Abstract
Introduction:
Nicotine and marijuana vaping among U.S. adolescents are public health priorities. Research has assessed demographic and risk factors related to vaping, but there is a dearth of research on protective factors for vaping. Based on the healthy youth development perspective, the developmental assets framework is used to assess cumulative protective factors and vaping in a national sample of adolescents.
Methods:
Data came from the nationally representative Monitoring the Future study, consisting of 12th graders (n=6,982) from the 48 contiguous U.S. states (2017–2019). Past 30–day nicotine and marijuana vaping and developmental assets (low, medium, or high) were examined. Covariates included demographics and other substance use. Weighted descriptive statistics, logistic regression, post-estimation analyses, and multiple imputation were used.
Results:
Students with higher assets were less likely to vape nicotine and marijuana, even after adjusting for covariates. The odds of nicotine vaping were lower for students with medium assets (AOR=0.65, 95% CI=0.54, 0.78) and high assets (AOR=0.22, 95% CI=0.16, 0.29) compared with students with low assets. Similarly, the odds of marijuana vaping were lower for youth with medium assets (AOR=0.54, 95% CI=0.42, 0.69) and high assets (AOR=0.09, 95% CI=0.05, 0.18) compared with low assets. Social competence and positive peer norms were strongly protective against both forms of vaping.
Conclusions:
The healthy youth development perspective applies to the critical issues of nicotine and marijuana vaping among adolescents. Promoting cumulative assets may help prevent vaping among U.S. adolescents, and increasing the specific assets of social competence and positive peer norms could be particularly fruitful.
INTRODUCTION
Nicotine and marijuana vaping among U.S. adolescents are public health priorities. Youth nicotine vaping has reached epidemic proportions,1-4 and increases risk for cigarette use and poor health outcomes.5,6 Marijuana vaping markedly increased in 2018 and 2019, and remains relatively high among U.S. adolescents.2,3 Vaping of tetrahydrocannabinol-containing products is a major concern because of its impact on development, and its link to the recent lung injury epidemic.1
Documenting prevalence and predictors of nicotine and marijuana vaping among U.S. adolescents is essential for prevention.7,8 Yet, there is a dearth of research on factors that protect against vaping; the limited number of studies that have assessed characteristics associated with nicotine and marijuana vaping have focused on demographics and risk factors,6-8 creating a critical need for research on factors that protect against vaping. Research on adolescent health has experienced a foundational shift away from a risk-based focus to a perspective geared towards promoting well-being and protecting against harm.9,10 This healthy youth development (HYD) perspective takes a strengths-based focus,9,11,12 primarily by promoting protective factors that develop strengths, such as competence, confidence, and caring.9,11,13 There are a range of frameworks within the HYD perspective that identify key protective factors linked to healthy development, and these factors protect against substance use as well.14,15 No recent research has applied these frameworks and factors to nicotine and marijuana vaping in a national sample of adolescents. This paper utilizes the developmental assets framework (DAF), based on the HYD perspective, which has previously been applied to other substance use such as cigarette smoking, combustible marijuana use, and alcohol use.16-19 The DAF offers a clear set of measurements and track record for assessing protective factors at the population level,16,20,21 and emphasizes the importance of cumulative factors rather than prioritizing certain factors.20,21
The DAF contends that protective factors can be assessed as internal and external assets, which can be measured dichotomously in order to capture prevalence of low and high levels of assets.16,21 Internal assets include asset subtypes of social competence, positive identity, commitment to learning, and positive values.16,21 Social competence concerns decision-making skills such as resistance to peer pressure.21 Positive identity involves a sense of purpose and satisfaction with life and future.21 Commitment to learning includes school bonding and school engagement.21 Positive values are captured via beliefs about equality and social justice, and helping other people.16 External assets comprise asset subtypes of empowerment, boundaries and expectations, and support.21 Empowerment measures a sense of safety in one’s neighborhood, school, and home.21 Boundaries and expectations can include positive peer influence, including perceived prevalence of substance use among peers.21 Support includes receiving support from family, and having positive family communication, as well as feeling supported by neighbors and having a caring neighborhood.21
This paper examines protective factors (herein labeled as “assets” in accordance with DAF) by assessing cumulative assets via the DAF. As described in the framework and previous research,20,21 more assets provide cumulative protection compared with individual protective factors alone. An emerging area of research builds on seminal healthy development research,22-26 and shows the importance of cumulative assets.17,20,27,28 Internal assets, such as social competence and positive identity, provide the internal resources and skills for adolescents to successfully navigate away from substance use at a young age; external assets provide the opportunity and resources (relationships, communities) for healthy development.12,20,21,27 In short, separate assets protect against issues such as substance use by addressing specific areas of an adolescent’s life, and cumulative assets create a context within which adolescents can thrive (e.g., by healthily responding to stress).12,26,27 Adolescents without these assets are at greater risk to use substances, particularly as a form of coping if they are exposed to stress and adverse experiences.12,27 Research shows that cumulative assets in childhood and adolescence protect against substance use19 and mental health problems in adulthood.20 Those who report low assets experience poorer health and developmental outcomes.20,28 As yet, this cumulative assets measure has not been applied to vaping in a national sample of adolescents.
METHODS
Study Sample
Data came from the nationally representative Monitoring the Future (MTF) study.3 The MTF study includes national, repeated cross-sectional samples of 12th graders from the 48 contiguous U.S. states recruited annually. The current MTF sample is a subset of all 12th graders surveyed in 2017–2019 (N=41,737) who completed 1 MTF questionnaire form among 6 randomly distributed questionnaire forms (n=6,982). These years were chosen because the prevalence of vaping increased at a record pace between 2017 and 2019,29,30 and the single form was chosen because it is the only form that includes protective factor and vaping measures. After removing missing data, the final analytic sample for the primary analyses included 4,590 students. The sample was majority non-Hispanic White (54.3%), followed by 19.5% Hispanic, 11.6% Other, 10.1% non-Hispanic Black, and 4.5% Asian. There were slightly more female participants in the sample (54.6%). This study was approved by the University of Michigan and University of Minnesota IRBs.
Measures
Past 30–day nicotine and marijuana vaping were examined separately. Any past 30–day use is the most common metric for examining current vaping,3 which was assessed by asking: On how many days in the past 30 days did you vape nicotine? and On how many days in the past 30 days did you vape marijuana? (recoded to 1=vaped, 0=did not vape).
A total of 9 DAF assets available in the MTF study were examined, including 5 internal and 4 external assets.16,21 The 9 assets (with DAF asset category labels in parentheses) included decision-making/resistance skills (social competence), life satisfaction (positive identity), sense of self/self-esteem (positive identity), school engagement/school bonding (commitment to learning), values of helping others and equality (positive values), safe school and neighborhood (empowerment), positive peer norms (boundaries and expectations), perceived support and connection with family (support), and positive neighborhood perceptions (support).
Social competence was assessed based on 2 items that asked: If one of your best friends were to offer you a cigarette, would you smoke it? and If one of your best friends were to offer you a marijuana cigarette, would you smoke it? (range: 1=definitely yes to 4=definitely no). The dichotomous cut off corresponded with definitely no for both questions (1=definitely no for both, 0=other). Research on smoking shows youth who do not report “definitive” resistance are susceptible to smoke,31 and youth could be more willing to use substances if they report less than definitely yes.32 Positive identity was assessed via a 4-item scale that included questions such as: How satisfied are you with your life as a whole? (1=completely not satisfied to 7=completely satisfied, α=0.84); an average score of greater than neutral was used for the cut off.16 Positive identity also entails a positive sense of self and self-esteem.21 Positive identity was also assessed via a 2-item scale that included the following questions: Compared to others your age across the country, how do you rate yourself on school ability? and How intelligent do you think you are compared to others your age? (range: 1=far below average to 7=far above average, α=0.85). An average score of greater than average was used for the cut off.16
Commitment to learning was captured via a 5-item scale that included items such as: How do you feel about going to school? (range: 1=I don’t like school at all to 5=I like it very much) and How important do you think the things you are learning in school are going to be for your life? (range: 1=not at all important to 5=very important). The standardized scale α was 0.81, and the dichotomous cut off was based on an average score of quite important/quite a lot or higher (i.e., ≥4).16 Positive values were assessed using a 5-item scale that included questions such as: How important is working to correct social and economic inequalities? and How important is making a contribution to society? (range: 1=not important to 4=extremely important, α =0.74). The dichotomous cut off was based on an average score of important or higher.16
Safety was assessed using a 2-question scale that asked how satisfied respondents were with personal safety in your neighborhood, on your job, and in your school—safety from being attacked and injured in some way and the safety of things you own from being stolen or destroyed in your neighborhood, on your job, or in your school (range: 1=completely not satisfied to 7=completely satisfied, α=0.78). The dichotomous cut off was based on an average score of greater than neutral (i.e., >4). A 5-item scale was used that captured perceptions of the number of peers that used cigarettes, marijuana, alcohol, e-cigarettes/e-pens, and get drunk once per week (range: 1=none to 5=all, α=0.84). The dichotomous measure for anti-substance use peer influence was based on an average score of less than some (i.e., ≤2).
Support was assessed using a single item that asked: How satisfied are you with the way you get along with your family? (range: 1=completely dissatisfied to 7=completely satisfied). The dichotomous cut off was based on anything greater than neutral (i.e., ≥5).16 Support was also assessed by using a single item that asked: How are satisfied are you with the neighborhood where you live? (range: 1=completely dissatisfied to 7=completely satisfied). The dichotomous cut off was based on a score above neutral (i.e., ≥5).
Dichotomous measures were constructed for each asset by determining whether youth possessed a respective asset using the aforementioned cut offs, which corresponded with previous research.16,21 Creating dichotomous measures from continuous scales loses variability,16 but there was good correspondence in prevalence of assets using binary measures compared to measures based on 0.5 SDs above the mean for the continuous distributions. After generating 9 dichotomous variables (representing the 9 assets), a count of the number of assets (range=0–9) was created. A final 3-category variable was generated utilizing an established approach for creating asset categories that captured low, medium, and high levels of assets (1= ≤3 assets, 2= 4–6 assets, 3= ≥7 assets).16,18,21 This categorical breakdown has high sensitivity, particularly in regards to capturing youth with low and high assets.16,21 The 3 groups are herein labeled as low (0–3), medium (4–6), and high (7–10).
Covariates included race/ethnicity (White=reference, Black, Hispanic, Asian, Other), sex (1=female, 0=male), a measure of SES (maximum parental education [1=a parent had college degree, 0=no parent had a college degree]); urbanicity (urban=reference, small city, rural); and college plans measured by whether participants had definitive plans to attend a 4-year college (1=definitely plan to attend, 0=other).33 To account for possible geographic differences such as state marijuana laws, 4 dichotomous measures for region of country were included as covariates: West (reference group), Upper Midwest, South, and Northeast. Differences in access to vaping products were also accounted for, which is strongly associated with vaping among youth,34 by including a measure for ease of obtaining a vaping device (1=very/fairly easy, 0=other). Additional control variables included dichotomous measures (1=yes, 0=no) for past 30–day cigarette, alcohol, and marijuana (not including vaping) use, as well as binge drinking in the past 2 weeks (≥5 drinks in a row).
Statistical Analysis
Analyses consisted of descriptive statistics, logistic regression, and post-estimation analyses. Separate logistic regressions for nicotine and marijuana were conducted. All covariates were used for both nicotine and marijuana, except 30-day marijuana use was excluded (not including vaping) from the marijuana vaping model because of the extreme association between other forms of marijuana use and marijuana vaping.2 The reference group in the regression models was the low assets group. Two regression models for each outcome were examined: Model 1 included demographics, regions, and vaping device access, and Model 2 added substance use (current cigarette, alcohol, and marijuana use, and current binge drinking) to show the associations of assets even after adjusting for other current substance use. Post-estimation analyses were conducted to examine predicted probabilities of vaping, adjusting for demographics. Predicted scores across all levels of assets were compared (Bonferroni method was used to account for multiple testing). Interactions between asset levels and demographics (race/ethnicity, sex, and parental education) were tested; no interactions were statistically significant (results not included). Weights were used to account for the complex, stratified survey design of the MTF study. Multiple imputation was used for missing data. Supplemental analyses: (1) adjusted for cohort year (2017, 2018, or 2019) and (2) examined the prevalence and associations for each of the 9 individual assets (using multivariable logistic regression). All analyses were completed with Stata, version 15 software.
RESULTS
The prevalence of current vaping was 18.7% for nicotine and 8.3% for marijuana (Table 1). Most youth had medium assets (55.0%). Other prevalence levels were 25.9% for low assets, and 19.1% for high assets. Approximately 51.7% of the sample had a parent with a college degree. Most students lived in small cities (e.g., suburbs; 45.8%), followed by urban (34.9%) and rural areas (19.3%). The majority of students had definitive plans to attend a 4-year college (56.8%).
Table 1.
Weighted Descriptive Statistics for Monitoring the Future Sample, 2017–2019
| Variables | % or Mean (SE) |
|---|---|
| Vaping outcomes (past 30 days) | |
| Nicotine | 18.7% (1.02) |
| Marijuana | 8.3% (0.56) |
| Protective factor levels | |
| Low (0–3) | 25.9% (0.73) |
| Medium (4–6) | 55.0% (0.75) |
| High (7–9) | 19.1% (0.67) |
| Race/ethnicity | |
| White | 50.5% (2.21) |
| African American/Black | 12.1% (1.08) |
| Hispanic | 21.3% (2.03) |
| Asian | 4.3% (0.52) |
| Other | 11.8% (0.76) |
| Sex | |
| Male | 47.0% (0.93) |
| Female | 53.0% (0.93) |
| Parental education | |
| Some college or less | 48.3% (1.49) |
| College degree or more | 51.7% (1.49) |
| Urban/rural location | |
| Urban | 34.9% (3.47) |
| Small urban | 45.8% (3.35) |
| Rural | 19.3% (1.48) |
| College plans | |
| Definitive plans to attend 4 year college | 43.2% (1.08) |
| Other | 56.8% (1.08) |
| Region of country | |
| South | 40.6% (2.19) |
| Northeast | 16.6% (1.62) |
| Upper Midwest | 22.6% (1.68) |
| West | 20.2% (1.94) |
| Easy to obtain nicotine vaping device | 76.9% (1.03) |
| Past 30-day substance use | |
| Cigarettes | 8.0% (0.47) |
| Alcohol | 32.2% (0.97) |
| Marijuana (other than vaping) | 22.6% (0.78) |
| Binge drinking in past 2 weeks | 12.0% (0.64) |
Notes: Unweighted N=6,982. Weights were used to generate estimates, which account for the complex survey design of the Monitoring the Future study; SEs are in parentheses; multiple imputation was used for missing data.
Table 2 presents logistic regression results for nicotine vaping. In Model 1 (without substance use covariates), compared with youth with low assets, the odds of nicotine vaping were lower for students with medium assets (AOR=0.65, 95% CI=0.54, 0.78) and high assets (AOR=0.22, 95% CI=0.16, 0.29). In Model 1, each race/ethnicity had lower odds of vaping compared with non-Hispanic White students, and female students had lower odds relative to male students. Ease of obtaining a vaping device was positively associated with vaping. In Model 2 (with substance use covariates), compared with youth with low assets, the odds of nicotine vaping were lower for students with high assets (AOR=0.49, 95% CI=0.35, 0.69), but the difference between low and medium assets was nonsignificant after adjusting for other substance use. Past 30–day use of cigarettes, alcohol, and marijuana (other than vaping) was associated with higher odds of vaping. Binge drinking was associated with higher odds of vaping. Associations remained nearly identical and statistically significant in analyses that adjusted for cohort year.
Table 2.
Weighted Logistic Regression Results for Current Nicotine and Marijuana Vaping Among U.S. 12th Graders (Baseline Years 2017–2019)
| Nicotine vaping | Marijuana vaping | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Variables | AOR (95% CI) | AOR (95% CI) | ||
| Level of assets | ||||
| Low (reference group) | – | – | – | – |
| Medium/high | 0.65 (0.54, 0.78) | 0.88 (0.70, 1.11) | 0.54 (0.42, 0.69) | 0.63 (0.48, 0.82) |
| High | 0.22 (0.16, 0.29) | 0.49 (0.35, 0.69) | 0.09 (0.05, 0.18) | 0.16 (0.08, 0.31) |
| Race/ethnicity (vs White) | ||||
| African American/Black | 0.32 (0.22, 0.48) | 0.32 (0.21, 0.49) | 0.51 (0.30, 0.86) | 0.78 (0.45, 1.37) |
| Hispanic | 0.40 (0.28, 0.55) | 0.41 (0.29, 0.58) | 0.96 (0.64, 1.43) | 1.29 (0.83, 2.01) |
| Asian | 0.44 (0.24, 0.81) | 0.57 (0.30, 1.11) | 0.70 (0.36, 1.34) | 1.08 (0.57, 2.05) |
| Other | 0.71 (0.54, 0.93) | 0.74 (0.54, 1.02) | 1.41 (0.98, 2.04) | 1.80 (1.19, 2.70) |
| Female (vs male) | 0.64 (0.53, 0.78) | 0.70 (0.56, 0.88) | 0.57 (0.45, 0.73) | 0.63 (0.48, 0.82) |
| Parental education (vs some college or less) | ||||
| College degree or more | 1.19 (1.00, 1.43) | 1.16 (0.94, 1.43) | 1.11 (0.84, 1.45) | 1.04 (0.79, 1.37) |
| Urbanicity (vs urban) | ||||
| Small city | 1.12 (0.85, 1.47) | 1.33 (0.97, 1.83) | 0.83 (0.58, 1.18) | 0.91 (0.63, 1.32) |
| Rural | 1.07 (0.78, 1.47) | 1.15 (0.79, 1.68) | 0.44 (0.28, 0.70) | 0.40 (0.24, 0.65) |
| Definitive plans to attend 4 year college (vs other) | 1.04 (0.86, 1.25) | 1.07 (0.87, 1.32) | 0.98 (0.74, 1.30) | 0.97 (0.71, 1.33) |
| Region of country | ||||
| South | 0.88 (0.62, 1.26) | 0.90 (0.60, 1.35) | 0.63 (0.40, 0.99) | 0.55 (0.34, 0.89) |
| Northeast | 0.79 (0.54, 1.18) | 0.73 (0.46, 1.15) | 1.15 (0.71, 1.86) | 1.19 (0.73, 1.93) |
| Upper Midwest | 0.88 (0.61, 1.27) | 0.91 (0.59, 1.39) | 0.83 (0.51, 1.34) | 0.80 (0.48, 1.33) |
| West (reference) | ||||
| Easy to obtain nicotine vaping device | 4.63 (3.19, 6.71) | 3.68 (2.43, 5.57) | 2.98 (1.90, 4.67) | 2.25 (1.37, 3.71) |
| Past 30-day substance use | ||||
| Cigarettes | – | 1.63 (1.18, 2.26) | 1.89 (1.35, 2.64) | |
| Alcohol | – | 3.01 (2.37, 3.83) | 3.92 (2.91, 5.29) | |
| Marijuana (other than vaping) | – | 3.78 (3.01, 4.75) | – | |
| Binge drinking in past 2 weeks | – | 1.65 (1.25, 2.17) | 1.81 (1.32, 2.50) | |
Notes: Unweighted N=6,982. Bolded ORs indicate statistical significance (p<0.05). Multiple imputation was used for missing data. Model 1 includes protective factors and demographics, Model 2 includes protective factors, demographics, and current substance use.
In Model 1 for marijuana vaping, compared with youth who reported having low assets, the odds of marijuana vaping were lower for youth with medium assets (AOR=0.54, 95% CI=0.42, 0.69) and high assets (AOR=0.09, 95% CI=0.05, 0.18). Black (compared with non-Hispanic White) and female (compared with male) adolescents had lower odds of vaping. Students in rural areas compared with large urban areas, and in the South compared with West, had lower odds of vaping. Ease of obtaining a vaping device was positively associated with vaping. In Model 2, compared with youth who reported having low assets, the odds of marijuana vaping were lower for youth with medium assets (AOR=0.63, 95% CI=0.48, 0.82) and high assets (AOR=0.16, 95% CI=0.08, 0.31), adjusting for other substance use. Past 30–day use of cigarettes and alcohol were associated with higher odds of vaping. Binge drinking was associated with higher odds of vaping. Associations remained nearly identical and statistically significant in analyses that adjusted for cohort year.
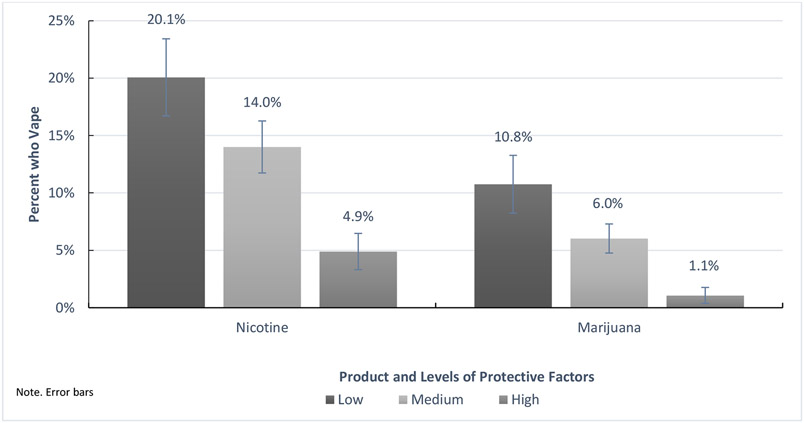
As shown in Figure 1, postestimation results demonstrated that there were marked differences in probabilities of nicotine vaping between students who reported low assets compared with students with high assets: a difference of approximately 15 percentage points (20.1% vs 4.9%, respectively). There was also a marked difference in predicted probabilities of marijuana vaping between students who reported low assets compared with students with high assets: a difference of 10 approximately percentage points (10.8% vs 1.1%).
Figure 1.
Predicted probabilities of past 30-day vaping of nicotine or marijuana across levels of assets.
As shown in Appendix Table 1, there were marked differences in prevalence of the 9 individual assets, ranging from high prevalence for assets such as positive peer norms (73.1%) and family support (69.9%) to low prevalence of assets such as social competence (39.6%) and commitment to learning (13.3%). In multivariable models (Appendix Table 2), adjusting for covariates and other assets, adolescents who reported having social competence and positive peer norms were less likely to report nicotine vaping (AOR=0.25, 95% CI=0.18, 0.34 vs AOR=0.34, 95% CI=0.28, 0.42) and marijuana vaping (AOR=0.04, 95% CI=0.02, 0.12 vs AOR=0.27, 95% CI=0.21, 0.36), with both assets exhibiting strong associations.
DISCUSSION
Increasing prevalence of nicotine and marijuana vaping among adolescents in the U.S. is a critical public health problem to address because vaping nicotine increases the risk of future combustible use and it exposes youth to harmful toxins,1,5,6 and marijuana vaping affects development and is associated with e-cigarette or vaping use–associated lung injury.1 U.S. adolescents who report more developmental assets were less likely to report current nicotine and marijuana vaping, even after adjusting for other substance use. Having high assets is most protective compared with medium levels of assets when other risk behaviors are reported. Assets that align with DAF’s social competence category and positive peer norms are particularly important assets for vaping.
The HYD perspective can be used to identify factors in adolescence that protect against nicotine and marijuana vaping. The assets framework provides an established roadmap for generating a single measure of cumulative assets.16,20 Developmental assets have been linked to other substance use outcomes, such as cigarette smoking and alcohol use,19 but research has not applied cumulative assets to nicotine and marijuana vaping. As cumulative assets were associated with vaping outcomes, programs should follow evidence-based practice that promotes healthy development by building multiple assets, which creates an environment where youth thrive and avoid substance use.10-15 Promoting cumulative assets can help adolescents cope with stress, thereby reducing risk for vaping. If practitioners only have capacity to promote a single asset, addressing decision-making skills or peer norms could be fruitful. For example, the measure for “social competency” could be considered refusal self-efficacy, and therefore this form of self-efficacy could be an intervention target. In the case of peer norms, personalized feedback interventions that address (mis)perceptions of peer vaping behaviors (e.g., youth often overestimate their peers’ substance use)35 could alter norms around vaping, which could subsequently reduce adolescent vaping.
CONCLUSIONS
The HYD perspective can be applied to nicotine and marijuana vaping among adolescents. Nicotine and marijuana vaping continue to be public health issues, and researchers and practitioners need to develop an evidence base for effective interventions. Rather than strictly focusing on risk-based targets, the HYD allows for a strengths-based approach that not only protects adolescents against the harms of vaping but also promotes healthy development more broadly. Although the current results are cross-sectional and therefore the results do not demonstrate causal relationships, the project shows that promoting protective factors is a promising approach to decreasing vaping.
Supplementary Material
ACKNOWLEDGMENTS
Research reported in this publication as well as data collection were supported by the National Institute on Drug Abuse of NIH (grant number R01DA001411). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH. The authors report no conflicts of interest. No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.King BA, Jones CM, Baldwin GT, Briss PA. The EVALI and youth vaping epidemics — implications for public health. N Engl J Med. 2020;382(8):689–691. 10.1056/nejmp1916171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patrick ME, Miech RA, Kloska DD, Wagner AC, Johnston LD. Trends in marijuana vaping and edible consumption from 2015 to 2018 among adolescents in the US. JAMA Pediatr. 2020;174(9):900–902. 10.1001/jamapediatrics.2020.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miech R, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future National Survey Results on Drug Use, 1975–2019: Volume I, Secondary School Students. Ann Arbor, MI; 2020. 10.3998/2027.42/150622. [DOI] [Google Scholar]
- 4.Cullen KA, Ambrose BK, Gentzke AS, et al. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students — United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2018;67(45):1276–1277. 10.15585/mmwr.mm6745a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soneji S, Barrington-trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(4):788–797. 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glantz SA, Bareham DW. E-cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. 2018;39:215–235. 10.1146/annurev-publhealth-040617-013757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kritikos AF, Johnson JK, Hodgkin D. Past 30–day marijuana vaping: prevalence and predictors of use in a nationally representative study of U.S. youth. Am J Prev Med. 2021;60(2):258–266. 10.1016/j.amepre.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parks MJ, Davis L, Wilhelm AK, McMorris BJ, Borowsky IW, Shlafer RJ. Parental incarceration and youth tobacco product use: implications for prevention and the e-cigarette epidemic. Addict Behav. 2020;107:106428. 10.1016/j.addbeh.2020.106428. [DOI] [PubMed] [Google Scholar]
- 9.Sieving RE, McRee AL, McMorris BJ, et al. Youth–adult connectedness: a key protective factor for adolescent health. Am J Prev Med. 2017;52(3 suppl 3):S275–S278. 10.1016/j.amepre.2016.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–2478. 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernat DH, Resnick MD. Healthy youth development: science and strategies. J Public Health Manag Pract. 2006;12(suppl 6):S10–S16. 10.1097/00124784-200611001-00004. [DOI] [PubMed] [Google Scholar]
- 12.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescent’s from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–832. 10.1001/jama.1997.03550100049038. [DOI] [PubMed] [Google Scholar]
- 13.Viner RM, Ozer EM, Denny S, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–1652. 10.1016/s0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- 14.Catalano RF, Fagan AA, Gavin LE, et al. Worldwide application of prevention science in adolescent health. Lancet. 2012;379(9826):1653–1664. 10.1016/s0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oesterle S, Kuklinski MR, Hawkins JD, Skinner ML, Guttmannova K, Rhew IC. Long-term effects of the communities that care trial on substance use, antisocial behavior, and violence through age 21 years. Am J Public Health. 2018;108(5):659–665. 10.2105/ajph.2018.304320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leffert N, Benson PL, Scales PC, Sharma AR, Drake DR, Blyth DA. Developmental assets: measurement and prediction of risk behaviors among adolescents. Appl Dev Sci. 1998;2(4):209–230. 10.1207/s1532480xads0204_4. [DOI] [Google Scholar]
- 17.Syvertsen AK, Scales PC, Toomey RB. Developmental Assets framework revisited: confirmatory analysis and invariance testing to create a new generation of assets measures for applied research. Appl Dev Sci. In press. Online May 23, 2019. 10.1080/10888691.2019.1613155. [DOI] [Google Scholar]
- 18.Scales PC, Benson PL, Leffert N, Blyth DA. Contribution of developmental assets to the prediction of thriving among adolescents. Appl Dev Sci. 2000;4(1):27–46. 10.1207/s1532480xads0401_3. [DOI] [Google Scholar]
- 19.Scales P, Leffert N, Lerner R. Developmental Assets: A Synthesis of the Scientific Research on Adolescent Development. Minneapolis, MN: Search Institute; 2004. [Google Scholar]
- 20.Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample. JAMA Pediatr 2019;173(11):e193007. 10.1001/jamapediatrics.2019.3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scales PC. Reducing risks and building developmental assets: essential actions for promoting adolescent health. J Sch Health. 1999;69(3):113–119. 10.1111/j.1746-1561.1999.tb07219.x. [DOI] [PubMed] [Google Scholar]
- 22.Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthopsychiatry. 1987;57(3):316–331. 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 23.Sameroff A. Transactional models in early social relations. Hum Dev. 1975;18(1–2):65–79. 10.1159/000271476. [DOI] [Google Scholar]
- 24.Werner EE, Smith RS. Overcoming odds: High risk Child from birth to adulthood. Cornell University Press; 1992. [Google Scholar]
- 25.Cicchetti D, Toth SL, Maughan A. An ecological-transactional model of child maltreatment. In: Sameroff AJ, Lewis M, Miller SM, eds. Handbook of Developmental Psychopathology. Boston, MA: Springer; 2000:689–722. 10.1007/978-1-4615-4163-9_37. [DOI] [Google Scholar]
- 26.Masten AS. Ordinary magic: resilience processes in development. Am Psychol. 2001;56(3):227–238. 10.1037/0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 27.Hays-Grudo J, Morris AS, Beasley L, Ciciolla L, Shreffler K, Croff J. Integrating and synthesizing adversity and resilience knowledge and action: the ICARE model. Am Psychol. 2021;76(2):203–215. 10.1037/amp0000766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morris A, Hays-Grudo J, Zapata M, Treat A, Kerr K. Adverse and protective childhood experiences and parenting attitudes: the role of cumulative protection in understanding resilience. Advers Resil Sci. 2021;2:181–192. 10.1007/s42844-021-00036-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Trends in adolescent vaping, 2017–2019. N Engl J Med. 2019;381(15):1490–1491. 10.1056/nejmc1910739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miech R, Leventhal A, Johnston L, O’Malley PM, Patrick ME, Barrington-Trimis J. Trends in use and perceptions of nicotine vaping among US youth from 2017 to 2020. JAMA Pediatr. 2021;175(2):185–190. 10.1001/jamapediatrics.2020.5667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Portnoy DB, Wu CC, Tworek C, Chen J, Borek N. Youth curiosity about cigarettes, smokeless tobacco, and cigars: prevalence and associations with advertising. Am J Prev Med. 2014;47(2 suppl 1):S76–S86. 10.1016/j.amepre.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Lewis MA, Litt DM, King KM, Garcia TA, Waldron KA, Lee CM. Consideration of future consequences as a moderator of the willingness-behavior relationship for young adult marijuana use and consequences. Addict Behav. 2018;87:8–16. 10.1016/j.addbeh.2018.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patrick ME, Couper MP, Parks MJ, Laetz V, Schulenberg JE. Comparison of a web-push survey research protocol with a mailed paper and pencil protocol in the Monitoring the Future panel survey. Addiction. 2021;116(1):191–199. 10.1111/add.15158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kreslake JM, Simard BJ, O’Connor KM, Patel M, Vallone DM, Hair EC. E-cigarette use among youths and young adults during the COVID-19 pandemic: United States, 2020. Am J Public Health. 2021;111(6):1132–1140. 10.2105/ajph.2021.306210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee CM, Neighbors C, Kilmer JR, Larimer ME. A brief, web-based personalized feedback selective intervention for college student marijuana use: a randomized clinical trial. Psych Addict Behav. 2010;24(2):265–273. 10.1037/a0018859. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.