000225439.39352.ce. [DOI] [PubMed] [Google Scholar]
- 94.Enoch S., Leaper D.J. Basic science of wound healing. Surgery. 2008;26:31–37. doi: 10.1016/j.mpsur.2007.11.005. [DOI] [Google Scholar]
- 95.Barnes L.A., Marshall C.D., Leavitt T., Hu M.S., Moore A.L., Gonzalez J.G., Longaker M.T., Gurtner G.C. Mechanical forces in cutaneous wound healing: Emerging therapies to minimize scar formation. Adv. Wound Care. 2018;7:47–56. doi: 10.1089/wound.2016.0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nita L.E., Ghilan A., Rusu A.G., Neamtu I., Chiriac A.P. New trends in bio-based aerogels. Pharmaceutics. 2020;12:449. doi: 10.3390/pharmaceutics12050449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Batista M.P., Gonçalves V.S.S., Gaspar F.B., Nogueira I.D., Matias A.A., Gurikov P. Novel alginate-chitosan aerogel fibres for potential wound healing applications. Int. J. Biol. Macromol. 2020;156:773–782. doi: 10.1016/j.ijbiomac.2020.04.089. [DOI] [PubMed] [Google Scholar]
- 98.Keil C., Hübner C., Richter C., Lier S., Barthel L., Meyer V., Subrahmanyam R., Gurikov P., Smirnova I., Haase H. Ca-Zn-Ag alginate aerogels for wound healing applications: Swelling behavior in simulated human body fluids and effect on macrophages. Polymers. 2020;12:2741. doi: 10.3390/polym12112741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Akhtar M.A., Ilyas K., Dlouhý I., Siska F., Boccaccini A.R. Electrophoretic deposition of copper (II)-chitosan complexes for antibacterial coatings. Int. J. Mol. Sci. 2020;21:2637. doi: 10.3390/ijms21072637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gritsch L., Maqbool M., Mouriño V., Ciraldo F.E., Cresswell M., Jackson P.R., Lovell C., Boccaccini A.R. Chitosan/hydroxyapatite composite bone tissue engineering scaffolds with dual and decoupled therapeutic ion delivery: Copper and strontium. J. Mater. Chem. B. 2019;7:6109–6124. doi: 10.1039/C9TB00897G. [DOI] [PubMed] [Google Scholar]
- 101.Kruppke B., Heinemann C., Farack J., Weil S., Aflalo E.D., Sagi A., Hanke T. Hemocyanin modification of chitosan scaffolds with calcium phosphate phases increase the osteoblast/osteoclast activity ratio—A co-culture study. Molecules. 2020;25:4580. doi: 10.3390/molecules25194580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Radwan-Pragłowska J., Piątkowski M., Janus Ł., Bogdał D., Matysek D., Cablik V. Microwave-assisted synthesis and characterization of antioxidant chitosan-based aerogels for biomedical applications. Int. J. Polym. Anal. Charact. 2018;23:721–729. doi: 10.1080/1023666X.2018.1504471. [DOI] [Google Scholar]
- 103.Ryu S., Song P.I., Seo C.H., Cheong H., Park Y. Colonization and infection of the skin by S. aureus: Immune system evasion and the response to cationic antimicrobial peptides. Int. J. Mol. Sci. 2014;15:8753–8772. doi: 10.3390/ijms15058753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Öztürk-Çolak A., Moussian B., Araújo S.J., Casanova J. A feedback mechanism converts individual cell features into a supracellular ECM structure in Drosophila trachea. eLife. 2016;5:179. doi: 10.7554/eLife.09373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moussian B., Seifarth C., Müller U., Berger J., Schwarz H. Cuticle differentiation during Drosophila embryogenesis. Arthropod Struct. Dev. 2006;35:137–152. doi: 10.1016/j.asd.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 106.Merzendorfer H., Zimoch L. Chitin metabolism in insects: Structure, function and regulation of chitin synthases and chitinases. J. Exp. Biol. 2003;206:4393–4412. doi: 10.1242/jeb.00709. [DOI] [PubMed] [Google Scholar]
- 107.Romano P., Fabritius H., Raabe D. The exoskeleton of the lobster Homarus americanus as an example of a smart anisotropic biological material. Acta Biomater. 2007;3:301–309. doi: 10.1016/j.actbio.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 108.Kaya M., Sargin I., Al-Jaf I., Erdogan S., Arslan G. Characteristics of corneal lens chitin in dragonfly compound eyes. Int. J. Biol. Macromol. 2016;89:54–61. doi: 10.1016/j.ijbiomac.2016.04.056. [DOI] [PubMed] [Google Scholar]
- 109.Nikolov S., Petrov M., Lymperakis L., Friák M., Sachs C., Fabritius H.-O., Raabe D., Neugebauer J. Revealing the design principles of high-performance biological composites using ab initio and multiscale simulations: The example of lobster cuticle. Adv. Mater. 2010;22:519–526. doi: 10.1002/adma.200902019. [DOI] [PubMed] [Google Scholar]
- 110.Fabritius H.-O., Ziegler A., Friák M., Nikolov S., Huber J., Seidl B.H.M., Ruangchai S., Alagboso F.I., Karsten S., Lu J., et al. Functional adaptation of crustacean exoskeletal elements through structural and compositional diversity: A combined experimental and theoretical study. Bioinspir. Biomim. 2016;11:55006. doi: 10.1088/1748-3190/11/5/055006. [DOI] [PubMed] [Google Scholar]
- 111.Muthukrishnan S., Merzendorfer H., Arakane Y., Yang Q. Chitin organizing and modifying enzymes and proteins involved in remodeling of the insect cuticle. Adv. Exp. Med. Biol. 2019;1142:83–114. doi: 10.1007/978-981-13-7318-3_5. [DOI] [PubMed] [Google Scholar]
- 112.Sviben S., Spaeker O., Bennet M., Albéric M., Dirks J.-H., Moussian B., Fratzl P., Bertinetti L., Politi Y. Epidermal cell surface structure and chitin-protein coassembly determine fiber architecture in the locust cuticle. ACS Appl. Mater. Interfaces. 2020;12:25581–25590. doi: 10.1021/acsami.0c04572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shen X., Shamshina J.L., Berton P., Gurau G., Rogers R.D. Hydrogels based on cellulose and chitin: Fabrication, properties, and applications. Green Chem. 2016;18:53–75. doi: 10.1039/C5GC02396C. [DOI] [Google Scholar]
- 114.Ganesan K., Budtova T., Ratke L., Gurikov P., Baudron V., Preibisch I., Niemeyer P., Smirnova I., Milow B. Review on the production of polysaccharide aerogel particles. Materials. 2018;11:2144. doi: 10.3390/ma11112144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rani M., Agarwal A., Negi Y.S. Review: Chitosan based hydrogel polymeric beads—As drug delivery system. BioResource. 2010;5:276–2807. [Google Scholar]
- 116.Hozumi K., Nomizu M. Mixed peptide-conjugated chitosan matrices as multi-receptor targeted cell-adhesive scaffolds. Int. J. Mol. Sci. 2018;19:2713. doi: 10.3390/ijms19092713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Higashi B., Mariano T.B., de Abreu Filho B.A., Gonçalves R.A.C., de Oliveira A.J.B. Effects of fructans and probiotics on the inhibition of Klebsiella oxytoca and the production of short-chain fatty acids assessed by NMR spectroscopy. Carbohydr. Polym. 2020;248:116832. doi: 10.1016/j.carbpol.2020.116832. [DOI] [PubMed] [Google Scholar]
- 118.Bhardwaj N., Kundu S.C. Silk fibroin protein and chitosan polyelectrolyte complex porous scaffolds for tissue engineering applications. Carbohydr. Polym. 2011;85:325–333. doi: 10.1016/j.carbpol.2011.02.027. [DOI] [Google Scholar]
- 119.Xu Z., Shi L., Yang M., Zhang H., Zhu L. Fabrication of a novel blended membrane with chitosan and silk microfibers for wound healing: Characterization, in vitro and in vivo studies. J. Mater. Chem. B. 2015;3:3634–3642. doi: 10.1039/C5TB00226E. [DOI] [PubMed] [Google Scholar]
- 120.Zhu N., Li M.G., Guan Y.J., Schreyer D.J., Chen X.B. Effects of laminin blended with chitosan on axon guidance on patterned substrates. Biofabrication. 2010;2:45002. doi: 10.1088/1758-5082/2/4/045002. [DOI] [PubMed] [Google Scholar]
- 121.Orellana S.L., Giacaman A., Vidal A., Morales C., Oyarzun-Ampuero F., Lisoni J.G., Henríquez-Báez C., Morán-Trujillo L., Concha M., Moreno-Villoslada I. Chitosan/chondroitin sulfate aerogels with high polymeric electroneutralization degree: Formation and mechanical properties. Pure Appl. Chem. 2018;90:901–911. doi: 10.1515/pac-2016-1111. [DOI] [Google Scholar]
- 122.Mehrabani M.G., Karimian R., Mehramouz B., Rahimi M., Kafil H.S. Preparation of biocompatible and biodegradable silk fibroin/chitin/silver nanoparticles 3D scaffolds as a bandage for antimicrobial wound dressing. Int. J. Biol. Macromol. 2018;114:961–971. doi: 10.1016/j.ijbiomac.2018.03.128. [DOI] [PubMed] [Google Scholar]
- 123.Cui L., Xiong Z., Guo Y., Liu Y., Zhao J., Zhang C., Zhu P. Fabrication of interpenetrating polymer network chi-tosan/gelatin porous materials and study on dye adsorption properties. Carbohydr. Polym. 2015;132:330–337. doi: 10.1016/j.carbpol.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 124.Gilarska A., Lewandowska-Łańcucka J., Horak W., Nowakowska M. Collagen/chitosan/hyaluronic acid-based injectable hydrogels for tissue engineering applications-design, physicochemical and biological characterization. Colloids Surf. B. 2018;170:152–162. doi: 10.1016/j.colsurfb.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 125.Chen C., Yang H., Tang B., Yang W.-J., Jin D.-C. Identification and functional analysis of chitinase 7 gene in white-backed planthopper, Sogatella furcifera. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2017;208–209:19–28. doi: 10.1016/j.cbpb.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 126.Ho M.-H., Wang D.-M., Hsieh H.-J., Liu H.-C., Hsien T.-Y., Lai J.-Y., Hou L.-T. Preparation and characterization of RGD-immobilized chitosan scaffolds. Biomaterials. 2005;26:3197–3206. doi: 10.1016/j.biomaterials.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 127.Tiğli R.S., Gümüşderelioğlu M. Evaluation of RGD- or EGF-immobilized chitosan scaffolds for chondrogenic activity. Int. J. Biol. Macromol. 2008;43:121–128. doi: 10.1016/j.ijbiomac.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 128.Masuko T., Minami A., Iwasaki N., Majima T., Nishimura S.-I., Lee Y.C. Thiolation of chitosan. Attachment of proteins via thioether formation. Biomacromolecules. 2005;6:880–884. doi: 10.1021/bm049352e. [DOI] [PubMed] [Google Scholar]
- 129.Hozumi K., Nomizu M. Cell adhesion activity of peptides conjugated to polysaccharides. Curr. Protoc. Cell Biol. 2018;80:e53. doi: 10.1002/cpcb.53. [DOI] [PubMed] [Google Scholar]
- 130.Silva S.S., Motta A., Rodrigues M.T., Pinheiro A.F.M., Gomes M.E., Mano J.F., Reis R.L., Migliaresi C. Novel genipin-cross-linked chitosan/silk fibroin sponges for cartilage engineering strategies. Biomacromolecules. 2008;9:2764–2774. doi: 10.1021/bm800874q. [DOI] [PubMed] [Google Scholar]
- 131.Butler M.F., Clark A.H., Adams S. Swelling and mechanical properties of biopolymer hydrogels containing chitosan and bovine serum albumin. Biomacromolecules. 2006;7:2961–2970. doi: 10.1021/bm060133y. [DOI] [PubMed] [Google Scholar]
- 132.Cheng Y., Hu Z., Zhao Y., Zou Z., Lu S., Zhang B., Li S. Sponges of carboxymethyl chitosan grafted with collagen peptides for wound healing. Int. J. Mol. Sci. 2019;20:3890. doi: 10.3390/ijms20163890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ganesan K., Heyer M., Ratke L., Milow B. Facile preparation of nanofibrillar networks of ‘’Ureido-Chitin’’ containing ureido and amine as chelating functional groups. Chemistry. 2018;24:19332–19340. doi: 10.1002/chem.201804405. [DOI] [PubMed] [Google Scholar]
- 134.Aegerter M.A., Leventis N. Aerogels Handbook. Springer Science Business Media LLC; New York, NY, USA: 2011. [Google Scholar]
- 135.Yamasaki S., Sakuma W., Yasui H., Daicho K., Saito T., Fujisawa S., Isogai A., Kanamori K. Nanocellulose xerogels with high porosities and large specific surface areas. Front. Chem. 2019;7:316. doi: 10.3389/fchem.2019.00316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ganesan K., Dennstedt A., Barowski A., Ratke L. Design of aerogels, cryogels and xerogels of cellulose with hierarchical porous structures. Mater. Des. 2016;92:345–355. doi: 10.1016/j.matdes.2015.12.041. [DOI] [Google Scholar]
- 137.Li J., Sun X., Zhang K., Yang G., Mu Y., Su C., Pang J., Chen T., Chen X., Feng C. Chitosan/Diatom-Biosilica aerogel with controlled porous structure for rapid hemostasis. Adv. Healthc. Mater. 2020;9:e2000951. doi: 10.1002/adhm.202000951. [DOI] [PubMed] [Google Scholar]
- 138.Guo X., Xu D., Zhao Y., Gao H., Shi X., Cai J., Deng H., Chen Y., Du Y. Electroassembly of Chitin nanoparticles to construct freestanding hydrogels and high porous aerogels for wound healing. ACS Appl. Mater. Interfaces. 2019;11:34766–34776. doi: 10.1021/acsami.9b13063. [DOI] [PubMed] [Google Scholar]
- 139.Feng P., Luo Y., Ke C., Qiu H., Wang W., Zhu Y., Hou R., Xu L., Wu S. Chitosan-based functional materials for skin wound repair: Mechanisms and applications. Front. Bioeng. Biotechnol. 2021;9:650598. doi: 10.3389/fbioe.2021.650598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jing X., Sun Y., Ma X., Hu H. Marine polysaccharides: Green and recyclable resources as wound dressings. Mater. Chem. Front. 2021;5:5595–5616. doi: 10.1039/D1QM00561H. [DOI] [Google Scholar]
- 141.Jin T., Liu T., Lam E., Moores A. Chitin and chitosan on the nanoscale. Nanoscale Horiz. 2021;6:505–542. doi: 10.1039/D0NH00696C. [DOI] [PubMed] [Google Scholar]
- 142.Ueno H., Mori T., Fujinaga T. Topical formulations and wound healing applications of chitosan. Adv. Drug Deliv. Rev. 2001;52:105–115. doi: 10.1016/S0169-409X(01)00189-2. [DOI] [PubMed] [Google Scholar]
- 143.Lovskaya D., Menshutina N., Mochalova M., Nosov A., Grebenyuk A. Chitosan-based aerogel particles as highly effective local hemostatic agents. Production process and in vivo evaluations. Polymers. 2020;12:2055. doi: 10.3390/polym12092055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.López-Iglesias C., Barros J., Ardao I., Gurikov P., Monteiro F.J., Smirnova I., Alvarez-Lorenzo C., García-González C.A. Jet cutting technique for the production of chitosan aerogel microparticles loaded with vancomycin. Polymers. 2020;12:273. doi: 10.3390/polym12020273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ko E., Kim H. Preparation of chitosan aerogel crosslinked in chemical and ionical ways by non-acid condition for wound dressing. Int. J. Biol. Macromol. 2020;164:2177–2185. doi: 10.1016/j.ijbiomac.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 146.Fan X., Li Y., Li X., Wu Y., Tang K., Liu J., Zheng X., Wan G. Injectable antibacterial cellulose nanofiber/chitosan aerogel with rapid shape recovery for noncompressible hemorrhage. Int. J. Biol. Macromol. 2020;154:1185–1193. doi: 10.1016/j.ijbiomac.2019.10.273. [DOI] [PubMed] [Google Scholar]
- 147.Neville A.C., Luke B.M. A two-system model for chitin-protein complexes in insect cuticles. Tissue Cell. 1969;1:689–707. doi: 10.1016/S0040-8166(69)80041-8. [DOI] [PubMed] [Google Scholar]
- 148.Mrak P., Bogataj U., Štrus J., Žnidaršič N. Cuticle morphogenesis in crustacean embryonic and postembryonic stages. Arthropod Struct. Dev. 2017;46:77–95. doi: 10.1016/j.asd.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 149.Uv A., Moussian B. The apical plasma membrane of Drosophila embryonic epithelia. Eur. J. Cell Biol. 2010;89:208–211. doi: 10.1016/j.ejcb.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 150.Wang Y., Farine J.-P., Yang Y., Yang J., Tang W., Gehring N., Ferveur J.-F., Moussian B. Transcriptional control of quality differences in the lipid-based cuticle barrier in Drosophila suzukii and Drosophila melanogaster. Front. Genet. 2020;11:887. doi: 10.3389/fgene.2020.00887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Dong W., Dobler R., Dowling D.K., Moussian B. The cuticle inward barrier in Drosophila melanogaster is shaped by mitochondrial and nuclear genotypes and a sex-specific effect of diet. PeerJ. 2019;7:e7802. doi: 10.7717/peerj.7802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Caldwell P.E., Walkiewicz M., Stern M. Ras activity in the Drosophila prothoracic gland regulates body size and developmetal rate via ecdysone release. Curr. Biol. 2005;15:1785–1795. doi: 10.1016/j.cub.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 153.Li T., Bender M. A conditional rescue system reveals essential functions for the ecdysone receptor (EcR) gene during molting and metamorphosis in Drosophila. Development. 2000;127:2897–2905. doi: 10.1242/dev.127.13.2897. [DOI] [PubMed] [Google Scholar]
- 154.Liu S., Li K., Gao Y., Liu X., Chen W., Ge W., Feng Q., Palli S.R., Li S. Antagonistic actions of juvenile hormone and 20-hydroxyecdysone within the ring gland determine developmental transitions in Drosophila. Proc. Natl. Acad. Sci. USA. 2018;115:139–144. doi: 10.1073/pnas.1716897115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jindra M., Palli S.R., Riddiford L.M. The juvenile hormone signaling pathway in insect development. Annu. Rev. Entomol. 2013;58:181–204. doi: 10.1146/annurev-ento-120811-153700. [DOI] [PubMed] [Google Scholar]
- 156.Pesch Y.-Y., Hesse R., Ali T., Behr M. A cell surface protein controls endocrine ring gland morphogenesis and steroid production. Dev. Biol. 2019;445:16–28. doi: 10.1016/j.ydbio.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 157.Raabe D., Al-Sawalmih A., Yi S.B., Fabritius H. Preferred crystallographic texture of alpha-chitin as a microscopic and macroscopic design principle of the exoskeleton of the lobster Homarus americanus. Acta Biomater. 2007;3:882–895. doi: 10.1016/j.actbio.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 158.Vincent J.F. Arthropod cuticle: A natural composite shell system. Compos. Part A Appl. Sci. Manuf. 2002;33:1311–1315. doi: 10.1016/S1359-835X(02)00167-7. [DOI] [Google Scholar]
- 159.Bouligand Y. Twisted fibrous arrangements in biological materials and cholesteric mesophases. Tissue Cell. 1972;4:189–217. doi: 10.1016/S0040-8166(72)80042-9. [DOI] [PubMed] [Google Scholar]
- 160.Dirks J.-H., Taylor D. Fracture toughness of locust cuticle. J. Exp. Biol. 2012;215:1502–1508. doi: 10.1242/jeb.068221. [DOI] [PubMed] [Google Scholar]
- 161.Rajabi H., Jafarpour M., Darvizeh A., Dirks J.-H., Gorb S.N. Stiffness distribution in insect cuticle: A continuous or a dis-continuous profile? J. R. Soc. Interface. 2017;14:20170310. doi: 10.1098/rsif.2017.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Vincent J.F.V., Wegst U.G.K. Design and mechanical properties of insect cuticle. Arthropod Struct. Dev. 2004;33:187–199. doi: 10.1016/j.asd.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 163.Rajabi H., Dirks J.-H., Gorb S.N. Insect wing damage: Causes, consequences and compensatory mechanisms. J. Exp. Biol. 2020;223:223. doi: 10.1242/jeb.215194. [DOI] [PubMed] [Google Scholar]
- 164.Behr M., Riedel D. Glycosylhydrolase genes control respiratory tubes sizes and airway stability. Sci. Rep. 2020;10:13377. doi: 10.1038/s41598-020-70185-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Arakane Y., Muthukrishnan S., Kramer K.J., Specht C.A., Tomoyasu Y., Lorenzen M.D., Kanost M., Beeman R.W. The tribolium chitin synthase genes TcCHS1 and TcCHS2 are specialized for synthesis of epidermal cuticle and midgut peritrophic matrix. Insect Mol. Biol. 2005;14:453–463. doi: 10.1111/j.1365-2583.2005.00576.x. [DOI] [PubMed] [Google Scholar]
- 166.Nikolov S., Fabritius H., Petrov M., Friák M., Lymperakis L., Sachs C., Raabe D., Neugebauer J. Robustness and optimal use of design principles of arthropod exoskeletons studied by ab initio-based multiscale simulations. J. Mech. Behav. Biomed. Mater. 2011;4:129–145. doi: 10.1016/j.jmbbm.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 167.Wang Y., Carballo R.G., Moussian B. Double cuticle barrier in two global pests, the whitefly Trialeurodes vaporariorum and the bedbug Cimex lectularius. J. Exp. Biol. 2017;220:1396–1399. doi: 10.1242/jeb.156679. [DOI] [PubMed] [Google Scholar]
- 168.Locke M. The wigglesworth lecture: Insects for studying fundamental problems in biology. J. Insect Physiol. 2001;47:495–507. doi: 10.1016/S0022-1910(00)00123-2. [DOI] [PubMed] [Google Scholar]
- 169.Hegedus D., Erlandson M., Gillott C., Toprak U. New insights into peritrophic matrix synthesis, architecture, and function. Annu. Rev. Entomol. 2009;54:285–302. doi: 10.1146/annurev.ento.54.110807.090559. [DOI] [PubMed] [Google Scholar]
- 170.Tonning A., Hemphälä J., Tång E., Nannmark U., Samakovlis C., Uv A. A transient luminal chitinous matrix is required to model epithelial tube diameter in the Drosophila trachea. Dev. Cell. 2005;9:423–430. doi: 10.1016/j.devcel.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 171.Tsarouhas V., Senti K.-A., Jayaram S.A., Tiklova K., Hemphala J., Adler J., Samakovlis C. Sequential pulses of apical epithelial secretion and endocytosis drive airway maturation in Drosophila. Dev. Cell. 2007;13:214–225. doi: 10.1016/j.devcel.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 172.Dong B., Hannezo E., Hayashi S. Balance between apical membrane growth and luminal matrix resistance determines epithlial tubule shape. Cell Rep. 2014;7:941–950. doi: 10.1016/j.celrep.2014.03.066. [DOI] [PubMed] [Google Scholar]
- 173.Behr M., Wingen C., Wolf C., Schuh R., Hoch M. Wurst is essential for airway clearance and respiratory-tube size control. Nat. Cell Biol. 2007;9:847–853. doi: 10.1038/ncb1611. [DOI] [PubMed] [Google Scholar]
- 174.Luschnig S., Bätz T., Armbruster K., Krasnow M.A. Serpentine and vermiform encode matrix proteins with chitin binding and deacetylation domains that limit tracheal tube length in Drosophila. Curr. Biol. 2006;16:186–194. doi: 10.1016/j.cub.2005.11.072. [DOI] [PubMed] [Google Scholar]
- 175.Wang S., Jayaram S.A., Hemphälä J., Senti K.-A., Tsarouhas V., Jin H., Samakovlis C. Septate-junction-dependent luminal deposition of chitin deacetylases restricts tube elongation in the Drosophila trachea. Curr. Biol. 2006;16:180–185. doi: 10.1016/j.cub.2005.11.074. [DOI] [PubMed] [Google Scholar]
- 176.Kelkenberg M., Odman-Naresh J., Muthukrishnan S., Merzendorfer H. Chitin is a necessary component to maintain the barier function of the peritrophic matrix in the insect midgut. Insect Biochem. Mol. Biol. 2015;56:21–28. doi: 10.1016/j.ibmb.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 177.Jaspers M.H.J., Pflanz R., Riedel D., Kawelke S., Feussner I., Schuh R. The fatty acyl-CoA reductase waterproof mediates airway clearance in Drosophila. Dev. Biol. 2014;385:23–31. doi: 10.1016/j.ydbio.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 178.Shaik K.S., Meyer F., Vázquez Á.V., Flötenmeyer M., Cerdán M.E., Moussian B. δ-Aminolevulinate synthase is required for apical transcellular barrier formation in the skin of the Drosophila larva. Eur. J. Cell Biol. 2012;91:204–215. doi: 10.1016/j.ejcb.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 179.Itakura Y., Inagaki S., Wada H., Hayashi S. Trynity controls epidermal barrier function and respiratory tube maturation in Drosophila by modulating apical extracellular matrix nano-patterning. PLoS ONE. 2018;13:e0209058. doi: 10.1371/journal.pone.0209058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Agrawal S., Kelkenberg M., Begum K., Steinfeld L., Williams C.E., Kramer K.J., Beeman R.W., Park Y., Muthukrishnan S., Merzendorfer H. Two essential peritrophic matrix proteins mediate matrix barrier functions in the insect midgut. Insect Biochem. Mol. Biol. 2014;49:24–34. doi: 10.1016/j.ibmb.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 181.Muthukrishnan S., Mun S., Noh M.Y., Geisbrecht E.R., Arakane Y. Insect cuticular chitin contributes to form and function. Curr. Pharm. Des. 2020;26:3530–3545. doi: 10.2174/1381612826666200523175409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Moussian B., Tang E., Tonning A., Helms S., Schwarz H., Nusslein-Volhard C., Uv A.E. Drosophila knickkopf and retroative are needed for epithelial tube growth and cuticle differentiation through their specific requirement for chitin filament organization. Development. 2006;133:163–171. doi: 10.1242/dev.02177. [DOI] [PubMed] [Google Scholar]
- 183.Pesch Y.-Y., Riedel D., Behr M. Obstructor a organizes matrix assembly at the apical cell surface to promote enzymatic cuticle maturation in Drosophila. J. Biol. Chem. 2015;290:10071–10082. doi: 10.1074/jbc.M114.614933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Noh M.Y., Muthukrishnan S., Kramer K.J., Arakane Y., Riddiford L.M. Tribolium castaneum RR-1 cuticular protein TcCPR4 is required for formation of pore canals in rigid cuticle. PLoS Genet. 2015;11:e1004963. doi: 10.1371/journal.pgen.1004963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Muthukrishnan S., Arakane Y., Yang Q., Zhang C.-X., Zhang J., Zhang W., Moussian B. Future questions in insect chitin biology: A microreview. Arch. Insect Biochem. Physiol. 2018;98:e21454. doi: 10.1002/arch.21454. [DOI] [PubMed] [Google Scholar]
- 186.Chaudhari S.S., Arakane Y., Specht C.A., Moussian B., Kramer K.J., Muthukrishnan S., Beeman R.W. Retroactive maintains cuticle integrity by promoting the trafficking of Knickkopf into the procuticle of Tribolium castaneum. PLoS Genet. 2013;9:e1003268. doi: 10.1371/journal.pgen.1003268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Arakane Y., Lomakin J., Gehrke S.H., Hiromasa Y., Tomich J.M., Muthukrishnan S., Beeman R.W., Kramer K.J., Kanost M.R., Stern D.L. Formation of rigid, non-flight forewings (Elytra) of a beetle requires two major cuticular proteins. PLoS Genet. 2012;8:e1002682. doi: 10.1371/journal.pgen.1002682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Noh M.Y., Muthukrishnan S., Kramer K.J., Arakane Y. Development and ultrastructure of the rigid dorsal and flexible ventral cuticles of the elytron of the red flour beetle, Tribolium castaneum. Insect Biochem. Mol. Biol. 2017;91:21–33. doi: 10.1016/j.ibmb.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 189.Dittmer N.T., Hiromasa Y., Tomich J.M., Lu N., Beeman R.W., Kramer K.J., Kanost M.R. Proteomic and transcriptomic analyses of rigid and membranous cuticles and epidermis from the Elytra and Hindwings of the red flour beetle, Tribolium castaneum. J. Proteome Res. 2012;11:269–278. doi: 10.1021/pr2009803. [DOI] [PubMed] [Google Scholar]
- 190.Tetreau G., Dittmer N.T., Cao X., Agrawal S., Chen Y.R., Muthukrishnan S., Haobo J., Blissard G.W., Kanost M.R., Wang P. Analysis of chitin-binding proteins from Manduca sexta provides new insights into evolution of peritrophin A-type chitin-binding domains in insects. Insect Biochem. Mol. Biol. 2015;62:127–141. doi: 10.1016/j.ibmb.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Liu J., Li S., Li W., Peng L., Chen Z., Xiao Y., Guo H., Zhang J., Cheng T., Goldsmith M.R., et al. Genome-wide annotation and comparative analysis of cuticular protein genes in the noctuid pest Spodoptera litura. Insect Biochem. Mol. Biol. 2019;110:90–97. doi: 10.1016/j.ibmb.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 192.Zhou D., Duan B., Sun Y., Ma L., Zhu C., Shen B. Preliminary characterization of putative structural cuticular proteins in the malaria vector Anopheles sinensis. Pest Manag. Sci. 2017;73:2519–2528. doi: 10.1002/ps.4649. [DOI] [PubMed] [Google Scholar]
- 193.Willis J.H. Structural cuticular proteins from arthropods: Annotation, nomenclature, and sequence characteristics in the genomics era. Insect Biochem. Mol. Biol. 2010;40:189–204. doi: 10.1016/j.ibmb.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Jasrapuria S., Specht C.A., Kramer K.J., Beeman R.W., Muthukrishnan S., Palli S.R. Gene families of cuticular proteins analogous to Peritrophins (CPAPs) in Tribolium castaneum have diverse functions. PLoS ONE. 2012;7:e49844. doi: 10.1371/journal.pone.0049844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Li Z.-L., Tian S., Yang H., Zhou X., Xu S., Zhang Z., Gong J., Hou Y., Xia Q. Genome-wide identification of chitin-binding proteins and characterization of BmCBP1 in the silkworm, Bombyx mori. Insect Sci. 2019;26:400–412. doi: 10.1111/1744-7917.12552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Dittmer N.T., Tetreau G., Cao X., Jiang H., Wang P., Kanost M.R. Annotation and expression analysis of cuticular proteins from the tobacco hornworm, Manduca sexta. Insect Biochem. Mol. Biol. 2015;62:100–113. doi: 10.1016/j.ibmb.2014.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Jasrapuria S., Arakane Y., Osman G., Kramer K.J., Beeman R.W., Muthukrishnan S. Genes encoding proteins with peritrophin A-type chitin-binding domains in Tribolium castaneum are grouped into three distinct families based on phylogeny, expression and function. Insect Biochem. Mol. Biol. 2010;40:214–227. doi: 10.1016/j.ibmb.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 198.Tajiri R., Ogawa N., Fujiwara H., Kojima T. mechanical control of whole body shape by a single cuticular protein obstructor-e in Drosophila melanogaster. PLoS Genet. 2017;13:e1006548. doi: 10.1371/journal.pgen.1006548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Noh M.Y., Kramer K.J., Muthukrishnan S., Kanost M.R., Beeman R.W., Arakane Y. Two major cuticular proteins are required for assembly of horizontal laminae and vertical pore canals in rigid cuticle of Tribolium castaneum. Insect Biochem. Mol. Biol. 2014;53:22–29. doi: 10.1016/j.ibmb.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 200.Behr M., Hoch M. Identification of the novel evolutionary conserved obstructor multigene family in invertebrates. FEBS Lett. 2005;579:6827–6833. doi: 10.1016/j.febslet.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 201.Tiklova K., Tsarouhas V., Samakovlis C. Control of airway tube diameter and integrity by secreted chitin-binding proteins in Drosophila. PLoS ONE. 2013;8:e67415. doi: 10.1371/journal.pone.0067415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Petkau G., Wingen C., Jussen L.C.A., Radtke T., Behr M. Obstructor-A is required for epithelial extracellular matrix dynamics, exoskeleton function, and tubulogenesis. J. Biol. Chem. 2012;287:21396–21405. doi: 10.1074/jbc.M112.359984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhang M., Ji Y., Zhang X., Ma P., Wang Y., Moussian B., Zhang J. The putative chitin deacetylases Serpentine and Vermiform have non-redundant functions during Drosophila wing development. Insect Biochem. Mol. Biol. 2019;110:128–135. doi: 10.1016/j.ibmb.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 204.Arakane Y., Dixit R., Begum K., Park Y., Specht C.A., Merzendorfer H., Kramer K.J., Muthukrishnan S., Beeman R.W. Analysis of functions of the chitin deacetylase gene family in Tribolium castaneum. Insect Biochem. Mol. Biol. 2009;39:355–365. doi: 10.1016/j.ibmb.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 205.Yu R.-R., Liu W.-M., Zhao X.-M., Zhang M., Li D.-Q., Zuber R., Ma E.-B., Zhu K.Y., Moussian B., Zhang J.-Z. LmCDA1 organizes the cuticle by chitin deacetylation in Locusta migratoria. Insect Mol. Biol. 2019;28:301–312. doi: 10.1111/imb.12554. [DOI] [PubMed] [Google Scholar]
- 206.Yu R., Liu W., Li D., Zhao X., Ding G., Zhang M., Ma E., Zhu K.Y., Li S., Moussian B., et al. Helicoidal organization of chitin in the cuticle of the migratory locust requires the function of the chitin deacetylase 2 enzyme (LmCDA2) J. Biol. Chem. 2016;291:24352–24363. doi: 10.1074/jbc.M116.720581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zhang T., Ma P., Zhou J., He Y., Liu W., Liu X., Zhang X., Yu R., Zhang M., Moussian B., et al. Group I CDAs are responsible for a selective CHC-independent cuticular barrier in Locusta migratoria. Pestic. Biochem. Physiol. 2021;175:104854. doi: 10.1016/j.pestbp.2021.104854. [DOI] [PubMed] [Google Scholar]
- 208.Zhang M., Ma P.-J., Zhang T.-T., Gao Z.-M., Zhao P., Liu X.-J., Zhang X.-Y., Liu W.-M., Yu R.-R., Moussian B., et al. Roles of LmCDA1 and LmCDA2 in cuticle formation in the foregut and hindgut of Locusta migratoria. Insect Sci. 2020;28:1314–1325. doi: 10.1111/1744-7917.12874. [DOI] [PubMed] [Google Scholar]
- 209.Chaudhari S.S., Arakane Y., Specht C.A., Moussian B., Boyle D.L., Park Y., Kramer K.J., Beeman R.W., Muthukrishnan S. Knickkopf protein protects and organizes chitin in the newly synthesized insect exoskeleton. Proc. Natl. Acad. Sci. USA. 2011;108:17028–17033. doi: 10.1073/pnas.1112288108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Li K., Zhang X., Zuo Y., Liu W., Zhang J., Moussian B. Timed Knickkopf function is essential for wing cuticle formation in Drosophila melanogaster. Insect Biochem. Mol. Biol. 2017;89:1–10. doi: 10.1016/j.ibmb.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 211.Arakane Y., Muthukrishnan S. Insect chitinase and chitinase-like proteins. Cell. Mol. Life Sci. 2010;67:201–216. doi: 10.1007/s00018-009-0161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Dixit R., Arakane Y., Specht C.A., Richard C., Kramer K.J., Beeman R.W., Muthukrishnan S. Domain organization and phylogenetic analysis of proteins from the chitin deacetylase gene family of Tribolium castaneum and three other species of insects. Insect Biochem. Mol. Biol. 2008;38:440–451. doi: 10.1016/j.ibmb.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 213.Zhu Q., Arakane Y., Beeman R.W., Kramer K.J., Muthukrishnan S. Functional specialization among insect chitinase family genes revealed by RNA interference. Proc. Natl. Acad. Sci. USA. 2008;105:6650–6655. doi: 10.1073/pnas.0800739105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Noh M.Y., Muthukrishnan S., Kramer K.J., Arakane Y. A chitinase with two catalytic domains is required for organization of the cuticular extracellular matrix of a beetle. PLoS Genet. 2018;14:e1007307. doi: 10.1371/journal.pgen.1007307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Pesch Y.-Y., Riedel D., Behr M. Drosophila Chitinase 2 is expressed in chitin producing organs for cuticle formation. Arthropod Struct. Dev. 2017;46:4–12. doi: 10.1016/j.asd.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 216.Irons S.L., Chambers A.C., Lissina O., King L.A., Possee R.D. Protein production using the baculovirus expression system. Curr. Protoc. Protein Sci. 2018;91:5.5.1.–5.5.22.. doi: 10.1002/cpps.45. [DOI] [PubMed] [Google Scholar]
- 217.Erko M., Hartmann M.A., Zlotnikov I., Valverde Serrano C., Fratzl P., Politi Y. Structural and mechanical properties of the arthropod cuticle: Comparison between the fang of the spider Cupiennius salei and the carapace of American lobster Homarus americanus. J. Struct. Biol. 2013;183:172–179. doi: 10.1016/j.jsb.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 218.Chaudhari S.S., Moussian B., Specht C.A., Arakane Y., Kramer K.J., Beeman R.W., Muthukrishnan S. Functional specialization among members of Knickkopf family of proteins in insect cuticle organization. PLoS Genet. 2014;10:e1004537. doi: 10.1371/journal.pgen.1004537. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.