Abstract
Sarcopenia is a generalised skeletal muscle disorder characterised by reduced muscle strength and mass and associated with a range of negative health outcomes. Currently, resistance exercise (RE) is recommended as the first-line treatment for counteracting the deleterious consequences of sarcopenia in older adults. However, whilst there is considerable evidence demonstrating that RE is an effective intervention for improving muscle strength and function in healthy older adults, much less is known about its benefits in older people living with sarcopenia. Furthermore, evidence for its optimal prescription and delivery is very limited and any potential benefits of RE are unlikely to be realised in the absence of an appropriate exercise dose. We provide a summary of the underlying principles of effective RE prescription (specificity, overload and progression) and discuss the main variables (training frequency, exercise selection, exercise intensity, exercise volume and rest periods) that can be manipulated when designing RE programmes. Following this, we propose that an RE programme that consists of two exercise sessions per week and involves a combination of upper- and lower-body exercises performed with a relatively high degree of effort for 1–3 sets of 6–12 repetitions is appropriate as a treatment for sarcopenia. The principles of RE prescription outlined here and the proposed RE programme presented in this paper provide a useful resource for clinicians and exercise practitioners treating older adults with sarcopenia and will also be of value to researchers for standardising approaches to RE interventions in future sarcopenia studies.
Keywords: sarcopenia, resistance exercise, exercise prescription, muscle strength, physical performance, older people
Key Points
Resistance exercise is currently recommended as a first-line treatment for sarcopenia.
The research–practice gap represents a challenge for clinicians and exercise practitioners delivering exercise.
Resistance exercise programmes should consist of two full-body exercise sessions per week performed with a relatively high degree of effort.
Introduction
Sarcopenia is a generalised skeletal muscle disorder characterised by reduced skeletal muscle strength and mass [1, 2] and associated with a range of adverse health outcomes [3–5] as well as high social and economic costs [6]. The revised European Working Group on Sarcopenia in Older People (EWGSOP2) definition has made it easier to identify and diagnose sarcopenia in clinical practice [1] meaning that there is a pressing need for evidence-based treatment strategies. Current clinical practice guidelines advocate resistance exercise (RE) as the primary strategy for treatment of sarcopenia [7]. Resistance exercise—also commonly referred to as weight training, strength training or resistance training—is typically exercise that requires muscles to hold or work against an applied force or weight [8]. It can involve the use of resistance machines, free weights, bodyweight exercises and resistance bands. The recommendation to use RE as a treatment for sarcopenia is underpinned by robust evidence demonstrating that RE programmes can, under controlled conditions, improve muscle strength, mass and physical performance in middle-aged and older adults [9–11].
Despite the potential of RE as a therapeutic strategy for sarcopenia, RE programmes are not routinely offered to patients [12] and there is considerable variation in those that are delivered in clinical practice [13]. This highlights the need to lessen the theory–practice gap around effective sarcopenia management and to support clinicians and exercise practitioners to deliver effective RE programmes [14, 15]. As adaptations to RE are specific to the training stimulus (i.e. the physiological stress placed on the body) induced by the exercise dose (i.e. the exercise performed), improvements in muscle strength and physical performance are likely to be realised only if the exercise dose is appropriately prescribed to each individual. The exercise dose is determined by a combination of variables including exercise frequency, volume and intensity. Understanding how to manipulate these variables effectively is key to maximising the potential of RE as a treatment for sarcopenia. Here, we build on previous discussion of RE as a countermeasure for sarcopenia [16] and will embed this information in the context of applied practice to support clinicians and exercise practitioners to design and deliver effective RE programmes to older adults with sarcopenia.
Prescribing resistance exercise for sarcopenia
Rationale
There is consistent evidence for the benefits of RE as a treatment for the individual components of sarcopenia across a range of population groups [9, 11, 17, 18]. However, evidence in older adults diagnosed with sarcopenia remains limited (see Supplementary Information available at Age and Ageing online for summary), even though RE is recommended as a first-line treatment in clinical practice [7]. A key consideration in developing a pragmatic approach for the treatment of sarcopenia is that the therapeutic potential of exercise can be realised only if older adults receive an appropriate exercise dose, yet previous work suggests that the principles of exercise prescription are often overlooked or misapplied (e.g. non-individualised, lacking progression) [13]. We therefore propose a pragmatic person-centred approach, based on established principles from sport and exercise science, to guide individualised RE prescription for older adults with sarcopenia. Such an approach can inform the design and delivery of RE in older adults with sarcopenia pending more definitive evidence from randomised controlled trials.
As older adults with sarcopenia are also likely to be at an increased risk for falls [19] and display reduced cardiorespiratory fitness [20], exercise programmes delivered to these individuals often involve a combination of exercise modes (e.g. RE, balance training, aerobic training). These multicomponent exercise programmes are likely to be the most efficacious approach for all-round fitness improvement in older adults compared to a single exercise mode alone [21–23]. However, as prescription of each exercise mode involves the manipulation of specific variables, and RE is the most efficacious method for improving muscle strength and mass in older people, the following sections of this manuscript will focus on RE alone.
Principles of exercise training
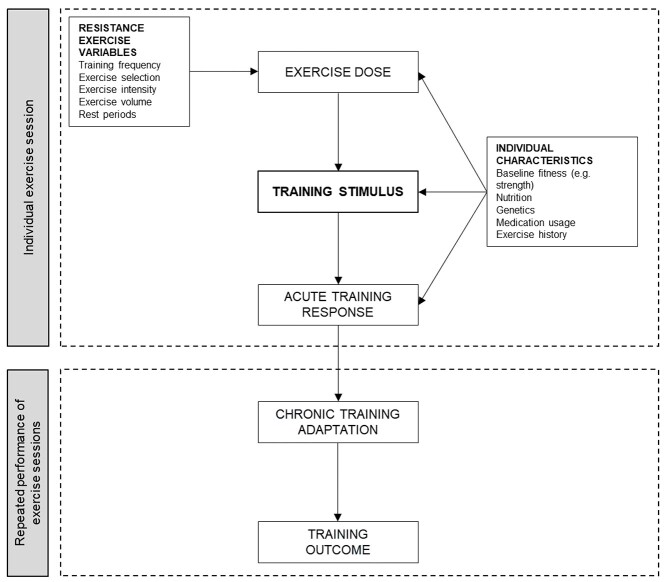
Exercise training involves the repeated and systematic performance of individual exercise sessions over a period of time with the aim of improving physical ability (e.g. muscle strength) or skill [24]. This process (Figure 1) involves prescribing an exercise dose in order to induce a training stimulus. The acute response to training and any resultant chronic training adaptation is driven by the training stimulus (i.e. the physiological stress placed on the individual). Whilst individual and contextual factors can influence the training stimulus, its primary determinant is the exercise dose [25, 26]. Several principles of exercise training are fundamental to ensure the provision of a safe, individualised and effective RE dose. These principles should be embedded in the design of any RE intervention to enable the exercise programme to stimulate positive training responses to achieve its desired outcomes. These principles are specificity, overload and progression and are defined in Table 1.
Figure 1.
The training process (adapted from Impellizzeri and colleagues [25, 26]).
Table 1.
Principles of exercise training
| Specificity | Responses to exercise training are specific to the stimulus induced by the exercise dose. |
| Overload | A greater than habitual stress or load on the body is needed to induce adaptation. |
| Progression | A gradual and systematic increase in stress placed on the body is necessary to induce continual training adaptation over time. |
In the context of exercise training, the principle of specificity refers to the idea that acute training responses and chronic training adaptations are tightly coupled to the stimulus derived from the exercise performed [27]. As such, the exercise prescribed must be specifically targeted to induce improvements in the desired outcome. For example, if a goal of the RE programme is to improve the individual’s ability to rise from a chair, then exercises that target the muscle groups and the specific movement patterns involved in this activity should be selected. Overload refers to the need for exercise to place a greater than habitual stress on the body in order for adaptation to occur [28]. Over the course of a training programme, the body continually adapts to the exercise stimulus provided. As such, there is a need to systematically increase the stress placed upon the body during training to drive continued adaptation. This is done through progression of the training stimulus [29]. Several approaches can be used to effectively guide RE progression [30] and decisions about when and how to progress the training stimulus should be individualised and consider tolerance of the exercise (e.g. is the increase in training stress manageable for the individual), specific goals of the RE programme and enjoyment. A progressive increase in stress may be achieved by manipulating one or more of the RE variables outlined in the following section.
Monitoring and evaluating the acute training response to each exercise session enables the exercise practitioner to identify when the training stimulus should be progressed or regressed to ensure appropriate overload. Ratings of perceived exertion (RPE), where the individual is asked to provide a subjective evaluation of how strenuous the exercise was, can be a useful method to guide exercise prescription [31, 32]. This approach has the added benefit of encouraging individuals to recognise the sensations of effort associated with exercise of the desired intensity. Qualitative feedback from individuals can also provide useful information about the training programme. For example, is the individual experiencing significant post-exercise muscle soreness and is this having an impact on his or her ability to perform activities of daily living or quality of life? Discussing these issues can help older adults to better understand exercise training effects and support them to actively engage in the design and delivery of their exercise programme as opposed to being passive recipients.
A proposed resistance exercise prescription for sarcopenia
Overview
The aim of this section is to provide an illustration of what a simple yet easily modifiable RE prescription for older adults with sarcopenia could involve. Exercise variables including training frequency, exercise selection, exercise intensity, volume and rest periods represent the primary considerations when designing RE programmes. Manipulating these variables can modify the stimulus and adaptations induced by RE. To complement our proposed recommendations, readers are directed to work further discussing the nuances of RE prescription in older adults [8, 16, 29, 33]. Our illustrative RE prescription for sarcopenia is presented in Table 2.
Table 2.
A proposed resistance exercise prescription for older adults with sarcopenia
| Training frequency | Two sessions per week | |
| Exercise selection |
Lower body Squat/leg press Knee extension Leg curl Calf raise |
Upper body Chest press Seated row Pull down |
| Exercise intensity |
Repetition-continuum based prescription 40–60% 1RM progressing to 70–85% 1RM |
RPE-based prescription RPE 3–5 on CR10 scale progressing to RPE 6–8 |
| Exercise volume | 1–3 sets of 6–12 repetitions | |
| Rest periods |
Within session 60–120 s between sets; 3–5 min between exercises Between sessions At least 48 h |
|
1RM, 1 Repetition Maximum (the maximal amount of weight that can be lifted for one complete repetition); RPE, Rating of Perceived Exertion; CR10, Category Ratio 10 scale (see [52] for guidance).
Training frequency
Exercise programmes for older adults typically involve between 1 and 3 RE sessions per week [34–36]. Uncertainty remains as to what the optimal training frequency is for increasing muscle strength and it remains unknown whether RE frequency alone has a significant effect on training-induced gains [37, 38]. RE programmes involving two training sessions per week may offer greater benefit compared to once weekly training for improving muscle strength, yet it remains unclear how much of a meaningful additive effect a third session per week provides [39, 40]. Substantial benefits can be gained from two RE sessions per week [10, 34, 36] and those prescribing exercise should be mindful that prescribing a greater number of RE sessions will not necessarily induce greater effects (i.e. quality over quantity). Adding in regular functional resistance–based exercises for older adults to perform at home in between scheduled exercise sessions may provide extra benefit and may also help support behaviour change and the formation of positive habits that may be important for ongoing exercise engagement [41]. A lower weekly RE frequency has the advantage of allowing the individual a greater time to recover between each exercise session while also having important resource implications for delivery. As such, two training sessions per week should represent the standard prescription for older adults with sarcopenia. However, in those individuals with low baseline muscle strength or severe sarcopenia, a single RE session per week could still confer significant benefit [39]. In these individuals, it would be appropriate for RE programmes to begin with a single weekly training session before progressing to two sessions per week over time. As the individual progresses through the training programme, increasing the number of weekly RE sessions can be an effective strategy to ensure that appropriate overload is provided.
Exercise selection
Older adults with sarcopenia should perform whole-body RE targeting the major muscle groups. Exercises that target muscles of the lower body should form the foundation of the RE programme because of their role in performing activities of daily living including walking, rising from a chair and climbing stairs [42, 43]. Exercises that involve the quadriceps, hamstrings, gluteals, calves and the muscles of the ankle and foot should be prioritised. Upper-body muscle strength is relevant for performing basic and instrumental activities of daily living such as dressing, cooking and self-care [44]. Performing exercises that require the individual to grip could have a positive effect on forearm and grip strength, which are needed to successfully perform instrumental activities of daily living. Exercises that target the back, chest, shoulder and arm muscles should also be included. Clinicians and exercise practitioners should also consider incorporating functional strength movements (e.g. repeated sit-to-stands) into the exercise prescription as these may transfer more closely into improvements in functional ability [45, 46]. If appropriate for the individual, these functional strength movements could be performed at home as a supplement to the structured RE sessions. The work of Ribeiro and colleagues discusses exercise selection in more detail [47].
For older adults with sarcopenia, decisions relating to the choice of specific exercises should be based on the individual characteristics, limitations and needs of the individual. The examples of exercises provided in Table 2 are not exhaustive and clinicians and exercise practitioners are encouraged to work with the individual to identify which exercises are most appropriate and enjoyable. Particularly in the early stages of an RE programme, the number of exercises performed may need to be limited to manage fatigue. Ensuring that exercises are performed with the correct technique should be the main consideration rather than attempting to overload an individual with too many exercises early in a training programme. As the programme develops, the training stimulus can be progressed by increasing the number of exercises performed. Those delivering exercise programmes are also encouraged to consider prescribing simple exercises that can be performed at home without equipment (e.g. multiple sets of sit-to-stands or wall press) between exercise sessions [41]. This may have the added benefit of increasing overall exercise dose and the speed with which individuals would start to feel beneficial effects, potentially aiding adherence.
Exercise intensity
Exercise intensity is typically defined in either relative (i.e. relative to the individual’s own strength capacity) or absolute (i.e. the amount of resistance used) terms and is often referred to as ‘load’. However, load and intensity are not synonymous [48] and it may be more appropriate to view what is traditionally termed intensity in terms of how much effort is required to perform the activity [49]. RE intensity has typically been prescribed based on the repetition continuum that proposes that performing a specific number of repetitions using a specific load induces specific adaptations [29]. Relative loads are typically presented as a percentage of one repetition maximum (%1RM; the maximum amount of weight that can be lifted in a single repetition; e.g. 85% 1RM) or as a Repetition Maximum (RM) load (the most weight that can be lifted for a defined number of repetitions; e.g. 6RM, 10RM). However, exercise practitioners working with older adults should be aware that the 1RM may represent a specific skill [50] and require considerable familiarisation [51]. As such, ratings of perceived exertion (RPE) may provide a more practical method to prescribe intensity [52]. An alternative approach is to prescribe RE intensity using an effort-based approach [53, 54].
A wide range of RE intensities can induce meaningful increases in muscle strength [29], although the optimal intensity for RE for older adults and those with sarcopenia remains to be determined. Previous work has suggested that higher intensity RE may be the most effective prescription for improving muscle strength [55], although this is far from definitive as RE at both moderate [56] and low intensities can induce substantial improvements [29, 57]. From an exercise prescription perspective, it appears that the most consistent message is that RE should be performed with a relatively high degree of effort [58, 59]. As a pragmatic guide, muscles should feel tense, warm or shaky by the end of the first set of an exercise. In the most simplistic terms, if older adults perform the RE until fatigue this is likely to provide an appropriate training stimulus. However, it is important to consider that an RE session that induces a substantial amount of fatigue (e.g. performing multiple sets to momentary failure) may induce too much discomfort, which could be problematic for older adults unfamiliar with RE. In addition, movement velocity (the speed the movement is performed at) also contributes to the intensity of the exercise and manipulating this can induce differential adaptation [60]. Resistance exercise performed at high speed with lighter loads (i.e. power training) is an effective strategy for improving muscle power and functional performance in older people [56] and can be incorporated into RE programmes [61]. Practitioners and clinicians should focus on the development of correct technique before encouraging movements to be performed at high velocity to reduce the chance of injury. We have provided options for how the clinician and exercise practitioner could prescribe RE intensity when working with older adults with sarcopenia in Table 2. Our suggestions are by no means definitive and are intended to support the decision making of exercise practitioners in an applied context.
In the early stages of an RE programme, the intensity prescribed is likely to be lower as the training sessions are more focused on familiarising the individual with the technical demands of exercise. Time is needed for individuals to become familiarised with the exercises at the beginning of any RE programme and it is important to emphasise the development of correct technique in these early stages. Baseline assessment of muscle strength can help to determine the initial intensity of exercises, which is often a trial-and-error approach, and clinicians and exercise practitioners should work with the individuals to ensure they are actively invested in the design and evolution of their exercise programme. Those patients with severe sarcopenia or who are especially deconditioned may see substantial benefits from RE at a lower intensity (e.g. 30–60% 1RM) or using bodyweight only [41]. In those older adults with higher baseline strength and function, intensity may need to be greater to promote positive adaptation (50–70% 1RM). Over the course of the training programme, intensity may need to progress to 70–85%1RM to optimise gains in muscular strength [33]. Repeated assessment of muscle strength (e.g. RM) and physical performance (e.g. 5-repetition sit-to-stand [62]) can help guide progression of the training dose and this process can also be used as a motivational tool with the individual to support engagement and adherence.
Exercise volume
Exercise volume refers to the amount of exercise completed during a training session and is typically represented as the product of the number of sets and repetitions of each exercise performed. An inverse relationship exists between repetitions and intensity; the higher the intensity, the fewer repetitions that are typically performed. Particularly in the early stages of an RE programme, the number of sets completed does not appear to be the primary variable responsible for increases in muscle strength with similar results observed when comparing 1–3 sets [63]. A single set of each exercise may be capable of significantly increasing muscle function and physical performance in short-term RE programmes, although longer-term gains in muscle strength may be higher when performing 2–3 sets [34, 64]. In general, sets consisting of 6–12 repetitions appear to be appropriate [28, 29, 33]. Increasing the volume of exercise, typically by increasing the number of sets and repetitions of individual exercises, is an effective strategy to ensure progressive overload throughout the programme.
Rest periods
Within an exercise session, rest periods refer to the time for recovery between sets and exercises and are largely determined by the interaction of other training variables including exercise selection, intensity and volume. Rest periods typically range from 60 to 180 s between sets and 3 to 5 min between exercises in RE programmes involving older adults. However, it remains to be determined what the optimal rest periods during RE should be. It may be that periods of 60–120 s can help to maximise muscular strength gains [65], although this is far from being definitive [34]. Especially in the early stages of an RE programme, rest periods should be largely determined based on the individual’s tolerance of the exercise stimulus and the exercise practitioner should work with the individual to ensure these are appropriate. The amount of rest between exercise sessions also represents an important consideration for RE programming. A minimum of 48 h between RE sessions is recommended. However, exercise practitioners should work with the individual to understand if a longer duration is needed between exercise sessions—for example, if fatigue or muscle soreness is having detrimental effects on the ability to perform instrumental activities of daily living on non-exercise days.
Other considerations
There are several other considerations that are also relevant to the prescription and delivery of RE in older adults. Several exercise modes (e.g. free weights, resistance bands, resistance machines) can be utilised to deliver an appropriate RE stimulus for older adults, and exercise practitioners should not view a lack of advanced equipment as a barrier to effective RE delivery. It is acknowledged that the availability of exercise equipment will be influenced by where the exercise intervention takes place. It is important to note, however, that the choice of exercise mode can influence the nature of the training stimulus; for example compared with resistance machines, free weights require extra muscular activity to stabilise and control movement [66]. In the early stages of an RE programme or in those with severe sarcopenia, there may be a preference for chair-based exercise or activities that use resistance bands or utilise the patient’s own bodyweight. While chair-based exercise may be appropriate for those with balance limitations or at the beginning of an RE programme, practitioners should aim to move beyond this exercise mode as soon as is safe because of the limited potential to progressively overload the individual. As the RE programme develops, bodyweight and resistance band exercises may also not provide enough stimulus to induce training adaptation. More advanced RE prescription could include barbells, kettlebells and medicine balls or floor-based exercises (e.g. prone back extensions). In terms of exercise order, the American College of Sports Medicine (ACSM) has recommended that multi-joint exercises be performed before single-joint exercises for a particular muscle group and that within each session the larger muscle groups be exercised before smaller muscle groups [29]. The highest priority exercises of the programme should be performed at the beginning of the exercise session [67]. Finally, the muscle action or contraction type (e.g. isometric, isokinetic) utilised during training can also influence adaptation [68].
Exercise programme duration represents an important determinant of longer-term outcomes. For example, an effective exercise prescription for falls prevention needs to include at least 50 h of challenging balance and progressive strength training [69]. It remains unknown how long RE programmes need to be to elicit meaningful and long-lasting benefits in the context of sarcopenia. However, it appears that at least 12 weeks of RE is necessary based on the evidence presented in this paper [70]. Short-duration programmes are unlikely to allow older people to become familiar with the habit of exercising and don’t enable sufficient progression of the exercise dose (e.g. from one RE session per week to two or from bodyweight exercises to free weights). While it seems reasonable to suggest that RE programmes of a longer duration would lead to greater improvements in relevant outcomes, this is only likely to be the case if the exercise is appropriately prescribed and delivered based on the fundamental principles of exercise prescription as discussed earlier.
Implications for exercise delivery and future directions
Implications for clinical and applied practice
The exercise prescription we have provided can be applied by clinicians and exercise practitioners treating older adults with sarcopenia to deliver meaningful resistance exercise in clinical practice. There are, however, several issues that need to be considered in order to maximise the potential of RE as a treatment for older adults diagnosed with sarcopenia.
In the first instance, thought needs to be given as to how to identify older adults who are likely to benefit from RE. Assessing muscle strength (e.g. grip strength, chair stand test) is a practical and time-efficient method to identify individuals with probable sarcopenia [1]. However, sarcopenia is not routinely assessed in clinical practice. In this regard, flagging risk factors (e.g. older age, those requiring oral steroid treatment, history of falls, low physical activity, multimorbidity [71]) and opportunistic screening in primary care (e.g. annual health checks using the SARC-F questionnaire [72]) could be useful. It may be appropriate to introduce sarcopenia screening within existing older people’s services, for example, those that already deliver Comprehensive Geriatric Assessment (CGA). Individuals requiring CGA will likely have risk factors for sarcopenia and warrant screening. Next steps may include improving sarcopenia awareness amongst specialist multi-disciplinary team members with discussion encouraged around implementation of assessment in acute and community settings. Knowledge and skills can then be cascaded to broaden awareness and case-finding.
Care pathway development is also needed to support delivery of RE as a treatment for sarcopenia. Specialist healthcare professionals, such as a physiotherapist, may be best to assess, design and review safe and effective RE programmes using our recommendations. Delivery could be in partnership with other rehabilitation professionals across healthcare and community settings as happens within falls prevention exercise delivery. This approach could support continued progression and long-term engagement but would require barriers to participation such as accessibility to be understood and addressed [73]. Holistic assessment of an older adult’s health, physical deficits, motivation and individualised goal setting is imperative to achieving best outcomes in clinical practice.
Issues relating to how RE is delivered (e.g. group-based or individual, supervised or home based), where it is delivered (e.g. gym, hospital, primary care, own home, community venues) and who it is delivered by (e.g. physiotherapists, specialist exercise practitioners, exercise physiologists, others) represent important considerations in the design and delivery of an exercise programme. While decision making relating to these can be constrained by systemic limitations (e.g. staff or facility availability), exercise practitioners should consider the potential effects of RE programmes delivered using different approaches. For example, as well as potential physical or functional benefits, group-based RE provides opportunity for peer support and social engagement [74], while exercise adherence is generally higher in supervised programmes [75]. At a more fundamental level, more work is needed to understand and influence the systemic limitations (e.g. commissioning, funding, facilities, equipment) to deliver RE to older adults with sarcopenia in clinical practice.
In practice, exercise programmes are often short, and patients may discontinue participation after only a few sessions. Strategies that promote ongoing engagement (e.g. beyond six weeks) in older adults with sarcopenia are needed to maximise the potential benefits of RE. All of those involved in the care of an older person including health and care professionals (e.g. physiotherapists, doctors, dieticians), family members and carers have a role to play in reinforcing positive messaging about RE [76]. Older adults may need signposting to appropriate services or support if they want to exercise at home and a package of education and knowledge transfer needs to accompany an exercise prescription. There is the need to educate older adults undertaking RE, many of whom will be unfamiliar with exercise, that post-exercise muscular soreness is a normal part of the response to RE. There is also a need to consider an individual’s specific stage of behaviour change in the design and delivery of an RE programme, for example, ensuring that older people don’t experience excessive fatigue or discomfort until they become accustomed to the sensations associated with RE (e.g. muscle fatigue, soreness) or begin to see positive effects. Failure to manage this issue carefully may have implications for attendance and adherence.
Implications for research and future directions
As highlighted, there remains a pressing need for further studies involving older adults diagnosed with sarcopenia in order to improve the evidence base in this area. Higher quality intervention studies and trials of longer duration, which incorporate substantial follow-up periods, are required. Researchers should embed the principles of RE prescription outlined in this manuscript when designing future trials in older adults with sarcopenia, and authors should report these studies in accordance with the Consensus on Exercise Reporting Template (CERT) [77]. This will enable clinicians and exercise practitioners to replicate effective programmes in clinical practice. In terms of RE programme design, questions remain about the frequency of training sessions, the intensity of exercise and the duration of exercise programmes for older adults diagnosed with sarcopenia. It is important that researchers evaluate the impact of RE on the ability to perform ADLs and quality of life and not just focus on physiological outcomes (e.g. muscle strength and mass) when designing future studies [45, 46]. More work is also needed to evaluate the minimal dose of RE needed to improve outcomes in this population. This has important implications for service design and delivery and such work could help define future clinical care guidelines for sarcopenia.
Not all the issues highlighted here need to be evaluated through intervention studies or randomised control trials; benchmarking studies that develop a comprehensive understanding of what exercise is being delivered and how it is delivered, within real-world practice, will also be helpful. Identifying pragmatic questions from patients and the public as well as from clinicians would also help to identify further avenues for research. Exploring the potential for creative approaches to exercise delivery could also help to broaden the appeal and acceptability of RE to older adults. This could include the use of remote or virtual activities to support the face-to-face delivery of RE for older people with sarcopenia. Qualitative work on how best to engage and promote adherence to RE programmes in older people with sarcopenia would also be valuable.
Conclusion
Resistance exercise is a promising intervention for the treatment of sarcopenia. However, as with other therapeutic strategies, appropriate prescription of RE is essential to maximise its beneficial effects. The limited availability of relevant studies means that it is not currently possible to provide a fully evidence-based prescription of RE for sarcopenia and there remains a need for relevant intervention studies and trials involving older adults diagnosed with sarcopenia to provide this information. This review provides a pragmatic approach where RE programmes are developed based on the fundamental principles of exercise training including specificity, overload and progression and individualised to induce the desired adaptive response in each older adult. The proposed RE prescription outlined in this paper provides a useful resource for clinicians and exercise practitioners treating older adults with sarcopenia and may also be of value to researchers for standardising approaches to RE interventions in sarcopenia studies.
Supplementary Material
Contributor Information
Christopher Hurst, AGE Research Group, Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK; NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Sian M Robinson, AGE Research Group, Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK; NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Miles D Witham, AGE Research Group, Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK; NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Richard M Dodds, AGE Research Group, Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK; NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Antoneta Granic, AGE Research Group, Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK; NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Charlotte Buckland, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK; AGILE, Chartered Society of Physiotherapy, London, UK.
Sarah De Biase, AGILE, Chartered Society of Physiotherapy, London, UK.
Susanne Finnegan, AGILE, Chartered Society of Physiotherapy, London, UK; Warwick Clinical Trials Unit, University of Warwick, Coventry, UK.
Lynn Rochester, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK; Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK.
Dawn A Skelton, Research Centre for Health (ReaCH), School of Health and Life Sciences, Glasgow Caledonian University, Glasgow, UK.
Avan A Sayer, AGE Research Group, Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, UK; NIHR Newcastle Biomedical Research Centre, Newcastle University and Newcastle upon Tyne NHS Foundation Trust, Newcastle upon Tyne, UK.
Declaration of Conflicts of Interest
DAS is a Director of Later Life Training, a not-for-profit company that delivers training to health and fitness professionals in evidence-based exercise prescription for frailer older people. All other authors have no conflict of interest to report.
Declaration of Sources of Funding
This work was supported by the National Institute for Health Research (NIHR) Newcastle Biomedical Research Centre based at the Faculty of Medical Sciences, Newcastle University and the Newcastle upon Tyne Hospitals NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
References
- 1. Cruz-Jentoft AJ, Bahat G, Bauer J et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. The Lancet 2019; 393: 2636–46. [DOI] [PubMed] [Google Scholar]
- 3. Landi F, Liperoti R, Russo A et al. Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr 2012; 31: 652–8. [DOI] [PubMed] [Google Scholar]
- 4. Landi F, Cruz-Jentoft AJ, Liperoti R et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing 2013; 42: 203–9. [DOI] [PubMed] [Google Scholar]
- 5. Tanimoto Y, Watanabe M, Sun W et al. Association of sarcopenia with functional decline in community-dwelling elderly subjects in Japan: sarcopenia and functional decline. Geriatr Gerontol Int 2013; 13: 958–63. [DOI] [PubMed] [Google Scholar]
- 6. Pinedo-Villanueva R, Westbury LD, Syddall HE et al. Health care costs associated with muscle weakness: a UK population-based estimate. Calcif Tissue Int 2019; 104: 137–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dent E, Morley JE, Cruz-Jentoft AJ et al. International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging 2018; 22: 1148–61. [DOI] [PubMed] [Google Scholar]
- 8. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA et al. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009; 41: 1510–30. [DOI] [PubMed] [Google Scholar]
- 9. Straight CR, Lindheimer JB, Brady AO, Dishman RK, Evans EM. Effects of resistance training on lower-extremity muscle power in middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med 2016; 46: 353–64. [DOI] [PubMed] [Google Scholar]
- 10. Grgic J, Garofolini A, Orazem J, Sabol F, Schoenfeld BJ, Pedisic Z. Effects of resistance training on muscle size and strength in very elderly adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med 2020; 50: 1983–99. [DOI] [PubMed] [Google Scholar]
- 11. Liu C, Latham NK, Cochrane Bone, Joint and Muscle Trauma Group . Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev 2009; 3. 10.1002/14651858.CD002759.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Offord NJ, Clegg A, Turner G, Dodds RM, Sayer AA, Witham MD. Current practice in the diagnosis and management of sarcopenia and frailty—results from a UK-wide survey. J Frailty Sarcopenia Falls 2019; 4: 71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Witham MD, Chawner M, de Biase S et al. Content of exercise programmes targeting older people with sarcopenia or frailty—findings from a UK survey. JFSF 2020; 05: 17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barton CJ, King MG, Dascombe B et al. Many physiotherapists lack preparedness to prescribe physical activity and exercise to people with musculoskeletal pain: a multi-national survey. Phys Ther Sport 2021; 49: 98–105. [DOI] [PubMed] [Google Scholar]
- 15. Sasso JP, Eves ND, Christensen JF, Koelwyn GJ, Scott J, Jones LW. A framework for prescription in exercise-oncology research: editorial. J Cachexia Sarcopenia Muscle 2015; 6: 115–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Law TD, Clark LA, Clark BC. Resistance exercise to prevent and manage sarcopenia and dynapenia. Annu Rev Gerontol Geriatr 2016; 36: 205–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Strasser B, Steindorf K, Wiskemann J, Ulrich CM. Impact of resistance training in cancer survivors: a meta-analysis. Med Sci Sports Exerc 2013; 45: 2080–90. [DOI] [PubMed] [Google Scholar]
- 18. Cheema BS, Chan D, Fahey P, Atlantis E. Effect of progressive resistance training on measures of skeletal muscle hypertrophy, muscular strength and health-related quality of life in patients with chronic kidney disease: a systematic review and meta-analysis. Sports Med 2014; 44: 1125–38. [DOI] [PubMed] [Google Scholar]
- 19. Yeung SSY, Reijnierse EM, Pham VK et al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 2019; 10: 485–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chien M-Y, Kuo H-K, Wu Y-T. Sarcopenia, cardiopulmonary fitness, and physical disability in community-dwelling elderly people. Phys Ther 2010; 90: 1277–87. [DOI] [PubMed] [Google Scholar]
- 21. Hurst C, Weston KL, McLaren SJ, Weston M. The effects of same-session combined exercise training on cardiorespiratory and functional fitness in older adults: a systematic review and meta-analysis. Aging Clin Exp Res 2019; 31: 1701–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cadore EL, Rodríguez-Mañas L, Sinclair A, Izquierdo M. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: a systematic review. Rejuvenation Res 2013; 16: 105–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cadore EL, Izquierdo M. How to simultaneously optimize muscle strength, power, functional capacity, and cardiovascular gains in the elderly: an update. Age (Dordr) 2013; 35: 2329–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Viru A, Viru M. Nature of training effects. In: Exercise and Sport Science. Philadelphia, PA: Lippincott Williams & Wilkins, 2000; 67–95. [Google Scholar]
- 25. Impellizzeri FM, Marcora SM, Coutts AJ. Internal and external training load: 15 years on. Int J Sports Physiol Perform 2019; 14: 270–3. [DOI] [PubMed] [Google Scholar]
- 26. Impellizzeri FM, Rampinini E, Marcora SM. Physiological assessment of aerobic training in soccer. J Sports Sci 2005; 23: 583–92. [DOI] [PubMed] [Google Scholar]
- 27. Coffey VG, Hawley JA. Concurrent exercise training: do opposites distract?: concurrent exercise training. J Physiol 2017; 595: 2883–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kraemer WJ, Ratamess NA. Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc 2004; 36: 674–88. [DOI] [PubMed] [Google Scholar]
- 29. Ratamess N. Progression models in resistance training for healthy adults. Med Sci Sports Exerc 2009; 41: 687–708. [DOI] [PubMed] [Google Scholar]
- 30. Buskard ANL, Jacobs KA, Eltoukhy MM et al. Optimal approach to load progressions during strength training in older adults. Med Sci Sports Exerc 2019; 51: 2224–33. [DOI] [PubMed] [Google Scholar]
- 31. Scott BR, Duthie GM, Thornton HR, Dascombe BJ. Training monitoring for resistance exercise: theory and applications. Sports Med 2016; 46: 687–98. [DOI] [PubMed] [Google Scholar]
- 32. Hurst C, Weston KL, Weston M. The effect of 12 weeks of combined upper- and lower-body high-intensity interval training on muscular and cardiorespiratory fitness in older adults. Aging Clin Exp Res 2019; 31: 661–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fragala MS, Cadore EL, Dorgo S et al. Resistance training for older adults: position statement from the National Strength and Conditioning Association. J Strength Cond Res 2019; 33: 2019–52. [DOI] [PubMed] [Google Scholar]
- 34. Borde R, Hortobágyi T, Granacher U. Dose–response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med 2015; 45: 1693–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Silva NL, Oliveira RB, Fleck SJ, Leon ACMP, Farinatti P. Influence of strength training variables on strength gains in adults over 55 years-old: a meta-analysis of dose–response relationships. J Sci Med Sport 2014; 17: 337–44. [DOI] [PubMed] [Google Scholar]
- 36. Kneffel Z, Murlasits Z, Reed J, Krieger J. A meta-regression of the effects of resistance training frequency on muscular strength and hypertrophy in adults over 60 years of age. J Sports Sci 2021; 39: 351–8. [DOI] [PubMed] [Google Scholar]
- 37. Grgic J, Schoenfeld BJ, Davies TB, Lazinica B, Krieger JW, Pedisic Z. Effect of resistance training frequency on gains in muscular strength: a systematic review and meta-analysis. Sports Med 2018; 48: 1207–20. [DOI] [PubMed] [Google Scholar]
- 38. Ralston GW, Kilgore L, Wyatt FB, Buchan D, Baker JS. Weekly training frequency effects on strength gain: a meta-analysis. Sports Med-Open 2018; 4: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Taaffe DR, Duret C, Wheeler S, Marcus R. Once-weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. J Am Geriatr Soc 1999; 47: 1208–14. [DOI] [PubMed] [Google Scholar]
- 40. Farinatti PTV, Geraldes AAR, Bottaro MF, Lima MVIC, Albuquerque RB, Fleck SJ. Effects of different resistance training frequencies on the muscle strength and functional performance of active women older than 60 years. J Strength Cond Res 2013; 27: 2225–34. [DOI] [PubMed] [Google Scholar]
- 41. Harvey JA, Chastin SFM, Skelton DA. Breaking sedentary behaviour has the potential to increase/maintain function in frail older adults. JFSF 2018; 03: 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Skelton DA, Greig CA, Davies JM, Young A. Strength, power and related functional ability of healthy people aged 65–89 years. Age Ageing 1994; 23: 371–7. [DOI] [PubMed] [Google Scholar]
- 43. Puthoff ML, Nielsen DH. Relationships among impairments in lower-extremity strength and power, functional limitations, and disability in older adults. Phys Ther 2007; 87: 1334–47. [DOI] [PubMed] [Google Scholar]
- 44. Hairi NN, Cumming RG, Naganathan V et al. Loss of muscle strength, mass (sarcopenia), and quality (specific force) and its relationship with functional limitation and physical disability: the concord health and ageing in men project. J Am Geriatr Soc 2010; 58: 2055–62. [DOI] [PubMed] [Google Scholar]
- 45. Skelton DA, McLaughlin AW. Training functional ability in old age. Physiotherapy 1996; 82: 159–67. [Google Scholar]
- 46. Skelton DA, Young A, Greig CA, Malbut KE. Effects of resistance training on strength, power, and selected functional abilities of women aged 75 and older. J Amer Geriat Soc 1995; 43: 1081–7. [DOI] [PubMed] [Google Scholar]
- 47. Ribeiro AS, Nunes JP, Schoenfeld BJ. Selection of resistance exercises for older individuals: the forgotten variable. Sports Med 2020; 50: 1051–7. [DOI] [PubMed] [Google Scholar]
- 48. Steele J. Intensity; in-ten-si-ty; noun. 1. Often used ambiguously within resistance training. 2. Is it time to drop the term altogether? Br J Sports Med 2014; 48: 1586–8. [DOI] [PubMed] [Google Scholar]
- 49. Steele J, Fisher J, Giessing J, Gentil P. Clarity in reporting terminology and definitions of set endpoints in resistance training: issues & opinions: resistance training endpoints. Muscle Nerve 2017; 56: 368–74. [DOI] [PubMed] [Google Scholar]
- 50. Buckner SL, Jessee MB, Mattocks KT et al. Determining strength: a case for multiple methods of measurement. Sports Med 2017; 47: 193–5. [DOI] [PubMed] [Google Scholar]
- 51. Amarante do Nascimento M, Borges Januário RS, Gerage AM, Mayhew JL, Cheche Pina FL, Cyrino ES. Familiarization and reliability of one repetition maximum strength testing in older women. J Strength Cond Res 2013; 27: 1636–42. [DOI] [PubMed] [Google Scholar]
- 52. Buckley JP, Borg GAV. Borg’s scales in strength training; from theory to practice in young and older adults. Appl Physiol Nutr Metab 2011; 36: 682–92. [DOI] [PubMed] [Google Scholar]
- 53. P. Fisher J, Steele J, Androulakis-Korakakis P, Smith D, Gentil P, Giessing J. The strength-endurance continuum revisited:a critical commentary of the recommendation ofdifferent loading ranges for different muscular adaptations. J Trainol 2020; 9: 1–8. [Google Scholar]
- 54. Schoenfeld BJ, Grgic J, Van Every DW, Plotkin DL. Loading recommendations for muscle strength, hypertrophy, and local endurance: a re-examination of the repetition continuum. Sports 2021; 9: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Peterson MD, Rhea MR, Sen A, Gordon PM. Resistance exercise for muscular strength in older adults: a meta-analysis. Ageing Res Rev 2010; 9: 226–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Steib S, Schoene D, Pfeifer K. Dose–response relationship of resistance training in older adults: a meta-analysis. Br J Sports Med 2010; 42: 902–14. [DOI] [PubMed] [Google Scholar]
- 57. Serra-Rexach JA, Bustamante-Ara N, Hierro Villarán M et al. Short-term, light- to moderate-intensity exercise training improves leg muscle strength in the oldest old: a randomized controlled trial. J Am Geriatr Soc 2011; 59: 594–602. [DOI] [PubMed] [Google Scholar]
- 58. Morton RW, Colenso-Semple L, Phillips SM. Training for strength and hypertrophy: an evidence-based approach. Curr Opin Physio 2019; 10: 90–5. [Google Scholar]
- 59. Fisher JP, Ironside M, Steele J. Heavier and lighter load resistance training to momentary failure produce similar increases in strength with differing degrees of discomfort. Muscle Nerve 2017; 56: 797–803. [DOI] [PubMed] [Google Scholar]
- 60. Davies TB, Kuang K, Orr R, Halaki M, Hackett D. Effect of movement velocity during resistance training on dynamic muscular strength: a systematic review and meta-analysis. Sports Med 2017; 47: 1603–17. [DOI] [PubMed] [Google Scholar]
- 61. Cadore EL, Casas-Herrero A, Zambom-Ferraresi F et al. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age 2014; 36: 773–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Dodds RM, Murray JC, Granic A et al. Prevalence and factors associated with poor performance in the 5-chair stand test: findings from the cognitive function and ageing study II and proposed Newcastle protocol for use in the assessment of sarcopenia. J Cachexia Sarcopenia Muscle 2021; 12: 308–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Abrahin O, Rodrigues R, Nascimento V, Da Silva Grigoletto MC, Sousa E, Marcal A. Single- and multiple-set resistance training improves skeletal and respiratory muscle strength in elderly women. Clin Interv Aging 2014; 9: 1775–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Galvao DA, Taaffe DR. Resistance exercise dosage in older adults: single-versus multiset effects on physical performance and body composition. J Am Geriatr Soc 2005; 53: 2090–7. [DOI] [PubMed] [Google Scholar]
- 65. Grgic J, Schoenfeld BJ, Skrepnik M, Davies TB, Mikulic P. Effects of rest interval duration in resistance training on measures of muscular strength: a systematic review. Sports Med 2018; 48: 137–51. [DOI] [PubMed] [Google Scholar]
- 66. Haff GG. Roundtable discussion: machines versus free weights. Strength and Conditioning Journal 2000; 22: 18–30. [Google Scholar]
- 67. Nunes JP, Grgic J, Cunha PM et al. What influence does resistance exercise order have on muscular strength gains and muscle hypertrophy? A systematic review and meta-analysis. Eur J Sport Sci 2021; 21: 149–57. [DOI] [PubMed] [Google Scholar]
- 68. Roig M, O’Brien K, Kirk G et al. The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: a systematic review with meta-analysis. Br J Sports Med 2009; 43: 556–68. [DOI] [PubMed] [Google Scholar]
- 69. Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JCT. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 2008; 56: 2234–43. [DOI] [PubMed] [Google Scholar]
- 70. Chen N, He X, Feng Y, Ainsworth BE, Liu Y. Effects of resistance training in healthy older people with sarcopenia: a systematic review and meta-analysis of randomized controlled trials. Eur Rev Aging Phys Act 2021; 18: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Hurst C, Murray JC, Granic A et al. Long-term conditions, multimorbidity, lifestyle factors and change in grip strength over 9 years of follow-up: findings from 44,315 UK biobank participants. Age Ageing 2021; 50: 2222–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 2016; 7: 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Cavill NA, Foster CEM. Enablers and barriers to older people’s participation in strength and balance activities: a review of reviews. JFSF 2018; 03: 105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Dismore L, Hurst C, Sayer AA, Stevenson E, Aspray T, Granic A. Study of the older adults’ motivators and barriers engaging in a nutrition and resistance exercise intervention for sarcopenia: an embedded qualitative project in the MIlkMAN pilot study. Gerontol Geriatr Med 2020; 6: 233372142092039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Picorelli AMA, Pereira LSM, Pereira DS, Felício D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother 2014; 60: 151–6. [DOI] [PubMed] [Google Scholar]
- 76. Schutzer K. Barriers and motivations to exercise in older adults. Prev Med 2004; 39: 1056–61. [DOI] [PubMed] [Google Scholar]
- 77. Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med 2016; 50: 1428–37. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.