Abstract
Background:
OHIP’s original seven-domain structure does not fit empirical data, but a psychometrically sound and clinically more plausible structure with the four OHRQoL dimensions Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact has emerged. Consequently, use and scoring of available OHIP versions needs to be revisited.
Aim:
We assessed how well the overall construct OHRQoL and its four dimensions were measured with several OHIP versions (20, 19, 14, and 5 items) to derive recommendations which instruments should be used and how to score them.
Methods:
Data came from the “Dimensions of OHRQoL Project” and used the project’s learning sample (5,173 prosthodontic patients and general population subjects with 49-item OHIPs data). We computed correlations among OHIP versions’ summary scores. Correlations between OHRQoL dimensions, on one hand, and OHIP versions’ domain scores or OHIP-5’s items, on the other hand, were also computed. OHIP use and scoring recommendation were derived for psychometric solid but also practical OHRQoL assessment.
Results:
Summary scores of 5-, 14-, 19- and 49-item versions correlated highly (r= 0.91–0.98), suggesting similar OHRQoL construct measurement across versions. The OHRQoL dimensions Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact were best measured by the OHIP domain scores for Physical Disability, Physical Pain, Psychological Discomfort, and Handicap, respectively.
Conclusion:
Recommendations were derived which OHIP should be preferably used and how OHIP versions should be scored to capture the overall construct and the dimensions of OHRQoL. Psychometrically solid and practical OHRQoL assessment in all settings across all oral health conditions can be achieved with the 5-item OHIP.
1. Background
Dental patient-reported outcomes (dPROs) capture what matters to dental patients and are, therefore, needed to determine which treatments are most effective from patients’ perspectives.1 Scores of dPRO measures (dPROMs) quantifying this impact in numbers, are therefore necessary for evidence-based dentistry,2,3 and value-based oral health care,4 and effective dentist-patient communication.5
One of the most widely used multi-item dPROM is the Oral Health Impact Profile (OHIP).6 This dPROM aims to measure the multidimensional attribute oral health-related quality of life (OHRQoL.) Within the larger OHRQoL attribute, several smaller attributes, so called dimensions, exist. A fundamental measurement principle exists for instruments measuring multidimensional attributes: The number and nature of instrument scores needs to reflect the number and nature of the attributes the instrument intends to measure. This aspect of validity is called structural validity and is a prerequisite for score reliability as well as for other types of validity.
The OHIP was developed based on WHO’s International Classification of Impairments, Disabilities, and Handicaps from 1980. Experts assigned 49 items to seven attributes, so called domains, based on Locker’s model of oral health.7 However, several studies have demonstrated that this seven-domain structure does not fit empirical data.8–13 Instead, the set of four dimensions Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact was identified through exploratory factor analysis14 and subsequently replicated through confirmatory factor analysis,15 validation analyses,16 and correlation analyses17 as a psychometrically sound and clinically more plausible structure for OHIP in particular and OHRQoL in general. Furthermore, systematic reviews provided evidence that the four dimensions were the underlying attributes for dPROMs in general, regardless of whether they are oral disease-generic18 or oral disease-specific.19 Finally, it could be demonstrated in a study involving 15,800 patients from 32 countries of all World Health Organization regions that the dimensions Oral Function, Orofacial Pain, Orofacial Appearance and Psychosocial Impact are the major reasons why dental patients seek care.20 If indeed the structure of OHRQoL is composed of four dimensions, as these studies using different methodological approaches consistently demonstrated, this structure needs to be reflected in the scoring of the OHIP to satisfy basic measurement principles. Four dimension scores, reflecting this structure, would allow to characterize the impact of oral disease with a standardized metric21–25 and could also serve as the criteria to determine the efficacy, effectiveness, and efficiency of dental interventions.
In light of these new findings about attributes measured by OHIP, there is a need to revisit the use and scoring of different OHIP versions.
Aim
We assessed how well the overall construct OHRQoL and its four dimensions were measured with several OHIP versions (20, 19, 14, and 5 items) in order to derive recommendations regarding which instruments to use and how to score them.
2. Methods
2.1. Study design and data
Data came from the Dimensions of OHRQoL (DOQ) Project26 using the project’s learning sample (5,173 prosthodontic patients and general population subjects with OHIP-496 data.)
2.2. OHIP versions
The most widely used OHIP versions have 496, 20,27 19,28 14,29 and 5 items.30,31 All versions provide a summary score and all versions, apart from the 5-item OHIP, also provide seven domain scores.
The original OHIP is a 49-item instrument.6 Items are grouped into seven domains (Table 1): Functional Limitation (9 items), Physical Pain (9 items), Psychological Discomfort (5 items), Physical Disability (9 items), Psychological Disability (6 items), Social Disability (5 items), and Handicap (6 items). For each of the 49 OHIP questions, subjects rate on an ordinal scale (0 “never,” 1 “hardly ever,” 2 “occasionally,” 3 “fairly often,” 4 “very often”) how frequently they have experienced a specific oral health impact.
An OHIP version specifically adapted for edentulous subjects (OHIP-Edent, Table 1) has 19 items: Functional Limitation (3 items), Physical Pain (4 items), Psychological Discomfort (2 items), Physical Disability (3 items), Psychological Disability (2 items), Social Disability (3 items), and Handicap (2 items). 28
A 20-item version is very similar to the 19-item version but the Functional Limitation domain contains 4 instead of 3 items (Table 1). 27
The most widely used OHIP version has 14 items (Table 1), with 2 items for each of the seven domains. 29
The shortest OHIP version has 5 items (Table 1). 30,31 Contrary to the 49-, 20-, 19-, and 14-item OHIP versions, OHIP-5 does not categorize items into a set of seven domains. OHIP-5 was designed to capture 90% of the information contained in the OHIP-49 summary score with a minimum number of items.31 Because OHRQoL information in OHIP is contained in the dimensions Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact,32 OHIP-5 contains one item for each of these four dimensions together with a second item for Oral Function. The items “chewing difficulty” or “felt less flavor in food,” “painful aching,” “uncomfortable about appearance,” and “difficulty doing usual jobs” are, from a conceptual point of view, single-item measures for the dimensions of Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact, respectively. In addition, the instrument has an overall summary score.
Table 1.
How 49-, 20-, 19-, 14- and 5-item OHIPs actually measure the overall construct OHRQoL [represented by ] and its dimensions Oral Function [represented by
] and its dimensions Oral Function [represented by ], Orofacial Pain [
], Orofacial Pain [ ], Orofacial Appearance [
], Orofacial Appearance [ ], and Psychosocial Impact [■] in comparison to how factor-analytic studies determined the dimensional structure of OHIP
], and Psychosocial Impact [■] in comparison to how factor-analytic studies determined the dimensional structure of OHIP
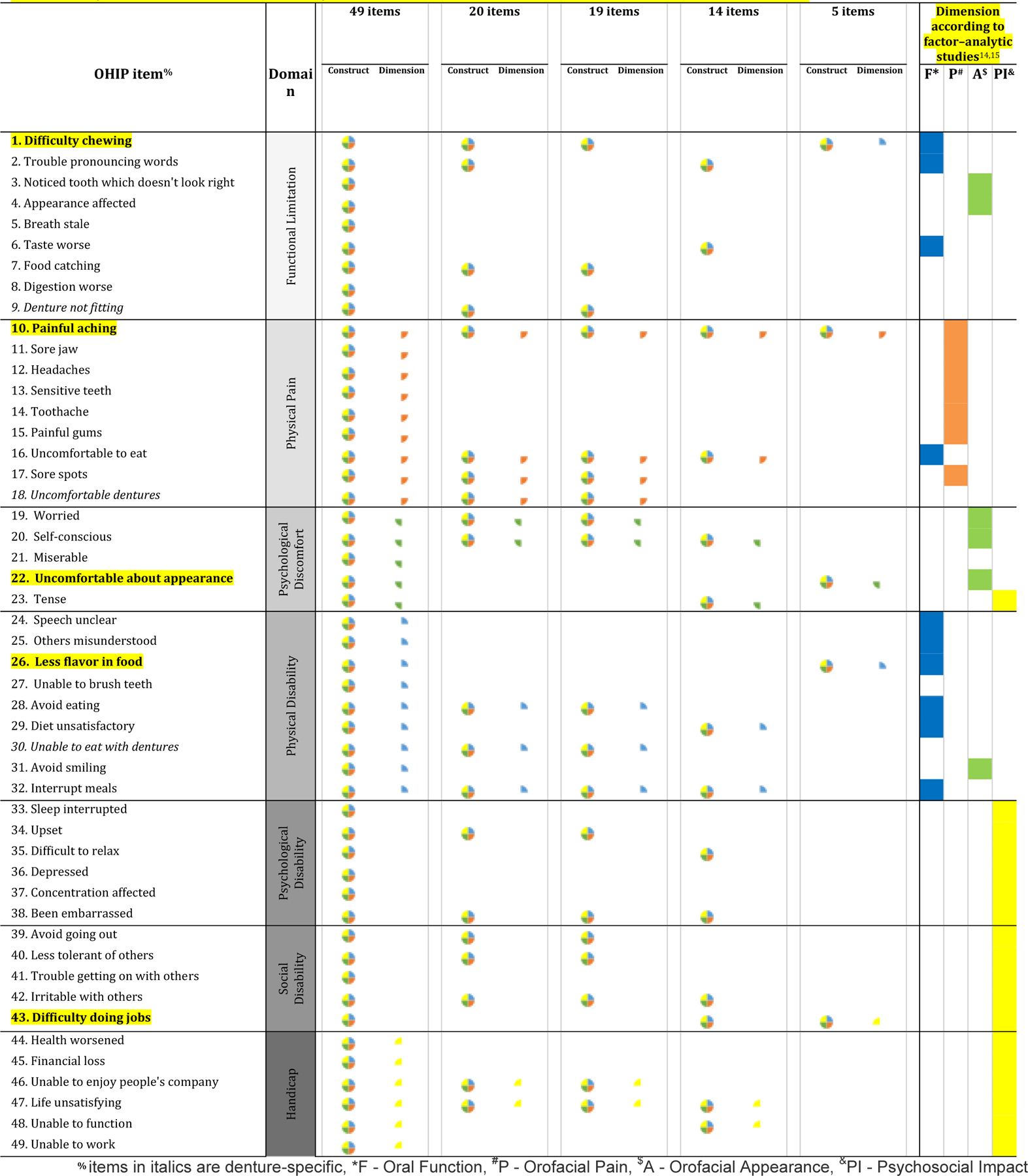
|
2.3. OHIP’s dimensional structure
OHIP’s structure was determined in a four-step process:
Using the DOQ Project’s26 Learning Sample, an exploratory factor analysis found a four-factor solution in 5,173 subjects and the factors were named Oral Function, Orofacial Pain, Orofacial Appearance and Psychosocial Impact.14
Using the DOQ Project’s26 Validation Sample, a confirmatory factor analysis in an independent sample of 5,022 subjects corroborated the four-factor model.15
Four OHRQOL dimensions can occur in 16 combinations, that is, sets of dimensions, and all these combinations are expected to occur based on clinical expertise. Indeed, in DOQ Project participants 26, all expected 16 combinations of OHRQoL dimensions were observed and agreed with expectations.16
OHIP-derived dimensions should generalize to other OHRQoL instruments. All questions from two widely used OHRQoL instruments, the Oral Impact on Daily Performance, OIDP33 and the Geriatric Oral Health Assessment index, GOHAI34) as well as culturally specific OHIP items should fit clinicians’ predictions about the items’ dimensional OHRQoL impact. In 267 international prosthodontic patients, OHRQoL items fit the predictions of clinicians where OHRQoL impact can be expected, providing evidence for the generalisability of OHIP-derived dimensions to other OHRQoL instruments.17
Which OHIP items belong to each of the four OHRQoL dimensions is presented in the last four columns of Table 1.
2.4. Data analyses
We aimed to determine how well (i) the overall OHRQoL construct and (ii) the OHRQoL dimensions are measured by OHIP versions with 20, 19, 14, and 5 items.
Measurement of the OHRQoL construct: All 49 OHIP items were summed and the resulting summary score formed a measure of the construct (Table 1, column “49 items” and “construct”).
Measurement of OHRQoL dimensions: Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact were represented by the 10, 7, 6, and 18 OHIP items, respectively, that formed these dimensions in factor analyses (Table 1, last four columns).14,15 All items per dimension were summed and the resulting score formed a measure of that dimension.
Two sets of correlations were computed:
1. Correlations among summary scores of OHIP versions
To study how well the 19-, 14-, and 5-item OHIP summary scores capture the overall OHRQoL construct (measured by the OHIP-49 summary score), Pearson correlation coefficients among these three versions, on the one hand, and the OHIP-49 summary score, on the other, were computed. In the correlation analysis, the OHIP-20 version was excluded because of its similarity with OHIP-19.
2. Correlations between OHIP domain scores as well as OHIP-5’s items, on the one hand, and OHRQOL dimensions on the other
To study how well the 19- and 14-item OHIP domain scores or the 5-item OHIP’ individual items capture the four OHRQoL dimensions, all domain score correlations and all OHIP-5 item correlations (all Pearson correlation coefficients) with the four OHRQoL dimensions scores were computed.
To characterize the precision of correlations, typically 95% confidence intervals are presented. In 5,173 subjects, a 0.50 correlation has a 95% confidence interval width of 0.04 and the same number is 0.02 for a correlation of 0.90. We omitted 95% confidence intervals because of ample precision for all correlations.
2.5. Deriving OHIP use and scoring recommendations
Based on the findings reported in the result section but also taking into account the burden to collect OHRQoL information, we derived recommendations which instrument should be used and how it should be scored. Recommendations are based on the principle that OHRQoL assessment should be possible in all research and dental practice setting and therefore needs to impose minimal burden.
3. Results
3.1. Correlations between OHIP version summary scores
The 5-, 14-, 19- and 49-item versions correlated highly. Summary scores between the six pairs of versions correlated from r=0.91 to 0.98 (Table 2), indicating that all versions measured OHRQoL equally well, i.e., they were practically interchangeable.
Table 2.
Correlations between OHIP summary scores with different number of items for 5,173 prosthodontic patients and general population subjects
| Correlation matrix | OHIP version | |||
|---|---|---|---|---|
| 49 | 19 | 14 | ||
| OHIP version | 19 | 0.98 | - | - |
| 14 | 0.97 | 0.96 | - | |
| 5 | 0.93 | 0.92 | 0.91 | |
3.2. Correlations between OHIP domain and OHRQoL dimension scores
Across OHIP-49, 19, and 14 (Table 3) a consistent pattern was observed for the different domains:
Table 3.
Correlations between OHIP-49 domain scores and OHRQoL dimensions scores (highest correlation per OHRQoL dimensions in bold and consistent domain-dimension pattern shaded)
| OHIP version with domains$ | OHRQoL dimension# | |||
|---|---|---|---|---|
| Oral Function | Orofacial Pain | Orofacial Appearance | Psychosocial Impact | |
| OHIP-49 | ||||
| Functional Limitation [9 items] | 0.87 | 0.67 | 0.83 | 0.83 |
| Physical Pain [9 items] | 0.73 | 0.98 | 0.68 | 0.71 |
| Psychological Discomfort [5 items] | 0.74 | 0.66 | 0.92 | 0.79 |
| Physical Disability [9 items] | 0.96 | 0.62 | 0.75 | 0.82 |
| Psychological Disability [6 items] | 0.74 | 0.61 | 0.71 | 0.85 |
| Social Disability [5 items] | 0.66 | 0.50 | 0.56 | 0.84 |
| Handicap [6 items] | 0.71 | 0.54 | 0.62 | 0.93 |
| OHIP-19 | ||||
| Functional Limitation [3 items] | 0.78 | 0.60 | 0.65 | 0.70 |
| Physical Pain [4 items] | 0.81 | 0.84 | 0.68 | 0.77 |
| Psychological Discomfort [2 items] | 0.66 | 0.61 | 0.90 | 0.68 |
| Physical Disability [3 items] | 0.88 | 0.56 | 0.64 | 0.69 |
| Psychological Disability [2 items] | 0.70 | 0.56 | 0.73 | 0.75 |
| Social Disability [3 items] | 0.63 | 0.48 | 0.55 | 0.79 |
| Handicap [2 items] | 0.67 | 0.48 | 0.62 | 0.84 |
| OHIP-14 | ||||
| Functional Limitation [2 items] | 0.85 | 0.48 | 0.58 | 0.68 |
| Physical Pain [2 items] | 0.78 | 0.79 | 0.66 | 0.68 |
| Psychological Discomfort [2 items] | 0.70 | 0.61 | 0.81 | 0.74 |
| Physical Disability [2 items] | 0.85 | 0.56 | 0.61 | 0.72 |
| Psychological Disability [2 items] | 0.69 | 0.53 | 0.69 | 0.78 |
| Social Disability [2 items] | 0.61 | 0.49 | 0.51 | 0.81 |
| Handicap [2 items] | 0.64 | 0.47 | 0.55 | 0.84 |
Oral Function was best measured by OHIP Physical Disability scores
Orofacial Pain was best measured by OHIP Physical Pain scores
Orofacial Appearance was best measured by OHIP Psychological Discomfort scores
Psychosocial Impact was best measured by OHIP Handicap scores
OHIP-5’s individual items measured OHRQoL dimensions well (Table 4). They reached correlation magnitudes close to the OHIP-14’s two-item domains (Table 3). In fact, Orofacial Pain and Orofacial Appearance were measured better by OHIP-5 items than by OHIP-14 domains. The other two dimensions were better measured by OHIP-14 than by OHIP-5 items. OHIP-5 items achieved slightly better discrimination among OHRQoL dimensions. For the item “difficulty chewing any foods,” the correlation with Oral Function was 0.78 and the second highest correlation (with Psychosocial Impact) was 0.61, resulting in a difference of 0.17. The same difference for OHIP-14 domains was 0.13, indicating a slightly worse discrimination among the two dimensions. Similar findings were observed for the dimensions Orofacial Pain and Orofacial Appearance. Only for the dimension Psychosocial Impact, OHIP-14 domains achieved better discrimination than OHIP-5 items.
Table 4.
Correlations between OHIP-5 scores and OHRQoL dimensions scores (highest correlation per OHRQoL dimensions in bold and dimension assignment shaded)
| OHIP-5 item* | OHRQoL dimension# | |||
|---|---|---|---|---|
| Oral Function | Orofacial Pain | Orofacial Appearance | Psychosocial Impact | |
| Difficulty chewing any foods | 0.78 | 0.56 | 0.60 | 0.61 |
| Painful aching in your mouth | 0.56 | 0.81 | 0.53 | 0.55 |
| Felt uncomfortable about the appearance | 0.64 | 0.52 | 0.85 | 0.66 |
| Difficulty doing your usual jobs | 0.58 | 0.45 | 0.46 | 0.74 |
OHIP-5 item “felt less flavor in food” is also a measure of Oral Function but is omitted here
see Table 1 for the relationship between items to dimensions
4. Discussion
The main finding from the present study was that the 5-, 14-, 19- and 49-item versions correlated highly, indicating that these versions measured OHRQoL equally well. Given that these versions, including the longest (OHIP-49), the most widely used (OHIP-14), and even the version claiming to be specific to edentulous subjects (OHIP-19) were practically interchangeable, we propose that the short version (OHIP-5) can replace the longer versions. The availability of a psychometrically sound instrument with minimal burden will facilitate future use of OHIP in both research and clinical settings.
It is noteworthy that OHIP-19 is a disease-specific instrument for edentulous patients as compared to OHIP-14 and OHIP-49 which are oral disease-generic, i.e., applicable for all oral conditions. Disease-specific instruments have advantages in their target populations and should by definition be less suitable for other populations. However, in prosthodontic patients and general population subjects included in the present study, OHIP-19 behaved as an oral disease-generic instrument. The pattern of domain-dimensions correlations, i.e., which domains were highest for the four dimensions, was identical compared to OHIP-14 and OHIP-49. OHIP-19 domain correlations were slightly larger than those for OHIP-14 and lower than for OHIP-49, as expected from an instrument with this number of items. Thus, the OHIP-19 seems to be applicable in other populations than edentulous patients.
Literature results are available to compare the observed correlations among OHIP sum scores with previous studies. OHIP-5 and OHIP-49 correlated with r=0.94 and r=0.91 in German general population subjects and TMD patients, respecitively.31 In Dutch TMD patients all summary scores correlated above 0.90.35 In Japanese dental patients, OHIP-5 correlated 0.92 with OHIP-4936 and this number was also observed in the adult Swedish general population.37 In Spanish-speaking dental patients OHIP-5 correlated with the 14- as well as the 49-item version with r=0.95.38
Literature results for the correlation between OHIP domains scores and OHRQoL dimensions scores or between OHIP-5 items and OHRQoL dimensions scores are not available. However, a consistent pattern of linking the domain Physical Disability with the dimension Oral Function, Physical Pain with Orofacial Pain, Psychological Discomfort with Orofacial Appearance, and Handicap with Psychosocial Impact OHIP-5 provides support for the findings. OHIP-5 with its items used as indicators to assess the OHRQoL dimensions appeared an informative and low-burden alternative to the most widely applied OHIP version, the OHIP-14. An independent validation of this finding is desirable.
The database for these findings came from 35 individual studies containing a diverse set of international prosthodontic patients and general population subjects from six countries.26 Results should have a high potential for generalizability and are supported by excellent precision due to the large sample size.
The study has also limitations. If the four dimensions Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial are the necessary and sufficient components of the patient’s oral health experience, OHIPs with 4, 8, 12, 16 etc. items, representing each dimension with an increasing number of indicators would be the logical consequence. However, an OHIP with 5 items is already available in several languages (for example: Arabic39 Dutch,35 German,31 Hungarian,40 Japanese, 36 Spanish,38 Swedish37.) The OHIP with 5 items – all dimensions are characterized with one item except for Oral Function which is characterized by 2 items – allows four-dimensional assessment of OHRQoL and comes very close to a conceptually pure 4-item version. OHIP-5 is psychometrically sound and results for a four-item version will likely only marginally differ. Longer OHIPs with 8, 12, 16 etc. items are not appealing because of the burden related to the instrument application.
Because two systematic reviews provided evidence that currently available oral disease-generic18 or oral disease-specific19 multi-item dPROMs for adults essentially measure only the four OHRQoL dimensions, and this task could also be accomplished with OHIP-5, it is our firm opinion that enough OHRQoL instruments have already been developed. Instrument development requires substantial time and resources because of the need for psychometric evaluation in different settings, transformation into other languages, or development of frameworks for score interpretation (normative values, minimal important differences etc.) - just to name a few steps that follow after an instrument is created.
Instead of creating new OHIPs, including an OHIP-4, or other multi-item dPROMs to capture disease and treatment impact available resources should be used to implement OHIP-5 across all settings for all oral health conditions. The project “Mapping Oral Disease Impact with a Common Metric” (MOM).41, a project that aims to standardize perceived oral health assessment across all settings for oral diseases in both research and clinical practice, recommends OHIP-5 is the core metric to capture patient-perceived oral health.42
5. Recommendations
5.1. Best OHRQoL characterization
We recommend a four-dimensional characterization of OHRQoL using the dimensions Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact. The best measures for OHRQoL dimensions would be summary scores of the items identified in factor analyses of OHIP-49.14,15 Four scores, describing the dimensions, should be accompanied by a summary score derived from all 49 items, describing the total OHRQoL impact. The most comprehensive measure of the OHRQoL construct is the OHIP-49 summary score.
Table 1 presents which OHIP items are used to measure the overall OHRQoL construct and which items are used to measure OHRQoL dimensions when using the 49-item version.
5.2. Practical OHRQoL characterization
Because OHRQoL measurement needs to be practical and OHIP-49 application is burdensome, abbreviated versions are necessary to allow OHRQoL assessment in all research and dental practice settings.
We have recommendations both for studies collecting new studies using OHIP (Figure 1, Panel A) and for already available OHIP studies in the literature (Figure 1 Panel B.)
Figure 1.
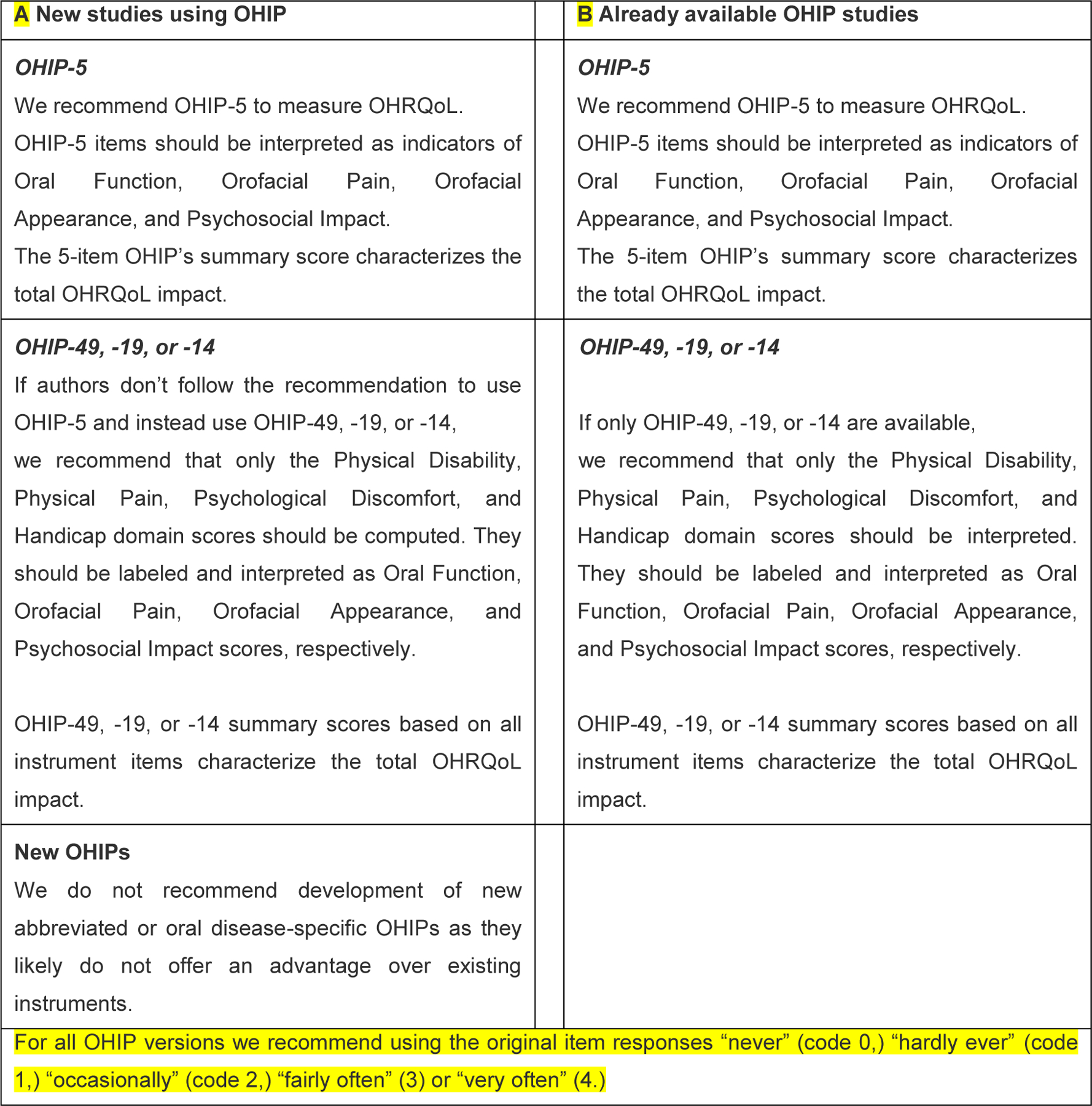
Practical Oral Health-Related Quality of Life chacterization using the 5-item, 14-item, 19-item, and the 49-item Oral Health Impact Profile
Table 1 presents which OHIP items are used to measure the overall OHRQoL construct and which items are used to measure OHRQoL dimensions when using abbreviated OHIP versions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CRediT author statement
John MT: Conceptualization, Methodology, Formal analysis, Writing - Original Draft, Writing - Review & Editing, Project administration, Funding acquisition
Omara M: Conceptualization, Methodology, Writing - Review & Editing
Su N: Conceptualization, Methodology, Writing - Review & Editing
List T: Conceptualization, Methodology, Writing - Review & Editing
Sekulic S: Conceptualization, Methodology, Writing - Review & Editing
Häggman-Henrikson B: Conceptualization, Methodology, Writing - Review & Editing
Visscher CM: Conceptualization, Methodology, Writing - Review & Editing
Bekes K: Conceptualization, Methodology, Writing - Review & Editing
Reissmann DR: Conceptualization, Methodology, Writing - Review & Editing
Baba K: Conceptualization, Methodology, Writing - Review & Editing
Schierz O: Conceptualization, Methodology, Writing - Review & Editing
Theis-Mahon N: Conceptualization, Methodology, Writing - Review & Editing
Fueki K: Conceptualization, Methodology, Writing - Review & Editing
Stamm T: Conceptualization, Methodology, Writing - Review & Editing
Bondemark L: Conceptualization, Methodology, Writing - Review & Editing
Oghli I: Conceptualization, Methodology, Writing - Review & Editing
van Wijk A: Conceptualization, Methodology, Writing - Review & Editing
Larsson P: Conceptualization, Methodology, Writing - Review & Editing
References
- 1.John MT. Health Outcomes Reported by Dental Patients. Journal of Evidence-Based Dental Practice. 2018;18(4):332–335. [DOI] [PubMed] [Google Scholar]
- 2.Reissmann DR. Dental Patient-Reported Outcome Measures Are Essential for Evidence-Based Prosthetic Dentistry. Journal of Evidence-Based Dental Practice. 2019;19(1):1–6. [DOI] [PubMed] [Google Scholar]
- 3.Hua F Increasing the Value of Orthodontic Research Through the Use of Dental Patient-Reported Outcomes. Journal of Evidence-Based Dental Practice. 2019;19(2):99–105. [DOI] [PubMed] [Google Scholar]
- 4.Listl S Value-Based Oral Health Care: Moving Forward With Dental Patient-Reported Outcomes. Journal of Evidence-Based Dental Practice. 2019;19(3):255–259. [DOI] [PubMed] [Google Scholar]
- 5.Palaiologou A, Kotsakis GA. Dentist-Patient Communication of Treatment Outcomes in Periodontal Practice: A Need for Dental Patient–Reported Outcomes. Journal of Evidence-Based Dental Practice. 2020;20(2). [DOI] [PubMed] [Google Scholar]
- 6.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11(1):3–11. [PubMed] [Google Scholar]
- 7.Locker D Measuring oral health: a conceptual framework. Community dental health. 1988;5(1):3–18. [PubMed] [Google Scholar]
- 8.Segu M, Collesano V, Lobbia S, et al. Cross-cultural validation of a short form of the Oral Health Impact Profile for temporomandibular disorders. Community Dent Oral Epidemiol. 2005;33(2):125–130. [DOI] [PubMed] [Google Scholar]
- 9.Mumcu G, Hayran O, Ozalp DO, et al. The assessment of oral health-related quality of life by factor analysis in patients with Behcet’s disease and recurrent aphthous stomatitis. Journal of oral pathology & medicine. 2007;36(3):147–152. [DOI] [PubMed] [Google Scholar]
- 10.Baker SR, Gibson B, Locker D. Is the oral health impact profile measuring up? Investigating the scale’s construct validity using structural equation modelling. Community dentistry and oral epidemiology. 2008;36(6):532–541. [DOI] [PubMed] [Google Scholar]
- 11.Souza RF, Leles CR, Guyatt GH, Pontes CB, Vecchia MP della, Neves FD. Exploratory factor analysis of the Brazilian OHIP for edentulous subjects. Journal of oral rehabilitation. 2010;37(3):202–208. [DOI] [PubMed] [Google Scholar]
- 12.Montero J, Bravo M, Vicente MP, Galindo MP, Lopez JF, Albaladejo A. Dimensional structure of the oral health-related quality of life in healthy Spanish workers. Health and quality of life outcomes. 2010;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baker SR. Testing a conceptual model of oral health: A structural equation modeling approach. Journal of Dental Research. 2007;86(8):708–712. [DOI] [PubMed] [Google Scholar]
- 14.John MT, Reissmann DR, Feuerstahler L, et al. Exploratory factor analysis of the oral health impact profile. Journal of Oral Rehabilitation. 2014;41(9):635–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John MT, Feuerstahler L, Waller N, et al. Confirmatory factor analysis of the oral health impact profile. Journal of Oral Rehabilitation. 2014;41(9):644–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.John MT, Rener-Sitar K, Baba K, et al. Patterns of impaired oral health-related quality of life dimensions. Journal of Oral Rehabilitation. 2016;43(7):519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.John MT, Reissmann DR, Čelebid A, et al. Integration of oral health-related quality of life instruments. Journal of Dentistry. 2016;53:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mittal H, John MT, Sekulid S, Theis-Mahon N, Rener-Sitar K. Patient-Reported Outcome Measures for Adult Dental Patients: A Systematic Review. Journal of Evidence-Based Dental Practice. 2019;19(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rener-Sitar K, John MT, Truong V, Tambe S, Theis-Mahon N. Nonmalignant Oral Disease–Specific Dental Patient-Reported Outcome Measures for Adult Patients: A Systematic Review. Journal of Evidence-Based Dental Practice. 2021;21(1). [DOI] [PubMed] [Google Scholar]
- 20.John MT, Sekulid S, Bekes K, et al. Why Patients Visit Dentists – A Study in all World Health Organization Regions. Journal of Evidence-Based Dental Practice. 2020;20(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Omara M, Stamm T, Bekes K. Four-dimensional oral health-related quality of life impact in children: A systematic review. Journal of Oral Rehabilitation. 2021;48(3):293–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Su N, van Wijk A, Visscher CM. Psychosocial oral health-related quality of life impact: A systematic review. Journal of Oral Rehabilitation. 2021;48(3):282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oghli I, List T, Su N, Häggman-Henrikson B. The impact of oro-facial pain conditions on oral health-related quality of life: A systematic review. Journal of Oral Rehabilitation. 2020;47(8):1052–1064. [DOI] [PubMed] [Google Scholar]
- 24.Larsson P, Bondemark L, Häggman-Henrikson B. The impact of oro-facial appearance on oral health-related quality of life: A systematic review. Journal of Oral Rehabilitation. 2021;48(3):271–281. [DOI] [PubMed] [Google Scholar]
- 25.Schierz O, Baba K, Fueki K. Functional oral health-related quality of life impact: A systematic review in populations with tooth loss. Journal of Oral Rehabilitation. 2021;48(3):256–270. [DOI] [PubMed] [Google Scholar]
- 26.John MT, Reißmann DR, Feuerstahler L, et al. Factor analyses of the Oral Health Impact Profile - Overview and studied population. Journal of Prosthodontic Research. 2014;58(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allen PF, O’Sullivan M, Locker D. Determining the minimally important difference for the Oral Health Impact Profile-20. European Journal of Oral Sciences. 2009;117(2):129–134. [DOI] [PubMed] [Google Scholar]
- 28.Allen F, Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. International Journal of Prosthodontics. 2002;15(5):446–450. [PubMed] [Google Scholar]
- 29.Slade GD. Derivation and validation of a short‐form oral health impact profile. Community Dent Oral Epidemiol. 1997;25(4):284–290. [DOI] [PubMed] [Google Scholar]
- 30.Naik A, John MT, Kohli N, Self K, Flynn P. Validation of the English-language version of 5-item Oral Health Impact Profile. Journal of prosthodontic research. 2016;60(2):85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.John MT, Miglioretti DL, LeResche L, Koepsell TD, Hujoel P, Micheelis W. German short forms of the oral health impact profile. Community dentistry and oral epidemiology. 2006;34(4):277–288. [DOI] [PubMed] [Google Scholar]
- 32.John MT, Hujoel P, Miglioretti DL, LeResche L, Koepsell TD, Micheelis W. Dimensions of oral-health-related quality of life. Journal of dental research. 2004;83(12):956–960. [DOI] [PubMed] [Google Scholar]
- 33.Adulyanon S, Sheiham A. A new socio-dental indicator of oral impacts on daily performances. J Dent Res. 1996;75(IADR Abstracts):231 (abstract). [Google Scholar]
- 34.Atchison KA, Dolan TA. Development of the Geriatric Oral Health Assessment Index. J Dent Educ. 1990;54(11):680–687. [PubMed] [Google Scholar]
- 35.van der Meulen MJ, John MT, Naeije M, Lobbezoo F. Developing abbreviated OHIP versions for use with TMD patients. Journal of Oral Rehabilitation. 2012;39(1):18–27. [DOI] [PubMed] [Google Scholar]
- 36.Baba K, Inukai M, John MT. Feasibility of oral health-related quality of life assessment in prosthodontic patients using abbreviated Oral Health Impact Profile questionnaires. Journal of Oral Rehabilitation. 2008;35(3):224–228. [DOI] [PubMed] [Google Scholar]
- 37.Larsson P, John MT, Hakeberg M, Nilner K, List T. General population norms of the Swedish short forms of oral health impact profile. Journal of oral rehabilitation. 2014;41(4):275–281. [DOI] [PubMed] [Google Scholar]
- 38.Simancas-Pallares M, John MT, Enstad C, Lenton P. The Spanish Language 5-Item Oral Health Impact Profile. International Dental Journal. 2020;70(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alhajj MN, Halboub E, Khalifa N, et al. Translation and validation of the Arabic version of the 5-item Oral health impact profile: OHIP5-Ar. Health and Quality of Life Outcomes. 2018;16(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Szabó G, John MT, Szántó I, Marada G, Kende D, Szentpétery A. Impaired oral health-related quality of life in Hungary. Acta Odontologica Scandinavica. 2011;69(2). [DOI] [PubMed] [Google Scholar]
- 41.Sekulic S, John MT, Häggman-Henrikson B, Theis-Mahon N. Dental patients’ functional, pain-related, aesthetic, and psychosocial impact of oral conditions on quality of life—Project overview, data collection, quality assessment, and publication bias. Journal of Oral Rehabilitation. 2021;48(3):246–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.John MT, Häggman-Henrikson B, Sekulic S, et al. Mapping Oral Disease Impact with a Common Metric (MOM)—Project summary and recommendations. Journal of Oral Rehabilitation. 2021;48(3):305–307. [DOI] [PubMed] [Google Scholar]


