This systematic review and meta-analysis evaluates the risk of both all-cause and cause-specific mortality among persons with autism spectrum disorder or attention-deficit/hyperactivity disorder and their first-degree relatives.
Key Points
Question
Are persons with autism spectrum disorder (ASD) or attention-deficit/hyperactivity disorder (ADHD) at a higher risk of dying compared with the general population?
Findings
In this systematic review and meta-analysis of 27 studies, persons with ASD or ADHD had higher mortality rates than the general population. When causes of death were examined, ASD and ADHD were associated with higher mortality due to unnatural causes (eg, injury, poisoning, and other), and only persons with ASD had an increased risk of mortality from natural causes of death (eg, neurologic, respiratory system, and cancer).
Meaning
Having ASD or ADHD may be associated with higher mortality risks.
Abstract
Importance
Autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) are childhood-onset disorders that may persist into adulthood. Several studies have suggested that they may be associated with an increased risk of mortality; however, the results are inconsistent.
Objective
To assess the risk of mortality among persons with ASD or ADHD and their first-degree relatives.
Data Sources
A search of MEDLINE, Embase, Scopus, Web of Science, and PsycINFO (published from inception to April 1, 2021) was supplemented by searching reference lists of the retrieved articles.
Study Selection
Cohort and case-control studies that reported mortality rate ratios (RRs) in persons with ASD or ADHD and/or their first-degree relatives compared with the general population or those without ASD/ADHD were included.
Data Extraction and Synthesis
Screening, data extraction, and quality assessment were performed by at least 2 researchers independently. A random-effects model was used to meta-analyze individual studies and assessed heterogeneity (I2).
Main Outcomes and Measures
All-cause mortality in association with ASD or ADHD. Secondary outcome was cause-specific mortality.
Results
Twenty-seven studies were included, with a total of 642 260 individuals. All-cause mortality was found to be higher for persons with ASD (154 238 participants; 12 studies; RR, 2.37; 95% CI, 1.97-2.85; I2, 89%; moderate confidence) and persons with ADHD (396 488 participants; 8 studies; RR, 2.13; 95% CI, 1.13-4.02; I2, 98%; low confidence) than for the general population. Among persons with ASD, deaths from natural causes (4 studies; RR, 3.80; 95% CI, 2.06-7.01; I2, 96%; low confidence) and deaths from unnatural causes were increased (6 studies; RR, 2.50; 95% CI, 1.49-4.18; I2, 95%; low confidence). Among persons with ADHD, deaths from natural causes were not significantly increased (4 studies; RR, 1.62; 95% CI, 0.89-2.96; I2, 88%; low confidence), but deaths from unnatural causes were higher than expected (10 studies; RR, 2.81; 95% CI, 1.73-4.55; I2, 92%; low confidence).
Conclusions and Relevance
This systematic review and meta-analysis found that ASD and ADHD are associated with a significantly increased risk of mortality. Understanding the mechanisms of these associations may lead to targeted strategies to prevent avoidable deaths in high-risk groups. The substantial heterogeneity between studies should be explored further.
Introduction
Autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) are common childhood onset neurodevelopmental disorders,1,2 with estimated worldwide prevalence of 58.6 million cases among children and young people 20 years and younger.2 Although the cause of ASD and ADHD remains largely unknown, a complex interaction of multiple factors is thought to contribute to the development of both conditions, generally persisting into adulthood.3,4,5 Both disorders have been found to be associated with psychosocial functional impairments and a range of adverse outcomes in patients and their families.4,5,6,7,8,9
Deaths in people with mental disorders have been examined in multiple epidemiologic studies10,11,12 suggesting that people with these disorders may experience a significant reduction in life expectancy, with increased mortality rates over the general population. Similarly, several studies13,14,15,16,17,18,19 have suggested that persons with ASD or ADHD may be associated with an increased risk of mortality; however, the results are inconsistent. For example, Pickett et al13 reported a 2-fold higher mortality rate ratio (RR) of 2.4 (95%, 2.2-2.8) in persons with ASD compared with those without it in the California Development Disability System. Bilder et al14 showed a mortality RR of 11.59 (95% CI, 6.24-21.53) in the Utah/University of California, Los Angeles Autism Epidemiologic Study. However, Smith et al15 suggested a nonstatistically significant increase in mortality (RR, 1.10; 95% CI, 0.50-2.50) in a large cohort study of school pupils with and without ASD. Conversely, Dalsgaard et al16 and Sun et al17 suggested increased mortality risk in persons with ADHD in large population-based cohorts from Denmark (fully adjusted RR, 2.07; 95% CI, 1.70-2.50) and Sweden (RR, 3.94; 95% CI, 3.51-4.43), respectively. London and Landes18 suggested similar results, with an adjusted RR of 1.78 (95% CI, 1.01-3.12). More recently, a nationwide population-based cohort study in Taiwan19 showed that having ADHD was associated with having a marginally increased risk of mortality after full adjustment (fully adjusted hazard ratio, 1.07; 95% CI, 1.00-1.17).
To our knowledge, no systematic review and meta-analysis of epidemiologic studies has specifically evaluated the mortality risk and main causes of death in persons with ASD or ADHD. A systematic review20 of studies published until 2010 examined ASD and 2 outcomes (epilepsy and mortality). Only 5 studies investigating mortality associations were located,20 so lack of data precluded exploring potential variations in all-cause mortality and quantifying cause-specific mortality risks. Therefore, in our study, we conducted a comprehensive knowledge synthesis to identify and evaluate all available observational studies of mortality associations in people with ASD or ADHD, which provide more complete information, and the most updated epidemiologic evidence than previous studies. Our systematic review and meta-analysis of epidemiologic studies for ASD and ADHD has only become possible in the past few years because several large population-based observational studies16,17,19,21 have been published that have reported similar mortality-related outcome measures. In this study, we aimed to evaluate the risk of both all-cause and cause-specific mortality among persons with ASD or ADHD and their first-degree relatives.
Methods
Our systematic review was reported in accordance with the 2020 Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.22 We also reported this study in accordance with the guidance provided in the Meta-analysis of Observational Studies in Epidemiology (MOOSE) reporting guideline23 (eTables 1 and 2 in the Supplement). We developed and registered a review protocol (PROSPERO registration number: CRD42017059955). Our methods are briefly described here (and explained in more detail in the protocol24 and in eTables 1-12 in the Supplement).
Information Sources and Search Strategy
An information specialist (A.A.-A.) searched MEDLINE (via PubMed), Scopus, Embase, Web of Science Core Collection, and PsycINFO (via ProQuest) to identify all relevant observational studies in humans that examined the risk of mortality among persons with ASD or ADHD, published from inception to April 1, 2021, without language restrictions. The search strategies for all electronic databases are presented in the eTable 5 in the Supplement. References of all relevant primary studies and review articles were also screened to identify additional data sources.
Eligibility Criteria
To be included, primary studies had to be observational (cohort, case-control) studies of persons with ASD or ADHD according to standard operationalized diagnostic criteria (eg, International Classification of Diseases, Ninth Revision [ICD-9] or Tenth revision [ICD-10] or third, fourth, or fifth editions of the Diagnostic and Statistical Manual of Mental Disorders criteria; ASD, ICD-9 codes 299.0 and 299.8 and ICD-10 code F84; ADHD, ICD-9 codes 314.00 and 314.01 and ICD-10 code F90) and report the mortality RR for the risk of mortality in people with ASD/ADHD compared with the general population or those without ASD/ADHD, or have enough data (eg, number of cases and sample size; observed and expected cases) to compute these estimates. We excluded studies in which ASD or ADHD were not the exposure of interest and mortality was not reported as the outcome. Studies not presenting study-specific data or sufficient data for an outcome measure to be calculated were also excluded. We excluded case reports, case series, in vitro studies, and animal studies.
Outcomes
The primary outcome was all-cause mortality (ICD-10 codes A00-Y98 and ICD-9 codes 001-E999). Cause-specific mortality rates were evaluated as a secondary outcome of interest (eTable 3 in the Supplement).
Screening and Selection Process
Two investigators (F.C.-L., D.M.S.-G., and/or M.R.) independently screened all titles and abstracts and retrieved the full text of any article considered definitely or possibly eligible. The same investigators reviewed the full-text articles against the eligibility criteria. Any disagreement between these investigators was resolved by discussion.
Data Extraction and Quality Assessment
Two investigators (F.C.-L., D.M.S.-G., and/or M.R.) independently extracted relevant information from the included studies: first author, publication year and period of recruitment, country, study design, setting, coverage, mean or median age (or age range), proportion of women participants, ethnicity, comorbidities, social status, diagnostic criteria and ascertainment of outcome, consideration of confounding factors, the number of participants with fatal outcome, and maximally adjusted RR estimates with 95% CIs. When relevant fatal outcome data were not available, we directly contacted the corresponding author of the study to request the information (eTable 7 in the Supplement). Two pairs of investigators (F.C.-L., M.J.P., D.M.S.-G., and M.R.) independently undertook methodologic quality assessment of included studies using the Newcastle-Ottawa scale25 and allocated stars for adherence to the prespecified criteria. This scale ranges from 0 (lowest quality) to 9 (highest quality) stars and judges each study regarding selection of study groups, comparability, and ascertainment of the outcome. We considered studies with 0 to 3, 4 to 6, and 7 to 9 stars to represent high, moderate, and low risk of bias, respectively. Discrepant scores were resolved by discussion among investigators.
Data Analysis
To measure the association between the mortality in people with ADHD or ASD and the mortality in the reference control group, we did meta-analysis using the inverse variance random effects model26 (with the DerSimonian-Laird between-study variance estimator) to pool weighted all-cause and specific-cause mortality RR estimates. We explored the contributions from natural and unnatural causes of death. Unnatural deaths were defined based on ICD codes (ICD-10 codes V01-Y98 or ICD-9 codes E800-999); the remaining deaths were classified as natural. All meta-analyses were conducted for ADHD and ASD separately. We assessed heterogeneity between studies using the P value of Cochran Q test27 and the I2 statistic (with 95% CIs),28 which could reflect either genuine heterogeneity or bias. The I2 statistic ranges between 0% and 100% (with values of 0%-25% and 75%-100% taken to indicate low and considerable heterogeneity, respectively). We also calculated 95% prediction intervals, which further account for heterogeneity between studies and indicate the uncertainty for the effect that would be expected in a new study examining that same association.29 To assess the robustness of pooled results and explore possible reasons for heterogeneity, prespecified subgroup analyses24 were performed according to sex (male or female), number of comorbidities (including 0, 1, 2, or any), age group at first diagnosis of ASD or ADHD (prior to age 18 years or at 18 years or older), number of participants with ASD or ADHD (<500 vs 500-1000 vs >1000), setting (community, inpatient care, or outpatient care), follow-up (less than 1 year, 1-5 years, >5 years), study quality (low vs moderate vs high risk of bias), and statistical adjustment for potential confounders (yes vs no). Small study effects (the tendency for exposure effects estimated in smaller studies to differ from those estimated in larger studies, which can result from reporting biases, methodologic heterogeneity, epidemiologic heterogeneity, or other factors) was estimated visually by funnel plots or by Begg test and the weighted regression test of Egger. P values were determined using the Woolf method. P values were 2-tailed, and statistical significance was set at less than .05. We performed all data analyses using Stata version 17 (StataCorp).
Credibility Assessment
We applied a set of criteria to classify the credibility (or certainty) of the evidence from meta-analysis based on the Global Burden of Disease30 and GRADE system31 (eTable 10 in the Supplement).
With the publication of this article, the full data set will be freely available online in the Open Science Framework,32 a secure online repository for research data. Amendments to the original protocol are listed in the eTable 4 in the Supplement.
Results
Extent of Relevant Literature Identified
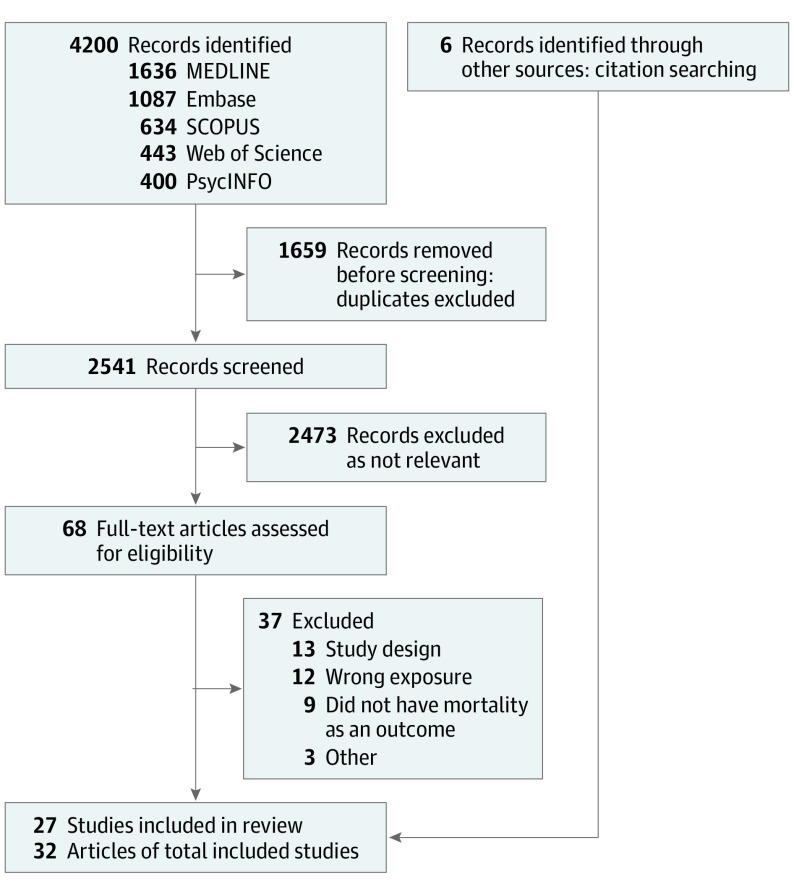
We screened 2541 titles and abstracts, followed by 68 full-text articles (Figure 1). Twenty-seven epidemiologic studies published in 32 articles13,14,15,16,17,18,19,21,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56 met our inclusion criteria.
Figure 1. Flow Diagram of Study Selection.
Description of Studies and Participants
Table 1 and eTable 8 in the Supplement summarize the characteristics of the included studies. All studies were published in English from 1988 through 2021. Twenty-three studies13,14,15,16,17,18,33,34,35,36,37,38,39,40,41,42,44,45,46,47,48,49,50,51,52,53,54,56 were from North America and Europe (11 in the US,13,14,18,33,34,35,36,37,41,42,46,50,51,53 5 in Denmark,16,38,39,44,49,52,56 3 in Sweden,17,40,47 2 in Finland,45,54 and 2 in the UK15,48). Seventeen studies were retrospective cohorts,13,14,15,16,18,21,33,34,35,36,37,38,39,43,44,48,50,52,53,54,55,56 8 were prospective cohorts,17,19,40,41,42,45,46,49 and 2 were retrospective case-control studies.47,51 Fourteen studies13,14,15,21,34,35,38,39,40,47,48,49,50,53,54,55,56 included 206 162 participants with ASD, and 12 studies16,17,18,19,33,36,37,41,42,44,45,46,51,52 included 433 761 participants with ADHD. The number of participants with ASD ranged from 120 to 35 929, and the number of participants with ADHD ranged from 110 to 275 980. The proportion of female participants ranged from 14% to 100%. Median (range) follow-up was 16 (3-33) years. Twelve studies15,21,33,36,37,40,42,46,48,50,52,55 followed up participants to young adult age (mean age, <40 years). Only 3 studies14,36,37,43 included first-degree relatives of people with ADHD or ASD diagnosis.
Table 1. Summary Characteristics of Included Studies.
| Source | Study design (country) | Setting; coverage | Study years (follow-up, y) | No. of participants | Sex and age | No. of fatal cases | Main outcome(s) | Causes of death | Comparator |
|---|---|---|---|---|---|---|---|---|---|
| Kuperman et al,33 1988 | Retrospective cohort (US) | Inpatient; population-based | 1970-1985 (9.1) | 110 People with ADHD | 20.0% Female; mean age, 12.3 y at admission and 22.1 y at follow-up | 1 | Specific cause of death | Yes | General population |
| Pickett et al,13 2006; Shavelle et al,34 2001; Shavelle et al,35 1998 | Retrospective cohort (US) | Community; population-based | 1983-1997 and 1998-2002 (9.5) | 13 111 People with ASD | 20.6% Female; most aged ≥4 y at first evaluation | 280 | All-cause and specific cause of death | Yes | General population |
| Barkley et al,36 2008; Barkley et al,37 1990 | Retrospective cohort (US) | Outpatient; health services | 1979-1996 (17) | 158 People with ADHD and their parents | 9% Female; aged ≥4 y at first evaluation and 21 y at follow-up | 3 | All-cause and specific cause of death | Yes | Participants without hyperactivity |
| Mouridsen et al,38 2008; Isager et al,39 1999 | Retrospective cohort (Denmark) | Inpatient; population-based | 1960-2006 (35.5) | 341 People with ASD | 24.9% Female; mean age, 7.5 y at admission and 43.4 y at follow-up | 26 | All-cause and specific cause of death | Yes | General population |
| Gillberg et al,40 2010 | Prospective cohort (Sweden) | Community; population-based | 1962-2008 (33.2) | 120 People with ASD | 29.2% Female; early childhood at admission and mean age, 33.2 y at follow-up | 9 | All-cause and specific cause of death | Yes | General population |
| Klein et al,41 2012 | Prospective cohort (US) | Community; school-based | 1970-NA (33) | 207 People with ADHD | All male; mean age, 8.3 y at first evaluation and 41 y at follow-up | 15 | All-cause of death | No | Participants without ADHD |
| Barbaresi et al,42 2013 | Prospective cohort (US) | Community; population-based | 1976-2009 (NA) | 367 People with ADHD | 28.0% Female; mean age, 10.4 y at diagnosis and 27.0 y at follow-up | 7 | All-cause and specific cause of death | Yes | Participants without ADHD |
| Bilder et al,14 2013 | Retrospective cohort (US) | Community; population-based | 1982-2011 (25) | 305 People with ASD and their siblings | 25.2% Female; mean age, 10.8 y at diagnosis and 35.8 y at follow-up | 29 | All-cause and specific cause of death | Yes | General population; siblings |
| Fairthorne et al,43 2014 | Retrospective cohort (Australia) | Community; population-based | 1983-2010 (NA) | 2041 Mothers of children with ASD | All women; 77% aged 20-34 y with mean age at death of 42 y | 24 | All-cause and specific cause of death | Yes | Participants without ASD or intellectual disability |
| Dalsgaard et al,16 2015; Scott et al,44 2017 | Retrospective cohort (Denmark) | Community; population-based | 1981-2013 (32) | 32 061 People with ADHD | 26.4% Female; mean age, 12.3 y at diagnosis | 107 | All-cause and specific cause of death | Yes | General population |
| Koisaari et al,45 2015 | Prospective cohort (Finland) | Community; health services (maternity hospital) | 1971-2004 (40) | 122 People with ADHD | 29.5% Female; aged ≥5 y at first evaluation and mean age of 40 y at follow-up | 11 | All-cause and specific cause of death | Yes | Participants without ADHD |
| Hetchtman et al,46 2016 | Prospective cohort (US) | Community; school-based | 1992-2008 (16) | 476 People with ADHD | 19.7% Female; mean age, 8.5 y at diagnosis and 24.7 y at follow-up | 11 | All-cause and specific cause of death | Yes | Participants without ADHD |
| Hirvikoski et al,47 2016 | Retrospective case-cohort/case-control (Sweden) | Mixed; population-based | 1987-2009 (NA) | 27 122 People with ASD | 31.1% Female; mean age, 19.8 y at diagnosis | 706 | All-cause and specific cause of death | Yes | General population |
| Hosking et al,48 2016 | Retrospective cohort (UK) | Outpatient; population-based | 2009-2013 (3) | 1532 People with ASD | 58.1% Female; mean age, 39.9 y at follow-up | 15 | All-cause of death | No | General population |
| London and Landes,18 2016 | Retrospective cohort (US) | Community; population-based | 2007-2011 (4) | 654 People with ADHD | 54.4% Female; mean age, 47.6 y at follow-up | 13 | All-cause and specific cause of death | Yes | General population |
| Schendel et al,49 2016 | Prospective cohort (Denmark) | Community; population-based | 1980-2013 (NA) | 20 492 People with ASD | 22.4% Female; most aged >9 y at diagnosis with median age of 19.0 y at death | 68 | All-cause and specific cause of death | Yes | General population |
| Chen et al,19 2019 | Prospective cohort (Taiwan) | Mixed; population-based | 2000-2013 (14) | 275 980 People with ADHD | 24.1% Female; mean age, 9.6 y at evaluation | 727 | All-cause and specific cause of death | Yes | General population |
| Hwang et al,21 2019 | Retrospective cohort (Australia) | Community; population-based | 2001-2015 (NA) | 35 929 People with ASD | 20.5% Female; age ranged, 5-64 y and mean age, 35.0 y at death | 244 | All-cause and specific cause of death | Yes | General population |
| Kirby et al,50 2019 | Retrospective cohort (US) | Community; population-based | 1998-2017 (20) | 16 904 People with ASD | 24.0% Female; mean age, 18.4 y at follow-up | 49 | Specific cause of death | Yes | General population |
| Sun et al,17 2019 | Prospective cohort (Sweden) | Community; population-based | 1983-2013 (11.1) | 86 670 People with ADHD | 33.2% Female; mean age, 14.3 y at diagnosis | 424 | All-cause and specific cause of death | Yes | General population |
| Yeh et al,51 2019 | Retrospective case-control (US) | Mixed; population-based | 2000-2013 (NA) | 4416 People with ADHD | 22.5% Female; most aged 40-64 y at evaluation | 67 | Specific cause of death | Yes | General population |
| Fitzgerald et al,52 2019 | Retrospective cohort (Denmark) | Community; population-based | 1995-2014 (21.5) | 32 540 People with ADHD | 30.8% Female; mean age, 21.5 at follow-up | 35 | Specific cause of death | Yes | General population |
| Akobirshoev et al,53 2020 | Retrospective cohort (US) | Inpatient; population-based | 2004-2014 (NA) | 34 237 People with ASD | 24.7% Female; mean age, 33.1 y at evaluation | 462 | All-cause of death | No | General population |
| Jokiranta-Olkoniemi et al,54 2021 | Retrospective cohort (Finland) | Mixed; population-based | 1987-2015 (NA) | 4695 People with ASD | 20.4% Female; mean age, 8.0 y at diagnosis | 53 | All-cause and specific cause of death | Yes | Participants without ASD |
| Huang et al,55 2021 | Retrospective cohort (Taiwan) | Mixed; population-based | 2000-2015 (8.1) | 6599 People with ASD | 22.8% Female; mean age, 11.9 y at evaluation | 119 | All-cause of death | No | General population |
| Kõlves et al,56 2021 | Retrospective cohort (Denmark) | Community; population-based | 1995-2016 (NA) | 35 020 People with ASD | 26.6% Female; most aged 10-29 y | 53 | Specific cause of death | Yes | General population |
| Smith et al,15 2021 | Retrospective cohort (Scotland, UK) | Community; school-based | 2008-2015 (3.9) | 9754 People with ASD | 14.0% Female; most aged 10-19 y | 6 | All-cause of death | No | Participants without ASD |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; NA, not available.
There were 49 individual study estimates for all-cause mortality in persons with ASD or ADHD and/or their first-degree relatives (eTable 9 in the Supplement). Seventeen studies14,16,17,18,19,33,38,39,40,47,48,49,51,56 provided adjusted RR estimates to control for several covariates (eg, age, sex, calendar year, or other). Twenty-one studies13,14,16,17,18,19,21,33,34,35,36,37,38,39,40,42,43,44,45,46,47,49,50,51,52,54,56 reported information on 12 cause-specific mortality outcomes. The most studied ICD-10 categories were external causes of mortality (such as injuries, unintentional incidents, suicides, and poisoning), accounting for 1215 cases (61.2%) in 21 studies13,14,16,17,19,21,33,34,35,36,37,38,39,40,42,43,44,45,46,47,49,50,51,52,54,56; followed by diseases of the circulatory system, accounting for 190 cases (9.6%) in 8 studies14,17,21,38,39,40,43,45,47 and neoplasms, accounting for 168 cases (8.5%) in 7 studies13,14,17,21,34,35,40,43,47 (eFigure 23 in the Supplement). Infectious diseases accounted 8 cases (0.4%) in 4 studies14,38,39,40,47 and complications of pregnancy, childbirth, and puerperium only accounted 1 case (0.1%) in 1 study.43 Regarding the methodologic quality (eTable 10 in the Supplement), 16 studies13,14,16,17,19,21,33,34,35,38,39,40,42,44,47,48,49,52,55,56 (59%) had low risk of bias and 11 studies15,18,36,37,41,43,45,46,49,51,53,54 had moderate risk of bias (Newcastle-Ottawa Scale values, 4-9).
Main Findings From Meta-analyses
Our all-cause meta-analyses focused the risk of dying in persons with ASD or ADHD compared with the general population and included 21 studies13,14,15,16,17,18,19,21,34,35,36,37,38,39,40,41,42,44,45,46,47,48,49,53,54,55 that contributed 46 data points (Table 2; eFigure 23 and eTable 9 in the Supplement). Thirty-four of 46 all-cause mortality RR estimates (74%) suggested an increased risk of mortality in individuals with ASD or ADHD. Among participants with ASD, all-cause mortality was increased in both sexes combined (12 studies13,14,15,21,34,35,38,39,40,47,48,49,53,54,55; RR, 2.37; 95% CI, 1.97-2.85; I2, 89%; moderate confidence) and separately for male individuals (8 studies13,14,34,35,38,39,40,47,49,53,54; RR, 2.09; 95% CI, 1.50-2.92; I2, 94%; low confidence) and female individuals (8 studies13,14,34,35,38,39,40,47,49,53,54; RR, 4.87; 95% CI, 3.07-7.73; I2, 91%; low confidence). Among persons with ADHD, all-cause mortality was also increased in both sexes combined (8 studies16,17,18,19,36,37,42,44,45,46; RR, 2.13; 95% CI, 1.13-4.02; I2, 98%; low confidence), and separately for male individuals (5 studies16,17,19,41,44,45; RR, 2.43; 95% CI, 1.01-5.83; I2, 99%; low confidence) and female individuals (4 studies16,17,19,44,45; RR, 2.84; 95% CI, 1.02-7.89; I2, 97%; low confidence) (Table 2 and Figure 2 and Figure 3). Meta-analysis for all-cause mortality among first-degree relatives was not possible, with only 3 studies reporting outcome data (1 study14 in siblings of children with ASD, 1 study43 in mothers of children with ASD, and 1 study36,37 in parents of children with ADHD).
Table 2. Description of Main Results of Meta-analysis for Association of ASD or ADHD With Risk of Mortalitya.
| Outcomes of interest | No. | RR (95% CI) | P value for effect estimate | I2 (95% CI) | 95% Prediction interval | P value for heterogeneity | Confidence | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Studies | Participants with ASD or ADHD | Death cases | Pooled | Largest study | ||||||
| Primary outcome, all-cause mortality | ||||||||||
| All-cause mortality, ASD | ||||||||||
| Both | 12 | 154 238 | 2017 | 2.37 (1.97-2.85) | 2.06 (1.64-2.58) | <.001 | 89 (82-93) | 1.25-4.48 | <.001 | Moderate (probable) |
| Male | 8 | 75 085 | 1071 | 2.09 (1.50-2.92) | 1.25 (1.08-1.45) | <.001 | 94 (90-96) | 0.68-6.40 | <.001 | Low (suggestive) |
| Female | 8 | 25 338 | 562 | 4.87 (3.07-7.73) | 2.75 (2.09-3.64) | <.001 | 91 (85-95) | 1.09-21.78 | <.001 | Low (suggestive) |
| All-cause mortality, ADHD | ||||||||||
| Both | 8 | 396 488 | 1302 | 2.13 (1.13-4.02) | 1.07 (1.00-1.17) | .02 | 98 (97-99) | 0.28-16.42 | <.001 | Low (suggestive) |
| Male | 5 | 291 201 | 982 | 2.43 (1.01-5.83) | 1.04 (0.94-1.14) | .046 | 99 (98-99) | 0.10-58.40 | <.001 | Low (suggestive) |
| Female | 4 | 103 839 | 302 | 2.84 (1.02-7.89) | 1.24 (1.04-1.48) | .045 | 97 (96-99) | 0.03-277.30 | <.001 | Low (suggestive) |
| Secondary outcomes, cause-specific mortality | ||||||||||
| Natural causes, ASD | ||||||||||
| Both | 4 | 65 421 | 613 | 3.80 (2.06-7.01) | 2.59 (2.36-2.85) | <.001 | 96 (92-98) | 0.22-66.96 | <.001 | Low (suggestive) |
| Male | 2 | 22 430 | 256 | 2.95 (2.35-3.69) | 2.85 (2.50-3.24) | <.001 | 10 (NA) | NA | .29 | Low (suggestive) |
| Female | 2 | 9387 | 220 | 6.57 (0.60-71.91) | 2.44 (2.12-2.80) | .123 | 79 (NA) | NA | .03 | Low (not conclusive) |
| Natural causes, ADHD | ||||||||||
| Both | 4 | 394 833 | 516 | 1.62 (0.89-2.96) | 0.91 (0.80-1.15) | .1 | 88 (72-95) | 0.11-23.10 | <.001 | Low (not conclusive) |
| Male | 3 | 290 908 | 348 | 1.22 (0.74-2.01) | 0.83 (0.72-1.15) | .43 | 80 (36-94) | 0.00-451.06 | .007 | Low (not conclusive) |
| Female | 3 | 103 803 | 138 | 2.02 (0.91-4.48) | 1.03 (0.82-1.30) | .09 | 91 (77-97) | 0.00-39.6x103 | <.001 | Low (not conclusive) |
| Unnatural causes, ASD | ||||||||||
| Both | 6 | 117 345 | 318 | 2.50 (1.49-4.18) | 3.75 (2.85-4.92) | .001 | 95 (92-97) | 0.38-16.35 | <.001 | Low (suggestive) |
| Male | 4 | 61 031 | 182 | 1.94 (0.83-4.49) | 3.48 (2.57-4.74) | .12 | 96 (94-98) | 0.03-112.04 | <.001 | Low (not conclusive) |
| Female | 4 | 22 712 | 58 | 3.61 (1.71-7.60) | 2.63 (1.46-4.76) | .001 | 79 (45-92) | 0.15-88.22 | .002 | Low (suggestive) |
| Unnatural causes, ADHD | ||||||||||
| Both | 10 | 432 900 | 847 | 2.81 (1.73-4.55) | 1.51 (1.51-1.72) | <.001 | 92 (88-95) | 0.61-12.91 | <.001 | Low (suggestive) |
| Male | 5 | 316 851 | NA | 2.49 (1.36-4.56) | 1.45 (1.25-1.67) | .003 | 97 (96-98) | 0.23-26.59 | <.001 | Low (suggestive) |
| Female | 5 | 114 816 | NA | 2.98 (1.46-6.10) | 1.82 (1.32-2.51) | .003 | 92 (85-96) | 0.20-44.17 | <.001 | Low (suggestive) |
| Neoplasms, ASD both | 2 | 40 233 | 109 | 2.05 (1.46-2.87) | 1.80 (1.46-2.23) | <.001 | 53 (NA) | NA | .14 | Low (suggestive) |
| Nervous system, ASD both | 4 | 61 066 | 102 | 10.79 (5.42-21.10) | 7.49 (5.78-9.72) | <.001 | 85 (64-94) | 0.52-219.57 | <.001 | Low (suggestive) |
| Respiratory system, ASD both | 2 | 40 233 | 62 | 3.87 (1.80-8.32) | 2.68 (1.99-3.62) | .001 | 86 (NA) | NA | .007 | Low (suggestive) |
| Digestive system, ASD both | 2 | 40 233 | 40 | 4.59 (2.29-9.19) | 3.31 (2.25-4.87) | <.001 | 76 (NA) | NA | .0 | Low (suggestive) |
| Congenital malformations, ASD both | 2 | 40 233 | 37 | 11.74 (4.49-30.74) | 19.10 (11.94-30.55) | <.001 | 87 (NA) | NA | .005 | Low (suggestive) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; NA, not available; RR, risk ratio.
Outcomes with at least 2 studies for meta-analysis. Predictive intervals were inestimable with less than 3 studies.
Figure 2. Risk of All-Cause Mortality in People With Autism Spectrum Disorder (ASD).
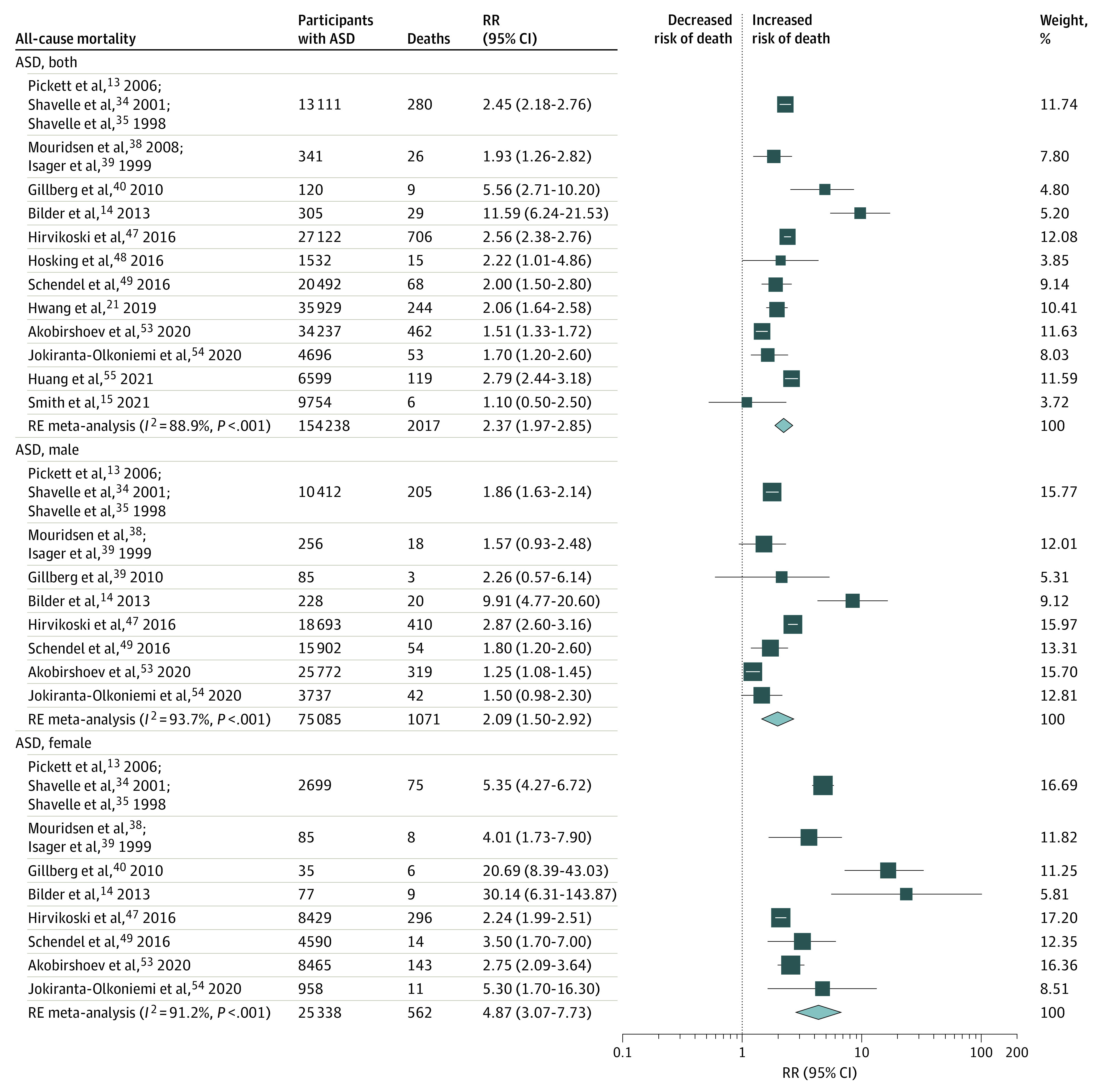
The size of each box indicates the effect of each study by weight assigned using the random-effects (RE) model; diamond, estimated effect size; and width of diamond, the precision of the estimate (95% CI). RR indicates risk ratio.
Figure 3. Risk of All-Cause Mortality in People With Attention-Deficit/Hyperactivity Disorder (ADHD).
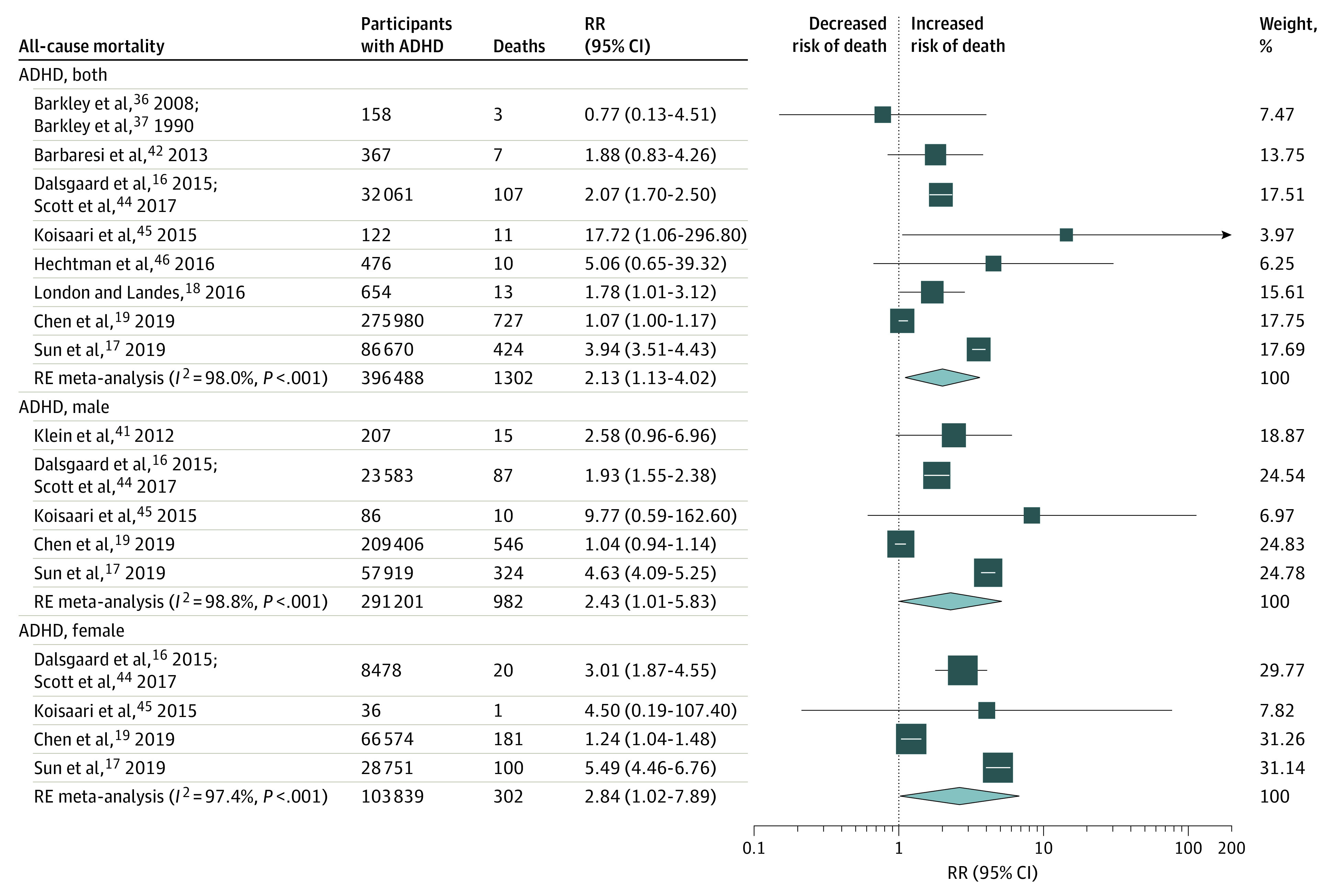
The size of each box indicates the effect of each study by weight assigned using the random-effects (RE) model; diamond, estimated effect size; and width of diamond, the precision of the estimate (95% CI). RR indicates risk ratio.
Secondary outcome meta-analyses focused on the cause-specific mortality RR in persons with ASD or ADHD compared with the general population and included 17 studies13,16,17,19,21,33,34,35,36,37,38,39,42,44,45,46,47,49,51,52,54,56 that contributed 89 data points (Table 2 and eTable 9 and eFigures 1-7 in the Supplement). A total of 67 of 87 cause-specific mortality RR estimates (75%) were increased. Among persons with ASD, deaths from natural causes (4 studies13,34,35,47,49,54; RR, 3.80; 95% CI, 2.06-7.01; I2, 96%; low confidence) and deaths from unnatural causes were increased (6 studies13,34,35,47,49,50,54,56; RR, 2.50; 95% CI, 1.49-4.18; I2, 95%; low confidence). Among persons with ADHD, deaths from natural causes were not significantly increased (4 studies16,17,19,44,45; RR, 1.62; 95% CI, 0.89-2.96; I2, 88%; low confidence), but deaths from unnatural causes were higher than expected (10 studies16,17,19,33,36,37,42,44,45,46,51,52; RR, 2.81; 95% CI, 1.73-4.55; I2, 92%; low confidence).
Additional Analyses
The full details of the additional analyses are reported in eFigures 1 to 23 in the Supplement. Statistical heterogeneity was not substantially reduced when analyses were stratified by prespecified (exploratory) subgroup analyses such as number of comorbidities, age group at first diagnosis, number of participants (sample size), setting, follow-up period, study quality, and adjustment for potential confounders. Overall, the I2 statistic indicated that data were heterogeneous in many of the pooled analyses, and therefore, these summary measures must be interpreted with appropriate caution. Insufficient data were available to do preplanned subgroup analyses24 by diagnostic criteria, ethnicity, geographic region, or year of publication as there were not enough data. We undertook a funnel plot, and Begg and Egger tests of the 12 studies examining all-cause mortality in people with ASD, with results showing no clear evidence of small study effects (eFigure 22 in the Supplement).
Discussion
This systematic review and meta-analysis comprehensively assess for the first time, to our knowledge, the available evidence regarding the risk of mortality in persons with ASD or ADHD. We included 27 epidemiologic studies in our quantitative evaluation, 16 of which were judged to be at low risk of bias. We found that ASD and ADHD are associated with a significantly increased risk of all-cause mortality. However, the results should be interpreted with caution because there was evidence of heterogeneity between study estimates of the mortality risks. When we examined causes of death, ASD and ADHD were associated with higher mortality risk due to unnatural (external) causes, and only persons with ASD had an increased risk of mortality from natural causes of death, but the evidence was judged as only low confidence. Fewer studies exist examining the risk of mortality among first-degree relatives of persons with ASD or ADHD, to our knowledge.
Several mechanisms, including health determinants and biological pathways, have been suggested as potential factors that might explain the excess premature mortality among children and young persons with ASD or ADHD. However, establishing a causal relationship is difficult because the associations between mortality and childhood-onset developmental disorders are complex. Severe mental and behavioral disorders appear to be associated with reduced life expectancy, both in terms of mortality from external causes and mortality from other medical conditions or diseases.10,11 Findings from previous studies and reviews have suggested that children and adults with ASD/ADHD are associated with coexisting mental and neurologic conditions (such as oppositional and conduct disorders, tic disorders, epilepsy, depression, anxiety, and substance use disorders).3,4,5,57 As children and young persons with ASD/ADHD age, they often experience emotional and social difficulties.3,4,5 Some people also exhibit impulsive forms of behavior with negative impacts on their quality of life. Behaviors such as impulsivity and/or inattention can be contributing factors for injuries and unintentional incidents in children with ASD/ADHD.58,59
Previous studies16,17,49 have tested potential modifying effects of comorbidity on mortality risk for persons with ASD/ADHD. For example, Dalsgaard et al,16 Sun et al,17 and Schendel et al49 suggested increased mortality RRs in persons with ADHD or ASD with comorbid neurologic or mental conditions (eg, oppositional defiant disorder, conduct disorder, or substance use disorder). However, it should be noted that presence of ASD and/or ADHD with any distinct additional medical condition (the so-called comorbidity or multimorbidity) may be confounded by previous exposures (such as socioeconomic factors, environmental factors, and childhood abuse).60 Prevention efforts to reduce mortality in persons with ASD or ADHD may need to address the conditions that appear to mediate causes of death. While potentially preventable, reducing excess premature mortality (eg, due to external causes) can be challenging. For example, systematic screening would be advisable in health services and social care, and preventive education can be feasible in almost all circumstances. However, some persons with ADHD/ASD are often from socioeconomically disadvantaged groups/areas and are more likely to be exposed to environmental risk factors (eg, substance misuse, violence) than other populations.61,62,63 Similarly, studies64,65 have shown that persons with ADHD or ASD may be less likely to receive timely diagnosis and prompt care. All these factors are possible complications of ASD/ADHD, so the implication for practice is that health care professionals should recognize their importance.
Strengths and Limitations
This study had several strengths and limitations. We used established methods to leverage a large number of records identified from each database searched and contacted study authors to identify relevant outcome data. However, our search strategy could have omitted abstracts that did not state all-cause or cause-specific mortality as an included outcome. Observational studies in this area are increasingly conducted within large routinely collected electronic health databases, sometimes with hundreds of thousands of health care users. These studies generate precise estimates of exposure effects, which sometimes may be inaccurate because of potential residual confounding. For example, electronic health records data may have limitations when used for research, including limited information on lifestyle and socioeconomic determinants of health. In this systematic review, there was heterogeneity in the included studies in terms of the design, settings, populations, and outcomes. Some of the included studies have a restricted age of follow-up (eg, individuals younger than 40 years). We used study-level data instead of individual participant data, so the small number of studies (and events) for most cause-specific mortality estimates limited the subgroup analyses that could be conducted to account for potential sources of heterogeneity. Furthermore, our results might have limited generalizability because the studies were mostly conducted in Western countries. Although we adopted reproducible definitions, our meta-analyses were challenged by the reporting of events in studies. None of the primary studies examined and reported all the fatal outcomes of interest. Also, incomplete reporting is common in the literature and limited our possibilities to optimally synthesize the data for some specific causes of death. Future studies should adopt rigorous protocols when studying the effects of ASD/ADHD on health, which should clearly define all outcomes and exposures, how the study population was selected, how data were collected, and that all relevant potential confounders should be accounted for. Reporting guidelines, such as the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline,66 and the Reporting of Studies Conducted Using Observational Routinely-Collected health Data (RECORD) statement,67 should be rigorously implemented for individual study reports. Finally, small study effects were not quantitatively assessed for most of the outcomes because there were inadequate numbers of included studies to properly assess a funnel plot or use more sophisticated methods.
Conclusions
We found suggestive evidence that ASD and ADHD are associated with a significantly increased risk of mortality. Understanding the mechanisms of these associations may lead to targeted strategies to prevent avoidable deaths in high-risk groups of children and young people as an approach to improve public health. For example, clinicians and health care professionals can be encouraged to routinely collect information on behavioral, medical conditions, and health outcomes related to ASD/ADHD, emphasizing the need to recognize and address modifiable vulnerability factors and prevent delays in health care provision. Additionally, we hope that these estimates can shed some light for future studies related to examining mortality-related health estimates in persons with ASD or ADHD.
eTable 1. PRISMA 2020 checklist
eTable 2. MOOSE checklist
eTable 3. Coding and classification of causes of death
eTable 4. Methods clarifications/modifications from the protocol
eTable 5. Search strategy
eTable 6. List of excluded studies
eTable 7. List of studies with authors contacted for additional clarifications or data
eTable 8. Main characteristics of included studies
eTable 9. Main results of individual studies
eTable 10. Methodological quality assessment of included studies (Newcastle-Ottawa Scale
eTable 11. Grading certainty (or credibility) of evidence for summary estimates
eTable 12. Summary statistics of risk of cancer in people with anorexia nervosa
eFigure 1. Secondary outcome. Unnatural causes of death among ASD/ADHD people
eFigure 2. Secondary outcome. Natural causes of death among ASD/ADHD people
eFigure 3. Secondary outcome. Deaths caused by nervous system disorders among ASD people
eFigure 4. Secondary outcome. Deaths caused by neoplasms among ASD people
eFigure 5. Secondary outcome. Deaths caused by respiratory system diseases among ASD people
eFigure 6. Secondary outcome. Deaths caused by digestive system diseases among ASD people
eFigure 7. Secondary outcome. Deaths caused by congenital malformations among ASD people
eFigure 8. Subgroup analyses. ASD comorbidity and all-cause mortality among ASD people
eFigure 9. Subgroup analyses. ADHD comorbidity and all-cause mortality among ADHD people
eFigure 10. Subgroup analyses. Age group at first diagnosis and all-cause mortality among ASD people
eFigure 11. Subgroup analyses. Age group at first diagnosis and all-cause mortality among ADHD people
eFigure 12. Subgroup analyses. Cohort/sample size and and all-cause mortality among ASD people
eFigure 13. Subgroup analyses. Cohort/sample size and and all-cause mortality among ADHD people
eFigure 14. Subgroup analyses. Setting and all-cause mortality among ASD people
eFigure 15. Subgroup analyses. Setting and all-cause mortality among ADHD people
eFigure 16. Subgroup analyses. Follow-up (in years) and all-cause mortality among ASD people
eFigure 17. Subgroup analyses. Follow-up (in years) and all-cause mortality among ADHD people
eFigure 18. Subgroup analyses. Study-quality/risk of bias and all-cause mortality among ASD people
eFigure 19. Subgroup analyses. Study-quality/risk of bias and all-cause mortality among ADHD people
eFigure 20. Subgroup analyses. Adjustment for potential confounders and all-cause mortality among ASD people
eFigure 21. Subgroup analyses. Adjustment for potential confounders and all-cause mortality among ADHD people
eFigure 22. Funnel plot for primary outcome of all-cause mortality in people with ASD (12 studies)
eFigure 23. Treemap summarizing the amount of data according to specific causes of death
References
- 1.Kassebaum N, Kyu HH, Zoeckler L, et al. ; Global Burden of Disease Child and Adolescent Health Collaboration . Child and adolescent health from 1990 to 2015: findings from the Global Burden of Diseases, Injuries, and Risk Factors 2015 Study. JAMA Pediatr. 2017;171(6):573-592. doi: 10.1001/jamapediatrics.2017.0250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thapar A, Cooper M, Rutter M. Neurodevelopmental disorders. Lancet Psychiatry. 2017;4(4):339-346. doi: 10.1016/S2215-0366(16)30376-5 [DOI] [PubMed] [Google Scholar]
- 4.Lord C, Elsabbagh M, Baird G, Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392(10146):508-520. doi: 10.1016/S0140-6736(18)31129-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395(10222):450-462. doi: 10.1016/S0140-6736(19)33004-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandin S, Lichtenstein P, Kuja-Halkola R, Larsson H, Hultman CM, Reichenberg A. The familial risk of autism. JAMA. 2014;311(17):1770-1777. doi: 10.1001/jama.2014.4144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erskine HE, Norman RE, Ferrari AJ, et al. Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2016;55(10):841-850. doi: 10.1016/j.jaac.2016.06.016 [DOI] [PubMed] [Google Scholar]
- 8.Nourredine M, Gering A, Fourneret P, et al. Association of attention-deficit/hyperactivity disorder in childhood and adolescence with the risk of subsequent psychotic disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(5):519-529. doi: 10.1001/jamapsychiatry.2020.4799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drmic IE, Szatmari P, Volkmar F. Life course health development in autism spectrum disorders. In: Halfon N, Forrest CB, Lerner RM, Faustman EM, eds. Handbook of Life Course Health Development. Springer; 2018. doi: 10.1007/978-3-319-47143-3_11 [DOI] [PubMed] [Google Scholar]
- 10.Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827-1835. doi: 10.1016/S0140-6736(19)32316-5 [DOI] [PubMed] [Google Scholar]
- 11.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334-341. doi: 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153-160. doi: 10.1002/wps.20128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pickett JA, Paculdo DR, Shavelle RM, Strauss DJ. 1998-2002 Update on “causes of death in autism”. J Autism Dev Disord. 2006;36(2):287-288. doi: 10.1007/s10803-005-0066-x [DOI] [PubMed] [Google Scholar]
- 14.Bilder D, Botts EL, Smith KR, et al. Excess mortality and causes of death in autism spectrum disorders: a follow up of the 1980s Utah/UCLA autism epidemiologic study. J Autism Dev Disord. 2013;43(5):1196-1204. doi: 10.1007/s10803-012-1664-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith GS, Fleming M, Kinnear D, et al. Mortality in 787,666 school pupils with and without autism: a cohort study. Autism. 2021;25(1):300-304. doi: 10.1177/1362361320944037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dalsgaard S, Østergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196. doi: 10.1016/S0140-6736(14)61684-6 [DOI] [PubMed] [Google Scholar]
- 17.Sun S, Kuja-Halkola R, Faraone SV, et al. Association of psychiatric comorbidity with the risk of premature death among children and adults with attention-deficit/hyperactivity disorder. JAMA Psychiatry. 2019;76(11):1141-1149. doi: 10.1001/jamapsychiatry.2019.1944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.London AS, Landes SD. Attention deficit hyperactivity disorder and adult mortality. Prev Med. 2016;90:8-10. doi: 10.1016/j.ypmed.2016.06.021 [DOI] [PubMed] [Google Scholar]
- 19.Chen VC, Chan HL, Wu SI, et al. Attention-deficit/hyperactivity disorder and mortality risk in Taiwan. JAMA Netw Open. 2019;2(8):e198714. doi: 10.1001/jamanetworkopen.2019.8714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woolfenden S, Sarkozy V, Ridley G, Coory M, Williams K. A systematic review of two outcomes in autism spectrum disorder: epilepsy and mortality. Dev Med Child Neurol. 2012;54(4):306-312. doi: 10.1111/j.1469-8749.2012.04223.x [DOI] [PubMed] [Google Scholar]
- 21.Hwang YIJ, Srasuebkul P, Foley KR, Arnold S, Trollor JN. Mortality and cause of death of Australians on the autism spectrum. Autism Res. 2019;12(5):806-815. doi: 10.1002/aur.2086 [DOI] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. doi: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting: Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012. doi: 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 24.Catalá-López F, Hutton B, Page MJ, et al. Risk of mortality among children, adolescents, and adults with autism spectrum disorder or attention deficit hyperactivity disorder and their first-degree relatives: a protocol for a systematic review and meta-analysis of observational studies. Syst Rev. 2017;6(1):189. doi: 10.1186/s13643-017-0581-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed April 22, 2021. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 26.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 27.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–29. doi: 10.2307/3001666 [DOI] [Google Scholar]
- 28.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. doi: 10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
- 30.GBD 2016 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345-1422. doi: 10.1016/S0140-6736(17)32366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guyatt GH, Oxman AD, Vist GE, et al. ; GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-926. doi: 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Catalá-López F, Hutton B, Page MJ, et al. Risk of mortality among persons with autism spectrum disorder or attention deficit hyperactivity disorder and their first-degree relatives: a systematic review and meta-analysis of observational studies. OSF. Updated October 17, 2021. Accessed January 10, 2022. doi: 10.17605/OSF.IO/2NJUD [DOI]
- 33.Kuperman S, Black DW, Burns TL. Excess mortality among formerly hospitalized child psychiatric patients. Arch Gen Psychiatry. 1988;45(3):277-282. doi: 10.1001/archpsyc.1988.01800270095011 [DOI] [PubMed] [Google Scholar]
- 34.Shavelle RM, Strauss DJ, Pickett J. Causes of death in autism. J Autism Dev Disord. 2001;31(6):569-576. doi: 10.1023/A:1013247011483 [DOI] [PubMed] [Google Scholar]
- 35.Shavelle RM, Strauss D. Comparative mortality of persons with autism in California, 1980-1996. J Insur Med. 1998;30(4):220-225. [PubMed] [Google Scholar]
- 36.Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. The Guilford Press; 2008. [Google Scholar]
- 37.Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I: an 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1990;29(4):546-557. doi: 10.1097/00004583-199007000-00007 [DOI] [PubMed] [Google Scholar]
- 38.Mouridsen SE, Brønnum-Hansen H, Rich B, Isager T. Mortality and causes of death in autism spectrum disorders: an update. Autism. 2008;12(4):403-414. doi: 10.1177/1362361308091653 [DOI] [PubMed] [Google Scholar]
- 39.Isager T, Mouridsen SE, Rich B. Mortality and causes of death in pervasive developmental disorders. Autism. 1999;3(1):7-16. doi: 10.1177/1362361399003001002 [DOI] [Google Scholar]
- 40.Gillberg C, Billstedt E, Sundh V, Gillberg IC. Mortality in autism: a prospective longitudinal community-based study. J Autism Dev Disord. 2010;40(3):352-357. doi: 10.1007/s10803-009-0883-4 [DOI] [PubMed] [Google Scholar]
- 41.Klein RG, Mannuzza S, Olazagasti MA, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69(12):1295-1303. doi: 10.1001/archgenpsychiatry.2012.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637-644. doi: 10.1542/peds.2012-2354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fairthorne J, Hammond G, Bourke J, Jacoby P, Leonard H. Early mortality and primary causes of death in mothers of children with intellectual disability or autism spectrum disorder: a retrospective cohort study. PLoS One. 2014;9(12):e113430. doi: 10.1371/journal.pone.0113430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scott JG, Giørtz Pedersen M, Erskine HE, et al. Mortality in individuals with disruptive behavior disorders diagnosed by specialist services: a nationwide cohort study. Psychiatry Res. 2017;251:255-260. doi: 10.1016/j.psychres.2017.02.029 [DOI] [PubMed] [Google Scholar]
- 45.Koisaari T, Michelsson K, Holopainen JM, et al. Traffic and criminal behavior of adults with attention deficit-hyperactivity with a prospective follow-up from birth to the age of 40 years. Traffic Inj Prev. 2015;16(8):824-830. doi: 10.1080/15389588.2015.1029068 [DOI] [PubMed] [Google Scholar]
- 46.Hechtman L, Swanson JM, Sibley MH, et al. ; MTA Cooperative Group . Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. J Am Acad Child Adolesc Psychiatry. 2016;55(11):945-952.e2. doi: 10.1016/j.jaac.2016.07.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016;208(3):232-238. doi: 10.1192/bjp.bp.114.160192 [DOI] [PubMed] [Google Scholar]
- 48.Hosking FJ, Carey IM, Shah SM, et al. Mortality among adults with intellectual disability in England: comparisons with the general population. Am J Public Health. 2016;106(8):1483-1490. doi: 10.2105/AJPH.2016.303240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schendel DE, Overgaard M, Christensen J, et al. Association of psychiatric and neurologic comorbidity with mortality among persons with autism spectrum disorder in a Danish population. JAMA Pediatr. 2016;170(3):243-250. doi: 10.1001/jamapediatrics.2015.3935 [DOI] [PubMed] [Google Scholar]
- 50.Kirby AV, Bakian AV, Zhang Y, Bilder DA, Keeshin BR, Coon H. A 20-year study of suicide death in a statewide autism population. Autism Res. 2019;12(4):658-666. doi: 10.1002/aur.2076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yeh HH, Westphal J, Hu Y, et al. Diagnosed mental health conditions and risk of suicide mortality. Psychiatr Serv. 2019;70(9):750-757. doi: 10.1176/appi.ps.201800346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fitzgerald C, Dalsgaard S, Nordentoft M, Erlangsen A. Suicidal behaviour among persons with attention-deficit hyperactivity disorder. Br J Psychiatry. 2019;1-6. doi: 10.1192/bjp.2019.128 [DOI] [PubMed] [Google Scholar]
- 53.Akobirshoev I, Mitra M, Dembo R, Lauer E. In-hospital mortality among adults with autism spectrum disorder in the United States: a retrospective analysis of US hospital discharge data. Autism. 2020;24(1):177-189. doi: 10.1177/1362361319855795 [DOI] [PubMed] [Google Scholar]
- 54.Jokiranta-Olkoniemi E, Gyllenberg D, Sucksdorff D, et al. Risk for premature mortality and intentional self-harm in autism spectrum disorders. J Autism Dev Disord. 2021;51(9):3098-3108. doi: 10.1007/s10803-020-04768-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huang JS, Yang FC, Chien WC, et al. Risk of substance use disorder and its associations with comorbidities and psychotropic agents in patients with autism. JAMA Pediatr. 2021;175(2):e205371. doi: 10.1001/jamapediatrics.2020.5371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kõlves K, Fitzgerald C, Nordentoft M, Wood SJ, Erlangsen A. Assessment of suicidal behaviors among individuals with autism spectrum disorder in Denmark. JAMA Netw Open. 2021;4(1):e2033565. doi: 10.1001/jamanetworkopen.2020.33565 [DOI] [PubMed] [Google Scholar]
- 57.Hossain MM, Khan N, Sultana A, et al. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: an umbrella review of systematic reviews and meta-analyses. Psychiatry Res. 2020;287:112922. doi: 10.1016/j.psychres.2020.112922 [DOI] [PubMed] [Google Scholar]
- 58.Steenfeldt-Kristensen C, Jones CA, Richards C. The prevalence of self-injurious behaviour in autism: a meta-analytic study. J Autism Dev Disord. 2020;50(11):3857-3873. doi: 10.1007/s10803-020-04443-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ruiz-Goikoetxea M, Cortese S, Aznarez-Sanado M, et al. Risk of unintentional injuries in children and adolescents with ADHD and the impact of ADHD medications: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;84:63-71. doi: 10.1016/j.neubiorev.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 60.Momen NC, Plana-Ripoll O, Agerbo E, et al. Association between mental disorders and subsequent medical conditions. N Engl J Med. 2020;382(18):1721-1731. doi: 10.1056/NEJMoa1915784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Roman-Urrestarazu A, van Kessel R, Allison C, Matthews FE, Brayne C, Baron-Cohen S. Association of race/ethnicity and social disadvantage with autism prevalence in 7 million school children in England. JAMA Pediatr. 2021;175(6):e210054. doi: 10.1001/jamapediatrics.2021.0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Russell AE, Ford T, Williams R, Russell G. The association between socioeconomic disadvantage and attention deficit/hyperactivity disorder (ADHD): a systematic review. Child Psychiatry Hum Dev. 2016;47(3):440-458. doi: 10.1007/s10578-015-0578-3 [DOI] [PubMed] [Google Scholar]
- 63.Kim JH, Kim JY, Lee J, et al. Environmental risk factors, protective factors, and peripheral biomarkers for ADHD: an umbrella review. Lancet Psychiatry. 2020;7(11):955-970. doi: 10.1016/S2215-0366(20)30312-6 [DOI] [PubMed] [Google Scholar]
- 64.Smith KA, Gehricke JG, Iadarola S, Wolfe A, Kuhlthau KA. Disparities in service use among children with autism: a systematic review. Pediatrics. 2020;145(suppl 1):S35-S46. doi: 10.1542/peds.2019-1895G [DOI] [PubMed] [Google Scholar]
- 65.Malik-Soni N, Shaker A, Luck H, et al. Tackling healthcare access barriers for individuals with autism from diagnosis to adulthood. Pediatr Res. 2021;1-8. doi: 10.1038/s41390-021-01465-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 67.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee . The Reporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. PRISMA 2020 checklist
eTable 2. MOOSE checklist
eTable 3. Coding and classification of causes of death
eTable 4. Methods clarifications/modifications from the protocol
eTable 5. Search strategy
eTable 6. List of excluded studies
eTable 7. List of studies with authors contacted for additional clarifications or data
eTable 8. Main characteristics of included studies
eTable 9. Main results of individual studies
eTable 10. Methodological quality assessment of included studies (Newcastle-Ottawa Scale
eTable 11. Grading certainty (or credibility) of evidence for summary estimates
eTable 12. Summary statistics of risk of cancer in people with anorexia nervosa
eFigure 1. Secondary outcome. Unnatural causes of death among ASD/ADHD people
eFigure 2. Secondary outcome. Natural causes of death among ASD/ADHD people
eFigure 3. Secondary outcome. Deaths caused by nervous system disorders among ASD people
eFigure 4. Secondary outcome. Deaths caused by neoplasms among ASD people
eFigure 5. Secondary outcome. Deaths caused by respiratory system diseases among ASD people
eFigure 6. Secondary outcome. Deaths caused by digestive system diseases among ASD people
eFigure 7. Secondary outcome. Deaths caused by congenital malformations among ASD people
eFigure 8. Subgroup analyses. ASD comorbidity and all-cause mortality among ASD people
eFigure 9. Subgroup analyses. ADHD comorbidity and all-cause mortality among ADHD people
eFigure 10. Subgroup analyses. Age group at first diagnosis and all-cause mortality among ASD people
eFigure 11. Subgroup analyses. Age group at first diagnosis and all-cause mortality among ADHD people
eFigure 12. Subgroup analyses. Cohort/sample size and and all-cause mortality among ASD people
eFigure 13. Subgroup analyses. Cohort/sample size and and all-cause mortality among ADHD people
eFigure 14. Subgroup analyses. Setting and all-cause mortality among ASD people
eFigure 15. Subgroup analyses. Setting and all-cause mortality among ADHD people
eFigure 16. Subgroup analyses. Follow-up (in years) and all-cause mortality among ASD people
eFigure 17. Subgroup analyses. Follow-up (in years) and all-cause mortality among ADHD people
eFigure 18. Subgroup analyses. Study-quality/risk of bias and all-cause mortality among ASD people
eFigure 19. Subgroup analyses. Study-quality/risk of bias and all-cause mortality among ADHD people
eFigure 20. Subgroup analyses. Adjustment for potential confounders and all-cause mortality among ASD people
eFigure 21. Subgroup analyses. Adjustment for potential confounders and all-cause mortality among ADHD people
eFigure 22. Funnel plot for primary outcome of all-cause mortality in people with ASD (12 studies)
eFigure 23. Treemap summarizing the amount of data according to specific causes of death