Abstract
Dental fear and anxiety (DFA) is common across the lifespan and represents a barrier to proper oral health behaviors and outcomes. The aim of this study is to present a conceptual model of the relationships between DFA, general anxiety/fear, sensory over-responsivity (SOR), and/or oral health behaviors and outcomes. Two rounds of literature searches were performed using the PubMed database. Included articles examined DFA, general anxiety/fear, SOR, catastrophizing, and/or oral health behaviors and outcomes in typically developing populations across the lifespan. The relationships between the constructs were recorded and organized into a conceptual model. A total of 188 articles were included. The results provided supporting evidence for relationships between DFA and all other constructs included in the model (general anxiety/fear, SOR, poor oral health, irregular dental attendance, dental behavior management problems [DBMP], and need for treatment with pharmacological methods). Additionally, SOR was associated with general anxiety/fear and DBMP; general anxiety/fear was linked to poor oral health, irregular attendance, and DBMP. This model provides a comprehensive view of the relationships between person factors (e.g., general anxiety/fear, SOR, and DFA) and oral health behaviors and outcomes. This is valuable in order to highlight connections between constructs that may be targeted in the development of new interventions to improve oral health behaviors and outcomes as well as the experience of DFA.
Keywords: dental anxiety, dental fear, oral health behaviors, general anxiety, sensory over-responsivity, dental behavior management problems
1. Introduction
Dental fear is defined as a negative reaction to specific threatening stimuli associated with dental treatment, whereas dental anxiety is an excessive or impairing negative emotional state experienced by dental patients [1,2]. These terms are often used interchangeably or even combined as a single term, dental fear and anxiety (DFA) [1,2], which has been linked to many negative oral health behaviors and outcomes (e.g., [3,4,5,6,7,8,9,10,11]). DFA is primarily associated with previous negative dental experiences and most often develops in childhood [12,13,14,15,16]; however, literature suggests that DFA is common across the lifespan. Pediatric prevalence estimates range from 5% to 42%, with most reports clustering around 20% [2,5,16,17,18]. Similarly, 11–32% of adults report experiencing DFA [16,19,20,21,22].
A number of reviews have focused on DFA, including examinations of prevalence [2,16,17,22,23,24], trajectory over the lifespan [16], DFA-specific assessments [1,25,26], and management techniques [16,24,27,28]. Likewise, much research has reported—with overall inconsistent findings—on the relationship between DFA and sociodemographic characteristics, including age, gender, education, race/ethnicity, geographic location, and culture [2,29,30,31,32,33,34,35,36]. However, less attention has been paid to the relationship between DFA and other person factors such as general anxiety/fear and over-responsivity to sensory stimuli. Similar to DFA, general anxiety/fear and sensory over-responsivity (SOR) have been linked to negative oral health behaviors and outcomes in typical and clinical populations (e.g., [37,38,39,40,41,42,43,44]). Therefore, the purpose of this paper is to synthesize the current literature in order to present a conceptual model of DFA, other person factors which have the potential to be targeted in future interventions (e.g., general anxiety/fear and sensory over-responsivity), and their associations with each other and oral health behaviors and outcomes.
2. Materials and Methods
2.1. Search Strategy
A literature search was performed in an iterative manner, using the PubMed database, with the aim of identifying articles that examined DFA, other person factors, and their relationship with oral health behaviors and outcomes. Initial search terms included: dental fear, dental anxiety, dental behavior, oral health, caries, sensory processing, sensory over-responsiv*, sensory sens*, and combinations of these terms. Based on abstract review, the relevant publications were selected and reviewed. Following the review of these articles, new search terms were incorporated, such as: general anxiety, anxiety, catastrophizing, sedation, general anesthesia, dental attendance, tooth decay, dental behavior management problems, and oral health-related quality of life. Reference lists from relevant literature (including systematic reviews and meta-analyses) were reviewed to identify additional articles. Related articles and “cited by” queries in PubMed and Google Scholar databases were also reviewed for all articles included.
2.2. Inclusion and Exclusion Criteria
Articles were included if they examined the relationship between person factors (e.g., DFA, SOR, general anxiety/fear, and catastrophizing) and oral health behaviors and outcomes across the lifespan and were published in English. Systematic reviews, meta-analyses, unpublished data, and studies purposively recruiting clinical populations were excluded. As this study aimed to examine person factors that influence oral health behaviors and outcomes that may be targeted in future interventions, other articles focusing on constructs such as age, gender, race/ethnicity, parental DFA, socioeconomic status, and dentist behavior were excluded.
2.3. Model Development
Following a review of articles from the initial search, several constructs related to DFA and/or SOR were identified by the authors (e.g., irregular attendance, oral health-related quality of life, and dental behavior management problems). In the second round of literature searches, articles examining these constructs and other person factors (general anxiety/fear and catastrophizing) were identified. Articles that met the inclusion criteria were reviewed and relationships between constructs recorded. In an iterative process, constructs were organized into a conceptual model to visually depict the associations between factors. As 97% of the included studies did not examine a causal link between constructs, lines were used in lieu of arrows so as not to infer relationship directionality (see Figure 1 for preliminary conceptual model). In the final model, lines were included only if three or more independent studies reported relationships between constructs (see Figure 2 for final conceptual model).
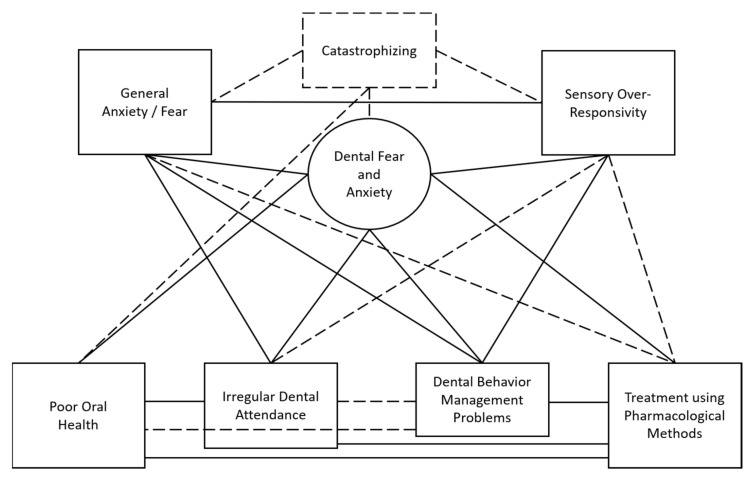
Figure 1.
Preliminary conceptual model. Note. Dashed lines indicate relationships with support from only two or fewer independent studies (e.g., did not meet required inclusion criteria for final model).
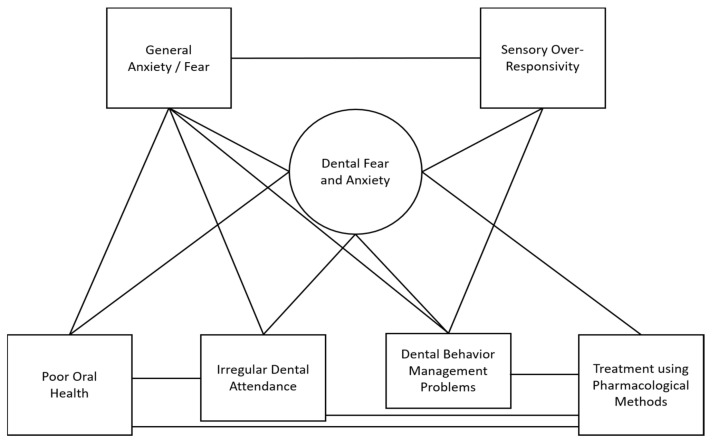
Figure 2.
Conceptual model of the relationships between dental fear and anxiety, general anxiety/fear, sensory over-responsivity, and oral health behaviors and outcomes.
3. Results
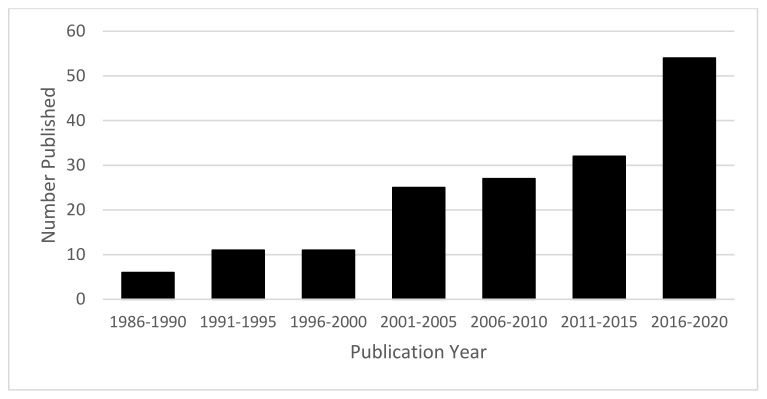
The final conceptual model is presented in Figure 2. A total of 188 studies were included, comprising 100 studies examining a pediatric population, 86 examining an adult population, and 2 examining a population across the lifespan. Studies were published from 1989 to 2021, with a trend towards greater interest in more recent years (see Figure 3). Primary authors were from a total of 34 different countries, most frequently from the United States (n = 30), followed by Brazil (n = 19), the United Kingdom (n = 17), Sweden (n = 16), Finland (n = 13), and India (n = 10).
Figure 3.
Number of articles included in conceptual model by year of publication. Note. Articles published in 2021 (n = 21) not included in figure.
3.1. Relationships between Person Factors
3.1.1. DFA: General Anxiety/Fear
Thirty articles examined the association between DFA and general anxiety/fear (n = 11 pediatric, n = 19 adult). The majority of both pediatric [43,45,46,47,48,49,50,51,52,53] and adult studies [29,39,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] reported a relationship between DFA and general anxiety/fear. Only one pediatric study [69] and two adult studies [13,70] found no significant association between general anxiety/fear and DFA.
3.1.2. DFA: Sensory Over-Responsivity
Ten articles reported a relationship between DFA and sensory sensitivities (n = 6 pediatric, n = 4 adult). From caregiver reports, child differences in sensory processing were found to be significantly associated with DFA [43]; in a study examining dental-anxiety-provoking stimuli, children reported being mildly to severely afraid of multiple sensory-related stimuli during dental care (e.g., tactile, olfactory, gustatory, visual, and vestibular) [71]. In four qualitative studies exploring factors contributing to children’s DFA, the resulting themes included sensory-related challenges triggered by tactile, visual, auditory, olfactory, and/or gustatory stimuli [72,73,74,75]. In a study of adolescents and young adults, sensory-related aspects of previous negative dental experiences (e.g., sight, smell, and sounds of dental treatment) were significantly associated with dental fear [76]. In adults, SOR was also linked to DFA [13,38,77], with two sensory-processing patterns related to over-responsivity (sensory sensitivity and sensation avoiding) significantly associated with high levels of DFA in a sample of female undergraduates [13], and the majority of dentally anxious adults participating in a qualitative interview study reporting that the sight and sound of dental equipment, the smell of the environment, and the vibration of the drill was distressing and increased DFA [38].
3.1.3. General Anxiety/Fear: Sensory Over-Responsivity
The relationship between SOR and general anxiety/fear was examined in eleven studies (n = 5 pediatric, n = 6 adult). SOR was significantly associated with higher levels of general anxiety/fear in children [43,78,79] as well as adults [13,80,81,82,83]. One study of preschool children found that 43% of those with SOR had a concurrent anxiety disorder, and that symptoms of SOR in preschool significantly predicted general anxiety symptoms at age six [84]. In another study, children with elevated SOR were four times more likely to have clinically relevant internalizing scores, including signs of anxiety [85]. In adults, two sensory processing patterns related to SOR (sensory sensitivity and sensation avoiding) were significantly correlated with increased state and trait anxiety [86].
3.2. Relationships between Oral Health Behaviors and Outcomes and Person Factors
3.2.1. Oral Health: DFA
Seventy-nine studies examined the relationship between DFA and oral health (n = 41 pediatric, n = 38 adult). A significant association was found between high DFA and poor oral health-related quality of life (OHRQoL), a multidimensional measure evaluating oral health status and its related functional and psychosocial impacts [87], in children [88,89,90,91,92] as well as adults [93,94,95,96,97,98,99,100,101,102]. Significant relationships were also reported between high levels of DFA and measures of poor oral health (e.g., caries experience, gingival health, and toothbrushing frequency) in children [3,5,6,7,17,50,51,53,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122] and adults [4,61,65,66,93,99,102,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142]. Nine pediatric studies [143,144,145,146,147,148,149,150,151] and three adult studies [56,63,151,152] found no significant associations between DFA and poor oral health or OHRQoL measures.
3.2.2. Oral Health: General Anxiety/Fear
Eight studies (n = 3 pediatric, n = 5 adult) examined the relationship between general anxiety/fear and oral health. Children with higher general anxiety/fear were significantly more likely to have caries [108] as well as significantly decreased toothbrushing frequency [153]. One study of adults reported that increased general anxiety/fear was significantly associated with worse OHRQoL [94]. The remaining four studies reported mixed results with various outcome measures. General anxiety/fear was significantly associated with: decayed, missing, and/or filled teeth (DMFT) [39,154]; self-perceived dental problems but not oral symptoms in the past 12 months [58]; and recurrent but not overall caries [150]. One study found no association between general anxiety and caries status [152].
3.2.3. Dental Attendance: DFA
The relationship between DFA and dental attendance was examined in 57 articles (n = 15 pediatric, n = 42 adult). The avoidance of or infrequent dental visits were linked with higher levels of DFA in children and adolescents [3,7,45,50,110,121,148,155,156,157,158,159] as well as adults [4,8,21,39,40,54,57,61,62,63,65,66,101,102,125,126,129,131,133,135,136,138,140,142,160,161,162,163,164,165,166,167,168,169,170,171,172,173]. Sporadic dental attendance as a child, compared to regular attendance, was associated with increased DFA in adulthood [174]. In a qualitative study interviewing dentally anxious adults, all participants expressed that they avoided going to the dentist (e.g., missed appointments, infrequent attendance, and several years of non-attendance), and some reported avoiding care despite the presence of acute pain [38]. Conversely, one study reported a significant relationship between greater child DFA and the likelihood of a dental visit in the past 12 months [175]. Only four studies found no association between DFA and attendance in children [113,119] or adults [134,176].
3.2.4. Dental Attendance: General Anxiety/Fear
The relationship between general anxiety/fear and dental attendance was examined in seven studies (n = 7 adult). Four studies reported a significant association between irregular attendance and increased general anxiety/fear [40,56,57,58], whereas three studies found no significant association [39,160,169].
3.2.5. Dental Behavior Management Problems: DFA
Twenty-eight articles explored the relationship between dental behavior management problems (DBMPs) and DFA (n = 26 pediatric, n = 2 adult). In children, DBMPs were found to be significantly associated with high DFA in both retrospective [41,50,177,178,179,180,181] and prospective studies [9,10,52,114,145,146,157,182,183,184,185,186,187,188,189,190,191]. One study found that over 75% of children with high DFA had a history of DBMP [192], and another reported that dentally anxious children were almost 2.5 times more likely to behave negatively during care [9]. One study found mixed results with a significant association between previous negative behavior and DFA, but no association between current negative behavior and DFA [180]. Only one study reported no association between negative behavior and DFA following adjustment for covariates (e.g., order of dental visits) [193].
The relationship between DFA and DBMPs was only examined in two studies with adult populations. In a sample of university employees, there was a significant correlation between the number of fear behaviors reported (e.g., grabbing the dentist’s hand, refusing treatment, crying) and increased DFA [61]. Additionally, one qualitative study reported that “a few [high DFA adult] participants…admitted being physically aggressive toward the dentist in the past” [38].
3.2.6. Dental Behavior Management Problems: General Anxiety/Fear
Five studies examined the relationship between general anxiety/fear and DBMP (n = 4 pediatric, n = 1 adult). In children, a history of DBMP was significantly associated with increased general anxiety/fear [9,41,50]. In a sample of dentally anxious adults, those with high trait anxiety were 2.4 times more likely to be difficult to treat (e.g., inability to open the mouth and cooperate with oral examination) [194]. Only one study reported no association between negative behavior during treatment and general anxiety/fear [52].
3.2.7. Dental Behavior Management Problems: Sensory Over-Responsivity
Four studies examined the association between sensory sensitivity and DBMPs (n = 3 pediatric, n = 1 adult). Children’s negative reactions to auditory, tactile, olfactory, and movement stimuli were significantly associated with a lack of cooperation during dental treatment [37,43]. Negative reactions to touch and noise were also associated with a need for behavior management strategies during previous treatment [37]. Based on survey results, significantly more parents of children with oral SOR reported that it was moderately–extremely difficult for the dentist to clean their child’s teeth, that the child’s uncooperative behaviors increased at the dentist, and that the dentist used restraint often or almost always during prophylaxis, compared to parents of children without oral SOR [195]. In addition, adults that were challenging to treat due to difficulties with behavioral cooperation were significantly more likely to report fearing dental-related smells, sounds, and tactile experiences [194].
3.2.8. Use of Pharmacological Interventions: DFA
Sixteen studies examined the relationship between DFA and the need for pharmacological intervention for dental treatments, including extractions, restorations, prophylaxis, and/or radiography (n = 9 pediatric, n = 5 adult, n = 2 lifespan). Five studies found that DFA was the first or second most commonly reported reason for the use of pharmacological methods to treat children [11,196,197,198,199]; six additional studies reported that increased dental fear in children was significantly associated with a history of treatment under general anesthesia and/or sedation [3,110,111,200,201,202]. In adults, DFA was the second most common reason for referral for treatment under general anesthesia [11], increased DFA was significantly associated with an increased likelihood of referral for sedation [8,203,204,205], and 85% of adults with high DFA reported that they were possibly or definitely interested in receiving future treatment with sedation or GA [161]. DFA was reported to be the most common reason for treatment under general anesthesia throughout the lifespan (3–66 years), irrespective of gender, except for males aged 12–17 years [199].
3.3. Relationships between Oral Health Behaviors and Outcomes
3.3.1. Oral Health: Dental Attendance
Eighteen articles examined the relationship between oral health and dental attendance (n = 4 pediatric, n = 14 adult). In children, irregular dental attendance was associated with DMFT [7,122,206] and poor OHRQoL [207]. In 13 studies of adults, irregular dental attendance was associated with poor oral health (e.g., DMFT and self-report of poor oral health) [8,56,66,96,100,125,135,160,167,169,171,208,209]. One study reported no significant association between dental attendance and change in OHRQoL over a 12-month period in adults [210].
3.3.2. Oral Health: Pharmacological Methods
The association between oral health and the need for pharmacological methods during treatment was examined in 12 articles (n = 7 pediatric, n = 3 adult, n = 2 lifespan). Poor oral health was reported as the first [196,197] and third [11] most common reason for treatment under general anesthesia for children and the second or third most common across the lifespan [11,199]. Children who had undergone treatment under general anesthesia had significantly more decayed, filled, and/or extracted teeth than those who had never undergone general anesthesia [110,202,211]. One study reported that approximately 11% of adult referrals for treatment under general anesthesia were due to an excessive need for treatment [11], and two studies of adults found that those who were treated with sedation had significantly worse oral health [203,204]. Two studies did not support the link between oral health status and the need for care using pharmacological methods [8,212], and one study found that oral health (DMFT score) increased the odds of choosing general anesthesia for restorative treatment, but not to a significant degree [200].
3.3.3. Dental Behavior Management Problems: Pharmacological Methods
The relationship between DBMPs and the use of pharmacological methods was explored in three studies (n = 2 pediatric, n = 1 lifespan). In one study, extreme non-cooperation was found to be the most common reason for a general anesthesia referral for both children and adults [11]. Uncooperative behaviors and severe management problems contributed to referrals for sedation in one study [213], whereas 63% of children with a history of DBMP reported undergoing treatment with sedation at one or more previous appointments [214].
3.3.4. Dental Attendance: Pharmacological Methods
The relationship between dental attendance and the use of pharmacological methods was examined in four studies (n = 1 pediatric, n = 3 adult). One study found that children who went to the dentist only when something was wrong were 2.5 times more likely to have undergone treatment using general anesthesia [202]. Adults with irregular attendance patterns were significantly more likely to be referred for treatment using sedation [8,203]. One article reported no significant association between attendance and the use of pharmacological methods in adults [204].
4. Discussion
This model provides a more comprehensive view of the relationship between person factors and oral health behaviors and outcomes than previously reported in the literature. For instance, our review found supporting evidence for relationships between DFA, general anxiety/fear, SOR, as well as multiple oral health behaviors and outcomes. The explicit linking of these constructs highlights connections that may be targeted in the development of new interventions to improve oral health behaviors and outcomes as well as the experience of DFA. Because only 3% of the studies examined causal links between constructs, more research is necessary to determine the directionality of these relationships and the precise impacts that these person factors may have on oral health behaviors and outcomes.
Additional relationships exist between the constructs included in our model; however, lines were included in our final model only when links were supported by a minimum of three independent studies (see Figure 1 for the model including relationships below the stated threshold). Fewer than three studies reported relationships between: SOR and pharmacological methods [37,195], general anxiety/fear and pharmacological methods [204], and SOR and irregular attendance [195]. Additionally, relationships between oral health behaviors and outcomes were reported below our minimum threshold, including: DBMP and poor oral health [179,215] and DBMP and irregular attendance [179]. Lastly, although this model focuses on DFA, general anxiety/fear, and SOR, there are other person factors, such as catastrophizing, which may also play a role in dental challenges. Catastrophizing refers to “an exaggerated negative orientation toward stressful or painful situations” [216] (p. 123) and has been associated with poor oral health in one study [88]. Interestingly, research has also reported relationships between catastrophizing and the other person factors reported here—SOR [217,218], general anxiety/fear [219], and DFA [38,73,88,139,155,216,220]. It is important to continue to examine the relationships between these constructs in future research.
Although the relationship between general anxiety/fear, DFA, and oral health behaviors and outcomes has previously been studied, the inclusion of SOR in the understanding and conceptualization of DFA and oral health outcomes and behaviors for neurotypical individuals represents a new addition to the literature. Historically, dental research examining SOR and oral health behaviors and outcomes has focused on clinical populations, including children with autism spectrum disorder, Down syndrome, and attention-deficit/hyperactivity disorder. In these groups, sensory sensitivities have been linked to dental-related challenges in the home and/or clinic environments [42,43,44,221,222,223,224,225,226,227,228,229,230,231,232,233], with the National Institute of Dental and Craniofacial Research [234] suggesting that minimizing sensory stimuli in the dental environment may support the reduction of uncooperative behaviors in children with autism spectrum disorder.
Many of the interventions designed to address DFA in children, such as modeling or distraction techniques, have limited evidence to support their use [15,28,235,236]. Research findings examining distraction and modeling techniques are mixed, with some studies reporting a decrease in DFA, whereas others found either mixed results or no difference (e.g., [237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254]). Tell–show–do, one of the most popular techniques utilized by dentists, likewise has little evidence to support its efficacy; however, it is widely accepted by children and parents, and there are no contraindications for its use [28]. In addition, many review articles note the lack of quality and certainty of the evidence of these intervention studies [28,255,256,257]. For individuals with extreme levels of DFA, psychological interventions (e.g., cognitive behavioral therapy, systematic desensitization, exposure therapy) have shown success in reducing DFA and increasing dental attendance [204,238,258,259,260,261,262,263,264,265,266,267]; however, dentists may encounter challenges utilizing and implementing these types of training- and time-intensive intervention techniques [238,268].
Sensory-based methods of stress and anxiety management have been proposed to decrease DFA in dental patients. For example, the “4S principle” aims to reduce four triggers of DFA in the environment: sights (e.g., needles and drills), sounds (e.g., drilling), sensations (e.g., vibrations), and smells (e.g., clinical odors) [269,270]; however, this intervention has not yet been studied. The utilization of other sensory-based interventions during dental care has been investigated, with most reporting preliminary success. For example, aromatherapy was found to have a calming effect for children during dental care and adults in the dental office waiting room [271,272,273,274,275]. Heart rate and physiological anxiety were reduced during dental treatments when using a weighted blanket for deep pressure sensations [276,277,278]. Lastly, a sensory adapted dental environment, designed to decrease noxious stimuli and increase calming stimuli, decreased physiological and behavioral distress in typically developing children and those with disabilities [44,279,280,281,282,283]; this intervention is now included in the American Academy of Pediatric Dentistry’s [284] list of best practices as a potential basic behavior guidance technique for use with dental patients with anxiety or special healthcare needs.
Given the high prevalence of both DFA and SOR in neurotypical individuals, a call for action in both practice and research is appropriate. For example, screening for DFA and SOR using simple pre-visit questionnaires [229] will provide additional information about patient experience, allowing the dentist to then approach treatment with greater knowledge and confidence as well as the option to implement strategies to improve care. Lastly, research is needed to examine the predictive contribution of DFA and SOR to oral health behaviors and outcomes, as well as the rigorous examination of interventions designed to target these constructs in efforts to improve care for those with DFA and/or SOR.
Although this model highlights important factors which should be considered in the discussion surrounding DFA, several limitations should be noted. First, multiple challenges arose when synthesizing the included studies to develop our model, specifically regarding differences in construct naming, definition, and measurement. Multiple studies utilized the same assessment tool but referred to the outcome by different names. For example, the Children’s Fear Survey Schedule—Short Form (CFSS-SF) was stated to measure general anxiety in some studies (e.g., [49,50]) but general fear in others (e.g., [48]). Due to this challenge, we utilized the broader general anxiety/fear term in our model. In regard to construct measurement and definition, DFA was frequently assessed using many different tools (e.g., Children’s Fear Survey Schedule—Dental Subscale, Modified Child Dental Anxiety Scale, Dental Anxiety Question, and Dental Anxiety Survey); however, even in studies utilizing the same tool, there was often variability in the cut-off points for defining the presence/absence of DFA and/or the categorization of high versus low levels of fear (e.g., [94,148]). Second, a PRISMA flowchart was not created because the literature searches that informed the development of this review and model were conducted in an inductive and iterative manner. Lastly, the search strategy for this study included only one database; a systematic review and meta-analysis including multiple databases is a necessary next step to confirm the findings reported here.
5. Conclusions
This model contributes to the literature by including other person factors such as general anxiety/fear and sensory over-responsivity to the conversation surrounding DFA and oral health behaviors and outcomes. It is important to consider these factors as they may exacerbate the challenges experienced in the dental clinic, possibly in individuals both with and without comorbid DFA. In addition, knowledge regarding the association between DFA, these additional person factors, and oral health behaviors and outcomes have the potential to inform the development of more targeted interventions to improve care for this population.
Acknowledgments
At the time of the study, this author was at the T.H. Chan Division of Occupational Science & Occupational Therapy, Herman Ostrow School of Dentistry, University of Southern California, Los Angeles, CA 90089, USA.
Author Contributions
Conceptualization, L.I.S.D.; methodology, L.I.S.D. and M.G.; investigation, L.I.S.D., M.G., W.G., N.H. and J.C.P.; writing—original draft preparation, L.I.S.D. and M.G. writing—review and editing, L.I.S.D. and J.C.P.; visualization, L.I.S.D. and M.G.; supervision, L.I.S.D. and J.C.P.; project administration, L.I.S.D.; funding acquisition, L.I.S.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Center for Medical and Rehabilitation Research, Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD), grant number K12 HD055929, and the National Institute of Dental and Craniofacial Research (NIDCR), grant number U01 DE024978.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Armfield J.M. How do we measure dental fear and what are we measuring anyway? Oral Health Prev. Dent. 2010;8:107–115. [PubMed] [Google Scholar]
- 2.Cianetti S., Lombardo G., Lupatelli E., Pagano S., Abraha I., Montedori A., Caruso S., Gatto R., De Giorgio S. Dental fear/anxiety among children and adolescents. A systematic review. Eur. J. Paediatr. Dent. 2017;18:121–130. doi: 10.23804/ejpd.2017.18.02.07. [DOI] [PubMed] [Google Scholar]
- 3.Coxon J.D., Hosey M.T., Newton J.T. The oral health of dentally anxious five- and eight-year-olds: A secondary analysis of the 2013 Child Dental Health Survey. Br. Dent. J. 2019;226:503–507. doi: 10.1038/s41415-019-0148-3. [DOI] [PubMed] [Google Scholar]
- 4.Guentsch A., Stier C., Raschke G.F., Peisker A., Fahmy M.D., Kuepper H., Schueler I. Oral health and dental anxiety in a German practice-based sample. Clin. Oral Investig. 2017;21:1675–1680. doi: 10.1007/s00784-016-1951-8. [DOI] [PubMed] [Google Scholar]
- 5.Kakkar M., Wahi A., Thakkar R., Vohra I., Shukla A.K. Prevalence of dental anxiety in 10-14 years old children and its implications. J. Dent. Anesth. Pain Med. 2016;16:199–202. doi: 10.17245/jdapm.2016.16.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murthy A.K., Pramila M., Ranganath S. Prevalence of clinical consequences of untreated dental caries and its relation to dental fear among 12–15-year-old schoolchildren in Bangalore city, India. Eur. Arch. Paediatr. Dent. 2014;15:45–49. doi: 10.1007/s40368-013-0064-1. [DOI] [PubMed] [Google Scholar]
- 7.Rajasekaran U., Singh M., Goutam M., Bhalla A., Grover N., Galav A., Patil S. A Cross-sectional Study to assess the Perception of Psychosocial Elements among Pediatric Patients visiting Dental Clinics. J. Contemp. Dent. Pract. 2017;18:1021–1024. doi: 10.5005/jp-journals-10024-2168. [DOI] [PubMed] [Google Scholar]
- 8.Milgrom P., Newton J.T., Boyle C., Heaton L.J., Donaldson N. The effects of dental anxiety and irregular attendance on referral for dental treatment under sedation within the National Health Service in London. Community Dent. Oral Epidemiol. 2010;38:453–459. doi: 10.1111/j.1600-0528.2010.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baier K., Milgrom P., Russell S., Mancl L., Yoshida T. Children’s fear and behavior in private pediatric dentistry practices. Pediatr. Dent. 2004;26:316–321. [PubMed] [Google Scholar]
- 10.Jain A., Suprabha B.S., Shenoy R., Rao A. Association of temperament with dental anxiety and behaviour of the preschool child during the initial dental visit. Eur. J. Oral Sci. 2019;127:147–155. doi: 10.1111/eos.12606. [DOI] [PubMed] [Google Scholar]
- 11.Savanheimo N., Sundberg S.A., Virtanen J.I., Vehkalahti M.M. Dental care and treatments provided under general anaesthesia in the Helsinki Public Dental Service. BMC Oral Health. 2012;12:45. doi: 10.1186/1472-6831-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin Y.-L., Yen Y.-Y., Chen H.-S., Liu Y.-C., Chang C.-S., Chen C.-M., Chen F.-L., Hsu C.-C., Lee C.-H., Hu C.-Y., et al. Child dental fear in low-income and non-low-income families: A school-based survey study. J. Dent. Sci. 2014;9:165–171. doi: 10.1016/j.jds.2013.02.022. [DOI] [Google Scholar]
- 13.Ogawa M., Harano N., Ono K., Shigeyama-Tada Y., Hamasaki T., Watanabe S. Association between sensory processing and dental fear among female undergraduates in Japan. Acta Odontol. Scand. 2019;77:525–533. doi: 10.1080/00016357.2019.1610190. [DOI] [PubMed] [Google Scholar]
- 14.Oliveira M.A., Bendo C.B., Ferreira M.C., Paiva S.M., Vale M.P., Serra-Negra J.M. Association between Childhood Dental Experiences and Dental Fear among Dental, Psychology and Mathematics Undergraduates in Brazil. Int. J. Environ. Res. Public Health. 2012;9:4676–4687. doi: 10.3390/ijerph9124676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Locker D., Liddell A., Dempster L., Shapiro D. Age of onset of dental anxiety. J. Dent. Res. 1999;78:790–796. doi: 10.1177/00220345990780031201. [DOI] [PubMed] [Google Scholar]
- 16.Seligman L.D., Hovey J.D., Chacon K., Ollendick T.H. Dental anxiety: An understudied problem in youth. Clin. Psychol. Rev. 2017;55:25–40. doi: 10.1016/j.cpr.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Grisolia B.M., dos Santos A.P.P., D’Hyppolito I.M., Buchanan H., Hill K., Oliveira B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021;31:168–183. doi: 10.1111/ipd.12712. [DOI] [PubMed] [Google Scholar]
- 18.Uziel N., Meyerson J., Winocur E., Nabriski O., Eli I. Management of the Dentally Anxious Patient: The Dentist’s Perspective. Oral Health Prev. Dent. 2019;17:35–41. doi: 10.3290/j.ohpd.a4198. [DOI] [PubMed] [Google Scholar]
- 19.Åstrøm A.N., Skaret E., Haugejorden O. Dental anxiety and dental attendance among 25-year-olds in Norway: Time trends from 1997 to 2007. BMC Oral Health. 2011;11:10. doi: 10.1186/1472-6831-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirova D.G., Atanasov D.T., Lalabonova C.K., Janevska S. Dental Anxiety in Adults in Bulgaria. Folia Medica. 2010;52:49–56. doi: 10.2478/v10153-010-0047-5. [DOI] [PubMed] [Google Scholar]
- 21.Saatchi M., Abtahi M., Mohammadi G., Mirdamadi M., Binandeh E.S. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent. Res. J. 2015;12:248–253. [PMC free article] [PubMed] [Google Scholar]
- 22.Silveira E.R., Cademartori M.G., Schuch H.S., Armfield J.A., Demarco F.F. Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. J. Dent. 2021;108:103632. doi: 10.1016/j.jdent.2021.103632. [DOI] [PubMed] [Google Scholar]
- 23.Klingberg A.P.G. Dental anxiety and behaviour management problems in paediatric dentistry—A review of background factors and diagnostics. Eur. Arch. Paediatr. Dent. 2008;9:11–15. doi: 10.1007/BF03262650. [DOI] [PubMed] [Google Scholar]
- 24.Klingberg G., Broberg A.G. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int. J. Paediatr. Dent. 2007;17:391–406. doi: 10.1111/j.1365-263X.2007.00872.x. [DOI] [PubMed] [Google Scholar]
- 25.Porritt J., Buchanan H., Hall M., Gilchrist F., Marshman Z. Assessing children’s dental anxiety: A systematic review of current measures. Community Dent. Oral Epidemiol. 2013;41:130–142. doi: 10.1111/j.1600-0528.2012.00740.x. [DOI] [PubMed] [Google Scholar]
- 26.Yon M.J.Y., Che K.J., Gao S.S., Duangthip D., Lo E.C.M., Chu C.H. An introduction to assessing dental fear and anxiety in children. Healthcare. 2020;8:86. doi: 10.3390/healthcare8020086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Appukuttan D.P. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Clin. Cosmet. Investig. Dent. 2016;8:35–50. doi: 10.2147/CCIDE.S63626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Armfield J.M., Heaton L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013;58:390–407. doi: 10.1111/adj.12118. [DOI] [PubMed] [Google Scholar]
- 29.Yildirim T.T., Dundar S., Bozoglan A., Karaman T., Dildes N., Kaya F.A., Altintas E., Oztekin F., Atas O., Alan H. Is there a relation between dental anxiety, fear and general psychological status? Peer J. 2017;5:e2978. doi: 10.7717/peerj.2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alasmari A.A., Aldossari G.S., Aldossary M.S. Dental Anxiety in Children: A Review of the Contributing Factors. J. Clin. Diagn. Res. 2018;12:SG01–SG03. doi: 10.7860/JCDR/2018/35081.11379. [DOI] [Google Scholar]
- 31.Folayan M.O., Idehen E.E., Ojo O.O. The modulating effect of culture on the expression of dental anxiety in children: A literature review. Int. J. Paediatr. Dent. 2004;14:241–245. doi: 10.1111/j.1365-263X.2004.00563.x. [DOI] [PubMed] [Google Scholar]
- 32.Heaton L.J., Smith T.A., Raybould T.P. Factors Influencing Use of Dental Services in Rural and Urban Communities: Considerations for Practitioners in Underserved Areas. J. Dent. Educ. 2004;68:1081–1089. doi: 10.1002/j.0022-0337.2004.68.10.tb03853.x. [DOI] [PubMed] [Google Scholar]
- 33.Hilton I.V., Stephen S., Barker J.C., Weintraub J.A. Cultural factors and children’s oral health care: A qualitative study of carers of young children. Community Dent. Oral Epidemiol. 2007;35:429–438. doi: 10.1111/j.1600-0528.2006.00356.x. [DOI] [PubMed] [Google Scholar]
- 34.Murad M.H., Ingle N.A., Assery M.K. Evaluating factors associated with fear and anxiety to dental treatment—A systematic review. J. Fam. Med. Prim. Care. 2020;9:4530–4535. doi: 10.4103/jfmpc.jfmpc_607_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siegel K., Schrimshaw E.W., Kunzel C., Wolfson N.H., Moon-Howard J., Moats H.L., Mitchell D.A. Types of Dental Fear as Barriers to Dental Care among African American Adults with Oral Health Symptoms in Harlem. J. Health Care Poor Underserved. 2012;23:1294–1309. doi: 10.1353/hpu.2012.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yakar B., Kaygusuz T.O., Pirinçci E. Evaluation of Dental Anxiety and Fear in Patients who admitted to the Faculty of Dentistry: Which Patients are More Risky in terms of Dental Anxiety. Ethiop. J. Health Sci. 2019;29:719–726. doi: 10.4314/ejhs.v29i6.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nissan S., Yochman A., Blumer S., Kharouba J., Peretz B. Children’s Responses to Sensory Stimuli and their Behavior in the Dental Office. J. Clin. Pediatr. Dent. 2017;41:10–17. doi: 10.17796/1053-4628-41.1.10. [DOI] [PubMed] [Google Scholar]
- 38.Cohen S.M., Fiske J.D., Newton J.T. The impact of dental anxiety on daily living. Br. Dent. J. 2000;189:385–390. doi: 10.1038/sj.bdj.4800777. [DOI] [PubMed] [Google Scholar]
- 39.Alkan A., Cakmak O., Yilmaz S., Cebi T., Gurgan C. Relationship between Psychological Factors and Oral Health Status and Behaviours. Oral Health Prev. Dent. 2015;13:331–339. doi: 10.3290/J.OHPD.A32679. [DOI] [PubMed] [Google Scholar]
- 40.Bernson J.M., Elfström M.L., Hakeberg M. Dental coping strategies, general anxiety, and depression among adult patients with dental anxiety but with different dental-attendance patterns. Eur. J. Oral Sci. 2013;121:270–276. doi: 10.1111/eos.12039. [DOI] [PubMed] [Google Scholar]
- 41.Gustafsson A., Broberg A., Bodin L., Berggren U., Arnrup K. Dental behaviour management problems: The role of child personal characteristics. Int. J. Paediatr. Dent. 2010;20:242–253. doi: 10.1111/j.1365-263X.2010.01046.x. [DOI] [PubMed] [Google Scholar]
- 42.Stein L.I., Polido J.C., Cermak S.A. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr. Dent. 2013;35:230–235. [PubMed] [Google Scholar]
- 43.Stein L.I., Lane C.J., Williams M.E., Dawson M.E., Polido J.C., Cermak S.A. Physiological and Behavioral Stress and Anxiety in Children with Autism Spectrum Disorders during Routine Oral Care. BioMed Res. Int. 2014;2014:694876. doi: 10.1155/2014/694876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cermak S.A., Stein Duker L.I., Williams M.E., Dawson M.E., Lane C.J., Polido J.C. Sensory Adapted Dental Environments to Enhance Oral Care for Children with Autism Spectrum Disorders: A Randomized Controlled Pilot Study. J. Autism Dev. Disord. 2015;45:2876–2888. doi: 10.1007/s10803-015-2450-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bedi R., Sutcliffe P., Donnan P.T., Mcconnachie J. The prevalence of dental anxiety in a group of 13- and 14-year-old Scottish children. Int. J. Paediatr. Dent. 1992;2:17–24. doi: 10.1111/j.1365-263X.1992.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 46.Chellappah N.K., Vignehsa H., Milgrom P., Lam L.G. Prevalence of dental anxiety and fear in children in Singapore. Community Dent. Oral Epidemiol. 1990;18:269–271. doi: 10.1111/j.1600-0528.1990.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 47.D’Alessandro G., Alkhamis N., Mattarozzi K., Mazzetti M., Piana G. Fear of dental pain in Italian children: Child personality traits and parental dental fear. J. Public Health Dent. 2016;76:179–183. doi: 10.1111/jphd.12127. [DOI] [PubMed] [Google Scholar]
- 48.Folayan M.O., Idehen E.E., Ojo O.O. Dental anxiety in a subpopulation of African children: Parents ability to predict and its relation to general anxiety and behaviour in the dental chair. Eur. J. Paediatr. Dent. 2004;5:19–23. [PubMed] [Google Scholar]
- 49.Klingberg G., Berggren U., Norén J.G. Dental fear in an urban Swedish child population: Prevalence and concomitant factors. Community Dent Health. 1994;11:208–214. [PubMed] [Google Scholar]
- 50.Klingberg G., Berggren U., Carlsson S.G., Noren J.G. Child dental fear: Cause-related factors and clinical effects. Eur. J. Oral Sci. 1995;103:405–412. doi: 10.1111/j.1600-0722.1995.tb01865.x. [DOI] [PubMed] [Google Scholar]
- 51.Milgrom P., Mancl L., King B., Weinstein P. Origins of childhood dental fear. Behav. Res. Ther. 1995;33:313–319. doi: 10.1016/0005-7967(94)00042-I. [DOI] [PubMed] [Google Scholar]
- 52.Salem K., Kousha M., Anissian A., Shahabi A. Dental Fear and Concomitant Factors in 3-6 Year-old Children. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012;6:70–74. doi: 10.5681/joddd.2012.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xiang B., Wong H.M., Perfecto A.P., McGrath C.P.J. The association of socio-economic status, dental anxiety, and behavioral and clinical variables with adolescents’ oral health-related quality of life. Qual. Life Res. 2020;29:2455–2464. doi: 10.1007/s11136-020-02504-7. [DOI] [PubMed] [Google Scholar]
- 54.Moore R., Birn H., Kirkegaard E., Brodsgaard I., Scheutz F. Prevalence and characteristics of dental anxiety in Danish adults. Community Dent. Oral Epidemiol. 1993;21:292–296. doi: 10.1111/j.1600-0528.1993.tb00777.x. [DOI] [PubMed] [Google Scholar]
- 55.Abrahamsson K.H., Berggren U., Carlsson S.G. Psychosocial aspects of dental and general fears in dental phobic patients. Acta Odontol. Scand. 2000;58:37–43. doi: 10.1080/000163500429415. [DOI] [PubMed] [Google Scholar]
- 56.Boman U.W., Lundgren J., Berggren U., Carlsson S.G. Psychosocial and dental factors in the maintenance of severe dental fear. Swed. Dent. J. 2010;34:121–127. [PubMed] [Google Scholar]
- 57.Doganer Y., Aydogan U., Yesil H.U., Rohrer J., Williams M.D., Agerter D.C. Does the trait anxiety affect the dental fear? Braz. Oral Res. 2017;31:e36. doi: 10.1590/1807-3107bor-2017.vol31.0036. [DOI] [PubMed] [Google Scholar]
- 58.Fiset L., Milgrom P., Weinstein P., Melnick S. Common fears and their relationship to dental fear and utilization of the dentist. Anesth. Prog. 1989;36:258–264. [PMC free article] [PubMed] [Google Scholar]
- 59.Fuentes D., Gorenstein C., Hu L.W. Dental anxiety and trait anxiety: An investigation of their relationship. Br. Dent. J. 2009;206:E17. doi: 10.1038/sj.bdj.2009.253. [DOI] [PubMed] [Google Scholar]
- 60.Hakeberg M., Hägglin C., Berggren U., Carlsson S.G. Structural relationships of dental anxiety, mood, and general anxiety. Acta Odontol. Scand. 2001;59:99–103. doi: 10.1080/000163501750157252. [DOI] [PubMed] [Google Scholar]
- 61.Kaakko T., Milgrom P., Coldwell S.E., Getz T., Weinstein P., Ramsay D.S. Dental fear among university employees: Implications for dental education. J. Dent. Educ. 1998;62:415–420. doi: 10.1002/j.0022-0337.1998.62.6.tb03210.x. [DOI] [PubMed] [Google Scholar]
- 62.Milgrom P., Kleinknecht R.A., Elliott J., Hsing L.H., Choo-Soo T. A cross-cultural cross validation of the dental fear survey in South East Asia. Behav. Res. Ther. 1990;28:227–233. doi: 10.1016/0005-7967(90)90005-4. [DOI] [PubMed] [Google Scholar]
- 63.Pohjola V., Mattila A.K., Joukamaa M., Lahti S. Anxiety and depressive disorders and dental fear among adults in Finland. Eur. J. Oral Sci. 2011;119:55–60. doi: 10.1111/j.1600-0722.2010.00795.x. [DOI] [PubMed] [Google Scholar]
- 64.Pohjola V., Kunttu K., Virtanen J.I. Psychological Distress, Dental Health, and Dental Fear among Finnish University Students: A National Survey. Int. J. Environ. Res. Public Health. 2021;18:10245. doi: 10.3390/ijerph181910245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Skaret E., Raadal M., Berg E., Kvale G. Dental anxiety among 18-yr-olds in Norway, Prevalence and related factors. Eur. J. Oral Sci. 1998;106:835–843. doi: 10.1046/j.0909-8836.1998.eos106402.x. [DOI] [PubMed] [Google Scholar]
- 66.Strøm K., Skaare A.B., Willumsen T. Dental anxiety in 18-year-old Norwegians in 1996 and 2016. Acta Odontol. Scand. 2020;78:13–19. doi: 10.1080/00016357.2019.1637933. [DOI] [PubMed] [Google Scholar]
- 67.Witcraft S.M., Wickenhauser M.E., Maack D.J., Dixon L.J. What sensitivities matter in dental anxiety? Investigating sensitivity to anxiety, pain, and disgust. Psychol. Health Med. 2021;26:313–321. doi: 10.1080/13548506.2020.1781911. [DOI] [PubMed] [Google Scholar]
- 68.Zinke A., Hannig C., Berth H. Psychological distress and anxiety compared amongst dental patients–results of a cross-sectional study in 1549 adults. BMC Oral Health. 2019;19:1–6. doi: 10.1186/s12903-019-0719-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Townend E., Dimigen G., Fung D. A clinical study of child dental anxiety. Behav. Res. Ther. 2000;38:31–46. doi: 10.1016/S0005-7967(98)00205-8. [DOI] [PubMed] [Google Scholar]
- 70.Locker D., Poulton R., Thomson W.M. Psychological disorders and dental anxiety in a young adult population. Community Dent. Oral Epidemiol. 2001;29:456–463. doi: 10.1034/j.1600-0528.2001.290607.x. [DOI] [PubMed] [Google Scholar]
- 71.Vanhee T., Mourali S., Bottenberg P., Jacquet W., Abbeele A.V. Stimuli involved in dental anxiety: What are patients afraid of?: A descriptive study. Int. J. Paediatr. Dent. 2020;30:276–285. doi: 10.1111/ipd.12595. [DOI] [PubMed] [Google Scholar]
- 72.Gao X., Hamzah S., Yiu C.K.Y., McGrath C., King N.M., Knösel M., Spallek H., Archaya A., Lyons E., Lu A.S. Dental Fear and Anxiety in Children and Adolescents: Qualitative Study Using YouTube. J. Med. Internet Res. 2013;15:e29. doi: 10.2196/jmir.2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jones L.M., Watson R. Stress and Anxiety: Appli-cations to Social and Environmental Threats, Psychological Well-Being, Occupational Challenges, and Developmental Psychology. Logos Verlag; Berlin/Heidelberg, Germany: 2014. An exploration of children’s dental anxiety: Triggers, coping and needs; pp. 261–270. [Google Scholar]
- 74.O’Grady A., Gray-Burrows K., Tahmassebi J. Inside the waiting room: Process drama and dramatic distancing for involving children in research on dental anxiety. Arts Health. 2021:1–16. doi: 10.1080/17533015.2021.1894465. [DOI] [PubMed] [Google Scholar]
- 75.Tahmassebi J.F., Malik M., Berg N., Pavitt S., Gray-Burrows K., O’Grady A. Using process drama to explore the causes of dental anxiety in primary-school children. Eur. Arch. Paediatr. Dent. 2021;22:869–877. doi: 10.1007/s40368-021-00623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rajeev A., Patthi B., Janakiram C., Singla A., Malhi R., Kumari M. Influence of the previous dental visit experience in seeking dental care among young adults. J. Fam. Med. Prim. Care. 2020;9:609–613. doi: 10.4103/jfmpc.jfmpc_1109_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brady P., Dickinson C., Whelton H. Dental anxiety prevalence and surgery environment factors: A questionnaire-based sur-vey of attenders in Ireland. SAAD Dig. 2012;28:13–22. [Google Scholar]
- 78.Goldsmith H.H., Van Hulle C.A., Arneson C.L., Schreiber J.E., Gernsbacher M.A. A Population-Based Twin Study of Parentally Reported Tactile and Auditory Defensiveness in Young Children. J. Abnorm. Child Psychol. 2006;34:378–392. doi: 10.1007/s10802-006-9024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lane S.J., Reynolds S., Dumenci L. Sensory Overresponsivity and Anxiety in Typically Developing Children and Children with Autism and Attention Deficit Hyperactivity Disorder: Cause or Coexistence? Am. J. Occup. Ther. 2012;66:595–603. doi: 10.5014/ajot.2012.004523. [DOI] [PubMed] [Google Scholar]
- 80.Kinnealey M., Koenig K.P., Smith S. Relationships between Sensory Modulation and Social Supports and Health-Related Quality of Life. Am. J. Occup. Ther. 2011;65:320–327. doi: 10.5014/ajot.2011.001370. [DOI] [PubMed] [Google Scholar]
- 81.Kinnealey M., Fuiek M. The relationship between sensory defensiveness, anxiety, depression and perception of pain in adults. Occup. Ther. Int. 1999;6:195–206. doi: 10.1002/oti.97. [DOI] [Google Scholar]
- 82.Neal J.A., Edelmann R.J., Glachan M. Behavioural inhibition and symptoms of anxiety and depression: Is there a specific relationship with social phobia? Br. J. Clin. Psychol. 2002;41:361–374. doi: 10.1348/014466502760387489. [DOI] [PubMed] [Google Scholar]
- 83.Pfeiffer B., Kinnealey M. Treatment of sensory defensiveness in adults. Occup. Ther. Int. 2003;10:175–184. doi: 10.1002/oti.184. [DOI] [PubMed] [Google Scholar]
- 84.Carpenter K.L.H., Baranek G.T., Copeland W.E., Compton S., Zucker N., Dawson G., Egger H.L. Sensory Over-Responsivity: An Early Risk Factor for Anxiety and Behavioral Challenges in Young Children. J. Abnorm. Child Psychol. 2019;47:1075–1088. doi: 10.1007/s10802-018-0502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ben-Sasson A., Carter A.S., Briggs-Gowan M.J. Sensory over-responsivity in elementary school: Prevalence and social-emotional correlates. J. Abnorm. Child Psych. 2009;37:705–716. doi: 10.1007/s10802-008-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Engel-Yeger B., Dunn W.W. The relationship between sensory processing difficulties and anxiety level of healthy adults. Br. J. Occup. Ther. 2011;74:210–216. doi: 10.4276/030802211X13046730116407. [DOI] [Google Scholar]
- 87.Locker D., Allen F. What do measures of ‘oral health-related quality of life’ measure? Community Dent. Oral Epidemiol. 2007;35:401–411. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 88.Carrillo-Díaz M., Crego A., Armfield J.M., Romero M. Self-assessed oral health, cognitive vulnerability and dental anxiety in children: Testing a mediational model. Community Dent. Oral Epidemiol. 2012;40:8–16. doi: 10.1111/j.1600-0528.2011.00646.x. [DOI] [PubMed] [Google Scholar]
- 89.Goyal A., Sharma A., Gaur T., Singh J., Pachori Y., Chhabra K.G., Chhabra C. Impact of dental fear on oral health-related quality of life among school going and non-school going children in Udaipur city: A cross-sectional study. Contemp. Clin. Dent. 2014;5:42–48. doi: 10.4103/0976-237x.128662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Luoto A., Lahti S., Nevanperä T., Tolvanen M., Locker D. Oral-health-related quality of life among children with and without dental fear. Int. J. Paediatr. Dent. 2009;19:115–120. doi: 10.1111/j.1365-263X.2008.00943.x. [DOI] [PubMed] [Google Scholar]
- 91.Merdad L., El-Housseiny A.A. Do children’s previous dental experience and fear affect their perceived oral health-related quality of life (OHRQoL)? BMC Oral Health. 2017;17:47. doi: 10.1186/s12903-017-0338-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Slabšinskienė E., Kavaliauskienė A., Žemaitienė M., Vasiliauskienė I., Zaborskis A. Dental Fear and Associated Factors among Children and Adolescents: A School-Based Study in Lithuania. Int. J. Environ. Res. Public Health. 2021;18:8883. doi: 10.3390/ijerph18168883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Almoznino G., Zini A., Aframian D.J., Kaufman E., Lvovsky A., Hadad A., Levin L. Oral Health Related Quality of Life in Young Individuals with Dental Anxiety and Exaggerated Gag Reflex. Oral Health Prev. Dent. 2015;13:435–440. doi: 10.3290/J.OHPD.A33921. [DOI] [PubMed] [Google Scholar]
- 94.Costa F.S., Cademartori M.G., Silva M.F., Nascimento G., Shqair A.Q., Pinheiro R.T., Demarco F.F., Goettems M.L. Anxiety symptoms have a direct effect on oral health perception in young women. Qual. Life Res. 2018;27:1583–1588. doi: 10.1007/s11136-018-1797-4. [DOI] [PubMed] [Google Scholar]
- 95.Khan S.D.A.A., Alqannass N.M., Alwadei M.M., Alnajrani M.D., Alshahrani Z.M., Al Alhareth A.Y., Alqahtani K.M. Assessment of the relationship between dental anxiety and oral health-related quality of life. J. Pharm. Bioallied Sci. 2021;13:359. doi: 10.4103/jpbs.JPBS_742_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kumar S., Bhargav P., Patel A., Bhati M., Balasubramanyam G., Duraiswamy P., Kulkarni S. Does dental anxiety influence oral health-related quality of life? Observations from a cross-sectional study among adults in Udaipur district, India. J. Oral Sci. 2009;51:245–254. doi: 10.2334/josnusd.51.245. [DOI] [PubMed] [Google Scholar]
- 97.McGrath C., Bedi R. The association between dental anxiety and oral health-related quality of life in Britain. Community Dent. Oral Epidemiol. 2004;32:67–72. doi: 10.1111/j.1600-0528.2004.00119.x. [DOI] [PubMed] [Google Scholar]
- 98.Mehrstedt M., John M.T., Tönnies S., Micheelis W. Oral health-related quality of life in patients with dental anxiety. Community Dent. Oral Epidemiol. 2007;35:357–363. doi: 10.1111/j.1600-0528.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 99.Ng S.K.S., Leung W.K. A community study on the relationship of dental anxiety with oral health status and oral health-related quality of life. Community Dent. Oral Epidemiol. 2008;36:347–356. doi: 10.1111/j.1600-0528.2007.00412.x. [DOI] [PubMed] [Google Scholar]
- 100.Pohjola V., Lahti S., Suominen-Taipale L., Hausen H. Dental fear and subjective oral impacts among adults in Finland. Eur. J. Oral Sci. 2009;117:268–272. doi: 10.1111/j.1600-0722.2009.00631.x. [DOI] [PubMed] [Google Scholar]
- 101.Song Y., Luzzi L., Chrisopoulos S., Brennan D. Dentist-patient relationships and oral health impact in Australian adults. Community Dent. Oral Epidemiol. 2020;48:309–316. doi: 10.1111/cdoe.12534. [DOI] [PubMed] [Google Scholar]
- 102.Sukumaran I., Taylor S., Thomson W.M. The Prevalence and Impact of Dental Anxiety among Adult New Zealanders. Int. Dent. J. 2021;71:122–126. doi: 10.1111/idj.12613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Alsadat F.A., El-Housseiny A.A., Alamoudi N.M., Elderwi D.A., Ainosa A.M., Dardeer F.M. Dental fear in primary school chil-dren and its relation to dental caries. Niger. J. Clin. Pract. 2018;21:1454–1460. doi: 10.4103/njcp.njcp_160_18. [DOI] [PubMed] [Google Scholar]
- 104.Alvesalo I., Murtomaa H., Milgrom P., Honkanen A., Karjalainen M., Tay K.-M. The Dental Fear Survey Schedule: A study with Finnish children. Int. J. Paediatr. Dent. 1993;3:193–198. doi: 10.1111/j.1365-263X.1993.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 105.Barreto K.A., Dos Prazeres L.D.K.T., Lima D.S.M., Soares F.C., Redivivo R.M.M.P., da Franca C., Colares V. Factors associated with dental anxiety in Brazilian children during the first transitional period of the mixed dentition. Eur. Arch. Paediatr. Dent. 2017;18:39–43. doi: 10.1007/s40368-016-0264-6. [DOI] [PubMed] [Google Scholar]
- 106.Chakradhar K., Dolar D., Kulkarni S., Reddy B.S., Reddy M.P., Srilatha A. Correlation of dental anxiety with oral health status and treatment needs among 12-year old indian school going children. Acta Biomed. 2020;91:e2020095. doi: 10.23750/abm.v91i4.8682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dahlander A., Soares F., Grindefjord M., Dahllöf G. Factors Associated with Dental Fear and Anxiety in Children Aged 7 to 9 Years. Dent. J. 2019;7:68. doi: 10.3390/dj7030068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Folayan M.O., Kolawole K.A., Onyejaka N.K., Agbaje H.O., Chukwumah N.M., Oyedele T.A. General anxiety, dental anxiety, digit sucking, caries and oral hygiene status of children resident in a semi-urban population in Nigeria. BMC Oral Health. 2018;18:66. doi: 10.1186/s12903-018-0529-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Goettems M.L., Shqair A.Q., Bergmann V.F., Cadermatori M.G., Correa M.B., Demarco F.F. Oral health self-perception, dental caries, and pain: The role of dental fear underlying this association. Int. J. Paediatr. Dent. 2018;28:319–325. doi: 10.1111/ipd.12359. [DOI] [PubMed] [Google Scholar]
- 110.Haworth S., Dudding T., Waylen A., Thomas S.J., Timpson N.J. Ten years on: Is dental general anaesthesia in childhood a risk factor for caries and anxiety? Br. Dent. J. 2017;222:299–304. doi: 10.1038/sj.bdj.2017.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Howard K.E., Freeman R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int. J. Paediatr. Dent. 2007;17:281–288. doi: 10.1111/j.1365-263X.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- 112.Kim A.H., Ahn E.S., An S.Y. Factors affecting dental fear in Korean adolescents. J. Korean Dent. Sci. 2017;10:22–28. doi: 10.5856/JKDS.2017.10.1.22. [DOI] [Google Scholar]
- 113.Nermo H., Willumsen T., Johnsen J.-A.K. Changes in dental anxiety among 15- to 21-year-olds. A 2-year longitudinal analysis based on the Tromsø study: Fit futures. Community Dent. Oral Epidemiol. 2018;47:127–133. doi: 10.1111/cdoe.12434. [DOI] [PubMed] [Google Scholar]
- 114.Nicolas E., Bessadet M., Collado V., Carrasco P., Rogerleroi V., Hennequin M. Factors affecting dental fear in French children aged 5–12 years. Int. J. Paediatr. Dent. 2010;20:366–373. doi: 10.1111/j.1365-263X.2010.01054.x. [DOI] [PubMed] [Google Scholar]
- 115.Olak J., Saag M., Honkala S., Nõmmela R., Runnel R., Honkala E., Karjalainen S. Children’s dental fear in relation to dental health and parental dental fear. Stomatologija. 2013;15:26–31. [PubMed] [Google Scholar]
- 116.Panda S., Quadri M., Hadi I., Jably R., Hamzi A., Jafer M. Does Dental Fear in Children Predict Untreated Dental Caries? An Analytical Cross-Sectional Study. Children. 2021;8:382. doi: 10.3390/children8050382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Raadal M., Strand G.V., Amarante E.C., Kvale G. Relationship between caries prevalence at 5 years of age and dental anxiety at 10. Eur. J. Paediatr. Dent. 2002;3:22–26. [PubMed] [Google Scholar]
- 118.Da Silveira E.R., Goettems M.L., Demarco F.F., Azevedo M.S. Clinical and Individual Variables in Children’s Dental Fear: A School-Based Investigation. Braz. Dent. J. 2017;28:398–404. doi: 10.1590/0103-6440201601265. [DOI] [PubMed] [Google Scholar]
- 119.Soares F.C., Lima R., de Barros M.V.G., Dahllöf G., Colares V. Development of dental anxiety in schoolchildren: A 2-year prospective study. Community Dent. Oral Epidemiol. 2017;45:281–288. doi: 10.1111/cdoe.12290. [DOI] [PubMed] [Google Scholar]
- 120.Soares F.C., Lima R.A., Salvador D.M., de Barros M.V.G., Dahllöf G., Colares V. Reciprocal longitudinal relationship between dental fear and oral health in schoolchildren. Int. J. Paediatr. Dent. 2019;30:286–292. doi: 10.1111/ipd.12598. [DOI] [PubMed] [Google Scholar]
- 121.Torriani D.D., Ferro R.L., Bonow M.L.M., Santos I.S., Matijasevich A., Barros A.J., Demarco F.F., Peres K.G. Dental Caries Is Associated with Dental Fear in Childhood: Findings from a Birth Cohort Study. Caries Res. 2014;48:263–270. doi: 10.1159/000356306. [DOI] [PubMed] [Google Scholar]
- 122.Wang X., Bernabe E., Pitts N., Zheng S., Gallagher J.E. Dental caries thresholds among adolescents in England, Wales, and Northern Ireland, 2013 at 12, and 15 years: Implications for epidemiology and clinical care. BMC Oral Health. 2021;21:137. doi: 10.1186/s12903-021-01507-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.DeDonno M. Dental anxiety, dental visits and oral hygiene practices. Oral Health Prev. Dent. 2012;10:129–133. [PubMed] [Google Scholar]
- 124.Locker D., Liddell A. Clinical correlates of dental anxiety among older adults. Community Dent. Oral Epidemiol. 1992;20:372–375. doi: 10.1111/j.1600-0528.1992.tb00702.x. [DOI] [PubMed] [Google Scholar]
- 125.Armfield J.M. What goes around comes around: Revisiting the hypothesized vicious cycle of dental fear and avoidance. Community Dent. Oral Epidemiol. 2012;41:279–287. doi: 10.1111/cdoe.12005. [DOI] [PubMed] [Google Scholar]
- 126.Armfield J.M., Stewart J.F., Spencer A.J. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007;7:1. doi: 10.1186/1472-6831-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Armfield J.M., Slade G.D., Spencer A.J. Dental fear and adult oral health in Australia. Community Dent. Oral Epidemiol. 2009;37:220–230. doi: 10.1111/j.1600-0528.2009.00468.x. [DOI] [PubMed] [Google Scholar]
- 128.Eitner S., Wichmann M., Paulsen A., Holst S. Dental anxiety—An epidemiological study on its clinical correlation and effects on oral health. J. Oral Rehabil. 2006;33:588–593. doi: 10.1111/j.1365-2842.2005.01589.x. [DOI] [PubMed] [Google Scholar]
- 129.Heyman R.E., Slep A.M.S., White-Ajmani M., Bulling L., Zickgraf H.F., Franklin M.E., Wolff M.S. Dental Fear and Avoidance in Treatment Seekers at a Large, Urban Dental Clinic. Oral Health Prev. Dent. 2016;14:315–320. doi: 10.3290/J.OHPD.A36468. [DOI] [PubMed] [Google Scholar]
- 130.Julihn A., Agholme M.B., Grindefjord M., Modéer T. Risk factors and risk indicators associated with high caries experience in Swedish 19-year-olds. Acta Odontol. Scand. 2006;64:267–273. doi: 10.1080/00016350600613534. [DOI] [PubMed] [Google Scholar]
- 131.Kanaffa-Kilijanska U., Kaczmarek U., Kilijańska B., Frydecka D. Oral health condition and hygiene habits among adult patients with respect to their level of dental anxiety. Oral. Health Prev. Dent. 2014;12:233–239. doi: 10.3290/j.ohpd.a31668. [DOI] [PubMed] [Google Scholar]
- 132.Mehrstedt M., Tönnies S., Eisentraut I. Dental fears, health status, and quality of life. Anesth. Prog. 2004;51:90–94. [PMC free article] [PubMed] [Google Scholar]
- 133.Meng X., Heft M.W., Bradley M.M., Lang P.J. Effect of fear on dental utilization behaviors and oral health outcome. Community Dent. Oral Epidemiol. 2007;35:292–301. doi: 10.1111/j.1600-0528.2007.00315.x. [DOI] [PubMed] [Google Scholar]
- 134.Oliveira M., Vale M.P., Bendo C., Paiva S.M., Serra-Negra J.M. Influence of negative dental experiences in childhood on the development of dental fear in adulthood: A case-control study. J. Oral Rehabil. 2017;15:100–441. doi: 10.1111/joor.12513. [DOI] [PubMed] [Google Scholar]
- 135.Pohjola V., Lahti S., Vehkalahti M.M., Tolvanen M., Hausen H. Association between dental fear and dental attendance among adults in Finland. Acta Odontol. Scand. 2007;65:224–230. doi: 10.1080/00016350701373558. [DOI] [PubMed] [Google Scholar]
- 136.Schuller A.A., Willumsen T., Holst D. Are there differences in oral health and oral health behavior between individuals with high and low dental fear? Community Dent. Oral Epidemiol. 2003;31:116–121. doi: 10.1034/j.1600-0528.2003.00026.x. [DOI] [PubMed] [Google Scholar]
- 137.Samorodnitzky G.R., Levin L. Self-assessed dental status, oral behavior, DMF, and dental anxiety. J. Dent. Educ. 2005;69:1385–1389. doi: 10.1002/j.0022-0337.2005.69.12.tb04038.x. [DOI] [PubMed] [Google Scholar]
- 138.Silveira E.R., Cademartori M.G., Schuch H.S., Corrêa M.B., Ardenghi T.M., Armfield J., Horta B.L., Demarco F.F. The vicious cycle of dental fear at age 31 in a birth cohort in Southern Brazil. Community Dent. Oral Epidemiol. 2021;49:354–361. doi: 10.1111/cdoe.12609. [DOI] [PubMed] [Google Scholar]
- 139.Sullivan M.J.L., Neish N.R. Catastrophizing, anxiety and pain during dental hygiene treatment. Community Dent. Oral Epidemiol. 1998;26:344–349. doi: 10.1111/j.1600-0528.1998.tb01971.x. [DOI] [PubMed] [Google Scholar]
- 140.Stouthard M.E.A., Hoogstraten J. Prevalence of dental anxiety in the Netherlands. Community Dent. Oral Epidemiol. 1990;18:139–142. doi: 10.1111/j.1600-0528.1990.tb00039.x. [DOI] [PubMed] [Google Scholar]
- 141.Syed S., Bilal S., Dawani N., Rizvi K. Dental anxiety among adult patients and its correlation with self-assessed dental status and treatment needs. J. Pak. Med Assoc. 2013;63:614–618. [PubMed] [Google Scholar]
- 142.Yildirim T.T. Evaluating the Relationship of Dental Fear with Dental Health Status and Awareness. J. Clin. Diagn. Res. 2016;10:ZC105–ZC109. doi: 10.7860/JCDR/2016/19303.8214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Abanto J., Vidigal E.A., Carvalho T.S., de Sá S.N.C., Bönecker M. Factors for determining dental anxiety in preschool children with severe dental caries. Braz. Oral Res. 2017;31:e13. doi: 10.1590/1807-3107bor-2017.vol31.0013. [DOI] [PubMed] [Google Scholar]
- 144.Buldur B., Güvendi O.N. Conceptual modelling of the factors affecting oral health-related quality of life in children: A path analysis. Int. J. Paediatr. Dent. 2020;30:181–192. doi: 10.1111/ipd.12583. [DOI] [PubMed] [Google Scholar]
- 145.Amorim Júnior L.A., Rodrigues V.B.M., Costa L.R., Corrêa-Faria P. Is dental anxiety associated with the behavior of sedated children? Braz. Oral Res. 2021;35:1–8. doi: 10.1590/1807-3107bor-2021.vol35.0088. [DOI] [PubMed] [Google Scholar]
- 146.Boka V., Arapostathis K., Karagiannis V., Kostanos N., van Loveren C., Veerkamp J. Dental fear and caries in 6-12 year old children in Greece. Determination of dental fear cut-off points. Eur. J. Paediatr. Dent. 2017;18:45–50. doi: 10.23804/ejpd.2017.18.01.10. [DOI] [PubMed] [Google Scholar]
- 147.Laureano I.C.C., Farias L., Fernandes L.H.F., de Alencar C.R.B., Forte F.D.S., Honório D.R., Cavalcanti A.L. Dental Fear in Children: Association with Dental Caries and Molar Incisor Hypomineralization. Braz. Dent. J. 2020;31:673–679. doi: 10.1590/0103-6440202003880. [DOI] [PubMed] [Google Scholar]
- 148.Nermo H., Willumsen T., Johnsen J.-A.K. Prevalence of dental anxiety and associations with oral health, psychological distress, avoidance and anticipated pain in adolescence: A cross-sectional study based on the Tromsø study, Fit Futures. Acta Odontol. Scand. 2019;77:126–134. doi: 10.1080/00016357.2018.1513558. [DOI] [PubMed] [Google Scholar]
- 149.Taani D.Q., El-Qaderi S.S., Abu Alhaija E.S.J. Dental anxiety in children and its relationship to dental caries and gingival condition. Int. J. Dent. Hyg. 2005;3:83–87. doi: 10.1111/j.1601-5037.2005.00127.x. [DOI] [PubMed] [Google Scholar]
- 150.Vignehsa H., Chellappah N.K., Milgrom P., Going R., Teo C.S. A clinical evaluation of high- and low-fear children in Singa-pore. ASDC J. Dent. Child. 1990;57:224–228. [PubMed] [Google Scholar]
- 151.Wong H.M., Peng S., Perfecto A., McGrath C.P.J. Dental anxiety and caries experience from late childhood through adolescence to early adulthood. Community Dent. Oral Epidemiol. 2020;48:513–521. doi: 10.1111/cdoe.12563. [DOI] [PubMed] [Google Scholar]
- 152.Folayan M.O., El Tantawi M., Oginni A., Adeniyi A., Alade M., Finlayson T.L. Psychosocial, education, economic factors, decision-making ability, and caries status of mothers of children younger than 6 years in suburban Nigeria. BMC Oral Health. 2020;20:131. doi: 10.1186/s12903-020-01120-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pohjola V., Nurkkala M., Virtanen J.I. Psychological distress, oral health behaviour and related factors among adolescents: Finnish School Health Promotion Study. BMC Oral Health. 2021;21:6. doi: 10.1186/s12903-020-01357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Veeraboina N., Doshi D., Kulkarni S., Patanapu S.K., Dantala S.N., Adepu S. Association of state and trait anxiety with oral health status among adult dental patients. Acta Bio Med. 2020;91:e2020070. doi: 10.23750/abm.v91i3.8986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Carrillo-Diaz M., Crego A., Armfield J.M., Romero-Maroto M. Treatment experience, frequency of dental visits, and children’s dental fear: A cognitive approach. Eur. J. Oral Sci. 2012;120:75–81. doi: 10.1111/j.1600-0722.2011.00921.x. [DOI] [PubMed] [Google Scholar]
- 156.Milgrom P., Vignehsa H., Weinstein P. Adolescent dental fear and control: Prevalence and theoretical implications. Behav. Res. Ther. 1992;30:367–373. doi: 10.1016/0005-7967(92)90048-L. [DOI] [PubMed] [Google Scholar]
- 157.Paryab M., Hosseinbor M. Dental anxiety and behavioral problems: A study of prevalence and related factors among a group of Iranian children aged 6-12. J. Indian Soc. Pedod. Prev. Dent. 2013;31:82–86. doi: 10.4103/0970-4388.115699. [DOI] [PubMed] [Google Scholar]
- 158.Tickle M., Jones C., Buchannan K., Milsom K.M., Blinkhorn A.S., Humphris G.M. A prospective study of dental anxiety in a cohort of children followed from 5 to 9 years of age. Int. J. Paediatr. Dent. 2009;19:225–232. doi: 10.1111/j.1365-263X.2009.00976.x. [DOI] [PubMed] [Google Scholar]
- 159.Wogelius P., Poulsen S. Associations between dental anxiety, dental treatment due to toothache, and missed dental appointments among six to eight-year-old Danish children: A cross-sectional study. Acta Odontol. Scand. 2005;63:179–182. doi: 10.1080/00016350510019829. [DOI] [PubMed] [Google Scholar]
- 160.Abrahamsson K.H., Berggren U., Hakeberg M., Carlsson S.G. Phobic dental avoidance and regular dental care in fearful dental patients: A comparative study. Acta Odontol. Scand. 2001;59:273–279. doi: 10.1080/000163501750541129. [DOI] [PubMed] [Google Scholar]
- 161.Chanpong B., Haas D.A., Locker D. Need and Demand for Sedation or General Anesthesia in Dentistry: A National Survey of the Canadian Population. Anesth. Prog. 2005;52:3–11. doi: 10.2344/0003-3006(2005)52[3:NADFSO]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Domoto P., Weinstein P., Kamo Y., Wohlers K., Fiset L., Tanaka A. Dental fear of Japanese residents in the United States. Anesth. Prog. 1991;38:90–95. [PMC free article] [PubMed] [Google Scholar]
- 163.Erten H., Akarslan Z.Z., Bodrumlu E. Dental fear and anxiety levels of patients attending a dental clinic. Quintessence Int. 2006;37:304–310. [PubMed] [Google Scholar]
- 164.Goettems M.L., Schuch H.S., Demarco F.F., Ardenghi T.M., Torriani D.D. Impact of dental anxiety and fear on dental care use in Brazilian women. J. Public Health Dent. 2014;74:310–316. doi: 10.1111/jphd.12060. [DOI] [PubMed] [Google Scholar]
- 165.Kurki P., Korhonen M., Honkalampi K., Suominen A.L. Patients’ multifaceted views of dental fear in a diagnostic interview. Acta Odontol. Scand. 2021;79:194–204. doi: 10.1080/00016357.2020.1817545. [DOI] [PubMed] [Google Scholar]
- 166.Liinavuori A., Tolvanen M., Pohjola V., Lahti S. Longitudinal interrelationships between dental fear and dental attendance among adult Finns in 2000–2011. Community Dent. Oral Epidemiol. 2019;47:309–315. doi: 10.1111/cdoe.12458. [DOI] [PubMed] [Google Scholar]
- 167.Milgrom P., Coldwell S.E., Getz T., Weinstein P., Ramsay D.S. Four Dimensions of Fear of Dental Injections. J. Am. Dent. Assoc. 1997;128:756–762. doi: 10.14219/jada.archive.1997.0301. [DOI] [PubMed] [Google Scholar]
- 168.Moore R., Brodsgaard I., Mato T.K., Kwan H.W., Shiau Y.Y., Knudsen R. Fear of injections and report of negative dentist behav-ior among Caucasian American and Taiwanese adults from dental school clinics. Community Dent. Oral. Epidemiol. 1996;24:292–295. doi: 10.1111/j.1600-0528.1996.tb00862.x. [DOI] [PubMed] [Google Scholar]
- 169.Schneider A., Andrade J., Tanja-Dijkstra K., White M., Moles D.R. The psychological cycle behind dental appointment attendance: A cross-sectional study of experiences, anticipations, and behavioral intentions. Community Dent. Oral Epidemiol. 2016;44:364–370. doi: 10.1111/cdoe.12221. [DOI] [PubMed] [Google Scholar]
- 170.Singh K.A., Brennan D.S. Use of dental services among middle-aged adults: Predisposing, enabling and need variables. Aust. Dent. J. 2021;66:270–277. doi: 10.1111/adj.12828. [DOI] [PubMed] [Google Scholar]
- 171.Sohn W., Ismail A.I. Regular dental visits and dental anxiety in an adult dentate population. J. Am. Dent. Assoc. 2005;136:58–66. doi: 10.14219/jada.archive.2005.0027. [DOI] [PubMed] [Google Scholar]
- 172.Teo C.S., Foong W., Lui H.H., Vignehsa H., Elliott J., Milgrom P. Prevalence of dental fear in young adult Singaporeans. Int. Dent. J. 1990;40:37–42. [PubMed] [Google Scholar]
- 173.Yu J., Jiang R., Nie E.-M., Zhang C.-Y., Li X. The Prevalence of Dental Anxiety Associated with Pain among Chinese Adult Patients in Guangzhou. Pain Res. Manag. 2021;2021:7992580. doi: 10.1155/2021/7992580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Levin L., Eli L., Ashkenazi M. Dental Anxiety among Young Israeli Male Adults as Related to Treatment Received during Childhood. J. Public Health Dent. 2006;66:147–151. doi: 10.1111/j.1752-7325.2006.tb02571.x. [DOI] [PubMed] [Google Scholar]
- 175.Nelson C.I., Wright C.D., Brumbaugh J.T., Neiswanger K., Crout R.J., Lilly C.L., Marazita M.L., McNeil D.W. Predictors of use of dental care by children in north-central Appalachia in the USA. PLoS ONE. 2021;16:e0250488. doi: 10.1371/journal.pone.0250488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nair M.A., Shankarapillai R., Chouhan V. The dental anxiety levels associated with surgical extraction of tooth. Int. J. Dent. Clin. 2009;1:20–23. [Google Scholar]
- 177.Arnrup K., Broberg A.G., Berggren U., Bodin L. Lack of cooperation in pediatric dentistry--the role of child personality characteristics. Pediatr. Dent. 2002;24:119–128. [PubMed] [Google Scholar]
- 178.Gustafsson A., Arnrup K., Broberg A.G., Bodin L., Berggren U. Child dental fear as measured with the Dental Subscale of the Children’s Fear Survey Schedule: The impact of referral status and type of informant (child versus parent) Community Dent. Oral Epidemiol. 2010;38:256–266. doi: 10.1111/j.1600-0528.2009.00521.x. [DOI] [PubMed] [Google Scholar]
- 179.Klingberg G., Lofqvist L.V., Bjarnason S., Noren J.G. Dental behavior management problems in Swedish children. Community Dent. Oral Epidemiol. 1994;22:201–205. doi: 10.1111/j.1600-0528.1994.tb01841.x. [DOI] [PubMed] [Google Scholar]
- 180.Soares J.P., Cardoso M., Bolan M. Demystifying behaviour and dental anxiety in schoolchildren during endodontic treatment for primary teeth—controlled clinical trial. Int. J. Paediatr. Dent. 2019;29:249–256. doi: 10.1111/ipd.12468. [DOI] [PubMed] [Google Scholar]
- 181.Ten Berge M., Veerkamp J.S.J., Hoogstraten J., Prins P.J.M. The dental subscale of the children’s fear survey schedule: Predictive value and clinical usefulness. J. Psychopath. Behav. Assess. 2002;24:115–118. doi: 10.1023/A:1015392825448. [DOI] [Google Scholar]
- 182.AlGharebi S., Al Halabi M., Kowash M., Khamis A.H., Hussein I. Children’s dental anxiety (self and proxy reported) and its association with dental behaviour in a postgraduate dental hospital. Eur. Arch. Paediatr. Dent. 2021;22:29–40. doi: 10.1007/s40368-020-00517-x. [DOI] [PubMed] [Google Scholar]
- 183.Alshoraim M.A., El-Housseiny A.A., Farsi N.M., Felemban O.M., AlAmoudi N.M., Alandejani A.A. Effects of child characteristics and dental history on dental fear: Cross-sectional study. BMC Oral Health. 2018;18:33. doi: 10.1186/s12903-018-0496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Aminabadi N.A., Adhami Z.E., Oskouei S.G., Najafpour E., Jamali Z. Emotional Intelligence Subscales: Are They Correlated with Child Anxiety and Behavior in the Dental Setting? J. Clin. Pediatr. Dent. 2013;38:61–66. doi: 10.17796/jcpd.38.1.k754h164m3210764. [DOI] [PubMed] [Google Scholar]
- 185.Buldur B. Pathways between parental and individual determinants of dental caries and dental visit behaviours among children: Validation of a new conceptual model. Community Dent. Oral Epidemiol. 2020;48:280–287. doi: 10.1111/cdoe.12530. [DOI] [PubMed] [Google Scholar]
- 186.Gao S., Lu J., Li P., Yu D., Zhao W. Prevalence and risk factors of children’s dental anxiety in China: A longitudinal study. BMJ Open. 2021;11:e043647. doi: 10.1136/bmjopen-2020-043647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Klaassen M., Veerkamp J., Hoogstraten J. Predicting dental anxiety. The clinical value of anxiety questionnaires: An explora-tory study. Eur. J. Paediatr. Dent. 2003;4:171–176. [PubMed] [Google Scholar]
- 188.Milgrom P., Jie Z., Yang Z., Tay K.M. Cross-cultural validity of a parent’s version of the Dental Fear Survey Schedule for chil-dren in Chinese. Behav. Res. Ther. 1993;32:131–135. doi: 10.1016/0005-7967(94)90094-9. [DOI] [PubMed] [Google Scholar]
- 189.Nakai Y., Hirakawa T., Milgrom P., Coolidge T., Heima M., Mori Y., Ishihara C., Yakushiji N., Yoshida T., Shimono T. The Children’s Fear Survey Schedule-Dental Subscale in Japan. Community Dent. Oral Epidemiol. 2005;33:196–204. doi: 10.1111/j.1600-0528.2005.00211.x. [DOI] [PubMed] [Google Scholar]
- 190.Ramos-Jorge M.L., Marques L.S., Pavia S.M., Serra-Negra J.M., Pordeus I. Predictive factors for child behaviour in the dental environment. Eur. Arch. Paediatr. Dent. 2006;7:253–257. doi: 10.1007/BF03262561. [DOI] [PubMed] [Google Scholar]
- 191.Versloot J., Veerkamp J.S.J., Hoogstraten J. Dental anxiety and psychological functioning in children: Its relationship with behaviour during treatment. Eur. Arch. Paediatr. Dent. 2008;9:36–40. doi: 10.1007/BF03262654. [DOI] [PubMed] [Google Scholar]
- 192.Wogelius P., Poulsen S., Sørensen H.T. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol. Scand. 2003;61:178–183. doi: 10.1080/00016350310003468. [DOI] [PubMed] [Google Scholar]
- 193.Cademartori M.G., Costa V.P.P., Corrêa M.B., Goettems M.L. The influence of clinical and psychosocial characteristics on children behaviour during sequential dental visits: A longitudinal prospective assessment. Eur. Arch. Paediatr. Dent. 2020;21:43–52. doi: 10.1007/s40368-019-00444-6. [DOI] [PubMed] [Google Scholar]
- 194.Ihara Y., Fukuda K.-I., Saita N., Ichinohe T. Male Gender and High Trait Anxiety Are 2 Major Factors Associated With Severe Dental Fear and Avoidance. Anesth. Prog. 2018;65:177–180. doi: 10.2344/anpr-65-03-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Stein Duker L.I., Pham P.K., Polido J.C., Cermak S.A. Oral care and sensory over-responsivity in typically developing children. Pediatr. Dent. 2022 under review. [PubMed] [Google Scholar]
- 196.MacCormac C., Kinirons M. Reasons for referral of children to a general anaesthetic service in Northern Ireland. Int. J. Paediatr. Dent. 1998;8:191–196. doi: 10.1046/j.1365-263X.1998.00086.x. [DOI] [PubMed] [Google Scholar]
- 197.Rajavaara P., Rankinen S., Laitala M.-L., Vähänikkilä H., Yli-Urpo H., Koskinen S., Anttonen V. The influence of general health on the need for dental general anaesthesia in children. Eur. Arch. Paediatr. Dent. 2017;18:179–185. doi: 10.1007/s40368-017-0284-x. [DOI] [PubMed] [Google Scholar]
- 198.Savanheimo N., Vehkalahti M.M., Pihakari A., Numminen M. Reasons for and parental satisfaction with children’s dental care under general anaesthesia. Int. J. Paediatr. Dent. 2005;15:448–454. doi: 10.1111/j.1365-263X.2005.00681.x. [DOI] [PubMed] [Google Scholar]
- 199.Taskinen H., Kankaala T., Rajavaara P., Pesonen P., Laitala M.-L., Anttonen V. Self-reported causes for referral to dental treatment under general anaesthesia (DGA): A cross-sectional survey. Eur. Arch. Paediatr. Dent. 2014;15:105–112. doi: 10.1007/s40368-013-0071-2. [DOI] [PubMed] [Google Scholar]
- 200.Kopczynski K., Meyer B.D. Examining Parental Treatment Decisions within a Contemporary Pediatric Dentistry Private Practice. Patient Prefer. Adherence. 2021;15:645–652. doi: 10.2147/PPA.S300684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.MacPherson L.M.D., Pine C., Tochel C., Burnside G., Hosey M.T., Adair P. Factors influencing referral of children for dental extractions under general and local anaesthesia. Community Dent Health. 2005;22:282–288. [PubMed] [Google Scholar]
- 202.Ramdaw A., Hosey M.T., Bernabe E. Factors associated with use of general anaesthesia for dental procedures among British children. Br. Dent. J. 2017;223:339–345. doi: 10.1038/sj.bdj.2017.763. [DOI] [PubMed] [Google Scholar]
- 203.Boyle C.A., Newton J.T., Milgrom P. Who is referred for sedation for dentistry and why? Br. Dent. J. 2009;206:E12. doi: 10.1038/sj.bdj.2009.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Coolidge T., Irwin S.P., Leyster K.A., Milgrom P. Determinants of receiving intravenous sedation in a sample of dentally-fearful patients in the USA. SAAD Dig. 2012;28:52–60. [PMC free article] [PubMed] [Google Scholar]
- 205.Sirin Y., Yildirimturk S., Ay N. Do state-trait anxiety and previous unpleasant dental experiences predict the need for sedation in women having third molar surgery? Br. J. Oral Maxillofac. Surg. 2020;58:530–534. doi: 10.1016/j.bjoms.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 206.Tickle M., Williams M., Jenner T., Blinkhorn A. The effects of socioeconomic status and dental attendance on dental caries’ experience, and treatment patterns in 5-year-old children. Br. Dent. J. 1999;186:135–137. doi: 10.1038/sj.bdj.4800042. [DOI] [PubMed] [Google Scholar]
- 207.Menegazzo G.R., Knorst J.K., Emmanuelli B., Mendes F.M., Ardenghi D.M., Ardenghi T.M. Effect of routine dental attendance on child oral health-related quality of life: A cohort study. Int. J. Paediatr. Dent. 2019;30:459–467. doi: 10.1111/ipd.12625. [DOI] [PubMed] [Google Scholar]
- 208.Aldossary A., Harrison V.E., Bernabé E. Long-term patterns of dental attendance and caries experience among British adults: A retrospective analysis. Eur. J. Oral Sci. 2015;123:39–45. doi: 10.1111/eos.12161. [DOI] [PubMed] [Google Scholar]
- 209.Hagman J., Wide U., Werner H., Hakeberg M. Oral health and oral health behavior in young adults with caries disease. BDJ Open. 2021;7:1–6. doi: 10.1038/s41405-021-00084-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Crocombe L.A., Brennan D.S., Slade G.D. The influence of dental attendance on change in oral health-related quality of life. Community Dent. Oral Epidemiol. 2012;40:53–61. doi: 10.1111/j.1600-0528.2011.00634.x. [DOI] [PubMed] [Google Scholar]
- 211.Kvist T., Zedrén-Sunemo J., Graca E., Dahllöf G. Is treatment under general anaesthesia associated with dental neglect and dental disability among caries active preschool children? Eur. Arch. Paediatr. Dent. 2014;15:327–332. doi: 10.1007/s40368-014-0118-z. [DOI] [PubMed] [Google Scholar]
- 212.Lee H., Faundez L., Yarbrough C., Lewis C., LoSasso A. Patterns in Pediatric Dental Surgery under General Anesthesia across 7 State Medicaid Programs. JDR Clin. Transl. Res. 2020;5:358–365. doi: 10.1177/2380084420906114. [DOI] [PubMed] [Google Scholar]
- 213.Vinckier F., Gizani S., Declerck D. Comprehensive dental care for children with rampant caries under general anaesthesia. Int. J. Paediatr. Dent. 2001;11:25–32. doi: 10.1046/j.1365-263x.2001.00204.x. [DOI] [PubMed] [Google Scholar]
- 214.Arnrup K., Broberg A.G., Berggren U., Bodin L. Treatment outcome in subgroups of uncooperative child dental patients: An exploratory study. Int. J. Paediatr. Dent. 2003;13:304–319. doi: 10.1046/j.1365-263X.2003.00482.x. [DOI] [PubMed] [Google Scholar]
- 215.Williamson R., Oueis H., Casamassimo P.S., Thikkurissy S. Association between early childhood caries and behavior as meas-ured by the child behavior checklist. Pediatr. Dent. 2008;30:505–509. [PubMed] [Google Scholar]
- 216.Sullivan M.J., Neish N.R. Psychological predictors of pain during dental hygiene treatment. Probe. 1997;31:123–126. [PubMed] [Google Scholar]
- 217.Engel-Yeger B., Dunn W. Relationship between Pain Catastrophizing Level and Sensory Processing Patterns in Typical Adults. Am. J. Occup. Ther. 2011;65:e1–e10. doi: 10.5014/ajot.2011.09004. [DOI] [Google Scholar]
- 218.Meredith P.J., Rappel G., Strong J., Bailey K.J. Sensory Sensitivity and Strategies for Coping with Pain. Am. J. Occup. Ther. 2015;69:6904240010. doi: 10.5014/ajot.2015.014621. [DOI] [PubMed] [Google Scholar]
- 219.Granot M., Ferber S.G. The Roles of Pain Catastrophizing and Anxiety in the Prediction of Postoperative Pain Intensity: A prospective study. Clin. J. Pain. 2005;21:439–445. doi: 10.1097/01.ajp.0000135236.12705.2d. [DOI] [PubMed] [Google Scholar]
- 220.De Jongh A., Muris P., Ter Horst G., Van Zuuren F., De Wit C. Cognitive Correlates of Dental Anxiety. J. Dent. Res. 1994;73:561–566. doi: 10.1177/00220345940730021201. [DOI] [PubMed] [Google Scholar]
- 221.Brown J., Brown J., Woodburn J. Dental services for children with autism spectrum disorder. Learn Disabil. Pract. 2014;17:20–25. doi: 10.7748/ldp2014.03.17.3.20.e1527. [DOI] [Google Scholar]
- 222.Dunn W., Little L., Dean E., Robertson S., Evans B. The State of the Science on Sensory Factors and Their Impact on Daily Life for Children: A scoping review. OTJR: Occup. Particip. Health. 2016;36:S3–S26. doi: 10.1177/1539449215617923. [DOI] [PubMed] [Google Scholar]
- 223.Green D., Flanagan D. Understanding the autistic dental patient. Gen. Dent. 2008;56:167–171. [PubMed] [Google Scholar]
- 224.Khrautieo T., Srimaneekarn N., Rirattanapong P., Smutkeeree A. Association of sensory sensitivities and toothbrushing cooperation in autism spectrum disorder. Int. J. Paediatr. Dent. 2020;30:505–513. doi: 10.1111/ipd.12623. [DOI] [PubMed] [Google Scholar]
- 225.Kuhaneck H.M., Chisholm E.C. Improving dental visits for individuals with autism spectrum disorders through an understanding of sensory processing. Spéc. Care Dent. 2012;32:229–233. doi: 10.1111/j.1754-4505.2012.00283.x. [DOI] [PubMed] [Google Scholar]
- 226.Stein L.I., Polido J.C., Mailloux Z., Coleman G.G., Cermak S.A. Oral care and sensory sensitivities in children with autism spectrum disorders. Spéc. Care Dent. 2011;31:102–110. doi: 10.1111/j.1754-4505.2011.00187.x. [DOI] [PubMed] [Google Scholar]
- 227.Stein Duker L.I., Henwood B.F., Bluthenthal R.N., Juhlin E., Polido J.C., Cermak S.A. Parents’ perceptions of dental care challenges in male children with autism spectrum disorder: An initial qualitative exploration. Res. Autism Spectr. Disord. 2017;39:63–72. doi: 10.1016/j.rasd.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Stein Duker L.I., Floríndez L.I., Como D.H., Tran C.F., Henwood B.F., Polido J.C., Cermak S.A. Strategies for success: A qualitative study of caregiver and dentist approaches to improving oral care for children with autism. Pediatr. Dent. 2019;41:E4–E12. [PMC free article] [PubMed] [Google Scholar]
- 229.Stein Duker L.I. Adapting oral care protocols to support children with sensory sensitivities: Occupational therapy and dentis-try. In: Nelson T.M., Webb J.R., editors. Dental Care for Children with Special Needs: A Clinical Guide. Springer; Cham, Switzerland: 2019. pp. 77–98. [Google Scholar]
- 230.Thomas N., Blake S., Morris C., Moles D.R. Autism and primary care dentistry: Parents’ experiences of taking children with autism or working diagnosis of autism for dental examinations. Int. J. Paediatr. Dent. 2017;28:226–238. doi: 10.1111/ipd.12345. [DOI] [PubMed] [Google Scholar]
- 231.Stein Duker L.I., Richter M., Lane C.J., Polido J.C., Cermak S.A. Oral care experiences and challenges for children with Down syndrome: Reports from caregivers. Pediatr. Dent. 2020;42:430–435. [PMC free article] [PubMed] [Google Scholar]
- 232.Stein Duker L.I., Martinez M., Lane C.J., Polido J.C., Cermak S.A. Association between oral care challenges and sensory over-responsivity in children with Down syndrome. Int. J. Paediatr. Dent. 2021:1–12. doi: 10.1111/ipd.12933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Ghanizadeh A. Parents reported oral sensory sensitivity processing and food preference in ADHD. J. Psychiatr. Ment. Health Nurs. 2013;20:426–432. doi: 10.1111/j.1365-2850.2011.01830.x. [DOI] [PubMed] [Google Scholar]
- 234.National Institute of Dental and Craniofacial Research Practical Oral Care for People with Autism. NIH Publication No. 09-5190. [(accessed on 1 November 2021)];2019 Available online: https://www.nidcr.nih.gov/sites/default/files/2017-09/practical-oral-care-autism.pdf.
- 235.Bradt J., Teague A. Music interventions for dental anxiety. Oral Dis. 2018;24:300–306. doi: 10.1111/odi.12615. [DOI] [PubMed] [Google Scholar]
- 236.Goettems M.L., Zborowski E.J., Costa F.D.S., Costa V.P.P., Torriani D.D. Nonpharmacologic Intervention on the Prevention of Pain and Anxiety During Pediatric Dental Care: A Systematic Review. Acad. Pediatr. 2017;17:110–119. doi: 10.1016/j.acap.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 237.Prado I.M., Carcavalli L., Abreu L.G., Serra-Negra J.M., Paiva S.M., Martins C.C. Use of distraction techniques for the management of anxiety and fear in paediatric dental practice: A systematic review of randomized controlled trials. Int. J. Paediatr. Dent. 2019;29:650–668. doi: 10.1111/ipd.12499. [DOI] [PubMed] [Google Scholar]
- 238.Weisfeld C.C., Turner J.A., Dunleavy K., Ko A., Bowen J.I., Roelk B., Eissa R., Benfield E., Robertson K. Dealing with Anxious Patients: A Systematic Review of the Literature on Nonpharmaceutical Interventions to Reduce Anxiety in Patients Undergoing Medical or Dental Procedures. J. Altern. Complement. Med. 2021;27:717–726. doi: 10.1089/acm.2020.0504. [DOI] [PubMed] [Google Scholar]
- 239.Aditya P., Prasad M.G., Nagaradhakrishna A., Raju N.S., Babu D.N. Comparison of effectiveness of three distraction techniques to allay dental anxiety during inferior alveolar nerve block in children: A randomized controlled clinical trial. Heliyon. 2021;7:e08092. doi: 10.1016/j.heliyon.2021.e08092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Asokan S., Priya P.G., Natchiyar S.N., Elamathe M. Effectiveness of distraction techniques in the management of anxious chil-dren—A randomized controlled pilot trial. J. Indian Soc. Pedod. Prev. Dent. 2020;38:407–412. doi: 10.4103/JISPPD.JISPPD_435_20. [DOI] [PubMed] [Google Scholar]
- 241.Azher U., Srinath S.K., Nayak M. Effectiveness of Bubble Breath Play Therapy in the Dental Management of Anxious Children: A Pilot Study. J. Contemp. Dent. Pract. 2020;21:17–21. doi: 10.5005/jp-journals-10024-2741. [DOI] [PubMed] [Google Scholar]
- 242.Kharouba J., Peretz B., Blumer S. The effect of television distraction versus Tell-Show-Do as behavioral management techniques in children undergoing dental treatments. Quintessence Int. 2020;51:486–494. doi: 10.3290/j.qi.a44366. [DOI] [PubMed] [Google Scholar]
- 243.Pande P., Rana V., Srivastava N., Kaushik N. Effectiveness of different behavior guidance techniques in managing children with negative behavior in a dental setting: A randomized control study. J. Indian Soc. Pedod. Prev. Dent. 2020;38:259–265. doi: 10.4103/JISPPD.JISPPD_342_20. [DOI] [PubMed] [Google Scholar]
- 244.Garrocho-Rangel A., Ibarra-Gutiérrez E., Rosales-Bérber M., Esquivel-Hernández R., Esparza-Villalpando V., Pozos-Guillén A. A video eyeglasses/earphones system as distracting method during dental treatment in children: A crossover randomised and controlled clinical trial. Eur. J. Paediatr. Dent. 2018;19:74–79. doi: 10.23804/ejpd.2018.19.01.14. [DOI] [PubMed] [Google Scholar]
- 245.Jimeno F.G., Bellido M.M., Fernández C.C., Rodríguez A.I.L., Pérez J.L., Quesada J.R.B. Effect of audiovisual distraction on children’s behaviour, anxiety and pain in the dental setting. Eur. J. Paediatr. Dent. 2015;15:297–302. [PubMed] [Google Scholar]
- 246.Marwah N., Prabhakar A.R., Raju O.S. Music distraction-its efficacy in management of anxious pediatric dental patients. J. Indian Soc. Pedod. Prev. Dent. 2005;23:168–170. doi: 10.4103/0970-4388.19003. [DOI] [PubMed] [Google Scholar]
- 247.Torres-Gomez J., Arnason S., Hoopes W., Vandewalle K. Management of dental anxiety via distraction technique. J. Clin. Exp. Dent. 2021;13:e350–e356. doi: 10.4317/jced.57660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Alnamankany A. Video modelling and dental anxiety in children. A randomised clinical trial. Eur. J. Paediatr. Dent. 2019;20:242–246. doi: 10.23804/ejpd.2019.20.03.14. [DOI] [PubMed] [Google Scholar]
- 249.Elangovan A., Mungara J., Injeti M., Joseph E., Sakthivel R., Selvaraju G. Child’s dental fear: Cause related factors and the influence of audiovisual modeling. J. Indian Soc. Pedod. Prev. Dent. 2013;31:215. doi: 10.4103/0970-4388.121815. [DOI] [PubMed] [Google Scholar]
- 250.Sakthivel R., Poornima V., Jayanthi M., Nilaya Reddy V., Selvaraju G., Sakthivel M.R. Evaluation of anxiety and the effect of modeling in children undergoing orthopantomographic examination. J. Indian Acad. Oral. Med. Radiol. 2013;25:274–277. [Google Scholar]
- 251.Karekar P., Bijle M.N., Walimbe H. Effect of Three Behavior Guidance Techniques on Anxiety Indicators of Children Undergoing Diagnosis and Preventive Dental Care. J. Clin. Pediatr. Dent. 2019;43:167–172. doi: 10.17796/1053-4625-43.3.4. [DOI] [PubMed] [Google Scholar]
- 252.Howard K.E., Freeman R. An evaluation of the PALS after treatment modelling intervention to reduce dental anxiety in child dental patients. Int. J. Paediatr. Dent. 2009;19:233–242. doi: 10.1111/j.1365-263X.2009.00977.x. [DOI] [PubMed] [Google Scholar]
- 253.Farhat-McHayleh N., Harfouche A., Souaid P. Techniques for managing behaviour in pediatric dentistry: Comparative study of live modelling and tell-show-do based on children’s heart rates during treatment. J. Can. Dent. Assoc. 2009;75:283. [PubMed] [Google Scholar]
- 254.Vishwakarma A.P., Bondarde P.A., Patil S.B., Dodamani A., Vishwakarma P.Y., Mujawar S.A. Effectiveness of two different behavioral modification techniques among 5–7-year-old children: A randomized controlled trial. J. Indian Soc. Pedod. Prev. Dent. 2017;35:143–149. doi: 10.4103/JISPPD.JISPPD_257_16. [DOI] [PubMed] [Google Scholar]
- 255.Liu Y., Gu Z., Wang Y., Wu Q., Chen V., Xu X., Zhou X. Effect of audiovisual distraction on the management of dental anxiety in children: A systematic review. Int. J. Paediatr. Dent. 2018;29:14–21. doi: 10.1111/ipd.12430. [DOI] [PubMed] [Google Scholar]
- 256.Robertson M., Araujo M.P., Innes N. Anxiety and fear management in paediatric dentistry using distraction techniques. Evid. Based Dent. 2019;20:50–51. doi: 10.1038/s41432-019-0020-y. [DOI] [PubMed] [Google Scholar]
- 257.Zhang C., Qin D., Shen L., Ji P., Wang J. Does audiovisual distraction reduce dental anxiety in children under local anesthesia? A systematic review and meta-analysis. Oral Dis. 2017;25:416–424. doi: 10.1111/odi.12849. [DOI] [PubMed] [Google Scholar]
- 258.Boman U.W., Carlsson V., Westin M., Hakeberg M. Psychological treatment of dental anxiety among adults: A systematic review. Eur. J. Oral Sci. 2013;121:225–234. doi: 10.1111/eos.12032. [DOI] [PubMed] [Google Scholar]
- 259.Coldwell S.E., Getz T., Milgrom P., Prall C.W., Spadafora A., Ramsay D.S. CARL: A LabVIEW 3 computer program for conducting exposure therapy for the treatment of dental injection fear. Behav. Res. Ther. 1998;36:429–441. doi: 10.1016/S0005-7967(97)10038-9. [DOI] [PubMed] [Google Scholar]
- 260.Coldwell S.E., Wilhelm F.H., Milgrom P., Prall C.W., Getz T., Spadafora A., Chiu I.-Y., Leroux B.G., Ramsay D.S. Combining alprazolam with systematic desensitization therapy for dental injection phobia. J. Anxiety Disord. 2007;21:871–887. doi: 10.1016/j.janxdis.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 261.Hauge M.S., Stora B., Vassend O., Hoffart A., Willumsen T. Dentist-administered cognitive behavioural therapy versus four habits/midazolam: An RCT study of dental anxiety treatment in primary dental care. Eur. J. Oral Sci. 2021;129:e12794. doi: 10.1111/eos.12794. [DOI] [PubMed] [Google Scholar]
- 262.Kebriaee F., Shirazi A.S., Fani K., Moharreri F., Soltanifar A., Khaksar Y., Mazhari F. Comparison of the effects of cognitive behavioural therapy and inhalation sedation on child dental anxiety. Eur. Arch. Paediatr. Dent. 2014;16:173–179. doi: 10.1007/s40368-014-0152-x. [DOI] [PubMed] [Google Scholar]
- 263.Kvale G., Berggren U., Milgrom P. Dental fear in adults: A meta-analysis of behavioral interventions. Community Dent. Oral Epidemiol. 2004;32:250–264. doi: 10.1111/j.1600-0528.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 264.Öst L.G., Kvale G. Effects of cognitive behavioural treatments: A systematic review and meta-analysis. In: Öst L.G., Skaret E., editors. Cognitive Behaviour Therapy for Dental Phobia and Anxiety. Wiley-Blackwell; Hoboken, NJ, USA: 2013. pp. 163–182. [Google Scholar]
- 265.Porritt J., Rodd H., Morgan A., Williams C., Gupta E., Kirby J., Creswell C., Newton T., Stevens K., Baker S., et al. Development and Testing of a Cognitive Behavioral Therapy Resource for Children’s Dental Anxiety. JDR Clin. Transl. Res. 2017;2:23–37. doi: 10.1177/2380084416673798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Shahnavaz S., Hedman-Lagerlöf E., Grindefjord M., Reuterskiöld L., Dahllöf G. Cognitive Behavioral Therapy for Children with Dental Anxiety: A randomized controlled trial. JDR Clin. Transl. Res. 2016;1:234–243. doi: 10.1177/2380084416661473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Shahnavaz S., Hedman-Lagerlöf E., Hasselblad T., Reuterskiold L., Kaldo V., Dahllöf G. Internet-Based Cognitive Behavioral Therapy for Children and Adolescents With Dental Anxiety: Open Trial. J. Med. Internet Res. 2018;20:e12. doi: 10.2196/jmir.7803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Heyman R., Wojda A., Eddy J., Haydt N., Geiger J., Slep A.S. Dentist-Perceived Barriers and Attractors to Cognitive-Behavioral Treatment Provided by Mental Health Providers in Dental Practices. Adv. Dent. Res. 2018;29:35–41. doi: 10.1177/0022034517737023. [DOI] [PubMed] [Google Scholar]
- 269.Hmud R., Walsh L.J. Dental anxiety: Causes, complications and management approaches. J. Minim. Interv. Dent. 2009;2:67–78. [Google Scholar]
- 270.Walsh L.J. Anxiety prevention: Implementing the 4 S principle in conservative dentistry. Auxilliary. 2007;17:24–26. [Google Scholar]
- 271.Cai H., Xi P., Zhong L., Chen J., Liang X. Efficacy of aromatherapy on dental anxiety: A systematic review of randomised and quasi-randomised controlled trials. Oral Dis. 2021;27:829–847. doi: 10.1111/odi.13346. [DOI] [PubMed] [Google Scholar]
- 272.Arslan I., Aydinoglu S., Karan N.B. Can lavender oil inhalation help to overcome dental anxiety and pain in children? A randomized clinical trial. Eur. J. Pediatr. 2020;179:985–992. doi: 10.1007/s00431-020-03595-7. [DOI] [PubMed] [Google Scholar]
- 273.Ghaderi F., Solhjou N. The effects of lavender aromatherapy on stress and pain perception in children during dental treatment: A randomized clinical trial. Complement. Ther. Clin. Pract. 2020;40:101182. doi: 10.1016/j.ctcp.2020.101182. [DOI] [PubMed] [Google Scholar]
- 274.Jadhav G.R., Mittal P. Evaluation of aromatherapy on success rate of inferior alveolar nerve block in teeth with irreversible pulpitis: A prospective randomized clinical trial. Quintessence Int. 2020;51:864–870. doi: 10.3290/j.qi.a45172. [DOI] [PubMed] [Google Scholar]
- 275.Purohit A., Singh A., Purohit B., Shakti P., Shah N. Is aromatherapy associated with patient’s dental anxiety levels? A systematic review and meta-analysis. J. Dent. Anesthesia Pain Med. 2021;21:311–319. doi: 10.17245/jdapm.2021.21.4.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Chen H.Y., Yang H., Chi H.J., Chen H.M. Physiological effects of deep touch pressure on anxiety alleviation: The weighted blanket approach. J. Med. Biol. Eng. 2012;33:463–470. doi: 10.5405/jmbe.1043. [DOI] [Google Scholar]
- 277.Chen H.-Y., Yang H., Meng L.-F., Chan P.-Y.S., Yang C.-Y. Effect of deep pressure input on parasympathetic system in patients with wisdom tooth surgery. J. Formos. Med. Assoc. 2016;115:853–859. doi: 10.1016/j.jfma.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 278.Chen H.-Y., Yang H., Chi H.-J., Chen H.-M. Parasympathetic effect of deep pressure input on third molar extraction in adolescents. J. Formos. Med Assoc. 2019;118:1317–1324. doi: 10.1016/j.jfma.2019.05.026. [DOI] [PubMed] [Google Scholar]
- 279.Shapiro M., Melmed R.N., Sgan-Cohen H.D., Eli I., Parush S. Behavioural and physiological effect of dental environment sensory adaptation on children’s dental anxiety. Eur. J. Oral Sci. 2007;115:479–483. doi: 10.1111/j.1600-0722.2007.00490.x. [DOI] [PubMed] [Google Scholar]
- 280.Shapiro M., Sgan-Cohen H.D., Parush S., Melmed R.N. Influence of Adapted Environment on the Anxiety of Medically Treated Children with Developmental Disability. J. Pediatr. 2009;154:546–550. doi: 10.1016/j.jpeds.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 281.Shapiro M., Melmed R.N., Sgan-Cohen H.D., Parush S. Effect of sensory adaptation on anxiety of children with developmental disabilities: A new approach. Pediatr. Dent. 2009;31:222–228. [PubMed] [Google Scholar]
- 282.Kim G., Carrico C., Ivey C., Wunsch P.B. Impact of sensory adapted dental environment on children with developmental disabilities. Spéc. Care Dent. 2019;39:180–187. doi: 10.1111/scd.12360. [DOI] [PubMed] [Google Scholar]
- 283.Potter C.N., Wetzel J.L., Learman K.E. Effect of sensory adaptations for routine dental care in individuals with intellectual and developmental disabilities: A preliminary study. J. Intellect. Dev. Disabil. 2019;44:305–314. doi: 10.3109/13668250.2017.1409597. [DOI] [Google Scholar]
- 284.American Academy of Pediatric Dentistry . The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry; Chicago, IL, USA: 2021. Behavior guidance for the pediatric dental patient; pp. 306–324. [Google Scholar]