Abstract
BACKGROUND:
Little is known about the relationship between social determinants of health (SDH) and medication adherence among Medicaid beneficiaries with hypertension (HTN).
METHODS:
We conducted a posthoc subgroup analysis of 3,044 adult Medicaid beneficiaries who enrolled in a parent prospective cohort study and had a diagnosis of HTN based on their Medicaid claims during a 24-month period prior to study enrollment. We calculated the Proportion of Days Covered (PDC) by at least one antihypertensive medication during the first 12 months after study enrollment using the prescription claims data. We measured numerous SDH at the time of study enrollment and we categorized our HTN cohort into four social risk groups based on their response profiles to the SDH variables. We compared the mean PDC by the different levels of the SDH factors. We modeled the odds of being covered by an antihypertensive medication daily throughout the follow-up period by social risk group, adjusted for age, sex, and disease severity using a generalized linear model.
RESULTS:
The non-random sample was predominately black (93%), female (62%) and had completed high school (77%). The mean PDC varied significantly by different SDH such as food insecurity (49% - 56%), length of time living at present place (47% - 57%), smoking status (50% - 56%), etc. Social risk group was a significant predictor of medication adherence. Participants in the two groups with the most social risks were 36% (aOR=0.64; 95% CI 0.53, 0.78) and 20% (aOR=0.80; 95% CI 0.70, 0.93) less adherent to their hypertension therapy compared to participants in the group with the fewest social risks.
CONCLUSIONS:
Social risks are associated with lower antihypertensive medication adherence in the Medicaid population.
Keywords: Social Determinants of Health, Hypertension, Medication Adherence
INTRODUCTION
Almost half of all adults in the United States (45%) have hypertension (HTN).1 Multiple classes of antihypertensive medications are available to effectively control blood pressure.2 Controlled HTN reduces the risk of mortality and cardiovascular disease.2, 3 It is estimated that a small 2-mm Hg reduction in diastolic blood pressure decreases the incidence of coronary heart disease by 6% and stroke by 17%.4 Despite the clear benefits of antihypertensive medications on blood pressure control and cardiovascular disease, less than half of adults with HTN take their blood pressure medications as prescribed.2, 5, 6
Medication adherence has traditionally been viewed as a patient-driven problem.7 The World Health Organization (WHO) developed a conceptual framework of medication adherence that emphasizes its multifactorial and dynamic nature. According to the WHO model, medication adherence is influenced by the interplay of five major types of barriers: patient-related, healthcare system-related, therapy-related, condition-related, and social and economic factors.7 There is strong evidence of the negative impact of unfavorable social and economic factors, also known as social determinants of health (SDH), on health outcomes.8–10 Yet, relatively few studies have evaluated the relationship between SDH and antihypertensive medication adherence (AHMA).11–17 The purpose of this study is to quantify the influence of SDH on AHMA in a Medicaid population. We hypothesized that after controlling for age, sex and illness severity, adverse SDH would be associated with lower AHMA.
METHODS
Overview
In this prospective cohort study, we use self-reported SDH information that we collected during an interview at time of enrollment in the Medicaid Cohort of the District of Columbia (MCDC) study and participants’ Medicaid claims data to evaluate the relationship between SDH and AHMA. We used the Medicaid claims data in the 2-year period prior to study enrollment to identify MCDC participants with a diagnosis of HTN and to estimate their illness severity. We used the Medicaid claims data during the first 12 months post study enrollment to determine whether they were covered by at least one antihypertensive medication during a 1-year follow-up period. We categorized our HTN cohort into four social risk groups based on their SDH interview data using latent class analysis. We determined whether the participants were covered by an antihypertensive medication each day of the follow-up period as a function of social risk group, age, sex, and illness severity using a generalized linear model. The George Washington University institutional review board approved this study. The data that support the findings of this study are available from the corresponding author upon request.
Parent Study
The parent study consists of 8,943 adult beneficiaries insured by the DC Medicaid program who enrolled in the MCDC study between September of 2017 and December of 2018 at the time of a healthcare visit to the emergency department, a primary care clinic or an obstetrics and gynecology clinic affiliated with one of two medical facilities located in Washington, DC.18 Participants were between the ages of 18 and 64 at enrollment, insured solely by the DC Medicaid program, and had access to a telephone. At enrollment, participants completed a SDH questionnaire administered by a research assistant and agreed to allow the study team to obtain a copy of their DC Medicaid claims data for a 4-year period (2 years pre and 2 years post study enrollment).
Study Population
We relied on the Medicaid claims data for the 24-month period prior to and including the day of study enrollment to identify participants in the MCDC with HTN. The claims data include both eligibility information (i.e. dates of Medicaid coverage, reason for eligibility, demographics, etc) as well as detailed billing information such as type of claim (i.e. inpatient, outpatient, pharmacy, professional, etc), first and last date of service, diagnosis codes, and provider name. We searched all Medicaid claims during the 24-month period for a diagnosis of HTN, defined as a diagnosis code between I10.x and I16.x according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems International Classification of Diseases (ICD-10).19 We defined an MCDC participant as having hypertension if they had a HTN diagnosis code associated with at least one inpatient visit or two outpatient encounters.20
Using the above criteria, we identified 3,050 (34%) MCDC participants with HTN during the 2-year pre study enrollment period for this posthoc subgroup analysis. We excluded six participants with a HTN diagnosis during the 2-year pre study enrollment period who were not covered by Medicaid for at least one day during the 1-year follow-up period so our final sample size for this analysis is 3,044. Almost two-thirds (64%) of participants met our definition based on having at least two outpatients visits with an HTN diagnosis code during the 2-year pre-study enrollment period, one-third (34%) had an HTN diagnosis code associated with at least one inpatient visit and one outpatient encounter. Only 2% met our HTN definition based solely on at least one inpatient HTN diagnosis code. (see Supplemental Figure 1).
Social Risk
At the time of enrollment, all participants completed a face-to-face interview with a trained research assistant. The interview was designed to measure SDH according to the World Health Organization’s conceptual model.21 Using validated questions or short scales, we measured the following SDH: (1) structural determinants of health inequities (i.e. education, employment status, race, sex, and sexual orientation); (2) material circumstances (i.e. food insecurity, housing instability, housing conditions, trouble paying bills,); (3) health behaviors (i.e. smoking, drinking, drug use, exercise); and (4) psychological factors (marital status, living arrangements, loneliness). The SDH questions asked participants to describe their current state at the time of study enrollment (i.e. health behaviors, loneliness) or their circumstances within the past one (i.e. food insecurity, financial strain,) or two year period (i.e. jail/prison, abusive relationship) prior to study enrollment. In other words, all SDH factors were measured prior to the medication adherence one-year post study enrollment period.
Because SDH are correlated with one another18, considering all SDH factors simultaneously in a multivariate regression model, may mask relationships and lead to important associations being undetected. To counter this, we used latent class analysis (LCA) to categorize our HTN cohort into unique social risk groups based on their response profiles to 21 SDH variables. We dichotomized all of the 21 SDH factors to make it easier to interpret the social risk groups and we ran models with 2 – 6 groups. The LCA estimates an individual’s probability of being in each of different groups given their pattern of responses on the SDH questions. We chose a four group solution for our HTN cohort based on fit, classification diagnostics and ease of interpretation.18, 22
Participants in social risk group 1 reported the fewest social adversities and were most likely to be employed (62%); we refer to group 1 as “employed and least social adversity.” They comprise one-third of the HTN sample. Participants in group 1 were the most likely to report living with children (53%). Group 2 participants, 19% of the sample, were more similar to social risk group 1 in terms of employment (48%) but they were the most likely to report financial strain of all four groups; we refer to social risk group 2 as “employed and high financial strain.” The majority of participants in group 2 reported difficulty paying their phone (68%), rent/mortgage (76%) and/or utilities (80%) in the past year.
Social risk group 3 participants, 37% of the sample, were mostly unemployed (85%) and without a high school degree (42%). They were distinguished by reporting limited to no internet access at home (76%) and no access to a car for medical appointments (63%) but did not commonly report other material resource issues such as food insecurity or housing instability. We labeled social risk group 3 “unemployed and limited internet and car access.” Social risk group 4 participants (11%) reported the most social adversities in all dimensions so we named this group “unemployed with the most social adversity”. Similar to social risk group 3, the unemployment rate was high (88%) and almost one-third did not have a high school degree (31%). Participants in group 4 reported high rates of unhealthy behaviors such as smoking (74%) and illicit drug use (20%), problems with food insecurity (73%) and housing instability (76%). Table 1 displays the prevalence of the 21 SDH risk factors for our four social risk groups and Figure 1 highlights the group differences using a line graph.
Table 1.
Presence of Social Adversities By Social Risk Group*.
| Social Risk Group | |||||
|---|---|---|---|---|---|
| Social Risk Factor† | Overall N=3,044 | Group 1 N=1,017 | Group 2 N=570 | Group 3 N=1,111 | Group 4 N=346 |
| A. Structural | |||||
| No High School Degree/GED | 708 (23%) | 45 (4%) | 87 (15%) | 467 (42%) | 109 (32%) |
| Not Working | 1934 (64%) | 390 (38%) | 294 (52%) | 944 (85%) | 306 (88%) |
| B. Intermediary- Social | |||||
| Not Married (single/never married /separated/divorced/widowed) | 2577 (85%) | 803 (79%) | 476 (84%) | 994 (89%) | 304 (88%) |
| Living with Children | 1148 (38%) | 538 (53%) | 286 (50%) | 251 (23%) | 73 (21%) |
| Relationship with Someone who Threatened/Physically Hurt You | 944 (31%) | 196 (19%) | 198 (35%) | 349 (31%) | 201 (58%) |
| Been in Jail or Prison | 1127 (37%) | 216 (21%) | 144 (25%) | 545 (49%) | 222 (64%) |
| Lonely A Good bit/Most/All of the Time | 597 (20%) | 50 (5%) | 111 (19%) | 213 (19%) | 223 (64%) |
| C. Intermediary- Health Behaviors | |||||
| Current Smoker | 1389 (46%) | 240 (24%) | 224 (39%) | 669 (60%) | 256 (74%) |
| Drinks Alcohol (male > 14/week; female > 7/week) | 140 (5%) | 18 (2%) | 21 (4%) | 74 (7%) | 27 (8%) |
| Uses Illicit Drugs | 159 (5%) | 2 (0%) | 9 (2%) | 78 (7%) | 70 (20%) |
| Vigorous Exercise < 3 times/week | 1624 (53%) | 434 (43%) | 306 (54%) | 675 (61%) | 209 (60%) |
| D. Intermediary – Financial Strain | |||||
| Trouble Paying Phone Bill | 654 (21%) | 40 (4%) | 386 (68%) | 57 (5%) | 171 (49%) |
| Trouble Paying Utilities | 905 (30%) | 125 (12%) | 457 (80%) | 133 (12%) | 190 (55%) |
| Trouble Paying Rent/Mortgage | 707 (23%) | 39 (4%) | 433 (76%) | 52 (5%) | 183 (53%) |
| E. Intermediary- Material Resources | |||||
| No Car Access for Medical Appointments | 1373 (45%) | 203 (20%) | 217 (38%) | 701 (63%) | 252 (73%) |
| Limited to No Internet Access at Home | 1556 (51%) | 231 (23%) | 220 (39%) | 848 (76%) | 257 (74%) |
| Food Insecure | 658 (22%) | 30 (3%) | 172 (30%) | 202 (18%) | 254 (73%) |
| Does Not Live in House Or Apartment | 307 (10%) | 7 (1%) | 13 (2%) | 169 (15%) | 118 (34%) |
| Poor Housing Conditions | 496 (16%) | 64 (6%) | 144 (25%) | 130 (12%) | 158 (46%) |
| Housing Instability | 763 (25%) | 38 (4%) | 192 (34%) | 268 (24%) | 265 (77%) |
| Living in Same Place < 1 Year | 635 (21%) | 139 (14%) | 96 (17%) | 265 (24%) | 135 (39%) |
Group 1= employed and fewest social risks; Group 2= employed and high financial strain; Group 3= unemployed and limited internet and car access; Group 4= unemployed and many social risks.
All SDH risk factors vary significantly by social risk group (p < 0.001).
Figure 1.
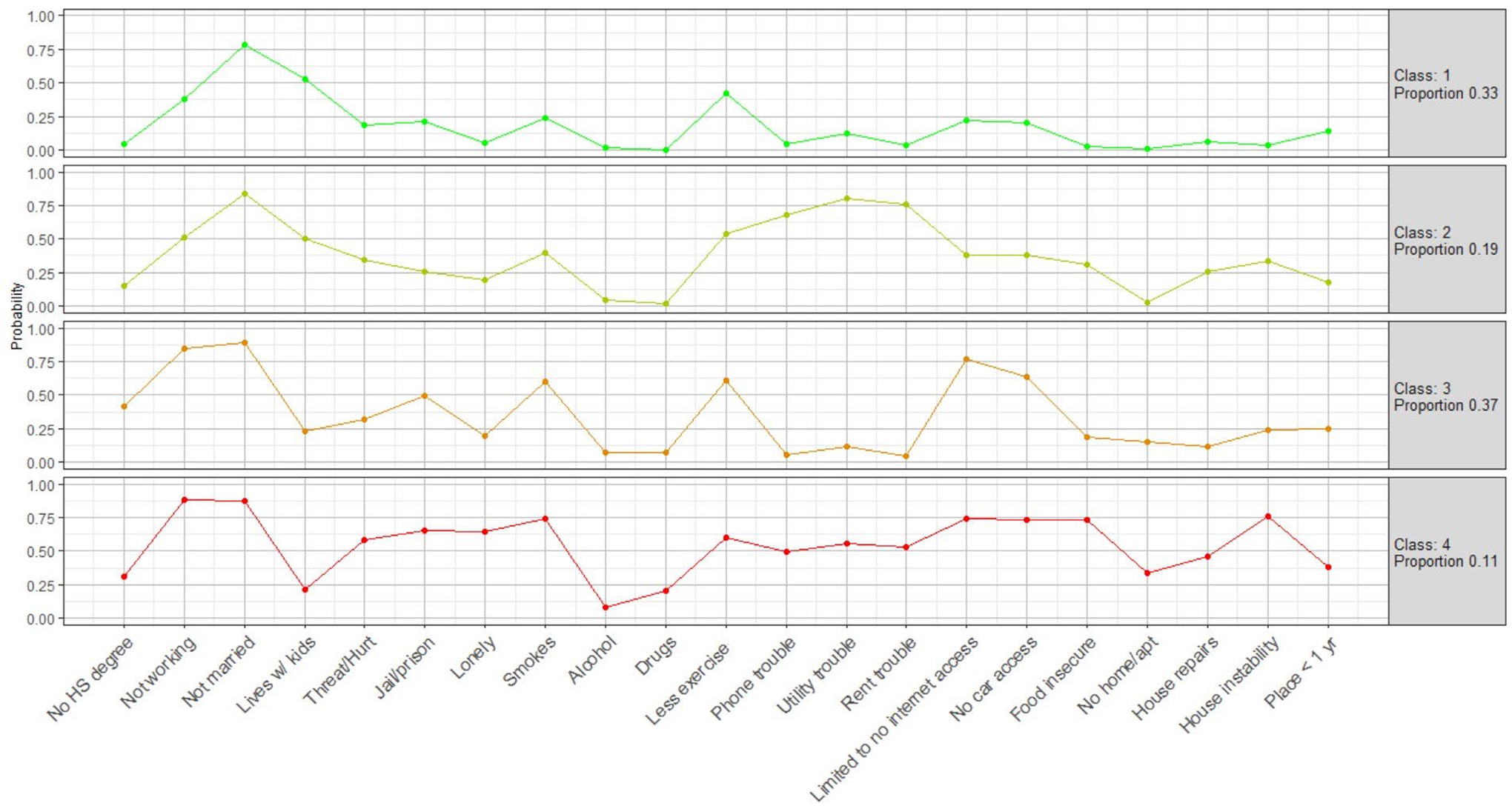
The Probability Of Each Social Adversity By The Four Social Risk Groups.
Class 1: Employed and Fewest Social Risks, Class 2: Employed and High Financial Strain, Class 3: Unemployed and Limited Internet and Car Access, Class 4: Unemployed and Many Social Risks
Illness Severity
We also used the 24-month pre-study enrollment claims data to estimate illness severity according to the Chronic Disability Payment System (CDPS). The CDPS is a risk adjustment measure developed specifically for the Medicaid population.23, 24 The CDPS classifies medical diagnoses using the ICD-10 diagnosis codes and national drug codes (NDC) documented in the encounter and pharmacy claims data into 20 major diagnosis categories and 15 major pharmacy groups and then within each category stratifies by level of severity. It does not include any SDH information. The CDPS applies weights to the different categories and severities to estimate an overall CDPS score. A higher score reflects more severe illness. In a population-based sample of Medicaid beneficiaries, the mean CDPS score ranged from 0.55 among adults to 1.60 for dual eligible disabled adults.25
Table 2 shows the distribution of the four social risk groups by age and sex as well as the CDPS. These factors were not included in the latent class analysis but are correlated with social adversities and all vary significantly by social risk group. The mean age across the four social risk groups ranges from 49 to 52 years (data not shown). Social risk groups 1 and 2 have a higher proportion of females (68% - 72%) whereas the sex distribution is more evenly distributed in social risk groups 3 and 4 (52% - 53%). Most striking is the association between the CDPS and the social risk groups. Social risk groups 3 and 4 are much more likely to be represented in the higher range of the illness severity distribution.
Table 2.
Demographic and Illness Severity Distribution By Social Risk Group*.
| Demographics and Illness Severity | Overall N=3,044 | Group 1 N=1,017 | Group 2 N=570 | Group 3 N=1,111 | Group 4 N=346 |
|---|---|---|---|---|---|
| A. Demographics | |||||
| Age at Time of Study Enrollment † | |||||
| 18 – 39 | 623 (20%) | 281 (28%) | 143 (25%) | 136 (12%) | 63 (18%) |
| 40 – 55 | 1,416 (47%) | 491 (48%) | 281 (49%) | 479 (43%) | 165 (48%) |
| 56+ | 1,005 (33%) | 245 (24%) | 146 (26%) | 496 (45%) | 118 (34%) |
| Sex † | |||||
| Male | 1,168 (38%) | 321 (32%) | 158 (28%) | 522 (47%) | 167 (48%) |
| Female | 1,876 (62%) | 696 (68%) | 412 (72%) | 589 (53%) | 179 (52%) |
| B. Chronic Disability Payment System † | |||||
| Lowest quartile (healthiest) | 761 (25%) | 378 (37%) | 175 (31%) | 172 (15%) | 36 (10%) |
| Lower middle | 761 (25%) | 271 (27%) | 163 (29%) | 242 (22%) | 85 (25%) |
| Lower upper | 761 (25%) | 228 (22%) | 121 (21%) | 317 (29%) | 95 (27%) |
| Upper quartile (sickest) | 761 (25%) | 140 (14%) | 111 (19%) | 380 (34%) | 130 (38%) |
Group 1= employed and fewest social risks; Group 2= employed and high financial strain; Group 3= unemployed and limited internet and car access; Group 4= unemployed and many social risks.
The difference between groups is significant at p<0.001.
Outcome Measure
Our primary outcome was AHMA which we measured both in aggregate as well as daily during the 1-year follow-up period. The aggregate AHMA measure we used was the proportion of days covered (PDC), a validated and widely used measure of medication adherence that is based on the fill dates and days supply for each prescription medication fill.26, 27 To calculate the PDC, first, we identified all antihypertensive medications filled by each participant during the 1-year follow-up period. The Medicaid pharmacy claims include the following information: date prescription was filled, national drug code (NDC)28, generic and brand name of the drug dispensed according to the drug code, the number of days supply of the medication, and whether the prescription was new or a refill.
We identified all NDCs for the following seven classes of antihypertensive medications: (1) diuretics; (2) ACE inhibitors, ACE Inhibitor/diuretic combinations; (3) Calcium Channel Blockers (DHP), Calcium Channel Blockers (NonDHP); (4) Angiotensin Receptor Blockers, Angiotensin Receptor Blockers/diuretic combinations, Angiotensin Receptor Modulators combinations; (5) Sympatholytics; (6) Beta Blockers, Beta Blockers/Diuretic combinations; and (7) Bidil, hydralazine. We merged our antihypertensive NDC list with the NDC data field in the Medicaid pharmacy claims and isolated all antihypertensive prescription medications filled by participants.
Second, for each participant, we defined their AHMA follow-up period as the date of study enrollment until 365 days later or until the end of their Medicaid coverage, whichever came first. The AHMA follow-up period varied among participants (mean=346 days, SD=58) depending on how long they had been enrolled in the Medicaid program during the 1-year follow-up period; 91% were enrolled in Medicaid for the entire 1-year period.
Third, for each day during the AHMA follow-up period, we determined whether the participant had an HTN prescription fill that covered that day. When a refill occurred early (i.e. before the previous refill ran out), we assumed the new refill coverage started the day after the end date of the previous refill supply. If a participant had a supply of more than one HTN prescription medication at the same time, we did not double count the medications, instead we counted each day as covered by an HTN medication because we could not determine whether the participant was supposed to be taking concurrent HTN medications or was switching from one medication to another. If the participant was hospitalized during the AHMA follow-up period, we assumed that the beneficiary received their medication during the hospital stay.
The average PDC for each participant is the total number of days with a HTN prescription divided by the total AHMA follow-up days. The average PDC has a possible range of 0 to 1 with zero meaning that the participant did not fill any HTN medication (primary non adherence) and 1 meaning the participant had at least one HTN medication for each day during the AHMA follow-up period (i.e. perfect secondary adherence).
Statistical Methods
The analysis was conducted in two stages. First, we examined the relationship between the PDC and age, sex, individual SDH factors, social risk group and quartiles of the Chronic Disability Payment System (CDPS) score by calculating the mean PDC and standard error (SE) for each response category of the predictor variables. We tested for statistically significant differences in the mean PDC by each predictor using one way ANOVA.
Second, we used a quasi-binomial generalized linear model (GLM) to evaluate the relationship between social risk group and daily AHMA, controlling for age, sex and the CDPS. We modeled the odds of each participant being covered by a HTN prescription medication daily during the AHMA follow-up period. We assumed AHMA could be correlated across days since one prescription fill covered more than one day of medicine. This correlation was accounted for using robust variance estimates with observations grouped by person. We log transformed the CDPS score because of its highly skewed right distribution and included it in the multivariate model as a natural cubic spline with three degrees of freedom to allow for a nonlinear relationship with the outcome. We tested for all possible interaction effects among the predictor variables.
Finally, as a sensitivity analysis, we dropped the participants with an average PDC of zero (i.e. primary non adherence) and compared the GLM results with the regression results of the full sample. We used R software, version 3.6.2, poLAC for the latent class analysis and GLM that is part of the R package called “stats” for the quasi-binomial GLM.
RESULTS
Participant Characteristics
Of the 3,044 in the AHMA study, 99% of those with HTN had a diagnosis of essential HTN (I10). A smaller percentage of participants had a diagnosis of hypertensive heart disease (I11: 13%), hypertensive chronic kidney disease (I12: 7%) or both (I13: 4%). Five percent had a diagnosis of hypertensive crisis (I16); secondary hypertension was rare (I15: 1%).
Almost one-third (28%) of our participants were taking a single anti-hypertensive drug during the follow-up period (Table 3). Most commonly, patients were prescribed an ACE inhibitor, calcium channel blocker, diuretic or a combination. Figure 2 demonstrates the distribution of the PDC during the AHMA follow-up period. Twenty percent of our sample were primary non adherent (i.e. never filled any antihypertensive medications) and 16% of our sample had optimal AHMA (i.e. PDC=1). Thirty-seven percent of the sample had a PDC of 80% or greater, a common cutoff used to define good adherence.
Table 3.
Number and Types of Antihypertension Medication Classes Prescribed to Study Sample. (N=3,044).
| Hypertension Medication Class | N | Column Percent |
|---|---|---|
| No HTN prescriptions filled | 600 | 20% |
| Single Medication Class | 865 | 28% |
| Diuretics | 244 | |
| Angiotensin-converting enzyme (ACE) inhibitors, ACE Inhibitor/diuretic combinations (ACE) | 232 | |
| Calcium channel blockers (CCB) | 235 | |
| Angiotensin receptor blockers, angiotensin receptor blockers/diuretic angiotensin receptor modulators (AR) | 88 | |
| Beta blockers, beta blockers/diuretic combinations (BB) | 51 | |
| Sympatholytics | 13 | |
| Bidil, hydralazine | 2 | |
| Two Medication Classes * | 811 | 27% |
| Diuretics plus CCB | 184 | |
| Diuretics plus ACE | 150 | |
| Diuretics plus AR | 51 | |
| ACE plus CCB | 128 | |
| AR plus CCB | 84 | |
| BB plus CCB | 58 | |
| Other two class combinations | 156 | |
| Three Medication Classes * | 499 | 16% |
| Diuretics + BB + CCB | 50 | |
| Diuretics + AR + CCB | 64 | |
| Diuretics + ACE + CCB | 132 | |
| Other 3 class combinations | 253 | |
| Four Medication Classes * | 194 | 6% |
| Five or more Medication Classes * | 75 | 2% |
Only listed two or more medication classes if N ≥ 50.
Figure 2.
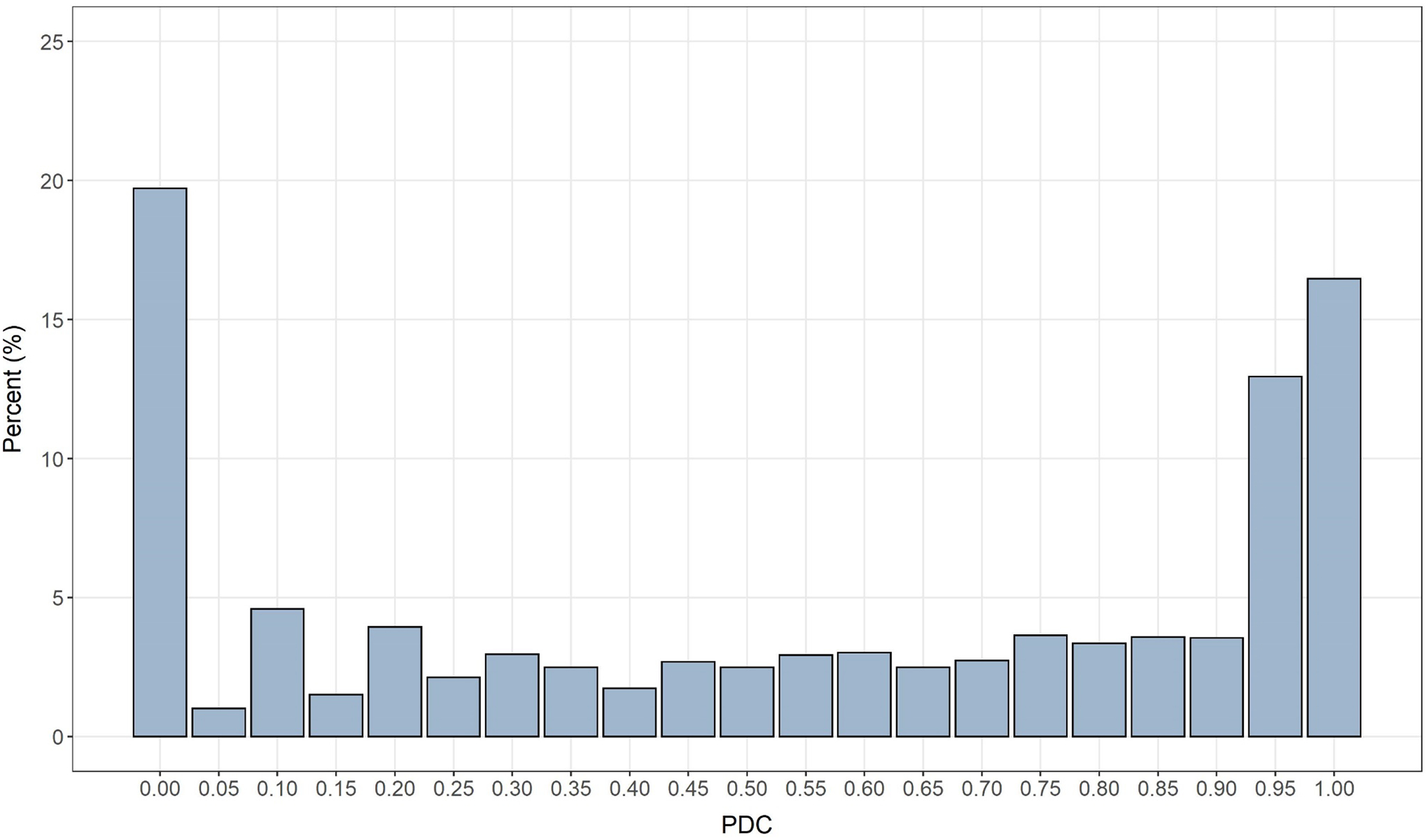
Percent Distribution of the Proportion of Days Covered (PDC) By An Antihypertensive Medication Among Participants with Hypertension.
Table 4 displays the mean PDC by SDH factors. The majority of our study sample was black (93%) and female (62%). More than three-quarters (77%) of our cohort had a high school degree and 36% were working at the time of study enrollment. The mean PDC was significantly higher with each age group (33% - 61%) (p < 0.001). The average PDC varied significantly for many of the SDH factors, commonly by 5% or more. For example, participants who reported they had been in a relationship with someone who threatened or physically hurt them had an average PDC of 50% compared to those who had not (55%) (p < 0.05). Participants who reported living at their present residence for five years or more had an average PDC of 57% compared to 47% of those living at their residence for less than one year (p < 0.001). Finally, the mean PDC increased significantly by each CDPS quartile (47% - 58%) (p < 0.001).
Table 4.
Mean Proportion of Days Covered (Standard Error) By Social Determinants of Health And Chronic Disability Payment System (N=3,044).
| Proportion of Days Covered | ||
|---|---|---|
| Characteristic | N (%) | Mean (SE) |
| A. Demographics | ||
| Age at Time of Study Enrollment † | ||
| 18 – 39 | 623 (20%) | 0.33 (0.01) |
| 40 – 55 | 1,416 (47%) | 0.56 (0.01) |
| 56+ | 1,005 (33%) | 0.61 (0.01) |
| B. Structural Social Determinant of Health | ||
| Sex | ||
| Male | 1,168 (38%) | 0.52 (0.01) |
| Female | 1,876 (62%) | 0.54 (0.01) |
| Race * | ||
| Black | 2,820 (93%) | 0.53 (0.01) |
| White | 40 (1%) | 0.47 (0.07) |
| Latino | 39 (1%) | 0.48 (0.06) |
| Other | 144 (5%) | 0.56 (0.03) |
| Sexual orientation | ||
| Heterosexual/bisexual | 2,839 (93%) | 0.53 (0.01) |
| Gay/Lesbian/Other | 127 (4%) | 0.55 (0.03) |
| DK or Refused | 78 (3%) | 0.48 (0.05) |
| Education * | ||
| < High school degree | 708 (23%) | 0.54 (0.01) |
| High school degree/GED | 1,472 (48%) | 0.53 (0.01) |
| Some college/associate’s degree | 654 (22%) | 0.53 (0.02) |
| Bachelor’s degree+ | 208 (7%) | 0.56 (0.03) |
| Employment Status * † | ||
| Working full-time (1 or 2 jobs) | 705 (23%) | 0.52 (0.01) |
| Working part-time | 405 (13%) | 0.53 (0.02) |
| Not working but looking for work | 710 (23%) | 0.47 (0.01) |
| Not working due to disability/ill | 996 (33%) | 0.59 (0.01) |
| Not working for other reasons | 223 (8%) | 0.51 (0.03) |
| C. Psychosocial | ||
| Marital Status * † | ||
| Married/living together | 467 (15%) | 0.56 (0.02) |
| Single/Never married | 1,886 (62%) | 0.51 (0.01) |
| Widowed/separated/divorced | 689 (23%) | 0.57 (0.01) |
| Living Arrangements * † | ||
| Living alone | 720 (24%) | 0.56 (0.01) |
| Living with adults only | 1,171 (38%) | 0.57 (0.01) |
| Living with children only | 256 (8%) | 0.40 (0.02) |
| Living with children and adults | 890 (29%) | 0.50 (0.01) |
| Been in a Relationship With Someone Who Threatened or Physically Hurt You ‡ | ||
| Yes | 913 (30%) | 0.50 (0.01) |
| No | 2,049 (67%) | 0.55 (0.01) |
| Don’t know/refused | 82 (3%) | 0.50 (0.05) |
| Ever Been in Jail or Prison ‡ | ||
| Yes | 1,092 (36%) | 0.50 (0.01) |
| No | 1,869 (61%) | 0.55 (0.01) |
| Don’t know/refused | 83 (3%) | 0.46 (0.04) |
| Frequency of Feeling Lonely * † | ||
| Good bit/most/all of the time | 591 (19%) | 0.49 (0.02) |
| Some or a little of the time | 806 (26%) | 0.52 (0.01) |
| None of the time | 1,626 (53%) | 0.56 (0.01) |
| D. Health Behaviors | ||
| Has a Doctor For Health Needs * † | ||
| Yes | 2676 (88%) | 0.55 (0.01) |
| No | 358 (12%) | 0.37 (0.02) |
| Current Smoker* † | ||
| Yes | 1385 (46%) | 0.50 (0.01) |
| No | 1649 (54%) | 0.56 (0.01) |
| Alcohol Consumption ‡ | ||
| None | 1949 (64%) | 0.54 (0.01) |
| 1 – 3 drinks per week | 620 (20%) | 0.53 (0.02) |
| ≥ 4 drinks per week | 475 (16%) | 0.49 (0.02) |
| Uses Illicit Drugs † | ||
| Yes | 159 (5%) | 0.41 (0.03) |
| No | 2885 (95%) | 0.54 (0.01) |
| Engages in Vigorous Physical Activity * † | ||
| No | 1151 (38%) | 0.57 (0.01) |
| 1 to 2 days a week | 471 (15%) | 0.53 (0.02) |
| 3 to 4 days a week | 476 (16%) | 0.53 (0.02) |
| ≥ 5 days per week | 944 (31%) | 0.48 (0.01) |
| E. Material Resources | ||
| Internet Access at Home * † | ||
| No internet access at home | 466 (15%) | 0.59 (0.02) |
| Internet access by phone or computer | 1079 (35%) | 0.51 (0.01) |
| Internet access by phone and computer | 1482 (49%) | 0.53 (0.01) |
| Has Access to Car For Medical Appointments * | ||
| Yes | 1661 (55%) | 0.52 (0.01) |
| No | 1370 (45%) | 0.54 (0.01) |
| Trouble Paying Phone/Rent or Mortgage/Utilities | ||
| No trouble | 1750 (57%) | 0.54 (0.01) |
| One of the bills | 657 (22%) | 0.52 (0.02) |
| Two of the bills | 302 (10%) | 0.53 (0.02) |
| All three bills | 335 (11%) | 0.54 (0.02) |
| Food Insecurity*‡ (“Worried food would run out before you could buy more?”, “Food ran out and you didn’t have money to buy more?” | ||
| None | 1430 (47%) | 0.56 (0.01) |
| Sometimes true to one question | 953 (31%) | 0.51 (0.01) |
| Always true to one question | 304 (10%) | 0.50 (0.02) |
| Always true to both questions | 354 (12%) | 0.49 (0.02) |
| Housing Situation | ||
| House | 806 (26%) | 0.52 (0.01) |
| Apartment | 1931 (63%) | 0.54 (0.01) |
| Other | 307 (10%) | 0.49 (0.02) |
| Housing Condition Problems | ||
| None | 1909 (63%) | 0.53 (0.01) |
| One | 639 (21%) | 0.54 (0.02) |
| Two or more | 496 (16%) | 0.53 (0.02) |
| Worried About Housing Stability | ||
| Yes | 763 (25%) | 0.52 (0.01) |
| No | 2281 (75%) | 0.54 (0.01) |
| Length of Time Living at Present Place * † | ||
| < 1 year | 628 (21%) | 0.47 (0.02) |
| 1 – 2 years | 356 (12%) | 0.49 (0.02) |
| 2 – 4 years | 643 (21%) | 0.53 (0.02) |
| 5+ years | 1402 (46%) | 0.57 (0.01) |
| Social Risk Group | ||
| Group 1: employed and the least social adversity | 1017 (33%) | 0.54 (0.01) |
| Group 2: employed and high financial strain | 570 (19%) | 0.54 (0.02) |
| Group 3: unemployed and limited internet and car access | 1111 (37%) | 0.54 (0.01) |
| Group 4: unemployed the most social adversity | 346 (11%) | 0.48 (0.02) |
| F. Chronic Disability Payment System † | ||
| Lowest quartile (healthiest) | 761 (25%) | 0.47 (0.01) |
| Lower middle | 760 (25%) | 0.52 (0.01) |
| Lower upper | 762 (25%) | 0.55 (0.01) |
| Upper quartile (sickest) | 761 (25%) | 0.58 (0.01) |
Missing data not shown in table when < 25 responses.
The difference between groups is significant at p<0.001.
The difference between groups is significant at p < 0.05.
Main Outcome
Figure 3 displays the adjusted daily odds ratio of having an antihypertensive prescription medication during the AHMA follow-up period by social risk group. Compared to social risk group 1 (employed and least social adversity), participants in social risk group 4 (unemployed and most social adversity) had a 36% lower odds of having an antihypertensive prescription medication (aOR=0.64; 95% CI 0.53, 0.78). Participants in social risk group 3 (unemployed and limited internet and car access) had a 20% lower odds (aOR=0.80; (95% CI 0.70, 0.93) of having an antihypertensive prescription medication during the AHMA follow-up period compared to those in social risk group 1. Participants in social risk group 2 had a 5% lower odds (aOR=0.95; 95% CI 0.80 – 1.11) of having an antihypertensive prescription medication during follow-up compared to those in social risk group 1.
Figure 3.
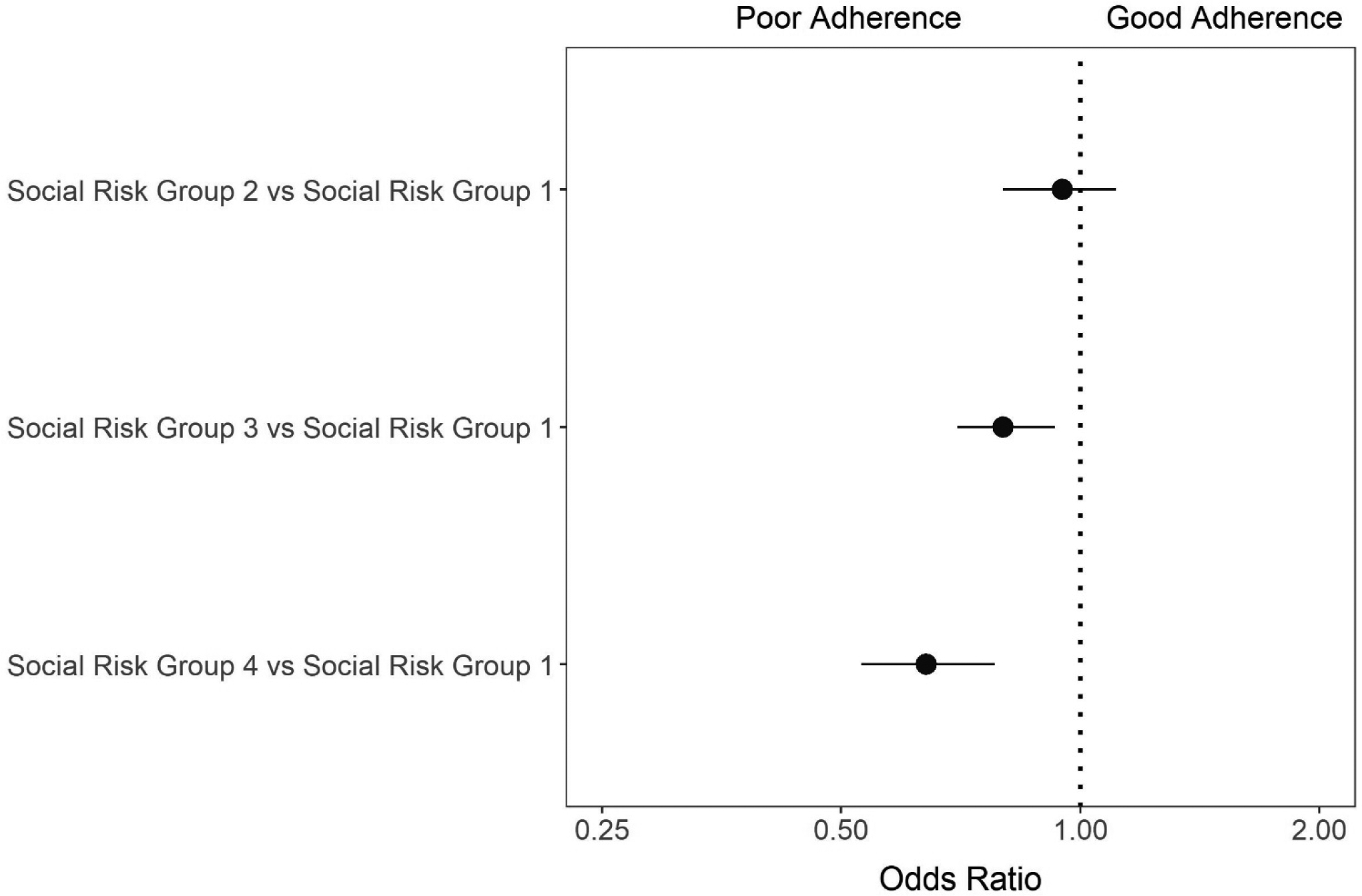
Odds Ratio Of Being Covered By An Antihypertensive Medication Daily During Follow-Up Period By Social Risk Group, Adjusted for Age, Sex and Chronic Disability Payment Score.
Group 1 = Employed and the least social adversity
Group 2 = Employed and high financial strain
Group 3 = Unemployed and limited internet and car access
Group 4 = Unemployed and the most social adversity
When we excluded the participants who never filled at least one antihypertensive prescription during the AHMA follow-up period, the results were qualitatively the same (see supplemental table 1).
DISCUSSION
We observed suboptimal AHMA in the majority of adult Medicaid beneficiaries with HTN in our cohort. When examined individually, there were significant differences in AHMA by many SDH. After grouping participants into four social risk groups, participants with more social adversities had a lower daily odds of having an antihypertensive prescription medication during the AHMA follow-up period compared to those with the fewest social adversities. Our results suggest that if we want to achieve optimal AHMA in the Medicaid population, health insurance coverage for prescription medications is insufficient, we must address social adversities that inhibit patients from managing their medications and health effectively.
Previous literature has not found a consistent relationship between SDH and AHMA. We suspect that this is likely due to methodological issues.29 Past studies have often relied on cross-sectional data11, 16, 17, self-reported measures of AHMA11, 15–17, and few SDH12, 13, 15. The most commonly studied SDH factors have been income29, health literacy13, stress17, discrimination15 and racial/ethnic bias12. The majority of these studies have focused on a single SDH such as perceived discrimination and not taken into account other types of SDH factors such as health behaviors or material resources (i.e. housing instability, food insecurity, etc).
The results of this study are consistent with a growing body of evidence that shows that social adversities negatively impact health outcomes including mortality30, 31, disease prevalence32–34, self-reported health32, 35, 36 and healthcare utilization37, 38. It is not surprising that we found that adverse SDH negatively impact AHMA in a Medicaid population. There are multiple ways that SDH can influence medication adherence.8, 34 First, social determinants shape health behaviors. For example, education increases health literacy8, 39 and health literacy is associated with medication adherence.40 Second, people with adverse social risk factors often live in disadvantaged neighborhoods that make it more challenging to maintain a healthy lifestyle.33 Physical environments that are unsafe and lack easy access to needed goods and services may contribute to medication non adherence.41 Third, adverse social and environmental circumstances cause stress and unhealthy behaviors are more likely to occur under stressful conditions. Prolonged stress can cause depression and depression is a risk factor for poor AHMA.42, 43
In this study, we grouped participants into four social risk groups. While we did this because of the correlation among individual social determinants of health, our results clearly show that within the socioeconomic domain of the WHO medication adherence model, our adult Medicaid participants commonly face more than one social adversity.44 Participants in social risk group 2, employed and high financial strain, reported different problems than participants in social risk group 3, unemployed and limited internet and car access. These finding suggest that even within a Medicaid population, tailored interventions to improve adherence that are customized to address the specific problems of each beneficiary will be more likely to succeed than a one size fits all intervention.45
The study results also provide evidence of the value of conducting a multidimensional SDH assessment. It is likely that the influence of different SDH factors will vary depending on the health outcome, the patient population and whether the risk factor exists alone or in the presence of other risk factors. Multidimensional SDH assessments allows us to better understand the complex interplay between structural and intermediary determinants of health, health outcomes and the healthcare delivery system. Furthermore, they will give us the insight we need to develop multilevel and multisector solutions to existing health disparities.
Consistent with a number of other studies, younger age and male sex were associated with poorer AHMA.46, 47 For example, Bautista et al found in a nationally representative sample that non-persistence with HTN medication was about 2.5 times higher among adults between the ages of 30 – 49 compared to those 50 or older and 31% higher for males compared to females.47
The results of this study should be interpreted in the context of the following limitations. First, our results may be influenced by measurement error. It is possible that some of the participants, particularly those who never filled any antihypertensive prescription medications, may not have hypertension or may be controlling it through lifestyle changes. However, when we repeated our analysis without the participants who had an average PDC of zero, which means they never filled an antihypertensive prescription, our results were the same. It is also likely that we overestimated AHMA because we did not calculate separate PDCs for participants who filled more than one class of antihypertensive medications since we could not determine whether participants were supposed to be taking more than one medication or were switching from one to the other.
Second, we did not evaluate whether the influence of SDH on AHMA varied by drug type or therapeutic complexity. Third, while we measured a broad array of SDH factors, we did not include all factors that may influence AHMA such as health literacy, social support, stress, etc. In addition, our SDH factors were measured at a single point of time whereas AHMA was measured over a 24-month period prior to study enrollment. Some of the social and economic risk factors may have changed during the 1-year AHMA follow-up period.
Fourth, the relationship we found between SDH and AHMA should be interpreted as an association since it is possible that reverse causality may have occurred and that poor adherence leads to adverse social circumstances to occur (e.g. poor health causes unemployment) rather than vice versa. Since the DC Medicaid program does not require a co-pay for any covered prescription medications, it does not limit the number of prescriptions allowed per month and it does provide access to all therapeutic HTN drug classes, it is not likely that participants’ medication adherence was negatively impacted by cost-sharing policies. It is possible however, that in states with cost-sharing policies, good adherence may cause a Medicaid beneficiary to reduce or go without other material resources.
Finally, the generalizability of the results are limited because the participants are not a random sample of adult Medicaid beneficiaries with HTN but rather they were identified and enrolled in the parent study at the time of a healthcare visit. If our sample participants are more actively engaged in their health than Medicaid beneficiaries overall, then we may have underestimated the relationship between SDH and AHMA. It is also likely that the influence of SDH on AHMA may be larger in a sample that is more heterogeneous in terms of household income.
Despite these limitations, the results of our study suggest that adverse social determinants of health negatively impact AHMA. Going forward, if we want to reduce the cardiovascular health disparities that we observe among socially disadvantaged populations, we must address the social, economic and environmental risk factors that do not promote healthy behaviors, including medication adherence, at the individual, community and policy levels.
Supplementary Material
What Is Known.
Half of all adults in the United States have hypertension, however less than half adhere to their antihypertensive medication
Unfavorable social and economic factors, also known as social determinants of health, negatively impact a variety of health outcomes but little is known about their relationship to antihypertensive medication adherence
What This Study Adds.
In this Medicaid sample, two-thirds of participants demonstrated suboptimal adherence (i.e. < 80%) according to the proportion of days covered by an antihypertensive medication
Participants with more social adversities had poorer medication adherence compared to those with fewer, controlling for age, sex and disease burden
Adverse social determinants of health negatively impact antihypertensive medication adherence in a Medicaid sample with good prescription medication coverage
SOURCES OF FUNDING
This project was supported by NIH Grants #R01 MD011607-02 (Principal Investigator: McCarthy) and 3R01MD011607-02S1(Wilder).
NON-STANDARD ABBREVIATIONS AND ACRONYMS
- HTN
Hypertension
- SDH
Social Determinants of Health
- AHMA
Antihypertensive Medication Adherence
- MCDC
Medicaid Cohort of the District of Columbia
- LCA
Latent Class Analysis
- CDPS
Chronic Disability Payment System
- PDC
Proportion of Days Covered
- GLM
Generalized Linear Model
Footnotes
Meetings: This work has not been presented previously in whole or part.
COI: No financial conflicts of interest. (NONE)
DISCLOSURES
None.
REFERENCES
- 1.Centers for Disease Control and Prevention. High Blood Pressure. Facts about Hypertension in the United States https://www.cdc.gov/bloodpressure/facts.htm Published [1/28/2020]. Updated [7/19/2021]. Accessed [4/1/2021].
- 2.Kronish IM and Ye S. Adherence to cardiovascular medications: lessons learned and future directions. Progress in cardiovascular diseases. 2013;55:590–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brunström M and Carlberg B. Association of Blood Pressure Lowering With Mortality and Cardiovascular Disease Across Blood Pressure Levels: A Systematic Review and Meta-analysis. JAMA Intern Med. 2018;178:28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cook NR, Cohen J, Hebert PR, Taylor JO and Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–9. [PubMed] [Google Scholar]
- 5.Fryar CD, Ostchega Y, Hales CM, Zhang G and Kruszon-Moran D. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. NCHS Data Brief. 2017 (289):1–8. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria From the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2015–2018. Atlanta, GA: US Department of Health and Human Services; 2021. https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html Updated [3/22/2021]. Accessed [2/21/2021]. [Google Scholar]
- 7.Sabate E Adherence to Long-term Therapies: Evidence for Action. Geneva, World Health Organization, 2003. 1–211. ISBN 92 4 154599 2. [Google Scholar]
- 8.Braveman P and Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129 Suppl 2:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L and Curry LA. Variation In Health Outcomes: The Role Of Spending On Social Services, Public Health, And Health Care, 2000–09. Health Aff (Millwood). 2016;35:760–8. [DOI] [PubMed] [Google Scholar]
- 11.Bandi P, Goldmann E, Parikh NS, Farsi P and Boden-Albala B. Age-Related Differences in Antihypertensive Medication Adherence in Hispanics: A Cross-Sectional Community-Based Survey in New York City, 2011–2012. Prev Chronic Dis 2017;14:E57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blair IV, Steiner JF, Hanratty R, Price DW, Fairclough DL, Daugherty SL, Bronsert M, Magid DJ and Havranek EP. An investigation of associations between clinicians’ ethnic or racial bias and hypertension treatment, medication adherence and blood pressure control. J Gen Intern Med. 2014;29:987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNaughton CD, Jacobson TA and Kripalani S. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Couns. 2014;96:165–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H and Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forsyth J, Schoenthaler A, Chaplin WF, Ogedegbe G and Ravenell J. Perceived discrimination and medication adherence in black hypertensive patients: the role of stress and depression. Psychosomatic medicine. 2014;76:229–36. [DOI] [PubMed] [Google Scholar]
- 16.Lewis LM, Schoenthaler AM and Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. Journal of clinical hypertension (Greenwich, Conn). 2012;14:250–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang AW, Dulin A, Nadimpalli S and Risica PM. Stress, adherence, and blood pressure control: A baseline examination of Black women with hypertension participating in the SisterTalk II intervention. Preventive medicine reports. 2018;12:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCarthy ML, Zheng Z, Wilder ME, Elmi A, Kulie P, Johnson S and Zeger SL. Latent Class Analysis to Represent Social Determinant of Health Risk Groups in the Medicaid Cohort of the District of Columbia. Med Care. 2021;59:251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organzation(1992). International Classification of Diseases and related health problems (10th revision, ICD-10-CM). Geneva, Switzerland. [Google Scholar]
- 20.Gillingham M SAS Programming with Medicare Administrative Data. Cary, North Carolina: SAS Institute Inc.; 2014. [Google Scholar]
- 21.Solar O, Irwin A. A Conceptual Framework For Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). 2010. https://www.who.int/publications/i/item/9789241500852 Published [7/13/2010]. Accessed [9/29/2019]. [Google Scholar]
- 22.Lanza ST, Collins l.M., Lemmon D, Shafer JL PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling. 2007;14:671–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kronick R, Dreyfus T, Lee L and Zhou Z. Diagnostic risk adjustment for Medicaid: the disability payment system. Health Care Financ Rev. 1996;17:7–33. [PMC free article] [PubMed] [Google Scholar]
- 24.Kronick R, Gilmer T, Dreyfus T and Lee L. Improving health-based payment for Medicaid beneficiaries: CDPS. Health Care Financ Rev. 2000;21:29–64. [PMC free article] [PubMed] [Google Scholar]
- 25.Kronick RG, Bella T, Gilmer TP,Somers SA The Faces of Medicaid II: Recognizing the Care Needs of People with Multiple Chronic Conditions. Center for Health Care Strategies. https://www.chcs.org/resource/the-faces-of-medicaid-ii-recognizing-the-care-needs-of-people-with-multiple-chronic-conditions/ Published [10/2007]. Accessed [11/18/2019]. [Google Scholar]
- 26.Pharmacy Quality Alliance. Adherence: PQA Adherence Measures. https://www.pqaalliance.org/adherence-measures Published [2018]. Accessed [5/18/2018].
- 27.Martin BC, Wiley-Exley EK, Richards S, Domino ME, Carey TS and Sleath BL. Contrasting measures of adherence with simple drug use, medication switching, and therapeutic duplication. Ann Pharmacother. 2009;43:36–44. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Federal Drug Administration. National Drug Code Directory. https://www.fda.gov/drugs/drug-approvals-and-databases/national-drug-code-directory Updated [12/18/2020]. Accessed [1/15/2021].
- 29.Alsabbagh MH, Lemstra M, Eurich D, Lix LM, Wilson TW, Watson E and Blackburn DF. Socioeconomic status and nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Value Health. 2014;17:288–96. [DOI] [PubMed] [Google Scholar]
- 30.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A and Cutler D. The Association Between Income and Life Expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galea S, Tracy M, Hoggatt KJ, Dimaggio C and Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Braveman PA, Cubbin C, Egerter S, Williams DR and Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100 Suppl 1:S186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA and Sperling LS. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation. 2018;137:2166–2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marmot M and Bell R. Social determinants and non-communicable diseases: time for integrated action. Bmj. 2019;364:l251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Minkler M, Fuller-Thomson E and Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med. 2006;355:695–703. [DOI] [PubMed] [Google Scholar]
- 36.Case A and Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences of the United States of America. 2015;112:15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zulman DM, Maciejewski ML, Grubber JM, Weidenbacher HJ, Blalock DV, Zullig LL, Greene L, Whitson HE, Hastings SN and Smith VA. Patient-Reported Social and Behavioral Determinants of Health and Estimated Risk of Hospitalization in High-Risk Veterans Affairs Patients. JAMA network open. 2020;3:e2021457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJ, Schow M, Atlas SJ and Wexler DJ. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175:257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schillinger D, Barton LR, Karter AJ, Wang F and Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang NJ, Terry A and McHorney CA. Impact of health literacy on medication adherence: a systematic review and meta-analysis. Ann Pharmacother. 2014;48:741–51. [DOI] [PubMed] [Google Scholar]
- 41.August KJ and Billimek J. A theoretical model of how neighborhood factors contribute to medication nonadherence among disadvantaged chronically ill adults. Journal of health psychology. 2016;21:2923–2933. [DOI] [PubMed] [Google Scholar]
- 42.Bautista LE, Vera-Cala LM, Colombo C and Smith P. Symptoms of depression and anxiety and adherence to antihypertensive medication. Am J Hypertens. 2012;25:505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cené CW, Dennison CR, Powell Hammond W, Levine D, Bone LR and Hill MN. Antihypertensive medication nonadherence in black men: direct and mediating effects of depressive symptoms, psychosocial stressors, and substance use. Journal of clinical hypertension (Greenwich, Conn). 2013;15:201–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lauffenburger JC, Isaac T, Bhattacharya R, Sequist TD, Gopalakrishnan C and Choudhry NK. Prevalence and Impact of Having Multiple Barriers to Medication Adherence in Nonadherent Patients With Poorly Controlled Cardiometabolic Disease. The American journal of cardiology. 2020;125:376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu HY, Yu YJ, Zhang QH, Hu HY and Li M. Tailored Interventions to Improve Medication Adherence for Cardiovascular Diseases. Frontiers in pharmacology. 2020;11:510339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qvarnström M, Kahan T, Kieler H, Brandt L, Hasselström J, Bengtsson Boström K, Manhem K, Hjerpe P and Wettermark B. Persistence to antihypertensive drug treatment in Swedish primary healthcare. Eur J Clin Pharmacol. 2013;69:1955–64. [DOI] [PubMed] [Google Scholar]
- 47.Bautista LE. Predictors of persistence with antihypertensive therapy: results from the NHANES. Am J Hypertens. 2008;21:183–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


