Abstract
Objectives
Report the injury epidemiology of law enforcement and firefighter recruits.
Design
A systematic epidemiological review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 guidelines was completed.
Data sources
Five online databases were searched from database inception to 5 May 2021.
Eligibility criteria for selecting studies
Prospective and retrospective studies that reported data on musculoskeletal injuries sustained by law enforcement or firefighter recruits were included. We reported on all components of injury where data were available. All injury incidence rates were calculated as per 1000 training days (Poisson 95% CI) to allow comparisons between studies. Study quality was assessed using the Joanna Briggs Institute Quality Assessment Checklist for Prevalence Studies.
Results
No studies reporting firefighter recruits were identified. Eight published studies that reported on injuries to law enforcement recruits were identified. The studies were all low quality, and the credibility of the evidence was assessed as very low. Seven studies reported medical attention injuries, and one study reported the number of medical withdrawals from a recruit training programme. The prevalence of law enforcement recruits with medical attention injuries ranged from 13.7% to 24.5%. The overall medical attention injury incidence rate for law enforcement recruits ranged from 1.67 injuries per 1000 training days (Poisson 95% CI 1.00 to 2.34 injuries per 1000 training days) to 4.24 injuries per 1000 training days (Poisson 95% CI 2.97 to 5.51 injuries per 1000 training days).
Conclusion
This review reported the prevalence and incidence rates for musculoskeletal injuries in law enforcement officers. However, the credibility of the evidence is very low.
PROSPERO registration number
CRD42021251084.
Keywords: epidemiology, injuries, public health
Summary box.
What is already known?
Injuries to law enforcement officers and firefighters have been reported throughout the literature. Still, no systematic review has been performed reporting recruit injury epidemiology, even though this population complete strenuous physical training.
What are the new findings?
No studies have reported the injury profile of firefighter recruits.
Medical attention injuries in law enforcement recruits ranged from 13.7% to 24.5%.
Law enforcement officers’ medical attention injury incidence rate ranged from 1.67 to 4.24/1000 training days.
Most law enforcement officers’ medical attention injuries are distributed between the upper limb (12.5%–38.2%), trunk/spine/abdomen (19.1%–50%) and lower limb (25%–41.1%).
Background
Tactical operators (such as law enforcement officers or firefighters) undergo intense and strenuous physical training programmes as a part of their qualification process to prepare for the demands of their role, with the duration of training differing between professions and countries.1–3 These intense training programmes are important as they mirror the demands of the occupation and ensure law enforcement officers and firefighters are job-ready. However, these job-specific physical training programmes have been shown to result in injuries.1–3 Therefore, it is reasonable to expect musculoskeletal injuries to law enforcement officers and firefighters are common during their training processes.
No reviews to date have specifically explored the injury profiles of law enforcement and firefighter recruits during their academy training and physical preparation programmes.4 5 In firefighters, a 2019 systematic review of injury epidemiology detailed operational workplace injuries in fully qualified personnel.4 This review reported the proportion of injuries, ranging from 9% to 74%4 of participants. No studies were identified that reported injuries during prequalification recruit physical training. However, this review did exclude studies that provided interventions,4 potentially limiting the number of available studies and in the absence of large epidemiological studies, worth including with literature reviews.
A second systematic review reported injury occurrence in law enforcement officers, ranging from 28% to 81% of the population.5 However, few studies defined what was classified as an injury (eg, medical attention injury or time-loss definitions), and occupational injuries (eg, mental health concerns following a distressing work incident) were also included that do not apply to recruits in pre-deployment physical preparation programmes.5 As opposed to the review of firefighters, studies reporting injuries to law enforcement recruits were identified.5 Some of these studies involving recruits reported the definition of an injury (eg, medical attention or time-loss definitions). They demonstrated the proportion of medical attention injuries within police recruits during basic training between 15% and 26%.3 6 Given the sparsity of studies identified in these reviews, the inclusion of randomised controlled trials (RCTs) of injury prevention that include a standard practice (eg, natural history arm) should be considered to overcome the lack of epidemiological studies, and overcome the small samples that may lead to the imprecision of results.7
The challenge for clinicians and researchers who develop physical preparation and injury prevention programmes is that no reviews report how much training and preparation time is lost when firefighter and law enforcement recruits are injured during basic training, what injuries are most common, and what mechanisms of injury cause recruit injury. The nature of musculoskeletal injuries within law enforcement and firefighter recruit training are potentially more comparable to sports injuries than typical occupational injuries (eg, neck and back pain from workplace sitting)8 as the injuries are usually related to the fitness component of the recruits training.9 10 However, studies have not differentiated important components of the injury landscape potentially relevant in prevention models.11 Several different components related to injures can be reported: severity of injury (any injury, medical attention injury, time-loss injury or career-ending injury), relationship to activity (directly, indirectly, or not related), mode of onset (sudden or gradual), mechanism of injury (direct contact, indirect contact or non-contact), subsequent injury, body area, tissue type or pathology type.12 Injury data can also be presented in different ways: Injury frequency (number of injuries reported within the sample), injury proportion (percentage of different injuries within the injured participants), injury prevalence (the portion of the sample which has an injury during a specific time frame), injury incidence (the number of new injuries experienced over a specified time frame), injury incidence rate (the number of new injuries experienced when accounting for exposure), injury severity (the time-loss due to injury) or injury burden (the injury incidence combined with the injury severity).12 These components help inform researchers and clinicians where the ‘injury problem’ lies within their physical training programme and can help inform the development of programmes less likely to result in injury.12
The International Olympic Committee consensus statement on the methods for recording and reporting epidemiological data by Bahr et al12 highlights the importance of defining and classifying the health problems associated with physical activity. The reviews identified above,4 5 have not extracted and reported the data suggested by Bahr et al,12 which may be more meaningful for real-world translation. As an example, previous reviews have not differentiated the different injury types (eg, medical attention vs time loss) that are important for translating prevention strategies into clinical practice and policy. This enables clinicians and researchers to examine risk factors for injury and then implement prevention strategies to reduce the burden of injury. This systematic review aimed to determine the injury epidemiology of law enforcement and firefighter recruits.
Methods
Guidelines
The protocol for this systematic review was designed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-Protocols,13 with the final systematic review informed by the recent updates to the PRISMA.14
Data management
Records and data related to study selection were stored online using Covidence (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org). Extracted data was managed and stored using Microsoft teams and password-protected laptop computers. To facilitate systematic review transparency,15 16 the final data spreadsheet is also freely available (Murphy, Myles (2022): Musculoskeletal injury epidemiology in law enforcement and firefighter recruits during physical training: a systematic review. figshare. Dataset. https://doi.org/10.6084/m9.figshare.19076567.v1).
Criteria for considering studies for this review
Types of studies
Prospective and retrospective studies which reported data on musculoskeletal injury were included. We included both cross-sectional and longitudinal studies (including RCTs of injury prevention interventions). For example, RCTs of an intervention within a specific injury population (eg, the effect of orthotics in police or firefighter recruits with stress fractures) were excluded, but RCTs that examined injury prevention (eg, the effect of orthotics in preventing stress fractures within police or firefighter recruits) were included provided they had a control arm without an intervention. Only published studies were included within this review (ie, grey literature excluded). Non-English language studies were also excluded. Prior work suggested that inclusion or exclusion of non-English articles do not influence the effect estimates yet may narrow CIs.17
Types of participants
We included law enforcement and firefighter recruits, regardless of sex, geographical location, age and physical activity levels.
Types of injuries
All musculoskeletal injuries sustained by participants were included. Injuries were defined as all medical attention and time-loss following the International Olympic Committee reporting standards.12 A further type of injury, an injury requiring withdrawal from the recruit training programme, was also included.
Search methods for identification of studies
Search strategies were implemented from inception until the 5 May 2021 by a single author (MCM), who exported the records into Covidence.
Electronic searches
Searches were performed using free text and MESH terms (online supplemental appendix A) to identify published articles on the following electronic databases: PubMed, CINAHL, CENTRAL, SPORTDiscus and Web of Science. Only peer-reviewed, English language, human trials were included. However, these limitations were adapted to individual databases as necessary (online supplemental appendix B). Search results were piloted and validated by ensuring searches included key research papers (Orr et al3 Orr et al 18 and Orr et al19).
bmjsem-2021-001289supp001.pdf (53.8KB, pdf)
Searching other resources
Reference lists of relevant reviews and included studies were screened, and backwards citation tracking was performed via Web of Science to identify potentially relevant studies. Content experts evaluated the list of included studies to help identify any other relevant studies. The ePublication lists of key journals in the field (ie, journals where other included studies had been published) were screened to detect studies that had yet to be indexed in the databases.
Selection of studies
Two review authors (H-AG/MCM or H-AG/MN) independently assessed the titles and abstracts of potential studies identified by the search strategy for their eligibility. When the study’s eligibility was unclear from the title and abstract, the full paper was assessed. Studies that did not match the inclusion criteria for this review were excluded, and the reasons for excluding full-text articles were recorded within the PRISMA flow chart.20 Disagreements between authors regarding study inclusion were resolved by discussion. Studies were not anonymised before assessment.
Data management
Data extraction
Two review authors (H-AG/MN) independently extracted data from included studies and input the data into Microsoft Excel. For any discrepancies or disagreements, the review authors resolved these via consensus. Where consensus could not be achieved, a third author (MCM) made a majority decision after assessing the study. The following information was extracted: primary author, year of publication, country of origin, funding source, study design (retrospective or prospective data collection), study population (law enforcement or firefighter recruits), sample size (n), duration of recruit training (weeks), method of exposure to physical training (hours), mean (SD) baseline demographics (age, gender, height, weight and body mass index), all descriptive injury data inclusive of measures of variability: severity of injury, relationship to activity, mode of onset, mechanism of injury, new or subsequent injury, body area, tissue type or pathology type, and all injury data analysis inclusive of measures of variability: injury frequency, injury proportion, injury prevalence, injury incidence, injury incidence rate, injury severity and injury burden.
Dealing with missing data
Where a method of exposure was not provided (eg, the number of training hours was not reported), it was assumed that 1 week of recruit training represented five training exposure days. Three studies did not specify whether the injuries reported were based on the total number of injuries or the number of injured participants.3 19 21 To include within analysis, we assumed they reported the number of injured participants.
Assessment of quality in included studies
Two review authors (H-AG and MN) independently assessed the quality of included studies. Where there were disagreements between review authors, they were resolved by discussion. However, where consensus could not be achieved, a majority decision was made by a third review author (MCM). The Joanna Briggs Institute, Quality Assessment Checklist for Prevalence Studies, was used to assess the study quality in the included studies.
Assessment of diversity and heterogeneity
Given the variety in recruit training protocols (eg, differing durations or differing programmes) between studies, we had anticipated significant clinical diversity among the included populations. Total variation across all studies included within meta-analysis was planned to be explored using the I² statistic, but due to substantial clinical diversity precluding meta-analysis, this was not performed.
Assessment of reporting biases
The possible influence of publication and small study biases on review findings was considered. The influence of small study biases was addressed by the risk of bias criterion ‘study size’. Studies with fewer than 50 injuries represent a high risk of small sample bias. Studies with between 50 and 200 injuries were classified as the moderate risk of small sample bias, and studies with greater than 200 injuries were classified as low risk of small sample bias.7
Data synthesis
Law enforcement and firefighter data were presented separately. Data analysis was conducted using SPSS V.27 (SPSS). All demographic data were described using mean and SD. We reported on all components of injury where data were available:
Injury presented as a count and proportion.
Injury prevalence was presented as a percentage over a specified time frame.
Injury incidence was presented as the number of new injuries over a specified time frame.
The injury incidence rate was presented as the number of injuries per measure of exposure.
Injury severity was presented as the mean (SD) time loss.
The injury burden was presented as the mean injury incidence multiplied by the mean injury severity (95% CIs).
All injury incidence rates were calculated as per 1000 training days (Poisson 95% CI) to allow comparisons between studies. Due to substantial clinical diversity, the limited number of studies and no studies reporting injury metrics such as severity, several planned procedures were unable to be performed, including data pooling to determine overall injury incidence, overall injury incidence rate, overall injury severity and overall injury burden with 95% CIs and meta-regression of the influence of demographic variables on the pooled effect estimates.
Sensitivity analysis
A sensitivity analysis had been planned but was not performed due to the limited number of studies.
Subgroup analysis
A subgroup analysis had been planned but was not performed due to the limited number of studies.
Assessment of the certainty of the body of evidence
The assessment for overall certainty of the body of evidence differs in systematic epidemiological reviews compared with traditional systematic reviews of diagnostic accuracy or interventions. It can be adjusted for different models (eg, exposure).22 Therefore, assessment of the certainty of the body of evidence was assessed using the Grades of Recommendations, Assessment, Development and Evaluation (GRADE) approach,23 adapted for use in epidemiological studies.22 The GRADE approach involved making an overall judgement on the quality of the body of evidence-based on the overall quality with studies being upgraded or downgraded based on different factors such as the risk of bias and sample size.23
Results
Selection of studies
Collectively, 2112 records were identified, eight records met the selection criteria following the full-text screening of 15 articles (figure 1). Reasons for full-text exclusion are reported in online supplemental appendix C.
Figure 1.
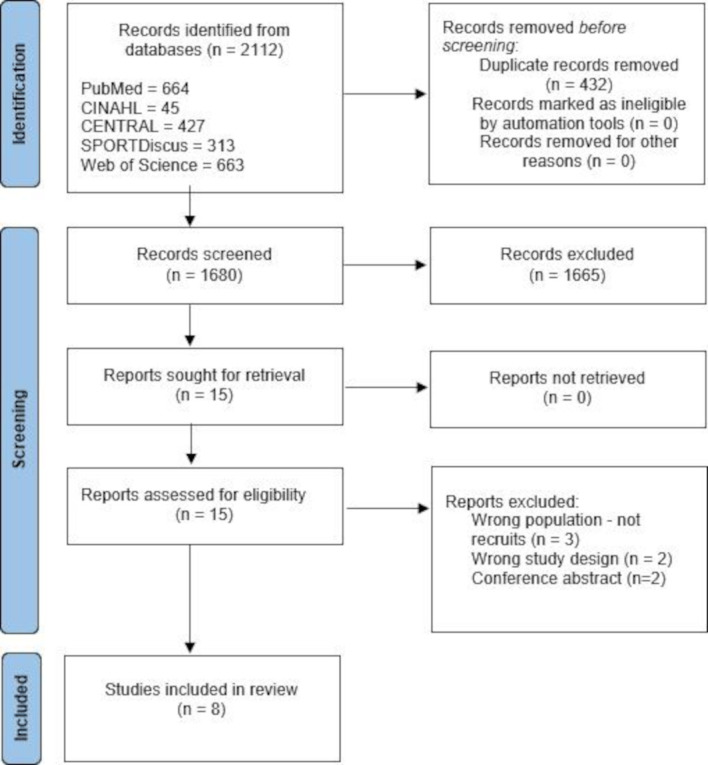
PRISMA flow chart. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Study information
All included studies investigated injury in law enforcement recruits.1–3 18 19 21 24 25 No studies investigating injury in firefighter recruits were identified. Full study data are provided in table 1. Seven of the included studies (87.5%) represented a cohort study,1–3 19 21 24 25 whereas one study (12.5%) was a randomised trial.18 Three studies (37.5%) were conducted in Australia,3 18 19 two studies (25%) in the USA,2 21 one study (12.5%) in China,25 one study (12.5%) in Israel1 and one study (12.5%) in New Zealand.24 Six studies (75%) investigated injuries within Police officers,3 18 19 21 24 25 one study (12.5%) in border police1 and one study (12.5%) in Federal Bureau of Investigation recruits.2 The duration of training varied from 10 to 21 weeks.1–3 18 19 21 24 25 No studies reported external funding.
Table 1.
Study information for law enforcement recruits
| Study | Country | Study design | Funding source | Sampling time frame | Injury reporting (prospective/ retrospective) | Injury definition (all, medical attention, time-loss or required withdrawal from recruit training programme) | Injury nature provided (eg, fracture) | Injury region provided (eg, knee) |
| Constantini et al 20101 | Israel | Prospective intervention with historical control | Private | 1996–2005 (control) | Prospective | Medical attention | Yes | Yes |
| Knapik et al 20112 | USA | Prospective cohort | Internally—Federal Bureau of Investigation and US Army Public Health Command | 2009–2010 | Prospective | Medical attention | Yes | No |
| Lockie et al 201921 | USA | Retrospective cohort | No funding | Not reported | Prospective | Withdrawal from programme | No | No |
| Orr et al 20163 | Australia | Retrospective cohort | Not reported | 2013–2014 | Prospective | Medical attention | No | No |
| Orr et al 201618 | Australia | Randomised controlled trial | Not reported | Not reported | Prospective | Medical attention | No | Yes |
| Orr et al 201719 | Australia | Retrospective cohort | No funding | 2013 | Prospective | Medical attention | No | No |
| Tomes et al 202024 | New Zealand | Retrospective cohort | Not reported | Not reported | Prospective | Medical attention | No | Yes |
| Wang et al 200325 | China | Retrospective cohort | Not reported | 1999–2000 | Prospective | Medical Attention | No | No |
Seven studies (87.5%) reported medical attention injuries only1–3 18 19 24 25 and one study (12.5%) reported injuries resulting in discharge from the training programme.21 Four studies (50%) supplied some data on the region of injury. However, no studies supplied sufficient information to classify injuries according to their nature. Data collection for all studies was prospective, though medical records were obtained via the law enforcement agency database retrospectively. As the injury data for included studies were originally recorded within a database and provided to included studies on request, authors were not contacted for additional information as lack of detail was unlikely to be related to study reporting, and instead a result of database limitations.
Participant demographics
Complete demographic details are presented in table 2. Four studies (50%) reported the sex split with a range of 0%–100% female recruits being included.1 2 21 25 Three studies (37.5%) reported other demographic information for participants.1 21 25
Table 2.
Demographic information for law enforcement recruits
| Study | Recruit type | Duration of recruit training (weeks) | Total sample size (n) | Total injured participants (n) | Total injuries (n) | Total sample mean (SD) age (years) | Total sample mean (SD) height (cm) | Total sample mean (SD) weight (kg) | Total sample mean (SD) BMI (m/kg2) | Total sample gender (% female) |
| Constantini et al 20101 | Border Police | 16 | 1423 | 82 | 215 | Not reported | Not reported | Not reported | Not reported | 100 |
| Knapik et al 20112 | Federal Bureau of Investigation | 21 | 531 | Not reported | 256 | Not reported | Not reported | Not reported | Not reported | 20 |
| Lockie et al 201921 | Police | Not reported | 401 | 18 | Not reported | 27.3 (5.92) | 174 (12) | 80.27 (14.38) | Not reported | 17 |
| Orr et al 20163 | Police | 12 | 1021 | 158 | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Orr et al 201618 | Police | 10 | 287 | Not reported | 24 | Not reported | Not reported | Not reported | Not reported | Not reported |
| Orr et al 201719 | Police | 12 | 169 | 43 | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Tomes et al 202024 | Police | 16 | 243 | Not reported | 68 | Not reported | Not reported | Not reported | Not reported | Not reported |
| Wang et al 200325 | Police | Not reported | 805 | 111 | 130 | 18.7 (1.02) | 170.36 (5.31) | 62.5 (8.8) | 21.52 (2.68) | 0 |
BMI, body mass index.
Assessment of heterogeneity
Demographic information within studies was poorly reported, precluding judgement of whether studies were sufficiently homogenous for meta-analysis. Studies had a varied proportion of females within the sample. Law enforcement recruit training was performed in various countries for different occupations and was performed across different years/decades, suggesting that training programmes may not be similar. Meta-analysis was not conducted due to concerns regarding clinical diversity within the included samples, and statistical heterogeneity was not calculated.
Injury profiles
Injury frequency and proportion
A total of 412 injured participants were reported within 3606 participants across five studies (62.5%).1 3 19 21 25 A total of 693 injuries were reported within 3076 participants across five studies (62.5%).1 2 18 24 25 Two studies (25%) reported the total number of injuries and the number of injured participants.1 25 Three studies (37.5%) reported the number of injured participants only.3 19 21 Three studies (37.5%) reported the total number of injuries only.2 18 24 The proportion of different injury regions was reported in two studies (online supplemental appendix D). One study of medical attention injuries in Australian police recruits reported 3/24 (12.5%) injuries occurred to the abdomen, lower back, lumbar spine and pelvis, 12/24 (50%) injuries occurred to the knee and lower leg and 6/24 (25%) injuries occurred to the ankle and foot with 3/24 injuries (12.5%) undesignated.18 Another study of medical attention injuries in New Zealand police recruits reported 13/68 (19.1%) injuries occurred in the trunk and spine, 26/68 (38.2%) injuries occurred in the upper limb and 28/68 (41.1%) injuries occurred in the lower limb with one injury (1.6%) not being allocated to a body region.24
Injury prevalence
The prevalence of medical attention injuries (ie, the number of injuries overall, irrespective of whether multiple injures were within a single participant) or injured participants (ie, the number of participants injured irrespective of the number of overall injuries) for the duration of their recruit training programme was provided for all studies. The prevalence of police recruits with medical attention injuries ranged from 13.7% to 24.5%.3 19 21 25 The prevalence of medical attention injuries within police recruits ranged from 8.4% to 27.9%.24 25 The prevalence of Federal Bureau of Investigation recruits with medical attention injuries was not reported.2 The prevalence of medical attention injuries within FBI recruits was 48.2%.2 The prevalence of Israeli border police recruits with stress fractures requiring medical attention was 6.8%.1 The prevalence of stress fractures requiring medical attention within border police recruits was 17.8%.1
Injury incidence and injury incidence rate
Two studies were not included within calculations of the injury incidence rates as they did not provide the duration of the recruit training programme.21 25 The injury incidence rates for overall medical attention injuries, injury incidence rates for medical attention injuries per body region were calculated, and injury incidence rates for stress fractures requiring medical attention were calculated. The overall medical attention injury rates are presented in figure 2. The overall medical attention injury incidence rate for police recruits ranged from 1.67 injuries per 1000 training days (Poisson 95% CI 1.00 to 2.34 injuries per 1000 training days) to 4.24 injuries per 1000 training days (Poisson 95% CI 2.97 to 5.51 injuries per 1000 training days). FBI recruits’ overall medical attention injury incidence rate was 4.59 injuries per 1000 training days (Poisson 95% CI 4.03 to 5.15 injuries per 1000 training days).
Figure 2.
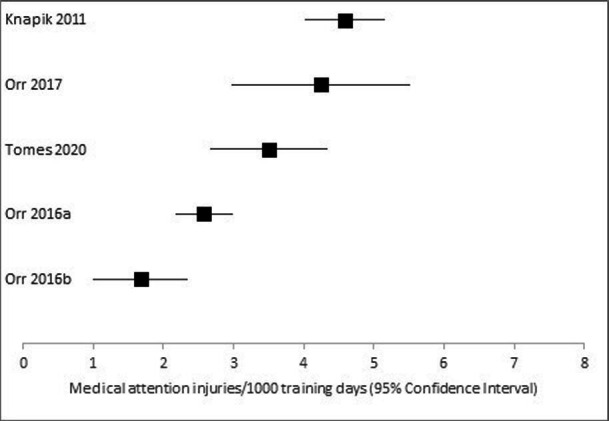
Overall medical attention injury incidence rates.
Injury incidence rates within Australian police recruits for injury regions were calculated as 0.21 abdomen, lower back, lumbar spine and pelvis injuries per 1000 training days (Poisson 95% CI 0.01 to 0.45 injuries per 1000 training days), 0.84 knee and lower leg injuries per 1000 training days (Poisson 95% CI 0.36 to 1.31 injuries per 1000 training days) and 0.42 ankle and foot injuries per 1000 training days (Poisson 95% CI 0.08 to 0.75 injuries per 1000 training days). The injury incidence rates within New Zealand police recruits for injury regions were calculated as 0.67 trunk and spine injuries per 1000 training days (Poisson 95% CI 0.31 to 1.03 injuries per 1000 training days), 1.34 upper limb injuries per 1000 training days (Poisson 95% CI 0.82 to 1.85 injuries per 1000 training days) and 1.44 lower limb injuries per 1000 training days (Poisson 95% CI 0.91 to 1.97 injuries per 1000 training days). The injury incidence rates for stress fractures in Israeli border police recruits were calculated as 2.22 stress fractures per 1000 training days (Poisson 95% CI 1.92 to 2.52 injuries per 1000 training days).
Injury severity and burden
One study in US police recruits reported that 18/401 (4.5%) recruits were discharged from the training programme due to injuries. No other studies reported on the severity or burden of injury.21
Assessment of quality in included studies
The overall quality for each study was assessed as low (table 3).1–3 18 19 21 24 25 Two studies were low quality for the sample frame as they were greater than 10 years old and unlikely to represent current populations.1 25 Two studies were assessed as unclear quality due to sample size. They did not report the number of participants who had injuries2 24 and three studies were assessed as low quality as they had fewer than 50 injured participants.3 19 21 All studies were judged as low quality for describing the subject and setting as no study presented participant age, height, weight, and the training programme.1–3 18 19 21 24 25 Statistical analysis was considered not applicable as we purely extracted injury numbers. The response rate was also considered not applicable as all studies used a database to collect prospective injury data and later sourced these medical records.
Table 3.
Quality of included studies
| Study | 1. Was the sample frame appropriate to address the target population? | 2. Were study participants sampled in an appropriate way? | 3. Was the sample size adequate? | 4. Were the study subjects and the setting described in detail? | 5. Was the data analysis conducted with sufficient coverage of the identified sample? | 6. Were valid methods used for the identification of the condition? | 7. Was the condition measured in a standard, reliable way for all participants? | 8. Was there appropriate statistical analysis? | 9. Was the response rate adequate, and if not, was the low response rate managed appropriately? | Overall judgement |
| Constantini et al 20101 | Low | High | High | Low | High | High | High | Not applicable | Not applicable | Low |
| Knapik et al 20112 | High | High | Unclear | Low | High | High | High | Not applicable | Not applicable | Low |
| Lockie et al 201921 | High | High | Low | Low | High | Unclear | High | Not applicable | Not applicable | Low |
| Orr et al 20163 | High | High | Low | Low | Unclear | High | High | Not applicable | Not applicable | Low |
| Orr et al 201618 | High | High | High | Low | Unclear | High | High | Not applicable | Not applicable | Low |
| Orr et al 201719 | High | High | Low | Low | Unclear | High | High | Not applicable | Not applicable | Low |
| Tomes et al 202024 | High | High | Unclear | Low | High | High | High | Not applicable | Not applicable | Low |
| Wang et al 200325 | Low | High | High | Low | High | High | High | Not applicable | Not applicable | Low |
Assessment of the certainty of the body of evidence
Injury incidence rates were based on data extracted from individual studies (number of injuries and the duration of the recruit training programme). However, the certainty of the injury incidence rates presented within this systematic review was judged to be very low, suggesting that the true injury incidence rate may be substantially different. The certainty of the evidence was downgraded as all studies were of low quality,1–3 18 19 21 24 25 indirectness (some studies did not appear representative of the target population, and all studies failed to present sufficient demographic and exposure data1–3 18 19 21 24 25 and inconsistency (the 95% CIs of the injury incidence rate, within figure 2, did not overlap in all studies).
Discussion
This systematic review identified eight studies that presented injury data within law enforcement officers. Unfortunately, we were unable to identify any studies which reported injury epidemiology within firefighter recruits, of the eight studies assessing injury epidemiology in law enforcement officers, seven defined injuries using a medical attention definition and one defined injury as career-ending. Therefore, this review provides insight into the epidemiology of medical attention and retirement injuries in law enforcement officers. However, we could not identify any studies reporting all injuries or time-loss injuries within law enforcement recruits.
All studies reported the number of overall injuries or the number of injured recruits; however, only two studies reported both. The lack of reporting the number of injuries and number of injured participants by 75% of studies limited the sample size to calculate injury frequency and injury proportion, decreasing confidence in the estimate. Only two studies, both in police officers, provided sufficient detail to report the injury incidence of the body region.18 24 One aim of injury monitoring is to identify the injuries which end up being the most significant26 as far as time-loss for the recruit, resource allocation for the organisation and being of the largest financial expense. However, only one study reported on the severity and burden of injury.21 Even more limiting is that this study did not provide the injury region or injury nature, limiting the design specificity of injury risk reduction programmes. All studies included within this review obtained injury reports retrospectively from the partner organisation database, which had collected data prospectively. While this design removes the influence of recall bias, typically seen within retrospective studies,27 it does mean that injury data provided is limited to that routinely collected by the organisation. This means the capacity to report various components of injury is not possible unless already collected by the organisation.
Injury prevention interventions for law enforcement officers would appear to require a programme targeting upper limb, spinal and lower limb injury given the distribution of injury regions. However, no studies have reported injury severity and injury burden. Further research into the injuries that are most costly to law enforcement officers, and their respective organisations is recommended prior to the development of prevention interventions. Thus, ensuring prevention interventions target those injuries associated with the largest injury burden.
The sparsity of data on injuries to firefighter recruits and data related to all injury and time-loss injury in law enforcement recruits was surprising given the number of recruits trained internationally and the financial burden associated with injured recruits. According to a 2014–15 Australian police report, the average cost to train a police recruit is $A84 000.28 Therefore, based on the data from Lockie et al,21 we extrapolated that the cost of 18/401 recruits leaving the programme due to injury would cost upwards of $A350 000/100 recruits commencing a training programme. Based on an annual report from one of eight Australian states or territories, 150 additional police recruits were to be recruited over the 2020–2021 calendar year29 that, based on the estimates above, could result in a financial loss of over half a million $A due to recruits leaving the programme due to injury.
In a sports injury setting, athletes are screened for injury risk factors. An injury risk reduction programme is implemented to eliminate these risk factors, subsequently reducing the burden of injuries.30 31 However, according to the Translating Research into Injury Prevention Practice framework, an important step in reducing injuries is by accurate injury epidemiology.26 Our review has identified that no studies have reported the injury epidemiology of firefighter recruits and that the certainty of the evidence detailing the injury epidemiology of law enforcement recruits is very low. Therefore, further investigation of the injury epidemiology within firefighter and law enforcement recruit populations is needed before developing meaningful injury risk reduction interventions.
Limitations
All studies included within this review reported injuries documented as medical records, which means that data are limited to what is reported to the employer (eg, the Police or FBI) during recruit training. We would suggest that for future injury epidemiology studies investigating law enforcement and firefighter recruits, data collection is planned prospectively and includes more detailed injury and exposure data (such as that suggested by Bahr et al for sports injury populations)12 but is also conscious of the burden of reporting on key stakeholders.32 This would involve reporting the mechanism of injury (eg, running or resistance training), further breaking down injuries into regions (such as the injury regions provided by the International Classification of Disease), reporting the type of injury (eg, tendon injury vs bone injury).12 We would also suggest future studies provide more in-depth analysis inclusive of other injury metrics such as injury severity and burden to inform which injuries result in the most time lost from recruit training.
As detailed within the methods, no studies provided a measure of training exposure (eg, the number of training hours was not reported), so it was assumed that 1 week of recruit training represented five training exposure days for calculating the injury incidence rate. Without an accurate measure of training exposure, the assumption that 1 week of training represented five training days may not be accurate. Additionally, when a study did not specify whether the injuries reported were based on the total number of injuries or the number of injured participants, to include within incident rate analysis, it was assumed they reported the number of injured participants. Future studies should consider including training exposure and more clarity about new vs subsequent/recurrent injuries to enable a more accurate calculation of incidence rates.
Conclusion
This review could not identify any studies reporting the injury epidemiology of firefighter recruits. This review was able to identify eight published studies that reported the injury epidemiology of law enforcement recruits. However, the studies were all of low quality, and the credibility of the evidence was assessed as very low. Seven studies reported medical attention injuries, and one study reported the number of medical withdrawals from a recruit training programme. The prevalence of police recruits with medical attention injuries ranged from 13.7% to 24.5%. The overall medical attention injury incidence rate for police recruits ranged from 1.67 injuries per 1000 training days (Poisson 95% CI 1.00 to 2.34 injuries per 1000 training days) to 4.24 injuries per 1000 training days (Poisson 95% CI 2.97 to 5.51 injuries per 1000 training days). No studies reported on the severity or burden of injuries.
Acknowledgments
MM has been supported by the Australian Governments Research Training Programme Scholarship. MM and NHH are partly supported by the Defence Science Centre (WA), within the Department of Defence, Science and Technology, on behalf of the Commonwealth of Australia. We would like to acknowledge Dr Lauren Fortington for her assistance in developing the systematic review protocol and manuscript.
Footnotes
Twitter: @myles_physio, @PatrickOwenPhD
Contributors: MCM conceived the idea. MCM, PJO, PC and NHH designed the methods. MCM. MN, H-AG and MN performed all screening and data extraction. MCM performed all analyses. MCM, H-AG, MN, PJO, PC and NHH contributed to developing the final manuscript.
Funding: Defence Science Centre Collaborative Research Grant funded by the Defence Science Centre (WA), within the Department of Defence, Science and Technology on behalf of the Commonwealth of Australia.
Disclaimer: The funder had no decision making in any aspect of the study design, execution, interpretation or decision for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.Constantini N, Finestone AS, Hod N, et al. Equipment modification is associated with fewer stress fractures in female Israel border police recruits. Mil Med 2010;175:799–804. 10.7205/MILMED-D-09-00253 [DOI] [PubMed] [Google Scholar]
- 2.Knapik JJ, Grier T, Spiess A, et al. Injury rates and injury risk factors among federal Bureau of investigation new agent trainees. BMC Public Health 2011;11:920. 10.1186/1471-2458-11-920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orr R, Pope R, Peterson S, et al. Leg power as an indicator of risk of injury or illness in police recruits. Int J Environ Res Public Health 2016;13:237. 10.3390/ijerph13020237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orr R, Simas V, Canetti E, et al. A profile of injuries sustained by firefighters: a critical review. Int J Environ Res Public Health 2019;16:3931. 10.3390/ijerph16203931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyons K, Radburn C, Orr R, et al. A profile of injuries sustained by law enforcement officers: a critical review. Int J Environ Res Public Health 2017;14:142. 10.3390/ijerph14020142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orr RM, Ferguson D, Schram B, et al. The relationship between aerobic test performance and injuries in police recruits. Int J Exerc Sci 2020;13:1052–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dechartres A, Trinquart L, Boutron I, et al. Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ 2013;346:f2304. 10.1136/bmj.f2304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kallings LV, Blom V, Ekblom B, et al. Workplace sitting is associated with self-reported general health and back/neck pain: a cross-sectional analysis in 44,978 employees. BMC Public Health 2021;21:875. 10.1186/s12889-021-10893-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knapik JJ, Graham B, Cobbs J, et al. A prospective investigation of injury incidence and injury risk factors among army recruits in military police training. BMC Musculoskelet Disord 2013;14:32. 10.1186/1471-2474-14-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma J, Greeves JP, Byers M, et al. Musculoskeletal injuries in British Army recruits: a prospective study of diagnosis-specific incidence and rehabilitation times. BMC Musculoskelet Disord 2015;16:106. 10.1186/s12891-015-0558-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortington LV, Hart NH. Models for understanding and preventing fractures in sport. In: Robertson GAJ, Maffuli N, eds. Fractures in sport: Springer nature, 2021: 75–84. [Google Scholar]
- 12.Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE extension for sport injury and illness surveillance (STROBE-SIIS)). Br J Sports Med 2020;54:372–89. 10.1136/bjsports-2019-101969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Travers MJ, Murphy MC, Debenham JR, et al. Should this systematic review and meta-analysis change my practice? Part 1: exploring treatment effect and trustworthiness. Br J Sports Med 2019;53:1488–92. 10.1136/bjsports-2018-099958 [DOI] [PubMed] [Google Scholar]
- 16.Travers MJ, Murphy MC, Debenham JR, et al. Should this systematic review and meta-analysis change my practice? Part 2: exploring the role of the comparator, diversity, risk of bias and confidence. Br J Sports Med 2019;53:1493–7. 10.1136/bjsports-2018-099959 [DOI] [PubMed] [Google Scholar]
- 17.Morrison A, Polisena J, Husereau D, et al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care 2012;28:138–44. 10.1017/S0266462312000086 [DOI] [PubMed] [Google Scholar]
- 18.Orr RM, Ford K, Stierli M. Implementation of an Ability-Based training program in police force recruits. J Strength Cond Res 2016;30:2781–7. 10.1519/JSC.0000000000000898 [DOI] [PubMed] [Google Scholar]
- 19.Orr R, Pope R, Stierli M, et al. Grip strength and its relationship to police recruit task performance and injury risk: a retrospective cohort study. Int J Environ Res Public Health 2017;14:941. 10.3390/ijerph14080941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lockie R, Balfany K, Bloodgood A, et al. The influence of physical fitness on reasons for Academy separation in law enforcement recruits. Int J Environ Res Public Health 2019;16:372. 10.3390/ijerph16030372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan RL, Thayer KA, Bero L, et al. GRADE: assessing the quality of evidence in environmental and occupational health. Environ Int 2016;92-93:611–6. 10.1016/j.envint.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.GRADE Working Group . Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. In: Schünemann H, Brożek J, Guyatt G, et al., eds, 2013. https://gradepro.org/ [Google Scholar]
- 24.Tomes C, Schram B, Pope R, et al. What is the impact of fitness on injury risk during police academy training? A retrospective cohort study. BMC Sports Sci Med Rehabil 2020;12:39. 10.1186/s13102-020-00188-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang X, Wang PS, Zhou W. Risk factors of military training-related injuries in recruits of Chinese People’s Armed Police Forces. Chinese J Traumatol = Zhonghua chuang shang za zhi 2003;6:12–17. [PubMed] [Google Scholar]
- 26.Finch C. A new framework for research leading to sports injury prevention. Journal of science and medicine in sport 2006;9(1-2):3-9; discussion 10. [DOI] [PubMed]
- 27.Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol 1990;43:87–91. 10.1016/0895-4356(90)90060-3 [DOI] [PubMed] [Google Scholar]
- 28.Kannis A. Questions on notice from 15 February 2016 hearing. In: Committee CDaJS, ed, 20168. Available: https://www.parliament.wa.gov.au/parliament/commit.nsf/($lookupRelatedDocsByID)/156EE2193819063948257F7E002917C3/$file/49175193.pdf
- 29.Western Australian Police Force . Annual report, 2020. Available: https://www.police.wa.gov.au/About-Us/Our-Agency/Annual-report
- 30.Crossley KM, Patterson BE, Culvenor AG, et al. Making football safer for women: a systematic review and meta-analysis of injury prevention programmes in 11 773 female football (soccer) players. Br J Sports Med 2020;54:1089–98. 10.1136/bjsports-2019-101587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murphy MC, Chivers P, Mahony K, et al. Risk factors for dominant‐shoulder injury in elite female Australian cricket players: a prospective study. Transl Sports Med 2020;3:404–14. 10.1002/tsm2.158 [DOI] [Google Scholar]
- 32.Murphy MC, Glasgow P, Mosler AB. Self-reported measures of training exposure: can we trust them, and how do we select them? Br J Sports Med 2021;55:891–2. 10.1136/bjsports-2021-104498 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2021-001289supp001.pdf (53.8KB, pdf)


