Abstract
BACKGROUND
While injuries experienced during hurricanes and other tropical cyclones have been relatively well- characterized through traditional surveillance, less is known about tropical cyclones’ impacts on non-injury morbidity, which can be triggered through pathways that include psychosocial stress or interruption in medical treatment.
METHODS
We investigated daily emergency Medicare hospitalizations (1999–2010) in 180 United States counties, drawing on an existing cohort of high-population counties. We classified counties as exposed to tropical cyclones when storm-associated peak sustained winds were ≥ 21 m/s at the county center; secondary analyses considered other wind thresholds and hazards. We matched storm-exposed days to unexposed days by county and seasonality. We estimated change in tropical cyclone-associated hospitalizations over a storm period from 2 days before to 7 days after the storm’s closest approach, compared to unexposed days, using generalized linear mixed-effect models.
RESULTS
For 1999–2010, 175 study counties had at least one tropical cyclone exposure. Cardiovascular hospitalizations decreased on the storm day, then increased following the storm, while respiratory hospitalizations were elevated throughout the storm period. Over the 10-day storm period, cardiovascular hospitalizations increased 3% (95% confidence interval [CI]: 2%, 5%) and respiratory hospitalizations increased 16% (95% CI: 13%, 20%) compared to matched unexposed periods. Relative risks varied across tropical cyclone exposures, with strongest association for the most restrictive wind-based exposure metric.
CONCLUSIONS
In this study, tropical cyclone exposures were associated with a short-term increase in cardiorespiratory hospitalization risk among the elderly, based on a multi-year/multi-site investigation of US Medicare beneficiaries ≥ 65 years.
Keywords: Cyclone, Hurricane, Tropical Storm, Natural disasters, Medicare, Hospitalization
INTRODUCTION
Tropical cyclones pose an important threat to human health in the United States (US), and with climate change, their average intensities, rainfall rates, and storm surge inundation levels are projected to increase.1,2 While fatality and injury tolls from major US tropical cyclones are typically estimated via post-disaster surveillance,3,4 much less is known about non-injury morbidity risks, particularly compared to other climate-related disasters like heat waves.5 Tropical cyclones can, however, trigger or exacerbate illness through psychosocial stress, interruption in medical treatment, and post-storm exposures such as heat and mold.4,6,7
Some studies have examined the effects of individual tropical cyclones on hospitalizations and other emergency medical visits for cardiorespiratory disease,6 especially for Hurricanes Katrina8–10 and Sandy.11–13 However, it is unclear if the adverse risks observed for these storms persist across other tropical cyclones and locations. Single-event case studies form an important component of disaster research, as such studies engage with complexity in the event and resonate across disciplines and among non-scientists.14 However, disaster case studies have limitations, including in terms of external validity.14 Further, it can be difficult to aggregate or compare evidence across single-storm studies because of differences in study methodology, and in meta-analyses publication bias often results in overestimation of associations.15–17 Multi-year/multi-site studies can supplement case studies by providing: (1) a more precise and less biased estimate of the typical association between exposure and health risk;16–18 (2) evidence of consistency in health associations across multiple exposures;19 and (3) a clearer picture of heterogeneity—as well as factors that contribute to this heterogeneity—across associations observed for different events and at different sites.16
The elderly are particularly vulnerable to health risks during extreme weather events,20 as many have functional limitations or other conditions that compromise their ability to stay safe during disasters.21 For 1963–2012, there were eight times as many hurricane-attributed indirect deaths among individuals ≥ 70 years compared to those who were younger.22 In the US, the percentage of the population aged ≥ 65 years is expected to increase in the coming decades,20 and one-fifth of Americans aged ≥ 65 years live in counties prone to tropical cyclone exposure.23 Despite a growing interest in how natural disasters affect human health24 and recognition that the elderly are disproportionately affected,25 few studies specifically examine health risk among the elderly associated with tropical cyclones, especially through multi-event analysis rather than case studies.26
To address these research gaps, we examined the associations between tropical cyclone exposures and emergency hospital admissions for cardiovascular and respiratory diseases among Medicare beneficiaries for 180 high-population counties in the eastern US for 1999–2010. To our knowledge, this is the largest-scale study to date, in terms of the number of tropical cyclone exposures investigated, to explore patterns in emergency hospitalizations among the elderly during tropical cyclones.
METHODS
Tropical cyclone exposure classification
As storm-induced wind has historically been identified as a key force in storm-related destruction,27 we used storm-related peak sustained winds as our primary metric in classifying county-level tropical cyclone exposure. We avoided using Federal Emergency Management Agency disaster declarations to determine exposure, as they are subject to political and economic factors,28,29 and previous epidemiological research has found exposure assessment directly based on storm hazards is preferable.30 We first identified, from Atlantic-basin storms recorded in the National Hurricane Center’s revised Atlantic hurricane database (HURDAT2),31 all storms that crossed or neared the eastern US in 1999–2010, identifying all that passed within 250 kilometers of at least one US county (top panel, Figure 1). For each storm in this subset, we then modeled ground-level peak sustained wind speed at each county’s population mean center using a double exponential wind speed model (middle panel, Figure 1).32,33 Based on these modeled wind speeds, we classified a study county as exposed if the storm brought peak sustained winds ≥ 21 m/s to the county center (bottom panel, Figure 1), which is the approximate threshold for strong gale-force winds on the Beaufort wind scale.34 This threshold represents local winds at which there can be damage to structures (especially roofs), power outages, and difficulty walking outside.35–37 As a secondary analysis, we considered other wind thresholds (12, 15, and 18 m/s) to explore the influence of the exposure threshold choice on hospitalization risk estimates.
Figure 1:
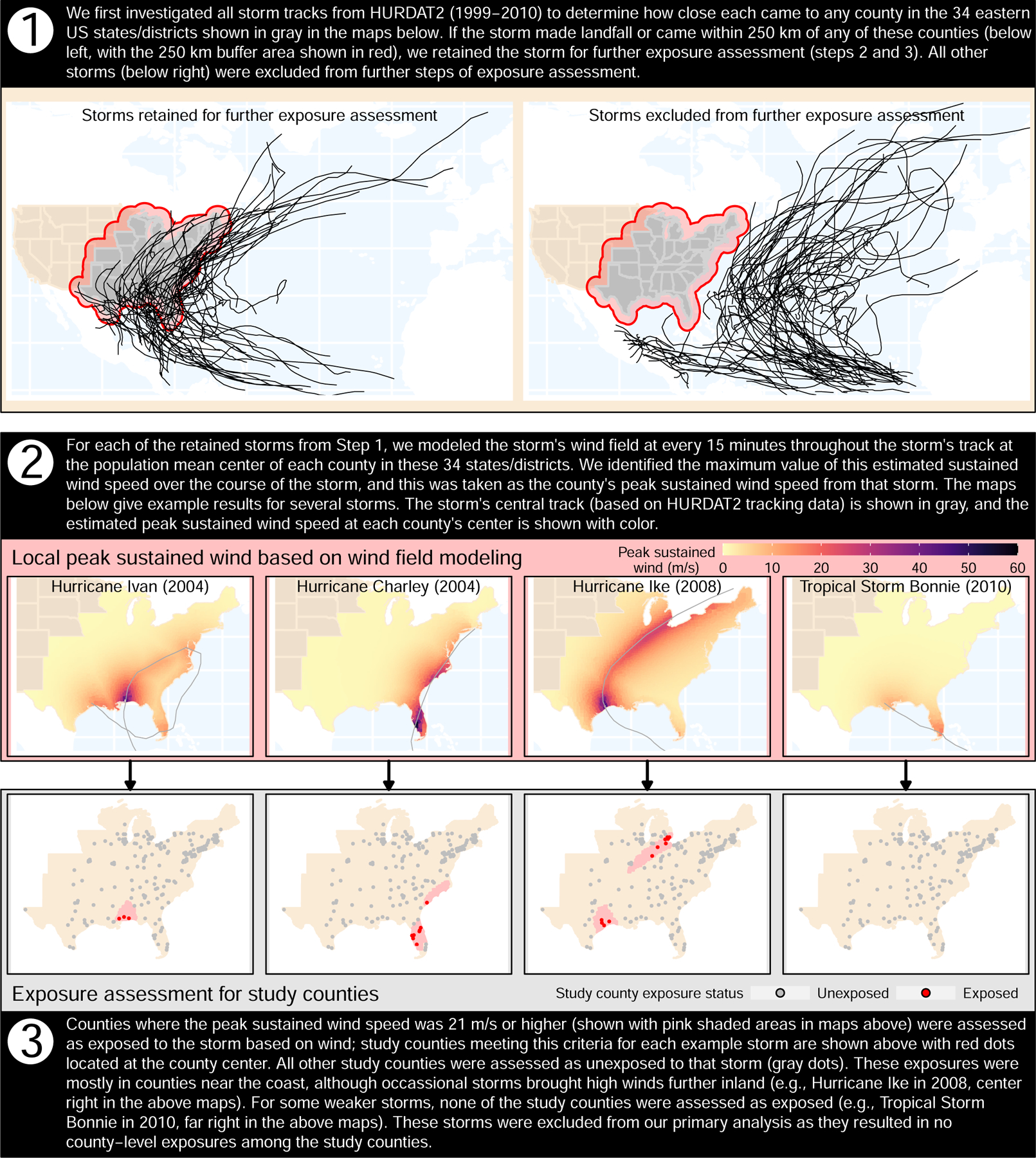
Illustration of the steps taken in exposure assessment for the primary analysis in this study. The 34 eastern US states/districts shown here are: Alabama, Arkansas, Connecticut, Delaware, the District of Columbia, Florida, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Mississippi, Missouri, New Hampshire, New Jersey, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, Vermont, Virginia, West Virginia, and Wisconsin. County population mean centers are based on the 2010 US Census. Storm tracks are based on the National Hurricane Center’s revised Atlantic hurricane database (HURDAT2).
As a further secondary analysis, we considered exposure assessments based on other hazards, since tropical cyclones can pose threats to human health without strong winds.38 We separately assessed county-level exposure based on rainfall, flooding, and tornadoes.39 We calculated cumulative rainfall for 1 day before to 1 day after the storm’s closest approach to the county (eFigure 1) using precipitation data from the North American Land Data Assimilation System, phase 2 (NLDAS-2).40,41 We obtained data for flood and tornado events from the National Oceanic and Atmospheric Administration (NOAA)’s Storm Events database.42,43 Finally, we also investigated distance of the county from the storm, used previously as an exposure metric for tropical cyclone studies.44 We considered four thresholds for rain- and distance-based metrics. Further details on this exposure assessment are provided in the eAppendix, with details on validation previously published.45
Study population
For 180 eastern US study counties (Figure 1 eFigure 2), we used aggregated daily county-wide counts of emergency Medicare hospital admissions for cardiovascular and respiratory disease, using fee-for-service Medicare claims made within 1 January 1999–31 December 2010 for beneficiaries ≥ 65 years residing in the county. All hospitalizations were recorded by county of residence. The original study population includes most high-population counties in the US, with data aggregated at the county level, and was used previously to examine health effects of other ambient environmental exposures, including air pollution46 and heat.47 Given our focus on Atlantic-basin tropical cyclones, here we investigate only the 180 counties in the cohort in 34 states/districts in the eastern half of the US (Figure 1, eFigure 2). In 2010, the study counties included over half the total population of these 34 eastern states (eTable 1). Compared to other counties in these states, the study counties tended to differ in race and ethnicity and had a slightly smaller percent of the population aged ≥ 65 years (eTable 2). Cause of disease was classified based on the International Classification of Diseases, Ninth Revision (ICD-9). Cardiovascular disease hospitalizations were based on the combined number of hospital admissions coded as 390–459, including hospitalizations for heart failure (ICD-9 428), cerebrovascular disease (430–438), heart rhythm disturbance (426–427), peripheral vascular disease (440–448), ischemic heart disease (410–414 and 429), and acute myocardial infarction (410). Respiratory disease hospitalizations were based on the combined number of hospitalizations with ICD-9 codes 464–466, 480–487, and 490–493, including hospitalizations for respiratory tract infection (464–466, 480–487), chronic obstructive pulmonary disease (COPD, ICD-9, 490–492), and asthma (493).
Statistical analysis
We aimed to estimate the overall county-wide change in the hospitalization rates during tropical cyclone exposure, compared to expected rates had the storm not occurred. While time series48 and case–crossover49 study designs can be considered to answer this research question, both could introduce bias if disasters pose extended impacts on county’s health with incorrect model specification of this extended period.50 We instead adapted a matched study design used previously for multi-event, multi-site studies of heat waves51 and wildfires,52 with disaster-exposed days matched to similar unexposed days within county.
Specifically, we compared emergency hospital admissions during tropical cyclone exposures to matched unexposed periods in other years in the same county and time of year, conducting a separate analysis for each storm exposure metric considered. We first identified any storm-exposed days under a given exposure metric. For each county-level storm exposure, we identified the date of exposure (“lag 0”) as the date the storm’s central track was closest to that county (eFigure 3). We matched each storm-exposed day to 10 unexposed days, randomly selected from candidate days that were: (1) in the same county; (2) in a different year; (3) within a 7-day window of the exposure’s day of year; (4) at least 8 days before or 3 days after any other storm day in the county, so that no days in the period from 2 days before to 7 days after the candidate day coincided with a different storm; and (5) outside 11–24 September 2001, to exclude potential impact from a severe man-made disaster. For each storm-exposed day and its 10 matched unexposed days, we pulled hospitalization data from 2 days before to seven days after the storm’s closest approach, including days prior to the storm to investigate for risks associated with pre-storm preparations and exposures.
Separately for each combination of exposure metric and disease outcome, we fit a generalized linear mixed-effect model to the matched multi-county data, including an unconstrained distributed lag function of storm exposure:53
| (1) |
where:
is the number of emergency hospital admissions for a certain cause in the study population on day t for county c;
is the expected number of hospitalizations among the study population on day t for county c;
is the total number of Medicare beneficiaries residing in county c on day t who were not already hospitalized, included as an offset;
α is the model intercept;
are random intercepts for each county;
is an unconstrained distributed lag function53 of storm exposure variable x. is the coefficient estimating the association between TC exposure and hospital admission at lag l from day t, the day of the storm’s closest approach to study county c. is the indicator variable representing whether a given day at lag l from day t for county c is part of an exposed storm period or part of a matched unexposed period.
is a vector of categorical variables for year on day t, and is a vector of associated coefficients;
is a vector of categorical variables for day of week on day t, and is a vector of associated coefficients.
Based on estimated coefficients, we calculated both lag-specific and storm-period (two days before to seven days after the storm’s closest approach to the county) relative risks (RRs) compared to matched unexposed days or periods. We calculated the lag-specific RRs on each day in the storm period as . The storm-period RRs, which estimate how the sum of hospitalizations across the 10-day storm period changed from total hospitalizations in matched unexposed periods, were calculated as .54 We used the delta method54 to calculate the standard errors for the storm-period RRs.
There were a few very severe tropical cyclone exposures within our study population. To investigate if the main, multi-storm results were driven by these exposures, we estimated single-storm associations for the ten most severe exposures (based on storm-associated winds within the county) using separate models, and also estimated the average associations between hospitalizations and all other tropical cyclone exposures (i.e., excluding the ten most severe tropical cyclone exposures), using a mixed-effects model as in eq. 1. To ensure adequate statistical power in these sensitivity analyses, we limited them to study counties with >50,000 Medicare beneficiaries.
We conducted sensitivity analyses to ensure primary results were robust to choices in the study design and statistical model. First, when selecting candidate unexposed days for matching, we considered more rigorous exclusion criteria, expanding to exclude any day within 2 weeks of another storm exposure in the county. Second, we investigated alternative statistical models, to look for potential issues from assumptions in the main statistical model. Specifically, we investigated for problematic overdispersion, limitations in the assumption that random county-level intercepts were normally distributed, and indications that long-term patterns in outcomes differed by county. Finally, to further examine potential unmeasured confounding from long-term temporal trends, we conducted a negative exposure control analysis, in which the storm periods were replaced by days 2 weeks before the storm. Further details on these sensitivity analyses are in the eAppendix.
RESULTS
For 1999–2010, 74 Atlantic-basin tropical cyclones made landfall or passed near the eastern US and so were considered further in our exposure assessment (Figure 1, top panel). Of the 180 counties considered, 175 had at least one storm exposure under at least one exposure metric, although exposure frequency and number of exposed counties varied by metric (Table 1). For all exposure classifications considered, our analysis included ≥ 100 storm exposures, and analyses were based in all cases on several thousand observed hospitalizations during storm-exposed and matched unexposed periods (Table 1).
Table 1:
Number of tropical cyclone (TC) exposures and emergency hospital admissions under each of the TC exposure metrics investigated. For continuous exposure measurements (peak sustained wind, cumulative rainfall, and distance to storm track), the number of exposures is given for each of the thresholds of exposure considered in the study. For any storm-exposed day in a county, the unexposed days were in other years in the same county; within a 7-day window of the exposure’s day of year; at least 8 days before or 3 days after any other storm day in the county; and outside 11–24 September 2001.
| Cardiovascular hospitalizations | Respiratory hospitalizations | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Exposure | No. of exposed countiesa | No. of tropical cyclone exposuresb | Storm-exposed daysc | Matched unexposed daysd | Storm-exposed daysd | Matched unexposed daysd |
| Peak sustained winds | ||||||
| 12 m/s | 145 | 558 | 71,357 | 71,026 | 21,512 | 20,770 |
| 15 m/s | 116 | 338 | 47,462 | 47,131 | 14,542 | 13,776 |
| 18 m/s | 86 | 217 | 34,185 | 33,857 | 10,751 | 9,923 |
| 21 m/s | 54 | 123 | 20,351 | 19,661 | 6,496 | 5,747 |
| Cumulative rainfall | ||||||
| 50 mm | 169 | 919 | 119,634 | 116,332 | 35,936 | 34,991 |
| 75 mm | 155 | 505 | 66,062 | 64,548 | 20,181 | 19,209 |
| 100 mm | 123 | 267 | 34,001 | 33,168 | 10,338 | 9,795 |
| 125 mm | 88 | 133 | 16,489 | 15,880 | 5,124 | 4,623 |
| Distance to storm track | ||||||
| 100 km | 159 | 590 | 75,520 | 73,799 | 22,783 | 21,877 |
| 75 km | 150 | 452 | 58,790 | 57,974 | 17,874 | 17,101 |
| 50 km | 136 | 309 | 39,903 | 39,693 | 12,355 | 11,814 |
| 25 km | 95 | 149 | 20,315 | 20,135 | 6,143 | 5,893 |
| Flood event(s) | ||||||
| 151 | 570 | 78,286 | 76,296 | 23,266 | 22,531 | |
| Tornado event(s) | ||||||
| 55 | 111 | 16,246 | 16,037 | 4,767 | 4,682 | |
Total number of counties that were exposed to at least one TC based on a certain exposure metric.
Total TC exposures among study counties under a given exposure metric, where a single storm can result in multiple storm exposures if it hits multiple study counties.
Total hospital admissions among Medicare beneficiaries, summed across storm periods for all storm exposures, for all exposed study counties under a certain exposure metric.
Total hospital admissions (divided by ten to scale to the number of matched unexposed days per exposed day) for the entire storm period for all exposed counties under a certain exposure metric.
For tropical cyclone wind exposures ≥ 21 m/s, we identified 123 exposures in 54 study counties, with local winds from strong gale– to hurricane-force (Table 1, eFigure 4). Across these exposures, cardiovascular hospitalizations were 6% lower (RR: 0.94, 95% CI: 0.89–0.98) on the day of a storm’s closest approach compared to matched unexposed days among Medicare beneficiaries in the study counties (Figure 2, top left panel, lag 0). Storm-day decreases were particularly notable for cerebrovascular disease (RR: 0.86, 95% CI, 0.77–0.96) and peripheral vascular disease (RR: 0.79, 95% CI, 0.59–1.04), whereas other specific cardiovascular causes demonstrated less change on the day of the storm (Table 2). Following the storm, cardiovascular hospitalization risks were elevated compared to matched unexposed days, with highest risks 2–3 days post-storm (RRs: 1.12 [95% CI, 1.07–1.16] at lag 2 and 1.08 [95% CI, 1.04–1.13] at lag 3; Figure 2, top left panel). Over the full storm period considered, risks for cardiovascular disease admissions were slightly higher (RR: 1.03, 95% CI: 1.02–1.05) compared with matched unexposed periods (Figure 3), with highest increases for heart failure (RR: 1.08, 95% CI: 1.04–1.11) (Table 2). Under other wind thresholds considered, cardiovascular hospitalization risks were also elevated across the storm period, with a similar temporal pattern, although associations were dampened for lower-threshold classifications (Figure 3, eFigure 5).
Figure 2:
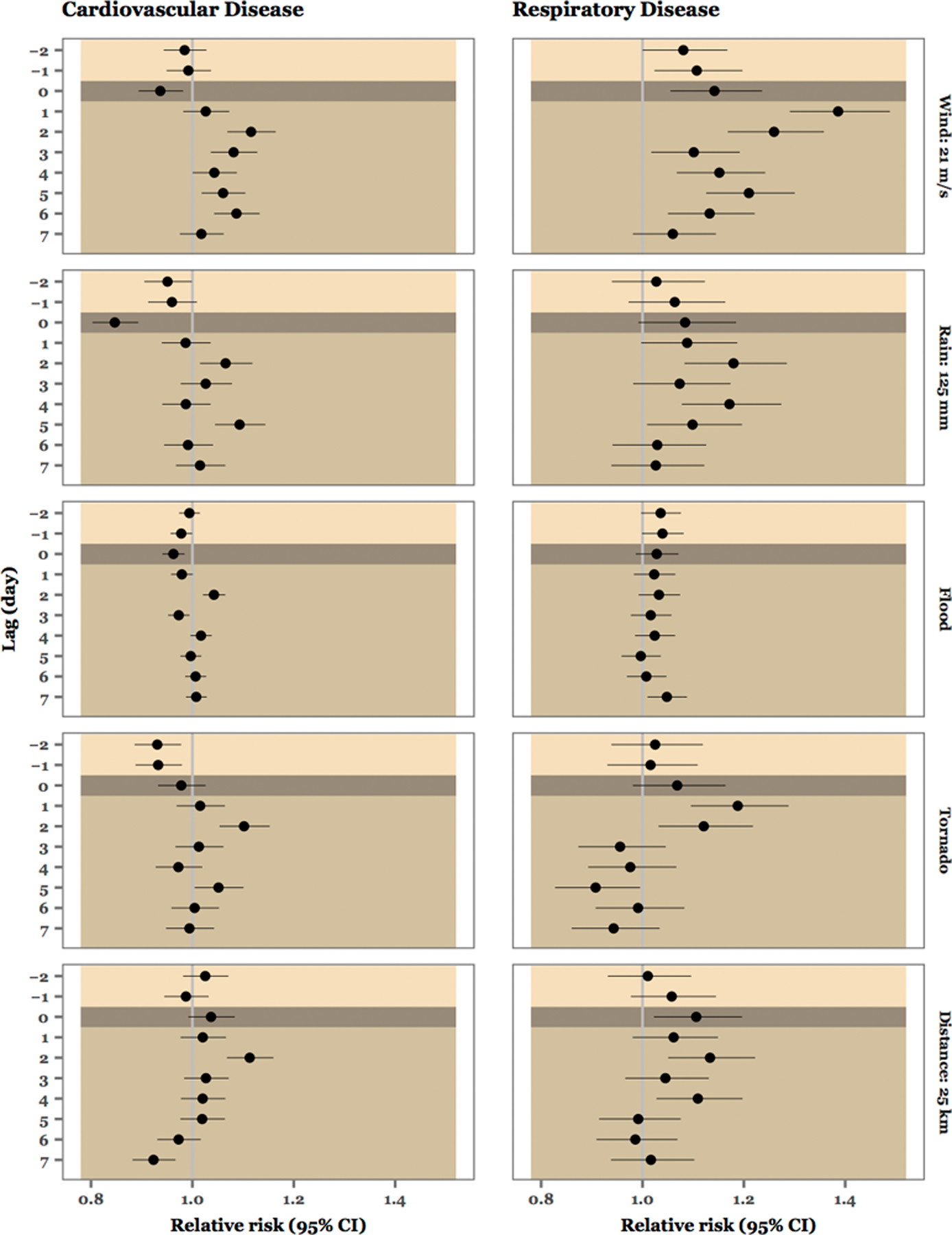
Estimates of lag-specific relative risks of cardiovascular (left) and respiratory (right) hospitalizations on days during storm periods compared to matched unexposed days, for all storms and across all exposed counties, for each of the five exposure metrics considered (labeled on right). Circles show point estimates and horizontal lines show 95% confidence intervals. The gray vertical line shows as a reference a relative risk of 1 (i.e., no observed association between tropical cyclone exposure and hospitalization risk). Shading divides the lag period among pre-storm days (lightest shade), the day of the storm’s closest approach (darkest shade), and post-storm days (intermediate shade).
Table 2:
Observed hospitalizations on storm-exposed period and matched unexposed period and estimates of relative risk for cause-specific hospital admissions associated with tropical cyclone exposures. These results are based on defining exposure as storm-related peak sustained winds of ≥21 m/s at the county’s population mean center. Cardiovascular disease hospitalizations combine hospital admissions coded as 390–459, including hospitalizations for heart failure (ICD-9 428), cerebrovascular disease (430–438), heart rhythm disturbance (426–427), peripheral vascular disease (440–448), ischemic heart disease (410–414 and 429), and acute myocardial infarction (410). Respiratory disease hospitalizations combine hospitalizations with ICD-9 codes 464–466, 480–487, and 490–493, including hospitalizations for respiratory tract infection (464–466, 480–487), chronic obstructive pulmonary disease (COPD, ICD-9, 490–492), and asthma (493).
| Cause of hospitalization | Hospital admission | Relative risk | ||
|---|---|---|---|---|
|
|
||||
| Storm-exposed daysa | Matched unexposed daysb |
Storm dayc |
Storm periodd |
|
| Cardiovascular causes | ||||
| All cardiovascular diseases considered | 20,351 | 19,661 | 0.94 (0.89, 0.98) | 1.03 (1.02, 1.05) |
| Acute myocardial infarction | 2,387 | 2,278 | 1.00 (0.88, 1.14) | 1.05 (1.00, 1.10) |
| Cerebrovascular disease | 3,709 | 3,671 | 0.86 (0.77, 0.96) | 1.00 (0.96, 1.03) |
| Heart failure | 4,898 | 4,669 | 1.00 (0.91, 1.10) | 1.08 (1.04, 1.11) |
| Heart rhythm disturbance | 3,164 | 3,237 | 0.91 (0.81, 1.03) | 1.02 (0.98, 1.06) |
| Ischemic heart disease | 5,494 | 5,122 | 0.95 (0.87, 1.04) | 1.03 (1.00, 1.06) |
| Peripheral vascular disease | 699 | 685 | 0.79 (0.59, 1.04) | 1.05 (0.96, 1.14) |
| Respiratory causes | ||||
| All respiratory diseases considered | 6,496 | 5,747 | 1.14 (1.06, 1.24) | 1.16 (1.13, 1.20) |
| Asthma | 531 | 470 | 1.22 (0.93, 1.59) | 1.20 (1.07, 1.34) |
| Chronic obstructive pulmonary disease | 2,442 | 1,972 | 1.47 (1.31, 1.66) | 1.31 (1.23, 1.39) |
| Respiratory tract infection | 3,523 | 3,304 | 0.94 (0.84, 1.06) | 1.08 (1.03, 1.12) |
Total hospital admissions for the entire storm period for all exposed counties under a certain exposure metric.
Total hospital admissions (divided by ten to scale to the number of matched unexposed days per exposed day) for the entire storm period for all exposed counties under a certain exposure metric.
Estimates on the single day of the storm’s closest approach to the study county.
Estimates for the entire storm period, from two days before to seven days after the storm’s closest approach.
Figure 3:
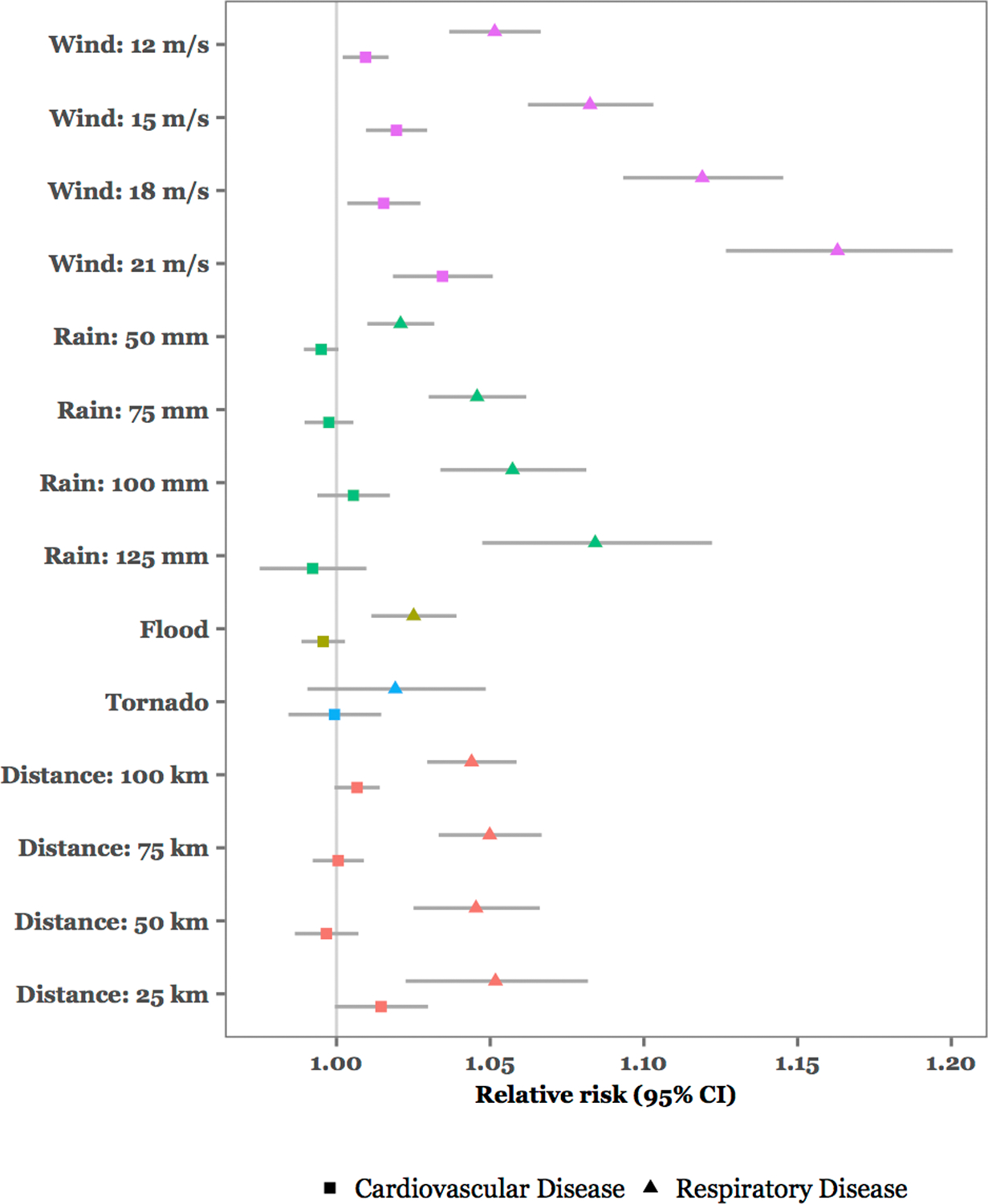
Estimates of relative risks of hospitalization for the full storm period considered (2 days before to 7 days after the storm’s closest approach to the county) compared with matched non-storm periods, for all storms and across all exposed counties. Color is used to represent different exposure metrics (peak sustained winds; cumulative rainfall; flood events; tornado events; and distance from the county center to the storm track). For continuous metrics (peak sustained winds, rainfall, distance to storm track), the threshold used to classify exposure for each estimate is noted on the x-axis. Point estimates are shown with circles for cardiovascular disease and triangles for respiratory disease. Horizontal lines show 95% confidence intervals. The gray vertical line shows as a reference a relative risk of 1 (i.e., no observed association between tropical cyclone exposure and hospitalization risk).
For tropical cyclone wind exposures ≥ 21 m/s, respiratory disease hospitalizations were 14% higher (RR: 1.14, 95% CI: 1.06–1.24) on the day of the storm’s closest approach and remained elevated for several days after the storm, with highest risks on the 2 days after the storm (RR of 1.39 [95% CI, 1.29–1.49] at lag 1 and 1.26 [95% CI, 1.17–1.36] at lag 2; Figure 2, top right panel). Further, for respiratory hospitalizations there was some evidence of elevated risk the 2 days before the storm (Figure 2). Across the storm period, respiratory hospitalization risk steadily increased with higher wind thresholds (Figure 3), with a 16% (RR: 1.16, 95% CI: 1.13–1.20; Figure 3) increase compared to matched unexposed periods under the threshold of ≥ 21 m/s. Storm-associated risks were particularly high for chronic obstructive pulmonary disease (COPD) and asthma, which were 31% (RR: 1.31, 95% CI, 1.23–1.39) and 20% (RR: 1.20, 95% CI, 1.07–1.34) higher across the storm period, respectively, compared with matched unexposed periods (Table 2).
When we examined exposure metrics based on rain, flooding, tornadoes, and distance of the county from the storm, for cardiovascular hospitalizations we found some evidence of a decrease on the day of the storm for most metrics and an increase two days after the storm (Figure 2, eFigure 5), but little evidence of an overall change across the 10-day storm period compared to matched unexposed periods (Figure 3). For respiratory hospitalizations, there was some evidence of increases on the storm day and immediately following the storm, as well as an increase across the storm period, although the size of the associations was in all cases smaller than when storm exposure was defined based on storm-associated peak sustained winds of ≥ 21 m/s at the county center (Figures 2, 3, eFigure 6).
We separately estimated the risks associated with the ten most severe tropical cyclone wind exposures in study counties with >50,000 Medicare beneficiaries (eFigure 2). These represent all exposures in these higher-population counties in which the local peak sustained winds exceeded hurricane-force (eFigure 4). For these severe single-storm exposures, risk for respiratory hospitalization was consistently elevated across the storm periods (eTable 3, “Storm-period estimates”). At the most extreme, we estimated a RR of 1.75 (95% CI, 1.45–2.10) for respiratory Medicare hospitalizations in Broward County, FL, during Hurricane Wilma in 2005, which translated to approximately 43 (95% CI, 31–53) excess respiratory hospitalizations. Storm-period associations for cardiovascular hospitalizations, conversely, varied across these severe exposures, as did associations on the single day of the storm’s closest approach for both respiratory and cardiovascular hospitalizations (eTable 3).
To investigate whether the overall associations observed for tropical cyclone wind exposures (Figures 2 and 3) were driven by these ten most severe events, we compared the estimated RRs of cardiovascular and respiratory hospitalizations in counties with >50,000 Medicare beneficiaries when estimated both with and without these ten events. For both cardiovascular and respiratory hospitalizations, estimated storm-related increases almost halved when excluding these exposures. Cardiovascular hospitalizations were estimated to increase 1.4% across the storm period when all storm exposures were considered versus 0.8% when excluding the ten most severe events, while respiratory hospitalizations were estimated to increase 13.5% across the storm period when all storm exposures were considered versus 8.4% when excluding the ten most severe exposures (eFigure 7).
We conducted a number of sensitivity analyses of our main results and found they were robust to study design and statistical modeling choices (eAppendix), including selection criteria for matched unexposed days (eFigure 8) and adjustment for overdispersion, long-term trends, and county-level differences (eFigure 9). Dispersion diagnostics confirmed evidence of only minor overdispersion (eTable 4).55 Finally, we investigated the potential for unmeasured confounding from long-term temporal trends using a negative control analysis (eFigure 10). RR estimates for negative control exposure were near 1, and only one of twenty had a 95% confidence interval that excluded 1, as expected for a Type I error rate of 5%. We therefore found nothing that suggests that our main results were biased by confounding from long-term trends.
DISCUSSION
This study identified a consistent pattern, across dozens of tropical cyclone exposures, of increased risk for cardiorespiratory hospitalizations during and immediately after storms, adding to a growing understanding of the associations between climate-related exposures and the health of older adults.20 Study counties were all urban, so associations may differ in rural counties.
The biological mechanisms by which tropical cyclones may increase cardiorespiratory disease risk are not established, but some hypotheses are plausible. First, they can induce acute psychological stress, which in turn may trigger both respiratory56 and cardiovascular events.57 Takatsubo cardiomyopathy is especially likely to be triggered by acute emotional stress58 and can lead to heart failure and arrhythmia. Furthermore, tropical cyclone-related hazards can damage infrastructure like transportation and electricity, disrupting medical treatment or hampering medication adherence,6 a particular concern among the elderly, as many have multiple chronic conditions. For example, in a rapid assessment of health status among older adults after Hurricane Charley in Florida, 28% of households reported that at least one older adult was impeded from receiving routine or follow-up care for a pre-existing condition in the two weeks after hurricane.59 This disruption could play some role in the health impacts observed in this study, but could also cause health impacts beyond the period considered here, which ends one week after each storm.
Tropical cyclones can also elevate exposures to environmental hazards, including heat from non-functioning air conditioning7 and air pollution due to debris movement and use of generators.60,61 Bioaerosols can also present an immediate threat. While new mold growth would be too delayed to explain risk observed in this study, mold can be an immediate risk as well; for example, one study observed that mold levels doubled the day after Hurricane Ike in Hamilton County, OH, as damage and winds increased exposure to pre-existing mold in the environment.62
Previous smaller-scale studies have also found evidence of tropical cyclone-associated increases in cardiorespiratory outcomes.8,10,12,63 For example, in the 2 weeks following Hurricane Sandy’s landfall, New Jersey hospitals in highly impacted areas had 22% more visits for myocardial infarctions and 7% more visits for stroke compared to previous years.12 Similarly, in the 2 weeks after Hurricane Iniki, several medical facilities in Kauai, HI, observed increases in visits for asthma and cardiovascular disease.63 Notably, in this study we found higher storm-associated risks for respiratory than cardiovascular Medicare hospitalizations, with increases particularly high for COPD and asthma (Table 2). Many home medical devices are used for respiratory support, especially oxygen therapy,64 and those relying on this equipment are particularly vulnerable to loss of power.64
We observed a lagging pattern in risks of cardiorespiratory hospitalizations across storm exposure periods, with highest increases on days following the storm. For cardiovascular hospitalizations, on the day of the storm’s closest approach we observed an appreciable decrease in risk. Similar storm-day decreases, followed by increases in following days, have been found in previous, smaller-scale studies of tropical cyclone exposure and overall hospital use.13,65–67 This storm-day decrease may represent a delay in seeking treatment, rather than a true reduction in health risk, as suggested by the increased risk following storms. Such a delay may be caused by infrastructure damage preventing patients from travelling to hospitals or calling emergency services68, as well as limited 911 service when a mandatory evacuation order has been issued.69 For respiratory hospitalizations we also found highest risk following the storm; however, risk also increased on the storm day, which may be linked to the need for electronic medical equipment among those with chronic respiratory conditions.64 During the 2003 blackout, for example, respiratory hospitalizations among all New York City residents were increased compared with similar days in different years, whereas no changes were observed for cardiovascular hospitalizations.70
Under wind-based exposure definitions, we also found that respiratory hospitalizations were appreciably increased in the 2 days prior to a storm’s closest approach (Figure 2 and eFigure 6). This finding suggests the potential for storm-associated respiratory risk among the elderly during pre-storm preparations and evacuation. Tropical cyclones are large weather systems, for which winds and rainfall can precede the storm day. Prior to the storm, strong winds may elevate ambient concentrations of environmental exposures like pollen, which has been associated with increased risk of respiratory outcomes.71 Further, pre-storm preparations (e.g., boarding up windows) may create physical triggers for health outcomes, and pre-storm evacuation can bring its own health risks. For example, one study investigated all Medicare-eligible residents of nursing homes in counties where at least one nursing home was evacuated for Hurricane Katrina and found overall hospitalization rates in 30-day period beginning 4 days prior to landfall increased more than 2% (9.87% vs. 7.21% and 7.53%) compared with previous years.10
We found that tropical cyclones varied in their cardiorespiratory risks (eTable 3), with some evidence suggesting this variation may be explained in part by the severity of wind. When we removed the ten most severe tropical cyclone wind exposures from analysis, elevated risk for both respiratory and cardiovascular disease hospitalizations were much smaller compared with estimates when all tropical cyclone exposures were considered (eFigure 7). Further, associations were clearest when exposure was measured based on storm winds ≥ 21 m/s, rather than on lower wind thresholds or other storm hazards (Figures 2 and 3). A heightened risk from the most intense tropical cyclone wind exposures—where the storm brought local peak sustained winds of hurricane-force (eTable 3)—might be related to increased infrastructure damage with stronger winds27 and associated increases in psychological stress, need for post-storm clean-up, and problems adhering to typical medical care.6 For example, physical exertion during clean-up may trigger cardiovascular events,6,22 and a storm that causes more damage would require more extensive clean-up work in the community. Studies on exposures from post-storm clean-up and reconstruction, including of personal property, have found that tropical cyclones can not only exacerbate pre-existing respiratory disease, but also cause new onset of respiratory disease or symptoms.72,73 While our study population includes people who are homebound and unable to assist in post-storm clean-up, some in our study population would likely have a role in cleaning up damage to their own homes or volunteering in clean-up efforts in their community and so may be exposed through this route.
Individual-level exposure misclassification is possible for some study subjects because exposure is assigned based on a county-level estimate. This exposure assessment could result from spatial heterogeneity in the storm’s physical hazards, especially for hazards that tend to be localized within a county, like storm-associated tornadoes. By contrast, other hazards vary more slowly across space, like wind and rain. Individual exposure misclassification could also result from differences in residential building characteristics and evacuation choices across individuals in the county. However, while these mechanisms could create individual-level exposure misclassification when considering direct exposure to the physical hazards of a storm, much of the cardiorespiratory health risk of tropical cyclone exposure might follow through indirect pathways, including pathways that do not require personal exposure to the initial physical hazard. For example, severe winds in a person’s wider community may cause a power outage at the person’s home, even if the storm-associated winds are lower at the home, because power relies on the stability of a large-scale grid. Similarly, while evacuation can avoid personal exposure to the physical hazards of a storm, it introduces a secondary pathway of health risk, including through psychological stress. These factors add nuance when considering the likelihood and implications of individual-level exposure misclassification to tropical cyclone hazards based on use of county-level exposure assessment.
Tropical cyclones are multi-hazard events, and a county affected by one exposure (e.g., severe wind) might also be exposed to others (e.g., flooding, extreme precipitation). In this study, we analyzed exposure based on each hazard separately. We found the strongest signal—and evidence of increasing risk with increasing severity—for the wind-based exposure assessment. Future research could explore co-exposure to multiple hazards of the storm, to help clarify causal pathways and evidence of synergy in effects when a county is concurrently exposed to multiple storm hazards.
Supplementary Material
Sources of funding:
The results reported herein correspond to specific aims of grant R00ES022631 to investigator Anderson from the National Institute of Environmental Health Sciences. This work was also supported by grant 1331399 from the National Science Foundation, grant 83587201–0 from the US Environmental Protection Agency, the Climate Change Solutions Fund from the Vice President for Research of Harvard University, and grants R01MD012769 and R01 ES028033 from the National Institute of Environmental Health Sciences.
Footnotes
Declaration of competing financial interests: None.
Data availability:
Data used in this paper were obtained from Medicare claims data. Due to data protection regulations, this data is not publicly available. Computing code used for this analysis is available at https://gitlab.com/MeilinYan/hurricane_hospitalization_risk.
References
- 1.Sobel AH, Camargo SJ, Hall TM, Lee C-Y, Tippett MK, Wing AA. Human influence on tropical cyclone intensity. Science 2016;353(6296):242–6. [DOI] [PubMed] [Google Scholar]
- 2.Knutson T, Camargo SJ, Chan JC, et al. Tropical cyclones and climate change assessment: Part II. Projected response to anthropogenic warming. Bulletin of the American Meteorological Society 2020;101(3):E303–22. [Google Scholar]
- 3.Shultz JM, Russell J, Espinel Z. Epidemiology of tropical cyclones: The dynamics of disaster, disease, and development. Epidemiologic Reviews 2005;27(1):21–35. [DOI] [PubMed] [Google Scholar]
- 4.Bourque LB, Siegel JM, Kano M, Wood MM. Weathering the storm: The impact of hurricanes on physical and mental health. The Annals of the American Academy of Political and Social Science 2006;604(1):129–51. [Google Scholar]
- 5.Cheng J, Xu Z, Bambrick H, et al. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environmental Research 2019;177:108610. [DOI] [PubMed] [Google Scholar]
- 6.Ryan B, Franklin RC, Burkle FM Jr, et al. Identifying and describing the impact of cyclone, storm and flood related disasters on treatment management, care and exacerbations of non-communicable diseases and the implications for public health. PLoS Currents Diasters 2015; [DOI] [PMC free article] [PubMed]
- 7.Shultz JM, Galea S. Preparing for the next Harvey, Irma, or Maria—addressing research gaps. New England Journal of Medicine 2017;377(19):1804–6. [DOI] [PubMed] [Google Scholar]
- 8.Becquart N, Naumova E, Singh G, Chui K. Cardiovascular disease hospitalizations in Louisiana parishes’ elderly before, during and after Hurricane Katrina. International Journal of Environmental Research and Public Health 2019;16(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma AJ, Weiss EC, Young SL, et al. Chronic disease and related conditions at emergency treatment facilities in the New Orleans area after Hurricane Katrina. Disaster Medicine and Public Health Preparedness 2008;2(1):27–32. [DOI] [PubMed] [Google Scholar]
- 10.Dosa D, Feng Z, Hyer K, Brown LM, Thomas K, Mor V. Effects of Hurricane Katrina on nursing facility resident mortality, hospitalization, and functional decline. Disaster Medicine and Public Health Preparedness 2010;4(S1):S28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McQuade L, Merriman B, Lyford M, et al. Emergency department and inpatient health care services utilization by the elderly population: Hurricane Sandy in the state of New Jersey. Disaster Medicine and Public Health Preparedness 2018;12(6):730–8. [DOI] [PubMed] [Google Scholar]
- 12.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB, others. The effect of Hurricane Sandy on cardiovascular events in New Jersey. Journal of the American Heart Association 2014;3(6):e001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim H, Schwartz RM, Hirsch J, Silverman R, Liu B, Taioli E. Effect of Hurricane Sandy on Long Island emergency departments visits. Disaster Medicine and Public Health Preparedness 2016;10(3):344–50. [DOI] [PubMed] [Google Scholar]
- 14.Grynszpan D, Murray V, Llosa S. Value of case studies in disaster assessment? Prehospital and Disaster Medicine 2011;26(3):202–5. [DOI] [PubMed] [Google Scholar]
- 15.Ioannidis JP. Exposure-wide epidemiology: Revisiting Bradford Hill. Statistics in Medicine 2016;35(11):1749–62. [DOI] [PubMed] [Google Scholar]
- 16.Dominici F Air pollution and health: What can we learn from an hierarchical approach? Invited commentary. American Journal of Epidemiology 2002;1:11–5. [DOI] [PubMed] [Google Scholar]
- 17.Goodman SN. The methodologic ozone effect. Epidemiology 2005;16(4):430–5. [DOI] [PubMed] [Google Scholar]
- 18.Samet J, Dominici F, Zeger S, Schwartz J, Dockery D. The National Morbidity, Mortality, and Air Pollution Study. Part I: Methods and Methodologic Issues. Research Report for the Health Effects Institute 2000;(94(Pt 1)):5–14. [PubMed] [Google Scholar]
- 19.Bradford Hill A The environment and disease: Association or causation? Journal of the Royal Society of Medicine 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- 20.Gamble JL, Hurley BJ, Schultz PA, Jaglom WS, Krishnan N, Harris M. Climate change and older Americans: State of the science. Environmental Health Perspectives 2013;121(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayhorn CB. Cognitive aging and the processing of hazard information and disaster warnings. Natural Hazards Review 2005;6(4):165–70. [Google Scholar]
- 22.Rappaport EN, Blanchard BW. Fatalities in the United States indirectly associated with Atlantic tropical cyclones. Bulletin of the American Meteorological Society 2016;97(7):1139–48. [Google Scholar]
- 23.Zimmerman R, Restrepo CE, Nagorsky B, Culpen AM. Vulnerability of the elderly during natural hazard events. 2009;
- 24.Dominici F, Levy JI, Louis TA. Methodological challenges and contributions in disaster epidemiology. Epidemiologic Reviews 2005;27(1):9–12. [DOI] [PubMed] [Google Scholar]
- 25.Benson WF, Aldrich N. CDC’s disaster planning goal: Protect vulnerable older adults. CDC Health Aging Program 2007.
- 26.Saulnier DD, Ribacke KB, von Schreeb J. No calm after the storm: A systematic review of human health following flood and storm disasters. Prehospital and Disaster Medicine 2017;32(5):568–79. [DOI] [PubMed] [Google Scholar]
- 27.Pita GL, Pinelli J-P, Gurley KR, Hamid S. Hurricane vulnerability modeling: Development and future trends. Journal of Wind Engineering and Industrial Aerodynamics 2013;114:96–105. [Google Scholar]
- 28.McCarthy FX. FEMA’s disaster declaration process: A primer [Internet]. 2014. Available from: https://fas.org/sgp/crs/homesec/R43784.pdf
- 29.Logue JN, Melick ME, Hansen H. Research issues and directions in the epidemiology of health effects of disasters. Epidemiologic Reviews 1981;3(1):140–62. [DOI] [PubMed] [Google Scholar]
- 30.Grabich SC, Horney JA, Konrad CE, Lobdell DT. Measuring the storm: Methods of quantifying hurricane exposure with pregnancy outcomes. Natural Hazards Review 2015;17(1):06015002. [Google Scholar]
- 31.Landsea CW, Franklin JL. Atlantic hurricane database uncertainty and presentation of a new database format. Monthly Weather Review 2013;141:3576–92. [Google Scholar]
- 32.Willoughby HE, Darling RW, Rahn ME. Parametric representation of the primary hurricane vortex. Part II: A new family of sectionally continuous profiles. Monthly Weather Review 2006;134(4):1102–20. [Google Scholar]
- 33.Anderson B, Schumacher A, Guikema S, Quiring S, Ferreri J. Stormwindmodel: Model tropical cyclone wind speeds [Internet]. 2017. Available from: https://CRAN.R-project.org/package=stormwindmodel
- 34.World Meteorological Organization. Global guide to tropical cyclone forecasting. Secretariat of the World Meteorological Organization; 2017. [Google Scholar]
- 35.Bobrowsky PT. Encyclopedia of Natural Hazards. Springer:Dordrecht; 2013. [Google Scholar]
- 36.Costa IC, Venturini LF, da Rosa MA. Wind speed severity scale model applied to overhead line reliability simulation. Electric Power Systems Research 2019;171:240–50. [Google Scholar]
- 37.Dhunny AZ, Samkhaniani N, Lollchund MR, Rughooputh SD. Investigation of multi-level wind flow characteristics and pedestrian comfort in a tropical city. Urban Climate 2018;24:185–204. [Google Scholar]
- 38.Rappaport EN. Loss of life in the United States associated with recent Atlantic tropical cyclones. Bulletin of the American Meteorological Society 2000;81(9):2065–73. [Google Scholar]
- 39.Anderson B, Yan M, Ferreri J, et al. hurricaneexposure: Explore and map county-level hurricane exposure in the United States [Internet]. 2017. Available from: https://cran.r-project.org/package=hurricaneexposure
- 40.Rui H, Mocko D. README Document for North America Land Data Assimilation System Phase 2 (NLDAS-2) Products. Greenbelt, Maryland: 2014. [Google Scholar]
- 41.Al-Hamdan MZ, Crosson WL, Economou SA, et al. Environmental public health applications using remotely sensed data. Geocarto International 2014;29(1):85–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.NOAA, National Centers for Environmental Information. Storm Events Database [Internet]. 2018; Available from: https://www.ncdc.noaa.gov/stormevents/
- 43.Anderson B, Chen Z. noaastormevents: Explore NOAA Storm Events Database [Internet]. 2019. Available from: https://cran.r-project.org/package=noaastormevents
- 44.Czajkowski J, Simmons K, Sutter D. An analysis of coastal and inland fatalities in landfalling US hurricanes. Natural Hazards 2011;59(3):1513–31. [Google Scholar]
- 45.Anderson GB, Ferreri J, Al-Hamdan M, et al. Assessing United States county-level exposure for research on tropical cyclones and human health. Environmental Health Perspectives In Press; National Institute of Environmental Health Science. 10.1289/EHP6976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peng RD, Chang HH, Bell ML, et al. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among Medicare patients. Journal of the American Medical Association 2008;299(18):2172–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD. Heat-related emergency hospital- izations for respiratory diseases in the Medicare population. American Journal of Respiratory and Critical Care Medicine 2013;187(10):1098–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schwartz J, Marcus A. Mortality and air pollution in London: A time series analysis. American Journal of Epidemiology 1990;131(1):185–94. [DOI] [PubMed] [Google Scholar]
- 49.Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H. Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology 2001;12(2):186–92. [DOI] [PubMed] [Google Scholar]
- 50.Yan M, Wilson A, Peel JL, et al. Community-wide mortality rates in Beijing, China, during the July 2012 Flood compared with unexposed periods. Epidemiology 2020;31(3):319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. Journal of the American Medical Association 2014;312(24):2659–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu JC, Wilson A, Mickley LJ, et al. Wildfire-specific fine particulate matter and risk of hospital admissions in urban and rural counties. Epidemiology 2017;28(1):77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gasparrini A Modeling exposure-lag-response associations with distributed lag non-linear models. Statistics in Medicine 2014;33(5):881–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bobb JF, Ho KK, Yeh RW, et al. Time-course of cause-specific hospital admissions during snowstorms: An analysis of electronic medical records from major hospitals in Boston, Massachusetts. American Journal of Epidemiology 2017;185(4):283–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Korner-Nievergelt F, Roth T, von Felten S, Guelat J, Almasi B, Korner-Nievergelt P. Bayesian Data Analysis in Ecology Using Linear Models with R, BUGS, and Stan. Elsevier:London; 2015. [Google Scholar]
- 56.Rietveld S, Everaerd W, Creer T. Stress-induced asthma: A review of research and potential mechanisms. Clinical and Experimental Allergy 2000;30(8):1058. [DOI] [PubMed] [Google Scholar]
- 57.Steptoe A, Kivimä M. Stress and cardiovascular disease. Nature Reviews Cardiology 2012;9(6):360. [DOI] [PubMed] [Google Scholar]
- 58.Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (Tako-tsubo) cardiomyopathy. Journal of the American College of Cardiology 2010;55(4):333–41. [DOI] [PubMed] [Google Scholar]
- 59.Centers for Disease Control and Prevention. Rapid assessment of the needs and health status of older adults after Hurricane Charley–Charlotte, DeSoto, and Hardee Counties, Florida, August 27–31, 2004. MMWR Morbidity and Mortality Weekly Report 2004;53(36):837. [PubMed] [Google Scholar]
- 60.Chen B, Shawn L, Connors N, et al. Carbon monoxide exposures in New York City following Hurricane Sandy in 2012. Clinical Toxicology 2013;51(9):879–85. [DOI] [PubMed] [Google Scholar]
- 61.Lane K, Charles-Guzman K, Wheeler K, Abid Z, Graber N, Matte T. Health effects of coastal storms and flooding in urban areas: A review and vulnerability assessment. Journal of Environmental and Public Health 2013;2013. [DOI] [PMC free article] [PubMed]
- 62.Schmidlin TW. Public health consequences of the 2008 Hurricane Ike windstorm in Ohio, USA. Natural Hazards 2011;58(1):235–49. [Google Scholar]
- 63.Hendrickson LA, Vogt RL, Goebert D, Pon E. Morbidity on Kauai before and after Hurricane Iniki. Preventive Medicine 1997;26(5):711–6. [DOI] [PubMed] [Google Scholar]
- 64.Molinari NAM, Chen B, Krishna N, Morris T. Who’s at risk when the power goes out? The at-home electricity-dependent population in the United States, 2012. Journal of Public Health Management and Practice: JPHMP 2017;23(2):152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Platz E, Cooper HP, Silvestri S, Siebert CF. The impact of a series of hurricanes on the visits to two central Florida emergency departments. The Journal of Emergency Medicine 2007;33(1):39–46. [DOI] [PubMed] [Google Scholar]
- 66.Smith CM, Graffeo CS. Regional impact of Hurricane Isabel on emergency departments in coastal southeastern Virginia. Academic Emergency Medicine 2005;12(12):1201–5. [DOI] [PubMed] [Google Scholar]
- 67.Mortensen K, Dreyfuss Z. How many walked through the door?: The effect of Hurricane Katrina evacuees on Houston emergency departments. Medical Care 2008;46(9):998–1001. [DOI] [PubMed] [Google Scholar]
- 68.Jangi S Facing uncertainty—dispatch from Beth Israel Medical Center, Manhattan. New England Journal of Medicine 2012;367(24):2267–9. [DOI] [PubMed] [Google Scholar]
- 69.National Governors Association. 2014. Governor’s Guide to Mass Evacuation. https://www.nga.org/wp-content/uploads/2018/08/GovGuideMassEvacuation.pdf.
- 70.Lin S, Fletcher BA, Luo M, Chinery R, Hwang S-A. Health impact in New York City during the Northeastern blackout of 2003. Public Health Reports 2011;126(3):384–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.D’Amato G, Liccardi G, Frenguelli G. Thunderstorm-asthma and pollen allergy. Allergy 2007;62(1):11–6. [DOI] [PubMed] [Google Scholar]
- 72.Rando RJ, Lefante JJ, Freyder LM, Jones RN. Respiratory health effects associated with restoration work in post-Hurricane Katrina New Orleans. Journal of Environmental and Public Health 2012;2012:462478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gargano LM, Locke S, Jordan HT, Brackbill RM. Lower respiratory symptoms associated with environmental and reconstruction exposures after Hurricane Sandy. Disaster Medicine and Public Health Preparedness 2018;12(6):697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in this paper were obtained from Medicare claims data. Due to data protection regulations, this data is not publicly available. Computing code used for this analysis is available at https://gitlab.com/MeilinYan/hurricane_hospitalization_risk.


