Abstract
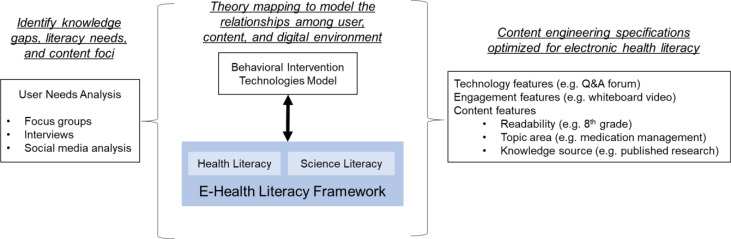
Women of low income and education have lower levels of peripartum depression (PPD) literacy, limiting their ability to recognize symptoms and make informed healthcare decisions. Existing digital solutions and underlying development frameworks for PPD lack an integrative approach addressing health literacy and related disparities. Therefore, we develop an integrative framework for digital content engineering in PPD self-management consisting of (a) user needs analysis, (b) inclusion of eHealth literacy principles (science and health literacy), and (c) mapping user needs to the Behavioral Intervention Technology model. Results revealed that perinatal women seeking mental health care prefer information in multisensory formats, and knowledge needs were identified in areas such as medication management and coping with abnormal results. Results were mapped to eHealth literacy features of whiteboard videos covering essential PPD knowledge, and social media features where patients can articulate information needs. Initial evaluation of proposed features against existing PPD self-management solutions are discussed.
Introduction
Peripartum depression (PPD) affects approximately one out of 10 women in the United States [1], and may cause significant maternal and neonatal morbidity [2]. PPD can affect any woman, but those with characteristics such as belonging to minority groups or of low socioeconomic status (SES) are the most vulnerable [3]. Additionally, women of minority groups such as African-Americans and Latinas are likely to experience disparities in accessing and completing adequate treatment [4]. Digital health technologies have been touted as a viable solution that can improve access to PPD care, and previous research has tested such solutions in the areas of PPD screening [5] and remote delivery of therapy programs [6]. Other areas of PPD care where digital interventions have been explored are self-monitoring of mental health status [7], and providing of social support during pregnancy [8]. Results from these previous interventions show that digital solutions can improve the management of PPD and lead to better mental health outcomes for perinatal women [9].
The indispensable role of health literacy in reducing disparities related to PPD is well-established. For example, low health literacy can adversely impact women’s ability to correctly recognize depression symptoms [10] and to proactively initiate the seeking of help and information for depression and other mental health disorders [11, 12]. Low health literacy is also associated with less understanding of PPD treatment options [10]. And, it has been shown that women with low literacy are likely to experience adverse socioeconomic conditions such as employment insecurity [13], making it more difficult to access mental health care resources. Within the context of PPD, existing work that evaluates digital health technology interventions includes randomized controlled trials [14], feasibility studies [15], and qualitative studies [16, 17] regarding interventions such as applications and text messages. Some of these studies have shown that health literacy is an important factor in women’s engagement with digital information sources. For example, Guendelman and colleagues [17] explored the role of eHealth literacy in disadvantaged perinatal women’s engagement with digitalhealth-seeking activities, and found that it was positively correlated with higher web-based seeking activities. A qualitative study by Pineros-Leano and colleagues [16] also indicated that clinic staff viewed reduction in literacy barriers as an advantage of having women complete PPD screening evaluations through an electronic tablet format. Clinic staff specifically mentioned the abilities to swiftly adapt screening questions to multiple languages, and to have them read aloud to the patient, as unique literacy components offered by the tablet. Although some of these studies briefly mention examples of how digital tools can address health literacy factors, existing literature underexplores the development and application of content engineering methods guided by health literacy principles for PPD digital health solutions.
While previous research shows that digital interventions can improve PPD health outcomes for vulnerable populations [9], it is now well known that sometimes digital health technologies themselves can create new disparities or exacerbate existing ones [18]. This phenomenon has been termed a “digital divide” in healthcare [19], and it refers to how the benefits of digital health solutions do not always reach all populations, including the ones who can benefit the most from them. In the case of PPD, existing literature [17] indicates health literacy barriers can prevent some women from fully enjoying the benefits of digital health technology solutions. In order to prevent such inequities and facilitate increased comprehension and engagement with digital information resources, the purpose of this study is to outline an integrative content engineering framework to supplement existing design and development processes of PPD digital solutions. To achieve this, we analyze women’s information and technology needs regarding PPD through the lens of health literacy theory. Our aim is to contribute new knowledge towards the production of easily digestible digital content that can increase women’s knowledge regarding PPD, and ultimately result in improved health outcomes for this population. We incorporate principles from the eHealth literacy framework (specifically, learning categories and the literacy domains of health and science) into the behavior intervention technology model. This allows us to propose and outline eHealth literacy features which present essential PPD information in an engaging and minimalist manner (examples: whiteboard videos and social media channels), and which can vastly improve women’s knowledge and understanding of this important condition.
Methods
Theoretical Rationale: eHealth Literacy
Health literacy is a term that has recently undergone a redefinition in August 2020 by the U.S. Department of Health and Human Services’ Healthy People 2030 initiative [20]. The term has been expanded to include both personal health literacy and organizational health literacy. Personal health literacy is “the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others” [20], while organizational health literacy is “the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others” [20]. This new definition is meant to highlight the important role of organizations in enabling individuals to reach optimal levels of health literacy.
With the rapid rise in use of digital health technologies, an additional separate term was created to reflect how health literacy fits into this new digital health landscape. The term is electronic health literacy (or eHealth literacy), and is defined as “the ability to search, locate, understand and use health information through electronic resources and use this knowledge to resolve health-related problems” [21]. Some theoretical frameworks have been derived to further elaborate on the concept of eHealth literacy. One of the earliest is Norman and Skinner’s “Lily Model’’ [21], which establishes six types of literacy (traditional, information, health, science, media, and computer) as its subcomponents. Chan and Kaufman [22] expanded on this framework and created the “eHealth Literacy Framework” by addition of cognitive elements from “Bloom’s Taxonomy” [23], which is extensively used to plan and execute educational objectives. It is a collection of action words that describe how a user processes and synthesizes new knowledge [23] and contains six categories of learning, from the simple level of remembering to the complex level of creating. Additional literacy skills and factors in predicting patient’s use of health information technology were also added to include privacy and security concerns, need for information and self-management, computer anxiety, and convenience and advantages of information from health professionals [24,25].
While there are multiple health literacy frameworks, Chan and Kaufman’s offers the most user-ready, systematic process of attributing different literacy domains and cognitive tasks to digital health features. It allows developers to determine at what cognitive level each health literacy domain is applied in digital features. In this paper, we utilize this framework in conjunction with our Digilego framework, which comprises of user needs analysis and BIT model [26] to develop theory-driven digestible digital solutions for PPD management.
Figure 1 presents an overview of out integrative framework. The main components of the framework-(a) mixed-methods needs analysis, (b) theory mapping, and (c) content specifications are as discussed below.
Figure 1:
Incorporation of eHealth Literacy Framework into PPD-specific Digital Health Technologies
User Needs Analysis: We conducted a mixed-methods user needs analysis consisting of focus groups, interviews, and social media analysis. While these datasets were originally produced during previous work [27, 28], in this study we use them to inform the mapping of health literacy digital features to the condition of PPD. Two focus groups were conducted with a total of nine patients seeking prenatal care at a Maternal and Fetal Medicine clinic in Houston, TX. Each session lasted approximately thirty minutes. Additionally, ten patients were individually interviewed. The purpose of the focus groups and interviews was to discover themes regarding the use of digital technologies in the self-management of mental health during the peripartum period. They followed a semi-structured format in which question guides were used to facilitate open discussion. Question guides included the topic of educational content and design, the information they receive from currently available products, and their current knowledge of depression (example questions: “What kind of information do you actually get from these apps?”, “How would you like any educational materials of the app to be prepared?). Ground theory analysis was used to extract themes from focus group and interview recordings, in which open coding was done on a line-by-line basis to derive the concepts being brought up by the participant. This was followed by axial coding, in which patterns and relationships between concepts were delineated to produce major themes. Information from our focus groups and interviews was complemented with analysis from social media data. We chose to analyze online PPD forums from the websites of BabyCenter [29] and What To Expect [30]. Both of these websites are highly popular with pregnant women, and host very active social forums. While women do not have to be diagnosed with PPD in order to participate in the PPD-specific forums, inclusion of diagnosed and non-diagnosed women in our social media sample allows us to model our literacy features towards any woman who is seeking mental health resources. A total of 5,532 posts were extracted from What to Expect, and 56,483 posts from BabyCenter. We manuallylabeled 850 user posts with the following five categories: Breastfeeding, Family and Friends, Medications, SymptomDisclosure, and Social Support. Similar to our focus groups and interviews, these categories were derived using grounded theory analysis. We then applied machine learning (ML) models to scale up the qualitative labels to the entire dataset. We specifically applied three ML classifiers to our labeled dataset: Logistic Regression (LR), RandomForest (RF), and Support Vector Machine (SVM). Our automatic text classification was multilabel, meaning multiplecategories were allowed per each user post. To achieve this, we applied the one-vs-the-rest multilabel strategy, wherea binary classifier is trained per category, and then categories are fitted against each other. Our automatic text classification was completed using Python’s sciKit-learn package [31]. The classifiers were evaluated with the measures of recall, precision, and F1 score. After evaluation, we applied the best performing model to the previouslyunlabeled dataset from BabyCenter.
Mapping Health Literacy to PPD: We then employed Mohr’s Behavior Intervention Technology (BIT) Model to incorporate health literacy principles into PPD digital features. This model asks the five questions of Why? How? What? and When? This model can be easily applied to not only the general technology development process but also to specific components of the technology [32]. To help us answer the question of How?, we have used the literacy skills and learning categories previously described as part of the eHealth Literacy Framework. We then finalized a set of PPD literacy features to be integrated with our digital solution, MomMind [28]. An example that illustrates this mapping process is: the task of articulating a question about perinatal mental health through the literacy feature of social media forums is related to the eHealth Literacy Framework cognitive task of analyzing information within the literacy domain of health.
Initial Evaluation: We have also conducted an initial market evaluation of our proposed features against literacy features in existing PPDapplications, as measured by their reading grade level and cognitive task complexity. To
evaluate the readinggrade level of the application’s content, we used the Flesch-Kincaid readability test [33]. This is a measure that is widely used, and it is based on a mathematical equation factoring the text’s total words, syllables, and sentences. Scores of the test range from 0-100, with lower scores indicating a more difficult reading level and higher scores indicating an easier reading level. Cognitive task complexity was determined through the six categories of learning described in the eHealth literacy framework (i.e., understanding, applying, evaluating). This evaluation can help guide future researchers and developers in assigning the appropriate complexity level of their health literacy content.
Results
a). User Needs Analysis
Focus Groups and Interviews
The majority of our focus group and interview participants were young: 10 were 25-34 years old, five were 18-24 years old, and four in the category of 35-44 years old. The ethnical composition of our sample was: seven identified as Hispanic, six as Black, four as White, one as Asian, and one as Other. One participant had an education level of some high school, three participants were high school graduates, five participants had some college credit, five had an associate’s degree, four had received technical training, and one had a bachelor’s degree. 14 out of 19 participants were low-income women. The main source of pregnancy information for participants was the internet (n=17). 11 participants reported seeking additional information from non-digital sources like their doctors or friends and family. Our focus groups and interviews revealed various literacy themes, including preferred formats for educational materials. The majority of participants preferred to consume educational content through dynamic formats (e.g., slide shows, videos, audio) that would make the process of understanding the content more amenable to them. This is illustrated in Comments 1 and 2. Such formats were also preferred because they are a good fit for the busy schedules of expectant and new mothers.
Comment 1: “… kind of like how it is now through a slideshow or, you know, just kind of something similar tothat. Short videos.”
Comment 2: “If you could actually listen to them instead of reading, it’s better because I’m a mother so I don’t always have time to read.”
Participants also mentioned the importance of separating topics into sub-topics for a well-paced presentation of the material (Comment 3). This is in line with previous research that suggests separating information into blocks of about seven units makes it easier for the learner to retain information in memory [34].
Comment 3: “Well, when I was in school, I started off like the main topic and then I have bulletins that will help break down. You know, okay, like if it was for a symptom it brings it down to like, what I should do, or how I should treat it, any medication… broken down to the bullets or sections.”
Participants also expressed the at times frustrating experience of following up with their doctors after having read information from digital sources (e.g., social media). It was difficult for them to discern when to trust these sources, and when to contact their doctors if such sources indicated a possibly abnormal event in their pregnancy. This indicates a barrier for participants in using the information they receive from non-traditional sources, as Comment 4 shows.
Comment 4: “Sometimes I’ll come to my doctor (with the app) and show ‘Look, this says this is not normal’ and they’ll say ‘Oh no, don’t trust those things’. Well, then I don’t want to bug you every five minutes for the nine months we get to go through this. I was told this would not happen to me.”
Social Media Analysis
Evaluation of our selected ML models indicated that the RF model had the best performance (Table 1). Therefore, we applied this model to predict categories for user comments in our unlabeled dataset of 56,484 user posts from BabyCenter. The category used most by our chosen model was “Social Support” with 50,337 comments, followed by “Medications” with 10,499. “Symptom Disclosure” was applied to 6522 posts, and “Family and Friends” to 2275 posts. The least used category was “Breastfeeding” with 532 comments. The high frequency of the “Social Support” category indicates that women use channels such as online social forums both to receive and provide support regarding PPD at various levels: emotional (words of encouragement), informational (sharing of scientific and health concepts regarding PPD), and instrumental (practical tools to help manage PPD, such as relaxation techniques). Therefore, it is
Table 1-. Automatic Text Classification Model Performance.
| Model | |||||||||
| Category | Logistic Regression | Random Forest | Support Vector Machine | ||||||
| Precision | Recall | F1 Score | Precision | Recall | F1 Score | Precision | Recall | F1 Score | |
| Family and Friends | 0.89 | 0.59 | 0.71 | 0.86 | 0.67 | 0.75 | 0.80 | 0.77 | 0.78 |
| Medications | 0.95 | 0.73 | 0.83 | 0.93 | 0.83 | 0.88 | 0.88 | 0.78 | 0.83 |
| Symptom Disclosure | 0.71 | 0.68 | 0.69 | 0.72 | 0.70 | 0.71 | 0.67 | 0.65 | 0.66 |
| Social Support | 0.62 | 0.85 | 0.72 | 0.64 | 0.83 | 0.73 | 0.68 | 0.72 | 0.70 |
| Breastfeeding | 1.00 | 0.26 | 0.41 | 0.98 | 0.66 | 0.79 | 0.98 | 0.56 | 0.71 |
important that discussion participants are able to critically process the information from such channels by having sufficient baseline knowledge about the condition. A specific health literacy component that we can derive from this result is that all women need a simple introduction to PPD that covers essential information such as its definition, symptoms, and possible treatments. The high number of “Medications” post also indicates that women who seek PPD care need educational materials that will help them understand practical topics such as how to better managetheir medication (i.e., different medication options, usual dose, frequency) and the medication effects on breastfeedingand baby’s health.
b). Theory mapping
Table 2 shows our mapping of the BIT model to health literacy components for PPD. The goal of incorporating health literacy components into the content of our educational platform is to make our content as learnable as possible to the majority of women. Ultimately, this will allow them to use new knowledge to make the best decisions about their mental health (i.e., deciding to disclose symptoms to their doctors) and sustain positive health behaviors (i.e., routine mental health screening). To accomplish the goal of making our content highly learnable, we will follow results from previous research on education and psychology. For example, studies have shown that presenting content to the user in short segments helps improve long-term memory retention [34, 35]. Therefore, our content will be presented in brief whiteboard videos. As also indicated by our participant demographics, the education level of our participants ranged from some high school to a college degree. To assure that our materials are written at a literacy level that can be well understood by all, we have selected to write our educational modules at a reading level of eighth grade.
Table 2-. Behavioral Intervention Technology Model Mapping to Health Literacy for PPD.
| BIT Component | Mapping to PPD (Examples) |
| Why | Improving PPD health literacy by increasing user knowledge. Aim is for the user to access and retain educational materials about PPD. |
| How (conceptual) | The eHealth Literacy Framework, which combines six categories of literacy (health literacy being one of them) and six categories of learning. Overall, this framework represents 36 unique ways to engage users into improving their health literacy. Example: Participant’s health literacy on PPD can be improved by helping them understand the differences between various treatment options, allowing them to make the best decision with their doctors. |
| What | Educational Modules: Separation of content into brief multiple units Allow user to consume content at their own pace (ability to pause, stop) Providing user opportunities to articulate what they have learned (interactivity with providers and peers, journaling) |
| How (Technical) | Multimedia storytelling techniques (Whiteboard videos, presentations) Maximum of eighth grade reading level (as determined by the Flesch-Kincaid reading test) Avoidance of technical jargon Aesthetically pleasing fonts and colors Goal Setting Progress Monitoring |
| When | Educational modules delivered once a week to prevent user fatigue while maintaining user engagement. |
c). Content specifications
Table 3 shows a granular mapping of the eHealth literacy framework to proposed PPD digital modules in our MomMind digital platform. In this mapping, we have concentrated on the specific literacy domains of health literacy and science literacy. Our results indicate that our platform has the potential to improve our users’ literacy levels in these domainsby helping them achieve the cognitive tasks of understanding important PPD health topics and science concepts.
Table 3-. Mapping of the eHealth Literacy Framework to PPD Digital Modules.
| Digital Features (MomMind Modules) | Applicable Literacy Domain (s) | Literacy Techniques | Cognitive Task(s) | Media Options and Example User Interactions |
| “My Diary”: journaling feature where user can freely document their thoughts and emotions. | Science, Health | Writing diary entry | Remembering events; Analyzing events | Text, Audio, Pictures Example: User writes diary entry about activity they did with baby and includes picture |
| “Mom Talk”: Social forum component where participants can discuss PPD topics | Science, Health | Reading other users’ post; Writing by creating posts or replying to posts |
Analyzing other’s posts; Evaluating information in other’s post |
Text, Audio, Video Example: User discusses an article about healthy sleeping habits with forum peers |
| “My Care”: represents the clinical profile of the user, including provider profile and medication information | Health | Reading provider’s answers; Writing questions to providers |
Analyzing answers from providers | Text Example: User can learn about PPD medication management by asking their doctor about potential side effects through the “Ask your provider a question!” form. |
| “My Library”: repository of evidence-based educational PPD information | Science, Health | Viewing educational content | Understanding PPD concepts presented in multimedia educational videos | Text, Video, Audio Example: User can learn about hormonal changes in the peripartum period through viewing a whiteboard video. |
| “How am doing today?”: PPD survey repository | Health | Reading survey questions; Selecting best answer |
Understanding survey questions; Evaluating survey results |
Text Example: User completes PPD screening presentedin written format |
d). Initial Evaluation
Our initial market evaluation of literacy features in our proposed digital platform for PPD management against five selected commercial applications for PPD management [36-40] showed that most applications addressed health literacy through educational modules and brief tips for PPD symptom management (Table 4). It was found that two of the applications had content written for the college readinglevel, one had content written for the high school reading level, and one had content written for the eight-grade level.The content of MomMind was written at the sixth-grade level, making it the easiest to read. These results indicate thatmost available market applications for PPD management have content which will be most useful to women of high education levels. The application which had the highest level of cognitive task (applying) was PPD Act, which presented weekly practical tips to its users. Three applications (Postpartum Depression, Postpregnancy Recovery, and MomMind) had the lowest complexity level of cognitive task from the eHealth literacy framework by presenting PPD information that the user can recall from their long-term memory if needed.
Table 4-. Initial Evaluation of PPD Market Products and MomMind.
| Application Name | Example of Digital Feature related to PPD Health Literacy | Sample Health Literacy Content | Flesch-Kincaid Reading Grade Level |
Cognitive Task |
|---|---|---|---|---|
| Moment Health | “Community”: Link to Facebook group where participants can write posts to discuss PPD topics and ask questions to fellow new parents. | Not Available | Not Applicable | Understanding PPD-related information from user posts |
| PPD Act | Weekly tips to better manage PPD symptoms. | “Protected sleep time is critical for women thatsuffer from PPD. Aim for at least 5 hours of uninterrupted sleep at night” | 10.1 | Applying weekly tips into routine behavior |
| MGHPDS | Link to the Massachusetts General Hospital’s Center for Women’s Mental Health website, containing recent PPD research articles. | “Although new mothers describe breastfeeding asa meaningful and fulfilling aspect of caring for their infants, breastfeeding is also a common source of stress and anxiety.” | 13.1 | Analyzing information from research articles |
| Postpartum Depression | PPD education modules which present information in a Question-and-Answer format, and modules with recommendations to alleviate PPD symptoms. | “Postpartum depression is a mood disorder that can affect women after childbirth. Mothers withpostpartum depression experience feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for them to complete dailycare activities for themselves or for others” |
13.7 | Remembering information from PPD education modules |
| Post Pregnancy Recovery | Topic modules concentrating on physical recovery in the postpartum period; one module is dedicated to PPD information. | “The postpartum period refers to the first six weeks after childbirth. This is a joyous time, butit’s also a period of adjustment and healing for mothers. During these weeks, you’ll bond with your baby and you’ll have a post-delivery checkup with your doctor” |
8 | Remembering information from PPD topic modules |
| MomMind | “My library” (described in Table 2). | “In fact, 6% of pregnant women and 10% of newmothers experience anxiety. This can occur along with depression, or on its own.” |
6.8 | Recall information from library content |
Discussion
Our user needs analysis provided us with an in-depth dwelling into the world of perinatal women who are seeking mental health resources and the hurdles they face in their journey. Our target population (low-income women seeking mental health care) has an educational level of mostly some college, but the lowest education level achieved was some high school. Most were also low-income and of minority groups. Overall, these characteristics indicate to us that any educational materials presented to this population should be at a maximum reading level of 8th grade, to assure thatthe materials can be understood by everyone. We also found that this population was most interested in learning about topics that served as gateways into further discussion and information about mental health and PPD (breastfeeding, family environment, medications). Our user needs analysis could have been strengthened by including in our focus group and interview samples women of different backgrounds who have been diagnosed with PPD.
Our theory mapping of the BIT model and the eHealth literacy framework to literacy features for PPD allowed us to model the relationship between our target users, our content, and the digital environment. This mapping suggests that cognitive tasks such as remembering, analyzing, and applying PPD information would increase our user’s PPD health and science literacy. From this mapping, we derived the following two categories of health literacy features that should be included in digital solutions for PPD self-management:
-
a)
Brief, multimedia educational materials: As indicated by our participant’s focus group and interview comments, participants prefer to receive information in a manner that is not just text. They specifically mentioned video and audio as formats that are engaging. They also suggested information should be broken down into bite-size chunks that can be consumed in short spans of time. Another conclusion we can make from our user needs analysis is that many women lack essential knowledge on PPD, such as its definition, symptoms, and available treatment. Therefore, our proposed application will contain brief whiteboard videos that will present women with this essential knowledge on PPD.
-
b)
Channels where the user can articulate and analyze information: The combined results of our social media analysis, focus groups, and interviews revealed that the ability to discuss PPD information with peers and providers was an important component in increasing women’s health literacy. For example, our social media analysis revealed that online PPD forums was a very important source of information where women would share knowledge on a wide range of PPD areas, from recommendations on clinical treatment to sharing of local support resources. For this reason, in our proposed digital platform we include the features of a social forum where women can interact with fellow patients from the clinic they are attending, as well as the ability to have bidirectional communication with their providers to ask questions about the peripartum period and PPD.
The strength of our mapping process is that it is based on well-established literacy and technology theories. However, a main limitation of our study is lack of extensive evaluation of our selected literacy features with PPD stakeholders, including patients and clinicians. Additionally, our literacy features should be evaluated across users with high and low levels of health literacy. As part of future steps in our research program, we will focus on implementing these features and evaluating them in formative and summative evaluation studies to understand the effects of our framework on patient engagement, psychosocial outcomes, and PPD self-management capabilities. Our study adds important knowledge that is currently missing in existing literature: it explores the theoretical application of health literacy principles in the development and application of content engineering methods for digital health solutions in PPD management.
Conclusion
Health literacy is an important factor in empowering patients to make the best health decisions and reaching optimal health outcomes. With the rapid rise in use of electronic sources to distribute health information, it is critical that developers and providers incorporate electronic health literacy factors into digital health solutions to assure that such sources can be easily understood and used by the intended target audience. Such literacy factors can range from media type through which the information is delivered to the reading level at which the information is written. The integrative framework we describe in this study allows us to guide the work of future researchers, digital health designers, and developers to determine the ways in which literacy principles and digital features should be engineered. Ultimately, this framework can result in digital health technologies that promote equity in access to health resources.
Acknowledgements
We would like to thank patients and staff at the UTPhysician’s Women’s Center at TMC who participated in this study for their time and insights. Research reported in this publication was partly supported by the National Library of Medicine of the National Institutes of Health under award numbers 1R01LM012974-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Figures & Table
References
- 1.Centers for Disease Control and Prevention. Depression among women. 2020 May. Accessed from: https://www.cdc.gov/reproductivehealth/depression/index.htm.
- 2.Langan RC, Goodbred AJ. Identification and Management of Peripartum Depression. AFP. 2016 May 15;93(10):852–8. [PubMed] [Google Scholar]
- 3.Hanley GE, Park M, Oberlander TF. Socioeconomic status and treatment of depression during pregnancy: a retrospective population-based cohort study in British Columbia, Canada. Arch Womens Ment Health. 2018 Dec;21(6):765–775. doi: 10.1007/s00737-018-0866-6. doi: 10.1007/s00737-018-0866-6. Epub 2018 Jun 2. PMID: 29860622. [DOI] [PubMed] [Google Scholar]
- 4.Lara-Cinisomo S, Clark CT, Wood J. Increasing diagnosis and treatment of perinatal depression in Latinas and African American women: addressing stigma is not enough. Women's Health Issues. 2018 May 1;28(3):201–4. doi: 10.1016/j.whi.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawson A, Dalfen A, Murphy K, Milligan N, Lancee W. Use of Text Messaging for Postpartum Depression Screening and Information Provision. Psychiatric Services. 2019;70(5):389–395. doi: 10.1176/appi.ps.201800269. doi: 10.1176/appi.ps.201800269. PMID: 30717643. [DOI] [PubMed] [Google Scholar]
- 6.Kim DR, Hantsoo L, Thase ME, Sammel M, Epperson CN. Computer-assisted cognitive behavioral therapy for pregnant women with major depressive disorder. Journal of women's health. 2014;23(10):842–848. doi: 10.1089/jwh.2014.4867. doi:10.1089/jwh.2014.4867. PMID: 25268672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doherty K, Barry M, Marcano-Belisario J, Arnaud B, Morrison C, Car J, Doherty G. A Mobile App for the Self-Report of Psychological Well-Being During Pregnancy (BrightSelf): Qualitative Design Study. JMIR mental health; 2018;5(4):e10007. doi: 10.2196/10007. doi:10.2196/10007. PMID: 30482742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niksalehi S, Taghadosi M, Mazhariazad F, Tashk M. The effectiveness of mobile phone text messaging support for mothers with postpartum depression: A clinical before and after study. J Family Med Prim Care. 2018;7(5):1058–62. doi: 10.4103/jfmpc.jfmpc_120_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhat A, Mao J, Unützer J, Reed S, Unger J. Text messaging to support a perinatal collaborative care model for depression: a multi-methods inquiry. General hospital psychiatry; 2018;52:14–20. doi: 10.1016/j.genhosppsych.2018.01.005. PMID: 29494854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fonseca A, Silva S, Canavarro MC. Depression Literacy and Awareness of Psychopathological Symptoms During the Perinatal Period. J Obstet Gynecol Neonatal Nurs. 2017 Mar-Apr;46(2):197–208. doi: 10.1016/j.jogn.2016.10.006. doi: 10.1016/j.jogn.2016.10.006. Epub 2017 Jan 9. PMID: 28082210. [DOI] [PubMed] [Google Scholar]
- 11.Shieh C, Broome ME, Stump TE. Factors associated with health information-seeking in low-income pregnant women. Women & health. 2010 Aug 31;50(5):426–42. doi: 10.1080/03630242.2010.506152. [DOI] [PubMed] [Google Scholar]
- 12.Cheng C, Beauchamp A, Elsworth GR, Osborne RH. Applying the Electronic Health Literacy Lens: Systematic Review of Electronic Health Interventions Targeted at Socially Disadvantaged Groups. J Med Internet Res. 2020 Aug 13;22(8):e18476. doi: 10.2196/18476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zaslow MJ, Hair EC, Dion MR, Ahluwalia SK, Sargent J. Maternal Depressive Symptoms and Low Literacy as Potential Barriers to Employment in a Sample of Families Receiving Welfare: Are There Two-Generational Implications? Women & Health. 2001 Jul 13;32(3):211–51. doi: 10.1300/J013v32n03_03. [DOI] [PubMed] [Google Scholar]
- 14.Shorey S, Ng YPM, Ng ED, Siew AL, Mörelius E, Yoong J, Gandhi M. Effectiveness of a Technology-Based Supportive Educational Parenting Program on Parental Outcomes (Part 1): Randomized Controlled Trial. J Med Internet Res. 2019 Feb 13;21(2):e10816. doi: 10.2196/10816. doi: 10.2196/10816. PMID: 30758289; PMCID: PMC6391716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baumel A, Tinkelman A, Mathur N, Kane JM. Digital Peer-Support Platform (7Cups) as an Adjunct Treatment for Women With Postpartum Depression: Feasibility, Acceptability, and Preliminary Efficacy Study. JMIR mHealth and uHealth. 2018;6(2):e38. doi: 10.2196/mhealth.9482. doi:10.2196/mhealth.9482. PMID: 29439944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pineros-Leano M, Tabb KM, Sears H, Meline B, Huang H. Clinic staff attitudes towards the use of mHealth technology to conduct perinatal depression screenings: a qualitative study. Fam Pract. 2015 Apr;32(2):211–5. doi: 10.1093/fampra/cmu083. doi: 10.1093/fampra/cmu083. Epub 2014 Dec 22. PMID: 25535280; PMCID: PMC7340322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guendelman S, Broderick A, Mlo H, Gemmill A, Lindeman D. Listening to Communities: Mixed-Method Study of the Engagement of Disadvantaged Mothers and Pregnant Women With Digital Health Technologies. Journal of Medical Internet Research. 2017;19(7):e240. doi: 10.2196/jmir.7736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Washington (DC): National Academies Press (US); 2016 Jun 22. Roundtable on the Promotion of Health Equity and the Elimination of Health Disparities; Board on Population Health and Public Health Practice; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine. The Promises and Perils of Digital Strategies in Achieving Health Equity: Workshop Summary. 2, Technology and Health Disparities. Available from: https://www.ncbi.nlm.nih.gov/books/NBK373436/ [PubMed] [Google Scholar]
- 19.Makri A. Bridging the digital divide in health care. The Lancet Digital Health. 2019 Sep 1;1(5):e204–5. [Google Scholar]
- 20.Health Literacy in Healthy People 2030 | health.gov [Internet] [cited 2021 Feb 9]. Available from: https://health.gov/our-work/healthy-people/healthy-people-2030/health-literacy-healthy-people-2030.
- 21.Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. 2006;8(2):e9. doi: 10.2196/jmir.8.2.e9. 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan CV, Kaufman DR. A Framework for Characterizing eHealth Literacy Demands and Barriers. Journal of Medical Internet Research. 2011;13(4):e94. doi: 10.2196/jmir.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bloom’s Taxonomy [Internet] Vanderbilt University. 2010 [cited 2021 Jan 2]. Available from: https://cft.vanderbilt.edu/guides-sub-pages/blooms-taxonomy/
- 24.Koopman RJ, Petroski GF, Canfield SM, Stuppy JA, Mehr DR. Development of the PRE-HIT instrument: patient readiness to engage in health information technology. BMC family practice. 2014 Dec;15(1):1–9. doi: 10.1186/1471-2296-15-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Norgaard O, Furstrand D, Klokker L, Karnoe A, Batterham R, Kayser L, Osborne RH. The e-health literacy framework: a conceptual framework for characterizing e-health users and their interaction with e-health systems. Knowledge Management & E-Learning: An International Journal. 2015;7(4):522–40. [Google Scholar]
- 26.Myneni S, Rogith D, Franklin A. Digilego: A standardized analytics-driven consumer-oriented connected health framework. In International Conference on Social Computing, Behavioral-Cultural Modeling and Prediction and Behavior Representation in Modeling and Simulation. 2018 Jul 10. pp. 263–273. Springer, Cham.
- 27.Zingg A, Carter L, Rogith D, Franklin A, Selvaraj S, Refuerzo J, Myneni S. Digital Technology Needs in Maternal Mental Health: A Qualitative Inquiry. 31st Medical Informatics Europe Conference. 2021. (Unpublished manuscript, Accepted) [DOI] [PubMed]
- 28.Zingg A, Rogith D, Refuerzo J, Myneni S. Digilego for Peripartum Depression: A Novel Patient-Facing Digital Health Instantiation. In: Proceedings of the American Medical Informatics Association 2020 Virtual Annual Symposium. [conference proceedings on the Internet] 2020 November. pp. 14–18. Available from: AMIA 2020 Virtual Annual Symposium Digital Collection https://s4.goeshow.com/amia/annual/2020/index.cfm. [PMC free article] [PubMed]
- 29.BabyCenter. Postpartum Depression and Related Topics [Internet] 2020 [cited 2020 April 8]. Available from: https://community.babycenter.com/groups/a15325.
- 30.What to Expect. About What To Expect[Internet] 2020[cited 2020 April 8]. Available from: https://www.whattoexpect.com/about-what-to-expect/
- 31.sklearn.multiclass.OneVsRestClassifier — scikit-learn 0.23.2 documentation [Internet] [cited 2020 Dec 8]. Available from: https://scikit-learn.org/stable/modules/generated/sklearn.multiclass.OneVsRestClassifier.html.
- 32.Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions. Journal of Medical Internet Research. 2014;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kincaid JP, Fishburne RP, Jr, Rogers RL, Chissom BS. Derivation of new readability formulas (automated readability index, fog count and flesch reading ease formula) for navy enlisted personnel. Naval Technical Training Command Millington TN Research Branch. 1975 Feb 1.
- 34.Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychological Review. 1956;63(2):81–97. doi: 10.1037/h0043158. [DOI] [PubMed] [Google Scholar]
- 35.Thalmann M, Souza AS, Oberauer K. How does chunking help working memory? J Exp Psychol Learn Mem Cogn. 2019 Jan;45(1):37–55. doi: 10.1037/xlm0000578. doi: 10.1037/xlm0000578. Epub 2018 Apr 26. PMID: 29698045. [DOI] [PubMed] [Google Scholar]
- 36.Moment Health. Moment Health, 2018. Vers. 1.2.2. Google Play, https://play.google.com/store/apps/details?id=io.momenthealth.app&hl=en_US.
- 37.PPD ACT. University of North Carolina at Chapel Hill, 2017. Vers. 3.0.0.110. Google Play, https://play.google.com/store/apps/details?id=com.pactforthecure.app.
- 38.MGHPDS. MGH Perinatal Depression Scale, 2017. Vers. 1.0.6. Apple App Store, https://apps.apple.com/us/app/mghpds/id1239621118.
- 39.Postpartum Depression. Pinkdev, 2017. Vers. 1.3. Google Play, https://play.google.com/store/apps/details?id=postnatal.postpartum.depression&hl=en_US.
- 40.Post Pregnancy Recovery. Hilltop_apps, 2018. Vers. 1.0. Google Play, https://play.google.com/store/apps/details?id=com.andromo.dev695852.app777161&hl=en_US.