Abstract
Background & aim
Bystander response to out-of-hospital cardiac arrest (OHCA) may relate to area-level factors, including socioeconomic status (SES). We aimed to examine whether OHCA among individuals in more disadvantaged areas are less likely to receive bystander cardiopulmonary resuscitation (CPR) compared to those in more advantaged areas.
Methods
We analysed data on OHCAs in New South Wales, Australia collected prospectively through a statewide, population-based register. We excluded non-medical arrests; arrests witnessed by a paramedic; occurring in a medical centre, nursing home, police station; or airport, and among individuals with a Do-Not-Resuscitate order. Area-level SES for each arrest was defined using the Australian Bureau of Statistics’ Index of Relative Socioeconomic Disadvantage and its relationship to likelihood of receiving bystander CPR was examined using hierarchical logistic regression models.
Results
Overall, 39% (6622/16,914) of arrests received bystander CPR (71% of bystander-witnessed). The OHCA burden in disadvantaged areas was higher (age-standardised incidence 76–87/100,000/year in more disadvantaged quintiles 1–4 versus 52 per 100,000/year in most advantaged quintile 5). Bystander CPR rates were lower (38%) in the most disadvantaged quintile and highest (42%) in the most advantaged SES quintile. In adjusted models, younger age, being bystander-witnessed, arresting in a public location, and urban location were all associated with greater likelihood of receiving bystander CPR; however, the association between area-level SES and bystander CPR rate was not significant.
Conclusions
There are lower rates of bystander CPR in less advantaged areas, however after accounting for patient and location characteristics, area-level SES was not associated with bystander CPR. Concerted efforts to engage with communities to improve bystander CPR in novel ways could improve OHCA outcomes.
Keywords: Out-of-hospital cardiac arrest, Bystander cardiopulmonary resuscitation, Socioeconomic status, Health equity, Administrative data
Introduction
Provision of cardiopulmonary resuscitation (CPR) by bystanders has been well documented to make a significant difference to survival and neurological outcomes from out-of-hospital cardiac arrest (OHCA).[1], [2] The proportion of OHCA that receive bystander CPR as documented in registries varies considerably – across countries, within countries, and even at the neighbourhood level.[3], [4], [5] Importantly, variation in CPR rates and willingness to perform CPR have been associated with individual factors such as the age and gender of arrest patients and that of bystanders[6], [7], [8]; previous CPR training[9], [10]; relationship to the arrest victim11; arrest location (whether residential or public)12; whether arrest was witnessed; and area-level sociodemographic factors, such as level of economic disadvantage, population density, and ethnic composition.[3], [13], [14], [15], [16]
A recent meta-analysis reported a significant association between community-level socio-economic status (SES) and bystander CPR and survival rates for OHCA patients.5 However, the authors highlight multiple limitations, including high heterogeneity and the need to calculate pooled effects using recalculated crude odds ratios (OR) because their methods precluded them from using adjusted OR from individual studies. In addition, their analysis was limited to studies from certain countries (n = 5) and regions, none from Australia. Area-level characteristics associated with community response to cardiac-arrest emergencies may be specific to countries or regions. Studies from North America have highlighted the relationship between bystander CPR rates and area-level racial composition, with 30–60% lower odds of receiving bystander CPR in neighbourhoods with greater proportions of Hispanic and low-income Black residents compared to predominantly white neighbourhoods.[17], [18] High-risk neighbourhoods in England (marked by a high OHCA incidence and low bystander-CPR rates) were described as those with a greater proportion of ethnic minorities, residents born outside the United Kingdom, and people working in non-managerial roles, as well as a greater level of deprivation.16 However, not all countries report this trend of variation in community response by area-level deprivation or other factors. For example, Fake et al., (2013) found no evidence of any association between bystander CPR rates and area-level socioeconomic status (SES) in Wellington, New Zealand.19 In the state of Victoria, Australia, bystander CPR in witnessed cases was found to be lower in more densely populated areas.[14], [20]
In New South Wales (NSW), Australia’s most populous state, there is a lack of research examining bystander response rates at the community or small-area level or looking at disparities associated with area-level demographic features. Understanding whether people responding to cardiac-arrest emergencies react differently in distinct areas and identifying the reasons behind any such differences is an important first step to targeting training and intervention efforts to high-risk areas.[9], [15] Therefore, the aim of this study was to examine whether people experiencing cardiac arrest in more disadvantaged areas of NSW are less likely to receive bystander CPR compared with more advantaged areas.
Methods
Study design
This study was based on a retrospective analysis of a statewide, population-based register made available by the NSW Ministry of Health. This Population Health Risks and Outcomes Register (PHROR) is maintained by the Centre for Epidemiology and Evidence at NSW Ministry of Health (MoH) and contains linked de-identified unit record data of records from (1) NSW Out-of-hospital Cardiac Arrest Registry (OHCAR): (obtained from NSW Ambulance); (2) Emergency Department Data Collection; (3) Admitted Patient Data Collection; and (4) Registry of Births, Deaths and Marriages.21 The Centre for Health Record Linkage carried out linkages of the OHCAR to data from the other three registers.22 OHCAR includes all OHCA seen by NSW ambulance who record data for each case to meet the Utstein Registry standard and definitions.23 We obtained data for the three-year period from January 2017 to December 2019. Ethical approval was obtained from The University of Sydney Human Ethics Research Committee (Ref: 2021/017).
Setting
NSW has an estimated population of eight million residents, with over three-quarters living in urban areas.24 Emergency response in NSW is provided by NSW Ambulance Emergency Medical Services (EMS), which includes road and aeromedical paramedics and doctors, as well as volunteer ambulance officers in remote areas.[21], [25] Details on the location of each arrest are available at the Local Government Area (LGA) level, an administrative unit for which boundaries are defined by each state. There are 129 LGAs in NSW, ranging in size from 5.7 km2 in major cities to 53,000 km2 in rural regions, with a population density ranging from less than one to more than 8900 people per square km.[24], [26] Information on area-level sociodemographic characteristics such as socioeconomic status, age structure, population density, and remoteness was obtained from the Australian Bureau of Statistics (ABS).[27], [28] The remoteness status of each LGA (whether urban, regional, or rural) was based on the Accessibility and Remoteness Index for Area (ARIA) score, which classifies areas based on their relative access to services.27 When part of an LGA was given a different status from the rest of the area, the LGA was assigned the ARIA status assigned to the majority of the area. The ABS Socioeconomic Index for Areas (SEIFA) classification incorporates a range of Census data related to the social and economic conditions of individuals.[28], [31] Geographic areas, including LGAs, are assigned a SEIFA decile ranking using a weighted combination of multiple socioeconomic variables. In the current study, LGAs were assigned to quintiles of relative socioeconomic disadvantage created by merging two adjacent decile rankings.28
Study cohort
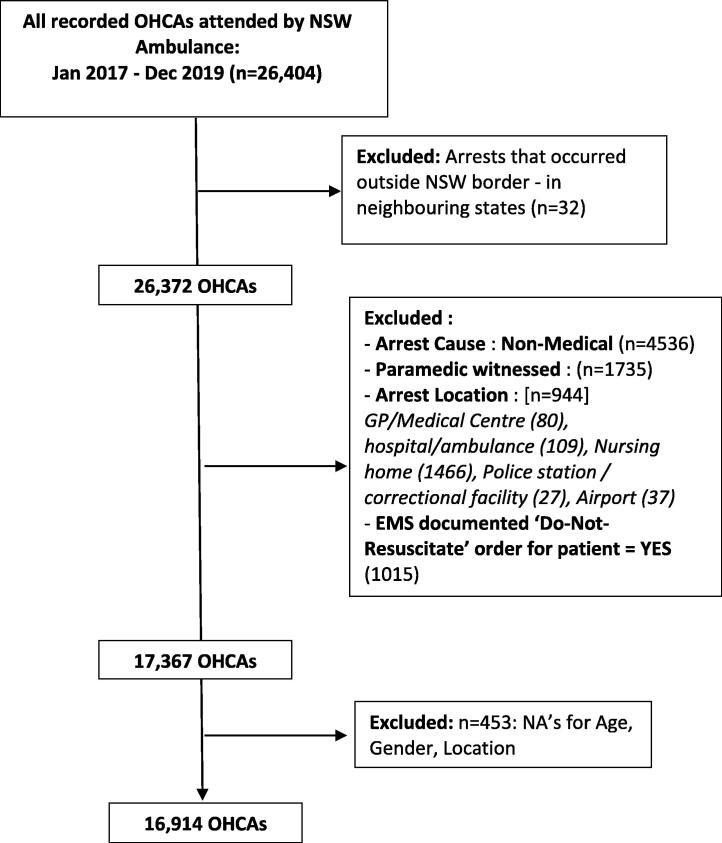
OHCAs that occurred across all age groups and those due to a medical cause were included in this study, excluding causes such as trauma, hanging, overdose, drowning, and other non-medical causes, given the differences in bystander response rates in such situations.29 In addition, arrests that were witnessed by EMS and those that occurred in a medical facility, hospital, nursing home, or police station were excluded given the likelihood that resuscitation would be provided by medical staff or other trained personnel on-site. Arrests that occurred at the airport were excluded because we could not assign SES in a way comparable to residential neighbourhoods. Patients with an active Do-Not-Resuscitate order confirmed by EMS were also excluded. These exclusion criteria align with previous research in this area.[6], [30] Fig. 1 shows these exclusions and their impact on the final study cohort.
Fig. 1.
Study cohort (Decision on Inclusion/Exclusion of variables).
Measures
Dependent variable
Bystander CPR, defined as “CPR provided by any person who happens to be near the victim and is not part of the organised emergency response system”, was categorised as a binary outcome (“yes” versus “no”).23 A small proportion of responses (3.3%) identified as “unknown/not stated” were included under the “no” category for our analyses.
Primary independent variable
The primary independent variable was SEIFA’s Index of Relative Socioeconomic Disadvantage (IRSD) – comprising low income, little or no qualifications, and low-skill occupations31 – recoded into quintiles and assigned at the LGA level (hereafter referred to as SES quintiles).
Covariates
Covariates were based on prior literature, data availability, and clinical reasoning.[11], [32] Age and sex of the OHCA victim, witnessed status (whether or not an arrest was witnessed by a bystander), and location of the OHCA – whether public (a non-residential location or public place including streets, parks, sporting grounds, school, public transport, public toilets, or vehicles) or private (a residential location) – were included in adjusted models, given the evidence that these are significant predictors of bystander CPR.[12], [33] Area-level remoteness and accessibility to services based on ARIA score was also included as a covariate in adjusted models.
Statistical analysis
Analyses were conducted at the individual level using R, version 4.1.0.34 Descriptive statistics were calculated for dependent, independent, and covariate variables before developing specific regression models (using t-tests for means and Pearson’s chi-squared tests for proportions). Unadjusted logistic regression models were used to examine the association between variables of interest and bystander CPR, then hierarchical logistic regression models were developed to examine the relationship between area-level socioeconomic status and the likelihood of receiving bystander CPR adjusted for individual and area-level covariates. We used fixed effects for individual-level variables and random-effects for area-level variables to account for clustering within LGAs. Multicollinearity testing of area-level independent variables was conducted to determine the final multivariable model (see supplementary information), with population density excluded from this final model due to high collinearity with ARIA categories (urban–rural classification). We also examined whether area-level SES was related to the odds of bystander CPR in a cohort restricted to bystander-witnessed arrests to explore the consistency of our findings (supplementary information).
Results
Of the 26,372 out-of-hospital cardiac arrests attended by NSW EMS between January 2017 and December 2019, 16,914 arrests (64%) met our inclusion criteria, with the majority of these occurring in people older than 55 years (80%), in males (65%), in a private/residential location (90%), and in urban areas (67%) (Table 1). Overall, 26% of arrests were witnessed by a bystander, but only 22% of those in a private location were witnessed, compared with 63% in a public location. Overall bystander CPR rate was 39%. Over a third (35%) of all arrests two-thirds (67%) of witnessed arrests in a private residence received bystander CPR compared with 75% of all arrests and 87% of witnessed arrests in a public location. Bystander CPR rates were highest among younger people (50% among those < 55) and males (41%), and for arrests in urban locations (40%), densely populated areas (41%) and more advantaged areas (42%).
Table 1.
Distribution of cardiac arrest characteristics (individual and area-level) by bystander CPR.
| Characteristics of OHCA cases | No Bystander CPR | Received Bystander CPR | p value |
|---|---|---|---|
| OHCA CASES (16,914) | 10,292 (60.9%) | 6622 (39.2%) | |
| Age (in years) | <0.001* | ||
| Mean: 67.8 (SD‡: ±17.7) | 70.0 (SD ± 16.4) | 64.3 (SD ± 18.9) | |
| Median: 70.0 (IQR¥:58–81) | 72 (IQR:60–82) | 67 (IQR: 55–78) | |
| NUMBER (%) | NUMBER (%) | NUMBER (%) | |
| Age group (in years) | <0.001* | ||
| < 55: 3258 (19.3) | 1639 (15.9) | 1619 (24.4) | |
| 55–75: 6974 (41.2) | 4065 (39.5) | 2909 (43.9) | |
| > 75: 6682 (39.5) | 4588 (44.6) | 2094 (31.6) | |
| Sex of OHCA patients | 0.001* | ||
| Female: 5890 (34.8) | 3741 (36.3) | 2149 (32.5) | |
| Male: 11,024 (65.2) | 6551 (63.7) | 4473 (67.5) | |
| Bystander witnessed | <0.001* | ||
| No: 12493 (73.9) [Includes Unknown 1416 (8.2)] | 9000 (87.4) | 3493 (52.7) | |
| Yes: 4421 (26.1) ^ | 1292 (12.6) | 3129 (47.3) | |
| Location of Arrest | <0.001* | ||
| Private residence: 15,219 (90.0) | 9864 (95.8) | 5355 (80.9) | |
| Public place: 1695 (10.0) | 428 (4.2) | 1267 (19.1) | |
| ARIA#categories | <0.001* | ||
| Urban: 11293 (66.8) | 6740 (65.5) | 4553 (68.8) | |
| Inner Regional: 4417 (26.1) | 2826 (26.8) | 1725 (25.1) | |
| Outer Regional & Remote: 1204 (7.1) | 798 (7.8) | 406 (6.1) | |
| Population Density people/square km | 0.009* | ||
| > 3000: 3607 (21.3) | 2134 (20.7) | 1473 (22.2) | |
| 1000–3000: 2026 (12.0) | 1171 (11.4) | 855 (12.9) | |
| 200–1000: 4921 (29.1) | 2984 (29.0) | 1937 (29.3) | |
| 10–200: 3312 (19.6) | 2044 (19.9) | 1268 (19.1) | |
| < 10: 3048 (18.0) | 1959 (19.0) | 1089 (16.4) | |
| SES*Quintiles | 0.0005* | ||
| Most advantaged quintile 5: 3890 (23.0) | 2258 (21.9) | 1632 (24.6) | |
| Quintile 4: 5527 (32.7) | 3426 (33.3) | 2101 (31.7) | |
| Quintile 3: 2629 (15.3) | 1637 (15.9) | 992 (15.0) | |
| Quintile 2: 2389 (14.1) | 1445 (14.0) | 944 (14.3) | |
| Most disadvantaged quintile 1: 2479 (14.7) | 1526 (14.8) | 953 (14.4) |
Overall bystanders used an Automated External Defibrillator (AED) in 3% of all arrests and 8% of witnessed arrests. The proportion of arrests in which AED was used was significantly greater in public settings (22% of all arrests; 28% of witnessed arrests) compared with the negligible use in private settings (0.6% of all arrests; 1.4% of witnessed arrests). Table 2 shows the distribution of key population features and arrest characteristics in LGAs grouped into SES quintiles. Each SES quintile comprised approximately 25 LGAs, with a greater proportion of urban LGAs included in the two most advantaged quintiles (4 and 5). These two quintiles also had relatively younger populations, with 16–17% of residents aged over 65 years compared with 20–21% in the more disadvantaged quintiles (1–3). The age-standardised OHCA incidence rate in the most advantaged SES area (quintile 5) was significantly lower compared with all other areas (52 per 100,000/year versus 76–87 per 100,000/year in the remaining four quintiles). The most advantaged areas (quintile 5) had higher rates of bystander CPR provision and use of an AED, faster EMS response times, and a greater proportion of cases surviving the event and reaching the hospital alive (Table 2). Distribution of population and OHCA characteristics across SES quintiles shows consistent findings in a broader cohort of ‘all EMS-attended medical cause arrests in NSW’ and is described in Supplementary section Table S1.
Table 2.
Population features and cardiac arrest characteristics across Local Government Areas (LGAs) in SES quintiles.
| Most disadvantaged quintile 1 |
Quintile 2 |
Quintile 3 |
Quintile 4 |
Most advantaged quintile 5 |
P value | |
|---|---|---|---|---|---|---|
| POPULATION FEATURES (LGAs) | ||||||
| Total Persons | 880,912 | 1,047,654 | 928,383 | 2,538,241 | 2,593,051 | |
| Prop Age > 65yrs | <0.001* | |||||
| Mean (SD) | 21% ±5% | 20% ±5% | 21% ±5% | 17% ±5% | 16% ±4% | |
| Range | (11–31%) | (10–29%) | (11–31%) | (7–27%) | (6–26%) | |
| Pop Dens per/km2 | <0.001* | |||||
| Median | 1.8 | 2.52 | 5.14 | 91.17 | 1271.57 | |
| Range | (0.03–3308.6) | (0.11–3393.2) | (0.1–490.1) | (1.02–8997.3) | (0.01–7884.5) | |
| Total LGAs (number) | 26 | 26 | 26 | 25 | 26 | |
| Urban LGAs | 2 | 3 | 2 | 12 | 21 | |
| Inner regional LGAs | 8 | 9 | 16 | 10 | 4 | |
| Outer regional/remote LGAs# | 16 | 14 | 8 | 3 | 1 | |
| ARREST CHARACTERISTICS: Number (%) | ||||||
| Total arrests (16,914) | 2479 (14.7) | 2389 (14.1) | 2629 (15.5) | 5527 (32.7) | 3890 (23.0) | |
| Crude Incidence rate/100,000 persons/year | 93.8 | 76.0 | 94.4 | 72.6 | 50.0 | <0.001* |
| Age-Adjusted rate/100,000 persons/year | 87.14 | 82.37 | 76.55 | 76.1 | 52.13 | <0.001* |
| Age of arrest patients | ||||||
| Mean (SD) | 67.4 (±17.1) | 66.7 (±18.4) | 68.4 (±16.9) | 67.3 (±17.8) | 68.8 (±17.8) | <0.001* |
| Sex of arrest patients | <0.001* | |||||
| Female (n = 5890) | 816 (32.9) | 810 (33.9) | 890 (33.9) | 1980 (35.8) | 1394 (35.8) | |
| Male (n = 11024) | 1663 (67.1) | 1579 (66.1) | 1739 (66.1) | 3547 (64.2) | 2496 (64.2) | |
| Location of arrests | <0.001* | |||||
| Private residence (n = 15,219) | 2257 (91.0) | 2192 (91.8) | 2381 (90.6) | 4990 (90.3) | 3399 (87.4) | |
| Public place (n = 1695) | 222 (9.0) | 197 (8.2) | 248 (9.4) | 537 (9.7) | 491 (12.6) | |
| Bystander witnessed | <0.001* | |||||
| No (n = 8034) | 1185 (74.5) | 1163 (74.9) | 1250 (73.1) | 2676 (74.3) | 1760 (71.8) | |
| YES (n = 2871) | 406 (25.5) | 390 (25.1) | 460 (26.9) | 924 (25.7) | 691 (28.2) | |
| Bystander response | ||||||
| CPR provided (n = 6622) | 953 (38.4) | 944 (39.5) | 992 (37.7) | 2101 (38.0) | 1632 (42.0) | <0.001* |
| No CPR (n = 10292) | 1526 (61.6) | 1445 (60.5) | 1637 (62.3) | 3426 (62.0) | 2258 (58.0) | |
| AED Used (n = 456) | 61 (2.5) | 39 (1.6) | 61 (2.3) | 150 (2.7) | 145 (3.7) | <0.001* |
| No AED (n = 16458) | 2418 (97.5) | 2350 (98.4) | 2568 (97.7) | 5377 (97.3) | 3745 (96.3) | |
| EMS response (min:secs): Mean (SD) | 13.3 (±12.1) | 10.7 (±9.1) | 12.7 (±11.3) | 11.1 (±13.8) | 11.1 (±7.8) | <0.001* |
| EMS-attempted resuscitations(n = 6911) | 1009 (40.7) | 1036 (43.4) | 981 (37.3) | 2229 (40.3) | 1656 (42.6) | <0.001* |
| Initial rhythm shockable (n = 2112) | 281 (11.3) | 277 (11.6) | 328 (12.5) | 687 (12.4) | 539 (13.9) | <0.001* |
| Any ROSC‡(n = 2265) | 285 (11.5) | 333 (13.9) | 296 (11.3) | 736 (13.3) | 616 (15.8) | <0.001* |
| Survived event/to ED^(n = 1761) | 220 (8.9) | 258 (10.8) | 245 (9.3) | 562 (10.2) | 476 (12.2) | <0.001* |
| Survived to hospital discharge (n = 755) | 88 (3.6) | 99 (4.2) | 113 (4.3) | 238 (4.3) | 217 (5.6) | 0.001* |
| Survived to discharge in Utstein subset∞(n = 422) | 47 (26.7) | 50 (27.3) | 67 (31.2) | 137 (30.0) | 121 (32.7) | 0.568 |
Note: NSW OHCAR records data as per Utstein Registry standard and definitions.23
ARIA Index: LGAs have been grouped into 'Urban (major cities)', 'Inner regional towns' and the more remote 'Outer regional and remote areas') based on Accessibility and Remoteness Index of Australia (ARIA).
In some LGAs, certain areas may be classified as 'Inner regional' while remainder could be 'Outer regional'. Here we have used the ARIA classification that is applicable to majority of the region. Note that 'Outer regional/remote' LGAs in Q1 and Q2 contributed to less than 20% of OHCA cases given that these are sparsely populated areas.
ROSC: Return of Spontaneous Circulation.
ED: Emergency department.
Utstein subset (n = 422): case definition: Bystander-witnessed arrest, shockable rhythm, EMS-attempted resuscitation.
In unadjusted models, younger age, being male, being witnessed, arresting in a public place, an urban area, densely populated locations, or more advantaged areas were each associated with greater odds of receiving bystander CPR (Table 3). In the hierarchical multivariable model, age, witnessed status, location of arrest (public or private residence), and remoteness and accessibility index (urban, regional or rural) were significantly associated with the odds of receiving bystander CPR and after controlling for these factors, we found no significant variation across the SES quintiles (Table 4).
Table 3.
Unadjusted/Crude Odds Ratios for bystander CPR provision.
| Variable | Bystander CPR Odds Ratio- Crude | 95% CI | p value |
|---|---|---|---|
| CARDIAC ARREST CHARACTERISTICS | |||
| Age (OHCA patient) | |||
| < 55 years | Reference | ||
| 55–75 years | 0.72 | 0.67–0.79 | <0.001* |
| > 75 years | 0.46 | 0.42–0.50 | <0.001* |
| Gender (OHCA patient) | |||
| Male | Reference | ||
| Female | 0.84 | 0.79–0.90 | <0.001* |
| Witnessed status | |||
| Witnessed by bystander | Reference | ||
| Not witnessed by bystander | 0.16 | 0.15–0.17 | <0.001* |
| Location of Arrest | |||
| Public location | Reference | ||
| Private/Residential | 0.18 | 0.16–0.21 | <0.001* |
| AREA LEVEL CHARACTERISTICS | |||
| Population Density/km2 | |||
| Very high density > 3000 | Reference | ||
| 1000–3000 | 1.04 | 0.86–1.27 | 0.680 |
| 200–1000 | 1.01 | 0.87–1.17 | 0.904 |
| 10–200 | 0.90 | 0.77–1.03 | 0.134 |
| Very low density < 10 | 0.78 | 0.68–0.90 | <0.001* |
| ARIA categories | |||
| Urban areas | Reference | ||
| Inner regional areas | 0.86 | 0.77–0.95 | 0.004* |
| Outer regional and remote areas | 0.72 | 0.62–0.83 | <0.001* |
| SES_Quintiles | |||
| Most advantaged quintile 5 | Reference | ||
| Quintile 4 | 0.85 | 0.74–0.98 | <0.025* |
| Quintile 3 | 0.80 | 0.69–0.93 | <0.004* |
| Quintile 2 | 0.77 | 0.65–0.91 | 0.002* |
| Most disadvantaged quintile 1 | 0.77 | 0.66–0.91 | 0.002* |
Note: Odds ratios are from logistic regression models except for area-level variables (Population density, ARIA, SES) which were calculated from generalised models including random effects to account for clustering at the area (LGA) level.
Table 4.
Adjusted odds ratios for provision of bystander CPR across SES quintiles after controlling for known confounding variables.
| Variable | Bystander CPR Odds Ratio- Adjusted |
95% CI | p value |
|---|---|---|---|
| AGE (OHCA patient) | |||
| < 54 years | Reference | ||
| 55–74 Years | 0.70 | 0.64–0.77 | <0.001* |
| > 75 Years | 0.47 | 0.43–0.52 | <0.001* |
| Gender (OHCA patient) | |||
| Male | Reference | ||
| Female | 1.02 | 0.94–1.09 | 0.673 |
| Witnessed status | |||
| Witnessed by bystander | Reference | ||
| Not witnessed by bystander | 0.18 | 0.17–0.20 | <0.001* |
| Location of Arrest | |||
| Public location | Reference | ||
| Private/Residential | 0.32 | 0.29–0.37 | <0.001* |
| ARIA categories | |||
| Urban areas | Reference | ||
| Inner regional areas | 0.86 | 0.75–0.99 | 0.036* |
| Outer regional/remote areas | 0.74 | 0.62–0.90 | <0.002* |
| SES_Quintiles | |||
| Most advantaged quintile 5 | Reference | ||
| Quintile 4 | 0.89 | 0.77–1.02 | 0.103 |
| Quintile 3 | 0.92 | 0.77–1.11 | 0.403 |
| Quintile 2 | 0.90 | 0.74–1.08 | 0.257 |
| Most disadvantaged quintile 1 | 0.93 | 0.77–1.12 | 0.426 |
Note: Population density not included in final model due to multicollinearity with ARIA variable – see Supplementary section examining multicollinearity and explanation of reasons for preference given to including ARIA over Population density.
In sensitivity analyses, we restricted the cohort to: (a) arrests witnessed by a bystander (n = 4421, 26% of study cohort) and (b) arrests in urban areas (n = 11,293, 67% of study cohort) (Tables S2–S5). In hierarchical multivariable models restricted to the witnessed cohort, there was a significant relationship with SES quintile, compared with the most advantaged (quintile 5), bystander CPR was less likely in more disadvantaged quintiles: quintile 2 (OR: 0.68; 95%CI: 0.52–0.88), quintile 4 (OR: 0.79; 95%CI: 0.64–0.96) (Table S3). Additionally, there was no longer an association between an area’s urban–rural status and the likelihood of receiving bystander CPR. The sensitivity analysis restricted to the urban cohort was consistent with the main results with no association of area-level SES and the odds of receiving bystander CPR (Tables S4 and S5).
Discussion
In a study cohort that included both bystander-witnessed and un-witnessed arrests, bystander CPR rates appeared higher in the most advantaged areas, but after accounting for age, witnessed status, public place, and urban location in hierarchical models, area-level socioeconomic disadvantage was not significantly associated with rates of bystander CPR. In analyses restricted to bystander-witnessed arrests only, there was an association, with some of the more disadvantaged quintiles having lower odds of bystander CPR compared with the most advantaged SES quintile but the odds by area-level remoteness and accessibility becoming non-significant.
This relationship between area-level socioeconomic disadvantage (based on factors such as income level and median real-estate prices) and lower odds of bystander CPR has been reported by studies analysing cohorts restricted to witnessed cases or with EMS-attempted resuscitation in the United States, England and Taiwan.[13], [16] Other studies have found associations between area-level minority population groups distribution and bystander CPR rates.[27], [30] Area-level socioeconomic disadvantage and a greater proportion of ethnic-minority residents may be correlated and together explain lower bystander CPR.16 However, not all studies have found an association between bystander CPR rates and area-level disadvantage.[14], [19] For example, Fake et al., (2013) did not link community disadvantage to bystander OHCA response in Wellington, New Zealand.19 Population density may also be a factor in the provision of bystander CPR, and our study identified slightly greater odds of receiving bystander CPR among arrests in more populated and urban locales across NSW. However, studies including one in the neighbouring state of Victoria, Australia have found the converse: bystander CPR rates were lower in more densely populated urban areas.[14], [20]
The bystander CPR rates we observed are comparable to rates reported by cardiac-arrest registries in other states of Australia, as well as in several other countries that maintain cardiac-arrest registries.[14], [36], [37] In our data, bystander AED use was very low (<1%) in all arrests occurring at home, which constituted over 90% of cardiac arrests from a medical cause. We were underpowered to examine variation in AED use by area-level SES, but this finding draws attention to the huge gap in a modifiable factor that significantly impacts outcomes for OHCA. Research into expanding the use of defibrillators has examined options such as dispatch of first responders equipped with AEDs and strengthening a citizen-responder system (especially in remote areas); making public AEDs accessible for longer hours; and drone delivery systems, all of which may make a difference to OHCA outcomes in the future. Innovative solutions addressing residential OHCAs that are least likely to have access to public AEDs currently are especially required.
The findings of this study suggest that bystander CPR may be one of the factors that lower-SES communities can address, but that a combination of activities may be needed to address the larger problem of higher OHCA incidence in lower-SES areas to improve overall outcomes. Our study also highlights the disproportionately higher burden of OHCA in less advantaged areas across the state of New South Wales, Australia, a finding consistent with other studies.13 Future policy measures should design interventions to address underlying cardiovascular risk factors to achieve improvement in heart health within lower-SES communities along with strategies to address the early identification of cardiovascular disease. Public-health programs could also focus on OHCA recognition, the chain of survival, and tailoring messaging on the importance of CPR training for family, carers, and friends of people with underlying heart disease in these areas.38
We note the current study has several limitations inherent to observational study designs. However, the registry data we integrated was prospectively collected and includes every OHCA attended by NSW Ambulance, a major strength. Although the study setting has a large population, relatively few OHCA occurred in some lower SES quintiles, reducing the power of analyses examining SES. In addition, our main analyses included unwitnessed arrests, where it is often impossible to know how much time has elapsed since a person experienced an OHCA and thus difficult to assess if it may have seemed futile to attempt CPR. All emergency calls in NSW receive telephone assistance and CPR guidance when an OHCA is suspected by the call-taker.35 Information on whether bystander response was self-initiated or followed resuscitation guidance from emergency call-takers was not recorded specifically in our dataset. While some information was recorded on whether the call-taker provided instructions (Yes/No/Unknown or Unrecorded), it was unrecorded for 52% of bystander-witnessed arrests and 55% of bystander-unwitnessed arrests and this precluded analysis. Hence, the influence of call-taker instructions is uncertain. Also, there was insufficient data on quality of CPR and bystander characteristics. There is some evidence that telephone guidance increases the odds of bystander CPR; however, there is mixed data on whether the quality of such guided CPR provides the same survival benefits as CPR performed by trained responders.[39], [40] Community CPR training rates have been associated with bystander CPR rates in Australia and overseas.[9], [10] Future studies to better understand whether CPR was self-initiated or if guidance by emergency call-takers was necessary for bystanders to intervene could provide greater insight into where training efforts should be targeted. Like other studies, our results have underlined the significantly poorer outcomes for arrests that occur at home, irrespective of area-level disadvantage.[41], [42] This finding highlights the need to develop innovative strategies in education and training of the wider community, as well as approaches to reach out to population groups that may be less likely to have received recent CPR training. Widescale education programs that target large sections of society, encourage a culture of action, and build community members’ confidence and willingness to respond to a cardiac-arrest emergency can make a significant difference to OHCA outcomes.[43], [44] In-depth analyses to understand factors such as age and gender, attitudes to learning and administering CPR within various population subgroups, and barriers and facilitators to training and responding to an OHCA emergency would support the design and implementation of tailored strategies to increase training and confidence to perform CPR and, in turn, increase bystander CPR rates in the community.
Conclusions
Overall, only a quarter of cardiac arrests in the community were witnessed, and about a third of witnessed arrests did not receive bystander CPR. After controlling for relevant factors, there was no association in the overall cohort between area-level socioeconomic disadvantage and the odds of receiving bystander CPR in our study cohort, but regional and remote areas had lower odds of bystander response compared with urban areas. The restricted analysis of witnessed-only arrests identified a significant but small association with socioeconomic disadvantage index. In absolute terms, bystander CPR rates were lower in more disadvantaged areas and coupled with the higher rates of OHCA and poorer access to healthcare services in more disadvantaged areas, our findings highlight the disproportionate burden of OHCA in less advantaged areas of NSW. A concerted effort to engage with larger sections of NSW communities and develop simple, scalable programs focussing on bystander response education would likely translate into higher bystander-initiated response rates and positive outcomes for OHCA.
CRediT authorship contribution statement
Sonali Munot: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Data curation, Writing – original draft, Visualization, Project administration. Emily J. Rugel: Conceptualization, Writing – review & editing, Supervision. Amy Von Huben: Formal analysis, Software, Data curation, Writing – review & editing. Simone Marschner: Writing – review & editing. Julie Redfern: Conceptualization, Funding acquisition. Sandra Ware: Writing – review & editing. Clara K. Chow: Conceptualization, Funding acquisition, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
This project is funded by the National Health and Medical Research Council partnership grant [APP1168950]. JR is supported by a Career Development Fellowship [APP1143538]. Munot S and AVH are supported by a Westmead Applied Research Centre PhD scholarship and Munot S additionally by a Charles Perkins Centre Westmead supplementary scholarship. CKC is supported by a NHMRC Investigator grant [APP1195326]. No funding source had involvement in the study design, collection, analysis, data interpretation, or manuscript drafting. We would like to acknowledge Lee Taylor and Michael Nelson from the NSW Ministry of Health. PHROR data was provided by the NSW Ministry of Health in accordance with ethical approval.
Data statement
Data is confidential and we do not have sharing permissions.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100205.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Sasson C., Rogers M.A., Dahl J., Kellerman A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 2.Hasselqvist-Ax I., Riva G., Herlitz J., et al. Early Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2015;372(24):2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 3.Starks M.A., Schmicker R.H., Peterson E.D., et al. Resuscitation Outcomes Consortium (ROC). Association of Neighborhood Demographics With Out-of-Hospital Cardiac Arrest Treatment and Outcomes: Where You Live May Matter. JAMA Cardiol. 2017;2(10):1110–1118. doi: 10.1001/jamacardio.2017.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gräsner J.T., Lefering R., EuReCa K.RW., et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Lee S., Ahn K.O., Cha M.I. Community-level socioeconomic status and outcomes of patients with out-of-hospital cardiac arrest: a systematic review and meta-analysis. Medicine. 2021;100:e24170. doi: 10.1097/MD.0000000000024170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blewer A.L., McGovern S.K., Schmicker R.H., et al. Gender Disparities Among Adult Recipients of Bystander Cardiopulmonary Resuscitation in the Public. Circ Cardiovasc Qual Outcomes. 2018;11:e004710. doi: 10.1161/CIRCOUTCOMES.118.004710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park H.J., Jeong W.J., Moon H.J., et al. Factors Associated with High-Quality Cardiopulmonary Resuscitation Performed by Bystander. Emerg Med Int. 2020;2020:8356201. doi: 10.1155/2020/8356201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krammel M., Schnaubelt S., Weidenauer D., et al. Gender and age-specific aspects of awareness and knowledge in basic life support. PLoS One. 2018;3:e0198918. doi: 10.1371/journal.pone.0198918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bray J.E., Straney L., Smith K., et al. Regions With Low Rates of Bystander Cardiopulmonary Resuscitation (CPR) Have Lower Rates of CPR Training in Victoria, Australia. J Am Heart Assoc. 2017;6:e005972. doi: 10.1161/JAHA.117.005972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson M.L., Cox M., Al-Khatib S.M., et al. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sato N., Matsuyama T., Kitamura T., et al. Disparities in Bystander Cardiopulmonary Resuscitation Performed by a Family Member and a Non-family Member. J Epidemiol. 2021;31:259–264. doi: 10.2188/jea.JE20200068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swor R.A., Jackson R.E., Compton S., et al. Cardiac arrest in private locations: different strategies are needed to improve outcome. Resuscitation. 2003;58:171–176. doi: 10.1016/s0300-9572(03)00118-7. [DOI] [PubMed] [Google Scholar]
- 13.van Nieuwenhuizen B.P., Oving I., Kunst A.E., et al. Socio-economic differences in incidence, bystander cardiopulmonary resuscitation and survival from out-of-hospital cardiac arrest: A systematic review. Resuscitation. 2019;141:44–62. doi: 10.1016/j.resuscitation.2019.05.018. [DOI] [PubMed] [Google Scholar]
- 14.Straney L.D., Bray J.E., Beck B., Bernard S., Lijovic M., Smith K. Are sociodemographic characteristics associated with spatial variation in the incidence of OHCA and bystander CPR rates? A population-based observational study in Victoria, Australia. BMJ Open. 2016;6:e012434. doi: 10.1136/bmjopen-2016-012434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fosbøl E.L., Dupre M.E., Strauss B., et al. Association of neighborhood characteristics with incidence of out-of-hospital cardiac arrest and rates of bystander-initiated CPR: implications for community-based education intervention. Resuscitation. 2014;85:1512–1517. doi: 10.1016/j.resuscitation.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Brown T.P., Booth S., Hawkes C.A., et al. Characteristics of neighbourhoods with high incidence of out-of-hospital cardiac arrest and low bystander cardiopulmonary resuscitation rates in England. Eur Heart J Qual Care Clin Outcomes. 2019;5:51–62. doi: 10.1093/ehjqcco/qcy026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moon S., Bobrow B.J., Vadeboncoeur T.F., et al. Disparities in bystander CPR provision and survival from out-of-hospital cardiac arrest according to neighborhood ethnicity. Am J Emerg Med. 2014;32:1041–1045. doi: 10.1016/j.ajem.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Sasson C., Magid D.J., Chan P., et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fake A.L., Swain A.H., Larsen P.D. Survival from out-of-hospital cardiac arrest in Wellington in relation to socioeconomic status and arrest location. N Z Med J. 2013;126:28–37. [PubMed] [Google Scholar]
- 20.Nehme Z., Andrew E., Cameron P.A., et al. Population density predicts outcome from out-of-hospital cardiac arrest in Victoria, Australia. Med J Aust. 2014;200:471–475. doi: 10.5694/mja13.10856. [DOI] [PubMed] [Google Scholar]
- 21.Dyson S. NSW Ambulance Cardiac Arrest Registry 2017 Report. Rozelle (New South Wales, Australia): NSW Ambulance, 2019. (Accessed 15 June 2021, at https://www.ambulance.nsw.gov.au/__data/assets/pdf_file/0005/552452/NSW-Ambulance-Cardiac-Arrest-Registry-Report-2017.pdf).
- 22.Centre for Health Record Linkage (CHeReL). [Internet]. New South Wales and Australian Capital Territory, Australia. (Accessed 15 December 2021 at https://www.cherel.org.au/).
- 23.Perkins G.D., Jacobs I.G., Nadkarni V.M., et al. Utstein collaborators. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American heart association, European resuscitation council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 24.Australian Bureau of Statistics (Australia). Population Size and growth. ‘Table 04. Estimated Resident Population, States and Territories (Number)’, times series spreadsheets, cat no. 3101.0 Australian Demographic Statistics, 2019. (Accessed 10 June 2021, at https://www.abs.gov.au/AUSSTATS/abs@.nsf/mf/3101.0).
- 25.New South Wales Ambulance. [Internet]. New South Wales, Australia: Ambulance services: Operations. (Accessed 15 December 2021 at https://www.ambulance.nsw.gov.au/our-services/operations accessed December 2021).
- 26.Australian Bureau of Statistics (Australia) - Quickstats, 2016. (Accessed 15 May 2021, at https://www.abs.gov.au/websitedbs/D3310114.nsf/Home/2016%20search%20by%20geography).
- 27.Australian Bureau of Statistics (Australia). Australian Statistical Geography Standard (ASGS): Volume 5 - Remoteness Structure, cat. no. 1270.0.55.005, 2016. (Accessed 15th March 2021, at 1270.0.55.005 - Australian Statistical Geography Standard (ASGS): Volume 5 - Remoteness Structure, July 2016).
- 28.Australian Bureau of Statistics (Australia). Socio-Economic Indexes for Areas (SEIFA), Australia, 2016; ‘Tables 2 in Local Government Area (LGA) SEIFA Summary, 2016; Index of Relative Socio-economic Disadvantage, 2016, cat. no. 2033.0.55.001. (Accessed 05 March 2021, at https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016?OpenDocument).
- 29.Deasy C., Bray J., Smith K., et al. Traumatic out-of-hospital cardiac arrests in Melbourne, Australia. Resuscitation. 2012;83:465–470. doi: 10.1016/j.resuscitation.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 30.Lee S.Y., Song K.J., Shin S.D., et al. A disparity in outcomes of out-of-hospital cardiac arrest by community socioeconomic status: A ten-year observational study. Resuscitation. 2018;126:130–136. doi: 10.1016/j.resuscitation.2018.02.025. [DOI] [PubMed] [Google Scholar]
- 31.Australian Bureau of Statistics (Australia). Socio-Economic Indexes for Areas (SEIFA)– Technical paper, 2006; latest issue released 26 March 2008, cat. no. 2039.0.55.001, 2008. (Accessed 05 March 2021, at https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2039.0.55.0012006?OpenDocument).
- 32.Dobbie F., MacKintosh A.M., Clegg G., Stirzaker R., Bauld L. Attitudes towards bystander cardiopulmonary resuscitation: Results from a cross-sectional general population survey. PLoS One. 2018;13:e0193391. doi: 10.1371/journal.pone.0193391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karlsson V., Dankiewicz J., Nielsen N., et al. Association of gender to outcome after out-of-hospital cardiac arrest–a report from the International Cardiac Arrest Registry. Crit Care. 2015;19:182. doi: 10.1186/s13054-015-0904-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2019. (Accessed 3 May 2020, at URL https://www.R-project.org/).
- 35.New South Wales Ambulance. [Internet]. Other Corporate Publications: Out-of-hospital cardiac arrest. (Accessed on 15 December 2021, at https://www.ambulance.nsw.gov.au/about-us/corporate-publications).
- 36.Ball J, Nair R, Sathish-Kumar K. Victorian Ambulance Cardiac Arrest Registry Annual report 2019-20; Doncaster (Victoria, Australia): Produced by Centre for Research and Evaluation, Ambulance Victoria, 2021. (Accessed 10 April 2021, at https://www.ambulance.vic.gov.au/wp-content/uploads/2021/02/VACAR-Annual-Report-2019-2020_FINAL_Feb2021.pdf).
- 37.London Ambulance Service, NHS Trust: Cardiac Arrest Annual Report 2018/19. London: Produced by Clinical Audit and Research Unit, LAS, NHS trust, 2021. (Accessed 11 Feb 2021, at https://www.londonambulance.nhs.uk/wp-content/uploads/2020/01/Cardiac-Arrest-Annual-Report-2018-2019.pdf).
- 38.Blewer A.L., Schmicker R.H., Morrison L.J., et al. Variation in Bystander Cardiopulmonary Resuscitation Delivery and Subsequent Survival From Out-of-Hospital Cardiac Arrest Based on Neighborhood-Level Ethnic Characteristics. Circulation. 2020;141:34–41. doi: 10.1161/CIRCULATIONAHA.119.041541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang Y., Meng Q., Munot S., Nguyen T.N., Redfern J., Chow C.K. Assessment of Community Interventions for Bystander Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020;3:e209256. doi: 10.1001/jamanetworkopen.2020.9256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee Y.J., Hwang S.S., Shin S.D., Lee S.C., Song K.J. Effect of National Implementation of Telephone CPR Program to Improve Outcomes from Out-of-Hospital Cardiac Arrest: an Interrupted Time-Series Analysis. J Korean Med Sci. 2018;33:e328. doi: 10.3346/jkms.2018.33.e328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shah M., Bartram C., Irwin K., et al. Evaluating Dispatch-Assisted CPR Using the CARES Registry. Prehosp Emerg Care. 2018;22:222–228. doi: 10.1080/10903127.2017.1376133. [DOI] [PubMed] [Google Scholar]
- 42.Ting P., Ho A., Lin X., et al. Nationwide trends in residential and non-residential out-of-hospital cardiac arrest and differences in bystander cardiopulmonary resuscitation. Resuscitation. 2020;151:103–110. doi: 10.1016/j.resuscitation.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 43.Hansen S.M., Hansen C.M., Folke F., et al. Bystander Defibrillation for Out-of-Hospital Cardiac Arrest in Public vs Residential Locations. JAMA Cardiol. 2017;2:507–514. doi: 10.1001/jamacardio.2017.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Perkins G.D., Lockey A.S., de Belder M.A., Moore F., Weissberg P., Gray H. Community Resuscitation Group. National initiatives to improve outcomes from out-of-hospital cardiac arrest in England. Emerg Med J. 2016;33:448–451. doi: 10.1136/emermed-2015-204847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.