Abstract
Background
Telehealth has many benefits, in routine care and especially during times of epidemics in which restrictions to direct patient/healthcare-provider interaction exist.
Objective
To explore the availability, application, and implementation of telehealth services during the Covid-19 era, designed for the aged population (age 65 and more).
Methods
This systematic review/analysis was conducted by searching the most popular databases including PubMed, Embase, and Web of Science. We included studies that clearly defined any use of telemedicine services in any aspect of healthcare during the COVID-19 pandemic, aimed at the elderly population, published in peer-reviewed journals. We independently assessed search results, extracted the relevant studies, and assessed their quality.
Results
3225 articles were identified after removing duplicates. After reading the full texts of 40 articles, 11 articles were finally included. Among the telehealth services, there were services aimed for triage and control during the outbreak of the COVID-19 pandemic, remote monitoring and treatment, follow-ups online meetings for patients residing in health centers, and application of online services.
Conclusions
Although the elderly population may benefit the most from telehealth services, especially during pandemics and social distancing restrictions, not enough services were developed and implemented to satisfy the needs of this population.
Keywords: telehealth, telemedicine, coronavirus, COVID-19, elderly, old
Introduction
Telehealth is the delivery of healthcare services by healthcare professionals through information and communication technologies (ICT), where distance separates between the participants.1
During the last years, with the impressive development of Internet and communication infrastructure, telehealth has become a convenient and safe method for patients to obtain reliable information and medical consultation.2
Telehealth services can use real-time or store-and-forward techniques,3 and due to the rapid advancement of technology, most people nowadays have the necessary equipment, such smartphones and webcams, to provide direct communication with the healthcare providers.4-5
There are many benefits in using telehealth, especially in routine care and in cases where a direct patient-healthcare provider interaction is not mandatory. Remote care can improve the access to care and reduces the use of health center resources, while reducing the risk of infection transmission.6-7
Another important advantage of telemedicine, beside of being beneficial in keeping both patients and health workers safe, is improving the access to healthcare givers, especially in cases of chronic conditions.8-9 In general, this technology may be for patients an effective and available, thus attractive, option.
Patients are usually interested in using telehealth, but some obstacles are still present, especially for people who are technologically challenged, having low health literacy or operational difficulties, or when technical failures appear.10-12
The difficulties in implementing telehealth solutions are also influenced by financial and medical-legal considerations. In addition, some of the physicians themselves are troubled with technical difficulties, and many issues concerning the decision-making capability in this constellation, and the appropriate standards of the quality, safety, and privacy, that should be maintained in such services.13-18
Telemedicine, a term referring specifically to the remote clinical services, may be beneficial especially at times of epidemic situations and also contributes to increase disease control, clinical case management, and epidemiological research.19
Telemedicine and virtual care can be integrated into the healthcare system as an approach to maximize the efficiency of healthcare delivery.20
It employs real-time interactive visual, textual audio, and data communications to deliver medical care, consultation, diagnosis, transfer of medical data, guidelines, and treatment. Telemedicine and eHealth platforms can be deployed by using telephone, Internet Protocol (IP) over Internet voice call, or video consultations.21
For many years, television systems (such as video conferencing) have been used to provide healthcare consultations and programs for people in different places. Recently, these systems are delivered also to people who are hospitalized or quarantined, enabling minimizing the risk of exposure to other people.22-23
Although telemedicine can start with telephone consults, other computer technologies such as webcam-enabled personal computers, smartphones, and high-speed internet, can be employed to provide healthcare to patients.24-25
Telemedicine is adopted either synchronous or asynchronous. Synchronous telemedicine platforms support both patients and physician to establish real-time sessions (video or phone) while exchanging vital data simultaneously.26
Asynchronous consultation may be most suitable when adopting in non-urgent cases or in routine outpatient follow-ups. Thus, a patient can send initial medical request and follow-up photos and videos attached to a description of how they are feeling or recovering. In the next step, the physician will review the documents, and the patients will be messaged electronically. A phone call may be set up or in-person visit can be re-scheduled, if the case is urgent.24
Since December 2019, the world has been facing an epidemic threat to global health, caused by a novel coronavirus, “SARS-CoV-2”.27 On 11 February 2020, the World Health Organization officially named the novel coronavirus disease as “COVID-19,” and in March 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) a pandemic.28
Elderly people and those who have underlying medical conditions (such as cardiac disease, hypertension, or diabetes) are at greater risk of developing an intensive and severe form of the disease.29-33
On the other hand, people who are not currently infected with COVID-19, but are being at greater risk of “catching” the infection (e.g., elderly people and people with underlying diseases), should be able to get their continuous routine healthcare without being at a risk due to exposure to others.34
One of the main means in controlling the transmission of Covid-19 is making “social distancing,” achieved by the reduction of direct contact between people.34-35 In addition, travel restrictions have been imposed, and most cities worldwide have been quarantined for some period of time.36
Although the ultimate solution for COVID-19 is still vague but will probably be multidimensional, one of the effective ways will be the use of technologies such as telemedicine to ensure optimal and safe healthcare delivery while minimizing the risk of exposure to other patients, who may be infected.19
COVID-19 has catalyzed rapid use of ICT (Information communication Technology) such as telemedicine and virtual software platforms to deliver healthcare at a distance.37
To enable patients’ access to medical care, many countries have revised regulations to allow hospitals and health centers to adopt telemedicine.38-39
Telehealth had become an important tool for the general population, healthcare providers, and patients with COVID-19, enabling patients to maintain in real-time contact with healthcare providers for advice on their health problems, especially when people are in quarantine. Remote medical treatment, using telemedicine services, can promote the patients’ access to professional medical advice without having to wait for a long period of time. It reduces unnecessary visits to clinics and hospitals, in ordinary times and especially during the Covid-19 outbreak, and even lessen anxiety among patients.40-43
By minimizing in-person visits and reducing face-to-face contact between physicians and patients, the use of virtual care solutions can decrease the transmission of the virus and also protect medical practitioners from infection.44
Synchronous and asynchronous telemedicine and eHealth platforms were implemented in providing clinical services during the COVID-19 pandemic. In order to reduce exposure, telephone and online surveys are employed as an important method to prevent outpatients from infection exposure. By using synchronous teleconsultation, in the first stage, the physician conducts a preliminary screening of patient digitally and gives suggestions to continue to stay home or to visit the hospital.45
Telemedicine could also be practiced within hospital wards; for instance, to help attending nurses in intensive care units treating COVID-19 patients in the rehabilitation program guided by physiotherapists.43 Patients discharged from the hospital can also be followed up through telemedicine as it provides a medium to easily monitor patients.41-43
In their scoping review on the use of telehealth during the COVID-19 pandemic, Doraiswamy et al.46 have found that 12.9% of the articles focused on the use of telehealth for medicine in general with no reference to any specialty. The majority of the remaining articles focused on telehealth use in the following medical specialties: internal medicine (23%), preventive medicine (10.3%), psychiatry (7.7%), surgery (6.6%), neurology (6.1%), otolaryngology (4.2%), and dermatology (4.2%). The top five subspecialties deploying telehealth were endocrinology (5.5%), oncology (4.6%), geriatrics (4.2%), cardiovascular (3.7%), and orthopedics (1.8%).
In the context of the COVID-19 pandemic, telehealth has been used broadly as an aid to the active management of patients with COVID-19, for surveillance, triage, and diagnosis; treatment including e-prescriptions; follow-up care; and rehabilitation.
Telehealth has been also complemented by the use of wearable devices and self-care equipment, such as glucometers, handheld blood pressure monitors, pulse oximeters, and digital stethoscopes.47
With the current COVID-19 pandemic, aging adults are one of the highest risk populations for virus contraction, and are at a higher risk for severe complications and death relative to the rest of the population.48
In the US, the policy changes reflect the severity of the current public health emergency and importance of protecting vulnerable populations, such as the elderly. As a means of decreasing transmission between patients and providers, the CDC (Center for disease Control) currently encourages ambulatory care settings as enable alternatives to face-to-face triage and visits. As a result, the current waiver allows reimbursement for visits via telehealth from a variety of providers, including physicians, nurse practitioners, clinical psychologists, dieticians, and licensed clinical social workers. Furthermore, the Health Insurance Portability and Accountability Act (HIPAA) restrictions have been eased to allow for use of everyday communication technologies such as FaceTime, Zoom, or Skype.49
Telemedicine visits have been reported even in cases in which the elderly patients were residents of a facility, and then RN assessment helped to supplement the physical exam.
In 2019, Medicare began reimbursing for other limited telehealth applications, in addition to full telehealth visits, including virtual check-ins (short telephone check-ins initiated by the patient), e-visits (communication via online patient portal between patient and provider), and the possibility of sending captured videos or images to the provider as well.50
Concerning the elderly population, clearly, telehealth has the potential to increase equality in care, especially in times such as the Covid-19 era, but unfortunately, it can also further exacerbate disparities.51-54
Furthermore, as the healthcare system becomes more and more virtual, there is a risk of increasing disparities among populations who have limited access to the resources (such as internet) essential for the effective use of telemedicine (including ethnic minorities, patients living in rural areas, patients with limited English proficiency, with low literacy, or with low income).55
As well stated by Ortega et al.,53 paradoxically, “populations lacking technological access to telemedicine services, tend to be from the same underserved populations that have worse health outcomes and would benefit most from ongoing telemedicine-enabled care.”52,56
This lack of access to healthcare is further reflected in the significant disparities aggravated by the COVID-19 pandemic.57 Kruse et al.58 reported that age-related barriers exist due to lack of exposure to the new technology and patients’ lack of training and claimed that the technology acceptance gap among older patients is consistent with the patients’ preferences for face-to-face care.
Nevertheless, there is a misconception that older people do not have internet or network connection, which serves as a platform for telehealth solutions. In fact, most of them do have such accessibility, however, they find it difficult to use. Current data indicate that most older adults (70%) have and utilize a computer, smartphone, or tablet with internet access at home. However, regarding the use of telehealth, there is limited reach among the elderly population.59
It should be noted that most of the studies dealing with telemedicine during Covid-19 were case studies. In addition, most of the systematic reviews or meta-analyses done so far on COVID-19 concerned the use of telemedicine of the entire population, and as far as is known did not deal with this specific population, which needs these services the most.
Therefore, in this systematic review, we explored the availability, application, and implementation of telehealth services during the Covid-19 pandemic designed for the aged population (age 65 and more), who needed them the most during this challenging period.
Methods
Study design
This systematic review was conducted based on systematic reviews and meta-analyses (PRISMA) guidelines.
(Available at http://www.prisma-statement.org/).60-61
In face of the importance and urgent attention of the issue investigated in our study, and the limited available evidence on the topic, while the Covid-19 pandemic is still extant, the protocol of this systematic review was not registered in the appropriate site.
Search strategy and data sources
A comprehensive search was performed by a specialized experienced librarian in the following electronic databases: PubMed, Embase, and Web of Science, to identify relevant and published studies.
The search was conducted on Titles and Abstracts.
We made no restrictions publication status, but we included only studies written in English. The following search was used:
(“COVID19”, OR “COVID-19″, “COVID 19”, “Coronavirus”, “Novel coronavirus”, “Novel CoV”, “2019-nCoV”, “2019-CoV”, “Wuhan coronavirus”, “SARS-CoV-2″, “SARS2”, “SARS-Related”, “SARS-Associated”, “Severe Acute Respiratory Syndrome”, “Middle East respiratory syndrome”, “MERS”, “Novel coronavirus pneumonia”) AND (“Tele”, OR “Telemedicine”, “Tele-medicine”, “Telehealth”, “Tele-health”, “Telecare”, “Mobile Health”, “mHealth”, “Electronic health”, “ehealth”, ‘e-health”, “Internet”, “Online consultation”, “Online Reference Service”, “Network Information Reference”, “Mobile Application”, “Mobile App”, “Mobile phone”, “Telephone”, “Home telehealth services”, “Medical informatics”, “Technology”), AND (“Elderly” OR “Aged population”, “Aging”, “Age> 65″, “Senior”, “Old”, “Retried”, “Older adults”, “Chronic”, “Geriatric”, “Outpatients”).
Lastly, we also thoroughly reviewed the selected articles’ references (reference by reference), in order to identify additional studies not found during the preliminary searches.
Eligibility criteria
All studies reporting and evaluating the role of telehealth services aimed for the elderly population (age 65 years and more) during the COVID-19 were included in our analysis.
The word “chronic” was added to the initial search since chronic diseases are usually more common in the elderly population, but during the data extraction we included only articles relating particularly to the elderly population.
Studies were included if they clearly described any kind of telehealth service or application aimed for the elderly population (age 65 and more), during the COVID-19 era (since December 2019), till the date of the data extraction (27.12.2020).
As cited by Shaw1, “Telehealth is the use of electronic communications to provide and deliver a host of health-related information and health care services, including, but not limited to physical therapy-related information and services, over large and small distances. Telehealth encompasses a variety of health care and health promotion activities, including, but not limited to, education, advice, reminders, interventions, and monitoring of interventions.”
Telehealth applications include live (synchronous) videoconferencing [a two-way audiovisual link between a patient and a care provider]; store-and-forward (asynchronous) videoconferencing [transmission of a recorded health history to a health practitioner, usually a specialist]; remote patient monitoring (RPM) [the use of connected electronic tools to record personal health and medical data in one location for review by a provider in another location, usually at a different time]; and mobile health (mHealth) [health care and public health information provided through mobile devices].
The term “health information technology” (health IT) is a broad category of solutions that includes technologies to store, share, and analyze health information. Telemedicine technology is a subset of health IT that refers specifically to remote clinical services.
The analysis included all studies in English representing any sorts of use of telehealth tools in all aspects and levels of healthcare (primary, secondary, or tertiary), aimed for providing clinical and consultation services, assessment of symptoms, diagnosis, and triage of patients, either concerning Covid-19 symptoms or not, and that were purposed and used specifically for the elderly population, in this time period.
Studies reporting methods which are not based on telemedicine technology, duplicate publications, review or opinion articles, and letters to the editor were excluded, as well as studies with incomplete information.
Study selection and data extraction
Two authors/reviewers (MH and AGE) who performed the literature search also independently checked and implemented the inclusion and exclusion criteria and screened the studies, based initially on the titles and abstracts of the studies.
The special website Rayyan was used, and any disagreements were solved after a conversation and discussion between the authors. The authors screened at the first step, all titles and abstracts with the pre-defined criteria, labeled and categorized the articles into three groups (“eligible,” “not eligible,” and “unclear”/“maybe”).
In the second step, the authors reviewed and examined the full texts of the potentially eligible or “unclear” studies that did not have enough details in their abstracts, to ensure eligibility and identify for final inclusion. All reasons for exclusion of ineligible studies were documented, and the process of study selection was handled and processed using the PRISMA flow diagram.
Finally, data was extracted from all papers/studies which met the eligibility criteria for the review.
The following data were extracted and analyzed: (1) Basic information: title, first author, publication year, country, study design; (2) participants: baseline characteristics, sample size; (3) results: type of telehealth service used for different contents of consultation (e.g., symptoms, diagnosis, therapy and prevention, or policy), and eventually the key outputs of studies and effects of telehealth.
Quality assessment
Two reviewers (MH and AGE) assessed independently the quality of reports and studies using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool.62
According to this assessment, we formed a special table describing the “Summary of Findings,” showing the overall grading of body of evidence for each outcome described in each study.
According to the methodology evaluation tool recommended by the Agency for Healthcare Research and Quality, the quality is downgraded according to five considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) and upgraded according to three considerations (large magnitude of effect, dose-response relation, and plausible confounders or biases). Finally, the quality of evidence is classified as high, moderate, low, or very low, reflecting the extent to which we are sure about the correctness of the effect estimates.63
Evidence synthesis
In order to analyze and synthesize the results of the included studies, we conducted a narrative synthesis of overall evidence by comparing the data.
We first conducted a preliminary synthesis and determined the evaluation mechanisms and tools in each study, then we explored the relationships within and between studies, and finally we determined the robustness of the synthesis.64
Data of the included studies was described and presented in the text and tables. The authors met frequently and discussed the disagreements, in order to reach consensus on the findings.
The evaluation tools for each service described in the selected studies were examined and presented in a separate Table.
Results
Search results
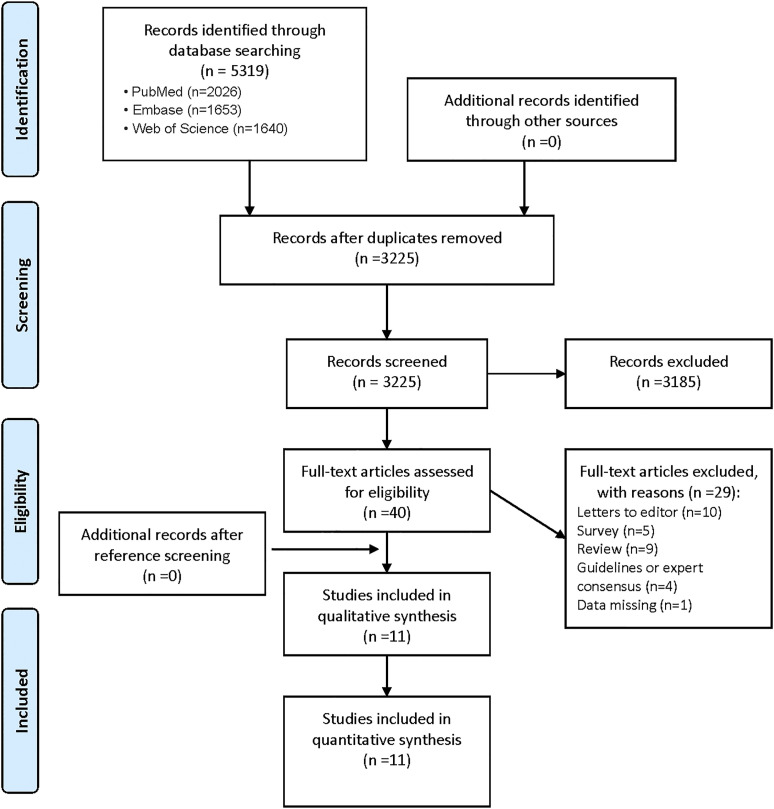
The details on the literature search and the selection are shown in Figure 1.
Figure 1.
PRISMA 2009 Flow Diagram.
A total of 5319 articles were identified in the database, of which 3225 articles were left after deleting the duplicates.
Following the removal of duplicate studies and screening titles and abstracts of the different study reports, we finally appraised 40 relevant studies in full text.
11 studies were finally included after reviewing the full texts.65-75 No additional suitable studies were found after reference screening.
Characteristics of the included studies
In this meta-analysis, we analyzed the articles in two ways: one, an analysis of the various components of the studies, and the other, a characterization of the telemedicine assessment, focusing on the question of whether the assessment was made, and the results of the evaluation studies.
Characteristics of the included studies are demonstrated in Table 1.
Table 1.
Characteristics of the included studies.
| Author/Date | Country | Design of study | Type of telehealth | Period | Key outputs/Contents of consultation | Effects/conclusions |
|---|---|---|---|---|---|---|
| Yi, X et al. Aug 202065 community nursing services during the COVID-19 pandemic: The Singapore experience | Singapore | Descriptive/Case study | Community nursing team for old adults [4038 residents] | 7 Apr 2020 till Jun 2020 | • Teleconsultation | • Community nurses play a key role in health and social care services integration |
| • Home visits with essential needs | • Their efforts in empowering older persons on self-care proved to be beneficial during the pandemic | |||||
| • Virtual outreach, community outreach, and screening activities | ||||||
| • Practicing beyond the community: COVID-19 patients were admitted to appropriate facilities | • Community nurses moved smoothly from FTF consults toward teleconsultations and kept their services accessible during the pandemic | |||||
| Tan, Laurence Lc et al. Sep 202066 using telemedicine for outpatient geriatric care during the novel coronavirus outbreak: Experience from the first 15 patients | Singapore | Descriptive/Case study | Telemedicine specialist outpatient clinic (Tele-SOC) unit: run by 1 geriatrician and assisted by a geriatric nurse [15 patients] | 7 Apr 2020 till Jun 2020 | Video conferencing application | • Tele-SOC provided a good alternative to physical consultations for selected groups of the geriatric population in order to minimize their exposure to virus transmission |
| • All patients needed caregivers to set up the video conferencing application to participate in the Tele-SOC consultations | ||||||
| • Communication was deemed to be satisfactory by majority of the patients and caregivers | ||||||
| Fatyga, E et al. May 202067 the coronavirus disease 2019 pandemic: Telemedicine in elderly patients with type 2 diabetes | Poland | Cross-sectional study | Telephone-based medical advice in the Silesia region in elderly patients with type 2 diabetes [ 86 patients] | 16 Mar 2020 to 31 Mar 2020 | • Telephone -based consultation | • The antidiabetic drug or its dose were modified using e-prescriptions in 22 seniors (26%) due to hyper or hypoglycemia |
| • None of the diabetics required urgent, additional contact with physicians due to comorbidities | ||||||
| • The subjects declared no symptoms typical of COVID-19, but everyone was following the individual rules of protection against SARS-CoV-2 infection | ||||||
| • The advice was focused on glycemic control, emotional status, and behavioral change | • Most of them felt anxiety because of the current situation and the risk of being infected with SARS-CoV−2 | |||||
| • Telemedicine can improve glycemic control and reduce anxiety in patients with type 2 diabetes during the COVID -19 outbreak | ||||||
| Cilia, R et al. May 202068 telemedicine for parkinsonism: A two-step model based on the COVID-19 experience in Milan, Italy | Milan, Italy | Descriptive/Case study | Telephone assistance and video consultations in patients with Parkinson’s disease [525 patients] | Mar 12th to 14 May 2020 | 1st step—remote telenursing assistance service (“ParkinsonCare”) | • The remote telenursing assistance was positioned as a new service outside the regular care facilities and was made available free of charge to patients |
| • Triage protocols were in place for specific common medical issues allowing for standardized assessment of the problem plus delivery of tailored advice | ||||||
| 2nd step—regulation-compliant video consultations with experienced neurologists | • The remote consultation service was operated by case managers, who were not originally part of the patient’s care team | |||||
| • The authors propose a two-pronged model to optimize the management of patients with parkinsonism | ||||||
| Ben Hassen H, et al. Jun 202070 a home hospitalization system based on the internet of things, fog computing, and cloud computing | Tunisia | Cross-sectional study | Internet of things (IoT), fog computing, and cloud computing [5 patients] | 2020 | Home hospitalization system [ especially for the elderly] based on the internet of things (IoT), fog computing, and cloud computing | • The system allows patients to recover and receive treatment in their homes and among their families, where the patients’ health and the environmental factors of the hospitalization rooms are monitored periodically, through a vital signs sensing unit and environmental sensing units that are installed in the hospitalization rooms and mobile applications developed for this purpose |
| • This system also enables doctors, patients, and their family to manage and monitor hospitalization operations through their mobile applications | ||||||
| • This system has received very good acceptance by patients and doctors | ||||||
| Akgül, A May 202069 online counseling for new onset symptoms/signs in 65+ patients with lympho-venous diseases in the era of COVID-19 | Istanbul, TURKEY | Descriptive/Case study | WhatsApp and skype online platforms [22 patients] | 22 Mar 2020 to 5 Apr 2020 | 22 follow-up cases (mean age 68) of potential COVID-19 infections for new onset symptoms/signs in 65+ patients with lymphedema/venous disease | • The author performed appropriate recommendations for admission of the patients as well as their families to pandemic hospitals where available |
| • Followed-up patients who were treated for COVID-19 also received post-discharged advice for cardiovascular system | ||||||
| Motolese, F et al. Oct 202071 Parkinson’s disease remote patient monitoring during the COVID-19 lockdown | Italy | Prospective cohort study | Phone calls and EncephaLog HomeTM smartphone application for PD (Parkinson’s disease) patients.[54 patients] | Mar to May 2020 | • 54 non-demented PD patients who were supposed to attend the outpatient clinic were recruited | • Majority of patients were compliant and satisfied by the provided monitoring program |
| • They were provided with a smartphone application providing indicators of gait, tapping, tremor, memory, and executive functions | • some of the application outcomes were statistically correlated to clinical parameters, but further validation is required | |||||
| • Questionnaires exploring non-motor symptoms and quality of life were administered through phone calls | • Available technologies can be used for telemedicine, even in a population with limited skills and in a critical situation like a pandemic—which could considerably affect the health of neurological patients directly or indirectly | |||||
| Van Dijk, SDM et al. May 202072 (Vi)-rushed into online group schema therapy-based day-treatment for older adults by the COVID-19 outbreak in the Netherlands | The Netherlands | Prospective cohort study | Online therapy program [using “webex”] for older adults with chronic affective disorders and personality problems [4 patients] | 20-week period from Nov 2019 till Apr 2020 | • Four patients, aged 64−70 years, started our online program | • Therapists were positive about the online capabilities and resilience of patients to adapt to the new situation |
| • The usual treatment (given twice weekly in an open group) was transformed into an online program using “webex” with minimal changes | • Prejudices on limited effectiveness of online psychotherapy were counteracted | |||||
| • Sending homework by email and mail seems to facilitate therapy adherence | ||||||
| Truong, J et al. Oct 202073 From the COVID-19 epicenter: Using telemedicine to serve the needs of the geriatric population | New York USA | Retrospective review of patients 65 and older | The patients were evaluated remotely by a ED provider on a telemedicine platform a desktop or mobile phone (TH) during the local pandemic surge, in northern Manhattan/NY [ 140 charts] | From Mar 1, to 30 Apr 2020 | • Overall, 20% of patients in the cohort were advised to seek emergent care | • Telemedicine (TH) was used as a tool to shift non-emergent care from overburdened emergency departments and to provide routine and urgent healthcare to the community who were directed to self-isolate and often fearful of seeking care during the pandemic |
| • There was significant growth in use of TH (telehealth) from pre- pandemic period | • Geriatric telemedicine showed an exponential growth during the pandemic | |||||
| • TH program efforts to promote its use to redirect patients away from the ED were successful | ||||||
| Patel, S et al. Sep 202074 ordinary care in extraordinary times | Ireland | Prospective cohort study | Remote video consultations by using mobile tablet technology. [657 residents of 16 nursing homes and other long-stay facilities] | From Apr 2020 [still going] | • Aiming to facilitate routine psychiatric and medical care in the local nursing homes and long-stay facilities in the northwest of Ireland | • Nursing homes and other long-stay facilities with their vulnerable older residents pose a significant challenge in providing routine care with the current necessary restrictions in place due to COVID-19 |
| • It is imperative that such care continues and the installation of mobile technology within these facilities provides a solution to these challenges | ||||||
| Weiss, Erica F et al. Nov 202075 telehealth for the cognitively impaired older adults and their caregivers: Lessons from a coordinated approach | NY, USA | Descriptive/Case study | Video visits [85 patients] | 18 Mar–18 May 2020 | • To effectively address the needs of the cognitively impaired older adults as well as their caregivers, a model was adopted and provided collaborative tele medical care to new and established patients with cognitive issues | • The CCARRE (coordinated care at risk/Remote elderly’ program) team included a bilingual/bicultural social worker and a neurologist conducting the telehealth visit with a patient and the identified healthcare proxy or caregiver on record |
| • 85 patients were evaluated as part of CCARRE during this period | ||||||
| • The coordinated team transition to telehealth, led to new insights into areas of urgent need for the diverse, cognitively impaired population and their caregivers | ||||||
| • The “coordinated care at risk/Remote elderly” program (CCARRE)- demonstrates a unique approach to reaching the culturally diverse and vulnerable population using telehealth | • The CCARRE model provided access to the healthcare system during a time when it was challenging to make contact with the primary care physicians | |||||
| • The authors support the use of telehealth as a complementary tool to in office assessments for their most vulnerable populations |
The included studies were published in various international peer-review journals between May 2020 and November 2020.
The 11 included studies were carried out in eight countries: Singapore (n = 2), USA (n = 2), Italy (n = 2), Poland (n = 1), Tunisia (n = 1), Turkey (n = 1), the Netherlands (n = 1), and Italy (n = 1).
Based on the study design, five studies were descriptive/case studies, two were cross-sectional, three were prospective cohorts (one of them is still ongoing), and one was a retrospective review.
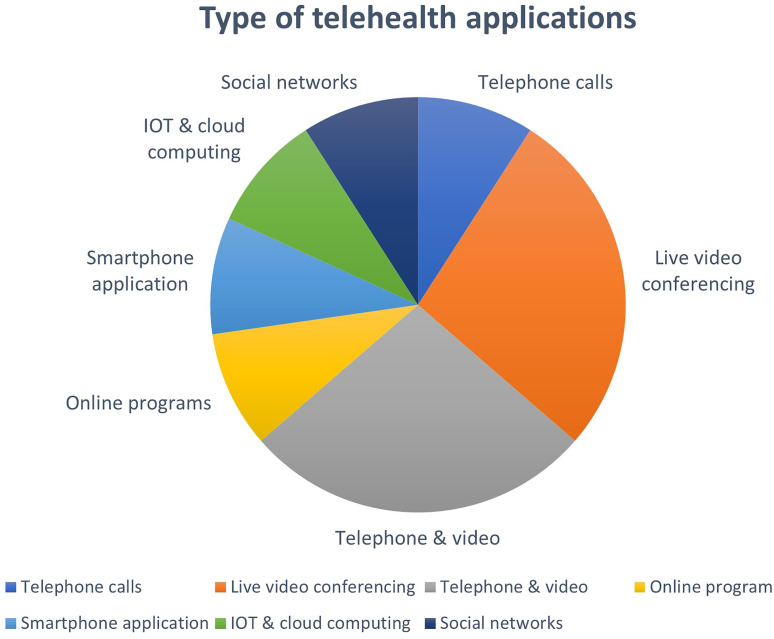
In the included studies, different types of telehealth applications were applied, including telephone calls (n = 1), live video conferencing (n = 3), both telephone and video (n = 3), online program (n = 1), smartphone application (n = 1), IoT (internet of things) and cloud computing (n = 1), and even “regular” social networks (n = 1). It is displayed in Figure 2.
Figure 2.
Types of telehealth applications used.
The contents of the services included consultations for immediate/acute symptoms, therapy, and prevention, for Covid-19-related issues, or for routine health maintenance issues.
Among the telehealth services for the elderly patients, there were services aimed for control and triage during the outbreak of the COVID-19 pandemic, distance monitoring and treatment, follow-up online visits for patients residing in health centers, and operation of online services.
One study described the remote evaluation of patients by an ED (emergency department) provider on a telemedicine platform on a desktop or mobile phone during the local pandemic surge, in northern Manhattan/NYC.73
Most services were mainly related for the treatment and surveillance of chronic conditions such as Parkinson’s disease,68,71 diabetes,67 chronic affective disorder,72 psychiatric mental care,74 cognitively impaired old adults,75 lympho-venous disease,69 and consultations for the geriatric population given at nursery homes or home hospitalization by nurses and physicians.65-66
The evaluation tools for each service described in the selected studies were examined and described in Table 2.
Table 2.
Evaluation tools of the telemedicine services described in the studies.
| Author/Date | Name of study | Design of study | Evaluation tool |
|---|---|---|---|
| Yi, X et al. Aug 202065 | Community nursing services during the COVID-19 pandemic: The Singapore experience | Descriptive/Case study | • An online platform was created to assess the team’s readiness to tackle the COVID-19 outbreak and seek suggestions to overcome the challenges in view of the emerging situation and influx of information on the spread of COVID-19 |
| • The survey helped the senior management team to quickly evaluate the frontline community nurses’ responses to the pandemic as well as adjust the preparation work needed | |||
| • The survey showed that approximately 90% of the community nurses were confident in handling the outbreak situation | |||
| Tan, Laurence Lc et al. Sep 202066 | Using telemedicine for outpatient geriatric care during the novel coronavirus outbreak: Experience from the first 15 patients | Descriptive/Case study | • The authors collected demographics and diagnoses of the first 15 patients who were seen by Tele-SOC [telemedicine specialist outpatient clinic] over a 2-week period |
| • Feedback was given by the patients or their caregivers (if patients were unable to provide due to a lack of mental capacity) via phone calls using a structured interview format based on a questionnaire created by Tele-SOC. | |||
| • The same set of questionnaires with variations in 4 questions was completed by the healthcare professionals | |||
| Fatyga, E et al. May 202067 | The coronavirus disease 2019 pandemic: Telemedicine in elderly patients with type 2 diabetes | Cross-sectional study | • Semi-structured telephone interview was used in all patients, and this was based on the 5 topic areas: Current glycemic control, comorbidities, provision of medicines and food products, compliance with individual protection against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, and anxiety associated with the current pandemic |
| Cilia, R et al. 20 May2068 | Telemedicine for parkinsonism: A two-step model based on the COVID-19 experience in Milan, Italy | Descriptive/Case study | • Over two-thirds of patients/caregivers (70%) provided positive feedback, comments were not provided in 28% of cases, and 2% were disappointed by the lack of home-care nursing |
| • Based on their successful experience during the COVID-19 crisis, the authors propose a two-pronged model to optimize the management of patients with parkinsonism | |||
| • The radically new element that the authors introduce here consists of a remote consultation service by case managers, who were not originally part of the patient’s care team | |||
| Ben Hassen H, et al. Jun 202070 | A home hospitalization system based on the internet of things, fog computing, and cloud computing | Cross-sectional study | • To evaluate the home hospitalization system proposed in this paper, the authors have used the system usability scale (SUS), as this scale provides a fast and reliable tool for measuring ease of use and allows the evaluation of a variety of services and products, including mobile devices, mobile applications, and websites |
| • To detect most usability problems, it is acceptable to evaluate with five users; based on this, five hospitalized patients between the ages of 45 and 61 years and five doctors were selected to conduct usability testing | |||
| Akgül, A May 202069 | Online counseling for new onset symptoms/signs in 65+ patients with lympho-venous diseases in the era of COVID-19 | Descriptive/Case study | • No evaluation exists |
| • According to the author—he performed “appropriate” recommendations for admission of the patients as well as their families to pandemic hospitals where available. Followed-up patients who were treated for COVID-19 also received post-discharged advice for cardiovascular system | |||
| Motolese, F et al. October 202071 | Parkinson’s disease remote patient monitoring during the COVID-19 lockdown | Prospective cohort study | • The smartphone application EncephaLog Home™ was validated |
| • Subjects were phone-checked weekly throughout a 3-week period for compliance, upcoming issues, and for an evaluation questionnaire at the end of the observation period. The latter was sent to patients by email and mailed back to the physician via email or regular mail | |||
| • The analysis of data coming from the final evaluation questionnaire showed that 37 (84%) subjects evaluated their experience as “satisfying” (16, 36.4%) or “very satisfying” (21, 48%) and 21 cases (48%) perceived themselves as “safer” (17, 39.5%) or “much safe” (4, 9.3%) thanks to the RPM (remote patient monitoring). However, 17 (37.2%) required “occasional” support and 9 (21%) “frequent to regular” support by the caregiver. Similarly, a minority (11, 26%) perceived the app as difficult | |||
| Van Dijk, SDM et al. May 202072 | (Vi)-rushed into online group schema therapy based day-treatment for older adults by the COVID-19 outbreak in the Netherlands | Prospective cohort study | • Treatment adherence was 100%. Patients felt being taken seriously |
| • The psychomotor therapy turned out to be much easier than expected, active movements (gymnastics), relaxation, and mindful exercises (e.g., tai chi) were well received by the patients | |||
| Truong, J et al. Oct 202073 | From the COVID-19 epicenter: Using telemedicine to serve the needs of the geriatric population | Retrospective review of patients 65 and older | • The authors conducted a retrospective chart review of patients 65 and older who were evaluated remotely by an ED provider on a telemedicine platform |
| • Chart extraction methods were developed and performed by 5 emergency physicians | |||
| • Categories and characteristics were defined in advance and included demographics, technical limitations, referral to ED, and death occurring during the time of the chart review | |||
| Patel, S et al. Sep 202074 | Ordinary care in extraordinary times | Prospective cohort study | • There is a future evaluation |
| • This project will be evaluated to assess the impact and feasibility of using mobile tablets in long-stay facilities during the COVID-19 crisis. All patients residing at 1 of the 16 long-stay facilities and undergoing a psychiatry of old age assessment using the mobile tablets will be recruited for this study | |||
| • A brief patient/keyworker and assessing staff satisfaction survey will be offered at the end of each consultation to assess the impact of the video consultations and evaluation of the service | |||
| Weiss, Erica F et al. Nov 202075 | Telehealth for the cognitively impaired older adult and their caregivers: Lessons from a coordinated approach | Descriptive/Case study | • Feedback from patient, caregiver, and primary care providers were informally solicited |
| • Referrals to community-based organizations and clinical trials were made, as appropriated |
Quality assessment
Our systematic review included 11 studies. The quality of included studies was very poor: Most studies (9 out of 11) scored 5 or less out of 11 in the evaluation by the AHRQ [Agency for Healthcare Research and Quality] tool. Only two studies were scored above 7 (Table 3).
Table 3.
Qualitative assessment/risk of bias of the studies.
| The numbers 1 to 11 refer to the items of the tool |
| 1. Defining the source of information (survey, record review) |
| 2. Listing the inclusion and exclusion criteria for exposed and unexposed subjects or referring to previous publications |
| 3. Indicate time period used for identifying patients |
| 4. Indicating whether the subjects were recruited consecutively (if not population-based) |
| 5. Indicating if evaluators of subjective components of the study were masked from the participants |
| 6. Description of any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) |
| 7. Explaining any exclusions of patients from the analysis |
| 8. Description how confounding was assessed and/or controlled |
| 9. If applicable, explaining how missing data were handled in the analysis |
| 10. Summarizing patient response rates and completeness of data collection |
| 11. Clarification of the expected follow-up (if any), and the percentage of patients with incomplete data or follow-up |
Discussion
In this systematic review, we aimed to explore the availability and implementation of telehealth services designed for the aged population (age 65 and more) during the Covid-19 outbreak.
Prior findings
COVID-19 is an infectious disease that has led to a pandemic and influenced the lives of many people throughout the world. The mode of spread of this virus is by person-to-person transmission through respiratory droplets transfer. The best preventive strategy, nowadays, is to avoid being exposed to the virus, at least until the COVID-19 vaccines are available worldwide.76
Several strategies have been suggested and implemented for infection prevention and control of the pandemic, including wearing of face masks, keeping social distancing, and more.77 As mentioned, elderly people and those with underlying medical problems are more susceptible to develop a severe and intensive form of the Covid-19 disease.21-25
In order to reduce the number of people who obtain unnecessary face-to-face healthcare services, patients can be contacted by healthcare personnel through telecommunication tools for assessment and care. It is therefore of great importance to examine studies of telemedicine services aimed for the elderly population.
Several meta-analyses and systematic reviews have been reported recently concerning the role of telemedicine and its application among the general population during the coronavirus epidemics.40,78-79 We wanted to find out which telehealth solutions were developed and implemented for the elderly population during this time.
Even before the COVID-19 pandemic, older adults with complex medical disease had a limited access to healthcare.80-81 Older people with chronic health conditions were affected not only by the scaled-down community services, but also by the disruption of acute-care services in medical institutions. These included early discharges from hospitals to continue care at home, rescheduling non-urgent elective procedures, and outpatient appointments.69
Several studies found that using telemedicine has many benefits. They offer an efficient and safe way for the people to consult healthcare professionals about the symptoms in various health conditions and diseases (including infectious diseases), treatment and prevention modalities, services aimed for public health issues24, and also psychological, supportive, and other issues of utmost concern to the patients.54,82
Phone calls and digital health consultations were described as able to facilitate screening or even giving treatment to patients from a distance, without making face-to-face visits, and also succeeded in improving the decision-making processes among healthcare professionals in ambulatory and non-ambulatory/urgent settings.82
Several studies found that poor access to healthcare may lead to higher mortality rates compared with patients with frequent follow-up visits.83-84 As reported by Fung et al.:85 “the Covid-19 pandemic further exacerbated the access-to-care problem due to reduced clinic visits, transportation restrictions, and other societal measures to mitigate the pandemic.”
In addition, among older populations, a mental and physical health deterioration may be caused due to lack of sufficient social interaction and physical activity during the COVID-19 pandemic.86
Nowadays, clinicians are trying to find more and more ways and channels to deliver an effective and accessible virtual healthcare for the older population, while keeping the regulations made for slowing the spread of the disease.85,87,88
Studies indicate the complexity of using telemedicine for older people. They reveal that there is a misconception about the accessibility to it, the preferences, and the technological capabilities of this population.88-91 This is a misleading assumption because many older people do have access to the Internet. The obstacle is not necessarily the accessibility, but a low ability to use telemedicine, lack of literacy, lack of assistance from others, and also physical and cognitive disabilities.54
The elderly population may be less experienced with the advanced technology and may also have aging-related obstacles to using that technology,89,92-93 as well as barriers in patient confidence.87-89,93-94
Indeed, a recent study estimated that “38% of Medicare beneficiaries were unready to engage in home telehealth.”91 Other studies showed that older adults and their families even expressed concern regarding the use of home telemedicine technology.88-92,95-96
However, many older patients can effectively engage in telehealth, when given the opportunity,89,96-100 especially when convenience is a primary consideration.101 Several studies also described a successful experience for older adults in cases in which special equipment was provided and installed, enabling them to experience home telehealth services.96-98,100-102
Our findings
Our study confirmed our primary hypothesis:
Although older patients may benefit the most from using home telehealth visits, which improve their access to care, especially in the Covid-19 era, in which the necessity of such solutions was undoubtedly proved, still, paradoxically, there are not enough telehealth solutions addressed and aimed at this special population, and it seems that not enough efforts were made to satisfy this purpose.
In addition, it can be said that the evaluation tools conducted in some of the studies used different methodological methods so that it is difficult to compare them. Most of them were not based on theoretical models, and some measured the impact of telemedicine use in the short term rather than the long term. Also, most assessment studies lack reference and adaptation to the different age groups within the groups of the elderly.
Implications and recommendations
In our analysis, we have showed that, although the elderly population may benefit the most from telehealth services, especially during a pandemic and social distancing restrictions, still, not enough services were developed and implemented directly to satisfy the needs of this population.
One of the main reasons for this is the common assumption that older people do not have access to Internet use. Compared to this approach, studies have found that telemedicine and virtual care are the future of healthcare. It offers the elderly population an efficient and safe tool, consulting healthcare professionals from a distance, about the symptoms of acute illnesses, and about managing and treating chronic conditions, and many other issues. We believe that telehealth solutions will continue to exist and reveal their diverse benefits long after the current pandemic has passed.
It is important to emphasize that telehealth enables patients to consult with the healthcare providers whenever they need to—usually from their homes, without having to travel for long distances, or to wait for a long time, wasting time and money. It enables accessing medical information conveniently and quickly, while reducing the risk of being exposed to infections.
Among the most significant benefits of telehealth technologies will be the ways in which they will enable healthcare providers to effectively address and treat chronic diseases, which are one of the major health problems nowadays, and the largest cause of death. Patients with chronic illnesses, who usually belong to the elderly population, can receive quality care easily from their homes, without having to travel and wait for an in-person visit.
Telemedicine has become an essential aspect of healthcare across all populations but has particularly significant implications for the care of elderly individuals. Beyond this global pandemic, future telehealth policy should consider the benefits of improved access to care for those living with frailty, immobility, dementia, mental health needs, and/or chronic disease states.
Many older adults may have trouble accessing telemedical services. Telephone visits may improve access for the some of them, who are inexperienced with technology or have visual impairment, but phone visits are suboptimal for care that requires visual assessment. Policy makers should recognize and bridge this digital divide.
In order to retain the benefits of telemedicine, additional initiatives and evaluation studies must be put in place to address the challenges and the barriers that elderly patients are experiencing and facing in accessing these services. Nevertheless, some of the studies described in our analysis showed that despite the apparent challenges, when given the opportunity, many older patients can, surprisingly, can use telehealth in an effective way.
Healthcare providers can contribute to the growing body of knowledge around the use of telehealth to care for at risk populations. They should find solutions which will be tailored for the needs of the elderly population and consider the special obstacles and difficulties this population may have.
We suggest using simple, uncomplicated devices (such as tablets), which will be supplied to the elderly people enabling them to easily communicate with their physicians or other healthcare providers. Lectures and demonstrations on telehealth opportunities given to the general population can help addressing this digital divide. Another option is to train and prepare special health-related or technology-related personnel who can visit the elderly patients several times a month, and help them operating the telehealth devices, thus connecting them to their remote healthcare professionals.
We believe that appropriate and successful digital solutions should be tailored and developed specifically for the elderly sub-groups, and aim to address their needs, desires, and everyday activities, not only in pandemic crises. Solutions, as demonstrated in this systematic review, show that despite the hesitations of operating telehealth solutions for older patients, it can be done and be effective. This emphasizes the phrase: “where there’s a will there’s a way”.
This will deeply change the healthcare process and use of health services of this specific population and will transfer the point of care from the physician’s office to the patient.
The gain of implementing efficient telehealth solutions for the elderly population will be mutual: the elders will benefit from accessible health services, and improving their health and compliance, even in pandemic situations, and the medical system will benefit from reducing the burden on the physicians and hospitals, and by saving the costs of untreated complicated chronic diseases.
It is recommended that future studies will be examined by their effectiveness not only in the short term but also in the long term, as well as be based on a theoretical infrastructure. Furthermore, it is important that studies evaluate the differences in use between sub-groups within the target population of the elderly.
It is also recommended that further research also expands on the challenges facing healthcare workers who use telemedicine for the elderly population. It is essential to evaluate two-way communication to examine the effectiveness of telemedicine services for both the elderly patient and the public health worker.
We also recommend that there be further training of both healthcare providers and patients (especially the elderly) on how to use efficiently and effectively telehealth tools, enabling quality clinical practice by using online platforms.
Strengths and limitations
This study was performed during the Covid-19 pandemic, and includes articles published since the beginning of the outbreak until the date of data extraction (27.12.2020), for a period of approximately 13 months. We identified relevant articles through a comprehensive search of the literature, using well-defined inclusion criteria.
The telehealth solutions described here, designed for the elderly population, are also important in strengthening the advantages of patient-centered healthcare, especially during the Covid-19 pandemic.
However, there may be additional studies published after the date of data extraction, missing from the search-engines we used, or published in a different language other than English.
Acknowledgements
The authors want to thank the librarian Ms Tal Kaminski for her assistance in data extraction. This article is in memory of my mother- Rachel Haimi, who passed away several months ago at the age of 87, not from Covid-19 infection, but due the lack of appropriate medical attention caused by the Covid-19 restrictions.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Motti Haimi https://orcid.org/0000-0001-8751-9793
Anat Gesser-Edelsburg https://orcid.org/0000-0003-4467-8799
References
- 1.Shaw DK. Overview of telehealth and its application to cardiopulmonary physical therapy. Cardiopulm Phys Ther J 2009; 20(2): 13–18. [PMC free article] [PubMed] [Google Scholar]
- 2.Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis [Internet]. BMJ Open 2017; 7: e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradford N, Caffery L, Smith A. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. 2016; 16(4): 3808. [PubMed] [Google Scholar]
- 4.Valle J, Godby T, Paul DP, et al. Use of smartphones for clinical and medical education. Health Care Manag 2017; 36(3): 293–300. [DOI] [PubMed] [Google Scholar]
- 5.Jahanshir A, Karimialavijeh E, Sheikh H, et al. Smartphones and medical applications in the emergency department daily practice. Emerg (Tehran) 2017; 5(1): e14. [PMC free article] [PubMed] [Google Scholar]
- 6.Charles BL. Telemedicine can lower costs and improve access. Healthc Financ Manag 2000; 54: 66–69. [PubMed] [Google Scholar]
- 7.Chauhan V, Galwankar S, Arquilla B, et al. Novel coronavirus (COVID-19): Leveraging telemedicine to optimize care while minimizing exposures and viral transmission. J Emergencies, Trauma Shock [Internet] 2020; 13(1): 20–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehrotra A, Jena AB, Busch AB, et al. Utilization of telemedicine among rural medicare beneficiaries [Internet], JAMA - J Amer Med Assoc 2016: 315: 2015. DOI: 10.1001/jama.2016.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corbett JA, Opladen JM, Bisognano JD. Telemedicine can revolutionize the treatment of chronic disease. Int J Cardiol: Hypertens [Internet] 2020; 7: 100051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sauers-Ford HS, Hamline MY, Gosdin MM, et al. Acceptability, usability, and effectiveness: a qualitative study evaluating a pediatric telemedicine program. Acad Emerg Med 2019; 26(9): 1022–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol Pract 2020; 8: 1489–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth [Internet]. 2010. [Google Scholar]
- 13.Morenz AM, Wescott S, Mostaghimi A, et al. Evaluation of barriers to telehealth programs and dermatological care for American Indian individuals in rural Communities. JAMA Dermatol [Internet] 2019; 155(8): 899–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. The BMJ 2020: 368: m1182. [DOI] [PubMed] [Google Scholar]
- 15.Nittari G, Khuman R, Baldoni S, et al. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed J E Health 2020;26(12):1427–1437. doi: 10.1089/tmj.2019.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haimi M, Brammli-Greenberg S, Waisman Y, et al. Physicians' experiences, attitudes and challenges in a pediatric telemedicine service. Pediatr Res 2018; 84(5): 650–656. DOI: 10.1038/s41390-018-0117-6. [DOI] [PubMed] [Google Scholar]
- 17.Haimi M, Brammli-Greenberg S, Waisman Y, et al. The role of non-medical factors in physicians' decision-making process in a pediatric telemedicine service. Health Inform J 2020; 26(2): 1152–1176. DOI: 10.1177/1460458219870660. [DOI] [PubMed] [Google Scholar]
- 18.Haimi M, Brammli-Greenberg S, Baron-Epel O, et al. Assessing patient safety in a pediatric telemedicine setting: a multi-methods study. BMC Med Inform Decis Makpmcid 2020; 20(1): 63PMC7126468. DOI: 10.1186/s12911-020-1074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou X, Snoswell CL, Harding LE, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed E-Health 2020; 26: 377–379. [DOI] [PubMed] [Google Scholar]
- 20.Kadir MA. Role of telemedicine in healthcare during COVID-19 pandemic in developing countries. Telehealth Med Today 2020; 5(2): 1–5. DOI: 10.30953/tmt.v5.187. [DOI] [Google Scholar]
- 21.Okereafor K, Adebola O, Djehaiche R. Exploring the potentials of telemedicine and other non-contact electronic health technologies in controlling the spread of the novel coronavirus disease (COVID-19). IJITE 2020; 8(4): 1–13. [Google Scholar]
- 22.John O. Video consultations for triage of patients with Covid-19. The BMJ 2020; 369: m1583. [DOI] [PubMed] [Google Scholar]
- 23.Greenhalgh T, Wherton J, Shaw S, et al. Video consultations for Covid-19. The BMJ 2020; 368: m998. [DOI] [PubMed] [Google Scholar]
- 24.Leite H., Gruber T., Hodgkinson I.R. (2020), “Flattening the infection curve–understanding the role of telehealth in managing COVID-19”. Leadership in Health Services 2020; 33(2): 221–226. 10.1108/LHS-05-2020-084. [DOI] [Google Scholar]
- 25.Vidal-Alaball J Acosta-Roja R Pastor Hernández N Sanchez Luque U Morrison D Narejos Pérez S Perez-Llano J Salvador Vèrges A López Seguí F.. Telemedicine in the Face of the COVID-19 Pandemic. Aten Primaria 202052(6):418–422. doi: 10.1016/j.aprim.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grimes CL, Balk EM, Crisp CC, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: review of existing evidence. Int Urogynecol J 2020: 1; 1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hui DS, I Azhar E, Madani TA, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health — The latest 2019 novel coronavirus outbreak in Wuhan, China [Internet]. Inter J Infec Dise 2020; 91: 264–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020. 2020, [Internet]. [cited 2021 Apr 17]. Available from:https://www.who.int/director-general/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
- 29.Coronavirus Disease (COVID-19) . 2021. [Internet]. [cited 2021 Apr 17]. Available from:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19.
- 30.Pedrozo-Pupo JC, Campo-Arias A. Depression, perceived stress related to COVID, post-traumatic stress, and insomnia among asthma and COPD patients during the COVID-19 pandemic. Chronic Respir Dis 2020; 17:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caratozzolo S, Zucchelli A, Turla M, et al. The impact of COVID-19 on health status of home-dwelling elderly patients with dementia in East Lombardy, Italy: results from COVIDEM network. Aging Clin Exp Res 2020; 32(10): 2133–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kriaucioniene V, Bagdonaviciene L, Rodríguez-Pérez C, et al. Associations between changes in health behaviours and body weight during the Covid-19 quarantine in lithuania: the lithuanian covidiet study. Nutrients 2020; 12(10): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients 2020; 12(6): 1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26(5): 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. New Engl J Med 2020; 382(18): 1679–1681. [DOI] [PubMed] [Google Scholar]
- 36.Papadimos TJ, Marcolini EG, Hadian M, et al. Ethics of outbreaks position statement. Part 2. Crit Care Med 2018; 46(11): 1856–1860. [DOI] [PubMed] [Google Scholar]
- 37.Remote treatment delivery in response to the COVID-19 pandemic. Wright JH, Caudill R Psychother Psychosom. 2020; 89(3):130–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cho H, Ippolito D, Yu YW. Contact tracing mobile apps for COVID-19: privacy considerations and related trade-offs, 2020. arXiv preprint 28 arXiv:2003.11511. [Google Scholar]
- 39.Sodhi M. Telehealth policies impacting federally qualified health centers (FQHCs) in face of COVID‐19. J Rural Health 2020. 37(1): 158–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gao Y, Liu R, Zhou Q, et al. Application of telemedicine during the coronavirus disease epidemics: a rapid review and meta-analysis. Ann Translational Med 2020; 8(10): 626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bokolo AJ. Use of telemedicine and virtual care for remote treatment in response to COVID-19 Pandemic. J Med Syst 2020; 44(7): 132. DOI: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci 2021; 190(1): 1–10. DOI: 10.1007/s11845-020-02299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bokolo AJ. Application of telemedicine and eHealth technology for clinical services in response to COVID-19 pandemic. Health Technol 2021; 11: 359–366. DOI: 10.1007/s12553-020-00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhai Y, Wang Y, Zhang M, et al. From isolation to coordination: how can telemedicine help combat the COVID-19 outbreak 2020. [Google Scholar]
- 45.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020; 6(2): e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Doraiswamy S, Abraham A, Mamtani R, et al. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res 2020; 22(12): e24087. DOI: 10.2196/24087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ding X, Clifton D, Ji N, et al. Wearable sensing and telehealth technology with potential applications in the coronavirus pandemic. IEEE Rev Biomed Eng 2021; 14: 48–70. DOI: 10.1109/RBME.2020.2992838 [DOI] [PubMed] [Google Scholar]
- 48.Older adults. Centers for disease control and prevention. 2020. https://www.cdc.gov/coro navirus/2019-ncov/need-extra-precautions/older-adults.html. Published April 30, 2020. Accessed July 27, 2020.
- 49.Ambulatory Care Settings . Centers for disease control and prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html #Published May 26, 2020. Accessed July 27, 2020.
- 50.Vergara J, Parish A, Smallheer B. Telehealth: opportunities in geriatric patient care during COVID-19. Geriatr Nurs 2020; 41(5): 657–658. DOI: 10.1016/j.gerinurse.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fhon JRS, Silva LM, Leitón-Espinoza ZE, et al. Hospital care for elderly COVID-19 patients. Rev Latino-am Enfermagem 2020; 28: e3396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Garcia-Fernandez L, Romero-Ferreiro V, David Lopez-Roldan P, et al. Mental health in elderly Spanish people in times of COVID-19 outbreak. Am J Geriatr Psychiatry 2020; 28(10): 1040–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ortega G, Rodriguez JA, Maurer LR, et al. Telemedicine, COVID-19, and disparities: policy implications. Health Pol Tech 2020; 9(3): 368–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Elbeddini A, Prabaharan T, Almasalkhi S, et al. Barriers to conducting deprescribing in the elderly population amid the COVID-19 pandemic. Res Soc Administrative Pharm RSAP 2020; 17(1): 1942–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States. Communities in Action: Pathways to Health Equity. Baciu A, Negussie Y, Geller A, Weinstein JN, editors. Washington (DC): National Academies Press (US); 2017Jan 11. PMID: 28418632. [PubMed] [Google Scholar]
- 56.Demographics of internet and home broadband usage in the United States pew research center. 2021. Available from:https://www.pewresearch.org/internet/fact-sheet/internet-broadband/
- 57.Nouri S, Khoong EC, Lyles CR, et al. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. Nejm Catalyst Innovations in Care Delivery. 2020. [Google Scholar]
- 58.Kruse CS, Karem P, Shifflett K, et al. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018; 24: 4–12. DOI: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Greenwald P, Stern ME, Clark S, et al. Older adults and technology: in telehealth, they may not be who you think they are. Int J Emerg Med 2018; 11: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.PRISMA [Internet]. 2021. [cited 2021 May 21]. Available from:http://www.prisma-statement.org/ [Google Scholar]
- 61.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. The BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Norris SL, Meerpohl JJ, Akl EA, et al. The skills and experience of GRADE methodologists can be assessed with a simple tool. J Clin Epidemiol 2016; 79: 150–158.e1. [DOI] [PubMed] [Google Scholar]
- 63.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336(7650): 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Popay J, Roberts H, Sowden A, et al. “Guidance on the conduct of narrative synthesis in systematic reviews. A Product from the ESRC Methods Programme. Computer Science. Version 1.” 2006. [Google Scholar]
- 65.Yi X, Jamil NB, Gaik ITC, et al. Community nursing services during the COVID-19 pandemic: the Singapore experience. Br J Community Nurs 2020; 25(8): 390–395. [DOI] [PubMed] [Google Scholar]
- 66.Tan LL, Pillay VD, Chia JW, et al. Using telemedicine for outpatient geriatric care during the novel coronavirus outbreak: experience from the first 15 patients. Ann Acad Med Singap 2020; 49(9): 699–703. [PubMed] [Google Scholar]
- 67.Fatyga E, Dziȩgielewska-Gȩsiak S, Wierzgoń A, et al. The coronavirus disease 2019 pandemic: telemedicine in elderly patients with type 2 diabetes. Pol Arch Inter Med, 2020; 130(5):452–454.Doi: 10.20452/pamw.15346. [DOI] [PubMed] [Google Scholar]
- 68.Cilia R, Mancini F, Bloem BR, et al. Telemedicine for parkinsonism: a two-step model based on the COVID-19 experience in Milan, Italy. Parkinsonism Relat Disord, 75, 2020: 130–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Akgül A. Online counselling for new onset symptoms/signs in 65+ patients with lympho-venous diseases in the era of COVID-19. Turkiye Klinikleri J Med Sci 2020; 40(2): 125–126. [Google Scholar]
- 70.ben Hassen H, Ayari N, Hamdi B. A home hospitalization system based on the Internet of things, Fog computing and cloud computing. Inform Med Unlocked 2020; 20: 100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Motolese F, Magliozzi A, Puttini F, et al. Parkinson’s disease remote patient monitoring during the COVID-19 lockdown. Front Neurol 2020; 11: 567413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.van Dijk SDM, Bouman R, Folmer EH, et al. (Vi)-rushed into online group schema therapy based day-treatment for older adults by the COVID-19 outbreak in the Netherlands. Am J Geriatr Psychiatry 2020; 28(9): 983–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Truong J, Heravian A, Olsen E, et al. 54 From the COVID-19 epicenter: using telemedicine to serve the needs of the geriatric population. Ann Emerg Med 2020; 76(4): S22. [Google Scholar]
- 74.Patel S, Gannon A, Cryan M, et al. Ordinary care in extraordinary times. Ir J Psychol Med. 2020;1–5. doi: 10.1017/ipm.2020.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Weiss EF, Malik R, Santos T, et al. Telehealth for the cognitively impaired older adult and their caregivers: lessons from a coordinated approach. Neurodegenerative Dis Manag 2021; 11(1): 83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kucharski AJ, Russell TW, Diamond C, et al. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect Dis 2020; 20(5): 553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Adhikari SP, Meng S, Wu YJ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty, 2020: 9: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 2020; 20: 1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tebeje TH, Klein J. Applications of e-health to support person-centered health care at the time of COVID-19 pandemic. Telemed E-health 2021; 27(2): 150–158. [DOI] [PubMed] [Google Scholar]
- 80.Chiu YW, Teitelbaum I, Misra M, et al. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol 2009; 4(6): 1089–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.St Peter WL, Wazny LD, Patel UD. New models of chronic kidney disease care including pharmacists: improving medication reconciliation and medication management. Curr Opin Nephrol Hypertens, 2013; 22: 656–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kirsh S, Su GL, Sales A, et al. Access to outpatient specialty care: solutions from an integrated health care system. Am J Med Qual, 2015; 30: 88–90. [DOI] [PubMed] [Google Scholar]
- 83.Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc 2020; 27(6): 853–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Thompson S, James M, Wiebe N, et al. Cause of death in patients with reduced kidney function. J Am Soc Nephrol 2015; 26(10): 2504–2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fung E, Chang TI, Chertow GM, et al. Receipt of nephrology care and clinical outcomes among veterans with advanced CKD. Am J Kidney Dis 2017; 70(5): 705–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.D’Adamo H, Yoshikawa T, Ouslander JG. Coronavirus disease 2019 in Geriatrics and long-term care: the ABCDs of COVID-19. J Am Geriatr Soc 2020; 68(5): 912–917. [DOI] [PubMed] [Google Scholar]
- 87.Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging 2020; 1: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dewar S, Lee PG, Suh TT, et al. Uptake of virtual visits in A geriatric primary care clinic during the COVID-19 pandemic, J Am Geriatr Soc 2020; 68: 1392–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hawley CE, Genovese N, Owsiany MT, et al. Rapid integration of home telehealth visits amidstCOVID-19: what do older adults need to succeed? J Ame Geri Soc 2020; 68(11): 2431–2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Eghtesadi M. Breaking social isolation amidst COVID-19: a viewpoint on improving access to technology in long-term care facilities, J Am Geriatr Soc 2020; 68: 949–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Perry LP. To all doctors: what you can do to help as a bunch of older people are about to get sick and die, J Am Geriatr Soc, 2020; 68: 944–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Phillips NA, Chertkow H, Pichora-Fuller MK, et al. Special issues on using the montreal cognitive assessment for telemedicine assessment during COVID-19. J Am Geriatr Soc 2020; 68: 942–944. [DOI] [PubMed] [Google Scholar]
- 93.van den Berg N, Schumann M, Kraft K, et al. Telemedicine and telecare for older patients - a systematic review. Maturitas Elsevier Ireland Ltd 2012; 73: 94–114. [DOI] [PubMed] [Google Scholar]
- 94.Forducey PG, Glueckauf RL, Bergquist TF, et al. Telehealth for persons with severe functional disabilities and their caregivers: facilitating self-care management in the home setting. Psychol Serv 2012; 9(2): 144–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lam K, Lu AD, Shi Y, et al. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med 2020; 180: 1389–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Moo LR, Gately ME, Jafri Z, et al. Home-based video telemedicine for dementia management. Clin Gerontologist 2020; 43(2): 193–203. [DOI] [PubMed] [Google Scholar]
- 97.Pimentel CB, Gately M, Barczi SR, et al. GRECC connect: geriatrics telehealth to empower health care providers and improve management of older veterans in rural communities. Fed Pract. 2019; 36(10): 464–470. [PMC free article] [PubMed] [Google Scholar]
- 98.Slightam C, Gregory AJ, Hu J, et al. Patient perceptions of video visits using veterans' affairs telehealth tablets: Survey study. J Med Internet Res 2020; 22(4): e15682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Appleman ER, O’Connor MK, Rockefeller W, et al. Using Video Telehealth to Deliver Patient-Centered Collaborative Care: The G-IMPACT Pilot. Clin Gerontol. 2020; 31:1–10. doi: 10.1080/07317115.2020.1738000. [DOI] [PubMed] [Google Scholar]
- 100.Gately ME, Trudeau SA, Moo LR. Feasibility of telehealth-delivered home safety evaluations for caregivers of clients with dementia. OTJR Occup Participation Health 2020; 40(1): 42–49. [DOI] [PubMed] [Google Scholar]
- 101.Batsis JA, DiMilia PR, Seo LM, et al. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc 2019; 67: 1737–1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Moo LR, Jafri Z, Morin PJ. Home-based video telehealth for veterans with dementia. Federal practitioner: for the health care professionals of the VA. DoD, and PHS 2014; 31(12): 36–38. [PMC free article] [PubMed] [Google Scholar]