Abstract
Background:
Lesbian, gay, and bisexual individuals (―sexual minorities‖ [SMs]) are overrepresented among individuals suffering from alcohol and other drug (AOD) problems. However, little is known regarding differences, particularly in functioning and well-being, between SMs and heterosexuals in recovery from AOD problems.
Method:
Cross-sectional, nationally representative sample of US adults who resolved an AOD problem (N = 2002; National Recovery Study [Kelly et al, 2017]). Univariate analyses tested for differences between SMs and heterosexuals on socio-demographic, AOD use/treatment and clinical/legal factors. Unadjusted regressions tested for group differences on indices of current functioning and well-being. Multivariable regressions investigated factors that differentiated groups to understand which might explain any observed group disparities in functioning and well-being. LOWESS analyses explored differences across time in recovery on functioning/well-being.
Results:
Prevalence of SMs in the US recovery population was 11.7% (n=220). Compared with heterosexuals (88.3%, n=1666), SMs had shorter time in recovery (OR=0.97; 95% CI: 0.96, 0.99); were less likely to be employed (OR=0.64; 95% CI: 0.43, 0.96); and more likely to have a co-occurring psychiatric disorder (OR=2.24; 95% CI: 1.49, 3.37), an arrest history (OR=1.61; 95% CI: 1.08, 2.39), and report opioids as primary substance (OR=2.50; 95% CI: 1.18, 5.28). Unadjusted models showed, compared to heterosexuals, SMs had significantly worse levels on all functioning and well-being outcomes. Adjusted models explained most differences, except for psychological distress.
Conclusion:
SMs evince more problematic clinical/legal histories and face greater psychosocial challenges in recovery. Research is needed to understand the unique experiences of recovering SMs in order to better address observed functioning and well-being disparities.
Keywords: recovery, gay, lesbian, bisexual, addiction, LGBTQ
1. Introduction
Alcohol and other drug (AOD) disorders are a major public health concern in most middle- and high-income countries globally, conferring a prodigious burden of disease, injury, premature mortality, and economic costs (NIDA, 2020; SAMHSA, 2019; WHO, 2018). Sexual minorities [SMs], including adults who identify as lesbian, gay, or bisexual, are overrepresented among the AOD disorder population and suffer higher rates of mental health morbidity and comorbidity (Cochran et al., 2003; Lee et al., 2015). Compared to heterosexuals, SMs are between 50% and 250% more likely to report a psychiatric disorder (Kerridge et al., 2017).
Compared to the majority heterosexual population, SMs report hazardous drinking (Hughes, 2011; Hughes et al., 2014) and experience AOD disorders at significantly higher rates (Boyd et al., 2019; Chaudhry & Reisner, 2019; Cochran et al., 2003; Duncan et al., 2019; Grella et al., 2011; Hughes et al., 2010; Kecojevic et al., 2017; Kecojevic et al., 2012; Kerridge et al., 2017; McCabe et al., 2010; McCabe et al., 2009; McCabe et al., 2019; Mereish & Bradford, 2014; Rosario et al., 2014; Schuler et al., 2018; Valentino, 2020), and are approximately two times more likely to report any past year alcohol use disorder (AUD) or drug use disorder (DUD) (SM AUD, 21.5% and heterosexual AUD, 12.8%; SM DUD, 7.7% and heterosexual DUD, 3.8%; (Boyd et al., 2019)). Also, in terms of severity of disorder, 7.2% of SMs report severe AUD in the past-year, compared to only 2.9% of heterosexuals (Boyd et al., 2019). This increased prevalence of AOD disorders appears to be the case regardless of age—SMs show an approximate doubling of risk compared to heterosexuals in every age group (Han et al., 2020; Peralta et al., 2019).
Conceptually, the increased risk for AOD disorders and other psychiatric disorders encountered by SMs might be explained by epigenetic stress and coping theories (e.g., (Folkman & Moskowitz, 2000; Gottlieb, 2007; Lazarus, 2000)). Minority stress, for example, which refers to the unique, chronic interpersonal stressors that SMs face, including stigma, discrimination, and prejudice (Meyer, 2003), may serve as an epigenetic factor triggering onset of other substance use and mental health conditions. At the same time, SM may also have access to fewer social-psychological resources which could help to buffer against these increased stressors (e.g., social support; (Bryan et al., 2017; Gilbert & Zemore, 2016; Lee et al., 2016; Lehavot & Simoni, 2011; McCabe et al., 2010; McCabe et al., 2019; Slater et al., 2017; Vu et al., 2019)). Research has also documented greater rates of unemployment and homelessness among SM individuals stemming from discriminatory practices (Mallory and Sears, 2015).
Due to SMs being a uniquely high-risk population for AOD and related mental health problems, SMs have been shown to utilize more treatment services to resolve an AOD problem compared to heterosexuals (Grella et al., 2011; Grella et al., 2009; Hughes, 2011; McCabe et al., 2013; US Department of Health and Human Services, 2018). Allen and Mowbray (2016) found about 24% of gay and lesbian individuals with an AUD and 29% of bisexual individuals with an AUD sought treatment compared to about 14% of heterosexual individuals with an AUD (Allen & Mowbray, 2016).
In spite of higher treatment utilization, SMs also report more barriers to treatment compared to heterosexuals. Bisexual individuals, for example, have been shown to be substantially more likely to endorse barriers, such as, ―Did not think anyone could help,‖ when compared to heterosexual individuals (about 50% and 13%; respectively, (Allen & Mowbray, 2016)).Furthermore, SMs struggle finding treatment services that cater to their unique needs (Hughes, 2011), as very few SM-specific treatment programs exist (Mericle et al., 2018). Additional barriers are fears of discrimination (Jeong et al., 2016), stigma (Jeong et al., 2016), harassment (Brown et al., 2016), and being misunderstood (Brown et al., 2016). Therefore, even though SMs utilize treatment services at higher rates, a significant portion of SMs may delay seeking needed treatment (Allen & Mowbray, 2016; Corliss et al., 2006).
There is emerging literature on AOD disorder treatment amongst SMs, yet little is known about characteristics of recovering SMs. Also, while SMs are known to experience more treatment barriers, greater knowledge regarding SMs’ well-being and functioning across the recovery continuum would help inform SM-tailored services and policies. Such knowledge includes how SMs compare with the heterosexual majority in terms of AOD use and mental health histories, services used, recovery pathways followed, comfort in disclosing a history of an AOD problem, and quality of life (QOL) and psychological functioning. Research on such trajectories among those with significant AOD histories is emerging (Earnshaw et al., 2019; Kelly et al., 2017; Kelly et al., 2018), but little is known regarding the SM population, in particular, and how SMs compare to heterosexuals in terms of their characteristics, clinical histories, and well-being in recovery.
The current study uses a nationally representative sample of US adults who have successfully resolved a significant AOD problem (National Recovery Study; Kelly et al., 2017) to address these knowledge gaps for SMs, in part, by comparing their characteristics and experiences to those of their heterosexual counterparts. Specifically, the current study attempts to answer three main research questions: 1. What is the prevalence of SMs among those in the US population who have resolved a significant AOD problem; 2. How are SM and heterosexual individuals similar or different in terms of their demographics, clinical histories, and problem resolution pathways; and 3. To what extent do SM and heterosexual individuals differ in terms of QOL and psychological functioning and well-being outcomes following AOD problem resolution, and what factors in particular might explain any observed disparities. Greater knowledge regarding how SMs experience the recovery process compared to the majority heterosexual population could inform and enhance more targeted strategies and services to better meet the AOD recovery needs of this high-risk population.
2. Method
2.1. Sample and Procedure
Data for the current study comes from the National Recovery Study (NRS), described in more detail elsewhere (Earnshaw et al., 2019; Kelly et al., 2017; Kelly et al., 2018). In short, the NRS is a nationally representative sample of US adults (18+ years) who have resolved a significant AOD problem. Participants answered ―yes‖ to the screener question ―Did you used to have a problem with drugs or alcohol, but no longer do?‖ Data was collected using the survey company GfK via their KnowledgePanel (GfK, 2013), which is a geo-demographically representative sample that gathered adults via address-based sampling from 97% of all US households based on the US Postal Service’s Delivery Sequence File (see (Kelly et al., 2017) for more details).
From the KnowledgePanel, a subset of 39,809 US adults were invited by GfK to participate in the NRS by being asked the screener question. Of the 39,809 people who were sent the screener question, 25,229 responded (63.4%), which is a comparable response rate to other nationally representative surveys (Centers for Disease Control and Prevention, 2013; Grant et al., 2015). Out of 25,229 respondents, 2002 individuals answered ―yes‖ to the screener question and completed the survey (excludes 283 individuals who began the survey but did not complete it). Median time to completion was 24 minutes.
To ensure that the resulting sample represented the US population, differences between the sample and the US population were accounted for via sample weights created by Gfk using iterative proportional fitting methods (Battaglia et al., 2009). Base weights accounted for over- or under-coverage of geodemographic characteristics of those invited to respond to the screener question and systematic differential response to the screener question. Then, base weight adjustments were made so sample characteristics mapped onto eight geo-demographic benchmarks including gender, age, race/Hispanic ethnicity, education, census geographical region, household income, home ownership status, and metropolitan area (United States Census Bureau, 2015). This procedure produced unbiased estimates of the population of US adults for those in the NRS. Participants were 46.8 years of age, on average, and 60% were female. Most participants were Non-Hispanic White (61.3%), followed by Hispanic (17.5%), Non-Hispanic Black (13.9%), and other race/ethnicity (7.4%). Approximately half of participants were employed (54.3%), had at least some college education (51.5%), and reported a household income less than 50,000 USD (52.1%). Approximately one-third of participants had a lifetime psychiatric disorder and approximately half had an arrest history. With regard to substance use history, alcohol was the most frequently reported primary substance (58.7%). Six percent of the sample reported opioids as their primary substance.
All procedures were approved by the Partners HealthCare Institutional Review Board. Aims of this study were not pre-registered and thus results should be considered exploratory.
2.2. Measures
Sexual Orientation and other Socio-demographic and Clinical Characteristics
Participants reported their sexual orientation with response choices for ―heterosexual or straight,‖ ―gay or lesbian,‖ ―bisexual‖, or ―Something else‖. Additional demographics assessed were age, gender, race, education, and current employment status. Participants reported history of AUD, DUD, and any positive diagnoses of 16 other psychiatric disorders (Dennis, 2002). Specifically, participants were asked which of 16 common psychiatric disorders they’d ever been told they had by any clinician. Participants reported their history of arrests and court involvement to reflect criminal justice history.
Substance use history
Participants were asked which substances they have used 10+ times in their life based on a list of 15 substances (GAIN-I; (Dennis M, 2002)). For each substance endorsed, participants answered (1) whether they considered the substance a problem, (2) age of first use, and (3) primary substance (Brown et al., 1998), categorized into 1 of 4 primary substance groups: alcohol, cannabis, opioids, or other drugs. Additionally, participants reported how long it had been since resolving their problem (trichotomized into 0–5 years, 5–15 years, 15+ years) and whether they considered themselves ―in recovery‖ (yes/no). They also reported the number of ―serious attempts‖ made to resolve their AOD problem before they ―overcame‖ it.
Problem resolution pathway
Problem resolution pathway was broken down into ―assisted‖ vs ―unassisted‖ pathways. Participants were categorized as having used an ―assisted‖ resolution pathway if they reported lifetime use of any of the following professional or non-professional recovery management services: (1) professionally-assisted recovery support (e.g., outpatient or inpatient/residential treatment); (2) anti-relapse/craving medication (e.g., naltrexone [oral and injectable]) (Miller & Delboca, 1994)); (3) mutual-help groups (e.g., Alcoholics Anonymous); and (4) other community-based recovery support with trained staff (e.g., sober living environments, faith-based recovery services, or recovery community centers). Participants were categorized as having used an ―unassisted‖ resolution pathway if they reported never having used any of these services.
Disclosure comfort
The disclosure comfort scale was informed by findings from Romo et al. (2016) (Romo et al., 2016). Participants rated how comfortable they felt disclosing their status as someone who has resolved an AOD problem on a scale ranging from 1 = ―not at all comfortable‖ to 5 = ―completely comfortable.‖ Participants were asked about their disclosure comfort to a variety of recipients, including (1) to family, (2) to friends, (3) to co-workers, (4) to someone they are meeting for the first time, (5) in a public setting (e.g., at a community event), and (6) in the media (e.g., a newspaper article). The overall scale had strong internal reliability (α = 0.90) and disclosure comfort was scored by averaging across all six items.
Quality of Life
QOL was assessed using the EUROHIS-QOL (Schmidt et al., 2006), which is a widely used 8-item measure of QOL, adapted from the World Health Organization Quality of Life—Brief Version (α = 0.90).
Psychological Functioning and Well-being Outcomes
Participants rated their happiness on a scale from 1 = ―completely unhappy‖ to 5 = ―completely happy‖ (Meyers & Smith, 1995). They rated the extent to which ―I have high self-esteem‖ was true on a scale from 1 = ―not very true‖ to 5 = ―very true‖ (Robins et al., 2001). Recovery capital was assessed using the Brief Assessment of Recovery Capital (BARC-10; (Vilsaint et al., 2017)), which is a validated 10-item scale abridged from the Addiction Recovery Capital Scale (α = 0.93; (Groshkova et al., 2013)). Finally, psychological distress was assessed using the Kessler-6 (Kessler et al., 2003), which is a 6-item measure of psychiatric symptoms experienced during the past 30 days (α = 0.93).
2.3. Statistical Analysis
We compared the distribution of socio-demographics, clinical characteristics, AOD history, problem resolution pathways, and disclosure comfort between SM (lesbian, gay, or bisexual) and heterosexual participants using unadjusted logistic regression models. Sexual orientation was included as a binary outcome with each socio-demographic, AOD history, and clinical characteristic included as an independent variable in separate unadjusted logistic models. To examine the associations between sexual orientation and well-being outcomes (i.e., QOL, psychological distress, happiness, self-esteem, recovery capital), we built a series of regression models. First, we estimated the unadjusted association between sexual orientation and well-being outcomes (Table 2, Model 1). To explore whether observed differences in well-being outcomes by sexual orientation changed with time spent in recovery, we added the main effect of time spent in recovery (in years) and an interaction between sexual orientation and time spent in recovery (Table 2, Model 2). We then added in time spent in recovery and other socio-demographic characteristics that significantly differed by sexual orientation (Table 2, Model 3). In the fully adjusted model (Table 2, Model 4), we added the substance history, justice system involvement, and clinical variables that differed by sexual orientation to Model 3. Post-hoc analyses explored which of the socio-demographic, clinical, substance use history, and justice involvement variables appeared to explain the association between sexual orientation status and well-being outcomes individually (Table 3). Locally weighed scatterplot and smoothing (LOWESS) were computed to illustrate changes by time spent in recovery by sexual orientation grouping (figure 1). In all models, the reference group was heterosexual participants. All models incorporated survey weights and were conducted in Stata, Version 14.
Table 2.
Association between sexual orientation and well-being outcomes
| Model 1: Unadjusted | Model 2: Interaction with time in recovery | Model 3: Adjusted for time in recovery and employment | Model 4: Fully adjusted model | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| B | 95% CI | B | 95% CI | B | 95% CI | B | 95% CI | |
| Outcome: Quality of Life | ||||||||
| Sexual minority (ref=heterosexual) | −1.93 | 3.37, −0.49 | − 1.19 | −3.35, 0.96 | −1.26 | −2.62, 0.11 | −0.61 | −2.08, 0.87 |
| Time in recovery (years) | 0.15 | 0.11, 0.19 | 0.15 | 0.11, 0.19 | 0.15 | 0.10, 0.19 | ||
| Employed (ref=unemployed) | 2.94 | 2.06, 3.82 | 3.17 | 2.26, 4.07 | ||||
| Primary substance: opioids (ref=other) | −0.77 | −3.09, 1.54 | ||||||
| Psychiatric diagnosis | −2.56 | −3.51, −1.61 | ||||||
| Prior arrest(s) | −0.66 | −1.56, 0.23 | ||||||
| Sexual minority x Time in recovery | −0.04 | −0.20, 0.11 | ||||||
| Outcome: Psychological Distress | ||||||||
| Sexual minority (ref=heterosexual) | 2.42 | 1.09, 3.76 | 2.80 | 0.77, 4.82 | 2.03 | 0.75, 3.30 | 1.39 | 0.12, 2.67 |
| Time in recovery (years) | −0.14 | −0.17, −0.11 | −0.15 | −0.18, −0.12 | −0.13 | −0.16, −0.09 | ||
| Employed (ref=unemployed) | −0.63 | −1.33, 0.06 | −0.57 | −1.29, 0.15 | ||||
| Primary substance: opioids (ref=other) | 0.75 | −0.71, 2.20 | ||||||
| Psychiatric diagnosis | 4.01 | 3.20, 4.82 | ||||||
| Prior arrest(s) | 0.38 | −0.32, 1.07 | ||||||
| Sexual minority x Time in recovery | −0.07 | −0.21, 0.06 | ||||||
| Outcome: Happiness | ||||||||
| Sexual minority (ref=heterosexual) | −0.27 | −0.48, −0.05 | −0.33 | −0.64, −0.02 | −0.20 | −0.41, 0.00 | −0.13 | −0.35, 0.10 |
| Time in recovery (years) | 0.02 | 0.01, 0.02 | 0.02 | 0.01, 0.03 | 0.02 | 0.01, 0.02 | ||
| Employed (ref=unemployed) | 0.18 | 0.06, 0.31 | 0.20 | 0.07, 0.33 | ||||
| Primary substance: opioids (ref=other) | −0.14 | −0.45, 0.16 | ||||||
| Psychiatric diagnosis | −0.31 | −0.45, −0.17 | ||||||
| Prior arrest(s) | −0.10 | −0.23, 0.03 | ||||||
| Sexual minority x Time in recovery | 0.01 | −0.01, 0.03 | ||||||
| Outcome: Self-Esteem | ||||||||
| Sexual minority (ref=heterosexual) | −0.35 | −0.58, −0.13 | −0.20 | −0.54, 0.14 | −0.28 | −0.50, −0.05 | −0.14 | −0.37, 0.09 |
| Time in recovery (years) | 0.03 | 0.02, 0.03 | 0.03 | 0.02, 0.03 | 0.02 | 0.02, 0.03 | ||
| Employed (ref=unemployed) | 0.19 | 0.03, 0.34 | 0.20 | 0.05, 0.36 | ||||
| Primary substance: opioids (ref=other) | −0.38 | −0.72, −0.04 | ||||||
| Psychiatric diagnosis | −0.58 | −0.75, −0.41 | ||||||
| Prior arrest(s) | −0.01 | −0.16, 0.15 | ||||||
| Sexual minority × Time in recovery | −0.01 | −0.03, 0.01 | ||||||
| Outcome: Recovery Capital | ||||||||
| Sexual minority (ref=heterosexual) | −2.61 | −4.72, −0.51 | −2.00 | −5.28, 1.28 | −1.91 | −3.97, 0.15 | −1.61 | −3.70, 0.48 |
| Time in recovery (years) | 0.23 | 0.16, 0.29 | 0.23 | 0.17, 0.29 | 0.19 | 0.13, 0.25 | ||
| Employed (ref=unemployed) | 1.73 | 0.38, 3.08 | 1.78 | 0.43, 3.12 | ||||
| Primary substance: opioids (ref=other) | −2.92 | −5.84, 0.00 | ||||||
| Psychiatric diagnosis | −3.06 | −4.45, −1.66 | ||||||
| Prior arrest(s) | −0.56 | −1.86, 0.74 | ||||||
| Sexual minority x Time in recovery | −0.01 | −0.26, 0.23 | ||||||
Note: Bolded entries are statistically significant at p<0.05.
Table 3.
Post-hoc analyses investigating which clinical/legal variables (i.e., primary substance, psychiatric diagnosis, arrest history) might explain associations between sexual orientation and well-being outcomes
| Confounder: Primary | Confounder: Psychiatric | Confounder: | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| substance (opioids, ref=other) | diagnosis | Arrest history | ||||
|
|
|
|
||||
| B | 95% CI | B | 95% CI | B | 95% CI | |
| Outcome: Quality of Life | ||||||
| Sexual minority (ref=heterosexual) | −1.08 | −2.53, 0.36 | −0.84 | −2.23, 0.56 | −1.14 | −2.50, 0.21 |
| Time in recovery (years) | 0.16 | 0.12, 0.20 | 0.14 | 0.10, 0.18 | 0.15 | 0.11, 0.19 |
| Employed (ref=unemployed) | 3.45 | 2.53, 4.37 | 2.59 | 1.73, 3.44 | 2.95 | 2.07, 3.83 |
| Potential confounder | −1.26 | −3.51, 0.98 | −2.81 | −3.73, −1.89 | −0.86 | −1.72, 0.01 |
| Outcome: Psychological Distress | ||||||
| Sexual minority (ref=heterosexual) | 2.07 | 0.73, 3.41 | 1.44 | 0.20, 2.68 | 1.96 | 0.70, 3.21 |
| Time in recovery (years) | −0.15 | −0.18, −0.12 | −0.13 | −0.16, −0.10 | −0.15 | −0.18, −0.12 |
| Employed (ref=unemployed) | −1.02 | −1.77, −0.26 | −0.15 | −0.82, 0.51 | −0.64 | −1.33, 0.06 |
| Potential confounder | 1.34 | −0.25, 2.94 | 3.91 | 3.15, 4.67 | 0.52 | −0.16, 1.20 |
| Outcome: Happiness | ||||||
| Sexual minority (ref=heterosexual) | −0.19 | −0.41, 0.04 | −0.15 | −0.36, 0.06 | −0.19 | −0.40, 0.02 |
| Time in recovery (years) | 0.02 | 0.01, 0.03 | 0.02 | 0.01, 0.02 | 0.02 | 0.01, 0.03 |
| Employed (ref=unemployed) | 0.23 | 0.10, 0.37 | 0.14 | 0.02, 0.26 | 0.19 | 0.06, 0.31 |
| Potential confounder | −0.20 | −0.50, 0.09 | −0.35 | −0.48, −0.22 | −0.11 | −0.23, 0.01 |
| Outcome: Self-Esteem | ||||||
| Sexual minority (ref=heterosexual) | −0.23 | −0.47, 0.00 | −0.18 | −0.40, 0.03 | −0.27 | −0.50, −0.05 |
| Time in recovery (years) | 0.03 | 0.02, 0.03 | 0.02 | 0.02, 0.03 | 0.03 | 0.02, 0.03 |
| Employed (ref=unemployed) | 0.27 | 0.11, 0.43 | 0.11 | −0.04, 0.26 | 0.19 | 0.03, 0.34 |
| Potential confounder | −0.44 | −0.78, −0.10 | −0.63 | −0.79, −0.47 | −0.04 | −0.19, 0.11 |
| Outcome: Recovery Capital | ||||||
| Sexual minority (ref=heterosexual) | −2.16 | −4.26, −0.05 | −1.41 | −3.43, 0.62 | −1.78 | −3.82, 0.27 |
| Time in recovery (years) | 0.21 | 0.15, 0.27 | 0.21 | 0.15, 0.27 | 0.23 | 0.17, 0.29 |
| Employed (ref=unemployed) | 2.14 | 0.78, 3.50 | 1.30 | −0.01, 2.60 | 1.73 | 0.38, 3.08 |
| Potential confounder | −3.29 | −6.29, −0.28 | −3.44 | −4.85, −2.04 | −1.05 | −2.36, 0.26 |
Note: Bolded entries are statistically significant at p<0.05.
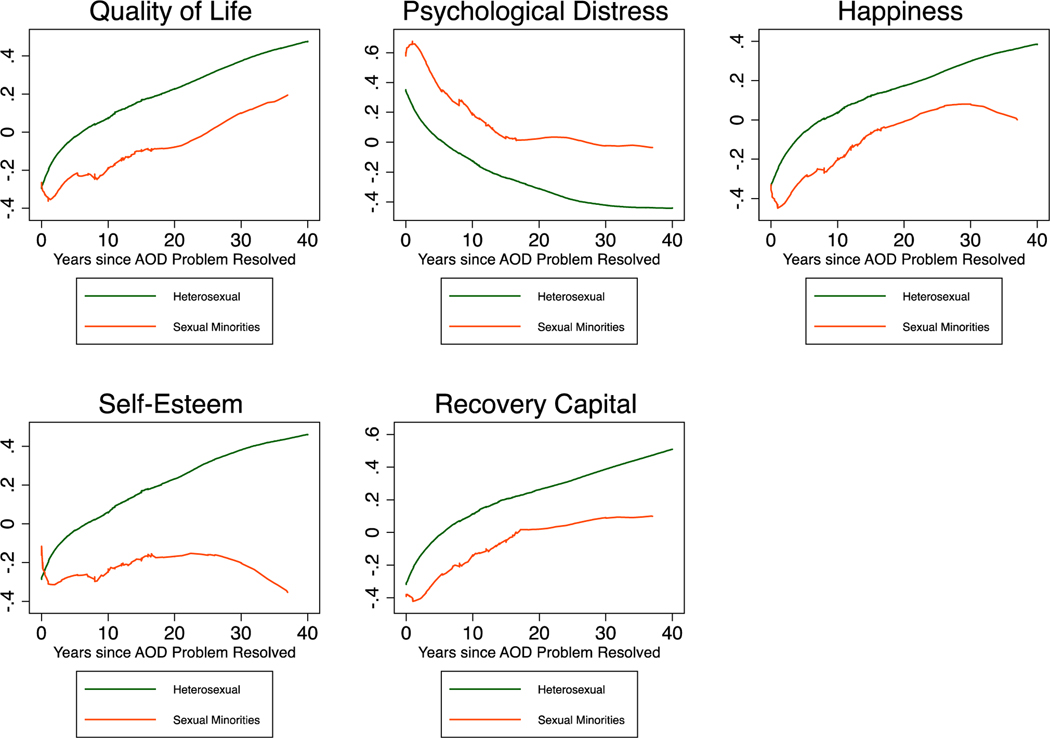
Figure 1. Well-being outcomes by time in recovery and sexual orientation (standardized Z-scores).
Note: All analyses of between-group differences by time spent in recovery were non-significant
3. Results
3.1. Prevalence of SM individuals among those in the US population who have resolved a significant AOD problem
The proportion of the sample that identified as SM (lesbian, gay, or bisexual) was 11.7% (Table 1). The SM group included n=17 individuals who self-identified as ―Something else‖ other than heterosexual or lesbian, gay, or bisexual.
Table 1.
Characteristics of the study population
| Heterosexual (n=1666; 88.34%) | Sexual Minority (n=220; 11.66%) | OR (95% CI) | |
|---|---|---|---|
| Socio-demographic characteristics | |||
| Age, M(SE) | 47.08 (0.56) | 44.3 (129) | 0.99 (0.98, 1.00) |
| Male gender, n(%) | 987.3 (59.27) | 144.0 (65.50) | 1.30 (0.87, 1.95) |
| Race Ethnicity, n(%) | |||
| White, Non-Hispanic | 1032.2 (61.96) | 123.3 (56.06) | REF |
| Black, Non-Hispanic | 231.9 (13.92) | 29.2 (13.29) | 1.06 (0.54, 2.05) |
| Hispanic | 289.5 (17.38) | 40.5 (18.41) | 1.17 (0.66, 2.07) |
| Other, Non-Hispanic | 112.3 (6.74) | 26.9 (12.24) | 2.01 (0.96, 4.19) |
| Household Income, n(%) | |||
| Less than 50,000 USD | 869.4 (52.19) | 113.3 (51.54) | REF |
| 50,000 USD or greater | 796.6 (47.81) | 106.6 (48.46) | 1.03 (0.68, 1.54) |
| Employment, n(%) | |||
| Unemployed | 739.7 (44.40) | 122.1 (55.51) | REF |
| Employed | 926.3 (55.60) | 97.8 (44.49) | 0.64 (0.43, 0.96) |
| College Education, n(%) | |||
| No College | 828.9 (49.76) | 86.2 (39.21) | REF |
| College | 837.0 (50.24) | 133.7 (60.79) | 1.54 (0.99, 2.38) |
| Substance use history and recovery pathways | |||
| Age of onset (primary substance), M(SE) | 19.81 (0.23) | 20.8 (0.65) | 1.02 (1.00, 1.05) |
| Years Since AOD Problem Resolved, M(SE) | 12.5 (.35) | 9.68 (0.76) | 0.97 (0.96, 0.99) |
| Number of quit attempts, M(SE) | 5.34 (0.57) | 5.78 (131) | 1.00 (0.99, 1.02) |
| Primary substance, n(%) | |||
| Alcohol | 862.5 (59.91) | 99.5 (49.86) | 0.67 (0.43, 1.02) |
| Cannabis | 195.0 (13.55) | 17.6 (8.81) | 0.62 (0.27, 1.43) |
| Opioid | 73.9 (5.14) | 23.8 (11.92) | 2.50 (1.18, 5.28) |
| Other | 308.1 (21.40) | 58.7 (29.40) | 1.53 (0.95, 2.46) |
| Outpatient addiction treatment, n(%) | 274.4 (16.47) | 48.7 (22.13) | 1.44 (0.87, 2.39) |
| Inpatient addiction treatment, n(%) | 244.1 (14.65) | 41.6(18.90) | 1.36 (0.83, 2.22) |
| How comfortable are you disclosing your status as a person in recovery, M(SE) | |||
| Family | 3.89 (0.05) | 3.65 (0.14) | 0.89 (0.78, 1.02) |
| Friends | 3.80 (0.05) | 3.71 (0.13) | 0.96 (0.83, 1.10) |
| Co-Workers, | 3.04 (0.06) | 2.87 (0.15) | 0.94 (0.83, 1.06) |
| Someone you’re meeting for the first time | 2.58 (0.05) | 2.48 (0.14) | 0.96 (0.85, 1.08) |
| In a public setting, | 2.53 (0.05) | 2.49(0.13) | 0.98 (0.88, 1.10) |
| In the media | 2.30 (0.05) | 2.17 (0.13) | 0.95 (0.84, 1.07) |
| Other clinical and criminal justice history variables | |||
| Psychiatric diagnosis (excluding AUD/SUD), n(%) | 517.4 (31.06) | 110.4 (50.22) | 2.24 (1.49, 3.37) |
| Have you ever been arrested?, n(%) | 829.9 (50.09) | 135.7 (61.74) | 1.61 (1.08, 2.39) |
Note: Bolded entries are statistically significant at p<0.05.
Note: Table frequencies are weighted to reflect population estimates and thus contain non-integer/decimal placed values.
3.2. Differences between SM and heterosexual groups in terms of their demographics, clinical histories, and problem resolution pathways
SM participants were less likely to be employed relative to heterosexual participants (OR=0.64; 95% CI: 0.43, 0.96). SM participants were more likely than heterosexual participants to have a co-occurring psychiatric disorder (OR=2.24; 95% CI: 1.49, 3.37) and arrest history (OR=1.61; 95% CI: 1.08, 2.39). We did not observe differences in age, gender, race/ethnicity, household income, or education by sexual orientation.
Of all participants who reported opioids as their primary substance, SM participants were over-represented; SMs displayed 2.5-fold greater odds of reporting opioids as their primary substance relative to heterosexual participants (95% CI: 1.18, 5.28), but were not significantly different across other substances. Also, SMs reported significantly fewer years since problem resolution relative to heterosexual participants (OR=0.97; 95% CI: 0.96, 0.99). The prevalence of prior inpatient or outpatient treatment history, number of serious quit attempts, disclosure comfort, and age of onset of regular substance use did not differ as a function of sexual orientation (ps>.05; Table 1).
3.3. SM and heterosexual group differences in QOL, psychological functioning, and well-being outcomes following AOD problem resolution, and factors that might explain observed disparities
Relative to heterosexual participants, SM participants reported significantly lower levels of QOL, happiness, self-esteem, recovery capital, and higher levels of psychological distress overall (Table 2; Model 1). When examining these between-group differences over time in recovery (i.e., tests of the group x time interaction), while the groups look quite different over time on these outcomes (see Figure 1), there was considerable variability within groups over time in recovery contributing to the failure to detect statistically significant differences (Table 2, Model 2).
To investigate which of the identified variables on which the SM and heterosexual groups differed (see section 3.3) might help explain the observed disparities on well-being outcomes, we conducted model building analyses controlling for these variables. The rationale for this approach is that if, on adding variables into the model that differed between groups, we see an attenuation in the magnitude of the group difference regarding well-being outcomes and/or the effect is rendered non-significant, it would suggest that these variables may partially explain the observed disparity.
In Table 2, Model 3, we began this process by controlling for time in recovery as well as employment - which was the only socio-demographic variable that differed by sexual orientation. Controlling for these two variables, we found some attenuation in the associations between sexual orientation and our well-being outcomes. However, all well-being outcomes remained either significant or marginally significant (see Table 2, Model 3), suggesting that these variables failed to fully explain the observed between-group well-being disparity. Continuing this investigation further, we next included the clinical/legal variables that showed between-group differences in our prior analyses (i.e., primary substance, co-occurring psychiatric diagnosis, and arrest history; see section 3.3.). When adding these to the model, we no longer observed significant associations between sexual orientation and our well-being outcomes of QOL, happiness, self-esteem, and recovery capital (Table 2, Model 4). However, SM participants continued to display significantly greater psychological distress relative to heterosexual participants (Mean Difference=1.39; 95% CI: 0.12, 2.67).
To determine which of the three clinical/legal variables, in particular, was responsible for explaining the sexual orientation group differences on our well-being outcomes of QOL, happiness, self-esteem, and recovery capital, we conducted additional post-hoc analyses (Table 3). While again adjusting for time in recovery and employment, we sequentially investigated the attenuating effect of including each of these three potential explanatory variables individually. When adding either primary substance or arrest history to the model, we found some moderate attenuation in the association between sexual orientation and our well-being outcomes. In contrast, adding co-occurring psychiatric diagnosis to this model substantially attenuated the associations between sexual orientation and well-being outcomes, such that the associations between sexual orientation and well-being outcomes were all rendered non-significant, except for psychological distress. This suggests that the presence of a co-occurring psychiatric diagnosis might be a more major factor in helping to explain these disparities in functioning and well-being.
4. Discussion
This investigation estimated the national prevalence of SMs in recovery and compared SM and heterosexual individuals on socio-demographic, clinical, and service use characteristics as well as indices of QOL, functioning, and well-being. The prevalence of SM individuals in recovery translates into approximately 2.6 million adults in the US general population. Compared to heterosexual individuals, SM individuals differed on several socio-demographic and clinical/legal factors. Notably, the SM group showed significant disadvantages across well-being outcomes in recovery, which appeared to be partially accounted for by differences in socio-demographic and clinical/legal factors.
4.1. Prevalence of SM individuals in Recovery
In the recovery sample, 11.7% of individuals identified as SM. This percentage is notable because the estimated number of SM individuals in the US population is 4.5% (Conron & Goldberg, 2020). This means that the SM community is over-represented in the recovery population. Having a substantial number of SM individuals in recovery is consistent with previous literature indicating SM individuals are about two times more likely to have any AOD disorder (Boyd et al., 2019). Furthermore, this is the first estimate of the number of SMs in the US adult population who are in recovery – 2.6 million – demonstrating that SM people represent a large constituency of the AOD recovery population.
4.2. Differences between SM and heterosexual individuals in terms of demographics, clinical histories, and problem resolution pathways
When comparing characteristics between SM and heterosexual individuals, differences arose on several socio-demographic and clinical/legal factors: employment, years since problem resolution, opioids as primary substance, co-occurring psychiatric disorder, and arrest history. SM individuals were significantly less likely to be employed relative to heterosexual individuals, which could be due to increased levels of discrimination and mental health severity (Meyer, 2003). More research is needed to understand the exact reasons for this disparity, but it may point to a need for providing employment assistance services to SM individuals in recovery. SM individuals also reported significantly fewer years since AOD problem resolution, meaning SMs, on average, have fewer years of sustained long-term recovery. This may signify that more SM individuals struggle to maintain long-term recovery. Possibly greater psychiatric comorbidity and minority stress that this group is shown to experience (Meyer, 2003) distinguish and may well complicate their recovery trajectories compared to heterosexual individuals.
SMs reported significantly more co-occurring psychiatric disorders compared to heterosexuals, which is consistent with and supported by past literature (Cochran et al., 2003; Kerridge et al., 2017; Lee et al., 2015). The trauma, stress, and strain of coping with a SM status in a predominantly heterosexual society may lead to a higher density of psychopathology through experiences of internalized homophobia and discrimination (Hequembourg & Dearing, 2013; McCabe et al., 2019). SMs were also 2.5 times more likely to report opioids as their primary substance compared to heterosexuals. However, it is important to note that this was a small portion of the sample as the vast majority in both groups reported alcohol as their primary substance. Prior evidence suggests that SM individuals are more likely to use opioids compared to heterosexual individuals (Duncan et al., 2019; Kecojevic et al., 2012). Further research is needed to understand this phenomenon and whether opioid pharmacodynamics and pharmacokinetics may mitigate the kinds of specific stress associated with SM status better than other substances. However, this is pure speculation as there is not good evidence for people choosing a drug for a specific symptom profile. Qualitative research could potentially inform the phenomenology in this regard.
SMs were significantly more likely to report an arrest history, having 61% higher odds of being arrested at some point in their life relative to heterosexuals. We do not know the reason for such arrests and more work is needed to understand this increased arrest prevalence. It is possible that higher rates of intimate partner violence (Rollè et al., 2018), violence perpetrated by police officers (National Coalition of Anti-Violence Programs, 2016), and potentially discrimination related to substance use (e.g., searching vehicles for substances without probable cause) may explain higher arrests rates among SM compared to heterosexual adults. It is plausible that increased levels of stress, discrimination, and stigma experienced by SMs may contribute to this phenomenon. Finally, contrary to prior research findings, we did not find that SM individuals were more likely have received prior treatment for AOD. Despite statistical non-significance, the effect sizes reflected a 44% greater odds of prior outpatient treatment and a 36% higher odds of receiving inpatient treatment for the SM group. The non-significant effects despite arguably meaningful magnitude differences thus reflect the substantial variability inherent in these group treatment estimates and the high heterogeneity more generally in this population sample of ―AOD problem resolvers‖ which includes people with very mild problems through to severe disorders.
4.3. SM and heterosexual group differences in QOL, psychological functioning, and well-being outcomes following AOD problem resolution, and factors that might explain observed disparities
Significant disparities were observed in well-being outcomes by group. Specifically, SMs experienced lower levels of current QOL, happiness, self-esteem, and recovery capital, and higher levels of current psychological distress, relative to heterosexuals overall. It is noteworthy how stable the differences disadvantaging the SM group were across well-being outcomes. We also found, when examining significant socio-demographic and clinical/legal factors in the univariate models, disparities in well-being in recovery, in part, were explained by employment, years since problem resolution, opioids as primary substance, co-occurring psychiatric disorder, and arrest history. These differences appeared to be explained more by the clinical/legal factors, yet, despite including these significant factors in the model - in an attempt to try to explain what may be accounting for these differences - there still remained a significant independent effect of SM status on psychological distress. Thus, while the constellation of factors in this study could be conceived as partially explaining why the SM group exhibited disparities in psychological distress, there are other factors not included here that might help explain the increased psychological distress in SMs. It is possible that SMs are experiencing the additional burden related to the double stigma of ongoing experiences of discrimination related to SM status as well as that of being in recovery from an AOD problem - which itself carries significant discrimination (Vilsaint et al., 2020). Future research is needed to clarify factors underlying SMs’ greater distress to inform treatment and recovery support services for this high-risk group.
4.4. Limitations
The study was cross-sectional thus, although differences between groups by time in recovery suggested changes in psychosocial and well-being indices over time, it needs to be confirmed using prospective analyses. In addition, gay and lesbian individuals were clustered together with those identifying as bisexual and were not separated by gender. Analyses on these subgroups will be important for future research to examine given the reported different experiences of such groups that may further moderate the overall pattern findings reported here. Also, many included individuals started their recovery journey at various points during the past 40 years and it is possible that the progress made by the gay rights movement in recent years (e.g., marriage equality) may affect SM individuals’ recovery journeys differently. Another limitation is the survey did not assess experiences of discrimination and homophobia, both internal and external, that may have affected SM individuals’ well-being in recovery. These are important areas for future investigation. Finally, because these analyses were not pre-registered and multiple tests were conducted, potentially inflating type I error rates, analyses here should be considered exploratory and findings tentative pending further confirmation with more rigorous a priori structured testing.
4.5. Conclusions and Implications
Overall, we found there is a substantial number of SM individuals in the US AOD recovery population – 2.6 million (11.7%). Comparing SM and heterosexual individuals, we found significant differences on several socio-demographic and clinical/legal factors disadvantaging SM individuals. Furthermore, SM individuals were significantly disadvantaged across all indices of psychological functioning and well-being once in AOD recovery. These differences in well-being outcomes appeared to be at least partially explained by a constellation of stressors (e.g., history of psychiatric comorbidity). However, despite potentially accounting for some of these disparities with measured model variables, the SM group still experienced greater psychological distress that was not explained by factors in this study. It is plausible that ongoing greater distress may be related to ongoing sexual orientation-based stigma and discrimination. Further qualitative and quantitative research is needed to investigate this and also whether social and structural stigma lead to public and internalized discrimination that make it more difficult for SM individuals to experience the same levels of well-being in recovery as their heterosexual counterparts.
This study also has important policy and health care implications for the SM recovery community. Given how SMs are a high-risk population for AOD problems and comorbidity (Boyd et al., 2019; Cochran et al., 2003; Lee et al., 2015) and appear to be disadvantaged in recovery, investing in more SM-sensitive and appropriate treatment and recovery support options should be a key priority. Indeed, national data estimates that only about one in five AOD treatment programs in the United States (17.6%; Williams and Fish, 2020) offer SM-specific programming suggesting that both development and adoption of more fitting services that can engage and better meet the needs of the SM community are sorely neeed..
Highlights.
Prevalence of sexual minorities in the US recovery population was 11.7%.
Sexual minorities are less likely to be employed in recovery.
Sexual minorities are more likely to have a co-occurring psychiatric disorder.
Sexual minorities are more likely to have an arrest history.
Sexual minorities had significantly worse levels of well-being in recovery.
Acknowledgments
Role of Funding Source
This work was supported by Massachusetts General Hospital Recovery Research Institute (No: RRI081715N) and NIAAA (K24AA022136; K23AA025707).
Funding: This work was supported by Massachusetts General Hospital Recovery Research Institute and NIAAA (K24AA022136; K23K23AA025707)
Footnotes
Declarations of interests: None.
Author Disclosures
Conflict of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen JL, & Mowbray O. (2016). Sexual orientation, treatment utilization, and barriers for alcohol related problems: Findings from a nationally representative sample. Drug Alcohol Depend, 161, 323–330. 10.1016/j.drugalcdep.2016.02.025 [DOI] [PubMed] [Google Scholar]
- Battaglia MP, Hoaglin DC, & Frankel MR (2009). Practical Considerations in Raking Survey Data. Survey Practice, 2(5), 1–10. 10.29115/SP-2009-0019 [DOI] [Google Scholar]
- Boyd CJ, Veliz PT, Stephenson R, Hughes TL, & McCabe SE (2019). Severity of Alcohol, Tobacco, and Drug Use Disorders Among Sexual Minority Individuals and Their “Not Sure” Counterparts. LGBT Health, 6(1), 15–22. 10.1089/lgbt.2018.0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A, Rice SM, Rickwood DJ, & Parker AG (2016). Systematic review of barriers and facilitators to accessing and engaging with mental health care among at-risk young people. Asia Pac Psychiatry, 8(1), 3–22. 10.1111/appy.12199 [DOI] [PubMed] [Google Scholar]
- Brown S, Myers M, Lippke L, Tapert S, Stewart D, & Vik P. (1998). Psychometric Evaluation of the Customary Drinking and Drug Use Record (CDDR): A Measure of Adolescent Alcohol and Drug Involvement. Journal of Studies on Alcohol, 59(4), 427. 10.15288/jsa.1998.59.427 [DOI] [PubMed] [Google Scholar]
- Bryan AEB, Kim H-J, & Fredriksen-Goldsen KI (2017). Factors associated with high-risk alcohol consumption among LGB older adults: The roles of gender, social support, perceived stress, discrimination, and stigma. The Gerontologist, 57(Suppl 1), S95–S104. 10.1093/geront/gnw100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2013). Unweighted Response Rates for the NHANES 2011–2012. Centers for Disease Control and Prevention. [Google Scholar]
- Chaudhry AB, & Reisner SL (2019). Disparities by Sexual Orientation Persist for Major Depressive Episode and Substance Abuse or Dependence: Findings from a National Probability Study of Adults in the United States. LGBT Health, 6(5), 261–266. 10.1089/lgbt.2018.0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Mays VM, & Sullivan JG (2003). Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol, 71(1), 53–61. 10.1037//0022-006x.71.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron KJ, & Goldberg SK (2020). Adult LGBT Population in the United States. The Williams Institute, UCLA. https://williamsinstitute.law.ucla.edu [Google Scholar]
- Corliss HL, Grella CE, Mays VM, & Cochran SD (2006). Drug use, drug severity, and help-seeking behaviors of lesbian and bisexual women. J Womens Health (Larchmt), 15(5), 556–568. 10.1089/jwh.2006.15.556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M TJ, White M, Unsicker J, Hodgkins D. (2002). Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures. Chestnut Health Systems. Retrieved June 5, 2020 from https://chestnut.app.box.com/v/GAIN-I-Materials/file/63671257181
- Duncan DT, Zweig S, Hambrick HR, & Palamar JJ (2019). Sexual Orientation Disparities in Prescription Opioid Misuse Among U.S. Adults. Am J Prev Med, 56(1), 17–26. 10.1016/j.amepre.2018.07.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bergman BG, & Kelly JF (2019). Whether, when, and to whom?: An investigation of comfort with disclosing alcohol and other drug histories in a nationally representative sample of recovering persons. J Subst Abuse Treat, 101, 29–37. 10.1016/j.jsat.2019.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, & Moskowitz JT (2000). Positive affect and the other side of coping. Am Psychol, 55(6), 647–654. 10.1037//0003-066x.55.6.647 [DOI] [PubMed] [Google Scholar]
- GfK. (2013). KnowledgePanel Design Summary. GfK. http://www.knowledgenetworks.com/knpanel/docs/knowledgepanel(R)-design-summary-description.pdf [Google Scholar]
- Gilbert PA, & Zemore SE (2016). Discrimination and drinking: A systematic review of the evidence. Soc Sci Med, 161, 178–194. 10.1016/j.socscimed.2016.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb G. (2007, Jan). Probabilistic epigenesis. Dev Sci, 10(1), 1–11. 10.1111/j.1467-7687.2007.00556.x [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, & Hasin DS (2015). Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Cochran SD, Greenwell L, & Mays VM (2011). Effects of sexual orientation and gender on perceived need for treatment by persons with and without mental disorders. Psychiatr Serv, 62(4), 404–410. 10.1176/ps.62.4.pss6204_0404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Greenwell L, Mays VM, & Cochran SD (2009). Influence of gender, sexual orientation, and need on treatment utilization for substance use and mental disorders: findings from the California Quality of Life Survey. BMC Psychiatry, 9, 52. 10.1186/1471-244x-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groshkova T, Best D, & White W. (2013). The Assessment of Recovery Capital: Properties and psychometrics of a measure of addiction recovery strengths. Drug and Alcohol Review, 32(2), 187–194. 10.1111/j.1465-3362.2012.00489.x [DOI] [PubMed] [Google Scholar]
- Han BH, Miyoshi M, & Palamar JJ (2020). Substance Use Among Middle-Aged and Older Lesbian, Gay, and Bisexual Adults in the United States, 2015 to 2017. Journal of General Internal Medicine. 10.1007/s11606-020-05635-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hequembourg AL, & Dearing RL (2013). Exploring shame, guilt, and risky substance use among sexual minority men and women. J Homosex, 60(4), 615–638. 10.1080/00918369.2013.760365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T. (2011). Alcohol use and alcohol-related problems among sexual minority women. Alcoholism Treatment Quarterly, 29(4), 403–435. 10.1080/07347324.2011.608336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T, McCabe SE, Wilsnack SC, West BT, & Boyd CJ (2010). Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction, 105(12), 2130–2140. 10.1111/j.13600443.2010.03088.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Johnson TP, Steffen AD, Wilsnack SC, & Everett B. (2014). Lifetime Victimization, Hazardous Drinking, and Depression Among Heterosexual and Sexual Minority Women. LGBT Health, 1(3), 192–203. 10.1089/lgbt.2014.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong YM, Veldhuis CB, Aranda F, & Hughes TL (2016). Racial/ethnic differences in unmet needs for mental health and substance use treatment in a community-based sample of sexual minority women. J Clin Nurs, 25(23–24), 3557–3569. 10.1111/jocn.13477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Jun HJ, Reisner SL, & Corliss HL (2017). Concurrent polysubstance use in a longitudinal study of US youth: associations with sexual orientation. Addiction, 112(4), 614–624. 10.1111/add.13681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Wong CF, Schrager SM, Silva K, Bloom JJ, Iverson E, & Lankenau SE (2012,). Initiation into prescription drug misuse: differences between lesbian, gay, bisexual, transgender (LGBT) and heterosexual high-risk young adults in Los Angeles and New York. Addict Behav, 37(11), 1289–1293. 10.1016/j.addbeh.2012.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, & White WL (2017). Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug Alcohol Depend, 181, 162–169. 10.1016/j.drugalcdep.2017.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, & Bergman BG (2018). Beyond Abstinence: Changes in Indices of Quality of Life with Time in Recovery in a Nationally Representative Sample of U.S. Adults. Alcohol Clin Exp Res, 42(4), 770–780. 10.1111/acer.13604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerridge BT, Pickering RP, Saha TD, Ruan WJ, Chou SP, Zhang H, Jung J, & Hasin DS (2017). Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug Alcohol Depend, 170, 82–92. 10.1016/j.drugalcdep.2016.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE, & Zaslavsky AM (2003). Screening for Serious Mental Illness in the General Population. Archives of General Psychiatry, 60(2), 184–189. 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Lazarus RS (2000). Toward better research on stress and coping. Am Psychol, 55(6), 665–673. 10.1037//0003-066x.55.6.665 [DOI] [PubMed] [Google Scholar]
- Lee JH, Gamarel KE, Bryant KJ, Zaller ND, & Operario D. (2016). Discrimination, Mental Health, and Substance Use Disorders Among Sexual Minority Populations. LGBT Health, 3(4), 258–265. 10.1089/lgbt.2015.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Gamarel KE, Kahler CW, Marshall BD, van den Berg JJ, Bryant K, Zaller ND, & Operario D. (2015). Co-occurring psychiatric and drug use disorders among sexual minority men with lifetime alcohol use disorders. Drug Alcohol Depend, 151, 167–172. 10.1016/j.drugalcdep.2015.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. J Consult Clin Psychol, 79(2), 159–170. 10.1037/a0022839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallory C, Sears B. (2015). Evidence of Employment Discrimination Based on Sexual Orientation and Gender Identity: An Analysis of Complaints Filed with State Enforcement Agencies, 2008–2014. Willams Institute. [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, & Boyd CJ (2010). The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American journal of public health, 100(10), 1946–1952. 10.2105/AJPH.2009.163147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction, 104(8), 1333–1345. 10.1111/j.1360-0443.2009.02596.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, West BT, Veliz P, & Boyd CJ (2019). DSM-5 Alcohol Use Disorder Severity as a Function of Sexual Orientation Discrimination: A National Study. Alcohol Clin Exp Res, 43(3), 497–508. 10.1111/acer.13960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Hughes TL, & Boyd CJ (2013). Sexual orientation and substance abuse treatment utilization in the United States: results from a national survey. J Subst Abuse Treat, 44(1), 4–12. 10.1016/j.jsat.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EH, & Bradford JB (2014). Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs, 75(1), 179–188. 10.15288/jsad.2014.75.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle AA, de Guzman R, Hemberg J, Yette E, Drabble L, & Trocki K. (2018). Delivering LGBT-sensitive substance use treatment to sexual minority women. J Gay Lesbian Soc Serv, 30(4), 393–408. 10.1080/10538720.2018.1512435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers RJ, & Smith JE (1995). Clinical guide to alcohol treatment: The Community Reinforcement Approach. Guilford Press. [Google Scholar]
- Miller W, & Delboca F. (1994). MEASUREMENT OF DRINKING BEHAVIOR USING THE FORM-90 FAMILY OF INSTRUMENTS. Journal of Studies on Alcohol(s12), 112–118. [DOI] [PubMed] [Google Scholar]
- NIDA. (2020). Trends & Statistics. Retrieved May 27, 2020 from https://www.drugabuse.gov/related-topics/trends-statistics#supplemental-references-for-economic-costs
- Peralta RL, Victory E, & Thompson CL (2019). Alcohol use disorder in sexual minority adults: Age- and sex- specific prevalence estimates from a national survey, 2015–2017. Drug Alcohol Depend, 205, 107673. 10.1016/j.drugalcdep.2019.107673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins RW, Hendin HM, & Trzesniewski KH (2001). Measuring Global Self-Esteem: Construct Validation of a Single-Item Measure and the Rosenberg Self-Esteem Scale. Personality and Social Psychology Bulletin, 27(2), 151–161. 10.1177/0146167201272002 [DOI] [Google Scholar]
- Romo LK, Dinsmore DR, & Watterson TC (2016). “Coming out” as an alcoholic: how former problem drinkers negotiate disclosure of their nondrinking identity. Health Communication, 31(3), 336–345. 10.1080/10410236.2014.954090 [DOI] [PubMed] [Google Scholar]
- Rosario M, Reisner SL, Corliss HL, Wypij D, Calzo J, & Austin SB (2014). Sexual-orientation disparities in substance use in emerging adults: a function of stress and attachment paradigms. Psychol Addict Behav, 28(3), 790–804. 10.1037/a0035499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. (2019). Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, SAMHSA. https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR1PDFW090120.pdf [Google Scholar]
- Schmidt S, Mhlan H, & Power M. (2006). The EUROHIS-QOL 8-item index: psychometric results of a cross-cultural field study. The European Journal of Public Health, 16(4), 420–428. 10.1093/eurpub/cki155 [DOI] [PubMed] [Google Scholar]
- Schuler MS, Rice CE, Evans-Polce RJ, & Collins RL (2018). Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug Alcohol Depend, 189, 139–146. 10.1016/j.drugalcdep.2018.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater ME, Godette D, Huang B, Ruan WJ, & Kerridge BT (2017). Sexual Orientation-Based Discrimination, Excessive Alcohol Use, and Substance Use Disorders Among Sexual Minority Adults. LGBT Health, 4(5), 337–344. 10.1089/lgbt.2016.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2015). Current Population Survey (CPS) https://www.census.gov/programs-surveys/cps/about.html [Google Scholar]
- U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (2018). National Survey on Drug Use and Health 2016 (NSDUH-2016-DS0001). Retrieved from https://datafiles.samhsa.gov/
- Valentino T. (2020). Cigarette Use Linked with Substance Use Among Sexual, Gender Minority Populations. Addiction Professional. https://www.psychcongress.com/article/cigaretteuse-linked-substance-use-among-sexual-gender-minority-populations?utm_campaign=NCAD%20Enews&utm_medium=email&_hsmi=95059391&_hsenc=p2ANqtz-9o4knbIyRX2Qq3KbcbFXhc9L7iRr9FAoZ7oKYWsqD7D15Ui9cQqpwZEoERX_UzmOrcJmKT1EFXn082jasPO4Q78RXLw&utm_content=95059391&utm_source=hs_email [Google Scholar]
- Vilsaint CL, Hoffman LA, & Kelly JF (2020). Perceived discrimination in addiction recovery: Assessing the prevalence, nature, and correlates using a novel measure in a U.S. National sample. Drug Alcohol Depend, 206, 107667. 10.1016/j.drugalcdep.2019.107667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, & White W. (2017). Development and validation of a Brief Assessment of Recovery Capital (BARC-10) for alcohol and drug use disorder. Drug and Alcohol Dependence, 177, 71–76. 10.1016/j.drugalcdep.2017.03.022 [DOI] [PubMed] [Google Scholar]
- Vu M, Li J, Haardorfer R, Windle M, & Berg CJ (2019). Mental health and substance use among women and men at the intersections of identities and experiences of discrimination: insights from the intersectionality framework. BMC Public Health, 19(1), 108. 10.1186/s12889-019-6430-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams ND, Fish JN. The availability of LGBT-specific mental health and substance abuse treatment in the United States. Health Serv Res. 2020;55(6):932–943. doi: 10.1111/1475-6773.13559. Epub 2020 Sep 24. PMID: 32970327; PMCID: PMC7704474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2018). United States of America: Alcohol. Retrieved May 27, 2020 from https://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/usa.pdf?ua=1