Abstract
Since the eradication of polio in most parts of the world, Guillain-Barré syndrome (GBS) has become the most common cause of acute flaccid paralysis. GBS is an autoimmune disorder of the peripheral nervous system characterized by weakness, usually symmetrical, evolving over a period of several days or more. Since laboratories began to isolate Campylobacter species from stool specimens some 20 years ago, there have been many reports of GBS following Campylobacter infection. Only during the past few years has strong evidence supporting this association developed. Campylobacter infection is now known as the single most identifiable antecedent infection associated with the development of GBS. Campylobacter is thought to cause this autoimmune disease through a mechanism called molecular mimicry, whereby Campylobacter contains ganglioside-like epitopes in the lipopolysaccharide moiety that elicit autoantibodies reacting with peripheral nerve targets. Campylobacter is associated with several pathologic forms of GBS, including the demyelinating (acute inflammatory demyelinating polyneuropathy) and axonal (acute motor axonal neuropathy) forms. Different strains of Campylobacter as well as host factors likely play an important role in determining who develops GBS as well as the nerve targets for the host immune attack of peripheral nerves. The purpose of this review is to summarize our current knowledge about the clinical, epidemiological, pathogenetic, and laboratory aspects of campylobacter-associated GBS.
Over the past 2 decades, our understanding of the role of Campylobacter jejuni subsp. jejuni (referred to simply as C. jejuni in this review) as well as other Campylobacter species in causing human infection has greatly increased. We now know that C. jejuni is the most common cause of bacterial gastroenteritis in the United States, surpassing Salmonella in most studies. It is estimated that over 2.5 million cases occur each year in the United States (156). With the development of better culture and serologic techniques, it has been possible to define new associations of campylobacter infection with new diseases.
Since laboratories began to isolate Campylobacter from stool specimens some 20 years ago, there have been many reports of Guillain-Barré syndrome (GBS) following Campylobacter infection. Only during the past few years has strong evidence supporting this association developed (103). The purpose of this review is to summarize our current knowledge about the clinical, epidemiological, pathogenetic, and laboratory aspects of campylobacter-associated GBS.
GBS
Since the eradication of polio in most parts of the world, GBS has become the most common cause of acute flaccid paralysis. GBS is an autoimmune disorder of the peripheral nervous system (PNS) characterized by weakness, usually symmetrical, evolving over a period of several days or more (2). Affected persons rapidly develop weakness of the limbs, weakness of the respiratory muscles, and areflexia (loss of reflexes). The disease is self-limited, with muscle strength usually reaching a nadir within 2 to 3 weeks, followed by partial or complete recovery taking place over weeks to months. Up to 20% of patients may require mechanical ventilation (83, 127, 171). Although most people have an uneventful recovery, 15 to 20% of GBS patients are left with severe neurologic deficits (8, 22, 30, 53, 134, 170). Mortality rates of GBS have been reduced to 2 to 3% in the developed world but remain higher in much of the developing world (34, 171). Because C. jejuni-associated GBS may be more severe than GBS occurring after another inciting event, the proportion of patients who die, require mechanical ventilation, and have severe residual neurologic deficits may be higher in this group. Despite two beneficial treatments, plasmapheresis and intravenous human immunoglobulin (IVIG) administration, that have lowered the patient fatality rate of GBS (40, 53, 122, 165), GBS remains a major public health burden.
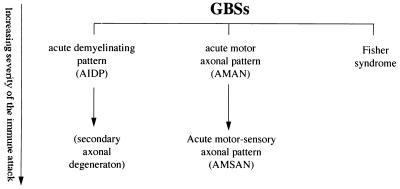
Until recently, GBS was defined as a single homogeneous clinical entity. New studies, however, show that GBS can be divided into several electrophysiological and pathologic patterns (38, 49, 50, 54, 55, 63, 100, 128, 130, 159). As observed by various clinical, electrophysiological, and pathologic techniques, these different patterns suggest that there are different immune targets of an autoimmune response in the PNS. A proposed physiological and pathological classification of GBS by Griffin et al. (49) is shown in Fig. 1. The most frequently encountered pattern of GBS in Europe and North America is acute inflammatory demyelinating polyneuropathy (AIDP) (8, 121, 124), characterized by an immune-mediated attack on myelin and varying degrees of lymphocytic infiltration. In severe cases, axonal degeneration may accompany the demyelination. Less frequently encountered in North America and Europe but common in China (50, 100), Japan (152, 175, 185, 186), Mexico (126), and probably other regions of world are the axonal patterns, in which axons appear to be the target of the immune attack.
FIG. 1.
Interrelationships among the forms of GBS. Reprinted from reference 62 with permission of the publisher.
Two patterns of predominantly axonal involvement can be distinguished. The first pattern, originally called axonal GBS (37) and more recently termed acute motor-sensory axonal neuropathy (AMSAN) is usually severe, involving both motor and sensory fibers (37, 38, 49). The second, a form limited to nearly pure motor involvement, is a pattern termed acute motor axonal neuropathy (AMAN) (49, 100). AMAN appears to be at the more-benign end of a continuous pathogenic spectrum, with more-severe cases producing the AMSAN pattern. A final related disorder, Miller-Fisher syndrome, is characterized by acute onset of unsteadiness of gait (ataxia), areflexia, and an inability to move the eyes, usually associated with nonreactive pupils (ophthalmoplegia) (39).
Incidence and Seasonality
The median annual incidence of clinically defined GBS in the developed world is 1.3 cases (range, 0.4 to 4.0 cases) per 100,000 (17, 66). Until recently, it was generally thought that GBS did not have any significant seasonal variation; however, annual summertime peaks occur in China and some data suggests seasonal variation in Mexico, Spain, and Korea (29, 63, 100, 101, 126, 163). In northern China, these annual summertime peaks are attributed to the AMAN form of GBS, while the AIDP form does not have such a seasonal distribution (63, 100). Outbreaks of GBS are rare but have been reported (21, 78). In 1978, during an outbreak of gastroenteritis affecting >5,000 people, caused by contaminated water in El-Sult, Jordan, 16 persons developed GBS 8 to 24 days after the onset of diarrhea (82, 148).
Demographic Characteristics
GBS, as clinically defined, is slightly more common in males than in females (65, 67). In the United States, GBS also may be slightly more common in whites than in blacks (67). The incidence of GBS increases with age, but some studies have shown an early peak among 15 to 30 year olds (36, 144), suggesting a possible bimodal distribution of cases by age. The AIDP form of GBS appears to affect an older population in Western countries, whereas the AMAN form tends to affect primarily children and young adults (100).
Evidence of a Link between C. jejuni Infection and GBS
For more than 100 years, a variety of preceding infectious illnesses (mostly viral and upper respiratory) have been described in association with GBS (35, 45, 66, 117, 141, 160, 162). However, gastrointestinal illnesses occurring in up to 20% of GBS patients were recognized many decades ago (25). Campylobacter infection was first reported as a potential cause of GBS in 1982 in a 45-year-old man who developed severe GBS with irreversible neurologic damage 2 weeks after a gastrointestinal illness caused by Campylobacter infection (132). Shortly thereafter, several reports described patients who developed GBS soon after infection with C. jejuni (31, 106, 125, 149, 172). From these initial reports, it appeared that male GBS patients outnumbered females by a factor of 3 to 1 (103). Second, even with the earliest reports, it was clear that C. jejuni-associated cases of GBS were more severe and more likely to involve axonal injury (31, 106, 132, 134, 185). Based on the time course from the onset of enteritis to the onset of neurologic symptoms (1 to 3 weeks), this temporal relationship suggested that humoral immunopathogenic mechanisms were operative.
Serologic Studies
Since the median duration of excretion of Campylobacter in stools of infected persons is only 16 days (155) and because of the 1- to 3-week lag time between infection and the onset of GBS, many GBS patients with preceding Campylobacter infection might have falsely negative stool cultures. Because of the limitations of culture techniques, serologic studies in combination with cultures and clinical histories are useful in identifying patients likely to have had a previous campylobacter infection (103). A variety of antibody assays for detecting isotype-specific antibodies have been published; however, there are no standards for testing with regard to antigens used or endpoints for positivity. Most assays, however, utilize protein-rich antigens that detect antibodies to common, cross-reactive epitopes and are not Campylobacter serotype specific. Enzyme-linked immunosorbent assay appears to be the most commonly used method to measure antibodies in serum (18, 60, 104, 113).
The immune response to campylobacter infection is similar to other infectious diseases. Immunoglobulin G (IgG) and IgM levels in serum rise in response to infection and remain elevated for 3 to 4 weeks before declining to the baseline (18), but IgA levels in serum appear during the first few weeks of infection and then fall rapidly (18, 76, 98). IgA antibodies can also be detected in the feces and urine of some patients with infection and appear to be detectable only during the first weeks after acute infection (90, 114, 173). Testing paired sera and demonstrating a significant (i.e., fourfold) increase or decrease in immunoglobulin levels are useful for confirming a recent infection; however, demonstrating such a seroconversion may be difficult and depends upon the timing of the sample collection (60).
Numerous investigators have looked for evidence of Campylobacter infection in series of GBS patients, using serologic methods. Not surprisingly, these serologic studies documented a high prevalence of antibodies to C. jejuni in the serum of patients with GBS (52, 63, 77, 87, 135, 150, 170). Using immunodot assays to determine the frequency of C. jejuni antibodies, Gruenewald and colleagues found that 3 (18%) of 17 patients with GBS in an uncontrolled population had elevated titers in two or more immunoglobulin classes (52). Similarly, using a complement fixation technique, Winer and colleagues found that 14% of 99 patients with GBS had positive C. jejuni serologic tests, compared to only 2% of controls (170). Kaldor and Speed, in a nonblinded serologic study of 56 patients with GBS and 57 controls found 38% of the patients and none of the controls met their criteria for positive serologic responses (77). In a large, blinded, case-control study, Mishu et al. evaluated 118 GBS patients in the United States and 113 controls; 36% of the GBS patients were seropositive for Campylobacter. GBS patients were more than five times likelier than controls to have serologic evidence of recent Campylobacter infection (104). Serologic tests were done as a part of a Japanese study of GBS patients, and 36% of the patients were seropositive for Campylobacter (87). In a prospective study, Ho et al. showed that Campylobacter infections are common in both AMAN and AIDP patients from China and that, depending upon the definition of seropositivity, rates of infection ranged from 24 to 76% for AMAN patients (63).
Culture Surveys
Although serologic studies suggested that some patients with GBS had preceding Campylobacter infection, culture studies were needed to make a stronger case for this intriguing association. Culture-based studies could underestimate the occurrence of infection because of variation in culture techniques, the delayed onset of GBS after infection, and the low likelihood of positive cultures several weeks after infection.
As reported previously (111), “the ability to recover Campylobacter from patients with GBS is related to the duration of excretion of the organism following the patient’s acute diarrheal illness. The convalescent excretion of Campylobacter organisms after acute infection has been studied. In a study of children from Thailand, Taylor et al. (157) found that the duration of excretion was 14 ± 2 days for children <1 year old and 8 ± 2 days for children 1–5 years old. In a cohort study of Mexican children <5 years of age, Calva et al. (24) found that the duration of excretion of the organism was 7 days (range, 7–26). Early studies by Karmali and Fleming (80) showed that the duration of excretion in 4% of untreated children continued up to 6 weeks after the onset of symptoms. At 2 weeks, about two-thirds of the patients were positive for Campylobacter infection by culture, and at 4 weeks, one-third of patients were still positive. About 50% of the patients with Campylobacter infection had negative stool cultures 2 weeks after the onset of diarrheal illness in a Swedish series (155). Convalescent carriage of Campylobacter organisms averaged 37.6 days (range, 15–69) in a Norwegian study (79).”
Nevertheless, several investigators have succeeded in isolating C. jejuni from the stools of patients with GBS at the onset of their neurologic symptoms. As reported previously (111), “It is difficult to determine the frequency of Campylobacter infection among patients with GBS because few studies have systematically done cultures for Campylobacter species. Kuroki et al. (87) recovered C. jejuni from 30% of patients with GBS, whereas Rees et al. (129) had a recovery rate of only 8%. Ropper (135) recovered Campylobacter organisms from 4 (44.4%) of 9 patients with diarrhea preceding GBS.”
Overall, Campylobacter was cultured from the stools of 8 to 50% of GBS patients very soon after the onset of neurologic symptoms (52, 87, 129, 135, 149). From both serologic and culture studies, it is estimated that at least 30 to 40% of GBS patients are infected with Campylobacter 10 days to 2 weeks prior to the onset of their neurologic symptoms. Because of the lag time between C. jejuni infection and the onset of neurologic symptoms, these numbers likely underestimate the association between C. jejuni infection and GBS.
The vast majority of isolates obtained from patients with GBS have been reported as C. jejuni. It is not known whether C. coli, which causes diarrheal illness that is indistinguishable clinically from C. jejuni infection and is difficult to differentiate from C. jejuni by phenotypic methods, is also associated with GBS (110). More recently, C. upsaliensis was recovered from a U.S. patient with AMAN (61), suggesting that other Campylobacter species may well be important in GBS. This has important implications for the culture methods used to investigate Campylobacter and GBS.
Campylobacter Serotypes Associated with GBS
As previously discussed (111), “typing studies are critical to our understanding of the epidemiology and pathogenesis of Campylobacter-associated GBS. In particular, serotyping studies have led to the identification of potentially unique strains involved in the pathogenesis of GBS. Two major serotyping schemes are used worldwide and detect heat-labile (HL) (96) and O (120) antigens. The HL serotyping scheme originally described by Lior (96) detects over 100 serotypes of C. jejuni, C. coli, and C. lari. Uncharacterized bacterial surface antigens and, in some serotypes, flagella are the serodeterminants for this serotyping system (4). The Penner O serotyping scheme (120) detects 60 types of C. jejuni and C. coli (118) and is based on detection of LPS antigens.”
Although serologic and culture studies showed that some patients with GBS had evidence of infection, the landmark study of Kuroki and colleagues (87) solidified the association of Campylobacter and GBS. In that study conducted in Japan, Kuroki et al. isolated C. jejuni from 14 of 46 GBS patients (30.4%) compared with only 6 (1.2%) of 503 subjects in a healthy control population. By O serotyping to characterize the isolates, 10 of 12 available isolates had the same O serotype, O:19. This serotype, however, occurred in only 1.7% of 1,150 C. jejuni isolates from patients with uncomplicated gastrointestinal infection. Lectin typing of the 10 O:19 strains showed that all belonged to lectin type 8, whereas only 1 of 14 O:19 strains from uncomplicated enteritis cases belonged to this type. A recent analysis of 31 strains of C. jejuni from GBS patients by Yuki et al. (180) showed that 52% of strains were O:19 strains but that these strains occurred in 5% of 215 strains from patients with uncomplicated gastroenteritis. In isolates from patients with Miller-Fisher syndrome, O:2 strains were overrepresented compared to control isolates (71 and 38%, respectively) although only seven patients were studied (180). Thus, this study provided clear evidence that certain types of C. jejuni were associated with the development of GBS.
Further studies, however, have shown that other O serotypes that occur more frequently in uncomplicated infections were being isolated from patients with GBS. In particular, O:41 strains have been recently found to be highly associated with GBS patients in South Africa (46, 92). O serotypes from GBS patients that have been reported include O:1, O:2, O:4, O:4 complex, O:5, O:10, O:16, O:23, O:37, O:44, and O:64 (9, 73, 87, 129, 140, 145, 180, 182, 183). In contrast, an association of specific HL (Lior) serotypes in GBS has not been found at this time. For example, among eight strains of C. jejuni O:19 that were studied by flagellin gene typing, there were four different HL serotypes represented, including HL7, HL23, HL70, and HL84 (112). Yuki et al. found that among 16 O:19 strains from GBS patients, 12 (75%) were serotype HL7 whereas only 3 of 11 (27%) O:19 strains from non-GBS patients were serotype HL7 (180). Thus, these studies suggest that there may be subtypes of C. jejuni involved in eliciting GBS and/or that host susceptibility plays an important role in determining the outcome of uncomplicated Campylobacter infection.
In various studies, the occurrence of O:19 strains causing uncomplicated gastrointestinal infection has been estimated at 1 to 6% (3, 44, 75, 102). Serotype O:19 has also been found in laboratory animals, including dogs, cats, and primates (158). Several outbreaks of campylobacter infection in which O:19 serotypes were implicated have been reported (75, 119); however, only in one case associated with O:19 did the patient develop GBS (138).
Risk of Developing GBS after C. jejuni Infection
Although C. jejuni infections appear to commonly precede GBS, C. jejuni infections occur far more commonly than GBS; therefore, the risk of developing GBS after infection with Campylobacter is actually quite low. The U.S. Centers for Disease Control and Prevention estimates there are 1,000 cases of C. jejuni infection per 100,000 per year (156). The National Center for Health Statistics Hospital Discharge data documented 7,874 GBS cases in the United States in 1995. Therefore, assuming that 30% of GBS cases are preceded by C. jejuni infection and that the U.S. population is 250 million, it can be estimated that 1 of every 1,058 cases of C. jejuni infection is followed by GBS.
The risk of developing GBS may be higher after infection with C. jejuni type O:19. Of 12 C. jejuni isolates from Japanese GBS patients, 10 were serotype O:19 (87). This O:19 type represents less than 2% of C. jejuni isolates from patients with uncomplicated enteritis in Japan. The association between O:19 and GBS is not as strong outside of Japan. For example, in the United States, two of seven GBS-associated Campylobacter isolates were serotype O:19 (105); this is still significant, since O:19 accounts for only 3% of isolates from patients with uncomplicated enteritis. In a British study (129), four Campylobacter isolates from GBS patients were serotyped; two were nontypeable, and the other two were not type O:19. Assuming that 20% of GBS-associated C. jejuni isolates are serotype O:19, then the risk of developing GBS after infection with C. jejuni type O:19 is estimated to be 1 in 158.
Although not well defined, some investigators have reported that GBS following Campylobacter infection may be more severe and result in more irreversible neurologic damage than GBS following other putative infections. Of 58 GBS patients studied by Vriesendorp and colleagues (167), 10 had serologic evidence of recent C. jejuni infection, and of these, 3 (30%) had severe disease. Severe disease was defined as fulminating disease with quadriplegia and ventilatory dependence within 24 to 48 h of onset. None of the 48 patients without recent C. jejuni infection had severe disease. In a British study of 101 GBS patients, 23% of GBS patients with Campylobacter infection were unable to walk unassisted 1 year after the onset of symptoms, compared with only 9% of uninfected GBS patients (129). Similarly, in The Netherlands 14 of 24 C. jejuni-infected GBS patients treated with plasma exchange were unable to walk unassisted 6 months after the onset of their symptoms, compared with only 12% of similarly treated GBS patients without evidence of preceding Campylobacter infection (74). Additional prospective studies on a larger number of patients with and without Campylobacter infection and defined according to clinical and electrophysiological criteria are needed to substantiate these reports.
PATHOGENESIS
Peripheral nerves are composed of numerous motor and sensory fibers. The motor fibers originate from motor neurons in the ventral horns of the spinal cord and carry nerve impulses to the muscles. The sensory fibers carry nerve impulses from the specialized sensory receptors in the periphery to the spinal cord. Their cell body resides in the dorsal root ganglia next to the spinal cord. In order to speed the conduction of these nerve impulses, some of these fibers are wrapped by insulating layers of myelin formed by Schwann cells. Between two adjacent myelin sheaths is a gap called the node of Ranvier, where sodium channels are concentrated. This specialized structure allows nerve impulses to regenerate. The myelin sheaths prevent impulses from leaking away and allow impulses to jump from one node to the next. The nerve impulses can be efficiently conducted at up to 75 m/s by the myelinated nerves.
Access to the PNS by the immune system requires that the blood-nerve barrier be altered. Specialized endothelial cells line the blood vessels inside the endoneurium (the connective tissue enveloping individual nerve fibers within a peripheral nerve). Part of the blood-nerve barrier is due to the presence of negatively charged sialic acid containing glycoconjugates in the lumen that repel negatively charged molecules (94, 123). Tight junctions between endothelial cells contribute to this barrier. Entry of molecules around the nerve is also limited by the perineurium (the connective tissue sheath surrounding a fascicle of nerve fibers in a peripheral nerve). This structure consists of layers of specialized fibroblasts, each layer of which is bounded by a basal lamina with tight junctions between adjacent perineural cells. However, the blood-nerve barrier is not as tight as the blood-brain barrier, so that small amounts of circulating proteins such as albumin, IgG, and exogenously administered horseradish peroxidase (none of which can enter the central nervous system [CNS]) (99) can gain entrance to the endoneurial space (7). This relative leakiness may render the PNS more vulnerable than the CNS to antibody-mediated disorders. The blood-nerve barrier is particularly leaky within the dorsal root ganglia and is altogether absent at nerve terminals in the periphery (for example, at the neuromuscular junction), making these areas especially vulnerable to immune-mediated attacks.
Mechanisms of Immune Injury to Nerve Fibers in GBS
AIDP.
On physical examination, patients with AIDP present with flaccid paralysis, areflexia, and usually some sensory loss. Electrophysiological testing typically reveals findings suggestive of demyelination in both motor and sensory nerves (43, 63). Pathologically, macrophage-mediated demyelination and lymphocytic infiltrates are evident (8, 50). As previously discussed (62), “AIDP has long been presumed to be a T-cell-mediated disorder based on the lymphocytic inflammation found in many cases (8) and on the analogy to experimental allergic neuritis (EAN) (for reviews, see references 6 and 57 to 59). Many markers of T-cell activation can be detected in the serum of AIDP patients, including soluble interleukin-2 receptor and gamma interferon (14). However, several lines of evidence have suggested the importance of antibody-mediated nerve fiber damage in AIDP, including the response to plasmapheresis (40, 53), the presence of antimyelin antibodies as detected in complement activation assays (85, 86), the frequent presence of antiglycoconjugate antibodies, and the demonstration of demyelinating immunoglobulins in sera by either injecting the sera intraneurally (153) or incubating the sera with nerve or Schwann cells in vitro (16, 85, 142, 143).”
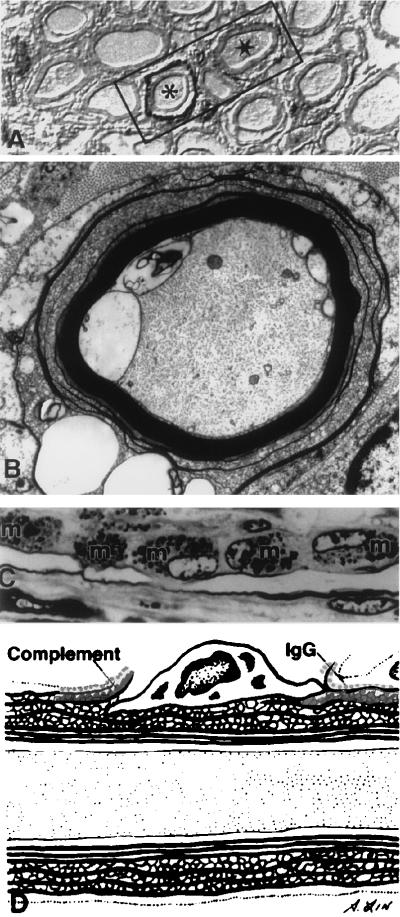
Recently, Griffin and colleagues evaluated the immunopathology of early and unusually well-preserved autopsied AIDP patients from northern China (49–51, 54, 55) (Fig. 2). As reviewed by Ho et al. (62), in two dying patients at 7 and 9 days, the expected lymphocytic inflammation and complete demyelination were found (154). However, in a patient that died 3 days after onset, inflammation was scanty and only a few fibers had as yet completed demyelination. Tissue stained with markers of complement activation demonstrated complement activation products (C3d and the membrane attack complex C5b-9) on the outermost surface of the Schwann cell (Fig. 2A). Electron microscopy showed that most of these fibers had early vesicular changes in the myelin sheaths, usually beginning in the outer lamellae of the sheath (Fig. 2B). The resulting pathologic picture closely resembled the appearance of nerve fibers that are exposed to antigalactocerebroside antibody in the presence of complement (139). Thus, an attractive scenario is that an antibody directed against antigens on the outermost surface of the Schwann cell (the abaxonal Schwann cell plasmalemma) binds complement, which results in sublytic complement activation and the development of transmembrane pores formed by complement. The subsequent entry of calcium might be sufficient to activate calcium-sensitive enzymes, potentially including phospholipase A2 and proteases capable of degrading myelin proteins. Macrophages then participate in removal of damaged myelin (Fig. 2C and D) (124).
FIG. 2.
Immunopathology of the AIDP form of GBS. (A) Nerve fiber stained with markers of complement activation C3d on the outermost surface of the Schwann cell; (B) electron micrograph showing early vesicular changes in the myelin sheath (m); (C) macrophages participate in the removal of damaged myelin; (D) cartoon of the overall process. Reprinted from reference 62 with permission of the publisher.
According to Ho et al. (62), the nature of the antigen on the abaxonal Schwann cell plasmalemma that may be involved in AIDP is uncertain, but it is likely to be a glycolipid (70, 71). Recent studies by Kusunoki and colleagues (88) suggest that galactocerebroside could be such an antigen in at least some cases. It is likely that other immune mechanisms operate in other cases. In instances such as the Chinese cases described above, the chief role of T cells may be to open the blood-nerve barrier, but in other cases demyelination may be more directly T-cell mediated and comparable to that in EAN.
Axonal forms of GBS.
(i) AMSAN.
Ten years ago, Feasby and colleagues suggested that certain cases of GBS were due to primary axonal degeneration without preceding demyelination and that the target antigen might lie on the axon (37). As reviewed by Ho et al. (62), patients typically had fulminant and widespread paralysis with slow and usually incomplete recovery. The electrodiagnostic findings and pathology were dominated by changes compatible with Wallerian-like degeneration (a sequence of degenerative cellular events with disappearance of the axon and myelin in the distal axon when an axon is transected) of motor and sensory fibers (37, 38). Feasby et al. suggested that the axon rather than the Schwann cell or myelin was the primary target. The resulting controversy reflected in part the difficulties in distinguishing electrophysiologically among primary axonal degeneration, axonal degeneration consequent to severe inflammatory attack on the myelin sheath (secondary or bystander axonal degeneration), and demyelination of the immediate preterminal axon (15, 33, 38). In EAN, the animal model of an immunologic attack on PNS myelin, the extent of secondary axonal degeneration correlates with the dose of myelin antigen used in immunization (56); thus, in an animal immunized with high-dose antigen, secondary axonal degeneration is a prominent feature of this inflammatory demyelinating disorder. For this reason, some have suggested that an alternative interpretation of the acute severe cases with extensive evidence of axonal degeneration described by Feasby was that they represented very severe cases of AIDP (33, 161).
According to Ho et al. (62), autopsy studies performed on patients who died shortly after the onset of weakness have confirmed Feasby’s proposal that axons may be the primary target of immune attacks in some cases of GBS (49, 50). In these early cases, axon degenerations were seen without evidence of primary demyelination. These axonal cases have in general had very little inflammation, even early in the course of infection (49, 50). The term AMSAN has recently been suggested for this form of GBS (49).
(ii) AMAN.
As reviewed by Ho et al. (62), another pattern of GBS, purely motor by clinical and electrodiagnostic findings and termed AMAN, has been identified (49, 50, 100), and this pattern of GBS can usually be distinguished from other forms of GBS (63). The clinical features of the AMAN pattern have largely been established by studies in northern China. Every summer, hundreds of children and young adults with GBS inundate the hospitals of northern China. Over 70% of GBS patients studied at one hospital, the Second Teaching Hospital in Shijiazhuang, showed the clinical and electrodiagnostic picture termed AMAN (63, 100). AMAN is characterized by weakness or paralysis without sensory loss. Electrodiagnostic data suggest that motor fibers can be lost selectively, while sensory nerve fibers are preserved and features of demyelination are absent (63, 100). It is now clear that the AMAN pattern of GBS occurs frequently in other parts of Asia (29) and less often in North America (61, 72), Europe (97, 128, 129), and Latin America (126). The AMAN pattern is closely associated with antecedent Campylobacter infection (63, 129, 130, 177).
(iii) Pathology of AMAN.
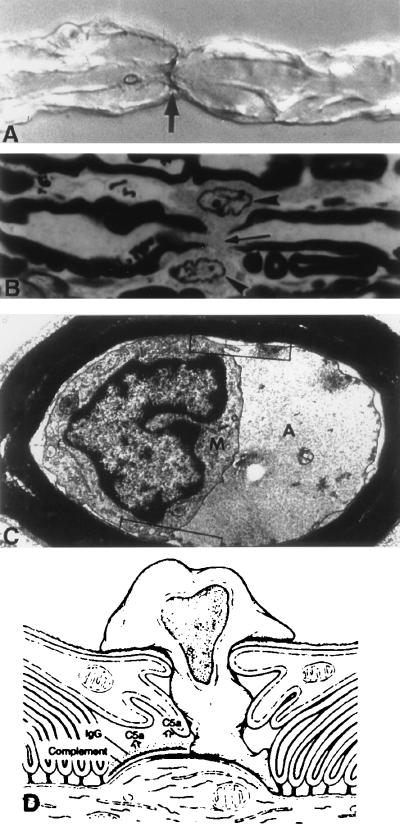
As reviewed by Ho et al. (62), in these axonal patterns lymphocytic infiltration is usually absent or scanty (37, 50, 100). The earliest identifiable change is found in the nodes of Ranvier of motor fibers (51, 55). The nodal gap lengthens at a time when the fibers appear otherwise normal. Immunopathologically, this change correlates with the binding of IgG and the activation of complement, as reflected by the presence of complement activation marker C3d on the nodes of Ranvier (Fig. 3A) (55). Also, at early times, macrophages are recruited to the nodes of Ranvier (Fig. 3B) (51, 55), perhaps as a result of the elaboration of C5a and other complement-derived chemoattractants. These macrophages insert processes into the nodal gap, penetrate the overlying basal lamina of the Schwann cell (51), and then encircle the node and frequently dissect beneath the myelin sheath attachment sites of the paranode to enter the periaxonal space of the internode (Fig. 3C and D).
FIG. 3.
Immunopathology of the AMAN form of GBS. (A) Immunostained nerve fiber showing presence of C3d on the node of Ranvier (arrow); (B) macrophage recruitment to the nodes and insertion (arrowheads) into the nodal gap (arrow); (C) electron micrograph showing a macrophage surrounding the axon (A) in the periaxonal space without damage to the myelin (M); (D) cartoon depicting the entire process. Reprinted from reference 62 with permission of the publisher.
According to Ho et al. (62), “many fibers express complement activation markers in the periaxonal space, that is, the 11-nm space between the axolemma and the Schwann cell. This periaxonal space is normally extremely regular in its spacing, and it is sealed from both ions and macromolecules of the endoneurial fluid by junctional complexes between the myelin terminal loops and the axolemma. The intrusion of the macrophage probably opens the periaxonal space to endoneurial constituents and allows antibody and complement to enter the internodal region. Immunocytochemical studies have demonstrated that the antigen to which IgG binds is on the axolemma (as it is in the node of Ranvier). As the macrophages invade the periaxonal space, the axon collapses away from the Schwann cell, resulting in a marked dilatation of the periaxonal space (51). However, most of the axon evidently survives for some time, even though surrounded by macrophages. The end stage of this occurs when motor axons interrupt and degenerate, extending as far up as the ventral root exit zone (50, 100).”
Miller-Fisher syndrome.
According to Ho et al. (62), “The Miller-Fisher syndrome of ataxia, ophthalmoparesis, and areflexia is usually accompanied by serum antibodies that recognize the ganglioside GQ1b (28, 169, 179). Recent studies have shown that these anti-GQ1b antibodies can alter synaptic release at motor nerve terminals (23, 133). This result at first seems anomalous, since weakness is not a feature of Miller-Fisher syndrome; however, this finding suggests that a small amount of antigen is present even in motor nerve terminals of somatic musculature and that the antiganglioside antibody can block normal quantal release. The population of motor fibers most heavily enriched in GQ1b-reactive antigens are the oculomotor fibers, whose function is affected in the Miller-Fisher syndrome (27). Whether the ataxia is due to sensory abnormalities with loss of proprioception (sensory ataxia) or to cerebellar disease (cerebellar ataxia) remains controversial, but anti-GQ1b antibodies are known to stain both sensory neurons in the dorsal root ganglia and a population of cerebellar neurons (179).”
GLYCOCONJUGATES, CAMPYLOBACTER, AND GBS
Gangliosides are sialic acid-containing glycosphingolipids present in the plasma membrane of vertebrate tissues and are the major surface molecules in both the PNS and the CNS, representing 10% of the total lipid content (108). They are synthesized in neuronal somata and are actively transported to specific sites of enrichment, such as synapses and nodes of Ranvier. Where different gangliosides are enriched in the nervous system can be found by using toxins and lectins that have high specificities of different oligosaccharides epitopes. Cholera toxin, which has high affinity to the GM1 epitope, binds to the nodes of Ranvier and paranodes, including the paranodal Schwann cell (32, 145). Peanut agglutinin, which has high affinity to asialo-GM1, binds to the nodes of Ranvier only (5, 145). Tetanus toxin, which binds to the B series gangliosides (disialosyl gangliosides, e.g., GT1b and GD1b), shows binding to both nodal and internodal axons (145).
Antiglycoconjugate Antibodies
Antiglycoconjugate antibodies, often referred to as antiganglioside antibodies, are frequently found in both AMAN and AIDP patients (63, 69, 71, 84, 168, 178, 187). Some immunochemical evidence supports the hypothesis that glycolipids (rather than glycoproteins) are the target antigen in GBS (168). Yuki et al. found that the proportion of patients with IgG and IgM antibodies against GM1 were higher for patients infected with O:19 strains than for patients infected with non-O:19 strains (86 versus 45% for IgG and 79 versus 40% for IgM) (180). These antiglycoconjugate antibodies are more frequently detected in the sera of AMAN patients than in those of AIDP patients. In particular, IgG anti-GM1 antibodies are reported to be relatively specific for AMAN and are rarely found in other disorders (84). However, this assay has not proved to be sensitive; less than 50% of Chinese AMAN patients are positive for this antibody (63). IgG anti-GD1a antibodies appear to be a more specific marker for the axonal form of GBS (64, 97, 184, 186).
An important issue in evaluating the possible role of antiglycoconjugate antibodies in GBS is whether appropriate antigens are at the sites of known antibody binding in nerve fibers. Studies of ganglioside localization indicate that GM1-like epitopes are concentrated at the nodal region as well as at the paranodal myelin loops (32, 145), the same sites where IgG and complement have been shown to bind in autopsied AMAN patients (51, 55). With regard to the predominantly motor involvement in AMAN cases, it is noteworthy that when human motor and sensory roots were compared, Ogawa-Goto et al. found that motor nerve myelin contained abundant GM1 (15% of total gangliosides) whereas sensory nerve myelin contained only trace amounts (115). GT1b and possibly GD1a also appear to be concentrated on the axolemma and may act as ligands for the myelin-associated glycoprotein. Myelin-associated glycoprotein is concentrated on the Schwann cell adaxonal surface (174) and has been postulated to bind to axonal GT1b or GD1a in the periaxonal space.
MOLECULAR MIMICRY AND GBS
While the proof that Campylobacter causes GBS still awaits definitive evidence, several lines of evidence support the hypothesis that structural features of Campylobacter elicit an autoimmune-mediated attack against host nerve tissue. Some GBS patients have antiganglioside antibodies, some lipopolysaccharides (LPS) of C. jejuni organisms isolated from GBS patients have ganglioside-like structures, and ganglioside-like moieties are present on relevant sites on nerve fibers.
Some post-Campylobacter infection GBS patients have antibodies against the sugar antigen Gal(β1-3)GalNAc, a sequence of sugars present in the ganglioside GM1 (9, 185). These antibodies may be overrepresented in axonal cases but occur in demyelinating cases as well (185). The correlation of antiganglioside antibodies in some patients with GBS but not in others may be in large part due to technical factors for assaying these antibodies (168). A variety of models, including intraneural injection of antibodies and the mouse hemidiaphragm model, have shown physiologic effects of sera containing anti-GM1 and anti-GQ1b, supporting the role of these targets in the pathogenesis of GBS (168).
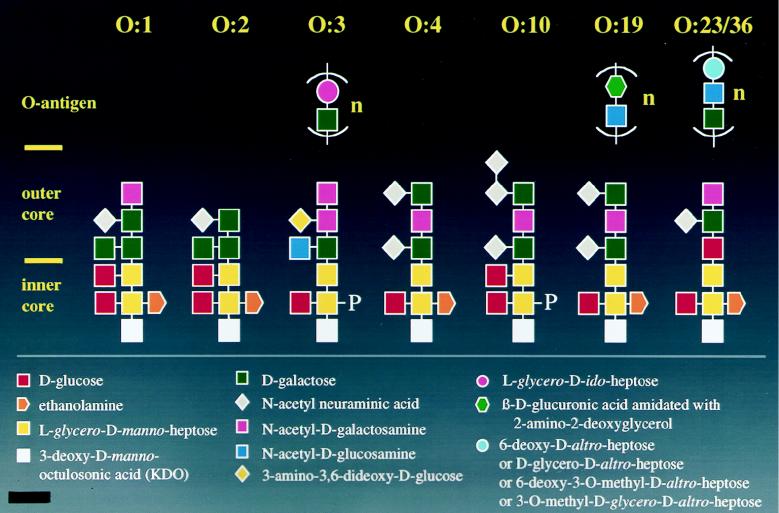
Several studies show a striking homology, if not identity, with the core oligosaccharides of Campylobacter LPS and a number of different glycosphingolipids of the ganglioside group (Fig. 4). Yuki et al. (181) were among the first groups to report the structural similarity of a GBS-associated strain of C. jejuni O:19 with GM1. Extensive structural analysis of LPS from different serotypes of Campylobacter by Aspinall and colleagues (11) showed that the type strain of serotype O:19 contains core oligosaccharides with structural identity to both GM1 and GD1a, whereas two O:19 strains from patients with GBS show structural similarity to GM1, GT1a, and GD3 (Fig. 5). The repeating O-antigenic region from serotype O:19 and O:19 strains from two patients with GBS has been deduced as well and contains a disaccharide repeating unit similar to that in hyaluronic acid (10). Additional studies on serotypes O:1, O:23, and O:36 show structural similarity to GM2 and, in serotype O:4, similarity to GD1a (13). In contrast, structural studies on the type strain of O:2 did not show similarity with any known glycolipid. Serotype O:2 strains isolated from GBS patients have yet to be characterized; thus, it is not known whether such strains also have glycolipid-like structures (12). Other studies using toxin binding and immunochemical analysis have identified putative ganglioside-like epitopes on C. jejuni (9, 116, 176, 182), including the presence of GQ1b on the LPS of C. jejuni isolated from patients with Miller-Fisher syndrome (73, 183), and have identified patients’ antibodies that also reacted against GQ1b-like antigens (179). Patients with either GBS or Miller-Fisher syndrome with specific serotypes of Campylobacter, O:2 or HL4, were found to be more likely to develop anti-GQ1b antibodies than those patients infected with other serotypes (180).
FIG. 4.
Structures of different gangliosides with terminal saccharide structures as reported for isolates of C. jejuni.
FIG. 5.
Known structures of core molecules and O antigen-like polysaccharides from C. jejuni serotypes that contain potential cross-reactive epitopes with different gangliosides. O:1 contains a GM2-like epitope; O:2 contains a GM4 epitope; O:3 contains no cross-reactive epitope; O4 contains a GD1a epitope; O:10 contains a GT1a-like epitope; O:19 may contain several ganglioside epitopes, including GM1 and GD1a, but also GT1a and GD3 (not shown); and O:23/36 contains a GM2-like epitope. Also see the review by Moran et al. (108). Courtesy of Ben Fry.
Strains of C. jejuni may contain smooth LPS with characteristic O antigen repeats or low-molecular-weight LPS characteristic of Neisseria or Haemophilus lipooligosaccharides (109). Fry et al. recently showed that a 16-kb region of C. jejuni 81116 DNA could express O antigens in Escherichia coli and visualized the region with O:6 antiserum using Western blot analysis (41). Further analysis of this region showed the presence of 11 genes with homology to LPS biosynthetic genes (losA to losM). While most of the los genes appear to be homologous to various transferases, losI is similar to NeuD, an enzyme involved in sialic acid transfer, and losK may also be involved in sialic acid synthesis (42). These findings will be important in sorting out whether all or only certain types of Campylobacter have the genetic machinery to produce ganglioside-like antigens.
Taken together, these observations suggest that the antigenic structure of the strain of C. jejuni determines the form of GBS that follows. These examples of possible molecular mimicry have prompted a search for reactivity of serum antibodies against glycoconjugates in other GBS cases. The other targets of antibody from GBS patients that have been demonstrated are the gangliosides LM1 (71) and GD1a (178) as well as the unusual ganglioside N-acetylamino-GD1a (89). Another recent study examined 80 GBS sera for reactivity against galactocerebroside (GalC) and identified anti-GalC antibodies in four cases (89); all four followed previous Mycoplasma pneumoniae infection (89), suggesting that a GalC-like antigen may be expressed in this organism.
HOST SUSCEPTIBILITY TO DEVELOPING GBS
Although certain types of Campylobacter may be implicated in GBS, host factors may play an even more important role in developing GBS. Some C. jejuni strains isolated from diarrhea patients contain similar GM1 ganglioside-like epitopes (145), and yet these patients do not develop antiganglioside antibody. Thus, how pathogenic antibodies develop may depend on the interaction between the microbe and the immune system.
It is unclear whether host genetic factors are important in GBS. Several investigators have studied HLA molecules in patients with GBS (1, 91, 93, 130, 151). Chiba et al. (26) were unable to find HLA class I associations in patients with GBS or Miller-Fisher syndrome; however, insensitive serologic analysis for class I (A, B, and C) and class II (DR and DQ) were performed. Yuki et al. (178) demonstrated an increased frequency of HLA B35 in patients with GBS following Campylobacter infection; only five patients were studied. In a more recent study by Yuki et al. (180), B35 was only slightly increased in GBS patients (21%) versus controls (13.9%). Gorodezky et al. (48) suggested a possible association of GBS with DR3 in Mexican patients. In a well-controlled study by Rees et al., 83% of C. jejuni-positive GBS patients had HLA DQB1*03, compared with 49% of the C. jejuni-negative GBS patients (P = 0.05) (130). However, Yuki et al. did not find DQB1*03 to be associated with GBS (180). Preliminary studies on patients in China with either the AMAN or AIDP form of GBS indicate that certain HLA alleles are overrepresented in the different forms of AMAN as compared to controls (107). This raises the interesting issue of whether solely host factors determine the outcome of GBS.
ANIMAL MODELS OF DISEASE
EAN is a T-cell-mediated disease in Lewis rats and is considered to be the in vivo model for GBS (136). Injection of Lewis rats with proteins or peptides derived from myelin of the PNS induces a primarily T-cell-mediated disease with pathologic features of GBS (demyelination). The model has not, however, been found to be an animal model for Campylobacter-induced GBS (137, 166). Only recently has there been some suggestion that animal models of Campylobacter-induced GBS can be developed and used to study pathogenic mechanisms. Based on a case of GBS in a human following exposure to paralyzed chickens with pathology similar to that of human AMAN, Li et al. (95) used a C. jejuni isolate from a patient with AMAN to develop an animal model of AMAN. Numerous chickens infected with C. jejuni isolated from an AMAN patient developed paralysis, and examination of their nerves showed Wallerian-like degeneration similar to that seen in the human form of the disease (95). These preliminary studies suggest that an animal model of AMAN can be developed by using the specific strain of C. jejuni.
DIAGNOSTIC CONSIDERATIONS
As discussed by Nachamkin (111), “the isolation of Campylobacter organisms from patients with GBS will greatly depend upon the methods used and upon whether the patient has been given antimicrobial therapy for a previous illness. Antimicrobial agents, including the fluoroquinolones and macrolides, commonly used for treating diarrheal disease have excellent activity against Campylobacter species. Such agents quickly clear Campylobacter organisms from the gastrointestinal tract, making the isolation of the organisms nearly impossible… . Other antimicrobial agents used to treat seemingly unrelated illnesses may also affect the recovery of Campylobacter species. It is important, therefore, to elicit a history of antimicrobial use from patients with GBS, as their use will have a marked impact on culture results.”
For optimal isolation of Campylobacter from patients with GBS, multiple stool samples should be obtained for increased sensitivity (87, 146, 164). Only one study of GBS patients has examined this issue. As reported previously (111), “Kuroki et al. (87) found that of 14 GBS patients with Campylobacter-positive stool cultures, 57% were detected with 1 sample, 93% were detected with 2 samples, and all were detected with 3 samples.” Thus, multiple stool samples (or rectal swabs) should be obtained from GBS patients immediately upon admission to the hospital, preferably 3 over a 3-day period. Samples should be transported to the laboratory in a suitable transport medium such as Cary-Blair medium. Both direct plating and enrichment methods should be used (110, 111).
A number of primary selective media can be used for isolating C. jejuni and C. coli, including blood-containing (131, 147) and blood-free media (19, 47, 68, 81; reviewed in reference 110). As previously described (111), “enrichment culture methods are designed to isolate Campylobacter organisms from samples containing low numbers of organisms. In cases of Campylobacter associated GBS, we presume that the level of Campylobacter in the stool, if present, is likely to be lower than the concentration during the acute diarrheal illness. Thus, enrichment cultures should be included among the laboratory tests for patients with GBS. A study by Taylor et al. (157) clearly showed that enrichment cultures dramatically improved the yield of Campylobacter organisms when most GBS patients would be seen. An increase of as much as 31% over conventional plating techniques was seen when patients were cultured >20 days after the onset of their diarrheal illness.” A number of enrichment culture media can be used. In our studies in Northern China and elsewhere, we have had good success with Preston enrichment broth (20).
THERAPY
The major reduction of mortality in GBS has been due to advances in supportive care of critically ill patients. However, increased understanding of the immunologic basis of this disease over the past 15 years has allowed us to change the natural course of this disease. Plasmapheresis was the first therapy shown to be effective in speeding up the course of recovery (40, 53). In this procedure, a patient’s blood is removed and centrifuged to separate the cellular and plasma components and the cellular components, diluted with artificial plasminate, are reinfused to the patient. The therapeutic effect is presumably due to the removal of inciting circulating factors such as antibodies. Another effective therapy is administration of IVIG. There have been two controlled studies of the use of IVIG in GBS (122, 165). Both indicated that IVIG is as effective as plasmapheresis in the treatment of GBS (122, 165). The mechanism of action of infused immunoglobulin is not clear, but one possibility is that pooled immunoglobulins contain anti-idiotypic antibodies that inactivate the disease-specific antibodies.
CONCLUSIONS AND FUTURE DIRECTIONS
Based on serologic and culture evidence, the association of Campylobacter with the development of GBS now appears firmly established. However, much work remains to determine how Campylobacter can induce this disease. A recent consensus meeting on Campylobacter and GBS was conducted by the National Institutes of Health and outlined several areas of research (91) for the future as follows. (i) Conduct additional surveillance studies to provide a better estimate of infection rates and incidence of GBS and to obtain a much better picture of the epidemiology of Campylobacter-induced GBS. (ii) Encourage studies to assess the host susceptibility to GBS. (iii) Standardized microbiological laboratory procedures are needed to ensure isolation of Campylobacter strains associated with GBS. (iv) Serologic assays for diagnosis of C. jejuni infections need to be standardized and validated. (v) A diagnostic test specific for various Campylobacter species is needed, since a large number of Campylobacter infections likely goes unrecognized. (vi) An animal model for Campylobacter enteritis with ensuing GBS is urgently needed. (vii) There should be a Campylobacter strain bank established in which bacterial strains isolated from patients who develop GBS (or variants) can be deposited. These strains should be available to researchers in the field. (viii) There is a need for standardized reagents, particularly monoclonal antibodies, that can be used to identify bacterial epitopes and which can be tested for their ability to react with different neural targets. (ix) Better typing systems (phenotypic and molecular) are needed. (x) Additional studies on the pathogenesis of the different forms of GBS are needed.
REFERENCES
- 1.Adams D, Gibson J D, Thomas P K, Batchelor J R, Hughes R A, Kennedy L, Festenstein H, Sachs J. HLA antigens in Guillain-Barre syndrome. Lancet. 1977;ii:504–505. doi: 10.1016/s0140-6736(77)91626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams R D, Victor M. Diseases of the peripheral nerves. In: Adams R D, Victor M, editors. Principles of neurology. New York, N.Y: McGraw-Hill, Inc.; 1993. pp. 1117–1169. [Google Scholar]
- 3.Albert M J, Leach A, Asche V, Hennessy J, Penner J L. Serotype distribution of Campylobacter jejuni and Campylobacter coli isolated from hospitalized patients with diarrhea in central Australia. J Clin Microbiol. 1992;30:207–210. doi: 10.1128/jcm.30.1.207-210.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alm R A, Guerry P, Power M E, Lior H, Trust T J. Analysis of the role of flagella in the heat-labile Lior serotyping scheme of thermophilic campylobacters by mutant allele exchange. J Clin Microbiol. 1991;29:2438–2445. doi: 10.1128/jcm.29.11.2438-2445.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Apostolski S, Sadiq S A, Hays A, Corbo M, Suturkova-Milosevic L, Chaliff P, Stefansson K, LeBaron R G, Ruoslahti E, Hays A P, Latov N. Identification of Gal(β1-3)GalNAc bearing glycoproteins at the nodes of Ranvier in peripheral nerve. J Neurosci Res. 1994;38:134–141. doi: 10.1002/jnr.490380203. [DOI] [PubMed] [Google Scholar]
- 6.Arnason B G W, Soliven B. Acute inflammatory demyelinating polyradiculopathy. In: Dyck P J, Thomas P K, Griffin J W, Low P A, Poduslo J F, editors. Peripheral neuropathy. W. B. Philadelphia, Pa: Saunders; 1993. pp. 1437–1497. [Google Scholar]
- 7.Arvidson B. Cellular uptake of exogenous horseradish peroxidase in mouse peripheral nerve. Acta Neuropathol. 1977;37:35–41. doi: 10.1007/BF00684538. [DOI] [PubMed] [Google Scholar]
- 8.Asbury A K, Arnason B G, Adams R D. The inflammatory lesion in idiopathic polyneuritis. Medicine. 1969;48:173–215. doi: 10.1097/00005792-196905000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Aspinall G O, Fujimoto S, McDonald A G, Pang H, Kurjanczyk L A, Penner J L. Lipopolysaccharides from Campylobacter jejuni associated with Guillain-Barré syndrome patients mimic human gangliosides in structure. Infect Immun. 1994;62:2122–2125. doi: 10.1128/iai.62.5.2122-2125.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aspinall G O, McDonald A G, Pang H. Lipopolysaccharides of Campylobacter jejuni serotype O:19: structures of O antigen chains from the serostrain and two bacterial isolates from patients with Guillain-Barre syndrome. Biochemistry. 1994;33:250–255. doi: 10.1021/bi00167a033. [DOI] [PubMed] [Google Scholar]
- 11.Aspinall G O, McDonald A G, Pang H, Kurjanczyk L A, Penner J L. Lipopolysaccharides of Campylobacter jejuni serotype O:19: structures of core oligosaccharide regions from the serostrain and two bacterial isolates from patients with the Guillain-Barre syndrome. Biochemistry. 1994;33:241–249. doi: 10.1021/bi00167a032. [DOI] [PubMed] [Google Scholar]
- 12.Aspinall G O, McDonald A G, Raju T S, Pang H, Kurjanczyk L A, Penner J L, Moran A P. Chemical structure of the core region of Campylobacter jejuni serotype O:2 lipopolysaccharide. Eur J Biochem. 1993;213:1029–1037. doi: 10.1111/j.1432-1033.1993.tb17850.x. [DOI] [PubMed] [Google Scholar]
- 13.Aspinall G O, McDonald A G, Raju T S, Pang H, Molan A P, Penner J L. Chemical structures of the core regions of Campylobacter jejuni serotypes O:1, O:4, O:23, and O:36 lipopolysaccharides. Eur J Biochem. 1993;213:1017–1027. doi: 10.1111/j.1432-1033.1993.tb17849.x. [DOI] [PubMed] [Google Scholar]
- 14.Bansil S, Mithen F A, Cook S D, Sheffet A, Rohowsky-Kochan C. Clinical correlation with serum-soluble interleukin-2 receptor levels in Guillain-Barre syndrome. Neurology. 1991;41:1302–1305. doi: 10.1212/wnl.41.8.1302. [DOI] [PubMed] [Google Scholar]
- 15.Berciano J, Coria F, Monton F, Calleja J, Figols J, Lafarga M. Axonal form of Guillain-Barre syndrome: evidence for macrophage-associated demyelination. Muscle Nerve. 1993;16:744–751. doi: 10.1002/mus.880160709. [DOI] [PubMed] [Google Scholar]
- 16.Birchem R, Mithen F A, L’Empereur K M, Wessels M M. Ultrastructural effects of Guillain-Barre serum in cultures containing only rat Schwann cells and dorsal root ganglion neurons. Brain Res. 1987;421:173–185. doi: 10.1016/0006-8993(87)91288-1. [DOI] [PubMed] [Google Scholar]
- 17.Black R E, Levine M M, Clements M L, Hughs T P, Blaser M J. Experimental Campylobacter jejuni infections in humans. J Infect Dis. 1988;157:472–480. doi: 10.1093/infdis/157.3.472. [DOI] [PubMed] [Google Scholar]
- 18.Blaser M J, Duncan D J. Human serum antibody response to Campylobacter jejuni infection as measured in an enzyme-linked immunosorbent assay. Infect Immun. 1984;44:292–298. doi: 10.1128/iai.44.2.292-298.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bolton F J, Hutchinson D M, Coates D. Blood-free selective medium for isolation of Campylobacter jejuni from feces. J Clin Microbiol. 1984;19:169–171. doi: 10.1128/jcm.19.2.169-171.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolton F J, Robertson L. A selective medium for isolating Campylobacter jejuni/coli. J Clin Pathol. 1982;35:462–467. doi: 10.1136/jcp.35.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breman J G, Hayner J S. Guillain-Barre syndrome and its relationship to swine influenza vaccination in Michigan, 1976–1977. Am J Epidemiol. 1984;119:880–889. doi: 10.1093/oxfordjournals.aje.a113810. [DOI] [PubMed] [Google Scholar]
- 22.Briscoe D M, McMenamin J B, O’Donahue N V. Prognosis in Guillain-Barre syndrome. Arch Dis Child. 1987;62:733–735. doi: 10.1136/adc.62.7.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buchwald B, Weishaupt A, Toyka K V, Dudel J. Immunoglobulin G from a patient with Miller-Fisher syndrome rapidly and reversibly depresses evoked quantal release at the neuromuscular junction of mice. Neurosci Lett. 1995;201:163–166. doi: 10.1016/0304-3940(95)12155-2. [DOI] [PubMed] [Google Scholar]
- 24.Calva J J, Ruiz-Palacios G M, Lopez-Vidal A B, Ramos A, Bojalil R. Cohort study of intestinal infection with Campylobacter in Mexican children. Lancet. 1988;i:503–505. doi: 10.1016/s0140-6736(88)91297-4. [DOI] [PubMed] [Google Scholar]
- 25.Campbell A M G. The aetiology of polyneuritis. Proc R Soc Med. 1958;51:157–159. doi: 10.1177/003591575805100304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiba A, Kusinoki S, Kuwata S, Juji T, Sibata Y, Kanazawa I. HLA and anti-GQ1b IgG antibody in Miller Fisher syndrome and Guillain-Barre syndrome. J Neuroimmunol. 1995;61:85–88. doi: 10.1016/0165-5728(95)00079-h. [DOI] [PubMed] [Google Scholar]
- 27.Chiba A, Kusunoki S, Obata H, Machinami R, Kanazawa I. Serum anti-GQ1b antibody is associated with ophthalmoplegia in Miller Fisher syndrome and Guillain-Barre syndrome: clinical and immunohistochemical studies. Neurology. 1993;43:1911–1917. doi: 10.1212/wnl.43.10.1911. [DOI] [PubMed] [Google Scholar]
- 28.Chiba A, Kusunoki S, Shimizu T, Kanazawa I. Serum IgG antibody to ganglioside GQ1b is a possible marker of Miller Fisher syndrome. Ann Neurol. 1992;31:677–679. doi: 10.1002/ana.410310619. [DOI] [PubMed] [Google Scholar]
- 29.Coe C J. Guillain-Barre syndrome in Korean children. Yonsei Med J. 1989;30:81–87. doi: 10.3349/ymj.1989.30.1.81. [DOI] [PubMed] [Google Scholar]
- 30.Cole G F, Matthew D J. Progress in severe Guillain-Barre syndrome. Arch Dis Child. 1987;62:288–291. doi: 10.1136/adc.62.3.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Constant O C, Bentley C C, Denman A M, Lehane J R, Larson H E. The Guillain-Barre syndrome following Campylobacter enteritis with recovery after plasmapheresis. J Infect. 1983;6:89–91. doi: 10.1016/s0163-4453(83)95881-4. [DOI] [PubMed] [Google Scholar]
- 32.Corbo M, Quattrini A, Latov N, Hays A P. Localization of GM1 and Gal(β1-3)GalNAc antigenic determinants in peripheral nerve. Neurology. 1993;43:809–814. doi: 10.1212/wnl.43.4.809. [DOI] [PubMed] [Google Scholar]
- 33.Cros D, Triggs W J. There are no neurophysiologic features characteristic of “axonal” Guillain-Barre syndrome. Muscle Nerve. 1994;17:675–677. doi: 10.1002/mus.880170617. [DOI] [PubMed] [Google Scholar]
- 34.de Jager A E, Sluiter H J. Clinical signs in severe Guillain-Barre syndrome: analysis of 63 patients. J Neurol Sci. 1991;104:143–150. doi: 10.1016/0022-510x(91)90303-o. [DOI] [PubMed] [Google Scholar]
- 35.Dowling P C. Role of infection in Guillain-Barre syndrome: laboratory confirmation of herpesviruses in 41 cases. Ann Neurol. 1981;9:44–55. doi: 10.1002/ana.410090709. [DOI] [PubMed] [Google Scholar]
- 36.Dowling P C, Menonna J P, Cook S D. Guillain-Barre syndrome in greater New York-New Jersey. JAMA. 1977;238:317–318. [PubMed] [Google Scholar]
- 37.Feasby T E, Gilbert J J, Brown W F, Bolton C F, Hahn A F, Koopman W F, Zochodne D W. An acute axonal form of Guillain-Barre polyneuropathy. Brain. 1986;109:1115–1126. doi: 10.1093/brain/109.6.1115. [DOI] [PubMed] [Google Scholar]
- 38.Feasby T E, Hahn A F, Brown W F, Bolton C F, Gilbert J J, Koopman W J. Severe axonal degeneration in acute Guillain-Barre syndrome: evidence of two different mechanisms? J Neurol Sci. 1993;116:185–192. doi: 10.1016/0022-510x(93)90324-r. [DOI] [PubMed] [Google Scholar]
- 39.Fisher M. An unusual variant of acute idiopathic polyneuritis (syndrome of ophthalmoplegia ataxia and areflexia) N Engl J Med. 1956;255:57–65. doi: 10.1056/NEJM195607122550201. [DOI] [PubMed] [Google Scholar]
- 40.French Cooperative Group on Plasma Exchange in Guillain-Barre Syndrome. Efficacy of plasma exchange in Guillain-Barre syndrome: role of replacement fluids. Ann Neurol. 1987;22:753–761. doi: 10.1002/ana.410220612. [DOI] [PubMed] [Google Scholar]
- 41.Fry B N, Korolik V, Teunis B J J, ten Brinke J A, Pennings M T T, Van Der Zeijst B A M. Molecular biology of Campylobacter: natural transformation and lipopolysaccharides. Thesis. Utrecht, The Netherlands: University of Utrecht; 1997. Identification of the locus encoding Campylobacter O-antigens and its expression in Escherichia coli; pp. 78–85. [Google Scholar]
- 42.Fry B N, ten Brinke J A, Teunis B J J, Zalm R, Korolik V, Van Der Zeijst B A M. Molecular biology of Campylobacter: natural transformation and lipopolysaccharides. Thesis. Utrecht, The Netherlands: University of Utrecht; 1997. Molecular characterization of the lipopolysaccharide biosynthesis locus of Campylobacter jejuni 81116; pp. 88–116. [Google Scholar]
- 43.Gao C Y, Ho T W, Wang G L, Zhang G H, Mao J X, Li C Y, Griffin J W, Asbury A K, McKhann G M, Cornblath D R. Electrodiagnostic studies of Guillain-Barre syndrome in northern China. In: Kimura J, Kaji R, editors. Physiology of ALS and related disorders. Amsterdam, The Netherlands: Elsevier; 1997. pp. 119–128. [Google Scholar]
- 44.Georges-Courbot M C, Baya C, Beraud A M, Meunier D M Y, Georges A J. Distribution and serotypes of Campylobacter jejuni and Campylobacter coli in enteric Campylobacter strains isolated from children in the Central African Republic. J Clin Microbiol. 1986;23:592–594. doi: 10.1128/jcm.23.3.592-594.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Glaze D G. Guillain-Barre syndrome. In: Feigen R D, Cherry J D, editors. Pediatric infectious diseases. 4th ed. Philadelphia, Pa: W. B. Saunders; 1992. pp. 470–482. [Google Scholar]
- 46.Goddard E A, Lastovica A J, Argent A C. Campylobacter O:41 isolation in Guillain-Barre syndrome. Arch Dis Child. 1997;76:526–528. doi: 10.1136/adc.76.6.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goossens H, Vlaes L, Galand I, Van den Borre C, Butzler J-P. Semisolid blood-free selective-motility medium for the isolation of campylobacters from stool specimens. J Clin Microbiol. 1989;27:1077–1080. doi: 10.1128/jcm.27.5.1077-1080.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gorodezky C, Varela B, Castro-Escobar L E, Chavez-Negrete A, Escobar-Gutierrez A, Martinez-Mata J. HLA-DR antigens in Mexican patients with Guillain-Barre sydrome. J Neuroimmunol. 1983;4:1–7. doi: 10.1016/0165-5728(83)90058-9. [DOI] [PubMed] [Google Scholar]
- 49.Griffin J W, Li C Y, Ho T W, Tian M, Gao C Y, Xue P, Mishu B, Cornblath D R, Macko C, McKhann G M, Asbury A K. Pathology of the motor-sensory axonal Guillain-Barre syndrome. Ann Neurol. 1996;39:17–28. doi: 10.1002/ana.410390105. [DOI] [PubMed] [Google Scholar]
- 50.Griffin J W, Li C Y, Ho T W, Xue P, Macko C, Cornblath D R, Gao C Y, Yang C, Tian M, Mishu B, McKhann G M, Asbury A K. Guillain-Barre syndrome in northern China: the spectrum of neuropathologic changes in clinically defined cases. Brain. 1995;118:577–595. doi: 10.1093/brain/118.3.577. [DOI] [PubMed] [Google Scholar]
- 51.Griffin J W, Li C Y, Macko C, Ho T W, Hsieh S-T, Xue P, Wang F A, Cornblath D R, McKhann G M, Asbury A K. Early nodal changes in the acute motor axonal neuropathy pattern of the Guillain-Barre syndrome. J Neurocytol. 1996;25:33–51. doi: 10.1007/BF02284784. [DOI] [PubMed] [Google Scholar]
- 52.Gruenewald R, Ropper A H, Lior H, Chan J, Lee R, Molinaro V S. Serologic evidence of Campylobacter jejuni/coli enteritis in patients with Guillain-Barre syndrome. Arch Neurol. 1991;48:1080–1082. doi: 10.1001/archneur.1991.00530220102027. [DOI] [PubMed] [Google Scholar]
- 53.Guillain-Barre Study Group. Plasmapheresis and acute Guillain-Barre syndrome. Neurology. 1985;35:1096–1104. [PubMed] [Google Scholar]
- 54.Hafer-Macko C, Hsieh S-T, Li C Y, Ho T W, Sheikh K A, Cornblath D R, McKhann G M, Asbury A K, Griffin J W. Acute motor axonal neuropathy: an antibody-mediated attack on axolemma. Ann Neurol. 1996;40:635–644. doi: 10.1002/ana.410400414. [DOI] [PubMed] [Google Scholar]
- 55.Hafer-Macko C, Sheikh K A, Li C Y, Ho T W, Cornblath D R, McKhann G M, Asbury A K, Griffin J W. Immune attack on the Schwann cell surface in acute inflammatory demyelinating polyneuropathy. Ann Neurol. 1996;39:625–635. doi: 10.1002/ana.410390512. [DOI] [PubMed] [Google Scholar]
- 56.Hahn A F, Feasby T E, Steele A, Lovgren D S, Berry J. Demyelination and axonal degeneration in Lewis rat experimental allergic neuritis depend on myelin dosage. Lab Invest. 1988;59:115–126. [PubMed] [Google Scholar]
- 57.Hartung H-P, Pollard J D, Harvey G K, Toyka K V. Immunopathogenesis and treatment of the Guillain-Barre syndrome—part I. Muscle Nerve. 1995;18:137–153. doi: 10.1002/mus.880180202. [DOI] [PubMed] [Google Scholar]
- 58.Hartung H-P, Pollard J D, Harvey G K, Toyka K V. Immunopathogenesis and treatment of the Guillain-Barre syndrome—part II. Muscle Nerve. 1995;18:154–164. doi: 10.1002/mus.880180203. [DOI] [PubMed] [Google Scholar]
- 59.Hartung H-P, Stoll G, Toyka K V. Immune reactions in the peripheral nervous system. In: Dyck P J, Thomas P K, Griffin J W, Low P A, Poduslo J F, editors. Peripheral neuropathy. W. B. Philadelphia, Pa: Saunders; 1993. pp. 418–444. [Google Scholar]
- 60.Herbrink P, Van den Munckhof H A M, Bumkens M, Lindeman J, Van Dijk W C. Human serum antibody response in Campylobacter jejuni enteritis as measured by enzyme-linked immunosorbent assay. Eur J Clin Microbiol Infect Dis. 1988;7:388–393. doi: 10.1007/BF01962343. [DOI] [PubMed] [Google Scholar]
- 61.Ho T W, Hsieh S-T, Nachamkin I, Willison H J, Sheikh K, Kiehlbauch J, Flanigan K, McArthur J C, Cornblath D R, McKhann G M, Griffin J W. Motor nerve terminal degeneration provides a potential mechanism for rapid recovery in acute motor axonal neuropathy after Campylobacter infection. Neurology. 1997;48:717–724. doi: 10.1212/wnl.48.3.717. [DOI] [PubMed] [Google Scholar]
- 62.Ho T W, McKhann G M, Griffin J W. Human autoimmune neuropathies. Annu Rev Neurosci. 1998;21:187–226. doi: 10.1146/annurev.neuro.21.1.187. [DOI] [PubMed] [Google Scholar]
- 63.Ho T W, Mishu B, Li C Y, Gao C Y, Cornblath D R, Griffin J W, Asbury A K, Blaser M J, McKhann G M. Guillain-Barre syndrome in northern China: relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain. 1995;118:597–605. doi: 10.1093/brain/118.3.597. [DOI] [PubMed] [Google Scholar]
- 64.Ho, T. W., H. Willison, I. Nachamkin, C. Y. Li, D. R. Cornblath, A. K. Asbury, J. W. Griffin, and G. M. McKhann. Anti-GD1a antibody distinguishes axonal from demyelinating forms of Guillain-Barre syndrome. Submitted for publication. [DOI] [PubMed]
- 65.Hughes R A C. Guillain-Barre syndrome. London, United Kingdom: Springer-Verlag; 1991. [Google Scholar]
- 66.Hughes, R. A. C., and J. H. Rees. 1997. Clinical and epidemiologic features of Guillain-Barre syndrome. Clin. Infect. Dis. 176(Suppl. 2):S92–S98. [DOI] [PubMed]
- 67.Hurwitz E S, Holman R C, Nelson D B, Schonberger L B. National surveillance for Guillain-Barre syndrome: January 1978–March 1979. Neurology. 1983;33:150–157. doi: 10.1212/wnl.33.2.150. [DOI] [PubMed] [Google Scholar]
- 68.Hutchinson D N, Bolton F J. Improved blood free selective medium for the isolation of Campylobacter jejuni from faecal specimens. J Clin Pathol. 1984;37:956–957. doi: 10.1136/jcp.37.8.956-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ilyas A A, Dalakas M C, Brady R O, Quarles R H. Sulfated glucuronyl glycolipids reacting with anti-myelin-associated-glycoprotein monoclonal antibodies including IgM paraproteins in neuropathy: species distribution and partial characterization of epitopes. Brain Res. 1986;385:1–9. doi: 10.1016/0006-8993(86)91540-4. [DOI] [PubMed] [Google Scholar]
- 70.Ilyas A A, Mithen F A, Dalakas M C, Chen Z-W, Cook S D. Antibodies to acidic glycolipids in Guillain-Barre syndrome and chronic inflammatory demyelinating polyneuropathy. J Neurol Sci. 1992;107:111–121. doi: 10.1016/0022-510x(92)90217-9. [DOI] [PubMed] [Google Scholar]
- 71.Ilyas A A, Willison H J, Quarles R H, Jungawala F B, Cornblath D R, Trapp B D, Griffin D E, Griffin J W, McKhann G M. Serum antibodies to gangliosides in Guillain-Barre syndrome. Ann Neurol. 1988;23:440–447. doi: 10.1002/ana.410230503. [DOI] [PubMed] [Google Scholar]
- 72.Jackson C E, Barohn R J, Mendell J R. Acute paralytic syndrome in three American men. Comparison with Chinese cases. Arch Neurol. 1993;50:732–735. doi: 10.1001/archneur.1993.00540070050014. [DOI] [PubMed] [Google Scholar]
- 73.Jacobs B C, Endtz H P, van der Meche F G A, Hazenberg M P, Actereekte H A M, van Doorn P A. Serum anti-GQ1b IgG antibodies recognize surface epitopes on Campylobacter jejuni from patients with Miller Fisher syndrome. Ann Neurol. 1995;37:260–264. doi: 10.1002/ana.410370218. [DOI] [PubMed] [Google Scholar]
- 74.Jacobs B C, Schmitz P I M, van der Meche F G A. Campylobacter jejuni infection and treatment for Guillain-Barre syndrome. N Engl J Med. 1996;335:208–209. doi: 10.1056/NEJM199607183350315. [DOI] [PubMed] [Google Scholar]
- 75.Jones D M, Sutcliffe E M, Abbott J D. Serotyping of Campylobacter species by combined use of two methods. Eur J Clin Microbiol. 1985;4:562–565. doi: 10.1007/BF02013395. [DOI] [PubMed] [Google Scholar]
- 76.Kaldor J, Pritchard H, Serpell A, Metcalf W. Serum antibodies in Campylobacter enteritis. J Clin Microbiol. 1983;18:1–4. doi: 10.1128/jcm.18.1.1-4.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kaldor J, Speed B R. Guillain-Barre syndrome and Campylobacter jejuni: a serologic study. Br Med J. 1984;288:1867–1870. doi: 10.1136/bmj.288.6434.1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kaplan J E, Poduska P J, McIntosh G C, Hopkins R S, Ferguson S W, Schonberger L B. Guillain-Barre syndrome in Larimer County, Colorado: a high incidence area. Neurology. 1985;35:581–584. doi: 10.1212/wnl.35.4.581. [DOI] [PubMed] [Google Scholar]
- 79.Kapperud G, Lassen J, Ostroff S M, Aasen S. Clinical features of sporadic campylobacter infections in Norway. Scand J Infect Dis. 1992;24:741–749. doi: 10.3109/00365549209062459. [DOI] [PubMed] [Google Scholar]
- 80.Karmali M A, Fleming P C. Campylobacter enteritis in children. J Pediatr. 1979;94:527–533. doi: 10.1016/s0022-3476(79)80004-9. [DOI] [PubMed] [Google Scholar]
- 81.Karmali M A, Simor A E, Roscoe M, Flemming P C, Smith S S, Lane J. Evaluation of a blood-free, charcoal-based, selective medium for the isolation of Campylobacter organisms from feces. J Clin Microbiol. 1986;23:456–459. doi: 10.1128/jcm.23.3.456-459.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Khoury S H. Guillain-Barre syndrome: epidemiology of an outbreak. Am J Epidemiol. 1978;107:433–438. doi: 10.1093/oxfordjournals.aje.a112561. [DOI] [PubMed] [Google Scholar]
- 83.Koobatian T J, Birkhead G S, Schramm M M, Vogt R L. The use of hospital discharge data for public health surveillance of Guillain-Barre syndrome. Ann Neurol. 1991;30:618–621. doi: 10.1002/ana.410300418. [DOI] [PubMed] [Google Scholar]
- 84.Kornberg A J, Pestronk A, Bieser K, Ho T W, McKhann G M, Wu H S, Jiang Z. The clinical correlates of high-titer IgG anti-GM1 antibodies. Ann Neurol. 1994;35:234–237. doi: 10.1002/ana.410350217. [DOI] [PubMed] [Google Scholar]
- 85.Koski C L, Chou D K H, Jungalwala F B. Anti-peripheral nerve myelin antibodies in Guillain-Barre syndrome bind a neutral glycolipid of peripheral myelin and cross-react with Forssman antigen. J Clin Invest. 1989;84:280–287. doi: 10.1172/JCI114152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Koski C L, Humphrey R, Shin M L. Anti-peripheral myelin antibodies in patients with demyelinating neuropathy: quantitative and kinetic determination of serum antibody by complement component 1 fixation. Proc Natl Acad Sci USA. 1985;82:905–909. doi: 10.1073/pnas.82.3.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kuroki S, Saida T, Nukina M, Haruta T, Yoshioka M, Kobayashi Y, Nakanishi H. Campylobacter jejuni strains from patients with Guillain-Barre syndrome belong mostly to Penner serogroup 19 and contain B-N-acetylglucosamine residues. Ann Neurol. 1993;33:243–247. doi: 10.1002/ana.410330304. [DOI] [PubMed] [Google Scholar]
- 88.Kusunoki S, Chiba A, Hitoshi S, Takizawa H, Kanazawa I. Anti-Gal-C antibody in autoimmune neuropathies subsequent to mycoplasma infection. Muscle Nerve. 1995;18:409–413. doi: 10.1002/mus.880180407. [DOI] [PubMed] [Google Scholar]
- 89.Kusunoki S, Chiba A, Kon K, Ando S, Arisawa K, Tate A, Kanazawa I. N-acetylgalactosaminyl GD1a is a target molecule for serum antibody in Guillain-Barre syndrome. Ann Neurol. 1994;35:570–576. doi: 10.1002/ana.410350510. [DOI] [PubMed] [Google Scholar]
- 90.Lane E M, Batchelor R, Bourgeois A L, Burr D H, Olson J G. Urine and fecal IgA responses during naturally acquired infection with Campylobacter jejuni. Lancet. 1987;i:1141. doi: 10.1016/s0140-6736(87)91694-1. . (Letter.) [DOI] [PubMed] [Google Scholar]
- 91.Lang, D. R., B. M. Allos, and M. J. Blaser. 1997. Workshop summary and recommendations regarding the development of Guillain-Barre syndrome following Campylobacter infection. J. Infect. Dis. 176(Suppl. 2):S198–S200. [DOI] [PubMed]
- 92.Lastovica, A. J., E. A. Goddard, and A. C. Argent. 1997. Guillain-Barre syndrome in South Africa associated with Campylobacter jejuni O:41 strains. Clin. Infect. Dis. 176(Suppl. 2):S139–S143. [DOI] [PubMed]
- 93.Latovitzki N, Suciu-Foca N, Penn A S, Olarte M R, Chutorian A M. HLA typing and Guillain-Barre syndrome. Neurology. 1979;29:743–745. doi: 10.1212/wnl.29.5.743. [DOI] [PubMed] [Google Scholar]
- 94.Lawrenson J G, Reid A R, Allt G. Molecular characterization of anionic sites on the luminal front of endoneurial capillaries in sciatic nerve. J Neurocytol. 1994;23:29–37. doi: 10.1007/BF01189814. [DOI] [PubMed] [Google Scholar]
- 95.Li C Y, Xue P, Gao C Y, Tian W Q, Liu R C, Yang C. Experimental Campylobacter jejuni infection in the chicken: an animal model of axonal Guillain-Barré syndrome. J Neurol Neurosurg Psychiatry. 1996;61:279–284. doi: 10.1136/jnnp.61.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lior H, Woodward D L, Edgar J A, Laroche L J, Gill P. Serotyping of Campylobacter jejuni by slide agglutination based on heat-labile antigenic factors. J Clin Microbiol. 1982;15:761–768. doi: 10.1128/jcm.15.5.761-768.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lugaresi A, Ragno M, Torrieri F, DiGuglielmo G, Fermani P, Uncini A. Acute motor axonal neuropathy with high titer IgG and IgA anti-GD1a antibodies following Campylobacter enteritis. J Neurol Sci. 1997;147:193–200. doi: 10.1016/s0022-510x(96)05349-x. [DOI] [PubMed] [Google Scholar]
- 98.Mascart-Lemone F O, Duchateau J R, Oosterom J, Butzler J-P, Delacroix D L. Kinetics of anti-Campylobacter jejuni monomeric and polymeric immunoglobulin A1 and A2 response in serum during acute enteritis. J Clin Microbiol. 1987;25:1253–1257. doi: 10.1128/jcm.25.7.1253-1257.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mato M, Ookawara S, Sugamata M, Aikawa E. Evidences for the possible function of the fluorescent granular perithelial cells in brain as scavengers of high molecular-weight waste products. Experientia. 1984;40:399–402. doi: 10.1007/BF01952574. [DOI] [PubMed] [Google Scholar]
- 100.McKhann G M, Cornblath D R, Griffin J W, Ho T W, Li C Y, Jiang Z, Wu H S, Zhaori G, Liu Y, Jou L P, Liu T C, Gao C Y, Mao J Y, Blaser M J, Mishu B, Asbury A K. Acute motor axonal neuropathy: a frequent cause of acute flaccid paralysis in China. Ann Neurol. 1993;33:333–342. doi: 10.1002/ana.410330402. [DOI] [PubMed] [Google Scholar]
- 101.McKhann G M, Cornblath D R, Ho T W, Li C Y, Bai A Y, Wu H S, Yei Q F, Zhang W C, Zhaori Z, Jiang Z, Griffin J W, Asbury A K. Clinical and electrophysiologic aspects of acute paralytic disease of children and young adults in northern China. Lancet. 1991;338:593–597. doi: 10.1016/0140-6736(91)90606-p. [DOI] [PubMed] [Google Scholar]
- 102.McMyne P M S, Penner J L, Mathias R G, Black W A, Hennessy J N. Serotyping of Campylobacter jejuni isolated from sporadic cases and outbreaks in British Columbia. J Clin Microbiol. 1982;16:281–285. doi: 10.1128/jcm.16.2.281-285.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mishu B, Blaser M J. Role of infection due to Campylobacter jejuni in the initiation of Guillain-Barre syndrome. Clin Infect Dis. 1993;17:104–108. doi: 10.1093/clinids/17.1.104. [DOI] [PubMed] [Google Scholar]
- 104.Mishu B, Ilyas A A, Koski C L, Vriesendorp F, Cook S D, Mithen F A, Blaser M J. Serologic evidence of previous Campylobacter jejuni infection in patients with the Guillain-Barre syndrome. Ann Intern Med. 1993;118:947–953. doi: 10.7326/0003-4819-118-12-199306150-00006. [DOI] [PubMed] [Google Scholar]
- 105.Mishu B, Patton C M, Blaser M J. Microbiologic characteristics of Campylobacter jejuni strains isolated from patients with Guillain-Barre syndrome. Clin Infect Dis. 1993;17:538. [Google Scholar]
- 106.Molnar G K, Mertsola J, Erkko M. Guillain-Barre syndrome associated with Campylobacter infection. Br Med J. 1982;285:652. doi: 10.1136/bmj.285.6342.652. . (Letter.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Monos D, Papaioakim M, Argyris E, Iordanidou E, Nachamkin I, Asbury A K, Ho T W, Li C Y, Griffin J W, Cornblath D R, McKhann G M. Differential distribution of HLA alleles in two forms of Guillain-Barre syndrome. Ann Neurol. 1996;40:M121. . (Abstract.) [Google Scholar]
- 108.Moran A P, Appelmelk B J, Aspinall G O. Molecular mimicry of host structures by lipopolysaccharides of Campylobacter and Helicobacter spp.: implications in pathogenesis. J Endotoxin Res. 1996;3:521–531. [Google Scholar]
- 109.Moran A P, Prendergast M M, Appelmelk B J. Molecular mimicry of host structures by bacterial lipopolysaccharides and its contribution to disease. FEMS Immunol Med Microbiol. 1996;16:105–115. doi: 10.1111/j.1574-695X.1996.tb00127.x. [DOI] [PubMed] [Google Scholar]
- 110.Nachamkin I. Campylobacter and Arcobacter. In: Murray P R, Baron E J, Pfaller M A, Tenover F C, Yolken R H, editors. Manual of clinical microbiology. Washington, D.C: ASM Press; 1995. pp. 483–491. [Google Scholar]
- 111.Nachamkin, I. 1997. Microbiologic approaches for studying Campylobacter in patients with Guillain-Barre syndrome. J. Infect. Dis. 176(Suppl. 2):S106–S114. [DOI] [PubMed]
- 112.Nachamkin I, Ung H, Patton C M. Analysis of HL and O serotypes of Campylobacter strains by the flagellin gene typing system. J Clin Microbiol. 1996;34:277–281. doi: 10.1128/jcm.34.2.277-281.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nachamkin I, Yang X-H. Human antibody response to Campylobacter jejuni flagellin protein and a synthetic N-terminal flagellin peptide. J Clin Microbiol. 1989;27:2195–2198. doi: 10.1128/jcm.27.10.2195-2198.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nachamkin I, Yang X-H. Local immune responses to the Campylobacter flagellin in acute Campylobacter gastrointestinal infection. J Clin Microbiol. 1992;30:509–511. doi: 10.1128/jcm.30.2.509-511.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ogawa-Goto K, Funamoto N, Abe T, Nagashima K. Myelin gangliosides of human peripheral nervous system: an enrichment of GM1 in the motor nerve myelin isolated from cauda equina. J Neurochem. 1992;59:1844–1849. doi: 10.1111/j.1471-4159.1992.tb11018.x. [DOI] [PubMed] [Google Scholar]
- 116.Oomes P G, Jacobs B C, Hazenberg M P H, Banffer J R J, van der Meche F G A. Anti-GM1 IgG antibodies and Campylobacter bacteria in Guillain-Barre syndrome, evidence of molecular mimicry. Ann Neurol. 1995;38:170–175. doi: 10.1002/ana.410380208. [DOI] [PubMed] [Google Scholar]
- 117.Osler W. Principles and practice of medicine. New York, N.Y: Appleton; 1892. [Google Scholar]
- 118.Patton C M, Wachsmuth I K. Typing schemes: are current methods useful? In: Nachamkin I, Blaser M J, Tompkins L S, editors. Campylobacter jejuni: current status and future trends. Washington, D.C: American Society for Microbiology; 1992. pp. 110–128. [Google Scholar]
- 119.Patton C M, Wachsmuth I K, Evins G M, Kiehlbauch J A, Plikaytis B D, Troup N, Tompkins L, Lior H. Evaluation of 10 methods to distinguish epidemic-associated Campylobacter strains. J Clin Microbiol. 1991;29:680–688. doi: 10.1128/jcm.29.4.680-688.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Penner J L, Hennessy J N. Passive hemagglutination technique for serotyping Campylobacter fetus subsp. jejuni on the basis of soluble heat-stable antigens. J Clin Microbiol. 1980;12:732–737. doi: 10.1128/jcm.12.6.732-737.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Peterman A F, Daly D D, Dion F R, Keith H M. Infectious neuronitis (Guillain-Barre syndrome) in children. Neurology. 1959;9:533–538. [Google Scholar]
- 122.Plasma Exchange/Sandoglobulin Guillain-Barre Syndrome Trial Group. Randomised trial of plasma exchange, intravenous immunoglobulin, and combined treatments in Guillain-Barre syndrome. Lancet. 1997;349:225–230. [PubMed] [Google Scholar]
- 123.Poduslo J F, Curran G L. Macromolecular permeability across the blood-nerve and blood-brain barrier. Proc Natl Acad Sci USA. 1994;91:5705–5709. doi: 10.1073/pnas.91.12.5705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Prineas J W. Acute idiopathic polyneuritis. An electron microscope study. Lab Invest. 1972;26:133–147. [PubMed] [Google Scholar]
- 125.Pryor W M, Freiman J S, Gillies M A, Tuck R R. Guillain-Barre syndrome associated with Campylobacter infection. Aust N Z J Med. 1984;14:687–688. doi: 10.1111/j.1445-5994.1984.tb05033.x. [DOI] [PubMed] [Google Scholar]
- 126.Ramos-Alvarez M, Bessudo L, Sabin A. Paralytic syndromes associated with noninflammatory cytoplasmic or nuclear neuronopathy: acute paralytic disease in Mexican children, neuropathologically distinguishable from Landry-Guillain-Barre syndrome. JAMA. 1969;207:1481–1492. [PubMed] [Google Scholar]
- 127.Rantala H, Uhari M, Niemela M. Occurrence, clinical manifestations, and prognosis of Guillain-Barre syndrome. Arch Dis Child. 1991;66:706–708. doi: 10.1136/adc.66.6.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rees J H, Gregson N A, Hughes R A C. Anti-ganglioside GM1 antibodies in Guillain-Barre syndrome and their relationship to Campylobacter jejuni infection. Ann Neurol. 1995;38:809–816. doi: 10.1002/ana.410380516. [DOI] [PubMed] [Google Scholar]
- 129.Rees J H, Soudain S E, Gregson N A, Hughes R A. Campylobacter jejuni infection and Guillain-Barre syndrome. N Engl J Med. 1995;333:1374–1379. doi: 10.1056/NEJM199511233332102. [DOI] [PubMed] [Google Scholar]
- 130.Rees J H, Vaughan R W, Kondeatis E, Hughes R A C. HLA-class II alleles in Guillain-Barre syndrome and Miller Fisher syndrome and their association with preceding Campylobacter jejuni infection. J Neuroimmunol. 1995;62:53–57. doi: 10.1016/0165-5728(95)00102-8. [DOI] [PubMed] [Google Scholar]
- 131.Reller L B, Mirrett S, Reimer L G. Abstracts of the Annual Meeting of the American Society for Microbiology. Washington, D.C: American Society for Microbiology; 1983. Controlled evaluation of an improved selective medium for isolation of Campylobacter jejuni, abstr. C-274; p. 357. [Google Scholar]
- 132.Rhodes K M, Tattersfield A E. Guillain-Barre syndrome associated with Campylobacter infection. Br Med J. 1982;285:173–174. doi: 10.1136/bmj.285.6336.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Roberts M, Willison H, Vincent A, Newsom-Davis J. Serum factor in Miller-Fisher variant of Guillain-Barre syndrome and neurotransmitter release. Lancet. 1994;343:454–455. doi: 10.1016/s0140-6736(94)92694-8. [DOI] [PubMed] [Google Scholar]
- 134.Ropper A H. Severe acute Guillain-Barre syndrome. Neurology. 1986;36:429–432. doi: 10.1212/wnl.36.3.429. [DOI] [PubMed] [Google Scholar]
- 135.Ropper A H. Campylobacter diarrhea and Guillain-Barre syndrome. Arch Neurol. 1988;45:655–656. doi: 10.1001/archneur.1988.00520300075022. [DOI] [PubMed] [Google Scholar]
- 136.Rostami A M. Guillain Barre syndrome: clinical and immunological aspects. Springer Semin Immunopathol. 1995;17:29–42. doi: 10.1007/BF00194098. [DOI] [PubMed] [Google Scholar]
- 137.Rostami, A. M. 1997. P2-reactive T cells in inflammatory demyelination of the peripheral nerve. Clin. Infect. Dis. 176(Suppl. 2):S160–S163. [DOI] [PubMed]
- 138.Sacks J J, Lieb S, Baldy L M, Berta S, Patton C M, White M C, Bigler W J, Witte J J. Epidemic campylobacteriosis associated with a community water supply. Am J Public Health. 1986;76:424–428. doi: 10.2105/ajph.76.4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Saida K, Saida T, Brown M J, Silberberg D H. In vivo demyelination induced by intraneural injection of antigalactocerebroside serum. Am J Pathol. 1979;95:99–116. [PMC free article] [PubMed] [Google Scholar]
- 140.Salloway S, Mermel L A, Seamans M, Aspinall G O, Shin J E N, Kurjanczyk A, Penner J L. Miller-Fisher syndrome associated with Campylobacter jejuni bearing lipopolysaccharide molecules that mimic human ganglioside GD3. Infect Immun. 1996;64:2945–2949. doi: 10.1128/iai.64.8.2945-2949.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sanders E A, Peters A C, Gratana J W, Hughes R A C. Guillain-Barre syndrome after varicella-zoster infection. Report of two cases. J Neurol. 1987;234:437–439. doi: 10.1007/BF00314094. [DOI] [PubMed] [Google Scholar]
- 142.Sawant-Mane S, Clark M B, Koski C L. In vitro demyelination by serum antibody from patients with Guillain-Barre syndrome requires terminal complement complexes. Ann Neurol. 1991;29:397–404. doi: 10.1002/ana.410290410. [DOI] [PubMed] [Google Scholar]
- 143.Sawant-Mane S, Estep A, 3rd, Koski C L. Antibody of patients with Guillain-Barre syndrome mediates complement-dependent cytolysis of rat Schwann cells: susceptibility to cytolysis reflects Schwann cell phenotype. J Neuroimmunol. 1994;49:145–152. doi: 10.1016/0165-5728(94)90190-2. [DOI] [PubMed] [Google Scholar]
- 144.Schonberger L B, Hurwitz E S, Katona P, Holman R C, Bregman D J. Guillain-Barre syndrome: its epidemiology and associations with influenza vaccination. Ann Neurol. 1981;9:31–38. doi: 10.1002/ana.410090707. [DOI] [PubMed] [Google Scholar]
- 145.Sheikh, K. A., I. Nachamkin, T. W. Ho, H. J. Willison, J. Veitch, B. S. Ung, C. Y. Li, B.-G. Shen, D. R. Cornblath, A. K. Asbury, G. M. McKhann, and J. W. Griffin. Campylobacter jejuni lipopolysaccharides in Guillain-Barre syndrome: molecular mimicry and host susceptibility. Neurology, in press. [DOI] [PubMed]
- 146.Sjogren E, Lindblom G B, Kaijser B. Comparison of different procedures, transport media, and enrichment media for isolation of Campylobacter species from healthy laying hens and humans with diarrhea. J Clin Microbiol. 1987;25:1966–1968. doi: 10.1128/jcm.25.10.1966-1968.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Skirrow M B. Campylobacter enteritis: a “new” disease. Br Med J. 1977;ii:9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sliman N A. Outbreak of Guillain-Barre syndrome associated with water pollution. Br Med J. 1978;1:751–752. doi: 10.1136/bmj.1.6115.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Speed B, Kaldor J, Cavanagh P. Guillain-Barre syndrome associated with Campylobacter jejuni enteritis. J Infect Dis. 1984;8:85–86. doi: 10.1016/s0163-4453(84)93516-3. [DOI] [PubMed] [Google Scholar]
- 150.Speed B R, Kaldor J, Watson J, Newton-John H, Tee W, Noonan D, Dwyer B W. Campylobacter jejuni/Campylobacter coli associated Guillain-Barre syndrome. Med J Aust. 1987;147:13–16. doi: 10.5694/j.1326-5377.1987.tb133228.x. [DOI] [PubMed] [Google Scholar]
- 151.Stewart G J, Pollard J D, McLeod J G, Wolnizer C M. HLA antigens in the Landry-Guillain-Barre syndrome and chronic relapsing polyneuritis. Ann Neurol. 1978;4:285–289. doi: 10.1002/ana.410040317. [DOI] [PubMed] [Google Scholar]
- 152.Sugita K, Ishii M, Takanashi J, Niimi H, Yuki N. Guillain-Barre syndrome associated with IgM anti-GM1 antibody following Campylobacter jejuni enteritis. Eur J Pediatr. 1994;153:181–183. doi: 10.1007/BF01958981. [DOI] [PubMed] [Google Scholar]
- 153.Sumner A, Said G, Idy I, Metral S. Syndrome de Guillain-Barre. Rev Neurol. 1982;138:17–24. [PubMed] [Google Scholar]
- 154.Sumner A J. The physiology of peripheral nerve disease. W. B. Philadelphia, Pa: Saunders; 1980. [Google Scholar]
- 155.Svedhem A, Kaijser B. Campylobacter fetus subspecies jejuni: a common cause of diarrhea in Sweden. J Infect Dis. 1980;142:353–359. doi: 10.1093/infdis/142.3.353. [DOI] [PubMed] [Google Scholar]
- 156.Tauxe R V. Epidemiology of Campylobacter jejuni infections in the United States and other industrialized nations. In: Nachamkin I, Blaser M J, Tompkins L S, editors. Campylobacter jejuni: current status and future trends. Washington, D.C: American Society for Microbiology; 1992. pp. 9–19. [Google Scholar]
- 157.Taylor D N, Echeverria P, Pitarangsi C, Seriwatana J, Bodhidatta L, Blaser M J. Influence of strain characteristics and immunity on the epidemiology of Campylobacter infections in Thailand. J Clin Microbiol. 1988;26:863–868. doi: 10.1128/jcm.26.5.863-868.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Taylor N S, Elenberger M A, Wu P Y, Fox J G. Diversity of serotypes of Campylobacter jejuni and Campylobacter coli isolated in laboratory animals. Lab Anim Sci. 1989;39:219–221. [PubMed] [Google Scholar]
- 159.Thomas P K. The Guillain-Barre syndrome: no longer a simple concept. J Neurol. 1992;239:361–362. doi: 10.1007/BF00812150. [DOI] [PubMed] [Google Scholar]
- 160.Thornton C A, Latif A S, Emmanuel J C. Guillain-Barre syndrome associated with human immunodeficiency virus infection in Zimbabwe. Neurology. 1991;41:812–815. doi: 10.1212/wnl.41.6.812. [DOI] [PubMed] [Google Scholar]
- 161.Triggs W J, Cros D, Gominak S C, Zuniga G, Beric A I, Shahani B T, Ropper A H, Roongta S M. Motor nerve inexcitability in Guillain-Barre syndrome. Brain. 1992;115:1291–1302. doi: 10.1093/brain/115.5.1291. [DOI] [PubMed] [Google Scholar]
- 162.Tsukada N, Koh C S, Inoue A, Yanagisawa N. Demyelinating neuropathy associated with hepatitis B virus infection. J Neurol Sci. 1987;77:203–216. doi: 10.1016/0022-510x(87)90123-7. [DOI] [PubMed] [Google Scholar]
- 163.Valenciano E N, Perez-Gallardo F, Gonzales A, Enrech J. Outbreak of paralytic illness of unknown etiology in Albecete, Spain. Am J Epidemiol. 1971;94:450–456. [PubMed] [Google Scholar]
- 164.Valenstein P, Pfaller M, Yungbluth M. The use and abuse of routine stool microbiology: a College of American Pathologists Q-probes study of 601 institutions. Arch Pathol Lab Med. 1996;120:206–211. [PubMed] [Google Scholar]
- 165.van der Meche F G A, Schmitz P I M Dutch Guillain-Barre Study Group. A randomized trial comparing intravenous immune globulin and plasma exchange in Guillain-Barre syndrome. N Engl J Med. 1992;326:1123–1129. doi: 10.1056/NEJM199204233261705. [DOI] [PubMed] [Google Scholar]
- 166.Vriesendorp, F. J. 1997. Insights into Campylobacter jejuni induced Guillain-Barre syndrome from the Lewis rat model of experimental allergic neuritis. Clin. Infect. Dis. 176(Suppl. 2):S164–S168. [DOI] [PubMed]
- 167.Vriesendorp F J, Mishu B, Blaser M, Koski C L. Serum antibodies to GM1, peripheral nerve myelin, and Campylobacter jejuni in patients with Guillain-Barre syndrome and controls: correlation and prognosis. Ann Neurol. 1993;34:130–135. doi: 10.1002/ana.410340206. [DOI] [PubMed] [Google Scholar]
- 168.Willison, H., G. O’Hanlon, G. Paterson, C. P. O’Leary, J. Veitch, G. Wilson, M. Roberts, T. Tang, and A. Vincent. 1997. Mechanisms of action of anti-GM1 and anti-GQ1b ganglioside antibodies in Guillain-Barre syndrome. Clin. Infect. Dis. 176(Suppl. 2):S144–S149. [DOI] [PubMed]
- 169.Willison H J, Veitch J, Patterson G, Kennedy P G E. Miller Fisher syndrome is associated with serum antibodies to GQ1b ganglioside. J Neurol Neurosurg Psychiatry. 1993;56:204–206. doi: 10.1136/jnnp.56.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Winer J B, Hughes R A C, Osmond C. A prospective study of acute idiopathic neuropathy. 2. Antecedent events. J Neurol Neurosurg Psychiatry. 1988;51:613–618. doi: 10.1136/jnnp.51.5.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Winer S J, Evans J G. Guillain-Barre syndrome in Oxfordshire: clinical features in relation to age. Age Ageing. 1993;22:164–170. doi: 10.1093/ageing/22.3.164. [DOI] [PubMed] [Google Scholar]
- 172.Wroe S J, Blumhardt L D. Polyneuritis with cranial nerve involvement following Campylobacter jejuni infection. J Neurol Neurosurg Psych. 1985;48:593. doi: 10.1136/jnnp.48.6.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wu S-J, Pazzaglia G, Haberberger R L, Oprandy J J, Sieckmann D G, Watts D M, Hayes C. Detection of immunoglobulin A in urine specimens from children with Campylobacter-associated diarrhea by a chemiluminescent indicator-based Western immunodot assay. J Clin Microbiol. 1993;31:1394–1396. doi: 10.1128/jcm.31.5.1394-1396.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yang L J S, Zeller C B, Shaper N L, Kiso M, Hasegawa A, Shapiro R E, Schnaar R L. Gangliosides are neuronal ligands for myelin-associated glycoprotein. Proc Natl Acad Sci USA. 1996;93:814–818. doi: 10.1073/pnas.93.2.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yuki N. Pathogenesis of axonal Guillain-Barre syndrome: hypothesis. Muscle Nerve. 1994;17:680–682. doi: 10.1002/mus.880170619. [DOI] [PubMed] [Google Scholar]
- 176.Yuki N, Handa S, Tai T, Takahashi M, Saito K, Tsujino Y, Taki T. Ganglioside-like epitopes of lipopolysaccharides from Campylobacter jejuni (PEN 19) in three isolates from patients with Guillain-Barre syndrome. J Neurol Sci. 1995;130:112–116. doi: 10.1016/0022-510x(95)00045-4. [DOI] [PubMed] [Google Scholar]
- 177.Yuki N, Sato S, Fujimoto S, Yamada Y, Kinoshita A, Itoh T. Serotype of Campylobacter jejuni, HLA, and the Guillain-Barre syndrome. Muscle Nerve. 1992;16:968–969. [PubMed] [Google Scholar]
- 178.Yuki N, Sato S, Itoh T, Miyatake T. HLA-B34 and acute axonal polyneuropathy following Campylobacter infection. Neurology. 1991;41:1561–1563. doi: 10.1212/wnl.41.10.1561. [DOI] [PubMed] [Google Scholar]
- 179.Yuki N, Sato S, Tsuji S, Ohsawa T, Miyatake T. Frequent presence of anti-GQ1b antibody in Fisher’s syndrome. Neurology. 1993;43:414–417. doi: 10.1212/wnl.43.2.414. [DOI] [PubMed] [Google Scholar]
- 180.Yuki N, Takahashi M, Tagawa Y, Kashiwase K, Tadokoro K, Saito K. Association of Campylobacter jejuni serotype and antiganglioside antibody in Guillain-Barre syndrome and Fisher’s syndrome. Ann Neurol. 1997;42:28–33. doi: 10.1002/ana.410420107. [DOI] [PubMed] [Google Scholar]
- 181.Yuki N, Taki T, Inagaki F, Kasama T, Takahashi M, Saito K, Handa S, Miyatake T. A bacterium lipopolysaccharide that elicits Guillain-Barre syndrome has a GM1 ganglioside structure. J Exp Med. 1993;178:1771–1775. doi: 10.1084/jem.178.5.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Yuki N, Taki T, Takahashi M, Saito K, Tai T, Miyatake T, Handa S. Penner’s serogroup 4 of Campylobacter jejuni has a lipopolysaccharide that bears a GM1 ganglioside epitope as well as one that bears a GD1a epitope. Infect Immun. 1994;62:2101–2103. doi: 10.1128/iai.62.5.2101-2103.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Yuki N, Taki T, Takahashi M, Saito K, Yoshino H, Tai T, Handa S, Miyatake T. Molecular mimicry between GQ1b ganglioside and lipopolysaccharides of Campylobacter jejuni isolated from patients with Fishers syndrome. Ann Neurol. 1994;36:791–793. doi: 10.1002/ana.410360517. [DOI] [PubMed] [Google Scholar]
- 184.Yuki N, Yamada M, Sato S, Ohama E, Kawase Y, Ikuta F, Miyatake T. Association of IgG anti-GD1a antibody with severe guillain barre syndrome. Muscle Nerve. 1993;16:642–647. doi: 10.1002/mus.880160610. [DOI] [PubMed] [Google Scholar]
- 185.Yuki N, Yoshino H, Sato S, Miyatake T. Acute axonal polyneuropathy associated with anti-GM1 antibodies following Campylobacter enteritis. Neurology. 1990;40:1900–1902. doi: 10.1212/wnl.40.12.1900. [DOI] [PubMed] [Google Scholar]
- 186.Yuki N, Yoshino H, Sato S, Shinozawa K, Miyatake T. Severe acute axonal form of Guillain-Barre syndrome associated with IgG anti-GD1a antibodies. Muscle Nerve. 1992;15:899–903. doi: 10.1002/mus.880150806. [DOI] [PubMed] [Google Scholar]