Abstract
Aim
To conduct a systematic literature review of the existing evidence on incidence, characteristics and outcomes after out-of-hospital cardiac arrest (OHCA) in patients with psychiatric illness.
Methods
We searched Embase, Medline, PsycINFO and Web of Science using a comprehensive electronic search strategy to identify observational studies reporting on OHCA incidence, characteristics or outcomes by psychiatric illness status. One reviewer screened all titles and abstracts, and a second reviewer screened a random 10%. Two reviewers independently performed data extraction and quality assessment.
Results
Our search retrieved 11,380 studies, 10 of which met our inclusion criteria (8 retrospective cohort studies and two nested case-control studies). Three studies focused on depression, whilst seven included various psychiatric conditions. Among patients with an OHCA, those with psychiatric illness (compared to those without) were more likely to have: an arrest in a private location; an unwitnessed arrest; more comorbidities; less bystander cardiopulmonary resuscitation; and an initial non-shockable rhythm. Two studies reported on OHCA incidence proportion and two reported on survival, showing higher risk, but lower survival, in patients with psychiatric illness.
Conclusion
Psychiatric illness in relation to OHCA incidence and outcomes has rarely been studied and only a handful of studies have reported on OHCA characteristics, highlighting the need for further research in this area. The scant existing literature suggests that psychiatric illness may be associated with higher risks of OHCA, unfavourable characteristics and poorer survival. Future studies should further investigate these links and the role of potential contributory factors such as socioeconomic status and comorbidities.
Keywords: Psychiatric illness, Out-of-hospital cardiac arrest, Systematic review, Resuscitation, Management, Survival
Introduction
Out-of-hospital cardiac arrest (OHCA) is an acute event characterised by an interruption of mechanical cardiac activity leading to absence of systematic blood circulation.1 Estimated annual incidence of OHCA ranges from 30-97 per 100,000 population in Europe and other high-income countries including the United States, Japan and Australia.2 Most OHCAs have a cardiac cause, with less common causes including trauma, drowning, burns, and drug overdose. OHCA survival remains relatively low; in 2015 survival to hospital discharge or 30-day survival of OHCA following resuscitation by Emergency Medical Services (EMS) ranged from 3.1 to 20.4 % (based on data from 16 national and regional OHCA registries from predominantly high-income countries).2 Recently, progress at both national and international levels in most high-income countries has led to the development of resuscitation guidelines and implementation of prevention strategies, resulting in slightly improved OHCA outcomes over the past 10 years.3., 4., 5., 6. However, these strategies might not have improved survival in some sub-groups, with one study reporting that 30-day OHCA survival improved over time in people without psychiatric illness, but not in people with psychiatric illness.6 There is evidence that the latter may have an increased risk of, and poorer survival from, OHCA.6., 7. This may reflect the excess burden of cardiovascular disease (CVD) in people with psychiatric illness. The life expectancy of this vulnerable group is 10–12 years shorter than the general population, with CVD the major contributory factor.8., 9., 10., 11., 12. Moreover, it is well-known that favourable OHCA outcomes are linked to: arrest in a public location; witnessed arrest; early receipt of bystander cardiopulmonary resuscitation (CPR); presence of initial shockable rhythm; and early defibrillation in patients with initial shockable rhythms,13 each of which may be associated, directly or indirectly, with psychiatric illness status.6., 9., 14., 15. For example, existing studies suggest that people living in more socioeconomically deprived areas are more likely to have comorbidities and less likely to receive bystander CPR.3., 14.
Whilst psychiatric illness in relation to CVD has been widely studied, the links between psychiatric illness and OHCA incidence and outcome has been far less studied. Given the growing recognition of mental health disparities in physical disease occurrence and outcomes,8., 10., 12. it is timely to review the existing evidence in this area to gain insight into the methodological limitations of existing studies, identify gaps in understanding and direct future research. Therefore, we carried out a systematic review of the existing evidence on incidence, characteristics and outcome of OHCA among patients with psychiatric illness.
Methods
Search strategy
The protocol of this review is registered with PROSPERO (CRD42021229545). We followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines to report this review.16 We sought to identify observational studies reporting on the incidence, and patient and event-related characteristics of OHCA and outcome of OHCA in patients with prior psychiatric illness. We developed a detailed electronic search strategy containing a wide range of terms for psychiatric illness and OHCA (Appendix 1). We searched Embase, Medline, PsycINFO and Web of Science from inception to 11th December 2021 for articles in English only. All titles and abstracts were screened for eligibility by one reviewer (RA) and a random sample of 10% of all retrieved results were screened by a second reviewer (LB). Full texts of potentially relevant articles were then independently assessed against the eligibility criteria by both reviewers (RA and LB). Reference lists of all included articles were scanned to identify additional relevant articles not identified in the electronic search.
Inclusion and exclusion criteria
We included observational studies published in English that reported on psychiatric illnesses in adults and children including depressive disorders, anxiety disorders, bipolar disorders, dissociative disorders and schizophrenia and other psychotic disorders, with or without an included comparison group. We included studies that reported on either of the following: OHCA incidence, patient- and OHCA event-related characteristics, 30-day survival or survival to hospital discharge. We excluded case reports, intervention studies and studies that reported on dementia and neurocognitive disorders.
Assessment of risk of bias
Risk of bias of included studies was assessed independently by two reviewers (RA and LB) using the Newcastle-Ottawa Quality Assessment Scale (NOS) with a maximum score of nine for the highest quality.17 Any disagreements related to study selection, quality assessment or data extraction were resolved by discussion with other investigators (CJ and NH). Initially, we planned to use the The Critical Appraisal Skills Programme (CASP) checklist to assess risk of bias,18 but authors sought to use the NOS scale instead as it can be slightly modified based on the subject.19
Data extraction
The following information from eligible articles was independently extracted by two reviewers (RA and LB): study design and setting; population characteristics; definition and ascertainment of psychiatric illness; patient and OHCA event-related characteristics including sex, age, location of arrest, witness status, initial cardiac rhythm, receipt of bystander CPR, survival to discharge and 30-day survival. Where there was overlap in articles populations (i.e., articles reported same outcomes based on the same cohort), we extracted results from the most inclusive article in terms of longest follow-up or largest study population. Since included articles were heterogeneous in terms of study population, psychiatric illness definitions and assessed outcomes, we performed a narrative synthesis of study findings rather than a meta-analysis.20
Results
Study selection
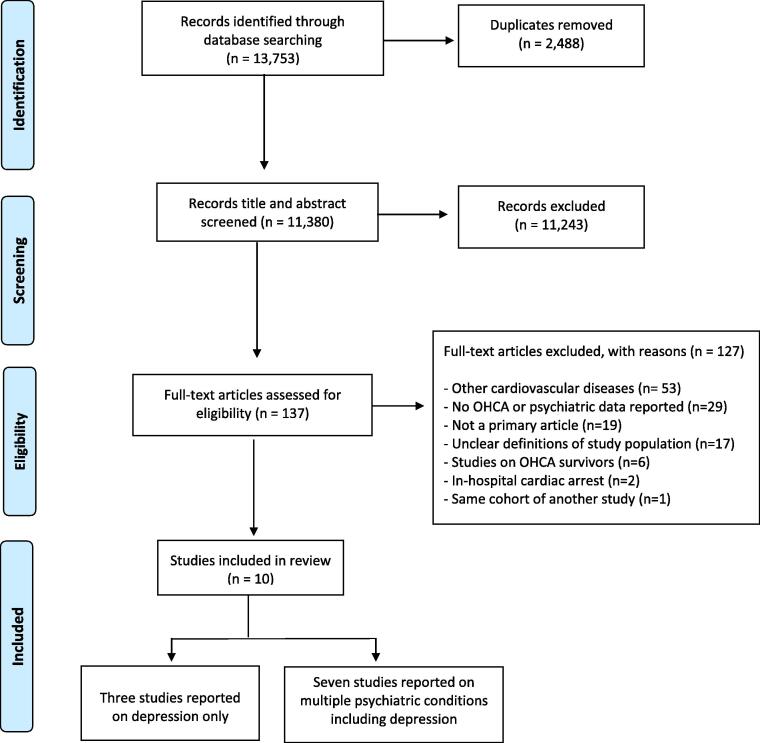
After removing duplicates, our initial literature search identified 11,380 articles. Based on screening of titles and abstracts we excluded 11,243 irrelevant articles. We reviewed the full text of the remaining 137 articles, twelve of which met our inclusion criteria (Fig. 1). However, in two instances, study populations overlapped and similar findings reported in both articles,6., 21., 22., 23. therefore we included the article with longer follow-up period in one instance6 and the largest population in the other one.23 Hand-searching of references lists did not yield any additional relevant articles or potentially relevant articles in non-English.
Fig. 1.
Study selection flowchart. Abbreviations: OHCA: Out-of-hospital cardiac arrest.
Study characteristics
The characteristics of the nine included studies are summarised in Table 1. Eight were retrospective cohort studies6., 7., 24., 25., 26., 27., 28., 29. and two were nested case-control studies.23., 30. All used registry data from Europe,6., 25., 29., 30., 31. Japan,7., 26. Canada24, 27 and the United States.23 Studies varied markedly in terms of type of psychiatric illness included, study population, and assessed outcomes. Three studies included patients with depression,23., 25., 27. whilst seven studies included a range of psychiatric conditions. Studies varied in their definition of psychiatric illness (Table 1). Studies also varied in OHCA patients’ eligibility criteria, although all studies excluded OHCAs caused by non-cardiac causes including trauma, drowning, burns and drug overdose. Two studies reported on the risk of OHCA incidence,23., 30. two studies reported data on survival,6., 7. one compared the 30-day survival in patients with versus without psychiatric illness6 whilst the other study compared survival to hospital discharge between patients with and without schizophrenia or mood disorders7.6., 7. The remaining studies reported on OHCA characteristics (Table 1). The gender difference in the prevalence of psychiatric illness among OHCA patients was reported in five studies.7., 23., 24., 29., 30. Seven studies included those 18 or 20 years or older,7., 23., 24., 29., 30. two studies included both children and adults24., 29. and one study25 did not report the age range of included participants.
Table 1.
Characteristics of included studies.
| First author, year of publication, country | Study design [study period] | Study populationa | Study participants [number with psychiatric illness] | Age, yearsb(SD) | Sex (% female) | Type and ascertainment of psychiatric illness | OHCA outcomes and characteristics reported | NOS score |
|---|---|---|---|---|---|---|---|---|
| Empana, 2006, USA23 | Nested Case-control [1980–1994] | Adults aged ≥ 18 years with OHCA identified from ambulatory medical records; controls matched by age and sex | 2,228 Cases/4,164 Controls [300 /327] | Cases: 66.3 (10.2); Controls: 66.2 (9.9) | 30.0 | Clinical depression, primary care records and antidepressant medication prescriptions | Incidence proportion, sex, comorbidities | 5 |
| Wissenberg, 2014, Denmark 29 | Retrospective cohort [2001–2010] | People aged ≥ 12 with OHCA with attempted resuscitation (The Danish Cardiac Arrest Registry). | 19,372 [2,674] | Median 72; IQR (62–80) | 32.6 | Psychiatric illness, hospital admission records | Sex | 6 |
| Ko, 2016, Canada 27 | Retrospective cohort [2005–2010] | Adults aged ≥ 20 years with complete information on OHCA characteristics (RescuNET cardiac arrest Registry) | 9,882 [389] | 68.8 (16.1) | 36.1 | Depression, linkage to hospital admission and primary care records | Age and rhythm | 6 |
| Rajan, 2016, Denmark28 | Retrospective cohort [2005–2012] | People aged ≥ 18 (The Danish Cardiac Arrest Registry) | 13,860 [2,146] | Range 58–82 | 32.1 | Psychiatric illness, hospital admission records | Rhythm conversion | 6 |
| Ishida, 2019, Japan26 | Retrospective cohort [2010–2017] | People aged ≥ 18 with complete information on medical history who had ROSC and transported to Tokyo metropolitan Bokutoh Hospital | 649 [49] | Range 18–103 | 23.8 | Psychiatric illness, hospital admission records | Location of arrest and comorbidities | 4 |
| Allan, 2018, Canada24 | Retrospective cohort [2009–2012] | People aged 2–45, (RescuNET cardiac arrest database) | 608 [117] | 35.4 (8.9) | 23.7 | Mood disorder, psychosis, other psychiatric historyc and any psychiatric history, history of psychiatric disease diagnosis or antidepressant or antipsychotic prescription, hospital admission records and prescriptions records | Age and sex | 5 |
| Barcella, 2019, Denmark6 | Retrospective cohort [2001–2015] | People aged ≥ 18 (The Danish Cardiac Arrest Registry) | 27,523 [4,772] | Median 71; IQR (62–81) | 31.0 | Any psychiatric illness except dementia and mental organic disorder, patients who used antipsychotics and/or lithium and patients who used only antidepressants, medical diagnosis and prescriptions history multisource recordsd | Survival, rhythm, location of arrest, witness status, bCPR, comorbidities and income | 8 |
| Ishida, 2020, Japan7 | Retrospective cohort [2011–2017] | People aged ≥ 18 with a complete information on medical history who were transported to Tokyo metropolitan Bokutoh Hospital | 2,631 [157] | Range 18–108 | 31.6 | Diagnosis of schizophrenia or mood disorders, hospital admission records | Survival, age, sex and rhythm | 6 |
| Hulleman, 2020, Netherlands25 | Retrospective cohort [2009–2012] | OHCA patients with a complete information on medical history, ARREST registry | 1,404 [120] | 67.9 (14.5) | 20.1 | Depression, ascertained through primary care records | Rhythm and location of arrest | 4 |
| Barcella, 2021, Denmark 30 | Nested Case-control [2001–2015] | People aged 18–100 (The Danish Cardiac Arrest Registry); controls matched by age and sex | 35,017 Cases/175,085 Controls [802 /4,009] | Cases: Median 72; IQR (62–81); Controls: Median 72; IQR (62–81) | 66.9 | Schizophrenia and bipolar disorder, medical diagnosis and prescriptions history multisource recordsd | Incidence proportion and comorbidities | 8 |
bCPR: Bystander Cardiopulmonary Resuscitation; CIHI: Canadian Institute for Health Information; EMS: Emergency Medical Services; IQR: interquartile range; NOS: Newcastle-Ottawa Scale (0–9) OHCA: Out-of-hospital cardiac arrest; ROSC: Return of Spontaneous Circulation; SD: Standard deviation.
All studies excluded OHCAs from presumed non-cardiac causes such as traumas, burns, drowning and electrocution.
Age is in mean years (SD) unless otherwise stated.
Includes one diagnosis of obsessive–compulsive disorder, borderline personality disorder, or suicide attempt.
Danish Psychiatric Central Research Register, the Danish National Patient Register and the National Prescription Register.
Risk of bias for individual studies
The number of awarded stars ranged between 4 and 8 (out of a total of 9 stars using the NOS scale); four studies received 5 or fewer stars.23., 24., 25., 26. One of the main potential risks of bias was the lack of a clear definition of psychiatric illness eligibility criteria in some studies, giving rise to a potentially high risk of selection bias.23., 25., 28., 29. Another potential risk of bias identified in three studies was the inclusion of patients with psychotropic medication use within the psychiatric illness group without reporting the indication for use.6., 23., 24. All five studies6,7., 27., 28. that assessed the association between psychiatric illness and OHCA incidence, characteristics or survival adjusted for age and sex. However, none of the studies adjusted for socioeconomic status, which may be associated with higher risk of OHCA incidence, unfavourable characteristics and poorer survival.6., 7., 27., 28., 30.
Incidence of OHCA
Table 2 summarises the key findings of included studies. Other relevant outcomes are summarised in supplemental Table 3. The two studies that reported on OHCA incidence were nested case-control studies.23., 30. One study was from the United States that included 300 OHCA cases and 327 controls.23 A history of depression was associated with a 43% increased odds of OHCA risk (odds ratio (OR) 1.43, 95% CI 1.18 to 1.73) after adjusting for history of CVD, diabetes, smoking and alcohol consumption. A further classification of depression into less severe and severe showed that, compared to no history of depression, the odds of OHCA incidence was 30% higher for less severe depression and 70% higher for severe depression (Table 2).23 The other study was a Danish study and assessed schizophrenia (457 cases versus 2,285 controls) and bipolar disorder (345 cases versus 2,285 controls) separately.30 For both psychiatric illnesses (schizophrenia and bipolar disorder), cases had three to four times higher rates of OHCA than matched controls.30
Table 2.
Summary of key findings from studies reporting on psychiatric illness and incidence, characteristics and survival of OHCA.
| Author, Year of publication | Study participants [number with psychiatric illness] | Factors adjusted for in statistical models | Key findings |
|---|---|---|---|
| Empana, 200623 | 2,228 Cases/4,164 Controls [300 /327] | Smoking, alcohol use, hypertension, diabetes, history of MI and CHF |
|
| Wissenberg, 201429 | 19,372 [2,674] | NA |
|
| Ko, 201627 | 9,882 [389] | Age, sex, income, comorbidities, EMS response time, location of arrest, witness status and bCPR |
|
| Rajan, 201628 | 13,860 [2,146] | Age, sex, comorbidities, location of arrest, witness status, bCPR, time from recognition of arrest to rhythm analysis by the EMS, and year of arrest |
|
| Ishida, 201926 | 649 [49] | NA | Patients with versus without psychiatric illness were more likely to have:
|
| Allan, 201824 | 608 [117] | NA | Among patients < 45yrs:
|
| Barcella, 2019 6 | 27,523 [4,772] | Age, sex and year of arrest | Patients with versus without psychiatric illness have:
|
| Ishida, 20207 | 2,631 [157] | Age, sex, comorbidities, witness status, location of arrest | Patients with schizophrenia or mood disorders have:
|
| Hulleman, 202025 | 1,404 [120] | NA |
|
| Barcella, 2021, Denmark30 | 35,017 Cases/175,085 Controls [802 /4,009] | NA |
|
bCPR: Bystander Cardiopulmonary Resuscitation; CHF: Congestive Heart failure; CI: Confidence Interval; EMS: Emergency Medical Services; HR: Hazard ratio; MI: Myocardial infarction; OHCA: Out-of-hospital Cardiac Arrest; OR: Odds Ratio; ROSC: Return of Spontaneous Circulation; PEA: Pulseless electrical activity (classified as non-shockable rhythm).
Severe depression defined by depression with history of referral to a mental health clinic and/or hospitalisation for depression in the year before OHCA.
Patient- and OHCA event-related characteristics
As previously mentioned, there are well-established characteristics associated with favourable OHCA outcomes.13 Our review found that some of these characteristics, such as presence of an initial non-shockable cardiac rhythm and arrest in a private location, consistently differed by psychiatric illness status across studies, whereas findings for other characteristics such as age and sex were inconsistent between studies.
Differences by sex
Four studies reported results by sex. In three of these, individuals with a psychiatric illness who experienced an OHCA were more likely to be female,7., 24., 29. but the fourth study23 (which included patients with depression) found no similar increased risks to females. Additionally, results from a subgroup analysis in the Danish study6 found that the association between psychiatric illness and lower 30-day survival was similar for males and females. A subgroup analysis stratified by sex showed that only women with psychiatric illness are more likely to have an OHCA in a public location (OR 1.25, 95% CI 1.09 to1.42) compared to women without psychiatric illness.6 However, only men with psychiatric illness are less likely to receive bystander CPR (OR 0.68, 95% CI 0.62 to 0.75) compared with men without psychiatric illness (supplemental Table 3).6
Initial cardiac rhythm
All five studies that reported on the initial cardiac rhythm in patients with OHCA found that those with versus without psychiatric illness were more likely to have an initial non-shockable cardiac rhythm.6., 7., 25., 27., 28. Moreover, one study28 including 13,860 OHCAs found lower odds of conversion from initial non-shockable to shockable cardiac rhythm in patients with psychiatric illness after adjustment for age, sex, comorbidities and other covariates (OR 0.66, 95% CI 0.55 to 0.79) (Table 2).
Location of arrest and witness status
Early recognition of collapsed patients is a key factor associated with favourable outcomes and is highly dependent on the location of arrest.13., 32.
Of three studies, two studies found that patients with depression25 and schizophrenia and mood disorders7 were more likely to have their OHCA at home compares to patients without psychiatric illness. In contrast, as mentioned in the previous paragraph, the Danish study found that women but not men, with psychiatric illness were more likely to have an OHCA in a public location.6 However, patients with psychiatric illness had more unwitnessed arrests and lower chances of receiving bystander CPR among those who had witnessed arrests.6 Interestingly, the Danish study also found that, compared to people without psychiatric illness, those with substance-induced mental disorders were less likely to have an OHCA in a public location (OR 0.74, 95% CI 0.64 to 0.85) whilst individuals with bipolar disorder, schizophrenia or other psychotic disorders had a higher risk of OHCA in public locations.6
OHCA survival
Two studies reported on OHCA survival, with both finding lower survival in patients with psychiatric illness.6., 7. The largest study included 27,523 OHCA patients, of which 4,772 had a history of psychiatric illness diagnosis.6 This Danish cohort study found that, after adjusting for age, sex and year of OHCA, odds of 30-day survival were 63% lower in patients with a hospital diagnosis of psychiatric illness versus patients without psychiatric illness.6 The association was consistent across all types of psychiatric illness, with the effect most pronounced among patients with schizophrenia and other psychotic disorders (OR 0.21, 95% CI 0.14 to 0.30). The same study also found that 30-day survival in people without psychiatric illness increased from 2001-2015, whilst in patients with psychiatric illness it remained fairly stable. The magnitude of the association between psychiatric illness and reduced 30-day survival was greater where the OHCA had occurred in a public location (OR 0.28, 95% CI 0.23 to 0.34) as compared to a private location (OR 0.43, 95% CI 0.36 to 0.52) (supplemental Table 3).6
In a much smaller Japanese retrospective cohort study of 157 patients with schizophrenia or mood disorders and 2,474 patients without any history of psychiatric illness, OHCA survival to hospital discharge was slightly lower in patients with schizophrenia or mood disorders versus patients without psychiatric illness (7.6% versus 10.2%; Table 2 & supplementary Table 3).7 These rates were not adjusted for confounding factors and are limited by the small sample size.
Discussion
This systematic review uncovers a major gap in the literature on incidence, characteristics and outcomes of OHCA in patients with psychiatric illness. Only four studies have reported on OHCA incidence and/or outcomes in relation to psychiatric illness, with a few more having reported on OHCA characteristics. Among included studies we found marked heterogeneity with regards to study population, psychiatric illness definitions and assessed outcomes. Although there is limited literature in this area, findings from existing studies were generally consistent in terms of psychiatric illness being associated with unfavourable patient- and OHCA event-related characteristics and lower OHCA survival.
Two studies that reported on risk of OHCA incidence compared people with and without depression in one study,23 and schizophrenia or bipolar disorder versus no mental illness in another study.30 Previous research has established that depression, schizophrenia and bipolar disorders are risk factors for CVD occurrence in healthy populations and mortality in patients with existing CVD including coronary artery disease, cerebrovascular disease, peripheral artery disease and heart failure.33., 34., 35. Given that most OHCA events are of a cardiac origin, it is likely that the increased CVD risk includes increased risk of the cardiac causes that eventually lead to OHCA. Mechanisms by which psychiatric illnesses may affect OHCA risk could be similar to the mechanisms by which psychiatric illnesses are associated with CVD incidence and poorer outcomes including behavioural and biological mechanisms.33., 36. These mechanisms are complex and not yet fully understood.37 Other studies found that risk of adverse cardiovascular events such as sudden cardiac death and ventricular arrhythmia is associated with psychotropic drug use even among patients without existing CVD.38., 39. Additionally, a Danish data linkage study that was not included in this review found that antipsychotic drugs is associated with increased risk of OHCA.40
Both studies that reported on OHCA survival in relation to psychiatric illness found lower survival in patients with psychiatric illness.6., 7. This lower survival may be partly due to differing OHCA characteristics, with psychiatric illness linked to factors associated with unfavourable OHCA outcomes. For example, receiving bystander CPR is associated with a two- to three-fold higher 30-day survival than those who do not receive bystander CPR.31 Earlier research has identified factors contributing to the chance of receiving bystander CPR, some of which are associated with psychiatric illness, including location of arrest, witness status and socioeconomic status.5., 15., 41. The studies included in our review report that people with psychiatric illness experience more unwitnessed OHCAs and are less likely to receive bystander CPR.6., 7., 26. However, there are indications that these differences may not fully explain lower OHCA survival in patients with psychiatric illness. To illustrate, one study reported that psychiatric illness remained associated with lower 30-day survival when analyses were restricted to only witnessed OHCAs with bystander CPR.6 Other important factors that could affect the survival of those who received bystander CPR are initial cardiac rhythm and use of Automatic External Defibrillator (AED).5 However, findings from our review suggested that OHCA patients with psychiatric illness were less likely to present with an initial shockable cardiac rhythm, therefore they may be less likely to benefit from bystander AED use. The lower chance of a shockable initial cardiac rhythm among patients with a psychiatric illness might be due to more frequent comorbidities, private location of arrest and use of psychotropic medication, which has been linked to reduced heart rate variability and QT prolongation.42., 43. It is known that the prevalence of psychiatric illnesses is higher among more socioeconomically deprived groups.44 However, our review found that existing studies have rarely included information on socioeconomic status; just one study reported on this, finding a higher proportion of OHCA patients with psychiatric illness in the low-income group).6 According to existing literature, bystander CPR rates are lower in more socioeconomically deprived areas and community-based resuscitation strategies like CPR training and provision of public access defibrillators are less evident in more deprived areas.41., 45. Our review found no evidence of a gender difference in OHCA survival among patients with psychiatric illness. However, patients with OHCA and psychiatric illness were more likely to be female, which is in agreement with studies suggesting that women have more comorbidities at the time of OHCA.29., 46. In the general population, there is conflicting evidence on how subsequent survival differs by sex, despite females being more likely to present with less favourable characteristics.2., 13., 15., 47., 48.
In addition to the differences in OHCA characteristics, delivery of in-hospital clinical care may also differ by psychiatric illness, which could impact survival. For example, there are well-established, although poorly understood, mental health disparities in the management of patients following myocardial infarction, one of the major cardiovascular events that can result in OHCA.36., 49. There is also evidence that after OHCA, people with psychiatric illness are less likely to undergo coronary angiography or receive an implantable cardioverter-defibrillator after accounting for sex, age, comorbidities, socioeconomic status and OHCA characteristics.50
Strengths and limitations
To the best of our knowledge, this is the first systematic review of studies describing incidence, characteristics and outcome of OHCA in patients with psychiatric illnesses. Moreover, we identified studies using a comprehensive electronic search strategy and performed independent double extraction of data and quality assessment. Our review has some limitations. First, we did not perform double screening of title and abstract for all retrieved articles. However, the second reviewer screened a random selection of 10% of titles and abstracts, which revealed a high agreement between the reviewers. Second, for feasibility reasons, we restricted our search to articles published in English only, which means that we will not have included relevant articles published in other languages. Excluding studies in non-English language could bias the review findings in terms of potentially excluding studies from selected settings, particularly low and middle-income countries, which could reduce the generalisability of findings.
We identified a number of limitations related to the included studies themselves, which may limit the conclusions that can be drawn. First, ascertainment and definition of psychiatric illness varied between studies, contributing to the marked heterogeneity and reducing comparability of findings between studies. Second, collecting accurate data in a pre-hospital setting is challenging and may vary between countries particularly for events like OHCA where the patient is unconscious, which may also contribute to the marked heterogeneity.51 Last, no study took into account the role played by socioeconomic status in the link between psychiatric illnesses and OHCA incidence or outcome, which is an important gap given that socioeconomic status is a known risk factor for low OHCA survival.14., 44.
Implications
The paucity of studies addressing OHCA in patients with psychiatric illness indicates a major knowledge gap in this area. It is imperative that we clarify, from studies across different settings and populations, the extent to which individual psychiatric illnesses are associated with increased OHCA risk and survival and why such disparities exist. Further studies investigating the association between psychiatric illnesses and OHCA in more depth are warranted. Studies should consider the effect of socioeconomic factors, psychotropic medication use, and comorbidities on patient- and OHCA event-related characteristics and how these factors contribute to survival in OHCA patients with psychiatric illness as a whole and stratified by type of psychiatric illness. Moreover, collaborative work between EMS services and hospitals is required to link pre-hospital and in-hospital data to investigate the effect of in-hospital treatment, such as coronary revascularisation, on OHCA survival.52 A better understanding of the effect of psychiatric illnesses on OHCA outcomes may help in explaining part of the overall observed lower life expectancy in patients with psychiatric illness.
Conclusion
This review highlights the scarcity of studies reporting on psychiatric illness in relation to OHCA incidence, characteristics and outcomes. History of psychiatric illness appears to be a risk factor for increased OHCA risk, unfavourable OHCA characteristics and poorer survival, but further high quality studies are needed to more fully understand this important issue.
CRediT authorship contribution statement
Raied Alotaibi: Conceptualization, Methodology, Writing – original draft. Nynke Halbesma: Conceptualization, Methodology, Writing – review & editing, Supervision. Laura A.E. Bijman:Screening, Data Extraction, Writing - Review. Gareth Clegg: Writing – review & editing, Supervision. Daniel J. Smith: Writing – review & editing. Caroline A. Jackson: Conceptualization, Methodology, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Dr Halbesma is supported by a British Heart Foundation Intermediate Basic Science Research Fellowship (FS/16/36/32205).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100214.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Jacobs I., Nadkarni V., Bahr J., et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation. Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 2.Kiguchi T., Okubo M., Nishiyama C., et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 3.Blewer A.L., Ho A.F.W., Shahidah N., et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. The Lancet Public Health. 2020;5:e428–e436. doi: 10.1016/S2468-2667(20)30140-7. [DOI] [PubMed] [Google Scholar]
- 4.Wu Z., Panczyk M., Spaite D.W., et al. Telephone cardiopulmonary resuscitation is independently associated with improved survival and improved functional outcome after out-of-hospital cardiac arrest. Resuscitation. 2018;122:135–140. doi: 10.1016/j.resuscitation.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 5.Yan S., Gan Y., Jiang N., et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Critical Care. 2020;24:1–13. doi: 10.1186/s13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barcella C.A., Mohr G.H., Kragholm K., et al. Out-of-hospital cardiac arrest in patients with psychiatric disorders—Characteristics and outcomes. Resuscitation. 2019;143:180–188. doi: 10.1016/j.resuscitation.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Ishida T., Sugiyama K., Tanabe T., et al. Lower Proportion of Fatal Arrhythmia in Sudden Cardiac Arrest Among Patients With Severe Mental Illness Than Nonpsychiatric Patients. Psychosomatics. 2020;61:24–30. doi: 10.1016/j.psym.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Correll C.U., Solmi M., Veronese N., et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16:163–180. doi: 10.1002/wps.20420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Majewski D., Ball S., Finn J. Systematic review of the relationship between comorbidity and out-of-hospital cardiac arrest outcomes. BMJ open. 2019;9 doi: 10.1136/bmjopen-2019-031655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walker E.R., McGee R.E., Druss B.G. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawrence D., Hancock K.J., Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. Bmj. 2013;346 doi: 10.1136/bmj.f2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hjorthøj C., Stürup A.E., McGrath J.J., Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4:295–301. doi: 10.1016/S2215-0366(17)30078-0. [DOI] [PubMed] [Google Scholar]
- 13.Dyson K., Brown S.P., May S., et al. International variation in survival after out-of-hospital cardiac arrest: A validation study of the Utstein template. Resuscitation. 2019;138:168–181. doi: 10.1016/j.resuscitation.2019.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Chamberlain R.C., Barnetson C., Clegg G.R., Halbesma N. Association of measures of socioeconomic position with survival following out-of-hospital cardiac arrest: a systematic review. Resuscitation. 2020 doi: 10.1016/j.resuscitation.2020.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Blewer A.L., McGovern S.K., Schmicker R.H., et al. Gender disparities among adult recipients of bystander cardiopulmonary resuscitation in the public. Circulation: Cardiovascular Quality and Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.118.004710. e004710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page M.J., McKenzie J.E., Bossuyt P.M., et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. Journal of Clinical Epidemiology. 2021;134:103–112. doi: 10.1016/j.jclinepi.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Wells G., Shea B., O’connell D., et al. Ottawa Hospital Research Institute; Clinical Epidemiology: 2016. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Google Scholar]
- 18.Singh J. Critical appraisal skills programme. Journal of Pharmacology and Pharmacotherapeutics. 2013;4:76. [Google Scholar]
- 19.Zeng X., Zhang Y., Kwong J.S., et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. Journal of evidence-based medicine. 2015;8:2–10. doi: 10.1111/jebm.12141. [DOI] [PubMed] [Google Scholar]
- 20.Deeks J.J., Higgins J.P., Altman D.G., Group C.S.M. Analysing data and undertaking meta-analyses. Cochrane handbook for systematic reviews of interventions. 2019:241–284. [Google Scholar]
- 21.Granfeldt A., Wissenberg M., Hansen S.M., et al. Clinical predictors of shockable versus non-shockable rhythms in patients with out-of-hospital cardiac arrest. Resuscitation. 2016;108:40–47. doi: 10.1016/j.resuscitation.2016.08.024. [DOI] [PubMed] [Google Scholar]
- 22.Empana J.-P., Jouven X., Lemaitre R., et al. Marital status and risk of out-of-hospital sudden cardiac arrest in the population. European Journal of Preventive Cardiology. 2008;15:577–582. doi: 10.1097/HJR.0b013e3283083e04. [DOI] [PubMed] [Google Scholar]
- 23.Empana J., Jouven X., Lemaitre R., et al. Clinical depression and risk of out-of-hospital cardiac arrest. Archives of internal medicine. 2006;166:195–200. doi: 10.1001/archinte.166.2.195. [DOI] [PubMed] [Google Scholar]
- 24.Allan K.S., Morrison L.J., Pinter A., et al. Unexpected high prevalence of cardiovascular disease risk factors and psychiatric disease among young people with sudden cardiac arrest. Journal of the American Heart Association. 2019;8 doi: 10.1161/JAHA.118.010330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hulleman M., Oving I., Homma P.C., et al. The contribution of comorbidity and medication use to poor outcome from out-of-hospital cardiac arrest at home locations. Resuscitation. 2020;151:119–126. doi: 10.1016/j.resuscitation.2020.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Ishida T., Miyazaki K., Yukawa T., et al. Etiology of out-of-hospital cardiac arrest in psychiatric patients: Chart review. Psychiatry and clinical neurosciences. 2019;73:243–247. doi: 10.1111/pcn.12813. [DOI] [PubMed] [Google Scholar]
- 27.Ko D.T., Qiu F., Koh M., et al. Factors associated with out-of-hospital cardiac arrest with pulseless electric activity: a population-based study. American heart journal. 2016;177:129–137. doi: 10.1016/j.ahj.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 28.Rajan S., Folke F., Hansen S.M., et al. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation. 2016;114:157–163. doi: 10.1016/j.resuscitation.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 29.Wissenberg M., Hansen C.M., Folke F., et al. Survival after out-of-hospital cardiac arrest in relation to sex: a nationwide registry-based study. Resuscitation. 2014;85:1212–1218. doi: 10.1016/j.resuscitation.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 30.Barcella C.A., Mohr G., Kragholm K., et al. Risk of out-of-hospital cardiac arrest in patients with bipolar disorder or schizophrenia. Heart. 2021 doi: 10.1136/heartjnl-2020-318078. [DOI] [PubMed] [Google Scholar]
- 31.Rajan S., Wissenberg M., Folke F., et al. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation. 2016;134:2095–2104. doi: 10.1161/CIRCULATIONAHA.116.024400. [DOI] [PubMed] [Google Scholar]
- 32.Nolan J., Soar J., Eikeland H. The chain of survival. Resuscitation. 2006;71:270–271. doi: 10.1016/j.resuscitation.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 33.Whooley M.A., Wong J.M. Depression and cardiovascular disorders. Annual review of clinical psychology. 2013;9:327–354. doi: 10.1146/annurev-clinpsy-050212-185526. [DOI] [PubMed] [Google Scholar]
- 34.Seligman F., Nemeroff C.B. The interface of depression and cardiovascular disease: therapeutic implications. Annals of the New York Academy of Sciences. 2015;1345:25–35. doi: 10.1111/nyas.12738. [DOI] [PubMed] [Google Scholar]
- 35.Adibfar A., Saleem M., Lanctot K., Herrmann N. Potential biomarkers for depression associated with coronary artery disease: a critical review. Current molecular medicine. 2016;16:137–164. doi: 10.2174/1566524016666160126144143. [DOI] [PubMed] [Google Scholar]
- 36.Fleetwood K., Wild S.H., Smith D.J., et al. Severe mental illness and mortality and coronary revascularisation following a myocardial infarction: a retrospective cohort study. BMC medicine. 2021;19:1–13. doi: 10.1186/s12916-021-01937-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.De Hert M., Detraux J., Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues in clinical neuroscience. 2018;20:31. doi: 10.31887/DCNS.2018.20.1/mdehert. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vohra J. Heart; Lung and Circulation: 2020. Sudden Cardiac Death in Schizophrenia: A Review. [DOI] [PubMed] [Google Scholar]
- 39.Risgaard B., Waagstein K., Winkel B.G., et al. Sudden cardiac death in young adults with previous hospital-based psychiatric inpatient and outpatient treatment: a nationwide cohort study from Denmark. The Journal of clinical psychiatry. 2015;76:1122–1129. doi: 10.4088/JCP.14m09742. [DOI] [PubMed] [Google Scholar]
- 40.Weeke P., Jensen A., Folke F., et al. Antipsychotics and associated risk of out-of-hospital cardiac arrest. Clinical Pharmacology & Therapeutics. 2014;96:490–497. doi: 10.1038/clpt.2014.139. [DOI] [PubMed] [Google Scholar]
- 41.Abdulhay N.M., Totolos K., McGovern S., et al. Socioeconomic disparities in layperson CPR training within a large US city. Resuscitation. 2019;141:13–18. doi: 10.1016/j.resuscitation.2019.05.038. [DOI] [PubMed] [Google Scholar]
- 42.Huffman J.C., Celano C.M., Beach S.R., Motiwala S.R., Januzzi J.L. Depression and cardiac disease: epidemiology, mechanisms, and diagnosis. Cardiovasc Psychiatry Neurol. 2013;2013 doi: 10.1155/2013/695925. 695925- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piña I.L., Di Palo K.E., Ventura H.O. Psychopharmacology and cardiovascular disease. Journal of the American College of Cardiology. 2018;71:2346–2359. doi: 10.1016/j.jacc.2018.03.458. [DOI] [PubMed] [Google Scholar]
- 44.Scottish Government: Scottish Out-of-Hospital Cardiac Arrest data linkage project: 2018-2019 results.
- 45.Dobbie F., MacKintosh A.M., Clegg G., Stirzaker R., Bauld L. Attitudes towards bystander cardiopulmonary resuscitation: Results from a cross-sectional general population survey. PloS one. 2018;13 doi: 10.1371/journal.pone.0193391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blom M.T., Oving I., Berdowski J., van Valkengoed I.G., Bardai A., Tan H.L. Women have lower chances than men to be resuscitated and survive out-of-hospital cardiac arrest. European heart journal. 2019;40:3824–3834. doi: 10.1093/eurheartj/ehz297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Feng D., Li C., Yang X., Wang L. Gender differences and survival after an out-of-hospital cardiac arrest: a systematic review and meta-analysis. Internal and Emergency Medicine. 2020:1–11. doi: 10.1007/s11739-020-02552-4. [DOI] [PubMed] [Google Scholar]
- 48.Lei H., Hu J., Liu L., Xu D. Sex differences in survival after out-of-hospital cardiac arrest: a meta-analysis. Critical Care. 2020;24:1–13. doi: 10.1186/s13054-020-03331-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mitchell A.J., Lawrence D. Revascularisation and mortality rates following acute coronary syndromes in people with severe mental illness: comparative meta-analysis. The British Journal of Psychiatry. 2011;198:434–441. doi: 10.1192/bjp.bp.109.076950. [DOI] [PubMed] [Google Scholar]
- 50.Barcella C.A., Mohr G.H., Kragholm K.H., et al. Out-of-hospital cardiac arrest in patients with and without psychiatric disorders: differences in use of coronary angiography, coronary revascularization, and implantable cardioverter-defibrillator and survival. Journal of the American Heart Association. 2019;8 doi: 10.1161/JAHA.119.012708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sanders A.B. Cardiac arrest and the limitations of clinical trials. Mass Medical Soc. 2011 doi: 10.1056/NEJMe1108108. [DOI] [PubMed] [Google Scholar]
- 52.Eisenberg M., Lippert F., Shin S., et al. Utstein Abbey; Stavanger, Norway: 2016. Improving survival from out-of-hospital cardiac arrest: a call to establish a global resuscitation alliance. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.