Summary
Background
In the current century, sleep apnoea has become a significant public health problem due to the obesity epidemic. To increase awareness, improve diagnostics, and improve treatment, Finland implemented a national sleep apnoea programme from 2002 to 2010. Here, we present changes in the societal burden caused by sleep apnoea from 1996 to 2018.
Methods
National register data were collected from the Care Register for Health Care, Statistics Finland, the Social Insurance Institution of Finland, and the Finnish Centre for Pensions. Disease prevalence, use of healthcare and social services, and societal costs were estimated.
Findings
The number of sleep apnoea patients increased in secondary care from 8 600 in 1996 to 61 000 in 2018. There was a continuous increase in outpatient visits in secondary care from 9 700 in 1996 to 122 000 in 2018 (1 160%) and in primary care from 10 000 in 2015 to 29 000 in 2018 (190%). Accordingly, the cumulative annual number of days off work for sleep apnoea increased from 1 100 to 46 000. However, disability pensions for sleep apnoea decreased from 820 to 550 (33%) during the observation period. Societal costs per patient decreased over 50% during the observation period (€2 800 to €1 200).
Interpretation
The number of sleep apnoea patients in Finland increased remarkably during the observation period. To control this burden, diagnostic methods and treatment were revised and follow up was reorganised. Consequently, there was a significant decrease in societal costs per patient. The decrease in disability pensions suggests earlier diagnosis and improved treatment. The national sleep apnoea programme was one of the initiators for these improved outcomes.
Funding
The Finnish Institute for Health and Welfare and the Hospital District of Helsinki and Uusimaa (HUH), Helsinki, Finland.
Keywords: Sleep apnoea, Obesity, Public health, Respiratory programme
Research in Context.
Evidence before this study
We searched PubMed for studies about optimising diagnostics, treatment methods, and follow up of sleep apnoea until May 2021. Additionally, we searched data on health economics associated with sleep apnoea diagnostics and initiation and follow up of treatment to compare our results and the Finnish treatment model with other countries. We found data on increased cost effectiveness with no negative effects on treatment results about diagnosing sleep apnoea and starting auto-CPAP treatment at home.
Added value of this study
We present comprehensive register data on the burden caused by sleep apnoea in Finland during last 22 years. We show that the increased prevalence of sleep apnoea can be controlled by increasing the efficiency of diagnostic and treatment pathways, which subsequently results in control of costs.
Implications of all the available evidence
Limited data were available on the effects of using telemedicine or other reduced outpatient treatment. Data about follow-up models in sleep apnoea on individual treatment results and population-level cost effectiveness were scarce. Comparing data between hospitals in a Nordic country was somewhat difficult, as treatment pathways may vary by hospital and year. Comparing data between countries is not possible as registers and insurance systems vary. The high prevalence of obesity remains a public health problem.
Alt-text: Unlabelled box
Introduction
The prevalence rate of symptomatic sleep apnoea in adults in high income countries is estimated to be as high as 17%. Risk factors include male sex, overweight, and age >50 years. Multiple comorbidities (such as cardiovascular diseases and diseases associated with obesity), impaired quality of life, and early death are associated especially with severe untreated sleep apnoea.1, 2, 3, 4
At least 70% of sleep apnoea patients are obese.2, 3, 4 Significant global lifestyle and environmental changes during the last 100 years have increased risk factors for weight gain5. In Finland, 11.7% of men and 18.2% of women were obese in 1980; the corresponding values were 26.1% and 27.5% in 2017.6,7
General awareness of sleep apnoea is low.4,8 Various global campaigns have increased awareness about sleep apnoea among the general public and professionals.9,10 The Finnish national sleep apnoea programme (2002-2010) is an example of these campaigns. The goals for the Finnish programme included reducing the percentage of patients with severe sleep apnoea, maintaining work capacity and functional capacity of sleep apnoea patients, and improving cost effectiveness of prevention and treatment of sleep apnoea.9
To standardise the diagnostics and treatment of sleep apnoea, various national and international guidelines have been published over recent decades,2, 3, 4 with no remarkable changes during the last 20 years. Continuous positive airway pressure (CPAP) therapy has been considered the gold standard treatment for decades.2,4,11, 12, 13, 14 Other current alternative treatment methods include other PAP therapies (past 20-30 years) and oral appliances for mild-to-moderate sleep apnoea (past 15 years) in addition to lifestyle changes.2, 3, 4,12, 13, 14 In the 1990s, operative treatment of the pharynx, including methods such as uvulo-pharyngo-plasty (UPP) and uvulo-palato-pharyngo-plasty (UPPP), was used for treating sleep apnoea. However, subsequent studies have shown that these operations treated snoring rather than apnoeas.12
The pathway for diagnosing and treating sleep apnoea has become more efficient in Finland in the past 20 years; inpatient diagnostics and treatment in secondary care has become increasingly outpatient based.9,14 In this descriptive article, we first describe the burden of sleep apnoea from 1996 to 2018 in Finland from the societal perspective, followed by the change in the burden of sleep apnoea from the perspective of outpatient clinics of respiratory diseases in the two largest university hospitals in Finland. In addition, we describe the responses of health care to control the increasing prevalence of sleep apnoea.
Materials and methods
The Finnish health care system is described in supplementary material 1.
Study population
This study includes two separate cohorts. One cohort consists of all Finns who used public health services between January 1, 1996 to December 31, 2018. Data from their health service use and social benefits were collected from the registers of the Finnish Centre for Pensions, Social Insurance Institution of Finland (SII), and Care Register for Health Care.15, 16, 17 The population of Finland was in 5.1 million in 1996 and 5.5 million in 2018.
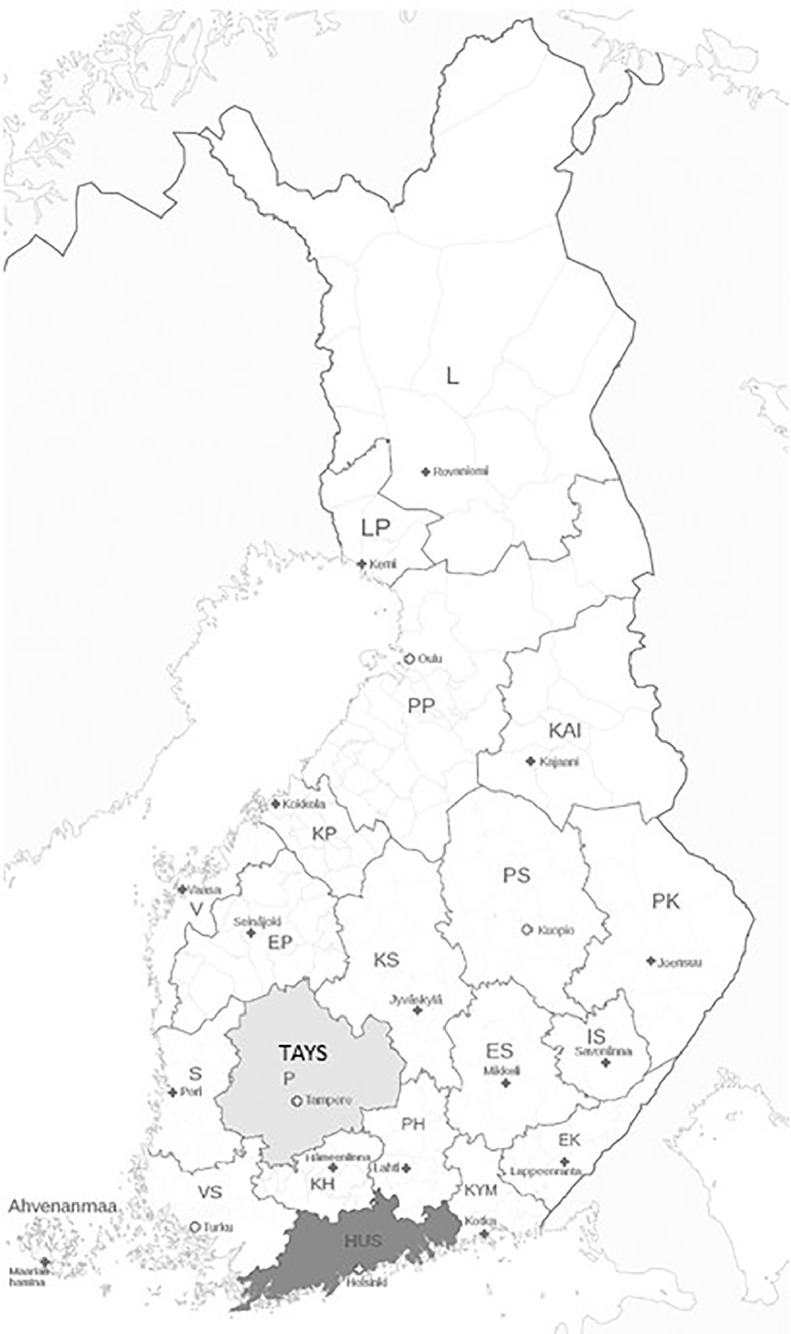
The other cohort includes subjects who were treated in secondary care outpatient clinics of respiratory diseases in the areas of the Tampere University Hospital (TAYS) or Helsinki University Hospital (HUH) from January 1, 2010 to December 31, 2019. The population of the TAYS catchment area was 409 454 inhabitants on December 31, 2010 and 436 392 inhabitants on December 31, 2019; the corresponding values for HUH were 1 528 279 and 1 685 983, respectively (Picture 1). This total population of 2 122 375 subjects was 38.4% of the Finnish population in 2019.18
Picture 1.
A map of Finland and the districts of Tampere University Hospital (TAYS) and Helsinki University Hospital (HUH).
Study design
We report the annual change in the burden of sleep apnoea according to national register data from January 1, 1996 to December 31, 2018. We also report the annual change in the burden caused by sleep apnoea in secondary-care outpatient clinics of respiratory diseases in TAYS and HUH from January 1, 2010 or 2012 to December 31, 2019 per population of 100 000 inhabitants for each year.
Data
Finnish public health care and social security system have comprehensive and obligatory registers maintained by national authorities, including systematically collected register data from all persons who have used these services. The following data were used for the nationwide cohort: Finnish Centre for Pensions, new disability pensions due to sleep apnoea15; SII, sick-leave days directly due to sleep apnoea16; and Care Register for Health Care, use of public inpatient and outpatient services with separate data from primary and secondary care (inpatient services as number of inpatient days and outpatient services as numbers of visits).17 Only events with sleep apnoea as the primary diagnosis were included.
For the hospital cohort, data were applied separately from the hospital discharge registers in the areas of TAYS and HUH. In both areas, the need for sleep apnoea treatment is assessed and treatment is initiated in secondary care. The criteria to initiate CPAP treatment for diagnosed sleep apnoea remained the same during the follow-up period.
HUH includes seven separate hospital areas. For outpatient visits, data were included for each year from the hospitals where statistics were available and where CPAP was initiated for sleep apnoea during a doctor's appointment (i.e. not by phone or in groups) (2010-2011 Helsinki, Lohja; 2012 Helsinki, Jorvi, Lohja; 2013-2016 Helsinki, Jorvi, Peijas; 2017 Helsinki, Hyvinkää, Jorvi, Peijas; 2018 Helsinki, Hyvinkää, Jorvi, Peijas, Raasepori; 2019 Helsinki, Jorvi). Statistics for the initiation of a new CPAP treatment were available from the areas of Helsinki and Hyvinkää.
Classification of diseases
Data were searched using the International Classification of Diseases 10 (ICD-10) code of sleep apnoea (G47.3).
Analysis methods
As most of the decisions for treating sleep apnoea are made in secondary care in Finland, the annual prevalence of sleep apnoea was estimated according to the records in the Care Register for Health Care for secondary care.
Yearly inpatient service use was accessible for the entire observation period from the Care Register for Health Care for primary and secondary care.
Data were available from 1998 for outpatient visits in secondary care. For the preceding 2 years, the number of outpatient visits were extrapolated according to the annual prevalence for each year with missing data and the average number of visits per patient observed in the following years. For primary care, the number of outpatient visits was available only from 2015. Due to the short time series of primary care visits, we did not attempt to extrapolate the missing years.
Indirect costs were estimated from disability pensions and sick leaves in which sleep apnoea was indicated as the reason for pension or sick leave. Indirect costs were reported as lost productivity by using the human capital method. The number of disability pensions and sick-leave days were converted to lost years of productivity. The cost of 1 year of lost productivity was assessed according to Kapiainen et al19 and adjusted for each year according to the index of wage and salary earnings from Statistics Finland.18
Direct (out- and inpatient care in primary and secondary care) and indirect costs (lost productivity from sick leaves and disability pensions) were calculated according to the service use and unit costs for each service for estimating the yearly burden. The follow-up results for the 22-year observation period are presented in an annual time series.
All costs are converted into 2018 prices by using Statistics Finland's consumer price index.18 See supplementary material 2 for a more detailed description of the cost estimation.
The burden of sleep apnoea in TAYS and HUH is visualised in the annual number of initiated new CPAP treatments and first visits for sleep apnoea, for non-sleep apnoea, and for any respiratory disease in outpatient clinics of respiratory diseases. All numbers are expressed per 100 000 inhabitants. Population was counted separately for each year according to each year's catchment area (described above).18
Ethical aspects
The data were based on national statistical register data or hospital discharge register data without any personal identifiers. Therefore, this study does not fall under the purview of laws regarding medical research.
Role of the funding source
The Finnish Institute for Health and Welfare funded the data collection. Financial support for manuscript writing was provided by the Hospital District of Helsinki and Uusimaa (corresponding author TM). Otherwise, study design and execution and manuscript writing were part of the authors’ regular duties.
Results
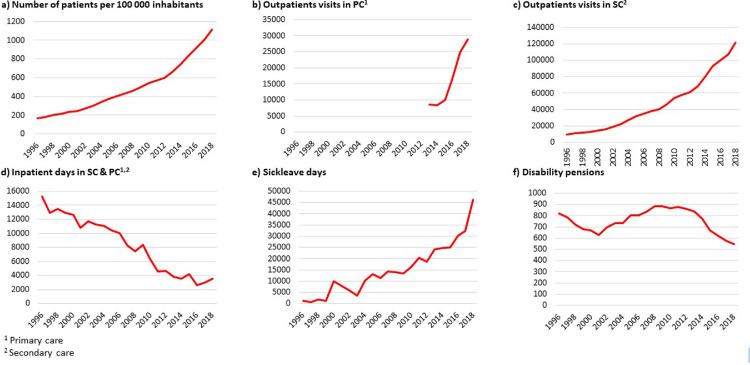
The annual number of patients treated for sleep apnoea as their first diagnosis in secondary care increased from 8 600 in 1996 to 61 000 in 2018 (610% increase) in Finland. There was a constant increase in outpatient visits in secondary care from 9 700 to 122 000 (1 160%); outpatient visits in primary care increased from 10 000 in 2015 to 29 000 in 2018 (190%). The number of inpatient days decreased from 15 000 in 1996 to 3 500 in 2018 (77%). The share of primary care inpatient days out of total inpatient days was approximately 5% during the observation period. During the 23-year follow-up period, the number of sick-leave days increased from 1 100 to 46 000 (4 100%) while disability pensions decreased slightly from 820 to 550 (33%) (Figure 1a-1f). See supplementary material 2 for full data.
Figure 1.
The total number of sleep apnoea patients, outpatient visits in primary and secondary care, hospital (inpatient) days in secondary and primary care, sick-leave days, and disability pensions during the observation period (1996 to 2018).
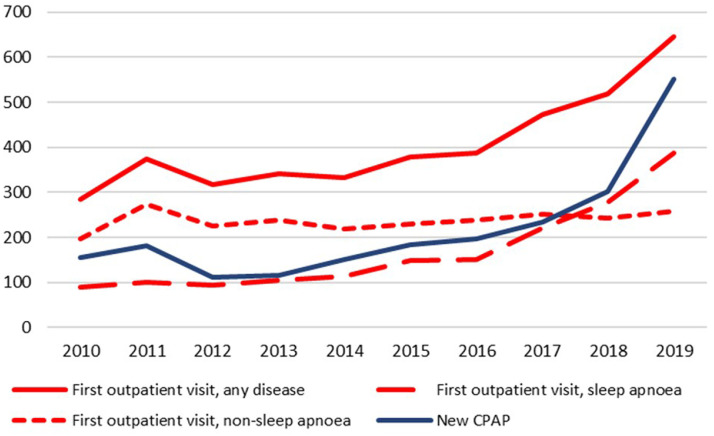
During the 10-year period from 2010 to 2019, outpatient visits for all respiratory conditions in the outpatient units of TAYS and HUH respiratory clinics increased from 285 to 645 per 100 000 inhabitants (227%). At the same time, the number of new patients with sleep apnoea increased from 89 to 388 per 100 000 inhabitants (439%). The share of sleep apnoea visits of all respiratory visits increased from 31% to 60%, explaining 83% of the increase in new patients.
The number of new CPAP treatments increased in the Tampere, Helsinki, and Hyvinkää Hospital areas from 156 to 551 per 100 000 inhabitants (353%) from 2010 to 2019 (Figure 2).
Figure 2.
Change in the burden of sleep apnoea from 2010 to 2019 in the outpatient clinics of respiratory diseases in TAYS and HUH and number of initiated new CPAP treatments in TAYS, Helsinki, and Hyvinkää. All numbers are per 100 000 inhabitants.
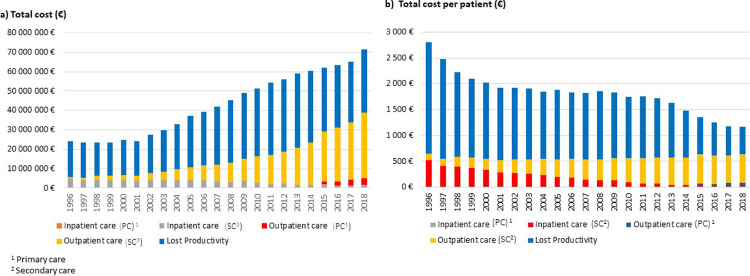
The total costs for sleep apnoea increased from €24 million in 1996 to €72 million (200%) (€68 million [180%] without primary care outpatient visits) in 2018 (Figure 3a). The cost per patient decreased from €2 800 to €1 200 (57%) (€1 100 [61%] without primary care outpatient visits) (Figure 3b). See supplementary material 2 for full cost data.
Figure 3.
a-b. a) Total direct healthcare and indirect disability/lost productivity costs for sleep apnoea during the 23-year period from 1996 to 2018. b) Per patient costs.
Discussion
The sleep apnoea programme (2002-2010)9 and general changes in the Finnish society increased the awareness of sleep apnoea in the present century. Currently, the prevalence of sleep apnoea is increasing in Finland. However, we showed in this descriptive article that changes in diagnostic methods, treatment initiation, and follow up from inpatient-based to outpatient-based treatment have helped control the total burden in Finland. In addition, the cost per treated patient has decreased over 50% in Finland.
Sleep apnoea is a significant public health problem.1,3 Although the Finnish prevalence of obstructive sleep apnoea is not known, it has been estimated that up to 1.5 million people aged 30-69 years would have an apnoea hypopnea index (AHI) ≥5/h (mild increase) and 854 000 people have AHI ≥15 (mid increase) (50.4% and 29.5% of the Finnish population aged 30-69 years, respectively).20 However, in addition to AHI ≥5/h, the diagnosis of obstructive sleep apnoea syndrome requires symptoms of sleep apnoea. Therefore, AHI values are not considered as clinically relevant. During the follow-up period, there was a large increase in the proportion of patients with new sleep apnoea (increases of 610% at the national level and 439% in the two observed hospital district areas).
During our follow-up period, general awareness of sleep apnoea has increased with the support of various educational efforts, such as the Finnish sleep apnoea programme in 2002-2012.9 The national programme sought to promote prevention, treatment, and rehabilitation of sleep apnoea. The goals included decreasing incidence, maintaining work and functional capacity, ensuring recovery of most sleep apnoea patients, reducing severe sleep apnoea, decreasing hospitalisations for sleep apnoea, and improving the cost effectiveness of prevention and treatment. The means for achieving these goals included obesity prevention, early diagnosis and active treatment, enhancing knowledge about risk factors and treatment, encouraging scientific research, and recommending a greater role for primary health care in prevention and treatment.9 Most of these goals have been realised, except for decreasing sleep apnoea incidence and obesity prevention.
The increase in the prevalence of sleep apnoea is exceptional when compared with other respiratory public health problems. The prevalence of asthma in adults (10% in 2006 and 10.9% in 2016)21 and the prevalence of COPD is stable in Finland.22 National population surveys show similar results for asthma and COPD.7 In addition, sleep apnoea has currently been widely addressed in Finnish media after the death of a famous Finnish singer in February 2019 who was known to have sleep apnoea.23 and since, a sudden increase in the amount of referrals from primary care to secondary health care sleep policlinics was observed in 2019.
CPAP is the gold standard treatment for sleep apnoea.2, 3, 4,13 In our data, there was a continuous increase in the number of initiated new CPAP treatments. Auto-titrating CPAP (auto-CPAP) provides an alternative to traditional fixed-pressure CPAP with no significant differences in efficacy.3,13,24 In Finland, auto-CPAP devices currently are typically chosen as the first line of treatment. Instructions are provided by health care professionals and treatment is then started at home. This reduces costs and has no difference in efficacy compared to classical CPAP initiated in the ward.24 Selected patients may need other PAP treatments, which are mainly initiated in the ward.2, 3, 4,13
During the last 15 years, oral appliances have been shown to be a useful alternative to CPAP for mildly or moderately overweight patients with mild-to-moderate obstructive sleep apnoea and for those with severe disease refractory to CPAP.4,25 We did not have data on oral appliances. In addition, lifestyle modifications, including weight loss and increased physical activity, are an important part of treatment for every sleep apnoea patient.2, 3, 4,13 In addition, surgical treatments for sleep apnoea have changed from larynx surgery to bariatric surgery that treats obesity.2, 3, 4,12,25, 26, 27
During last decades Finland has used practical methods in the diagnostics of sleep apnoea. Over the last 15 years, manually scored portable devices (overnight polygraphies or polysomnographies) that capture (at minimum) nasal airflow, respiratory movements, and pulse oximetry during one night of sleep have been used as a primary tool in diagnosing sleep apnoea, in addition to clinical history and clinical examination.4,14 Examinations are currently performed predominantly ambulatory at home, which is reliable and save costs compared to polysomnography performed at the ward.3
To control the current increasing prevalence of sleep apnoea with increased number of patients, the Finnish health care system has also adopted other more efficient services and treatment pathways for both the patient and the health care system. According to our data, the total costs have been controlled and disability pensions for sleep apnoea have decreased, indicating improved treatment and earlier diagnosis.
During the last 10 years, diagnosing sleep apnoea at home by primary care and starting CPAP treatment at home by secondary care have saved resources in secondary care.3,4,9,14 Lifestyle modifications and treatment of comorbidities occur mostly in primary care; only the most difficult diseases are treated in secondary care, such as bariatric surgery in obesity.26 The prices of CPAP devices have decreased because of the mandatory bidding process in the public health care system. Treatment of sleep apnoea is almost free of charge for all residents in Finland and the health care system provides all consumables and new CPAP devices as required. As there are more patients living a long time with CPAP treatment, the decrease in device prices does not lead to a decrease in the total cost of sleep apnoea treatment.
The role of a traditional doctor's appointment is currently minimal. Remote video appointments or phone calls before starting CPAP treatment are used in many hospitals. Information on sleep apnoea is provided and CPAP treatment is started in groups in some hospitals (oral statement, Dr Hanna Tapanainen Hyvinkää Hospital, Adel Bachour HUH, Hannele Hasala TAYS). In some parts of Finland, the private sector participates in the CPAP initiation process under select conditions (service vouchers for patients from the public sector; oral statement, Adel Bachour HUH). Additionally, digitalisation has played an important role in the change of treatment pathways in recent years. Telehealth options can replace or supplement some or all steps in the evaluation, testing, treatment, management, and follow up of sleep apnoea, potentially saving time and reducing costs.28 Additionally, digital services, such as weight control groups on the internet and digital coaching for weight management are beneficial for sleep apnoea patients.
During follow up, we observed an increase in sick-leave days from around 1 000 to 46 000 (3 980%). We assume this is associated with the changes in European and national guidelines in driving permissions. According to current tightened instructions (the latest update was in 2018) professional drivers (such as bus or truck drivers) are not allowed to drive with untreated sleep apnoea and are on sick leave until sleep apnoea is shown to be treated.29 At the same time, the amount of decreased disability pensions can be explained by the fact that sleep apnoea is a treatable disease and when treated it does not lead to disability pensions.3,4
One part of the treatment and costs is adherence and follow up. During the past 20 years, various initiatives, such as behavioural interventions, patient coaching, and device development have advanced. However, long-term CPAP adherence has not improved over the last 20 years and remains a problem.11 CPAP adherence in Finland is approximately 57% to 67%.30,31 Traditionally, CPAP treatment was followed regularly according to local practices by nurses or doctors in secondary or primary care in Finland. In recent years, routine follow up is performed increasingly via remote access by nurses according to local practice. There is no international consensus on how to organize CPAP follow up. Initial compliance at day 12 and at 6 months predicts future adherence and possible treatment abandonment as well as 5-year follow up.32 On the other hand, a third of patients with routine appointments contact health care professionals between the routine appointments.33 It is generally assumed in Finland that CPAP follow up should be intensified during the first year of CPAP therapy. However, when CPAP treatment is successful after 1 year,32 it remains unclear if routine follow up is necessary or if on-demand follow-up visits are a suitable alternative for those who need it. Both in Finland and abroad there are examples of how the follow up of CPAP treatment is organised successfully in primary care.34,35 For problematic cases, such as occupational drivers and other special groups, the follow up of CPAP treatment is organised in secondary care.4
Our cohorts were comprehensive and included mostly or exclusively Finnish subjects. However, weaknesses that are generally associated with register data were also weaknesses in our data. As there was no control population, it was not possible to demonstrate causality. The outcomes observed over the follow-up period may have occurred without any programme. However, a corresponding national approach has been shown to be effective in addressing other public health problems, such as the national asthma programme (1994-2004; resulting in a reduction in severe asthma and overall costs) and the diabetes prevention programme (2000-2010) in type 2 diabetes (resulting in increased awareness of diabetes).36,37 It is likely that changes in compiling statistics in registers and treatment methods affected the results. Some indicators for evaluating the health care system, such as waiting time from diagnosis to treatment, were not possible to define.
Using the human capital method to estimate indirect costs overestimates the true cost to society, since absent employees can be replaced when there is unemployment in the economy. However, the friction-cost method, which would take this into consideration, is also problematic as it is difficult to estimate the time it takes to replace the absent employee. The friction-cost method also does not consider the costs to society from sick-leave reimbursements and disability pensions, which last the whole duration of the absence from work.
Finally, there are probably some differences between hospitals in treating sleep apnoea and in the criteria for initiating CPAP treatment. However, as the last Finnish national guideline for sleep apnoea was published in 2017, most Finnish hospitals and doctors likely followed this guideline.4
Conclusion
In this descriptive article, we described the Finnish experience in diagnosing and treating sleep apnoea. In spite of the six-fold increase in the number of sleep apnoea patients, Finland has managed the increasing costs mainly by using practical diagnostic methods, reducing inpatient visits, shifting possible work from doctors to nurses and technicians, buying sleep apnoea materials according to local regulations (yielding cost savings but insuring quality), and by abolishing routine follow-up visits (in non-professional driving group) when CPAP therapy is successful after 1 year of follow up. These measures allowed our sleep apnoea patients to continue to benefit from public health insurance without restricting access criteria.
Contributors
FH, R-LL, TM, and HH collected and analysed most of the data. TM outlined the first version of the manuscript. All authors interpreted the data, contributed to the writing process, and read and agreed to the published version of the manuscript.
Declaration of interests
The corresponding author Tiina Mattila performed this study with financial support from the Hospital District of Helsinki and Uusimaa. All other co-authors conducted the work related to this study as part of their regular duties. Sanna Toppila-Salmi has got grants (GSK) and consultancy fees (ALK Abello, AstraZeneca, ERT, Novartis, Sanofi Pharma, Roche Products) outside of this work. Tari Haahtela has got lecture fees (GSK, Mundipharma, Orion Pharma, Sanofi) outside of this work. The corresponding author and the other authors do not have any relevant conflicts of interest.
Acknowledgments
Acknowledgments
The Finnish Institute for Health and Welfare funded collection of the data. Financial support from the Hospital District of Helsinki and Uusimaa awarded to the first author allowed data analysis and preparation of the manuscript. Additionally, we acknowledge chief doctor Hanna Tapanainen from Hyvinkää Hospital for CPAP data from Hyvinkää Hospital.
Data sharing statement
The data analysed in this study are not directly available to others. Anybody may apply for a study permit and access to the data from the appropriate registers from Findata and from the relevant hospital districts. Other related documents, including memos and plans for this study (mainly in Finnish), will be available 2 years after publication for researchers upon reasonable request (tiina.m.mattila@hus.fi).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100338.
Appendix. Supplementary materials
References
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2019;15(2):335–343. doi: 10.5664/jcsm.7640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel SR. Obstructive Sleep Apnea. Ann Intern Med. 2019;171(11):ITC81–ITC96. doi: 10.7326/AITC201912030. [DOI] [PubMed] [Google Scholar]
- 4.A working committee of Finnish Medical Society Duodecim, Finnish Society for Respiratory specialists and Finnish Sleep Research Society. Finnish practical guideline for Sleep apnoea (in Finnish). 2021. www.kaypahoito.fi.
- 5.Williams EP, Mesidor M, Winters K, Dubbert PM, Wyatt SB. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr Obes Rep. 2015 Sep;4(3):363–370. doi: 10.1007/s13679-015-0169-4. [DOI] [PubMed] [Google Scholar]
- 6.Aromaa A, Heliovaara M, Impivaara O, Maatela J, Joukamaa M, Klaukka T, et al. Health, functional limitations and need for care in Finland. Basic results from the Mini-Finland Health Survey (in Finnish with English Summary). Publications of the Social Insurance Institution 1989. Helsinki and Turku, Finland. Available at: http://hdl.handle.net/10138/162843. Date last accessed October 25, 2020.
- 7.Koponen P BK Lundqvist A, Sääksjärvi K, Koskinen S. National FinHealth survey - Terveys, toimintakyky ja hyvinvointi Suomessa - FinTerveys 2017-tutkimus (in Finnish, part of report in English). 4/2018. National Institute for health and welfare, Helsinki, Finland. https://www.thl.fi/en/web/thlfi-en/research-and-expertwork/population-studies/national-finhealth-study). Date last accessed September 24, 2021.
- 8.Sia CH, Hong Y, Tan LWL, van Dam RM, Lee CH, Tan A. Awareness and knowledge of obstructive sleep apnea among the general population. Sleep Med. 2017;36:10–17. doi: 10.1016/j.sleep.2017.03.030. [DOI] [PubMed] [Google Scholar]
- 9.Ministry of Social Affairs and Health . Vol. 4. Publications of Ministry of Social Affairs and Health; 2002. https://www.filha.fi/wp-content/uploads/2019/05/Valtakunnallinen-uniapneaohjelma-2002-2012.pdf (National programme for Sleep Apnoea 2002-2012 (in Finnish, absract in English)). Date last accessed September 20, 2021. [Google Scholar]
- 10.World sleep day. Available from: https://worldsleepday.org/. Date last accessed May 20, 2021
- 11.Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45(1):43. doi: 10.1186/s40463-016-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spicuzza L, Caruso D, Di Maria G. Therapeutic Advances in Chronic Disease. Ther Adv Chronic Dis. 2015;6(5):273–285. doi: 10.1177/2040622315590318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2019;15(2):301–334. doi: 10.5664/jcsm.7638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obstructive Sleep Apnoea Syndrome . Report of a joint Nordic Project. Elanders Infologistics Väst AB; Mölnlycke: 2007. A systematic Review 2007. [Google Scholar]
- 15.Finnish Centre for Pensions. https://www.etk.fi/en/. Date last accessed September 20, 2020
- 16.Social Insurance Institution of Finland, statistics. https://www.kela.fi/. Date last accessed May 20, 2020.
- 17.Care Register for Health Care (HILMO). National Institute for Health and Welfare, Helsinki, Finland. https://www.thl.fi/en/web/thlfi-en/statistics/data-collection. In Finnish: https://www.thl.fi/fi/tilastot/tiedonkeruut/hoitoilmoitusjarjestelma-hilmo. Date last accessed May 15, 2021.
- 18.Statistics Finland, statistics. Available from: https://www.stat.fi/. Date last accessed September 20, 2020.
- 19.Kapiainen S, Väisänen A, Haula T. Terveyden- ja sosiaalihuollon yksikkökustannukset Suomessa vuonna 2011 (Unit costs in social services and healthcare in Finland 2011) Terveyden ja hyvinvoinnin laitos (National Institute for Health and Welfare) 2014;3 [Google Scholar]
- 20.Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respiratory Med. 2019 Aug;7(8):687–698. doi: 10.1016/S2213-2600(19)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hisinger-Mölkänen H, Pallasaho P, Haahtela T, Lindqvist A, Sovijärvi A, Piirilä P. The increase of asthma prevalence has levelled off and symptoms decreased in adults during 20 years from 1996 to 2016 in Helsinki, Finland. Respir Med. 2019;155:121–126. doi: 10.1016/j.rmed.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 22.Vasankari TM, Impivaara O, Heliovaara M, Heistaro S, Liippo K, Puukka P, et al. No increase in the prevalence of COPD in two decades. Eur Respir J. 2010;36(4):766–773. doi: 10.1183/09031936.00178109. [DOI] [PubMed] [Google Scholar]
- 23.Keränen T. Respiratory outpatient clinics are crowded for new sleep apnoea patients (in Finnish) Finnish Med J. 2020;75(1–2):24. [Google Scholar]
- 24.Ayas NT, Patel SR, Malhotra A, Schulzer M, Malhotra M, Jung D, et al. Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep. 2004;27(2):249–253. doi: 10.1093/sleep/27.2.249. [DOI] [PubMed] [Google Scholar]
- 25.Prinsell JR. Maxillomandibular advancement surgery for obstructive sleep apnea syndrome. J Am Dent Assoc. 2002;133(11) doi: 10.14219/jada.archive.2002.0079. 1489–40. [DOI] [PubMed] [Google Scholar]
- 26.Peromaa-Haavisto P, Tuomilehto H, Kossi J, Virtanen J, Luostarinen M, Pihlajamaki J, et al. Obstructive sleep apnea: the effect of bariatric surgery after 12 months. A prospective multicenter trial. Sleep Med. 2017;35:85–90. doi: 10.1016/j.sleep.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 27.Ashrafian H, Toma T, Rowland SP, Harling L, Tan A, Efthimiou E, et al. Bariatric Surgery or Non-Surgical Weight Loss for Obstructive Sleep Apnoea? A Systematic Review and Comparison of Meta-analyses. Obes Surg. 2015 Jul;25(7):1239–1250. doi: 10.1007/s11695-014-1533-2. [DOI] [PubMed] [Google Scholar]
- 28.Schutte-Rodin S. Telehealth, telemedicine, and obstructive sleep apnea. Sleep Med Clin. 2020;15(3):359–375. doi: 10.1016/j.jsmc.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Intructions for driving health for doctors (in Finnish or Swedish). Traficom, Finland. https://www.traficom.fi/sites/default/files/media/regulation/Ajoterveyden%20arviointiohjeet%20laakareille.pdf. Date last accessed December 15, 2021.
- 30.Avellan-Hietanen H, Maasilta P, Bachour A. Restarting CPAP therapy for sleep apnea after a previous failure. Respir Care. 2020;65(10):1541–1546. doi: 10.4187/respcare.07766. [DOI] [PubMed] [Google Scholar]
- 31.Kreivi H-R, Maasilta P, Bachour A. Persistence of upper-airway symptoms during CPAP compromises adherence at 1 year. Respir Care. 2016;61(5):652–657. doi: 10.4187/respcare.04113. [DOI] [PubMed] [Google Scholar]
- 32.van Zeller M, Severo M, Santos AC, Drummond M. 5-Years APAP adherence in OSA patients – do first impressions matter? Respir Med. 2013;107(12):2046–2052. doi: 10.1016/j.rmed.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 33.Avellan-Hietanen H, Brander P, Bachour A. Symptoms during CPAP therapy are the major reason for contacting the sleep unit between two routine contacts. J Clin Sleep Med. 2019;15(1):47–53. doi: 10.5664/jcsm.7568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brander P, Lehto J, Kunnas-Vaikkinen V, Kamarainen J, Vetelasuo U, Pietinalho A. Uniapnean CPAP-hoidon seuranta terveyskeskuksessa (in Finnish) Finn Med J. 2015;9:563–568. [Google Scholar]
- 35.Sanchez-de-la-Torre M, Nadal N, Cortijo A, Masa JF, Duran-Cantolla J, Valls J, et al. Role of primary care in the follow-up of patients with obstructive sleep apnoea undergoing CPAP treatment: a randomised controlled trial. Thorax. 2015;70(4):346–352. doi: 10.1136/thoraxjnl-2014-206287. [DOI] [PubMed] [Google Scholar]
- 36.Wikström K, Lindström J, Tuomilehto J, Saaristo TE, Helakorpi S, Korpi-Hyövälti E, et al. National diabetes prevention program (DEHKO): awareness and self-reported lifestyle changes in Finnish middle-aged population. Public Health. 2015 Mar;129(3):210–217. doi: 10.1016/j.puhe.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 37.Haahtela T, Tuomisto LE, Pietinalho A, Klaukka T, Erhola M, Kaila M, et al. A 10 year asthma programme in Finland: major change for the better. Thorax. 2006;61(8):663–670. doi: 10.1136/thx.2005.055699. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.