Abstract
Trichosporon asahii (Trichosporon beigelii) infections are rare but have been associated with a wide spectrum of clinical manifestations, ranging from superficial involvement in immunocompetent individuals to severe systemic disease in immunocompromised patients. We report on the recent recovery of T. asahii isolates with reduced susceptibility in vitro to amphotericin B (AMB), flucytosine, and azoles from six nongranulocytopenic patients who exhibited risk factors and who developed either superficial infections (four individuals) or invasive infections (two individuals) while in intensive care units. The latter two patients responded clinically and microbiologically to AMB treatment. All six isolates were closely related according to random amplified polymorphic DNA studies and showed 71% similarity by amplified fragment length polymorphism analysis, suggesting a common nosocomial origin. We also review the literature pertaining to T. asahii infections and discuss the salient characteristics of this fungus and recent taxonomic proposals for the genus.
Trichosporon infections are associated with a wide spectrum of clinical manifestations, ranging from superficial cutaneous involvement in immunocompetent individuals to severe systemic disease in immunocompromised patients (9, 44). Trichosporon asahii (Trichosporon beigelii) has increasingly been described as an opportunistic pathogen involved in disseminated infections in patients with profound granulocytopenia (9, 11, 26). Less commonly reported risk factors associated with infections caused by this agent include treatment with immunosuppressive drugs, transplantation, AIDS, extensive burns, and the presence of implanted prosthetic devices (9, 11, 14, 20, 24, 27, 29).
Trichosporon species were the most common non-Candida cause of fungemia at a national cancer institute (23). Disseminated Trichosporon infections in immunocompromised patients are frequently fatal, despite therapy with amphotericin B (AMB) (9, 44, 46). This antifungal agent has been shown to have a limited in vitro effect against Trichosporon species. In contrast, azoles have been demonstrated to have in vitro activity against members of this genus and their use has been associated with favorable responses in animal models (2, 3, 9, 27, 31, 32, 45, 46).
We report on the recent recovery of T. asahii isolates resistant in vitro to AMB and azoles from six nongranulocytopenic patients who developed either invasive or superficial infections while hospitalized in different intensive care units (ICUs). We describe the demographic and major clinical characteristics of these patients and review the literature pertaining to T. asahii infections. Results from molecular biology-based studies based on random amplified polymorphic DNA (RAPD) and amplified fragment length polymorphism (AFLP) analyses suggest that the isolates recovered from specimens of these six patients were closely related. In addition, we discuss the salient characteristics of this fungus and recent taxonomic proposals for the genus.
MATERIALS AND METHODS
Case reports.
The demographic and major clinical characteristics of the six patients who developed T. asahii infections in ICUs are presented in Table 1.
TABLE 1.
Characteristics of patients with invasive T. asahii infection in ICUsa
| Patient | Sex/age (yr) | Underlying condition(s) | Cause of ICU admission | Predisposing conditions | Time (days) of onset of infection | Manifestation | Culture source | Treatment | Infection outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/57 | NIDDM, CRF, COPD | Respiratory and renal failure | Peritoneal dialysis, ventilation, bacterial infection, antibiotics | 16 | Purulent peritonitis | Peritoneal fluid | AMB, catheter removal | Cure |
| 2 | M/45 | NIDDM | Multiple penetrating trauma in a marketplace | Central line, ventilation, bacterial infection, antibiotics | 21 | Fever, necrotic skin lesions | Skin biopsy specimen, urine | AMB | Cure |
| 3 | M/70 | NIDDM, HTN, IHD | Head trauma | Central line, ventilation, bacterial infection, antibiotics, TPN | 14 | None | Urine | None | NR |
| 4 | F/76 | PVD, CAF | Head trauma | Indwelling catheters, ventilation, bacterial infection, antibiotics | 21 | None | Urine | AMBb | NR |
| 5 | M/70 | NIDDM, HTN, IHD | Spontaneous cerebellar hemorrhage | Central line, ventilation, bacterial infection, antibiotics, TPN | 9 | None | Urine | None | NR |
| 6 | M/80 | IHD, CAF | Head trauma, subdural hematoma | Ventilation, bacterial infection, antibiotics | 14 | None | Urine | None | NR |
Abbreviations: F, female; M, male; CRF, chronic renal failure; COPD, chronic obstructive pulmonary disease; HTN, hypertension; IHD, ischemic heart disease; TPN, total parental nutrition; PVD, peripheral vascular disease; CAF, chronic atrial fibrillation; ICU, intensive care unit; NR, not relevant.
AMB treatment was instituted because of concurrent candidemia.
(i) Patient 1.
A 57-year-old woman with a history of non-insulin-dependent diabetes mellitus (NIDDM), chronic renal failure, and chronic obstructive pulmonary disease was admitted to an internal medicine ICU with acute respiratory failure secondary to a respiratory infection. In addition, the patient had acute renal failure with metabolic acidosis. She was placed on mechanical ventilation and peritoneal dialysis and was treated with intravenous ceftriaxone and erythromycin. Her hospital course was subsequently complicated by upper gastrointestinal bleeding and respiratory infection with Acinetobacter baumannii, which was treated with ceftazidime followed by imipenem. On day 16, she developed a spiking fever with purulent peritonitis. Culture of the peritoneal fluid yielded T. asahii. Treatment with AMB was instituted upon receipt of laboratory results indicating the recovery of a fungus in culture. The patient responded to the administration of AMB and removal of the peritoneal dialysis catheter with resolution of the fever; there was no recurrence of the fungal infection.
(ii) Patient 2.
A 45-year-old man with a history of NIDDM was admitted to a general ICU following multiple penetrating trauma sustained in a vegetable market accident which resulted in rib fractures with pneumohemothorax and pulmonary contusion. The patient was placed on mechanical ventilation, and vasopressors were administered. During the first 2 weeks after admission he suffered from recurrent respiratory infections with gram-negative bacteria, for which he received piperacillin-tazobactam and imipenem. Multiple cultures inoculated with urine specimens obtained between days 21 and 42 yielded T. asahii. In addition, on day 21 the patient was noted to have numerous necrotic skin nodules. True hyphae, pseudohyphae, and blastoconidia were microscopically observed in Cellufluor (Polysciences, Inc., Worthington, Pa.)-stained sections of a specimen of one of the skin lesions obtained by biopsy on day 35. A culture inoculated with portions of this skin biopsy specimen yielded T. asahii and Candida parapsilosis. No other active focus of infection was identified, and a diagnosis of systemic T. asahii infection was made. The patient was treated with AMB for 2 weeks, with general improvement and resolution of the fever and cutaneous lesions.
(iii) Patient 3.
A 70-year-old man with a history of NIDDM, hypertension, and ischemic heart disease was admitted to a neurosurgical ICU with left temporal bone fracture, brain contusion, and left hemiparesis following head trauma. The patient was placed on mechanical ventilation and treated by use of hyperventilation, mannitol, and furosemide. He experienced recurrent respiratory infections and intravenous catheter-associated sepsis, which were treated with broad-spectrum antibiotics (vancomycin, piperacillin-tazobactam, and cefepime) and total parenteral nutrition. Cultures of urine specimens collected on days 14 and 21 were positive for T. asahii. He had concurrent respiratory bacterial infection and C. parapsilosis candidemia, for which he was treated with AMB. There was no evidence of systemic T. asahii involvement.
(iv) Patient 4.
A 76-year-old woman with a history of peripheral vascular disease and chronic atrial fibrillation was admitted to a general ICU with intraventricular hemorrhage following head trauma. A ventriculostomy was performed, and mechanical ventilation was started. The patient was subsequently transferred to a neurosurgical ICU, where she suffered from recurrent aspiration pneumonia and pressure sores with bacteremia. She was treated with gentamicin and cloxacillin, followed by ceftazidime and metronidazole. A culture of a urine specimen collected on day 21 was positive for T. asahii and Candida glabrata. No clinical findings compatible with systemic infection were present. The patient was not treated with antifungal drugs, and subsequent cultures yielded only bacterial pathogens.
(v) Patient 5.
A 70-year-old man with a history of NIDDM, hypertension, and ischemic heart disease was admitted to a neurosurgical ICU in a comatose state following spontaneous cerebellar hemorrhage. He underwent craniotomy and was placed on mechanical ventilation and total parenteral nutrition. After a temporary improvement he developed a respiratory infection due to Pseudomonas aeruginosa and Klebsiella pneumoniae that was treated with piperacillin-tazobactam and later with imipenem. His condition deteriorated, with development of acute respiratory distress syndrome and severe metabolic acidosis. On day 9, a culture of a single urine specimen grew T. asahii. P. aeruginosa continued to be recovered in concurrent cultures of respiratory specimens and subsequent cultures of urine specimens. On day 18, the patient died of bacterial sepsis with multiorgan failure and disseminated intravascular coagulation.
(vi) Patient 6.
An 80-year-old man with a history of chronic atrial fibrillation and anticoagulation treatment was admitted to a neurosurgical ICU with acute subdural hematoma following a head injury. He was treated with fresh frozen plasma and hydantoin, was placed on mechanical ventilation, and underwent gastrostomy for feeding. An initial respiratory bacterial infection and intravenous catheter-associated sepsis were treated with ciprofloxacin and clindamycin. Multiple cultures inoculated with urine specimens collected between days 14 and 54 of his hospitalization were all positive for T. asahii. He had concurrent respiratory, urinary, and systemic bacterial infections, which responded to broad-spectrum antibiotics. There was no evidence for systemic T. asahii infection.
Patients 1 and 2 were epidemiologically unrelated, as they had no contact with each other, came from different cities, and were admitted to ICUs located in separate hospitals, and there was no contact between them. Patients 3 to 6 developed asymptomatic T. asahii mucosal colonization in the same neurosurgical ICU, with patients 3 to 5 hospitalized in that ICU during the same month.
Microscopic examination, isolation, and identification.
Preparations from the skin biopsy specimens were mounted on glass slides in a solution containing Cellufluor (Polysciences, Inc.), KOH, and glycerol and were examined microscopically by epifluorescence microscopy (34).
Yeast isolates were recovered from peritoneal fluid specimens (patient 1), portions of a skin biopsy specimen (patient 2), and urine specimens (patients 2 to 6) after 48 h of incubation at 30°C on Emmons' modified Sabouraud glucose agar (SGA) supplemented with 50 μg of chloramphenicol per ml and 5 μg of gentamicin per ml. A single colony recovered from each specimen was then transferred from SGA to CHROMagar Candida medium (CHROMagar, Paris, France), incubated at 30°C, and examined for colony color after 24 and 48 h. In addition, selected colonies of each isolate were transferred to fresh SGA and maintained at 30°C. Furthermore, each patient's isolate was deposited in the culture collection of the Centraalbureau voor Schimmelcultures (CBS) Fungal Biodiversity Center, Utrecht, The Netherlands (see Table 2 for the hospitals' internal accession numbers and CBS's accession numbers). Finally, the type strain of T. asahii (strain CBS 2479) was obtained from the same culture collection.
TABLE 2.
Susceptibilities of T. asahii isolates to antifungal drugs
| Patient no. (isolate no.) | MIC (mg/liter)a
|
||||
|---|---|---|---|---|---|
| AMB | FLC | ITC | KTC | 5FC | |
| 1 (P-8869; CBS 8973) | 8 (2.0) | 48 (32) | 1.5 (ND) | 0.5 (ND) | >32 (128) |
| 2 (P-9164, CBS 8975) | 1.5 (1.0) | 64 (32) | 1.0 (ND) | 0.75 (ND) | >32 (>512) |
| 3 (P-0116; CBS 8969) | 1.5 (>32) | 98.0 (32) | 1.5 (ND) | 1.0 (ND) | >32 (>512) |
| 4 (P-0221; CBS 8971) | >32 (2.0) | 128 (32) | 1.5 (ND) | 1.0 (ND) | >32 (>500) |
| 5 (P-0148; CBS 8970) | >32 (8.0) | 64 (32) | 1.0 (ND) | 1.0 (ND) | >32 (>512) |
| 6 (P-0791; CBS 8972) | 2 (>32) | 48 (64) | 2.0 (ND) | 0.75 (ND) | >32 (>512) |
| CBS-2479 (type strain) | 0.125 (0.25) | 32 (16) | 1.0 (ND) | 0.75 (ND) | >32 (128) |
| Susceptibility breakpointsb | 1 | 2–8 | 0.125 | 0.5 | 8–16 |
MICs were determined by the Etest method. Abbreviations: AMB, amphotericin B; FLC, fluconazole; ITC, itraconazole; KTC, ketoconazole; 5FC, flucytosine; ND, not detected. MICs in parentheses were determined by the NCCLS broth microdilution method (30).
Colonies from 48-h SGA cultures were evaluated for (i) sensitivity to cycloheximide, as determined by their growth on Mycosel agar (BBL, Cockeysville, Md.); (ii) growth at 37, 42, and 45°C on SGA; (iii) urease activity on Christensen's urea medium; (iv) carbohydrate and nitrogen assimilation patterns by means of API ID 32C and the API 20C AUX yeast assimilation systems (bioMérieux, Marcy l'Etoile, France); and (v) in vitro antifungal susceptibility testing by the Etest (AB Biodisk, Solna, Sweden) and National Committee for Clinical Laboratory Standards (NCCLS) methods (30). Conidial morphology and ontogeny on cornmeal-Tween agar (Difco Laboratories, Detroit, Mich.) slide cultures were examined microscopically after 7 to 10 days of incubation at 30°C. All the clinical isolates are maintained in the CBS culture collection (Table 2).
In vitro antifungal susceptibility testing by Etest method.
The in vitro antifungal susceptibilities of the T. asahii isolates were determined with the Etest system (AB Biodisk) according to the manufacturer's instructions. The agar formulations used in these studies consisted of (i) RPMI 1640 medium (Sigma, St. Louis, Mo.) supplemented with 1.5% agar and 2% glucose and buffered to pH 7.0 with 0.165 M morpholinepropanesulfonic acid buffer (MOPS; Sigma) for the azoles and (ii) modified Casitone agar consisting of 9 g of Casitone (Difco) per liter, 5 g of yeast extract (Difco) per liter, 10 g of sodium citrate (Sigma) per liter, and 20 g of glucose per liter for AMB and flucytosine. These media were dispensed into 90-mm plates to a depth of 4.0 mm. Cell suspensions from 48-h SGA cultures were prepared in sterile 0.85% NaCl and adjusted to the turbidity of a 1.0 McFarland standard. The MIC was defined as the lowest concentration of antifungal agent at which the border of the elliptical inhibition zone intercepted the readable scale on the strip. Candida krusei ATCC 6258 and C. parapsilosis ATCC 22019 served as quality control organisms for all tests.
In vitro antifungal susceptibility testing by broth dilution method.
The in vitro susceptibilities of the isolates were also determined by the broth microdilution method according to the recommendations of NCCLS (method M27-A [30]), as applied by Espinel-Ingroff et al. (12) for Trichosporon spp. These tests involved the use of filter-sterilized solutions of 0.2 ml of RPMI 1640 broth medium (Sigma) buffered to a final pH of 7.0 with 0.165 M MOPS (Sigma) and 1 M NaOH and inoculated with 104 cells per ml. For tests involving AMB, the RPMI 1640 medium was supplemented with 2% glucose. The microtitration plate for each test was incubated at 35°C for 48 h. The MIC was defined as the lowest drug concentration that resulted in complete inhibition of visible growth.
Molecular diagnosis and DNA relatedness.
Identification of the isolates was based on the sequencing of the D1/D2 domain of the large-subunit ribosomal DNA and of the internal transcribed spacer (ITS) regions in the ribosomal DNA, performed as described by Fell et al. (13). The DNA relatedness of the isolates was based on RAPD and AFLP analyses. The RAPD analysis used primers M13, GTG5, OPA2, and OPA4, as described by Boekhout et al. (5). The patterns of the individual primers were compared and summarized in one overall classification scheme. In addition, AFLP studies were conducted as reported by Boekhout et al. (6), except that in addition to the selective primer EcoRI-AC[FAM], the less selective primer EcoRI-A[FAM] in combination with primer MseI-G was also used. Data were analyzed with the Bionumerics software package (version 1.01; Applied Maths, Kortrijk, Belgium) using the whole densitometric curve of the fingerprint. Similarity values were calculated using the pairwise Pearson's product-moment correlation value (35).
RESULTS
Culture results.
White to cream-colored, folded colonies with low white aerial hyphae were recovered on SGA plates inoculated with the isolates from the six patients. Initial microscopic examination of portions of these colonies, as well as slide cultures, demonstrated round to oval, budding yeast-like cells and true hyphae forming cylindrical arthroconidia. The overall micro- and macroscopic appearances were consistent with those for members of the genus Trichosporon. The isolates formed rough, blue colonies on CHROMagar Candida. They grew on SGA at 30 and 37°C but not at 45°C, showed resistance to cycloheximide on Mycosel agar, and hydrolyzed urea on Christensen's medium. Excellent T. asahii identification profiles were obtained with the API 20C AUX and API ID 32C yeast assimilation test systems (biocodes of 6744774 and 7757675227, respectively).
Diagnosis and DNA relatedness by molecular biology-based methods.
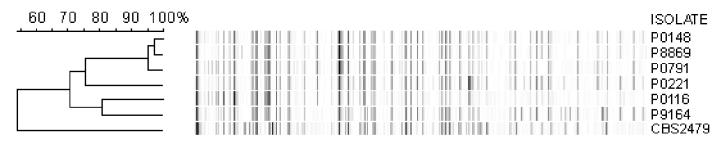
D1/D2 and ITS sequence analysis showed that the sequences of both of these regions in isolates P-0116, P-0148, P-0221, P-0791, and P-8869 (see Table 2 for the sources of the isolates) were the same as those of the type strain of T. asahii, strain CBS 2479 (GenBank accession numbers AF105393 and AY055381). RAPD analysis based on four primers (primers M13, GTG5, OPA2, and OPA4) resulted in clustering of the isolates into two closely related groups, i.e., type 1, composed of isolates P-0116 and P-0221, and type 1A, containing isolates P-0148, P-8869, and P-0791 (isolate P-9164 was not studied by RAPD analysis). The results of AFLP analysis showed good correlations with the data obtained by RAPD analysis. By AFLP analysis with the selective primer EcoRI-A[FAM], RAPD type 1A isolates P-0148, P-8869, and P-0791 formed a tight cluster with 95% similarity (Fig. 1). These isolates also clustered by AFLP analysis with the more specific primer, primer EcoRI-AC[FAM] (data not shown). The isolates of type 1 by RAPD analysis (isolates P-0221 and P-0116) and isolate P-9164 were more divergent by the AFLP analysis. However, the AFLP binding patterns of isolates P-0116 and P-9164 were 81% similar.
FIG. 1.
Clustering of Trichosporon obtained with primers with the adenosine extension. The clustering was obtained by the unweighted pair group method using arithmetic averages and shows the relationships between isolates of T. asahii on the basis of AFLP analysis with selective primer EcoRI-A[FAM] in combination with primer MseI-G.
Antifungal susceptibility.
The MICs of six antifungal drugs for the T. asahii isolates obtained by Etest method are presented in Table 2. As indicated, the isolates had reduced in vitro susceptibilities to AMB, flucytosine, and the azoles. Similar results were obtained when the NCCLS broth microdilution test was conducted (Table 2). In contrast, the type strain was sensitive to AMB (MICs, 0.125 mg/liter by the Etest and 0.25 mg/liter by the NCCLS method; Table 2). In addition, the fluconazole MIC for this strain was relatively high (32 mg/liter by the Etest and 16 mg/liter by the NCCLS procedure). However, we found that fluconazole MICs were higher for our clinical isolates (48 to 128 mg/liter by the Etest and 32 to 64 mg/liter by the NCCLS procedure; Table 2).
DISCUSSION
On the basis of the excellent identification profiles obtained by tests with the API ID 32C and API 20C AUX systems, the isolates' colony and microscopic morphologies, and the D1/D2 sequences of the large-subunit ribosomal DNAs, we identified the fungi recovered from the patients' specimens as T. asahii. Patients 1 and 2 developed invasive T. asahii infections with purulent peritonitis and systemic dissemination, respectively, whereas the other four patients had superficial mucosal colonization without evidence of systemic involvement. T. asahii is occasionally found in nature and can be recovered as a soil saprobe or from leaf litter (39). This species has been isolated from various types of clinical specimens from immunocompromised patients, including blood, skin biopsy, and urine specimens (9, 21, 22, 29, 41). Invasive infection with T. asahii is frequently associated with granulocytopenia and impaired phagocyte function (9, 41, 44). Factors that enhance mucosal colonization and subsequent invasion of Trichosporon species include broad-spectrum antibiotic treatment and breaks in mucosal barriers (7, 9, 26, 45). Thus, the pathogenesis of Trichosporon infection in the ICU setting may be similar to that of the more commonly observed Candida infection. Indeed, all six patients exhibited common risk factors such as trauma, prolonged mechanical ventilation, the presence of indwelling catheters, prior bacterial infections, and the use of broad-spectrum antibiotics. Of note, four of the patients suffered from diabetes mellitus, known to be associated with impaired leukocyte function. Although the clinical isolates were not all clonally related, a common nosocomial origin is suggested by their close relatedness according to RAPD analysis and their near similarity (71%) by AFLP analysis (Fig. 1).
T. asahii is the binomial in use for the species previously referred to as T. beigelii in descriptions of human mycoses. In 1992, Gueho et al. (15, 18) proposed significant taxonomic revisions for the genus Trichosporon. Subsequently, Sugita and colleagues (38, 40) expanded upon the proposals of Gueho et al., describing 17 species and five varieties within the genus. Of these species, six have been associated with different types of human infections (17, 38, 40): T. asahii and Trichosporon mucoides are involved in deep-seated infections, Trichosporon asteroides and Trichosporon cutaneum are found in superficial infections, and Trichosporon ovoides and Trichosporon inkin are involved in white piedra of the head and genital area (17, 19, 38, 40). Recently, comparative sequence analysis has suggested that these six medically relevant species can be readily identified by their ITS sequences in the ribosomal DNA, as determined by sequencing of PCR-amplified fragments. In addition, these studies demonstrated that conspecific strains have less than 1% nucleotide differences in the ITS regions (40).
Isolates recovered from specimens of the six patients were found by RAPD analysis to be closely related to each other. Results from the more sensitive AFLP analysis showed some differences in the isolates' banding patterns depending on the number of primers used in the studies. However, there was still a 71% similarity among the strains. Interestingly, patients 5 and 6, whose isolates (isolates P-0148 and P-0791, respectively) showed 97% similarity (Fig. 1), were hospitalized at the same time in the neurosurgical ICU of the same hospital.
It is clear from our results and from data in the literature (4, 8, 47) that the Etest is an acceptable method for determination of the antifungal susceptibilities of yeasts. Susceptibility studies of Cryptococcus neoformans, which is also a basidiomycete, have shown a good correlation (> 80%) between the results obtained with the Etest and by the NCCLS microdilution method (1, 8). Since similar comparative studies have not been conducted with T. asahii, we used both methods in our studies. Furthermore, data from recent papers demonstrated that elevation of the concentration of glucose from 0.2 to 2% in the RPMI 1640 medium optimized the growth of C. neoformans and was essential in distinguishing AMB-resistant and AMB-sensitive isolates of this yeast (1, 47). Therefore, the susceptibilities of our isolates to AMB were measured on glucose-supplemented RPMI 1640 medium.
All the clinical isolates in our study had reduced susceptibilities to AMB, flucytosine, and azoles (Table 2). There are only limited data in the literature regarding the susceptibilities of T. asahii isolates to antifungals. McGinnis et al. (28) showed that while T. asahii strains exhibited reduced susceptibilities to AMB (MICs, 1 to 4 mg/liter), they were susceptible to itraconazole and fluconazole (MICs, 0.125 to 1 and 0.5 to 4 mg/liter, respectively). The fluconazole MICs for two T. asahii isolates recovered from esophageal biopsy specimens of two patients were found to be relatively high (20 mg/liter), and the isolates were also resistant to nystatin. However, unlike the isolates recovered from the patients in our study, they were susceptible to AMB and flucytosine (MICs, <1 and <10 mg/liter, respectively) (25). A T. asahii strain isolated in cultures of blood from a patient who died from invasive trichosporonosis was found to be resistant to AMB in vitro (MIC, 2 mg/liter), but unlike our isolates, it was susceptible to fluconazole and itraconazole (MICs, 1 and 0.25 mg/liter, respectively) (10). Other reports did not distinguish between the different species of the T. beigelii group and were therefore not suitable for comparison.
The emergence of T. asahii isolates with reduced susceptibilities to common antifungal drugs is a matter for concern. While resistance to AMB is common among Trichosporon species (9, 16, 28, 42, 45, 46), this is only the second report, to the authors' knowledge, of strains with reduced susceptibilities to AMB, flucytosine, and azoles. Although T. cutaneum isolates recovered from nine patients with fungemia were recently reported to be resistant to antifungal antibiotics, only one was resistant to both AMB and azoles (22). However, the MICs for the latter isolate were much lower than those for the T. asahii isolates described in this report. Furthermore, in contrast to our patients, the AMB- and azole-resistant T. cutaneum strain was isolated from a patient previously treated with azoles, which might suggest drug-induced resistance.
While the mechanism of antifungal drug resistance in Trichosporon species is unknown, analysis of the isolates recovered in the present study could contribute to our understanding of the molecular basis of resistance. Increasing use of antifungal drugs in the ICU may lead to the selection and isolation of more resistant species in the future. To date, there are a paucity of data to correlate the clinical responses to and the in vitro activities of antifungal drugs, and the clinical significance of the results of in vitro susceptibility tests is not well established. Limited data suggest that the in vitro susceptibilities of Trichosporon species to the concentrations of azoles achievable in serum are associated with favorable clinical responses, even in neutropenic cancer patients whose granulocytopenia resolves (2, 9).
The two patients who had invasive infections with drug-resistant T. asahii responded clinically and microbiologically to AMB treatment and removal of the catheter. This emphasizes the importance of the patient's basic immune status in determining the outcomes of such infections. Furthermore, one should bear in mind that AMB might have modulatory effects on the immune system by upregulating the expression of proinflammatory cytokines and activating the mononuclear cells (37, 43). Hence, in vitro resistance to antifungal drugs may not be critical in immunocompetent patients, who may overcome the infection when the precipitating cause (e.g., a catheter) is removed, even if only partial inhibition of fungal growth is achieved through the use of antifungal drugs. However, immunocompromised patients may be dependent on fungicidal drug activity, so that infection with multidrug-resistant Trichosporon species may be catastrophic in this population.
ACKNOWLEDGMENT
We thank Ilana Sivan-Maltzov for technical assistance in the mycological study.
REFERENCES
- 1.Aller A I, Martin-Mazuelos E, Gutierrez M J, Bernal S, Chavez M, Recio F J. Comparison of the Etest and microdilution method for antifungal susceptibility testing of Cryptococcus neoformans to four antifungal agents. J Antimicrob Chemother. 2000;46:997–1000. doi: 10.1093/jac/46.6.997. [DOI] [PubMed] [Google Scholar]
- 2.Anaissie E, Gokaslan A, Hachem R, Rubin R, Griffin G, Robinson R, Sobel J, Bodey G. Azole therapy for trichosporonosis: clinical evaluation of eight patients, experimental therapy for murine infection, and review. Clin Infect Dis. 1992;15:781–787. doi: 10.1093/clind/15.5.781. [DOI] [PubMed] [Google Scholar]
- 3.Anaissie E J, Hachem R, Karyotakis N C, Gokaslan A, Dignani M C, Stephens L C, Tin U C. Comparative efficacies of amphotericin B, triazoles, and combination of both as experimental therapy for murine trichosporonosis. Antimicrob Agents Chemother. 1994;38:2541–2544. doi: 10.1128/aac.38.11.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arendrup M, Lundgren B, Jensen I M, Hansen B S, Frimodt-Moller N. Comparison of Etest and a tablet diffusion test with the NCCLS broth microdilution method for fluconazole and amphotericin B susceptibility testing of Candida isolates. J Antimicrob Chemother. 2001;47:521–526. doi: 10.1093/jac/47.5.521. [DOI] [PubMed] [Google Scholar]
- 5.Boekhout T, Kamp M, Gueho E. Molecular typing of Malassezia species with PFGE and RAPD. Med Mycol. 1998;36:365–372. doi: 10.1080/02681219880000581. [DOI] [PubMed] [Google Scholar]
- 6.Boekhout T, Theelen B, Diaz M, Fell J W, Hop W C, Abeln E C, Dromer F, Meyer W. Hybrid genotypes in the pathogenic yeast Cryptococcus neoformans. Microbiology. 2001;147:891–907. doi: 10.1099/00221287-147-4-891. [DOI] [PubMed] [Google Scholar]
- 7.Chan R M, Lee P, Wroblewski J. Deep-seated trichosporonosis in an immunocompetent patient: a case report of uterine trichosporonosis. Clin Infect Dis. 2000;31:621. doi: 10.1086/313968. [DOI] [PubMed] [Google Scholar]
- 8.Chang H C, Chang J J, Chan S H, Huang A H, Wu T L, Lin M C, Chang T C. Evaluation of Etest for direct antifungal susceptibility testing of yeasts in positive blood cultures. J Clin Microbiol. 2001;39:1328–1333. doi: 10.1128/JCM.39.4.1328-1333.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cox G M, Perfect J R. Cryptococcus neoformans var. neoformans and gattii and Trichosporon species. In: Ajello L, Hay R J, editors. Topley and Wilson's microbiology and microbial infections-medical mycology. 9th ed. New York, N.Y: Oxford University Press; 1998. pp. 461–484. [Google Scholar]
- 10.Ebright J R, Fairfax M R, Vazquez J A. Trichosporon asahii, a non-Candida yeast that caused fatal septic shock in a patient without cancer or neutropenia. Clin Infect Dis. 2001;33:E28–E30. doi: 10.1086/322640. [DOI] [PubMed] [Google Scholar]
- 11.Erer B, Galimberti M, Lucarelli G, Giardini C, Polchi P, Baronciani D, Gaziev D, Angelucci E, Izzi G. Trichosporon beigelii: a life-threatening pathogen in immunocompromised hosts. Bone Marrow Transplant. 2000;25:745–749. doi: 10.1038/sj.bmt.1702231. [DOI] [PubMed] [Google Scholar]
- 12.Espinel-Ingroff A, Barchiesi F, Hazen K C, Martinez-Suarez J V, Scalise G. Standardization of antifungal susceptibility testing and clinical relevance. Med Mycol. 1998;36(Suppl. 1):68–78. [PubMed] [Google Scholar]
- 13.Fell J W, Boekhout T, Fonseca A, Scorzetti G, Statzell-Tallman A. Biodiversity and systematics of basidiomycetous yeasts as determined by large-subunit rDNA D1/D2 domain sequence analysis. Int J Syst Evol Microbiol. 2000;50(Pt. 3):1351–1371. doi: 10.1099/00207713-50-3-1351. [DOI] [PubMed] [Google Scholar]
- 14.Finkelstein R, Singer P, Lefler E. Catheter-related fungemia caused by Trichosporon beigelii in non-neutropenic patients. Am J Med. 1989;86:133. doi: 10.1016/0002-9343(89)90247-7. [DOI] [PubMed] [Google Scholar]
- 15.Gueho E, de Hoog G S, Smith M T. Neotypification of the genus Trichosporon. Antonie Leeuwenhoek. 1992;61:285–288. doi: 10.1007/BF00713937. [DOI] [PubMed] [Google Scholar]
- 16.Gueho E, Improvisi L, Christen R, de Hoog G S. Phylogenetic relationships of Cryptococcus neoformans and some related basidiomycetous yeasts determined from partial large subunit rRNA sequences. Antonie Leeuwenhoek. 1993;63:175–189. doi: 10.1007/BF00872392. [DOI] [PubMed] [Google Scholar]
- 17.Gueho E, Improvisi L, de Hoog G S, Dupont B. Trichosporon on humans: a practical account. Mycoses. 1994;37:3–10. doi: 10.1111/j.1439-0507.1994.tb00277.x. [DOI] [PubMed] [Google Scholar]
- 18.Gueho E, Smith M T, de Hoog G S, Billon-Grand G, Christen R, Batenburg-van der Vegte W H. Contributions to a revision of the genus Trichosporon. Antonie Leeuwenhoek. 1992;61:289–316. doi: 10.1007/BF00713938. [DOI] [PubMed] [Google Scholar]
- 19.Gueho E M, Smith T, de Hoog G S. Trichosporon Behrend. In: Kurtzman C P, Fell J W, editors. The yeasts, a taxonomic study. 4th ed. Amsterdam, The Netherlands: Elsevier; 1998. pp. 857–858. [Google Scholar]
- 20.Hajjeh R A, Blumberg H M. Bloodstream infection due to Trichosporon beigelii in a burn patient: case report and review of therapy. Clin Infect Dis. 1995;20:913–916. doi: 10.1093/clinids/20.4.913. [DOI] [PubMed] [Google Scholar]
- 21.Itoh T, Hosokawa H, Kohdera U, Toyazaki N, Asada Y. Disseminated infection with Trichosporon asahii. Mycoses. 1996;39:195–199. doi: 10.1111/j.1439-0507.1996.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 22.Kataoka-Nishimura S, Akiyama H, Saku K, Kashiwa M, Mori S, Tanikawa S, Sakamaki H, Onozawa Y. Invasive infection due to Trichosporon cutaneum in patients with hematologic malignancies. Cancer. 1998;82:484–487. [PubMed] [Google Scholar]
- 23.Krcmery V, Jr, Mateicka F, Kunova A, Spanik S, Gyarfas J, Sycova Z, Trupl J. Hematogenous trichosporonosis in cancer patients: report of 12 cases including 5 during prophylaxis with itraconazol. Support Care Cancer. 1999;7:39–43. doi: 10.1007/s005200050221. [DOI] [PubMed] [Google Scholar]
- 24.Leaf H L, Simberkoff M S. Invasive trichosporonosis in a patient with the acquired immunodeficiency syndrome. J Infect Dis. 1989;160:356–357. doi: 10.1093/infdis/160.2.356. [DOI] [PubMed] [Google Scholar]
- 25.Lo Passo C, Pernice I, Celeste A, Perdichizzi G, Todaro-Luck F. Transmission of Trichosporon asahii oesophagitis by a contaminated endoscope. Mycoses. 2001;44:13–21. doi: 10.1046/j.1439-0507.2001.00614.x. [DOI] [PubMed] [Google Scholar]
- 26.Lyman C A, Garrett K F, Pizzo P A, Walsh T J. Response of human polymorphonuclear leukocytes and monocytes to Trichosporon beigelii: host defense against an emerging opportunistic pathogen. J Infect Dis. 1994;170:1557–1565. doi: 10.1093/infdis/170.6.1557. [DOI] [PubMed] [Google Scholar]
- 27.Martinez-Lacasa J, Mana J, Niubo R, Rufi G, Saez A, Fernandez-Nogues F. Long-term survival of a patient with prosthetic valve endocarditis due to Trichosporon beigelii. Eur J Clin Microbiol Infect Dis. 1991;10:756–758. doi: 10.1007/BF01972504. [DOI] [PubMed] [Google Scholar]
- 28.McGinnis M R, Pasarell L, Sutton D A, Fothergill A W, Cooper C R, Jr, Rinaldi M G. In vitro activity of voriconazole against selected fungi. Med Mycol. 1998;36:239–242. [PubMed] [Google Scholar]
- 29.Mirza S H. Disseminated Trichosporon beigelii infection causing skin lesions in a renal transplant patient. J Infect. 1993;27:67–70. doi: 10.1016/0163-4453(93)93838-u. [DOI] [PubMed] [Google Scholar]
- 30.National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved standard M27-A. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 31.Ogata K, Tanabe Y, Iwakiri K, Ito T, Yamada T, Dan K, Nomura T. Two cases of disseminated Trichosporon beigelii infection treated with combination antifungal therapy. Cancer. 1990;65:2793–2795. doi: 10.1002/1097-0142(19900615)65:12<2793::aid-cncr2820651231>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 32.Perfect J R, Schell W A. The new fungal opportunists are coming. Clin Infect Dis. 1996;22(Suppl. 2):S112–S118. doi: 10.1093/clinids/22.supplement_2.s112. [DOI] [PubMed] [Google Scholar]
- 33.Perparim K, Nagai H, Hashimoto A, Goto Y, Tashiro T, Nasu M. In vitro susceptibility of Trichosporon beigelii to antifungal agents. J Chemother. 1996;8:445–448. doi: 10.1179/joc.1996.8.6.445. [DOI] [PubMed] [Google Scholar]
- 34.Polacheck I, Salkin I F, Schenav D, Ofer L, Magen M, Haines J H. Damage to an ancient document by Aspergillus. Mycopathologia. 1989;106:89–93. [Google Scholar]
- 35.Rademaker J, de Bruijn F J. Characterization and classification of microbes by rep-PCR genomic fingerprinting and computer-assisted pattern analysis. 1997. Coordinating ed., G. Caetano-Anolle's and P. M. Greshof. John Wiley & Son. Inc., New York, N.Y. [Google Scholar]
- 36.Rex J H, Pfaller M A, Galgiani J N, Bartlett M S, Espinel-Ingroff A, Ghannoum M A, Lancaster M, Odds F C, Rinaldi M G, Walsh T J, Barry A L. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and Candida infections. Clin Infect Dis. 1997;24:235–247. doi: 10.1093/clinids/24.2.235. [DOI] [PubMed] [Google Scholar]
- 37.Reyes E, Cardona J, Prieto A, Bernstein E D, Rodriguez-Zapata M, Pontes M J, Alvarez-Mon M. Liposomal amphotericin B and amphotericin B-deoxycholate show different immunoregulatory effects on human peripheral blood mononuclear cells. J Infect Dis. 2000;181:2003–2010. doi: 10.1086/315517. [DOI] [PubMed] [Google Scholar]
- 38.Sugita T, Nakase T. Molecular phylogenetic study of the basidiomycetous anamorphic yeast genus Trichosporon and related taxa based on small subunit ribosomal DNA sequences. Mycoscience. 1998;39:7–13. [Google Scholar]
- 39.Sugita T, Nishikawa A, Ichikawa T, Ikeda R, Shinoda T. Isolation of Trichosporon asahii from environmental materials. Med Mycol. 2000;38:27–30. doi: 10.1080/mmy.38.1.27.30. [DOI] [PubMed] [Google Scholar]
- 40.Sugita T, Nishikawa A, Ikeda R, Shinoda T. Identification of medically relevant Trichosporon species based on sequences of internal transcribed spacer regions and construction of a database for Trichosporon identification. J Clin Microbiol. 1999;37:1985–1993. doi: 10.1128/jcm.37.6.1985-1993.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takamura S, Oono T, Kanzaki H, Arata J. Disseminated trichosporonosis with Trichosporon asahii. Eur J Dermatol. 1999;9:577–579. [PubMed] [Google Scholar]
- 42.Tashiro T, Nagai H, Nagaoka H, Goto Y, Kamberi P, Nasu M. Trichosporon beigelii pneumonia in patients with hematologic malignancies. Chest. 1995;108:190–195. doi: 10.1378/chest.108.1.190. [DOI] [PubMed] [Google Scholar]
- 43.Vonk A G, Netea M G, Denecker N E, Verschueren I C, van der Meer J W, Kullberg B J. Modulation of the pro- and anti-inflammatory cytokine balance by amphotericin B. J Antimicrob Chemother. 1998;42:469–474. doi: 10.1093/jac/42.4.469. [DOI] [PubMed] [Google Scholar]
- 44.Walling D M, McGraw D J, Merz W G, Karp J E, Hutchins G M. Disseminated infection with Trichosporon beigelii. Rev Infect Dis. 1987;9:1013–1019. doi: 10.1093/clinids/9.5.1013. [DOI] [PubMed] [Google Scholar]
- 45.Walsh T J, Lee J W, Melcher G P, Navarro E, Bacher J, Callender D, Reed K D, Wu T, Lopez-Berestein G, Pizzo P A. Experimental Trichosporon infection in persistently granulocytopenic rabbits: implications for pathogenesis, diagnosis, and treatment of an emerging opportunistic mycosis. J Infect Dis. 1992;166:121–133. doi: 10.1093/infdis/166.1.121. [DOI] [PubMed] [Google Scholar]
- 46.Walsh T J, Melcher G P, Rinaldi M G, Lecciones J, McGough D A, Kelly P, Lee J, Callender D, Rubin M, Pizzo P A. Trichosporon beigelii, an emerging pathogen resistant to amphotericin B. J Clin Microbiol. 1990;28:1616–1622. doi: 10.1128/jcm.28.7.1616-1622.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Warnock D W, Johnson E M, Rogers T R. Multi-centre evaluation of the Etest method for antifungal drug susceptibility testing of Candida spp. and Cryptococcus neoformans. BSAC Working Party on Antifungal Chemotherapy. J Antimicrob Chemother. 1998;42:321–331. doi: 10.1093/jac/42.3.321. [DOI] [PubMed] [Google Scholar]