Abstract
Background
Migrant populations in high-income countries have faced myriad health and social inequities during the COVID-19 pandemic. Migrants often work in frontline essential services that expose them to COVID-19. Migrant workers in meat processing plants have endured large COVID-19 outbreaks across multiple countries.
Objectives
We examine current scientific evidence around COVID-19 transmission, outcomes, and prevention for migrant workers and highlight meat processing plants as an example.
Sources
We performed a series of PubMed searches between January 1, 2020 and January 12, 2022.
Content
Migrant workers in high-income countries often work in occupations at high risk for COVID-19 transmission, contract COVID-19 at higher rates, and experience worse outcomes than native-born counterparts. For example, meat processing plants represent almost ideal environments for rapid and large-scale SARS-CoV-2 viral transmission; often, large migrant workforces confined to small workspaces perform physically demanding work in noisy environments that require shouting to communicate, increasing workers' respiratory rates and the quantity of aerosolized droplets expelled and thus increasing viral transmission risk. Although enhanced vaccination outreach programs remain an important equity approach for migrant worker safety, they alone are insufficient. The emergence and rapid spread of multiple increasingly transmissible SARS-CoV-2 variants of concern with variable vaccine escape properties, including Omicron in November 2021, highlight the importance of improved infection prevention and control strategies to protect migrant workers. Across countries, strategies such as improving ventilation and mask quality in many high-risk occupational settings are already required by employment law. Universal mandatory vaccination program should also be considered.
Implications
COVID-19 transmission prevention for migrant workers requires an aggressive multicomponent plan that includes (a) improved on-site ventilation and infection prevention and control strategies; (b) improved social supports such as paid sick leave; (c) mobile vaccination clinics and community engagement to overcome vaccine hesitancy and barriers; and (d) consideration of universal mandatory vaccination programs.
Keywords: COVID-19, Health equity, Mandatory vaccination, Meat processing plants, Migrants, Outbreaks, Vaccines
Background
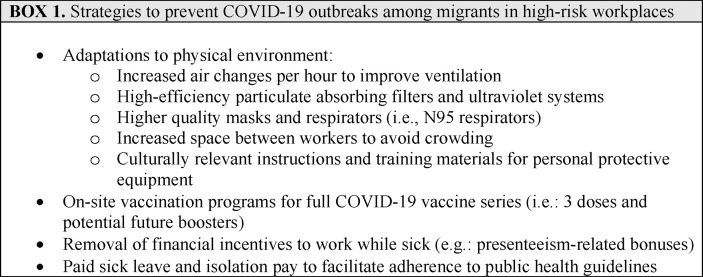
Migrants in high-income countries—including refugees, asylum seekers, undocumented migrants, transient migrant workers, and other newcomers—have faced myriad health and social inequities during the COVID-19 pandemic [[1], [2], [3], [4], [5], [6]]. Frontline migrant and racialized workers have experienced high COVID-19 infection, hospitalization, and death rates and impaired access to COVID-19 testing and health services [7] while filling critical roles that keep essential services operational [8,9].(see Fig. 1)
Fig. 1.
Summary of recommendations and interventions to prevent COVID-19 outbreaks among migrant workers in high-risk workplaces.
Across high-income countries, current public health guidelines emphasize prioritizing vaccination against COVID-19; however, given the complex social vulnerabilities migrant workers face, voluntary vaccination programs alone are insufficient. Like other frontline workers, migrant workers face high exposure risks and many access barriers for COVID-19 testing, healthcare, social, and settlement supports [4,7,8,10,11]. Meat processing plants in Europe and North America in particular represent an essential food service [12,13], yet are gruelling, low-paid occupational environments that attract mostly migrant workers [10,11] and have suffered large recurrent COVID-19 outbreaks throughout the pandemic [14,15]. Across North America and Europe, migrants make up 52%–70% of the workforce in meat processing plants [11,16,17].
Globally, various industries and workplaces that rely on migrant workers such as agriculture, manufacturing, and long-term care facilities have experienced large COVID-19 outbreaks due to both physical and social factors [11,[18], [19], [20]]. Meat processing plants in particular have endured multiple large COVID-19 outbreaks across several countries, including the United States, Germany, the United Kingdom, Spain, Italy, Canada, and Australia [1,2,[12], [13], [14],21,22]. In July 2020 in the United States, an estimated 8% and 4% of all COVID-19 infections and deaths, respectively, were associated with meat processing facilities [13]. In Canada, the large meat processing facility COVID-19 outbreak in High River, Alberta, in May 2020 that affected nearly 1000 workers is among the country's largest COVID-19 outbreaks [2]. These outbreaks have continued throughout 2021 [23], with mounting scientific evidence highlighting these facilities as uniquely conducive environments for SARS-CoV-2 transmission [1,3,10,12,15,23].
Since early 2021, SARS-CoV-2 variants of concern (VOCs) with increased transmissibility and virulence have emerged and spread through racialized and migrant worker communities and workplaces [[24], [25], [26], [27], [28], [29], [30], [31]]. In November 2021, the far more transmissible Omicron VOC with further immune and vaccine escape properties was identified and has since rapidly spread globally [30,31]. The efficacy and duration of vaccination-derived or infection-related immunity against Omicron is yet unclear but appears lower than in previous VOCs [30,31]. Therefore, despite aggressive vaccination campaigns in North America and Europe [32], the emergence of VOCs risks future outbreaks and poor health outcomes among migrant workers, as well as broader outward community transmission. As such, we must develop evidence-based strategies to mitigate the high potential human and economic costs associated with COVID-19 outbreaks among migrant workers [33,34].
Objectives
This narrative review examines the evidence around COVID-19 transmission, health outcomes, vaccinations, and other preventative approaches for migrant workers in high-income countries and explores meat processing plants as a specific example.
Migrant workers work in high-risk environments for COVID-19 transmission—the example of meat processing plants
International research and direct experience have shown that large occupational facilities that employ migrant workers, such as meat processing plants, represent environments that are highly conducive to rapid and large-scale viral spread [1,13,33]. Globally, meat processing plants have endured multiple large COVID-19 outbreaks across North America, Europe, and Australia [2,[12], [13], [14],21,22]. Since these outbreaks were first reported among meat processing facilities early in the pandemic in March through June 2020, scientists have learned much about the virus' transmission, viral dynamics, symptomatology, and effective nonpharmacologic infection prevention and control (IP&C) strategies [14,[35], [36], [37]]. Physical factors such as poor ventilation and loud environments, combined with large indoor workforces in close proximity that perform physically laborious fast-paced tasks, increase the risk of viral transmission [12,14,34,38]. Other physical factors such as cooled workspaces, medium-humidity recirculated air, and aerosolizing processes promote viral stability, viability, and spread of expelled viral particles [1,21,36]. These physical features combined with often large migrant workforces confined to small spaces for prolonged periods of time all likely contribute to increased viral transmission risk [14,36].
In meat processing plants, the work itself is physically demanding, and environments are often loud, requiring shouting to communicate. Combined, this increases both workers' respiratory rate and droplets expelled when communicating and thus likely further increases the viral transmission risk via increasing the quantity of SARS-CoV-2 virus expelled and aerosolized among infected workers [21,36]. Finally, although a recent study by Herstein et al. [14] showed that implementation of IP&C strategies such as using simple masks, two meter physical distancing, and installation of physical barriers between workers reduced SARS-CoV-2 transmission among meat processing plants in Nebraska, many of these measures were based on a now disproven droplet-based SARS-CoV-2 transmission paradigm [14]. The scientific community recently reached consensus on aerosolized SARS-CoV-2 transmission given the accumulated empirical evidence to support it over droplet or fomite (surface)-based transmission [35]. These data call into question the effectiveness of previously recommended mitigation strategies employed at many facilities, such as plexiglass barriers and surface cleaning. Indeed, the increased transmissibility of SARS-CoV-2 variants suggests that previously implemented IP&C measures in large occupational settings such as meat processing facilities must be reassessed with a new focus on air quality, improved ventilation, and improved mask type and quality used by workers [21,36].
Migrant workers are disproportionately affected and at higher risk for COVID-19 infection
Migrant workers in high-income countries across multiple industries face a much higher risk of contracting and suffering poor outcomes from COVID-19 than native born workers [34,38]. Disproportionately high COVID-19 infection, hospitalization, and death rates have been reported among racialized communities and migrant workforces in industries such as manufacturing, agriculture, distribution centres, and health care [8,9]. For example, the meat processing plant workforce in North America and Europe is composed largely of racialized immigrants, refugees, and temporary foreign workers (collectively known as migrants). In the United States, for example, 80.8% of frontline meat plant workers are visible non-White minorities (44.4% and 25.2% are Hispanic and Black, respectively), 51.5% are immigrants, and 45.1% live in low-income households (200% below the federal poverty line) [17]. In Canada, 13% and 67% of the meat processing industry's workforce are temporary foreign workers and immigrants respectively [16,39,40].
Migrant workers in high-income countries come from various ethnocultural communities in different phases of resettlement—from recently resettled refugees to first-generation citizens of resettlement countries [22]. They face language barriers, low health literacy, socioeconomic precarity, and fear of losing employment, which may reduce their ability to receive, understand, and act on COVID-19–related information aimed at reducing transmission, receiving health care, or protecting health. Furthermore, negative experiences due to racism or discrimination increase institutional mistrust—including the health system, government, employers, and unions [[41], [42], [43], [44]]. For example, due to the notoriety associated with various large COVID-19 outbreaks in meat processing facilities, migrant workers reported experiencing discrimination and being stigmatized as sources of community COVID-19 transmission [45]. Social factors such as overcrowded housing, transportation barriers, and poverty can also increase COVID-19 transmission risk [46]. Living in overcrowded housing or cohabitation in congregate housing with other migrant workers and transportation barriers that necessitate public transportation use or carpooling can increase viral exposure and make self-isolation and quarantine impossible.
Other socioeconomic factors such as low-paying work, lack of paid sick leave, and precarious immigration status linked to employment disincentivize migrant workers who develop COVID-19 symptoms to follow public health measures, isolate, or seek COVID-19 testing and instead incentivize working despite the knowledge that they may infect co-workers. Similarly, migrant workers are disincentivized from reporting COVID-19 exposures outside of work or participating in asymptomatic testing programs because many fear retribution for missing work or income loss due to lack of isolation pay [46,47]. Finally, migrant workers have reported presenteeism, a phenomenon that occurs when workers continue to work despite being ill, incentivized by monetary bonuses for not missing work due to illness or isolation [[46], [47], [48]].
Migrant workers may have misperceptions about COVID-19 and receive inaccurate health information from informal networks, especially if public health or occupational health and safety materials are not culturally tailored to or translated into primary languages [42,44,49,50]. Culturally tailored health information may include information delivered by trusted community leaders or that considers culture- and religion-specific concerns (i.e. Ramadan or Lent) [50]. Lack of translated culturally tailored health information from reputable sources combined with misinformation exposure through social networks and social media may further erode trust in health systems, employers, or public institutions. Mistrust can then lead to poor compliance with public health and occupational health guidance such as proper workplace personal protective equipment use and further increase infection risk [50,51].
Combined, environmental workplace factors, physically demanding work, language and health literacy barriers, socioeconomic precarity, overcrowded housing, transportation barriers, financial incentives, institutional mistrust, and misinformation exposure likely interact in complex ways to disproportionately increase COVID-19 transmission among migrant workers and their communities [15].
Migrant workers in frontline essential services suffer worse COVID-19–related clinical outcomes and higher mortality
In many high-income countries, agriculture is among the largest economic sectors and is considered essential infrastructure in a public health emergency [[47], [48], [49]]. Both Canadian and US governments have declared food production facilities essential infrastructure during the COVID-19 pandemic, recommending their protection and prioritizing their maintained function. For migrant workers, working in critical industries the COVID-19 pandemic has proven deadly and has exacerbated existing health inequities between them and the general population [[52], [53], [54], [55]]. A recently published systematic review by Hayward et al. summarizes 123 published studies and details the detrimental health impacts of COVID-19 among migrant workers across 15 high-income countries [8]. The authors highlight migrant populations as facing increased risk of contracting and being hospitalized due to COVID-19, often facing rates multiple times higher than their native-born compatriots—especially among migrants from racialized backgrounds such as sub-Saharan Africa, Latin America, South Asia, or the Middle East [8]. Furthermore, migrants face increased risks of dying from COVID-19 compared to native-born residents in Sweden, the United Kingdom, Canada, Denmark, Italy, and France [8]. For example, in Sweden, Somali, Lebanese, and Syrian migrants faced much higher risk of death from COVID-19 than Swedish-born residents (age- and sex-adjusted risk hazard ratios (95% CI): 12.4 (7.9–19.4), 6.2 (3.4–11.2), and 6.1 (4.3–8.8), respectively) [8,56].
To address these disproportionate risks, the Canadian National Advisory Committee on Immunizations recommended prioritizing key populations for COVID-19 immunization, including frontline essential workers at increased COVID-19 exposure risk [57], temporary foreign workers and newcomers living in congregate settings, and marginalized and racialized communities disproportionately affected by COVID-19 [57,58]. Many migrant workers in high-income countries meet all these criteria [57]. Protecting migrant workers through prioritized vaccination and other public health measures benefits broader society. Specifically, prioritized migrant worker outreach vaccination programs not only protect workers and their communities, but also food supply chains and agricultural economies. However, prioritized vaccinations alone are insufficient. Controlling the pandemic and protecting vulnerable migrant communities and essential workers demands that we better understand work-related health inequities and better address the social factors that drive them.
Recommendations
Improving vaccine access with outreach vaccination programs
Multistakeholder groups with representation from employers, public health, health system, and migrant-serving social agencies should coordinate to enhance migrant workers' access to COVID-19 vaccines by providing on-site workplace vaccinations. To overcome vaccine hesitancy and rebuild trust among migrants working in frontline essential services, health systems should provide immunizations in a culturally sensitive manner with translation and cultural brokering services [49,50,59]. On-site workplace vaccinations will address transportation barriers and inability or hesitancy to miss work to receive a vaccine [41,42,46,47]. Mobile vaccination units require (a) physical space including tents, chairs, tables, electricity, and heat; (b) supplies including syringes, vaccines, alcohol swabs, and emergency response kits; (c) data support and staff to register employees and track vaccinations within their appropriate health systems; (d) healthcare personnel including nurses, physicians, and support staff; and (e) social supports including workers' unions and immigrant-serving agencies to provide first-language translation and culturally concordant supports and health information for migrant workers [50,60].
Voluntary vaccination programs are not enough
Given the physical characteristics of crowded work environments that increase COVID-19 transmission risk and the social vulnerabilities migrants face, prioritizing migrants for vaccination will protect their health, their communities, and the broader economy. Although COVID-19 vaccines are widely available in high-income countries, high levels of vaccine hesitancy, low health literacy, poor access to healthcare services, experiences of racism and discrimination, and institutional mistrust hinder vaccination efforts [61]. As such, universal mandatory workplace vaccinations programs should be considered at identified high-risk workplaces and combined with improved culturally tailored social supports such as sick pay, healthcare access, improved communication, and employee engagement. However, if not applied universally to all employees (migrant and nonmigrant alike) or implemented poorly without appropriate communication and supports, mandatory vaccination programs may increase mistrust and migrant discrimination and hinder public health efforts. In contrast, universally applied and appropriately supported mandatory workplace vaccination programs can improve health equity and protect workplaces. Indeed, many countries have applied mandatory vaccination programs to high-risk healthcare settings [62] and workplaces such as meat processing plants in the United States [62].
Improve workplace safety standards and ventilation
The scientific understanding of COVID-19's viral transmission dynamics and aerosolized spread has advanced rapidly through the pandemic [12,35,36]. The SARS-CoV-2 Omicron variant's recent rapid global spread highlights the importance of applying this knowledge to improve IP&C and ventilation across all high-risk environments [[29], [30], [31]]. High-risk workplaces such as meat processing plants should improve workplace safety standards, provide higher quality respirator masks, and improve ventilation systems to address our improved understanding of COVID-19's aerosolized transmission [38]. The benefits of improving the physical work environment where migrant workers are found will almost certainly last beyond COVID-19 and, at a minimum, improve worker safety irrespective of any future SARS-CoV-2 VOCs [16].
Case Study: prevention approaches for meat plant migrant workers in Alberta, Canada
An integrated approach to address COVID-19 transmission risk in large meat processing plant facilities in Alberta, Canada, included physical improvements, social supports, healthcare access, and accessible, culturally tailored vaccination campaigns. New evidence surrounding SARS-CoV-2 transmission dynamics led to improved ventilation by increasing air changes per hour and installing high-efficiency particulate absorbing filters and ultraviolet systems [63]. Second, in addition to universal masking, employees used higher quality masks and received culturally tailored training materials on how to appropriately don and doff them [37]. Third, physical modifications were employed that increased space between workers to avoid crowding. Fourth, onsite workplace COVID-19 vaccination clinics were held with high employee uptake for first and second COVID-19 vaccine doses [64]. Fifth, unions advocated to remove financial incentives to attend work while ill or avoid mass testing to receive presenteeism-related bonuses [46]. Instead, paid sick leave and isolation pay was made broadly available and communicated to employees, to avoid financial penalties for appropriately following public health and occupational health measures [47,65]. In combination, these modifications will likely greatly reduce the risk of future COVID-19 outbreaks or of other respiratory-borne illnesses among migrant workers in these high-risk workplaces.
Variants, Omicron, and ongoing uncertainties
Although the scientific community has made great progress in understanding and preventing large outbreaks among migrant workers in high-risk workplaces, many uncertainties remain. For example, the protective effects and duration of natural immunity among workplaces that have already experienced large outbreaks among their workers are unknown, as is how natural immunity will be affected by new or emerging COVID-19 VOCs such as Omicron, which, at the time of writing, is rapidly spreading globally [29]. The degree of vaccine hesitancy among migrant workers is also unclear, as are the best strategies to improve trust among migrant communities. This is of increased importance given that third and even fourth dose booster vaccination campaigns are underway in many high-income countries, and emerging data suggest booster doses likely improve vaccine efficacy against Omicron [29]. Finally, thanks to the rapid development of multiple effective COVID-19 vaccines, a growing health equity argument exists for mandatory vaccination programs. As it is unclear how long their immune protection will last, and unclear how many employees would be willing to accept annual (or regular) immunizations, mandatory programs may be important. Finally, physical environment adaptations that reduce viral transmission risk in high-risk workplaces, such as increased space between workers to avoid crowding (as outlined in Fig. 1 ), may negatively affect processing rates and production speeds; however, these economic impacts must be weighed against the safety, risk, and detrimental economic impact of future outbreaks. Our collective scientific understanding of COVID-19 has changed rapidly but so has the virus itself; thus, we urgently need guidelines for mandatory vaccination programs and improved infection control measures.
Policy implications
The COVID-19 pandemic has revealed workplaces such as meat processing plants as high-risk environments for COVID-19 transmission and the migrant workers in high-income countries who work in them as particularly vulnerable to COVID-19 infection, severe outcomes, and death. The negative COVID-19–related economic and health consequences of workplace outbreaks can be mitigated by prioritizing frontline essential migrant workers for COVID-19 vaccination—but this alone is insufficient. Although population-wide vaccination campaigns are deemed the best opportunity to end the pandemic, relying on voluntary vaccination alone will unlikely suffice to reduce the COVID-19 risk among migrant workers.
Instead, preventing future COVID-19 outbreaks among migrant workers in high-risk workplaces requires an aggressive multicomponent plan including (a) on-site IP&C strategies and improved ventilation prepared by experts in occupational hygiene (i.e. where the hierarchy of controls is respected) [66]; (b) improved social supports such as paid sick leave; (c) migrant worker community engagement programs to build trust in public health interventions, vaccines, health institutions, and employers; and (d) consideration of universally applied mandatory vaccination mandates in high-risk workplaces, as some companies have now adopted [62].
Several of these changes can be implemented in law, as observed in Ontario, Canada's largest province. Human rights law allows for mandatory workplace vaccination, provided that accommodation is offered for legitimate, demonstrable medical or religious reasons [67]. Likewise, paid sick leave can be incorporated into employment standards law [68]. Moreover, where work conditions in the food industry are unsafe, the courts have backed public health officials issuing remedial orders, precautionarily so as to prevent large outbreaks occurring [69]. Given that large outbreaks occurred across worksites such as meat processing facilities, without these legal measures swiftly being brought to bear, suggests that public health officials and governments failed to act wisely and thus contributed to excess disease and mortality.
Conclusion
Migrant workers have suffered disproportionately increased rates of infection, hospitalization, and death compared to the general population in many high-income countries [8]. Large agricultural workplaces such as meat processing facilities, together with their migrant workforces, are essential services but high-risk environments for COVID-19 transmission. Many large-scale outbreaks have occurred across multiple jurisdictions, highlighting the impacts on broader community transmission and community health. Although many in public health are hopeful that broad vaccination uptake will help end the pandemic, reaching that outcome likely requires mandatory COVID-19 vaccination. Furthermore, the emergence of SARs-CoV-2 VOCs with significant immune and vaccine escape properties further calls into question the reliance on vaccinations alone. Building future resilience necessitates a broader public health approach that addresses the social determinants of health among migrant workers and other socially vulnerable populations and using other public health measures, improving facility-level ventilation and engineering improvements, and employing legal measures, which thus far have been mostly overlooked in the COVID-19 response until it was too late.
Transparency declaration
The authors have no conflicts of interest to declare. This review was supported by a project grant from the Canadian Institutes of Health Research.
Author contributions
GEF and KP contributed to the concept, design, and writing and have overseen the final manuscript preparation and submission. CEP, PER, AA, LH, and KM contributed to the occupational health, public health, and health policy content. All named authors engaged in the writing and review and gave final approval of the version of the guideline to be published.
Acknowledgements
We would like to gratefully thank the many meat processing plant workers in Alberta, Canada, who have participated in our ongoing research and greatly informed this work. We would also like to thank the University of Calgary Refugee Health YYC research team and our community scholars: Mussie Yemane, Adanech Sahilie, Minnella Antonio, Edna Ramirez Cerino, Michael Youssef, and Ajak Abraham Kuchkon, without whom we could not conduct meaningfully engaged community-based research. Finally, we are grateful for the continuous support of the United Food and Commercial Workers Union, Local 401, especially Mr. Thomas Hesse and Ms. Richelle Stewart.
Editor: L. Leibovici
References
- 1.Waltenburg M.A., Rose C.E., Victoroff T., Butterfield M., Dillaha J.A., Heinzerling A., et al. Coronavirus disease among workers in food processing, food manufacturing, and agriculture workplaces. Emerg Infect Dis. 2021;27:243–249. doi: 10.3201/eid2701.203821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Durand-Moreau Q., Adisesh A., Mackenzie G., Bowley J., Straube S., Chan X.H., et al. The Centre for Evidence-Based Medicine; 2020. COVID-19 in meat and poultry facilities: a rapid review and lay media analysis.https://www.cebm.net/covid-19/what-explains-the-high-rate-of-sars-cov-2-transmission-in-meat-and-poultry-facilities-2/ Available from: [Google Scholar]
- 3.Donahue M., Sreenivasan N., Stover D., Rajasingham A., Watson J., Bealle A., et al. Notes from the field: characteristics of meat processing facility workers with confirmed SARS-CoV-2 infection—Nebraska, April–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1020–1022. doi: 10.15585/mmwr.mm6931a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koh D. Migrant workers and COVID-19. Occup Environ Med. 2020;77:634–636. doi: 10.1136/oemed-2020-106626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenaway C., Hargreaves S., Barkati S., Coyle C.M., Gobbi F., Veizis A., et al. COVID-19: exposing and addressing health disparities among ethnic minorities and migrants. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa113. taaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liem A., Wang C., Wariyanti Y., Latkin C.A., Hall B.J. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. 2020;7 doi: 10.1016/S2215-0366(20)30076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arya N., Redditt V.J., Talavlikar R., Holland T., Brindamour M., Wright V., et al. Caring for refugees and newcomers in the post-COVID-19 era: evidence review and guidance for FPs and health providers. Can Fam Physician. 2021;67:575–581. doi: 10.46747/cfp.6708575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayward S.E., Deal A., Cheng C., Crawshaw A., Orcutt M., Vandrevala T.F., et al. Clinical outcomes and risk factors for COVID-19 among migrant populations in high-income countries: a systematic review. J Migr Heal. 2021;3:100041. doi: 10.1016/j.jmh.2021.100041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sze S., Pan D., Nevill C.R., Gray L.J., Martin C.A., Nazareth J., et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100630. doi: 10.1016/j.eclinm.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steinberg J., Kennedy E.D., Basler C., Grant M.P., Jacobs J.R., Ortbahn D., et al. COVID-19 outbreak among employees at a meat processing facility—South Dakota, March–April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1015–1019. doi: 10.15585/mmwr.mm6931a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reid A., Rhonda-Perez E., Schenker M.B. Migrant workers, essential work, and COVID-19. Am J Ind Med. 2021;64:73–77. doi: 10.1002/ajim.23209. [DOI] [PubMed] [Google Scholar]
- 12.Donaldson A.I. Aerosols in meat plants as possible cause of Covid-19 spread. Vet Rec. 2020;187:34–35. doi: 10.1136/vr.m2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor C.A., Boulos C., Almond D. Livestock plants and COVID-19 transmission. Proc Natl Acad Sci U S A. 2020;117:31706–31715. doi: 10.1073/pnas.2010115117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herstein J.J., Degarege A., Stover D., Austin C., Schwedhelm M.M., Lawler J.V., et al. Characteristics of SARS-CoV-2 transmission among meat processing workers in Nebraska, USA, and effectiveness of risk mitigation measures. Emerg Infect Dis. 2021;27:1032–1038. doi: 10.3201/eid2704.204800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waltenburg M.A., Victoroff T., Rose C.E., Butterfield M., Jervis R.H., Fedak K.M., et al. Update: COVID-19 among workers in meat and poultry processing facilities―United States, April–May 2020. Morb Mortal Wkly Rep. 2020;69:887. doi: 10.15585/mmwr.mm6927e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bragg B., Abes J.G., Bravante M. No safe place: documenting the migration status and employment conditions of workers in Alberta’s meatpacking industry during the pandemic—MIGRANT DIGNITY PROJECT. https://actiondignity.org/wp-content/uploads/2021/09/NO-SAFE-PLACE_FINAL.pdf REPORT TO COMMUNITY [Internet]. 2021 Aug [cited 2022 Jan 7]. Available from:
- 17.Fremstad S., Rho H.J., Brown H. Center for Economic and Policy Research; 2020. Meatpacking workers are a diverse group who need better protections.https://cepr.net/meatpacking-workers-are-a-diverse-group-who-need-better-protections/ [cited 2022 Jan 7]. Available from: [Google Scholar]
- 18.Canadian Institute for Health Information . CIHI; Ottawa, ON: 2020. Pandemic experience in the long-term care sector: how does Canada compare with other countries? [Google Scholar]
- 19.Augère Granier M.-L. Migrant seasonal workers in the European agricultural sector. EPRS Eur Parliam Res Serv. 2021:1–12. [Google Scholar]
- 20.Glover R.E., van Schalkwyk M.C.I., Akl E.A., Kristjannson E., Lotfi T., Petkovic J., et al. A framework for identifying and mitigating the equity harms of COVID-19 policy interventions. J Clin Epidemiol. 2020;128:35–48. doi: 10.1016/j.jclinepi.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guenther T., Czech-Sioli M., Indenbirken D., Robitailles A., Tenhaken P., Exner M., et al. Investigation of a superspreading event preceding the largest meat processing plant-related SARS-Coronavirus 2 outbreak in Germany. SSRN Electron J. 2020;12 doi: 10.15252/emmm.202013296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubenstein B.L., Campbell S., Meyers A.R., Crum D.A., Mitchell C.S., Hutson J., et al. Factors that might affect SARS-CoV-2 transmission among foreign-born and U.S.-born poultry facility workers - Maryland, May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1906. doi: 10.15585/mmwr.mm6950a5. –10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Douglas L., Food & Environment Reporting Network Mapping Covid-19 outbreaks in the food system | Food and Environment Reporting Network. Food & Environment Reporting. 2020 https://thefern.org/2020/04/mapping-covid-19-in-meat-and-food-processing-plants/ cited 2022 Jan 21]. Available from: [Google Scholar]
- 24.Walensky R.P., Walke H.T., Fauci A.S. SARS-CoV-2 variants of concern in the United States-challenges and opportunities. JAMA. 2021;325:1037–1038. doi: 10.1001/jama.2021.2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davies N.G., Jarvis C.I., Edmunds W.J., Jewell N.P., Diaz-Ordaz K., Keogh R.H. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature. 2021;593:270–274. doi: 10.1038/s41586-021-03426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernal J.L., Andrews N., Gower C., Gallagher E., Simmons R., Thelwall S., et al. Effectiveness of covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med. 2021;385:585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Planas D., Veyer D., Baidaliuk A., Staropoli I., Guivel-Benhassine F., Rajah M.M., et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature. 2021;596:276–280. doi: 10.1038/s41586-021-03777-9. [DOI] [PubMed] [Google Scholar]
- 28.Del Rio C., Malani P.N., Omer S.B. Confronting the delta variant of SARS-CoV-2, summer 2021. JAMA. 2021;326:1001–1002. doi: 10.1001/jama.2021.14811. [DOI] [PubMed] [Google Scholar]
- 29.del Rio C., Omer S.B., Malani P.N. Winter of Omicron—the evolving COVID-19 pandemic. JAMA. 2022;327:319–320. doi: 10.1001/jama.2021.24315. [DOI] [PubMed] [Google Scholar]
- 30.Callaway E. Omicron likely to weaken COVID vaccine protection. Nature. 2021;600:367–368. doi: 10.1038/d41586-021-03672-3. [DOI] [PubMed] [Google Scholar]
- 31.Burki T.K. Omicron variant and booster COVID-19 vaccines. Lancet Respir Med. 2022;10:e17. doi: 10.1016/S2213-2600(21)00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ritchie H., Mathieu E., Rodés-Guirao L., Appel C., Giattino C., Ortiz-Ospina E., et al. Coronavirus pandemic (COVID-19) 2020. https://ourworldindata.org/covid-vaccinations?country=OWID_WRL Coronavirus (COVID-19) Vaccinations. Our World In Data.
- 33.Middleton J., Reintjes R., Lopes H. Meat plants-a new front line in the covid-19 pandemic. BMJ. 2020;370:m2716. doi: 10.1136/bmj.m2716. [DOI] [PubMed] [Google Scholar]
- 34.Parks C.A., Nugent N.B., Fleischhacker S.E., Yaroch A.L. Food system workers are the unexpected but under protected COVID heroes. J Nutr. 2020;150:2006. doi: 10.1093/jn/nxaa173. –8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masotti F., Cattaneo S., Stuknyte M., Pica V., De Noni I. Transmission routes, preventive measures and control strategies of SARS-CoV-2 in the food factory. Crit Rev Food Sci Nutr. 2021:1–12. doi: 10.1080/10408398.2021.1879728. [DOI] [PubMed] [Google Scholar]
- 37.Brooks J.T., Butler J.C. Effectiveness of mask wearing to control community spread of SARS-CoV-2. JAMA. 2021;325:998. doi: 10.1001/jama.2021.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramos A.K., Lowe A.E., Herstein J.J., Schwedhelm S., Dineen K.K., Lowe J.J. Invisible no more: the impact of COVID-19 on essential food production workers. J Agromedicine. 2020;25:378–382. doi: 10.1080/1059924X.2020.1814925. [DOI] [PubMed] [Google Scholar]
- 39.Food Processing Skills Canada Securing Canada’s Meat Workforce: real challenges, practical solutions, fresh perspectives. 2019. www.fpsc-ctac.com [cited 2022 Jan 7]. Available from:
- 40.Zhang Y., Ostrovsky Y., Arsenault A. Foreign workers in the Canadian food manufacturing industry. 2021. https://www150.statcan.gc.ca/n1/pub/36-28-0001/2021004/article/00003-eng.htm Statistics Canada - Economic and Social Reports.
- 41.Eissa A., Lofters A., Akor N., Prescod C., Nnorom O. Increasing SARS-CoV-2 vaccination rates among Black people in Canada. Can Med Assoc J. 2021;193:E1220–E1221. doi: 10.1503/cmaj.210949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas C.M., Osterholm M.T., Stauffer W.M. Critical considerations for COVID-19 vaccination of refugees, immigrants, and migrants. Am J Trop Med Hyg. 2021;104:433–435. doi: 10.4269/ajtmh.20-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galletly C.L., Lechuga J., Dickson-Gomez J.B., Glasman L.R., McAuliffe T.L., Espinoza-Madrigal I. Assessment of COVID-19–related immigration concerns among Latinx immigrants in the US. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.17049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Campbell-Scherer D., Chiu Y., Ofosu N.N., Luig T., Hunter K.H., Jabbour B., et al. Illuminating and mitigating the evolving impacts of COVID-19 on ethnocultural communities: a participatory action mixed-methods study. Can Med Assoc J. 2021;193:E1203–E1212. doi: 10.1503/cmaj.210131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Small K., MacViver A., Gilligan M. Coronavirus: cargill meat-packing plant in High River, Alta., reopens amid ongoing talks with union. 2020. https://globalnews.ca/news/6900280/coronavirus-cargill-union-talks-alberta/ Global News [Internet]
- 46.Tilchin C., Dayton L., Latkin C.A. Socioeconomic factors associated with an intention to work while sick from COVID-19. J Occup Environ Med. 2021;63:363–368. doi: 10.1097/JOM.0000000000002147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vazquez J., Islam T., Beller J., Fiori K., Correa R., Correa D.J. Expanding paid sick leave as a public health tool in the Covid-19 pandemic. J Occup Environ Med. 2020;62:e598–e599. doi: 10.1097/JOM.0000000000001998. [DOI] [PubMed] [Google Scholar]
- 48.St-Denis X. Sociodemographic determinants of occupational risks of exposure to COVID-19 in Canada. Can Rev Sociol Can Sociol. 2020;57:399–452. doi: 10.1111/cars.12288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kadambari S., Vanderslott S. Lessons about COVID-19 vaccine hesitancy among minority ethnic people in the UK. Lancet Infect Dis. 2021;21:1204–1206. doi: 10.1016/S1473-3099(21)00404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crawshaw A.F., Deal A., Rustage K., Forster A.S., Campos-Matos I., Vandrevala T., et al. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J Travel Med. 2021;28:taab048. doi: 10.1093/jtm/taab048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turhan Z., Dilcen H.Y., Dolu İ. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr Psychol. 2021;22:1–10. doi: 10.1007/s12144-021-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tuyisenge G., Goldenberg S.M. COVID-19, structural racism, and migrant health in Canada. Lancet. 2021;397:650–652. doi: 10.1016/S0140-6736(21)00215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tam T., Chief Public Health Officer of Canada From risk to resilience: an equity approach to COVID-19 – the chief public health officer of Canada’s report on the state of public health in Canada 2020. https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html Canada.ca [Internet]. Ottawa; 2020 [cited 2021 Oct 25]. Available from:
- 54.Moriarty T.J., Boczula A.E., Thind E.K., Loreto N., McElhaney J.E. Excess all-cause mortality during the COVID-19 epidemic in Canada. https://rsc-src.ca/en/covid-19-policy-briefing/excess-all-cause-mortality-during-covid-19-epidemic-in-canada Ottawa; 2021 [cited 2021 Oct 25]. Available from:
- 55.Carlberg J. vol. 13. University of Calgary School of Public Policy; 2020. (Vulnerabilities and benefits of megascale agrifood processing facilities in Canada). [Google Scholar]
- 56.Hansson E., Albin M., Rasmussen M., Jakobsson K. Large differences in excess mortality in March-May 2020 by country of birth in Sweden. https://europepmc.org/article/med/32619245 Lakartidningen [Internet]. 2020 Jun 29 [cited 2022 Jan 11];117. Available from: [PubMed]
- 57.Faust J.S., Chen A.J., Nguemeni Tiako M.J., Du C., Li S.X., Krumholz H.M., et al. Leading causes of death among adults aged 25 to 44 years by race and ethnicity in Texas during the COVID-19 pandemic, March to December 2020. JAMA Intern Med. 2022;182:87–90. doi: 10.1001/jamainternmed.2021.6734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.National Advisory Committee on Immunization (NACI) Health Canada; Ottawa: 2021. Guidance on the prioritization of key populations for COVID-19 immunization.https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/guidance-prioritization-key-populations-covid-19-vaccination.html#a34 [Internet] [Google Scholar]
- 59.Reverby S.M. Racism, disease, and vaccine refusal: people of color are dying for access to COVID-19 vaccines. PLOS Biol. 2021;19 doi: 10.1371/journal.pbio.3001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Government of Canada Planning guidance for immunization clinics for COVID-19. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/planning-immunization-clinics-covid-19-vaccines.html#a2.3 vaccines [Internet]. 2021 [cited 2021 Nov 5]. Available from:
- 61.Parmet W.E., Goodman R.A., Farber A. Individual rights versus the public’s health—100 years after Jacobson v. Massachusetts. N Engl J Med. 2005;352:652–654. doi: 10.1056/NEJMp048209. [DOI] [PubMed] [Google Scholar]
- 62.Bunge J. Tyson Foods to require Covid-19 vaccines for all U.S. workers. The Wall Street Journal 2021. https://www.wsj.com/articles/tyson-foods-to-require-covid-19-vaccines-for-all-u-s-workers-11627992022 cited 2021 Oct 15]. Available from:
- 63.Addleman S., Leung V., Asadi L., Sharkawy A., McDonald J. Mitigating airborne transmission of SARS-CoV-2. Can Med Assoc J. 2021;193:E1010–E1011. doi: 10.1503/cmaj.210830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van Dijk M., Rohl E., McCutcheon J., Hoffart K. Vaccinate 2500 new immigrant meat plant employees. https://www.d4ahs.com/cargill [Internet]. Alberta Health Services Design Lab (D4AHS). 2021 [cited 2021 Nov 3]. Available from:
- 65.UFCW Local 401 Cargill workers accept new contract by 71% https://gounion.ca/news/cargill-workers-accept-new-contract-by-71/ [Internet]. 2021 [cited 2022 Jan 11]. Available from:
- 66.Ingram M., Wolf A.M.A., López-Gálvez N.I., Griffin S.C., Beamer P.I. Proposing a social ecological approach to address disparities in occupational exposures and health for low-wage and minority workers employed in small businesses. J Expo Sci Environ Epidemiol. 2021;31:404. doi: 10.1038/s41370-021-00317-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ontario Human Rights Commission . Government of Ontario; 2021. OHRC policy statement on COVID-19 vaccine mandates and proof of vaccine certificates | Ontario Human Rights Commission.http://www.ohrc.on.ca/en/news_centre/ohrc-policy-statement-covid-19-vaccine-mandates-and-proof-vaccine-certificates [cited 2021 Oct 15]. Available from: [Google Scholar]
- 68.Government of Ontario . Ministry of Labour, Training and Skills Development; 2021. Ontario COVID-19 Worker Income Protection Benefit.https://www.ontario.ca/page/covid-19-worker-income-protection-benefit [Google Scholar]
- 69.CanLII. Schuyler . Dr. Nesathurai; 2020. Farms limited v.https://www.canlii.org/en/on/onscdc/doc/2020/2020onsc4711/2020onsc4711.html ONSC 4711 (CanLII) [Internet]. Ontario Superior Court of Justice Divisional Court. 2020 [cited 2021 Oct 15]. Available from: [Google Scholar]