Abstract
Background:
Olive oil consumption has been shown to lower cardiovascular disease risk, but its associations with total and cause-specific mortality are unclear.
Objectives:
To evaluate whether olive oil intake is associated with total and cause-specific mortality in two prospective cohorts of U.S. men and women.
Methods:
We used multivariable-adjusted Cox proportional-hazards models to estimate hazard ratios for total and cause-specific mortality among 60,582 women (Nurses’ Health Study, 1990-2018) and 31,801 men (Health Professionals Follow-up Study, 1990-2018) who were free of cardiovascular disease or cancer at baseline. Diet was assessed by a semi-quantitative food frequency questionnaire every 4 years.
Results:
During 28 years of follow-up, 36,856 deaths occurred. The multivariable-adjusted pooled HR (95% CI) for all-cause mortality among participants who had the highest consumption of olive oil (>1/2 tablespoon/d or >7g/d) was 0.81 (0.78, 0.84) as compared to those who never or rarely consumed olive oil. Higher olive oil intake was associated with 19% lower risk of cardiovascular disease mortality [0.81(0.75, 0.87)], 17% lower risk of cancer mortality [0.83(0.78, 0.89)], 29% lower risk of neurodegenerative disease mortality [0.71(0.64, 0.78)], and 18% lower risk of respiratory disease mortality [0.82(0.72, 0.93)]. In substitution analyses, replacing 10g/d of margarine, butter, mayonnaise, and dairy fat with the equivalent amount of olive oil was associated with 8-34% lower risk of total and cause-specific mortality. No significant associations were observed when olive oil was compared with other vegetable oils combined.
Conclusions:
Higher olive oil intake was associated with lower risk of total and cause-specific mortality. Replacing margarine, butter, mayonnaise, and dairy fat with olive oil was associated with lower risk of mortality.
Keywords: Olive oil, plant oils, total mortality, cause-specific mortality, nutrition
CONDENSED ABSTRACT:
Findings from two cohort studies, including 60,582 women from the Nurses’ Health Study and 31,801 men from the Health Professional’s Follow-up Study (1990-2018), and 36,856 total deaths, showed that higher olive oil intake (>7g/d) was associated with 19% lower cardiovascular disease mortality risk, 17% lower cancer mortality risk, 29% lower neurodegenerative disease mortality risk, and 18% lower respiratory disease mortality risk, compared to those who never consumed olive oil. In substitution analyses, replacing 10g/d of margarine, butter, mayonnaise, and dairy fat with the equivalent amount of olive oil was associated with 8-34% lower risk of total and cause-specific mortality.
INTRODUCTION
Olive oil has been traditionally used as the main culinary and dressing fat in Mediterranean countries and is a key component of the Mediterranean diet. Well-known for its health benefits, it has become more popular worldwide in recent decades. Olive oil is high in monounsaturated fatty acids (MUFA), especially oleic acid, and other minor components including vitamin E and polyphenols, contributing to its anti-inflammatory and antioxidant properties(1).
In epidemiological studies, the consumption of olive oil has been associated with lower risk of cardiovascular disease (CVD). In the Nurses’ Health Study (NHS) and the Health Professionals Follow-up Study (HPFS), we have previously reported that greater olive oil consumption was associated with lower risk of CVD(2). These findings were consistent with results from the PREDIMED trial showing that compared to a control diet, participants allocated to a Mediterranean diet supplemented with a free provision of extra-virgin olive oil reduced the risk of a composite of CVD events by 31%(3). In a secondary analysis of the PREDIMED trial, baseline intake of olive oil was associated with lower risk of cardiovascular mortality(4). Other studies conducted in Mediterranean and European countries have also suggested that greater olive oil consumption is associated with lower risk of all-cause and cardiovascular mortality(5-7). However, to date, no large prospective studies have examined the association between total olive oil consumption and total and cause-specific mortality in the U.S. population, where the average consumption of olive oil is considerably lower than that in Mediterranean countries (Central Illustration). Therefore, we examined the association between total consumption of olive oil and total and cause-specific mortality in two large cohorts of U.S. men and women. In addition, we used statistical substitution models to estimate the risk of total and cause-specific mortality when margarine, butter, mayonnaise, dairy fat, and vegetable oils were replaced by an equivalent amount of olive oil.
Central Illustration: Potential mechanisms for olive oil intake and mortality.
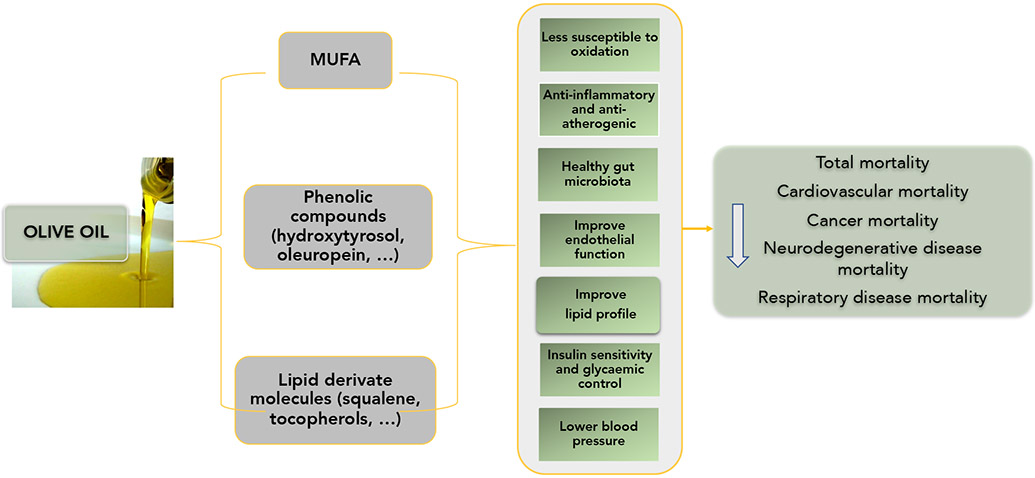
Olive oil is high in bioactive compounds and has been associated with lower risk of total and cause-specific mortality in 2 prospective cohorts including 92,383 U.S. men and women followed for up to 28 years. Potential mechanisms of these associations include olive oil being less susceptible to oxidation, having anti-inflammatory and anti-atherogenic properties, improving oxidative stress, endothelial function, lipid profile, insulin sensitivity and blood pressure.
METHODS
Study population
The analysis was conducted in two ongoing prospective cohort studies. The NHS was initiated in 1976 and included 121,701 women aged 30 to 55. The HPFS began in 1986, with 51,525 men aged 40 to 75 years. Both cohorts have been described previously(8, 9). In both cohorts, mailed questionnaires were administered biennially to assess lifestyle factors and health status, with a follow-up rate exceeding 90% for each 2-year cycle. The baseline for analysis for both cohorts was 1990, when olive oil consumption was first included as part of the food frequency questionnaires (FFQ). We excluded participants with a history of cardiovascular disease (CVD) or cancer at baseline, those with missing data (at baseline or during follow-up repeated assessments) for the consumption of olive oil, or who reported implausible intakes of total energy (<500 or >3500 kcal/d for women and <800 or >4200 kcal/d for men). After exclusions, a total of 60,582 women and 31,801 men remained for the analysis. The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, and those of participating registries as required.
Dietary assessment
Dietary intake was measured using a validated semiquantitative FFQ with over 130 items, repeatedly administered every 4 years. The reproducibility and validity of these FFQs have been described in previous reports(10). Participants were asked how often, on average, they had consumed specific foods, as well as types of fats, oils, and brand or type of oils used for cooking and added at the table in the preceding year. Total olive oil intake was calculated from the sum of three items in the questionnaire pertaining to questions related to the consumption of olive oil: olive oil use for salad dressings, olive oil added to food or bread, and olive oil used for baking and frying at home. One tablespoon was considered to be equivalent to 13.5 g of olive oil. The consumed amount of other vegetable oils (e.g., corn, safflower, soybean, canola) was calculated based on the participant's reported oil brand and type of fat used for cooking at home, including frying, sautéing, baking, and salad dressing. Data about homemade baked items and frying fats used at home were also incorporated. Total margarine was calculated based on the reported frequency of stick, tub, or soft margarine consumption and the amount of margarine added from baking and frying at home. The consumption of butter was calculated in the same manner. Intakes of dairy and other fats and nutrients were calculated based on the USDA and Harvard University Food Composition Database(11) and our biochemical analyses. Supplemental Table 1 shows the nutritional composition of olive oil and other types of fat.
Ascertainment of Death
Deaths were identified from state vital statistics records and the National Death Index or by reports from next of kin or the postal authorities. The follow-up for mortality in these cohorts is over 98% complete using these methods. Cause of death was determined by physician review of medical records, medical reports, autopsy reports, or death certificates. We used the International Classification of Diseases, Eighth Revision (ICD-8) in NHS and ICD-9 in HPFS, which were the ICD systems used at the time the cohorts began. Deaths were grouped into five major groups (CVD, cancer, neurodegenerative disease, respiratory disease, and all other causes, including suicide, injury, infections, diabetes, kidney disease, etc.) (Supplemental Table 2).
Assessment of covariates
Every 2 years, participants returned a mailed questionnaire that provided updated information on body weight, smoking status, physical activity, aspirin and other medications, multivitamin use, menopausal status and postmenopausal hormone use in women, and physician diagnoses of chronic diseases, including hypertension, hypercholesterolemia, and type 2 diabetes mellitus. Body mass index was calculated as weight in kilograms divided by the square of the height in meters. A modified Alternate Healthy Eating Index (AHEI) score, without the polyunsaturated fatty acids and the alcohol components, was used as an indicator of overall diet quality. This score was calculated based on 11 foods and nutrients that are predictive of chronic disease risk including fruit, vegetables, nuts and legumes, red and processed meat, whole grains, sodium, trans fat, and long chain omega-3(12). A higher score denotes greater adherence to the AHEI and better diet quality.
Statistical Analysis
Age-stratified Cox proportional hazards models were used to assess the associations between olive oil consumption and total and cause-specific mortality, separately for each cohort. Person time was calculated for each participant from baseline until the end of follow-up (June 30, 2018, for the NHS and January 31, 2018, for the HPFS) or death, whichever occurred first. We stopped updating dietary variables upon a report of cancer or CVD because changes in diet after the development of these conditions may confound the associations. Since most recent diet can have a stronger impact on mortality, we calculated the average of olive oil intake using the two most recent food frequency questionnaires (the average of 1990 and 1994 diets to predict death from 1994 to 1998, the average of 1994 and 1998 diets to predict death from 1998 to 2002, etc) using time-updated consumption. The cumulative average of olive oil from all available FFQs was used in a secondary analysis.
Olive oil consumption was categorized by frequency: never or <1 per month (reference), >0 to ≤4.5 grams/day (>0 to ≤1 teaspoon), >4.5 to ≤ 7 g/d (>1 teaspoon to ≤1/2 tablespoon), and >7 g/d (>1/2 tablespoon), and linear trends were evaluated using the Wald test on a continuous variable representing median intakes of each category. Multivariable Cox proportional hazards regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for total and cause-specific mortality according to olive oil intake categories. Model 1 adjusted for age and calendar time. Multivariable model 2 was further adjusted for ethnicity, Southern European/Mediterranean ancestry, marital status, living alone, smoking status, alcohol intake, physical activity, family history of diabetes, family history of myocardial infarction or cancer, personal history of hypertension or hypercholesterolemia, multivitamin use, aspirin use, in women postmenopausal status and menopausal hormone use, total energy intake, and body mass index. The categories for covariates are provided in the table footnotes. Model 3 was additionally adjusted for intake of red meat, fruits and vegetables, nuts, soda, whole grains (in quintiles), and trans fat.
Stratified analysis and potential interactions with several pre-specified subgroups including age (< or ≥ 65 years), BMI (<25, 25-30, or > 30 kg/m2), physical activity (above or below the median), family history of myocardial infarction, ancestry, baseline hypercholesterolemia, baseline hypertension, personal history of diabetes, and above or below the median of AHEI, total vegetable intake, green vegetable intake, lettuce intake, total meat (including red meat, processed meat, and poultry), and arachidonic acid were evaluated using the Wald test on cross-product terms based on olive oil intake (continuous variable) and the stratification variables.
We estimated the risk of total and cause-specific mortality in substitution analyses when replacing 10 g/d of other types of fats [margarine, butter, mayonnaise, other vegetable oils combined (corn, safflower, soybean, and canola), and dairy fat] with olive oil by including both continuous variables in the multivariable models and mutually adjusting for other types of fat. The difference in the coefficients from this multivariate model were used to estimate the hazard ratios and 95% CI for substituting 10 g/d of olive oil for the same amount of other fats.
Sensitivity analyses were conducted to test the robustness of the results. First, to account for potential confounding by socioeconomic status, the models were adjusted for census-tract median family income, median home value, and percentage with college degree. Second, to test whether the results were affected by selectively stopping updating diet, diet was continuously updated until the end of follow-up. Third, the models were adjusted for modified AHEI (without polyunsaturated fatty acids and alcohol components). Fourth, instead of using the average of the two most recent FFQ, the cumulative average of olive oil throughout follow-up was used. Fourth, the models were mutually adjusted for other types of fats. Fifth, the models were further adjusted for personal history of diabetes. Sixth, we conducted a sensitivity analysis excluding BMI from the models as BMI could be in the causal pathway. Seventh, we conducted a separate analysis for dementia-related death as the endpoint. Finally, we applied a competing risk regression model for cause-specific mortality by including olive oil as exposure and other risk factors as unconstrained covariates, allowing the effects of the covariates vary across cause-specific mortality(13).
Pooled HRs were obtained by combining data from both cohorts and stratifying by cohort (sex) and time period to increase statistical power and obtain summary estimates. Analyses were performed with the SAS statistical package (version 9.4, SAS Institute). Statistical tests were 2 sided, and p values of <0.05 were considered statistically significant.
RESULTS
During 28 years of follow-up, we documented 36,856 deaths (22,768 in NHS and 14,076 in HPFS). Mean consumption of olive oil increased from 1.6 g/d in 1990 to about 4 g/d in 2010, whereas margarine consumption decreased from around 12 g/d in 1990 to ~4 g/d in 2010; the intake of other fats remained stable (Supplemental Figure 1). The Spearman correlations between olive oil and other types of fat are presented in Supplemental Table 3. Baseline characteristics of participants according to frequency of olive oil consumption are shown in Table 1. Men and women with higher olive oil consumption tended to be more physically active, more likely to have a Southern European or Mediterranean ancestry, and less likely to smoke. Olive oil consumption was also associated with higher energy intake, a better AHEI score, and a greater consumption of fruits and vegetables as compared to those with lower consumption (Table 1). The mean consumption of total olive oil in the highest category (>0.5 tablespoon/day) was about 9 g/day at baseline, and included 5% of the cohort participants.
Table 1.
Age-standardized characteristics of the study population at 1990 by olive oil consumption
| Never or <1 per month |
>0–≤4.5 g/d (>0 to ≤1 teaspoon) |
>4.5–≤ 7 g/d >1 teaspoon to ≤1/2 TBS) |
>7 g/d (>1/2 TBS) |
|
|---|---|---|---|---|
| Nurses’ Health Study | ||||
| Number of participants | 32,360 | 22,684 | 2,393 | 3,145 |
| Total olive oil (g/d) | 0 (0) | 1.5 (1.2) | 5.8 (0.5) | 9 (4.7) |
| Age | 56.2 (7.2) | 56.1 (7) | 56.3 (7) | 56.5 (7) |
| Ethnicity, white, % | 97.6 | 98.2 | 98.8 | 98.8 |
| Southern European or Mediterranean ancestry, % | 14.7 | 18.9 | 24.5 | 27.6 |
| Family history of diabetes, % | 30.5 | 29.3 | 28.0 | 30.2 |
| Family history of cancer, % | 14.5 | 14.6 | 14.3 | 14.0 |
| Family history of myocardial infarction, % | 19.0 | 19.5 | 19.8 | 19.8 |
| Multivitamin use, % | 36.8 | 38.9 | 39.1 | 37.6 |
| Aspirin use, % | 44.5 | 47.0 | 47.7 | 44.0 |
| Baseline hypocholesterolemia, % | 28.3 | 31.2 | 31.3 | 32.6 |
| Baseline hypertension, % | 18.3 | 18.3 | 17.2 | 17.6 |
| Current menopausal hormone use, % | 28.9 | 30.7 | 31.4 | 30.0 |
| Current smoker, % | 16.3 | 16.6 | 15.5 | 12.8 |
| Former smoker % | 35.8 | 41.7 | 46.1 | 48.0 |
| BMI, kg/m2 | 25.8 (5) | 25.4 (4.7) | 25.3 (4.5) | 25.3 (4.6) |
| Alcohol intake, g/d | 4.1 (8.6) | 6 (10.1) | 7.3 (11) | 7.2 (10.9) |
| Physical activity, MET-h/wk | 14.4 (19.8) | 16.5 (22.9) | 18.3 (23.2) | 18.8 (25.9) |
| Total calories, kcal/d | 1702 (497) | 1762 (501) | 1907 (512) | 1989 (531) |
| Red and processed meat (servings/d) | 0.9 (0.6) | 0.9 (0.6) | 0.8 (0.6) | 0.8 (0.6) |
| Fruits and vegetables (servings/d) | 4.8 (1.9) | 5.3 (2) | 6 (2.1) | 6.4 (2.2) |
| Total nuts (servings/d) | 0.1 (0.2) | 0.1 (0.2) | 0.2 (0.2) | 0.2 (0.2) |
| Whole grains (servings/d) | 1.8 (1.5) | 1.9 (1.6) | 2.2 (1.7) | 2.3 (1.8) |
| Soda (servings/d) | 0.8 (0.9) | 0.8 (0.9) | 0.7 (0.8) | 0.8 (0.9) |
| AHEI score | 41.7 (10.3) | 44.3 (10.2) | 46.5 (10.2) | 47.3 (10.2) |
| Health Professional’s Follow-up Study | ||||
| Number of participants | 16,075 | 12,855 | 1,246 | 1,625 |
| Total olive oil (g/d) | 0 (0) | 1.5 (1.1) | 5.8 (0.5) | 9.1 (4.5) |
| Age | 56.8 (9.5) | 56.8 (9.4) | 56.9 (9.4) | 56.9 (9.3) |
| Ethnicity, white, % | 95.4 | 95.7 | 95.2 | 97.0 |
| Southern European or Mediterranean ancestry, % | 20.6 | 23.8 | 31.6 | 37.9 |
| Family history of diabetes, % | 21.1 | 22.1 | 20.6 | 22.9 |
| Family history of cancer, % | 38.0 | 37.3 | 38.6 | 36.9 |
| Family history of myocardial infarction, % | 31.9 | 32.0 | 35.4 | 33.3 |
| Multivitamin use, % | 37.3 | 39.5 | 41.7 | 42.8 |
| Aspirin use, % | 29.8 | 30.0 | 27.5 | 29.8 |
| Baseline hypocholesterolemia, % | 19.8 | 21.2 | 22.0 | 23.8 |
| Baseline hypertension, % | 21.1 | 21.3 | 19.8 | 20.2 |
| Current smoker, % | 8.2 | 7.3 | 7.4 | 5.3 |
| Former smoker % | 40.2 | 43.4 | 46.9 | 48.6 |
| BMI, kg/m2 | 25.6 (3.4) | 25.5 (3.2) | 25.5 (3.1) | 25.4 (3.2) |
| Alcohol intake (g/d) | 8.9 (13.8) | 11.2 (14.6) | 12.8 (15) | 13.3 (15) |
| Physical activity (MET-h/wk) | 36.6 (42.7) | 37.8 (39.5) | 40.3 (37.4) | 43.6 (45.4) |
| Total calories | 1897 (577) | 1927 (582) | 2063(604) | 2134 (605) |
| Red and processed meat (servings/d) | 1.1 (0.8) | 1 (0.8) | 1 (0.8) | 0.8 (0.7) |
| Fruits and vegetables (servings/d) | 5.2 (2.4) | 5.7 (2.4) | 6.6 (2.7) | 7.2 (2.9) |
| Total nuts (servings/d) | 0.2 (0.3) | 0.3 (0.3) | 0.3 (0.4) | 0.3 (0.5) |
| Whole grains (servings/d) | 1.0 (0.9) | 1.0 (0.9) | 1.1 (0.9) | 1.2 (1.1) |
| Soda (servings/d) | 0.8 (0.9) | 0.7 (0.9) | 0.7 (0.9) | 0.7 (0.9) |
| AHEI | 41.1 (10.9) | 44.3 (10.5) | 47.2 (10.7) | 48.7 (10.7) |
Abbreviations: AHEI, Alternative Healthy Eating Index (without the alcohol and polyunsaturated components, scored as 0-90, with higher scores representing healthier diets); BMI, body mass index; MET, metabolic equivalent task; TBS, tablespoon. Values are presented as mean (SD) or percentage, standardized to the age distribution of the study population.
Age-adjusted and multivariable-adjusted models showed a consistent, significant, inverse association between olive oil intake and total and cause-specific mortality (Table 2). After adjusting for demographic and lifestyle factors, the pooled multivariable-adjusted HR (95% CI) for participants in the highest category of olive oil consumption, as compared with those in the lowest category, were 0.81 (0.78, 0.84) for total mortality, 0.81 (0.75, 0.87) for cardiovascular mortality, 0.83 (0.78, 0.89) for cancer mortality, 0.71 (0.64, 0.78) for neurodegenerative mortality, and 0.82 (0.72, 0.93) for respiratory mortality. Significant inverse associations for total mortality and cause-specific mortality were also observed for each 5 additional grams increase in olive oil intake as a continuous variable. Olive oil consumption was also inversely associated with other causes of death (Supplemental Table 4).
Table 2.
Hazard Ratios (95% CI) of total and cause-specific mortality according to categories of total olive oil intake
| Categories of olive oil intake | |||||||
|---|---|---|---|---|---|---|---|
| Never or <1 per month |
>0–≤4.5 g/d (>0 to ≤1 teaspoon) |
>4.5–≤ 7 g/d >1 teaspoon to ≤1/2 |
>7 g/d (>1/2 |
P for trend | HR (95% CI) for 5 g increase in olive oil |
||
| TOTAL MORTALITY | |||||||
| NHS | Mean total olive oil (g/d) | 0 | 1.6 (± 1.1) | 5.8 (±0.7) | 14.0 (± 8.8) | ||
| N° cases/ Person-years | 10158/527,372 | 8266/603,179 | 1570/117,489 | 2774/238,877 | |||
| Age-adjusted model 1 | 1 (Ref.) | 0.73 (0.71, 0.75) | 0.71 (0.67, 0.75) | 0.62 (0.59, 0.65) | <0.001 | 0.90 (0.89, 0.91) | |
| Multivariable model 2 | 1 (Ref.) | 0.86 (0.84, 0.89) | 0.85 (0.81, 0.90) | 0.79 (0.75, 0.82) | <0.001 | 0.95 (0.94, 0.96) | |
| Multivariable model 3 | 1 (Ref.) | 0.87 (0.84, 0.89) | 0.86 (0.81, 0.91) | 0.79 (0.75, 0.82) | <0.001 | 0.95 (0.94, 0.96) | |
| HPFS | Mean total olive oil (g/d) | 0 | 1.6 (±1.1) | 5.7 (±0.7) | 13.7 (±8.5) | ||
| N° cases/ Person-years | 6359/271540 | 5065/308471 | 998/57641 | 1654/102670 | |||
| Age-adjusted model 1 | 1 (Ref.) | 0.77 (0.75, 0.80) | 0.75 (0.70, 0.80) | 0.68 (0.64, 0.71) | <0.0001 | 0.91 (0.90, 0.93) | |
| Multivariable model 2 | 1 (Ref.) | 0.91 (0.87, 0.94) | 0.88 (0.82, 0.94) | 0.84 (0.80, 0.89) | <0.0001 | 0.96 (0.95, 0.98) | |
| Multivariable model 3 | 1 (Ref.) | 0.92 (0.88, 0.95) | 0.89 (0.83, 0.95) | 0.86 (0.81, 0.91) | <0.0001 | 0.97 (0.95, 0.98) | |
| Pooled model 3 | 1 (Ref.) | 0.88 (0.86, 0.90) | 0.86 (0.82, 0.90) | 0.81 (0.78, 0.84) | <0.001 | 0.96 (0.95, 0.97) | |
| CARDIOVASCULAR DISEASE MORTALITY | |||||||
| NHS | N° cases/ P-years | 2263/527,372 | 1655/603,179 | 266/117,489 | 553/238,877 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.70 (0.66, 0.75) | 0.60 (0.53, 0.69) | 0.64 (0.59, 0.71) | <0.001 | 0.91 (0.89, 0.94) | |
| Multivariable model 2 | 1 (Ref.) | 0.82 (0.76, 0.87) | 0.73 (0.64, 0.83) | 0.84 (0.77, 0.93) | 0.002 | 0.98 (0.95, 1.01) | |
| Multivariable model 3 | 1 (Ref.) | 0.83 (0.77, 0.88) | 0.74 (0.65, 0.84) | 0.85 (0.77, 0.94) | 0.006 | 0.98 (0.95, 1.01) | |
| HPFS | N° cases/ Person-years | 1993/275615 | 1383/311810 | 269/58305 | 439/103761 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.73 (0.68, 0.78) | 0.71 (0.63, 0.81) | 0.65 (0.59, 0.72) | <0.0051 | 0.92 (0.89, 0.95) | |
| Multivariable model 2 | 1 (Ref.) | 0.84 (0.78, 0.90) | 0.82 (0.72, 0.94) | 0.81 (0.72, 0.90) | 0.0005 | 0.97 (0.94, 1.00) | |
| Multivariable model 3 | 1 (Ref.) | 0.84 (0.78, 0.90) | 0.81 (0.71, 0.93) | 0.79 (0.71, 0.88) | 0.0002 | 0.97 (0.94, 1.00) | |
| Pooled model 3 | 1 (Ref.) | 0.82 (0.78, 0.86) | 0.77 (0.70, 0.84) | 0.81 (0.75, 0.87) | <.0001 | 0.97 (0.95, 0.99) | |
| CANCER MORTALITY | |||||||
| NHS | N° cases/ P-years | 2431/527,372 | 2033/603,179 | 450/117,489 | 794/238,877 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.77 (0.73, 0.82) | 0.88 (0.79, 0.97) | 0.75 (0.69, 0.81) | <0.001 | 0.95 (0.93, 0.98) | |
| Multivariable model 2 | 1 (Ref.) | 0.84 (0.79, 0.89) | 0.96 (0.87, 1.07) | 0.84 (0.77, 0.91) | 0.02 | 0.98 (0.95, 1.00) | |
| Multivariable model 3 | 1 (Ref.) | 0.85 (0.80, 0.90) | 0.98 (0.88, 1.09) | 0.86 (0.78, 0.93) | 0.09 | 0.98 (0.96, 1.01) | |
| HPFS | N° cases/ P-years | 1290/229084 | 1880/387235 | 258/59343 | 336/74094 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.80 (0.75, 0.86) | 0.82 (0.72, 0.93) | 0.72 (0.64, 0.80) | <0.0001 | 0.92 (0.89, 0.95) | |
| Multivariable model 2 | 1 (Ref.) | 0.88 (0.82, 0.94) | 0.90 (0.79, 1.03) | 0.81 (0.72, 0.90) | 0.002 | 0.95 (0.91, 0.98) | |
| Multivariable model 3 | 1 (Ref.) | 0.89 (0.82, 0.95) | 0.92 (0.81, 1.05) | 0.83 (0.74, 0.93) | 0.01 | 0.95 (0.92, 0.99) | |
| Pooled model 3 | 1 (Ref.) | 0.86 (0.82, 0.90) | 0.94 (0.87, 1.02) | 0.83 (0.78, 0.89) | 0.001 | 0.97 (0.95, 0.99) | |
| NEURODEGENERATIVE DISEASE MORTALITY | |||||||
| NHS | N° cases/ P-years | 1901/527,372 | 1315/603,179 | 267/117,489 | 399/238,877 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.63 (0.58, 0.67) | 0.67 (0.59, 0.76) | 0.51 (0.45, 0.56) | <.0001 | 0.86 (0.83, 0.89) | |
| Multivariable model 2 | 1 (Ref.) | 0.84 (0.78, 0.90) | 0.89 (0.78, 1.01) | 0.69 (0.62, 0.77) | <.0001 | 0.92 (0.89, 0.95) | |
| Multivariable model 3 | 1 (Ref.) | 0.82 (0.76, 0.88) | 0.85 (0.74, 0.97) | 0.66 (0.59, 0.74) | <.0001 | 0.90 (0.87, 0.94) | |
| HPFS | N° cases/ P-years | 834/275027 | 653/310992 | 127/58189 | 196/103519 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.77 (0.69, 0.85) | 0.71 (0.59, 0.85) | 0.59 (0.50, 0.69) | <.00001 | 0.87 (0.82, 0.91) | |
| Multivariable model 2 | 1 (Ref.) | 1.02 (0.92, 1.14) | 0.94 (0.78, 1.14) | 0.88 (0.75, 1.03) | 0.07 | 0.95 (0.91, 1.00) | |
| Multivariable model 3 | 1 (Ref.) | 1.03 (0.93, 1.15) | 0.95 (0.79, 1.15) | 0.89 (0.75, 1.05) | 0.11 | 0.96 (0.92, 1.01) | |
| Pooled model 3 | 1 (Ref.) | 0.88 (0.83, 0.94) | 0.88 (0.78, 0.98) | 0.71 (0.64, 0.78) | <.0001 | 0.92 (0.89, 0.94) | |
| RESPIRATORY DISEASE MORTALITY | |||||||
| NHS | N° cases/ P-years | 867/527,372 | 713/603,179 | 121/117,48 | 204/238,877 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.77 (0.70, 0.86) | 90.69 (0.57, 0.84) | 0.59 (0.50, 0.68) | <.0001 | 0.86 (0.82, 0.91) | |
| Multivariable model 2 | 1 (Ref.) | 0.90 (0.81,0.99) | 0.80 (0.66, 0.97) | 0.73 (0.62, 0.85) | 0.0001 | 0.91 (0.87, 0.96) | |
| Multivariable model 3 | 1 (Ref.) | 0.95 (0.86, 1.05) | 0.88 (0.72, 1.07) | 0.80 (0.68, 0.95) | 0.008 | 0.94 (0.89, 0.98) | |
| HPFS | N° cases/ P-years | 487/276475 | 386/312247 | 73/58426 | 118/103937 | ||
| Age-adjusted model 1 | 1 (Ref.) | 0.82 (0.72, 0.94) | 0.76 (0.59, 0.98) | 0.70 (0.57, 0.85) | 0.001 | 0.91 (0.85, 0.97) | |
| Multivariable model 2 | 1 (Ref.) | 0.95 (0.83, 1.09) | 0.87 (0.68, 1.12) | 0.83 (0.67, 1.02) | 0.07 | 0.95 (0.89, 1.01) | |
| Multivariable model 3 | 1 (Ref.) | 0.97 (0.85, 1.12) | 0.90 (0.70, 1.16) | 0.88 (0.71, 1.09) | 0.21 | 0.97 (0.91, 1.03) | |
| Pooled model 3 | 1 (Ref.) | 0.95 (0.87, 1.03) | 0.88 (0.75, 1.03) | 0.82 (0.72, 0.93) | 0.002 | 0.94 (0.91, 0.98) | |
Results are expressed as Hazard Ratios (HR) and 95% Confidence Intervals (95% CI). Abbreviations: NHS, Nurses’ Health Study, HPFS, Health Professionals Follow-up Study. Model 2 was adjusted for age (years), ethnicity (white, non-white), Southern European/Mediterranean ancestry (yes, no), married (yes/no), living alone (yes/no), smoking status (never, former, current smoker 1-14 cigarettes per day, 15-24 cigarettes per day, or ≥ 25 cigarettes per day), alcohol intake (0, 0.1-4.9,5.0-9.9,10.0-14.9, and ≥ 15.0 g/d), physical activity (<3.0,3.0-8.9,9.0-17.9,18.0-26.9,≥27.00 metabolic equivalent task-h/week), family history of diabetes (yes/no), family history of myocardial infarction (yes/no), family history of cancer (yes/no), multivitamin use (yes/no), aspirin use (yes/no), history of hypertension (yes/no), history of hypercholesterolemia (yes/no), in women postmenopausal status and menopausal hormone use [premenopausal, postmenopausal (no, past, or current hormone use), total energy intake (kilocalories per day) and body mass index (calculated as weight in kilograms divides by height in meters squared). Model 3 was additionally adjusted for red meat, fruits and vegetables, nuts, soda, whole grains intake (in quintiles), and trans fat. Results were pooled using a pooled dataset and stratifying by cohort (sex) and time period.
Although participants were similar in education and occupation, in sensitivity analyses we adjusted for census-tract neighborhood median family income, home value, and percentage with college degree to control further for the potential confounding effects of socioeconomic status. However, these additional adjustments did not materially change the results (pooled HR for total mortality for high vs. low olive oil intake was 0.81 (0.78, 0.84) Supplemental Table 5). In addition, consistent results were observed when we continuously updated the diet regardless of the development of intermediate outcomes (pooled HR for total mortality comparing high vs. low intake: 0.93 (0.89, 0.97), P trend = 0.02). When the models for total olive oil were adjusted for the modified AHEI (excluding polyunsaturated fatty acids and alcohol) instead of adjusting for food groups, the estimates for total and cause-specific mortality were consistent with those in the primary analysis (Supplemental Table 6). Olive oil intake was also inversely associated with the risk of total and cause-specific mortality when we used the cumulative average instead of using the average of the two most recent FFQ (Supplemental Table 7). Similarly, when the models for olive oil were mutually adjusted for other types of fat, the estimates remained largely unchanged (Supplemental Table 8). Results were also consistent when we further adjusted the models for personal history of diabetes (pooled HR for total mortality comparing high vs. low intake: 0.81 (0.78, 0.84), P trend <0.001) and when BMI was excluded from the models (pooled HR for total mortality comparing high vs. low intake: 0.80 (0.78, 0.84), P trend <0.001). The pooled HR for dementia related mortality comparing high vs. low intake of olive oil was 0.73 (0.66, 0.81), P trend <0.001, after adjusting for potential confounders. Finally, when applying a competing risk regression model for cause-specific mortality, the results remained consistent with the primary analysis (Supplemental Table 9).
We found significant inverse associations for olive oil intake and total and cause-specific mortality in most of the pre-specified subgroup analyses (Table 3). Participants reporting Southern European and/or Mediterranean ancestry had higher consumption of olive oil; they had a 6% (HR: 0.94; 95% CI: 0.92, 0.96) lower risk of total mortality, slightly more pronounced than the 4% risk reduction in the non-Mediterranean ancestry subgroups (per each 5g increase in olive oil intake). Similar associations were also observed for participants below or above the median of AHEI.
Table 3.
Subgroup analyses for total and cause-specific mortality risk for 5g/d increase in olive oil intake
| Adjusted HR (95% CI) | |||||
|---|---|---|---|---|---|
| Subgroup | Total mortality | CVD mortality | Cancer mortality | Neurodegenerative mortality |
Respiratory mortality |
| Age | |||||
| Younger (< 65 years) | 0.97 (0.93, 1.01) | 0.90 (0.80, 1.02) | 0.99 (0.94, 1.05) | 0.99 (0.81, 1.22) | 0.85 (0.64, 1.13) |
| Older (≥ 65 years) | 0.89 (0.88, 0.90)* | 0.88 (0.86, 0.90) | 0.92 (0.90, 0.94)* | 0.83 (0.81, 0.86)* | 0.86 (0.83, 0.90)* |
| Body mass index, kg/m2 | |||||
| <25 | 0.95 (0.94, 0.96) | 0.96 (0.93, 0.99) | 0.96 (0.94, 0.99) | 0.92 (0.88, 0.95) | 0.97 (0.92, 1.02) |
| 25-30 | 0.94 (0.92, 0.97) | 0.97 (0.92, 1.01) | 0.97 (0.94, 1.01) | 0.88 (0.82, 0.94) | 0.89 (0.81, 0.98) |
| >30 | 0.95 (0.93, 0.98) | 0.97 (0.92, 1.03) | 0.98 (0.93, 1.03) | 0.88 (0.79, 0.98) | 0.89 (0.79, 1.00) |
| Physical activity | |||||
| Below median (<18.5 MET-h/wk) | 0.95 (0.94, 0.96) | 0.97 (0.95, 0.99) | 0.97 (0.95, 1.00) | 0.92 (0.88, 0.95) | 0.92 (0.88, 0.96) |
| Above median (>=18.5 MET-h/wk) | 0.94 (0.93, 0.96) | 0.97 (0.93, 1.00) | 0.94 (0.91, 0.97) | 0.93 (0.88, 0.97) | 0.90 (0.83, 0.98) |
| Family history of myocardial infarction | |||||
| No | 0.95 (0.94, 0.97) | 0.98 (0.96, 1.00) | 0.97 (0.95, 0.99) | 0.91 (0.88, 0.94) | 0.94 (0.90, 0.98) |
| Yes | 0.95 (0.93, 0.97) | 0.92 (0.88, 0.96)* | 0.98 (0.93, 1.01) | 0.96 (0.91, 1.01)* | 0.95 (0.88, 1.02) |
| Ancestry | |||||
| Southern European/Mediterranean | 0.94 (0.92, 0.96) | 0.96 (0.92, 0.99) | 0.96 (0.93, 0.99) | 0.91 (0.86, 0.95) | 0.95 (0.91, 0.99) |
| Other ancestry | 0.96 (0.94, 0.97) | 0.97 (0.94, 0.99) | 0.97 (0.95, 0.99) | 0.93 (0.90, 0.96) | 0.91 (0.84, 0.99) |
| Baseline hypercholesterolemia | |||||
| No | 0.96 (0.95, 0.97) | 0.98 (0.95, 1.00) | 0.97 (0.94, 0.99) | 0.92 (0.89, 0.95) | 0.95 (0.91, 0.99) |
| Yes | 0.95 (0.93, 0.97) | 0.94 (0.91, 0.98) | 0.98 (0.94, 1.02) | 0.94 (0.89, 0.98) | 0.92 (0.85, 0.99) |
| Baseline hypertension | |||||
| No | 0.96 (0.95, 0.97) | 0.98 (0.96, 1.01) | 0.97 (0.95, 0.99) | 0.92 (0.89, 0.95) | 0.94 (0.89, 0.98) |
| Yes | 0.96 (0.94, 0.98) | 0.94 (0.90, 0.98) | 0.98 (0.94, 1.02) | 0.93 (0.88, 0.98) | 0.96 (0.89, 1.03) |
| Personal history of diabetes | |||||
| No | 0.95 (0.94, 0.96) | 0.97 (0.95, 1.00) | 0.97 (0.95, 0.99) | 0.91 (0.88, 0.94) | 0.95 (0.92, 0.99) |
| Yes | 0.95 (0.93, 0.97) | 0.94 (0.90, 0.99) | 0.98 (0.93, 1.03) | 0.92 (0.86, 0.99) | 0.88 (0.78, 0.98) |
| AHEI | |||||
| Below median (<44 points) | 0.95 (0.94, 0.96) | 0.95 (0.91, 0.98) | 0.98 (0.95, 1.01) | 0.91 (0.86, 0.95) | 0.92 (0.87, 0.98) |
| Above median (>=44 points) | 0.97 (0.95, 0.98) | 0.98 (0.96, 1.00)* | 0.97 (0.94, 0.99) | 0.93 (0.90, 0.96) | 0.96 (0.91, 1.00) |
| Total vegetable intake | |||||
| Below median (<5 servings/d) | 0.94 (0.92, 0.95) | 0.91 (0.87, 0.96) | 1.01 (0.98, 1.04) | 0.89 (0.85, 0.94) | 0.89 (0.83, 0.95) |
| Above median (>=5 servings/d) | 0.96 (0.95, 0.97) | 0.99 (0.97, 1.02)* | 0.98 (0.96, 1.00) | 0.94 (0.91, 0.97) | 0.97 (0.93, 1.02)* |
| Green vegetable intake | |||||
| Below median (<1.4 servings/d) | 0.95 (0.93, 0.96) | 0.94 (0.91, 0.97) | 0.98 (0.95, 1.01) | 0.93 (0.90, 0.97) | 0.90 (0.85, 0.96) |
| Above median (>=1.4 servings/d) | 0.96 (0.95, 0.98) | 0.99 (0.97, 1.03)* | 0.96 (0.94, 0.99) | 0.91 (0.87, 0.95)* | 0.98 (0.93, 1.03)* |
| Lettuce intake | |||||
| Below median (<0.6 servings/d) | 0.95 (0.94, 0.96) | 0.95 (0.92, 0.98) | 0.97 (0.95, 1.00) | 0.92 (0.89, 0.96) | 0.93 (0.88, 0.98) |
| Above median (>=0.6 servings/d) | 0.96 (0.95, 0.98) | 0.99 (0.97, 1.03) | 0.97 (0.94, 0.99) | 0.92 (0.88, 0.96) | 0.96 (0.91, 1.01) |
| Total meat intake | |||||
| Below median (<1.3 servings/d) | 0.96 (0.94, 0.97) | 0.98 (0.95, 1.00) | 0.96 (0.94, 0.99) | 0.93 (0.90, 0.96) | 0.96 (0.92, 0.99) |
| Above median (>=1.3 servings/d) | 0.95 (0.94, 0.97) | 0.97 (0.94, 1.00) | 0.97 (0.94, 1.00) | 0.91 (0.86, 0.95) | 0.97 (0.93, 1.00) |
| Arachidonic acid | |||||
| Below median (<0.11 g/d) | 0.98 (0.96, 1.00) | 0.97 (0.93, 1.02) | 0.99 (0.95, 1.03) | 0.97 (0.93, 1.04) | 0.86 (0.78, 0.95) |
| Above median. (>0.11 g/d) | 0.96 (0.94, 0.97) | 0.97 (0.95, 1.00) | 0.97 (0.94, 0.99) | 0.90 (0.83, 0.97) | 0.97 (0.93, 1.00) |
Results are expressed as hazard ratios (HR) and 95% confidence intervals (95% CI). HRs for 5g increase in olive oil intake in each subgroup category. Abbreviations: AHEI, Alternative Healthy Eating Index Score; HPFS, Health Professionals- Follow-up Study; NHS, Nurses‘ Health Study, HPFS, Health Professionals Follow-up Study. Multivariable model was adjusted for age, ethnicity (white, non-white), Southern European/Mediterranean ancestry, married (yes/no), living alone (yes/no), smoking status (never, former, current smoker 1-14 cigarettes per day, 15-24 cigarettes per day, or ≥ 25 cigarettes per day), alcohol intake (0, 0.1-4.9,5.0-9.9,10.0-14.9, and ≥ 15.0 g/d), physical activity (<3.0,3.0-8.9,9.0-17.9,18.0-26.9,≥27.00 metabolic equivalent task-h/week), family history of diabetes, family history of myocardial infarction, family history of cancer, history of hypertension (yes/no), history of hypercholesterolemia (yes/no), multivitamin use, aspirin use, in women postmenopausal status and menopausal hormone use, total energy intake, BMI, red meat, fruits and vegetables, nuts, soda, whole grains intake (in quintiles), and trans fat.
Significant interaction
We estimated that replacing 10 g/d of margarine with 10 g/d of olive oil was associated with 13% lower risk of total mortality (HR) in multivariable-adjusted models [0.87 (95% CI: 0.85, 0.89)]. The respective HR estimate for butter was 0.86 (95% CI: 0.83, 0.88), for mayonnaise 0.81 (95% CI: 0.78, 0.84), and for dairy fat 0.87 (95% CI: 0.84, 0.89). These results were consistent for other causes of death including CVD, cancer, neurodegenerative disease, and respiratory disease mortality (Figure 1). HR and 95% CIs for all the comparisons are reported in Supplemental Table 10. Substituting olive oil for other vegetable oils was not significantly associated with total or cause-specific mortality.
Figure 1: Mortality associated with olive oil substituted for other fats.
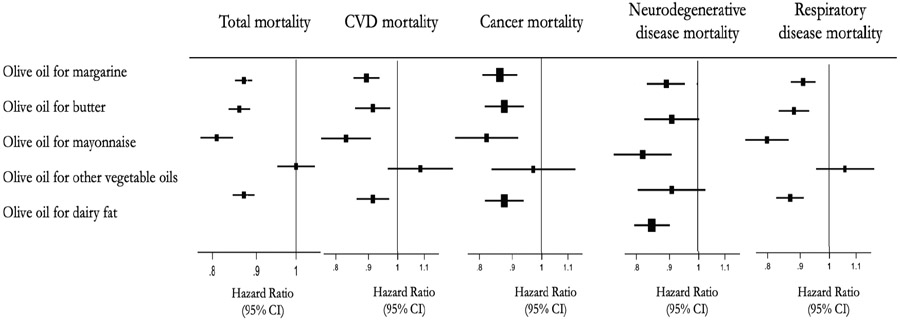
HR(95% CI) for mortality substituting 10g of olive oil for equivalent amount of other fats. Abbreviations: NHS, Nurses’ Health Study, HPFS, Health Professionals Follow-up Study. Model was adjusted for age, ethnicity, ancestry, married, living alone, smoking status, alcohol intake, physical, family history of diabetes, myocardial infarction or cancer, multivitamin use, aspirin use, in women postmenopausal status and menopausal hormone use, energy intake, BMI, red meat, fruits and vegetables, nuts, soda, whole grains, and the intake of trans fat, and mutually adjusted for the intake of other types of fat. Results were pooled using a pooled dataset and stratifying by cohort and time period.
DISCUSSION
In these two large prospective cohorts of US men and women, we found an inverse association between olive oil consumption and risk of total and cause-specific mortality after adjusting for lifestyle factors and for potential dietary confounders. As compared with those who never or rarely consume olive oil, those in the highest category of olive oil consumption (> 7 g/d) had 19% lower risk of total and CVD mortality, 17% lower risk of cancer mortality, 29% lower risk of neurodegenerative mortality, and 18% lower risk of respiratory mortality. Substituting 10 g/d of other fats, including margarine, butter, mayonnaise, and dairy fat, with olive oil was associated with reductions in the risk of total and cause-specific mortality. However, in general, no significant associations with total and cause-specific mortality were observed when other vegetable oils combined were substituted with olive oil. Overall, our data support current dietary recommendations to replace animal fats with unsaturated plant oils such as olive oil.
An inverse associations between olive oil consumption and risk of CVD has been well established in large prospective cohort studies and large clinical trials, especially in Mediterranean and European countries(2, 3, 14). However, large prospective cohort studies evaluating whether olive oil intake impacts total and cause-specific mortality were lacking. An Italian study of patients with a prior myocardial infarction, showed a 24% (HR: 0.76; 95% CI: 0.64, 0.91) lower risk of overall mortality for those consuming olive oil regularly compared to those who never consumed olive oil(5). The EPIC-Spanish cohort reported a 26% (HR: 0.74; 95% CI: 0.64, 0.87) reduction in the risk of overall mortality for those in the highest quartile of total olive oil intake compared to the lowest quartile(6). The Three City Study in France, including 8,973 participants, found that olive oil use was associated with lower risk of all-cause mortality in women but not men(7). In contrast, no associations were found between olive oil intake and all-cause mortality in a free living Greek population(15) and in an ancillary analysis of the PREDIMED trial(16). Our study, with longer follow-up, a larger sample size, and repeated measurements of diet, showed that olive oil consumption was associated with lower risk of overall mortality in both men and women. Of note, our study showed that benefits of olive oil can be observed even when consumed in lower average amounts than in Mediterranean countries. The mean consumption of olive oil in our U.S. population was 10 g/d, whereas in Mediterranean populations, such as the Spanish participants of the PREDIMED Study, the mean intake at baseline was 40 g/d(4).
Olive oil consumption may lower mortality risk in part through improving cardiometabolic risk factors(17). In line with previous observational studies conducted in Mediterranean and European countries, we observed that greater olive oil consumption was associated with 19% lower risk of CVD mortality in U.S men and women. In the PREDIMED trial, baseline total olive oil intake was inversely associated with CVD mortality: each 10 g/d increase in total olive oil consumption was associated with a 16% reduction in cardiovascular mortality(4). These results were supported by the findings of the EPIC-Spanish cohort, where a 44% reduction in CVD mortality was found in participants at the top quartile of total olive oil consumption as compared to those in the bottom quartile(6).
While previous prospective studies have found inverse associations between olive oil intake and CVD mortality, no significant associations with the risk of cancer mortality were observed. This may be due to the relatively small number of cancer deaths in these studies. With 9,537 cancer deaths, we found that the consumption of more than a half tablespoon per day of olive oil was associated with 16% lower risk of cancer mortality, compared to no olive oil. These associations were stronger in men than in women. Supporting our findings, a review of epidemiological studies suggested that olive oil can decrease the risk of upper digestive, respiratory, and breast cancer, and perhaps other sites(18). The PREDIMED trial showed that an intervention with Mediterranean diet supplemented with extra virgin olive oil substantially reduced the risk of breast cancer(19).
We also observed lower risk of neurodegenerative and respiratory disease mortality. Few prior studies have reported on these associations, however, some evidence suggests that olive oil consumption may reduce cognitive decline(20, 21). In the Three-City Study, participants who consumed more olive oil had lower risk of cognitive deficit for verbal fluency and visual memory. For cognitive decline during the 4-year follow-up, the association with intensive use was significant for visual memory (adjusted OR = 0.83, 95% CI: 0.69-0.99) but not for verbal fluency (OR = 0.85, 95% CI: 0.70-1.03) in multivariate analysis(20). In two random subsamples of 285 and 522 participants of the PREDIMED-Navarra trial, participants allocated to the Mediterranean Diet supplemented with extra virgin olive oil experienced better post-trial cognitive performance versus control in all cognitive domains and significantly better performance across fluency and memory tasks(21). Furthermore, adherence to Mediterranean diet has been associated with lower risk of cognitive impairment and Alzheimer’s disease in several prospective cohort studies(22). Mechanistic evidence is accruing in support of the hypothesis that olive oil, particularly the virgin variety rich in bioactive polyphenols, also reduces the underlying pathology of Alzheimer’s disease and other neurodegenerative diseases(23-25). However, further studies are needed to confirm the causality of these associations. The results for respiratory mortality are novel and to our knowledge no previous studies have evaluated these associations. One may speculate that mechanisms related to the anti-inflammatory and antioxidant properties of olive oil may have played a role in these findings but more research is needed.
To our knowledge, this study is the first to estimate the impact of replacing specific types of fat with olive oil in relation to total and cause-specific mortality. We estimated that substituting 10 g/d of other fats including margarine, butter, mayonnaise, and dairy fat with olive oil was associated with reductions in the risk of total and cause-specific mortality. Controlled feeding studies of vegetable oils rich in MUFAs, including olive oil, high-oleic-acid sunflower oil, high-oleic acid canola oil, and nuts, have consistently demonstrated beneficial effects on reducing cardiovascular risk factors(26), this seems particularly important for polyphenol-rich varieties of olive oil(27). Olive oil also exerts anti-inflammatory and anti-atherogenic effects and it may help reduce oxidative stress and improve endothelial function(28-30). Moreover, olive oil can improve the lipid profile, inflammatory biomarkers, insulin sensitivity, glycemic control, and decrease blood pressure(31-33). In a previous report from these cohorts, we found that higher olive oil intake was associated with lower levels of inflammatory biomarkers and a better lipid profile(2). Altogether, these potential mechanisms may have contributed to the observed inverse associations between olive oil intake and lower risk of mortality.
Strengths and limitations
Strengths of our study include the large sample size, long-term and high rates of follow-up, detailed and repeated measurements of diet and lifestyle, and numerous sensitivity analyses that support the robustness of our results. As with any observational study, the possibility of residual confounding cannot be ruled out despite adjusting for diet and lifestyle factors in our analysis. Higher olive oil intake could be a marker of a globally healthier diet and higher socioeconomic status. However, when we adjusted for food groups, AHEI, and also for socioeconomic variables, the results remained largely unchanged. Also, our study was conducted among a predominately non-Hispanic white population of health professionals, which minimizes potential confounding by socioeconomic factors but may limit generalizability. In our study, dietary assessment was conducted using validated self-reported FFQs which inevitably includes measurement errors. However, the use of averaged measurements reduced random measurement errors caused by within-person variation. Unfortunately, we could not distinguish between olive oil varieties containing different amounts of polyphenols and other non-lipid bioactive compounds.
Conclusions
In summary, we found that greater consumption of olive oil was associated with lower risk of total and cause-specific mortality. Replacing other types of fat such as margarine, butter, mayonnaise, and dairy fat with olive oil was associated with lower risk of mortality. Our results support current dietary recommendations to increase the intake of olive oil and other unsaturated vegetable oils in place of other fats to improve overall health and longevity.
Supplementary Material
Clinical Perspectives.
Competency in Patient Care:
In cohort studies of U.S. adults, replacing margarine, butter, mayonnaise, and dairy fat with olive oil is associated with lower risks of total and cause-specific mortality.
Translational Outlook:
Further studies are needed to confirm the association of olive oil consumption with reduced mortality, clarify the mechanisms responsible, and quantify the dose/volume boundaries around this effect.
Acknowledgements:
We would like to thank the participants and staff of the Nurses’ Health Study and Health Professionals Follow-up Study for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. The authors assume full responsibility for analyses and interpretation of these data.
Funding:
This work was supported by research grants UM1 CA186107, P01 CA87969, U01 CA167552, P30 DK046200, HL034594, HL088521, HL35464 and HL60712 from the National Institutes of Health. MG-F is supported by American Diabetes Association grant #1-18-PMF-029. J.S-S, is partially supported by the Catalan Institution for Research and Advanced Studies (ICREA) under the ICREA Academia program.
ABBREVIATIONS:
- MUFA
monounsaturated fatty acids
- HR
hazard ratio
- CI
confidence interval
- US
United States
- NHS
Nurses’ Health Study
- HPFS
Health Professionals Follow-up study
- FFQ
food frequency questionnaire
- AHEI
alternative healthy eating index
- PUFA
polyunsaturated fatty acids
- SFA
saturated fatty acids
Footnotes
Disclosures: No conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Gaforio JJ, Visioli F, Alarcón-de-la-Lastra C, et al. Virgin Olive Oil and Health: Summary of the III International Conference on Virgin Olive Oil and Health Consensus Report, JAEN (Spain) 2018. Nutrients 2019;11(9), ES2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guasch-Ferré M, Liu G, Li Y, et al. Olive Oil Consumption and Cardiovascular Risk in U.S. Adults. J Am Coll Cardiol. 2020;75:1729–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Estruch R, Ros E, Salas-Salvadó J, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med. 2018;379(14):1388–1389. [DOI] [PubMed] [Google Scholar]
- 4.Guasch-Ferré M, Hu FB, Martínez-González MA, et al. Olive oil intake and risk of cardiovascular disease and mortality in the PREDIMED Study. BMC Med. 2014;12:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barzi F, Woodward M, Marfisi RM, Tavazzi L, Valagussa F, Marchioli R. Mediterranean diet and all-causes mortality after myocardial infarction: results from the GISSI-Prevenzione trial. 2003;57(4):604–11. [DOI] [PubMed] [Google Scholar]
- 6.Buckland G, Mayen AL, Agudo A, et al. Olive oil intake and mortality within the Spanish population (EPIC-Spain). Am J Clin Nutr. 2012;96:142–149. [DOI] [PubMed] [Google Scholar]
- 7.Letois F, Mura T, Scali J, Gutierrez LA, Féart C, Berr C. Nutrition and mortality in the elderly over 10 years of follow-up: The Three-City study. Br J Nutr. 2016;116:882–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health 1997;6:49–62. [DOI] [PubMed] [Google Scholar]
- 9.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135:1114–26; [DOI] [PubMed] [Google Scholar]
- 10.Yuan C, Spiegelman D, Rimm EB, et al. Relative Validity of Nutrient Intakes Assessed by Questionnaire, 24-Hour Recalls, and Diet Records as Compared With Urinary Recovery and Plasma Concentration Biomarkers: Findings for Women. Am J Epidemiol. 2018;187:1051–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harvard TH Chan School of Public Health Nutrition Department. Food composition table. https://regepi.bwh.harvard.edu/health/nutrition/. [Google Scholar]
- 12.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 2012;142:1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang M, Spiegelman D, Kuchiba A, et al. Statistical methods for studying disease subtype heterogeneity. Stat. Med 2016;35:782–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martínez-González MA, Dominguez LJ, Delgado-Rodríguez M. Olive oil consumption and risk of CHD and/or stroke: a meta-analysis of case–control, cohort and intervention studies. Br. J Nutr 2014;112(2):248–59. [DOI] [PubMed] [Google Scholar]
- 15.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–2608. [DOI] [PubMed] [Google Scholar]
- 16.Guasch-Ferré M, Bulló M, Martínez-González MA, et al. Frequency of nut consumption and mortality risk in the PREDIMED nutrition intervention trial. BMC Med. 2013;11:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckland G, Gonzalez CA. The role of olive oil in disease prevention: A focus on the recent epidemiological evidence from cohort studies and dietary intervention trials. Br. J. Nutr 2015;113:S94–S101. [DOI] [PubMed] [Google Scholar]
- 18.Pelucchi C, Bosetti C, Negri E, Lipworth L, La Vecchia C. Olive oil and cancer risk: an update of epidemiological findings through 2010. Curr Pharm Des. 2011;17:805–812. [DOI] [PubMed] [Google Scholar]
- 19.Toledo E, Salas-Salvadó J, Donat-Vargas C, et al. Mediterranean Diet and Invasive Breast Cancer Risk Among Women at High Cardiovascular Risk in the PREDIMED Trial: A Randomized Clinical Trial. JAMA Intern Med. 2015;175:1752–60. [DOI] [PubMed] [Google Scholar]
- 20.Berr C, Portet F, Carriere I, et al. Olive oil and cognition: Results from the three-city study. Dement Geriatr Cogn Disord. 2009;28:357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martínez-Lapiscina EH, Clavero P, Toledo E, et al. Virgin olive oil supplementation and long-term cognition: the PREDIMED-NAVARRA randomized, trial. J Nutr Health Aging 2013;17:544–52. [DOI] [PubMed] [Google Scholar]
- 22.Serra-Majem L, Román-Viñas B, Sanchez-Villegas A, Guasch-Ferré M, Corella D, La Vecchia C. Benefits of the Mediterranean diet: Epidemiological and molecular aspects. Mol. Aspects Med 2019;67:1–55. [DOI] [PubMed] [Google Scholar]
- 23.Martorell M, Forman K, Castro N, Capó X, Tejada S, Sureda A. Potential Therapeutic Effects of Oleuropein Aglycone in Alzheimer’s Disease. Curr. Pharm. Biotechnol 2016;17:994–1001. [DOI] [PubMed] [Google Scholar]
- 24.Tsolaki M, Lazarou E, Kozori M, et al. A Randomized Clinical Trial of Greek High Phenolic Early Harvest Extra Virgin Olive Oil in Mild Cognitive Impairment: The MICOIL Pilot Study. J Alzheimer’s Dis. 2020;78:801–817. [DOI] [PubMed] [Google Scholar]
- 25.Brogi S, Sirous H, Calderone V, Chemi G. Amyloid ß fibril disruption by oleuropein aglycone: Long-time molecular dynamics simulation to gain insight into the mechanism of action of this polyphenol from extra virgin olive oil. Food Funct. 2020;11:8122–8132. [DOI] [PubMed] [Google Scholar]
- 26.Tindall AM, Petersen KS, Skulas-Ray AC, Richter CK, Proctor DN, Kris-Etherton PM. Replacing Saturated Fat With Walnuts or Vegetable Oils Improves Central Blood Pressure and Serum Lipids in Adults at Risk for Cardiovascular Disease: A Randomized Controlled-Feeding Trial. J Am Heart Assoc. 2019;8:e011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Medina-Remón A, Casas R, Tressserra-Rimbau A, et al. Polyphenol intake from a Mediterranean diet decreases inflammatory biomarkers related to atherosclerosis: a substudy of the PREDIMED trial. Br J Clin Pharmacol. 2017;83:114–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.López-Miranda J, Pérez-Jiménez F, Ros E, et al. Olive oil and health: summary of the II international conference on olive oil and health consensus report, Jaén and Córdoba (Spain) 2008. Nutr Metab Cardiovasc Dis. 2010;20:284–294. [DOI] [PubMed] [Google Scholar]
- 29.Covas M-I, de la Torre K, Farré-Albaladejo M, et al. Postprandial LDL phenolic content and LDL oxidation are modulated by olive oil phenolic compounds in humans. Free Radic. Biol. Med 2006;40:608–16. [DOI] [PubMed] [Google Scholar]
- 30.Bulló M, Lamuela-Raventós R, Salas-Salvadó J. Mediterranean diet and oxidation: nuts and olive oil as important sources of fat and antioxidants. Curr Top Med Chem. 2011;11:1797–1810. [DOI] [PubMed] [Google Scholar]
- 31.Fito M, Guxens M, Corella D, et al. Effect of a traditional Mediterranean diet on lipoprotein oxidation: a randomized controlled trial. Arch Intern Med. 2007;167:1195–1203. [DOI] [PubMed] [Google Scholar]
- 32.Ruiz-Canela M, Martínez-González MA. Olive oil in the primary prevention of cardiovascular disease. Maturitas 2011;68:245–250. [DOI] [PubMed] [Google Scholar]
- 33.Ros E, Martínez-González MA, Estruch R, et al. Mediterranean diet and cardiovascular health: Teachings of the PREDIMED study. Adv Nutr. 2014;5:330S–6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


