Abstract
The coronavirus disease 2019 (COVID-19) is a highly transmissible disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that poses a major threat to global public health. Although COVID-19 primarily affects the respiratory system, causing severe pneumonia and acute respiratory distress syndrome in severe cases, it can also result in multiple extrapulmonary complications. The pathogenesis of extrapulmonary damage in patients with COVID-19 is probably multifactorial, involving both the direct effects of SARS-CoV-2 and the indirect mechanisms associated with the host inflammatory response. Recognition of features and pathogenesis of extrapulmonary complications has clinical implications for identifying disease progression and designing therapeutic strategies. This review provides an overview of the extrapulmonary complications of COVID-19 from immunological and pathophysiologic perspectives and focuses on the pathogenesis and potential therapeutic targets for the management of COVID-19.
Subject terms: Infectious diseases, Respiratory tract diseases
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a highly contagious and pathogenic virus that was identified as a causative agent of the coronavirus disease 2019 (COVID-19).1 As of January 6, 2022, SARS-CoV-2 has infected nearly 289 million people and caused over 5.4 million deaths globally.2 Accumulating evidence suggests that SARS-CoV-2 infection primarily attacks the lung and causes respiratory diseases ranging from mild cold to more severe illness such as severe acute respiratory syndrome (ARDS), but it can also affect other organs and have systemic consequences with multiple organ injury.3 The extrapulmonary complications4 include a wide spectrum of disorders with cardiovascular,5 endothelial,6 coagulation,7 renal,8 hepatobiliary,9 gastrointestinal,10 endocrinological,11 neurological12 involvement, which may occur in severe and critically ill patients and are associated with prolonged hospitalization and increasing mortality risk. The extrapulmonary organ injury of COVID-19 may result from direct injury mediated by SARS-CoV-2 invasion, endothelial cell damage, or possible indirect mechanisms secondary to excessive local and systemic inflammatory responses. Angiotensin-converting enzyme 2 (ACE2)13 has been identified as the entry receptor for SARS-CoV-2. The widespread distribution of ACE2 across multiple organs and tissues makes the virus-mediated direct tissue damage a plausible mechanism of systematic injury.14 Moreover, dysregulated immune response, endothelial damage as well as thromboinflammation may also account for the extrapulmonary complications of COVID-19.6,15 In this review, we narratively summarized the published literature on extrapulmonary consequences of COVID-19, and provided a comprehensive perspective on the extrapulmonary organ-specific pathophysiology and potential therapeutic strategies for COVID-19, in order to help scientists and clinicians to identify and monitor the spectrum of disease, and to establish research priorities within this field.
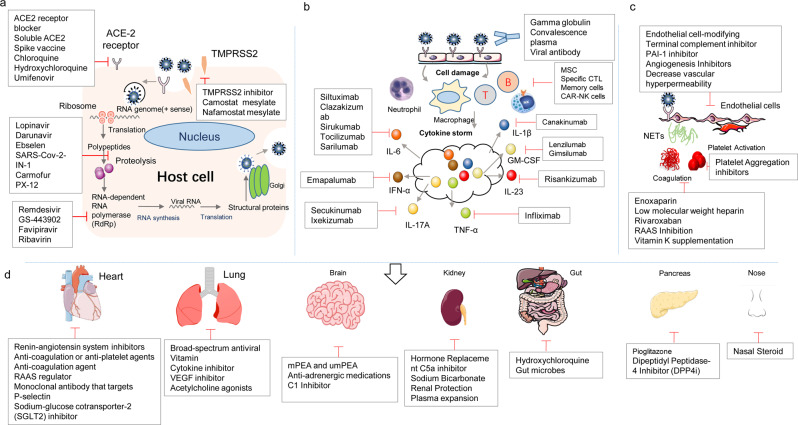
Pathogenesis of SARS-CoV-2 infection
Key mechanisms underlying pathophysiology of extrapulmonary organ injury secondary to SARS-CoV-2 infection include direct viral invasion, imbalance of renin–angiotensin-aldosterone system (RAS), dysregulation of the immune response, endothelial cell damage, and thromboinflammation. These mechanisms responsible for multiple organ involvement of COVID-19 has not yet been fully understood. ACE2-mediated virus entry and dysregulated RAS may be unique to SARS-CoV-2 infection, while immune dysregulation characterized by excessive release of proinflammatory cytokines and microcirculation disorder may occur in other critical conditions such as sepsis.
Direct mechanism of SARS-CoV-2 infection
SARS-CoV-2 is an enveloped virus with a positive-sense single-stranded RNA (+ssRNA) genome of around 30-kb. A mature SARS-CoV-2 particle contains four main structural components, including spike (S), envelope (E), membrane (M) glycoproteins, and nucleocapsid phosphoprotein (N). The S glycoprotein mediates virus entry into target cells. E protein is a small integral membrane protein acting on viral assembly, budding, envelope formation, and pathogenesis.16 N protein is an abundantly expressed RNA-binding protein that plays a critical role in the replication, transcription, and genome packaging of SARS-CoV-2. M protein is key for the assembly of viral particles through interacting with all other structural proteins. These interactions between structural proteins help form replication-incompetent virus-like particles (VLPs), which resemble the morphological structure of SARS-CoV-217 and are efficient platform for vaccine development.
SARS-CoV-2 can enter the host cells either via endocytosis or via direct fusion with the plasma membrane. The S protein binding to ACE2 represents the initial step of SARS-CoV-2 infection, thus it is the main target for the design of vaccines and inhibitors of viral entry. S protein includes S1 and S2 subunits. The S1 subunit comprises an N-terminal domain (NTD) and the receptor-binding domain (RBD).18 The RBD contains a conserved core and receptor-binding motif (RBM), which is a variable region of S protein responsible for direct binding to ACE2 and the key target of neutralizing antibodies.19,20 The S2 subunit mediates fusion of the viral envelope with host cellular membrane. It consists of a highly conserved fusion peptide (FP) domain, two heptad-repeat domains (HR1 and HR2), a central helix (CH), a connector domain (CD), transmembrane domain (TM), and cytoplasmic tail (CT).21
ACE2 was identified as the binding receptor of both SARS-CoV and SARS-CoV-2. The RBD of SARS-CoV-2 has a higher ACE2-binding affinity compared to that of SARS-CoV, supporting efficient cell entry.22 The enhanced affinity may increase the infectivity of SARS-CoV-2. The ACE2 gene expression was initially established in the heart, kidneys, and testes,23 while further studies showed a much broader distribution, such as the upper respiratory tract, lungs, intestine, liver, and pancreas.24–26 Moreover, neuropilin-1 (NRP1), expressed in the respiratory and olfactory epithelium, may be an additional cellular facilitator of SARS-CoV-2 cell entry and infectivity.27 In addition, an RNA sequencing analysis shows that although immune cells do not express ACE2 or TMPRSS2, another receptor for SARS-CoV-2, a transmembrane protein of the immunoglobulin cluster of differentiation (CD)147 provides a potential route for viral entry.28,29 SARS-CoV-2 can also exploit receptor-mediated endocytosis through interaction between its S protein with soluble ACE2 or soluble ACE2-vasopressin via angiotensin (Ang) II type receptor 1(AT1R) or arginine vasopressin receptor 1B (AVPR1B).30
After binding to the receptor, proteolytic cleavage of SARS-CoV-2 S protein enables the S2 subunit-assisted fusion of viral and cellular membranes. This process is mediated via certain host proteases including furin, cell surface transmembrane serine proteases 2 (TMPRSS2),31 cathepsins B and L, factor Xa and elastase. An insertion of four amino acids in the S1/S2 site of S protein provides a minimal cleavage motif (RRAR) recognized by proprotein convertase furin, which is a unique feature of SARS-CoV-2. S protein is cleaved at the S1/S2 site by furin and subsequent at the S2’ site by TMPRSS2, triggering an irreversible and extensive conformational change to mediate membrane fusion.32–34 Besides, inside the endosome, a pH-dependent endosomal protease cathepsin L can facilitate the cleavage and proteolytical activation of S protein for fusion within the endosomal membrane.35 Inhibition of these proteases, particularly TMPRSS2,36 might constitute a treatment option to treat COVID-19.
The following SARS-CoV-2 life cycle inside the cell is similar to that of other coronaviruses.37 SARS-CoV-2 releases viral genome into the cytoplasm to induce translation of open reading frame (ORF)1a and ORF1b into the large replicase polyproteins 1a (pp1a) and pp1ab. Subsequently, two viral proteases, a papain-like protease (PLpro) and a 3C-like protease (3CLpro) cleave pp1a and pp1ab into 16 nonstructural proteins (nsps) that assemble into replication-transcription complexes (RTCs) for RNA synthesis.38 The RNA-dependent RNA polymerase (RdRp) is the central enzyme of RTCs. The RTCs produce new genomic RNA by continuous synthesis and a set of subgenomic RNA.33 These further are translated into respective viral proteins. The viral structural proteins (S, E, and M) traffic through the endoplasmic reticulum (ER) to ER–Golgi intermediate compartment (ERGIC). The N protein package genomic RNA into helical structures in the cytoplasm, and interact with hydrophobic M protein in the ERGIC that serve to direct assembly and budding of the mature virion.39 These virions are transported to the cell surface in vesicles and then released through exocytosis into the extracellular region.33,34 The development of effective therapeutic strategies for COVID-19 relies on the knowledge of molecular mechanisms of SARS-CoV-2 infection.
Emerging SARS-CoV-2 variants
Like other RNA viruses, SARS-CoV-2 tends to evolve rapidly, producing mutants that differed significantly from its ancestral strains. A classification system was established to distinguish the emerging SARS-CoV-2 variants into variants of concern (VOCs) and variants of interest (VOIs). There are currently five main designated VOCs, including Alpha, Beta, Gamma, Delta, and Omicron variants. Alpha, Beta, Gamma, and Delta variants were first identified in the UK, South Africa, Brazil, and India, respectively.40 VOCs have been associated with increased transmissibility and viral virulence, decreased diagnostic sensitivity, and potential influence on vaccination.41 All VOCs carry mutation D614G that may enhance infectivity of SARS-CoV-2 by assembling more functional S protein into the virion.42 N501Y mutation located within the RBD is common to all variants except the Delta variant that contributes to increased affinity of the S protein to ACE2, promoting the viral attachment and its subsequent entry into the host cells.43,44
Alpha variant is also known as lineage B.1.1.7. Three B.1.1.7 S protein mutations are of particular concern: a two-amino-acid deletion at position 69–70 of the NTD; N501Y; and P681H, proximal to the furin cleavage site.45 Mutation P681H is a known region of importance for infection and transmission.28,46 The ∆H69/∆V70 deletion results in increased infectivity and evasion of the immune response.20 Beta variant known as multiple B.1.351 sublineages, includes nine mutations in S protein. K417N, E484K, and N501Y are located in the RBD.19 These changes confer enhanced affinity for ACE244 and help to escape from neutralization and reduce neutralization sensitivity to convalescent plasma.47 Gamma variant, also known as lineage P.1, harbors ten mutations in the S protein. Three mutations (L18F, K417N, E484K) are located in the RBD.18,48 This variant may have reduced neutralization by monoclonal antibody therapies, convalescent sera, and postvaccination sera.49 Delta variant referred to as the B.1.617.2 lineage, has a highly mutated NTD (T19R, G142D, Δ156-157, R158G, A222V). According to the reports,50,51 the Delta variant was resistant to neutralization by some anti-NTD and anti-RBD monoclonal antibodies.52 The Delta Plus variant also known as B.1.617.2.1 or AY.1, is a sublineage of the Delta variant. Five key mutations (T95I, A222V, G142D, R158G, and K417N) were significantly more prevalent in the Delta Plus than in the Delta variant.53 On 26 November 2021, WHO designated the newly emerging variant B.1.1.529 a VOC, named Omicron, which has a total of 60 mutations.
Indirect mechanisms of SARS-CoV-2 infection
Dysregulation of the immune response
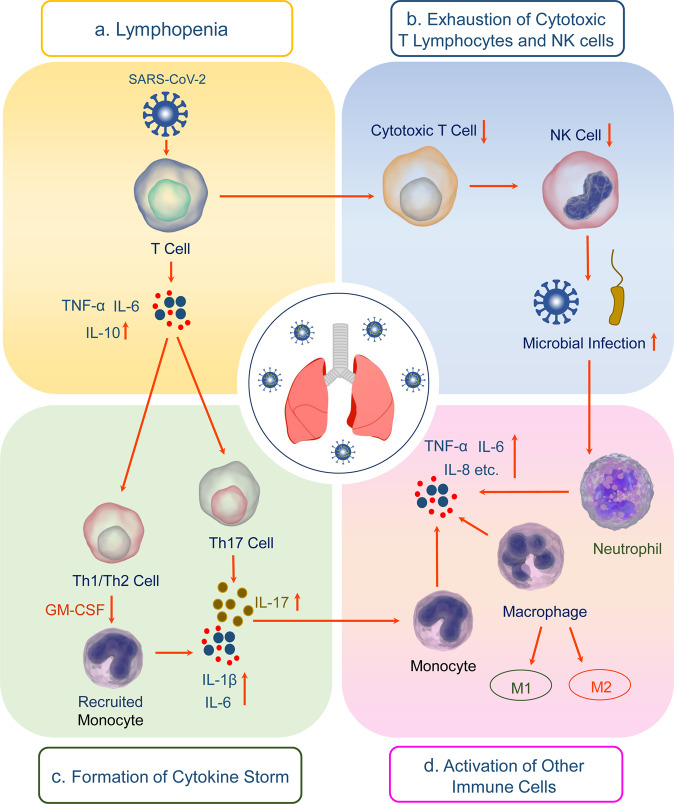
The pathogenesis of COVID-19 is triggered by SARS-CoV-2 infection and amplified by dysregulated immune responses. Impaired immune system and hyperinflammation induced by SARS-CoV-2, instead of the direct detrimental toxicity of virus, may account for severe disease with multiple organ involvement in severe and critically ill COVID-19 patients.54 Patients with ARDS and extrapulmonary complications have increased levels of circulating proinflammatory cytokines, chemokines and systemic inflammatory markers such as ferritin, lactate dehydrogenase (LDH), c-reactive protein (CRP), D-dimer, and neutrophil-to-lymphocyte ratio.55 As summarized in Fig. 1, increased proinflammatory of cytokines, lymphocytopenia, lymphocyte exhaustion, and upregulated antibodies may be involved in the immune pathogenesis of COVID-19.15
Fig. 1.
The potential mechanisms of SARS-CoV-2-induced immunopathology. a Lymphopenia, b Exhaustion of cytotoxic T lymphocytes and NK cells, c Cytokine storm, d Activation of other immune cells contribute to the pathogenesis and exacerbation of COVID-19
Innate immune response
As a frontline of defense, the innate immune response to SARS-CoV-2 infection triggers several signaling pathways to induce the production of IFN, proinflammatory cytokines and chemokines, and initiate adaptive immunity against SARS-CoV-2. Epithelial cells in the respiratory tract acting as the first line of innate immune sensing of SARS-CoV-2 infection, are a major source of chemokine interleukin (IL)-8 that plays an important role in regulating lung neutrophil recruitment and survival. Alveolar neutrophils and macrophages subsequently trigger the innate immune response to the virus.56 Neutrophils engulf and kill the viruses through the release of neutrophil extracellular traps (NETs), reactive oxygen species (ROS), and antimicrobial peptides.57 The enhanced infiltration of granulocytes and monocyte-macrophages is a common phenomenon in severe COVID-19 cases. Monocytes and macrophages are involved in the exacerbated and hypersensitive reactions contributing to the organ damage.58 Besides, multiple studies have shown decreased numbers and functionally exhaustion of natural killer (NK) cells during SARS-CoV-2 infection.59 The diminished NK cell cytotoxicity and immune regulation result in a critical inflammatory phenotype in COVID-19.60
The pattern-recognition receptors (PRRs) in/on the immune cells, involving toll-like receptors (TLRs) such as TLR3 or TLR7, and retinoic acid-inducible gene (RIG)-I-like receptors (RLRs) such as RIG-I and the melanoma differentiation-associated gene 5 (MDA5) recognize the pathogen-associated molecular patterns (PAMPs) derived from SARS-CoV-2, such as viral ssRNA genome, replication intermediates or double-stranded RNA (dsRNA), thereby initiating the antiviral responses.61 Endosomal TLR7 expressed in monocytes, dendritic cells (DCs) and macrophages recognizes viral genomic RNA and subsequently results in the activation of Janus kinase (JAK)/signal transducer and activator of transcription (STAT) signaling pathways, and its downstream transcription factors, activator protein-1 (AP-1), nuclear factor kappa B (NF-κB), interferon response factor (IRF) 3, and IRF7.62 These activated signaling pathways and transcription factors induce the rapid production of proinflammatory cytokines.63
The immune hallmark of severe COVID-19 is exaggerated secretion of cytokines, such as interleukin (IL)-1β, IL-2, IL-6, IL-8, IL-10, granulocyte macrophage-colony stimulating factor (GM-CSF), IFN-γ, and TNF-α, interferon-inducible protein-10 (IP10), macrophage inflammatory protein (MIP)-1α, tumor necrosis factor (TNF)-α, etc. This life-threatening condition related to systemic inflammation with sometimes lethal consequences is known as cytokine storm syndrome (CSS) or cytokine release syndrome (CRS), or just cytokine storm.64,65 Cytokine storm, an overwhelming inflammatory response results in the pathophysiology and mortality of SARS-CoV-2 infection. Cytokine storm is closely associated with macrophage activation syndrome (MAS), which is characterized by inflammatory systemic abnormality such as pancytopenia, hyperferritinemia, coagulopathy, hemodynamic instability, liver failure, neurological disorder, and can lead to ARDS or even multiorgan damage associated with unfavorable prognosis of COVID-19.66 MAS is resulted from the excessive proliferation of differentiated macrophages that cause hemophagocytosis and hypercytokinemia.67,68
As an important pleiotropic proinflammatory mediator, IL-6 is the main driver of cytokine storm through promoting the proliferation of myeloid progenitor cells and activation of leukocytes, inducing pyrexia, and escalating the secretion of acute-phase proteins in the severe cases of COVID-19.69 SARS-CoV-2 infection induces a wide range of immune cells including macrophages, neutrophils, DCs and lymphocytes to secrete excessive amounts of IL-6.70,71 Excessive IL-6 promotes the differentiation of Th17 cells and stimulates IL-17 production,72 and further recruits neutrophils, monocytes, and macrophages to the site of infection and inflammation and triggers a cascade of inflammatory cytokines, such as IL-1β and IL-6, leading to an IL-6 burst in its amplification cycle.73 Increased levels of IL-6 are significantly associated with the disease severity and adverse clinical outcome of COVID-19.74 The IL-6 signaling cascade is initiated by IL-6 binding to the membrane-bound or soluble IL-6 receptor (IL-6R) and a second transmembrane protein, glycoprotein 130 (gp130), which is referred to as classic signaling or trans-signaling, respectively.75 IL-6 classic signaling may have homeostatic and anti-inflammatory effects, whereas trans-signaling may regulate proinflammatory response.76 Expression of IL-6R is restricted to cells including hepatocytes and immune cells, but gp130 is ubiquitously expressed, possibly explaining the pleiotropic functions of IL-6. Recombinant humanized monoclonal antibodies against IL-6R or IL-6 are drug candidates for managing the cytokine storm secondary to SARS-CoV-2 infection77 through inhibiting the intercellular signaling pathway in gp130 expressing cells.
GM-CSF also has a critical role in mediating cytokine storm. Because of its function as a proinflammatory cytokine and a myeloid cell growth factor, GM-CSF may be another important driver of the immunopathological sequelae of SARS-CoV-2 infection.69 Upon SARS-CoV-2 infection, CD4+ T lymphocytes are rapidly differentiated into pathogenic T helper (Th) 1 cells that produce IL-6 and GM-CSF, subsequently inducing CD14+CD16+ monocytes to secrete high levels of IL-6 and GM-CSF and worsen the cytokine storm.78 Hence, a monoclonal antibody against GM-CSF may be effective to attenuate the immunopathogenesis of COVID-19.
IFN is innate cytokine that functions as the first-line defense against viral infection. Type I IFN, including IFN-α and IFN-β, triggers the expression of IFN-stimulated genes (ISGs), which directly suppress viral replication by various mechanisms, involving degradation of viral RNA or inhibition of viral transcription or translation.79,80 More than one-third of SARS-CoV proteins have inhibitory effects on type I IFN-mediated antiviral immune responses.81 Given most of the SARS-CoV-2 proteins exhibit high amino acid-sequence homology with those of SARS-CoV, it is speculated that SARS-CoV-2 proteins may exhibit inhibitory effects on IFN responses through similar mechanisms.80 SARS-CoV-2 have evolved mechanisms to evade the antiviral function of type I and III IFNs, including interference with the induction of IFN production or the downstream signaling pathways after IFN binding to the IFN receptors (IFNRs).80 Patients with severe or critically ill COVID-19 had highly impaired type I IFN response, characterized by low production and activity of type I IFN and ISGs.82 Compared to asymptomatic or mild COVID-19, severe cases are more likely to carry mutations in genes involved in type I IFN pathways or have autoantibodies against IFN that can neutralize high concentrations of type I IFN in vitro.83,84 However, increasing evidence also shows contradictory findings that severe COVID-19 patients have a robust type I IFN response, contrary to a delayed and likely suppressed IFN response found in the early phase of infection.85 Deeper understanding of the roles of IFNs response in SARS-CoV-2 infection is warrant further investigation.
Adaptive immune response
The adaptive immune system is also called specific or acquired immunity, including cellular immunity carried out by T cells and humoral immunity mediated by B cells that elicit protective immune response against pathogens in an antigen-specific manner.86 During viral infection, an effective adaptive immune response plays a crucial role in eliminating the virus and preventing the disease progression.87 Induction of an adaptive immune response against pathogens relies on the initial recognition and capture of antigens by antigen presenting cell (APC). The viral antigens are identified, processed, and presented by APCs to activate and guide the differentiation of CD4+ and CD8+ T cells into effector and memory cells.88 After being activated, CD4+ T cells differentiate into Th1, Th2 effector cells, and other subsets, characterized by distinct cytokine pattern.89 Th cells play critical roles in orchestrating the adaptive immune responses, through secretion of cytokines and chemokines that recruit immune cells and stimulate B cell differentiation and antibody production as well as activate CD8+ cytotoxic T lymphocytes (CTLs). Th1 cells produce IFN-γ, IL-2, and lymphotoxin α (LTα), and mediate immune responses against intracellular pathogens, whereas Th2 cells produce IL-4, IL-5, IL-9, IL-10, IL-13, and IL-25, and mediate host defense against extracellular parasites.90 CTLs can directly kill the virus-infected cells via exocytosis of lytic granules that contain perforin and granzymes or via the Fas pathway.91 T-follicular helper (Tfh) cells are a specialized subset of CD4+ T cells that can activate B cells to produce antibodies. The neutralizing antibodies exert protective activities through blocking SARS-CoV-2 infection in a later phase and conferring protection against future infection.92
Lymphopenia, particularly in peripheral CD4+ and CD8+ T cells, is frequently found and an early immunologic indicator of impending severe COVID-19.93,94 This lymphocytes depletion could be a manifestation of imbalance in both arms of immune responses, leading to dysregulated IFN production, hyperactivated neutrophils and macrophages, and delayed viral clearance. The prevalence of lymphopenia differed among the patients with different disease severities, with 72.7% developed in severe cases and 10.0% in the moderate case.94 Patients with severe COVID-19 showed considerably decrease in the counts of circulating memory CD4+ T cells, CD8+ T cells and regulatory T cells (Tregs).94 Despite reduced CD8+ T-cell counts, their histocompatibility complex (MHC) II cell surface receptor (HLA-DR) expression was higher in patients with severe COVID-19 than moderate cases. HLA-DR is primarily recognized as a marker of T-cell activation, but a recent study shows that CD8+HLA-DR+ T cells may constitute a Treg cell subset,95 and have immunosuppressive properties involving the inhibitory molecule the cytotoxic T lymphocyte antigen 4 (CTLA-4). High expressions of perforin and granzyme B in CD8+ T cells, low levels of TNF-α and IFN-γ in CD4+ T cells were related to disease severity of COVID-19.96 Moreover, CD8+ T cells more frequently displayed an exhausted phenotype in the severe COVID-19 cases. Patients with overtly symptomatic COVID-19 showed increased programmed cell death protein-1 (PD-1) and T-cell immunoglobulin domain and mucin domain-3 (TIM-3) expressions on CD8+T cells.97 These results indicate that functional impairment or exhaustion of T cells is correlated with disease severity and prognosis of patients with COVID-19. Moreover, SARS-CoV-2 infection may induce the downregulation of the MHC II expression on B cells, leading to decreased acquired immunity activation.98 An increased SARS-CoV-2-specific IgG antibody responses are strongly correlated with disease severity,99 suggesting that activation of B cells in severe COVID-19 patients is associated with adverse outcome.
Multiple underlying mechanisms may be responsible for lymphopenia and lymphocyte dysfunction. SARS-CoV-2 infects primarily epithelial cells in the respiratory tract through binding of S protein to ACE2. It is hypothesized that SARS-CoV-2 may suppress adaptive cellular immune response through infecting certain immune cells. However, some studies have demonstrated that only limited pulmonary macrophages or monocytes may express ACE2,100 which raises the possibility of the presence of additional receptors or cellular entry route such as antibody-dependent enhancement (ADE), granting SARS-CoV-2 an opportunity to infect host immune cells. The reduced T-cell numbers were inversely associated with IL-6, IL-10, and TNF-α levels. This phenomenon indicates that increased production of inflammatory cytokines may promote T-cell exhaustion and apoptosis that accompanies disease progression.101 Soluble IL-2 receptor can negatively regulate CD8+ T cells and induce lymphopenia via inhibition of IL-2 signaling.102 Moreover, lymphoid organ atrophy, such as the spleen and lymph node leads to further impairments of lymphocyte.103 Severe COVID-19 patients had an elevated level of lactic acid in the blood, which can suppress the proliferation of lymphocytes.104 Neutrophils with suppressive properties such as granulocytic myeloid-derived suppressor cells (G-MDSCs) and their possible role in suppressing CD4+ and CD8+ T lymphocytes expansion may also give rise to lymphopenia in severe SARS-CoV-2 infection.105
Endothelial cell damage
Endothelial biomarkers including von Willebrand factor (vWF), soluble P-selectin, and soluble thromboregulatory protein were elevated in severe COVID-19 patients, highlighting the importance of endothelial injury in the pathogenesis of COVID-19.106 Excessive matrix metalloproteinase-1 (MMP-1) and endothelial cell overactivation as evidenced by elevated soluble CD146, vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) are associated with disease severity of patients with COVID-19.107 In addition, Ang II, soluble E-selectin (sE-sel), and soluble thrombomodulin were elevated only in critically ill patients, while only vWF antigen increased with disease severity. Therefore, as markers of endothelial injury, circulating vWF and high molecular weight multimers are the best predictors of in-hospital mortality.108
Patients with COVID-19 have severe endothelial damage in their lungs, including viral invasion and rupture of the endothelial cell membrane.109 Another study identified the co-presence of SARS-CoV-2 N protein and ACE2 receptor on the pulmonary vascular endothelium in postmortem COVID-19 patient samples.110 Moreover, IFN-α or -β can promote SARS-CoV-2 pulmonary vascular infection by inducing the expression of ACE2 in human primary lung endothelial cells.111 S1 and S2 subunits of S protein mediate attachment and membrane fusion, respectively. In primary human pulmonary microvascular endothelial cells that naturally express ACE2, S1 subunits instead of intact S protein reduces transendothelial resistance (TER) and barrier function.112 Plasma mediators of severe COVID-19 patients can cause lung endothelial barrier failure.113
SARS-CoV-2 can not only cause lung endothelial cell damage, but also affect the endothelial cells in extrapulmonary organs. The study found that the endothelial cells of the vascular bed of different organs are affected in patients with COVID-19.114 Besides the lungs, endothelial-related inflammatory cells and apoptotic bodies clusters were found in the heart and small intestine. Moreover, another patient with COVID-19 has also found obvious endotheliitis in the heart, liver, kidney, and small intestine. In the circulatory system, COVID-19-induced endodermatitis is a small vasculitis and does not involve the major coronary arteries.115 Renal biopsy also revealed endothelial abnormalities, ranging from mild injury with enlarged subcutaneous space and/or loss of endothelial cell windows in the glomeruli to severe injury with swollen endothelial cells in the glomerular portal arterioles and fibrin thrombus.116
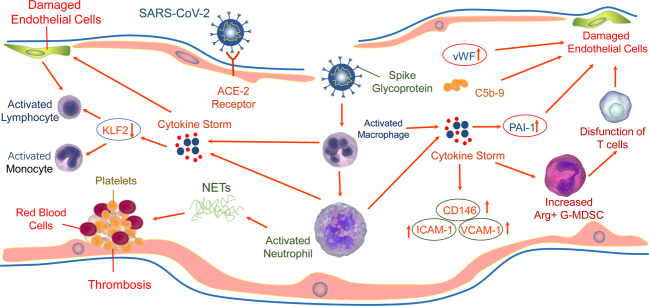
Endothelial injury may occur through direct invasion of endothelial cells or indirect effect of SARS-CoV-2 (Fig. 2). ACE2 on the surface of endothelial cells can be invaded by SARS-CoV-2.117 SARS-CoV-2 can also infect the endothelial cells of extrapulmonary organs. ACE2 was present in arterial and venous endothelial cells of all studied organs.24 The structure of the virus inclusion body was found in the kidney endothelial cells of patients who died from COVID-19 through electron microscopy.114 In addition, SARS-CoV-2 have been found in neural and capillary endothelial cells of frontal lobe in COVID-19 patients.118 The S protein of SARS-CoV-2 can directly damage endothelial cells, manifested as impaired mitochondrial function and endothelial nitric oxide synthase (eNOS) activity, as well as downregulation of ACE2, which may further aggravate endothelial dysfunction due to the disorders of RAS.119
Fig. 2.
Mechanisms of SARS-CoV-2 induced to endotheliopathy in COVID-19. SARS-CoV-2 directly invades endothelial cells or indirectly induces cytokine storm to cause endothelial cell damage. On the one hand, the SARS-CoV-2 receptor ACE2 expressed on the surface of endothelial cells can be directly invaded by the virus. On the other hand, cytokine storm destroys endothelial cells by inducing the release of PAI-1, promoting the degradation of endothelial glycocalyx to release HA fragments and destroying the endothelial barrier; downregulating the expression of KLF2 to induce adhesion and infiltration of monocytes/macrophages, or by immune dysregulation such as increased NETS generation and T-cell dysfunction. Finally, endothelial dysfunction could be further aggravated by complement activation, thrombosis, coagulation disorders and activation of immune cells. Meanwhile, circulating endothelial injury markers including vWF and sCD146 were elevated
In addition to directly infecting endothelial cells, SARS-CoV-2-related cytokine storm and invasive inflammation contribute to endothelial damage in extrapulmonary organs.114,120 The plasma of patients with severe COVID-19 can induce endothelial damage.113,121 The excessive inflammatory effect of cytokine storm may lead to endothelial activation and dysfunction. High serum TNF-α and IL-1β levels in patients with COVID-19 may downregulate the Kruppel-like factor 2 (KLF2) expression in human endothelial cells, and subsequently induce monocyte adhesion, leading to endodermatitis characterized by endothelial dysfunction and hypercoagulability, and lymphocytic monocyte infiltration in patients with COVID-19.122 IL-6 trans-signaling mediates the plasminogen activator inhibitor-1 (PAI-1) releasing from vascular endothelial cells in CRS. Increased levels of PAI-1 can result in endothelial dysfunction, induce cell senescence, thereby promoting local hypoxia.123 In the liver sinusoidal endothelial cells (LSEC), IL-6 trans-signaling leads to proinflammatory and procoagulant states endothelial lesions, and liver injury in COVID-19.124 In addition, macrophage and complement activation125 play a crucial role in endothelial damage and thrombosis in SARS-CoV-2 infection.126 Hyaluronic acid (HA) is a ubiquitous glycosaminoglycan and main constituent of the glycocalyx that is anchored to the vascular lumen and regulates a diverse repertoire of endothelial functions. SARS-CoV-2 infection-induced cytokine storm leads to abnormal degradation of endodermis glycocalyx, resulting in HA fragments that may cause dysfunction of endothelial barrier and vascular hyperpermeability in a ROCK- and CD44-dependent manner.127,128 The circulating granulocyte-myeloid-derived suppressor cells (G-MDSC) expressing high levels of arginase-1(Arg1) increased significantly in COVID-19 patients, which can deplete arginine in the plasma and inhibit T-cell receptor signal transduction, thereby leading to T-cell dysfunction, also impairing the production of nitric oxide and increasing endothelial cell dysfunction, and promoting intravascular coagulation.129 Moreover, due to sustained immune activation during COVID-19 convalescence, activated and infected endothelial cells may be susceptible to direct T-cell-mediated cytotoxicity that may intensify endothelial dysfunction in patients with COVID-19.130
Endothelial injury in COVID-19 patients can lead to dysregulation of coagulation factors and complement, as well as excessive activation of platelets, resulting in thrombosis and eventually clotting disorders. Moreover, endothelial injury recruits and activates immune cells including neutrophils and macrophages, as well as promotes the release of cytokines and the formation of NETs, etc., leading to proinflammatory reactions, which may further aggravate endothelial injury.
Coagulopathy
Coagulopathy is another common feature of COVID-19, which is depicted with thrombocytopenia, prolonged prothrombin time (PT), increased D-dimer levels, and/or decreased fibrinogen levels. In COVID-19, there were elevated D-dimer levels and fibrin degradation products accompanied by mild to moderate increase in PT and activated partial thromboplastin times (APTT).7 About 60% ICU patients had abnormally elevated D-dimer levels compared with a prevalence of 43% in non-severe patients.131 Moreover, increased D-dimer levels were associated with adverse prognosis.132 In severe COVID-19 patients, thrombotic complications are common due to the prothrombotic state and contribute significantly to mortality and morbidity.
The hypercoagulable state is more frequent in elderly COVID‐19 patients.133 COVID-19 patients with hypertension or diabetes mellitus are more likely to suffer lower extremity complications,134 and coagulopathy is a major extrapulmonary risk factor for mortality in hospitalized COVID-19 with type 2 diabetes rather than acute kidney injury (AKI) and acute cardiac injury.135
The most common thrombotic complications include deep vein thrombosis (DVT), pulmonary embolism (PE), and DIC. In severe COVID-19 patients admitted to ICU, the frequency of thrombotic complications was 31% of 184, composed by 27% Venous thromboembolism (VTE) events and 3.7% arterial thrombotic events. Moreover, age and coagulopathy were independent predictors of thrombotic complications.136 In total, 32 (24%) cases of PE were identified with computed tomography pulmonary angiogram (CTPA) in 135 COVID-19 patients, and the rate increased to 50% in ICU patients.137 Existing data of autopsies from COVID-19 patients showed that massive PE accounted for one-third of causes of death, with an additional one fourth with recent DVT but without PE. Overall, 75% of them were male and two-thirds were noted to have recent thrombosis in prostatic venous plexus.138 In all, 8% of patients matched overt DIC according to the International Society on Thrombosis and Hemostasis diagnostic criteria (ISTH).7 DIC was developed in 71.4% of patients who died from COVID-19, while it only occurred in 0.6% of those who survived.7
SARS-CoV-2-induced excessive immune response and inflammatory injury lead to endothelial dysfunction, dysregulation of coagulation factors and complement, platelet activation and death, as well as release of NETs, thereby promoting thrombosis (Fig. 2), and eventually resulting in an imbalance of the coagulation system, coagulation dysfunction, and a range of pulmonary and extrapulmonary complications. These multiple factors eventually result in pathological angiogenesis, thrombosis, and clotting disorders.
Viral infection can lead to systemic hypoxia, which may cause coagulation protein imbalance and increased activation of the coagulation cascade.139 Meanwhile, proteomics showed that in deceased COVID-19 patients, several coagulation factors such as prothrombin (F2), factor XI, XII, and XIIIa, etc. involved in the coagulation, anticoagulation, and fibrinolysis systems, were dysregulated, which may lead to coagulopathy in COVID-19.140 Elevated plasma levels of complement component 5 (C5) activation products, C5a and C5b-9 in the patients with COVID-19 indicated complement activation.141 S protein of SARS-CoV-2 can interfere with the function of complement factor H to activate complement bypass, and directly block the combination of complement factor H with heparin, leading to complement imbalance.142
In the context of COVID-19, platelets and platelet activation biomarkers are elevated in deceased patients.143,144 SARS-CoV-2 binds to platelets through S protein to promote platelet activation,145 activated platelets drive monocytes aggregation and increase the tissue factor (TF) expression, ultimately leading to the deterioration of coagulation.146 Transcriptomic analysis showed that SARS-CoV-2 infection markedly altered expression of genes related to platelet and triggered strong platelet hyperreactivity, leading to increased platelet activation and aggregation by activating mitogen-activated protein kinase (MAPK) pathway and subsequent thrombin production.147 SARS-CoV-2 particles were internalized by platelets in an ACE2-independent manner, resulting in rapid digestion, programmed cell death, and release of extracellular vesicles.148
NETs are a key factor for COVID-19-associated immunothrombosis, and plasma of patients with COVID-19 can induce the formation of NETs.149 Pulmonary autopsy also confirmed infiltration of NETs.150 Overactivated platelets recruit neutrophils, which increase the release of NETs.151 In addition, SARS-CoV-2 triggered NETs dependent of ACE2, viral replication, serine proteases, and protein arginine deiminase 4 (PAD4).152 NETs bind to the factor XII zymogen and induce coagulation in a factor XII-dependent manner.153 The accumulation of NETs in the vessels results in rapid occlusion of the affected vessels, microcirculation disruption, and organ injury.154
Dysregulation of immune thrombosis is a key indicator of the disease severity of COVID-19.151 Endothelial cell injury and activation, thrombin activation, platelet activation and aggregation, as well as neutrophil recruitment and activation are involved in the complex processes of immunothrombosis. In addition, COVID-19 patients showed excessive activation of non-phagocytic cell oxidase (Nox) 2, which induced oxidative stress to cause vascular occlusion, platelet aggregation, and ultimately thrombosis.155
Dysregulation of RAS system
Apart from acting as an entry receptor for SARS-CoV-2, ACE2 seems to be a protective molecule for the heart and kidneys, and viral binding may deregulate its protective effect. RAS system is involved in the regulation of cardiac, renal, and vascular physiology.13 RAS dysfunction is related to the development of acute lung injury and ARDS, and associated with poor prognosis.156 ACE2 negatively regulates RAS system and maintains physiological homeostasis, by converting Ang I to the nonapeptide Ang 1–9, an inactive form of Ang, and Ang II to the counter‑regulatory heptapeptide, Ang 1–7.157 These peptides have vasodilatory and antiproliferative effects, and have protective functions by interacting with MAS1 receptor, which is a G protein-coupled receptor.158 As a potent vasoconstrictor, Ang II mediates vasoconstriction via AT1R and vasodilatation through Ang II type 2 receptor (AT2R). In the context of SARS-CoV-2 infection, cleavage of ACE2 by a disintegrin and metallopeptidase domain 17 (ADAM17) and TMPRSS2 facilitates cell entry.158 This process may lead to ACE2 shedding and loss of protective function of ACE2, subsequently increase Ang II levels and finally induce AT1R stimulation and AT2R inactivation.159 This process triggers the secretion of aldosterone, vasopressin, and adrenocorticotropic hormone (ACTH), hypokalemia, sodium reabsorption, inflammation, cell proliferation, and lung injury. ACE2/Ang 1–7/MAS axis counterbalances the deleterious effect of the ACE/Ang II/AT1R axis. ACE2 downregulation leads to pulmonary vascular hyperpermeability and coagulation, which in turn results in multiple organ damage.160 The ACE2 downregulation promotes pathological changes in acute lung injury and participates in inflammatory and fibrotic responses,14,161 and aggravates disease progression of COVID-19.162 ACE2 deficiency in patients with advanced age, comorbidities such as cardiovascular disease, diabetes mellitus, or increased shedding of ACE2 due to the infection, may result in overactivity of the ACE/Ang II/AT1R axis, contributing to enhanced inflammation and thrombosis.163 Therefore, ACE2 acts as a key mediator and a therapeutic target for COVID-19.
ARDS and its association with extrapulmonary complications
SARS-CoV-2 predominantly displays a respiratory tissue tropism and commonly causes pulmonary complications such as pneumonia and, in severe cases, ARDS or hypoxemic respiratory failure. Meta-analysis has shown that 18% of patients hospitalized with COVID-19 had severe disease, with 15% developing ARDS.164 COVID‐19 associated ARDS is more likely to have worse outcomes than ARDS secondary to other predisposing causes, with mortality ranging from 26 to 61.5% in patients admitted to intensive critical care unit (ICU) and from 65.7 to 94% in those receiving mechanical ventilation.165
Although SARS-CoV-2 can affect various tissues and organs through widely distributed ACE2 in cardiovascular, renal, and gastrointestinal systems, etc. During the initial phases of infection, SARS-CoV-2 may be restricted to the respiratory tract, thus currently the laboratory diagnosis of SARS-CoV-2 infection is based on the detection of viral nucleic acid in the nasopharyngeal (NP) or oropharingeal (OP) swab. The intense intracellular replication of SARS-CoV-2 causes programmed cell death including apoptosis and pyroptosis induced by inflammasome, resulting in capillary leakage and proinflammatory cytokines release and tissue damage.166 The activation of inflammasome is triggered by viroporins-induced ion influx or by endoplasmic reticulum stress response. Pyroptosis of infected airway endothelial cells may allow SARS-CoV-2 to leak out into the bloodstream and circulate to other organs and infect ACE2-expressing cells at local sites, resulting in extrapulmonary organ injuries.114
Airway epithelial cells are the first gateway for SARS-CoV-2 invasion. Initial infection site is the ciliated cells within proximal airway epithelium, but in severe cases, infection or injures induced by SARS-CoV-2 occurs diffusely in the alveolar epithelium, leading to gas-exchange impairment and respiratory failure with a high mortality rate. In the gas-exchange region of the distal lung, the alveolar facultative progenitors, alveolar type 2 (AT2) epithelial cells are the main target of infection.167 AT2 cells are specialized to synthesize and secrete surfactant, which is indispensable to reduce alveolar surface tension and prevent alveoli from collapsing and is involved in pulmonary host defense. Infection in this region induces progressive hypoxia and inflammatory cell infiltrates, which drive ARDS in severe cases of COVID-19.168 AT2 cells also play a critical role in regulating alveolar hypercoagulation and fibrinolysis inhibition by PAI-1 and urokinase production. Infection of AT2 cells initiates the innate immune response that favors virus propagation to adjacent alveoli and perpetuates a hyperinflammatory state, resulting in ARDS with diffuse alveolar damage (DAD), microvasculature injury, hyaline membranes, thrombosis, and fibrin deposition in the alveoli.169,170
The evolution of ARDS can be divided into three phases, including acute exudative, proliferative, and fibrotic phases. In exudative phase, DAD and endothelial injury induce the formation of intra-alveolar hyaline membrane, as well as widening and edema in the lung interstitium. In the proliferative and fibrotic phases, AT2 cells hyperplasia, fibroblasts proliferation and chronic inflammation may lead to pulmonary fibrosis. Pulmonary fibrous strips and fibrosis were reported in 17% of COVID-19 patients.171 The hallmark in the pathophysiology of ARDS is the increase in permeability of the alveolar-capillary epithelial barrier that allows protein-rich fluid to enter the alveoli leading to pulmonary edema, hypoxemia, and consequent release of proinflammatory cytokines such as IL-1β, IL-6, IL-8, and TNF-α.172 Similar pathological changes of DAD in the lung are identified in COVID‐19 associated ARDS and the typical ARDS.173
Alveolar macrophages are critical for pathogen recognition, normal tissue homeostasis, the orchestration of lung inflammation and resolution of ARDS.174 Upon stimulation, alveolar macrophages can recruit neutrophils and monocytes via several chemokines such as IL-8 to the injury site in the lung. These cells contribute to the production of inflammatory mediators, such as ROS, proteases, cytokines, etc., which subsequently induce distal cell death, specifically AT2 epithelial cells. Moreover, alveolar macrophages can interact with lymphocytes, epithelial cells and mesenchymal stem cells (MSCs) in a paracrine manner, thereby augmenting inflammatory response and accentuating tissue injury.
ARDS is a progressive systemic inflammatory syndrome with lung involvement and extrapulmonary multi-organs damage. Elevated proinflammatory cytokines were observed in both bronchoalveolar lavage fluid (BALF) and plasma from patients with ARDS.175 COVID-19 associated ARDS is a typical “pulmonary” ARDS. The hallmark of severe ARDS secondary to COVID-19 is cytokine storm resulted from dysregulated inflammatory responses.176 In the meantime, the spillover of proinflammatory mediators into the peripheral bloodstream can maintain and augment the inflammatory response, causing extensive tissue damage to other organs. Endothelial cells are involved in the pathogeneses of both ARDS and extrapulmonary organ dysfunction, possibly through mediating systemic endotheliitis with marked infiltration of inflammatory cells and apoptotic bodies in various tissues and organs.114 The widespread endothelial inflammation alters integrity of vessel barrier and promotes procoagulant state and contributes to the tissue edema and organ ischemia, leading to histopathologic alterations and systemic complications in severe COVID-19 patients.177
Current evidence suggests that COVID-19-associated extrapulmonary organ injury can also be explained by cross-talk between the organs.178 Pulmonary complication is a key driver of increased mortality in patients with AKI, highlighting a bidirectional relationship. Recent studies confirmed the close relationship between alveolar and tubular damage, the lung–kidney cross-talk in ARDS.179 Cytokine such as IL-6 overproduction is involved in lung–kidney bidirectional damage.180 ARDS can induce renal medullary hypoxia, which is an additional insult to tubular cells.180 In addition, lung–heart,181 gut–lung,182 and brain–lung interactions,183 etc., have also been proposed as potential underlying mechanisms of SARS-CoV-2-induced multiorgan dysfunction.
Extrapulmonary complications
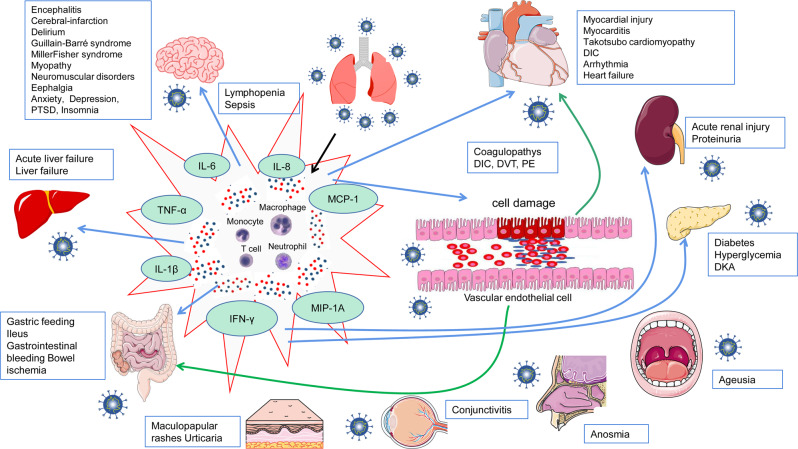
In addition to the respiratory system, many other important organ systems are also vulnerable to the SARS-CoV-2 infection, resulting in several extrapulmonary manifestations and complications (Fig. 3). The systemic manifestations of COVID-19 vary, but these complications are largely interwoven by certain shared mechanisms, involving direct viral cytotoxicity, immune disturbances, endothelial damage and thromboinflammation, and ACE2-associated RAS system dysregulation.
Fig. 3.
The extrapulmonary complications of COVID-19. SARS-CoV-2 infection has resulted in not only a pulmonary disease but also potentially systematic disease, which may cause long-term multiple organ-system complications including hyperinflammatory syndrome, vascular thrombosis, coagulopathy, cardiovascular, hepatobiliary, gastrointestinal, renal, neurologic, endocrinologic, ophthalmologic, nasal, oral, and dermatologic systems. Proposed mechanisms of the involvement of different organs or systems for COVID-19 caused by infection with SARS-CoV-2 include: direct viral toxicity through interaction of SARS-CoV-2 spike protein with the entry receptor ACE2; dysregulation of the immune response, T-cell lymphodepletion and hyperinflammation; endothelial cell damage and thromboinflammation. COVID-19 coronavirus disease 2019, SARS-CoV-2 severe acute respiratory syndrome coronavirus 2, DIC disseminated intravascular coagulation, PE pulmonary, DVT deep venous thrombosis, DKA diabetic ketoacidosis, PTSD post-traumatic stress disorder
Cardiovascular complications
Adverse cardiovascular events of COVID-19
Cardiovascular system is frequently involved during the development and exacerbation of COVID-19, particularly in patients with preexisting cardiovascular diseases such as hypertension, heart failure or coronary heart disease. There are several potential mechanisms, involving myocardial injury, exacerbation of the underlying cardiovascular comorbidities, as well as cardiovascular adverse effects of the drugs used in the treatment of COVID-19.
Myocardial injury defined as elevated serum cardiac troponin I concentrations or abnormalities in electrocardiogram (ECG) or echocardiogram, is a common complication in the development and exacerbation of COVID-19. The incidence of myocardial injury differed among patients with different severities of COVID-19, with 10% in mild cases, roughly 30% in hospitalized patients on admission and ~50% during hospitalization.184 An early study of 138 patients hospitalized with COVID-19 in Wuhan showed that myocardial injury was observed in 7.2% of hospitalized COVID-19 patients and 22% of those in the ICU.185 A report from China showed that during hospitalization roughly 12% of patients without a history of cardiovascular diseases showed elevated levels of troponin or cardiac arrest. It is worth noting that elevated high-sensitivity troponin I was found in 46% of the deceased COVID-19 patients but only 1% of the survivors.186 COVID-19-related myocarditis is characterized by myocardial injury without an ischemic cause and inflammatory infiltrates.187,188 Acute and delayed-onset myocarditis have been reported in previous cohorts as well as the autopsy studies of COVID-19 deaths.189 Fulminant myocarditis and cardiogenic shock were accompanied by atrial and ventricular arrhythmias.190 Takotsubo cardiomyopathy is a non-ischemic cardiomyopathy characterized by transient weakening of the cardiomyocytes and subsequent ballooning of the apex.191,192 In all, 2–7.75% of COVID-19 patients presenting with acute coronary syndrome were diagnosed with stress-induced cardiomyopathy. Nearly one-third of the COVID-19 patients with myocardial involvement were complicated by cardiogenic shock.191 COVID-19 may predispose patients to arterial and venous thrombosis.193 The critically ill patients with COVID-19 have high venous thromboembolism risk of 31–40%.136 The incidence of disseminated intravascular coagulation (DIC) was 71.4% in COVID-19 deaths. Lung microvasculature fibrin deposition can result in ARDS in patients concomitantly diagnosed with DIC.194 The COVID-19 associated myocardial injury and subsequent cardiac dysfunction may cause cardiac arrhythmias. Relative tachycardia and bradycardia frequently occurred in mild to critically ill patients with COVID-19.195 In all, 16.7% of patients hospitalized with COVID-19 and 44% of those referred to ICU developed cardiac arrhythmia.192,196,197 Abnormal PR interval behavior with increasing heart rate and QT prolongation are frequently observed in critically ill patients.196,198 it remains unclear whether high prevalence of heart failure in patients hospitalized with COVID-19 with a known history of cardiac disease, results from worsening of preexisting left ventricular dysfunction or newly developed cardiomyopathy. An early report on 113 COVID-19 deaths showed high incidence of cardiac complications including heart failure and acute cardiac injury.93 Cardiogenic shock was developed in one-third of COVID-19 cases with myocardial involvement and carried a high mortality of 26%.199
Newborns and children are expected to be less susceptible to COVID-19 partly because of the reduced function of ACE2 receptors. SARS-CoV-2 infection appears to be asymptomatic or mild in most children, some may develop a severe inflammatory syndrome with symptoms similar to Kawasaki disease or toxic shock syndrome. This Kawasaki-like illness have been called the multisystem inflammatory syndrome in children (MIS-C).200 Of recovered 99 competitive athletes with asymptomatic or mild SARS-CoV-2 infection, 3.3% had myopericarditis or pericarditis, which is associated with exercise-induced ventricular arrhythmias or cardiac symptoms.201 Myocardial injury and left ventricular dysfunction in pregnant women had a high mortality rate of 13.3%, which was attributed to malignant arrhythmias.202
Pathogenesis of cardiovascular complications of COVID-19
COVID-19 related myocardial injury is frequently observed and is associated with poor prognosis. The central pathophysiology of COVID-19 related myocardial injury involves a complex interplay between viral tropism, dysregulated host immune response, alteration in ACE2 and RAS system homeostasis, the vascular dysfunction, myocardial oxygen supply–demand imbalance as well as microvascular and macrovascular thrombosis.5,203,204
The cardiovascular pathology of COVID-19 can result from a direct SARS-CoV-2 cardiotoxicity. Human pluripotent stem cell-derived cardiomyocytes (hPSC-CMs) expressing ACE2 are permissive to SARS-CoV-2 replication. Notably, SARS-CoV-2-infected hPSC-CMs exhibit progressively impaired contractile and electrophysiological properties, and extensive cell death.205,206 Cardiac stromal cells can be infected by SARS-CoV-2, which could contribute to myocardial injury. Moreover, stromal cells exposed to SARS-CoV-2 can evolve into hyperinflammatory and pro-fibrotic phenotypes via ACE2-independent mechanism.
Platelet activation plays an important role in the pathogenesis of thrombotic events and cardiovascular complications. S protein of SARS-CoV-2 induces platelet activation directly to facilitate leukocyte–platelet aggregate formation, the release of coagulation factors and inflammatory mediator, thereby resulting in thrombosis formation. Furthermore, the MAPK cascade, considered as a downstream signaling of ACE/Ang II, mediates the activation effect of SARS-CoV-2 on platelet.145
Abundant expression of Th1 and Th2 cytokines lead to direct cardiac immunological injury and chemotaxis of neutrophil and macrophage.207,208 The inflammasome activation in the patients with COVID-19 is strongly related to hypercoagulopathy and cytokine storm, contributing to the COVID-19-associated cardiac injury. Under certain cardiovascular conditions, the inflammatory response triggered by the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome activation leads to hyperinflammation, which promotes cardiac injury and could be targeted for the treatment of COVID-19.209
The damage-associated molecular patterns (DAMP) ligands of the receptor for advanced glycation end products (RAGE) may exacerbate the local responses to infection in the heart, leading to severe cell stress and death, which in turn result in endothelial dysfunction, immune cell activation, oxidative stress, and upregulation of distinct factors such as early growth response 1 (EGR1). The inexorable accumulation of advanced glycation end products (AGEs) and other DAMP RAGE ligands relevant to cardiometabolic perturbation may prime the organs for amplification of inflammatory and tissue-damaging mechanisms upon SARS-CoV-2 infection.210 Nox2 is upregulated in pneumonia and closely associated with troponin elevation. Nox2-derived oxidative stress may contribute to myocardial injury via production of ROS, and thus inhibition of Nox2 may have therapeutic potential for COVID-19.211 Alteration in RAS after SARS-CoV-2 infection could predispose bradykinin storm. Given that bradykinin and its metabolites are inducers of endothelium-dependent vasodilation, vascular permeability, and pain via the activation of the G protein-coupled receptors B1 and B2, this signaling could be a new therapeutic target of cardiovascular dysfunction and thromboembolism induced by COVID-19.212
Renal complication
Adverse renal events of COVID-19
AKI is a frequent complication in inpatients with COVID-19, with an incidence ranging from 10 to 80%.213–217 A meta-analytic study including 49,692 COVID-19 patients demonstrated that AKI was a common and serious complication of COVID-19. The in-hospital mortality risk was significantly increased in COVID-19 patients complicated by AKI.218 Elevated serum creatinine and proteinuria are the main clinical features of COVID-19 with kidney injury. Another meta-analytic study219 including 4963 COVID-19 patients showed that 9.6% of patients had elevation of serum creatinine. Of these patients, 57.2% had proteinuria. Proteinuria was reported in COVID-19 patients who did not develop AKI, which may indicate subclinical renal damage. Proteinuria occurs in patients with nephropathy, and significant heterogeneity exists between studies.220–222
Pathogenesis of renal complications of COVID-19
Multiple possible mechanisms may be involved in COVID-19 associated AKI, including SARS-CoV-2-mediated injury, inflammatory response, cytokine storm SARS-CoV-2-induced, activation of the ACE/Ang II pathway, dysregulation of complement, hypercoagulation, and microangiopathy.223 In an autopsy study of 63 COVID-19 patients, the viral RNA presence in the kidneys is correlated with older age and increased comorbidities, as well as reduced survival time. These results indicate a potential association between the renal tropism of SARS-CoV-2 and adverse clinical outcome.224 Renal tubular epithelial cells and podocytes express ACE2,225 while the distal nephrons but not the proximal tubules express TMPRSS2.223
The hyperinflammatory state of COVID-19 can result in kidney injury. Previous studies have found that high levels of cytokine release and inflammatory response lead to microvascular dysfunction, capillary hyperpermeability and insufficient perfusion, causing renal microcirculatory dysfunction.226 The critically ill COVID-19 patient had increased IL-6 levels that were associated with kidney damage possibly due to lung–kidney cross-talk.180 The bidirectional relationship between alveolar and tubular damage, lung–kidney cross-talk in ARDS is confirmed by recent studies.179 ARDS can induce hypoxia in the renal medulla, which may result in renal tubular epithelial cells injury, subsequently leading to the upregulation of IL-6.180 Glomerular diseases have been found in COVID-19 patients with kidney involvement.227 The most common pathological feature of glomerular disease is collapsing glomerulopathy.228–232 Collapsing glomerulopathy is a distinct pathology related to COVID-19, which may affect patients carrying high-risk APOL1 genotypes.233,234 Kidney biopsy of COVID-19 patients who had APOL1 high-risk genotype showed collapsing glomerulopathy, tubuloreticular inclusions in endothelial cells, and acute tubular injury, without evidence of SARS-CoV-2 infection or replication in kidney cells.227 During viral infection, IFN and TLR3 activation is sufficient to upregulate APOL1 gene expression.235 These findings suggest plausible mechanisms involving “two-hit” of cytokine-mediated host response to SARS-CoV-2 infection and genetic susceptibility.227,233
Kidney injury may be related to blood coagulation disorder in COVID-19 patients. In a kidney autopsy report of a patient who died from COVID-19,236 the renal parenchyma showed diffuse coagulative cortical necrosis, with widespread glomerular microthrombi. Electron microscopy showed extensive cross-linked fibrin deposition and partially shed capillaries in the capillary lumen. It is suggested that thrombotic microangiopathy instead of DIC is manifestation of coagulopathy in COVID-19 patients with kidney injury.237–239 Glomerular ischemia and endothelial cell damage also appear in some cases.240 Glomerular ischemia was observed in patients with fibrin thrombi in the glomerular capillary loops, which may be related to coagulation activation in COVID-19 patients.6,241 In addition, an interaction between Ang II overactivity, and complement pathways could also influence AKI severity and outcomes.
COVID-19 patients often present the respiratory and gastrointestinal symptoms, which may cause fluid loss. Once the fluid is not refilled in time or insufficient, it may lead to insufficient renal perfusion. In a retrospective study of 5,449 COVID-19 patients,216 AKI occurred in 36.6% of patients, and a majority of AKI patients had urine sodium lower than 35 mmol/L, indicating a state of pre-renal azotemia. In addition, ARDS or respiratory failure can reduce cardiac output through hemodynamic changes and high chest pressure, which may cause systemic inflammation and reduced renal perfusion induced by hypoxemia, leading to AKI.8
Drug-induced nephrotoxicity may contributor to COVID-19-related kidney injury.242 Some antivirals, antibiotics, and nonsteroidal anti-inflammatory drugs (NSAIDs) given to patients with COVID-19 during hospitalization may have possible nephrotoxicity and be involved in the development of AKI.243 A retrospective observational study showed that exposure to vancomycin and use of NSAIDs were risk factors associated with the development of AKI.244
Gastrointestinal complications
Adverse gastrointestinal events of COVID-19
Diarrhea and other gastrointestinal symptoms are frequent in COVID-19 patients.1,93,245 Severe COVID-19 patients are more likely to develop gastrointestinal symptoms. The presence of digestive symptoms is associated with the disease severity.246 Gastrointestinal comorbidities of COVID-19 include hypomotility-related complications, gastrointestinal bleeding, and bowel ischemia.247 Gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain may precede or accompany with pulmonary symptoms in COVID-19 patients, and the incidence ranged from ~10 to 60%.247–250 The three most common symptoms were anorexia, diarrhea, and nausea or vomiting from a meta-analysis comprising 60 studies with 4243 patients.248 Anosmia and ageusia were commonly associated with nausea and anorexia after controlling for potential confounders.251
Gastrointestinal symptoms were more frequent in critically ill patients with COVID-19 than critically ill patients without COVID-19.252 Patients with COVID-19 who had diarrhea required more ventilator support and intensive care than those without diarrhea.250 The time from disease onset to admission in COVID-19 patients with gastrointestinal symptoms was longer than in those without gastrointestinal symptoms.246 The presence of gastrointestinal symptoms was associated with a high risk of ARDS, non-invasive mechanical ventilation and tracheal intubation, but not with mortality in COVID-19 patients.253 Patients with gastrointestinal symptoms had higher rates of positive results for a COVID-19 test than those without.254 Roughly 10% of COVID-19 patients presented initially with only gastrointestinal complaints without any respiratory symptoms, which may possibly cause a delay in COVID-19 diagnosis.246,255
Pathogenesis of gastrointestinal complications of COVID-19
Gastrointestinal injury associated with SARS-CoV-2 infection may be attributed to several proposed mechanisms, including direct cytotoxic damage, intestinal endothelial cell injury and thromboinflammation, dysregulated immune response.10 These mechanisms can interact with each other and in turn exacerbate gastrointestinal injury.10
The detection of SARS-CoV-2 RNA and viral protein in gastric, duodenal, and rectal glandular epithelial cells256 is indictive of the tropism of SARS-CoV-2 to the digestive system. Patients with diarrhea had higher positive rate for SARS-CoV-2 RNA in fecal samples than those without diarrhea.248 Current evidence shows that the gastrointestinal symptoms in COVID-19 may be caused by the direct effects of SARS-CoV-2 on the gastrointestinal tract. SARS-CoV-2 may invade the digestive system through ACE2, and growing evidence supports the possible fecal-oral transmission route of SARS-CoV-2. ACE2 is abundantly present in the gastrointestinal epithelial cells, with the highest expression in the small intestine, suggesting that the gastrointestinal tract may be susceptible to SARS-CoV-2 infection.256–258 TMPRSS2 had relatively high expression levels in both the small intestine and the colon.259 SARS-CoV-2 downregulates ACE2 expression by binding its S protein, thereby contributing to inflammation and injury of gastrointestinal epithelium.260–262 ACE2 deficiency in intestinal epithelial cells may be linked to malabsorption of nutrients, altered gut microbiota composition, and intestinal barrier dysfunction.263
The activation of coagulation promotes thrombin generation, activates complement system and inhibits fibrinolysis, which triggers thromboinflammation, leading to microthrombi deposition and microvascular dysfunction in the gastrointestinal system.94 COVID-19-related cytokine storm and hyperinflammatory immune state might induce gut mucosal immune system activation and enhance immune-mediated inflammatory response in the gastrointestinal system, which contribute to gastrointestinal injury.94,260,264,265 The gut microbiota plays a critical role in the maintenance of intestinal homeostasis, and altered microbiota composition is associated with intestinal inflammation. Evidences suggest that SARS-CoV-2 infection is associated with alterations in the gut microbiota.266 Gut microbiota may be involved in the magnitude of COVID-19 severity through modulation of host immune responses. Moreover, after resolution of COVID-19, the gut microbiota dysbiosis may be associated with persisting symptoms.267 The pathogenesis of the gut microbiota dysbiosis is multifactorial, possibly involving epithelial dysfunction, impaired production of antimicrobial peptide, as well as cytokine storm.266
Hepatobiliary complications
Adverse hepatobiliary events of COVID-19
Abnormal liver function tests have been frequently observed in COVID-19 patients, indicating that the liver is one of the most commonly affected extrapulmonary organs by SARS-CoV-2. Clinical case studies show that liver dysfunction is associated with increased risk of mortality in COVID-19 patients. The prevalence of liver injury ranged from 14.8 to 55% in COVID-19 patients.93,131,132,268–271 The pooled prevalence of liver function abnormalities was 19%.272 In a cohort including 2273 SARS-CoV-2-infected patients, acute liver injury is common but generally mild.273 Liver function abnormalities mainly manifest as slightly elevation in levels of alanine aminotransferase (ALT), total bilirubin (TBIL), and gamma-glutamyl transpeptidase (GGT).274 Aspartate aminotransferase (AST)-dominant elevation may be earlier, more frequent and significant in patients with severe COVID-19. AST levels showed the strongest correlation with mortality than other indicators of liver injury such as ALT, TBIL, and alkaline phosphatase (ALP) in COVID-19 patients.275,276 However, COVID-19 associated severe acute hepatitis has been rarely reported.277,278
It is noteworthy that liver dysfunction is closely correlated with disease severity of COVID-19. Patients with severe COVID-19 had higher prevalence of liver injury,1,131,185 and patients with liver dysfunction were at higher risks of disease progression.269,271,279 The incidence rate of liver injury in deceased patients with COVID-19 was 78%.274 Liver failure is observed in COVID-19 deaths and occurs more frequently among critically ill patients.280 Of 141 critically ill COVID-19 patients during their ICU stay, 4% developed acute acalculous cholecystitis and 1% developed acute pancreatitis.281 Patients with severe liver injury are more likely to have severe clinical course with high risk of mortality.
Patients with preexisting liver diseases such as non-alcoholic fatty liver disease,282,283 cirrhosis284–286 are more susceptible to SARS-CoV-2 infection and have worse clinical outcome. Chronic hepatitis B and C were more common in patients with liver injury than those without.287
Pathogenesis of hepatobiliary complications of COVID-19
Underlying mechanisms may be systemic hyperinflammation induced by cytokine storm, pneumonia-associated hypoxia, viral infection in hepatocytes or cholangiocytes and drug-induced liver injury. The cytokine storm may initiate a violent attack to the host and result in liver injury. Dramatical increase in a wide range of proinflammatory cytokines and chemokines such as GM-CSF and IL-6 was observed in patients with liver dysfunction than those with normal liver function.287 The liver biopsy showed that COVID-19-associated liver injury was likely immune-mediated.173 Taken together, the excessive inflammatory response triggered by SARS-CoV-2 infection may provoke liver injury.
Hypoxemia due to ARDS, systemic inflammatory response syndrome, dysfunction of other organs can contribute to ischemia or reperfusion-induced liver dysfunction in patients with COVID-19. Hypoxia-induced hepatocyte death and production of inflammatory cytokines can be found in hepatic ischemia/reperfusion models.288 Moreover, histopathological findings of the liver in COVID-19 patients showed the watery degeneration of a few hepatocytes, which was probably due to ischemia and hypoxia.269
SARS-CoV-2 was detected in a proportion of liver biopsy specimens in COVID-19 patients,289 but it remains unclear whether SARS-CoV-2 directly infects hepatocytes or cholangiocytes via ACE2. The upregulation of ACE2 expression in the liver was caused by compensatory proliferation of hepatocytes derived from the bile duct epithelial cells in a mouse model of acute liver injury. Some neonatal hepatocytes expressed ACE2 and were susceptible to SARS-CoV-2 infection during this compensatory process.290 Pathological and electron microscopic findings revealed typical coronavirus particles in the cytoplasm of hepatocytes from two cases of COVID-19.291 Histologically, the predominant histological features of SARS-CoV-2-infected liver were massive apoptosis and binuclear hepatocytes. The GGT and ALP levels were elevated in deceased patients, which may indicate biliary tract injury. All the aforementioned findings suggest that liver injury may not only involve hepatocyte damage but also cholangiocyte dysfunction in patients with COVID-19.
Drug-induced liver injury may also account for some hepatobiliary complications in COVID-19.292 Antipyretic therapy is frequently prescribed in COVID-19 patients. Acetaminophen may induce significant liver damage or even cause liver failure in a dose-dependent mechanism.293 In clinical practice, multiple drugs including antivirals,294 steroids and antibiotics were commonly prescribed in COVID-19 patients, particularly those with severe and critically ill disease.295 Some of these drugs may have potential hepatotoxicity and result in liver dysfunction.
Neurological and psychiatric complications
Adverse neurological and psychiatric events of COVID-19
Neurological manifestations of COVID-19 including the central nervous system (CNS)-associated and peripheral nervous system (PNS)-associated ones were present in 18.1–82.0% of the patients. The neurological symptoms were more common in those with severe COVID-19.12,296–298 COVID-19 has been reported to be associated with increased risk of mental health disorders,299 such as depression, anxiety, schizophrenia, phobia,300 obsessive–compulsive symptoms,301 post-traumatic stress disorder (PTSD).302 A significant proportion of patients experienced psychopathological complications, including 42% of anxiety, 31% of depression, 28% of PTSD, 20% of obsessive–compulsive symptoms, and 40% of insomnia.303 The neurological and psychiatric complications of COVID-19 involve encephalitis, cerebral infarction, delirium, Guillain–Barré syndrome,304–307 Miller Fisher syndrome,308 myopathy, neuromuscular disorders, cephalgia, etc.309 Frontline health workers during the COVID-19 pandemic have displayed symptoms of anxiety, depression, insomnia.310,311 Long-term isolation triggers mental disorders such as depression and anxiety in some individuals.312
Pathogenesis of neurological and psychiatric complications of COVID-19
There are many potential gateways of SARS-CoV-2 neuroinvasion from the periphery to the brain. The expression of ACE2 is relatively high in certain brain locations, such as the paraventricular nuclei of the thalamus and choroid plexus.313,314 ACE2 is also expressed on the ventrolateral medulla and the nucleus of the tractus solitaries, areas involved in the regulation of the respiratory cycle. This suggests that the virus may affect neurons regulating breathing.315 Coronavirus may directly infect sensory neurons in the olfactory epithelium and then spread to CNS from olfactory neurons.313,316 NRP1 is expressed of the olfactory epithelium, and can facilitate SARS-CoV-2 cell entry and infectivity.27 Moreover, the capillary blood vessels and lymphatics are abundant in the nasal mucosa, which may favor virus invasion.317,318 SARS-CoV-2 may possibly invade the brain from the bloodstream through the impaired blood–brain barrier319 and leak into the interstitial fluid and the cerebral spinal fluid through the intracerebral lymphatic system. SARS-CoV-2 may also enter the fourth ventricle directly through a damaged blood–cerebrospinal fluid barrier.320
The association between systemic inflammatory response and neurological or psychiatric diseases reflects that both innate and adaptive arms of immune system may affect the brain.321,322 Systemic inflammation leads to acute brain damage with cognitive impairments and psychiatric symptoms indicative of neurodegeneration.301,323 Nearly 80% of septic patients with bacteremia develop sepsis-associated encephalopathy324 and delirium.323 CNS-resident cells such as astrocytes and microglia represent the first line of defense of the CNS against systemic inflammation and infection. Systemic inflammation allows infiltration of various DAMPs into the nervous system, triggering reactive astrogliosis325 and microgliosis.326 Dystrophic astrocytes and microglia may be involved in the pathological development of neurodegenerative disorders.
Hypoxia inevitably damages the brain. The greatest central fatigue in acute hypoxia occurs when arterial oxygen saturation (SaO2) is ≤75%, a level that coincides with increasing impairments in neuronal activity.327 Hypoxia increases ROS production leading to oxidative damage to neural cells.328 Excessive ROS production can directly degenerate or modify cellular macromolecules, including membranes, proteins, lipids, and DNA, and result in activation of inflammatory cascade and protease secretion, finally contributing to brain injury.328 Brain hypoxia is also directly linked to activation of inflammatory pathways by stimulating hypoxia-inducible factors and the NF-κB signaling cascade, which promote the release of proinflammatory factors.329 Severe hypoxia may cause extensive damage to brain structure, leading to cognitive and neurodegeneration defects. Three main mechanisms appear to be responsible for the occurrence of ischemic strokes in COVID-19,330,331 including a hypercoagulable state, vasculitis, and cardiomyopathy. COVID-19 can induce an immune-thrombotic and DIC, which can explain for thrombosis on a consumptive basis.332 Other studies have suggested that thrombosis occurs in 20–30% of critically ill COVID-19 patients, even with prophylaxis.333,334
Stressors exacerbate both systemic inflammation and inflammatory damage to the brain by activating the hypothalamic–pituitary–adrenal axis.335 Levels of CRP demonstrate association with levels of depression.336 Neuroinflammation is largely associated with several neuropsychiatric and neurocognitive diseases,337 including depression, psychosis and neurodegeneration. Depression is a well-known risk factor of dementia, and psychological burden of COVID-19 may increase the neurodegenerative disease rates in the aftermath of the pandemic.338
Endocrine and metabolic complications
Adverse endocrine and metabolic events of COVID-19
Endocrine and metabolic systems can also be involved in COVID-19.339 Database from Chinese Centers for Disease Control and Prevention (CDC) showed that of 20,982 patients with COVID-19, 5.3% had diabetes.340 Among COVID-19 patients with chronic comorbidities, type 2 diabetes was the second most common morbidity (7.4%).341 Diabetes is one of the most relevant comorbidities associated with adverse prognosis of COVID-19.342–344 A study on 72,314 COVID-19 patients reported that the mortality rate of patients with diabetes was 7.3%, which was higher than those without diabetes (2.3%).345 A whole-population study showed that compared with patients without diabetes, the odds ratios for in-hospital COVID-19-related death were 3.51 in those with type 1 diabetes and 2.03 with type 2 diabetes.346 Pregnant women with diabetes might be more vulnerable to the severe effects of COVID-19.347
The resultant complications including hyperglycemia and diabetic ketoacidosis were associated with poor prognosis of COVID-19 patients. Acute hyperglycemic crisis, diabetic ketoacidosis and hypertonic hyperglycemia are serious acute metabolic complications usually caused by infection.348 Of 2366 patients hospitalized with COVID-19, 157 (6.6%) patients developed diabetic ketoacidosis, 94% of whom had preexisting type 2 diabetes, 0.6% had preexisting type 1 diabetes, and 5.7% patients had no previous diagnosis of diabetes.349
Approximately 15% of mild to moderate COVID-19 patients had thyroid dysfunction.350 Of 50 COVID-19 patients without previous history of thyroid disease, 56% (28/50) had low thyroid-stimulating hormone (TSH) levels.351 The levels of serum TSH and total triiodothyronine (T3) in patients with COVID-19 were significantly lower than in those without COVID-19.352 The degree of decrease in TSH and total T3 levels was positively correlated with the disease severity of COVID-19.351 Low free T3 due to nonthyroidal illness syndrome is associated with in-hospital mortality in patients in the ICU requiring mechanical ventilation.353
Pathogenesis of endocrine and metabolic complications of COVID-19
Insulin-producing pancreatic β cells express ACE2 and related entry mediators including TMPRSS2, NRP1, and transferrin receptor (TRFC), with selectively high expression of NRP1.354 Evidence demonstrates that SARS-CoV-2 can infect human pancreatic β cell, thereby attenuating the secretion of pancreatic insulin and inducing β cell apoptosis, which possibly contribute to worsening hyperglycemia seen in COVID-19 patients.354 Elevated blood glucose levels in COVID-19 patients are related to insulin resistance, which indicates pancreatic β-cell dysfunction or apoptosis, as well as insulin’s inability to dispose of glucose into cellular tissues.355 Whether ACE2 was expressed in thyroid tissue or other endocrine organs remains controversial.356
Cytokine disorders and T-cell depletion were observed in patients with diabetes, which may be associated with poor clinical outcomes.97,357–360 The function of NK cells that play important role in controlling infection is impaired in patients with type 2 diabetes. Glycated hemoglobin was an independent predictor of NK cell activity in patients with type 2 diabetes.361,362 In the animal model, hyperglycemia was found to be the main cause of systemic inflammation.363 Hyperglycemia and insulin resistance promote synthesis of advanced glycation end products and proinflammatory cytokines, oxidative stress, and adhesion molecules that mediate tissue inflammation,364 which may be underlying mechanisms responsible for adverse outcome in patients with diabetes. Potential pathogenetic links between COVID-19 and diabetes include disrupted glucose homeostasis, inflammation, altered immune status and activation of the RAS.11 Elevated glucose levels directly induce viral replication and proinflammatory cytokine production, which may favor SARS-CoV-2 infection and monocyte response through hypoxia-inducible factor-1a (HIF-1α)/glycolysis-dependent axis.365 Elevated cytokines, imbalance of Th1/Th2 cytokine ratio, decreased peripheral CD8+ T cells and NK cell counts contribute to the high mortality of COVID-19 patients with type 2 diabetes.366
Other extrapulmonary complications
Co-infection
The prevalence, incidence, and characteristics of existing viral or bacterial co-infection in COVID-19 patients is not well understood and has been raised as a major concern. It was reported in a meta-analysis of 28 studies including 3448 patients with COVID-19 showed that bacterial estimated co-infection was identified in 3.5% of patients and secondary bacterial infection in 15.5% of patients.367 The overall proportion of COVID-19 patients with bacterial infection was 7.1% but varied in different patient populations, ranging from 5.8% in hospitalized patients to 8.1% in critically ill cases and up to 11.6% in deceased cases.367 The most common organisms reported were Mycoplasma species, Haemophilus influenzae and Pseudomonas aeruginosa.367 Another meta-analysis of 30 studies including 3834 patients reported that 7% of hospitalized COVID-19 patients had a bacterial co-infection.368 The pooled proportion of a viral co-infection was 3%, with respiratory syncytial virus and influenza A being the most common pathogens.368 Another meta-analysis including 8 studies reported viral co-infections including rhinovirus/enterovirus and influenza A were the most frequent co-infected pathogen. Coronavirus, respiratory syncytial virus, parainfluenza, metapneumovirus, and influenza B virus were also reported as co-pathogens.369 To date, the reports on fungal co-infections are scarce or lack of detailed information. A study from China performing fungal culture in all 99 COVID-19 patients at admission confirmed five (5%) cases with fungal infection, including Aspergillus flavus, Candida glabrata, and C. albicans.370 Another study reported that 5.8% of the patients had fungal co-infection in 52 critically ill patients, including A. flavus, A. fumigatus, and C. albicans.371 A German study showed that COVID-19-associated invasive pulmonary aspergillosis (IPA) was found in five (26.3%) of 19 consecutive critically ill patients with ARDS.372 It should be critically paid attention to the probability of COVID-19 accompanied by fungal infections.373 The tuberculosis and SARS-CoV-2 co-infection has been rarely reported.374,375
A number of immunocompromised individuals were hospitalized with COVID-19 and some were diagnosed with secondary infections.376 The specific source and pathogens of these infections have not yet been fully identified. SARS-CoV-2 infection-induced diffuse alveolar injury combined with intra-alveolar neutrophilic infiltration and vascular congestion.377 These histologic damages could pave the way for secondary infections including bacterial or fungal infection such as COVID-19-associated invasive pulmonary aspergillosis (CAPA).373 Besides, COVID-19 patients are usually characterized by lymphopenia and immune dysfunction, which also help facilitate pathogen invasion.94 A case control study reported that steroids use was also a significant risk factor for bacterial infection in patients with severe to critically ill COVID-19.378 Critically ill patients were more likely to develop fungal co-infections.371
Ocular complication
According to a systematic review including 4432 patients from 35 studies, the prevalence rate of ocular manifestations was 11.3% in adult patients with COVID‐19.379 Ocular manifestations are non-specific, and conjunctivitis manifested as redness, watering, discharge, and foreign body sensations, is the most commonly reported.380 Other ocular complications include dry eye, blurred vision, ocular pain, photophobia and itchiness, etc. Notably, ocular signs and symptoms were the initial presentation in 3.3% COVID-19 patients.379 Patients with severe pneumonia have a significantly higher likelihood of ocular manifestations than mild-to-moderate pneumonia.
The conjunctiva is directly exposed to the environment, and easily contaminated with respiratory droplets or hands carrying the virus. A pooled data showed that the positive rate of SARS-CoV-2 RNA was 7.4% in the ocular surface of COVID-19 patients.379 Several studies have already demonstrated the expressions of ACE2 and TMPRSS2 in the cornea and conjunctiva, although their expressions were obviously lower in comparison to other tissues, such as lung and digestive tract.381 In vitro study demonstrated that SARS-CoV-2 can directly infect the corneal cells from human eyes and hESC-derived eye organoids.382 Although conjunctiva is unlikely to be a preferred entry gateway for SARS-CoV-2, the expressions of SARS-CoV-2 in tears and conjunctival secretions partially explain ocular complications.
Ear-nose-throat (ENT) complication
Mounting evidence indicates that olfactory and gustatory dysfunction is closely correlated with COVID-19.383 A systematic review summarized that olfactory and gustatory loss was observed in 41.0% and 38.2% of COVID-19 patients, respectively.384 In particular, some patients may only have olfactory or gustatory loss in the absence of other clinical symptoms. A multicenter study from Europe reported that 11.8% of patients presented with olfactory loss as their first symptoms.385 Most patients get recovery from the symptoms within 4–6 weeks of follow-up, and only 3.59% and 3.27% of patients with olfactory and gustatory loss, respectively, showed partial recovery beyond 8 weeks.386
The viruses may induce an inflammatory response of nasal mucosa or directly damage the olfactory neuroepithelium. SARS-CoV-2 may not directly enter olfactory sensory neurons due to lacking of ACE2 receptor expression, but rather attack the supporting and stem cells of olfactory epithelium expressing ACE2 receptor.387 COVID-19 patients with influenza-like illness displayed the increased frequency of olfactory loss.386 However, olfactory loss was also reported in COVID-19 patients without nasal symptoms or significant inflammation.388
Dermatologic complication
Cutaneous manifestations have been reported in 1.8% to 20.4% of COVID-19 patients.389 The appearance of skin varies, including maculopapular rashes, urticaria, petechiae/purpura, vesicles, chilblains, livedo racemosa, and distal ischemia or necrosis.390 The trunk is a prone area of skin lesions, but the involvement of extremities may also occur. Most of the skin lesions are self-resolving, and do not appear to be related to the disease severity. Cutaneous involvement may be primarily attributed to an immune response to viral protein or nucleotides, or vasculitis and thrombotic vasculopathy secondary to systemic consequences caused by COVID-19.391 Pathological examination revealed the existence of pauci-inflammatory thrombogenic vasculopathy in the purpuric skin lesions, and the colocalization of SARS-CoV-2 S protein with C4d and C5b-9 in both normally-appearing and grossly involved skin.392
Reproductive complication
A concern has been raised that SARS-CoV-2 may cause damage to testis, and even result in the infertility. In patients with COVID-19, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) levels were elevated, while testosterone and dihydrotestosterone levels markedly decreased.393 In recovered male patients, the count, concentration and motility of sperm were still declined slightly, although sexual hormones have returned to normal levels.394 Patients with a longer recovery time showed poorer sperm quality. Pathological studies conducted on deceased COVID-19 patients found vacuolation and detachment from the tubular basement membrane of Sertoli cells, the destruction of seminiferous tubules, the reduction of Leydig cells, and the inflammatory infiltrate of T lymphocytes in the interstitium.395 ACE2 and TMPRSS2 expression is abundant in spermatogonial cells, interstitial cells, and supporting cells of testis, suggesting the testis as a potential target of SARS-CoV-2 infection.396 The immune responses triggered by SARS-CoV-2 produce lots of inflammatory mediators and induce oxidative stress in testicular cells, potentially damaging the DNA of spermatozoa. In addition, SARS-CoV-2 causes damage to Leydig cells, and subsequently lowers testosterone secretion, which may ultimately disrupt the process of spermatogenesis.397
There is no evidence that pregnancy and childbirth alter susceptibility to SARS-CoV-2 infection. These studies did not report severe maternal complications in pregnant women with COVID-19. A few studies have revealed an increased risk of preterm birth and cesarean delivery, but it is unclear whether these results are directly related to SARS-CoV-2.398 There is no direct data supporting mother-to-child transmission of SARS-CoV-2, but newborns of COVID-19 infected mothers have tested positive for SARS-CoV-2-specific antibodies and were also presenting with increased IL-6 levels.399
Hematopoietic system complication
The hematopoietic system produces immune cells that can defeat viral infections and is a source of hematopoietic stem cells (HSC) and progenitor cells (HPC). Human HSC and HPC express ACE2 on the cell surface, making them susceptible to SARS-CoV-2 infection. SARS-CoV-2 S protein binds to ACE2, induces defects in human HPC colony-forming ability and inhibits the expansion of HSC and HPC subpopulations in vitro.400 In addition, in human very small embryonic stem cells (VSELs) and HSCs, the interaction of ACE2 with S protein activates the NLRP3 inflammasome, which may cause cell pyrolysis.401 The plasma of severe COVID-19 patients induces HPC to produce suppressive bone marrow cells in vitro, in relation to the high levels of IL-6 and IL-10 in plasma.402
The hemoglobin level of patients with severe COVID-19 significantly decreased, but the circulating nucleated red blood cells increased. SARS-CoV-2 may directly infect human erythroid progenitor cells, resulting in the formation and expansion of erythroid progenitor cell colonies, thereby increasing stress erythropoiesis.403
Multiomics analysis revealed increased proliferation and metabolic hyperactivity of plasmablasts in peripheral blood of patients with severe COVID-19, as well as IFN-activated circulating megakaryocyte expansion and increased erythrocyte production characterized by hypoxic signaling.404 Another study has shown that there is a tendency for myeloid skewing in circulating HSCs and HPCs in patients with COVID-19, and the frequency of common lymphoid progenitor cells is lower in severe patients, while granulocyte/macrophage progenitor cells/neutrophil-like cells appear in severe and fatal cases.405
The implication for therapeutics
Currently, antivirals, glucocorticoids, and immunoglobulin treatments are still debating for their effectiveness of significant improvement in the survival of patients with severe COVID-19. The unconstrained host inflammatory response is the main driver of the pathology of severe COVID-19. For COVID-19 in the acute setting, 6 mg daily of dexamethasone (equivalent to 40 mg of prednisone) for 10 days reduced mortality from 25·7% to 22·9%, The results were more striking in patients requiring oxygen or invasive ventilation.406 However, chronic glucocorticoids increased the odds of hospitalization for COVID-19 in patients with rheumatic disease.407 Systemic glucocorticoids increased the odds of COVID-19 related death in patients with inflammatory bowel disease.408 It is proposed that dexmedetomidine should be considered in COVID-19 patients admitted to ICU when sedation is required, during the early disease course to help prevent the onset or progression of multiorgan dysfunction.409 Further clinical studies are warranted to optimize the individual strategies with these medications.
Alternatively, targeting the key mechanisms responsible for the pathogenesis of COVID-19, including viral entry and replication, cytokine storm, lymphopenia and endothelial damage and thromboinflammation, may be promising treatment strategies for severe COVID-19 (Fig. 4 and Table 1). Potential anti- SARS-CoV-2 treatments can be divided into two categories depending on the target, one is acting on the host cells or immune system, and the other is on SARS-CoV-2 itself.
Fig. 4.
Potential therapeutic targets against COVID-19 which may be involved in virus replication, immune response, vascular endothelial coagulation system and important organs related complications. a SARS-CoV-2 virus invades host cells. Viral replication involves multiple steps: attachment, penetration, uncoating, replication, assembly, and release. b Viral infection induces an antiviral response, recruiting innate and adaptive immune cells such as macrophages, neutrophil, dendritic cells, T cells, B cells, and NK cells, and leads to cytokine storm. c SARS-CoV-2 invades endothelial cells and affects the coagulation system, increasing the risk of embolism and bleeding. d These host–virus interaction may affect multiple important organs and cause severe complications. The therapeutic targets of these steps are shown in this figure
Table 1.
Clinical studies of potential therapeutic options for COVID-19
| Target: organs or systems | Pathological phenomenon | Mechanism of action | Treatment | Clinical trial | Country | Number of patients | Trial phase |
|---|---|---|---|---|---|---|---|
| Virus | Virus entry into the host and binding with the host cell receptor | Blocking receptor-binding domain | Ensovibep | NCT04870164 | United Kingdom | 24 | Phase 1 |
| Virus | Virus entry into the host and binding with the host cell receptor | TMPRSS2 inhibitor | Camostat Mesilate | NCT04470544 | United States | 264 | Phase 2 |
| Virus | Virus entry into the host and binding with the host cell receptor | TMPRSS2 inhibitor | Camostat Mesilate | NCT04583592 | United States | 295 | Phase 2 |
| Virus | Virus entry into the host and binding with the host cell receptor | Block viral entry | RhACE2 APN01 | NCT04335136 | Turkey | 185 | Phase 2 |
| Virus | Viral replication and clearance | Antiviral activity | Niclosamide | NCT04558021 | Turkey | 200 | Phase 3 |
| Virus | Viral replication and clearance | Broad antiviral activity | Peg-IFN Lambda | NCT04534673 | United States | 40 | Phase 2 |
| Virus | Viral replication and clearance | Broad antiviral activity | Remdesivir | NCT04560231 | Pakistan | 30 | Phase 1 |
| Virus | Viral replication and clearance | Broad antiviral activity | Remdesivir | NCT04738045 | Egypt | 90 | Phase 4 |
| Virus | Viral replication and clearance | Broad antiviral activity | Favipiravir | NCT04499677 | United Kingdom | 240 | Phase 2 |
| Virus | Viral replication and clearance | Broad antiviral activity | Lopinavir/Ritonavir | NCT04466241 | Côte D’Ivoire | 294 | Phase 3 |
| Virus | Viral replication and clearance | Inhibit viral replication | Amantadine | NCT04952519 | Poland | 500 | Phase 3 |
| Virus | Viral replication and clearance | Inhibit viral replication | Amantadine hydrochloride | NCT04854759 | Poland | 200 | Phase 3 |
| Virus | Viral replication and clearance | Interference with viral proliferation | leflunomide | NCT04361214 | United States | 20 | Phase 1 |
| Virus | Viral replication and clearance | Antiviral activity | Nafamostat Mesilate | NCT04390594 | Senegal | 186 | Phase 3 |
| Virus | Viral replication and clearance | Antiviral activity | Niclosamide | NCT04753619 | Iraq | 150 | Phase 2 |
| Virus | Viral replication and clearance | Broad antiviral activity | Favipiravir | NCT04425460 | China | 256 | Phase 3 |
| Virus | Viral replication and clearance | Broad antiviral activity | Sofosbuvir | NCT04535869 | Egypt | 50 | Phase 3 |
| Virus | Viral replication and clearance | Broad antiviral activity | Ribavirin | NCT04828564 | Turkey | 100 | Phase 2 |
| Virus | Viral replication and clearance | Inhibit viral replication | Chlorpromazine (CPZ) | NCT04366739 | France | 40 | Phase 3 |
| Virus | Viral replication and clearance | Inhibit viral replication | Chlorpromazine | NCT04354805 | Egypt | 100 | Phase 3 |
| Virus | Viral replication and clearance | Antiviral activity | Nafamostat Mesylate | NCT04418128 | South Korea | 84 | Phase 3 |
| Virus | Viral replication and clearance | Broad antiviral activity | Favipiravir | NCT04400682 | Turkey | 30 | Phase 1 |
| Virus | Viral replication and clearance | Broad antiviral activity | Remdesivir | NCT04280705 | United States | 1062 | Phase 3 |
| Virus | Viral replication and clearance | Broad antiviral activity | Remdesivir | NCT04401579 | United States | 1033 | Phase 3 |
| Virus | Viral replication and clearance | Broad antiviral activity | Remdesivir | NCT04345419 | Egypt | 200 | Phase 2 |
| Virus | Viral replication and clearance | Broad antiviral activity | Favipiravir | NCT04407000 | Turkey | 30 | Phase 1 |
| Virus | Viral replication and clearance | Broad antiviral activity | Lopinavir and ritonavir | NCT04252885 | China | 86 | Phase 4 |
| Virus | Viral replication and clearance | Broad antiviral activity | Lopinavir/ritonavir | NCT04276688 | Hong Kong | 127 | Phase 2 |
| Virus | Viral replication and clearance | Interference with viral proliferation | LAU-7b: fenretinide | NCT04417257 | United States | 240 | Phase 2 |
| Virus | Viral replication and clearance | Broad antiviral activity | Favipiravir | NCT04501783 | Russian Federation | 168 | Phase 3 |
| Virus | Viral replication and clearance | Interference with viral proliferation | Leflunomide | NCT05007678 | United Kingdom | 178 | Phase 3 |
| Virus | Viral replication and clearance | Antiviral activity | Niclosamide | NCT04399356 | United States | 73 | Phase 2 |
| Virus | Viral replication and clearance | Broad antiviral activity | Favipiravir | NCT04359615 | Iran | 40 | Phase 4 |
| Virus | Viral replication and clearance | Broad antiviral activity | Sofosbuvir | NCT04530422 | Egypt | 250 | Phase 3 |
| Immune system | Cytokine storm | IL-6 Antagonist | Siltuximab, tocilizumab | NCT04486521 | Saudi Arabia | 860 | − |
| Immune system | Cytokine storm | IL-6 inhibitor | Clazakizumab | NCT04659772 | USA | 1 | Phase 2 |
| Immune system | Cytokine storm | IL-6 inhibitor | Clazakizumab | NCT04343989 | USA | 180 | Phase 2 |
| Immune system | Cytokine storm | Anti-IL-6 immunoglobulin G1 kappa (IgG1k) monoclonal antibody (mAb) | Sirukumab | NCT04380961 | USA | 212 | Phase 2 |
| Immune system | Cytokine storm | Anti-IL-6 receptor antibody | Tocilizumab | NCT04730323 | Pakistan | 93 | Phase 4 |
| Immune system | Cytokine storm | Anti-IL-6 receptor antibody | Sarilumab | NCT04661527 | Spain | 60 | Phase 2 |
| Immune system | Cytokine storm | Interferon gamma blocking antibody | Emapalumab | NCT04324021 | USA | 16 | Phase 2 Phase 3 |
| Immune system | Cytokine storm | Interleukin-IL-17A Antagonist | Secukinumab | NCT04403243 | Russia | 70 | Phase 2 |
| Immune system | Cytokine storm | IL-17 inhibitor | ixekizumab | NCT04724629 | Brazil | 60 | Phase 3 |
| Immune system | Cytokine storm | Tumor necrosis factor inhibitors | Infliximab | NCT04734678 | Egypt | 84 | − |
| Immune system | Cytokine storm | IL-1β inhibitor | Canakinumab | NCT04362813 | USA | 454 | Phase 3 |
| Immune system | Cytokine storm | GM-CSF inhibitor | Lenzilumab | NCT04351152 | USA | 520 | Phase 3 |
| Immune system | Cytokine storm | Monoclonal antibody against GM-CSF | Gimsilumab | NCT04351243 | USA | 227 | Phase 2 |
| Immune system | Cytokine storm | IL-23 inhibitor | Risankizumab | NCT04583956 | USA | 1 | Phase 2 |
| Immune system | Immunomodulatory | Immune support | Biological: HB-adMSCs | NCT04348435 | USA | 55 | Phase 2 |
| Immune system | Immunomodulatory | Specific cytotoxic T lymphocytes | SARS-CoV-2 antigen-specific cytotoxic T lymphocyte | NCT04742595 | USA | 16 | Phase 1 |
| Immune system | Immunomodulatory | Immunomodulatory | RAPA-501-Allo off-the-shelf therapy of COVID-19 | NCT04482699 | USA | 88 | Phase 1 Phase 2 |
| Immune system | Immunomodulatory | Immunomodulatory | NKG2D-ACE2 CAR-NK cells | NCT04324996 | China | 90 | Phase 1 Phase 2 |
| Immune system | Immunomodulatory | Reduce the proinflammatory state and promoting the regeneration of damaged tissues | MSC | NCT04611256 | Mexico | 20 | Phase 1 |
| Immune system | Immunomodulatory | Immunomodulatory | T memory cells and NK cells | NCT04578210 | Spain | 58 | Phase 1 Phase 2 |
| Immune system | Immunomodulatory | Regulates inflammation and immunity | Infusion IV of Mesenchymal Stem cells | NCT04416139 | Mexico | 10 | Phase 2 |
| Immune system | Anti-inflammatory effects | Anti-inflammatory effects | Autologous activated platelet-rich plasma | NCT04715360 | Indonesia | 30 | Phase 1 Phase 2 |
| Immune system | Anti-inflammatory effects | Inhibit the inflammatory response | UC-MSCs | NCT04339660 | China | 30 | Phase 1 Phase 2 |
| Immune system | Anti-inflammatory effects | Reduce lung inflammation and pathological impairment | MSC exosome inhalation | NCT04491240 | Russia | 30 | Phase 1 Phase 2 |
| Immune system | Immunomodulatory | Immune-mediated inflammatory | Mesenchymal stromal cells | NCT04361942 | Spain | 24 | Phase 2 |
| Immune system | Immunomodulatory | Virus neutralization. Other possible mechanisms include antibody-dependent cytotoxicity and phagocytosis | Convalescent plasma | NCT04476888 | Pakistan | 110 | − |
| Immune system | Immunomodulatory | Prevent or shut down the continuous inflammatory response caused by the virus | COVID-19 convalescent plasma | NCT04374526 | Italy | 29 | Phase 2 Phase 3 |
| Immune system | Immunomodulatory | Improve high inflammation state and respiratory function | Therapeutic plasma exchange | NCT04751643 | France | 132 | − |
| Immune system | Immunomodulatory | Immunomodulatory | Intravenous immunoglobulin (IVIG) | NCT04500067 | Ukraine | 76 | Phase 3 |
| Immune system | Immune reconstitution | Immune reconstitution | Recombinant interleukin-7 (CYT107) | NCT04442178 | USA | 48 | Phase 2 |
| Immune system | Immunomodulatory | Prevent or shut down the continuous inflammatory response caused by the virus | COVID-19 convalescent plasma (CCP) | NCT04421404 | USA | 42 | Phase 2 |
| Immune system | Immunomodulatory | Immunomodulatory | Monoclonal antibody to S protein of SARS-CoV-2 | NCT04840459 | USA | 1000 | Phase 2 |
| Immune system | Immunomodulatory | Immunomodulatory | SARS-CoV-2 antibody-based IVIG therapy | NCT04521309 | Pakistan | 50 | Phase 1 Phase 2 |
| Immune system | Immunomodulatory | Immunomodulatory | JS016 (anti-SARS-CoV-2 monoclonal antibody) | NCT04931238 | China | 200 | Phase 1 |
| Immune system | Immunomodulatory | Immunomodulatory | plasma therapy using convalescent plasma with antibody against SARS-CoV-2 | NCT04356534 | Ireland | 40 | − |
| immune system | Cytokine storm | Regulation of the inflammatory cytokine response | Vitamin D, Omega DHA/EPA, vitamin C, vitamin B complex, and zinc acetate | NCT04828538 | Mexico | 3600 | − |
| Immune system | Immune activation | Suppressor of cytokine activation | Zofin: derived from human amniotic fluid | NCT04384445 | USA | 20 | Phase 1、Phase 2 |
| Immune system | Intense inflammatory cascade | Adjunct immune modulation therapies | Vitamin C | NCT04401150 | Canada | 800 | Phase 3 |
| Immune system | Cytokine storm | Human normal immunoglobulin | IVIG | NCT04500067 | Ukraine | 76 | Phase 3 |
| Immune system | Cytokine storm | Human normal immunoglobulin | Human immunoglobulin | NCT04350580 | France | 146 | Phase 3 |
| Immune system | Cytokine storm | Immunosuppressant | Ciclesonide | NCT04377711 | USA | 400 | Phase 3 |
| Immune system | Cytokine storm | Vitamin | Cholecalciferol | NCT04552951 | Spain | 80 | Phase 4 |
| Immune system | Cytokine storm | Vitamin | Vitamin D3, vitamin C/Zinc, vitamin K2/D | NCT04780061 | Canada | 200 | Phase 3 |
| Immune system | Cytokine storm | Vitamin | Oral 25-hydroxyvitamin D3 | NCT04386850 | Islamic Republic | 1500 | Phase 2,3 |
| Immune system | Cytokine storm | Mesenchymal stem cells | HB-adMSCs | NCT04348435 | USA | 55 | Phase 2 |
| Immune system | Cytokine storm | Bone marrow-derived extracellular vesicles | DB-001 | NCT04493242 | USA | 120 | Phase 2 |
| immune system | Elevated numbers of neutrophils | NETs degradation | rhDNase I | NCT04409925 | Canada | 25 | Phase 1 |
| Endothelial | Pulmonary edema | Abl2/Arg inhibitors | Imatinib | NCT04794088 | Netherlands | 90 | Phase 2 |
| Endothelial | Acute respiratory distress syndrome | DNase inhibitors | Dornase alfa | NCT04355364 | France | 100 | Phase 3 |
| Endothelial | Excessive blood clotting | Vasodilator and inhibitor of platelet aggregation | Dipyridamole | NCT04391179 | United States | 100 | Phase 2 |
| Endothelial | Endothelial dysfunction | Endothelial cell modifying | Defibrotide | NCT04652115 | United States | 42 | Phase 2 |
| Endothelial | Endothelial dysfunction | Endothelial cell modifying | Defibrotide | NCT04348383 | Spain | 150 | Phase 2 |
| Endothelial | Complement-mediated diseases | Terminal complement inhibitor | Eculizumab | NCT04346797 | France | 120 | Phase 2 |
| Endothelial | Endothelial dysfunction | Increase NO production and release | Atorvastatin + l-arginine + folic acid + nicorandil + nebivolol | NCT04631536 | Lebanon | 80 | Phase 3 |
| Endothelial | Endothelial injury | PAI-1 inhibitor | TM5614 | NCT04634799 | United States | 80 | Phase 2 |
| Endothelial | Microvascular endothelial dysfunction | Platelet aggregation inhibitors | Iloprost | NCT04420741 | Denmark | 80 | Phase 2 |
| Endothelial | Vascular endothelial dysfunction | Restore endothelial glycocalyx and Inhibit thrombosis | Suloexide | NCT04483830 | Mexico | 243 | Phase 2 Phase 3 |
| Endothelial | Endothelial injury | C5a inhibitor | Ravulizumab | NCT04570397 | United States | 32 | Phase 3 |
| Endothelial | Vascular dilation | Angiogenesis inhibitors | BEVACIZUMAB | NCT04822818 | France | 174 | Phase 3 |
| Endothelial | Vascular leakage | decrease vascular hyperpermeability | FX06 | NCT04618042 | France | 50 | Phase 2 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04360824 | USA | 170 | Phase 4 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin, unfractionated heparin, atorvastatin, matched placebo | NCT04486508 | Iran | 600 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04354155 | USA | 40 | Phase 2 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Low-molecular-weight heparin, fondaparinux | NCT04359212 | Italy | 90 | – |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04408235 | Italy | 300 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Tinzaparin, unfractionated heparin | NCT04344756 | France | 808 | Phase 2 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04345848 | Switzerland | 200 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin, heparin | NCT04359277 | USA | 77 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Low-molecular-weight heparin (LMWH), unfractionated heparin (UFH) | NCT04362085 | Canada | 465 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04366960 | Italy | 189 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin, heparin, lovenox | NCT04367831 | USA | 100 | Phase 4 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Heparin | NCT04372589 | USA | 1200 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04373707 | France | 602 | Phase 4 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Low-molecular-weight heparin | NCT04393805 | Italy | 744 | – |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Rivaroxaban, enoxaparin | NCT04394377 | Brazil | 615 | Phase 4 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Enoxaparin | NCT04401293 | USA | 257 | Phase 3 |
| Coagulation system | Higher hypercoagulability | Anticoagulation | Rivaroxaban | NCT04416048 | Germany | 400 | Phase 2 |
| Coagulation system | Higher hypercoagulability | Platelet inhibition | Tirofiban, clopidogrel, acetylsalicylic acid, fondaparinux | NCT04368377 | Italy | 5 | Phase 2 |
| Coagulation system | Reduced vitamin K status | Vitamin K supplementation | Vitamin K2 in the form of menaquinone-7 (MK-7), placebo | NCT04770740 | Netherlands | 40 | Phase 2 |
| Cardiovascular | Dysfunction of RAAS | Recover the function of ACE2-RAAS | Recombinant bacterial ACE2 receptors-like enzyme of B38-CAP (rbACE2) | NCT04375046 | China | 24 | Phase 1 |
| Cardiovascular | Dysfunction of RAAS | RAAS inhibition | RAAS inhibitor | NCT04508985 | Canada | 40 | / |
| Cardiovascular | Cardiovascular disease or risk factors | Anti-inflammatory | Cannabidiol | NCT04615949 | Arizona, USA | 422 | Phase 2、Phase 3 |
| Vascular endothelial system | Coagulation disorders | Anticoagulant | Enoxaparin Atorvastatin | NCT04486508 | Islamic Republic | 600 | Phase 3 |
| Circulatory system | Vascular endothelial injury, cytokine storm | FXa inhibitor, HMG-CoA inhibitor | Apixaban, Atorvastatin | NCT04801940 | UK | 2631 | Phase 3 |
| Vascular endothelial system | Cytokine storm, vascular endothelial injury | Vitamin C | Vitamin C | NCT04401150 | Canada | 800 | Phase 3 |
| Vascular endothelial system | Vascular endothelial injury | Phyto preparation | Hesperidin | NCT04715932 | Canada | 216 | Phase 2 |
| Cardiac, kidney | multiorgan failure | Sodium–glucose cotransporter-2 (SGLT-2) inhibitor | Dapagliflozin | NCT04350593 | USA、Argentina、Brazil、Canada、India、Mexico、UK | 1250 | Phase 3 |
| Cardiovascular | Acute cardiac injury | Cardioprotective medicines | Aspirin, clopidogrel, rivaroxaban, atorvastatin, omeprazole | NCT04333407 | UK | 3170 | − |
| Cardiovascular | Thrombotic events | Anticoagulation or anti-platelet agents | Apixaban, aspirin | NCT04498273 | USA | 7000 | Phase 3 |
| Cardiovascular | Thrombotic events | Anti-inflammatory and antithrombotic function | Enoxaparin, unfractionated heparin, atorvastatin | NCT04486508 | Iran | 600 | Phase 3 |
| Cardiovascular | Dysregulated immune response | Immunomodulatory and cardiovascular drugs | EDP1815, dapagliflozin and Ambrisentan | NCT04393246 | UK | 1407 | Phase 2、Phase 3 |
| Cardiovascular | Cardiac injury | Reduce cardiac injury | Colchicine tablets | NCT04355143 | USA | 150 | Phase 2 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Rivaroxaban | NCT04757857 | Brazil | 1000 | Phase 4 |
| Cardiovascular | Thrombotic events | Antagonize plasminogen activator inhibitor | TM5614 | NCT04634799 | USA | 80 | Phase 1、Phase 2 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | NCT04492254 | Australia | 1370 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Apixaban | NCT04746339 | Brazil | 1000 | Phase 4 |
| Cardiovascular | Longer-term complications occurring in the convalescent phase | Improve the quality of life | Apixaban, atorvastatin | NCT04801940 | UK | 2631 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Rivaroxaban | NCT04416048 | Germany | 400 | Phase 2 |
| Cardiovascular | Endothelial dysfunction | Improve endothelial function | Atorvastatin + l-arginine + folic acid + nicorandil + nebivolol | NCT04631536 | Lebanon | 80 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin, apixaban | NCT04512079 | USA、Brazil、Colombia、India、Mexico | 3600 | Phase 4 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | NCT04400799 | Germany、Switzerland | 1000 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | NCT04646655 | Italy | 300 | Phase 3 |
| Cardiovascular | Viral injury of the vascular endothelium | Monoclonal antibody that targets P-selectin | Crizanlizumab | NCT04435184 | USA | 50 | Phase 2 |
| Cardiovascular | Myocardial infarction in combination with COVID-19 | Antiarrhythmic effect | Atorvastatin, atorvastatin-ezetimibe | NCT04900155 | Russian Federation | 200 | − |
| Cardiovascular | Thrombotic events | Antithrombotic therapy | Apixaban | NCT04650087 | USA | 5320 | Phase 3 |
| Cardiovascular | Thrombotic events | Thromboprophylaxis | Rivaroxaban | NCT04662684 | Brazil | 320 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | NCT04345848 | Switzerland | 200 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin, heparin | NCT04367831 | USA | 100 | Phase 4 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | NCT04354155 | USA | 40 | Phase 2 |
| Cardiovascular | Thrombotic events | Anticoagulation therapy | Therapeutic anticoagulation | NCT04362085 | Canada | 465 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Thromboprophylaxis | NCT04360824 | USA | 170 | Phase 4 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | NCT04373707 | France | 602 | Phase 4 |
| Cardiovascular | Acute pulmonary hypertension (aPH) and/or acute Cor pulmonale (ACP) | Decrease pulmonary arterial pressure | PDNO | NCT04885491/2020-002982-33 | Sweden | 16 | Phase 1、Phase 2 |
| Cardiovascular | Hyperviscosity | Plasma exchange | Therapeutic plasma exchange | NCT04441996 | USA | 20 | Phase 4 |
| Cardiovascular | Thrombotic events | Anticoagulation therapy | Edoxaban, colchicine | NCT04516941 | Belgium、Italy、Spain、Switzerland | 420 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation therapy | Tinzaparin | NCT04730856 | Spain | 600 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation therapy | Enoxaparin | NCT04508439 | Mexico | 130 | − |
| Cardiovascular | Coagulopathy | Anticoagulation therapy | Therapeutic anticoagulation | NCT04444700 | Brazil | 465 | Phase 3 |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | 2020-003125-39 | Germany | 1370 | − |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Low-molecular-weight heparin | 2020-001709-21 | France | 550 | − |
| Cardiovascular | Thrombotic events | Anticoagulation agent | Enoxaparin | 2020-005624-10 | Germany | 1000 | − |
| Cardiovascular | Downregulation of ACE2 | Anti-inflammatory and antithrombotic function-RAAS | Omega3-FA | NCT04658433 | Jordan | 100 | − |
| Cardiovascular | Cardiovascular disease or risk factors | Renin–angiotensin system inhibitors-RAAS | ACEi、ARB | NCT04591210 | Canada, Brazil, Mexico | 1155 | Phase 3 |
| Cardiovascular | Viral cell invasion | Increase ACE2 expression and improve mechanisms of host defense or hyperinflammation-RAAS | Discontinuation/continuation of ACEi、ARB | NCT04338009 | USA | 152 | − |
| Cardiovascular | ARDS | RAAS regulator | Telmisartan | NCT04355936 | Argentina | 400 | Phase 4 |
| Cardiovascular | Overaction of RAS | Similar peptide to Ang(1–7)-RAAS | TRV027 | NCT04419610 | UK | 30 | Phase 1 |
| Cardiovascular | Viral entry and viral replication | Recombinant human angiotensin-converting enzyme 2 -RAAS | RhACE2 APN01 | NCT04335136 | Austria、Denmark、Germany、Russian Federation、UK | 185 | Phase 2 |
| Respiratory system | Host viral entry | TMPRSS2 inhibitors | Nafamostat Mesilate | NCT04352400 | Italy | 256 | Phase 2、Phase 3 |
| Immune and respiratory system | Cytokine storm | Prophylactic corticosteroid | Methylprednisolone | NCT04355247 | Puerto Rico | 20 | Phase 2 |
| Respiratory system | Cytokine storm | Mesenchymal stem cells | Umbilical cord-derived mesenchymal stromal cells | NCT04333368 | France | 40 | Phase 1 |
| Respiratory system | Cytokine storm | Biomarker-tailored steroid | Methylprednisolone | NCT03852537 | USA | 44 | Phase 2 |
| Respiratory system | Viral growth | Broad-spectrum antiparasitic | Ivermectin | NCT04739410 | Pakistan | 50 | Phase 4 |
| Respiratory system | Cytokine storm | Antioxidant | Sodium pyruvate | NCT04871815 | USA | 50 | Phase 2,3 |
| Respiratory system | Cytokine storm | Antihistamines | Cetirizine and famotidine | NCT04836806 | USA | 160 | Phase 4 |
| Respiratory system | Viral growth | Broad-spectrum antiviral | Remdesivir | NCT04978259 | Finland | 202 | Phase 4 |
| Respiratory system | Viral growth | Broad-spectrum antiviral | Favipiravir | NCT04694612 | Nepal | 676 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiviral | Triazavirin | NCT04973462 | Egypt | 80 | Phase 4 |
| Respiratory system | Viral growth | Broad-spectrum antiviral | Ivermectin | NCT04673214 | Mexico | 114 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiviral | Lopinavir/ritonavir | NCT04466241 | Cote d’Ivoire | 294 | Phase 2,3 |
| Respiratory system | Host viral entry | Vaccine based on peptide antigens | EpiVacCorona | NCT04780035 | Russian Federation | 3000 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiparasitic | Nitazoxanide 500 mg oral tablet | NCT04406246 | Mexico | 150 | Phase 4 |
| Respiratory system | Viral growth, cytokine storm | Broad-spectrum antiviral | Ivermectin and doxycycline | NCT04523831 | Bangladesh | 400 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiviral | Ivermectin tablets, doxycycline tablets | NCT04729140 | USA | 150 | Phase 4 |
| Respiratory system | Cytokine storm | Antioxidant | Sodium pyruvate | NCT04824365 | USA | 60 | Phase 2,3 |
| Respiratory system | Viral growth | RNA polymerase inhibitor | Favipiravir | NCT04600999 | Hungary | 150 | Phase 3 |
| Respiratory system | Viral growth, Cytokine storm | ACE2 inhibitor | Hydroxychloroquine | NCT04354428 | USA | 300 | Phase 2,3 |
| Respiratory system | Host viral entry | Acetylcholine agonists | Nicotine patch | NCT04583410 | France | 1633 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiparasitic | AVIGAN | NCT04529499 | Kuwait | 780 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiparasitic | Ivermectin | NCT04646109 | Turkey | 66 | Phase 3 |
| Respiratory system | Viral growth | Broad-spectrum antiparasitic | Favipiravir | NCT04600895 | USA | 1150 | Phase 3 |
| Respiratory system | Cytokine storm | Cytokine inhibitor | Pirfenidone | NCT04856111 | India | 48 | Phase 4 |
| Respiratory system | Cytokine storm | M2 protein inhibitor | Amantadine hydrochloride | NCT04854759 | Poland | 200 | Phase 3 |
| Respiratory system | Cytokine storm | Convalescent plasma | Convalescent plasma | NCT04558476 | Belgium | 500 | Phase 2 |
| Respiratory system | Cytokine storm, vascular endothelial injury | VEGF inhibitor | Nintedanib 150 MG [Ofev] | NCT04541680 | France | 250 | Phase 3 |
| Respiratory system | Host viral entry | Acetylcholine agonists | Nicotine | NCT04608201 | France | 220 | Phase 3 |
| Respiratory system | Cytokine storm | Interferon beta-1a | SNG001 | NCT04732949 | USA | 610 | Phase 3 |
| Respiratory system | Cytokine storm | SSRI | Fluvoxamine | NCT04668950 | USA | 1100 | Phase 3 |
| Lung and coagulation system | Host viral entry and higher hypercoagulability | Protease TMPRSS2 inhibition | Nafamostat mesilate, placebo | NCT04352400 | Italy | 256 | Phase 3 |
| Respiratory system | Cytokine storm | IL-6-blocking antibodies | Clazakizumab, placebo | NCT04343989 | USA | 180 | Phase 2 |
| Nervous system | Cytokine storm, neuroinflammation | Endogenous molecule | mPEA and umPEA | NCT04568876 | Italy | 40 | Phase 4 |
| Central nervous system | Cytokine storm, sedatives needed | Sedation drugs | Isoflurane inhalant product, sevoflurane inhalant product | NCT04415060 | Canada | 752 | Phase 3 |
| Central Nervous System | Cytokine storm, sedatives needed | Anti-adrenergic medications | Propranolol hydrochloride | NCT04467086 | Canada | 108 | Phase 3 |
| Neuropsychological system | Cytokine storm, post-viral fatigue syndrome | C1 inhibitor | Ruconest | NCT04705831 | USA | 40 | Phase 4 |
| Peripheral nervous system | Cytokine storm, Nasopharyngitis | Phyto preparation | BNO 1030 | NCT04797936 | Ukraine | 133 | Phase 4 |
| Central nervous system | Cytokine storm | Analgesics | Cannabis, medical | NCT03944447 | USA | 200000 | Phase 2 |
| Central nervous system | Cytokine storm, acute brain damage | Surgery | Sphenopalatine ganglion block with local anesthetic | NCT04636034 | Denmark | 60 | Phase 3 |
| Neuropsychiatric system | Viral growth, Cytokine storm | ACE2 inhibitor | Hydroxychloroquine, apixaban | NCT04788355 | Brazil | 176 | Phase 3 |
| Neuropsychiatric system | Cytokine storm, brain damage | Nicotinamide riboside | Niagen | NCT04809974 | USA | 100 | Phase 4 |
| Respiratory system, Neuropsychiatric system | Cytokine storm | IL-6 blocker | Fluoxetine | NCT04377308 | USA | 2000 | Phase 4 |
| Central Nervous System | Cytokine storm | CB1 and CB2 agonists | Cannabidiol | NCT04467918 | Brazil | 100 | Phase 2,3 |
| Neuropsychiatric system | Cytokine storm, brain damage | NMDA inhibitor | Ketamine | NCT04769297 | USA | 30 | Phase 4 |
| Kidney | Cytokine storm | Hormone replacement therapy | Extracorporeal mesenchymal stromal cell therapy (SBI-101 Therapy) | NCT04445220 | United States | 22 | Phase 1, Phase 2 |
| Kidney | Cytokine storm | Hormone replacement therapy | AN-69 Oxiris membrane or the standard AN-69 membrane | NCT04597034 | Mexico | 35 | − |
| Kidney | AKI,ARDS and COVID-19 | Cytopheretic device | Device: SCD | NCT04395911 | United States | 22 | − |
| Kidney | Thrombotic microangiopathy | C5a inhibitor | Ravulizumab | NCT04570397 | United States | 32 | Phase 3 |
| Kidney | Host viral entry | Urine alkalinisation to prevent binding of SARS-COV-2 to renal tubular epithelial cells | Sodium Bicarbonate 150Meq/L/D5W Inj | NCT04655716 | United Kingdom | 80 | Phase 3 |
| Kidney | Acute kidney injury | Renal protection | Nicotinamide riboside | NCT04818216 | United States | 100 | Phase 2 |
| Kidney | Acute kidney injury | extracorporeal CO2 removal | Device: extracorporeal CO2 removal (ECCO2R) therapy | NCT04351906 | Germany | 20 | − |
| Kidney | Sepsis, severe acute kidney injury, COVID-19 | Plasma expansion with Ringer’s Acetate | 7,5 ml/kg mL Ringer’s acetate | NCT02765191 | Sweden | 20 | − |
| Gastrointestinal | Minimize/avoid any immune response | Immune response | inhalable hydroxychloroquine (HCQ) supportive and symptomatic treatment | NCT04477083 | Egypt | 40 | − |
| Gastrointestinal | / | / | Hydroxychloroquine | NCT04351620 | United States | 20 | Phase 1 |
| Gastrointestinal | / | / | No intervention | NCT04401124 | China | 500 | − |
| Gastrointestinal | Gut microbes | Gut microbes | Omni-Biotic Pro Vi 5 | NCT04813718 | Austria | 20 | − |
| Gastrointestinal | / | / | Swallowing evaluation with the EAT-10 and the volume-viscosity swallowing test (V-VST) | NCT04346212 | Spain | 300 | − |
| Gastrointestinal | / | / | / | NCT04838834 | United States | 472 | − |
| Gastrointestinal | / | / | Laparoscopic appendectomy | NCT04786041 | Israel | 200 | − |
| Endocrine system | Uncontrolled blood glucose | Antiviral drug combined with an anti-inflammatory |
Drug: Baricitinib Drug: Dexamethasone Drug: Remdesivir |
NCT04970719 | Bengal | 382 | Phase 3 |
| Endocrine system | β-cell function | Insulinotropic amino acids | Stimulation test with arginine infusion in order to verify the possible existence of damage to the beta cell function induced by COVID-19 infection | NCT04463849 | Italy | 90 | − |
| Endocrine system | Cytokine storm | Decrease blood sugar; increase ACE2 expression | Drug: Pioglitazone 30 mg | NCT04535700 | Spain | 76 | Phase 4 |
| Endocrine system | Interleukin-1 (IL-1) beta system | blocking IL-1beta activity | Drug: Canakinumab | NCT04510493 | Switzerland | 116 | Phase 3 |
| Endocrine system | Decrease in TNF-alpha, interleukin, hs CRP, leptin and other inflammatory markers | Anti-inflammatory and inflammation-resolving | Drug: Pioglitazone 45 mg | NCT04604223 | Kuwait | 1506 | Phase 4 |
| Endocrine system | Decrease blood sugar | Glucokinase (GK; hexokinase 4) activator | Drug: AZD1656 | NCT04516759 | Czech Republic | 156 | Phase 2 |
| Endocrine system | Decrease blood sugar | Dipeptidyl Peptidase-4 Inhibitor (DPP4i) | Drug: Linagliptin tablet | NCT04542213 | Mexico | 70 | Phase 3 |
| Endocrine system | Cytokine storm | Regulate immune function | Drug: cholecalciferol | NCT04733625 | Egypt | 56 | − |
| ENT | Cytokine storm | Nasal steroid | Ophtamesone | NCT04569825 | Iraq | 250 | Phase 1 |
| Pre-exposure phrophylaxis | Host viral entry | Pre-exposure phrophylaxis | Truvada | NCT04334928 | Spain | 1002 | Phase 3 |
ACE2 and TMPRSS2 have been characterized as possible host targets to block SARS-CoV-2 from entering host cells. It is reported that a designed peptide inhibiting SARS-CoV-2 binding to ACE2 and may theoretically block SARS-CoV-2 infection.410 Recombinant human ACE2 protein and anti-spike monoclonal antibody could inhibit SARS-CoV-2 S protein-induced platelet activation. MicroRNA molecules targeting ACE2 may be exploited to regulate the SARS-CoV-2 receptor. Administration of microRNA 200c inhibits both ACE2 mRNA and ACE2 protein levels in human iPSC-derived cardiomyocytes and primary cardiomyocytes of COVID-19 rat model, which is a potential regimen for cardiovascular complications of COVID-19.411 Besides, excessive ACE2 may competitively bind with SARS-CoV-2, thereby neutralizing the virus and rescuing cellular ACE2 activity which negatively regulates the RAS to protect the lung.410,412,413 Therefore, treatment with a soluble form of ACE2 may be effective against SARS-CoV-2 infection. Treatment with anti-androgenic drugs reduced ACE2 expression and protected hESC-derived lung organoids against SARS-CoV-2 infection. Umifenovir, trade name Arbidol has been used to treat COVID-19 in China. The primary mode of action of umifenovir is to inhibit viral attachment by binding to envelope protein.414 Camostat mesylate, an orally available serine protease inhibitor, is a potent inhibitor of TMPRSS2 and has been hypothesized as a potential antiviral drug against COVID-19, by inhibiting virus-cell membrane fusion and hence SARS-CoV-2 replication.259,415,416 Nafamostat mesylate, which is FDA-approved for indications unrelated to coronavirus infection, inhibits viral entry with roughly 15-fold higher efficiency than camostat mesylate, but requires intravenous dosing.417
Chloroquine and hydroxychloroquine may elevate endosomal pH and hinder viral entry and RNA release process.418 However, two randomized controlled trials, RECOVERY419 and WHO SOLIDARITY trials,420 confirmed that these regimens failed to provide any clinical benefit for COVID-19 patients.
Nsps participate in various steps of virus life cycle, including RNA transcription and translation, protein synthesis, processing and modification, virus replication and infection. Among these, nsp5 3CLpro, nsp3 PLpro, nsp12 RdRp and helicase are the most important targets for the development of small-molecule inhibitors because of their biological functions and vital enzyme active site.421 The protein sequence similarity between SARS-CoV-2 and SARS-CoV RdRp is up to 96%.422 Thus, broad-spectrum antiviral drugs acting on RdRp including nucleoside analogs, e.g., remdesivir, favipiravir, and molnupiravir, may potentially block SARS-CoV-2 replication.423,424 ACTT-1 study of intravenous remdesivir in adults who were hospitalized with COVID-19 showed that remdesivir was superior to placebo in shortening recovery time.425 However, DisCoVeRy study demonstrated no clinical benefit of remdesivir use in patients hospitalized for COVID-19 who were symptomatic for more than 7 days, and required oxygen support.426 Remdesivir undergoes intracellular activation to form an analog of adenosine triphosphate GS-443902 that selectively inhibits viral RNA polymerases and has broad-spectrum activity against coronavirus.427 In an animal model molnupiravir is orally active against SARS-CoV-2, and preliminary data of phase 2a trial showed that molnupiravir is highly effective at reducing SARS-CoV-2 RNA and has a favorable safety and tolerability profile.428 Protease inhibitors targeting viral 3CLpro are attractive therapeutic options for COVID-19.429 Protease inhibitor lopinavir–ritonavir showed significant inhibitory effects on SARS-CoV-2 in vitro.430 However, the LOTUS294 and RECOVERY431 clinical trials independently showed no benefit of using lopinavir–ritonavir in reducing mortality rate, hospital time nor progression to mechanical ventilator intervention. There are three SARS-CoV-2 virulence factors nsp1, nsp3c, and ORF7a related to interfering host’s innate immunity and assisting immune escape, suggesting that nsp1, nsp3c, and ORF7a may be potential targets for antiviral drug development.421,432 The efficacy of existing antiviral ribonucleoside and ribonucleotide analogs, such as remdesivir, can be decreased by the viral proofreading exonuclease nsp14-nsp10 complex. Nsp14-nsp10 inhibitors were identified that increase antiviral potency of remdesivir. A model compound, sofalcone, inhibits the exonuclease activity of SARS-CoV-2 in vitro, and synergistically enhances the antiviral effect of remdesivir.433 Nsp3 in SARS-CoV-2 serves to counteract the antiviral function of host Poly ADP-ribose polymerase (PARP) which is NAD+-consuming enzymes. Therefore, NAD+ and NAD+-consuming enzymes play crucial roles in immune responses against viral infection. Thorough mechanistic understandings of SARS-CoV-2 replication will likely facilitate the development of general antiviral strategies.434
A minimally pathogenic human betacoronavirus (OC43) was used to infect physiologically-relevant human pulmonary fibroblasts MRC5 to facilitate rapid antiviral discovery in a preclinical model. Several FDA-approved agents that can attenuate both OC43 and SARS-CoV-2 viral replication, including lapatinib, doramapimod, and tanespimycin. Importantly, lapatinib inhibited SARS-CoV-2 RNA replication by over 50,000-fold. Further, both lapatinib and doramapimod could be combined with remdesivir to improve antiviral activity in cells. These findings reveal novel therapeutic avenues that could limit SARS-CoV-2 infection.435
The knowledge accumulated to date indicates that COVID-19 severity and the associated mortality rate derive either from a dysregulated immunopathology induced directly by SARS-CoV-2 infection or by the tissue damage caused by the immune response against SARS-CoV-2.15 Therefore, the altered immune response represents the important target for therapeutic interventions aimed at modifying the immunopathogenesis of COVID-19. Targeting the specific COVID-19 immune profiles, such as by inhibiting inflammation or enhancing lymphocytes are promising treatment strategies for severe cases. Targeting cytokine storm and the signaling pathways have been considered as potentially effective strategies to modulate the hyperinflammatory response against SARS-CoV-2 infection.436 Anti-cytokine therapy such as IL-6, TNF-α and IL-1 antagonists have been suggested for the alleviation of hyperinflammation.357 In hospitalized COVID-19 patients with hypoxia and systemic inflammation, IL-6R antagonist tocilizumab improved survival and other clinical outcomes.437,438 However, a randomized trial in patients with severe or critical COVID-19, tocilizumab failed to improve clinical outcomes, and it might increase mortality.439 A randomized, double-blind trial did not show efficacy of another IL-6R antagonist sarilumab in patients admitted to hospital with COVID-19 and receiving supplemental oxygen.440 Anti-IL-6 monoclonal antibodies such as siltuximab and sirukumab are under investigation for COVID-19 patients. Aberrant high GM-CSF levels have been detected in circulating lymphocyte populations, excluding NKs and B cells, from patients with COVID-19 admitted to ICU.78 Therefore, the potential of GM-CSF-blocking antibodies such as lenzilumab (LIVE-AIR study) and gimsilumab to treat COVID-19 is being evaluated by researchers and pharmaceutical companies.441
Other possible strategies under clinical and preclinical investigation for inhibiting macrophage activation include the blockade of certain cytokines, inhibition of C-C chemokine receptor type 5 (CCR5)-mediated migration and CD14 blockade by monoclonal antibodies.441 Strategies such as MSC-based therapy, Treg-based therapy and blood purification may also represent alternative effective approach to alleviating SARS-CoV-2-related immunopathology.15 SARS-CoV-2 has demonstrated to induce apoptosis of circulating lymphocytes by P53 activation.442 T cells from COVID-19 patients expressed higher levels of the exhausted marker PD-1. Increasing PD-1 expression on T cells was observed as disease progressed.97 The efficacy of PD-1 monoclonal antibody, camrelizumab plus thymosin have been evaluated in a clinical trial for COVID-19 treatment.443 Circulating NK cell numbers were found significantly reduced in COVID-19 patients with severe disease,444 and showed increased expression of inhibitory receptor TIM-3.445 Chimeric antigen receptor (CAR) -engineered NK cells are also being tested for treating COVID-19.446
PAI-1 inhibitors significantly enhance the bronchoalveolar fibrinolytic system and relieve symptoms of COVID-19 by increasing fibrinolytic protein levels that effectively remove fibrin.447 There is increasing evidence that complement is involved in SARS-CoV-2 pathology, and that complement inhibitors may reduce the severity of COVID-19 complications and the number of intensive care or deaths, especially with ekuzumab showing preliminary efficacy.448 Defibrotide can counteract endothelial activation and hypercoagulability induced by NETs and histone H4, promote endothelial remodeling and prevent endothelial dysfunction.449 Blocking vascular endothelial growth factor (VEGF) and VEGF receptor -mediated signaling improves oxygen perfusion and anti-inflammatory responses, and reduces clinical symptoms in patients with severe COVID-19. A humanized monoclonal antibody against VEGF, Bevacizumab plus standard care can be very beneficial for patients with severe COVID-19.450 The lung function of COVID-19 patients improved significantly after FX06 administration, which may be attributed to its immunomodulatory properties and its ability to protect the endothelial barrier and reduce vascular hypertonicity.451
Given hypercoagulability was commonly seen in patients with COVID-19, studies suggest that low-molecular weight heparin (LMWH) should be used for early and long-term drug-induced thrombosis prevention.452 Consistently, in a cohort of critically ill COVID-19 patients with a high prevalence of thromboembolic events, enhanced thromboprophylaxis was associated with reduced ICU mortality without an increased hemorrhagic risk.453 However, results from some other multicenter studies did not support routine empirical use of prophylactic anticoagulation in patients with COVID-19.454–456 A retrospective analysis indicated that therapeutic anticoagulation was associated with lower mortality among hospitalized COVID-19 patients compared with prophylactic anticoagulation, although not statistically significant.457 While two other studies showed that therapeutic anticoagulation did not significantly improve the prognosis nor increase the risk of bleeding compared with prophylactic anticoagulation in patients hospitalized with COVID-19 and elevated D-dimer concentration.458,459 A study in France involving 10 patients with ischemic stroke caused by macrovascular embolism showed that early intravenous thrombolysis and mechanical thrombectomy recanalization did not reverse the adverse outcomes of patients.460 These controversial results demonstrate the complexity of coagulation in COVID-19 patients.
To date, the research on the mechanism of COVID-19 related coagulation disorders has proposed a series of molecules and pathways that may be used as clinical intervention targets. First, disorders in the coagulation system include colocalization of coagulation factor XII and NETs,153 increased biological function of CD142 which exposed onto surface of cell-released extracellular vesicles,461,462 overactivation of the complement component anaphylatoxin-NET axis,462 overactivation of platelet via binding to S protein by ACE2.145 Studies shows that by targeting these molecules will improve the coagulation state in vitro. Second, a reduction in fibrinolysis also plays an important role in COVID-19-associated coagulopathy, and promoting fibrinolytic activity is a possible way to change the coagulation disorder in patients.463–465 Third, studies have found that vascular endothelial cells activation and dysfunction mediate inflammation and abnormal coagulation in COVID-19 patients.106,107 In addition, some other factors can also play a role by influencing the above three systems, such as RAS,466 complement and coagulation cascade signaling,125,467,468 mineralocorticoid receptor (MR) and its downstream target galectin-3 (Gal-3),469 IL-6,124 extrahepatic vitamin K insufficiency,470 etc. These molecules and pathways form a complex network leading to the complexity of the disease and the difficulty of the treatment. Some drugs targeting the above molecules and pathways have entered clinical trials, such as inhaled rhDNase1 (targeting the NETs), recombinant bacterial ACE2 receptors-like enzyme of B38-CAP, RAS inhibitor, mineralocorticoid receptor antagonist (MRA) canrenoate potassium, the IL-6 inhibitor clazakizumab, vitamin K2, etc.
Accumulating literature has demonstrated the beneficial effects of n-3 polyunsaturated fatty acids (n-3 PUFA) toward the cardiovascular system, which include ameliorating uncontrolled inflammatory reactions, reduced oxidative stress and mitigating coagulopathy.471 Due to the favorable safety profile of n-3 PUFAs and their metabolites, it is reasonable to consider n-3 PUFAs as potential adjuvant therapies for the clinical management of COVID-19 patients. Targeting RAGE to prevent SARS-CoV-2-mediated multiple organ failure is also a promising therapy.472 Pharmacological agents frequently used in atherosclerotic conditions, such as statins and aspirin, appear to lower the incidence of serious COVID-19 complications and mortality rates.473 Oxytocin (OXT) can protect the heart and vasculature through suppressing hypertension and brain-heart syndrome, and promoting regeneration of injured cardiomyocytes.474 Exogenous OXT can be used safely without the side-effects seen in remdesivir and corticosteroid.474
A retrospective observational study of COVID-19 patients with type 2 diabetes found that sitagliptin treatment during hospitalization was associated with reduced mortality and improved clinical outcomes.475 Evidence suggests that insulin and dipeptidyl peptidase-4 (DDP4) inhibitors can be used safely in COVID-19 patients with diabetes. Metformin and sodium-glucose cotransporter-2 (SGLT-2) inhibitors might need to be withdrawn in patients at high risk of severe disease.476
SARS-CoV-2 vaccination
The vaccination of SARS-CoV-2 vaccine may become one of the most effective means to terminate COVID-19 epidemic. The current vaccine development mainly uses viral S protein, S protein receptor-binding domain, or S protein subunits as antigens. The technical strategies477 include: viral vaccines (live attenuated vaccines and inactivated vaccines), viral-vectored vaccines (replicating and non-replicating), nucleic acid vaccines (DNA vaccines and mRNA vaccines), protein subunit vaccines (recombinant protein vaccines, protein subunit vaccines and virus-like particle vaccines). As of January 7, 2022, 137 of the 331 vaccine projects announced by the WHO478 have entered the clinical trial stage. At present, several vaccines produced in China, the United States and Europe have been the first to vaccinate people on a large scale. However, the main challenge is the reduction of the protective power of the vaccine due to the mutation of the SARS-CoV-2. Efforts to develop polyvalent vaccines479 against different strains may be a solution, but the mutation of SARS-CoV-2 is rapid which makes the development of vaccine extremely difficult. Another option is to develop oral and spray vaccines.480 The advantage lies in that it can increase the mucosal immune response and improve the effectiveness of neutralizing antibodies; low-temperature storage is no longer required, and the transportation problem is solved, thereby facilitating use and promotion. A phase I clinical study481 showed that nebulization of one dose of the spray type vaccine Ad5-nCoV required only 1/5 of the dose for intramuscular injection, and nebulization of two doses of Ad5-nCoV produced antibody and cellular immune responses comparable to that of a single dose of intramuscular injection of this vaccine. Moreover, high levels of neutralizing antibodies can be produced by booster immunization using nebulization after intramuscular injection.
With the emergence of the delta variant, the third dose of vaccine booster has been implemented in various countries. In Israel, people who have been vaccinated with two doses of BNT162b2 vaccine for about 8 months received a third dose of BNT162b2 vaccine. It was found that the neutralization geometric mean titer (GMT) for the β variant increased more than the GMT for the wild-type virus,482 and the adverse events did not increase significantly. At least 12 days after the booster vaccination, the confirmed infection rate of the boosted group was 11.3 times lower than that of the unboosted group; the severe disease rate was reduced by 19.5 times.483 Preliminary data showed that the same three doses of inactivated virus vaccine can also enhance and maintain the immune response, and the peak antibody level is about 25 times higher than before the injection. Even six months after the injection, the antibody level is still comparable to the peak after the second dose. The above-mentioned researches focus on the effect of homologous prime-boost vaccinations, while heterologous prime-boost immunization strategies have also been under investigation and preliminary results demonstrate a significant increase in the level of neutralizing antibody.
Summary
In addition to pneumonia and ARDS, severe COVID-19 mainly involves multiple extrapulmonary organs and systems such as cardiovascular, renal, gastrointestinal, and hepatobiliary systems, as well as hematological, neurological, endocrine and metabolic systems, etc. SARS-CoV-2 may directly invade the host cells of multiple organs through the ACE2 that is widely distributed in various human tissues and TMPRSS2 or other possible entry routes. Moreover, cytokine storm and infiltration of inflammatory cells, dysregulated immune responses, coagulation dysfunction, and epithelial injury can induce multiorgan failure in the severe cases with COVID-19. Gaining a whole picture of the clinical features of multiorgan dysfunction in critically ill patients with COVID-19 is of highly great importance for both clinicians and researchers. Consequently, fulfilling the knowledge on the potential mechanisms underlying of SARS-CoV-2-induced pulmonary and extrapulmonary complications may ultimately lead to the development of potential therapeutic approaches for COVID-19, which will eventually eradicate COVID-19 across the globe. Nevertheless, given the rapidly evolving scenario due to the emergence of SARS-CoV-2 variants and ongoing vaccination campaigns, more studies are warranted to achieve comprehensive knowledge of the multifaceted interaction between the host and SARS-CoV-2.
Acknowledgements
We thank Mengxin Lu, Yuting Diao, Xue Hu, Meiwen Han, Xitang Li, Suping Hai, Qiang Gao, and Wenhui Wu for their assistance with literature searching. Received funding from: The National Key Research and Development Program of China (2021YFC2600200); Chinese National Thirteenth-Five Years Project in Science and Technology (2017ZX10202201); Science and Technology Department of Hubei (2020FCA044); Wuhan Science and Technology Bureau (2020020601012228, 2020020601012236); Huazhong University of Science and Technology (2020kfyXGYJ065).
Author contributions
Q.N. and D.W. contributed equally to this paper as co-first authors. Q.N., X.L. and M.H. contributed equally to this paper as co-corresponding authors. D.W., X.W., D.X., T.C., G.C., H.W., M.W., L.Z., J.H., T.L., K.M. and M.H. contributed to literature search, and writing of the manuscript. All authors have read and approved the article.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Qin Ning, Di Wu
Contributor Information
Qin Ning, Email: qning@vip.sina.com.
Meifang Han, Email: mfhan@foxmail.com.
Xiaoping Luo, Email: xpluo@tjh.tjmu.edu.cn.
References
- 1.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weekly epidemiological update on COVID-19. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---6-january-2022.
- 3.Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr. Probl. Cardiol. 2020;45:100618. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mokhtari T, et al. COVID-19 and multiorgan failure: a narrative review on potential mechanisms. J. Mol. Histol. 2020;51:613–628. doi: 10.1007/s10735-020-09915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seeherman, S. & Suzuki, Y. J. Viral infection and cardiovascular disease: implications for the molecular basis of COVID-19 pathogenesis. Int. J. Mol. Sci.22, 1659 (2021). [DOI] [PMC free article] [PubMed]
- 6.Nägele MP, Haubner B, Tanner FC, Ruschitzka F, Flammer AJ. Endothelial dysfunction in COVID-19: Current findings and therapeutic implications. Atherosclerosis. 2020;314:58–62. doi: 10.1016/j.atherosclerosis.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pei G, et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia. J. Am. Soc. Nephrol. 2020;31:1157–1165. doi: 10.1681/ASN.2020030276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alqahtani SA, Schattenberg JM. Liver injury in COVID-19: the current evidence. U. Eur. Gastroenterol. J. 2020;8:509–519. doi: 10.1177/2050640620924157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitsuyama, K. et al. Clinical features and pathogenic mechanisms of gastrointestinal injury in COVID-19. J. Clin. Med. 9, 3630 (2020). [DOI] [PMC free article] [PubMed]
- 11.Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat. Rev. Endocrinol. 2021;17:11–30. doi: 10.1038/s41574-020-00435-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mao L, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ashraf UM, et al. SARS-CoV-2, ACE2 expression, and systemic organ invasion. Physiol. Genomics. 2021;53:51–60. doi: 10.1152/physiolgenomics.00087.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwasaki M, et al. Inflammation triggered by SARS-CoV-2 and ACE2 augment drives multiple organ failure of severe COVID-19: molecular mechanisms and implications. Inflammation. 2021;44:13–34. doi: 10.1007/s10753-020-01337-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang L, et al. COVID-19: immunopathogenesis and immunotherapeutics. Signal Transduct. Target Ther. 2020;5:128. doi: 10.1038/s41392-020-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boson B, et al. The SARS-CoV-2 envelope and membrane proteins modulate maturation and retention of the spike protein, allowing assembly of virus-like particles. J. Biol. Chem. 2021;296:100111. doi: 10.1074/jbc.RA120.016175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siu YL, et al. The M, E, and N structural proteins of the severe acute respiratory syndrome coronavirus are required for efficient assembly, trafficking, and release of virus-like particles. J. Virol. 2008;82:11318–11330. doi: 10.1128/JVI.01052-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scialo, F. et al. SARS-CoV-2: one year in the pandemic. what have we learned, the new vaccine era and the threat of SARS-CoV-2 variants. Biomedicines9, 611 (2021). [DOI] [PMC free article] [PubMed]
- 19.Conceicao C, et al. The SARS-CoV-2 Spike protein has a broad tropism for mammalian ACE2 proteins. PLoS Biol. 2020;18:e3001016. doi: 10.1371/journal.pbio.3001016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lan J, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 21.Huang Y, Yang C, Xu XF, Xu W, Liu SW. Structural and functional properties of SARS-CoV-2 spike protein: potential antivirus drug development for COVID-19. Acta Pharm. Sin. 2020;41:1141–1149. doi: 10.1038/s41401-020-0485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J. Pharm. Anal. 2020;10:102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tipnis SR, et al. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J. Biol. Chem. 2000;275:33238–33243. doi: 10.1074/jbc.M002615200. [DOI] [PubMed] [Google Scholar]
- 24.Hamming I, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Geravandi S, Mahmoudi-Aznaveh A, Azizi Z, Maedler K, Ardestani A. SARS-CoV-2 and pancreas: a potential pathological interaction? Trends Endocrinol. Metab. 2021;32:842–845. doi: 10.1016/j.tem.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang L, et al. A human pluripotent stem cell-based platform to study SARS-CoV-2 tropism and model virus infection in human cells and organoids. Cell Stem Cell. 2020;27:125–136. doi: 10.1016/j.stem.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cantuti-Castelvetri L, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoffmann M, Kleine-Weber H, Pöhlmann S. A multibasic cleavage site in the spike protein of SARS-CoV-2 is essential for infection of human lung cells. Mol. Cell. 2020;78:779–784. doi: 10.1016/j.molcel.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ricci, D. et al. Innate immune response to SARS-CoV-2 infection: from cells to soluble mediators. Int. J. Mol. Sci. 22, 7017 (2021). [DOI] [PMC free article] [PubMed]
- 30.Yeung ML, et al. Soluble ACE2-mediated cell entry of SARS-CoV-2 via interaction with proteins related to the renin-angiotensin system. Cell. 2021;184:2212–2228. doi: 10.1016/j.cell.2021.02.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rahbar Saadat Y, Hosseiniyan Khatibi SM, Zununi Vahed S, Ardalan M. Host serine proteases: a potential targeted therapy for COVID-19 and influenza. Front Mol. Biosci. 2021;8:725528. doi: 10.3389/fmolb.2021.725528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Choudhary S, Sharma K, Silakari O. The interplay between inflammatory pathways and COVID-19: A critical review on pathogenesis and therapeutic options. Micro. Pathog. 2021;150:104673. doi: 10.1016/j.micpath.2020.104673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Romano, M., Ruggiero, A., Squeglia, F., Maga, G. & Berisio, R. A structural view of SARS-CoV-2 RNA replication machinery: RNA synthesis, proofreading and final capping. Cells9, 1267 (2020). [DOI] [PMC free article] [PubMed]
- 35.Zhao MM, et al. Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development. Signal Transduct. Target Ther. 2021;6:134. doi: 10.1038/s41392-021-00558-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takeda M. Proteolytic activation of SARS-CoV-2 spike protein. Microbiol Immunol. 2022;66:15–23. doi: 10.1111/1348-0421.12945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Indari O, Jakhmola S, Manivannan E, Jha HC. An update on antiviral therapy against SARS-CoV-2: how far have we come? Front Pharm. 2021;12:632677. doi: 10.3389/fphar.2021.632677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lai MM, Cavanagh D. The molecular biology of coronaviruses. Adv. Virus Res. 1997;48:1–100. doi: 10.1016/S0065-3527(08)60286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tracking SARS-CoV-2 variants. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (2021).
- 41.Khateeb J, Li Y, Zhang H. Emerging SARS-CoV-2 variants of concern and potential intervention approaches. Crit. Care. 2021;25:244. doi: 10.1186/s13054-021-03662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang L, et al. SARS-CoV-2 spike-protein D614G mutation increases virion spike density and infectivity. Nat. Commun. 2020;11:6013. doi: 10.1038/s41467-020-19808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gu H, et al. Adaptation of SARS-CoV-2 in BALB/c mice for testing vaccine efficacy. Science. 2020;369:1603–1607. doi: 10.1126/science.abc4730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Starr TN, et al. Deep mutational scanning of SARS-CoV-2 receptor binding domain reveals constraints on folding and ACE2 binding. Cell. 2020;182:1295–1310. doi: 10.1016/j.cell.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rambaut A, et al. A dynamic nomenclature proposal for SARS-CoV-2 lineages to assist genomic epidemiology. Nat. Microbiol. 2020;5:1403–1407. doi: 10.1038/s41564-020-0770-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peacock TP, et al. The furin cleavage site in the SARS-CoV-2 spike protein is required for transmission in ferrets. Nat. Microbiol. 2021;6:899–909. doi: 10.1038/s41564-021-00908-w. [DOI] [PubMed] [Google Scholar]
- 47.Weisblum, Y. et al. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. Elife. 9, e61312. Preprint at https://www.biorxiv.org/content/10.1101/2020.07.21.214759v1.full.pdf (2020). [DOI] [PMC free article] [PubMed]
- 48.Aleem, A., Akbar Samad, A. B. & Slenker, A. K. Emerging variants of SARS-CoV-2 and novel therapeutics against coronavirus (COVID-19). In StatPearls. Treasure Island (FL), StatPearls; (2021).
- 49.Wang P, et al. Increased resistance of SARS-CoV-2 variant P.1 to antibody neutralization. Cell Host Microbe. 2021;29:747–751. doi: 10.1016/j.chom.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cerutti G, et al. Potent SARS-CoV-2 neutralizing antibodies directed against spike N-terminal domain target a single supersite. Cell Host Microbe. 2021;29:819–833. doi: 10.1016/j.chom.2021.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu C, et al. Reduced neutralization of SARS-CoV-2 B.1.617 by vaccine and convalescent serum. Cell. 2021;184:4220–4236. doi: 10.1016/j.cell.2021.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Planas D, et al. Reduced sensitivity of SARS-CoV-2 variant delta to antibody neutralization. Nature. 2021;596:276–280. doi: 10.1038/s41586-021-03777-9. [DOI] [PubMed] [Google Scholar]
- 53.Kannan SR, et al. Evolutionary analysis of the delta and delta plus variants of the SARS-CoV-2 viruses. J. Autoimmun. 2021;124:102715. doi: 10.1016/j.jaut.2021.102715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lotfi R, Kalmarzi RN, Roghani SA. A review on the immune responses against novel emerging coronavirus (SARS-CoV-2) Immunol. Res. 2021;69:213–224. doi: 10.1007/s12026-021-09198-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin. Chem. Lab Med. 2020;58:1021–1028. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 56.Rokni M, Ghasemi V, Tavakoli Z. Immune responses and pathogenesis of SARS-CoV-2 during an outbreak in Iran: comparison with SARS and MERS. Rev. Med. Virol. 2020;30:e2107. doi: 10.1002/rmv.2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barnes, B. J. et al. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J. Exp. Med.217, e20200652 (2020). [DOI] [PMC free article] [PubMed]
- 58.Meidaninikjeh S, et al. Monocytes and macrophages in COVID-19: friends and foes. Life Sci. 2021;269:119010. doi: 10.1016/j.lfs.2020.119010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zheng M, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol. Immunol. 2020;17:533–535. doi: 10.1038/s41423-020-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Osman MS, van Eeden C, Cohen Tervaert JW. Fatal COVID-19 infections: is NK cell dysfunction a link with autoimmune HLH? Autoimmun. Rev. 2020;19:102561. doi: 10.1016/j.autrev.2020.102561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mohamed Khosroshahi L, Rokni M, Mokhtari T, Noorbakhsh F. Immunology, immunopathogenesis and immunotherapeutics of COVID-19; an overview. Int. Immunopharmacol. 2021;93:107364. doi: 10.1016/j.intimp.2020.107364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac. J. Allergy Immunol. 2020;38:1–9. doi: 10.12932/AP-200220-0772. [DOI] [PubMed] [Google Scholar]
- 63.Fung SY, Yuen KS, Ye ZW, Chan CP, Jin DY. A tug-of-war between severe acute respiratory syndrome coronavirus 2 and host antiviral defence: lessons from other pathogenic viruses. Emerg. Microbes Infect. 2020;9:558–570. doi: 10.1080/22221751.2020.1736644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen LYC, Quach TTT. COVID-19 cytokine storm syndrome: a threshold concept. Lancet Microbe. 2021;2:e49–e50. doi: 10.1016/S2666-5247(20)30223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen R, et al. Cytokine storm: the primary determinant for the pathophysiological evolution of COVID-19 deterioration. Front. Immunol. 2021;12:589095. doi: 10.3389/fimmu.2021.589095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Que, Y. et al. Cytokine release syndrome in COVID-19: a major mechanism of morbidity and mortality. Int. Rev. Immunol. 1–14 (2021). [DOI] [PMC free article] [PubMed]
- 67.McGonagle D, Ramanan AV, Bridgewood C. Immune cartography of macrophage activation syndrome in the COVID-19 era. Nat. Rev. Rheumatol. 2021;17:145–157. doi: 10.1038/s41584-020-00571-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rodriguez-Smith JJ, et al. Inflammatory biomarkers in COVID-19-associated multisystem inflammatory syndrome in children, Kawasaki disease, and macrophage activation syndrome: a cohort study. Lancet Rheumatol. 2021;3:e574–e584. doi: 10.1016/S2665-9913(21)00139-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen, L. Y. C., Hoiland, R. L., Stukas, S., Wellington, C. L. & Sekhon, M. S. Confronting the controversy: interleukin-6 and the COVID-19 cytokine storm syndrome. Eur. Respir J. 56, 4 (2020). [DOI] [PMC free article] [PubMed]
- 70.Tang Y, et al. Cytokine storm in COVID-19: the current evidence and treatment strategies. Front. Immunol. 2020;11:1708. doi: 10.3389/fimmu.2020.01708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li J, et al. Virus-host interactome and proteomic survey reveal potential virulence factors influencing SARS-CoV-2 pathogenesis. Med. 2021;2:99–112. doi: 10.1016/j.medj.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hou W, Jin YH, Kang HS, Kim BS. Interleukin-6 (IL-6) and IL-17 synergistically promote viral persistence by inhibiting cellular apoptosis and cytotoxic T cell function. J. Virol. 2014;88:8479–8489. doi: 10.1128/JVI.00724-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wu D, Yang XO. TH17 responses in cytokine storm of COVID-19: an emerging target of JAK2 inhibitor Fedratinib. J. Microbiol. Immunol. Infect. 2020;53:368–370. doi: 10.1016/j.jmii.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Coomes EA, Haghbayan H. Interleukin-6 in Covid-19: a systematic review and meta-analysis. Rev. Med. Virol. 2020;30:1–9. doi: 10.1002/rmv.2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kang S, Tanaka T, Narazaki M, Kishimoto T. Targeting interleukin-6 signaling in clinic. Immunity. 2019;50:1007–1023. doi: 10.1016/j.immuni.2019.03.026. [DOI] [PubMed] [Google Scholar]
- 76.Baran P, et al. The balance of interleukin (IL)-6, IL-6.soluble IL-6 receptor (sIL-6R), and IL-6.sIL-6R.sgp130 complexes allows simultaneous classic and trans-signaling. J. Biol. Chem. 2018;293:6762–6775. doi: 10.1074/jbc.RA117.001163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xu X, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl Acad. Sci. USA. 2020;117:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhou, Y. et al. Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl Sci. Rev.7, 998–1002 (2020). [DOI] [PMC free article] [PubMed]
- 79.Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kim YM, Shin EC. Type I and III interferon responses in SARS-CoV-2 infection. Exp. Mol. Med. 2021;53:750–760. doi: 10.1038/s12276-021-00592-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Totura AL, Baric RS. SARS coronavirus pathogenesis: host innate immune responses and viral antagonism of interferon. Curr. Opin. Virol. 2012;2:264–275. doi: 10.1016/j.coviro.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hadjadj J, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang, Q. et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science370, eabd4570 (2020). [DOI] [PMC free article] [PubMed]
- 84.Bastard, P. et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science370, eabd4585 (2020). [DOI] [PMC free article] [PubMed]
- 85.Lee JS, Shin EC. The type I interferon response in COVID-19: implications for treatment. Nat. Rev. Immunol. 2020;20:585–586. doi: 10.1038/s41577-020-00429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Garcia KC. Dual arms of adaptive immunity: division of labor and collaboration between B and T cells. Cell. 2019;179:3–7. doi: 10.1016/j.cell.2019.08.022. [DOI] [PubMed] [Google Scholar]
- 87.Liu WJ, et al. T-cell immunity of SARS-CoV: implications for vaccine development against MERS-CoV. Antivir. Res. 2017;137:82–92. doi: 10.1016/j.antiviral.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rokni M, Hamblin MR, Rezaei N. Cytokines and COVID-19: friends or foes? Hum. Vaccin Immunother. 2020;16:2363–2365. doi: 10.1080/21645515.2020.1799669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dong C, Flavell RA. Cell fate decision: T-helper 1 and 2 subsets in immune responses. Arthritis Res. 2000;2:179–188. doi: 10.1186/ar85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu J, Paul WE. CD4 T cells: fates, functions, and faults. Blood. 2008;112:1557–1569. doi: 10.1182/blood-2008-05-078154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chowdhury MA, Hossain N, Kashem MA, Shahid MA, Alam A. Immune response in COVID-19: a review. J. Infect. Public Health. 2020;13:1619–1629. doi: 10.1016/j.jiph.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.García LF. Immune response, inflammation, and the clinical spectrum of COVID-19. Front. Immunol. 2020;11:1441. doi: 10.3389/fimmu.2020.01441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen T, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen G, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Arruvito L, et al. Identification and clinical relevance of naturally occurring human CD8+ HLA-DR+ regulatory T cells. J. Immunol. 2014;193:4469–4476. doi: 10.4049/jimmunol.1401490. [DOI] [PubMed] [Google Scholar]
- 96.Zheng HY, et al. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell Mol. Immunol. 2020;17:541–543. doi: 10.1038/s41423-020-0401-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Diao B, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) Front. Immunol. 2020;11:827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wilk AJ, et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat. Med. 2020;26:1070–1076. doi: 10.1038/s41591-020-0944-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang B, et al. Immune phenotyping based on the neutrophil-to-lymphocyte ratio and IgG level predicts disease severity and outcome for patients with COVID-19. Front. Mol. Biosci. 2020;7:157. doi: 10.3389/fmolb.2020.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Keidar S, et al. Mineralocorticoid receptor blocker increases angiotensin-converting enzyme 2 activity in congestive heart failure patients. Circ. Res. 2005;97:946–953. doi: 10.1161/01.RES.0000187500.24964.7A. [DOI] [PubMed] [Google Scholar]
- 101.Moon C. Fighting COVID-19 exhausts T cells. Nat. Rev. Immunol. 2020;20:277. doi: 10.1038/s41577-020-0304-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang Y, et al. Potential contribution of increased soluble IL-2R to lymphopenia in COVID-19 patients. Cell Mol. Immunol. 2020;17:878–880. doi: 10.1038/s41423-020-0484-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cao X. COVID-19: immunopathology and its implications for therapy. Nat. Rev. Immunol. 2020;20:269–270. doi: 10.1038/s41577-020-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tan L, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct. Target Ther. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Peñaloza HF, Lee JS, Ray P. Neutrophils and lymphopenia, an unknown axis in severe COVID-19 disease. PLoS Pathog. 2021;17:e1009850. doi: 10.1371/journal.ppat.1009850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Goshua G, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Syed F, et al. Excessive matrix metalloproteinase-1 and hyperactivation of endothelial cells occurred in COVID-19 patients and were associated with the severity of COVID-19. J. Infect. Dis. 2021;224:60–69. doi: 10.1093/infdis/jiab167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Philippe A, et al. Circulating Von Willebrand factor and high molecular weight multimers as markers of endothelial injury predict COVID-19 in-hospital mortality. Angiogenesis. 2021;24:505–517. doi: 10.1007/s10456-020-09762-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ackermann M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Damiani S, et al. Pathological post-mortem findings in lungs infected with SARS-CoV-2. J. Pathol. 2021;253:31–40. doi: 10.1002/path.5549. [DOI] [PubMed] [Google Scholar]
- 111.Klouda, T. et al. Interferon-alpha or -beta facilitates SARS-CoV-2 pulmonary vascular infection by inducing ACE2. Angiogenesis10.1007/s10456-021-09823-4 (2021). [DOI] [PMC free article] [PubMed]
- 112.Colunga Biancatelli RML, et al. The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2021;321:L477–l484. doi: 10.1152/ajplung.00223.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Michalick, L. et al. Plasma mediators in patients with severe COVID-19 cause lung endothelial barrier failure. Eur. Respir. J. 57, 2002384 (2021). [DOI] [PMC free article] [PubMed]
- 114.Varga Z, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Maccio U, et al. SARS-CoV-2 leads to a small vessel endotheliitis in the heart. eBioMedicine. 2021;63:103182. doi: 10.1016/j.ebiom.2020.103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Akilesh S, et al. Multicenter clinicopathologic correlation of kidney biopsies performed in COVID-19 patients presenting with acute kidney injury or proteinuria. Am. J. Kidney Dis. 2021;77:82–93. doi: 10.1053/j.ajkd.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wagner JUG, et al. Increased susceptibility of human endothelial cells to infections by SARS-CoV-2 variants. Basic Res. Cardiol. 2021;116:42. doi: 10.1007/s00395-021-00882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Paniz-Mondolfi A, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) J. Med. Virol. 2020;92:699–702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lei Y, et al. SARS-CoV-2 spike protein impairs endothelial function via downregulation of ACE 2. Circ. Res. 2021;128:1323–1326. doi: 10.1161/CIRCRESAHA.121.318902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Colmenero I, et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br. J. Dermatol. 2020;183:729–737. doi: 10.1111/bjd.19327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rauch A, et al. Endotheliopathy is induced by plasma from critically Ill patients and associated with organ failure in severe COVID-19. Circulation. 2020;142:1881–1884. doi: 10.1161/CIRCULATIONAHA.120.050907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Xu S, et al. The zinc finger transcription factor, KLF2, protects against COVID-19 associated endothelial dysfunction. Signal Transduct. Target Ther. 2021;6:266. doi: 10.1038/s41392-021-00690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kang S, et al. IL-6 trans-signaling induces plasminogen activator inhibitor-1 from vascular endothelial cells in cytokine release syndrome. Proc. Natl Acad. Sci. USA. 2020;117:22351–22356. doi: 10.1073/pnas.2010229117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McConnell MJ, et al. Liver injury in COVID-19 and IL-6 trans-signaling-induced endotheliopathy. J. Hepatol. 2021;75:647–658. doi: 10.1016/j.jhep.2021.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cugno M, et al. Complement activation and endothelial perturbation parallel COVID-19 severity and activity. J. Autoimmun. 2021;116:102560. doi: 10.1016/j.jaut.2020.102560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Aid M, et al. Vascular disease and thrombosis in SARS-CoV-2-infected rhesus macaques. Cell. 2020;183:1354–1366. doi: 10.1016/j.cell.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Queisser, K. A. et al. COVID-19 generates hyaluronan fragments that directly induce endothelial barrier dysfunction. JCI Insight6, 17 (2021). [DOI] [PMC free article] [PubMed]
- 128.Stahl K, et al. Injury to the endothelial glycocalyx in critically ill patients with COVID-19. Am. J. Respir. Crit. Care Med. 2020;202:1178–1181. doi: 10.1164/rccm.202007-2676LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dean MJ, et al. Severe COVID-19 is characterized by an impaired type I interferon response and elevated levels of arginase producing granulocytic myeloid derived suppressor cells. Front. Immunol. 2021;12:695972. doi: 10.3389/fimmu.2021.695972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chioh, F. W. et al. Convalescent COVID-19 patients are susceptible to endothelial dysfunction due to persistent immune activation. eLife10, e64909 (2021). [DOI] [PMC free article] [PubMed]
- 131.Guan WJ, et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Yuan X, et al. Coagulopathy in elderly patients with coronavirus disease 2019. Aging Med. 2020;3:260–265. doi: 10.1002/agm2.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rastogi A, Dogra H, Jude EB. COVID-19 and peripheral arterial complications in people with diabetes and hypertension: a systematic review. Diabetes Metab. Syndr. 2021;15:102204. doi: 10.1016/j.dsx.2021.102204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chen, X. et al. Coagulopathy is a major extrapulmonary risk factor for mortality in hospitalized patients with COVID-19 with type 2 diabetes. BMJ Open Diabetes Res. Care8, e001851 (2020). [DOI] [PMC free article] [PubMed]
- 136.Klok FA, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bompard, F. et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur. Respir. J.56, 2001365 (2020). [DOI] [PMC free article] [PubMed]
- 138.Menter T, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77:198–209. doi: 10.1111/his.14134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Leng L, et al. Pathological features of COVID-19-associated lung injury: a preliminary proteomics report based on clinical samples. Signal Transduct. Target Ther. 2020;5:240. doi: 10.1038/s41392-020-00355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Nie X, et al. Multi-organ proteomic landscape of COVID-19 autopsies. Cell. 2021;184:775–791. doi: 10.1016/j.cell.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Cugno M, et al. Complement activation in patients with COVID-19: a novel therapeutic target. J. Allergy Clin. Immunol. 2020;146:215–217. doi: 10.1016/j.jaci.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yu, J. et al. Complement dysregulation is associated with severe COVID-19 illness. Haematologica10.3324/haematol.2021.279155 (2021). [DOI] [PMC free article] [PubMed]
- 143.Barrett TJ, et al. Platelet and vascular biomarkers associate with thrombosis and death in coronavirus disease. Circ. Res. 2020;127:945–947. doi: 10.1161/CIRCRESAHA.120.317803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Bongiovanni D, et al. SARS-CoV-2 infection is associated with a pro-thrombotic platelet phenotype. Cell Death Dis. 2021;12:50. doi: 10.1038/s41419-020-03333-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang S, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J. Hematol. Oncol. 2020;13:120. doi: 10.1186/s13045-020-00954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hottz ED, et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136:1330–1341. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Manne BK, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136:1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Koupenova M, et al. SARS-CoV-2 initiates programmed cell death in platelets. Circ. Res. 2021;129:631–646. doi: 10.1161/CIRCRESAHA.121.319117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Middleton EA, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Radermecker, C. et al. Neutrophil extracellular traps infiltrate the lung airway, interstitial, and vascular compartments in severe COVID-19. J. Exp. Med.217, e20201012 (2020). [DOI] [PMC free article] [PubMed]
- 151.Nicolai L, et al. Immunothrombotic dysregulation in COVID-19 pneumonia is associated with respiratory failure and coagulopathy. Circulation. 2020;142:1176–1189. doi: 10.1161/CIRCULATIONAHA.120.048488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Veras, F. P. et al. SARS-CoV-2-triggered neutrophil extracellular traps mediate COVID-19 pathology. J. Exp. Med.217, e20201129 (2020). [DOI] [PMC free article] [PubMed]
- 153.Englert H, et al. Defective NET clearance contributes to sustained FXII activation in COVID-19-associated pulmonary thrombo-inflammation. eBioMedicine. 2021;67:103382. doi: 10.1016/j.ebiom.2021.103382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Leppkes M, et al. Vascular occlusion by neutrophil extracellular traps in COVID-19. eBioMedicine. 2020;58:102925. doi: 10.1016/j.ebiom.2020.102925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Violi F, et al. Nox2 activation in Covid-19. Redox Biol. 2020;36:101655. doi: 10.1016/j.redox.2020.101655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gao YL, et al. Role of renin-angiotensin system in acute lung injury caused by viral infection. Infect. Drug Resist. 2020;13:3715–3725. doi: 10.2147/IDR.S265718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Datta PK, Liu F, Fischer T, Rappaport J, Qin X. SARS-CoV-2 pandemic and research gaps: understanding SARS-CoV-2 interaction with the ACE2 receptor and implications for therapy. Theranostics. 2020;10:7448–7464. doi: 10.7150/thno.48076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Samavati L, Uhal BD. ACE2, much more than just a receptor for SARS-COV-2. Front. Cell Infect. Microbiol. 2020;10:317. doi: 10.3389/fcimb.2020.00317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jin, Y. et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses12, 372 (2020). [DOI] [PMC free article] [PubMed]
- 160.Silhol F, Sarlon G, Deharo JC, Vaïsse B. Downregulation of ACE2 induces overstimulation of the renin-angiotensin system in COVID-19: should we block the renin-angiotensin system? Hypertens. Res. 2020;43:854–856. doi: 10.1038/s41440-020-0476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hamming I, et al. The emerging role of ACE2 in physiology and disease. J. Pathol. 2007;212:1–11. doi: 10.1002/path.2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ni W, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care. 2020;24:422. doi: 10.1186/s13054-020-03120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Verdecchia P, Cavallini C, Spanevello A, Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Sun P, et al. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J. Med Virol. 2020;92:612–617. doi: 10.1002/jmv.25735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wu C, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hou J, Hsu JM, Hung MC. Molecular mechanisms and functions of pyroptosis in inflammation and antitumor immunity. Mol. Cell. 2021;81:4579–4590. doi: 10.1016/j.molcel.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Carcaterra M, Caruso C. Alveolar epithelial cell type II as main target of SARS-CoV-2 virus and COVID-19 development via NF-Kb pathway deregulation: a physio-pathological theory. Med. Hypotheses. 2021;146:110412. doi: 10.1016/j.mehy.2020.110412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Mulay A, et al. SARS-CoV-2 infection of primary human lung epithelium for COVID-19 modeling and drug discovery. Cell Rep. 2021;35:109055. doi: 10.1016/j.celrep.2021.109055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bridges, J. P., Vladar, E. K., Huang, H. & Mason, R. J. Respiratory epithelial cell responses to SARS-CoV-2 in COVID-19. Thorax77, 203–209 (2021). [DOI] [PMC free article] [PubMed]
- 170.Martines RB, et al. Pathology and pathogenesis of SARS-CoV-2 associated with fatal coronavirus disease, United States. Emerg. Infect. Dis. 2020;26:2005–2015. doi: 10.3201/eid2609.202095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Pan Y, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur. Radio. 2020;30:3306–3309. doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Han S, Mallampalli RK. The acute respiratory distress syndrome: from mechanism to translation. J. Immunol. 2015;194:855–860. doi: 10.4049/jimmunol.1402513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Xu Z, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Aggarwal NR, King LS, D’Alessio FR. Diverse macrophage populations mediate acute lung inflammation and resolution. Am. J. Physiol. Lung Cell Mol. Physiol. 2014;306:L709–L725. doi: 10.1152/ajplung.00341.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Meduri GU, Annane D, Chrousos GP, Marik PE, Sinclair SE. Activation and regulation of systemic inflammation in ARDS: rationale for prolonged glucocorticoid therapy. Chest. 2009;136:1631–1643. doi: 10.1378/chest.08-2408. [DOI] [PubMed] [Google Scholar]
- 176.Mason RJ. Thoughts on the alveolar phase of COVID-19. Am. J. Physiol. Lung Cell Mol. Physiol. 2020;319:L115–L120. doi: 10.1152/ajplung.00126.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat. Rev. Immunol. 2020;20:389–391. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Guven G, Ince C, Topeli A, Caliskan K. Cardio-pulmonary-renal consequences of severe COVID-19. Cardiorenal Med. 2021;11:133–139. doi: 10.1159/000516740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Panitchote A, et al. Factors associated with acute kidney injury in acute respiratory distress syndrome. Ann. Intensive Care. 2019;9:74. doi: 10.1186/s13613-019-0552-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Husain-Syed F, Slutsky AS, Ronco C. Lung-kidney cross-talk in the critically ill patient. Am. J. Respir. Crit. Care Med. 2016;194:402–414. doi: 10.1164/rccm.201602-0420CP. [DOI] [PubMed] [Google Scholar]
- 181.Puri G, Singh VP, Naura AS. COVID-19 severity: lung-heart interplay. Curr. Cardiol. Rev. 2021;17:e230421189016. doi: 10.2174/1573403X16999201210200614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Sencio V, Machado MG, Trottein F. The lung-gut axis during viral respiratory infections: the impact of gut dysbiosis on secondary disease outcomes. Mucosal Immunol. 2021;14:296–304. doi: 10.1038/s41385-020-00361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Battaglini D, et al. Neurological manifestations of severe SARS-CoV-2 infection: potential mechanisms and implications of individualized mechanical ventilation settings. Front. Neurol. 2020;11:845. doi: 10.3389/fneur.2020.00845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Smilowitz NR, et al. Myocardial injury in adults hospitalized with COVID-19. Circulation. 2020;142:2393–2395. doi: 10.1161/CIRCULATIONAHA.120.050434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Wang D, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J. Am. Med. Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chen G, et al. Hypertension as a sequela in patients of SARS-CoV-2 infection. PLoS ONE. 2021;16:e0250815. doi: 10.1371/journal.pone.0250815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Weckbach LT, et al. Myocardial inflammation and dysfunction in COVID-19-associated myocardial injury. Circ. Cardiovasc Imaging. 2021;14:e012220. doi: 10.1161/CIRCIMAGING.120.011713. [DOI] [PubMed] [Google Scholar]
- 188.Vitiello A, Ferrara F. Pharmacological agents to therapeutic treatment of cardiac injury caused by Covid-19. Life Sci. 2020;262:118510. doi: 10.1016/j.lfs.2020.118510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bajaj R, et al. Delayed-onset myocarditis following COVID-19. Lancet Respir. Med. 2021;9:e32–e34. doi: 10.1016/S2213-2600(21)00085-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Gauchotte G, et al. SARS-Cov-2 fulminant myocarditis: an autopsy and histopathological case study. Int. J. Leg. Med. 2021;135:577–581. doi: 10.1007/s00414-020-02500-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Titi L, et al. Fatal Takotsubo syndrome in critical COVID-19 related pneumonia. Cardiovasc Pathol. 2021;51:107314. doi: 10.1016/j.carpath.2020.107314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Manzur-Sandoval D, Carmona-Levario P, García-Cruz E. Giant inverted T waves in a patient with COVID-19 infection. Ann. Emerg. Med. 2021;77:264–267. doi: 10.1016/j.annemergmed.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Bikdeli B, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Chang WT, Toh HS, Liao CT, Yu WL. Cardiac involvement of COVID-19: a comprehensive review. Am. J. Med Sci. 2021;361:14–22. doi: 10.1016/j.amjms.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ikeuchi K, Saito M, Yamamoto S, Nagai H, Adachi E. Relative bradycardia in patients with mild-to-moderate coronavirus disease, Japan. Emerg. Infect. Dis. 2020;26:2504–2506. doi: 10.3201/eid2610.202648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Manolis AS, et al. COVID-19 infection and cardiac arrhythmias. Trends Cardiovasc Med. 2020;30:451–460. doi: 10.1016/j.tcm.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Lakkireddy DR, et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Heart Rhythm. 2020;17:e233–e241. doi: 10.1016/j.hrthm.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Pavri BB, Kloo J, Farzad D, Riley JM. Behavior of the PR interval with increasing heart rate in patients with COVID-19. Heart Rhythm. 2020;17:1434–1438. doi: 10.1016/j.hrthm.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Guglin, M., Ballut, K., Ilonze, O., Jones, M. & Rao, R. Clinical variants of myocardial involvement in COVID-19-positive patients: a cumulative experience of 2020. Heart Fail. Rev. 1–13 (2021). [DOI] [PMC free article] [PubMed]
- 200.Alsaied T, et al. Review of cardiac involvement in multisystem inflammatory syndrome in children. Circulation. 2021;143:78–88. doi: 10.1161/CIRCULATIONAHA.120.049836. [DOI] [PubMed] [Google Scholar]
- 201.Cavigli L, et al. A prospective study on the consequences of SARS-CoV-2 infection on the heart of young adult competitive athletes: implications for a safe return-to-play. Int. J. Cardiol. 2021;336:130–136. doi: 10.1016/j.ijcard.2021.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Mercedes BR, et al. New-onset myocardial injury in pregnant patients with coronavirus disease 2019: a case series of 15 patients. Am. J. Obstet. Gynecol. 2021;224:387.e1–387.e9. doi: 10.1016/j.ajog.2020.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Giustino G, et al. Coronavirus and cardiovascular disease, myocardial injury, and arrhythmia: JACC focus seminar. J. Am. Coll. Cardiol. 2020;76:2011–2023. doi: 10.1016/j.jacc.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Amendola A, et al. Human cardiosphere-derived stromal cells exposed to SARS-CoV-2 evolve into hyper-inflammatory/pro-fibrotic phenotype and produce infective viral particles depending on the levels of ACE2 receptor expression. Cardiovasc Res. 2021;117:1557–1566. doi: 10.1093/cvr/cvab082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Marchiano S, et al. SARS-CoV-2 infects human pluripotent stem cell-derived cardiomyocytes, impairing electrical and mechanical function. Stem Cell Rep. 2021;16:478–492. doi: 10.1016/j.stemcr.2021.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Yiangou L, Davis RP, Mummery CL. Using cardiovascular cells from human pluripotent stem cells for COVID-19 research: why the heart fails. Stem Cell Rep. 2021;16:385–397. doi: 10.1016/j.stemcr.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Hamouche W, et al. Pathophysiology and pharmacological management of pulmonary and cardiovascular features of COVID-19. J. Mol. Cell Cardiol. 2021;153:72–85. doi: 10.1016/j.yjmcc.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Bavishi C, et al. Special Article—Acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog. Cardiovasc Dis. 2020;63:682–689. doi: 10.1016/j.pcad.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gedefaw, L. et al. Inflammasome activation-induced hypercoagulopathy: impact on cardiovascular dysfunction triggered in COVID-19 patients. Cells10, 916 (2021). [DOI] [PMC free article] [PubMed]
- 210.Roy D, Ramasamy R, Schmidt AM. Journey to a receptor for advanced glycation end products connection in severe acute respiratory syndrome coronavirus 2 infection: with stops along the way in the lung, heart, blood vessels, and adipose tissue. Arterioscler Thromb. Vasc. Biol. 2021;41:614–627. doi: 10.1161/ATVBAHA.120.315527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Violi F, Pastori D, Pignatelli P, Cangemi R. SARS-CoV-2 and myocardial injury: a role for Nox2? Intern. Emerg. Med. 2020;15:755–758. doi: 10.1007/s11739-020-02348-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.McCarthy CG, Wilczynski S, Wenceslau CF, Webb RC. A new storm on the horizon in COVID-19: bradykinin-induced vascular complications. Vasc. Pharm. 2021;137:106826. doi: 10.1016/j.vph.2020.106826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Robbins-Juarez SY, et al. Outcomes for patients with COVID-19 and acute kidney injury: a systematic review and meta-analysis. Kidney Int. Rep. 2020;5:1149–1160. doi: 10.1016/j.ekir.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Lee JR, et al. Characteristics of acute kidney injury in hospitalized COVID-19 patients in an urban academic medical center. Clin. J. Am. Soc. Nephrol. 2021;16:284–286. doi: 10.2215/CJN.07440520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.El Shamy O, et al. Coronavirus disease 2019 (COVID-19) hospitalized patients with acute kidney injury treated with acute peritoneal dialysis do not have infectious peritoneal dialysis effluent. Kidney Int. 2020;98:782. doi: 10.1016/j.kint.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Hirsch JS, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–218. doi: 10.1016/j.kint.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Husain-Syed F, et al. Acute kidney injury and urinary biomarkers in hospitalized patients with coronavirus disease-2019. Nephrol. Dial. Transpl. 2020;35:1271–1274. doi: 10.1093/ndt/gfaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Lin L, et al. Risk factors and prognosis for COVID-19-induced acute kidney injury: a meta-analysis. BMJ Open. 2020;10:e042573. doi: 10.1136/bmjopen-2020-042573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yang X, et al. Prevalence and impact of acute renal impairment on COVID-19: a systematic review and meta-analysis. Crit. Care. 2020;24:356. doi: 10.1186/s13054-020-03065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Mohamed MMB, Velez JCQ. Proteinuria in COVID-19. Clin. Kidney J. 2021;14:i40–i47. doi: 10.1093/ckj/sfab036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Karras A, et al. Proteinuria and clinical outcomes in hospitalized COVID-19 patients: a retrospective single-center study. Clin. J. Am. Soc. Nephrol. 2021;16:514–521. doi: 10.2215/CJN.09130620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Huart J, et al. Proteinuria in COVID-19: prevalence, characterization and prognostic role. J. Nephrol. 2021;34:355–364. doi: 10.1007/s40620-020-00931-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Batlle D, et al. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J. Am. Soc. Nephrol. 2020;31:1380–1383. doi: 10.1681/ASN.2020040419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Braun F, et al. SARS-CoV-2 renal tropism associates with acute kidney injury. Lancet. 2020;396:597–598. doi: 10.1016/S0140-6736(20)31759-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Delanghe, J. R., Speeckaert, M. M. & De Buyzere, M. L. The host’s angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Clin. Chim. Acta505, 192–193 (2020). [DOI] [PMC free article] [PubMed]
- 226.Zarbock A, Gomez H, Kellum JA. Sepsis-induced acute kidney injury revisited: pathophysiology, prevention and future therapies. Curr. Opin. Crit. Care. 2014;20:588–595. doi: 10.1097/MCC.0000000000000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Wu H, et al. AKI and collapsing glomerulopathy associated with COVID-19 and APOL 1 high-risk genotype. J. Am. Soc. Nephrol. 2020;31:1688–1695. doi: 10.1681/ASN.2020050558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Laboux T, Gibier JB, Pottier N, Glowacki F, Hamroun A. Correction to: COVID-19-related collapsing glomerulopathy revealing a rare risk variant of APOL1: lessons for the clinical nephrologist. J. Nephrol. 2021;34:379. doi: 10.1007/s40620-021-01037-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Noble R, et al. Collapsing glomerulopathy affecting native and transplant kidneys in individuals with COVID-19. Nephron. 2020;144:589–594. doi: 10.1159/000509938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Lazareth H, et al. COVID-19-related collapsing glomerulopathy in a kidney transplant recipient. Am. J. Kidney Dis. 2020;76:590–594. doi: 10.1053/j.ajkd.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Kadosh BS, Pavone J, Wu M, Reyentovich A, Gidea C. Collapsing glomerulopathy associated with COVID-19 infection in a heart transplant recipient. J. Heart Lung Transpl. 2020;39:855–857. doi: 10.1016/j.healun.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Kissling S, et al. Collapsing glomerulopathy in a COVID-19 patient. Kidney Int. 2020;98:228–231. doi: 10.1016/j.kint.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Laboux T, Gibier JB, Pottier N, Glowacki F, Hamroun A. COVID-19-related collapsing glomerulopathy revealing a rare risk variant of APOL1: lessons for the clinical nephrologist. J. Nephrol. 2021;34:373–378. doi: 10.1007/s40620-020-00935-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Friedman DJ. COVID-19 and APOL1: understanding disease mechanisms through clinical observation. J. Am. Soc. Nephrol. 2021;32:1–2. doi: 10.1681/ASN.2020111629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Hoilat GJ, Das G, Shahnawaz M, Shanley P, Bukhari SH. COVID-19 induced collapsing glomerulopathy and role of APOL1. Qjm. 2021;114:263–264. doi: 10.1093/qjmed/hcaa335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Jhaveri KD, et al. Thrombotic microangiopathy in a patient with COVID-19. Kidney Int. 2020;98:509–512. doi: 10.1016/j.kint.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Sharma S, Pavuluri S, Srinivasan K, Ghouse M. Thrombotic microangiopathy in a patient with COVID-19 infection and metastatic cholangiocarcinoma. J. Hematol. 2021;10:83–88. doi: 10.14740/jh825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Bascuñana A, et al. Thrombotic microangiopathy in a kidney transplant patient with COVID-19. Kidney Med. 2021;3:124–127. doi: 10.1016/j.xkme.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Airoldi A, et al. COVID-19-related thrombotic microangiopathy in a cirrhotic patient. Dig. Liver Dis. 2020;52:946. doi: 10.1016/j.dld.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Kashi M, et al. Severe arterial thrombosis associated with Covid-19 infection. Thromb. Res. 2020;192:75–77. doi: 10.1016/j.thromres.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Izzedine H, Jhaveri KD, Perazella MA. Vascular injury and COVID-19-related mortality: what lies below the tip of the iceberg? Clin. Nephrol. 2020;94:11–13. doi: 10.5414/CN110217. [DOI] [PubMed] [Google Scholar]
- 242.Izzedine H, Jhaveri KD, Perazella MA. COVID-19 therapeutic options for patients with kidney disease. Kidney Int. 2020;97:1297–1298. doi: 10.1016/j.kint.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Binois Y, et al. Acute kidney injury associated with lopinavir/ritonavir combined therapy in patients with COVID-19. Kidney Int. Rep. 2020;5:1787–1790. doi: 10.1016/j.ekir.2020.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.See YP, et al. Risk factors for development of acute kidney injury in COVID-19 patients: a retrospective observational cohort study. Nephron. 2021;145:256–264. doi: 10.1159/000514064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Villapol S. Gastrointestinal symptoms associated with COVID-19: impact on the gut microbiome. Transl. Res. 2020;226:57–69. doi: 10.1016/j.trsl.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Pan L, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am. J. Gastroenterol. 2020;115:766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Suresh Kumar, V. C. et al. Novelty in the gut: a systematic review and meta-analysis of the gastrointestinal manifestations of COVID-19. BMJ Open Gastroenterol. 7, e000417 (2020). [DOI] [PMC free article] [PubMed]
- 248.Cheung KS, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong Cohort: systematic review and meta-analysis. Gastroenterology. 2020;159:81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Lin L, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- 250.Wan Y, et al. Enteric involvement in hospitalised patients with COVID-19 outside Wuhan. Lancet Gastroenterol. Hepatol. 2020;5:534–535. doi: 10.1016/S2468-1253(20)30118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Redd WD, et al. Prevalence and characteristics of gastrointestinal symptoms in patients with severe acute respiratory syndrome coronavirus 2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020;159:765–767. doi: 10.1053/j.gastro.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.El Moheb M, et al. Gastrointestinal complications in critically ill patients with and without COVID-19. J. Am. Med. Assoc. 2020;324:1899–1901. doi: 10.1001/jama.2020.19400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Chen R, et al. Gastrointestinal symptoms associated with unfavorable prognosis of COVID-19 patients: a retrospective study. Front. Med. 2020;7:608259. doi: 10.3389/fmed.2020.608259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Nobel YR, et al. Gastrointestinal symptoms and coronavirus disease 2019: a case-control study from the United States. Gastroenterology. 2020;159:373–375. doi: 10.1053/j.gastro.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharm. Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Qi F, Qian S, Zhang S, Zhang Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys. Res. Commun. 2020;526:135–140. doi: 10.1016/j.bbrc.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zou X, et al. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020;14:185–192. doi: 10.1007/s11684-020-0754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Uhlén M, et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347:1260419. doi: 10.1126/science.1260419. [DOI] [PubMed] [Google Scholar]
- 259.Hoffmann M, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Trottein F, Sokol H. Potential causes and consequences of gastrointestinal disorders during a SARS-CoV-2 infection. Cell Rep. 2020;32:107915. doi: 10.1016/j.celrep.2020.107915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Li, S. et al. Clinical and pathological investigation of patients with severe COVID-19. JCI Insight5, 12 (2020). [DOI] [PMC free article] [PubMed]
- 262.D’Amico, F., Baumgart, D. C., Danese, S. & Peyrin-Biroulet, L. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention, and management. Clin. Gastroenterol. Hepatol. 18, 1663–1672 (2020). [DOI] [PMC free article] [PubMed]
- 263.Duvallet C, Gibbons SM, Gurry T, Irizarry RA, Alm EJ. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses. Nat. Commun. 2017;8:1784. doi: 10.1038/s41467-017-01973-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Tisoncik JR, et al. Into the eye of the cytokine storm. Microbiol. Mol. Biol. Rev. 2012;76:16–32. doi: 10.1128/MMBR.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Scaldaferri F, et al. The thrilling journey of SARS-CoV-2 into the intestine: from pathogenesis to future clinical implications. Inflamm. Bowel Dis. 2020;26:1306–1314. doi: 10.1093/ibd/izaa181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Zuo T, et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology. 2020;159:944–955. doi: 10.1053/j.gastro.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Yeoh YK, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut. 2021;70:698–706. doi: 10.1136/gutjnl-2020-323020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Li X, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Cai Q, et al. COVID-19: abnormal liver function tests. J. Hepatol. 2020;73:566–574. doi: 10.1016/j.jhep.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Cai Q, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75:1742–1752. doi: 10.1111/all.14309. [DOI] [PubMed] [Google Scholar]
- 271.Fan Z, et al. Clinical features of COVID-19-related liver functional abnormality. Clin. Gastroenterol. Hepatol. 2020;18:1561–1566. doi: 10.1016/j.cgh.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Mao R, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2020;5:667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Phipps MM, et al. Acute liver injury in COVID-19: prevalence and association with clinical outcomes in a large U.S. cohort. Hepatology. 2020;72:807–817. doi: 10.1002/hep.31404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Zhang B, et al. Clinical characteristics of 82 cases of death from COVID-19. PLoS ONE. 2020;15:e0235458. doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Lei F, et al. Longitudinal association between markers of liver injury and mortality in COVID-19 in China. Hepatology. 2020;72:389–398. doi: 10.1002/hep.31301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Ferm S, et al. Analysis of gastrointestinal and hepatic manifestations of SARS-CoV-2 infection in 892 patients in Queens, NY. Clin. Gastroenterol. Hepatol. 2020;18:2378–2379. doi: 10.1016/j.cgh.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Wander P, Epstein M, Bernstein D. COVID-19 presenting as acute hepatitis. Am. J. Gastroenterol. 2020;115:941–942. doi: 10.14309/ajg.0000000000000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Zhang C, Shi L, Wang F-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol. Hepatol. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Bloom PP, et al. Liver biochemistries in hospitalized patients with COVID-19. Hepatology. 2021;73:890–900. doi: 10.1002/hep.31326. [DOI] [PubMed] [Google Scholar]
- 280.Horvatits T, Drolz A, Trauner M, Fuhrmann V. Liver injury and failure in critical illness. Hepatology. 2019;70:2204–2215. doi: 10.1002/hep.30824. [DOI] [PubMed] [Google Scholar]
- 281.Kaafarani HMA, et al. Gastrointestinal complications in critically ill patients with COVID-19. Ann. Surg. 2020;272:e61–e62. doi: 10.1097/SLA.0000000000004004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Gao F, et al. Metabolic associated fatty liver disease increases coronavirus disease 2019 disease severity in nondiabetic patients. J. Gastroenterol. Hepatol. 2021;36:204–207. doi: 10.1111/jgh.15112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Targher G, et al. Risk of severe illness from COVID-19 in patients with metabolic dysfunction-associated fatty liver disease and increased fibrosis scores. Gut. 2020;69:1545–1547. doi: 10.1136/gutjnl-2020-321611. [DOI] [PubMed] [Google Scholar]
- 284.Iavarone M, et al. High rates of 30-day mortality in patients with cirrhosis and COVID-19. J. Hepatol. 2020;73:1063–1071. doi: 10.1016/j.jhep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Singh S, Khan A. Clinical characteristics and outcomes of coronavirus disease 2019 among patients with preexisting liver disease in the United States: a multicenter research network study. Gastroenterology. 2020;159:768–771. doi: 10.1053/j.gastro.2020.04.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Qi X, et al. Clinical course and risk factors for mortality of COVID-19 patients with pre-existing cirrhosis: a multicentre cohort study. Gut. 2021;70:433–436. doi: 10.1136/gutjnl-2020-321666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Wang M, et al. Clinical characteristics and risk factors of liver injury in COVID-19: a retrospective cohort study from Wuhan, China. Hepatol. Int. 2020;14:723–732. doi: 10.1007/s12072-020-10075-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Yang L, et al. Creg in hepatocytes ameliorates liver ischemia/reperfusion injury in a TAK1-dependent manner in mice. Hepatology. 2019;69:294–313. doi: 10.1002/hep.30203. [DOI] [PubMed] [Google Scholar]
- 289.Puelles VG, et al. Multiorgan and renal tropism of SARS-CoV-2. N. Engl. J. Med. 2020;383:590–592. doi: 10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Guan, G. W. et al. Exploring the mechanism of liver enzyme abnormalities in patients with novel coronavirus-infected pneumonia. Zhonghua Gan Zang Bing Za Zhi28, 100–106 (2020). [DOI] [PubMed]
- 291.Wang Y, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J. Hepatol. 2020;73:807–816. doi: 10.1016/j.jhep.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Wu J, Song S, Cao HC, Li LJ. Liver diseases in COVID-19: etiology, treatment and prognosis. World J. Gastroenterol. 2020;26:2286–2293. doi: 10.3748/wjg.v26.i19.2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Yoon E, Babar A, Choudhary M, Kutner M, Pyrsopoulos N. Acetaminophen-induced hepatotoxicity: a comprehensive update. J. Clin. Transl. Hepatol. 2016;4:131–142. doi: 10.14218/JCTH.2015.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Cao B, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N. Engl. J. Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Yao N, et al. Clinical characteristics and influencing factors of patients with novel coronavirus pneumonia combined with liver injury in Shaanxi region. Zhonghua Gan Zang Bing. Za Zhi. 2020;28:234–239. doi: 10.3760/cma.j.cn501113-20200226-00070. [DOI] [PubMed] [Google Scholar]
- 296.Karadaş Ö, Öztürk B, Sonkaya AR. A prospective clinical study of detailed neurological manifestations in patients with COVID-19. Neurol. Sci. 2020;41:1991–1995. doi: 10.1007/s10072-020-04547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Shehata, G. A. et al. Neurological complications of COVID-19: underlying mechanisms and management. Int. J. Mol. Sci. 22, 4081 (2021). [DOI] [PMC free article] [PubMed]
- 298.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Zhang WR, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Arpaci I, Karatas K, Baloglu M. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S) Pers. Individ Dif. 2020;164:110108. doi: 10.1016/j.paid.2020.110108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. J. Am. Med. Assoc. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Sun L, et al. Prevalence and risk factors for acute posttraumatic stress disorder during the COVID-19 outbreak. J. Affect Disord. 2021;283:123–129. doi: 10.1016/j.jad.2021.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Mazza MG, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Tiet, M. Y. & AlShaikh, N. Guillain-Barré syndrome associated with COVID-19 infection: a case from the UK. BMJ Case Rep.13, e236536 (2020). [DOI] [PMC free article] [PubMed]
- 305.Padroni, M. et al. Guillain-Barré syndrome following COVID-19: new infection, old complication? J. Neurol.267, 1877–1879 (2020). [DOI] [PMC free article] [PubMed]
- 306.Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19:383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Sedaghat Z, Karimi N. Guillain Barre syndrome associated with COVID-19 infection: a case report. J. Clin. Neurosci. 2020;76:233–235. doi: 10.1016/j.jocn.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Gutiérrez-Ortiz C, et al. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020;95:e601–e605. doi: 10.1212/WNL.0000000000009619. [DOI] [PubMed] [Google Scholar]
- 309.Pergolizzi, J. V., Jr. et al. Potential neurological manifestations of COVID-19: a narrative review. Postgrad. Med. 1–11 (2021). [DOI] [PMC free article] [PubMed]
- 310.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Lai J, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Li W, et al. Progression of mental health services during the COVID-19 outbreak in China. Int. J. Biol. Sci. 2020;16:1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J. Virol. 2008;82:7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Chen R, et al. The spatial and cell-type distribution of SARS-CoV-2 receptor ACE2 in the human and mouse brains. Front. Neurol. 2020;11:573095. doi: 10.3389/fneur.2020.573095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Montalvan V, Lee J, Bueso T, De Toledo J, Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin. Neurol. Neurosurg. 2020;194:105921. doi: 10.1016/j.clineuro.2020.105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Li K, et al. Middle East respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J. Infect. Dis. 2016;213:712–722. doi: 10.1093/infdis/jiv499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Lochhead JJ, Thorne RG. Intranasal delivery of biologics to the central nervous system. Adv. Drug Deliv. Rev. 2012;64:614–628. doi: 10.1016/j.addr.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 318.Lochhead JJ, Kellohen KL, Ronaldson PT, Davis TP. Distribution of insulin in trigeminal nerve and brain after intranasal administration. Sci. Rep. 2019;9:2621. doi: 10.1038/s41598-019-39191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem. Neurosci. 2020;11:995–998. doi: 10.1021/acschemneuro.0c00122. [DOI] [PubMed] [Google Scholar]
- 320.Li Z, et al. Neurological manifestations of patients with COVID-19: potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain. Front. Med. 2020;14:533–541. doi: 10.1007/s11684-020-0786-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Hickey WF, Hsu BL, Kimura H. T-lymphocyte entry into the central nervous system. J. Neurosci. Res. 1991;28:254–260. doi: 10.1002/jnr.490280213. [DOI] [PubMed] [Google Scholar]
- 322.Schwartz M, Deczkowska A. Neurological disease as a failure of brain-immune crosstalk: the multiple faces of neuroinflammation. Trends Immunol. 2016;37:668–679. doi: 10.1016/j.it.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 323.Ely EW, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. J. Am. Med. Assoc. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 324.Ren C, Yao RQ, Zhang H, Feng YW, Yao YM. Sepsis-associated encephalopathy: a vicious cycle of immunosuppression. J. Neuroinflammation. 2020;17:14. doi: 10.1186/s12974-020-1701-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Verkhratsky A, Zorec R, Parpura V. Stratification of astrocytes in healthy and diseased brain. Brain Pathol. 2017;27:629–644. doi: 10.1111/bpa.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Sierra A, et al. Surveillance, phagocytosis, and inflammation: how never-resting microglia influence adult hippocampal neurogenesis. Neural Plast. 2014;2014:610343. doi: 10.1155/2014/610343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Goodall S, Twomey R, Amann M. Acute and chronic hypoxia: implications for cerebral function and exercise tolerance. Fatigue. 2014;2:73–92. doi: 10.1080/21641846.2014.909963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Zhao, M. et al. Oxidative stress in hypoxic-ischemic encephalopathy: molecular mechanisms and therapeutic strategies. Int. J. Mol. Sci. 17, 2078 (2016). [DOI] [PMC free article] [PubMed]
- 329.Taylor CT, Doherty G, Fallon PG, Cummins EP. Hypoxia-dependent regulation of inflammatory pathways in immune cells. J. Clin. Investig. 2016;126:3716–3724. doi: 10.1172/JCI84433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Beyrouti R, et al. Characteristics of ischaemic stroke associated with COVID-19. J. Neurol. Neurosurg. Psychiatry. 2020;91:889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Oxley TJ, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N. Engl. J. Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Fox SE, et al. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir. Med. 2020;8:681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Middeldorp S, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J. Thromb. Haemost. 2020;18:1995–2002. doi: 10.1111/jth.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Poissy J, et al. Pulmonary embolism in patients with COVID-19: awareness of an increased prevalence. Circulation. 2020;142:184–186. doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 335.Marques-Deak A, Cizza G, Sternberg E. Brain-immune interactions and disease susceptibility. Mol. Psychiatry. 2005;10:239–250. doi: 10.1038/sj.mp.4001643. [DOI] [PubMed] [Google Scholar]
- 336.Guo Q, et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Kempuraj D, et al. COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation. Neuroscientist. 2020;26:402–414. doi: 10.1177/1073858420941476. [DOI] [PubMed] [Google Scholar]
- 338.Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch. Gen. Psychiatry. 2006;63:530–538. doi: 10.1001/archpsyc.63.5.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Gupta A, et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Team E. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi41, 145–151 (2020). [DOI] [PubMed]
- 341.Xu B, et al. Suppressed T cell-mediated immunity in patients with COVID-19: a clinical retrospective study in Wuhan, China. J. Infect. 2020;81:e51–e60. doi: 10.1016/j.jinf.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Feldman EL, et al. COVID-19 and diabetes: a collision and collusion of two diseases. Diabetes. 2020;69:2549–2565. doi: 10.2337/dbi20-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Singh AK, et al. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes. Metab. 2020;22:1915–1924. doi: 10.1111/dom.14124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Caballero AE, et al. COVID-19 in people living with diabetes: an international consensus. J. Diabetes Complications. 2020;34:107671. doi: 10.1016/j.jdiacomp.2020.107671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. J. Am. Med. Assoc. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 346.Barron E, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8:813–822. doi: 10.1016/S2213-8587(20)30272-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Murphy HR. Managing Diabetes In Pregnancy Before, During, And After COVID-19. Diabetes Technol. Ther. 2020;22:454–461. doi: 10.1089/dia.2020.0223. [DOI] [PubMed] [Google Scholar]
- 348.Kim NY, Ha E, Moon JS, Lee YH, Choi EY. Acute hyperglycemic crises with coronavirus disease-19: case reports. Diabetes Metab. J. 2020;44:349–353. doi: 10.4093/dmj.2020.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Stevens JS, et al. Diabetic ketoacidosis and mortality in COVID-19 infection. Diabetes Metab. 2021;47:101267. doi: 10.1016/j.diabet.2021.101267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Lui DTW, et al. Thyroid dysfunction in relation to immune profile, disease status, and outcome in 191 patients with COVID-19. J. Clin. Endocrinol. Metab. 2021;106:e926–e935. doi: 10.1210/clinem/dgaa813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Chen M, Zhou W, Xu W. Thyroid function analysis in 50 patients with COVID-19: a retrospective study. Thyroid. 2021;31:8–11. doi: 10.1089/thy.2020.0363. [DOI] [PubMed] [Google Scholar]
- 352.Gao W, et al. Thyroid hormone concentrations in severely or critically ill patients with COVID-19. J. Endocrinol. Investig. 2021;44:1031–1040. doi: 10.1007/s40618-020-01460-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Rothberger GD, et al. Low free T(3) is associated with worse outcomes in patients in the ICU requiring invasive mechanical ventilation. J. Intensive Care Med. 2021;36:313–318. doi: 10.1177/0885066619890822. [DOI] [PubMed] [Google Scholar]
- 354.Wu CT, et al. SARS-CoV-2 infects human pancreatic beta cells and elicits beta cell impairment. Cell Metab. 2021;33:1565–1576. doi: 10.1016/j.cmet.2021.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Hayden, M. R. An immediate and long-term complication of COVID-19 may be type 2 diabetes mellitus: the central role of β-cell dysfunction, apoptosis and exploration of possible mechanisms. Cells9, 2475 (2020). [DOI] [PMC free article] [PubMed]
- 356.Speer G, Somogyi P. Thyroid complications of SARS and coronavirus disease 2019 (COVID-19) Endocr. J. 2021;68:129–136. doi: 10.1507/endocrj.EJ20-0443. [DOI] [PubMed] [Google Scholar]
- 357.Mehta P, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Hou H, et al. Using IL-2R/lymphocytes for predicting the clinical progression of patients with COVID-19. Clin. Exp. Immunol. 2020;201:76–84. doi: 10.1111/cei.13450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Ruscitti P, Berardicurti O, Iagnocco A, Giacomelli R. Cytokine storm syndrome in severe COVID-19. Autoimmun. Rev. 2020;19:102562. doi: 10.1016/j.autrev.2020.102562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Liu R, et al. Decreased T cell populations contribute to the increased severity of COVID-19. Clin. Chim. Acta. 2020;508:110–114. doi: 10.1016/j.cca.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Lisco G, et al. Hypothesized mechanisms explaining poor prognosis in type 2 diabetes patients with COVID-19: a review. Endocrine. 2020;70:441–453. doi: 10.1007/s12020-020-02444-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Kim JH, et al. Relationship between natural killer cell activity and glucose control in patients with type 2 diabetes and prediabetes. J. Diabetes Investig. 2019;10:1223–1228. doi: 10.1111/jdi.13002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Ling PR, Smith RJ, Bistrian BR. Acute effects of hyperglycemia and hyperinsulinemia on hepatic oxidative stress and the systemic inflammatory response in rats. Crit. Care Med. 2007;35:555–560. doi: 10.1097/01.CCM.0000253310.02180.C2. [DOI] [PubMed] [Google Scholar]
- 364.Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can. J. Cardiol. 2018;34:575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Codo AC, et al. Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/glycolysis-dependent axis. Cell Metab. 2020;32:437–446. doi: 10.1016/j.cmet.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Han M, et al. Immunological characteristics in type 2 diabetes mellitus among COVID-19 patients. Front. Endocrinol. 2021;12:596518. doi: 10.3389/fendo.2021.596518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Langford BJ, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J. Infect. 2020;81:266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Lai CC, Wang CY, Hsueh PR. Co-infections among patients with COVID-19: the need for combination therapy with non-anti-SARS-CoV-2 agents? J. Microbiol. Immunol. Infect. 2020;53:505–512. doi: 10.1016/j.jmii.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Yang X, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Koehler P, et al. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020;63:528–534. doi: 10.1111/myc.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Pemán J, et al. Fungal co-infection in COVID-19 patients: should we be concerned? Rev. Iberoam. Micol. 2020;37:41–46. doi: 10.1016/j.riam.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Tadolini, M. et al. Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases. Eur. Respir. J.56, 2001398. 10.1183/13993003.01398-2020 (2020). [DOI] [PMC free article] [PubMed]
- 375.Stochino, C. et al. Clinical characteristics of COVID-19 and active tuberculosis co-infection in an Italian reference hospital. Eur. Respir. J. 56, 2001708 (2020). [DOI] [PMC free article] [PubMed]
- 376.Ritchie AI, Singanayagam A. Immunosuppression for hyperinflammation in COVID-19: a double-edged sword? Lancet. 2020;395:1111. doi: 10.1016/S0140-6736(20)30691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Tian S, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod. Pathol. 2020;33:1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Nasir N, Rehman F, Omair SF. Risk factors for bacterial infections in patients with moderate to severe COVID-19: a case-control study. J. Med Virol. 2021;93:4564–4569. doi: 10.1002/jmv.27000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Chen YY, Yen YF, Huang LY, Chou P. Manifestations and virus detection in the ocular surface of adult COVID-19 patients: a meta-analysis. J. Ophthalmol. 2021;2021:9997631. doi: 10.1155/2021/9997631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Almazroa, A. et al. Ocular transmission and manifestation for coronavirus disease: a systematic review. Int. Health ihab028 (2021). [DOI] [PMC free article] [PubMed]
- 381.Zhou L, et al. ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. Ocul. Surf. 2020;18:537–544. doi: 10.1016/j.jtos.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Eriksen AZ, Møller R, Makovoz B, Uhl SA, tenOever BR, Blenkinsop TA. SARS-CoV-2 infects human adult donor eyes and hESC-derived ocular epithelium. Cell Stem Cell28, 1205–1220.e7 (2021). [DOI] [PMC free article] [PubMed]
- 383.Hoang MP, et al. Olfactory and gustatory dysfunctions in COVID-19 patients: a systematic review and meta-analysis. Asian Pac. J. Allergy Immunol. 2020;38:162–169. doi: 10.12932/AP-210520-0853. [DOI] [PubMed] [Google Scholar]
- 384.Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R. Smell and taste dysfunction in patients with COVID-19: a systematic review and meta-analysis. Mayo Clin. Proc. 2020;95:1621–1631. doi: 10.1016/j.mayocp.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Lechien JR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur. Arch. Otorhinolaryngol. 2020;277:2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Gupta V, et al. Olfactory and gustatory dysfunction in COVID-19 patients from Northern India: a cross-sectional observational study. Indian J. Otolaryngol. Head. Neck Surg. 2021;73:1–8. doi: 10.1007/s12070-021-02391-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Butowt R, Bilinska K. SARS-CoV-2: olfaction, brain infection, and the urgent need for clinical samples allowing earlier virus detection. ACS Chem. Neurosci. 2020;11:1200–1203. doi: 10.1021/acschemneuro.0c00172. [DOI] [PubMed] [Google Scholar]
- 388.Kanjanaumporn J, Aeumjaturapat S, Snidvongs K, Seresirikachorn K, Chusakul S. Smell and taste dysfunction in patients with SARS-CoV-2 infection: a review of epidemiology, pathogenesis, prognosis, and treatment options. Asian Pac. J. Allergy Immunol. 2020;38:69–77. doi: 10.12932/AP-030520-0826. [DOI] [PubMed] [Google Scholar]
- 389.Kaya G, Kaya A, Saurat JH. Clinical and histopathological features and potential pathological mechanisms of skin lesions in COVID-19: review of the literature. Dermatopathology. 2020;7:3–16. doi: 10.3390/dermatopathology7010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Gottlieb M, Long B. Dermatologic manifestations and complications of COVID-19. Am. J. Emerg. Med. 2020;38:1715–1721. doi: 10.1016/j.ajem.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Suchonwanit P, Leerunyakul K, Kositkuljorn C. Cutaneous manifestations in COVID-19: lessons learned from current evidence. J. Am. Acad. Dermatol. 2020;83:e57–e60. doi: 10.1016/j.jaad.2020.04.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Magro C, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Abdel-Moneim A. COVID-19 pandemic and male fertility: clinical manifestations and pathogenic mechanisms. Biochemistry. 2021;86:389–396. doi: 10.1134/S0006297921040015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Ruan Y, et al. No detection of SARS-CoV-2 from urine, expressed prostatic secretions, and semen in 74 recovered COVID-19 male patients: a perspective and urogenital evaluation. Andrology. 2021;9:99–106. doi: 10.1111/andr.12939. [DOI] [PubMed] [Google Scholar]
- 395.Yang M, et al. Pathological findings in the testes of COVID-19 patients: clinical implications. Eur. Urol. Focus. 2020;6:1124–1129. doi: 10.1016/j.euf.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Wang, Z. & Xu, X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, leydig and sertoli cells. Cells9, 920 (2020). [DOI] [PMC free article] [PubMed]
- 397.Roychoudhury S, et al. Viral pathogenesis of SARS-CoV-2 infection and male reproductive health. Open Biol. 2021;11:200347. doi: 10.1098/rsob.200347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Mehan A, Venkatesh A, Girish M. COVID-19 in pregnancy: risk of adverse neonatal outcomes. J. Med Virol. 2020;92:2295–2297. doi: 10.1002/jmv.25959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Zeng H, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. J. Am. Med. Assoc. 2020;323:1848–1849. doi: 10.1001/jama.2020.4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Ropa J, Cooper S, Capitano ML, Van’t Hof W, Broxmeyer HE. Human hematopoietic stem, progenitor, and immune cells respond ex vivo to SARS-CoV-2 spike protein. Stem Cell Rev. Rep. 2021;17:253–265. doi: 10.1007/s12015-020-10056-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Ratajczak MZ, et al. SARS-CoV-2 entry receptor ACE2 is expressed on very small CD45(−) precursors of hematopoietic and endothelial cells and in response to virus spike protein activates the Nlrp3 inflammasome. Stem Cell Rev. Rep. 2021;17:266–277. doi: 10.1007/s12015-020-10010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Reyes, M. et al. Plasma from patients with bacterial sepsis or severe COVID-19 induces suppressive myeloid cell production from hematopoietic progenitors in vitro. Sci. Transl. Med. 13, eabe9599 (2021). [DOI] [PMC free article] [PubMed]
- 403.Huerga Encabo H, et al. Human erythroid progenitors are directly infected by SARS-CoV-2: implications for emerging erythropoiesis in severe COVID-19 patients. Stem Cell Rep. 2021;16:428–436. doi: 10.1016/j.stemcr.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Bernardes JP, et al. Longitudinal multi-omics analyses identify responses of megakaryocytes, erythroid cells, and plasmablasts as hallmarks of severe COVID-19. Immunity. 2020;53:1296–1314. doi: 10.1016/j.immuni.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Wilk, A. J. et al. Multi-omic profiling reveals widespread dysregulation of innate immunity and hematopoiesis in COVID-19. J. Exp. Med. 218, e20210582 (2021). [DOI] [PMC free article] [PubMed]
- 406.Group RC, et al. Dexamethasone in hospitalized patients with Covid-19. N. Engl. J. Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Gianfrancesco M, et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann. Rheum. Dis. 2020;79:859–866. doi: 10.1136/annrheumdis-2020-217871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Brenner EJ, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology. 2020;159:481–491. doi: 10.1053/j.gastro.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Zhao H, Davies R, Ma D. Potential therapeutic value of dexmedetomidine in COVID-19 patients admitted to ICU. Br. J. Anaesth. 2021;126:e33–e35. doi: 10.1016/j.bja.2020.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Richardson P, et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395:e30–e31. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Lu D, et al. MicroRNAs targeting the SARS-CoV-2 entry receptor ACE2 in cardiomyocytes. J. Mol. Cell Cardiol. 2020;148:46–49. doi: 10.1016/j.yjmcc.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Holshue ML, et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Martinez, M. A. Compounds with therapeutic potential against novel respiratory 2019 coronavirus. Antimicrob Agents Chemother64, e00399-20 (2020). [DOI] [PMC free article] [PubMed]
- 414.Choudhary S, Silakari O. Scaffold morphing of arbidol (umifenovir) in search of multi-targeting therapy halting the interaction of SARS-CoV-2 with ACE2 and other proteases involved in COVID-19. Virus Res. 2020;289:198146. doi: 10.1016/j.virusres.2020.198146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Liu F, et al. Patients of COVID-19 may benefit from sustained Lopinavir-combined regimen and the increase of Eosinophil may predict the outcome of COVID-19 progression. Int. J. Infect. Dis. 2020;95:183–191. doi: 10.1016/j.ijid.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Uno Y. Camostat mesilate therapy for COVID-19. Intern Emerg. Med. 2020;15:1577–1578. doi: 10.1007/s11739-020-02345-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Hoffmann, M. et al. Nafamostat mesylate blocks activation of SARS-CoV-2: new treatment option for COVID-19. Antimicrob Agents Chemother64, e00754-20 (2020). [DOI] [PMC free article] [PubMed]
- 418.Liu J, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Group RC, et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N. Engl. J. Med. 2020;383:2030–2040. doi: 10.1056/NEJMoa2022926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Consortium, WHOST. Repurposed antiviral drugs for Covid-19—interim WHO solidarity trial results. N. Engl. J. Med. 384, 497–511 (2021). [DOI] [PMC free article] [PubMed]
- 421.Wu C, et al. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm. Sin. B. 2020;10:766–788. doi: 10.1016/j.apsb.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Morse JS, Lalonde T, Xu S, Liu WR. Learning from the past: possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. Chembiochem. 2020;21:730–738. doi: 10.1002/cbic.202000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Wang Y, Anirudhan V, Du R, Cui Q, Rong L. RNA-dependent RNA polymerase of SARS-CoV-2 as a therapeutic target. J. Med. Virol. 2021;93:300–310. doi: 10.1002/jmv.26264. [DOI] [PubMed] [Google Scholar]
- 424.Ilaria Vicenti MZ, Saladini F. SARS-CoV-2 RNA-dependent RNA polymerase as a therapeutic target for COVID-19. Expert Opin. Ther. Pat. 2021;31:325–337. doi: 10.1080/13543776.2021.1880568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Beigel JH, et al. Remdesivir for the treatment of Covid-19—final report. N. Engl. J. Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Ader, F. et al. Remdesivir plus standard of care versus standard of care alone for the treatment of patients admitted to hospital with COVID-19 (DisCoVeRy): a phase 3, randomised, controlled, open-label trial. Lancet Infect. Dis.22, 209–221 (2022). [DOI] [PMC free article] [PubMed]
- 427.Gordon CJ, Tchesnokov EP, Feng JY, Porter DP, Gotte M. The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus. J. Biol. Chem. 2020;295:4773–4779. doi: 10.1074/jbc.AC120.013056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Cox RM, Wolf JD, Plemper RK. Therapeutically administered ribonucleoside analogue MK-4482/EIDD-2801 blocks SARS-CoV-2 transmission in ferrets. Nat. Microbiol. 2021;6:11–18. doi: 10.1038/s41564-020-00835-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Dampalla, C. S. et al. Postinfection treatment with a protease inhibitor increases survival of mice with a fatal SARS-CoV-2 infection. Proc. Natl Acad. Sci. USA118, e2101555118 (2021). [DOI] [PMC free article] [PubMed]
- 430.Kang CK, et al. In vitro activity of lopinavir/ritonavir and hydroxychloroquine against severe acute respiratory syndrome coronavirus 2 at concentrations achievable by usual doses. Korean J. Intern Med. 2020;35:782–787. doi: 10.3904/kjim.2020.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Griffin, S. Covid-19: lopinavir-ritonavir does not benefit hospitalised patients, UK trial finds. BMJ370, m2650, 10.1136/bmj.m2650 (2020). [DOI] [PubMed]
- 432.Thoms M, et al. Structural basis for translational shutdown and immune evasion by the Nsp1 protein of SARS-CoV-2. Science. 2020;369:1249–1255. doi: 10.1126/science.abc8665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Rona, G. et al. The NSP14/NSP10 RNA repair complex as a Pan-coronavirus therapeutic target. Cell Death Differ.29, 285–292 (2022). [DOI] [PMC free article] [PubMed]
- 434.Shang J, Smith MR, Anmangandla A, Lin H. NAD+-consuming enzymes in immune defense against viral infection. Biochem J. 2021;478:4071–4092. doi: 10.1042/BCJ20210181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Raymonda MH, et al. Pharmacologic profiling reveals lapatinib as a novel antiviral against SARS-CoV-2 in vitro. Virology. 2022;566:60–68. doi: 10.1016/j.virol.2021.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Roshanravan N, Seif F, Ostadrahimi A, Pouraghaei M, Ghaffari S. Targeting cytokine storm to manage patients with COVID-19: a mini-review. Arch. Med. Res. 2020;51:608–612. doi: 10.1016/j.arcmed.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Perrone F, et al. Tocilizumab for patients with COVID-19 pneumonia. The single-arm TOCIVID-19 prospective trial. J. Transl. Med. 2020;18:405. doi: 10.1186/s12967-020-02573-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Group RC. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397:1637–1645. doi: 10.1016/S0140-6736(21)00676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Veiga VC, et al. Effect of tocilizumab on clinical outcomes at 15 days in patients with severe or critical coronavirus disease 2019: randomised controlled trial. BMJ. 2021;372:n84. doi: 10.1136/bmj.n84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Lescure FX, et al. Sarilumab in patients admitted to hospital with severe or critical COVID-19: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 2021;9:522–532. doi: 10.1016/S2213-2600(21)00099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Lopez-Collazo E, Avendano-Ortiz J, Martin-Quiros A, Aguirre LA. Immune response and COVID-19: a mirror image of sepsis. Int. J. Biol. Sci. 2020;16:2479–2489. doi: 10.7150/ijbs.48400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Xiong Y, et al. Transcriptomic characteristics of bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerg. Microbes Infect. 2020;9:761–770. doi: 10.1080/22221751.2020.1747363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Khadke S, et al. Harnessing the immune system to overcome cytokine storm and reduce viral load in COVID-19: a review of the phases of illness and therapeutic agents. Virol. J. 2020;17:154. doi: 10.1186/s12985-020-01415-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Wang F, et al. Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia. J. Infect. Dis. 2020;221:1762–1769. doi: 10.1093/infdis/jiaa150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Varchetta S, et al. Unique immunological profile in patients with COVID-19. Cell Mol. Immunol. 2021;18:604–612. doi: 10.1038/s41423-020-00557-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Wang X, Gui J. Cell-mediated immunity to SARS-CoV-2. Pediatr. Investig. 2020;4:281–291. doi: 10.1002/ped4.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Kellici TF, Pilka ES, Bodkin MJ. Therapeutic potential of targeting plasminogen activator inhibitor-1 in COVID-19. Trends Pharm. Sci. 2021;42:431–433. doi: 10.1016/j.tips.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Diurno F, et al. Eculizumab treatment in patients with COVID-19: preliminary results from real life ASL Napoli 2 Nord experience. Eur. Rev. Med Pharm. Sci. 2020;24:4040–4047. doi: 10.26355/eurrev_202004_20875. [DOI] [PubMed] [Google Scholar]
- 449.Shi, H. et al. Endothelium-protective, histone-neutralizing properties of the polyanionic agent defibrotide. JCI Insight6, 17 (2021). [DOI] [PMC free article] [PubMed]
- 450.Pang J, et al. Efficacy and tolerability of bevacizumab in patients with severe Covid-19. Nat. Commun. 2021;12:814. doi: 10.1038/s41467-021-21085-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Zacharowski, K. & Studiengruppe, F. C. FX06-COVID: improvement of arterial oxygenation in intensive care patients with a severe course of COVID-19. Anaesthesist70, 71–72 (2021). [DOI] [PMC free article] [PubMed]
- 452.Terpos E, et al. Hematological findings and complications of COVID-19. Am. J. Hematol. 2020;95:834–847. doi: 10.1002/ajh.25829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Lavinio A, et al. Safety profile of enhanced thromboprophylaxis strategies for critically ill COVID-19 patients during the first wave of the pandemic: observational report from 28 European intensive care units. Crit. Care. 2021;25:155. doi: 10.1186/s13054-021-03543-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Flam B, Wintzell V, Ludvigsson JF, Mårtensson J, Pasternak B. Direct oral anticoagulant use and risk of severe COVID-19. J. Intern. Med. 2021;289:411–419. doi: 10.1111/joim.13205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Sadeghipour P, et al. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION Randomized Clinical Trial. J. Am. Med. Assoc. 2021;325:1620–1630. doi: 10.1001/jama.2021.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Flumignan RL, et al. Prophylactic anticoagulants for people hospitalised with COVID-19. Cochrane Database Syst. Rev. 2020;10:Cd013739. doi: 10.1002/14651858.CD013739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Nadkarni GN, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J. Am. Coll. Cardiol. 2020;76:1815–1826. doi: 10.1016/j.jacc.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Lopes RD, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet. 2021;397:2253–2263. doi: 10.1016/S0140-6736(21)01203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Perepu US, et al. Standard prophylactic versus intermediate dose enoxaparin in adults with severe COVID-19: a multi-center, open-label, randomized controlled trial. J. Thromb. Haemost. 2021;19:2225–2234. doi: 10.1111/jth.15450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Escalard S, et al. Treatment of acute ischemic stroke due to large vessel occlusion with COVID-19: experience from Paris. Stroke. 2020;51:2540–2543. doi: 10.1161/STROKEAHA.120.030574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Balbi C, et al. Circulating extracellular vesicles are endowed with enhanced procoagulant activity in SARS-CoV-2 infection. EBioMedicine. 2021;67:103369. doi: 10.1016/j.ebiom.2021.103369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Zhang Y, et al. Carboxypeptidase B blocks ex vivo activation of the anaphylatoxin-neutrophil extracellular trap axis in neutrophils from COVID-19 patients. Crit. Care. 2021;25:51. doi: 10.1186/s13054-021-03482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Bachler M, et al. Impaired fibrinolysis in critically ill COVID-19 patients. Br. J. Anaesth. 2021;126:590–598. doi: 10.1016/j.bja.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Heinz C, et al. Greater fibrinolysis resistance but no greater platelet aggregation in critically ill COVID-19 patients. Anesthesiology. 2021;134:457–467. doi: 10.1097/ALN.0000000000003685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Kruse JM, et al. Thromboembolic complications in critically ill COVID-19 patients are associated with impaired fibrinolysis. Crit. Care. 2020;24:676. doi: 10.1186/s13054-020-03401-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.Rysz S, et al. COVID-19 pathophysiology may be driven by an imbalance in the renin-angiotensin-aldosterone system. Nat. Commun. 2021;12:2417. doi: 10.1038/s41467-021-22713-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Tiwari R, et al. In silico and in vitro studies reveal complement system drives coagulation cascade in SARS-CoV-2 pathogenesis. Comput Struct. Biotechnol. J. 2020;18:3734–3744. doi: 10.1016/j.csbj.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.de Nooijer AH, et al. Complement activation in the disease course of coronavirus disease 2019 and its effects on clinical outcomes. J. Infect. Dis. 2021;223:214–224. doi: 10.1093/infdis/jiaa646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Jover, E. et al. Beneficial effects of mineralocorticoid receptor pathway blockade against endothelial inflammation induced by SARS-CoV-2 spike protein. Biomedicines9, 639 (2021). [DOI] [PMC free article] [PubMed]
- 470.Dofferhoff, A. S. M. et al. Reduced vitamin K status as a potentially modifiable risk factor of severe COVID-19. Clin. Infect. Dis.73, e4039–e4046 (2020). [DOI] [PMC free article] [PubMed]
- 471.Darwesh AM, Bassiouni W, Sosnowski DK, Seubert JM. Can N-3 polyunsaturated fatty acids be considered a potential adjuvant therapy for COVID-19-associated cardiovascular complications? Pharm. Ther. 2021;219:107703. doi: 10.1016/j.pharmthera.2020.107703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Chiappalupi S, et al. Targeting RAGE to prevent SARS-CoV-2-mediated multiple organ failure: hypotheses and perspectives. Life Sci. 2021;272:119251. doi: 10.1016/j.lfs.2021.119251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Sagris, M. et al. Inflammatory mechanisms in COVID-19 and atherosclerosis: current pharmaceutical perspectives. Int. J. Mol. Sci. 22, 6607 (2021). [DOI] [PMC free article] [PubMed]
- 474.Wang SC, Wang YF. Cardiovascular protective properties of oxytocin against COVID-19. Life Sci. 2021;270:119130. doi: 10.1016/j.lfs.2021.119130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Solerte SB, et al. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study. Diabetes Care. 2020;43:2999–3006. doi: 10.2337/dc20-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Kawalec P, Mikrut A, Lopuch S. The safety of dipeptidyl peptidase-4 (DPP-4) inhibitors or sodium-glucose cotransporter 2 (SGLT-2) inhibitors added to metformin background therapy in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab. Res. Rev. 2014;30:269–283. doi: 10.1002/dmrr.2494. [DOI] [PubMed] [Google Scholar]
- 477.Dai L, Gao GF. Viral targets for vaccines against COVID-19. Nat. Rev. Immunol. 2021;21:73–82. doi: 10.1038/s41577-020-00480-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.World Health Organization. COVID-19 vaccine tracker and landscape. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (2021).
- 479.Korber B, Hraber P, Wagh K, Hahn BH. Polyvalent vaccine approaches to combat HIV-1 diversity. Immunol. Rev. 2017;275:230–244. doi: 10.1111/imr.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586:516–527. doi: 10.1038/s41586-020-2798-3. [DOI] [PubMed] [Google Scholar]
- 481.Wu, S. et al. Safety, tolerability, and immunogenicity of an aerosolised adenovirus type-5 vector-based COVID-19 vaccine (Ad5-nCoV) in adults: preliminary report of an open-label and randomised phase 1 clinical trial. Lancet Infect. Dis.21, 1654–1664 (2021). [DOI] [PMC free article] [PubMed]
- 482.Falsey AR, et al. SARS-CoV-2 neutralization with BNT162b2 vaccine dose 3. N. Engl. J. Med. 2021;385:1627–1629. doi: 10.1056/NEJMc2113468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Bar-On YM, et al. Protection of BNT162b2 vaccine booster against Covid-19 in Israel. N. Engl. J. Med. 2021;385:1393–1400. doi: 10.1056/NEJMoa2114255. [DOI] [PMC free article] [PubMed] [Google Scholar]