Abstract
Extensive research has indicated food insecurity to be associated with depressive symptoms, both of which have been indicated to increase globally during the COVID-19 pandemic. Few studies, however, have made use of nationally representative and longitudinal data to investigate this relationship, making causal claims difficult. In South Africa (SA), as with other low- and middle-income contexts, population-based studies have generally focused on mothers during the perinatal period and other vulnerable groups. This study made use of Cross-Lagged Dynamic Panel Models to examine the relationship between household food insecurity and the depressive symptoms of adults across three waves of the National Income Dynamics Survey–Coronavirus Rapid Mobile Survey (NIDS-CRAM) study collected in 2020 and 2021, a dataset nationally representative of all adults in SA in 2017. Stratification of the sample by gender, parenthood and marital statuses allowed for the assessment of gender differences in family roles that might account for differential impacts of food insecurity on mental health outcomes. The findings of this study indicated a significant impact of food insecurity on the depressive symptoms of adults. Controlling for stable trait-like individual differences eliminated much of this relationship, indicating partial or full mediation by unobserved factors. Gender differences in food security's association with depressive symptoms amongst cohabitating parents following the inclusion of individual effects provided support for a gendered role response. These findings provide further evidence of the complex interactions between sex, gender and health.
Keywords: Longitudinal analysis, Mental health, Caregiving, Gender roles, South Africa
1. Introduction
The global COVID-19 pandemic has contributed significantly to an upward trend in food insecurity: Between 2019 and 2020, moderate and severe food insecurity rose by as much as it had in the previous five years combined (UNICEF, 2021). Here, food insecurity (FI) is defined as a limited or uncertain access to the quantity and quality of food necessary for active healthy lives or being unable to procure food through socially acceptable means (Anderson, 1990). The Food and Agriculture Organization (FAO) of the United Nations put the number of people going hungry globally in 2020 between 720 and 811 million, of which roughly 15% could be classified as chronically hungry. This represents an increase of 118 million when compared to 2019 (O et al., 2020).
In 2019, 15% of South African (SA) households reported running out of money to buy food over the past year. Research by Van der Berg and colleagues (Van der Berg et al., 2021) showed that in the initial months of the pandemic in SA, the rate of households reporting running out of money to buy food had risen steeply 47%, and rates of adult and child hunger had doubled to 15–21%. It was further indicated that more than a year after the pandemic was first declared, rates of FI in SA have not declined, and are significantly higher amongst households with children.
Global rates of depressive symptomology and psychological distress have similarly risen during the pandemic, particularly at its onset. A cross-country study of mental health outcomes amongst a sample of respondents predominantly from Europe, North Africa and Western Asia reported depressive symptom prevalence of 17.5% in April 2020 (Ammar et al., 2020), representing a 136% increase from pre-COVID levels. Nationally representative analyses of psychological responses during the early stages of the pandemic in China (Wang et al., 2020; Huang and Zhao, 2020) and Italy (Rossi et al., 2020), two of the initially worst hit nations, indicated similar prevalence of 16.5–20.1%. Nationally representative estimates for the United States (US) indicated a more than three-fold increase in depressive symptom prevalence between 2018 and 2020 (McGinty et al., 2020).
Data on the mental health consequences of COVID-19 in low- and middle-income countries (LMICs) has been, apart from China, rather limited, and in many cases neither population-based nor nationally representative. One of the few population-based studies of mental health responses in LMICs comes from Bangladesh (Newman, 2013), in which it was estimated that depressive symptom prevalence had increased from 25.3% pre-COVID (Mamun et al., 2021) to 33% in April 2020. A third of SA adults were similarly found to self-report depressive symptoms during the first three weeks of SA's hard lockdown (Human Sciences Research C, 2020). This can be compared to a pre-COVID (2017) estimate of 17% (Posel et al., 2021). Analysis of nationally representative data collected during the COVID-19 pandemic revealed that 24–29% of SA adults continued to demonstrate high levels of depressive symptoms at any time between July 2020 and May 2021, and at least half of SA adults had experienced depressive symptoms ever since the pandemic's onset (Hunt et al., 2021).
A growing empirical literature in both developed and developing country contexts has demonstrated FI to be a factor associated with greater depressive symptomology, independent of other well-documented risk factors such as poverty and low socioeconomic status (Wu and Schimmele, 2005; Weaver and Hadley, 2009; Jones, 2017; Joseph et al., 2021). This association has been established in adult populations (Sorsdahl et al., 2011; Martin et al., 2016; Allen et al., 2018; Perkins et al., 2018a), adolescent populations (Jebena et al., 2016; Rani et al., 2018; Fertig, 2019; Jesson et al., 2021), as well as amongst vulnerable groups (Normen et al., 2005; Maharaj et al., 2017).
The impact of FI on the psychological distress of adults is not well established in SA, and most studies have focused on relatively small, non-representative samples such as women during the perinatal period (Zar et al., 2019; Garman et al., 2019; Abrahams et al., 2018) and informal women workers with young children (Horwood et al., 2021). The consistency with which households, particularly those with children as residents, experience FI in SA, and the significant increase in rates of food insecurity, hunger, and depressive symptoms during the COVID-19 pandemic, demands a more systematic understanding of the pathways linking these outcomes. Therefore, this paper aims to build on the limited evidence on the relations between FI and depressive symptoms during the COVID-19 pandemic from the Global South using the case of South Africa. This association will be tested whilst controlling for confounding by sociodemographic factors known to determine food insecurity and depressive symptomology.
This study further aims to fill important gaps within the existing literature on gender differences in this relationship through considering the gender norms associated with and signified by marital and parental statuses (Ciciurkaite and Brown, 2018). Reductionist explanations for gender differences in depressive symptom prevalence tend to point towards singular causal biological and genetic factors, such as female hormones (Quinones, 2001) and hereditability (Kendler et al., 2001), as responsible. However, this tends to discount environmental contributors and the complex social experiences of men and women (Chonody and Siebert, 2008). Gender is not simply an artificact of biology but socially constructed and distinguished by “relationally defined social practice [s]” (Hatcher, 1993:108) (Hatcher, 1993).
It is for this reason that gender theory posits gender — defined as the socially constructed norms, behaviors and roles associated with men and women — to be the primary determinant of individual behavior in families (Ferree, 1990). Therefore, rather than adopting a sex differences approach that simply focuses on overall rates of depressive symptoms in men and women, this study adopts a gender theory approach that considers the social circumstances in which food insecurity has the greatest psychological impact for different men and women. This will assist in creating interventions targeted at individuals most affected by food FI and, consequently, most in need of assistance.
All but one of the handful of studies investigating gender differences in the food-security-depression relationship emanate from the Global North, and all are cross-sectional in nature (Wu and Schimmele, 2005; Ciciurkaite and Brown, 2018; Carter et al., 2011; Tseng et al., 2017; Lee et al., 2020a; Perkins et al., 2018b). The evidence indicates that both men and women are psychologically affected by FI, with some differences in the relative size of this relationship. To the best of the author's knowledge, only the studies of Ciciurkaite and Brown (2018) and Lee and colleagues (Lee et al., 2020a) take account of the interactions between gendered status roles and food insecurity in determining mental health outcomes.
Linear and non-linear regression techniques that do not fully deal with issues of omitted variables and causal direction are predominantly used for determining the FI-psychological-distress relationship. When panel data is available, the Cross-Lagged Panel Model (CLPM) has proven to be the most popular as it is able to investigate reciprocal influences between FI and depressive symptoms, as well as control for temporal stability in these variables (Biesanz and Hoyle, 2012). However, much criticism has been targeted at the CLPM, particularly for its inability to deal with omitted variable bias and separate out within- and between-person effects (Hamaker et al., 2015). Specifically, CLPM assumes that every person varies around a common group average in each of the covariates, when in reality “individuals [can] fluctuate around a person-specific mean that is higher for some individuals than for others” (Mund et al., 2019:4) (Mund and Nestler, 2019). Failure to account for these stable individual differences means that within- and between-person effects are conflated, leading to spurious findings (Hamaker et al., 2015; Berry and Willoughby, 2017).
The final, and possibly most important aim of this study, then, is to not only confirm existing findings on gender differences in FIs association with depressive symptomology, but to also determine whether the estimated relationships are robust to the inclusion of individual effects that capture, for example, differences in attitudes towards gender, social role beliefs, personality traits such as neuroticism, and masculinity/femininity self-constructions that could account for differences in the psychological impact of FI. Factors such as these have been indicated to correlate significantly with the depressive symptoms of women and men (Wupperman and Neumann, 2006; Addis, 2008; Thomeer et al., 2013), as well as with markers of poverty and socioeconomic status (Kågesten et al., 2016; Heise et al., 2019; Hatcher et al., 2019; Gibbs et al., 2018). This is achieved using data from a nationally representative, repeated cross-sectional survey together with a Fixed Effects Cross-Lagged Dynamic Panel method (Allison et al., 2017) that not only addresses issues of unobserved heterogeneity and simultaneity, but also problems of incidental parameters and the treatment of initial conditions that are common to dynamic panel models.
In the section that follows, several competing theories and hypotheses that link depressive symptoms and food insecurity to gender and its intersection with family roles are discussed and used to frame the hypotheses to be tested.
2. Food insecurity, psychological distress, and gender and family roles
Aside from the physiological effects of acute hunger such as emotional regulation depletion (Kruger and Lourens, 2016), the link between FI and psychological distress in family context is most often explained through the family stress framework (Conger et al., 2002). Specifically, adverse events such as a loss of income and employment lead to household strain and interpersonal conflict and, consequently, stress and adverse behavioral and mental health outcomes (Gee and Asim, 2018; Johnson and Markowitz, 2018).
The impact of FI on the psychological health of mothers has been of primary interest in empirical research, with little attention paid to paternal mental health (Tseng et al., 2017; Myers, 2020). This focus is conceivably because the burden of domestic responsibilities falls disproportionately on mothers and other female caregivers (Sevilla and Smith, 2020; Zamarro and Prados, 2021), and therefore women may be generally considered to be disproportionately impacted by stressors linked to providing for the physical and emotional needs of one's family (Simon, 1995). Furthermore — and perhaps relatedly — women have been indicated to report higher internalized indicators of psychological distress such as depressive symptoms than do men (McDonough and Walters, 2001). Men, conversely, have been shown to express psychological distress through greater substance abuse, anger, and somatic symptoms (Brown and Richman, 2012; Pollack et al., 1998; Leimkühler et al., 2007), and are less likely to make use of mental health services when experiencing depressive symptoms (Cleary, 2005; Addis and Mahalik, 2003), which is implicated in higher rates of suicide amongst men (Cleary, 2012).
The gendered response framework (Morrow and Nolen-Hoeksema, 1990) hypothesizes differences in socialization and life experiences that inform individuals' self-concept as responsible for the difference with which psychological distress manifests in men and women. For example, higher depressive symptomology amongst women parallels with a greater tendency amongst women to engage in ruminative responses, defined as persistent thoughts focusing on depressive symptoms and possible causes (Butler and Nolen-Hoeksema, 1994). Alignment to and failure to meet masculine ideals (e.g. traditional breadwinner and provider roles) have been shown to trigger externalizing problems and unhealthy coping (e.g. substance abuse), prompting suicidal ideation (Brownhill et al., 2005; Oliffe et al., 2012). Research focusing on men's help-seeking behavior has indicated a lower likelihood of seeking help to be related to conformity to masculine role norms and fear of rejection from significant others, as well as perceptions that the problem is non-normative and might be central to one's character or personality (Möller-Leimkühler, 2002).
Similarly, gendered responses to FI can be related to the specific challenges that economic hardship poses for men and women, many of which are tied to gendered roles in parenthood and marriage. Gender norms, roles, and behaviors, and by extension the “family identity”, are continually challenged and reformed. This is evidenced by women's use of other women to care for their children, increased participation of women in the labor market, changing technologies that allow for women to be “fathers”, as well as changing expectations of contemporary fatherhood (Sharp, 2010). However, even though there is no universal form of masculinity or femininity that can be applied to all societies at all times, the cultural pressures of hegemony mean that domestic duties do not yet fit within contemporary notions of masculinity. As such, care and household work continue to be interpreted as subordinate to financial provider roles, and therefore fall outside of masculine ideals (Connell, 1987; Coltrane, 2000).
According to social control theory (Durkheim, 1897/1951; Umberson, 1987), relationships and social bonds can regulate risky or unhealthy behavior. For example, cohabitation with a spouse or partner can provide a buffer against the negative effect of social stressors on mental health through the monitoring of healthy and unhealthy behaviors, as well as provide emotional and social support (Umberson, 1992; Umberson et al., 2013). Empirical evidence has found support for a positive effect of marriage on the psychological wellbeing of both men and women (Wu and Schimmele, 2005; Ciciurkaite and Brown, 2018; Lee et al., 2020a; Ross and Mirowsky, 1989; Brown, 2000), as well as indicated it to moderate the impact of social stressors on psychological distress (Dooley et al., 2000; Bierman, 2009). Social control theory, then, supports a role for gender norms in influencing the cushioning effect of marriage on individual mental health.
In the context of FI specifically, it is expected that women, in the role of primary caregiver and nurturer, are more likely to take on the burden of sacrificing their own nutritional needs and shielding their family from hunger when faced with food insecurity (Dinour et al., 2007), leading to increased stress (McIntyre et al., 2003; Olson, 2005). There are, then, arguably greater benefits from marriage and cohabitation for men than for women under adverse circumstances, as the latter group is more likely to monitor and regulate the health behaviors of the former. Numerous studies have found empirical evidence in support of a lower prevalence of depressive symptoms amongst married men compared to married women (Umberson et al., 2010; Grundström et al., 2021). Other research has suggested that masculine ideals assist men in masking their emotional expression and depression from public view through a reliance on female partners for emotional support in private (Coen et al., 2013).
Several studies have investigated whether the influence of marital status on psychological distress changes by experiences of FI. Hanson et al. (2007) find significantly higher levels of obesity linked to the consumption of calorically dense, nutritionally sparse foods amongst married women in food insecure households when compared to their unmarried and/or food secure counterparts. This, they argue, suggests a privileging of husband's nutritional needs, as no such effects were observed by either marital or food security status amongst men. Brown and Circiukaite (Ciciurkaite and Brown, 2018), conversely, find no significant moderating effect of marriage on the impact of FI on the depressive symptoms of either men or women in the US, although marriage is predicted to provide significant protective effects against alcohol abuse amongst men in the context of fully and marginally food secure households. Lee et al. (2020b) find married Korean men to experience the lowest levels of perceived depression regardless of food security status, and significantly lower rates of depression when compared to their single and divorced/widowed/separated counterparts in food insecure contexts.
Parenthood's association with psychological distress is, however, less straightforward than that of marital status, particularly given that parenthood can be both burdensome and rewarding (Nomaguchi, 2012). It is generally held that when children are minors the costs outweigh the benefits, whilst the converse is true once children are in adulthood (Umberson et al., 2010). This is supported by research that finds the psychological well-being of parents to be lower than that of childless adults during younger adulthood and when children are young (Nomaguchi and Milkie, 2003). However, evidence of lower levels of depression and higher self-esteem amongst those with children under 5 years old when compared to parents with children of school-going age has also been found (Nomaguchi, 2012). No significant differences in the levels of well-being amongst parents and childless adults have been evidenced at midlife and when children are adults (Pudrovska, 2008; Koropeckyj-Cox and Call, 2007). Overall, existing literature has determined that the contexts of marital status (Nomaguchi and Milkie, 2003; Zhang and Hayward, 2001; Kendig et al., 2007; Woo and Raley, 2005), gender (Tseng et al., 2017), and the timing of transition to parenthood can all exert important influences on the effects of parenthood on psychological distress (Knoester and Eggebeen, 2006; Booth et al., 2008; Mirowsky and Ross, 2002).
This ambiguity in the parenthood-psychological-distress relationship is somewhat removed once the research focus turns to stress factors that conflict with the ability to provide for children's needs, such as work-family balance and FI. In general, the negative effects of child-care stress are greatest amongst women, and low-income and single parents (Nomaguchi and Milkie, 2003; Crouter and Booth, 2014). Several early seminal studies concluded that the strain of the multiple roles of homemaker, parent and spouse placed severe demands on employed women, contributing to increased stress and frustration (Pearlin, 1975; Pearlin and Johnson, 1977). In recent decades, studies of dual-earner homes have found role strains to contribute to the increased psychological distress of mothers but not fathers (Nomaguchi et al., 2005), and that this is correlated with more traditional views of gender roles within the home (Goldberg and Perry-Jenkins, 2004).
Similarly, gender norms have been shown to have important consequences for psychological wellbeing in food insecure households. For example, gender roles and social expectations prescribe that a mother put the needs and well-being of her children before her own (DeVault, 1994), which includes shielding one's children from food insecurity and hunger. “Maternal deprivation” in response to an uncertain or limited access to food has been empirically linked to heightened stress and depressive symptoms amongst women (Whitaker et al., 2006; Hadley and Patil, 2006; Weigel et al., 2016), as well as obesity (Martin and Lippert, 2012).
Normative expectations can, however, also have consequences for fathers in the contexts of FI and economic hardship, as these can trigger perceptions of failed fatherhood and an inability to fulfill patriarchal roles of primary breadwinner and provider. Additionally, psychological distress linked to FI is further exacerbated when social stigma discourages men from seeking psychological assistance, as referred to earlier. Wu and Schimmele (2005), for example, found that although FI was related to higher rates of depressive symptoms amongst women than men, single fathers were the most negatively impacted of all groups. Tseng et al. (2017) find more pronounced levels of serious psychological distress among fathers than mothers, which they link to perceptions of failure to meet one's obligation as primary provider.
2.1. Hypotheses
The discussion above highlights the need to not only consider heterogeneous associations between FI and psychological distress by gender, but also that these differences may be explained by norms and roles that are played out in marriage and parenthood. In this regard, this study tests the following hypotheses:
(1) Hypothesis 1
Women present with greater prevalence of depressive symptoms than men.
(2) Hypothesis 2
Food insecurity is associated with higher depressive symptoms amongst both men and women.
(3) Hypothesis 3
Cohabitating with a spouse/partner will buffer against the negative effects of food insecurity on depressive symptoms;
(4) Hypothesis 4
Being a parent will augment the negative effects of food insecurity on depressive symptoms;
(5) Hypothesis 5
The effect of food insecurity on the depressive symptoms of married/cohabitating adults will be moderated by gender;
(6) Hypothesis 6
The effect of food insecurity on the depressive symptoms of parents will be moderated by gender;
(7) Hypothesis 7
Unobserved individual trait differences such as gender ideologies, personality, and the externalized behaviors confound the relationship between food insecurity and depressive symptoms.
These hypotheses are tested using samples of men and women that are stratified by family roles of parenthood and marital status. Hypothesis 7 is specifically tested comparing estimates from model specifications that exclude and include stable individual effects. In addition to the primary measures of food insecurity, parental and marital statuses, all analyses control for sociodemographic characteristics of race, level of education, the age-profile of children in the household, time spent in childcare responsibilities, employment status, main income source of the household, access to assistance with food and/or shelter from non-governmental organizations/churches/similar institutions and/or one's community/neighborhood.
3. Methods
3.1. Participants
Data for this study come from the National Income Dynamics Study–Coronavirus Rapid Mobile Survey (NIDS-CRAM) that aimed to track the socio-economic effects of the COVID-19 crisis in SA. Data is collected from a randomly drawn sample of adults aged 18-years and older, and broadly nationally representative of SA adults from 2017.1 Data was collected using Computer Assisted Telephone Interviewing (CATI) in five survey rounds over a period of 12 months from May 7, 2020 to May 11, 2021. Interviews lasted about 20 min and were conducted in all 11 official languages. Realized samples at each cross-section ranged from 4627 to 7073 respondents, and a total of 8157 respondents were surveyed at least once. The outcome of interest—adult reporting of depressed mood—was collected in Waves 2, 3 and 5, for which survey response rates were 80.2%, 68.8% and 68.2%, respectively. The final analytic sample for this study comprises a balanced panel (across Waves 2, 3 and 5) sample of 3456 respondents, of which 2170 are women and 1286 are men. Balanced sample weights provided with the data2 (weight name: w5_nc_bp_pweight_s) that correct for study attrition and top-up sampling were employed in all analyses.
A post hoc power calculation based on the sub-samples of women (n = 2170) and men (n = 1286) living with children indicated over 99% power for detecting a moderate effect size (Cohen's d; Cohen, 1988) of 0.5 (α = 0.05) between food secure and food insecure adults. Generally, there is 80% power to detect a moderate effect size of 0.5 in all stratified samples of at least 140. Since this study makes use of SEM, the method of MacCullum et al. (1996) that determines the minimum sample size necessary to achieve adequate power for carrying out hypothesis testing in such models is also conducted. Given 45 model degrees of freedom, a minimum necessary sample size of 231 is required to achieve 80% power (α = 0.05).
3.2. Measures
Baseline (Wave 2) summary statistics of the variables employed in this study — stratified by gender — are presented in Table 1. Depressive symptomology forms the outcome variable assessed, and primary predictor variables of interest include food insecurity, gender, marital/cohabitation status, and parental status. Sample descriptive statistics of sociodemographic characteristics that are included as additional controls in the analyses are also shown. On average, women are significantly more likely to be co-resident with a greater number of children, have a greater time burden of childcare, and rely on government grants as the main source of household income. Men, conversely, are significantly more likely to be living with a spouse/partner, more likely to be employed, and report their household's to be more dependent on labor market and/or business income.
Table 1.
Descriptive statistics of study sample, by gender.
| All (N = 3456) | Women (n = 2170) | Men (n = 1286) | p-value diff. | ||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Depressive symptoms | 1.30 | 1.63 | 1.28 | 1.59 | 1.31 | 1.66 | .766 |
| Fully food secure (%) | .62 | .49 | .59 | .49 | .66 | .47 | .005 |
| Marginal food security (%) | .24 | .42 | .25 | .43 | .22 | .41 | .200 |
| Low/very low food security (%) | .16 | .37 | .18 | .39 | .14 | .35 | .071 |
| Live with a spouse/partner (%) | .37 | .48 | .32 | .47 | .42 | .49 | .000 |
| Number of children 0–6 years in household | .67 | .99 | .81 | 1.08 | .52 | .84 | .000 |
| Number of children 7–17 years in household | 1.03 | 1.37 | 1.20 | 1.49 | .85 | 1.21 | .000 |
| Daily hours spent in childcare | 5.38 | 6.24 | 7.18 | 6.54 | 3.49 | 5.27 | .000 |
| Employed (%) | .44 | .50 | .35 | .48 | .54 | .50 | .000 |
| Household's main source of income… | |||||||
| … from labor market or business (%) | .41 | .49 | .32 | .47 | .51 | .50 | .000 |
| … from government grants (%) | .41 | .49 | .54 | .50 | .28 | .45 | .000 |
| Support with food/shelter from… | |||||||
| … NGO/church/similar (%) | .05 | .22 | .06 | .24 | .04 | .20 | .198 |
| … community/neighborhood (%) | .09 | .29 | .09 | .28 | .10 | .30 | .396 |
| Racial classification | |||||||
| African (%) | .79 | .41 | .81 | .40 | .77 | .42 | .250 |
| Colored (%) | .10 | .30 | .09 | .29 | .10 | .31 | .457 |
| White (%) | .02 | .14 | .01 | .11 | .03 | .16 | .245 |
| Indian/Asian (%) | .09 | .29 | .09 | .29 | .09 | .29 | .946 |
| Level of education attained | |||||||
| Primary school or less (%) | .15 | .35 | .18 | .38 | .11 | .32 | .000 |
| Some secondary schooling (%) | .36 | .48 | .34 | .47 | .38 | .49 | .088 |
| Complete secondary schooling (%) | .19 | .39 | .18 | .38 | .19 | .40 | .493 |
| Tertiary education (%) | .31 | .46 | .31 | .46 | .31 | .46 | .796 |
| Perceived at risk of getting COVID-19 (%) | .43 | .49 | .41 | .49 | .44 | .50 | .315 |
| Perceived uncertain risk of getting COVID-19 (%) | .42 | .49 | .45 | .50 | .40 | .49 | .103 |
| Perceived not at risk of getting COVID-19 (%) | .15 | .36 | .14 | .35 | .16 | .37 | .390 |
Notes: Balanced sample used. Values are weighted.
Source: NIDS-CRAM Wave 2 (2020).
Depressive symptoms. Positive screening for depressive symptoms was measured in waves 2, 3 and 5 using the widely used and validated Patient Health Questionnaire-2 (PHQ-2) instrument (Kroenker et al., 2009; Löwe et al., 2010). Respondents indicated how often, over the past two weeks, they had (1) little interest or pleasure in doing things, and (2) felt down, depressed, or hopeless. Responses fell on a 4-point scale: not at all (0), several days (1), more than half the days (2), and nearly every day (3). The total score—ranging from 0 to 6—is based on the sum of these two items. Overall, 22.3% of the study sample screened positive for depressive symptoms (PHQ-2 score≥3).
Household food insecurity. Household food insecurity (FI) was assessed in all waves of NIDS-CRAM. Respondents were asked whether their household had run out of money to buy food in the previous month, and whether anyone in their household had gone hungry in the last 7 days because there wasn't enough food. The latter question was proceeded by an assessment of hunger occurrence on a 5-point Likert scale of never (0), 1 or 2 days (1), 3 or 4 days (2), almost every day (3) and every day (4). A categorical indicator of FI was created as follows: a fully food secure household was defined as one that experienced none of the food insecurity conditions; a marginally food secure household is one that reported to have run out of money for food, but had no experiences of hunger amongst household members3; a household with low food security is one that reported incidences of hunger sometimes (i.e. 1–2 days); and finally, a household with very low food security is one in which more frequent occurrences of hunger (at least half of the days) occurred. The final two categories were combined given a small cell count.
Marital status and parental status. Marital status is measured by a dichotomous variable indicating whether respondents resided with a spouse or partner at the time of data collection. Individuals are stratified across two categories of marital status: individuals living with a spouse/partner at all time periods; and individuals not living with a spouse/partner at all time periods.4 A dichotomous variable indicating whether or not a respondent has biological and/or legally adopted children was constructed from information provided in the Wave 3 questionnaire.
Other controls. Respondents were asked about the number of children within their household aged 6 years and younger, and 17 years and younger. This information was used to construct two continuous variables of the number of children aged 0–6 years and the number of children aged 7–17 years. Respondents were also asked about the number of daily hours that they spent looking after children. This continuous variable was constrained to a range of 0–16 h; that is, reports of childcare exceeding 16 h were capped at that level. Responses to the question of how a respondent's household's primary income source changed over the past four weeks was used to create an indicator of ‘income increased’. A dichotomous variable of the employment status of the respondent (i.e. employed and not employed) and was also measured. Support and assistance with food and shelter were measured by a dichotomous indicator of whether assistance was received in the month prior to the interview from government, NGOs, churches and/or the local community.
3.3. Analytic strategy
The two key attractions for using panel data to make causal inference and infer causal direction is the ability to include lagged, endogenous regressors as well as control for unobserved, time-invariant characteristics. Fixed effects methods have been popular for addressing the latter, whilst Cross-Lagged Panel Models (CLPM) have been widely used for examining causal direction. Combining the two, however, can present with several estimation issues, such as uncertainty regarding initial conditions and error terms being correlated with covariates, or “incidental parameters problem” (Wooldridge, 2010).
Cross-lagged Dynamic Panel Models (CLDPM) (Allison et al., 2017; Williams et al., 2018) are a relatively recent analytic approach that involves the estimation of an individual-level fixed effects model using a structural equation modeling (SEM) framework and maximum likelihood (ML). This approach deals with the incidental parameters and initial conditions problems by controlling for unobserved confounders —through the inclusion of a latent individual effect — and lagged, endogenous covariates (Wooldridge, 2010). A further advantage of a dynamic ML-SEM approach is its ability to deal with issues of simultaneity. Whereas fixed effects models assume strict exogeneity (Halaby, 2004), the inclusion of lagged values of the dependent variable as a covariate accounts for the fact that food insecurity might be caused by depressive symptoms (weak exogeneity).
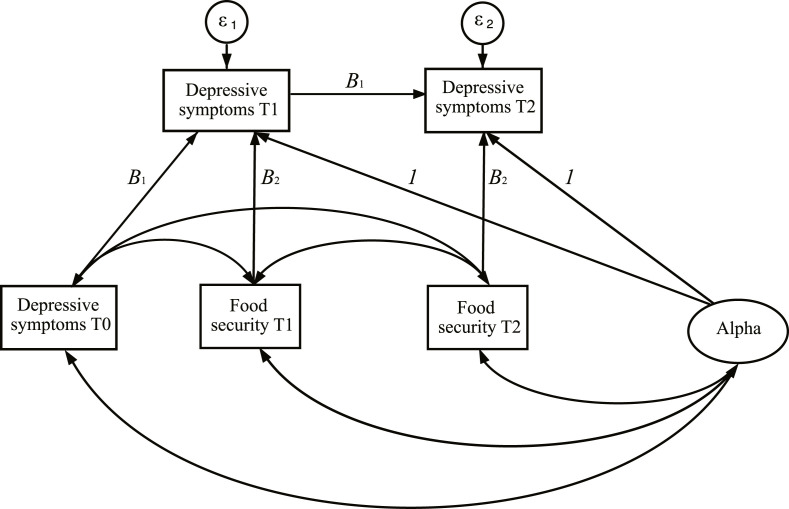
Fig. 1 depicts a path diagram of the 3-wave dynamic panel model estimated in the current analysis. For simplicity, the model includes only a single exogenous time-variant variable, x (food security), and an endogenous dependent variable, y (depressive symptoms). x at all T are permitted to freely correlate with one another and with y at T0. The coefficients on exogenous variables, represented by B in Fig. 1, are constrained to be the same at all T. The latent variable Alpha, representing the “individual effect” capturing time-invariant traits, is constrained to have a factor loading of 1.5 Alpha is permitted to covary with all exogenous variables apart from time-invariant covariates such as race and level of education. This distinguishes the CLDPM from the Random Intercepts CLPM (RI-CLPM), which assumes the within- and between-person effects to be orthogonal.
Fig. 1.
Path diagram for 3-wave dynamic panel model.
One of the primary differences between the CLPM and the CLDPM is the interpretation of the model coefficients. The inclusion of individual trait-like differences in the CLPM implies that the coefficient, B, is interpreted as a within-person effect of x on y. Specifically, B indicates the degree to which deviations from an individual's expected level of depressive symptoms can be predicted from deviations from their expected level of food insecurity, all else controlled for. The size and even direction of B can differ substantially when Alpha is excluded or included in the model. For example, in modelling the relationship between adolescent depression and parental responsiveness, Hamaker et al. (2015) show that a positive association predicted using CLPM is eliminated when using RI-CLMP. Although this implies that parents who are more responsive on average are more likely to have adolescents who suffer lower depressive symptoms on average, it does not provide a causal mechanism that can form a foundation for any intervention.
Of the 3456 respondents included in the analysis, 3.9%, 3.1%, and 1.2% had missing data on depressive symptoms at Waves 2, 3 and 5, respectively. Similarly, 0.7%, 0.5%, and 0.1% of the data was missing on household food security. Full information maximum likelihood (FIML) estimation was used to partially account for data that might not be missing at random. Measures of model fit include the root mean square error of approximation (RMSEA) and Bentler's comparative fix index (CFI) (Bentler, 1990). Acceptable model fit assumes meeting RMSEA<0.05 and CFI≥0.95.
Comparisons are made with two alterative model specifications: Model 1 that excludes a lagged dependent variable and the latent variable Alpha, which can be likened to a pooled cross-section regression analysis with time fixed effects; and Model 2 that includes a lagged dependent variable but excludes Alpha. Model 2 is most comparable to the existing empirical literature that controls for autoregression and reciprocity between FI and depressive symptoms. Analyses were performed using the sem and svy prefix functions in Stata MP 17 (StataCorp. 2021. Stata St, 2021). Two-tailed p-values <.05 were considered statistically significant, although values of 0.10 were also considered given small samples when data was stratified by gender, parental and marital statuses.
4. Results
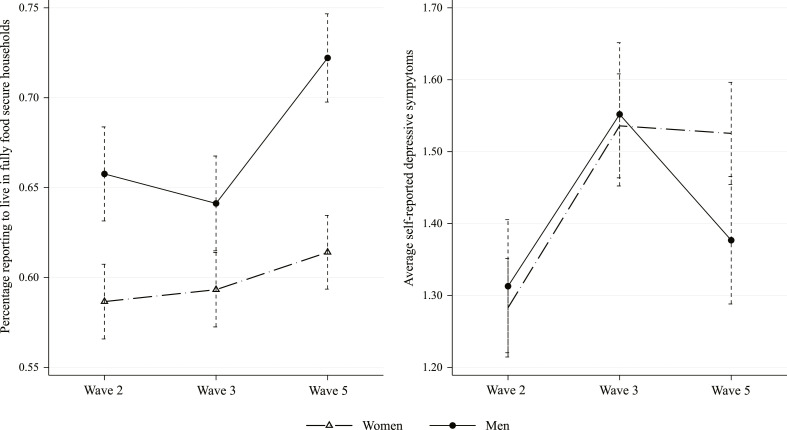
The percentage of men and women reporting to reside in food insecure households remained stable over Waves 2 and 3 at approximately 35% and 42%, respectively. Levels of food insecurity increased for both groups in Wave 5, although only significantly so for women (Fig. 2 ). In all waves, women reported significantly (p < .05) higher levels of food insecurity than men. The average depressive symptoms of men and women were not reported to be significantly different in either Wave 2 or Wave 3 (contrary to Hypothesis 1). Both groups experienced a significant (p < .05) worsening of mental health between Waves 2 and 3 (Fig. 2). However, whilst men's average depressive symptoms declined significantly (p < .05) between Waves 3 and 5, women's remained stable at around 1.52. Therefore, between Wave 3 and Wave 5, the gender gap in depressive symptoms increased from 0.03 (p = .596) to 0.15 (p = .008). This decline in men's depressive symptoms in Wave 5 corresponds with the improvement in food security.
Fig. 2.
Trends in depressive symptoms and household food security status, by gender. Note: 95% confidence intervals indicated by dashed lines around point estimates.
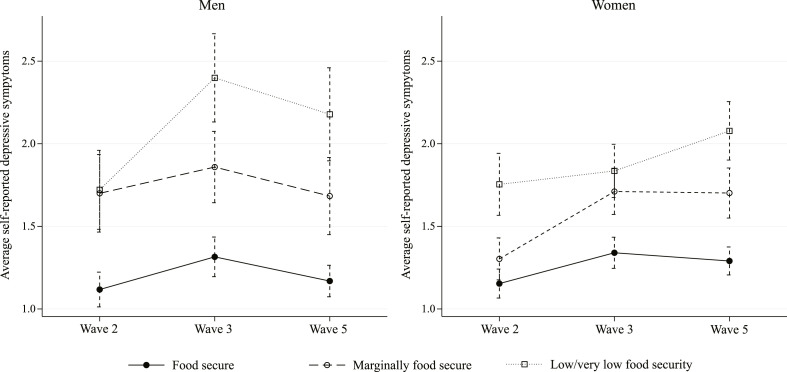
The average depressive symptoms of women and men living in households reported to be fully food secure were generally significantly (p < .05) lower than that of their less food secure counterparts at all time points (Fig. 3 ). Generally, no significant differences in the average depressive symptoms of men and women for a given level of household food security is observed (contrary to Hypothesis 1). Only in Wave 3 were men residing in households with low/very low food security observed to report significantly higher (p < .05) depressive symptoms than their female counterparts.
Fig. 3.
Adult depressive symptoms, by gender and household food security status. Note: 95% confidence intervals indicated by dashed lines around point estimates.
Only the average reported depressive symptoms of men residing in households with low/very low food security are found to be significantly (p < .05) higher in Waves 3 and 5 when compared to Wave 2. Specifically, between July 2020 and April 2021, men's average depressive symptoms in the most food insecure contexts increased by 0.46 (0.28 SD).6 Amongst women, average depressive symptoms across all household food security categories were observed to increase significantly (p < .05) between Wave 2 (July 2020) and Wave 5 (April 2021). The largest change of 0.4 (0.24 SD) was observed amongst women living in marginally food secure households. The cross-time trends indicate a widening gap in average depressive symptoms between men and women living in fully food secure households and their counterparts living in households with low/very low food security.
Estimates from gender-stratified ML-SEM models of depressive symptoms that control for food insecurity and sociodemographic characteristics are provided in Table A1 of the Appendix. Measures of model fit indicate Model 3 to outperform both Model 1 and Model 2 in terms of satisfying both the RMSEA and CFI criteria. Model 2, which is most comparable to the approach typically employed in existing empirical research, satisfies the RMSEA criterion but falls a bit short of satisfying CFI≥0.95.
The estimates of Model 2 indicate that, controlling for an array of sociodemographic factors, the depressive symptoms of men and women rise significantly with FI (in support of Hypothesis 2). Larger coefficients on marginal and low/very low food security are estimated for men than for women. The relationship between FI and depressive symptoms is attenuated by the inclusion of Alpha in Model 3 such that only partial support for Hypothesis 2 is found. Specifically, low/very low food security is estimated to significantly increase the depressive symptoms of women (b = 0.55, p < .01, 95% CI: 0.16. 94) relative to full food security, and marginal food security is estimated to significantly increase the depressive symptoms of men (b = 0.49, p < .05, 95% CI: 0.08, 0.90) relative to full food security. These are equivalent to a moderate effect size of low/very low food security on women's depressive symptoms of .33, and a moderate effect size of marginal food security on men's depressive symptoms of .30.
Model 2 further indicates that living with a spouse/partner significantly lowers the depressive symptoms of women (b = 0.21, p < .01, 95% CI: 0.05, 0.37), although no significant effect is estimated for men. This same association does not emerge in Model 3. Similarly, Model 2 for both genders predict statistically significant state dependency in depressive symptom history (men: b = 0.23, p < .001; women: b = 0.22, p < .001) and greater depressive symptomology amongst individuals who self-perceive themselves to be at risk of getting COVID-19 (men: b = 0.24, p < .05; women: b = 0.43, p < .001). These relationships are eliminated with the inclusion of Alpha in Model 3. No significant effects of children and childcare on depressive symptoms are found for either gender in any of the estimated models.
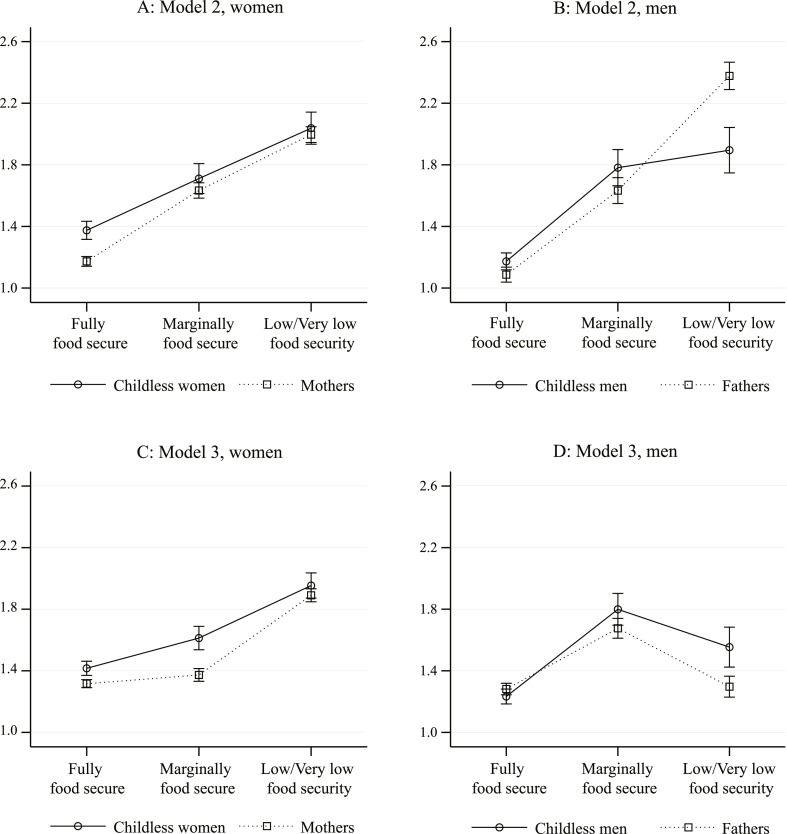
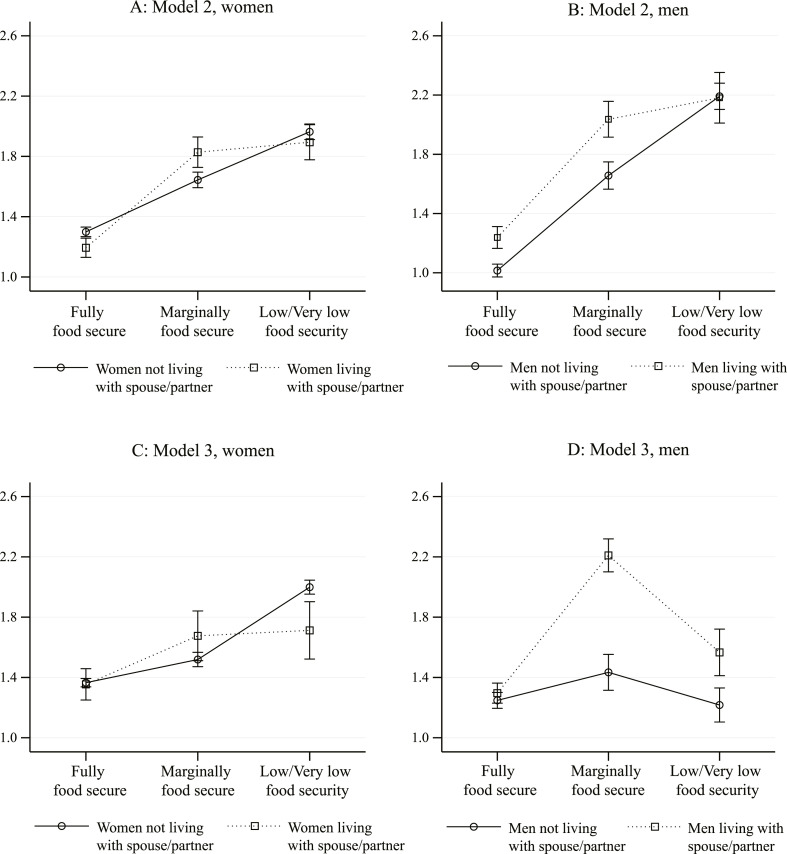
Tables A2 and A3 of the Appendix summarize the estimates of Model 2 and Model 3 using samples of women and men stratified by parental and marital statuses; specifically, childless versus parent, and cohabitating with a spouse/partner versus not living with a spouse/partner. The model estimation results are graphically depicted in Fig. 4, Fig. 5 . Specifically, panels A and B of both figures indicate the predicted depressive symptoms of women and men, respectively, using Model 2. Panels C and D indicate the predicted depressive symptoms using Model 3 excluding the impact of stable individual effects. In other words, the results of panels C and D indicate the association between FI and depressive symptoms factoring out potential confounding trait-like individual differences.
Fig. 4.
Predicted depressive symptoms, by gender and parental status. Note: 95% confidence intervals indicated by lines around point estimates.
Fig. 5.
Predicted depressive symptoms, by gender and marital status. Note: 95% confidence intervals indicated by lines around point estimates.
Using Model 2, parenthood is associated with better mental health outcomes amongst women in fully food secure households, although this decreases with rising FI (Fig. 4, panel A). Lower depressive symptoms linked to parenthood is also found among men living in fully and marginally food secure households, but having children is associated with a significantly greater depressive symptomology in the context of low/very low food security (Fig. 4, panel B). Therefore, any mental health benefits of having children are reduced in the context of low/very low food security (in partial support of Hypothesis 4), and more so in the case of men (in support of Hypothesis 6). It is also notable that the depressive symptoms of both mothers and fathers are significantly positively related to daily hours spent in childcare.
Controlling for individual trait-like differences, no significant association between mothers' depressive symptoms and FI is indicated (Model 3, column 8 of Table A2), and the gap in depressive symptoms between childless women and mothers living in marginally food secure households is widened to .24 (0.15 SD, p < .01) (Fig. 4, panel C). The depressive symptoms of childless women are, conversely, significantly increased when faced with low/very low food security relative to full food security (Model 3, column 4 of Table A2). Overall, however, the depressive symptoms of childless women and mothers are predicted to be similar in contexts of low/very low food security (Fig. 4, panel C), as the mental health of the former group are .81 (p < .05) or 0.49 SD lower when support with food/shelter is received from an NGO, church, or similar institution, whereas the depressive symptoms of mothers is 0.89 (p < .001) or 0.54 SD higher when social assistance is received from the community/neighborhood. Model 3 also predicts that each additional hour spent in childcare increases a mother's depressive symptoms by .05 (p < .05).
In the case of men, Model 3 predicts no significant (p < .05) association between FI and the depressive symptoms of men, irrespective of parental status (columns 4 and 8 of Table A3). The predicted depressive symptoms of fathers living in low/very low food security contexts declines by 1.00 (p < .001) or 0.60 SD when stable individual effects are accounted for (Fig. 2, panels B and D). The predicted depressive symptoms of childless men are similarly indicated to decline, although only by about 0.20 SD (p < .05).
Turning the focus to marital status, Model 2 indicates depressive symptoms to rise significantly with FI, irrespective of gender and whether an individual lives with a partner/spouse. Generally, no mental health benefit of cohabitation is found. However, the mental health cost of low/very low food security is estimated to be smaller amongst cohabitating men and women when compared to their non-cohabitating counterparts (in support of Hypothesis 3). As with parental status, the impact of FI on depressive symptoms is higher amongst cohabitating men than cohabitating women (in support of Hypothesis 5). Perceptions of being at risk of getting COVID-19 is associated with significantly greater depressive symptoms amongst non-cohabitating women (column 7 of Table A2), whilst living with school-going aged children and reporting labor/business income as a main source of income for their households is associated with significantly lower prevalence of depressive symptoms amongst cohabitating men (column 5 of Table A3).
Controlling for individual trait-like differences, FI is no longer estimated to be significantly related to the depressive symptoms of cohabitating women (column 6 of Table A2) or non-cohabitating men (column 8 of Table A3). However, low/very low food security contributes to significantly higher depressive symptoms amongst non-cohabitating women (column 8 of Table A2), whilst cohabitating men's depressive symptoms are significantly higher under contexts of marginal food security (column 6 of Table A3). Model 3, therefore, indicates a psychological benefit of cohabitation amongst women in low/very low food security settings once stable individual effects are accounted for (Fig. 5, panel C). Conversely, Model 3 indicates a psychological cost of cohabitation amongst men in less food secure contexts (Fig. 5, panel D), particularly in the case of marginal food security where cohabitating men are predicted to report depressive symptoms that are 0.50 SD (p < .001) higher than their non-cohabitating counterparts. It is worth noting that the negative effect of low/very low food security on depressive symptoms of men is, regardless of marital status, significantly reduced once stable individual effects are included ().
Finally, residing with school-going aged children is indicated to have converse effects on cohabitating men and women in Model 3; specifically, living with an additional school-going aged child increases cohabitating women's depressive symptoms by .60 or 0.36 SD (p < .01), whilst lowers cohabitating men's depressive symptoms by .30 or 0.18 SD (p < .05).
5. Discussion and conclusion
The present study undertook to empirically investigate the causal impact of food insecurity (FI) on self-reports of depressive symptoms of South African (SA) men and women, both of which have increased significantly since the onset of the COVID-19 pandemic, as well as to assess whether the impact varies by marital and parental statuses. The findings of this study contribute significantly to our understanding of the role that gender — defined as a set of complex and dynamic norms, behaviors and relational roles that structure society — plays in the mental health outcomes of different individuals.
This study did not find empirical evidence of a significant gender difference in average reported depressive symptoms amongst SA adults (contrary to Hypothesis 1). This is in opposition to international evidence from nationally representative samples (Salk et al., 2017), but in line with Gibbs et al.’s (Gibbs et al., 2018) analysis of SA youth living in informal settlements. Consistent with prior research (Pourmotabbed et al., 2020), support is found for a positive relationship between FI and depressive symptoms amongst both women and men (Hypothesis 2), even after controlling for an array of sociodemographic variables. This effect is indicated to be stronger amongst men than women; specifically, a moderate effect size of 0.52 of low/very low food security on the depressive symptoms of men is estimated, whilst for women it is 0.33. This is in keeping with findings from a recent meta-analysis (Smith et al., 2021) of high- and middle-income countries in which the risk of depression associated with FI was higher amongst men than women.
In contrast to existing evidence (Lee et al., 2020a; Umberson et al., 2010; Grundström et al., 2021), this study did not find a positive effect of marriage on the psychological wellbeing of men. However, in partial support of Hypothesis 3 and social control theory (Brown and Richman, 2012), the results did indicate cohabitation to buffer the effect of low/very low food security on depressive symptoms amongst men and women. The impact of FI on depressive symptoms is also found to be stronger amongst men than women, in support of Hypothesis 5. Similarly, parenthood is found to augment the effect of FI on the depressive symptoms of fathers only, providing partial support for Hypothesis 4 and support for Hypothesis 6.
Controlling for the effects of confounding due to unobserved stable individual traits alters the relationship between FI and depressive symptoms, particularly for men. Amongst parents and cohabitating women and non-cohabitating men, depressive symptoms are no longer significantly affected by experiences of marginal and low/very low food security accounting for individual differences. This suggests that the impact of FI on the depressive symptoms of these groups might be fully or partially mediated by unobservable factor/s. Amongst mothers, for example, this could be a greater proclivity for neuroticism and ruminative response (Wupperman and Neumann, 2006), as indicated by a significant positive effect of self-perceived risk of getting COVID-19 on depressive symptoms (b = 0.41, p < .001) that is eliminated at the within-individual level. In other words, mothers who report higher on average depressive symptoms are also more likely to report higher than average perceptions of being at risk of getting COVID-19.
As indicated in existing literature (Goldberg and Perry-Jenkins, 2004; DeVault, 1994), gender ideologies and role norms, and shame and anxiety arising from an inability to meet these, may explain the link that FI holds with depressive symptoms. This is alluded to in the results of this study by the fact that whilst FI no longer significantly impacts mothers' depressive symptoms with the inclusion of individual effects, the receipt of assistance with food and/or shelter from one's community/neighborhood emerges as having a significant and moderate effect size (0.54) on the depressive symptoms of mothers. Similarly, the effect of time spent in childcare more than doubles in magnitude. This indicates that mothers who reported higher than average depressive symptoms were also more likely to report spending fewer hours on average in childcare.
A similar argument could be made for men. After controlling for individual trait-like differences, only marginal food security is found to have a significant moderate effect (0.56) on the depressive symptoms of cohabitating men. All other significant effects of FI on depressive symptoms, particularly low/very low food security, are eliminated in all stratified male samples. In the case of fathers, the inclusion of individual effects eliminates a highly significant positive effect of daily time spent in childcare on depressive symptoms. This indicates — contrary to what was found for mothers — that fathers reporting higher than average depressive symptoms were also more likely to report spending more hours on average in childcare. Greater psychological distress tied to taking on a role traditionally reserved for one's female spouse/partner, or failing to meet one's assumed gender role, aligns with the expectations of the gendered response framework (Addis, 2008).
It is interesting, however, that the significant effect of marginal food security on the depressive symptoms of fathers remains after controlling for confounding due to unobservable stable individual traits. Marginal food insecurity, as measured in this study, is indicative of running out of money to buy food in the previous month, but without recent reports of hunger within the household. This could imply increased anxiety and stress about where and how future food supplies will be accessed, and/or shame and stigma linked to current methods for securing food such as a reliance on one's community or even partner/spouse. Gendered resource and relative resource theories (Goode, 1971; Macmillan and Gartner, 1999) emphasize power and the use of force by men to maintain dominance and attempt to re-exert gender role expectations and reduce feelings of shame when faced with a general lack of resources, or a lack of resources relative to their partners and wives (Basile et al., 2013). This is even more likely to occur when traditional as opposed to egalitarian gender ideologies and beliefs are held (Atkinson et al., 2005; Cools and Kotsadam, 2017).
Marginal food security, then, may be more strongly associated with a threat to meet a masculine ideal, whereas experiences of low/very low food security conceivably more hopeless require increasingly dramatic and maladaptive coping strategies to deal with or mask depressive symptoms. Hatcher et al. (2019), for example, find a significant indirect effect of FI, which in their study refers to experiences of hunger and going without food, on the depressive symptoms of SA men through a pathway of increased alcohol use. Employing multivariate regression analysis, Gibbs et al. (2018) find stealing due to hunger and controlling behavior towards one's partner to be significantly related to the depressive symptoms of SA men, yet, similar to this study, they find no significant relationship between going hungry and depressive symptoms. They do, however, find a significant impact of hunger on women's depressive symptoms, all else controlled for. This aligns with the results estimated for more vulnerable women samples in this study (e.g. non-cohabitating women)..
One reason for why the impact of marginal food security on cohabitating men's depressive symptoms is augmented after addressing potential confounding due to unobservable traits is because this correction might, in fact, be generating bias through controlling for an unobservable collider variable; that is, a variable that is affected by but not itself affecting the key model variables of FI and depressive symptoms. As shown by Elwert and Winship (2014), conditioning on a collider variable will open the flow of association between FI and depressive symptoms.
Possible contenders for this are relationship control, jealousy, and quarreling, as predicted by gendered resource theory. This has been empirically confirmed by Hatcher et al. (2019) in their study of SA men, in which these outcomes are shown to be associated with significantly greater levels of intimate partner violence (IPV). This can have spillover effects on the depressive symptoms of wives and partners, as exposure to IPV has been indicated to increase the depressive symptoms of women (Devries et al., 2013). Therefore, the lack of a significant effect of FI on the depressive symptoms of cohabitating women after controlling for individual effects may be similarly linked to relationship and interpersonal characteristics.
There are limitations to this study. Rapid assessment surveys that utilize Computer Assisted Telephone Interviewing (CATI) are constrained by time demands. This means that the measures used to evaluate food insecurity and mental health in this study are based on shorter survey modules than that which is more often used. The Patient Health Questionnaire-2 (PHQ-2) instrument used by this study is a widely used and validated short screening tool. It is less clear whether the two items used to measure food insecurity (FI) have allowed for an adequate assessment of the severity of FI. Validated short-form versions of the most frequently adopted household FI measures have been developed, such as the 6-item version of the 18-item Household Food Security Survey (HFSSM) used for households with children (Blumberg et al., 1999). Even shorter 2-item FI screens have been developed and demonstrated specificity and convergent validity in samples of families with children, such as the Hunger Vital SignTM (Hager et al., 2010) that was used by a rapid assessment study of the social needs of low-income households with children in the US during the first month of COVID-19. The questions used in this study are most like the 2-item screen of Swindle and colleagues (Swindle et al., 2013), although refer to much shorter retrospective periods. Future research is required to validate the short-form FI screens adopted by rapid response assessments such as NIDS-CRAM.
Despite these limitations, this study has several strengths. This represents the first longitudinal study to attempt to causally identify the relationship between food insecurity and depressive symptoms in SA using a large, random, and nationally representative sample, and makes use of a novel structural equation modelling technique with fixed effects that control for potential confounding and simultaneity. This study also represents one of the first attempts at determining gender differences in the FI-depressive-symptom relationship in a developing country context, as well as extends the very limited research on this relationship amongst fathers and assesses how differences by gender might be tied to gendered roles of parenthood and marriage. Understanding whether and why there is heterogeneity in food insecurity's association with depressive symptoms across gender provides important information regarding the circumstances under which men and women, particuarly those living with children, are most affected by food insecurity, and how they might be able to cope.
The findings of this study also indicate that social constructions of gender roles have significant influences on men's and women's mental health, and that the relationship between FI and depressive symptoms identified within existing literature potentially conflates within- and between-individual effects. Therefore, future research aiming to investigate the causal effect of FI on depressive symptoms should endeavor to include measures of gender beliefs, attitudes, and relationship characteristics.of journal.
Funding
The NIDS-CRAM study (i.e. Data Collection) is funded by the Allan & Gill Gray Philanthropy, the FEM Education Foundation and the Michael & Susan Dell Foundation. The funding body was not involved in the conceptualization, design, analysis and interpretation of our findings in this study. They also did not influence our choice of journal.
Credit author statement
Debra Lynne Shepherd: Responsible for full article conceptualization, methodology, data curation, writing, visualization, investigation, reviewing and editing.
Footnotes
The NIDS-CRAM sample is based on the last wave of the longitudinal National Income Dynamic Study (NIDS) that was conducted biennially from 2008 to in 2017. NIDS, as well as the special NIDS-CRAM survey, is conducted by the Southern Africa Labour and Development Research Unit (SALDRU) at the University of Cape Town. For more information about NIDS, visit http://www.nids.uct.ac.za/.
For more detail on the NIDS-CRAM weighting approach, see Ingle et al. (2021).
This could imply that members of the household were unable to eat preferred foods or whose diet became more monotonous.
Approximately 12% of men and women reported to be married in some but not all waves or reported being married but not living with their spouse/partner at all times.
This is the same as the random intercepts in latent growth curve modeling, except the difference here is that group means, captured by a constant term, are allowed to freely vary over time.
The standard deviation of the entire NIDS-CRAM sample is 1.65.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.114830.
Appendix.
Table A1.
ML-SEM estimates, by gender
| Women (n = 2170) | Men (n = 1286) | |||||||||||
| Model 1 | Model 2: dynamic | Model 3: dynamic fixed effects | Model 1 | Model 2: dynamic | Model 3: dynamic fixed effects | |||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |||||||
| b | se | b | se | b | se | b | se | b | se | b | se | |
| Depressive symptoms (lagged) | – | – | .22*** | .03 | .09 | .07 | – | – | .23*** | .03 | -.02 | .08 |
| Marginal food security | .40*** | .10 | .34*** | .09 | .15 | .16 | .47** | .15 | .40** | .13 | .49* | .21 |
| Low/very low food security | .75*** | .13 | .65*** | .11 | .55** | .20 | 1.05*** | .19 | .86*** | .17 | .22 | .26 |
| Live with spouse/partner | -.25** | .09 | -.21** | .08 | -.07 | .22 | .05 | .13 | .03 | .11 | .00 | .21 |
| Number of children 0–6 years old | -.01 | .04 | -.01 | .03 | -.11 | .08 | .06 | .06 | .07 | .06 | .16 | .10 |
| Number of children 7–17 years old | -.02 | .03 | -.01 | .03 | .13 | .09 | -.07 | .05 | -.07 | .05 | .01 | .08 |
| Daily hours spent in childcare | .01 | .01 | .00 | .01 | .01 | .01 | .03+ | .02 | .03 | .02 | .01 | .02 |
| Employed | .11 | .10 | .11 | .14 | .17 | .17 | -.05 | .14 | -.04 | .13 | .32 | .22 |
| Household's main income source | ||||||||||||
| Labor/business | .12 | .15 | .11 | .15 | -.30 | .23 | -.10 | .17 | -.07 | .16 | -.14 | .24 |
| Government grants | .11 | .12 | .11 | .11 | -.20 | .17 | -.22 | .18 | -.22 | .18 | -.48+ | .28 |
| Support from NGO/church/similar | -.14 | .27 | -.17 | .26 | .03 | .34 | -.18 | .34 | -.20 | .31 | -.18 | .48 |
| Support from community/neighborhood | .23 | .19 | .19 | .19 | .39 | .24 | -.06 | .26 | -.06 | .27 | .00 | .31 |
| African | -.33+ | .19 | -.21 | .15 | -.18 | .20 | -.27 | .20 | -.16 | .18 | -.21 | .21 |
| Colored | .32 | .23 | .31 | .19 | .49* | .23 | .42 | .28 | .31 | .24 | .40 | .30 |
| Primary school or less | -.15 | .13 | -.11 | .12 | -.19 | .15 | .05 | .18 | .12 | .17 | .08 | .23 |
| Complete secondary schooling | .06 | .14 | .04 | .12 | .06 | .13 | -.02 | .16 | -.02 | .13 | -.14 | .17 |
| Tertiary education | -.00 | .11 | -.02 | .09 | -.01 | .12 | -.26+ | .15 | -.21 | .13 | -.43* | .18 |
| Perceived at risk of getting COVID-19 | .43*** | .09 | .39*** | .08 | .18 | .16 | .24* | .12 | .21* | .11 | .10 | .15 |
| Uncertain of risk of getting COVID-19 | -.02 | .13 | -.03 | .13 | -.14 | .24 | -.36* | .15 | -.32* | .14 | -.33 | .21 |
| Constant T1 | 1.34*** | .23 | 1.01*** | .19 | 1.34*** | .31 | 1.56*** | .28 | 1.20*** | .26 | 1.57*** | .40 |
| Constant T2 | 1.31*** | .22 | .93*** | .18 | 1.32*** | .31 | 1.43*** | .27 | 1.00*** | .25 | 1.44*** | .42 |
| RMSEA [C195] | .041 [.035, .047] | .024 [.018, .030] | .006 [.000, .020] | .046 [.039, .054] | .035 [.027, .043] | |||||||
| CFI | .607 | .889 | .998 | .623 | .831 | |||||||
Notes: Balanced panel sample used. Data is weighted appropriately. SEM estimation is performed using Full Information Maximum Likelihood. ***p < .001, **p < .01, *p < .05, +p < .10.
Table A2.
ML-SEM estimates, women (n = 2170)
| Childless (n = 747) |
Mother (n = 1395) |
Living with spouse/partner (n = 518) |
Not living with spouse/partner (n = 1394) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 2: dynamic |
Model 3: dynamic fixed effects |
Model 2: dynamic |
Model 3: dynamic fixed effects |
Model 2: dynamic |
Model 3: dynamic fixed effects |
Model 2: dynamic |
Model 3: dynamic fixed effects |
|||||||||
| (1) |
(2) |
(3) |
(4) |
(5) |
(6) |
(7) |
(8) |
|||||||||
| b | se | b | se | b | se | b | se | b | se | b | se | b | se | b | se | |
| Depressive symptoms (lagged) | .28*** | .06 | .15 | .13 | .18*** | .03 | .06 | .08 | .29*** | .04 | .26 | .19 | .17*** | .04 | .04 | .08 |
| Marginal food security | .33* | .16 | .13 | .34 | .35** | .11 | -.08 | .21 | .44** | .14 | .16 | .27 | .32** | .12 | .18 | .21 |
| Low/very low food security | .64** | .21 | .71* | .34 | .69*** | .13 | -.07 | .25 | .50** | .18 | .06 | .37 | .63*** | .14 | .68** | .25 |
| Live with spouse/partner | -.25* | .12 | -.49 | .50 | -.133 | .10 | -.03 | .27 | – | – | – | – | – | – | – | – |
| Number of children 0–6 years old | -.03 | .07 | .10 | .16 | .02 | .04 | -.12 | .11 | .06 | .07 | .04 | .18 | -.04 | .04 | -.15 | .09 |
| Number of children 7–17 years old | .07 | .05 | .29* | .14 | -.02 | .03 | -.01 | .05 | .60** | .18 | .00 | .04 | .02 | .10 | ||
| Daily hours spent in childcare | -.02 | .02 | -.01 | .03 | .02* | .01 | .05* | .02 | .00 | .01 | -.02 | .03 | .00 | .01 | .02 | .02 |
| Employed | .23 | .17 | -.27 | .35 | .07 | .10 | .15 | .20 | -.02 | .16 | .15 | .21 | .18 | .13 | .15 | .23 |
| Household's main income source | ||||||||||||||||
| Labour/business | .08 | .23 | .45 | .37 | .19 | .14 | -.30 | .24 | -.04 | .26 | -.85 | .62 | .21 | .18 | -.07 | .26 |
| Government grants | .05 | .17 | -.26 | .23 | .17 | .13 | -.08 | .21 | -.06 | .20 | -.29 | .35 | .18 | .14 | -.15 | .20 |
| Support from NGO/church/similar | -.47 | .46 | -.81* | .35 | .02 | .27 | -.02 | .48 | .56 | .41 | .38 | .71 | -.26 | .33 | -.09 | .42 |
| Support from community/neighborhood | -.22 | .27 | -.25 | .59 | .48* | .23 | .89*** | .27 | .26 | .37 | .40 | .57 | .24 | .24 | .39 | .29 |
| African | -.27 | .19 | −1.12* | .53 | .06 | .23 | .18 | .28 | -.25 | .19 | -.29 | .27 | -.30 | .24 | -.29 | .31 |
| Colored | .37+ | .22 | .24 | .59 | .47+ | .28 | .83** | .32 | .32 | .22 | .55+ | .32 | .18 | .30 | .23 | .36 |
| Primary school or less | .04 | .16 | .16 | .28 | -.25+ | .14 | -.30+ | .17 | -.25 | .18 | -.67* | .26 | -.06 | .13 | -.07 | .16 |
| Complete secondary schooling | .10 | .23 | -.01 | .32 | .02 | .12 | -.01 | .15 | -.41* | .18 | -.28 | .21 | .24 | .15 | .26 | .17 |
| Tertiary education | -.02 | .17 | -.14 | .36 | .00 | .11 | -.06 | .15 | -.20 | .15 | -.22 | .23 | .10 | .13 | .13 | .16 |
| Perceived at risk of getting COVID-19 | .38** | .14 | .39 | .31 | .41*** | .10 | .16 | .21 | .23 | .15 | .30 | .33 | .39*** | .11 | .17 | .19 |
| Uncertain of risk of getting COVID-19 | -.22 | .19 | .18 | .34 | .10 | .18 | -.22 | .36 | -.05 | .20 | -.06 | .47 | -.03 | .17 | -.13 | .30 |
| Constant T1 | .98*** | .27 | 1.47* | .64 | .59* | .29 | 1.06* | .48 | .98** | .31 | .97+ | .58 | 1.01*** | .25 | 1.49*** | .35 |
| Constant T2 | 1.05*** | .25 | 1.75** | .64 | .43 | .27 | 1.24** | .46 | 1.05*** | .27 | 1.06+ | .56 | .90*** | .25 | 1.42*** | .37 |
Notes: Balanced panel sample used, and data is weighted appropriately. SEM estimation is performed using Full Information Maximum Likelihood. ***p < .001, **p < .01, *p < .05, +p < .10.
Table A3.
ML-SEM estimates, men (n = 1286)
| Childless (n = 492) | Father (n = 779) | Living with spouse/partner (n = 421) | Not living with spouse/partner (n = 712) | |||||||||||||
| Model 2: dynamic | Model 3: dynamic fixed effects | Model 2: dynamic | Model 3: dynamic fixed effects | Model 2: dynamic | Model 3: dynamic fixed effects | Model 2: dynamic | Model 3: dynamic fixed effects | |||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |||||||||
| b | se | b | se | b | se | b | se | b | se | b | se | b | se | b | se | |
| Depressive symptoms (lagged) | .22*** | .05 | .08 | .15 | .23*** | .04 | -.09 | .07 | .24*** | .06 | -.08 | .11 | .19*** | .04 | .00 | .12 |
| Marginal food security | .52* | .24 | .54 | .38 | .43** | .15 | .41+ | .23 | .63** | .21 | .93** | .30 | .60*** | .18 | .30 | .34 |
| Low/very low food security | .66+ | .34 | .34 | .41 | .99*** | .20 | .15 | .30 | .84** | .31 | .50 | .50 | 1.04*** | .22 | .09 | .37 |
| Live with spouse/partner | .10 | .18 | -.10 | .48 | -.03 | .13 | .04 | .23 | ||||||||
| Number of children 0–6 years old | -.01 | .09 | .14 | .21 | .09 | .07 | .13 | .11 | .07 | .08 | .09 | .14 | .04 | .07 | .04 | .12 |
| Number of children 7–17 years old | .02 | .08 | .16 | .19 | -.10+ | .06 | -.06 | .09 | −22** | .07 | .-.30* | .14 | .05 | .06 | .15 | .13 |
| Daily hours spent in childcare | -.03 | .02 | -.02 | .04 | .06*** | .02 | .03 | .02 | -.03+ | .02 | -.04 | .02 | .05* | .02 | .05+ | .03 |
| Employed | -.10 | .19 | .22 | .33 | .06 | .16 | .26 | .29 | .39+ | .21 | .69 | .45 | -.14 | .15 | .17 | .26 |
| Household's main income source | ||||||||||||||||
| Labour/business | .00 | .23 | .02 | .42 | -.09 | .22 | -.21 | .28 | -.76** | .25 | -.57+ | .34 | .28 | .19 | .19 | .31 |
| Government grants | -.21 | .26 | -.37 | .46 | -.25 | .25 | -.58+ | .34 | -.43 | .28 | -.25 | .37 | -.06 | .21 | -.52 | .37 |
| Support from NGO/church/similar | -.37 | .23 | .11 | .53 | -.25 | .48 | -.24 | .56 | .16 | .63 | .24 | .67 | -.36 | .36 | -.22 | .49 |
| Support from community/neighborhood | -.48 | .45 | -.08 | .60 | .24 | .27 | .04 | .34 | .68+ | .39 | .15 | .53 | -.32 | .25 | -.24 | .36 |
| African | -.36+ | .22 | -.53+ | .32 | .17 | .26 | .04 | .34 | -.12 | .25 | -.28 | .34 | -.12 | .23 | -.02 | .28 |
| Colored | .06 | .32 | .04 | .40 | .59+ | .33 | .72 | .47 | .09 | .32 | .04 | .44 | .47 | .31 | .87+ | .49 |
| Primary school or less | -.07 | .29 | -.00 | .41 | .27 | .19 | .13 | .27 | .10 | .24 | .01 | .31 | .32 | .24 | .34 | .32 |
| Complete secondary schooling | -.06 | .22 | -.01 | .28 | -.05 | .16 | -.21 | .23 | -.31 | .21 | -.55+ | .32 | .18 | .16 | .04 | .21 |
| Tertiary education | -.40+ | .21 | -.19 | .26 | -.23 | .15 | -.53* | .23 | -.30 | .24 | -.59 | .38 | -.09 | .16 | -.33 | .21 |
| Perceived at risk of getting COVID-19 | .23 | .17 | .10 | .24 | .22+ | .13 | .15 | .21 | .23 | .17 | -.02 | .29 | .22+ | .13 | .16 | .20 |
| Uncertain of risk of getting COVID-19 | -.53 | .25 | -.90** | .31 | -.19 | .18 | -.03 | .23 | -.24 | .24 | -.59* | .30 | -.40* | .18 | -.19 | .25 |
| Constant T1 | 1.66*** | .34 | 1.89** | .63 | .60 | .39 | 1.34** | .52 | 1.77*** | .41 | 2.36*** | .67 | .91** | .31 | 1.20* | .49 |
| Constant T2 | 1.42*** | .34 | 1.67* | .68 | .47 | .37 | 1.29* | .53 | 1.63*** | .40 | 2.31*** | .67 | .60* | .30 | .94+ | .53 |
Notes: Balanced panel sample used, and data is weighted appropriately. SEM estimation is performed using Full Information Maximum Likelihood. ***p < .001, **p < .01, *p < .05, +p < .10.
Source: NIDS-CRAM Waves 2 and 3 (2020) and Wave 5 (2021).
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abrahams Z., Lund C., Field S., Honikman S. Factors associated with household food insecurity and depression in pregnant South African women from a low socio-economic setting: a cross-sectional study. Soc. Psychiatr. Psychiatr. Epidemiol. 2018;53(4):363–372. doi: 10.1007/s00127-018-1497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addis M.E. Gender and depression in men. Clin. Psychol. Sci. Pract. 2008;15(3):153. [Google Scholar]
- Addis M.E., Mahalik J.R. Men, masculinity, and the contexts of help seeking. Am. Psychol. 2003;58(1):5. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- Allen N.L., Becerra B.J., Becerra M.B. Associations between food insecurity and the severity of psychological distress among African-Americans. Ethn. Health. 2018;23(5):511–520. doi: 10.1080/13557858.2017.1280139. [DOI] [PubMed] [Google Scholar]
- Allison P.D., Williams R., Moral-Benito E. Maximum likelihood for cross-lagged panel models with fixed effects. Socius. 2017;3 2378023117710578. [Google Scholar]
- Ammar A., Mueller P., Trabelsi K., et al. Psychological consquences of COVID-19 home confinement: the ECLB-COVID19 multicenter study. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0240204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Core indicators of nutritional status for difficult-to-sample populations. Anderson S.A., editor. J. Nutr. 1990;120:1559–1600. doi: 10.1093/jn/120.suppl_11.1555. [DOI] [PubMed] [Google Scholar]
- Atkinson M.P., Greenstein T.N., Lang M.M. For women, breadwinning can be dangerous: gendered resource theory and wife abuse. J. Marriage Fam. 2005;67(5):1137–1148. [Google Scholar]
- Basile K.C., Hall J.E., Walters M.L. Expanding resource theory and feminist-informed theory to explain intimate partner violence perpetration by court-ordered men. Violence Against Women. 2013;19(7):848–880. doi: 10.1177/1077801213497105. [DOI] [PubMed] [Google Scholar]
- Bentler P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berry D., Willoughby M.T. On the practical interpretability of cross‐lagged panel models: rethinking a developmental workhorse. Child Dev. 2017;88(4):1186–1206. doi: 10.1111/cdev.12660. [DOI] [PubMed] [Google Scholar]
- Bierman A. Marital status as contingency for the effects of neighborhood disorder on older adults' mental health. J. Gerontol.: Series B. 2009;64(3):425–434. doi: 10.1093/geronb/gbp010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biesanz J.C. In: Handbook of Structural Equation Modeling. Hoyle R.H., editor. The Guilford Press; 2012. Autoregressive longitudinal models; pp. 459–471. [Google Scholar]
- Blumberg S.J., Bialostosky K., Hamilton W.L., Briefel R.R. The effectiveness of a short form of the household food security scale. Am. J. Publ. Health. 1999;89(8):1231–1234. doi: 10.2105/ajph.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth A., Rustenbach E., McHale S. Early family transitions and depressive symptom changes from adolescence to early adulthood. J. Marriage Fam. 2008;70(1):3–14. [Google Scholar]
- Brown S.L. The effect of union type on psychological well-being: depression among cohabitors versus marrieds. J. Health Soc. Behav. 2000:241–255. [PubMed] [Google Scholar]
- Brown R.L., Richman J.A. Sex differences in mediating and moderating processes linking economic stressors, psychological distress, and drinking. J. Stud. Alcohol Drugs. 2012;73(5):811–819. doi: 10.15288/jsad.2012.73.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownhill S., Wilhelm K., Barclay L., Schmied V. ‘Big build’: hidden depression in men. Aust. N. Z. J. Psychiatr. 2005;39(10):921–931. doi: 10.1080/j.1440-1614.2005.01665.x. [DOI] [PubMed] [Google Scholar]
- Butler L.D., Nolen-Hoeksema S. Gender differences in responses to depressed mood in a college sample. Sex. Roles. 1994;30(5):331–346. [Google Scholar]
- Carter K.N., Kruse K., Blakely T., Collings S. The association of food security with psychological distress in New Zealand and any gender differences. Soc. Sci. Med. 2011;72(9):1463–1471. doi: 10.1016/j.socscimed.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Chonody J.M., Siebert D.C. Gender differences in depression: a theoretical examination of power. Affilia. 2008;23(4):338–348. [Google Scholar]
- Ciciurkaite G., Brown R.L. Food insecurity, psychological distress and alcohol use: understanding the salience of family roles for gender disparities. Health Sociol. Rev. 2018;27(3):294–311. [Google Scholar]
- Cleary A. Death rather than disclosure: struggling to be a real man. Ir. J. Sociol. 2005;14:155–176. [Google Scholar]
- Cleary A. Suicidal action, emotional expression, and the performance of masculinities. Soc. Sci. Med. 2012;74(4):498–505. doi: 10.1016/j.socscimed.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Coen S.E., Oliffe J.L., Johnson J.L., Kelly M.T. Looking for Mr. PG: masculinities and men's depression in a northern resource-based Canadian community. Health Place. 2013;21:94–101. doi: 10.1016/j.healthplace.2013.01.011. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Coltrane S. Research on household labor: modeling and measuring the social embeddedness of routine family work. J. Marriage Fam. 2000;62(4):1208–1233. [Google Scholar]
- Conger R.D., Wallace L.E., Sung Y., et al. Economic pressure in African American families: a replication and extension of the family stress model. Dev. Psychol. 2002;38:179. [PubMed] [Google Scholar]
- Connell R.W. Stanford University Press; 1987. Gender and Power: Society, the Person, and Sexual Politics. [Google Scholar]
- Cools S., Kotsadam A. Resources and intimate partner violence in Sub-Saharan Africa. World Dev. 2017;95:211–230. [Google Scholar]
- Crouter A.C., Booth A., editors. Work-family Challenges for Low-Income Parents and Their Children. Psychology Press; New York: 2014. [Google Scholar]
- DeVault M.L. University of Chicago Press; Chicago: 1994. Feeding the Family: the Social Organization of Caring as Gendered Work. [Google Scholar]
- Devries K.M., Mak J.K., Bacchus L.J., et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med. 2013;10(5) doi: 10.1371/journal.pmed.1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinour L.M., Bergen D., Yeh M.C. The food insecurity–obesity paradox: a review of the literature and the role food stamps may play. J. Am. Diet Assoc. 2007;107(11):1952–1961. doi: 10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Dooley D., Prause J., Ham-Rowbottom K.A. Underemployment and depression: longitudinal relationships. J. Health Soc. Behav. 2000:421–436. [PubMed] [Google Scholar]
- Durkheim E. The Free Press; New York: 1897/1951. Suicide. Translated by J.A. Spaulding and G. Simpson. [Google Scholar]
- Elwert F., Winship C. Endogenous selection bias: the problem of conditioning on a collider variable. Annu. Rev. Sociol. 2014;40:31–53. doi: 10.1146/annurev-soc-071913-043455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferree M.M. Beyond separate spheres: feminism and family research. J. Marriage Fam. 1990;52:866–884. [Google Scholar]
- Fertig A. 2019. The Long-Term Health Consequences of Childhood Food Insecurity. University of Kentucky Center for Poverty Research Discussion Paper Series. [Google Scholar]
- Garman E.C., Schneider M., Lund C. Perinatal depressive symptoms among low-income South African women at risk of depression: trajectories and predictors. BMC Pregnancy Childbirth. 2019;19(1):1–11. doi: 10.1186/s12884-019-2355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee K., Asim K. Parenting aggravation associated with food insecurity impacts children's behavior and development. Perspectives. 2018;2:71–77. [Google Scholar]
- Gibbs A., Jewkes R., Willan S., Washington L. Associations between poverty, mental health and substance use, gender power, and intimate partner violence amongst young (18-30) women and men in urban informal settlements in South Africa: a cross-sectional study and structural equation model. PLoS One. 2018;13(10) doi: 10.1371/journal.pone.0204956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg A.E., Perry-Jenkins M. Division of labor and working-class women's well-being across the transition to parenthood. J. Fam. Psychol. 2004;18(1):225. doi: 10.1037/0893-3200.18.1.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode W.J. Force and violence in the family. J. Marriage Fam. 1971;33:624–636. [Google Scholar]
- Grundström J., Konttinen H., Berg N., Kiviruusu O. Associations between relationship status and mental well-being in different life phases from young to middle adulthood. SSM-Popul. Health. 2021;14:100774. doi: 10.1016/j.ssmph.2021.100774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley C., Patil C.L. Food insecurity in rural Tanzania is associated with maternal anxiety and depression. Am. J. Hum. Biol.: Off. J. Human Biol. Assoc. 2006;18(3):359–368. doi: 10.1002/ajhb.20505. [DOI] [PubMed] [Google Scholar]
- Hager E., Quigg A., Black M., et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- Halaby C. Panel Models in Sociological Research. Annu. Rev. Sociol. 2004;30:507–544. [Google Scholar]
- Hamaker E.L., Kuiper R.M., Grasman R.P. A critique of the cross-lagged panel model. Psychol. Methods. 2015;20(1):102. doi: 10.1037/a0038889. [DOI] [PubMed] [Google Scholar]
- Hanson K.L., Sobal J., Frongillo E.A. Gender and marital status clarify associations between food insecurity and body weight. J. Nutr. 2007;137(6):1460–1465. doi: 10.1093/jn/137.6.1460. [DOI] [PubMed] [Google Scholar]
- Hatcher C. The handmaiden's tale: a feminist perspective. Aust. J. Commun. 1993;20:107–124. [Google Scholar]
- Hatcher A.M., Stöckl H., McBride R.S., et al. Pathways from food insecurity to intimate partner violence perpetration among peri-urban men in South Africa. Am. J. Prev. Med. 2019;56(5):765–772. doi: 10.1016/j.amepre.2018.12.013. [DOI] [PubMed] [Google Scholar]
- Heise L., Greene M.E., Opper N., et al. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. 2019;393(10189):2440–2454. doi: 10.1016/S0140-6736(19)30652-X. [DOI] [PubMed] [Google Scholar]
- Horwood C., Haskins L., Hinton R., et al. Addressing the interaction between food insecurity, depression risk and informal work: findings of a cross-sectional survey among informal women workers with young children in South Africa. BMC Wom. Health. 2021;21(1):1–12. doi: 10.1186/s12905-020-01147-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr. Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Sciences Research Council (HSRC) 2020 April 24. HSRC Responds to the Covid-19 Outbreak. http://www.hsrc.ac.za/uploads/pageContent/11529/COVID-19%20MASTER%20SLIDES %2026%20APRIL%202020%20FOR%20MEDIA% 20BRIEFING%20FINAL.pdf. [Google Scholar]
- Hunt X., Breet E., Stein D.J., Tomlinson M. 2021. The Covid-19 Pandemic, Hunger, and Depressed Mood Among South Africans. National Income Dynamics (NIDS)-Coronavirus Rapid Mobile Survey (CRAM) Wave 5 Working Paper. [Google Scholar]
- Ingle K., Brophy T., Daniels R.C. Southern Africa Labour and Development Research Unit; Cape Town: 2021. National Income Dynamics Study – Coronavirus Rapid Mobile Survey (NIDS-CRAM) 2020 - 2021 Panel User Manual. Beta 1 Release May 2021. Version 1. [Google Scholar]
- Jebena M.G., Lindstrom D., Belachew T., et al. Food insecurity and common mental disorders among Ethiopian youth: structural equation modeling. PLoS One. 2016;11(11) doi: 10.1371/journal.pone.0165931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jesson J., Dietrich J., Beksinska M., et al. Food insecurity and depression: a cross‐sectional study of a multi‐site urban youth cohort in Durban and Soweto, South Africa. Trop. Med. Int. Health. 2021;26(6):687–700. doi: 10.1111/tmi.13572. [DOI] [PubMed] [Google Scholar]
- Johnson A.D., Markowitz A.J. Food insecurity and family well-being outcomes among households with young children. J. Pediatr. 2018;196:275–282. doi: 10.1016/j.jpeds.2018.01.026. [DOI] [PubMed] [Google Scholar]
- Jones A.D. Food insecurity and mental health status: a global analysis of 149 countries. Am. J. Prevent. Med. 2017;53:264–273. doi: 10.1016/j.amepre.2017.04.008. [DOI] [PubMed] [Google Scholar]
- Joseph C., Feiner C., Leung C.W. Food insecurity is associated with serious psychological distress among low-income California adults. J. Health Psychol. 2021 doi: 10.1177/13591053211028913. 13591053211028913. [DOI] [PubMed] [Google Scholar]
- Kågesten A., Gibbs S., Blum R.W., et al. Understanding factors that shape gender attitudes in early adolescence globally: a mixed-methods systematic review. PLoS One. 2016;11(6) doi: 10.1371/journal.pone.0157805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendig H., Dykstra P.A., van Gaalen R.I., Melkas T. Health of aging parents and childless individuals. J. Fam. Issues. 2007;28(11):1457–1486. [Google Scholar]
- Kendler K.S., Gardner C.O., Neale M.C., Prescott C.A. Genetic risk factors for major depression in men and women: similar or different hereditabilities and same or partly distinct genes? Psychol. Med. 2001;31:605–616. doi: 10.1017/s0033291701003907. [DOI] [PubMed] [Google Scholar]
- Knoester C., Eggebeen D.J. The effects of the transition to parenthood and subsequent children on men's well-being and social participation. J. Fam. Issues. 2006;27(11):1532–1560. [Google Scholar]
- Koropeckyj-Cox T., Call V.R. Characteristics of older childless persons and parents: cross-national comparisons. J. Fam. Issues. 2007;28(10):1362–1414. [Google Scholar]
- Kroenker K., Spitzer R.L., Williams J.B., et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Lee J.W., Shin W.K., Kim Y. Impact of sex and marital status on the prevalence of perceived depression in association with food insecurity. PLoS One. 2020;15(6) doi: 10.1371/journal.pone.0234105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger L., Lourens M. Motherhood and the “Madness of Hunger”: “…Want Almal Vra vir My vir ‘n Stukkie Brood” (“…Because Everyone Asks Me for a Little Piece of Bread”) Cult. Med. Psychiatr. 2016;40:124–143. doi: 10.1007/s11013-015-9480-5. [DOI] [PubMed] [Google Scholar]
- Lee J., Kim H., Woo J., et al. Impacts of remaining single above the mean marriage age on mental disorders and suicidality: a nationwide study in Korea. J. Kor. Med. Sci. 2020;35(37) doi: 10.3346/jkms.2020.35.e319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leimkühler A.M., Heller J., Paulus N.C. Subjective well-being and ‘male depression’in male adolescents. J. Affect. Disord. 2007;98(1–2):65–72. doi: 10.1016/j.jad.2006.07.007. [DOI] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010;22:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- MacCallum R.C., Browne M.W., Sugawara H.M. Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods. 1996;1(2):130–149. [Google Scholar]
- Macmillan R., Gartner R. When she brings home the bacon: labor-force participation and the risk of spousal violence against women. J. Marriage Fam. 1999:947–958. [Google Scholar]
- Maharaj V., Tomita A., Thela L., et al. Food insecurity and risk of depression among refugees and immigrants in South Africa. J. Immigr. Minority Health. 2017;19(3):631–637. doi: 10.1007/s10903-016-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Sakib N., Gozal D., et al. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J. Affect. Disord. 2021;279:462–472. doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin M.A., Lippert A.M. Feeding her children, but risking her health: the intersection of gender, household food insecurity and obesity. Soc. Sci. Med. 2012;74(11):1754–1764. doi: 10.1016/j.socscimed.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin M.S., Maddocks E., Chen Y., et al. Food insecurity and mental illness: disproportionate impacts in the context of perceived stress and social isolation. Publ. Health. 2016;132:86–91. doi: 10.1016/j.puhe.2015.11.014. [DOI] [PubMed] [Google Scholar]
- McDonough P., Walters V. Gender and health: reassessing patterns and explanations. Soc. Sci. Med. 2001;52(4):547–559. doi: 10.1016/s0277-9536(00)00159-3. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., et al. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;234:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre L., Glanville N.T., Raine K.D., et al. Do low-income lone mothers compromise their nutrition to feed their children? Can. Med. Assoc. J. 2003;168(6):686–691. [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J., Ross C.E. Depression, parenthood, and age at first birth. Soc. Sci. Med. 2002;54(8):1281–1298. doi: 10.1016/s0277-9536(01)00096-x. [DOI] [PubMed] [Google Scholar]
- Möller-Leimkühler A.M. Barriers to help-seeking by men: a review of sociocultural and clinical literature with particular reference to depression. J. Affect. Disord. 2002;71(1–3):1–9. doi: 10.1016/s0165-0327(01)00379-2. [DOI] [PubMed] [Google Scholar]
- Morrow J., Nolen-Hoeksema S. Effects of responses to depression on the remediation of depressive affect. J. Pers. Soc. Psychol. 1990;58(3):519. doi: 10.1037//0022-3514.58.3.519. [DOI] [PubMed] [Google Scholar]
- Mund M., Johnson M.D., Nestler S. Changes in Size and Interpretation of Parameter Estimates in Within-Person Models in the Presence of Time-Invariant and Time-Varying Covariates. Front. Psychol. 2021:3663. doi: 10.3389/fpsyg.2021.666928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mund M., Nestler S. Beyond the cross-lagged panel model: next-generation statistical tools for analyzing interdependencies across the life course. Adv. Life Course Res. 2019;41:100249. doi: 10.1016/j.alcr.2018.10.002. [DOI] [PubMed] [Google Scholar]
- Myers C.A. Food insecurity and psychological distress: a review of the recent literature. Curr. Nutrition Rep. 2020;9:107–118. doi: 10.1007/s13668-020-00309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman M.S. Review of studies of mental health in Bangladesh, with a focus on depression. Int. J. Ment. Health Syst. 2013;42:48–77. [Google Scholar]
- Nomaguchi K.M. Parenthood and psychological well-being: clarifying the role of child age and parent–child relationship quality. Soc. Sci. Res. 2012;41(2):489–498. doi: 10.1016/j.ssresearch.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomaguchi K.M., Milkie M.A. Costs and rewards of children: the effects of becoming a parent on adults' lives. J. Marriage Fam. 2003;65(2):356–374. [Google Scholar]
- Nomaguchi K.M., Milkie M.A., Bianchi S.M. Time strains and psychological well-being: do dual-earner mothers and fathers differ? J. Fam. Issues. 2005;26(6):756–792. [Google Scholar]
- Normen L., Chan K., Braitstein P., et al. Food insecurity and hunger are prevalent among HIV-positive individuals in British Columbia, Canada. J. Nutr. 2005;135(4):820–825. doi: 10.1093/jn/135.4.820. [DOI] [PubMed] [Google Scholar]
- FAO, I. UNICEF . FAO; Rome: 2020. The State of Food Security and Nutrition in the World 2020. Transforming Food Systems for Affordable Healthy Diets. [Google Scholar]
- Oliffe J.L., Ogrodniczuk J.S., Bottorff J.L., et al. You feel like you can't live anymore”: suicide from the perspectives of Canadian men who experience depression. Soc. Sci. Med. 2012;74(4):506–514. doi: 10.1016/j.socscimed.2010.03.057. [DOI] [PubMed] [Google Scholar]
- Olson C.M. Food insecurity in women: a recipe for unhealthy trade-offs. Top. Clin. Nutr. 2005;20(4):321–328. [Google Scholar]
- Pearlin L.I. Life-span Developmental Psychology. Academic Press; 1975. Sex roles and depression; pp. 191–207. [Google Scholar]
- Pearlin L.I., Johnson J.S. Marital status, life-strains and depression. Am. Socio. Rev. 1977:704–715. [PubMed] [Google Scholar]
- Perkins J.M., Nyakato V.N., Kakuhikire B., et al. Food insecurity, social networks and symptoms of depression among men and women in rural Uganda: a cross-sectional, population-based study. Publ. Health Nutr. 2018;21(5):838–848. doi: 10.1017/S1368980017002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins J.M., Nyakato V.N., Kakuhikire B., et al. Food insecurity, social networks and symptoms of depression among men and women in rural Uganda: a cross-sectional, population-based study. Publ. Health Nutr. 2018;21(5):838–848. doi: 10.1017/S1368980017002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack W.S. In: New Psychotherapy for Men. Pollack W.S., Levant R.F., editors. John Wiley & Sons Inc; 1998. Mourning, melancholia, and masculinity: recognizing and treating depression in men; pp. 147–166. [Google Scholar]
- Posel D., Oyenubi A., Kollamparambil U. Job loss and mental health during the Covid-19 lockdown: evidence from South Africa. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0249352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourmotabbed A., Moradi S., Babaei A., et al. Food insecurity and mental health: a systematic review and meta-analysis. Publ. Health Nutr. 2020;23(10):1778–1790. doi: 10.1017/S136898001900435X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pudrovska T. Psychological implications of motherhood and fatherhood in midlife: evidence from sibling models. J. Marriage Fam. 2008;70(1):168–181. [Google Scholar]
- Quinones I.B. Women's mental health: reflections on the need for a comprehensive focus. Women’s Health Collect. 2001;6:44–49. [Google Scholar]
- Rani D., Singh J.K., Acharya D., et al. Household food insecurity and mental health among teenage girls living in urban slums in Varanasi, India: a cross-sectional study. Int. J. Environ. Res. Publ. Health. 2018;15(8):1585. doi: 10.3390/ijerph15081585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E., Mirowsky J. Explaining the social patterns of depression: control and problem solving—or support and talking? J. Health Soc. Behav. 1989:206–219. [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk R.H., Hyde J.S., Abramson L.Y. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017;143(8):783–822. doi: 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevilla A., Smith S. Baby steps: the gender division of childcare during the COVID-19 pandemic. Oxf. Rev. Econ. Pol. 2020;36(1):S169–S186. [Google Scholar]
- Sharp E. Available from Library and Archives Canada; 2010. Masculine Identity in a “Woman's” Role: Stay-At-Home Dads in Northern British Columbia. (Master's Thesis) [Google Scholar]
- Simon R.W. Gender, multiple roles, role meaning, and mental health. J. Health Soc. Behav. 1995:182–194. [PubMed] [Google Scholar]
- Smith L., Shin J.I., McDermott D.T., et al. Association between food insecurity and depression among older adults from low‐and middle‐income countries. Depress. Anxiety. 2021;38(4):439–446. doi: 10.1002/da.23147. [DOI] [PubMed] [Google Scholar]
- Sorsdahl K., Slopen N., Siefert K., et al. Household food insufficiency and mental health in South Africa. J. Epidemiol. Community Health. 2011;65(5):426–431. doi: 10.1136/jech.2009.091462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . vol. 17. StataCorp LLC; College Station, TX: 2021. (Stata Statistical Software: Release). [Google Scholar]
- Swindle T.M., Whiteside-Mansell L., McKelvey L. Food insecurity: validation of a two-item screen using convergent risks. J. Child Fam. Stud. 2013;22:932–941. [Google Scholar]
- Thomeer M.B., Umberson D., Pudrovska T. Marital processes around depression: a gendered and relational perspective. Soc. Ment. Health. 2013;3(3):151–169. doi: 10.1177/2156869313487224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng K.K., Park S.H., Shearston J.A., et al. Parental psychological distress and family food insecurity: sad dads in hungry homes. J. Dev. Behav. Pediatr. 2017;38(8):611–618. doi: 10.1097/DBP.0000000000000481. [DOI] [PubMed] [Google Scholar]
- UNICEF . 2021. The State of Food Security and Nutrition in the World 2021. Transforming Food Systems for Food Security, Improved Nutrition and Affordable Healthy Diets for All. Rome, FAO: FAO, IFAD, UNICEF, WFP and WHO. https://doi. org/10.4060/cb4474en. [Google Scholar]
- Umberson D. Family status and health behaviors: social control as a dimension of social integration. J. Health Soc. Behav. 1987;28:306–319. [PubMed] [Google Scholar]
- Umberson D. Gender, marital status and the social control of health behavior. Soc. Sci. Med. 1992;34(8):907–917. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- Umberson D., Pudrovska T., Reczek C. Parenthood, childlessness, and well-being: a life course perspective. J. Marriage Fam. 2010;72(3):612–629. doi: 10.1111/j.1741-3737.2010.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D., Thomeer M.B., Williams K. Family status and mental health: recent advances and future directions. Handb. Sociol. Mental Health. 2013:405–431. [Google Scholar]
- Van der Berg S., Patel L., Bridgman G. 2021. Food Insecurity in South Africa – Evidence from NIDS-CRAM Wave 5. National Income Dynamics (NIDS)-Coronavirus Rapid Mobile Survey (CRAM) Wave 5 Working Paper. [Google Scholar]
- Wang C., Pan R., Wan X., et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver L.J., Hadley C. Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol. Food Nutr. 2009;48(4):263–284. doi: 10.1080/03670240903001167. [DOI] [PubMed] [Google Scholar]
- Weigel M.M., Armijos R.X., Racines M., et al. Association of household food insecurity with the mental and physical health of low-income urban Ecuadorian women with children. J. Environ. Publ. Health. 2016:5256084. doi: 10.1155/2016/5256084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker C., Phillips S.M., Orzol S.M. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–e868. doi: 10.1542/peds.2006-0239. [DOI] [PubMed] [Google Scholar]
- Williams R., Allison P.D., Moral-Benito E. Linear dynamic panel-data estimation using maximum likelihood and structural equation modeling. STATA J. 2018;18(2):293–326. [Google Scholar]
- Woo H., Raley R.K. A small extension to "costs and rewards of children: the effects of becoming a parent on adults' lives. J. Marriage Fam. 2005:216–221. [Google Scholar]
- Wooldridge J.M. MIT press; 2010. Econometric Analysis of Cross Section and Panel Data. [Google Scholar]
- Wu Z., Schimmele C.M. Food insufficiency and depression. Socio. Perspect. 2005;48:481–504. [Google Scholar]
- Wupperman P., Neumann C.S. Depressive symptoms as a function of sex-role, rumination, and neuroticism. Pers. Indiv. Differ. 2006;40(2):189–201. [Google Scholar]
- Zamarro G., Prados M.J. Gender differences in couples' division of childcare, work and mental health during COVID-19. Rev. Econ. Househ. 2021;19(1):11–40. doi: 10.1007/s11150-020-09534-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zar H.J., Pellowski J.A., Cohen S., et al. Maternal health and birth outcomes in a South African birth cohort study. PLoS One. 2019;14(11) doi: 10.1371/journal.pone.0222399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Hayward M.D. Childlessness and the psychological well-being of older persons. J. Gerontol. B Psychol. Sci. Soc. Sci. 2001;56(5):S311–S320. doi: 10.1093/geronb/56.5.s311. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.