Abstract
Background
The adoption of an electronic health record (EHR) in the healthcare system has the potential to make healthcare service delivery effective and efficient by providing accurate, up-to-date, and complete information. Despite its great importance, the adoptions of EHR in low-income country settings, like Ethiopia, were lagging and increasingly failed. Assessing the readiness of stakeholders before the actual adoption of EHR is considered the prominent solution to tackle the problem. However, little is known about healthcare providers’ EHR readiness in this study setting. Accordingly, this research was conducted aiming at examining healthcare providers’ readiness for EHR adoption and associated factors in southwestern Ethiopia.
Methods
An institutional-based cross-sectional study was conducted from September 1 to October 30, 2021. A total of 423 healthcare providers working in public hospitals were selected using a simple random sampling technique. Multivariable logistic regression was fitted to identify determinant factors of overall healthcare providers’ readiness after the other covariates were controlled.
Result
In this study, the overall good readiness level of EHR adoption was 52.8% (n = 204) [95% CI of 47.9% to 56.6%]. Age, computer literacy, computer access at health facilities, attitude towards EHRs, awareness about EHRs, perceived benefit, and perceived technology self-efficacy were significantly associated with the overall health care providers’ readiness for the adoption of EHR using a cut point of P-value less than 0.05.
Conclusion
Around half of the respondents had a good level of overall healthcare providers’ readiness for the adoption of EHR which was considered inadequate. This finding implied that a huge effort is required to improve readiness before the actual implementation of EHRs. The finding implied that younger-aged groups were more ready for such technology which in turn implied; the older one needs more concern. Enhancing computer literacy, confidence building to raise self-efficacy of such technology, addressing the issue of computer availability at health facilities, building a positive attitude, awareness campaign of EHR, and recognizing the usefulness of such systems were the necessary measures to improve EHR readiness in this setting.
Additionally, further studies are recommended to encompass all types of EHR readiness such as organizational readiness, technology readiness, societal readiness, and so on. Additionally, exploring the healthcare provider opinion with qualitative study and extending the proposed study to other implementation settings are recommended to be addressed by future works.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-022-07688-x.
Keywords: E-health, Electronic health record, Electronic medical record, EHR adoption, Healthcare provider, Healthcare providers readiness, Health information technology, Pre-implementation phase, Southwest Ethiopia
Introduction
In this digital era, information communication technologies (ICTs) have been widely used and expanded in the healthcare industry to manage big data and voluminous health information [1]. Health information technology (HIT) is a broad concept that encompasses the use of ICT for health care services delivery [2]. The interest in implementing HIT in the healthcare system is growing rapidly worldwide during the past ten years [3, 4]. Among the different HIT initiatives in the international healthcare system, the EHR is seen as the backbone that supports the integration of various e-health tools [5].
According to the International Organization for Standardization (ISO), EHR means a repository of patient data in digital form, stored and exchanged securely, and accessible by multiple authorized users [6]. Adoption of those systems in the healthcare organization has several benefits including minimizing cost, increasing revenue, improving patient care, reducing the need for file space, data confidentiality, reducing medical errors, central patient data management, and sharing medical information [7–12].
Many countries in the world tried to implement an EHR which lead to a 46% global increase in the past five years [13–18]. However, more than 50% of those electronic record projects in the world were failed without providing their targeted benefits [19]. Particularly, the implementation of EHR remains a major challenge in the healthcare systems of low-income countries [20–23]. Only 15% of low-income countries have nationally adopted electronic record systems in health institutions [24]. Sub-Saharan countries are relatively more likely lagging in adopting those technologies due to the digital divide and different social issues such as electrical power interruption, health professionals’ technology resistance, and ICT infrastructure [18, 25–29].
On the other hand, literature shows tremendous progress in using and deploying EHR in a few countries of this region [30, 31]. Previous experience in the implementation of digital technologies implied EHR is feasible and cost-effective in resource-limited settings [32–37].
A readiness assessment is a prominent solution for the effective implementation of EHRs which portrays a proper image of existing conditions and the preparedness of health institutions and health professionals for the new system [38, 39]. Previous frameworks were conceptualized healthcare providers’ readiness as among different types of e-health readiness which is an integrated of core readiness and engagement readiness [33, 40–43].
Studies were conducted to assess healthcare providers’ readiness to adopt EHR in developed countries [44–47]. However, we argue that those results are not representative of the status in low-income countries’ settings due to the variation in digital technology penetration. On the other hand, studies were conducted to assess the organizational readiness level of EHR in low-income countries settings which were rated “inadequate readiness level” [41, 44, 48–51]. But, pre-implementation assessment in this setting rarely addressed EHR readiness in healthcare providers’ context, which was blamed among the main reason for the failure of those EHR projects [52–54].
In Ethiopia, studies had been carried out on knowledge, attitude, willingness, and acceptance of electronic records [18, 25, 55–62]. To the best of the researcher’s knowledge, very few studies were conducted on the readiness of electronic medical records (EMRs) at purposively selected primary health facilities in northwest Ethiopia which showed the level of readiness was 54.1% [63] and 62.3% [64]. Nevertheless, there were limited reports specifically on country-wide healthcare providers’ EHR readiness. Different efforts have been made to implement a digital health information system (HIS) in Ethiopia. The government of Ethiopia deployed District Health Information System 2 (DHIS2) to manage the national reporting system only. Additionally, the ministry of health (MOH) deployed EMR in a few Hospitals of central, eastern, and northern parts of Ethiopia as a pilot. But, the plans to scale up those EMRs to other hospitals were failed [65].
Moreover, the government of Ethiopia proposed to implement country-wide EHR which initiated the authors of this research to investigate the readiness level before the actual implementation. Previous progress in digitalization of healthcare such as the implementation of DHIS2, electronic community health information system (e-CHIS), and EMR in a few hospitals indicated that the implementation capability of the country-wide EHR if the pre-implementation activities are handled effectively and supported with research findings [56, 65–67].
The main hindering factors that influence the readiness of healthcare professionals in the implementation of an EHR are: sex [50, 68], age [50, 69–71], knowledge [30, 45, 50, 72–75], attitude [74, 76, 77], awareness [78, 79], innovativeness [75], training [63, 64, 80], computer literacy [50, 63, 72, 74], workload [81], management support [30, 82], experience [40, 44, 46, 57, 63, 64, 72, 83–86], self-efficacy [41, 68, 87], perceived benefit [30, 77, 88, 89], computer use, and internet access [90].
The authors of this study believed that investigating the user’s readiness and the necessary measurements to be taken is crucial for effective interventions before the adoption of such systems in Ethiopia. This study also enabled policy-makers in resource-limited settings to understand users’ needs before to having the actual system implementation. Therefore, this study was designed first; to show the level of EHR readiness, second, to assess factors impeding health care providers’ readiness towards EHR adoption in southwest Ethiopia.
Methods
Study design and setting
The institutional-based cross-sectional study design was conducted from September 1 to October 30, 2020. The study was conducted at public hospitals in Illu Aba Bora and Buno Bedele Zones, Oromia Region, Southwest Ethiopia. The capital city of Illu Aba Bora and Buno Bedele is Mettu and Bedele respectively. Mettu and Bedele cities are located 600 km and 580 km away from Addis Ababa, the capital city of Ethiopia. The two zones were demarcated as one administrative zone until recent times. The total population of those zones was 1,271,609. Among this, 636,986 and 634,623 were males and females respectively. Farming is the predominant source of income in the community to lead their life. In terms of infrastructure development, there were 5 hospitals (1 referral hospital, 1 General hospital, and 3 Primary hospitals) within the two zones. A total of 41 and 23 health centers were found in Illua Aba Bora and Buno Bedelle Zones respectively.
Study participants, sample size, and sampling procedures
All health professionals permanently working in Illu Aba Bora and Buno Bedele zones, southwest Ethiopia were eligible in this study. The sample size was calculated assuming the prevalence of healthcare providers’ EHR readiness level to be 50% since the study wasn’t found specifically on EHR readiness similar to the current study setting. We also consider the following assumptions: a 95% level of confidence, a 5% of margin of error, and a 5% of non-response rate. Finally, a sample size of 423 was obtained. Five fully functional hospitals and 1,398 healthcare providers working in those hospitals were found in Illu Aba Bora and Buno Bedele Zones during the data collection period of the study. We were proportionally allocated the total sample size, 423, to those five public hospitals found in the two zones. Then, health professionals were randomly selected in those hospitals (See Supplementary file 1 for detail).
Data collection tools and procedure
Data were collected using a pretested self-administered questionnaire. The questionnaire was adapted from related e-health studies conducted elsewhere in the world [30, 49, 50, 63, 85]. Pretested self-administered questioners were used. The content of the questioners contained five parts. Part1 assessed socio-demographic factors, part two was about behavioral and technical factors, part three assessed technological factors, and part four was about organizational factors. The last section of the questioners was about EHR readiness (13 item questions). A total of 76 item questioners, which took from 10–30 min to fill were used.
The validity of the questioners was checked using expert validity. The reliability was also checked using Cronbach alpha’s coefficient (e.g. overall Cronbach alpha for healthcare providers readiness = 0.86). The investigators provided two-day training for data collectors and supervisors. Two master holder health professionals as supervisors and 10 HITs/statisticians as data collectors participated in data the collection process. During data collection, participants were informed about the objective and processes of the study and the confidentiality of the information.
Measurements
In this study, we used the mean and median scores to dichotomize our variables such as EHR readiness, knowledge, attitude, awareness, computer literacy, personal innovativeness in information technology(PIIT), self-efficacy, perceived benefit, and management support. If the variable was normally distributed, we computed the mean score. On the other hand, we used the median score if the variable was not normally distributed [50, 64, 91].
Healthcare providers
All professionals working at health facilities and who have at least a diploma certificate in any health and medicine fields were operationalized as healthcare providers in this study [11, 63].
EHR readiness
The preparedness of healthcare providers to embrace changes brought by the introduction of a computerized system. In this study, EHR readiness was defined as stakeholders’ readiness about EHRs [33]. Healthcare providers incorporate both engagement and core readiness. Accordingly, we were concerned about healthcare providers’ overall readiness. So, we used a sum-up of engagement and core readiness [33, 50].
A total of 13 item Likert scale questioners were used in which 8 of those about core readiness and 5 of the items about engagement readiness. Engagement Readiness refers to the involvement of healthcare providers using EHR [33, 41]. Core Readiness refers to the need of EHR related to current conditions which include the importance of needs, planning, and accessibility such as appropriateness of EHR technology and integration of this technology with existing healthcare services, as well related to the core attributes of the target population that leads to the need for change [33, 41, 50]. In this case, respondents who scored the mean and above were considered as having a good level of healthcare providers’ readiness to adopt EHR. On the other hand, respondents who were scored below the mean were considered as having a poor level of healthcare providers’ readiness to adopt EHR [63, 64].
EHR knowledge
We used fourteen Likert scale questions that deal with the three aspects of EHR including what is EHR, fields of its application, and methods of its use. The questions ranged from “1=strongly disagree to 5= strongly agree”. Respondents were responded by “yes”, “No” or “Do not know”. Knowledge score was calculated as follows: 1 point for a correct answer and 0 points for don’t know & incorrect answer. Respondents who scored the mean and above were considered as having good knowledge, whereas those who scored below the mean were considered as having poor knowledge [45, 50, 78].
EHR attitude
Professional feeling towards using EHR. The attitude of the study participants was assessed by using six-item questions rated on a five-point Likert scale that ranged from "1 = strongly disagree" to "5 = strongly agree". Then, the scores of the Likert scale statement were dichotomized into two. Study participants who scored equal to and above the mean were considered as having a favorable attitude whereas participants who scored below the mean were considered as having an unfavorable attitude [45, 76, 92, 93].
Awareness toward EHR
This was measured by three Likert scale questions. Respondents were asked if they were aware of the relevant application of computerization in health care, the existence of EHR systems, and the benefit of EHR technologies. Study participants who scored the median and above were considered as aware of EHRs [74, 79].
Computer literacy
It was defined as the computer-related knowledge in a capacity to obtain, communicate, process, and understand the basic information to make appropriate health decisions. It was measured by five items of Likert scale questions ranging from”1 = strongly disagree to 5 = strongly agree”. Respondents who scored median and above were considered as having high computer literacy and those who were scored below the median score were indicated as having low computer literacy [63, 64].
Perceived self-efficacy
We used a modified computer self-efficacy scale which was adapted to be used by clinicians. This is a perceived technology self-efficacy to adopt electronic health records. Participants were asked to rate their confidence in using new EHR technologies, if available. A total of ten Likert scale questions ranging from “1 = strongly disagree to 5 = strongly agree” were used. Respondents who scored mean and above were considered as having good efficacy [41, 87, 94].
PIIT
It indicated "the willingness of an individual to try out any new information technology (IT)”. It was measured by four-item Likert scale questions ranging from “1 = strongly disagree to 5 = strongly agree”. Respondents who scored mean and above were considered innovative in IT [70].
Perceived benefit
This is assessing the participants’ subjective expected benefit from adopting the EHR system. It was measured by fourteen Likert scale questions ranging from “1 = no value to 5 = very important value” [41]. Respondents who scored mean and above were recoded as valuable and those who scored below mean were recoded as not valuable [41, 49].
Top management support
The necessary supports provided by senior managers that were measured with four-item Likert scale questions ranged from “1 = strongly disagree to 5 = strongly agree”. Respondents who scored mean and above were considered as having good management support and those who scored below the mean were considered as having poor management support [49].
Data processing and analysis
Data were entered checked, cleaned, and edited using Epi-data version 4.6. Then, the data were exported to STATA version 14.1 for further analysis. Binary logistic regression analysis was conducted to discover the effect of each study variable on the outcome variable. Predictor variables having a P-value < 0.2 on the bivariate analysis were entered into a multivariable logistic regression analysis to check for confounding effects. A forward stepwise technique was applied to identify explanatory variables that have a significant association with the outcome variables to build the multilevel Model. The strength of association was described at 95% CI and P-value less than 0.05 was considered as a cut point for multivariable logistic regression analysis. A multicollinearity test was conducted for the model and none of the variables scored above 10 for the test statistic.
Results
Socio-demographic characteristics
From 423 distributed questioners, 386 responses were received (with a response rate of 91.3%). Two hundred twenty-five (58.3%) of the respondents were males. In terms of health facility, 153(39.6%), 101(26.2%), and 132(34.2%) of the respondents were working at primary hospitals, general hospitals, and referral hospitals respectively. The mean age of the participants was 29.53 ± 8.7 years. The majority, 263(68.1%) of the respondents were first-degree holders.
This study revealed that the majority, 110(28.5%) of the respondents were nurses. In terms of the working unit, 149(38.6%) and 125(32.4%) of the respondents were working in IPD and OPD wards respectively. One hundred sixty-three (42.2%) of the respondents had less than six-year of experience and the mean of experience was 6.8 ± 5.3 years. On the other hand, 145(37.6%) of the respondents were responded as they had a workload in their facilities. Among the total respondents, 84(21.8%) were management members. In terms of their monthly income, 260(67.4%) of the study participants had salaries greater than 5,000 ETB (See Table 1 for details).
Table 1.
Socio-demographic characteristics of healthcare providers working at public hospitals in Southwest Ethiopia, 2021
| Variable | Category | Frequency (#) | Percent (%) | |
|---|---|---|---|---|
| Sex | Female | 161 | 41.7% | |
| Male | 225 | 58.3% | ||
| Type of health facility | Primary hospital | 153 | 39.6% | |
| General hospital | 101 | 26.2% | ||
| Referral hospital | 132 | 34.2% | ||
| Age | 21–30 | 214 | 55.4% | |
| 31–50 | 135 | 35.0% | ||
| > = 51 | 37 | 9.6% | ||
| Religion | Orthodox | 122 | 31.6% | |
| Muslim | 72 | 18.6% | ||
| Protestant | 179 | 46.4% | ||
| Others | 13 | 3.4% | ||
| Educational level | Diploma | 99 | 25.7% | |
| B.Sc. degree | 263 | 68.1% | ||
| Master and above | 24 | 6.2% | ||
| Profession/educational background | Medicine | 51 | 13.2% | |
| Nurse | 110 | 28.5% | ||
| Midwife | 89 | 23.1% | ||
| Public health officer | 45 | 11.6% | ||
| Pharmacy | 37 | 9.6% | ||
| Laboratory | 32 | 8.3% | ||
| Others | 22 | 5.7% | ||
| Ward | OPD | 125 | 32.4% | |
| IPD | 149 | 38.6% | ||
| MCH | 67 | 17.3% | ||
| Others | 45 | 11.7% | ||
| Work experience | Less than 6 | 163 | 42.2% | |
| 6–10 | 137 | 35.5% | ||
| Greater than 11 | 86 | 22.3% | ||
| Workload | No | 241 | 62.4% | |
| Yes | 145 | 37.6% | ||
| Management(mgt) member | Staff | 302 | 78.2% | |
| Mgt Member | 84 | 21.8% | ||
| Salary(in ETB) | < = 5,000 ETB | 126 | 32.6% | |
| > 5,000 ETB | 260 | 67.4% | ||
Behavioral and technical factors
In this study, behavioral and technical factors were incorporated awareness, EHR knowledge, Attitude toward EHR, PIIT, computer skill, perceived benefit, and perceived self-efficacy. Accordingly, 335(86.8%) of the respondents had awareness about EHR. On the other hand, 161(41.7%) and 181 (46.9%) of the respondents had good knowledge and favorable attitude respectively. The PIIT was 145(37.6%). Two hundred four (52.8%) of the respondents had sufficient computer Literacy. About, 183(47.4%) of the respondents had high perceived self-efficacy (See Table 2 for details).
Table 2.
Behavioral and technical factors among healthcare providers working at public hospitals in Southwest Ethiopia, 2021
| Variable | Category | Frequency (#) | Percent (%) |
|---|---|---|---|
| Awareness | Not aware | 51 | 13.2% |
| Aware | 335 | 86.8% | |
| EHR knowledge | Poor | 225 | 58.3% |
| Good | 161 | 41.7% | |
| Attitude toward EHR | Unfavorable | 205 | 53.1% |
| Favorable | 181 | 46.9% | |
| PIIT | Poor | 241 | 62.4% |
| Good | 145 | 37.6% | |
| Computer literacy | insufficient | 182 | 47.2% |
| sufficient | 204 | 52.8% | |
| Perceived benefit | No | 29 | 7.5% |
| Yes | 357 | 92.5% | |
| self-efficacy | Low | 203 | 52.6% |
| High | 183 | 47.4% |
Organizational and access to basic technology-related factors
Among the total respondents, only 91(23.6%) of them agreed that they had IT technical support in their health facility. In terms of superior management support, 148(38.3%) of the respondents got this support. The result of this study implied that almost no EHR training, which was 23(6.0%). Functional computer access in the working unit was 107(27.7%). On the other hand, only 58(15.0%) had an EHR manual in the working unit. One hundred thirty-four (34.7%) of the respondents accessed the internet service.
Additionally, 284(26.4%) of the respondents confirmed that they had access to uninterrupted electric power and 83(21.5%) of those respondents used software applications in the department. The report also implied only 34(8.8%) of the respondents used a computer at work daily. Two hundred twenty-nine (59.3%) of the respondents had experience in using email for exchanging information (See Table 3 for details).
Table 3.
Organizational and access to basic technology related factors among health professionals in Southwestern Ethiopia, 2021
| Variable | Category | Frequency (#) | Percent (%) |
|---|---|---|---|
| IT technical support | No | 295 | 76.4% |
| Yes | 91 | 23.6% | |
| Superior management support | No | 238 | 61.7% |
| Yes | 148 | 38.3% | |
| EHR Training | No | 363 | 94.0% |
| Yes | 23 | 6.0% | |
| Availability of functional computer at working unit | No | 279 | 72.3% |
| Yes | 107 | 27.7% | |
| EHR manual in the working unit | No | 328 | 85.0% |
| Yes | 58 | 15.0% | |
| Internet access in the working unit | No | 252 | 65.3% |
| Yes | 134 | 34.7% | |
| Uninterrupted electric power | No | 284 | 73.6% |
| Yes | 102 | 26.4% | |
| Software application in the department | No | 303 | 78.5% |
| Yes | 83 | 21.5% | |
| How often do you use a computer at work? | Never | 98 | 25.4 |
| Sometimes | 254 | 65.8 | |
| Daily | 34 | 8.8 | |
| Experience in using email for information exchange | No | 157 | 40.7% |
| Yes | 229 | 59.3% |
Readiness to adopt electronic health record
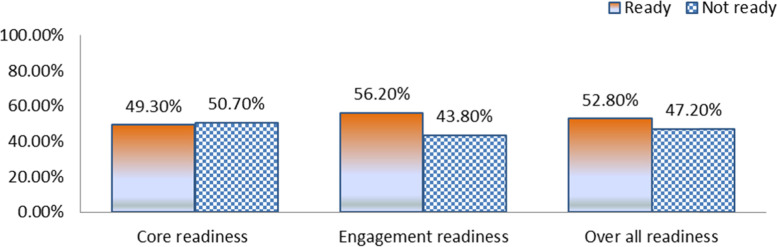
In this study, the overall EHRs adoption readiness was 52.8% (n = 204) [95% CI of 47.9% to 56.6%]. Among those, 190 (49.3%) had core readiness whereas 217 (56.2%) had engagement readiness (See Fig. 1 for detail).
Fig. 1.
Readiness to adopt electronic health record
Factors associated with readiness to adopt EHR
From the total variables entered into the bi-variable logistic regression model, age, computer skill, computer access, attitude, knowledge, awareness, perceived benefit, perceived self-efficacy, PIIT, training, and availability of technical support were factors associated with readiness to adopt EHR in the bi-variable analysis at P-value less than 0.02. Consequently, those variables were subjected to the multivariable logistic regression analysis to control potential confounders.
In the multivariate logistic regression analysis, respondents who were bellow age groups of less than 30 [AOR = 2.25, 95% CI (1.33–3.82)], computer literacy [AOR = 5.02, 95% CI (2.90–8.71)], computer access at health facilities[AOR = 2.76, 95% CI(1.44–5.27)], attitude towards EHRs [AOR = 4.60, 95% CI(2.63–8.04)], awareness about EHRs [AOR = 1.79, 95% CI(1.93–4.18)], perceived benefit about EHRs [AOR = 4.59, 95% CI(1.62–12.99)], and perceived technology self-efficacy [AOR = 4.7, 95% CI(2.71–8.17)] were significantly associated with overall health care providers readiness for the adoption of EHR at P-value less than 0.05 (See Table 4 for detail).
Table 4.
Multivariable logistic regression factors associated with the healthcare providers’ readiness level
| Variables | Category | EHR readiness level | Odds Ratio (95% CI) | ||
|---|---|---|---|---|---|
| Poor | Good | Crude (COR) | Adjusted (AOR) | ||
| Age | Above 30 | 97 | 75 | 1 | 1 |
| Bellow 30 | 85 | 129 | 1.96(1.31,2.95) | 2.25(1.33,3.82)* | |
| Computer literacy | Poor | 131 | 51 | 1 | 1 |
| Good | 53 | 151 | 7.32(4.67,11.48) | 5.02(2.90, 8.71)* | |
| Computer access | No | 160 | 119 | 1 | 1 |
| Yes | 22 | 85 | 5.19(3.07,8.79) | 2.76(1.44,5.27) * | |
| Attitude toward EHR | Unfavorable | 125 | 80 | 1 | 1 |
| Favorable | 57 | 124 | 3.40(2.23,5.18) | 4.60(2.63,8.04)* | |
| EHR knowledge | Poor knowledge | 127 | 98 | 1 | 1 |
| Good knowledge | 55 | 106 | 2.49(1.64,3.79) | 1.20(0.71,2.05) | |
| Awareness towards EHR | Not aware | 31 | 20 | 1 | |
| Aware | 151 | 184 | 1.90(1.03,3.45) | 1.79(1.93,4.18)* | |
| Perceived Innovativeness | No | 131 | 110 | 1 | 1 |
| Yes | 51 | 94 | 2.19(1.43,3.36) | 0.76(0.42,1.40) | |
| Perceived Benefit | Not beneficial | 24 | 5 | 1 | 1 |
| Beneficial | 180 | 177 | 4.72(1.76,12.65) | 4.59(1.62,12.99)* | |
| Perceived self-efficacy | Low | 130 | 73 | 1 | 1 |
| High | 52 | 131 | 4.49(2.92,6.90) | 4.7(2.71,8.17)* | |
| EHR training | No | 176 | 187 | 1 | 1 |
| Yes | 6 | 17 | 2.67(1.03,6.92) | 1.92(0.61,6.01) | |
| Technical support | No | 151 | 144 | 1 | 1 |
| Yes | 31 | 60 | 2.03(1.24, 3.31) | 1.87(0.95, 3.68) | |
*P-value < 0.05 for multivariable analysis, 1 = reference category
Discussion
This research assessed healthcare providers’ EHR readiness and associated factors in Southwest Ethiopia. Even if there are different types of EHR readiness, we, the authors of this research, focused on healthcare providers’ readiness. The overall healthcare providers’ readiness consisted of engagement readiness and core readiness. The overall good readiness level to implement EHR was 52.8% (n = 204) [95% CI of 47.9% to 56.6%]. One hundred ninety (49.3%) had a good level of core readiness whereas 217 (56.2%) had a good level of engagement readiness. Our finding corresponds with previous studies in Northern Ethiopia in which e-health readiness specifically to EMR was 54.1% [63], and also another study in Northern Ghana in which the overall readiness to implement EHR was 54.9% [50]. It was also in line with the study conducted in Iran and Myanmar in which the overall EHR readiness level was 56.0% [47] and 54.2% [73] respectively.
Our finding was comparably lower than previous findings of Northern Ethiopia in which the overall readiness of health professionals for an EMR system was 62.3% [64]. This could be due to the study in Northern Ethiopia being conducted at primary health facilities only whereas our study was incorporated primary hospitals, general hospitals, and referral hospitals. Additionally, the study conducted in Northern Ethiopia was using purposively selected primary health facilities which might inflate the report.
The finding was lower than the previous study in California whereas 73.0% [95] of fourth-year medical students were ready in using EHR. This could be due to the study setting and the variation in ICT infrastructure between the two countries. The other possible justification could be in the study of California, the EHR was already deployed but it was in the pre-implementation phase in the current study setting.
The current finding was slightly lower than the study conducted in Iran in which the level of EHR readiness was 57.2% [96]. This variation could be due to the study setting and study participants in which the study in Iran was conducted among nurses only. The other possible justification could be the tool variation and differences in ICT infrastructure. The study in Iran was conducted at one referral hospital only which might be the reason for this discrepancy. On the contrary, the finding in the current study was higher than the other study reported in Iran in which 28.6% [45] were ready for pre-implementation. This variation could be due to the variation in tools used, the study period, and the sampling technique. The study conducted in Iran used a survey of health workers found in one general hospital which might be the other possible reason for this variation.
Readiness to adopt EHRs was interlinked with socio-demographic, behavioral, technical, technological, and organizational factors. Healthcare providers aged below 30 were more likely to be ready to adopt EHR compared to who were aged above 30. This finding was supported by previous reports which stated younger aged healthcare providers were more engaged in using technology [50, 69]. The possible justification for this finding could be the innovative potential of the younger people. This implied that younger people are early adopters of e-health which strengthens previous research findings in e-health and IT technology adoption [71, 97].
The odd of healthcare providers who had favorable attitude were more likely to be ready than those who had unfavorable attitude. The finding was in line with previous studies [45, 74, 76, 77]. The possible justification for this could be the positive evaluation of healthcare providers to those technologies is a driving force to be more eager and committed to engaging in EHR.
Our finding implied healthcare providers who had good awareness were more likely to be ready. This finding was consistent with previous research findings [78, 79]. This implied that awareness campaigns enabled individuals to understand the values of EHRs and to take action.
The study implied that computer literacy played an important role in determining healthcare providers’ readiness to adopt EHRs in which respondents with high computer literacy were more ready than counterparts. This finding was supported by previous reports elsewhere in the world [50, 63, 72, 74]. This could be due to such skills helping to perform tasks in any computerized technology. This implied that computer skill is essential to processing and presenting information in computerized technology like EHR.
The study revealed healthcare providers were more likely to be ready when they believed that EHR is more beneficial. This finding was corresponding with previous research findings [30, 77]. This could be since healthcare providers who considered EHRs as beneficial were more likely to be motivated and be ready.
This study found that healthcare providers who had a good perceived self-efficacy were more likely to be ready. This finding was in line with previous studies elsewhere in the world [41, 68, 87]. This could be due to computer self-efficacy influencing individuals to be confident in their skills and abilities to perform tasks related to computer technology.
Healthcare providers who got computer access at facilities were ready to EHRs. This finding was supported by previous reports elsewhere in the world [63, 64]. This could be due to the availability of computer-enabled ones to practice digital tools. Moreover, computer accesses allow the daily practice of e-health technologies, so it enhances the skill and confidence to engage in EHR.
Strengths and limitations of the study
This study was the first study in Ethiopia to assess the detailed measurements to be taken in improving healthcare providers’ readiness level before EHR implementation. It also presented some highlights for measurements to be taken before EHR implementation in low-income country settings. However, causality cannot be inferred since the study was cross-sectional. The major limitation of the study was that it didn’t triangulate with qualitative findings. Additionally, it didn’t incorporate other types of readiness for instance organizational and technology readiness since there isn’t a compressive tool to incorporate all types of EHR health readiness.
Conclusions
Around half of the respondents had a good level of overall readiness for the adoption of EHR which was considered inadequate. This finding implied that a huge effort is required to improve readiness before the actual implementation of EHRs. Particularly above half of the healthcare providers had poor core readiness levels. What we have learned from this statement is that most of the healthcare providers were highly dissatisfied with the existing paper-based system and eager to implement EHR. The finding implied that younger-aged groups were more eager for such technology which in turn implied the older ones need more concern.
Enhancing computer literacy, building their confidence to rise self-efficacy such technology, building a positive attitude, awareness campaign of HER, and recognizing the usefulness of such systems were the necessary measures to improve EHR readiness in this setting. Further studies are recommended to encompass all types of EHR readiness such as organizational readiness, technology readiness, societal readiness, and so on. Additionally, exploring healthcare providers’ opinions with qualitative study and extending the proposed study to other implementation settings are recommended to be addressed by future works.
Supplementary Information
Acknowledgements
The authors are indebted to the Mettu University College of health science ethical review board for the approval of ethical clearance and each hospital for giving a supporting letter. The authors would like to extend their heartfelt thanks to healthcare providers, data collectors, and supervisors who participated in this study.
Abbreviations
- AOR
Adjusted Odds Ratio
- CI
Confidence Intervals
- COR
Crude Odds Ratio
- DHIS2
District Health Information System Two
- e-CHIS
Electronic Community Health Information System
- e-Health
Electronic Health
- EHR
Electronic Health Record System
- EMR
Electronic Medical Record
- HIS
Health Information System
- HIT
Health Information Technology
- ICT
Information Communication Technology
- ISO
International Organization for Standardization
- IT
Information Technology
- MOH
Ministry of Health
- PIIT
Personal Innovativeness in Information Technology
Authors’ contributions
HSN and SYK made significant contributions in the conception, design, data collection, supervision, data curation, investigation, data analysis, interpretation, and write-up of the manuscript. EBE and AAC have contributed to developing the proposal, validation, revising the manuscript, preparing figures, analysis, visualization, and interpretation of data as well. Finally, all authors (HSN, SYK, AAC, and EBE) reviewed and approved the final manuscript.
Funding
The author(s) received no specific funding for this work.
Availability of data and materials
The data will be available upon request from the corresponding author.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the ethical review board of Mettu University College of Health Science with ethical reference number: RPG/90/13. Informed consent was obtained from each study participant after they were informed of the objective and benefits of the study. To keep the confidentiality of the respondents, the data collection procedure was anonymous. Additionally, this study was conducted following the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing of interests
The authors have declared that no competing interests exist.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Habtamu Setegn Ngusie, Email: habtamuhi3@gmail.com.
Sisay Yitayih Kassie, Email: sishaimanot@gmail.com.
Alex Ayenew Chereka, Email: zemeneayenew@gmail.com.
Ermias Bekele Enyew, Email: ermiashi@gmail.com.
References
- 1.Aceto G, Persico V, Pescapé A. The role of Information and Communication Technologies in healthcare: taxonomies, perspectives, and challenges. J Netw Comput Appl. 2018;107(1):125–154. [Google Scholar]
- 2.Organization, W.H., Global diffusion of eHealth: making universal health coverage achievable: report of the third global survey on eHealth. 2017: World Health Organization.
- 3.Sligo J, et al. A literature review for large-scale health information system project planning, implementation and evaluation. Int J Med Informatics. 2017;97(3):86–97. doi: 10.1016/j.ijmedinf.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Sittig DF, Singh H. A new socio-technical model for studying health information technology in complex adaptive healthcare systems. Cognitive informatics for biomedicine. 2015;153(5):59–80. [Google Scholar]
- 5.LaForge K, et al. How 6 organizations developed tools and processes for social determinants of health screening in primary care: an overview. J Ambul Care Manage. 2018;41(1):2–14. doi: 10.1097/JAC.0000000000000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oliveira M, et al. Using ISO 25040 standard for evaluating electronic health record systems. Studies in Health Technology and Informatics. 2013;192:1137–1159. [PubMed] [Google Scholar]
- 7.Bagayokoa C, et al. Can ICTs contribute to the efficiency and provide equitable access to the health care system in Sub-Saharan Africa? The Mali experience. Yearb Med Inform. 2011;20(1):33–38. [PubMed] [Google Scholar]
- 8.Waithera L, Muhia J, Songole R. Impact of electronic medical records on healthcare delivery in Kisii Teaching and Referral Hospital. Med Clin Rev. 2017;3(4):21–34. [Google Scholar]
- 9.Williams F, Boren S. The role of the electronic medical record (EMR) in care delivery development in developing countries: a systematic review. J Innov Health Informatics. 2008;16(2):139–145. doi: 10.14236/jhi.v16i2.685. [DOI] [PubMed] [Google Scholar]
- 10.Hamilton C. The WHO-ITU national eHealth strategy toolkit as an effective approach to national strategy development and implementation. Medinfo. 2013;192(7):913–916. [PubMed] [Google Scholar]
- 11.Yehualashet G, Asemahagn M, Tilahun B. The attitude towards and use of electronic medical record system by health professionals at a referral hospital in northern Ethiopia: Cross-sectional study. J Health Informatics in Africa. 2015;3(1):25–37. [Google Scholar]
- 12.Al Alawi S, et al. Physician user satisfaction with an electronic medical records system in primary healthcare centres in Al Ain: a qualitative study. BMJ Open. 2014;4(11):55–69. doi: 10.1136/bmjopen-2014-005569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kortteisto K. Clinical decision support must be useful, functional is not enough: a qualitative study of computer-based clinical decision support in primary care. BMC Health Serv Res. 2012;12(1):349–362. doi: 10.1186/1472-6963-12-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lakew Y, et al. Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reprod Health. 2013;10(1):1–10. doi: 10.1186/1742-4755-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hennemann S, Beutel ME, Zwerenz R. Ready for eHealth? Health professionals’ acceptance and adoption of eHealth interventions in inpatient routine care. J Health Commun. 2017;22(3):274–284. doi: 10.1080/10810730.2017.1284286. [DOI] [PubMed] [Google Scholar]
- 16.Rehana Parvin, B. and M. Md Shahjahan, Knowledge, Attitude, and Practice of E-health among Doctors Working at Selected Private Hospitals in Dhaka, Bangladesh. Journal of Health Communication, 2016. 4(1): p. 15–27. 10.1080/10810730.2017.1284286.
- 17.Ahmad, B.I.e.J.P.T., User acceptance of health information technology (HIT) in developing countries: a conceptual model. Procedia Technology, 2014. 16(3): p. 1287–1296. 10.1016/j.protcy.2014.10.145.
- 18.Antonio A, Tuffley DJFI. The gender digital divide in developing countries. Multidisciplinary Digital Publishing Institute. 2014;6(4):673–687. [Google Scholar]
- 19.Ketikidis P, et al. Acceptance of health information technology in health professionals: an application of the revised technology acceptance model. Health Informatics J. 2012;18(2):124–34. doi: 10.1177/1460458211435425. [DOI] [PubMed] [Google Scholar]
- 20.Hassibian, M.R.J.R.I.J.o.M., Electronic health records acceptance and implementation in developing countries: Challenges and barriers. BMC Women's Health, 2013. 1(1): p. 6–11. 10.5812/rijm.15077.
- 21.Oluyemi A, Olayanju AR. Electronic health record design for inclusion in sub-Saharan Africa medical record informatics. Scientific African. 2017;14(1):10–11. [Google Scholar]
- 22.Odekunle, F.F., R.O. Odekunle, and S.J.I.j.o.h.s. Shankar, Why sub-Saharan Africa lags in electronic health record adoption and possible strategies to increase its adoption in this region. Int J Health Sci, 2017. 11(4): p. 59–64. [PMC free article] [PubMed]
- 23.Tata EB, Ambele MA, Pepper MS. Barriers to Implementing Clinical Pharmacogenetics Testing in Sub-Saharan Africa A Critical Review. Pharmaceutics. 2020;12(9):809–823. doi: 10.3390/pharmaceutics12090809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO. Electronic health record system implementation in healthcare system. World health organization 2020 [Cited 2021 Dec 16]. Available from: https://www.who.int/gho/goe/electronic_health_records/en/.
- 25.Bawack, R.E. and J.R.K.J.I.j.o.m.i. Kamdjoug, Adequacy of UTAUT in clinician adoption of health information systems in developing countries: The case of Cameroon. International Journal of Medical Informatics, 2018. 109(1): p. 15–22. 10.1016/j.ijmedinf.2017.10.016. [DOI] [PubMed]
- 26.Akanbi MO, et al. Use of electronic health records in sub-Saharan Africa: progress and challenges. J Trop Med. 2012;14(1):1. [PMC free article] [PubMed] [Google Scholar]
- 27.Castelnuovo B, et al. Implementation of provider-based electronic medical records and improvement of the quality of data in a large HIV program in Sub-Saharan Africa. PLoS ONE. 2012;7(12):51–63. doi: 10.1371/journal.pone.0051631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Were MC, et al. Creation and evaluation of EMR-based paper clinical summaries to support HIV-care in Uganda. Africa Int J Med Informatics. 2010;79(2):90–96. doi: 10.1016/j.ijmedinf.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yogeswaran P, Wright G. MEDINFO 2010. Johannesburg: IOS Press; 2010. EHR implementation in South Africa: How do we get it right? pp. 396–400. [PubMed] [Google Scholar]
- 30.Jawhari B, et al. Barriers and facilitators to Electronic Medical Record (EMR) use in an urban slum. Int J Med Informatics. 2016;94(3):246–254. doi: 10.1016/j.ijmedinf.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 31.Katurura, M.C., L.J.A.j.o.p.h.c. Cilliers, and f. medicine, Electronic health record system in the public health care sector of South Africa: A systematic literature review. African Journal of Primary Health Care & Family Medicine, 2018. 10(1): p. 1–8. 10.4102/phcfm.v10i1.1746 [DOI] [PMC free article] [PubMed]
- 32.Miyazaki K, et al. Assessing the feasibility of introducing an electronic health information system into Tuberculosis clinics and laboratories in Myanmar. Global Health & Medicine. 2020;2(4):247–254. doi: 10.35772/ghm.2020.01020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gallego, A.I., M.-P. Gagnon, and M.J.J.o.t.A.A.o.D. Desmartis, Assessing the cost of electronic health records: a review of cost indicators. Mary Ann Liebert Journal, 2010. 16(9): p. 1–8. 10.1089/tmj.2010.0014. [DOI] [PubMed]
- 34.Pagalday-Olivares P, et al. Exploring the feasibility of eHealth solutions to decrease delays in maternal healthcare in remote communities of Ghana. BMC Med Inform Decis Mak. 2017;17(1):1–13. doi: 10.1186/s12911-017-0552-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.SalifuYusif AH, Baig JS. An Exploratory Study of the Readiness of Public Healthcare Facilities in Developing Countries to Adopt Health Information Technology (HIT)/e-Health: the Case of Ghana. J Healthcare Info Res. 2020;4(2):189–214. doi: 10.1007/s41666-020-00070-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davies EH, et al. Demonstrating the feasibility of digital health to support pediatric patients in South Africa. Epilepsia Open. 2021;6(4):653–662. doi: 10.1002/epi4.12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.dos Santos Silva EK, et al. Cost-effectiveness in health: consolidated research and contemporary challenges. Humanities and Social Sciences Communications. 2021;8(1):1–10. [Google Scholar]
- 38.Kabelo Leonard Mauco, R.E.S., Maurice Mars Validation of an e-health readiness assessment framework for developing countries. BMC Health Services Research, 2020. 13(4): p. 575–593. 10.1186/s12913-020-05448-3. [DOI] [PMC free article] [PubMed]
- 39.Mauco KL, Scott RE, Mars M. Critical analysis of e-health readiness assessment frameworks: suitability for application in developing countries. J Telemed Telecare. 2018;24(2):110–117. doi: 10.1177/1357633X16686548. [DOI] [PubMed] [Google Scholar]
- 40.Mauco, K.L., R.E. Scott, and M.J.B.h.s.r. Mars, Validation of an e-health readiness assessment framework for developing countries. BMC Health Services Research, 2020. 20(1): p. 575–589. 10.1186/s12913-020-05448-3. [DOI] [PMC free article] [PubMed]
- 41.Kabukye JK. N de Keizer, RJPo Cornet, Assessment of organizational readiness to implement an electronic health record system in a low-resource settings cancer hospital: A cross-sectional survey. PloS one. 2020;15(6):234–271. doi: 10.1371/journal.pone.0234711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gholamhosseini L, Ayatollahi H. The design and application of an e-health readiness assessment tool. Health Information Management Journal. 2017;46(1):32–41. doi: 10.1177/1833358316661065. [DOI] [PubMed] [Google Scholar]
- 43.Mauco KL, Scott RE, Mars M. Development of an eHealth readiness assessment framework for Botswana and other developing countries: interview study. JMIR Med Inform. 2019;7(3):129–149. doi: 10.2196/12949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ajami S, et al. Readiness assessment of electronic health records implementation. Acta Informatica Medica. 2011;19(4):224–227. doi: 10.5455/aim.2011.19.224-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ghazisaeidi M, et al. An assessment of readiness for pre-implementation of electronic health record in Iran: a practical approach to implementation in general and teaching hospitals. Acta Med Iran. 2014;52(7):532–544. [PubMed] [Google Scholar]
- 46.Habibi-Koolaee M, Safdari R, Bouraghi H. Nurses readiness and electronic health records. Acta Inform Med. 2015;23(2):105–107. doi: 10.5455/aim.2015.23.105-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mirkarimi, A. and N.J.F.i.H.I. Behnampour, Readiness assessment of laboratory and imaging staff to implement electronic health records. Frontiers in Health Informatics, 2014. 3(2): p. 5–8. 10.5455/aim.2011.19.224-227.
- 48.Cherry, B.J.J.o.G.N., Assessing organizational readiness for electronic health record adoption in long-term care facilities. Journal of Gerontological Nursing, 2011. 37(10): p. 14–19. 10.3928/00989134-20110831-06. [DOI] [PubMed]
- 49.Paré G, et al. Clinicians' perceptions of organizational readiness for change in the context of clinical information system projects: insights from two cross-sectional surveys. Implement Sci. 2011;6(1):1–14. doi: 10.1186/1748-5908-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abdulai, A.-F. and F.J.P.o. Adam, Health providers’ readiness for electronic health records adoption: A cross-sectional study of two hospitals in northern Ghana. PloS one, 2020. 15(6): p. 231–256. 10.1371/journal.pone.0231569. [DOI] [PMC free article] [PubMed]
- 51.Durrani, H., et al. Health needs and eHealth readiness assessment of health care organizations in Kabul and Bamyan, Afghanistan. 2012 [Cited 2022 Jan 6]; 663–670]. Available from: https://apps.who.int/iris/handle/10665/118165. [DOI] [PubMed]
- 52.Granja C, Janssen W, Johansen MA. Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res. 2018;20(5):102–135. doi: 10.2196/10235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li J, et al. Health care provider adoption of eHealth: systematic literature review. Interactive journal of medical research. 2013;2(1):2468–2474. doi: 10.2196/ijmr.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khan I, et al. Investigating factors impelling the adoption of e-health: a perspective of African expats in China. SAGE Open. 2019;9(3):215–228. [Google Scholar]
- 55.Ahmed MH, et al. Intention to use electronic medical record and its predictors among health care providers at referral hospitals, north-West Ethiopia, 2019: using unified theory of acceptance and use technology 2 (UTAUT2) model. BMC Med Inform Decis Mak. 2020;20(1):1–11. doi: 10.1186/s12911-020-01222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berihun, B., D.D. Atnafu, and G.J.B.R.I. Sitotaw, Willingness to Use Electronic Medical Record (EMR) System in Healthcare Facilities of Bahir Dar City, Northwest Ethiopia. BioMed Research International, 2020. 2020(5): 2. 10.1155/2020/3827328. [DOI] [PMC free article] [PubMed]
- 57.Bisrat A, et al. Implementation challenges and perception of care providers on Electronic Medical Records at St. Paul’s and Ayder Hospitals. Ethiopia. BMC Med Inform Decis Mak. 2021;21(1):1–12. doi: 10.1186/s12911-021-01670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gebre-Mariam, M., et al. An electronic medical record (EMR) implementation framework for HIV care and treatment facilities in Ethiopia. 2012 [Cited 2022 Jan 30]; Available from: http://www.longwoods.com/content/22930.
- 59.Oumer A. Utilization of Electronic Medical Record and Associated Factors Among Health Professionals in Public Health Facilities With Service Delivery. Eastern Ethiopia. BMC Women's Health. 2020;7(4):123–135. [Google Scholar]
- 60.Yehualashet DE, et al. Barriers to the Adoption of Electronic Medical Record System in Ethiopia: A Systematic Review. J Multidiscip Healthc. 2021;14(3):25–37. doi: 10.2147/JMDH.S327539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shiferaw, K.B. and E.A.J.I.i.M.U. Mehari, Modeling predictors of acceptance and use of electronic medical record system in a resource limited setting: Using modified UTAUT model. Informatics in Medicine Unlocked. 2019. 17(2): 101–118. 10.1016/j.imu.2019.100182.
- 62.Kalayou MH, Endehabtu BF, Tilahun B. The Applicability of the Modified Technology Acceptance Model (TAM) on the Sustainable Adoption of eHealth Systems in Resource-Limited Settings. J Multi Healthcare. 2020;13(1):1827–1845. doi: 10.2147/JMDH.S284973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Biruk S, et al. Health Professionals’ readiness to implement electronic medical record system at three hospitals in Ethiopia: a cross sectional study. BMC Med Inform Decis Mak. 2014;14(1):115. doi: 10.1186/s12911-014-0115-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Awol SM, et al. Health professionals’ readiness and its associated factors to implement electronic medical record system in four selected primary hospitals in Ethiopia. Adv Med Educ Pract. 2020;11(2):147–162. doi: 10.2147/AMEP.S233368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Oumer A, et al. Utilization, Determinants, and Prospects of Electronic Medical Records in Ethiopia. Biomed Res Int. 2021;11(7):285–299. doi: 10.1155/2021/2230618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gebre-Mariam, M., B.J.I. Bygstad, and Organization, Digitalization mechanisms of health management information systems in developing countries. Inform Organ, 2019. 29(1): 1–22. 10.1016/j.infoandorg.2018.12.002.
- 67.Thangasamy P, et al. A pilot study on district health information software 2: challenges and lessons learned in a developing country: an experience from Ethiopia. J Multidiscip Healthc. 2016;3(5):46–51. [Google Scholar]
- 68.Jacobs RJ, et al. The role of self-efficacy, flexibility, and gender in pharmacy students' health information technology readiness. Curr Pharm Teach Learn. 2019;11(11):1103–1110. doi: 10.1016/j.cptl.2019.07.016. [DOI] [PubMed] [Google Scholar]
- 69.Alam K, et al. Determinants of access to eHealth services in regional Australia. Int J Med Informatics. 2019;131(5):103–119. doi: 10.1016/j.ijmedinf.2019.103960. [DOI] [PubMed] [Google Scholar]
- 70.Zhang X, et al. Using diffusion of innovation theory to understand the factors impacting patient acceptance and use of consumer e-health innovations: a case study in a primary care clinic. BMC Health Serv Res. 2015;15(71):1–15. doi: 10.1186/s12913-015-0726-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Haase R, et al. Profiles of eHealth Adoption in Persons with Multiple Sclerosis and Their Caregivers. Brain Sci. 2021;11(8):1087–1093. doi: 10.3390/brainsci11081087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jebraeily M, et al. Electronic health records: personnel readiness assessment. J Health Admin. 2010;13(39):17–24. [Google Scholar]
- 73.Oo HM, et al. Information and communication technology literacy, knowledge and readiness for electronic medical record system adoption among health professionals in a tertiary hospital, Myanmar: A cross-sectional study. PLoS ONE. 2021;16(7):253–269. doi: 10.1371/journal.pone.0253691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Melas CD, et al. An empirical investigation of technology readiness among medical staff based in Greek hospitals. Eur J Inf Syst. 2014;23(6):672–690. [Google Scholar]
- 75.Vydra, T.P., et al., Diffusion and use of tethered personal health records in primary care. Perspectives in Health Information Management, 2015. 12(1). 10.2196/jmir.4973. [PMC free article] [PubMed]
- 76.Mason P, et al. Overcoming barriers to implementing electronic health records in rural primary care clinics. The Qualitative Report. 2017;22(11):2943–2955. [Google Scholar]
- 77.Darko-Yawson, S. and G.J.P.C.S. Ellingsen, Assessing and improving EHRs data quality through a socio-technical approach. Procedia Computer Science, 2016. 98:243–250. 10.1016/j.procs.2016.09.039.
- 78.Aldebasi B, et al. Level of awareness of Saudi medical students of the internet-based health-related information seeking and developing to support health services. BMC Med Inform Decis Mak. 2020;20(1):1–8. doi: 10.1186/s12911-020-01233-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shea CM, et al. Stage 1 of the meaningful use incentive program for electronic health records: a study of readiness for change in ambulatory practice settings in one integrated delivery system. BMC Med Inform Decis Mak. 2014;14(1):119–126. doi: 10.1186/s12911-014-0119-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Johnson L. Effects of Electronic Health Record Implementation and Barriers to Adoption and Use: A Scoping Review and Qualitative Analysis of the Content. Life. 2013;10(12):327–341. doi: 10.3390/life10120327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Afrizal SH, et al. Narrative review for exploring barriers to readiness of electronic health record implementation in primary health care. Healthcare informatics research. 2019;25(3):141–152. doi: 10.4258/hir.2019.25.3.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim J, et al. Hospital characteristics are associated with readiness to attain stage 2 meaningful use of electronic health records. J Rural Health. 2017;33(3):275–283. doi: 10.1111/jrh.12193. [DOI] [PubMed] [Google Scholar]
- 83.Mirkarimi A, Behnampour N. Readiness assessment of laboratory and imaging staff to implement electronic health records. Front Health Inform. 2014;3(2):5–8. [Google Scholar]
- 84.Qureshi QA, Ahmad I, Nawaz A. Readiness for e-health in the developing countries like Pakistan. Gomal J Medical Sciences. 2012;10(1):160–163. [Google Scholar]
- 85.Ajami S, et al. Readiness assessment of electronic health records implementation. Acta Informatica Medica. 2011;19(4):224–236. doi: 10.5455/aim.2011.19.224-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fanta GB, Pretorius L, Erasmus L. Hospitals' Readiness to Implement Sustainable SmartCare Systems in Addis Ababa, Ethiopia. Portland International Conference on Management of Engineering and Technology (PICMET) 2019;5(2):1–9. [Google Scholar]
- 87.Tsai M-F, et al. Understanding physicians’ adoption of electronic medical records: Healthcare technology self-efficacy, service level and risk perspectives. Comp Standards Interfaces. 2019;66(1):103–134. [Google Scholar]
- 88.Kuo K-M, et al. An investigation of the effect of nurses’ technology readiness on the acceptance of mobile electronic medical record systems. Gomal J Med Sci. 2013;13(1):1–14. doi: 10.1186/1472-6947-13-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.De Benedictis A, et al. Electronic Medical Records implementation in hospital: An empirical investigation of individual and organizational determinants. PLoS One. 2020;15(6):e0234108. doi: 10.1371/journal.pone.0234108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Choi, N.G. and D.M.J.J.o.m.I.r. DiNitto, The digital divide among low-income homebound older adults: Internet use patterns, eHealth literacy, and attitudes toward computer/Internet use. JMIR Publications. 2013. 15(5): 93–108. 10.2196/jmir.2645. [DOI] [PMC free article] [PubMed]
- 91.Biruk S, et al. Health Professionals’ readiness to implement electronic medical record system at three hospitals in Ethiopia: a cross sectional study. BMC Med Inform Decis Mak. 2014;14(1):1–8. doi: 10.1186/s12911-014-0115-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hoerbst A, et al. Attitudes and behaviors related to the introduction of electronic health records among Austrian and German citizens. Int J Med Informatics. 2010;79(2):81–89. doi: 10.1016/j.ijmedinf.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 93.Dinev T, et al. Individuals’ attitudes towards electronic health records: A privacy calculus perspective. Int J Med Informatics. 2016;17(3):19–50. [Google Scholar]
- 94.Adams SL. Nurses knowledge, skills, and attitude toward Electronic Health Records (EHR) Advances in Healthcare Informatics and Analytics. Ann Inform Syst. 2015;19(1):265–277. [Google Scholar]
- 95.Lander L, et al. Self-perceptions of readiness to use electronic health records among medical students: survey study. JMIR Med Educ. 2020;6(1):175–185. doi: 10.2196/17585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Habibi-Koolaee M, Safdari R, Bouraghi H. Nurses readiness and electronic health records. Acta Inform Med. 2015;23(2):105–107. doi: 10.5455/aim.2015.23.105-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tavares, J. and T.J.J.o.m.I.r. Oliveira, Electronic health record patient portal adoption by health care consumers: an acceptance model and survey. JMIR Publications, 2016. 18(3): 49–65. 10.2196/jmir.5069. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data will be available upon request from the corresponding author.