Abstract
Background
After decades of decline since 2005, the global prevalence of undernourishment reverted and since 2015 has increased to levels seen in 2010 to 2011. The prevalence is highest in low‐ and middle‐income countries (LMICs), especially Africa and Asia. Food insecurity and associated undernutrition detrimentally affect health and socioeconomic development in the short and long term, for individuals, including children, and societies. Physical and economic access to food is crucial to ensure food security. Community‐level interventions could be important to increase access to food in LMICs.
Objectives
To determine the effects of community‐level interventions that aim to improve access to nutritious food in LMICs, for both the whole community and for disadvantaged or at‐risk individuals or groups within a community, such as infants, children and women; elderly, poor or unemployed people; or minority groups.
Search methods
We searched for relevant studies in 16 electronic databases, including trial registries, from 1980 to September 2019, and updated the searches in six key databases in February 2020. We applied no language or publication status limits.
Selection criteria
We included randomised controlled trials (RCTs), cluster randomised controlled trials (cRCTs) and prospective controlled studies (PCS). All population groups, adults and children, living in communities in LMICs exposed to community‐level interventions aiming to improve food access were eligible for inclusion. We excluded studies that only included participants with specific diseases or conditions (e.g. severely malnourished children).
Eligible interventions were broadly categorised into those that improved buying power (e.g. create income‐generation opportunities, cash transfer schemes); addressed food prices (e.g. vouchers and subsidies); addressed infrastructure and transport that affected physical access to food outlets; addressed the social environment and provided social support (e.g. social support from family, neighbours or government).
Data collection and analysis
Two authors independently screened titles and abstracts, and full texts of potentially eligible records, against the inclusion criteria. Disagreements were resolved through discussion or arbitration by a third author, if necessary.
For each included study, two authors independently extracted data and a third author arbitrated disagreements. However, the outcome data were extracted by one author and checked by a biostatistician.
We assessed risk of bias for all studies using the Effective Practice and Organization of Care (EPOC) risk of bias tool for studies with a separate control group.
We conducted meta‐analyses if there was a minimum of two studies for interventions within the same category, reporting the same outcome measure and these were sufficiently homogeneous. Where we were able to meta‐analyse, we used the random‐effects model to incorporate any existing heterogeneity. Where we were unable to conduct meta‐analyses, we synthesised using vote counting based on effect direction.
Main results
We included 59 studies, including 214 to 169,485 participants, and 300 to 124, 644 households, mostly from Africa and Latin America, addressing the following six intervention types (three studies assessed two different types of interventions).
Interventions that improved buying power:
Unconditional cash transfers (UCTs) (16 cRCTs, two RCTs, three PCSs): we found high‐certainty evidence that UCTs improve food security and make little or no difference to cognitive function and development and low‐certainty evidence that UCTs may increase dietary diversity and may reduce stunting. The evidence was very uncertain about the effects of UCTs on the proportion of household expenditure on food, and on wasting. Regarding adverse outcomes, evidence from one trial indicates that UCTs reduce the proportion of infants who are overweight.
Conditional cash transfers (CCTs) (nine cRCTs, five PCSs): we found high‐certainty evidence that CCTs result in little to no difference in the proportion of household expenditure on food and that they slightly improve cognitive function in children; moderate‐certainty evidence that CCTs probably slightly improve dietary diversity and low‐certainty evidence that they may make little to no difference to stunting or wasting. Evidence on adverse outcomes (two PCSs) shows that CCTs make no difference to the proportion of overweight children.
Income generation interventions (six cRCTs, 11 PCSs): we found moderate‐certainty evidence that income generation interventions probably make little or no difference to stunting or wasting; and low‐certainty evidence that they may result in little to no difference to food security or that they may improve dietary diversity in children, but not for households.
Interventions that addressed food prices:
Food vouchers (three cRCTs, one RCT): we found moderate‐certainty evidence that food vouchers probably reduce stunting; and low‐certainty evidence that that they may improve dietary diversity slightly, and may result in little to no difference in wasting.
Food and nutrition subsidies (one cRCT, three PCSs): we found low‐certainty evidence that food and nutrition subsidies may improve dietary diversity among school children. The evidence is very uncertain about the effects on household expenditure on healthy foods as a proportion of total expenditure on food (very low‐certainty evidence).
Interventions that addressed the social environment:
Social support interventions (one cRCT, one PCS): we found moderate‐certainty evidence that community grants probably make little or no difference to wasting; low‐certainty evidence that they may make little or no difference to stunting. The evidence is very uncertain about the effects of village savings and loans on food security and dietary diversity.
None of the included studies addressed the intervention category of infrastructure changes. In addition, none of the studies reported on one of the primary outcomes of this review, namely prevalence of undernourishment.
Authors' conclusions
The body of evidence indicates that UCTs can improve food security. Income generation interventions do not seem to make a difference for food security, but the evidence is unclear for the other interventions. CCTs, UCTs, interventions that help generate income, interventions that help minimise impact of food prices through food vouchers and subsidies can potentially improve dietary diversity. UCTs and food vouchers may have a potential impact on reducing stunting, but CCTs, income generation interventions or social environment interventions do not seem to make a difference on wasting or stunting. CCTs seem to positively impact cognitive function and development, but not UCTs, which may be due to school attendance, healthcare visits and other conditionalities associated with CCTs.
Plain language summary
Improving access to food in low‐ and middle‐income countries
Review question
We looked at the effect of community‐level interventions to improve access to nutritious food in low‐ and middle‐income countries (LMICs) on people, households and communities.
Background
Food security exists when people have physical, social and economic access to sufficient, safe, nutritious foods to be healthy. The number of people who do not have enough to eat in the world has started increasing since 2015. Most of these people live in LMICs, especially in Asia and Africa. Not being able to access nutritious food, either because of not having enough money or because of not having somewhere to shop or find food near where people live, affects the health and socioeconomic situation of people and societies, both in the short and long term. Strategies focusing on communities may be important for increasing access to food in LMICs.
Study characteristics
We found 59 studies assessing different interventions in LMICs, including 214 to 169,485 participants and 300 to 124,644 households, mainly in Africa and Latin America. Many studies assessed cash transfers, which are welfare programmes where money is provided to households. Of these, 21 studies evaluated unconditional cash transfers, where there are no conditions for receiving the money, and 14 studies assessed conditional cash transfers, where there are specific conditions required to meet in order to receive the money. Seventeen studies looked at income generation interventions (for example, livestock management or self‐help groups), four studies at food vouchers, four studies at providing food and nutrition subsidies, and two studies looked at social support interventions such as village savings and loans and community grant programmes.
Search date
The evidence is current to February 2020.
Key results
Interventions that improved buying power:
Unconditional cash transfers improve food security and make little or no difference to cognitive function (thoughts and understanding) and development (high‐quality evidence), may increase dietary diversity (variety of the foods that people or households eat from different food groups) and reduce stunting (poor growth) (low‐quality evidence). It is very uncertain whether UCTs reduce the proportion of household expenditure on food and reduce wasting. Regarding adverse outcomes, evidence from one trial indicates that UCTs reduce the proportion of infants who are overweight.
Conditional cash transfers make little to no difference in the proportion of household expenditure on food and slightly improve cognitive function in children (high‐quality evidence), probably slightly improve dietary diversity (moderate‐quality evidence), and may make little to no difference to stunting or wasting (low bodyweight) (low‐quality evidence). Evidence on adverse outcomes (two studies) shows that CCTs make no difference to the proportion of overweight children.
Income generation strategies make little or no difference to stunting or wasting (moderate‐quality evidence), may result in little to no difference to food security and may improve dietary diversity in children but not for households (low‐quality evidence).
Interventions that addressed food prices:
Food vouchers probably reduce stunting (moderate‐quality evidence), may slightly improve dietary diversity and may result in little to no difference in wasting (low‐quality evidence).
Food and nutrition subsidies may improve dietary diversity among school children (low‐quality evidence). We are very uncertain about the effects on household expenditure on healthy foods as a proportion of total expenditure on food (very low‐quality evidence).
Interventions that addressed the social environment:
Social support interventions such as community grants probably make little to no difference to wasting (moderate‐quality evidence) and may make little or no difference to stunting (low‐quality evidence). We are very uncertain about the effects of village savings and loans on food security or dietary diversity (very low‐quality evidence).
None of the included studies addressed the intervention category of infrastructure changes and none of the included studies reported on one of the primary outcomes: prevalence of undernourishment.
Some limitations of the review include not having all necessary information about what was measured (outcomes), judgements that had to be made regarding which outcome measures to report and inability to pool the results of all studies reporting on the same outcome. Another limitation was that we were unable to find out what specific intervention features enable or impede the effective implementation of the intervention.
Summary of findings
Summary of findings 1. Unconditional cash transfers compared to no intervention for food security.
| Unconditional cash transfers compared to no intervention for food security | ||||
| Patient or population: children, adults, households Setting: poor rural and urban households in LMICs Intervention: UCTs Comparison: no intervention | ||||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Prevalence of undernourishment | — | — | — | 0 included studies measured this outcome. |
| Proportion of household expenditure on food follow‐up: range 1–2 years | 1 study showed a clear effect favouring UCTs, 2 studies showed unclear effect potentially favouring UCTs and 2 studies showed clear effect favouring the control. Data not pooled. | 11271 households (5 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | Evidence is very uncertain about the effects of UCTs on the proportion of household expenditure on food. |
| Food security assessed with: proportion of households consuming > 1 meal per day; modified HFIAS; FSI follow‐up: range 1–2 years | 6 studies showed a clear effect favouring UCTs. A meta‐analysis of 3 of these studies showed a small improvement in food security scores (SMD 0.18, 95% CI 0.13 to 0.23; 6209 households) |
10,251 households, 7604 children (6 RCTs) | ⊕⊕⊕⊕ High | UCTs improve food security. |
| Dietary diversity assessed with: dietary diversity scores (i.e. number of food groups consumed); proportion with minimum dietary diversity follow‐up: range 1–2 years | 5 studies showed a clear effect favouring UCTs and 5 studies show an unclear effect potentially favouring UCTs. Data not pooled. |
12,631 households, 890 children (10 RCTs) | ⊕⊕⊝⊝ Lowa,b | UCTs may increase dietary diversity. |
| Stunting assessed with: HAZ < –2SD follow‐up: 2 years | 1 study showed a clear effect favouring UCTs, 2 studies showed an unclear effect favouring UCTs and 1 study showed an unclear effect favouring the control. A meta‐analysis of 2 of these studies showed a reduction in stunting with UCTs (OR 0.62, 95% CI 0.46 to 0.84; 2914 children) |
4713 children (4 RCTs) | ⊕⊕⊝⊝ Lowa,b | UCTs may reduce stunting. |
| Wasting assessed with: WHZ < –2SD follow‐up: range 2 years | 1 study showed an unclear effect potentially favouring UCTs and 3 studies showed an unclear effect potentially favouring the control. Data not pooled. | 6396 children (4 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | We are uncertain whether UCTs reduce wasting. |
| Cognitive function and development assessed with: cognitive test scores, language scores follow‐up: 2 years | 3 studies reported unclear effect potentially favouring intervention. | 10,813 children (3 RCTs) |
⊕⊕⊕⊕ High | UCTs make little or no difference on cognitive function and development. |
| *No meta‐analyses carried out. CI: confidence interval; FSI: Food Security Index; HAZ: height‐for‐age z‐score; HFIAS: Household Food Insecurity Access Scale; LMIC: low‐ and middle‐income country; OR: odds ratio; RCT: randomised controlled trial; SD: standard deviation; SMD: standardised mean difference; UCT: unconditional cash transfer; WHZ: weight‐for‐height z‐score. | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded one level for risk of bias: at least one study was at high overall risk of bias due to selection or attrition bias, or both. bDowngraded one level for inconsistency: there was wide variance of point estimates. cDowngraded one level for imprecision: wide confidence intervals.
Summary of findings 2. Conditional cash transfers compared to no intervention for food security.
| Conditional cash transfers compared to no intervention for food security | ||||
| Patient or population: children, adults, households Setting: poor urban and rural communities in LMICs Intervention: CCTs Comparison: no intervention | ||||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Prevalence of undernourishment | — | — | — | 0 included studies measured this outcome. |
| Proportion of household expenditure spent on food follow‐up: 9 months to 2 years | 1 study showed a clear effect potentially favouring the control and 1 study showed an unclear effect favouring the control. Data not pooled. | 4760 households (2 RCTs) | ⊕⊕⊕⊕ High | CCTs result in little to no difference in the proportion of household expenditure on food. |
| Food security | — | — | — | 0 included studies measured this outcome. |
| Dietary diversity assessed with: Food Consumption Score follow‐up: 7 months to 2.5 years | Meta‐analysis of 2 studies showed a clear effect favouring CCTs (MD 0.45, 95% CI 0.25 to 0.65) | 3937 households (2 RCTs) | ⊕⊕⊕⊝ Moderatea | CCTs probably slightly improve dietary diversity |
| Stunting assessed with: HAZ < –2SD follow‐up: range 20 months to 3 years | 3 studies showed an unclear effect potentially favouring CCTs and 1 study showed an unclear effect potentially favouring the control. A meta‐analysis of 3 of these studies showed an unclear effect favouring CCTs (MD –2.51, 95% CI –7.78, 2.75) |
3529 children (4 RCTs) | ⊕⊕⊝⊝ Lowa,b | CCTs may make little or no difference to the proportion of stunted children. |
| Wasting assessed with: WHZ < –2SD follow‐up: 2 years | A meta‐analysis of 2 studies showed an unclear effect favouring CCTs (MD –2.50 95% CI –8.04 to 3.04) | 2116 children (2 RCTs) | ⊕⊕⊝⊝ Lowb,c | CCTs may make little or no difference in wasting. |
| Cognitive function and development assessed with: cognitive test scores; cognitive and socioemotional outcomes scores follow‐up: range 9 months to 2 years | A meta‐analysis of 2 studies showed a slight improvement with CCTs (SMD 0.13, 95% CI 0.09 to 0.18) | 5383 children (2 RCTs) | ⊕⊕⊕⊕ High | CCTs slightly improve cognitive function in children. |
| *No meta‐analyses carried out. CCT: conditional cash transfer; CI: confidence interval; HAZ: height‐for‐age z‐score; MD: mean difference; RCT: randomised controlled trial; SD: standard deviation; SMD: standardised mean difference; WHZ: weight‐for‐height z‐score. | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded one level for risk of bias: at least one study was at high overall risk of bias due to selection or attrition bias, or both. bDowngraded one level imprecision: wide confidence intervals. cDowngraded one level for inconsistency: wide variation in point estimates.
Summary of findings 3. Income‐generation interventions compared to no intervention for food security.
| Income‐generation interventions compared to no intervention for food security | ||||
| Patient or population: children, adults, households Setting: poor rural communities in LMICs Intervention: income‐generation interventions (e.g. livestock transfers, community development programmes) Comparison: no intervention | ||||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Prevalence of undernourishment | — | — | — | 0 included studies reported this outcome. |
| Proportion of household expenditure on food follow‐up: range 1–2 years | 2 studies reported this outcome but did not provide relevant numerical data or indicated clearly the direction of effect. | 434 households (2 prospective controlled studies) | — | — |
| Food security assessed with: proportion experiencing food security; Household food security score follow‐up: 3–4 months | 1 trial reported no effect measure and 1 trial showed an unclear effect potentially favouring the control. | 2193 households (1 trial) | ⊕⊕⊝⊝ Lowa,b | Income‐generation interventions may result in little to no difference in food security. |
| Dietary diversity assessed with: DDS, HDDS, MDD follow‐up: 2 years | 2 trials showed a clear effect favouring income‐generation interventions, 1 trial showed an unclear effect favouring the intervention and 1 trial showed an unclear effect favouring control. A meta‐analysis of 3 of these studies showed that the intervention improved the proportion of children achieving MDD (OR 1.28, 95% CI 1.11 to 1.47) |
3677 households and 3790 children (4 RCTs) | ⊕⊕⊝⊝ Lowa,c | Income‐generation interventions may improve dietary diversity in children and may result in little or no difference to household dietary diversity. |
| Stunting assessed with: HAZ follow‐up: 12 months | Meta‐analysis of 2 studies showed no difference to stunting (OR 1.00, 95% CI 0.84 to 1.19) | 3466 children (2 RCTs) | ⊕⊕⊕⊝ Moderated | Income‐generation interventions probably make little or no difference to stunting. |
| Wasting assessed with: WHZ follow‐up: 2 years | Meta‐analysis of 2 studies showed unclear effect favouring the intervention (OR 1.13, 95% CI 0.92 to 1.40) | 3500 children (2 trials) | ⊕⊕⊕⊝ Moderated | Income‐generation interventions probably make little or no difference to wasting. |
| Cognitive function and development | — | — | — | 0 included studies reported this outcome. |
| CI: confidence interval; DDS: Dietary Diversity Score; HAZ: height‐for‐age z‐score; HDDS: Household Dietary Diversity Score; MDD: minimum dietary diversity; OR: odds ratio; RCT: randomised controlled trial; WHZ: weight‐for‐height z‐score. | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded one level for risk of bias: at least one study was at high overall risk of bias due to selection or attrition bias, or both. bDowngraded one level for indirectness: results are from a single study which assessed a public works programme and the effects may be different from other types of income generation interventions. Additionally public works programmes are often implemented in different ways in different settings. cDowngraded one level for inconsistency: wide variation in point estimates. dDowngraded one level for imprecision: wide confidence intervals.
Summary of findings 4. Food vouchers compared to no intervention for food security.
| Food vouchers compared to no intervention for food security | ||||
| Patient or population: poor households Setting: urban and agrarian communities in LMICs Intervention: food vouchers Comparison: no intervention | ||||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Prevalence of undernourishment | — | — | — | 0 included studies reported this outcome. |
| Proportion of household expenditure on food | — | — | — | 0 included studies reported this outcome. |
| Food security | — | — | — | 0 included studies reported this outcome. |
| Dietary diversity assessed with: FCS follow‐up: 7 months to 1 year | 2 studies reported improved dietary diversity (not pooled). | 2459 households (2 RCT) | ⊕⊕⊝⊝ Lowa,b | Food vouchers may improved dietary diversity slightly. |
|
Stunting (HAZ < –2SD) follow‐up: 12 months |
1 study reported reduced stunting (OR 0.48, 95% CI 0.31 to 0.73) | 1633 children (1 RCT) | ⊕⊕⊕⊝ Moderatec |
Food vouchers probably reduce stunting. |
|
Wasting (WHZ < –2SD) follow‐up: 12 months |
1 study reports an unclear effect potentially favouring the control (OR 1.17, 95% CI 0.75, 1.82) | 1633 children (1 RCT) | ⊕⊕⊝⊝ Lowc,d |
Food vouchers may result in little to no difference in wasting |
| Cognitive function and development | — | — | — | 0 included studies reported this outcome. |
| CI: confidence interval; FCS: Food Consumption Score; HAZ: height‐for‐age z‐score; OR: odds ratio; RCT: randomised controlled trial; SD: standard deviation; WHZ: weight‐for‐height z‐score. | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded one level for overall risk of bias: two studies at high risk of selection and attrition bias. bDowngraded one level for inconsistency: confidence intervals had minimal overlap. cDowngraded one level for indirectness: findings are from one single study that assessed a programme of fresh food vouchers redeemed at designated vendors. Food vouchers may be implemented in different ways across different settings, e.g. for staple foods alone, or with, no vendor‐ restrictions. dDowngraded one level for imprecision: findings ranged from an important harm to important benefit.
Summary of findings 5. Food and nutrition subsidies compared to no intervention for food security.
| Food and nutrition subsidies compared to no intervention for food security | ||||
| Patient or population: primary schools and households and members of healthcare plan Setting: urban and rural settings in LMICs Intervention: food and nutrition subsidies Comparison: no intervention | ||||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Prevalence of undernourishment | — | — | — | 0 included studies reported this outcome. |
| Proportion of household expenditure on food assessed with: ratio of healthy to total food expenditure follow‐up: 28 months | 1 study reported that food rebates of 10% improved the ratio of healthy, to total food expenditure | 169,485 households (1 prospective controlled study) | ⊕⊝⊝⊝ Very lowa,b | The evidence is very uncertain about the effects of food rebates on household expenditure on healthy foods. |
| Food security | — | — | — | 0 included studies reported this outcome. |
| Dietary diversity | 1 study reported a clear effect favouring nutrition subsidies. | 656 children (1 RCT) | ⊕⊕⊝⊝ Lowc,d |
Nutrition subsidies may improve dietary diversity among school children |
| Stunting | — | — | — | 0 included studies reported this outcome. |
| Wasting | — | — | — | 0 included studies reported this outcome. |
| Cognitive function and development | — | — | — | 0 included studies reported this outcome. |
| LMIC: low‐ and middle‐income country; RCT: randomised controlled trial. | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded one level for risk of bias: high risk of selection bias due to disparate baseline expenditure on healthy food as a ratio of total expenditure between households in the intervention and control group. bDowngraded one level for indirectness: results are from a single study that assessed food rebates at a supermarket in South Africa. The population was restricted to members of the health insurance company's program, who are usually healthier and wealthier in general. Effects in other populations may differ.
cDowngraded one level for indirectness: results are from a single study that assessed the effects of providing nutrition subsidies to schools. Subsidies to individuals or households may have different effects. dDowngraded one level for risk of bias: study was at high overall risk of bias due to attrition bias.
Summary of findings 6. Social support compared to no intervention for food security.
| Social support compared to no intervention for food security | ||||
| Patient or population: households at risk of food insecurity Setting: poor communities in LMICs Intervention: village savings and loans groups and community cash transfers Comparison: no intervention | ||||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Prevalence of undernourishment | — | — | — | 0 included studies reported this outcome. |
| Proportion of household expenditure on food | — | — | — | 0 included studies reported this outcome. |
| Food security assessed with: self‐reported months of food sufficiency follow‐up: 3 years | 1 study reported an unclear effect favouring village savings and loans | 1687 households (1 prospective controlled study) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effects of village savings and loan on food security. |
| Dietary diversity assessed with: HDDS follow‐up: 3 years | 1 study showed an unclear effect favouring the control. | 1615 households (1 prospective controlled study) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effects of village savings and loan on dietary diversity. |
|
Stunting assessed with: HAZ < –2SD follow‐up: 2 years |
1 study showed an unclear effect favouring the control. | 1481 children (1 RCT) | ⊕⊕⊝⊝ Lowb,c |
Community grants may make little or no difference to stunting. |
|
Wasting assessed with: WHZ < –2SD follow‐up: 2 years |
1 study showed an unclear effect favouring a community grant programme. | 1481 children (1 RCT) | ⊕⊕⊕⊝ Moderateb |
Community grants probably make little or no difference to wasting. |
| Cognitive function and development | — | — | — | 0 included studies reported this outcome. |
| *No meta‐analyses carried out. CI: confidence interval; HAZ: height‐for‐age z‐score; HDDS: Household Dietary Diversity Score; LMIC: low‐ and middle‐income country; RCT: randomised controlled trial; SD: standard deviation; WHZ: weight‐for‐height z‐score. | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded one level for indirectness: results from a single study which assessed the effects of microfinance program to villages in Mozambique. Effects of other types of social support interventions may be different. As this was a prospective controlled study the certainty of evidence started at low. bDowngraded one level for indirectness: results are from a single study which assessed the effects of a community cash transfer programme implemented in rural villages in Indonesia. Village management teams allocated funds to different types of social support interventions, Effects in urban populations and with different intervention implementation may differ.
cDowngraded one level for imprecision: wide confidence interval.
Background
Description of the condition
Food security "exists when all people, at all times, have physical, social and economic access to sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life" (FAO 2019). When these conditions are not met, the population and people within it are said to be food insecure.
Food insecurity and associated undernutrition affect health and socioeconomic development on different levels (Black 2013; Ecker 2012; Victora 2008). For adults, it has been associated with an increased risk of disability, morbidity and mortality, and with a decrease in income‐generation potential (Black 2008; Black 2013; Victora 2008). Food insecurity is also associated with mental health problems such as depression and anxiety, both in high‐income as well as low‐ and middle‐income settings (Arenas 2019; Carter 2011; Cole 2011; Hadley 2006; Hadley 2008; Maynard 2018). Children who are affected may experience impaired physical and cognitive development, and decreased school performance (Black 2008; Black 2013; Liu 2012; Victora 2008). At the macro‐level, undernutrition is associated with direct and indirect costs. Direct costs are due to increased healthcare costs for preventing and treating affected individuals (Black 2013; Victora 2008). Indirect costs are due to poor productivity and losses of human resources due to mental and physical under‐performance and death (Victora 2008). Given these far‐reaching consequences, and considering that food security is defined as a human right by the United Nations (FAO 2003), it is important to address food insecurity.
Building on the first 2010 to 2015 Millennium Development Goal (MDG), which was to eradicate extreme poverty and hunger, the second 2015 Sustainable Development Goal (SDG) aimed to end hunger by 2030 and sought to "achieve food security and improve nutrition and promote sustainable agriculture" (UN 2015). Progress towards this goal has been insufficient. Following decades of decline, the global prevalence of undernourishment, has, since 2015, increased to levels seen in 2010–2011, approximately 11% (FAO 2019). Although this prevalence is highest in Asia, it has been sharply increasing in Africa which is now home to 30% of the world's undernourished population (FAO 2019). The global number of undernourished people, estimated at 820 million in 2018, has been steadily rising particularly in Africa, Latin America and Western Asia. Globally, the prevalence and number of stunted children under five years of age has decreased since 2012, although this is uneven as Africa and Asia account for more than 90% of stunted and wasted children globally (FAO 2019; SOWC 2019). Factors that have delayed improvements in rates of chronic hunger include the food price crisis of 2008, brought about by trade restrictions of major food exporters, biofuels policies and increased commodity speculation, among others (Ecker 2012). The higher demand for food due to changing dietary patterns and growing population, and food price increases and volatility due to climate change are other factors that will contribute to food insecurity in the long term (Ecker 2012).
Food security is a complex concept that encompasses several different dimensions (Ecker 2012; FAO 2013; FAO 2019; Gross 2000), where 1. food availability refers to the quantity of food that is physically available in the relevant vicinity of a population during a given period (ACF‐IN 2008); 2. food access is a measure of the capacity of a household to acquire sufficient and appropriate foods to ensure a diet that is diverse, nutrient‐rich and safe, and that satisfies the nutrient needs of its members during a given period, which is often influenced by the proximity and price of food (ACF‐IN 2008; WHO 2013); 3. food utilisation refers to the intake of food by the people within a household and how the body assimilates the nutrients physiologically; and 4. food stability introduces the condition of time to the food security concept, that is it refers to chronic or transient food insecurity (FAO 2003). Chronic food insecurity refers to long‐term, persistent lack of food and results from continued problems with structural poverty, relating to the inability of the labour market to produce enough jobs to keep people out of poverty, low incomes and with lack of sufficient social safety nets to assist the poor (Ecker 2012; FAO 2003; Rank 2003). In contrast, transient food insecurity refers to food and nutrient shortages during certain periods of food crises due to natural disasters, economic collapse or conflict (Ecker 2012; FAO 2003). In addition, the nutrition dimension was added to the food security concept at the 2009 World Food Summit (Ecker 2012) as food insecurity is associated with nutrient deficiencies and poor nutritional outcomes. Furthermore, food and nutrient intake interact in a bidirectional manner with health status (Ecker 2012). This means that nutritional status is the primary measure of food security.
The four dimensions of food security operate at different levels of influence, although these are often inter‐related (Ecker 2012; Gross 2000). At the macro‐level (national, regional, global) and meso‐level (community), food security issues are mainly related to food availability and stability, whereas at the micro‐level they are mainly related to food access and utilisation by households and individuals (Ecker 2012; Gross 2000; Pinstrup‐Andersen 2009). Food security in one level does not ensure food security at another level (Gross 2000). For example, food might be available at the national level but not accessible for certain disadvantaged communities or districts, or among lower income or otherwise marginalised population groups. In Ghana, despite improvements in reducing poverty and increasing food production, there has been less progress in reducing undernutrition and disparities remain (FAO 2013; Hjelm 2013). There, poorer households and those headed by women tend to be more food insecure due to their low‐diversity diets compared with the wealthier or male‐headed households (FAO 2013; Hjelm 2013). In Nepal, there is still widespread undernutrition despite the country producing sufficient food, and those living in rural areas are at a higher risk of food insecurity and have a higher prevalence of undernutrition and stunting in children as poor infrastructures and poverty limit their physical and economic access to food (FAO 2013; MOHP 2012). Furthermore, households might have access to food, but this does not guarantee that all individuals in the household are able to access and utilise sufficient amounts of good quality and safe food. This is because the distribution of food within the household may be influenced by cultural beliefs, practices, attitudes, gender and age‐specific roles and responsibilities, as well as decision‐making hierarchies (Gittelsohn 2003; Pinstrup‐Andersen 2009; Renzaho 2010).
In addition to the burden of undernutrition, low‐ and middle‐income countries (LMICs) also have high rates of overweight and obesity that are on the rise (Hossain 2007; Popkin 2012; Subramanian 2011). In an analysis of data from 54 LMICs, 27% of women were overweight (Subramanian 2011). The prevalence of overweight in 2008 ranged from approximately 18% in low‐income countries to 59% in upper middle‐income countries, with a mean prevalence of 28% in the African region (WHO 2010). Among children under five years of age, the prevalence of overweight and obesity is also increasing, with 12.9% of boys and 13.4% of girls overweight in LMICs in 2013 (Ng 2014). Most of this burden is concentrated in Africa and Asia, regions that accounted for almost three‐quarters of the global share of overweight children in 2018 (FAO 2019; SOWC 2019). The increased rates of overweight and obesity are associated with the nutrition transition and poorer‐quality diets increasingly consisting of more affordable processed foods, high intake of refined sugars and fats, and increased intake of food away from home, further exacerbated by decreased levels of physical activity (Popkin 2012; SOWC 2019). In LMICs, the consumption of processed or junk foods and sugar‐sweetened beverages has increased, with 54% of the global consumption of soft drinks 1997 and 2010 occurring in LMICs (Basu 2013). These dietary patterns are partly the result of high food prices, which cause consumers, particularly those in poorer households, to buy less‐expensive foods. These are often energy dense (higher in calories) and less nutritious (containing fewer nutrients per serving size). Consumption of these foods is, therefore, associated with increased risk of overweight, obesity and micronutrient deficiencies. In this context, it is important to consider the quantity and quality of the food intake in any intervention.
Description of the intervention
Scoping review: preparation for this systematic review
The complexity of food security allows for a wide range of interventions addressing its different dimensions at varying levels of influence. In order to better conceptualise the framework for our review with regards to the type(s) of intervention(s) to assess, the eligibility criteria for study selection and the outcomes to be assessed, we conducted a scoping review of existing systematic reviews of interventions addressing food security in LMICs (more information about the methods is available on request).
We included 29 systematic reviews in the scoping review (references available on request). Fourteen reviews addressed food availability, mainly assessing food production interventions and food utilisation (13 reviews, including five which also addressed availability), specifically around issues of nutrition education for people to improve their dietary intake. Seven reviews addressed food access. The scoping review also revealed that the included reviews were unclear regarding the description of participants and settings, types of interventions and comparisons, or the outcomes they would assess (Table 7). The quality of reviews varied considerably, some with very low‐quality scores using the AMSTAR tool (Shea 2009).
1. Summary of PICOS and of AMSTAR scores of included systematic reviews, and how existing reviews informed the PICOS of a new Cochrane Review.
| Domain | Finding | How it informed our review question or methods |
| Setting |
|
We chose the community as the setting, defined as a group of people with diverse characteristics who were linked by social ties, share common perspectives and engage in joint action in geographical locations or settings (MacQueen 2001). |
| Participants |
|
As existing reviews specifically addressed specific high‐risk groups, we did not focus on these. Instead, we included all individuals across all ages that belonged to the community where relevant interventions had been implemented. |
| Intervention (including its duration) |
|
Of the 14 reviews that addressed food availability, 5 also assessed food utilisation (e.g. combination of community gardens and nutrition education). As fewer reviews addressed food access, we included interventions that had addressed this dimension of food security. We included interventions with any duration but extracted outcomes that were measured ≥ 3 months after implementation. |
| Control |
|
We included studies in which these interventions, individually or in combination, were compared to no intervention or to other eligible intervention. |
| Outcomes assessed | The specific outcomes assessed across the included reviews varied considerably and often they were not clearly specified at the outset. The most common and important outcomes reported in these reviews were related to dietary intake, anthropometric measurements, and biochemical and clinical indicators, to describe the impact of the intervention on nutritional status. Other outcomes measured included food purchase or expenditure, food production, morbidity and mortality, and breastfeeding initiation rates or duration. Often, reviews measured the same outcome in different ways. For example, anthropometric indicators assessed differed, as did their classifications, across the included reviews. This makes it difficult to compare results across reviews and to reach a conclusion about the effectiveness of a specific intervention. |
The most commonly specified outcomes measured food and nutrition security, and nutritional status. We also focused on these outcomes. Examples included: diet diversity scores and hunger measures; and anthropometric, biochemical and dietary intake indicators. We clearly defined, a priori, the specific outcome measures and metrics that we included in our review. |
| Study designs |
However, the definitions of the study design labels used were not always clear and varied across the included reviews. |
The study design labels used varied across included reviews and were not always clearly defined. We included both randomised and non‐randomised studies, as we expect that existing RCTs in the area of food security would be scarce. We wanted to include the best available evidence for our review question. We clearly defined the type of study designs included in our review. |
| Search strategies | Most reviews ran comprehensive searches. They used a comprehensive set of keywords and searched a variety of relevant databases. Only 5 reviews did not indicate search terms either in the text or in an appendix.
|
Our review included updated searches across a variety of relevant databases and websites. We drew on common keywords used across these included reviews. |
| Reporting | The methods sections of most reviews were often not reported clearly. The reporting of results in these reviews, in terms of characteristics of included studies, was also poor. | Poor reporting of the characteristics of included studies makes it difficult to assess the context in which these results were obtained. Thus, it is difficult to generalise the results. We clearly reported on the characteristics of included studies, so that the context in which the interventions were implemented was clearly understood. |
| AMSTAR scores |
|
Of the 8 high‐quality reviews, 5 assessed interventions that aimed to improve food availability or utilisation (or both), and 3 assessed interventions addressing food access. The other 2 included reviews that addressed food access were of low quality (AMSTAR = 4). We contributed to the evidence base on interventions addressing food access by producing a high‐quality systematic review that assessed the effectiveness of the interventions on relevant outcomes, such as nutritional status. |
BAS: before‐and‐after study; CCT: controlled clinical trial; CSS: cross‐sectional study; ITS: interrupted time series; LMIC: low‐ and middle‐income country; RCT: randomised controlled trial.
Interventions selected based on scoping review results
Based on the findings of the scoping review, we decided to focus this Cochrane Review on community‐level interventions that aim to improve access to nutritious food in LMICs; as we found that there are fewer reviews addressing food access compared to food availability or utilisation. Furthermore, we know that in many areas of LMICs, nutritious food is available at a national level, but physical distance and financial constraints prevent thousands of people from accessing the food (FAO 2013). As explained above, increased intake of ultraprocessed food products and sugar‐sweetened beverages has contributed to the rise in overweight and obesity in LMICs and poor diet quality is also responsible for micronutrient deficiencies. Thus, interventions should aim to improve access to nutritious food. Nutritious foods can be defined as those that are nutrient dense, that is providing substantial amounts of vitamins and minerals (Pennington 2007). This includes fresh or minimally processed foods from the different food groups, such as whole grains, lean meats, dairy products, legumes, vegetables and fruits, and excludes ultraprocessed products and sugar‐sweetened beverages that provide empty calories (Drewnowski 2005; Ministry of Health of Brazil 2014).
The interventions addressing food access include those aimed at infrastructure and transport, food prices, the social environment, coping strategies and buying power. In our scoping review, we found no systematic reviews addressing infrastructure and transport or coping strategies. We did, however, find reviews focusing on food prices, social environment and buying power, but these did not assess all relevant outcomes and not all were of good quality. Therefore, we included all these interventions addressing food access in this review.
We chose to assess community‐level interventions because every community member residing in the setting where they are implemented can potentially benefit from them (McLeroy 2003). These types of interventions have been shown to be effective (Bhandari 2003; Mohammadifard 2009), and include interventions that take place across cities or within community institutions, such as schools, neighbourhoods, churches or work sites. The intervention may involve individuals, families, organisations or public policy.
This review focused on LMICs as they experience the greatest burden from food insecurity and malnutrition and because another Cochrane Review will address food security in developed countries (Burns 2010).
How the intervention might work
Based on the literature cited in the above sections, and on guidance on how to use logic models in systematic reviews (Rohwer 2016), we developed a logic model that illustrates how interventions addressing food insecurity might work in improving the nutritional status of individuals (Figure 1). In this model, we present interventions that address food availability, access and utilisation. The interventions may operate at different levels of influence, including the macro (national, regional, global), meso (community) and micro (household and individual) levels. As mentioned above, food security at one level does not ensure food security at another level (Gross 2000). As our review focused on chronic food insecurity, the logic model does not include interventions that address transient food insecurity.
1.
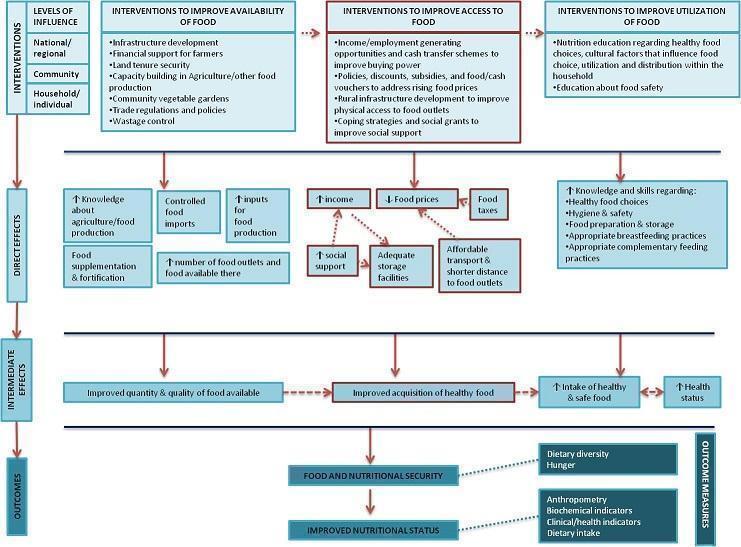
Food security logic model: how interventions influence food and nutritional security.
Although this logic model encompasses three dimensions of food security – availability, access and utilisation – we only explored how interventions addressing access to food may lead to food and nutrition security. As mentioned above, access to food concerns the ability of households (and communities) to acquire sufficient and appropriate foods to ensure a diet that is diverse, nutrient dense and safe, and that satisfies the nutrient needs of its members (ACF‐IN 2008; WHO 2013). This logic model provides examples of interventions that address the determinants of food access. These include income‐ or employment‐generating opportunities, coping strategies (e.g. borrowing money from a community fund, childcare), social grants, food price policies and regulations, rural infrastructure development, and food or cash vouchers. The direct effects of these interventions include increased financial resources in the household, reduced food prices, increased social support and assistance (e.g. from family, neighbours or the government), having adequate facilities to store food, and ensuring that there is affordable transport to food outlets as well as existence of food outlets closer to where people live (Cotta 2013; Ecker 2012; FAO 2012). Many of these factors interact with each other. For example, having more money may enable the household to buy a fridge to store fresh food, being able to borrow money increases the money available to buy food or the existence of adequate road infrastructure may lead to decreased food prices. These direct effects all lead to a common intermediate effect, which is better ability of households to acquire healthy and nutritious food. The acquisition of healthy food is dependent on there being food available. Being able to acquire healthy food makes it easier for households to make healthy food choices, which in turn influences their intake of healthy and safe food. This represents the interaction across the different dimensions of food security. When the intermediate effects across all dimensions of food security are in place – that is, when nutritious food is commonly available in sufficient quantities at fair prices – households are able to acquire healthy food, all individuals within the household can eat healthy food that meets their nutritional requirements as well as their preferences, and long‐term outcomes of food and nutrition security, and thus of improved nutritional status of everyone in the household and in the community, are achievable.
One potentially harmful unintended consequence of interventions that improve access to food is the increased risk of overweight or obesity (Cotta 2013; Ruel 2013), particularly if there is increased intake of energy‐dense ultraprocessed products and sugar‐sweetened beverages (Lignani 2011). People may choose to acquire these foods because of lower cost; lack of knowledge about healthy diets; or other social, cultural or individual preferences (Ruel 2013).
Although we are assessing interventions addressing access to food, it is important to note that, in order to have long‐term food and nutrition security, all three dimensions need to be in place: food needs to be available; people need to be able to access it; and they also need to know how to choose the food, prepare and store it appropriately (Pinstrup‐Andersen 2009; WHO 2013).
Why it is important to do this review
Although many interventions are being implemented to address food insecurity globally, the lack of sufficient improvements in levels of undernutrition over time, particularly in LMICs, highlights the need for the effectiveness of these interventions to be assessed. Furthermore, our scoping review highlighted that existing reviews addressing access to food in LMICs were not of high methodological quality. Therefore, we aimed to apply rigorous Cochrane Review methods to produce a high‐quality review to identify effective interventions addressing food access. This evidence would then inform relevant stakeholders' decisions about which interventions to implement in order to achieve desirable results and ensure that scarce resources are utilised efficiently. Furthermore, improving access to food would help improve overall food security and the health and nutritional status of populations, which are requisites for the socioeconomic development of individuals and societies (FAO 2003).
Objectives
Primary objective
To determine the effects of community‐level interventions that aim to improve access to nutritious food in LMICs, for both the whole community and for disadvantaged or at‐risk individuals or groups within a community, such as infants, children and women; elderly, poor or unemployed people; or minority groups.
Secondary objectives
To determine the features of community‐level interventions that enable or impair the effective implementation of these interventions to improve access to food.
To identify unintended consequences of interventions to improve access to food.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and cluster randomised controlled trials (cRCTs). We also included non‐randomised studies because: 1. we did not expect to find many RCTs that would answer our question; and 2. to increase the external validity of the review findings. In these studies, observations are made before and after an intervention has been implemented or an exposure has occurred, both in an intervention and a control group. These types of studies are sometimes referred to as prospective analytical cohort studies or controlled before‐after studies. We collectively termed them prospective controlled studies (PCS). We planned to include interrupted time series (ITS), but found none. ITS studies observe the effects of an intervention at multiple time points before and after an intervention. ITS studies needed to have at least three time points both before and after the intervention in order to be included.
Types of participants
We included all population groups living in communities in LMICs exposed to community‐level interventions aiming to improve food access. For the purpose of this review, we defined a community as a group of people with diverse characteristics who are linked by social ties, share common perspectives and engage in joint action in geographical locations or settings (MacQueen 2001). We included both adults and children living in those communities, as well as disadvantaged groups within those communities. LMICs were defined according to the World Bank 2020.
Most interventions addressing food insecurity are usually implemented in areas and among populations at high risk for food insecurity, such as low‐income areas, unemployed people, women and children. We did not restrict studies on the basis of social and demographic characteristics, and reported these characteristics in the review.
We excluded studies which only included participants with specific diseases or conditions (e.g. severely malnourished children) as these types of participants require specialised approaches to address malnutrition caused by these diseases or conditions.
Types of interventions
We included community‐level interventions that aim to improve access to food, as detailed in our logic model (Figure 1). Community‐level interventions were defined as those in which the community was the setting where the intervention was implemented, with every member of that community potentially benefiting from it (McLeroy 2003). This includes interventions that are district‐, city‐ or village‐wide or interventions that take place within community institutions such as schools, neighbourhoods, churches or work sites. The intervention may involve individuals, households, organisations or public policy. Based on the literature in this field, and on the findings of our scoping review, we decided to include the following interventions that address access to food (Table 8):
2. Definition of interventions included in the review.
| Category of intervention | Definition | Types of interventions |
| Improve buying power | Interventions that generate/increase/maintain income to ensure economic access to food and other basic needs. |
|
| Food prices | Interventions that reduce price of food and thus increase economic access to food. |
|
| Infrastructure/transport | Interventions that ensure people/communities have physical access to food/food outlets. |
|
| Social environment/support | Interventions that ensure people have social support/support network they can resort to for money/food in times of need, or access to adequate storage facilities (e.g. shared fridge) or services (e.g. transport/childcare) – leading to increased economic or physical access to food Social support can be instrumental, emotional, informational, or companionship. We were interested in instrumental social support, i.e. practical help that can be accessed in times of need. |
|
interventions that improve buying power (e.g. income‐generation opportunities, cash transfer schemes);
interventions addressing food prices (e.g. policies, discounts, vouchers and subsidies);
interventions addressing infrastructure and transport that affect physical access to food outlets;
interventions addressing the social environment and social support (e.g. social support from family, neighbours or government).
We included studies that compared these interventions, individually or in combination, to no intervention or to other eligible interventions, including treatment as usual.
We chose this broad approach because we did not expect to find many eligible studies to include for each of the intervention types.
As we anticipated variability in the duration of included interventions, we included interventions of any duration.
Although we were interested in interventions that have measured access to nutritious food, we did not apply this as an inclusion criterion. Instead, we captured this information when extracting the details of included interventions, if this was available.
We excluded interventions that addressed transient food insecurity (e.g. food aid during natural disasters and wars) and that provided short‐term relief from food insecurity (e.g. one‐off food voucher, food banks or soup kitchens). We also excluded interventions that provided food in the form of food baskets or in‐kind transfers of food. These types of interventions, according to our logic model, fall under the groups of interventions addressing availability and were, therefore, excluded. Other types of in‐kind transfers (e.g. livestock, food vouchers, etc), that were not directly providing food to participants but contributed to their economic access to food, were eligible for inclusion. Interventions that involved agricultural production also typically fall under 'food availability', however, if their aim was specifically to generate income, they were included.
Types of outcome measures
Given the complex nature of food security, we assessed outcomes at different levels, namely at the community, household and individual levels.
The findings of our scoping review showed that the types of outcomes measured across food security interventions vary considerably. For this reason, we took a broad approach regarding the outcomes to include.
Given that our main interest was in determining whether these interventions improve access to food and, consequently, food security and nutritional status, we included only interventions that had measured outcomes related to food access or nutritional status, or that used a food security measurement tool. We included any study that had at least one of the outcomes listed below.
Primary outcomes
Our primary outcomes included those that measure access to food at the household and community level. Following from our logic model, these were the following changes in the (FAO 2013; Smith 2006):
prevalence of undernourishment (i.e. proportion of people with insufficient intake to meet minimum dietary energy requirements (MDER) (inddex.nutrition.tufts.edu/data4diets/indicator/prevalence-undernourishment?back=/data4diets/indicators);
proportion of household expenditure on food (as proportion of household income or of total household expenditure);
proportion of households who were food secure (e.g. according to various measures or indices of food security and dietary diversity at an individual or household level), as measured in the included study.
Secondary outcomes
Secondary outcomes were those that reflect access to food and food availability and utilisation. Thus, they reflect nutritional status, which is the ultimate goal of food security interventions at the individual level. Following from our logic model, the secondary outcomes at the individual level were:
change in adequacy of dietary intake (e.g. food or energy intake and whether it meets energy and nutrient requirements; if intake was not assessed for adequacy, i.e. only calories reported, this was not reported in the review);
change in anthropometric indicators (e.g. stunting, wasting and underweight in children, according to height, weight, height‐for‐age z‐scores (HAZ), weight‐for‐height z‐scores (WHZ), and weight‐for‐age z‐scores (WAZ); underweight and overweight in adults according to body mass index (BMI) classifications);
change in biochemical indicators (e.g. micronutrient levels in the blood);
cognitive function and development during the intervention period (e.g. Denver Developmental Screening Test, Bayley Scales of Infant Development);
change in proportion of anxiety or depression (as described by the included study's authors);
morbidity (as described by the review authors);
adverse outcomes (e.g. proportion overweight or obese as a potentially harmful consequence of these type of interventions).
We only included outcomes that were measured at least three months after the intervention was implemented as outcomes measured earlier are not likely to reflect sustainable changes.
Search methods for identification of studies
Electronic searches
We searched electronic databases from 1980 onwards for relevant studies. We applied no language or publication status limits. We chose the year 1980 as the starting point because it was around this time that the term 'food security', encompassing access to food, started being used (Masset 2011). The initial searches were conducted in September 2016 in the following databases:
Ovid MEDLINE(R) Epub Ahead of Print 11 July 2016, Ovid MEDLINE 1946 to June week 5 2016, Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations 11 July 2016, Ovid MEDLINE Daily Update 11 July 2016;
Cochrane Central Register of Controlled Trials (CENTRAL): Issue 6, 2016 (the Cochrane Library/Wiley);
Embase (Elsevier);
GreenFILE (EBSCO);
AfricaBib (africabib.org);
AGRIS;
AGRICOLA;
AFRICAN HEALTHLINE, African Journals Online (via Africa‐Wide Information, EBSCO);
Trials Register of Promoting Health Interventions (TRoPHI);
WHO Global Index Medicus;
Web of Science (Conference Proceedings Citation Index, Science Citation Index Expanded, Social Science Citation Index);
Sociological Abstracts (ProQuest);
International Bibliography of the Social Sciences (IBSS) (ProQuest);
Global Health (EBSCO);
ClinicalTrials.gov;
WHO International Clinical Trials Registry Platform.
A combination of text words and controlled vocabulary terms related to the interventions and possible outcome measures were used to develop a sensitive search strategy. The search strategies for the different databases are available in Appendix 1, which is an adaptation of the search strategy for the Cochrane Review assessing interventions to improve food security in developed countries (Burns 2010). We applied a study design filter to the search that has been developed by Joy Oliver, the information specialist at Cochrane South Africa. The original search strategy for MEDLINE published with the protocol of this review had to be revised by a librarian and adapted for Ovid MEDLINE, as it retrieved an excessive number of results. The Ovid MEDLINE search strategy was then modified to be adapted for the other databases and reported as appendices in our full review. We recruited the Cochrane Public Health Group's information specialist to advise on and implement the search strategy.
The search was updated in April 2019 and February 2020. For the updates, we followed the recommendations of Garner 2016. The Cochrane Public Health Group's information specialist defined a minimum set of databases that would have identified the original included studies and optimised the remaining database searches to improve the balance of sensitivity and precision of the search strategies. We searched the following databases from 1980 onwards:
Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions;
CENTRAL (the Cochrane Library/Wiley);
Web of Science (Conference Proceedings Citation Index, Science Citation Index Expanded, Social Science Citation Index);
Global Health (EBSCO);
Sociological Abstracts (ProQuest);
International Clinical Trials Registry Platform.
The search strategies for each database included in the latest search, which is the same as for the April 2019 search, are available in Appendix 1. Appendix 2 presents the search strategies of the original search strategy in September 2016.
Some of the electronic databases specified above index a combination of published and unpublished studies, such as doctoral thesis and conference abstracts. Therefore, the electronic searches captured some of the unpublished studies. For further searching for unpublished studies, see Searching other resources.
Searching other resources
We identified additional studies through searching reference lists of similar reviews or contacting authors of included studies. However, much of the additional searches we were planning to undertake at the protocol stage were not carried out. We provide reasons in the Differences between protocol and review section.
Data collection and analysis
Selection of studies
Two author pairs (SD, AS, MV, AB, JO, VR, BS) independently screened all titles and abstracts retrieved to determine eligibility against the inclusion criteria. Full‐text copies of eligible titles and of those for which eligibility was unclear were retrieved for closer examination. Any disagreements regarding eligibility were resolved through discussion or through arbitration by a third author, if necessary. We recorded the reasons for excluding studies at the full‐text screening stage in the Characteristics of excluded studies table. We completed a PRISMA flow chart of study selection.
The initial title and abstract screening, from the first search, was carried out using Word documents. The full‐text screening and all subsequent screening was carried out using the Covidence platform.
Where we found relevant studies in a language other than English, Portuguese or Spanish, we planned to contact Cochrane Public Health for options for translations. We found studies in French, which a colleague reviewed against the eligibility criteria. As these were not eligible for inclusion, no translations were required. We found no studies in any other language that required translation.
We used EndNote X8 to manage the retrieved records and to remove duplicate reports of the same study. The study was considered the unit and all references related to the same study were grouped under the same identifier.
Data extraction and management
For each included study, author pairs (SD, AS, MV, AB, JO, VR, BS) extracted data independently and resolved disagreements through discussion or arbitration by a third author. We collected all data except those concerning outcomes using Covidence, using a standardised data collection form, which was piloted on two studies. One author extracted outcomes data using a standardised and piloted form in Microsoft Excel 2007 and a second author (a biostatistician; YB) checked all the data extracted. We based our data extraction form on the forms from Cochrane Public Health and Cochrane Effective Practice and Organisation of Care (EPOC), modified to suit our review. We extracted the following data.
Study design and methods (recruitment of participants, representativeness of sample, number of intervention groups, randomisation procedure, statistical methods).
Details about the participants, including PROGRESS‐Plus characteristics and number in each group at baseline and at the endpoint. PROGRESS‐Plus characteristics refer to characteristics of participants that can be used to identify disadvantaged groups and that allow us to differentiate the effects of the intervention across social categories (Tugwell 2010). These characteristics include: place of residence, race or ethnicity, occupation, gender, religion, education, socioeconomic status and social capital; and Plus characteristics include age). We extracted details about withdrawals and dropouts, if these were available.
Details about the intervention, including process measures (e.g. aims; social and cultural context; comparison interventions; length of the intervention; duration of follow‐up; implementation factors such as amount of conditional cash transfers, number of times transport is given or total amount of food vouchers given to each individual), and whether the intervention was universal or targeted. This information aimed to provide insight on the factors that may impair or facilitate implementation of the intervention, which addresses the second objective of this review. We also extracted information on whether the intervention aimed to improve access to nutritious food, how nutritious food was defined, if specific nutritious foods were targeted for increased access and what types of food were accessed by participants.
Description of outcomes used to measure effectiveness and how they were measured.
Primary outcomes at the household and community level.
Secondary outcomes at the individual level.
Other process measures including intervention cost and sustainability.
Source of study funding and sponsorship of the interventions.
We incorporated the Cochrane‐Campbell Methods Group Equity Checklist into our data extraction form (methods.cochrane.org/sites/methods.cochrane.org.equity/files/public/uploads/EquityChecklist2012.pdf); however, the included studies reported very little of this information.
We extracted information on potential confounders or moderators of the study outcomes. These included sociodemographic variables such as gender, ethnicity or race, and place of residence, and other PROGRESS‐Plus characteristics based on the details available in the studies.
When necessary, we contacted the authors of primary studies to for clarification or to seek missing information.
We used Review Manager 2014 for data management and analysis.
Assessment of risk of bias in included studies
Author pairs (SD, AS, MV, AB, JO, VR, BS) conducted the risk of bias assessment and resolved disagreements through discussion or arbitration by a third author. Risk of bias assessments were also carried out in Covidence.
We assessed the risk of bias for all RCTs and PCS using the EPOC risk of bias tool for studies with a separate control group (EPOC 2017). This tool assesses the same risk of bias domains as the Cochrane 'Risk of bias' tool for RCTs (Higgins 2011), namely sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data (including loss of clusters in the case of cRCTs), selective outcome reporting and other bias. It also includes additional domains to assess the risk of bias from inappropriate methods regarding: similarity of baseline outcome measurements, similarity of baseline characteristics and whether the study was protected against contamination. For other bias, we specifically assessed misclassification bias of the exposure, measurement bias and two domains related to cRCTs: incorrect analysis (i.e. whether the study adjusted for clustering) and recruitment bias. We assessed the risk of bias from lack of blinding of participants and personnel and of outcome assessors separately. We had planned to assess the risk of bias from lack of blinding separately for objective and subjective outcomes and to assess the risk of bias from incomplete outcome data separately for different outcomes. However, given the disparity and multiplicity of outcomes reported, we decided not to do this. However, we did consider whether the outcome was objective or subjective when assessing the risk of bias from lack of blinding.
We had planned to use the EPOC risk of bias tool for ITS study designs; however, we included no ITS studies.
For each item, we made a judgement of 'High risk', 'Unclear risk', or 'Low risk', with supportive information to justify these judgements provided in the Characteristics of included studies table. We incorporated the risk of bias assessment in the interpretation of our review findings, and we did not restrict analysis by degree of risk of bias. We presented a 'Risk of bias' graph and a summary figure.
To assess overall risk of bias at study level, we considered its risk of bias for two key domains: selection and attrition bias. For example, if a study was classified at high risk of either selection or attrition bias, it was classified as having overall high risk of bias.
Measures of treatment effect
Where data allowed, we conducted meta‐analysis using Review Manager 5 (Review Manager 2014). However, due to sparsely reported data, we were unable to conduct a meta‐analysis in many instances.
For binary outcomes, we planned to report the risk ratio (RR) of outcomes in the intervention group compared to the control group. Only one included study reported the RR as an overall effect measure for the intervention. The other 28 included studies that reported dichotomous outcomes reported the change in proportion using percentage points (pp) (68%) or using reported odds ratios (OR) (32%).
For continuous outcomes, and where baseline data were available, we reported the mean difference (MD) between the change in the intervention and control groups if the outcomes had been measured in the same way by all studies. If the continuous outcomes were measured in distinct ways in different studies in a comparison, we used the standardised mean difference (SMD) between the intervention and control groups. Where the change per group was not available, we used end values where randomisation was successful. If there was a reasonable risk of selection bias, and the change per group was not available, the study was not included in a meta‐analysis.
The included studies reported mostly estimates from regression or from difference‐in‐difference analyses, which were interpretable as an MD and thus were reported as such. None of the studies reported the effects per group, and in most cases the data were only available either for baseline or endline, and if it was available, often there was no measure of variance reported. Thus, we described the effect measures as reported in the included studies.
We reported 95% confidence intervals (CIs) alongside all effect estimates, when these were available or when it was possible to calculate them. Calculations of 95% CI were done in Review Manager (using the inverse variance option; Review Manager 2014) or using a Microsoft Excel 2007 spreadsheet with the formula to calculate the 95% CI from the regression estimate and standard error (SE) value. We report P values only where no 95% CI was reported or could be calculated to illustrate the strength of evidence for the effect size.
Unit of analysis issues
cRCTs that randomise groups rather than individuals to intervention groups and that report analyses at the individual level needed to also report the method used to account for clustering. A biostatistician (YB) checked all studies to ensure that the clustering effect had been accounted for correctly. If they had not taken the clustering effect into account in their analyses, we would have requested individual participant data, calculated an intracluster correlation coefficient (ICC), and re‐analysed the data appropriately. If we had been unable to obtain primary data, we would have attempted to find an appropriate ICC from the literature and adjust the sample size accordingly. We had planned to meta‐analyse the effect estimates and SEs from cRCTs using generic inverse‐variance methods in Review Manager 2014. If we had re‐analysed the data, we would have clearly marked the results as re‐analysed and we would have stated where re‐analysis had not been possible. However, we did not have to re‐analyse the data for included cRCTs as they all correctly accounted for clustering.
In cases where the outcomes were measured at multiple time points, we had planned to group the outcomes measured at similar time points where this was possible. For any particular outcome, if most studies were reporting a specific time point and only one study reported multiple time points, we reported the most commonly reported time point. In most cases, the time points were similar and, for the few instances where this was not the case, we extracted measures from all time points but reported the latest time point. Taking into account that the minimum duration after implementation at which we extracted outcomes was three months, the short‐term time point was three to six months.
We only considered outcomes reported immediately at the end of the intervention, not postintervention follow‐up.
In many cases, studies reported multiple outcome measures for the same outcome domains. To prioritise the outcomes, we selected the measure that provided the largest scale measure of the domain (i.e. the most comprehensive outcome). For example, in cases where individual and composite measures for the same outcome domain were reported for the same study, we preferentially reported composite measures as these are probably more useful to decision‐makers. For anthropometry, we did not report effects on weight and height units, but rather reported z‐scores for weight‐for‐age and height‐for‐age, in which weight and height are assessed against a reference standard. All outcomes reported in a study are presented in the Characteristics of included studies table, as well as an indication of which were selected for synthesis.
For interventions with multiple comparison groups, all groups that met this review's inclusion criteria were included. If there were more than two relevant comparison groups for the same intervention, we attempted to combine the relevant experimental and control groups to make a single pairwise comparison. This was the case in three studies, for which two interventions groups were combined. If this was not possible, we made multiple pairwise comparisons between the relevant groups and divided the sample size of the shared intervention group evenly across the comparisons to avoid double counting of participants in a meta‐analysis. If a meta‐analysis was not possible and we could not combine the results of different groups, we presented the results of all relevant groups.
Dealing with missing data
If there were unclear or missing data related to study methodology, participants lost to follow‐up, outcome data or statistics, we contacted the study's primary author via email. We recorded all communications with authors in Appendix 3.
We recorded all missing outcome data in the data extraction form and in the Characteristics of included studies table. If it was not possible to obtain missing outcome information after attempting to do so, we would have excluded these studies from the meta‐analysis. We did not exclude any studies due to missing outcome data.
Five included studies did not report the number analysed for at least one outcome (for which the number (n) is stated as not reported (NR)) (Ahmed 2019a; Ahmed 2019b; Andaleeb 2016; Ferre 2014; Hoddinott 2013). This lack of reporting reduces our confidence in the estimated treatment effect as we are unable to assess if the study was powered to detect an effect, analysed accounting for any clustering or if attrition bias was likely. In addition, it has been shown that trial sample sizes can influence treatment effect, with smaller studies reporting larger effect estimates (Dechartres 2013). With no sample sizes reported, it is difficult to ascertain whether this bias exists.
Assessment of heterogeneity
Where we were able to meta‐analyse, we assessed heterogeneity, or the variability among the studies included in a meta‐analysis, by visual inspection of overlap of CIs, and by assessing statistical heterogeneity with the Chi2 statistic (P < 0.1) (Deeks 2019). We calculated the I2 statistic to quantify heterogeneity; with an I2 statistic of 75% and above indicating substantial heterogeneity. We also calculated Tau2, which reflects the extent of variation among intervention effects in different studies, to assess heterogeneity (Deeks 2019). However, in most cases, we were unable to carry out meta‐analyses or create forest plots due to heterogeneity. Instead, we assessed clinical, methodological and conceptual heterogeneity, through tabulation of characteristics of studies included in the same synthesis. For specific comparisons and outcomes, we assessed clinical or conceptual heterogeneity by considering variability in the participants and interventions, or co‐interventions, including study duration, intervention dosing and outcome assessment. We assessed methodological heterogeneity by considering the variability in study design and risk of bias (Deeks 2019; Singh 2017).
Assessment of reporting biases
We had planned to assess the likelihood of reporting bias through funnel plots for each outcome with 10 or more included studies in a meta‐analysis (Sterne 2019). We would have assessed the funnel plots visually for sources of asymmetry, such as small‐study effects, publication bias or other. If it was likely that asymmetry was caused by small‐study effects, we would have conducted sensitivity analysis to explore how this affected the results and conclusions of the meta‐analysis. However, we were unable to do this as none of the compared outcomes were assessed by at least 10 studies.
Data synthesis
In most cases, we were unable to include all studies reporting a specific outcome domain in a meta‐analysis. This was due to studies reporting multiple measures for the same domain that could not be combined, either because there was missing information regarding variance measures, or because the effect measures reported could not be converted to a standardised metric. Therefore, we synthesised the data from all studies reporting on the same outcome domain using vote counting based on the effect direction method (McKenzie 2019). The results of individual studies were presented in one of four categories: 1. 'favours control' if the point estimate favoured the control and the 95% CI did not cross the null; 2. 'unclear effect; potentially favouring the control' if the point estimate favoured the control but the 95% CI crossed the null; 3. 'unclear effect; potentially favouring the intervention' if the point estimate favoured the intervention and the 95% CI crossed the null; and 4. 'favours intervention' if the point estimate favoured the intervention and the 95% CI did not cross the null. Where no CI was provided or could be calculated, we decided whether the effects were 'clear' or 'unclear' based on provided P values. However, P values did not inform the effect direction reported. Although this is a useful method to synthesise data when meta‐analysis is not possible, there are some limitations associated with this method, for example, it does not provide information on the magnitude of effects, does not account for differences in the relative sizes of the studies and is a less powerful method than that used to combine P values (McKenzie 2019).
Regarding the effect direction synthesis, we reported the number of studies with results in the different effect categories for each outcome domain, and the probability of observing this based on the multinomial distribution (for outcome domains with two or more studies and assuming the true proportion is 0.25 for all categories). This information was reported in the first paragraph reporting results for a specific outcome in the effects of interventions section. If a meta‐analysis of all studies in the outcome domain was possible, the multinomial distribution P value was not reported. To visually display the results for key outcomes included in the 'Summary of findings' tables, we created harvest plots for each comparison. These harvest plots depict data both from RCTs and from PCS for key summary of findings outcomes. We presented the results of the effect direction synthesis separately for RCTs and for PCS, in the Effects of interventions section.
In some instances, we were able to carry out a meta‐analysis, either for all studies reporting on the same outcome measure (n = 35), or for a subset of studies that could be combined in a meta‐analysis (n = 8). We conducted meta‐analyses in Review Manager 2014 if the included studies were sufficiently homogeneous (I2 < 75%) and if there was a minimum of two studies for any type of intervention being compared reporting the same outcome measure. Not pooling results in cases of high heterogeneity is an accepted approach in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2019). We also explored heterogeneity and reported this when there was high heterogeneity. We did not have sufficient data to carry out any subgroup analysis or meta‐regression to more formally explore heterogeneity. We carried out meta‐analyses separately for each outcome and type of study design, and we used the random‐effects model for all analyses to account for any existing heterogeneity. We generated forest plots for each comparison and outcome where meta‐analyses could be carried out (see Data and analyses).
In preparation for synthesis, we first grouped all studies assessing the same intervention categories to identify which studies could be grouped under each preplanned comparison, and no changes to prespecified grouping were required. The comparison groups were based on the pre‐specified types of interventions listed in table 2: cash transfers (unconditional; conditional), income generation interventions, food vouchers, food subsidies, and social support interventions. Under each comparison, we tabulated the available data and time frames reported for each outcome, which helped identify what data were available, and thus where meta‐analysis was possible and where we had to synthesise using effect direction. A meta‐analysis was possible if the effect and variance estimates were available for all studies or could be calculated from the available data, and if all effect estimates were of the same type (e.g. OR or MD) or could be converted for the comparison (e.g. OR to SMD). Where necessary, we converted OR to SMD, MD to SMD, or MD to SMD to OR.
We prepared two additional types of tables to aid visualisation of available data. One was the 'Overview of included studies' table, summarising main characteristics and reported outcomes of included studies for each comparison (McKenzie 2019). In this table, we organised studies first by study design, with RCTs first followed by PCS, and second according to their overall risk of bias (low, unclear and then high risk of bias). The second type were tables with the results for individual studies, for each comparison, for scrutiny by the reader. The studies in these tables were also ordered according to their overall risk of bias.
We had planned to assess and discuss the implementation factors common to effective interventions, if this information was reported in included studies or in published process evaluations that are mentioned in the study report. However, there was insufficient information from included studies on this.
Subgroup analysis and investigation of heterogeneity
We did not have enough data per outcome and comparison to carry out subgroup analyses. If data allowed, we would have conducted subgroup analysis to assess effectiveness for people at different levels of disadvantage. In updates of this review, we will include the following subgroups.
Geographic location (e.g. urban versus rural, country or region).
Sex (male versus female).
Age (e.g. elderly people, adults, children, infants).
Baseline nutritional status (e.g. underweight, overweight, micronutrient deficiencies).
We would also have assessed important implementation factors through subgroups analyses, including the following.
Intensity of intervention (high intensity versus low intensity, e.g. in relation to amount of food vouchers or of conditional cash transfers).
Length of study and follow‐up (e.g. three to six months, more than six months to less than two years, and two years and beyond).
Whether the intervention specifically aimed to improve access to nutritious food.
These analyses would have allowed further exploration of heterogeneity. In order to compare the different subgroups with each other, we would have conducted a standard heterogeneity test in Review Manager 2014 across the subgroup results, by calculating the I2 statistic. We would have made sure that the subgroup data being compared were independent.
Sensitivity analysis
We conducted a sensitivity analysis to assess risk of bias for outcomes with five or more studies. Studies with overall low risk of bias were included in the sensitivity analysis. We reported the results of study designs separately.
Summary of findings and assessment of the certainty of the evidence
The 'Summary of findings' tables include information regarding the number of participants and studies for key outcomes, a summary of the intervention effect and a measure of the certainty of evidence for each outcome according to GRADE considerations. GRADE is a system of rating certainty of evidence in systematic reviews (Guyatt 2010). We rated the overall certainty of evidence for a particular outcome on‐line with GRADEpro as high, moderate, low or very low. All RCTs started at high‐certainty evidence and the following factors were considered to downgrade the certainty: overall risk of bias, consistency of effect, imprecision, indirectness and publication bias. All PCS started at low‐certainty evidence and the following factors would have been considered to upgrade the certainty: large magnitude of effect, dose‐response gradient and effect of plausible residual confounding. We did not upgrade the certainty of evidence for PCS as there were existing reasons for downgrading (Schünemann 2019). As most of the evidence was not from pooled data, we used the 'Summary of findings' table format for narrative synthesis.
We had planned to include a 'Summary of findings' table for the primary outcomes of this review. However, we decided to also include some of the secondary outcomes. The choice of outcome categories and specific outcome measures to report in the 'Summary of findings' table were decided by the review author team through in‐depth discussion until consensus was reached, taking into consideration which outcomes would be useful to decision‐makers. The 'Summary of findings' tables included the following outcomes.
Prevalence of undernourishment.
Proportion of household expenditure on food.
Proportion of households who were food secure.
Dietary diversity.
Stunting.
Wasting.
Cognitive function and development.
Three authors met to rate the evidence per outcome for each of the 'Summary of findings' tables. Decisions about whether to downgrade or not were made through discussion and reaching consensus. Evidence on different outcomes was available from different study designs. Where there was evidence for a particular outcome from both RCTs and PCS, we reported the data from the RCTs in the 'Summary of findings' table. When there were no data from RCTs for a particular outcome, we reported data from PCS that reported that outcome. We reported the certainty of the evidence in the Effects of interventions for outcomes which assessed with GRADE. For other outcomes, we report the risk of bias, as an indicator of the certainty of the evidence to consider when interpreting the findings.
Results
Description of studies
Results of the search
We screened titles and abstracts of 15,477 deduplicated records identified through searching electronic databases and reference searching of eligible studies. Of these, we assessed the full texts of 463 records against the eligibility criteria. After assessing available full‐texts, we included 59 studies reported in 116 records in this review. Some interventions were reported in more than one study, and two records each reported on two different studies. Of the remaining records: we placed 39 studies under awaiting classification as we could not access them or they were conference abstracts, 11 studies are still ongoing and we excluded 297 records with reasons. In the Characteristics of excluded studies table, we report a subset of key excluded studies. The study selection process is described in Figure 2.
2.
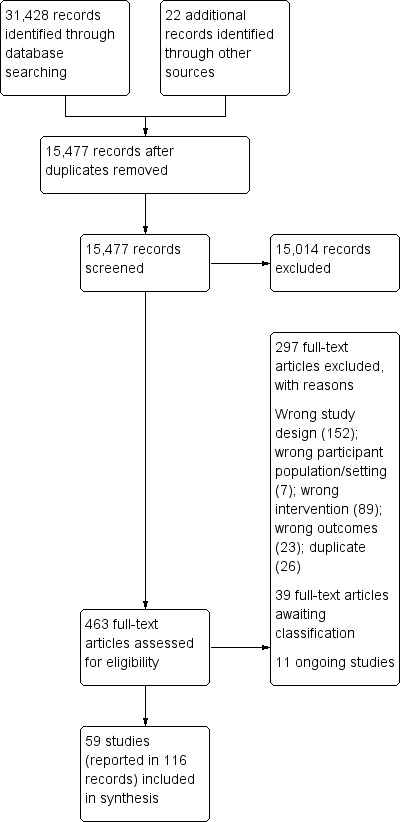
Study flow diagram.
Included studies
We included 59 studies in this review (Table 9). In this section we provide a summary overview of included studies. More details are provided in the results of interventions section, for studies included in each comparison, and in the Characteristics of included studies table.
3. Summary of included studies.
aBaird 2013 assesses both conditional and unconditional cash transfers. bFenn 2015 assesses both unconditional cash transfers and food vouchers. cHidrobo 2014 assesses both conditional cash transfers and food vouchers. dThis includes different interventions that aimed to generate income of participants (e.g. integrated agricultural programmes, community development programmes). ePorter 2016 assessed a public works (80%) (cash/food‐for‐work) or unconditional cash transfer government programme (20%). Results were reported for the entire population, not disaggregated according to intervention received.
RCT: randomised controlled trial.
Study design, sample size and follow‐up
Of the 59 studies included:
36 were RCTs: six with individual or household level randomisation (Baird 2013; Daidone 2014; Gangopadhyay 2015; Haushofer 2013; Jensen 2011; Macours 2012), and 30 with cluster/group randomisation (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Beegle 2017; Brugh 2018; Chen 2019; Darrouzet Nardi 2016; Evans 2014; Fenn 2015; Fernald 2011; Gertler 2000 (PROGRESA); Hidrobo 2014; Hjelm 2017; Hoddinott 2013; Kandpal 2016; Kurdi 2019; Kusuma 2017b; Kusuma 2017a; Maluccio 2005; Marquis 2018; Merttens 2013; Miller 2011; Olney 2016; Osei 2017; Pellerano 2014; Ponce 2017; Schwab 2013; Skoufias 2013; Tonguet Papucci 2015; Verbowski 2018);
23 were PCS (Aguero 2006; Alaofe 2016; Alaofe 2019; Andaleeb 2016; Andersen 2015; Asadullah 2015; Breisinger 2018; Brunie 2014; Chakrabarti 2018; Doocy 2017; Ferre 2014; Huerta 2006 (PROGRESA); Jodlowski 2016; Kangmennaang 2017; Katz 2001; Kennedy 1989; Leroy 2008 (PROGRESA); Lopez Arana 2016; Murshed E Jahan 2011; Porter 2016; Renzaho 2017; Sturm 2013; Weinhardt 2017). Huerta 2006 (PROGRESA) is a nested study of the PROGRESA cluster‐RCT (Gertler 2000 (PROGRESA)).
It is important to note that three studies, of different design, evaluated the same programme: PROGRESA (Gertler 2000 (PROGRESA); Huerta 2006 (PROGRESA); Leroy 2008 (PROGRESA)) (Table 10). In addition, two studies assessed the effects of a programme in Malawi in different study settings (Miller 2011; Brugh 2018), whereas two studies reported the effects of an income‐generation intervention during different periods (Alaofe 2016; Alaofe 2019).
4. Description of included studies assessing the effects of Mexico's PROGRESA/Oportunidades conditional cash transfer programme.
| Study ID | Linked references | Study design and duration | Description of intervention | Sampling | Outcomes reported |
| Gertler 2000 (PROGRESA) | Gertler 2004; Hoddinott 2000; Hoddinott 2003a; Hoddinott 2004(?); Skoufias 2001; Skoufias 2007; Fernald 2008; Fernald 2009 |
Cluster‐RCT conducted between 1998 and 2000, where communities were randomly allocated to either receive the intervention immediately (intervention group) or to receive the intervention 2 years later (control group). In reality, control communities started receiving the intervention in late 1999, about 1.5 years after the intervention communities. Timepoints of data collection (through household surveys – ENCEL):
|
'Oportunidades' (previously called Progresa) is a conditional cash transfer programme implemented by the Mexican government since April 1998. Women in eligible households receive cash transfers every 2 months (a food and an education transfer) if they adhered to specific conditionalities: all family members attend preventive health services regularly; children aged 0–5 years and lactating mothers attended nutrition monitoring clinics for growth monitoring, immunisation, to obtain nutrition supplements, and for nutrition and hygiene education; pregnant women attend antenatal care, receive nutritional supplements and health education. The education transfers included scholarships for school attendance and school supplies, and was dependent on children's school attendance. The value of the transfers was about 20–30% to the household consumption expenditure preintervention. |
506/50,000 eligible rural villages were randomly selected based on the index level of community poverty. Of these, 320 communities were allocated to the intervention group and 186 to the control group. Within each community, households were selected by proxy means testing and selection validated in a community assembly. Some studies assessed outcomes in a subsample of the study population. Fernald 2008 followed up on a sample of children in 2003: children aged 24–72 months in the 'Early intervention' group (from 144 communities), and children aged 2–5 years in the 'Late intervention' group (from 108 communities). Fernald 2009, followed up a sample of children in 2007: 1093 children aged 8–10 years in the 'Early intervention' group, and 700 children aged 9–10 years in the 'Late intervention' group. |
|
| Huerta 2006 (PROGRESA) | Rivera 2004; Gertler 2004; Behrman 2001 |
Nested cohort study conducted on a subset of the larger cRCT sample (described above), including a random selection of 205 of original intervention communities and 142 of original 186 control communities. Additional household surveys conducted on health and nutrition indicators. Time points of data collection:
|
As above | Subsample of children selected. Behrman 2005 (?) Rivera 2004: children aged < 12 months (461 children from 175 communities in the intervention and 334 children from 107 communities in the control). Gertler 2004 and Huerta 2006: sample sizes not reported |
No outcome data reported for exposed vs non‐exposed groups after 1 year of follow‐up (Rivera 2004; Huerta 2006) (?). |
| Leroy 2008 (PROGRESA) | N/A |
CBA: urban communities randomly selected for expansion of Oportunidades into 149 urban areas. The control group comprised eligible households that did not enrol in the programme. Time points of data collection through household surveys:
|
As above | Children aged < 24 months in 2002: 574 in intervention and 159 in control |
|
CBA: controlled before‐after study; cRCT: cluster randomised controlled trial; HAZ: height‐for‐age z‐score; N/A: not applicable/available; RCT: randomised controlled trial; WHZ: weight‐for‐height z‐score.
All studies had a control group. Most studies compared the intervention with a control group where there was no intervention implemented, six studies compared the intervention with another food security‐related intervention (Andaleeb 2016; Chakrabarti 2018; Gangopadhyay 2015; Hoddinott 2013; Renzaho 2017; Schwab 2013), and one study compared the intervention with another intervention unrelated to food security (Weinhardt 2017). Four studies had three intervention groups (Chen 2019;Gangopadhyay 2015;Ponce 2017; Verbowski 2018 ), four studies had four intervention groups (Brunie 2014; Fenn 2015; Hidrobo 2014; Skoufias 2013), and two studies had five intervention arms (Ahmed 2019a; Ahmed 2019b). In all but three cases the study groups were either not relevant for the review or they pertained to different comparisons, therefore, there were no issues with overlapping control groups. For three studies with two relevant intervention arms, these were combined. In some studies, the control group received the intervention at a later stage; this review only captured data for the period during which the control group was not yet receiving the intervention.
The unit of allocation or exposure to the intervention was at group level in 41 studies (including communities, electoral divisions, municipalities, parishes, districts, villages, other), at household level in 14 studies (Alaofe 2016; Andersen 2015; Asadullah 2015; Gangopadhyay 2015; Haushofer 2013; Huerta 2006 (PROGRESA); Jensen 2011; Jodlowski 2016; Kennedy 1989; Kurdi 2019; Leroy 2008 (PROGRESA); Macours 2012; Porter 2016; Sturm 2013), and individual level in four studies (including individuals, women, and children) (Aguero 2006; Baird 2013; Katz 2001; Murshed E Jahan 2011).
The sample size in included studies ranged from 214 to 169,485 participants and 300 to 124,644 households. All studies collected data on individual participants except for Sturm 2013, which collected supermarket sales data.
Maximum follow‐up was three months in one study (Hoddinott 2013), greater than three months to 12 months in 10 studies (Alaofe 2016; Alaofe 2019; Chen 2019; Fenn 2015; Gangopadhyay 2015; Hidrobo 2014; Jensen 2011; Miller 2011; Ponce 2017; Schwab 2013), greater than 12 months to two years in 25 studies, greater than two years to five years in 17 studies (Asfaw 2014; Baird 2013; Beegle 2017; Breisinger 2018; Brunie 2014; Chakrabarti 2018; Doocy 2017; Evans 2014;Hjelm 2017; Kurdi 2019; Lopez Arana 2016; Macours 2012; Murshed E Jahan 2011; Osei 2017; Sturm 2013; Tonguet Papucci 2015; Weinhardt 2017), and greater than five years to nine years in six studies (Aguero 2006; Andaleeb 2016; Andersen 2015; Asadullah 2015; Porter 2016; Renzaho 2017).
Interventions
Included interventions were classified according to the categories of interventions in our logic model (Figure 1; Table 8). See Table 9 for a summary of categories and types of interventions included in this review.
Fifty‐two studies assessed interventions aimed at increasing buying power, including:
unconditional cash transfers (18 RCTs: Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Baird 2013; Brugh 2018; Daidone 2014; Fenn 2015; Fernald 2011; Gangopadhyay 2015; Haushofer 2013; Hjelm 2017; Hoddinott 2013; Merttens 2013; Miller 2011; Pellerano 2014; Schwab 2013; Skoufias 2013; Tonguet Papucci 2015; three PCS: Aguero 2006; Breisinger 2018; Renzaho 2017), and
conditional cash transfers (nine RCTs: Baird 2013; Evans 2014; Gertler 2000 (PROGRESA); Hidrobo 2014; Kandpal 2016; Kurdi 2019; Kusuma 2017a; Macours 2012; Maluccio 2005; five PCS: Andersen 2015; Ferre 2014; Huerta 2006 (PROGRESA); Leroy 2008 (PROGRESA); Lopez Arana 2016), and
interventions to generate income (six RCTs: Beegle 2017; Darrouzet Nardi 2016; Marquis 2018; Olney 2016; Osei 2017; Verbowski 2018; 11 PCS: Alaofe 2016; Alaofe 2019; Asadullah 2015; Doocy 2017; Jodlowski 2016; Kangmennaang 2017; Katz 2001; Kennedy 1989; Murshed E Jahan 2011; Porter 2016; Weinhardt 2017). Under the income‐generation category, each individual study assessed different types of interventions, including agricultural programmes, livestock transfer programmes or community‐based programmes) (Table 11).
5. Income‐generation interventions – overview of included studies.
| Study (country of conduct) | Study design | Overall risk of biasa | Other key details of intervention | Population (sample size at baseline: Intervention/ Control) | Outcome domains and measures with available data | Time point of measurement |
| Darrouzet Nardi 2016 (Nepal) | cRCT | Unclear |
Programme name: Heifer training curriculum Programme description and frequency: participation in programme that focused on training regarding poverty alleviation, citizen empowerment, community development and optimisation of livestock management as means to generate income. Provider: NGO (Heifer International) Delivery: women's self‐help groups which met with a trained facilitator, supplemented by specific interactive instruction, workshops, guidance, and training. Biweekly meetings Co‐interventions: none reported |
Rural farming communities; HHs: 201/214; children (aged 6–60 months): 283/324 | Dietary diversity:
Anthropometry
|
1 and 2 years |
| Doocy 2017 (Democratic Republic of the Congo) | Prospective controlled study | High |
Programme name: Intervention implemented as part of the Jenga Jamaa II project Programme description and frequency: WEGs met weekly and meetings served as a delivery mechanism for a variety of interventions including literacy and numeracy, business and marketing training, and income‐generation activities. Savings and credit groups were started in each WEG. Beneficiaries were provided with a starter kit of basic materials for their income‐generation activity. Many WEG participants also received goats and energy‐efficient stoves. The FFS intervention provided farmers with experience‐based education on farming practices and postharvest handling as well as business and natural resource management skills. Each FFS group received semi‐monthly training sessions for 2 years. Each FFS group had a community demonstration plot, and group members also received starter packages of seeds and tools for use on individual farms. The FFS programmes focused on a variety of common crops in the region. The first year of training focused on knowledge of production systems and technologies; adoption of techniques and technologies and behaviour change were the focus in the second year Provider: ADRA Delivery: FFS – training sessions on agriculture techniques and other content by ADRA field agents. Co‐interventions: after they finished the FFS intervention (2 years) some transitioned to farmer business associations, which were intended to improve access to credit and marketing opportunities. |
Farming villages; HHs (WEG: 390/324; FFS: 338/324) | Food security:
Dietary diversity:
|
3.5 years |
| Weinhardt 2017 (Malawi) | Prospective controlled study (non‐equivalent control group) | Unclear |
Programme name: support to able‐bodied vulnerable groups to achieve food security (SAFE) programme Programme description and frequency: programme comprised 4 components
Provider: NGO (CARE Malawi) Delivery: community‐based programme Co‐interventions: agricultural education programme for a few intervention and control participants |
Rural HHs (598/301) | Food security:
Anthropometry:
|
18 and 36 months |
| Jodlowski 2016 (Zambia) | Prospective controlled study | Low |
Programme name: Copperbelt Rural Livelihoods Enhancement Support Project (CRLESP) Programme description and frequency: ongoing training and one‐off transfer of livestock contingent on training participation. 1 female livestock offspring per transferred female had to be donated to a Pass‐on‐the‐Gift HH. Provider: NGO (Heifer International) Delivery: NR Co‐interventions: none reported |
Rural households (105/178) | Dietary diversity:
|
6, 12 and 18 months |
| Asadullah 2015 (Bangladesh) | Prospective controlled study | High |
Programme name: challenging the frontiers of poverty reduction – targeting the ultra‐poor (CFPR‐TUP) Programme description and frequency: multicomponent intervention including orientation training, selection of income‐generation microenterprise by female participants with one‐off transfer of productive assets worth BDT 10,000 to support it (90% of households chose livestock combination), community savings, monthly health worker visits, weekly follow‐up for technical advice, building social capital (village support networks and sponsorship of community leaders), and weekly stipends (BDT 70). Provider: NGO (Bangladesh Rural Advancement Committee (BRAC)) Delivery: NGO staff deliver training and assets Co‐interventions: none reported |
Ultra‐poor households (2633/2993) | Food security
Morbidity:
|
3, 6 and 9 years |
| Marquis 2018 (Ghana) | cRCT | Low |
Programme name: Nutrition Links (NL) Programme description and frequency: 12‐month intervention was an integrated package of agricultural inputs and training as well as education in nutrition, health care and child stimulation for participants. The intervention had 4 main components
Provider: "Heifer's Passing on the Gift (POG) community development programme, project staff, district agricultural extension officers, district government staff, University of Ghana's Nutrition Research and Training Centre Delivery:
Co‐interventions: none reported |
Mother–infant pairs in rural communities (287/213). | Dietary diversity
Anthropometry:
|
1 year |
| Olney 2016 (Burkina Faso) | cRCT | Unclear |
Programme name: enhanced‐homestead food production (EHFP) Programme description and frequency: integrated agriculture and nutrition programme. Agriculture interventions included provision of land with inputs (crops, animals and implements) and training. Nutrition intervention included behaviour change communication strategy for health and nutrition behaviours, delivered through visits by community volunteers twice per month. Provider: NGO (Helen Keller International – HKI) Delivery: agriculture interventions rolled out first to female village farm leaders, who then trained other mothers. Nutrition education carried out by older women leaders or health committee members. Co‐interventions: none reported |
Villages with agricultural homesteads (30/25). HHs: 514 (health committee); 512 (older women leaders); 741 (control) | Dietary diversity:
Anthropometry:
|
2 years |
| Osei 2017 (Nepal) | cRCT | Unclear |
Programme name: Enhanced Homestead Food Production (EHFP) programme Programme description and frequency: training in improved gardening and poultry‐rearing practices; hosting of a village model farm, which served as a site for purchasing inputs and ongoing training for all the beneficiary women. For every season (rainy and winter) of the first year, each woman was given a one‐off free supply of seeds, saplings and locally bred chicks to establish their home gardens and poultry production. Throughout the period of the intervention, the women met monthly at the farm to refresh lessons on agriculture techniques and nutrition through social and behaviour change communications. During monthly home visits, the project staff and the female community health volunteers also reinforced the educational messages on breastfeeding and complementary feeding to all mothers. Provider: NGO (Helen Keller International – HKI) Delivery: 1 woman per group of intervention villages (5 or 6) was selected and trained by HKI and this woman then trained 20 other beneficiary women; meetings at farm; home visits by trained project staff, female community health volunteers and agriculture extension officers. Co‐interventions: none reported. |
Homesteads: mothers (1055/1051), children (1055/1051) | Food security
Anthropometry:
Biochemical indicators:
Morbidity:
|
2.5 years |
| Verbowski 2018 (Cambodia) | cRCT | Unclear |
Programme name: Fish on Farms (FoF) project using the Enhanced Homestead Food Production (EHFP) programme Programme description and frequency: basic agricultural inputs and training, and nutrition and hygiene education. The education focused on optimal nutrition for women and infants and young child practices, and the use of nutrient‐dense produce grown by farmers were demonstrated. The purpose of EHFP was to increase production and intakes of various types of vegetables, herbs and tree fruit. The aquaculture intervention was designed to increase the production of 3 types of small fish, which typically were consumed whole, as well as 3 types of large fish (typically sold for income or fillets consumed). Provider: NGO (Helen Keller International – HKI, local) Delivery: trained village health volunteers provided education sessions, through small group and 1‐to‐1 counselling. Cooking demonstrations were also conducted. Support was provided through village model farms (1 in each village). Co‐interventions: none reported. |
Rural HHs: EHFP + aquaculture (100), EHFP (100) and control (100) | Anthropometry:
Biochemical indicators:
Morbidity:
|
22 months |
| Murshed E Jahan 2011 (Bangladesh) | Prospective controlled study | Unclear |
Programme name: Development of Sustainable Aquaculture Project (DSAP) Programme description and frequency: farmers received support to efficiently implement integrated aquaculture‐agriculture (IAA) approaches under 2 models – 1 with a one‐off provision of a small grant for purchasing inputs (value not reported) and 1 without, with training provided (3 sessions in the first year, 2 in the second year and 1 in the third year). Provider: NGO; WorldFish Center Delivery: farmers trained in recording required information which was collected bi‐monthly by research assistants. Co‐interventions: none reported |
Small‐scale farmers (260/126). Within intervention farmers: 127 grant farmers, 133 non‐grant farmers |
Proportion of HH expenditure on food | 3 years |
| Kennedy 1989 (Kenya) | Prospective controlled study | Unclear |
Programme name: South Nyanza Sugar Factory (Sony) smallholder sugarcane outgrowers' scheme Programme description and frequency: farmers were enrolled into the scheme to provide sugarcane to a new factory, with payments to farmers after every harvest (24 months after planting) Provider: Kenyan government Delivery: contract agreement between farmers and factory. Co‐interventions: none reported |
Smallholder farm HHs (181/231). Within intervention: 139 sugar farmers and 42 new entrant |
Adequacy of dietary intake
Anthropometry
Morbidity:
|
2 years |
| Alaofe 2016 (Benin) | Prospective controlled study | Unclear |
Programme name: Solar Market Gardens (SMG) Programme description and frequency: drip irrigation powered by solar water pump, using a perennial stream or borehole, with continued maintenance and training to farmers provided. Provider: NGO (Solar Electric Light Fund – SELF) Delivery: installation of system and training of local technicians carried. Co‐interventions: women's agriculture group activities. |
Rural HHs (116/98) In both intervention and control groups, HHs included women who participated in women's agriculture groups (59/38) or not (60/60) |
Proportion of HH expenditure on food | 1 year |
| Alaofe 2019 (Benin) | Prospective controlled study | Unclear |
Programme name: Solar Market Garden (SMG) Programme description and frequency: Installation of a low‐pressure drip irrigation system, combined with a solar‐powered water pump in each intervention village. Each SMG was used jointly by 30–35 women belonging to the local women's agriculture group (each woman farmed her own land of 120 m2). Provider: NGO (Solar Electric Light Fund – SELF) Delivery: expanded installation of SMG systems (from programme reported in Alaofe 2016). Co‐interventions: women's agriculture group activities. |
Women in rural HHs (415/359). In both intervention and control groups, HHs included women who participated in women's agriculture groups (184/126) or not (228/233) |
Dietary diversity:
Anthropometry
Biochemical indictors:
Morbidity:
|
1 year |
| Kangmennaang 2017 (Malawi) | Prospective controlled study | High |
Programme name: the Malawi Farmer to Farmer Agroecology project (MAFFA). Programme description and frequency: farmers do their own experimentation with agroecological methods. Farmers are also encouraged to share knowledge gained with other farmers. MAFFA encourages farmers to adopt a suit of innovations rather than just a single innovation and to encourage farmer‐led learning. In addition to crop diversification, many farmers increased or began to apply compost and manure to their rain‐fed fields. Some farmers also experimented with botanical pesticides. Also, MAFFA goes beyond agroecological training to focus on knowledge sharing, leadership support, nutrition and attention to social inequalities. Provider: Soils, Food and Healthy Communities organisation of Ekwendeni Hospital, Chancellor College, University of Malawi as well as Malawian and Canadian scientists. Delivery: training, educational activities, campaigns, provision of seeds. Farmers shared knowledge with other farmers. Co‐interventions: none reported. |
Smallholder farm HHs (793/408) | Food security:
|
About 2 years |
| Beegle 2017 (Malawi) | cRCT | High |
Programme name: Malawi Social Action Fund's Public Works Programme (MASAF PWP). Programme description and frequency: the MASAF PWP aims to provide short‐term labour‐intensive activities. The programme was designed to be interlinked with Malawi's large‐scale fertiliser input subsidy programme through the implementation of the PWP in the planting months of the main agricultural season when the fertiliser distribution also occurs. Projects were mostly road rehabilitation or construction, with some afforestation and irrigation projects. The wage rate was USD 0.92/day for a total payment of USD 11.01 for a 12‐day wave, total of 4 waves. Provider: Malawi government Delivery: payments in the study districts were facilitated by the research team for the purposes of the evaluation, with physical delivery of the cash in conjunction with the district officials. Co‐interventions: the national fertiliser subsidy programme provided fertiliser coupons that allow two bags of fertiliser to be purchased for MK 500 each. These coupons are more likely to be available to treated HHs. |
10 poor and able‐bodied HHs per community were offered the programme; communities (144/38) | Food security:
Dietary diversity:
|
3/4 months |
| Porter 2016 (Ethiopia) | Prospective controlled study | High |
Programme name: Productive Safety Net Program (PSNP) Programme description and frequency: 80% public works programme (food/cash‐for‐work; USD 0.56/day in 2008) and 20% unconditional transfers to those unable to work (value NR). Programme operated seasonally but predictably, i.e. not emergency. Provider: Ethiopian government, with donor funding Delivery: centrally co‐ordinated by Government Co‐interventions: none reported |
Poor and food insecure rural HHs (682/924) | Anthropometry (results presented for all programme participants; not disaggregated according to type of intervention received)
|
5 and 7 years |
| Katz 2001 (Nepal) | Prospective controlled study | High |
Programme name: N/A Programme description and frequency: part‐time (5 hours/week) employment for women; distributing weekly supplements to and recording data on married women of child‐bearing age in own or neighbouring communities. Monthly income valued at USD 15 Provider: Joint undertaking by USAID, academic institutions (Johns Hopkins University), NGOs (National Society for the Prevention of Blindness, Kedia Seva Mandir) and the Nepalese government Delivery: NR Co‐interventions: approximately 31% of women employed by the project reported having additional cash employment, but amounts are unknown |
Women living in rural areas (350/520) | Anthropometry:
|
2 years |
aOverall risk of bias based on risk for selection and attrition bias
ADRA: Adventist Development and Relief Agency; BDT: Bangladeshi taka; BMI: body mass index; FFS: Farmer Field School; HAZ: height‐for‐age z‐score; HDDS: Household Dietary Diversity Score; HFIAS: Household Food Insecurity Access Scale; HH: household; LAZ: length‐for‐age z‐score; MUAC: mid‐upper arm circumference; NGO: non‐governmental organisation; NR: not reported; RCT: randomised controlled trial; SD: standard deviation; WLZ: weight‐for‐length z‐score; WAZ: weight‐for‐age z‐score; WEG: Women Empowerment Group.
Eight studies assessed interventions addressing food prices: four RCTs evaluated the effects of food vouchers (Fenn 2015; Hidrobo 2014; Jensen 2011; Ponce 2017); one cRCT (Chen 2019) and three PCS (Sturm 2013; Andaleeb 2016; Chakrabarti 2018) evaluated the effects of food and nutrition subsidies.
Two studies assessed social environment interventions: one cRCT (Kusuma 2017b) and one PCS (Brunie 2014) evaluated an intervention addressing the social environment, namely the effects of village savings and loans (VSL) and community grants.
Some studies assessed more than one type or category of intervention. Hidrobo 2014 and Fenn 2015 included a group for a CCT and another for food vouchers. Baird 2013 included two groups for conditional and unconditional cash transfers. Porter 2016 assessed a public works intervention providing either cash or food for work, or an UCT.
Participants
Twenty‐five studies included children or households in which children lived. Of these, five studies included households with children under 18 months of age (Andersen 2015; Fernald 2011; Marquis 2018; Olney 2016; Tonguet Papucci 2015); 10 studies included households with children under six years of age (Ahmed 2019a; Ahmed 2019b; Alaofe 2019; Daidone 2014; Fenn 2015; Kennedy 1989; Kurdi 2019; Osei 2017; Renzaho 2017; Verbowski 2018), and six with children under 18 years of age (Chen 2019; Kandpal 2016; Kusuma 2017b; Kusuma 2017a; Lopez Arana 2016; Pellerano 2014); three included households with children, without specifying their age (Aguero 2006; Asfaw 2014; Huerta 2006 (PROGRESA)). Baird 2013 included girls 13 to 22 years of age who had never married.
Five studies included adults; in one study, these were members of a healthcare plan (Sturm 2013), one included farmers (Murshed E Jahan 2011), one include men and women (Doocy 2017), and three studies included only women and their respective households (Alaofe 2016; Alaofe 2019; Katz 2001).
Twenty‐nine studies included households without specifying the inclusion of children (Andaleeb 2016; Asadullah 2015; Beegle 2017; Breisinger 2018; Brugh 2018; Brunie 2014; Chakrabarti 2018; Darrouzet Nardi 2016; Evans 2014; Ferre 2014; Gangopadhyay 2015; Gertler 2000 (PROGRESA); Haushofer 2013; Hidrobo 2014; Hjelm 2017; Hoddinott 2013; Jensen 2011; Jodlowski 2016; Kangmennaang 2017; Leroy 2008 (PROGRESA); Macours 2012; Maluccio 2005; Merttens 2013; Miller 2011; Ponce 2017; Porter 2016; Schwab 2013; Skoufias 2013; Weinhardt 2017).
We extracted information from included studies on the following PROGRESS‐Plus characteristics: age, place of residence, sex, ethnicity and language, occupation, education, socioeconomic status and social capital, where this was available. There was considerable variation in the reporting of these characteristics. Most studies (48/59) reported on an aspect of socioeconomic status, with 38 studies on age, 37 on sex, 34 on place of residence, 32 on education, 17 on ethnicity and language, 16 studies on occupation and 13 studies on social capital.
Setting and context
Most included studies were conducted in Africa (27): one each in Egypt (Breisinger 2018), the Democratic Republic of the Congo (Doocy 2017), Ghana (Marquis 2018), Ethiopia (Porter 2016), Lesotho (Pellerano 2014), Mozambique (Brunie 2014), Niger (Hoddinott 2013), and Tanzania (Evans 2014); two each in Benin (Alaofe 2016; Alaofe 2019), Burkina Faso (Olney 2016; Tonguet Papucci 2015), and South Africa (Aguero 2006; Sturm 2013); three in Zambia (Daidone 2014; Jodlowski 2016; Hjelm 2017); four in Kenya (Asfaw 2014; Haushofer 2013; Kennedy 1989; Merttens 2013); six in Malawi (Baird 2013; Beegle 2017; Brugh 2018; Kangmennaang 2017; Miller 2011; Weinhardt 2017).
Nineteen included studies were conducted in Asia: five in Bangladesh (Ahmed 2019a; Ahmed 2019b; Asadullah 2015; Ferre 2014; Murshed E Jahan 2011); four in Nepal (Darrouzet Nardi 2016; Katz 2001; Osei 2017; Renzaho 2017); three in India (Andaleeb 2016; Chakrabarti 2018; Gangopadhyay 2015) and two in China (Jensen 2011; Chen 2019), Indonesia (Kusuma 2017b; Kusuma 2017a); and one each in Cambodia (Verbowski 2018), Pakistan (Fenn 2015), and Philippines (Kandpal 2016).
Five included studies were conducted in South America: one each in Colombia (Lopez Arana 2016) and Peru (Andersen 2015), and three in Ecuador (Fernald 2011; Hidrobo 2014; Ponce 2017).
Two studies were conducted in Nicaragua, Central America (Macours 2012; Maluccio 2005), and four studies took place in Mexico, North America (Gertler 2000 (PROGRESA); Huerta 2006 (PROGRESA); Leroy 2008 (PROGRESA); Skoufias 2013). Two studies were conducted in Yemen, Middle East (Kurdi 2019; Schwab 2013).
All studies specifically targeted poor communities or households except two; one that included data from supermarkets in urban areas in South Africa (Sturm 2013), and one that targeted children enrolled in elementary schools in rural China (Chen 2019). Of those targeting communities, 24 studies did not specify the type of communities, 29 included rural communities, including farming communities, and four included urban communities.
Outcome measures
No included study assessed the primary outcome, namely the prevalence of undernourishment (i.e. people with insufficient food intake to meet their dietary requirements).
Eleven studies reported household expenditure on food (Alaofe 2016; Asfaw 2014; Brugh 2018; Ferre 2014; Hjelm 2017; Kennedy 1989; Macours 2012; Maluccio 2005; Merttens 2013; Miller 2011; Sturm 2013). Household expenditure was reported using different units, for example, household food expenditure per day, week or month; or as a proportion of total weekly or monthly household expenditure. One of these studies reported sales data, including the ratio of expenditure on healthy foods, on fruits and vegetables and on less desirable foods, compared to the total food expenditure (Sturm 2013).
Food security was reported as food security indices and dietary diversity measures. Thirteen studies reported food security outcomes using measures such as the proportion of participants experiencing food security or food deficit always, of households consuming more than one meal per day, Household Food Insecurity Access Scale (HFIAS) and Food Security Index (FSI) (Asadullah 2015; Beegle 2017; Brugh 2018; Brunie 2014; Daidone 2014; Doocy 2017; Haushofer 2013; Hjelm 2017; Kangmennaang 2017; Miller 2011; Osei 2017; Pellerano 2014; Weinhardt 2017). Twenty‐four studies reported on dietary diversity using a variety of measures including individual and Household Dietary Diversity Scores (HDDS), Food Consumption Scores (FCS), minimum dietary diversity (MDD) or minimum acceptable food consumption (Ahmed 2019a; Ahmed 2019b; Alaofe 2019; Asfaw 2014; Beegle 2017; Breisinger 2018; Brugh 2018; Brunie 2014; Chen 2019; Daidone 2014; Darrouzet Nardi 2016; Doocy 2017; Ferre 2014; Hidrobo 2014; Jodlowski 2016; Kurdi 2019; Marquis 2018; Merttens 2013; Miller 2011; Olney 2016; Pellerano 2014; Ponce 2017; Skoufias 2013; Tonguet Papucci 2015). Definitions for the food security and dietary diversity measures reported in included studies are provided in Table 12.
6. Food security and dietary diversity indices reported by included studies.
| Index/scale (study ID of studies reporting this measure) | Definition | Interpretation | Reference cited |
| Household food security indices | |||
|
Household Food Insecurity Access Scale (HFIAS) (Daidone 2014; Hjelm 2017; Kangmennaang 2017) or Household Food Insecurity Access Prevalence (HFIAP) (Doocy 2017; Osei 2017; Weinhardt 2017) |
HFIAS: sum of responses to 9 questions related to 4 domains of food security of a HH during the past 4 weeks. HFIAP: categorises HHs into 4 levels of HH food insecurity, based on the frequency and severity of food insecurity experienced by HHs. |
HFIAS: score ranges from 0 to 27. The higher the score the more food insecure the HH. HFIAP: categorised as: food secure, and mild, moderately and severely food insecure. |
Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. Version 3. Washington, DC: Academy for Educational Development;2006 |
|
Food Security Score (Beegle 2017) |
Scores HHs in terms of 4 levels of HH food insecurity, based on the frequency and severity of food insecurity experienced by HHs. | Ranges from –1 to –4; higher value indicates greater food security | World Food Programme |
|
Resilience index (Beegle 2017) |
Based on the World Food Program Coping Strategy Index. Weighted sum of the number of days in the past 7 days that HHs had to reduce the quantity and quality food consumed. | Higher values indicate food security | Maxwell D, Caldwell R. The Coping Strategies Index: Field methods Manual. Cooperative for Assistance and Relief Everywhere, Inc. (CARE), January 2008. |
|
Food Security Index (FSI) (Pellerano 2014) |
Study authors adapted the food security component of the Bristol Child Deprivation Index. It is a simple mean of 3 questions related to child food security. | Severe food deprivation: FSI > 2. | Gordon D, Nandy S, Pantazis C, Pemberton S, Townsend P. (2003), the Distribution of Child Poverty in the Developing World, Policy Press, Centre for International Poverty Research, University of Bristol, July 2003. |
|
Food Security Index (Haushofer 2013) |
Weighted mean of 17 outcome measures of food security and hunger. | The higher the index, the greater the food security | No reference cited |
| HHdietary diversity indices | |||
|
HDDS (Alaofe 2019; Breisinger 2018; Brunie 2014; Daidone 2014; Hidrobo 2014; Jodlowski 2016a; Kurdi 2019; Merttens 2013; Olney 2016b) |
Sum of the number of food groups consumed by a HH during the past day or week, or longer (e.g. 2 or 4 weeks). Food groups included cereals, roots and tubers, vegetables (included vitamin A‐rich vegetables and tubers, dark leafy vegetables and other), fruits (included vitamin A fruits and other), meat (includes organ meat and flesh meat), eggs, fish, pulses and legumes, fats and oil, sugar and sweets, milk and other milk product, and spices and beverages. | Score ranges from 0 to 12; higher score reflected higher level of dietary diversity. | Kennedy G, Ballard T, Dop M, 2011. Guidelines for Measuring Household and Individual Dietary Diversity. Food and Agriculture Organization, Rome. Swindale A, Bilinsky P. Household dietary diversity score (HDDS) for measurement of household food access: indicator guide (v.2). Washington (DC): FHI 360/FANTA; 2006. |
|
Dietary Diversity Index (DDI) (Hoddinott 2013; Pellerano 2014) or Dietary Diversity Score (DDS) (Asfaw 2014) or Food diversity composite score (Miller 2011) |
Sum of the number of food groups consumed by a HH during the past week. Food groups included main staples, pulses, vegetables, fruit, meat (or fish or egg); dairy products, sugar and oil. | Score ranges from 0 to 8; higher score reflects higher level of dietary diversity. | Ruel M. 2003. Operationalizing dietary diversity: a review of measurement issues and research priorities. Journal of Nutrition 133, 3911S–3926S. |
|
Dietary Diversity Index (DDI) (Hoddinott 2013); or Dietary Diversity Score (DDS) (Hidrobo 2014; Schwab 2013) |
Sum of the number of distinct food items consumed by a HH during the previous week. Depended on the number of food items included in the dietary questionnaire. | Score ranges from 0 to 25 (Hoddinott 2013); 0 to 40 (Hidrobo 2014); 0 to 39 (Schwab 2013); higher score reflects higher level of dietary diversity. | Ruel M. 2003. Operationalizing dietary diversity: a review of measurement issues and research priorities. Journal of Nutrition 133, 3911S–3926S. |
|
Food Consumption Score (FCS) (Ahmed 2019a; Ahmed 2019b; Beegle 2017; Hidrobo 2014; Hoddinott 2013; Pellerano 2014; Ponce 2017) |
Weighted sum of the consumption frequency of the 8 food groups consumed by a HH during the past week. Food groups include main staples, pulses, vegetables, fruit, meat (or fish or egg), dairy products, sugar and oil. | Maximum score is 112 or 126. Acceptable food consumption: FCS ≥ 35; Borderline food consumption: FCS between 21 and 35; Poor food consumption: FCS < 35 |
WFP, 2008. Food consumption analysis: Calculation and use of the food consumption score in food security analysis. World Food Programme, Rome |
| Individual dietary diversity indices | |||
|
Individual Child Dietary Diversity score (IDDS) (Darrouzet Nardi 2016; Hoddinott 2013; Marquis 2018; Pellerano 2014; Skoufias 2013; Tonguet Papucci 2015) |
Sum of number of food groups consumed by a child aged 6–23 months or a child aged < 5 years during the past 24 hours calculated from 17 foods, aggregated into 7 food groups: starchy staples (grains and white potatoes); vitamin A‐rich fruits and vegetables; other fruits and vegetables; offal, meat, and fish; eggs; legumes, nuts, and seeds; milk and dairy products | Score ranges from 0 to 7; higher score reflects higher level of dietary diversity. Minimum dietary diversity: Dietary Diversity Score ≥ 4 |
World Health Organization, 2010. Indicators for Assessing Infant and Young Child Feeding Practices. World Health Organization, Geneva. |
|
Individual Child Dietary Diversity Score (IDDS) (Brunie 2014) |
Sum of the number of different food groups consumed during the past day by a child aged < 5 years (12 food groups). | Score ranges from 0 to 12; higher score reflects higher level of dietary diversity | Guidelines for measuring household and individual dietary diversity. FAO Nutrition – 2007 – FAO, Rome (Italy) |
|
Women's Dietary Diversity Score (WDDS‐10) (Alaofe 2019) |
Sum of the number of food groups consumed during the past 24 hours calculated from the following food groups: starchy staples; beans and peas; nuts and seeds; dairy; flesh foods; eggs; vitamin A‐rich dark green leafy vegetables; other vitamin A‐rich vegetables and fruits; other fruits and other vegetables. | Score ranges from 0 to 10; higher score reflects higher level of dietary diversity | Kennedy G, Ballard T, Dop M, 2011. Guidelines for Measuring Household and Individual Dietary Diversity. Food and Agriculture Organization, Rome. |
aJodlowski 2016: modified HDDS to a total score out of 13. bOlney 2016: the egg food group was not included because of an oversight during survey design.
HH: household.
Six studies reported adequacy of dietary intake (Ahmed 2019a; Ahmed 2019b; Andaleeb 2016; Brugh 2018; Jensen 2011; Kennedy 1989). Measures reported included the proportion of calorie‐deficient households and of preschool children meeting caloric requirements; mineral and vitamin sufficiency indices; calorie‐deficient households; and ratio of caloric, protein and fat intake to the dietary recommendations. Many studies reported intake in terms of calories or nutrients consumed without relating it to a measure of adequacy; these measures were not reported in this review.
A variety of anthropometric measures were reported in included studies. Twenty‐seven studies reported on measures of stunting in children (i.e. chronic undernutrition), such as the proportion stunted (HAZ < –2 standard deviations (SD)), severely stunted (HAZ < –3SD) or mean HAZ (Aguero 2006; Ahmed 2019a; Ahmed 2019b; Andersen 2015; Asfaw 2014; Daidone 2014; Darrouzet Nardi 2016; Doocy 2017; Evans 2014; Fenn 2015; Fernald 2011; Ferre 2014; Kandpal 2016; Kennedy 1989; Kurdi 2019; Kusuma 2017b; Kusuma 2017a; Leroy 2008 (PROGRESA); Lopez Arana 2016; Macours 2012; Maluccio 2005; Marquis 2018; Merttens 2013; Osei 2017; Renzaho 2017; Tonguet Papucci 2015; Verbowski 2018). Twenty studies reported on measures of wasting in children (i.e. acute undernutrition), such the proportion wasted (WHZ < –2SD), severely wasted (WHZ < –3SD) or mean WHZ (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Daidone 2014; Evans 2014; Fenn 2015; Ferre 2014; Kennedy 1989; Kurdi 2019; Kusuma 2017b; Kusuma 2017a; Leroy 2008 (PROGRESA); Lopez Arana 2016; Maluccio 2005; Marquis 2018; Merttens 2013; Osei 2017; Renzaho 2017; Tonguet Papucci 2015; Verbowski 2018). Twenty‐seven studies reported on measures of underweight in women and children, including WAZ or the proportion of underweight based on these (i.e. WAZ < –2SD), BMI for age or mean BMI, or mid‐upper arm circumference (MUAC) (Alaofe 2019; Andersen 2015; Asfaw 2014; Brunie 2014; Chen 2019; Daidone 2014; Darrouzet Nardi 2016; Doocy 2017; Evans 2014; Fenn 2015; Ferre 2014; Kandpal 2016;Katz 2001Kennedy 1989; Kusuma 2017b; Kusuma 2017a; Lopez Arana 2016; Macours 2012; Maluccio 2005; Marquis 2018; Merttens 2013; Olney 2016; Osei 2017; Pellerano 2014; Renzaho 2017; Verbowski 2018; Weinhardt 2017).
Six studies reported biochemical outcomes, including haemoglobin in five studies (Chen 2019; Fenn 2015; Fernald 2011; Osei 2017; Verbowski 2018) and vitamin A and iron deficiency in one study (Alaofe 2019).
Five studies reported cognitive function and development outcomes using a variety of measures including Ravens Colored Matrixes and other cognitive tests, Early Childhood Development Index, individual cognitive function measures such as language and memory, and grade attainment (Andersen 2015; Baird 2013; Daidone 2014; Fernald 2011; Macours 2012). Definitions for cognitive function and development measures reported in included studies are described in Table 13.
7. Summary of cognitive function indices reported by included studies.
| Index or scale | Definition/ measurement | Interpretation | Reference |
|
Early Childhood Development Index (ECD) (Daidone 2014) |
Measures 4 developmental domains of children aged 3–7 years: physical (both gross and fine motor), language and cognition, socioemotional and approaches to learning. | Maximum score of 10; the higher the score the better functioning | — |
|
Raven's Colored Progressive Matrices test score (Baird 2013) |
Non‐verbal test that measures abstract reasoning of children aged ≥ 5 years. | Maximum test score 60; the higher the score the better the abstract reasoning. | — |
|
IDHC‐B test score MacArthur‐Bates Communicative Development Inventory (adapted Spanish version) (Fernald 2011) |
Measures early language skills of children aged 12–35 months using parental report. | Scores range from 0 to 100 with 0 indicating that a child had not said any word on the checklist and 100 indicating that a child had said every word on the list. | Jackson‐Maldonado D, Thal D, Marchman V, Newton T, Fenson L, Conboy B. (2003). MacArthur Inventarios del Desarrollo de Habilidades Comunicativas. User's Guide and Technical Manual. Baltimore: Brookes Publishing. |
|
TVIP test score Peabody Picture Vocabulary Test (PPVT) (adapted Spanish version). (Fernald 2011) |
Measures receptive language/vocabulary of children aged ≥ 36 months. | Age‐adjusted norms: mean score of 100 and standard deviation of 15 at every age. | — |
|
Woodcock‐Johnson‐Munoz battery test scores (Fernald 2011) |
WJ1 test measures long‐term memory in early childhood | Age‐adjusted percentile score | Woodcock, Richard, and Ana Munoz‐Sandoval. 1996. BaterıaWoodcock‐Munoz Pruebas de Aprovechamiento‐Revisada. Chicago: Riverside. |
| WJ2 test measures short‐term memory or immediate recall in early childhood | Age‐adjusted percentile score | ||
| WJ5 test measures visual integration, or visual‐spatial processing in early childhood | Age‐adjusted percentile score |
Four studies reported mental health outcomes including measures such as depression score, stress, psychological distress and psychological well‐being (Baird 2013; Fernald 2011; Haushofer 2013; Hjelm 2017).
Seventeen studies reported morbidity outcomes (Ahmed 2019a; Ahmed 2019b; Alaofe 2019; Asadullah 2015; Chen 2019; Daidone 2014; Evans 2014; Fenn 2015; Gertler 2000 (PROGRESA); Kandpal 2016; Kennedy 1989; Macours 2012; Merttens 2013; Osei 2017; Pellerano 2014; Tonguet Papucci 2015; Verbowski 2018). Various measures of morbidity were reported including incidence of respiratory infections, diarrhoea and anaemia; the proportion of participants who were ill in a specified reference period or the number of days or percent of time ill.
No studies reported specific adverse events. We had specified that overweight and obesity would be considered adverse events in this review, and three studies reported this outcome in young and older children (Andersen 2015; Lopez Arana 2016; Pellerano 2014); however, not as adverse events per se.
Funding and conflicts of Interest
Most included studies were funded either by non‐profit organisations (including research institutes, world bank, non‐government organisations, etc) or governmental/intergovernmental agencies (or both) except for one study that was funded by a for‐profit organisation (Elanco Animal Health; Jodlowski 2016). One study did not disclose their funding (Gangopadhyay 2015).
Of 59 included studies, 39 did not report on potential conflicts of interest (COI) and 27 did. Of those that reported their COI, all declared that none of the authors had any potential COI.
Excluded studies
We excluded 297 studies. Of the excluded studies: 152 had an ineligible study design, seven did not have an eligible population or setting, 89 did not address an eligible intervention, 23 did not report on relevant outcomes and 26 were duplicates. A selection of 85 key excluded studies is reported in the Characteristics of excluded studies table.
Studies awaiting classification
We placed 39 studies awaiting classification because we could not assess their eligibility properly without access to the full text, or they were conference abstracts with insufficient data to include them in the review (see Characteristics of studies awaiting classification table).
Ongoing studies
We identified two studies that could potentially be included in the review once completed. Eleven studies were identified as ongoing. More details on these studies are available in the Characteristics of ongoing studies table.
Risk of bias in included studies
See the Characteristics of included studies table for more details for each domain of bias assessed for each study. Figure 3 presents a summary of the judgements per risk of bias items and Figure 4 presents the summary of the risk of bias judgments for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Risk of selection bias is determined by whether participants were randomly allocated to the intervention groups (random sequence generation) and whether there was no possibility of altering the sequence while allocating participants to the intervention groups (allocation concealment).
Of the 36 included RCTs, 14 studies described adequate methods of random sequence generation and were at low risk of selection bias. Five studies described doing this using computer‐generated random numbers (Baird 2013; Beegle 2017; Fenn 2015; Marquis 2018; Verbowski 2018), one each used STATA software (Gertler 2000 (PROGRESA)) and a randomisation algorithm (Skoufias 2013), while the remaining seven studies randomised communities through public lottery events (Brugh 2018; Daidone 2014; Macours 2012; Maluccio 2005; Merttens 2013; Pellerano 2014; Tonguet Papucci 2015). Twenty‐two studies reported randomising individuals or clusters to intervention groups, but did not report how the random sequence had been generated and thus were at unclear risk of selection bias (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Chen 2019; Darrouzet Nardi 2016; Evans 2014; Fernald 2011; Gangopadhyay 2015; Haushofer 2013; Hidrobo 2014; Hjelm 2017; Hoddinott 2013; Jensen 2011; Kandpal 2016; Kurdi 2019; Kusuma 2017b; Kusuma 2017a; Miller 2011; Olney 2016; Osei 2017; Ponce 2017; Schwab 2013).
Of the 36 included RCTs, 20 reported that allocation was at the cluster level (communities, parishes, electoral divisions, etc.) and carried out at the beginning of the study, and these were classified at low risk of selection bias (Ahmed 2019a; Ahmed 2019b; Baird 2013; Beegle 2017; Brugh 2018; Chen 2019; Daidone 2014; Fenn 2015; Fernald 2011; Gertler 2000 (PROGRESA); Macours 2012; Maluccio 2005; Marquis 2018; Merttens 2013; Olney 2016; Osei 2017; Pellerano 2014; Schwab 2013; Skoufias 2013; Tonguet Papucci 2015). Three studies did not conceal allocation or report this, but household selection was done after villages had been allocated to each intervention group, and knowledge of allocation could have influenced the household selection process (Evans 2014; Hidrobo 2014; Kurdi 2019). In Gangopadhyay 2015, participants self‐selected into the intervention. These four studies were at high risk of selection bias. The remaining 12 studies did not report details on allocation concealment and were at unclear risk of selection bias (Asfaw 2014; Darrouzet Nardi 2016; Haushofer 2013; Hjelm 2017; Hoddinott 2013; Jensen 2011; Kandpal 2016; Kusuma 2017b; Kusuma 2017a; Miller 2011; Ponce 2017; Verbowski 2018).
All 23 PCS were at high risk of selection bias (both for random sequence and allocation concealment), according to EPOC's risk of bias tool guidance (EPOC 2017).
Baseline similarity in participants characteristics and outcome measures (selection bias)
Baseline imbalances in participant characteristics or outcome measures may occur in non‐randomised studies as well as in randomised studies in which the allocation procedure was not performed adequately.
Participants characteristics
In 46 included studies, there were no baseline imbalances reported for participant characteristics or, if there were, these were adjusted for in the analyses, and thus they were at low risk of selection bias (Figure 4). Four studies had significant differences at baseline that were not adjusted for in the analyses; thus they were at high risk of selection bias (Asadullah 2015; Beegle 2017; Kurdi 2019; Merttens 2013). Ten studies were at unclear risk of selection bias: six did not report any or some baseline characteristics (Aguero 2006; Breisinger 2018; Murshed E Jahan 2011; Ponce 2017; Porter 2016; Sturm 2013), one reported baseline characteristics but not whether these were balanced (Gangopadhyay 2015), one reported that characteristics were balanced at household level but not at province level (Jensen 2011), one reported discrepancies and it was unclear whether these were adjusted for in the analysis (Schwab 2013), and one only had baseline data for the group analysed, not for the entire sample (Chen 2019).
Outcome measures
Thirty‐one studies either were balanced at baseline with regards to outcome measures, or adjusted for any imbalance in the analyses, and were at low risk of selection bias (Figure 4). In seven studies there were significant baseline imbalances in relevant outcomes which were not controlled for in the analyses, and these were at high risk of selection bias (Andersen 2015; Asadullah 2015; Beegle 2017; Breisinger 2018; Merttens 2013; Renzaho 2017; Sturm 2013). The remaining 21 studies were classified at unclear risk of selection bias: 15 did not report any or relevant outcomes at baseline (Aguero 2006; Baird 2013; Chen 2019; Darrouzet Nardi 2016; Evans 2014; Gertler 2000 (PROGRESA); Hjelm 2017; Huerta 2006 (PROGRESA); Kandpal 2016; Kurdi 2019; Kusuma 2017b; Kusuma 2017a; Murshed E Jahan 2011; Porter 2016; Verbowski 2018); in three, the baseline data collection occurred after the intervention started, so true baseline data were not available (Hoddinott 2013; Lopez Arana 2016; Schwab 2013), in two studies it was unclear if reported imbalances were adjusted for (Doocy 2017; Osei 2017), and in one, although the outcomes were balanced at household level, there were imbalances at province level (Jensen 2011).
Blinding
Blinding participants and personnel to intervention allocation during the study helps prevent systematic differences in how participants are treated or behave during the trial due to knowledge of treatment allocation (performance bias). In the types of studies included in this review, blinding of participants and personnel was often not feasible; however, it is also unlikely that it would have influenced the behaviour of participants or personnel beyond that expected as part of the intervention, and thus less likely to be susceptible to performance bias. Thus, in all but one study included in this review, the risk of performance bias was low. One study was at high risk of performance bias as blinding was not possible and the delivery of the intervention, a nutrition subsidy to schools, was dependent on the school principal (Chen 2019).
Blinding of outcome assessors helps prevent systematic differences in how outcomes are assessed in either intervention groups due to knowledge of treatment allocation (detection bias). Fifteen studies were at low risk of detection bias; in 14 of these studies, blinding was not done; however, the outcomes measured and reported were objective and thus unlikely to have been influenced by knowledge of treatment allocation (Aguero 2006; Ahmed 2019a; Ahmed 2019b; Andersen 2015; Fernald 2011; Kusuma 2017b; Kusuma 2017a; Leroy 2008 (PROGRESA); Lopez Arana 2016; Marquis 2018; Osei 2017; Porter 2016; Renzaho 2017; Skoufias 2013). The other study was based on scanner sales data from supermarkets, which is not susceptible to detection bias due to lack of blinding (Sturm 2013). The remaining 44 studies were at high risk of detection bias either because there was no blinding or they included self‐reported or subjective outcomes that were susceptible to be influenced by knowledge of treatment allocation.
Protection against contamination (performance bias)
If the control group is exposed to the intervention intended for the intervention group, contamination occurs, introducing performance bias.
Thirty‐seven studies were at low risk of bias in this domain either because they reported evidence of no contamination, or because the intervention and control groups were allocated at the community/village/district level (i.e. in distinct geographical areas), which precludes contamination. Eight studies were at high risk of bias as they reported evidence of control group exposure to the intervention (Asfaw 2014; Doocy 2017; Ferre 2014; Huerta 2006 (PROGRESA); Jodlowski 2016; Kandpal 2016; Katz 2001; Kurdi 2019). The remaining 14 studies were at unclear risk (Aguero 2006; Andersen 2015; Asadullah 2015; Brunie 2014; Daidone 2014; Gertler 2000 (PROGRESA); Kangmennaang 2017; Lopez Arana 2016; Maluccio 2005; Murshed E Jahan 2011;Osei 2017; Ponce 2017; Porter 2016; Skoufias 2013). In these studies, the location or the distance between intervention and control communities was unclear, or the control and intervention households were in same community and there was potential for control households to have benefited from the intervention through interaction with intervention households (e.g. sharing), or communities were geographically near/adjacent.
Incomplete outcome data
Twenty‐five studies were at low risk of bias because they had low attrition (i.e. 10% or less) or because attrition between the groups was non‐differential or unrelated to the outcome. Seventeen studies were at high risk of attrition bias, because of high levels of attrition or they reported differential attrition between intervention groups or characteristics of those lost to follow‐up were different from those remaining in the study, or a combination of these (Andaleeb 2016; Asadullah 2015; Asfaw 2014; Chen 2019; Doocy 2017; Huerta 2006 (PROGRESA); Kandpal 2016; Kangmennaang 2017; Katz 2001; Kurdi Leroy 2008 (PROGRESA); Lopez Arana 2016; Merttens 2013; Ponce 2017; Schwab 2013; Skoufias 2013; Weinhardt 2017). Skoufias 2013 reported only a 5% difference in attrition between groups but lost one entire cluster and participants were excluded from the analysis were different than those included in the analysis, thus was classified at high risk. Seventeen studies were classified at unclear risk of attrition bias, as they either did not report attrition at all or did not report enough information to make this judgement (Aguero 2006; Alaofe 2016; Alaofe 2019; Beegle 2017; Brunie 2014; Chakrabarti 2018; Darrouzet Nardi 2016; Fernald 2011; Ferre 2014; Gertler 2000 (PROGRESA); Hjelm 2017; Kennedy 1989; Olney 2016; Osei 2017; Porter 2016; Sturm 2013; Verbowski 2018). Sturm 2013 analysed supermarket sales scanner data and did not report if any of these data were excluded or missing.
Selective reporting
Selective outcome reporting occurs when authors do not report on all outcomes prespecified and assessed in the study. Six studies were at low risk of bias, as they reported the same outcomes that were prespecified in the trial registry (Baird 2013; Fenn 2015; Haushofer 2013; Olney 2016; Verbowski 2018; Weinhardt 2017).
One study was at high risk of bias because some of the morbidity outcomes (oedema and measles) reported in protocol were not reported in the published paper (Tonguet Papucci 2015).
The remaining 52 studies were at unclear risk of bias as there were no protocols available.
Other potential sources of bias
Under other potential sources of bias we considered whether the study could have been influenced by 1. misclassification bias of the exposure (i.e. when exposure to the intervention was self‐reported); 2. measurement bias (i.e. whether outcomes were measured appropriately; 3. incorrect analysis, in the case of cRCTs (i.e. whether study data were adjusted for clustering. Such analyses do not lead to biased estimates of effect but in the meta‐analysis such studies receive undue weight leading to overprecision of the effect estimate); and 4. recruitment bias, in the case of cRCTs (i.e. whether recruitment of participants was done before allocation of clusters to intervention groups).
Twenty‐two studies were at low risk as no other potential sources of bias were identified. Six studies were at high risk of bias as at least one other potential source of bias was identified (Alaofe 2019; Asfaw 2014; Gertler 2000 (PROGRESA); Huerta 2006 (PROGRESA); Osei 2017; Schwab 2013). Asfaw 2014 was at high risk for misclassification bias as receipt of the intervention was based on self‐report. Three were at high risk of recruitment bias as clusters were assigned before households were recruited (Asfaw 2014; Gertler 2000 (PROGRESA); Osei 2017). Two studies were at high risk of measurement bias: in Huerta 2006 (PROGRESA) preliminary analyses showed evidence of reporting error regarding health outcomes, and in Alaofe 2019 dietary data were collected with only one 24‐hour recall. Schwab 2013 was at high risk of other bias due to the different timing of implementation of interventions in each group. The remaining 31 studies were at unclear risk of other bias; in these studies there was at least one of the other potential sources of bias for which there was insufficient information to make a judgement.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6
We present the effects of interventions on primary and secondary outcomes separately for each category of intervention as outlined below (see Table 8 for definitions of intervention categories and types).
-
Interventions that improved buying power:
Unconditional cash transfers
Conditional cash transfers
Income generation interventions
-
Interventions that addressed food prices:
Food prices – food vouchers
Food prices – food and nutrition subsidies
-
Interventions that addressed the social environment
Social support interventions (community grants/savings schemes)
We found no studies addressing the intervention category of infrastructure changes, which we had intended to include in the review.
The 'Summary of findings' tables provide an overview of effects on all primary outcomes and key secondary outcomes, for each comparison.
Comparison 1: unconditional cash transfers
Twenty‐one included studies assessed UCTs, where a specific amount of money was transferred to poor families monthly or once every two months, with no conditions regarding behaviours expected from the families. Fourteen cRCTs (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Baird 2013; Brugh 2018; Daidone 2014; Fenn 2015; Fernald 2011; Hjelm 2017; Merttens 2013; Miller 2011; Pellerano 2014; Skoufias 2013; Tonguet Papucci 2015), two RCTs (Gangopadhyay 2015; Haushofer 2013), and three PCS (Aguero 2006; Breisinger 2018; Renzaho 2017) assessed the effects of UCTs versus no intervention. Two cRCTs assessed UCTs versus food transfers (Hoddinott 2013; Schwab 2013).
Five cRCTs reported on the proportion of household expenditure on food (Asfaw 2014; Brugh 2018; Hjelm 2017; Merttens 2013; Miller 2011). Five cRCTs (Brugh 2018; Daidone 2014; Hjelm 2017; Miller 2011; Pellerano 2014) and one RCT (Haushofer 2013) reported on various food security measures, and 10 cRCTs reported on various dietary diversity measures (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Brugh 2018; Daidone 2014; Merttens 2013; Miller 2011; Pellerano 2014; Skoufias 2013; Tonguet Papucci 2015). Eight cRCTs (Asfaw 2014; Daidone 2014; Fernald 2011; Merttens 2013; Pellerano 2014; Tonguet Papucci 2015; Fenn 2015; Ahmed 2019a; Ahmed 2019b), and one PCS (Aguero 2006) reported various anthropometric measures. Two clusters RCT reported and biochemical indicators (Fernald 2011; Fenn 2015), and three cRCTs reported on cognitive function and development outcomes (Baird 2013; Daidone 2014; Fernald 2011). Three cRCTs (Baird 2013; Fernald 2011; Hjelm 2017) and one RCT (Haushofer 2013) reported on measures of mental well‐being. Seven cRCTs reported measures of morbidity (Ahmed 2019a; Ahmed 2019b; Daidone 2014; Fenn 2015; Merttens 2013; Pellerano 2014; Tonguet Papucci 2015), and one cRCT reported adverse effects (Pellerano 2014). Hoddinott 2013 and Schwab 2013, the cRCTs where the comparison group was food transfers, reported on measures of dietary diversity, and Schwab 2013 also reported measures of food security.
Further details about the studies in this comparison are presented in Table 14. Table 15 presents results of individual trials included and Table 16 presents results of individual PCS included, on all reported outcomes. The Table 1 and the harvest plot in Figure 5 summarise the effects of UCTs on key outcomes.
8. Unconditional cash transfers – overview of included studies.
| Study ID (country) | Study design | Overall risk of biasa | Other key details of intervention | Population (sample size at baseline: intervention/control) | Outcome domains and measures with available data | Timepoint of measurement |
| UCTs vs no intervention | ||||||
|
Baird 2013 (Malawi) |
cRCT | Low |
Programme name: Schooling, Income, and Health Risks study (SIHR). Includes unconditional and conditional groups. Amount and frequency of payments: payments split between guardian and girl in each HH. HH amount varied randomly (USD 4, USD 6, USD 8, USD 10 per month). Amount paid to girl beneficiaries varied randomly (USD 1, USD 2, USD 3, USD 4, USD 5 per month). Provider: NGOs Delivery: payments to girl beneficiaries at local distribution points Co‐interventions: none reported |
Adolescent girls who were never married, aged 13–22 years, in urban and rural HHs (526/1495) | Cognitive function and development:
Anxiety and depression:
|
1 and 2 years |
|
Brugh 2018 (Malawi) |
cRCT | Low |
Programme name: Malawi Social Cash Transfer Scheme (SCTS) Amount and frequency of payments: about USD 40 (depending on HH size and number of school‐aged children); monthly transfers. Top‐up payments made for children at primary and secondary school. At follow‐up, intervention HHs had received 5 or 6 bi‐monthly cash transfer payments, due to an administrative delay. Provider: Government Delivery: NR Co‐interventions: None reported |
Ultra‐poor and labour constrained HHs (1561/1729 HHs; Mangochi and Salima districts | HH expenditure on food:
Food security:
Dietary diversity:
Adequacy of dietary intake:
|
1 year |
|
Daidone 2014 (Zambia) |
cRCT | Low |
Programme name: Child Grant Programme (CGP) Amount and frequency of payments: about USD 12 per month, regardless of HH size; payments made every other month Provider: government Delivery: payments through local pay point manager Co‐interventions: none reported |
1260 HHs (7254 individuals)/1259 HHs (7091 individuals) | Food security:
Dietary diversity:
Anthropometry:
Cognitive function and development:
Morbidity: children aged 0–60 months
|
2 years |
|
Fenn 2015 (Pakistan) |
cRCT | Low |
Programme name: REFANI Pakistan standard cash transfer Amount and frequency of payments: PKR 1500 (about USD 14) disbursed monthly for 6 consecutive months. Provider: EU; DG ECHO; Action Against Hunger field staff. Delivery: mobile banks in a central location or central banks serving a number of villages. Verbal messaging from Action Against Hunger field staff at distribution that children should benefit from the transfers. Co‐interventions: WINS programme in all villages – provided outpatient treatment for children aged 6 (SD 59) months with SAM, micronutrient supplementation (children, pregnant and lactating women), and behaviour change communication. |
Poor and very poor agrarian HHs (standard cash group: 31 villages/632 HHs; Double cash group: 24 villages/600 HHs; fresh food voucher group: 31 villages/632 HHs; control group: 28 villages/632 HHs | Anthropometric indicators:
Biochemical indicators:
Morbidity: child:
|
6 and 12 months |
|
Pellerano 2014 (Lesotho) |
cRCT | Low |
Programme name: Lesotho Child Grants Programme (CGP) Amount and frequency of payments: about USD 12 per month every 3 months. From 2013 (after 2 years) transfer indexed to number of children in the HH. Payments not made as predicted; smaller number of payments made involving larger amounts. Provider: government; UNICEF‐Lesotho Delivery: cash‐in‐transit firm provided payments at community pay points. Co‐interventions: all CGP HHs received bi‐monthly top‐up for a specific period for a Food Emergency Grant. |
Ultra‐poor rural HHs with children 0–17 years (706/647 HHs) | Food security:
Dietary diversity:
Anthropometry:
Morbidity: children aged 0–5 years:
Adverse events:
|
2 years |
|
Tonguet Papucci 2015 (Burkina Faso) |
cRCT | Low |
Programme name: Moderate Acute Malnutrition Out (MAM'Out) project. Amount and frequency of payments: seasonal payments – about USD 17 from July to November. Provider: European Commission Humanitarian Aid (ECHO) trained project staff Delivery: mothers received card linked to electronic account and mobile phone. Payments provided via phones and cash withdrawal points. Co‐interventions: ongoing national social protection policy that promoted social transfer mechanisms to the poorest and most vulnerable. |
Poor rural HHs with ≥ 1 child aged < 1 year (644/634 children; 602/583 HHs) | Dietary diversity:
Anthropometric indicators:
Morbidity: child:
|
2.4 years |
|
Ahmed 2019a; Ahmed 2019b (Bangladesh) |
cRCT | Unclear |
Programme name: Transfer Modality Research Initiative (TMRI) (2 trials implemented in the North and South of Bangladesh reported in the same paper). Amount and frequency of payments: Monthly payment of BDT 1500 (about USD 19) per HH. Provider: United Nations' World Food Program (WFP); NGO (Eco‐Social Development Organization or ESDO) Delivery: a mobile phone was provided to the mother who collected payments from distribution sites using mobile verification of identity. Co‐interventions: none reported |
Rural HHs in the northwest and southern regions (North: 458/450; South: 454/464 HHs) | Dietary diversity:
Adequacy of dietary intake:
Anthropometric indicators:
Morbidity: children:
|
2 years |
|
Fernald 2011 (Ecuador) |
cRCT | Unclear |
Programme name: Bono de Desarrollo Humano (BDH) programme Amount and frequency of payments: USD 15 per month; could accumulate payments for up to 4 months. Provider: government Delivery: payments to mothers via the banking system. Co‐interventions: none reported |
Rural and urban parishes; poor families who had children aged 0–6 years at baseline (1388/681 children) | Anthropometry:
Biochemical:
Cognitive function and development:
Anxiety and Depression:
|
17 months |
|
Haushofer 2013 (Kenya) |
RCT | Unclear |
Programme name: N/A Amount and frequency of payments: total amount of KES 25,200 (USD 404). Either monthly (for 9 months) or a lump‐sum payment. A subgroup of intervention HHs received an additional KES 10,000 per month for 7 months (total KES 95,200 (USD 1525). Provider: NGO (GiveDirectly) Delivery: payments via mobile money service to recipients (women or men). Co‐interventions: none reported |
Poor villages and HHs (503/505 HHs) | Food security:
Anthropometry:
Anxiety and depression:
|
2 and 3 years |
|
Hjelm 2017 (Zambia) |
cRCT | Unclear |
Programme name: Zambia Multiple Category Cash Transfer Program (MCP) Amount and frequency of payments: transfers made every second month. Monthly amount of transfer of ZMW 55,000 (USD 11), irrespective of HH size. Provider: government Delivery: payments made through a local paypoint manager. Co‐interventions: none reported |
Socially vulnerable HHs in 2 rural districts with extreme poverty (1571/1515 HHs) | HH expenditure on food:
Food security:
Anxiety/depression:
|
2 and 3 years |
|
Miller 2011 (Malawi) |
cRCT | Unclear |
Programme name: Malawi Social Cash Transfer Scheme (SCTS) Amount and frequency of payments: about USD 40 (depending on HH size and number of school aged children); monthly transfers. Top‐up payments made for children at primary and secondary school. Provider: government Delivery: NR Co‐interventions: none reported |
Ultra‐poor and labour constrained HHs (366/386 HHs), Mchinji district | HH expenditure on food:
Food security:
Dietary diversity:
|
6 months, 1 year |
|
Asfaw 2014 (Kenya) |
cRCT | High |
Programme name: Kenya Cash Transfer Programme for Orphans and Vulnerable Children (CT‐OVC) Amount and frequency of payments: every 2 months (about USD 21) irrespective of HH size. Conditionalities: although the programme was unconditional, some districts imposed conditions (e.g. school attendance) and penalties Provider: Kenya government Delivery: payments made through local post offices. Co‐interventions: none reported. |
Ultra‐poor HHs with orphans and vulnerable children (CT‐OVC) (1542 HHs/755 HHs) | HH expenditure on food:
Dietary diversity:
Anthropometric indicators:
|
2 and 4 years |
|
Gangopadhyay 2015 (India) |
RCT | High |
Programme name: N/A Amount and frequency of payments: monthly cash transfer of INR 1000 (about USD 18). Provider: researchers Delivery: transfers were made through bank accounts opened for women beneficiaries Co‐interventions: none reported Note: comparison included control group with no bank account and not receiving transfer |
100 HHs/100 HHs | NR | — |
| Merttens 2013 (Kenya) | cRCT | High |
Programme name: Hunger Safety Net Programme (HSNP) pilot programme Amount and frequency of payments: transfer every 2 months of KES 2150 (at commencement) which increased to KES 3500 by the end of the intervention period. Some HHs had multiple nominated beneficiaries; the effective value of the transfer per HH member was smaller for larger HHs Provider: Ministry of State for the Development of Northern Kenya and Other Arid Lands Delivery: cash was loaded onto a biometric smartcard which could be used to collect the cash transfer from a range of paypoints (usually small shops). Several services providers contracted. Co‐interventions: none reported |
Impoverished rural HHs (1224/1212 HHs) | HH expenditure on food:
Dietary diversity:
Anthropometric indicators:
Morbidity: HHs
|
2 years |
|
Skoufias 2013 (Mexico) Other papers: Ramirez‐Luzuriaga 2016 Leroy 2010 |
cRCT | High |
Programme name: food support programme (PAL, Programa de Apoyo Alimentario). Included in‐kind and cash transfer groups. Health and nutrition education session offered but not compulsory. This review included cash + education group vs control group only. Amount and frequency of payments: about USD 14/month; disbursed every 2 months. Same amount for all HHs. Provider: Mexican Government's agency Delivery: distribution through stored of the government's agency DICONSA. Co‐interventions: none reported |
Poor rural HHs (1687/1663 HHs; 279/289 children) | Dietary diversity:
Anthropometric indicators:
|
1 and 2 years |
|
Aguero 2006 (South Africa) |
Prospective cohort study | High |
Programme name: Child Support Grant (CSG) Amount and frequency of payments: monthly payments made to the primary carer of the child, with no recording of what the carer used the money for. The initial monthly benefit was SAR 100 in 1998 and during the time of the 2004 survey it was SAR 170 (about USD 25). Provider: government Delivery: NR Co‐interventions: none reported |
30% of poorest children. subsample of African and Indian HHs with ≥ 1 child. 245/154 children |
Anthropometric indicators:
|
6 years |
|
Breisinger 2018 (Egypt) |
Prospective controlled study | High |
Programme name: Takaful cash transfer programme Amount and frequency of payments: Payments changed from quarterly to monthly, originally starting from a basic amount of EGP 325 per HH, which increased depending on the number of children in the HHs and their educational level. Conditionalities: programme had been designed to be conditional but not enforced yet at the time of the evaluation Provider: government; World Bank Delivery: some beneficiaries had to travel to collect the money Co‐interventions: none reported |
Poor HHs in districts where poverty rate was ≥ 50% (2190 beneficiaries/3813 non‐beneficiaries) | Diet diversity:
Anthropometric indicators:
Morbidity in children aged 0–5 years
|
11 months |
|
Renzaho 2017 (Nepal) |
Prospective controlled study | High |
Programme name: Child Cash Grant (CCG) Amount and frequency of payments: NPR 200 per month for up to 2 children for poor families with children aged < 5 years, as a complement to other government grants. Provider: government; Asia Development Bank, UNICEF‐Nepal Delivery: embedded within existing universal social transfer programmes Co‐interventions: both intervention and control groups received targeted resources transfers from the government for senior citizens, single women, endangered communities and people with disabilities. |
Poor communities and HHs with ≥ 1 child aged < 60 months (1500 HHs/1500 HHs) | Anthropometric indicators:
|
5 years |
| UCTs vs food transfers | ||||||
|
Hoddinott 2013 (Niger) |
cRCT | Unclear |
Programme name: N/A Amount and frequency of payments: cash received for time worked for 3 months, followed by another 3 months where cash was received unconditionally. USD 2/day worked to maximum of USD 50/month. Transfers made twice monthly. Provider: Nigerian NGOs contracted out to handle food transport, storage, distribution and cash payments Delivery: public works committee set up in each village to liaise with NGOs. NGOs charged a fixed percentage of total cash amount distributed. Co‐interventions: none reported but all receiving cash for work in previous 3 months |
Poor rural HHs (total 2187) | Dietary diversity:
|
3 months |
|
Schwab 2013 (Yemen) |
cRCT | High |
Programme name: N/A Amount and frequency of payments: HHs in cash group received 3 cash transfers of an amount equivalent to the local value of the food basket (about USD 50). Provider: transfers distributed in co‐ordination with local partners: the Yemen Post and Postal Savings Corporation (PPSC) in the case of cash transfers and Ministry of Education in the case of food transfers. Delivery: collection of cash at any time up to 25 days after disbursement. Initial meetings with beneficiaries to sensitise beneficiaries to the programme objectives and logistics. For cash transfer group, a second resensitisation campaign held after funds were transferred to reinforce messages. Transfers given out at district branches of the PPSC. Co‐interventions: none reported |
Poor HHs in rural communities (982/1001 HHs). | Food security:
Dietary diversity:
|
7 months |
aOverall Risk of Bias based on risk of selection and attrition bias.
ARI: acute respiratory infection; BDT: Bangladeshi taka; BMI: body mass index; CDS: Child Diet Score; CES‐D: Center for Epidemiologic Studies Depression Scale; cRCT: cluster randomised controlled trial; DDI: Dietary Diversity Index; DDS: Dietary Diversity Score; ECD: Early Childhood Development; EGP: Egyptian pound; FCS: Food Consumption Score; FSI: Food Security Index; GHQ‐12: 12‐item General Health Questionnaire; HAZ: height‐for‐age z‐score; Hb: haemoglobin; HDDS: Household Dietary Diversity Score; HFIAS: Household Food Insecurity Access Scale; HH: household; IDHC‐B: Inventario do Desenvolvemento de Habilidades Comunicativas – B; KES: Kenyan shilling; LAZ: length‐for‐age z‐score; MDD: minimum dietary diversity; MUAC: mid‐upper arm circumference; N/A: not applicable/available; NGO: non‐governmental organisation; NPR: Nepalese rupee; PKR: Pakistani rupee; SAM: severe acute malnutrition; SAR: South African rand; SD: standard deviation; UCT: unconditional cash transfer; WAZ: weight‐for‐age z‐score; WHZ; weight‐for‐height z‐score; ZMW: Zambian kwacha.
9. Unconditional cash transfers – results of included trials.
|
Study ID (risk of bias) |
Study design (n) | Unconditional cash transfers | No intervention | Effect measure (time point) | Effect directiona | Meta‐analysis (yes/no) | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | |||||
| Outcome 1.2: proportion of HH expenditure on food | ||||||||||
| 1.2.1 Outcome measure: proportion of total HH expenditure on food (weekly/monthly) | ||||||||||
| Brugh 2018 (+) | cRCT (3290 HHs) | 0.77 (0.11) | 0.70 (0.11) | 1561 | 0.77 (0.11) | 0.72 (0.11) | 1729 | pp –2 (SE 1) 95% CI –3.96 to –0.4; P < 0.1 (1 year) | ▲ | Yes (excluding Merttens, Asfaw which are missing variance estimate) |
| Miller 2011 (?) | cRCT (HHs) | 56% | 68% | 366 HHs | 52% | 48% | 386 HHs | pp 12, P < 0.0001 (1 year), 95% CI 5.924 to 18.076, SE 3.1 | ▼ | |
| Hjelm 2017 (?) | cRCT (3010 HHs) | 74 (16) | — | — | 77 (15) | — | — | pp 3.2, robust t‐statistic 1.815, 95% CI –0.328 to 6.728, SE 1.8 (2 years) | ▽ | |
| cRCT (2969 HHs) | 74 (16) | 74.5 | 1490 HHs | 77 (15) | 72.7 | 1479 HHs | pp 4.2 robust, SE 1.8, 95% CI 0.672 to 7.728, P < 0.05 (3 years) | ▼ | ||
| Merttens 2013 (‐) | cRCT (2436 HHs) | 76.5% | 77.3% | 1224 HHs | 79.8% | 81% | 1212 HHs | pp –0.4, P > 0.1 (1 year) | △ | |
| Asfaw 2014 (‐) | cRCT (1824 HHs) | 63% | 69.6% | 1286 HHs | 61% | 68.6% | 538 HHs | pp –0.95, P > 0.1 (2 years) | △ | |
| Outcome 1.3: proportion of HHs who were food secure | ||||||||||
| 1.3.1 Food security | ||||||||||
| 1.3.1.1 Outcome measure: proportion consuming > 1 meal/day | ||||||||||
| Brugh 2018 (+) | cRCT (3290 HHs) | 0.79 (0.40) | 0.94 (0.24) | 1561 | 0.82 (0.39) | 0.88 (0.34) | 1729 | DD 0.11, SE 0.03, pp 11, 95% CI 0.0512 to 0.1688, P < 0.001 (1 year) | ▲ | Yes |
| Miller 2011b (?) | cRCT (752 HHs) | About 45% | About 85% | 366 HHs | About 45% | About 45% | 386 HHs | pp 42, P < 0.0001 (1 year), SE 10.7 95% CI 21.028 to 62.972 |
▲ | |
| 1.3.1.2 Outcome measure: mean food security scores (HFIASc/FSId) (mean, SD) | ||||||||||
|
Daidone 2014 (+) HFIAS/Food Security Scale |
cRCT (2299 HHs) | — | 9.63 | 1158 HHs | — | 12.36 | 1141 HHs | MD 2.498, SE 0.59, 95% CI 1.3416 to 3.6544, P < 0.05, SE 1.3 (2 years) | ▲ | Yes |
|
Haushofer 2013 (?) (FSI) |
RCT (940 HHs) | — | — | 471 HHs | — | Mean –0.00 (SE 1.00) | 469 HHs | MD 0.25, 95% CI 0.13 to 0.37, P < 0.01 (2 years), SE 0.1 | ▲ | |
|
Hjelm 2017 (?) (HFIAS/food security scale) |
cRCT (3010 HHs) | 14.78 (5.49) | — | — | 14.68 (5.71) | — | — | MD 1.78, robust t‐statistic 3.76, 95% CI 0.8 to 2.76 P < 0.05 (2 years), SE 0.5 | ▲ | |
| cRCT (2970 HHs) | 14.78 (5.49) | 9.83 | 1490 HHs | 14.68 (5.71) | 12.47 | 1480 HHs | MD 2.69, robust t‐statistic 4.94, 95% CI 1.71 to 3.67, P < 0.05 (3 years), SE 0.5 | ▲ | ||
| 1.3.1.3 Outcome measure: severe food deprivation (FSI > 2) | ||||||||||
| Pellerano 2014 (+) | cRCT (2220 children aged 0–5 years) | 67.1% | 53.4% | 747 HHs | 69.3% | 72.2% | 739 HHs | pp –16.63, P < 0.05 (2 years), SE 8.5 | ▲ | N/A. Outcomes from same study. |
| Pellerano 2014 (+) | cRCT (5384 children aged 6–17 years) | 67.8% | 58.6% | 747 HHs | 73.9% | 70.7% | 739 HHs | pp –6.103, P < 0.1 (2 years), SE 3.7 | ▲ | |
| 1.3.2 Dietary diversity | ||||||||||
| 1.3.2.1 Outcome measure: dietary diversity scores, including composite FCS (weighted) (mean, SD) (scores refer to number food groups consumed; reference periods and scales vary) | ||||||||||
|
Daidone 2014 (+) HDDS 0–12 |
cRCT (2298 HHs) | — | 6.73 | 1158 | — | 5.30 | 1141 | MD 1.43 (2 years) | △ | Yes (except for Daidone, Merttens, pellerano – missing variance estimate) |
|
Pellerano 2014 (+) FCS 0–112 |
cRCT (1486 HHs) | 28.7 | 31.2 | 747 HHs | 28.9 | 30.4 | 739 HHs | MD 0.946, P > 0.1 (2 years) | △ | |
|
Brugh 2018 (+) HDDS 0–12 |
cRCT (3290 HHs) | 5.63 (1.78) | 5.85 (1.54) | 1561 | 5.64 (1.87) | 5.34 (1.44) | 1729 | MD 0.23 (SE 0.32), 95% CI –0.3972 to 0.8572, P > 0.05 (1 year) | △ | |
|
Miller 2011 (?) FDCS 1–8 |
cRCT (752 HHs) | 5 | 7 | 366 HHs | 5 | 4 | 386 HHs | MD 2.4, P < 0.0001 (1 year), SE 0.6. 95% CI 1.224 to 3.576 | ▲ | |
|
Ahmed 2019a (?) FCS 0–112 |
cRCT (HHs NR) | — | — | — | — | — | — | MD 6.84 points, SE 1.12, P < 0.01, 95% CI 4.6448 to 9.0352 (2 years) | ▲ | |
|
Ahmed 2019b (?) FCS 0–112 |
cRCT (HHs NR) | — | — | — | — | — | — | MD 2.62 points, SE 1.04, P < 0.05, 95% CI 0.5816 to 4.6584 (2 years) | ▲ | |
|
Merttens 2013 (‐) DDS 0–12 |
cRCT (2436 HHs) | 6.7 | 7.2 | 1224 HHs | 6.1 | 6.2 | 1212 HHs | MD 0.3, P > 0.1 (1 year) | △ | |
|
Asfaw 2014 (‐) DDS (0–8) |
cRCT (2369 HHs) | 5.225 | 6.177 | 1289 HHs | 5.697 | 5.843 | 540 HHs | MD 0.821, SE 0.3, P < 0.01 (2 years) | ▲ | |
| 1.3.2.2. Outcome measure: proportion with MDD (≥ 3–4 food groups)/acceptable food consumption (FCS > 35) | ||||||||||
| Tonguet Papucci 2015 (+) | cRCT (322 children aged 14–27 months) | — | 65.6% | 160 | — | 39.5% | 162 | OR 2.95, 95% CI 1.86 to 4.68, P < 0.001 (2 years) SMD 0.6, SE 0.1 |
▲ | Yes |
| Skoufias 2013 (‐) | cRCT (568 children) | 69.6% | 66. 7% | 279 | 72.7% | 59.9% | 289 | pp 10.6, 95% CI –6.65 to 27.85, P > 0.05 (2 years), SE 8.8 SMD 0.1, SE 0.1 |
△ | |
| 1.4 Change in adequacy of dietary intake | ||||||||||
| 1.4.1 Food poverty (per capita daily caloric intake < 2122 calories; proportion) | ||||||||||
| Ahmed 2019a (?) | cRCT (n NR) | — | — | — | — | — | — | MD –0.05, SE 0.03, 95% CI –0.1088 to 0.0088, P > 0.05 (2 years) | — | Yes |
| Ahmed 2019b (?) | cRCT (n NR) | — | — | — | — | — | — | MD –0.04, SE 0.04, P > 0.05, 95% CI –0.1184 to 0.0384 (2 years) | — | |
| 1.4.2 Proportion food energy deficient (total HH caloric availability < total HH caloric requirements) | ||||||||||
| Brugh 2018 (+) | cRCT (3290 HHs) | — | — | 1561 | — | — | 1729 | DD –0.1, SE 0.04, 95% CI –0.1784 to –0.0216; P < 0.05 (1 year) | ▲ | |
| 1.5Change in anthropometric indicators | ||||||||||
| 1.5.1Stunting(chronic undernutrition) | ||||||||||
| 1.5.1.1 Outcome measure: proportion stunted (HAZ < –2SD) | ||||||||||
| Tonguet Papucci 2015 (+) | cRCT | 27.7% | — | 630 children aged 0–15 months | 27.2% | — | 620 children aged 0–15 months | OR 0.73, 95% CI 0.47 to 1.14, P 0.17 (2 years) | △ | Yes (except Asfaw, Merttens – no measure of variance) |
| Fenn 2015 (+) | cRCT (1683 children) | n (%): 457 (50.9) | NR | 874 children | n (%): 437 (51.7) | NR | 809 children | OR 0.36, 95% CI 0.22 to 0.59, P < 0.001 (6 months) | ▲ | |
| cRCT (1664 children) | n (%): 457 (50.9) | NR | 849 children | n (%): 437 (51.7) | NR | 815 children | OR 0.54, 95% CI 0.36 to 0.81, P = 0.003 (12 months) | ▲ | ||
| Merttens 2013 (‐) | cRCT (1062 HHs) | 26.7% | 29.6% | — | 35.6% | 31.5% | — | pp 7.0, P > 0.1 (2 years) | ▽ | |
| Asfaw 2014 (‐) | cRCT | 41.5% | 35.7% | 442 children aged 0–59 months | 44% | 37% | 295 children aged 0–59 months | pp –4.63, P > 0.1 (2 years) | △ | |
| 1.5.1.2 Outcome measure: proportion with severe stunting (HAZ < –3SD) | ||||||||||
| Fenn 2015 (+) | cRCT (1683 children) | NR | NR | 874 children | NR | NR | 809 children | OR 0.47, 95% CI 0.28 to 0.77, P = 0.003 (6 months) | ▲ | No. SE not available for all studies. |
| cRCT (1664 children) | NR | NR | 849 children | NR | NR | 815 children | OR 0.59, 95% CI 0.38 to 0.92, P = 0.02 (12 months) | ▲ | ||
| Merttens 2013 (‐) | cRCT (n = 1062) | 11.6% | 13.4% | — | 15.2% | 15.1% | — | pp 1.9, P > 0.1 (2 years) | ▽ | |
| 1.5.1.3 Outcome measure: HAZ (mean, SD) | ||||||||||
| Daidone 2014 (+) | cRCT (2299 children aged 0–60 months) | — | –1.445 | 1158 | — | –1.491 | 1141 | MD 0.066, 95% CI –0.116 to 0.248, P > 0.05 (2 years) | △ | Yes |
| Tonguet Papucci 2015 (+) | cRCT (1250 children aged 0–15 months | –1.18 (1.44) | –1.96 (1.03) | 630 | –1.33 (1.24) | –1.99, SD 1.04) |
620 | MD –0.0005, 95% CI –0.004 to 0.003 z‐score/month, P = 0.78 | ▽ | |
| Fenn 2015 (+) | cRCT (1683 children) | –1.98 (1.65) | NR | 874 children | –1.97 (1.75) | NR | 809 children | MD 0.24, 95% CI 0.17 to 0.32, P < 0.001 (6 months) | ▲ | |
| cRCT (1664 children) | –1.98 (1.65) | NR | 849 children | –1.97 (1.75) | NR | 815 children | MD 0.21, 95% CI 0.10 to 0.31, P < 0.001 (12 months) | ▲ | ||
| Fernald 2011 (?) | cRCT (1196 children) | –0.5 (2.1) | –1.7 (1.2) | 797 | –0.7 (2.0) | –1.7 (1.2) | 399 | MD 0.01, 95% CI –0.18 to 0.19 (2 years) | △ | |
| Ahmed 2019a (?) | cRCT (n NR) | — | — | — | — | — | — | MD 0.132, SE 0.08, 95% CI –0.0248 to 0.2888, P > 0.05 (2 years) | △ | |
| Ahmed 2019b (?) | cRCT (n NR) | — | — | — | — | — | — | MD –0.097, SE 0.08, 95% CI –0.0598 to 0.2538, P > 0.05 (2 years) | △ | |
| Asfaw 2014 (‐) | cRCT (737 children aged 0–59 months) | –1.466 | –1.279 | 442 | –1.462 | –1.248 | 295 | MD –0.0272, 95% CI –0.503 to 0.449, P > 0.1 (2 years) | ▽ | |
| 1.5.2Wasting (acute undernutrition) | ||||||||||
| 1.5.2.1 Outcome measure: proportion wasted (WHZ < –2SD) (proportion) | ||||||||||
| Tonguet Papucci 2015 (+) | cRCT (1250 children aged 0–15 months | 26% | — | 630 | 192% | — | 620 | IRR 0.92, 95% CI 0,64 to 1.32; P = 0.66 (2 years) | △ | No. SE not available for all studies and different effect size for 1 study. |
| Fenn 2015 (+) | cRCT (1683 children) | n (%): 196 (22.0) | NR | 874 children | n (%): 184 (21.9) | NR | 874 children | OR 1.09, 95% CI 0.64 to 1.87, P = 0.75 (6 months) | ▽ | |
| cRCT (1664 children) | n (%): 196 (22.0) | NR | 849 children | n (%): 184 (21.9) | NR | 849 children | OR 1.10, 95% CI 0.71 to 1.71, P = 0.66 (12 months) | ▽ | ||
| Merttens 2013 (‐) | cRCT (1062 children) | 25.3% | 23.1% | — | 24.2% | 17.3% | — | pp 4.7, P > 0.1 | ▽ | |
| Asfaw 2014 (‐) | cRCT (737 children aged 0–59 months) | 6% | 9% | 648 | 9.4% | 6.9% | 341 | pp 5.95, P > 0.1 (2 years) | ▽ | |
| 1.5.2.2 Outcome measure: severe wasting (WHZ < –3SD) (proportion) | ||||||||||
| Fenn 2015 (+) | cRCT (1683 children) | 69 (7.7) | — | 874 children | 62 (7.4) | — | 874 children | OR 0.98, 95% CI 0.38 to 2.54, P = 0.97 (6 months) | △ | No. Variance only available for 1 of the 2 studies. |
| Merttens 2013 (‐) | cRCT (1062 children) | 6.8 | 6.2 | — | 8.0 | 3.5 | — | pp 3.9, P > 0.1 | ▽ | |
| 1.5.2.3 Outcome measure: WHZ (mean, SD) | ||||||||||
| Daidone 2014 (+) | cRCT (2299 children aged 0–69 months) | — | –0.0961 | 1158 | — | –0.154 | 1141 | MD 0.118, 95% CI –0.015 to 0.251 (2 years) | △ | Yes |
| Tonguet Papucci 2015 (+) | cRCT (1250 children aged 0–15 months) | –1.24 (1.23) |
–0.56 (0.95) | 630 | –1.07 (1.12) | –0.61 (0.93) | 620 | MD –0.003 z‐score/month, 95% CI –0.008 to 0.0003, P = 0.07 (2 years) | ▽ | |
| Fenn 2015 (+) | cRCT (1683 children) | –1.11 (1.34) | NR | 874 children | –1.15 (1.30) | NR | 874 children | MD 0.04, 95% CI –0.07 to 0.14, P = 0.5 (6 months) | △ | |
| cRCT (1664 children) | –1.11 (1.34) | NR | 849 children | –1.15 (1.30) | NR | 849 children | MD –0.08, 95% CI –0.19 to 0.04, P = 0.21 (12 months) | ▽ | ||
| Ahmed 2019a (?) | cRCT (n NR) | — | — | — | — | — | — | Coefficient –0.013, SE 0.07, 95% CI –0.1502 to 0.1242, P > 0.05 (2 years) | ▽ | |
| Ahmed 2019b (?) | cRCT (n NR) | — | — | — | — | — | — | Coefficient –0.088, SE 0.08, P > 0.05, 95% CI –0.2448 to 0.0688 (2 years) | ▽ | |
| Asfaw 2014 (‐) | cRCT (737 children aged 0–59 months) | –0.017 | –0.332 | 442 | 0.065 | –0.166 | 295 | MD –0.0838, 95% CI –0.339 to 0.171, P > 0.1 (2 years) | ▽ | |
| 1.5.3 Underweight | ||||||||||
| 1.5.3.1 Weight for age z‐score | ||||||||||
| 1.5.3.1.1 Outcome measure: proportion underweight (WAZ < –2SD) | ||||||||||
| Pellerano 2014 (+) | cRCT (total n: 6 month old 474; 12 month old 293) | 6 month old: 29.2; 12 month old: 36.6 | 6 month old: 10.6; 12 month old: 16.4 |
— | 6 month old: 11.0; 12 month old: 39.7 | 6 month old: 8.4 12 month old: 23.3 |
— | 6 month old: pp –15.60, P < 0.05 12 month old: pp –3.637, P > 0.05 (2 years) |
6 month old: ▲ 12 month old: △ |
No. Variance not available for all studies. |
| Merttens 2013 (‐) | cRCT (1062) | 30.7 | 24.9 | — | 33.7 | 24 | — | pp 3.9, P > 0.1 | ▽ | |
| Asfaw 2014 (‐) | cRCT (1435) | 20.6 | 21 | — | 19.6 | 19.1 | — | pp –0.62, P = 0.901 (2 years) | △ | |
| 1.5.3.1.2 Outcome measure: proportion severely underweight (WAZ < –3SD) | ||||||||||
| Merttens 2013 (‐) | cRCT (1062) | 9.8 | 8.9 | — | 10.9 | 6.9 | — | pp 3.2, P > 0.1 | ▽ | N/A |
| 1.5.3.1.3 Outcome measure: mean WAZ | ||||||||||
| Daidone 2014 (+) | cRCT (6825 children) | — | –0.900 | — | — | –0.963 | — | MD 0.128, 95% CI –0.05 to 0.261, P > 0.05 (2 years) | △ | Yes |
| Asfaw 2014 (‐) | cRCT 752 children aged 0–59 months) | –0.879 | –1.034 | 456 | –0.923 | –0.804 | 296 | MD –0.274, 95% CI –0.633 to 0.085, P > 0.1 (2 years) | ▽ | |
| 1.5.3.2 BMI (mean, SD) | ||||||||||
| Fenn 2015 (+) | cRCT 1208 HHs/mothers (flow diagram) | Median (IQR) 20.4 (18.3 to 23.5) | NR | 607 | median (IQR) 20.0 (18.1 to 22.7) | NR | 601 | Beta‐coefficient –0.10, 95% CI –0.36 to 0.16, P = 0.45 (6 months) | ▽ | |
| 1.5.5 Mid‐upper arm circumference (MUAC) (mean, SD) | ||||||||||
| Fenn 2015 (+) | cRCT (1208 HHs/mothers) | 24.4 (3.4) | NR | 607 | 24.3 (3.2) | NR | 601 | Beta‐coefficient 0.09, 95% CI –0.13 to 0.30, P = 0.41 (6 months) | △ | |
| cRCT (1683 children) | 13.5 (1.3) | NR | 874 | 13.5 (1.2) | NR | 809 | beta‐coefficient 0.06, 95% CI –0.02 to 0.15, P = 0.15 (6 months) | △ | ||
| 1.6Change in biochemical indicators | ||||||||||
| 1.6.1 Outcome measure: haemoglobin concentration (g/dL) (mean, SD) | ||||||||||
| Fenn 2015 (+) | cRCT (1208 HHs/mothers) | mean 103 (SD 18) | NR | 607 mothers | mean 100 (SD 19) | NR | 601 mothers | MD –0.42, 95% CI –0.63 to –0.20, P < 0.001 (6 months) | ▼ | |
| cRCT (1683 children) | mean 89 (17) | NR | 874 children | mean 88 (16) | NR | 809 children | MD –0.12, 95% CI –0.31 to 0.08, P = 0.24 (6 months) | ▽ | Yes | |
| Fernald 2011 (?) | cRCT (922 children) | 9.7 (1.3) | 10.4 (1.5) | — | 9.5 (1.3) | 10.3 (1.3) | — | MD 0.04, 95% CI –0.21 to 0.29, P > 0.1 | △ | |
| 1.7 Cognitive function and development | ||||||||||
| 1.7.1 Outcome measure: cognitive and development scales/indices (mean, SD) | ||||||||||
| Baird 2013 (+) | cRCT (RCPM; 2057 adolescents) | — | — | — | — | — | — | MD 0.136, SE 0.119, 95% CI –0.097 to 0.369, P > 0.1 (2 years) | △ | No (no n to calculate SMD) |
| Daidone 2014 (+) | cRCT (ECD Index; 5670 children) | — | 5.174 | — | — | 4.926 | — | MD 0.311, 95% CI –0.065 to 0.687, P > 0.1 (2 years) | △ | |
| 1.7.2 Outcome measure: Individual cognitive function measures scores (mean, SD) | ||||||||||
| Fernald 2011 (?) | cRCT (Language: TVIP; 1894 children 36 months and older) | — | — | — | — | — | — | MD 0.013, 95% CI –0.076 to 0.102, P > 0.1 (2 years) | △ | N/A |
| Language: IDHC‐B 1192 children aged 12–35 months) | — | 45.0 (35.1) | — | — | 42.3 (32.2) | — | MD 2.43, 95% CI –1.01 to 5.86, P > 0.1 (2 years) | △ | ||
| 1.8 Change in proportion of anxiety and depression | ||||||||||
| 1.8.1 Outcome measure: depression score (CES‐D scale) (mean change in score, SD) | ||||||||||
| Fernald 2011 (?) | cRCT (1430 mothers) | — | 19.6 (11.1) | — | — | 18.9 (10.6) | — | MD 0.71, 95% CI –0.84 to 2.25, P > 0.1 (2 years) | ▽ | Yes |
| Haushofer 2013 (?) | RCT (2140 adults) | — | — | 471 HHs | — | 26.48 (9.31) | 469 HHs | MD –0.99, 95% CI –1.54 to –0.44, P < 0.1 (3 years) | ▲ | |
| Hjelm 2017 (?) | cRCT (1765 HHs with adolescents) | — | — | — | — | — | — | Effect estimate 0.00, robust t‐statistic 0.00, P not significant (2 years) | — | |
| cRCT (2217 HHs with adolescents) | — | — | — | — | 19.24 | — | Effect estimate –0.54, 95% CI –1.80028 to 0.72028 (3 years) | △ | ||
| 1.8.2 Outcome measure: Perceived Stress Scale (mean, SD) | ||||||||||
| Fernald 2011 (?) | cRCT (n = 1430) | — | — | — | — | — | — | Top 3 income quartiles: MD 0.045, 95% CI –0.112 to 0.202, P > 0.1. Bottom income quartile: MD 0.177, 95% CI –0.017 to 0.371, P < 0.1 (2 years) |
▽ | Yes |
| Haushofer 2013 (?) | RCT (2140 adults) | — | — | — | — | 0.00 (1.00) | — | MD –0.14, 95% CI –0.258 to –0.022, P < 0.05 (3 years) | ▲ | |
| Hjelm 2017 (?) | cRCT (2490 HHs) | — | 9.58 (4.64) | — | — | 9.92 (4.73) | — | Effect estimate –0.42, 95% CI –1.12364 to 0.28364 (3 years) | △ | |
| 1.8.3 Outcome measure: proportion with psychological distress (psychological distress, anxiety and depression, social dysfunction, loss of confidence) | ||||||||||
| Baird 2013 (+) | cRCT (2089 adults) | — | — | — | — | 0.374 | — | pp –14.3, 95% CI –21.0 to –7.6, P < 0.001 (1 year) | ▲ | N/A |
| — | — | — | — | 0.308 | — | pp –3.8, 95% CI –13.14 to 5.8 P > 0.1 (2 years) | △ | |||
| 1.8.4 Outcome measure: Psychological Well‐being Score (mean, SD) | ||||||||||
| Haushofer 2013 (?) | RCT (2140 adults) | — | — | — | — | –0.00 (1.00) | — | Coefficient 0.20 SD, 95% CI 0.082 to 0.318, P < 0.1 (2 years) | ▲ | N/A |
| 1.9 Morbidity | ||||||||||
| 1.9.1 Outcome measure: incidence of respiratory infections (reference period: 1 and 2 weeks) | ||||||||||
| Daidone 2014 (+) | cRCT Proportion children aged 0–60 months with ARI in previous 2 weeks (n = 7232) |
— | 0.0511 | — | — | 0.0832 | — | pp –3.6, 95% CI –8.6 to 14.0, P > 0.05 (2 years) | △ | No. 2 different measures of effect that could not be compared (IRR vs OR/pp). |
| Fenn 2015 (+) | cRCT (1683 children) | n (%): 310 (34.3) | NR | 874 children | n (%): 273 (32.2) | NR | 809 children | OR, 0.73, 95% CI 0.51 to 1.03, P = 0.07 (6 months) | △ | |
| Tonguet Papucci 2015 (+) | cRCT Episodes/child‐month (1250 children aged 0–15 months) |
— | N 0.87, 95% CI 0.84 to 0.89 | — | — | N 0.95, 95% CI 0.92 to 0.97 | — | IRR 0.79, 95% CI 0.78 to 0.81, P < 0.001 (2 years) | ▲ | |
| Asfaw 2014 (‐) | cRCT 957 children aged 0–7 years) | — | — | 613 children | — | — | 344 children | IRR 0.556, t‐statistics –2.40, P < 0.05 (2 years) | — | |
| 1.9.2 Outcome measure: incidence diarrhoeal disease | ||||||||||
| Fenn 2015 (+) | cRCT (1683 children) | n (%): 228 (25.2) | NR | 874 children | n (%): 298 (35.0) | NR | 809 children | OR 1.05, 95% CI 0.67 to 1.63, P = 0.84 (6 months) | ▽ | No. Different measure of effect for one study (IRR vs OR/pp) |
| Daidone 2014 (+) | cRCT Proportion children aged 0–60 months with diarrhoea in previous 2 weeks (n = 7232) |
— | 0.0684 | — | — | 0.0925 | — | pp –4.9, 95% CI –8.9 to –0.9, P < 0.05 (2 years) | ▲ | |
| Tonguet Papucci 2015 (+) | cRCT Episodes/child/month (1250 children aged 0–15 months) |
— | n 0.85, 95% CI 0.82 to 0.88 | — | — | n 0.83, 95% CI 0.80 to 0.85 | — | IRR 1.00, 95% CI 0.97 to 1.03, P = 0.89 (2 years) | □ | |
| Ahmed 2019a (?) | cRCT (n NR) | — | — | — | — | — | — | Coefficient –0.003, pp –0.3, SE 0.02, 95% CI –0.0422 to 0.0362, P > 0.05 (2 years) | △ | |
| Ahmed 2019b (?) | cRCT (n NR) | — | — | — | — | — | — | Coefficient –0.009, pp –0.9, SE 0.02, 95% CI –0.0482 to 0.0302, P > 0.05 | △ | |
| 1.9.3 Outcome measure: proportion with any illness in previous reference period (1 month/3 months) | ||||||||||
| Pellerano 2014 (+) | cRCT (1996 children aged 0–5 years) | 38.9 | 31.4 | — | 36.7 | 45.3 | — | pp –15.38, P < 0.1 (2 years) | ▲ | No. Variance estimates not available for all studies. |
| Merttens 2013 (‐) | cRCT (n = 14,342) (includes injury) | 22.5 | 12.1 | — | 23.1 | 11.7 | — | pp 1.0, P > 0.05 (2 years) | ▽ | |
| 1.9.4 Proportion with anaemia (any) | ||||||||||
| Fenn 2015 (+) | cRCT (1683 children) | — | — | 874 children | — | — | 809 children | OR 1.13, 95% CI 0.68 to 1.86, P = 0.64 (6 months) | — | N/A |
| cRCT (1208 mothers) | — | — | 607 mothers | — | — | 601 mothers | OR 1.34, 95% CI 0.82 to 2.18, P = 0.24 (6 months) | — | ||
| 1.10 Adverse events: proportion who were overweight (according to International standards and Bukana Health Card) | ||||||||||
| Pellerano 2014 (+) | cRCT (total n: 6 months old: 474; 12 months old: 293) | 6 months old: 4.5; 12 months old: 6.0 | 6 months old: 2.2; 12 months old: 0.0 | — | 6 months old: 0.8; 12 months old: 0.0 | 6 months old: 2.0; 12 months old: 0.0 | — | 6 months old: pp –5.082, P > 0.05; 12 months old: pp –6.461, P > 0.05 (2 years) | △ | N/A |
aEach triangle represents one study; bValues are derived from graphs
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0; □: Effect measure is the null; (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias. FDCS: Food diversity consumption score; FCS: Food consumption score.
ARI: acute respiratory infection; CES‐D: Center for Epidemiologic Studies Depression Scale; CI: confidence interval; cRCT: cluster randomised controlled trial; DD: Diet diversity; DDS: Dietary Diversity Score; ECD: Early Childhood Development; FCS: Food Consumption Score; FDCS: Food Diversity Composite Score; FSI: Food Security Index; HAZ: height‐for‐age z‐score; HDDS: Household Dietary Diversity Score; HFIAS: Household Food Insecurity Access Scale; HH: household; IDHC‐B: Inventario do Desenvolvemento de Habilidades Comunicativas‐B; IQR: interquartile range; IRR: incidence rate ratio; MD: mean difference; MDD: minimum dietary diversity; n: number; NR: not reported; OR: odds ratio; pp: percentage point; RCPM: Ravens Coloured Progressive Matrices ; RCT: randomised controlled trial; SD: standard deviation; SE: standard error; SMD: standardised mean difference; TVIP: Test de Vocabulario en Imagenes Peabody; WHZ: weight‐for‐height z‐score.
10. Unconditional cash transfers – results of included prospective controlled studies.
|
Study ID (risk of bias) |
Study design (n) | Unconditional cash transfers | No intervention | Effect measure (time point) | Effect directiona | Meta‐analysis (yes/no) | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | |||||
| 1.3.2 Dietary diversity | ||||||||||
| 1.3.2.1 Outcome measure: Dietary diversity scores, including composite Food Consumption Score (FCS) (weighted) (mean, SD) (scores refer to number food groups consumed; reference periods and scales vary) | ||||||||||
| Breisinger 2018 (‐) | PCS (6003 HHs) – HDDS | NR | 9.58 (1.38) | 2190? | NR | 9.48 (1.55) | 3813? | MD (SE) 0.16 (0.117), 95% CI –0.06932 to 0.38932, P > 0.1 (1 year??) | △ | N/A |
| Breisinger 2018 (‐) | PCS (5799 HHs) – mother DDS) | NR | 4.21 (1.28) | 2190? | NR | 4.04 (1.26) | 3813? | MD 0.011 (SE 0.100), 95% CI –0.185 to 0.207, P > 0.1 (1 year?), | △ | |
| Breisinger 2018 (‐) | PCS (1684 HHs) DDS children aged 6–23 months | NR | 3.35 (1.73) | 2190? | NR | 3.39 (1.61) | 3813? | MD –0.342 (SE 0.209) 95% CI –0.752 to 0.068, P > 0.1 (1 year) | ▽ | |
| Breisinger 2018 (‐) | PCS (3202 HHs) DDS children aged 24–59 months | NR | 5.09 (1.37) | 2190? | NR | 4.89 (1.40) | 3813? | MD –0.057 (SE 0.144) 95% CI –0.33924 to 0.22524, P > 0.1 (1 year) | ▽ | |
| 1.5Change in anthropometric indicators | ||||||||||
| 1.5.1Height‐for‐age z‐scores; chronic undernutrition) | ||||||||||
| 1.5.1.1 Outcome measure: proportion stunted (HAZ < –2SD) | ||||||||||
| Renzaho 2017 (‐) | Prospective controlled study (n = 1491) | 66.7 | 59.8 | 748 | 63 | 52.9 | 743 | Adjusted DID (pp): –5.16, 95% CI –9.55 to –0.77 (5 years), SE 2.2 | ▲ | — |
| 1.5.1.3 Outcome measure: HAZ (mean, SD) | ||||||||||
| Aguero 2006 (‐) | PCS | — | –0.84 | — | –1.08 | — | NR (MD 0.15 at 45%, and 0.25 at 80% of nutritional window; data derived from graph (6 years)) | △ | No. SE not available for all studies. | |
| Renzaho 2017 (‐) | PCS (1491 children) | –2.6 (1.4) | –2.2 (1.4) | 748 | –2.3 (1.3) | –2.1 (1.3) | 743 | Adjusted DID: 0.18, 95% CI 0.09 to 0.27 (5 years) | ▲ | |
| 1.5.2WHZ; acute undernutrition/wasting | ||||||||||
| 1.5.2.1 Outcome measure: proportion wasted (WHZ < –2SD) (proportion) | ||||||||||
| Renzaho 2017 (‐) | PCS (1491 children) | 12.7 | 5.7 | 748 | 5.8 | 6.4 | 743 | Adjusted DID: pp –2.84, 95% CI –5.58 to –0.1 (5 years) | ▲ | |
| 1.5.2.3 Outcome measure: WHZ (mean, SD) | ||||||||||
| Renzaho 2017 (‐) | PCS (1491 children) | –0.8 (1.1) | –0.4 (1.0) | 748 | –0.5 (0.9) | –0.4 (1.1) | 743 | Adjusted DID: MD 0.19, 95% CI 0.09 to 0.3 (5 years) | ▲ | |
| 1.5.3 Weight‐for‐age z‐score (WAZ; underweight) | ||||||||||
| 1.5.3.1 Outcome measure: proportion underweight (WAZ < –2SD) | ||||||||||
| Renzaho 2017 (‐) | PCS (1491 children) | 50.7 | 34.8 | 748 | 37.3 | 28.9 | 743 | Adjusted DID: pp –7.35, 95% CI –11.62 to –3.08 (5 years) | ▲ | N/A |
| 1.5.3.3 Outcome measure: mean WAZ | ||||||||||
| Renzaho 2017 (‐) | PCS (1491 children) | –2.1 (1.1) | –1.6 (1.1) | 748 | –1.7 (1.0) | –1.4 (1.1) | 743 | Adjusted DID: 0.22, 95% CI 0.15 to 0.29 (5 years) |
▲ | N/A |
aEach triangle represents one study.
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
DDS: Dietary Diversity Score; DID: difference in differences; HAZ: height‐for‐age z‐score; HH: household; MD: mean difference; n: number; N/A: not applicable/available; NR: not reported; PCS: prospective controlled study; SD: standard deviation; SE: standard error; WAZ: weight‐for‐age z‐score; WHZ: weight‐for‐height z‐score.
5.
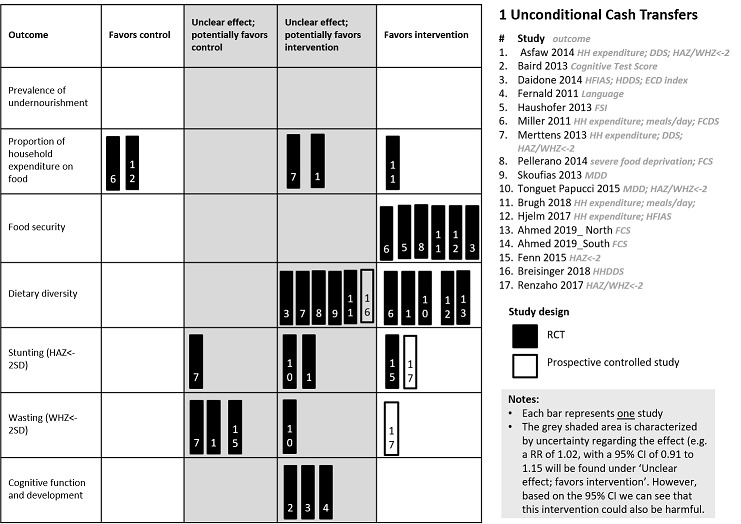
Harvest plot: unconditional cash transfers.
Primary outcomes
1.1 Change in prevalence of undernourishment
None of the included studies measured prevalence of undernourishment.
1.2 Proportion of household expenditure on food
As household income increases, the share of household expenditure on food should decrease relative to other household expenditure (INDDEX Project 2018). Five cRCTs reported this outcome (Asfaw 2014; Brugh 2018; Hjelm 2017; Merttens 2013; Miller 2011), with evidence being very uncertain about the effects of UCTs on the proportion of household expenditure on food (5 trials, 11,271 households; very low certainty evidence; Table 1). Effects varied across the five studies, with one study showing a clear effect favouring UCTs, two studies showing an unclear effect potentially favouring UCTs, and two studies show a clear effect favouring the control (P = 0.003; Figure 5). Three of these studies could be included in a forest plot but data could not be pooled due to high heterogeneity (I2 = 92%; Analysis 1.1). Miller 2011 and Brugh 2018 were two different studies assessing the Malawi cash transfer scheme and thus are the same in terms of the characteristics of participants and interventions although Miller 2011 was a pilot study. Hjelm 2017 assessed the Zambia cash transfer programme. These programmes differed in the amount provided by the cash transfer (USD 11 every second month which was fixed versus USD 40 monthly which varied depending on household size and the number of school‐aged children). As expected, the effect in Miller was worse than in the other studies.
1.1. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 1: Proportion of household expenditure on food
Brugh 2018 reported a clear effect favouring UCTs, with a decrease in the proportion of household expenditure on food by 2 percentage points at 1 year (pp –2, 95% CI –3.96 to –0.4; 3290 households). This study was at low overall risk of bias.
Asfaw 2014 and Merttens 2013 reported an unclear effect potentially favouring UCTs, showing a decrease in the proportion of monthly amount spent on food: Merttens 2013 by –0.4 pp at one year (2435 participants; P > 0.1) and Asfaw 2014 by –0.95 pp at two years (1824 participants; P > 0.1). These studies were both at high overall risk of bias.
Miller 2011 and Hjelm 2017 reported a clear effect favouring the control. Miller 2011 reported an increase in the proportion of total weekly expenditures on food by 12 pp in the intervention group compared to the control at one year (P < 0.0001, 752 participants); Hjelm 2017 reported an increase in per capita share of food expenditure of 4.2 pp (95% CI 0.67 to 7.72). Miller 2011 is at low overall risk of bias and Hjelm 2017 at unclear overall risk of bias.
1.3 Proportion of households who were food secure
Twelve trials reported on different food security and dietary diversity measures. Food security measures reflect the frequency and severity of food insecurity experienced by households within a specific reference period (e.g. past month), with a higher number usually indicating more food insecurity. Dietary diversity refers to the number of food groups or food items consumed, by households or individuals within a specific reference period (e.g. past 24 hours), with a higher number indicating better dietary diversity. In our analysis, we included composite measures for food security and dietary diversity (e.g. reported scores or indices), in preference to single outcome measures; details of their definitions and interpretations are presented in Table 12.
1.3.1 Food security
Five cRCTs and one RCT reported this outcome, with evidence showing that UCTs improve food security (6 trials, 10,251 households and 7604 children; high‐certainty evidence; Table 1). All six studies showed a clear effect favouring UCTs (P < 0.001; Figure 5). Miller 2011 and Brugh 2018 reported an increase in the proportion of people eating more than one meal per day with the UCTs: Miller 2011 reported an increase of 42 pp at one year follow‐up (P < 0.0001; 752 participants); Brugh 2018 reported an increase of 11 pp at one year (95% CI 5.12 to 16.9; 3290 households). Data from these studies could not be pooled due to high heterogeneity (I2 = 87%; Analysis 1.2). These two studies assessed cash transfers in Malawi and the characteristics of participants and interventions were the same, but Miller 2011 was a smaller pilot study and was at unclear overall risk of bias whereas Brugh 2018 was at low overall risk of bias. Daidone 2014, Haushofer 2013, and Hjelm 2017 reported food security scores; Hjelm 2017 using the FSI and Daidone 2014 and Haushofer 2013 using a food security scale based on the HFIAS, and for both of these the higher the value the more beneficial. A meta‐analysis of these three studies showed a slight improvement in scores (SMD 0.18, 95% CI 0.13 to 0.23; 6209 households; I2 = 0%; Analysis 1.3). Pellerano 2014 reported a decrease in severe food deprivation (FSI > 2) at two years in children aged from birth to five years (–16.63 pp; P < 0.05; 2220 children) and in children aged six to 17 years (82116.10 pp; P > 0.1; 5384 children) receiving the UCT compared to children in the control group. Brugh 2018, Daidone 2014, and Pellerano 2014 were at low overall risk of bias, whereas Haushofer 2013, Hjelm 2017, and Miller 2011 were at unclear overall risk of bias.
1.2. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 2: Proportion consuming > 1 meal/day
1.3. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 3: Food security scores
One cRCT at higher overall risk of bias compared food transfers with UCTs (Schwab 2013). They reported on the number of months of the previous six months that households had difficulty satisfying their food needs, with an unclear effect potentially favouring UCTs (MD –1.06; P > 0.05; 1983 households).
1.3.2 Dietary diversity
Ten cRCTs and one PCS reported dietary diversity measures.
Randomised controlled trials
Evidence showed that UCTs may increase dietary diversity (10 RCTs; 11,145 households and 3578 children; low‐certainty evidence; Table 1). Five cRCTs reported a clear effect favouring UCTs and five cRCTs reported an unclear effect potentially favouring UCTs (P < 0.001; Figure 5).
Ahmed 2019a, Ahmed 2019b, Asfaw 2014, Miller 2011, and Tonguet Papucci 2015 reported clear effects favouring UCTs. Miller reported an increase in the food diversity composite score (scale: 1 to 8) of 2.4 points more with UCTs compared to the control group (95% CI 1.22 to 3.58; 752 households). Ahmed 2019a reported an increase in FCS (scale: 0 to 112) with UCTs at two years of 6.84 points (95% CI 4.64 to 9.03; n NR) and Ahmed 2019b of 2.62 points (95% CI 0.58 to 4.66; n NR). Asfaw 2014 reported a mean dietary diversity score (scale 0 to 8) higher by 0.82 at two years (1824 households; P < 0.01). Tonguet Papucci 2015 reported the odds of achieving MDD, which were approximately three‐fold higher in the children from the UCT group (OR 2.95, 95% CI 1.86 to 4.68; n = 322; P < 0.001). Of these studies, Ahmed 2019a, Ahmed 2019b, and Miller 2011 were at unclear overall risk of bias; Asfaw 2014 was at high overall risk of bias and Tonguet Papucci 2015 was at low overall risk of bias.
Brugh 2018, Daidone 2014, Merttens 2013, Pellerano 2014, and Skoufias 2013 reported unclear effects potentially favouring UCTs. Four of these cRCTs reported an increase in the mean dietary diversity score at household level (scale: 0 to 12) (Brugh 2018: 0.23 points, 95% CI –0.39 to 0.86; 3290 households; Daidone 2014: 1.43 points; 2298 households; P = NR; Merttens 2013: 0.3 points; 2436 households; P = NR; Pellerano 2014: 0.16; 1486 households; P > 0.1). Skoufias 2013 reported an increase of 10.6 percentage points in the proportion of children in the intervention group achieving MDD, which referred to consuming at least three to six food groups, compared to the control group at two years (pp 10.6, 95% CI –6.65 to 27.85; 568 children; P > 0.05).
Three studies reporting diet diversity scores had sufficient data for a meta‐analysis, but results were not pooled due to high heterogeneity (I2 = 83%; Analysis 1.4) (Asfaw 2014; Brugh 2018; Miller 2011). These studies reported slightly different measures of dietary diversity but, in all cases, a higher value indicated higher dietary diversity. Two studies assessed a cash transfer programme in Malawi and Asfaw 2014 assessed the Kenya cash transfer programme. Both studies in Malawi included ultra‐poor households, the one in Kenya included households with orphans and vulnerable children, which may be more vulnerable. Asfaw 2014 was also at high overall risk of bias whereas the others were at unclear and low overall risk of bias. Two studies reporting the proportion of children with MDD could not be pooled due to high heterogeneity (I2 = 94%, Analysis 1.5) (Skoufias 2013; Tonguet Papucci 2015). The interventions in these two studies differed somewhat; Skoufias 2013, which was at high overall risk of bias, made a payment of approximately USD 14 every two months and accompanied by health education sessions that were not compulsory. Tonguet Papucci 2015 assessed seasonal cash payments of USD 17 (from July to November only), with no educational sessions, and payments were made to mothers. The effect was larger for Tonguet Papucci 2015, which was at low overall risk of bias.
1.4. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 4: Dietary Diversity Score including composite food consumption score (FCS) (weighted)
1.5. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 5: Proportion with minimum dietary diversity
Two cRCTs compared UCTs with food transfers (Hoddinott 2013; Schwab 2013). Both reported a clear effect on the FCS favouring UCTs (Hoddinott 2013: MD 4.65, 95% CI 2.41 to 6.87, n = NR; Schwab 2013: MD 4.52, 95% CI 6.85 to 2.19; 1581 households). Hoddinott 2013 was at unclear overall risk of bias and Schwab 2013 was at high overall risk of bias.
Prospective controlled studies
One PCS reported an unclear effect on the HDDS potentially favouring UCTs (0.16, 95% CI –0.07 to 0.39; 6003 households) (Table 15) (Breisinger 2018). This study was at high overall risk of bias.
Secondary outcomes
1.4 Change in adequacy of dietary intake
Three cRCTs reported change in adequacy of dietary intake (Ahmed 2019a; Ahmed 2019b; Brugh 2018). One study reported a clear effect favouring UCTs and two studies reported an unclear effect potentially favouring UCTs (P = 0.047) (Table 15).
Brugh 2018 reported a clear effect favouring the intervention on the proportion of households who were food energy deficient (i.e. where the total household caloric availability was lower than the total household caloric requirement) (pp –10, 95% CI –17.8 to –2.16; 3290 households). This study was at low overall risk of bias.
Ahmed 2019a and Ahmed 2019b reported an unclear effect potentially favouring UCTs. A meta‐analysis of these two studies showed that UCTs may make no difference to the proportion of households with food poverty, defined as per capita daily caloric intake below 2122 calories (MD –4.64, 95% CI –9.34 to 0.06, n = NR). These studies were at low overall risk of bias.
1.5 Change in anthropometric indicators
Ten cRCTs (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Daidone 2014; Fenn 2015; Fernald 2011; Merttens 2013; Pellerano 2014; Skoufias 2013; Tonguet Papucci 2015) and two PCS (Aguero 2006; Renzaho 2017) reported various anthropometric measures.
1.5.1 Stunting: height‐for‐age z‐scores < –2SD; chronic undernutrition)
Randomised controlled trials
Four cRCTs reported on the proportion of children who were stunted (Asfaw 2014; Fenn 2015; Merttens 2013; Tonguet Papucci 2015), with evidence showing that UCTs may reduce stunting (4 trials, 4713 children; low‐certainty evidence; Table 1). One study showed a clear effect favouring UCTs, two studies showed an unclear effect favouring UCTs, and one study showed an unclear effect favouring control (P = 0.047; Figure 5). A meta‐analysis of two of these studies showed a reduction in stunting with UCTs (OR 0.62, 95% CI 0.46 to 0.84; 2914 children; I2 = 0%; Analysis 1.7) (Fenn 2015; Tonguet Papucci 2015).
1.7. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 7: Proportion stunted (height‐for‐age z‐score (HAZ) < ‐2SD)
Fenn 2015 reported a clear effect favouring UCTs, with a reduction in the odds of stunting of 46% at 12 months (OR 0.54, 95% CI 0.36 to 0.81; 1664 children). There was a similar effect for the proportion of children who were severely stunted (HAZ < –3SD) (Table 15). This study was at low overall risk of bias.
Tonguet Papucci 2015 and Asfaw 2014 reported unclear effects potentially favouring UCTs. Tonguet Papucci 2015 reported a reduced likelihood of stunting in the intervention group compared to the control group at 24 months by 27% (OR 0.73, 95% CI 0.47 to 1.14; n = 1250; P = 0.17), but the effect ranged from a beneficial effect on the outcome to worsening the outcome. In Asfaw 2014, the intervention reduced the proportion of stunted children by 4.63 pp (P > 0.1). Tonguet Papucci 2015 was at low overall risk of bias whereas Asfaw 2014 was at high overall risk of bias.
Merttens 2013 reported an increase in the proportion of stunted children (pp 7.0; 1062 children; P > 0.1) and severely stunted children (pp 1.9; 1062 children; P > 0.1) among those in the UCT group compared to those in the control group. This study was at high overall risk of bias.
In addition to the proportion of stunting, six trials reported the effects on mean HAZ (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Daidone 2014; Fenn 2015; Fernald 2011); and one on mean z‐score per month (Tonguet Papucci 2015). A meta‐analysis showed an unclear effect of UCTs on HAZ (MD 0.07, 95% CI –0.04 to 0.18; I2 = 56%; Analysis 1.8). A sensitivity analysis performed using only studies at overall low risk of bias showed a clear effect favouring UCTs (MD 0.16, 95% CI 0.02 to 0.29; Appendix 4) (Daidone 2014; Fenn 2015).
1.8. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 8: HAZ
Prospective controlled studies
One PCS reported a clear effect favouring UCTs on stunting at five years (pp –5.16, 95% CI –9.55 to –0.77; 1491 children; Table 15; Figure 5) (Renzaho 2017).
Renzaho 2017 and Aguero 2006 also reported on the effect of UCTs on mean HAZ (data not pooled as SE was not available for either study). Renzaho 2017 reported a clear effect favouring UCTs at five years (pp 18, 95% CI 9 to 27; 1491 children). Aguero 2006 reported that after 72 months, the mean z‐score was better in children receiving the intervention (–0.84) than in those who only received the intervention after they were aged three years (–0.91) (566 children) or those who were rejected or were not yet receiving the intervention (–1.08) (399 children). Both studies are at high overall risk of bias.
Aguero 2006 also reported the effects of the intervention on HAZ for children receiving the child care grant for different periods of the critical nutritional window aged between 0 and 36 months. They found that for children receiving the intervention for less than 20% of this period there was no effect on HAZ. Compared to receiving a 'small dose', they found a significant impact on HAZ for children receiving the intervention during 45% to 80% of the nutrition window (mean change in HAZ 0.15 at 45%, and 0.25 at 80% of nutritional window; data derived from graphs).
1.5.2 Wasting: weight‐for‐height z‐score < –2SD (acute undernutrition)
Randomised controlled trials
Four cRCTs reported effects of UCTs on wasting (Asfaw 2014; Fenn 2015; Merttens 2013; Tonguet Papucci 2015). Evidence showed that there was uncertainty about whether UCTs reduce wasting (4 trials, 6396 children; very low‐certainty evidence; Table 1). One study showed an unclear effect potentially favouring UCTs and three studies showed an unclear effect potentially favouring the control (P = 0.016; Figure 5).
Tonguet Papucci 2015 reported an unclear effect potentially favouring the intervention, observing a 2% decrease in the risk of wasting at two years (incidence rate ratio (IRR) 0.92, 95% CI 0.64 to 1.32; 1250 children; P = 0.66). However, this effect ranged from a 36% reduction to a 32% increase in risk.
Asfaw 2014, Merttens 2013, and Fenn 2015 reported an unclear effect potentially favouring the control as they observed an increase in the proportion of wasting among children receiving UCTs, but reported a CI that crossed the null. In Fenn 2015, the odds of wasting was 10% higher among children receiving the intervention at one year (OR 1.10, 95% CI 0.71 to 1.71; 1664 children). At two years, the proportion of wasted children was 5.95 pp higher among those in the UCT group in Asfaw 2014 (989 children; P > 0.1) and 4.7 pp in Merttens 2013 (1062 children; P > 0.1). In Merttens 2013, the proportion of children younger than five years who were severely wasted also increased by 3.9 pp (P > 0.1). Both studies are at high overall risk of bias.
In addition to the effects on stunting, five cRCTs reported on the effect of UCTs on mean WHZ (Ahmed 2019a; Ahmed 2019b; Asfaw 2014; Daidone 2014; Fenn 2015) and one on mean WHZ/month (Tonguet Papucci 2015). A meta‐analysis of data from these studies showed that UCTs made no difference on WHZ (MD –0.02, 95% CI –0.10 to 0.06; I2 = 36%; Analysis 1.9). Two of these studies were at unclear overall risk of bias and one at high overall risk of bias. A sensitivity analysis of studies at low overall risk of bias studies changed the direction of effect to unclearly favour UCTs (MD 0.02, 95% CI –0.18 to 0.21; Appendix 4) (Daidone 2014; Fenn 2015).
1.9. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 9: Weight‐for‐height z‐score (WHZ)
Prospective controlled studies
One PCS reported on stunting, with effects clearly favouring UCTs (pp –2.84, 95% CI –5.58 to –0.1; 1491 children) (Figure 5) (Renzaho 2017). This study was at high overall risk of bias.
This study also reported on effect of UCTs on mean WHZ, also reporting a clear effect favouring UCTs (MD 0.19, 95% CI 0.09 to 0.03; 1491 children) (Table 16).
1.5.3 Underweight
1.5.3.1 Weight‐for‐age z‐scores < –2SD
Three cRCTs reported unclear effects of UCTs on the proportion of underweight children (Asfaw 2014; Merttens 2013; Pellerano 2014). Two trials reported unclear effects potentially favouring UCTs and one trial reported unclear effects potentially favouring the control (P = 0.047) (Table 15; Figure 5).
The two studies favouring the intervention reported an unclear effect potentially favouring UCTs on underweight (Asfaw 2014; Pellerano 2014). Pellerano 2014 reported a reduction in proportion of children aged from birth to 36 months who were underweight at two years by 3.64 pp when they were aged 12 months (P > 0.05), Asfaw 2014 reported a reduction of 0.62 pp in the proportion of children aged under five years who were underweight (pp –0.62; 1491 children; P > 0.1).
Merttens 2013 reported an unclear effect favouring the control, as they reported an increase in the proportion of children who were underweight or severely underweight in the UCT group (3.9 pp with UCT versus 3.2 pp with control; 1062 children; P > 0.1).
In addition to the effects of UCTs on underweight, two trials also reported on the effects of UCTs on mean WAZ (Asfaw 2014; Daidone 2014). A meta‐analysis of these two studies showed that UCTs may have no effect on underweight (MD –0.04, 95% CI –0.43, 0.35; 7577 children: I2 = 74%; Analysis 1.10). Daidone 2014 was at low overall risk of bias, whereas Asfaw 2014 was at high overall risk of bias. Daidone 2014 assessed a child grant programme and Asfaw 2014 assessed a cash transfer programme for households with orphans and vulnerable children, where in some districts some conditions, such as school attendance, and penalties were imposed even though the programme was unconditional.
1.10. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 10: Weight‐for‐age z‐score (WAZ)
1.5.3.2 Body mass index
One cRCT reported unclear effects potentially favouring the control on BMI of mothers at six months (MD –0.1, 95% CI –0.36 to 0.16; 1208 mothers; Table 15) (Fenn 2015).
1.5.3.3 Mid‐upper arm circumference
One cRCT reported unclear effects potentially favouring UCTs on MUAC measures for mothers and children (MD 0.09, 95% CI –0.13 to 0.3; 1208 mothers; MD 0.06, 95% CI –0.02 to 0.15; 1683 children; Table 15) (Fenn 2015).
1.6 Change in biochemical indicators
1.6.1 Haemoglobin concentration
Two cRCTs reported on the effects of UCTs on haemoglobin concentration (Fenn 2015; Fernald 2011). A meta‐analysis of these two studies showed an unclear effect of UCTs on haemoglobin in children (MD –0.06, 95% CI –0.21 to 0.09; 2605 children; Analysis 1.11). Fenn 2015 also reported on the effects in mothers, finding a clear effect favouring the control on haemoglobin in mothers receiving UCTs (MD –0.42, 95% CI –0.63 to –0.20; 1208 mothers). Both studies were at low overall risk of bias.
1.11. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 11: Haemoglobin concentration (g/dL)
1.7 Cognitive function and development
Three cRCTs reported different measures of cognitive function and development (Baird 2013; Daidone 2014; Fernald 2011). Evidence showed that UCTs make little or no difference on cognitive function and development (3 cRCTs; 10,813 children; high‐certainty evidence; Table 1). All three trials reported an unclear effect favouring the intervention (P = 0.016; Figure 5).
Baird 2013 reported an increase in the cognitive test score based on a version of Raven's Colored Progressive matrices at two years (MD 0.14 SDs, 95% CI 0.02 to 0.26; 2057 children) and Daidone 2014 reported an increase in the Early Childhood Development score among children receiving UCTs at two years (MD 0.31; 5670 children; P > 0.1) (Table 15). Fernald 2011 reported on scores after two years for language development in young children receiving UCTs, using two different measures: scores for early language skills of children aged 12 to 35 months using the Inventario do Desenvolvemento de Habilidades Comunicativas (IDHC)‐B tool (MD 2.43, 95% CI –1.01 to 5.86; 1192 children; P > 0.1), and scores for the receptive vocabulary test (Test de Vocabulario en Imagenes Peabody (TVIP)) in children older than 36 months (MD 0.01, 95% CI –0.08 to 0.10; 1894 children; P > 0.1). However, for both of these, the effect ranged from a decrease to an increase in scores. All cognitive measures reported in the included studies are summarised in Table 13.
1.8 Change in proportion of anxiety or depression (mental health indicators)
Three cRCTs (Baird 2013; Fernald 2011; Hjelm 2017) and one RCT (Haushofer 2013) reported different measures of mental health.
1.8.1 Depression
Fernald 2011, Haushofer 2013, and Hjelm 2017 reported effects of UCTs on depressive symptoms scores using the Center for Epidemiologic Studies Depression Scale (CES‐D) (higher scores indicate worse symptoms). The meta‐analysis indicated that UCTs do not make a difference in depression scores at two years (MD –0.41, 95% CI –1.31 to 0.49; 5787 participants; I2 = 36%; Analysis 1.12). Fernald 2011 assessed the effect of the intervention on men and women, Haushofer 2013 on mothers, and Hjelm 2017 on adolescents. Fernald 2011 and Haushofer 2013 were at low overall risk of bias and Hjelm 2017 was at unclear overall risk of bias.
1.12. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 12: Depression score (CES‐D scale)
1.8.2 Perceived stress
Two cRCTs (Fernald 2011; Hjelm 2017) and one RCT (Haushofer 2013) reported on the effects of UCTs on perceived stress using Cohen's Perceived Stress Scale (PSS) (lower values correspond to less stress). A meta‐analysis of Haushofer 2013 and Hjelm 2017 indicated that UCTs may reduce perceived stress (MD –0.15, 95% CI –0.26 to –0.03; n = 3570; I2 = 0%; Analysis 1.13). Fernald 2011 reported an increase in the perceived stress z‐score of mothers in the intervention group at two years, both for those in the bottom quartile of baseline expenditure (MD 0.18, 95% CI –0.02 to 0.37; n = 1430; P < 0.1) and for those in the top three quartiles of baseline expenditure at two years (MD 0.05, 95% CI –0.11 to 0.20; P > 0.1).
1.13. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 13: Perceived Stress Scale (PSS)
1.8.3 Psychological distress
One cRCT reported on psychological distress, a binary measure of psychological distress, anxiety and depression; social dysfunction; and loss of confidence based on the 12‐item General Health Questionnaire (GHQ‐12) (Baird 2013). Among girls who were attending school and exposed to a UCT compared to girls in the control group, the proportion of psychological distress was smaller by 14.3 pp at one year (95% CI –21.0 to –7.6), and by 3.8 pp at two years (95% CI –13.14 to 5.8; n = 2089; P > 0.1), but the effect at two years was imprecise.
1.9 Morbidity
Seven cRCTs reported on different morbidity measures (Ahmed 2019a; Ahmed 2019b; Daidone 2014; Fenn 2015; Merttens 2013; Pellerano 2014; Tonguet Papucci 2015).
1.9.1 Respiratory infections
Four cRCTs reported on the effects of UCTs on respiratory infections (Asfaw 2014; Daidone 2014; Fenn 2015; Tonguet Papucci 2015). Two trials reported a clear effect favouring the intervention and two trials reported an unclear effect potentially favouring the intervention (P = 0.023; Table 15). Data could not be pooled.
Asfaw 2014 and Tonguet Papucci 2015 reported clear effects favouring UCTs. Tonguet Papucci 2015 reported a 21% reduced incidence of acute respiratory tract infection episodes among children aged from birth to 15 months in the previous seven days, as refereed by mothers (IRR 0.79, 95% CI 0.78 to 0.81; 1250 children; P < 0.001). Asfaw 2014 reported a reduced risk of respiratory infections of 44% among children aged from birth to seven years (957 children; P < 0.05). Asfaw 2014 was at high overall risk of bias whereas Tonguet Papucci 2015 was at low overall risk of bias.
Daidone 2014 and Fenn 2015 reported unclear effects potentially favouring UCTs. Daidone 2014 reported that the proportion of children aged from birth to 60 months with acute respiratory tract infection in a two‐week reference period was lower by 3.6 pp in the intervention group compared to the control group (effect estimate –0.036, 95% CI –0.061 to –0.011; P > 0.05). In Fenn 2015, the odds of respiratory infections was 27% lower among children in the UCT group (OR 0.73, 95% CI 0.51 to 1.03; 1683 children). Both studies were at low overall risk of bias.
1.9.2 Diarrhoeal disease
Five cRCTs reported on the effects of UCTs on diarrhoeal disease (Ahmed 2019a; Ahmed 2019b; Daidone 2014; Fenn 2015; Tonguet Papucci 2015). One study reported a clear effect favouring UCTs, two studies reported an unclear effect potentially favouring UCTs, one study reported an unclear effect potentially favouring the control, and one study reported no effect (P = 0.047) (Table 15).
Daidone 2014 reported clear effects favouring UCTs. Among children aged from birth to 60 months in the UCT group, the proportion with diarrhoea in the previous two weeks reduced by 4.9 pp at one year (pp –4.9, 95% CI –8.9 to –0.9; 7232 children; P < 0.05).
Ahmed 2019a and Ahmed 2019b reported unclear effects potentially favouring UCTs. In Ahmed 2019a, there was a reduction in the proportion of children with diarrhoea of 0.3 pp (95% CI –0.04 to 0.04, n = NR), and in Ahmed 2019b of 0.9 pp (95% CI –0.05 to 0.03, n = NR). All studies were at low overall risk of bias.
Tonguet Papucci 2015 reported no difference between the groups in the incidence of diarrhoeal episodes in the previous seven days, as reported by the mother, after one year of the intervention (IRR 1.00, 95% CI 0.97 to 1.03; 1250 children; P = 0.89). This study was at low overall risk of bias.
1.9.3 Any illness
Two cRCTs reported on the effects of UCTs on the proportion of children or people who were ill (Merttens 2013; Pellerano 2014), one reporting a clear effect favouring UCTs and the other unclear effects favouring the control (P = 0.125) (Table 15).
Pellerano 2014 reported a reduction in the proportion of children who were ill in the previous month in the intervention compared to the control group by 15 pp at one year (from 39% to 31%) (pp –15,38; 1996 children; P < 0.1).
In Merttens 2013, there was no difference between the intervention and control groups in the proportion of people who reported being ill or injured in the previous three months, after one year of the intervention (pp 1.0; 14,342 participants; P > 0.1). In this study, these proportions reduced significantly in both intervention and control groups, and injuries were also included as an 'illness'. Pellerano 2014 was at low overall risk of bias whereas Merttens 2013 was at high overall risk of bias due to high risk of selection and attrition bias.
1.10 Adverse outcomes (proportion of participants overweight or obese)
Pellerano 2014, a cRCT, reported unclear effects potentially favouring UCTs on the proportion of infants who were overweight when they were aged six and 12 months, at two years of the intervention (6 months old: pp –5.08; 474 children; P > 0.05; 12 months old: pp –6.46; 293 children; P > 0.05) (Table 15).
Comparison 2: conditional cash transfers
Fourteen included studies assessed CCTs, where a specified amount of money was transferred to poor families regularly as long as they meet specific conditions. Nine were cRCTs (Baird 2013; Evans 2014; Gertler 2000 (PROGRESA); Hidrobo 2014; Kandpal 2016; Kurdi 2019; Kusuma 2017a; Macours 2012; Maluccio 2005) and five were PCS (Andersen 2015; Ferre 2014; Huerta 2006 (PROGRESA); Leroy 2008 (PROGRESA); Lopez Arana 2016). All studies compared CCTs with no intervention. However, requirements and other intervention components differed across studies. Requirements (or conditions) included regular check‐ups for children, school enrolment and regular attendance, vaccination, micronutrient supplementation for children or for pregnant women, and attending nutrition education sessions.
Two cRCTs (Macours 2012; Maluccio 2005) and one PCS (Ferre 2014) reported the proportion of household expenditure on food. Two cRCTs (Hidrobo 2014; Kurdi 2019) and one PCS (Ferre 2014) reported on dietary diversity measures. Seven cRCTs (Evans 2014; Gertler 2000 (PROGRESA); Kandpal 2016; Kusuma 2017a; Kurdi 2019; Macours 2012; Maluccio 2005; ) and four PCS (Andersen 2015Leroy 2008 (PROGRESA); Lopez Arana 2016; Ferre 2014) reported on various anthropometric measures. Two cRCTs (Baird 2013; Macours 2012) and one PCS (Andersen 2015) reported on cognitive function and development measures. One cRCT (Baird 2013) reported on psychological distress. Four cRCTs reported measures of morbidity (Evans 2014; Gertler 2000 (PROGRESA); Kandpal 2016; Macours 2012). Two PCS reported adverse measures of overweight (Andersen 2015; Lopez Arana 2016).
Further details about the studies in this comparison are presented in Table 17. Table 18 presents the results of cRCTs and Table 19 of PCS. Table 2 and harvest plot in Figure 6 summarise the results of CCTs on key outcomes.
11. Conditional cash transfers – overview of included studies.
| Study name (year) country of conduct | Study design | Overall risk of biasa | Other key detail of intervention | Population (sample size at baseline: intervention/ control) | Outcome domains and measures with available data | Timepoint of measurement |
|
Baird 2013 (Malawi) |
cRCT | Low |
Programme name: Schooling, Income, and Health Risks study (SIHR). Includes unconditional and conditional groups. Type, amount and frequency of payments: payments were split between guardian and girl in each HH. HH amount varied randomly from USD 4, USD 6, USD 8, to USD 10 per month. Amount paid to girl beneficiaries varied randomly from USD 1, USD 2, USD 3, USD 4, to USD 5 per month. Conditionalities: school attendance for 80% of the days during the previous month. Provider: 2 NGOs Delivery: payments to girl beneficiaries at local distribution points Co‐interventions: NR |
Adolescent girls who were never married from urban and rural HHs (1211/1495 girls) | Cognitive function and development:
Anxiety/depression:
|
1 and 2 years |
|
Macours 2012 (Nicaragua) |
cRCT | Low |
Programme name: Atención a Crisis Amount and frequency of payments: Standard payment of USD 145 per HH every 2 months. 3 intervention groups: 1. Standard transfer + education: additional USD 145 per HH and USD 25 per child for HHs with children aged 7–15 years; 2. Standard transfer + scholarship for vocational training; and 3. Standard transfer + lump sum to start non‐agricultural activity. Conditionalities: 1. Regular health check‐ups for children aged 0–5 years, school enrolment; 2. regular attendance, however not monitored in practice; and 3. developing a business plan. Provider: government Delivery: payments to child's primary carer. Co‐interventions: NR |
Poor rural HHs with 2377 children aged < 6 years (3002/1019 HHs) | HH expenditure on food:
Anthropometric indicators:
Anxiety/depression:
Cognitive function and development:
Morbidity – child
|
9 months (12 months for CES‐D) |
|
Maluccio 2005 (Nicaragua) |
cRCT | Low |
Programme name: Red de Protección Social Amount and frequency of payments: amount NR; payments every 2 months. Conditionalities: school attendance; preventive health care visits for children for growth and development monitoring, vaccination, and provision of antiparasites, vitamins, and iron supplements. Provider: government. Preventive health services provided by private healthcare providers. Delivery: NR Co‐interventions: NR |
Poor, rural HHs (1396 HHs) | HH expenditure on food:
Anthropometric indicators:
|
1 and 2 years |
|
Kusuma 2017a (Indonesia) |
cRCT | Unclear |
Programme name: Program Keluarga Harapan (PKH) Amount and frequency of payments: USD 60–220 per HH per year, depending on the number and age of children in the HH. Conditionalities: health: pre‐ and postnatal visits, iron supplementation and assisted deliveries for pregnant women, growth monitoring, immunisation and vitamin A supplementation of children aged < 5 years. Education: primary and junior secondary school enrolment and attendance rates of 85%. Provider: government Delivery: payment to mothers through local post offices Co‐interventions: NR |
Very poor urban HHs with children aged 24–36 months (1395 HHs) | Anthropometry:
|
2 years |
|
Gertler 2000 (PROGRESA) (Mexico) |
cRCT | Unclear |
Programme name: Oportunidades (previously known as PROGRESA) Type, amount and frequency of payments: scholarships of up to MXN 490 (January–June 98) and MXN 625 per HH (July–December 1999), every 2 months; payments for school supplies; and monthly payments for food. Conditionalities: health: attendance of preventive health services by every family member; growth monitoring and immunisation of children aged 0–5 years; nutrition supplements (for lactating women, children aged 6–23 months or low‐weight children), antenatal care for pregnant women. Education: school enrolment and school attendance > 85%. Provider: government Delivery: lump sum payment to mothers once completed forms were submitted by HHs to verify school attendance. Co‐interventions: NR |
Poor rural HHs (506 villages; 320/186) |
Anthropometric indicators:
Biochemical indicators:
Cognitive function and development:
Morbidity – Child
|
8, 12, 15, 20 months, 10 years |
|
Evans 2014 (Tanzania) |
cRCT | High |
Programme name: N/A Amount and frequency of payments: USD 12–36, depending on the number of people in the HH, every 2 months. Conditionalities: education: primary school enrolment and attendance for children aged 7–15 years; health: health facility visits for growth monitoring 6 times a year for children aged 0–5 years; vaccination and growth monitoring for children 0–2 years; yearly visit to health facility for elderly people (aged ≥ 60 years). Provider: Tanzania Social Action Fund (TASAF), World bank Delivery: payments disbursed by TASAF to bank accounts managed by local government authorities. Funds disbursed directly to community‐managed accounts who made payments to mothers. Co‐interventions: transfers from government/TASAF or from NGOs/religious organisation |
Poor HHs with vulnerable children or elderly people, or both (80 villages; 40/40) |
Anthropometric indicators: NR | 30 and 42 month |
|
Hidrobo 2014 (Colombia) |
cRCT | High |
Programme name: N/A Amount and frequency of payments: USD 40 per month per HH. Conditionalities: attendance of monthly nutrition sensitisation training sessions by HH members. Provider: World Food Programme (NPO) Delivery: money transferred on to pre‐programmed debit cards. Co‐interventions: NR |
Poor urban HHs (2357 HHs) | HH expenditure on food:
Dietary diversity:
|
7 months |
|
Kandpal 2016 (Philippines) |
cRCT | High |
Programme name: Pantawid Pamilyang Pilipino Programme Type, amount and frequency of payments: health grant of PHP 500 (USD 11) per HH per month; education grant of PHP 300 (USD 6.50) per child per month for ≤ 10 months/year, and for ≤ 3 children in the HH. Payments every 2 months. Conditionalities: health: clinic visits for immunisation and vaccination, growth monitoring, and management of childhood disease in children aged < 5 years; antenatal care for pregnant women, starting from the first trimester; school‐aged children (6–14 years) to receive deworming tablets 2 times/year; and HHs with children 0–14 years, the HH grantee (mother) or spouse (or both) had to attend family development sessions monthly. Education: enrolment of children aged 6–14 years in primary or secondary school and 85% school attendance every month. Provider: government Delivery: NR Co‐interventions: NR |
Poor HHs with children aged 0–14 years or pregnant women (714/ 704 HHs) | Anthropometric indicators:
Morbidity – child:
|
36 months |
|
Kurdi 2019 (Yemen) |
cRCT | High |
Programme name: Cash for Nutrition programme Amount and frequency of payments: payments every 3 months (YER 30,000 per month for 9 months in 2015; YER 10,000 (USD 30) per month for 12 months in 2016/2017) to mothers of children aged 2 years of age and pregnant women. Conditionalities: attending monthly nutrition‐focused trainings, complying with child monitoring and treatment of malnutrition. Attendance tracked but conditionality not strictly enforced. Provider: government, Yemen Emergency Crisis Response Project (funded by the World Bank) Delivery: nutrition sessions delivered by trained local women. Details of cash transfer not reported. Co‐interventions: unspecified other food distribution programmes. |
Women from poor and vulnerable (1001/999 women) | Diet diversity:
Anthropometric indicators:
|
2.5 years |
|
Andersen 2015 (Peru) |
Prospective controlled study | High |
Programme name: Juntos Amount and frequency of payments: PEN 100 (30 US dollars) each month regardless of HH composition. Conditionalities: regular health visits for children aged < 5 years, or pregnant and lactating women. Children aged 6–14 years with primary school attendance ≥ 85%. Provider: Peruvian government Delivery: NR Co‐interventions: NR |
Poor HHs with children aged 6–18 months (374/586 children) | Anthropometric indicators:
Cognitive function and development:
Adverse effects:
|
< 2 years and ≥ 2 years |
| Ferre 2014 (Bangladesh) |
Prospective controlled study | High |
Programme name: Shombhob project Amount and frequency of payments: BDT 400 per months for HHs with children 0–36 months and BDT 400 per month for HHs with primary school children (6–15 years). Conditionalities: Health: Attending growth monitoring of children aged 0 – 36 months, and nutrition session for mother/carer. Education: school attendance of at least 80% every month. Provider: Government Delivery: Cash cards provided to beneficiary mothers. Electronic transfer to their accounts with the Bangladesh Post Office (BPO). Withdrawal from mobile machines on a designated day during each payment cycle in each village, or from Upazila BPO branch office at any time point. |
Rural HHs (700/1587) | HH expenditure on food:
Dietary diversity:
Anthropometric indicators:
|
13 months |
| Huerta 2006 (PROGRESA) (Mexico) | Prospective controlled study | High |
Programme name: Oportunidades (previously known as PROGRESA) Type, amount and frequency of payments: SeeGertler 2000 (PROGRESA) Conditionalities: seeGertler 2000 (PROGRESA) Provider: Mexican government Delivery: seeGertler 2000 (PROGRESA) Co‐interventions: NR |
Poor rural HHs with ≥ 1 child aged < 5 years (205/142 communities) | Anthropometric indicators:
Biochemical indicators:
Morbidity – child:
|
14 and 26 months |
|
Leroy 2008 (PROGRESA) (Mexico) |
Prospective controlled study | High |
Programme name: Oportunidades (previously known as PROGRESA) Type, amount and frequency of payments: USD 32.5–41.3 per month (see Gertler 2000 (PROGRESA)) Conditionalities: seeGertler 2000 (PROGRESA) Provider: government of Mexico Delivery: see Gertler 2000 (PROGRESA) Co‐interventions: NR |
Poor and vulnerable urban HHs (733 children aged 0–24 months) |
Anthropometric indicators:
|
2 years |
|
Lopez Arana 2016 (Colombia |
Prospective controlled study | High |
Programme name: Familias en Acción Type, amount and frequency of payments: COP 40,000 for children aged < 7 years; COP 14,000 per primary school and COP 28,000 per secondary school child. Periodic payments. Conditionalities: children aged < 7 years to attend vaccination programmes and growth and development check‐ups regularly; children aged 7–17 years to attend ≥ 80% of school lessons. Provider: government, World Bank and Inter‐American Development Bank Delivery: transfer of cash to mothers into the HH bank account. Co‐interventions: some children participated in a childcare supplementary nutrition and psychosocial stimulation programme (Hogares Comunitarios programme). |
Poor HHs with children aged 0–17 years (9293/4424) | Anthropometric indicators:
Adverse events:
|
About 4 years |
aOverall Risk of Bias based on risk of selection and attrition bias.
BMIZ: body mass index‐for‐age z‐score; CES‐D: Center for Epidemiologic Studies Depression Scale; COP: Colombian peso; cRCT: cluster randomised controlled trial; DDI: Dietary Diversity Index; FCS: Food Consumption Score; GHQ‐12: 12‐item General Health Questionnaire; HAZ: height‐for‐age z‐score; Hb: haemoglobin; HDDS: Household Dietary Diversity Score; HH: household; LAZ: length‐for‐age z‐score; MXN: Mexican peso; N/A: not applicable/available; non‐governmental organisation; NPO: non‐profit organisation; NR: not reported; PEN: Yemeni rial; PHP: Philippine peso; TVIP: Test de Vocabulario en Imagenes Peabody; WAZ: weight‐for‐age z‐score; WHZ: weight‐for‐height z‐score; WLZ: weight‐for‐length z‐score; YER: Yemeni rial.
12. Conditional cash transfers – results of included trials.
| Study ID (risk of bias) | Study design (n) | Conditional cash transfers | No intervention | Effect measure (time point) | Effect directiona | Meta‐analysis (yes/no) | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | |||||
| Primary outcomes | ||||||||||
| 2.2: Proportion of HH expenditure on food | ||||||||||
| 2.2.1 Outcome measure: proportion of HH expenditure on food (weekly/monthly) | ||||||||||
| Maluccio 2005 (+) | cRCT (1490 HHs) | 69.8 | 70 | 766 | 70.2 | 66.5 | 724 | pp 3.9, SE 1.7, 95% CI 0.568 to 7.232, P < 0.01 (1 year) | ▼ | N/A |
| cRCT (1434 HHs) | — | — | 722 | — | — | 712 | pp 4.1, SE 1.3, 95% CI 1.552 to 6.648, P < 0.01 (2 years) | ▼ | ||
| 2.2.2 Outcome measure: proportion of food in total expenditures (SDs) | ||||||||||
| Macours 2012 (+) | cRCT (3326 HHs) | — | — | — | 70% | 70.7% | Effect 0.005, SD, SE 0.009, 95% CI –0.013 to 0.023, P > 0.1 (9 months) | ▽ | ||
| 2.3: Proportion of HHs who were food secure | ||||||||||
| 2.3.2 Dietary diversity | ||||||||||
| 2.3.2.2 Outcome measure: HDDS (0–12) (mean) | ||||||||||
| Hidrobo 2014 (‐) | cRCT (2087 HHs) | 9.23 | — | — | 9.11 | — | — | MD 0.46, SE 0.11, 95% CI 0.244 to 0.676, P < 0.01 (7 months) | ▲ | Yes |
| Kurdi 2019 (‐) | cRCT (1850 HHs) | — | — | 935 HHs | — | — | 915 HHs | MD 0.374, SE 0.262, 95% CI –0.13952 to 0.88752 (2.5 years) | △ | |
| Secondary outcomes | ||||||||||
| 2.5Change in anthropometric indicators | ||||||||||
| 2.5.1 Stunting (chronic undernutrition) | ||||||||||
| 2.5.1.1 Outcome measure: proportion stunted (HAZ < –2SD) | ||||||||||
| Maluccio 2005 (+) | cRCT (722 children aged < 5 years) | 41.9 | 37.1 | — | 40.9 | 41.5 | — | pp –5.3, 95% CI –11.376 to 0.776, P < 0.1 (2 years) | △ | Yes; this subset. This was entered as MD: difference in percentage stunted |
| Gertler 2000 (PROGRESA) (?) | cRCT (n at follow‐up 1062) | — | 0.396 | — | — | 0.410 | — | OR 0.914, P = 0.495 (20 months) | △ | |
| Kusuma 2017a (?) | cRCT (1394 children aged 24–36 months) | — | — | — | — | mean 0.55 | — | DID 0.035, SE 0.046, 95% CI –0.05516 to 0.12516 pp 3.5, 95% CI –5.5 to 12.5, P > 0.05 (2 years) |
▽ | Yes; this subset. This was entered as MD: difference in percentage stunted |
| Kandpal 2016 (‐) | cRCT (351 children aged < 36 months) | — | — | — | — | 49.701 | — | pp –3.768, 95% CI –13.830 to 6.294, P > 0.1 (36 months) | △ | |
| 2.5.1.2 Outcome measure: proportion with severe stunting (HAZ < –3SD) | ||||||||||
| Kusuma 2017a (?) | cRCT (1394 children aged 24–36 months) | — | — | — | — | mean 0.29 | — | DID 0.047, SE 0.053, 95% CI –0.05688 to 0.15088. pp 4.7, 95% CI –5.7 to 15.1, P > 0.05 (2 years) |
▽ | Yes |
| Kandpal 2016 (‐) | cRCT (351 children aged < 36 months) | –10.189 | 23.952 | pp –10.189, 95% CI –18.769 to –1.607 (3 years) | ▲ | |||||
| 2.5.1.3 Outcome measure: HAZ (mean, SD) | ||||||||||
| Maluccio 2005 (+) | cRCT (1036 children aged < 5 years) | –1.79 (1.14) | –1.65 (1.15) | 479 | –1.76 (1.15) | –1.80 (1.18) | 557 | MD 0.17, 95% CI 0.0132 to 0.327, P < 0.05 (2 years) | ▲ | Yes |
| Macours 2012 (+) | cRCT (3082 children aged < 6 years) | –1.27b | — | — | –1.08b | — | — | MD 0.072, 95% CI 0.005 to 0.139, P < 0.05 (9 months) | ▲ | |
| Evans 2014 (‐) | cRCT (102 children aged 0–4 years) | — | — | — | — | — | — | MD 0.86, 95% CI –2.358 to 3.718, P > 0.1 (1.5 years) | △ | |
| Kandpal 2016 (‐) | cRCT (351 children) | — | 0.284 | — | — | –1.903 | — | MD 0.284, 95% CI –0.034 to 0.600, P < 0.1 (3 years) | △ | |
| Kurdi 2019 (‐) | cRCT (1048 children) | — | — | — | — | — | — | MD 0.109, SE 0.146, 95% CI –0.18 to 0.395 (2.5 years) | △ | |
| 2.5.2Wasting (acute undernutrition) | ||||||||||
| 2.5.2.1 Outcome measure: proportion wasted (WHZ < –2SD) | ||||||||||
| Maluccio 2005 (+) | cRCT (722 children aged < 5 years) | 1.0% | 0.4% | 479 | 0.3 | 0.2 | 557 | pp –0.4, SE 0.5, 95% CI –1.38 to 0.58, P > 0.1 (2 years) | △ | Yes |
| Kusuma 2017a (?) | cRCT (1394 children aged 24–36 months) | — | — | — | — | Mean 0.19 | — | DID –0.063, SE 0.032, 95% CI –0.12572 to –0.00028, P < 0.05 | ▲ | |
| 2.5.2.2 Outcome measure: proportion severely wasted (WHZ < –3SD | ||||||||||
| Kusuma 2017a (?) | cRCT (1394 children aged 24–36 months) | — | — | — | — | Mean 0.09 | — | Beta –0.037, SE 0.022, 95% CI –0.08012 to 0.00612, P < 0.1 | △ | |
| 2.5.2.3 Outcome measure: WHZ (mean, SD) | ||||||||||
| Evans 2014 (‐) | cRCT (63 children aged 0–4 years) | — | — | — | — | — | — | MD –0.03, SE 0.45, 95% CI –0.9120 to 0.852, P > 0.1 (1.5 years) | ▽ | Yes |
| Kurdi 2019 (‐) | cRCT (1048 children) | — | — | — | — | — | — | MD 0.190, SE 0.148, 95% CI –0.10008 to 0.48008 (2.5 years) | △ | |
| 2.5.3 Underweight | ||||||||||
| 2.5.3.1 Outcome measure: proportion underweight (WAZ < –2SD) | ||||||||||
| Maluccio 2005 (+) | cRCT (722 children aged < 5 years) | 15.3 | 10.4 | — | 14.7 | 15.8 | — | pp –6, SE 2.6, P < 0.05 (2 years) | ▲ | Yes |
| Kusuma 2017a (?) | cRCT (1394 children aged 24–36 months) | — | — | — | — | Mean 0.38 | — | DID –0.040, SE 0.036, 95% CI –0.11056 to 0.03056, P > 0.05 | △ | |
| Kandpal 2016 (‐) | cRCT (390 children aged < 36 months) | — | — | — | — | 28.72 | — | pp –2.57, 95% CI –11.980 to 6.839 (3 years) | △ | |
| 2.5.3.2 Outcome measure: proportion severely underweight (WAZ < –3SD) | ||||||||||
| Kusuma 2017a (?) | cRCT (1394 children aged 24–36 months) | — | — | — | — | Mean 0.10 | — | DID –0.025, SE 0.024, 95% CI –0.07204 to 0.02204 | △ | |
| Kandpal 2016 (‐) | cRCT (390 children aged < 36 months) | — | — | — | — | 8.51 | — | pp 1.075, 95% CI –4.72 to 6.87, P > 0.1 (3 years) | ▽ | Yes |
| 2.5.3.3 Outcome measure: weight‐for‐age z‐score (WAZ) (mean standard deviation) | ||||||||||
| Macours 2012 (+) | cRCT (3082 children aged < 6 years) | –1.06 | — | — | –0.88 | — | — | MD 0.036, SE 0.037, 95% CI –0.037 to 0.109, P > 0.1 (9 months) | △ | Yes |
| Evans 2014 (‐) | cRCT (76 children 0–4 years) | — | — | — | — | — | — | MD –0.29, SE 1.25, 95% CI –2.74 to 2.16, P > 0.1 (1.5 years) | ▽ | |
| Kandpal 2016 (‐) | cRCT (390 children < 36 months) | — | 0.14 | — | — | — | — | MD 0.140, 95% CI –0.161 to 0.438, P > 0.1 (3 years) | △ | |
| 2.5.3.4 Outcome measure: BMI‐for‐age z‐score | ||||||||||
| Evans 2014 (‐) | cRCT (64 children aged 0–4 years) | — | — | — | — | — | — | MD –1.55, 95% CI –4.43 to 1.33, P > 0.1 (1.5 years) | ▽ | |
| 2.7 Cognitive function and development | ||||||||||
| 2.7.1 Outcome measure: cognitive test scores/cognitive and socioemotional outcomes (mean, SD) | ||||||||||
| Macours 2012 (+) | cRCT (3326 children) | — | — | — | — | — | — | MD 0.1211, SE 0.028, 95% CI 0.066 to 0.176 P < 0.01 (9 months) | ▲ | Yes |
| Baird 2013 (+) | cRCT (2057 schoolgirls) | — | — | — | — | — | — | MD 0.174, 95% CI 0.0799 to 0.268, SE 0.048, P < 0.01 (2 years) | ▲ | |
| 2.8 Change in proportion of anxiety and depression | ||||||||||
| 2.8.1 Outcome measure: proportion with psychological distress | ||||||||||
| Baird 2013 (+) | cRCT (2089 schoolgirls) | — | — | — | — | Mean 0.374, SE 0.02, P < 0.01 | — | pp –0.063, SE 0.03, P < 0.05 (1 year) | ▲ | N/A |
| — | — | — | — | Mean 0.308, SE 0.017, P < 0.01 | — | pp –0.039, SE 0.047, P > 0.1 (2 years) | △ | |||
| 2.9 Morbidity | ||||||||||
| 2.9.1 Outcome measure: proportion reporting being ill in past 4 weeks/parents seeking care for illness in past 2 weeks | ||||||||||
| Gertler 2000 (PROGRESA) (?) | cRCT (7703 children aged 0–35 months) | — | — | — | — | — | — | OR 0.777, P = 0.000 (20 months) | ▲ | Yes. Gertler subgroup 3–5 years selected as converting OR to SMD not possible due to missing group sizes. |
| cRCT (19,939 children aged 3–5 years at baseline) | 0.280 | 0.097 | — | 0.263 | 0.127 | — | Estimate –0.021, 95% CI –0.045 to 0.003 (20 months) | △ | ||
| Evans 2014 (‐) | cRCT (18,192 participants) | — | — | — | — | — | — | Estimate –0.04, 95% CI –0.099 to 0.019, P > 0.1 (32 months) | △ | |
| Kandpal 2016 (‐) | cRCT (456 children aged 6–36 months) | — | — | 229 | — | 41.85 | 227 | pp 9.830, 95% CI 0.179 to 19.481, P < 0.05 (36 months) | ▼ | |
| 2.9.2 Outcome measure: number of days ill in bed (SD) | ||||||||||
| Macours 2012 (+) | cRCT (3326 children) | — | — | — | — | 0.669 | — | MD –0.357 SD, SE 0.133, 95% CI –0.6178 to –0.096, P < 0.01 (9 months) | ▲ | |
| 2.9.3 Outcome measure: proportion with anaemia | ||||||||||
| Gertler 2000 (PROGRESA) (?) | cRCT (2010 children) | — | 0.410 | — | — | 0.483 | — | OR 0.745, P = 0.012 (20 months) | ▲ | |
aEach triangle represents one study. bValues derived from graphs
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
CI: confidence interval; cRCT: cluster randomised controlled trial; DID: difference in differences; HAZ: height‐for‐age z‐score; HDDS: Household Dietary Diversity Score; HH: household; MD: mean difference; n: number; N/A: not applicable/available; OR: odds ratio; pp: percentage point; SD: standard deviation; SE: standard error; SMD: standardised mean difference; WAZ: weight‐for‐age z‐score; WHZ: weight‐for‐height z‐score.
13. Conditional cash transfers – results of included prospective controlled studies.
| Study ID (risk of bias) | Study design (n) | Conditional cash transfers | No intervention | Effect measure (time point) | Effect directiona | Meta‐analysis (yes/no) | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | |||||
| Primary outcomes | ||||||||||
| 2.2 Proportion of HH expenditure on food | ||||||||||
| 2.2.1 Outcome measure: proportion of HH expenditure on food (weekly/monthly) | ||||||||||
| Ferre 2014 (‐) | PCS (n NR) | 3168/5548 = 0.57 | — | — | 3153/5780 = 0.55 | — | — | Proportion after study period is 337.0/378.8 = 0.89 (not impact) (13 months) | — | N/A |
| 2.3: Proportion of HHs who were food secure | ||||||||||
| 2.3.2 Dietary diversity | ||||||||||
| 2.3.2.1 Proportion with MDD | ||||||||||
| Ferre 2014 (‐) | Prospective controlled study (n = 1318 children) | 12.1 | — | — | 12.5 | — | — | MD 0.031, SE 0.05, 95% CI –0.067 to 0.129 (13 months) | △ | |
| Secondary outcomes | ||||||||||
| 2.5Change in anthropometric indicators | ||||||||||
| 2.5.1 Stunting (chronic undernutrition) | ||||||||||
| 2.5.1.1 Outcome measure: proportion stunted (HAZ < –2SD) | ||||||||||
| Ferre 2014 (‐) | Prospective controlled study (1580 children) | 47.2 | — | — | 43.3 | — | — | MD 0.034, SE 0.05, 95% CI –0.064 to 0.132 (13 months) | ▽ | Yes. Subset. (except Lopez‐Arana as OR could not be converted to SMD due to missing group sizes) |
| Andersen 2015 (‐) | Prospective controlled study (n = 188 children) | 91 (48.4%) | 72 (38.3%) | — | 80 (42.6%) | 76 (40.4%) | — | Treatment effect: –7.98, 95% CI –22.3 to 6.34, P = 0.27 (< 2 years) | △ | |
| Prospective controlled study (n = 169 children) | 101 (59.8%) | 67 (39.6%) | — | 84 (49.7%) | 81 (47.9%) | — | Treatment effect –18.3, 95% CI –38.3 to 1.59, P = 0.07 (≥ 2 years) | △ | ||
| Lopez Arana 2016 (‐) | Prospective controlled study (2874 children) | 391 (30.3%) | — | — | 442 (27.9%) | — | — | OR 0.92, 95% CI 0.82 to 1.05, P > 0.05 (4 years) | △ | |
| 2.5.1.2 Outcome measure: height‐for‐age z‐score (HAZ) (mean, SD) | ||||||||||
| Leroy 2008 (PROGRESA) (‐) | Prospective controlled study (432 children) | –1.29 (1.36) | — | — | –1.4 (1.16) | — | — | MD 0.1, 95% CI –0.086 to 0.306, P = 0.13 (2 years) | △ | Yes |
| Andersen 2015 (‐) | Prospective controlled study (n = 188 children) | –1.97 (1.1) | –1.76 (0.864) | — | –1.80 (1.02) | –1.71 (0.757) | — | MD 0.12, 95% CI –0.10 to 0.33, P = 0.28 (< 2 years) | △ | |
| Prospective controlled study (n = 169 children) | –2.11 (1.24) | –1.85 (0.829) | — | –2.08 (1.12) | –1.95 (0.813) | — | MD 0.14, 95% CI –0.20 to 0.49, P = 0.41 (≥ 2 years) | △ | ||
| Lopez Arana 2016 (‐) | Prospective controlled study (2874 children) | –1.47 (1.21) | — | — | –1.42 (1.13) | — | — | MD 0.00, 95% CI –0.10 to 0.11, P > 0.05 (4 years) | — | |
| 2.5.2:Wasting (acute undernutrition) | ||||||||||
| 2.5.2.1 Outcome measure: proportion wasted (WHZ < –2SD) | ||||||||||
| Ferre 2014 (‐) | Prospective controlled study (2244 children) | 27.8 | — | — | 22.9 | — | — | MD/DID –0.036, SE 0.04, 95% CI –0.1144 to 0.0424 (ages 22–46 months when enrolled) MD –0.125, SE 0.07, 95% CI –0.2622 to 0.0122 (aged 10–22 months when enrolled) pp –12.5 (13 months) |
△ | No. Lopez‐Arana/Ferre 2014 could not be converted to SMD due to missing group sizes. |
| Lopez Arana 2016 (‐) | Prospective controlled study (2874 children) | 25 (1.9%) | — | — | 14 (0.9%) | — | — | OR 0.25, 95% CI 0.09 to 0.74, P < 0.05 (4 years) | ▲ | |
| 2.5.2.2 Outcome measure: WHZ (mean, SD) | ||||||||||
| Leroy 2008 (PROGRESA) (‐) | Prospective controlled study (432 children) | 0.30 (1.07) | — | — | 0.33 (1.00) | — | — | MD 0.085, 95% CI –0.113 to 0.283, P = 0.2 (2 years) | △ | |
| 2.5.3 Underweight | ||||||||||
| 2.5.3.1 Outcome measure: proportion underweight (WAZ < –2SD) | ||||||||||
| Ferre 2014 (‐) | Prospective controlled study (1638 children) | 47.1 | — | — | 42.9 | — | — | MD/DID 0.046, SE 0.05, 95% CI –0.052 to 0.144 pp 4.6 (13 months) |
▽ | N/A |
| 2.5.3.2 Outcome measure: BMIZ (mean, SD) | ||||||||||
| Andersen 2015 (‐) | Prospective controlled study (n = 188 children) | 0.527 (1.15) | 0.145 (0.833) | — | 0.790 (0.986) | 0.436 (0.739) | — | MD –0.028, 95% CI –0.31 to 0.25, P = 0.84 (< 2 years) | ▽ | Yes |
| Prospective controlled study (n = 169 children) | 0.613 (1.23) | 0.248 (0.788) | — | 0.622 (1.3) | 0.622 (0.773) | — | MD –0.36, 95% CI –0.79 to 0.06, P = 0.09 (≥ 2 years) | ▽ | ||
| Lopez Arana 2016 (‐) | Prospective controlled study (2874 children) | — | — | — | — | — | — | MD 0.14, 95% CI 0.00 to 0.27, P < 0.05 (4 years) | △ | |
| 2.7 Cognitive function and development | ||||||||||
| 2.7.1 Outcome measure: language score (TVIP) (mean, SD) | ||||||||||
| Andersen 2015 (‐) | Prospective controlled study (n = 243 children) | –0.538 (0.782) | –0.718 (0.959) | — | –0.531 (0.761) | –0.552 (1.03) | — | Coefficient –0.15, 95% CI –0.37 to 0.066, P = 0.17 (≥ 2 years) | ▽ | N/A |
| 2.10: Adverse outcomes: overweight/obesity | ||||||||||
| 2.10.1 Outcome measure: overweight (BMI z‐score > –2SD) | ||||||||||
| Andersen 2015 (‐) | Prospective controlled study (n = 188 children) | n = 65, 34.6% | n = 24, 12.8% | — | n = 81, 43.1% | n = 34, 18.1% | — | pp 3.19, 95% CI –9.93 to 16.3, P = 0.63 (< 2 years) | ▽ | Yes |
| Prospective controlled study (n = 169 children) | n = 65, 37.9% | n = 28, 16.6% | — | n = 64, 37.9% | n = 42, 24.9% | — | pp –8.89, 95% CI –24.7 to 7.0, P = 0.27 (≥ 2 years); log OR –0.2784 | △ | ||
| Lopez Arana 2016 (‐) | Prospective controlled study (2874 children) | — | — | — | — | — | — | OR 1.30, 95% CI 0.83 to 2.03, P > 0.05 (4 years) | ▽ | |
| 2.10.2 Obesity | ||||||||||
| Lopez Arana 2016 (‐) | Prospective controlled study (2874 children) | 41 (3.2%) | — | — | 37 (2.3%) | — | — | OR 0.56, 95% CI 0.20 to 1.53, P > 0.05 | △ | |
aEach triangle represents one study.
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
BMIZ: body mass index‐for‐age z‐score; CI: confidence interval; DID: difference in differences; HAZ: height‐for‐age z‐score; HH: household; MD: mean difference; n: number; N/A: not applicable/available; NR: not reported; OR: odds ratio; PCS: prospective controlled study; SD: standard deviation; SE: standard error; TVIP: Test de Vocabulario en Imagenes Peabody; WAZ: weight‐for‐age z‐score; WHZ: weight‐for‐height z‐score.
6.
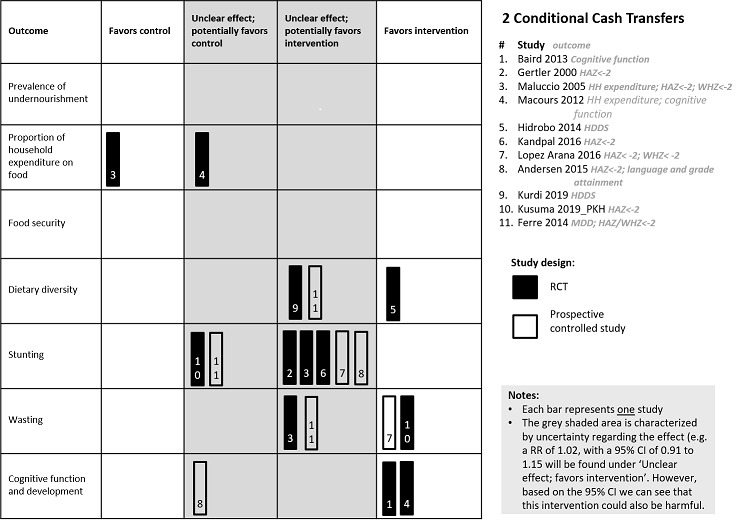
Harvest plot: conditional cash transfers.
Primary outcomes
2.1 Change in the prevalence of undernourishment
None of the included studies measured prevalence of undernourishment.
2.2 Proportion of household expenditure on food
Two cRCTs (Macours 2012; Maluccio 2005) and one PCS (Ferre 2014) reported proportion of household expenditure on food.
Randomised controlled trials
Evidence from two cRCTs indicated that CCTs result in little to no difference in the proportion of household expenditure on food (4760 households, 2 RCTs; high‐certainty evidence; Table 2). One study reported a clear effect favouring the control and one study reported an unclear effect potentially favouring the control (P = 0.125) (Figure 6). Both studies were at low overall risk of bias.
Maluccio 2005 reported clear effects favouring the control, with an increase in the proportion of household expenditure of 3.9 pp at one year (1490 households; P < 0.01) and of 4.1 pp at two years (1434 households; P < 0.01) (Table 18).
Macours 2012 reported an unclear effect potentially favouring the control because among those in the intervention group the proportion of household expenditure increased very slightly by 0.01 SDs (95% CI –0.01 to 0.02; 3326 households).
Prospective controlled studies
Ferre 2014 reported on this outcome but did not report an effect estimate (Table 19).
2.3 Proportion of households who were food secure
2.3.1 Food security
None of the studies in this comparison reported food security.
2.3.2 Dietary diversity
Randomised controlled trials
Evidence from two cRCTs indicated that CCTs probably slightly increase dietary diversity (3937 households; 2 cRCTs; moderate‐certainty evidence; Table 2; Figure 6) (Hidrobo 2014; Kurdi 2019). A meta‐analysis of these two studies, which reported FCS (scale: 0 to 112, higher score indicating better dietary diversity) showed a clear effect favouring CCTs (MD 0.45, 95% CI 0.25 to 0.65; 3937 households; I2 = 0%). Both trials were at high overall risk of bias.
Prospective controlled trials
Ferre 2014 reported an unclear effect potentially favouring CCT on the proportion of children with MDD (i.e. proportion of children aged six months and above fed from at least four food groups) (Figure 6). The proportion of children with MDD increased by 3.1 pp with CCTs compared to the control group at 13 months (MD 0.03, 95% CI –0.07 to 0.13, n = 1318) (Table 19).
Secondary outcomes
2.4 Change in adequacy of dietary intake
No included study reported the adequacy of dietary intake. Some studies reported caloric availability and intake; we have not reported these data as they do not relate to measures of adequacy.
2.5 Change in anthropometric indicators
Seven cRCTs (Evans 2014; Gertler 2000 (PROGRESA); Kandpal 2016; Kusuma 2017a; Kurdi 2019; Macours 2012; Maluccio 2005) and four PCS (Andersen 2015; Ferre 2014; Leroy 2008 (PROGRESA); Lopez Arana 2016) reported on various anthropometric measures.
2.5.1 Stunting: height‐for‐age z‐scores < –2SD (chronic undernutrition)
Cluster randomised controlled trials
Evidence from four cRCTs (Gertler 2000 (PROGRESA); Kandpal 2016; Kusuma 2017a; Maluccio 2005) showed that CCTs may make little or no difference to the proportion of stunted children (4 RCTs, 3529 children; low‐certainty evidence; Table 2). Three studies showed an unclear effect favouring CCTs and one study showed an unclear effect potentially favouring the control (P = 0.016) (Figure 6).
Gertler 2000 (PROGRESA), Kandpal 2016, and Maluccio 2005 reported an unclear effect potentially favouring CCTs. The proportion of stunted children was reduced among those receiving CCTs in these three studies; however, all the 95% CI crossed the null effect (Table 18). In Maluccio 2005, the proportion reduced by 5.3 pp at two years (95% CI –11.38 to 0.78; 722 children aged under 5 years); in Gertler 2000 (PROGRESA), the odds of children being stunted was lower by 8.6% at 1.6 years (OR 0.91; 1062 children; P = 0.495); and in Kandpal 2016 the proportion of stunted children was lower by 3.77 pp at three years (95% CI –13.83 to 6.29; 351 children younger than 36 months; P > 0.1). Kandpal 2016 also reported that, in the CCT group, the proportion of children who were severely stunted was reduced by 10.19 pp compared to the control group at three years (95% CI –18.77 to –1.61; 351 children).
Kusuma 2017a reported an unclear effect potentially favouring the control. Among children aged 24 to 36 months in the CCT group, the proportion of stunting increased by 3.5 pp (95% CI –5.5 to 12.5; 1394 children) (Table 18). This study reported a similar effect on the proportion of children who were severely stunted (HAZ < –3SD).
A meta‐analysis of three of these studies showed an unclear effect favouring CCTs (MD –2.51, 95% CI –7.78 to 2.75; 2467 children; I2 = 22%; Analysis 2.2) (Kandpal 2016; Kusuma 2017a; Maluccio 2005). The two studies that reported on the effects of CCTs on severe stunting could not be pooled due to high heterogeneity (I2 = 78%; Analysis 2.3) (Kandpal 2016; Kusuma 2017a). The cash transfer programmes evaluated in these studies are similar in the cash transfer amount and programme conditions; however, Kusuma 2017a included children aged 24 to 36 months whereas Kandpal 2016 included children under 36 months. They also differed in their overall risk of bias, with Kandpal 2016 at high and Kusuma 2017a at unclear risk.
2.2. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 2: Proportion stunted (height‐for‐age z‐score (HAZ) < ‐2SD) – RCTs
2.3. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 3: Proportion with severe stunting (HAZ < ‐3 SD) – RCTs
In addition to reporting the effects of CCTs on stunting, five cRCTs reported on mean HAZ (Evans 2014; Kandpal 2016; Kurdi 2019; Macours 2012; Maluccio 2005). A meta‐analysis of these studies indicated that CCTs improve mean HAZ (MD 0.09, 95% CI 0.04 to 0.15; 5619 children; I2 = 0%; Analysis 2.4). The follow‐up period ranged from nine months to three years. Three of the studies in this comparison were at high overall risk of bias (Evans 2014; Kandpal 2016; Kurdi 2019), and the others at low overall risk of bias. A sensitivity analysis of the studies at overall low risk of bias did not affect the results (Appendix 4) (Macours 2012; Maluccio 2005).
2.4. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 4: HAZ – RCTs
Prospective controlled studies
Three PCS reported on stunting (Lopez Arana 2016, Andersen 2015; Ferre 2014). Two reported unclear effects potentially favouring CCTs and one reported unclear effects potentially favouring the control (P = 0.047; Figure 6; Table 19). All studies were at high overall risk of bias.
Lopez Arana 2016 and Andersen 2015 reported unclear effects potentially favouring CCTs. Lopez Arana 2016 reported a reduction in stunting among 2874 children in the intervention group at four years but the CIs overlapped with the null effect (OR 0.92, 95% CI 0.82 to 1.05; P > 0.05). In Andersen 2015, there was a smaller proportion of stunted children in the intervention group, both among those receiving the intervention for less than two years (treatment effect: –7.98, 95% CI –22.3 to 6.34; 188 children; P = 0.27) as well as those receiving the intervention for longer than two years (treatment effect –18.3, 95% CI –38.3 to 1.59; 169 children; P = 0.07). Both of these studies were at high overall risk of bias.
Ferre 2014 reported unclear effects potentially favouring the control, with a higher proportion of stunted children in the CCT group by 3.4 pp at approximately one year (95% CI –6.4 to 13.2).
A meta‐analysis of two of these studies indicated an unclear effect potentially favouring CCTs (MD –5.63, 95% CI –26.59 to 15.34; 1749 children; I2 = 73%; Analysis 2.5) (Andersen 2015; Ferre 2014).
2.5. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 5: Proportion stunted (HAZ < ‐2 SD) – PCS
In addition to reporting the effects of CCTs on stunting, three PCS, all at high overall risk of bias, reported on mean HAZ (Andersen 2015; Leroy 2008 (PROGRESA); Lopez Arana 2016). The pooled analysis indicated that CCTs may or may not increase HAZ, as the effect could range from a small reduction to a significant increase in HAZ (MD 0.03, 95% CI –0.06 to 0.12; 3475 children, I2 = 0%; Analysis 2.6).
2.6. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 6: HAZ – PCS
2.5.2. Wasting: weight‐for‐height z‐scores < –2SD (acute undernutrition)
Four cRCTs (Evans 2014; Kurdi 2019; Kusuma 2017a; Maluccio 2005) and three PCS (Ferre 2014; Leroy 2008 (PROGRESA); Lopez Arana 2016) reported measures related to wasting.
Cluster randomised controlled trials
Evidence from two cRCTs indicated that CCTs may make little or no difference to wasting (2 trials, 2116 children; low‐certainty evidence; Table 2; Figure 6) (Maluccio 2005; Kusuma 2017a). A meta‐analysis showed an unclear effect favouring CCTs (MD –2.50, 95% CI –8.04 to 3.04; I2 = 70%; Analysis 2.7).
2.7. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 7: Proportion wasted (weight‐for‐height z‐score (WHZ) < ‐2 SD) – RCTs
Two other trials reported on the effects of CCTs on mean WHZ (Evans 2014; Kurdi 2019). A meta‐analysis indicated an unclear effect potentially favouring CCTs (MD 0.17, 95% CI –0.11 to 0.44; 1111 children; I2 = 0%; Analysis 2.8).
2.8. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 8: WHZ – RCTs
Prospective controlled studies
Two PCS reported on the effects of CCTs on wasting (Lopez Arana 2016; Ferre 2014). One study reported clear effects favouring CCTs and one study unclear effects potentially favouring CCTs (P = 0.125) (Figure 6; Table 19). Data could not be pooled. Both studies were at high overall risk of bias.
Lopez Arana 2016 reported a clear effect favouring CCTs. In this study the odds of wasting were reduced by 75% among children in the CCT group at four years (OR 0.25, 95% CI 0.09 to 0.74; 2874 children).
Ferre 2014 reported an unclear effect potentially favouring CCTs. The proportion of wasted children was lower in the CCT group at 13 months, by 3.6 pp for those that were aged 22 to 46 months when enrolled (MD –0.04, 95% CI –0.11 to 0.04) and by 13 pp for those aged 10 to 22 months when enrolled (MD –0.13, 95% CI –0.26 to 0.01). However, effects ranged from potential benefit to potential harm.
In addition, one PCS, at high overall risk of bias, reported an unclear effect on WHZ potentially favouring CCTs (Leroy 2008 (PROGRESA)). The mean WHZ was higher by 0.085 SDs at two years (95% CI –0.11 to 0.28; 432 children; P = 0.2).
2.5.3 Underweight
2.5.3.1 Weight‐for‐age z‐scores < –2SD)
Three cRCTs reported on the effects of CCTs on the proportion of children who were underweight (Kandpal 2016; Kusuma 2017a; Maluccio 2005). One study reported a clear effect favouring CCTs, and two studies reported unclear effects potentially favouring CCTs (Table 18). A meta‐analysis of these studies indicated that CCTs can help reduce underweight (MD –4.87, 95% CI –8.65 to –1.09; 2506 children; I2 = 0%; Analysis 2.9). The study clearly favouring CCTs was at low overall risk of bias. Two of these studies also reported the effects on severe stunting, showing the CCTs may not make a difference to this outcome (MD –1.08, 95% CI –4.73 to 2.57; 1784 children; I2 = 0%; Analysis 2.10) (Kandpal 2016; Kusuma 2017a).
2.9. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 9: Proportion underweight (weight‐for‐age z‐score (WAZ) < ‐2SD) – RCTs
2.10. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 10: Proportion severely underweight (WAZ < ‐3 SD) – RCTs
In addition, Evans 2014, Kandpal 2016, and Macours 2012 reported on the effects of CCTs on mean WAZ. The pooled analysis indicated that CCTs slightly increased WAZ by 0.04 SDs in a period ranging from nine months to three years after the intervention (MD 0.04, 95% CI –0.03 to 0.11; 3 trials, 3,548 children; I2 = 0%; Analysis 2.11). Two of these studies were at high overall risk of bias (Evans 2014; Kandpal 2016).
2.11. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 11: WAZ – RCTs
Prospective controlled studies
One PCS, at high overall risk of bias, reported an unclear effect favouring the control (Ferre 2014). The proportion of children who were underweight increased by 4.6 pp at 13 months among those in the CCT group compared to the control group, but the effects ranged from a decrease to an increase (MD 0.05, 95% CI –0.05 to 0.14; 1638 children) (Table 19).
2.5.3.2 Body mass index‐for‐age z‐score
Cluster randomised controlled trials
One cRCT at high overall risk of bias reported unclear effects on body mass index‐for‐age z‐score (BMIZ) potentially favouring the control at 1.5 years (MD –1.55, 95% CI –4.43 to 1.33; P > 0.1; 64 children aged 0 to 4 years; Table 18) (Evans 2014).
Prospective controlled studies
Two PCS, both at high overall risk of bias, reported on BMIZ, with effects ranging from unclear potentially favouring CCTs to unclear potentially favouring the control (P = 0.125) (Table 19) (Andersen 2015; Lopez Arana 2016). Studies could not be pooled due to high heterogeneity (I2 = 79%; Analysis 2.12). Both studies are at high overall risk of bias. In Lopez Arana 2016, some of the children also participated in a separate childcare supplementary nutrition programme, which could have influenced the effects of the cash transfer. This study included children aged from birth to 17 years, whereas Andersen 2015 included children aged six to 18 months only.
2.12. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 12: BMI‐for‐age z‐score – PCS
Lopez Arana 2016 reported unclear effects potentially favouring CCTs, with BMIZ increasing for children in the intervention group compared to those in the control group (MD 0.14, 95% CI 0.00 to 0.27; P < 0.05; Table 19).
Andersen 2015 reported unclear effects on BMIZ potentially favouring the control, both for those receiving the intervention for less than two years (MD –0.03, 95% CI –0.31 to 0.25, P = 0.84) and those receiving it for longer than two years (MD –0.36, 95% CI –0.79 to 0.06; P = 0.09) (Table 19).
2.6 Change in biochemical indicators
No included study addressing this comparison reported biochemical indicators.
2.7 Cognitive function and development
Two cRCTs (Baird 2013; Macours 2012) and one PCS (Andersen 2015) reported on cognitive function and development.
Cluster randomised controlled trials
Evidence from two cRCTs indicated that CCTs slightly improve cognitive function in children (2 RCTs, 5383 children; high‐certainty evidence; Table 2; Figure 6) (Baird 2013; Macours 2012). Pooled effects indicated that CCTs slightly improve different measures of cognitive function compared to control (SMD 0.13, 95% CI 0.09 to 0.18; I2 = 0%; Analysis 2.13). The measure used in Macours 2012 was a combined measure averaging the effect across two language tests, short‐ and long‐term memory tests, and two behavioural tests. Baird 2013 used the Ravens Coloured Progressive Matrices test score, which is a measure of abstract reasons in children from the age of five years. For both of these, the higher the score, the more beneficial the effect.
2.13. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 13: Cognitive test scores – RCTs
Prospective controlled studies
Andersen 2015 reported small unclear effects potentially favouring the control on the TVIP score, which is the Spanish‐speaking version of the Peabody Picture Vocabulary Test (PPVT), a test of receptive vocabulary that can be applied to children 36 months and older. The TVIP score was reduced by 0.15 SDs in the CCT group compared to the control group (MD –0.15, 95% CI –0.37 to 0.07; 243 children; P = 0.17; Table 19).
2.8 Change in proportion of anxiety or depression
One cRCT, at low overall risk of bias, reported on psychological distress, with effects ranging from clear effects favouring CCTs at one year to unclear effects potentially favouring CCTs at two years (Table 18) (Baird 2013). Psychological distress was assessed with the General Health Questionnaire 12, a tool used widely in clinical settings, in which psychological distress is a binary measure of psychological distress, anxiety and depression; social dysfunction; and loss of confidence. The study authors reported that the proportion of school girls with psychological distress reduced in the intervention group both at one year (pp –0.06; 2089 girls; P < 0.05) and at two years (pp –0.04; 2089 girls; P > 0.1). However, the change was very small and unlikely to be meaningful. This study was at low overall risk of bias.
2.9 Morbidity
Four cRCTs report on various morbidity measures (Table 18) (Evans 2014; Gertler 2000 (PROGRESA); Kandpal 2016; Macours 2012).
2.9.1 Illness
Three cRCTs reported the effects of CCTs on illness. A meta‐analysis of three of these studies indicated that CCTs may not make a difference to the proportion of people reporting being ill or that reporting seeking care for illness in the past two to four weeks (MD –0.28, 95% CI –5.92 to 5.35; 38,587 participants; Analysis 2.14).
2.14. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 14: Proportion reporting being ill in past 4 weeks/parents seeking care for illness past 2 weeks – RCTs
Macours 2012 reported a clear effect favouring CCTs on the number of days ill in bed, which was lower among children in the CCT group compared to the control by 0.357 SDs (MD –0.36, 95% CI –0.62 to –0.10; 3326 children; Table 18).
2.9.2 Anaemia
Gertler 2000 (PROGRESA) reported a clear effect favouring CCTs on anaemia. After 20 months of receiving the intervention, the odds of children being anaemic were 25.5% smaller in children receiving CCTs compared to those receiving no intervention (OR 0.75; 2010 children; P = 0.012). This study was at unclear overall risk of bias (Table 18).
2.10 Adverse outcomes (proportion of overweight/obesity)
A meta‐analysis of two PCS, both at high overall risk of bias, showed that CCTs make no difference to the proportion of overweight children aged under 18 years at two to four years of the intervention (OR 1.00, 95% CI 0.59 to 1.71; 3042 children; I2 = 60%; Analysis 2.15; Table 19) (Andersen 2015; Lopez Arana 2016).
2.15. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 15: Overweight (BMI z‐score > 2 SD)_PCS
Lopez Arana 2016 also reported on the effects of CCTs on obesity. This study reported an unclear effect favouring CCTs; the risk of obesity was reduced by 44% among children in the intervention group at four years (OR 0.56, 95% CI 0.20 to 1.53; 2874 children; P > 0.05). However, effects were uncertain as the CIs crossed the null effect.
Comparison 3: income‐generation interventions
Six cRCTs and 11 PCS assessed a variety of interventions aimed at generating income as a means to improve food security through increased economic access to food. Interventions included broad community development programmes that comprised training on livestock management, citizen empowerment, poverty alleviation delivered to women or women's self‐help groups (Darrouzet Nardi 2016; Doocy 2017; Osei 2017), training programmes to improve farming practices and sustainable agriculture (Doocy 2017; Kangmennaang 2017), and access to savings and investments and building capacity of local governance structures (Weinhardt 2017). Other interventions aimed to generate income through one‐off transfers of livestock with ongoing training (Asadullah 2015; Jodlowski 2016), and in some cases with additional intervention components such as health visits, access to community savings and technical advice (Asadullah 2015). Other studies focused on agriculture‐related interventions as a means to generate income: through an integrated agriculture and nutrition programme including training and input provision for crop farming or animal rearing (Marquis 2018; Olney 2016), development of a sustainable integrated agriculture‐aquaculture approaches (Murshed E Jahan 2011; Verbowski 2018), a sugarcane farmers scheme (Kennedy 1989), and implementation of a solar‐powered irrigation systems (Alaofe 2016; Alaofe 2019). Three PCS evaluated employment interventions, including public works programmes (Porter 2016; Beegle 2017), and part‐time employment for women (Katz 2001).
Four PCS assessed effects on food security outcomes (Asadullah 2015; Doocy 2017; Kangmennaang 2017; Weinhardt 2017). Three cRCTs (Beegle 2017; Darrouzet Nardi 2016; Olney 2016) and three PCS (Alaofe 2019; Doocy 2017; Jodlowski 2016) reported various measures of dietary diversity. Four cRCTs (Darrouzet Nardi 2016; Marquis 2018; Olney 2016; Verbowski 2018) and five PCS (Alaofe 2019; Doocy 2017; Katz 2001; Kennedy 1989; Weinhardt 2017) reported on various anthropometric measures. One cRCT (Verbowski 2018) and three PCS (Alaofe 2019; Asadullah 2015; Kennedy 1989) reported on morbidity outcomes.
Further details about the studies in this comparison are provided in Table 11. Results of individual trials included in this comparison are presented in Table 20 and PCS in Table 21. Table 3 and the harvest plot in Figure 7 summarise the effects on key outcomes.
14. Income‐generation interventions – results of included trials.
| Study ID (risk of bias) | Study design (n) | Income‐generation interventions | No intervention | Effect measure (time point) | Effect direction | Meta‐analysis (yes/no) | |||||||||||||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | ||||||||||||||||
| Primary outcomes | |||||||||||||||||||||
| 3.3 Proportion of HHs who were food secure | |||||||||||||||||||||
| 3.3.1 Food security | |||||||||||||||||||||
| 3.3.1.1 Outcome measure: proportion experiencing food security (based on HFIAS) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2614 HHs) | 79.7, 95% CI 77.2 to 82.0 | 53.6, 95% CI 51.0 to 56.1 | — | 87.4, 95% CI 85.3 to 89.3 | 78.3, 95% CI 76.0 to 80.4 | — | — (2.5 years) | — | No n for individual groups to calculate MD. | |||||||||||
| 3.3.1.2 Outcome measure: HH food security score (mean, SD) | |||||||||||||||||||||
| Beegle 2017 (‐) | RCT (2193 HHs) | — | — | 1083 HHs | — | –3.12 (1.29) | 1110 HHs | MD –0.060, SE 0.080, 95% CI –0.2168 to 0.0968 (3/4 months) | ▽ | ||||||||||||
| 3.3.1.3 Outcome measure: Resilience Index (mean, SD) | |||||||||||||||||||||
| Beegle 2017 (‐) | RCT (2195 participants) | — | — | — | — | –9.32 (9.84) | — | MD –0.224, SE 0.630 (3/4 months) | ▽ | ||||||||||||
| 3.3.1.4 Outcome measure: Principal Components Analysis index (mean, SD) | |||||||||||||||||||||
| Beegle 2017 (‐) | RCT (2123 participants) | — | — | — | — | 0.15 (2.08) | — | MD –0.029, SE 0.135 (3/4 months) | ▽ | ||||||||||||
| 3.3.2 Dietary diversity | |||||||||||||||||||||
| 3.3.2.1 Outcome measure: odds of consuming an additional food group based on the DDS | |||||||||||||||||||||
|
Darrouzet Nardi 2016 (?) (DDS 0–7) |
cRCT (2584 children) | — | — | — | — | — | — | OR 1.524, 95% CI 1.45 to 4.38, P = 0.001 (2 years) | ▲ | ||||||||||||
| 3.3.2.2 Outcome measure: HDDS (mean, SD)/Food Consumption Score | |||||||||||||||||||||
|
Olney 2016 (?) (HDDS 0–11) |
cRCT (1476 HHs) | 5.6 (1.93) | 5.6 (2.07) | 880 HHs | 5.8 (1.70) | 5.2 (2.11) | 596 HHs | MD 0.7, SE 0.44, 95% CI –0.1624 to 1.5624, P = 0.17 (2 years) | △ | Yes. SMD. | |||||||||||
|
Beegle 2017 (‐) (FCS 0–126) |
RCT (2201 HHs) | — | — | 1191 HHs | — | 38.82 (16.01) | 1110 HHs | MD –0.708, SE 1.072, 95% CI –2.80912 to 1.39312 (3/4 months) | ▽ | ||||||||||||
| 3.3.2.3 Outcome measure: MDD (n, %) | |||||||||||||||||||||
| Marquis 2018 (+) | cRCT (428 children) | 30.9 | 80.2 | 247 | 33.8 | 69.5 | 181 | OR 1.65, SE 0.41, 95% CI 0.8464 to 2.4536, P < 0.05 (12 months) | ▲ | Yes. Olney groups combined. | |||||||||||
| Darrouzet Nardi 2016 (?) | cRCT (2604 children) | — | — | — | — | — | — | OR 1.146, 95% CI 1.02 to 1.29, P = 0.021 (2 years) | ▲ | ||||||||||||
| Olney 2016 (?) | cRCT (758 children) | OWL: 7 (3.0) HC: 4 (1.7) |
OWL: 35 (15.0) HC: 43 (18.2) |
OWL: 220 HC: 231 |
8 (2.6) | 20 (6.3) | 307 | OWL villages vs control: pp 8.3, P = 0.17 HC villages vs control: pp 12.6, P = 0.08 (2 years) Combined effect: MD pp 10.08, 95% CI 1.02 to 19.14 |
▲ | ||||||||||||
| Secondary outcomes | |||||||||||||||||||||
| 3.5Change in anthropometric indicators | |||||||||||||||||||||
| 3.5.1 Stunting | |||||||||||||||||||||
| 3.5.1.1 Outcome measure: Height‐for‐Age z‐score (HAZ) (mean, SD or SE) | |||||||||||||||||||||
| Marquis 2018 (+) | cRCT (428 children) | –0.88 (1.27) | — | 247 | –0.78 (1.30) | — | 181 | MD 0.22, SE 0.06, P < 0.01, 95% CI 0.10 to 0.34 (12 months) | ▲ | No. Effect sizes calculated for Darrouzet (2 years) and Osei from group estimates. | |||||||||||
| Darrouzet Nardi 2016 (?) | cRCT (303 children) | –1.47 (0.07) | –1.38 (0.06) | — | –1.48 (0.06) | –1.41 (0.06) | — | MD 0.109, 95% CI 0.000 to 0.218, P = 0.048 (12 months) | △ | ||||||||||||
| 609 children | –1.47 (0.07) | –1.30 (0.06) | 305 | –1.48 (0.06) | –1.33 (0.06) | 304 | MD 0.03, SE 0.0049, 95% CI 0.020 to 0.040 (2 years) | ▲ | |||||||||||||
| Osei 2017 (?) | cRCT (2569 children) | –2.23 (0.03) | –2.1 (0.03) | 1299 | –2.4 (0.04) | –2.32 (0.03) | 1297 | MD 0.22, SE 0.0012, 95% CI 0.218 to 0.222 (2.5 years) | ▲ | ||||||||||||
| 3.5.1.2 Outcome measure: proportion stunted (HAZ < –2SD) (CI) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2569 children) | 57.7 | 55.1 | 1299 | 65.8 | 63.5 | 1297 | OR 0.94, 95% CI 0.74 to 1.19 (2.5 years) | △ | Yes. Verbowski groups combined | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (597 children) | 27.9 | 29.9 | 299 | 29.3 | 32.0 | 298 | MD pp –0.62, P = 0.927 (1.8 years) | MD pp 2.2, 95% CI –5.64 to 10.05 | ▽ | |||||||||||
| Verbowski 2018 (?) | cRCT (598 children) | 22.7 | 28.9 | 300 | 29.3 | 32.0 | 298 | MD pp 3.73, P = 0.453 (1.8 years) | |||||||||||||
| 3.5.2Wasting | |||||||||||||||||||||
| 3.5.2.1 Outcome measure: WHZ (mean, SD or SE) | |||||||||||||||||||||
| Marquis 2018 (+) | cRCT (428 children) | –0.37 (1.08) | — | 247 | –0.31 (1.24) | — | 181 | MD 0.07, SE 0.08, 95% CI –0.087 to 0.227, P > 0.10 (12 months) | △ | No. Effect for Osei calculated from group estimates. | |||||||||||
| Osei 2017 (?) | cRCT (2603 children) | –0.91 (0.03) | –0.85 (0.03) | 1300 | –0.93 (0.03) | –0.71 (0.03) | 1303 | MD –0.14, SE 0.0012, 95% CI –0.142 to –0.138 (2.5 years) | ▼ | ||||||||||||
| 3.5.2.2 Outcome measure: proportion wasted (WHZ < –2SD) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2603 children) | 10.6 | 10.5 | 1300 | 10.1 | 9.7 | 1303 | OR 1.03, 95% CI 0.70 to 1.52 (2.5 years) | ▽ | Yes. Verbowski groups combined. | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (597 children) | 6.7 | 10.2 | 299 | 8.3 | 8.9 | 298 | MD pp 2.75, P = 0.424 (22 months) | MD pp 3.19, 95% CI –1.95 to 8.33 | ▽ | |||||||||||
| Verbowski 2018 (?) | cRCT (598 children) | 8.4 | 13.0 | 300 | 8.3 | 8.9 | 298 | MD pp 3.80, P = 0.348 (22 months) | |||||||||||||
| 3.5.3 Underweight | |||||||||||||||||||||
| 3.5.3.1 Outcome measure: Weight‐for‐age z‐score (WAZ) (mean, SD or SE) | |||||||||||||||||||||
| Marquis 2018 (+) | cRCT (428 children) | –0.78 (1.12) | — | 247 | –0.68 (1.27) | — | 181 | MD 0.15, SE 0.07, P < 0.05 (12 months) | ▲ | Yes. Effect estimates calculated using group estimates. | |||||||||||
| Darrouzet Nardi 2016 (?) | cRCT (634 children) | –2.04 (0.07) | –1.97 (0.06) | 301 | –1.94 (0.06) | –1.89 (0.06) | 333 | NR (1 year) | — | ||||||||||||
| –2.04 (0.07) | –1.97 (0.06) | –1.94 (0.06) | –2.07 (0.06) | MD 0.10, 95% CI 0.09 to 0.11 (2 years) | ▲ | ||||||||||||||||
| Osei 2017 (?) | cRCT (2613 children) | –1.87 (0.03) | –1.77 (0.03) | 1306 | –1.97 (0.03) | –1.77 (0.03) | 1307 | MD 0.00, 95% CI –0.00 to 0.00 (2.5 years) | — | ||||||||||||
| 3.5.3.2 Outcome measure: percentage underweight (WAZ < 80% standard/ < –2SD) (includes severe underweight) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2613 children) | 43.4 | 41.0 | 1306 | 48.0 | 40.6 | 1307 | OR 1.15, 95% CI 0.91 to 1.46 (2.5 years) | ▽ | Yes. Verbowski groups combined. | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (597 children) | 23.5 | 32.0 | 299 | 23.0 | 28.8 | 298 | MD pp 2.75, P = 0.670 (22 months) | MD pp –1.16, 95% CI –9.02 to 6.70 | △ | |||||||||||
| Verbowski 2018 (?) | cRCT (598 children) | 26.1 | 28.8 | 300 | 23.0 | 28.8 | 298 | MD pp –3.63, P = 0.479 (22 months) | |||||||||||||
| 3.5.3.3 Outcome measure: BMI (kg/m2) (mean, SD or SE) | |||||||||||||||||||||
| Olney 2016 (?) | cRCT (1297 women) | 20.2 (2.22) | 20.7 (2.34) | 787 | 20.6 (2.27) | 21.1 (2.70) | 510 | MD 0.2, 95% CI –0.192 to 0.592, SE 0.20, P = 0.26 (2 years) | △ | Yes. Effect estimate for Osei calculated from group estimates. | |||||||||||
| Osei 2017 (?) | cRCT (2614 mothers) | 19.6 (0.07) | 19.8 (0.05) | 1182 | 20.1 (0.06) | 19.9 (0.05) | 1303 | MD –0.10, 95% CI –0.10 to –0.10 (2.5 years) | ▼ | ||||||||||||
| 3.5.3.4 Proportion of women who were underweight (BMI < 18.5 kg/m2) | |||||||||||||||||||||
| Olney 2016 (?) | cRCT (1297 women) | 23 | 15 | 787 | 15 | 16 | 510 | pp –8.7, P = 0.01 (2 years) | ▲ | No. Verbowski groups combined. | |||||||||||
| Osei 2017 (?) | cRCT (2614 mothers) | 28.2 | 28.6 | 1182 | 17.5 | 19.9 (0.05) | 1303 | OR 0.61, 95% CI 0.46 to 0.82 (2.5 years) | ▲ | ||||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (541 women) | 14.2 | 9.0 | 270 | 16.6 | 9.4 | 271 | MD pp 1.19, P = 0.920 (22 months) | MD 3.88, 95% CI –4.36 to 12.12 | ▽ | |||||||||||
| Verbowski 2018 (?) | cRCT (541 women) | 13.4 | 13.5 | 270 | 16.6 | 9.4 | 271 | MD pp 4.27, P = 0.347 (22 months) | |||||||||||||
| 3.6 Change in biochemical indicators | |||||||||||||||||||||
| 3.6.1 Mean haemoglobin concentration (children) (mean, SE) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2614 children) | 115.3 (0.1) | 114.3 (0.1) | 1307 | 113.6 (0.1) | 110.8 (0.1) | 1307 | MD 3.5, SE 0.0039, 95% CI 3.492 to 3.507 (2.5 years) | ▲ | Yes. Verbowski groups combined. | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (597 children) | 104.5 (13.7) | 108.4 (13.1) | 298 | 105.7 (13.6) | 107.1 (12.9) | 299 | MD 2.54, SE 1.43, P = 0.076 (22 months) | MD 2.48, 95% CI 0.51 to 4.46 | ▲ | |||||||||||
| Verbowski 2018 (?) | cRCT (597 children) | 104.1 (13.8) | 108.0 (12.3) | 298 | 105.7 (13.6) | 107.1 (12.9) | 299 | MD 2.43, SE 1.42, P = 0.088 (22 months) | |||||||||||||
| 3.6.2 Mean haemoglobin concentration (women) (mean, SD or SE) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2614 mothers) | 129.3 (0.1) | 126.5 (0.1) | 1307 | 129.6 (0.1) | 121.9 (0.1) | 1307 | MD 4.6, SE 0.0039, 95% CI 4.592 to 4.608 (2.5 years) | ▲ | Yes. Verbowski groups combined. | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (541 women) | 122.4 (12.1) | 122.9 (12.9) | 270 | 121.5 (12.5) | 121.1 (12.1) | 271 | MD 0.49, SE 1.33, P = 0.714 (22 months) | MD –0.07, 95% CI –1.92 to 1.78 | ▽ | |||||||||||
| Verbowski 2018 (?) | cRCT (541 women) | 121.7 (13.7) | 121.0 (11.9) | 270 | 121.5 (12.5) | 121.1 (12.1) | 271 | MD –0.63, SE 1.34, P = 0.637 (22 months) | |||||||||||||
| 3.9 Morbidity | |||||||||||||||||||||
| 3.9.1 Prevalence of anaemia (children) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2614 children) | 28.2 | 30.8 | 1307 | 31.6 | 42.5 | 1307 | OR 0.76, 95% CI 0.59 to 0.98 (2.5 years) | ▲ | Yes. Verbowski groups combined. | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (597 children) | 63.1 | 54.3 | 298 | 59.2 | 59.5 | 299 | MD pp –9.74, P = 0.119 (22 months) | MD pp –11.90, 95% CI –20.47 to –3.33 | ▲ | |||||||||||
| Verbowski 2018 (?) | cRCT (597 children) | 65.4 | 52.6 | 298 | 59.2 | 59.5 | 299 | MD pp –14.0, P = 0.023 (22 months) | |||||||||||||
| 3.9.2 Prevalence of anaemia (women) | |||||||||||||||||||||
| Osei 2017 (?) | cRCT (2614 mothers) | 19.6 | 24.6 | 1307 | 21.1 | 35.8 | 1307 | OR 0.62, 95% CI 0.48 to 0.82 (2.5 years) | ▲ | Yes. Verbowski groups combined. | |||||||||||
| Verbowski 2018 and aquaculture (?) | cRCT (541 women) | 38.9 | 35.8 | 270 | 40.4 | 38.7 | 271 | MD pp –1.10, P = 0.865 (22 months) | MD pp 1.34, 95% CI –7.94 to 10.61 | ▽ | |||||||||||
| Verbowski 2018 (?) | cRCT (541 women) | 41.9 | 43.5 | 270 | 40.4 | 38.7 | 271 | MD pp 4.14, P = 0.551 (22 months) | |||||||||||||
aEach triangle represents one study.
(+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias. ▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0.
BMI: body mass index; cRCT: cluster randomised controlled trial; CI: confidence interval; DDS: Dietary Diversity Score; EHFP: enhanced homestead food production; FCS: Food Consumption Score; HAZ: height‐for‐age z‐score; HC: health committee; HDDS: Household Dietary Diversity Score; HFIAS: Household Food Insecurity Score; HH: household; MD: mean difference; MDD: Minimum Dietary Diversity; n: number; NR: not reported; OR: odds ratio; OWL: older women leaders; pp: percentage point; SD: standard deviation; SE: standard error; SMD: standardised mean difference; WAZ: weight‐for‐age z‐score; WHZ: weight‐for‐height z‐score.
15. Income‐generation interventions – results of included prospective controlled studies.
| Study ID (risk of bias) | Study design (n) | Income‐generation interventions | No intervention | Effect measure (time point) | Effect of combined groups/calculated effect | Effect directiona | Meta‐analysis (yes/no) | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | ||||||
| Primary outcomes | |||||||||||
| 3.2: Proportion of HH expenditure on food | |||||||||||
| 3.2.1 Outcome measure: proportion of HH expenditure on food | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (378 HHs) | — | — | — | — | — | — | — (2 years) |
— | — | N/A |
| Alaofe 2016 (?) | Prospective controlled study (56 HHs) | — | — | — | — | — | — | — (1 year) |
— | — | |
| 3.3: Proportion of HHs who were food secure | |||||||||||
| 3.3.1 Food security | |||||||||||
| 3.3.1.1 Outcome measure: proportion experiencing food security (0 months with insufficient food in past 12 months)/ Doocy: based on HFIAS | |||||||||||
| Weinhardt 2017 (?) | Prospective controlled study (827 participants) | 165/564 (29.3%) | 309/564 (54.8%) | 564 | 71/262 (27.1%) | 117/263 (44.5%) | 263 | OR 1.36, 95% CI 0.93 to 1.97, P = 0.108 (1.5 years) | — | △ | N/A no effect measure for Doocy |
| 165/564 (29.3%) | 36 months: 308/531 (58.0%) | 71/262 (27.1%) | 129/245 (52.7%) | OR 1.12, 95% CI 0.75 to 1.67, P = 0.585 (3 years) | — | △ | |||||
| Doocy 2017 – FFS (‐) | Prospective controlled study (571 HHs) | 1.90% | 27.80% | 317 HHs | 0.40% | 14.60% | 254 HHs | — (3.5 years) | — | — | |
| Doocy 2017– WEG (‐) | Prospective controlled study (548 HHs) | 0,3% | 29.9% | 0.4% | 14.6% | — (3.5 years) | — | — | |||
| 3.3.1.2 Proportion experiencing food deficit always | |||||||||||
| Asadullah 2015 (‐) | Prospective controlled study (4038 HHs) | 60.1 | 15.3 | 2098 | 41.91 | 28.87 | 1940 | pp –28.85, P < 0.01 (3 years) | — | ▲ | — |
| 60.1 | 21.02 | 41.91 | 28.45 | pp –17.15, P < 0.01 (6 years) | — | ▲ | — | ||||
| 60.1 | 42.9 | 41.91 | 44.38 | pp –13.91, P < 0.01 (9 years) | — | ▲ | — | ||||
| 3.3.1.3 Outcome measure: HFIAS (mean, SD or SE) | |||||||||||
| Doocy 2017 – FFS (‐) | Prospective controlled study (571 HHs) | 14.4 (4.6) | 5.7 (5.1) | 317 | 14.8 (5.3) | 10.1 (6.1) | 254 | MD –4.6, 95% CI –5.0 to –4.2, P < 0.001 (3.5 years) | MD –4.23, 95% CI –4.96 to –3.49 | ▲ | No |
| Doocy 2017 – WEG (‐) | Prospective controlled study (548 HHs) | 15.3 (5.3) | 6.3 (5.5) | 294 | 14.8 (5.3) | 10.1 (6.1) | 254 | MD –3.85, 95% CI –4.26 to –3.43, P < 0.01 (3.5 years) | |||
| Kangmennaang 2017 (‐) | Prospective controlled study (1000 HHs) | 1.255 (0.029) | 1.173 (0.033) | 571 | 1.136 (0.044) | 1.359 (0.071) | 429 | MD –0.304, SE 0.095, P < 0.01 (about 2 years) | — | ▲ | |
| 3.3.1.4 Outcome measure: proportion of HHs improving a HFIAS category (95% CI) | |||||||||||
| Doocy 2017 – FFS (‐) | Prospective controlled study (571 HHs) | — | 55.3 (48.8 to 61.9) | 317 | — | 32.4 (24.6 to 40.3) | 254 | MD 22.9, 95% CI 12.7 to 33.1, P < 0.001 (3.5 years) | MD pp 24.21, 95% CI 16.67 to 31.76 | ▲ | N/A |
| Doocy 2017 – WEG (‐) | Prospective controlled study (548 HHs) | — | 59.5 | 294 | — | 31.5 | 254 | MD 25.8, 95% CI 14.6 to 36.9, P < 0.001 (3.5 years) | |||
| 3.3.2 Dietary diversity | |||||||||||
| 3.3.2.1 Outcome measure: probability weighted DDS (mean, SD) | |||||||||||
| Jodlowski 2016 (+) | Prospective controlled study (283 HHs) | — | — | 105 HHs | — | — | 178 HHs | MD –0.123, 95% CI –0.43 to 0.18, P > 0.1 (18 months) | — | ▽ | — |
| 3.3.2.2 Outcome measure: HDDS (mean, SD) | |||||||||||
| Jodlowski 2016 (+) | Prospective controlled study (283 HHs) | 5.86 (1.848) | — | 105 HHs | 5.747 (1.774) | — | 178 HHs | MD 0.267, 95% CI –0.13 to 0.66, P > 0.1 (18 months) | — | △ | Yes. (Doocy groups combined) |
| Alaofe 2019b (?) | Prospective controlled study (423 HHs) | 6.07 (1.26) | 6.50 (1.23) | 282 | 6.05 (1.26) | 6.24 (1.24) | 214 | MD 0.94, SE 0.24, 95% CI 0.4696 to 1.4104, P < 0.01 (1 year) | — | ▲ | |
| Doocy 2017 – FFS (‐) | Prospective controlled study (571 HHs) | 3.4 (1.4) | 3.4 (1.5) | 317 | 3.4 (1.5) | 4.8 (2.1) | 254 | MD 0.9, 95% CI 0.5 to 1.3, P < 0.001 (3.5 year) | MD 0.80, 95% CI 0.51 to 1.09 | ▲ | |
| Doocy 2017 – WEG (‐) | Prospective controlled study (548 HHs) | 3.4 (1.7) | 5.5 (2.2) | 294 | 3.4 (1.5) | 4.8 (2.1) | 254 | MD 0.69, 95% CI 0.27 to 1.10, P = 0.001 (3.5 year) | |||
| 3.3.2.3 Outcome measure: Women's Household Dietary Diversity Score (WDDS‐10) (mean, SD) | |||||||||||
| Alaofe 2019b (?) | Prospective controlled study (430 women) | 4.58 (1.04) | 4.91 (0.97) | 286 | 4.83 (0.97) | 4.01 (1.12) | 220 | MD 0.83, SE 0.19, P < 0.01, 95% CI 0.46 to 1.20 (1 year) | — | ▲ | — |
| 3.3.2.4 Outcome measure: proportion achieving target dietary diversity at endline according to HDDS | |||||||||||
| Doocy 2017 – FFS (‐) | Prospective controlled study (571 HHs) | 21.3 | 69.7 | 317 | 18.1 | 67.6 | 254 | MD 21.7, 95% CI 12.3 to 31.1, P < 0.001 (3.5 year) | MD 17.03, 95% CI 7.81 to 26.24 | ▲ | N/A |
| Doocy 2017 – WEG (‐) | Prospective controlled study (548 HHs) | 18.7 | 62.2 | 294 | 18.1 | 67.6 | 254 | MD 12.3, 95% CI 2.8 to 21.8, P = 0.011 (3.5 years) | |||
| 3.4 Change in adequacy of dietary intake | |||||||||||
| 3.4.1 Outcome measure: percentage of calorie‐deficient HHs (< 80% of caloric requirement/adult equivalent) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (374 HHs) | 30.7 | 28.1 | — | 30 | 28.7 | — | — (2 years) |
— | — | — |
| 3.4.2 Outcome measure: percentage of preschool‐aged children meeting caloric requirements | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (1297 children) | 69 | 66 | — | 58 | 62 | — | — (2 years) |
— | — | — |
| Secondary outcomes | |||||||||||
| 3.5Change in anthropometric indicators | |||||||||||
| 3.5.1 Stunting | |||||||||||
| 3.5.1.1 Outcome measure: HAZ (mean, SD or SE) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (746 children) | –1.34 | –1.67 | — | –1.50 | –1.76 | — | NR (2 years) |
— | — | — |
| 3.5.1.2 Outcome measure: proportion stunted (HAZ < –2SD) (CI) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (222 children) | — | 25.3 | 94 | — | 25.7 | 128 | NR (2 years) | — | — | N/A |
| Doocy 2017 – FFS (‐) | Prospective controlled study (471 children) | — | 60.2 (50.8 to 69.6) | 265 | — | 58.8 (50.1 to 67.5) | 206 | (adjusted) MD 1.4, 95% CI –10.7 to 13.6, P = 0.81 (3.5 year) | — | ▽ | |
| 3.5.2:Wasting | |||||||||||
| 3.5.2.1 Outcome measure: WHZ (mean, SD or SE) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (651 children) | –0.22 | –0.15 | — | –0.31 | –0.04 | — | NR (2 years) | — | — | — |
| 3.5.2.2 Outcome measure: proportion wasted (WHZ < –2SD) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (118 children) | — | 13.0 | 48 | — | 14.1 | 70 | NR (2 years) | — | — | — |
| 3.5.3 Underweight | |||||||||||
| 3.5.3.1 Outcome measure: WAZ (mean, SD or SE) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (198 children) | –1.03 | –1.14 | — | –1.17 | –1.10 | — | NR (2 years) | — | — | — |
| 3.5.3.2 Outcome measure: percentage underweight (WAZ < 80% standard/ < –2SD) (includes severe underweight) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (198 children) | — | 19.7 | 74 | — | 24.1 | 124 | NR (2 years) | — | — | No. Subset. Except Kennedy – effect could not be calculated. |
| Weinhardt 2017 (?) | Prospective controlled study (509 children) | 14.8% | 16.8% | 322 | 22.5% | 19.8% | 187 | OR 1.52, 95% CI 0.80 to 2.90, P = 0.205 (1.5 years) | — | ▽ | |
| Prospective controlled study (538 children) | 14.8% | 18.6% | 344 | 22.5% | 24.2% | 194 | OR 1.27, 95% CI 0.54 to 3.01, P = 0.585 (3 years) | — | ▽ | ||
| Doocy 2017 – FFS (‐) | Prospective controlled study (471 children) | — | 22.3 (14.8 to 29.8) | 265 | — | 29.8 (22.0 to 37.7) | 206 | (adjusted) MD –7.6, CI –17.7 to 2.5, P = 0.13 (3.5 year) |
— | △ | |
| 3.5.3.3 Outcome measure: BMI (kg/m2) (mean, SD or SE) | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (753 women) | — | 22.3 | — | — | 22.2 | — | NR (2 years) | — | — | No. No effect estimate for Kennedy and variance estimate cannot be calculated for Asadullah (missing group sizes) |
| Alaofe 2019b (?) | Prospective controlled study (359 women) | 23.01 (2.94) | 22.95 (3.73) | 256 | 22.03 (3.14) | 21.69 (3.24) | 167 | MD 0.43, SE 0.24, 95% CI –0.0504 to 0.8904, P < 0.1 (1 year) | — | △ | |
| Asadullah 2015 (‐) | Prospective controlled study (3547 women) | 19.0 | 18.95 | — | 19.17 | 18.98 | — | MD 0.14, P = 0.29 | — | △ | |
| 3.5.3.4 Proportion of women who were underweight (BMI < 18.5 kg/m2) | |||||||||||
| Alaofe 2019b (?) | Prospective controlled study (359 women) | 4.88 | 3.10 | 256 | 6.57 | 14.08 | 167 | MD –0.22, SE 0.27, 95% CI –0.749 to 0.309, P > 0.1 (1 year) | — | △ | — |
| 3.5.3.5 Outcome measure: mid‐upper arm circumference (mean, SD) | |||||||||||
| Katz 2001 (‐) | Prospective controlled study (718 women) | 22.8 (2.0) | — | 335 | 23.0 (2.2) | — | 383 | MD in intervention group –0.20 cm MD in control group –0.25 cm, P = 0.67 (2 years) |
— | — | — |
| 3.6 Change in biochemical indicators | |||||||||||
| 3.6.1 Proportion with iron deficiency | |||||||||||
| Alaofe 2019b (?) | Prospective controlled study (68 women) | 15.3% | 13.5% | — | 17.9% | 12.8% | — | DID –0.11, SE 0.83, 95% CI –0.94 to 0.72, P > 0.05 (1 year) | — | △ | — |
| 3.6.2 Proportion with vitamin A deficiency | |||||||||||
| Alaofe 2019b (?) | Prospective controlled study (60 women) | 14.3% | 5.8% | — | 20.2% | 10.8% | — | DID 0.54, SE 0.95, 95% CI –0.41 to 1.49, P > 0.05 (1 year) | — | ▽ | — |
| 3.9 Morbidity | |||||||||||
| 3.9.1 Outcome measure: proportion seriously ill in past year | |||||||||||
| Asadullah 2015 (‐) | Prospective controlled study (4038 HHs) | 23.38% | 15.89 | — | 24.24 | 17.17 | — | pp –1.72, P > 0.1 (3 years) | — | △ | — |
| 23.38 | 12.93 | — | 24.24 | 12.53 | — | pp –0.78, P > 0.1 (6 years) | — | △ | — | ||
| 23.38 | 22.16 | — | 24.24 | 22.37 | — | pp –0.70, P > 0.1 (9 years) | — | △ | — | ||
| 3.9.2 Outcome measure: % time ill | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (1055 children) | — | 29.8 | — | — | 31.2 | — | NR (2 years) | — | — | — |
| Prospective controlled study (420 women) | — | 23.8 | — | — | 24.3 | — | NR (2 years) | — | — | — | |
| 3.9.3 Outcome measure: % time ill with diarrhoea | |||||||||||
| Kennedy 1989 (?) | Prospective controlled study (1055 children) | — | 4.6 | — | — | 4.0 | — | NR (2 years) | — | — | — |
| 3.9.4 Prevalence of anaemia (women) | |||||||||||
| Alaofe 2019b (?) | Prospective controlled study (126 women) | 49.3% | 36.9% | — | 49% | 53.2% | — | MD –1.25, SE 0.58, 95% CI –1.83 to –0.67, P < 0.05 (1 year) | — | ▲ | — |
| 3.9.5 Prevalence of iron‐deficiency anaemia (women) | |||||||||||
| Alaofe 2019b (?) | Prospective controlled study (564 women) | 6.6% | 4.2% | — | 13.8% | 8.4% | — | MD –0.99, SE 1.40, 95% CI –2.39 to 0.41, P > 0.05 (1 year) | — | △ | — |
aEach triangle represents one study. bThis study also has a component comparing the intervention plus a working group versus a comparison group with a working group. Results are not presented here.
(+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias; ▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0.
CI: confidence interval; DDS: Dietary Diversity Score; DID: difference in differences; FFS: Farmer Field School; HAZ: height‐for‐age z‐score; HDDS: Household Dietary Diversity Score; HFIAS: Household Food Insecurity Scale; HH: household; MD: mean difference; N/A: not applicable/available; NR: not reported; OR: odds ratio; PCS: prospective controlled study; SD: standard deviation; SE: standard error; WAZ: weight‐for‐age z‐score; WEG: Women Empowerment Group; WHZ: weight‐for‐height z‐score.
7.
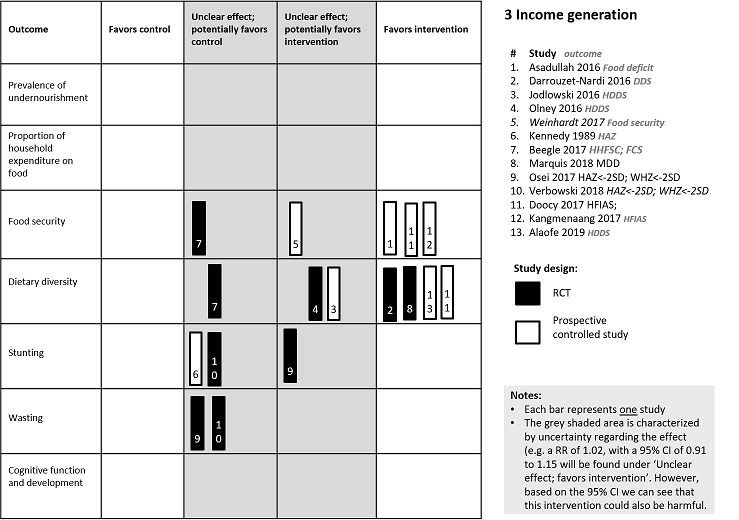
Harvest plot: income‐generation interventions.
Primary outcomes
3.1 Change in the prevalence of undernourishment
None of the included studies measured prevalence of undernourishment.
3.2 Proportion of household expenditure on food
We found no evidence about the effect of income‐generation interventions on the proportion of household expenditure on food. Although two PCS mentioned this outcome in their manuscript, they did not report relevant numerical data or indicate clearly the direction of the effect (Alaofe 2016; Kennedy 1989). Four other PCS reported total expenditure on food, not in relation to income or total expenditure and these results are thus not reported here (Asadullah 2015; Jodlowski 2016; Katz 2001; Murshed E Jahan 2011).
3.3 Proportion of households who were food secure
Two cRCTs reported the effects on food security of interventions where households received training for activities such as livestock management, aquaculture interventions and community development through women's self‐help groups (Darrouzet Nardi 2016; Osei 2017), whereas two cRCTs assessed the effects of an integrated agriculture and nutrition programme (Olney 2016; Marquis 2018). In one cRCT, households participated in a public works programme in Malawi (Beegle 2017). Six PCS assessing different interventions reported different food security or dietary diversity measures (Alaofe 2019; Asadullah 2015; Doocy 2017; Jodlowski 2016; Kangmennaang 2017; Weinhardt 2017).
3.3.1 Food security
Cluster randomised controlled trials
Evidence from one cRCT suggested that income‐generation interventions may result in little to no difference in food security of households who receive these interventions, compared to households who do not (MD –0.06, 95% CI –0.22 to 0.1; 2193 households; low‐certainty evidence; Table 3). A cRCT from Malawi showed an unclear effect potentially favouring the control on household food security scores, after three to four months (Figure 7) (Beegle 2017). One RCT did not report an overall effect estimate for the proportion of households experiencing food security (based on HFIAS) after 2.5 years, following the implementation of an agricultural and nutrition training programme in women from rural villages In Nepal (Osei 2017).
Prospective controlled studies
Three PCS reported clear effects favouring the intervention on measures of food security and one PCS reported unclear effects favouring the intervention (P = 0.01) (Figure 7).
Asadullah 2015, Doocy 2017, and Kangmennaang 2017 reported a clear effect favouring the intervention. In Asadullah 2015, among participants receiving a multicomponent intervention including training and transfer of productive assets for an income‐generation enterprise, the proportion of households that reported always experiencing a food deficit decreased compared to the control group over a period of nine years (at 3 years: pp –28.85; P < 0.01; at 6 years: pp –17.15; P < 0.0; at 9 years: pp –13.91; P < 0.01; all 4038 households). In Doocy 2017, the combined effect of both groups of the interventions (where farmer field schools and women empowerment groups in farming villages) showed a clear effect favouring the intervention, with a decrease in mean HFIAS compared to control villages not receiving any intervention (MD –4.23, 95% CI –4.96 to –3.49; 1119 households). In Kangmennaang 2017, the implementation of a training and development programme for farmers resulted in a clear effect favouring the intervention, with a decrease in mean HFIAS in intervention households compared to control households (MD –0.30; 1000 households; P < 0.01) (Table 21). These studies could not be pooled due to high heterogeneity (I2 = 99%; Analysis 3.1). Both studies are at high overall risk of bias. The interventions differed. Doocy 2017 assessed a programme including women empowerment groups, where weekly meetings and training were provided regularly as well as start‐up materials, and farmer field schools, where farmers received semi‐monthly training in farming practices as well as business and administration. Kangmennaang 2017 assessed an intervention in which farmers experimented with agroecological innovations and which also included sharing knowledge and training on various aspects including leadership.
3.1. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 1: HFIAS – PCS
Weinhardt 2017 reported an unclear effect potentially favouring the intervention. This study assessed a multilevel health and development intervention including training on farming practices, and access to VSLs groups. The odds of being food secure (i.e. household that had zero months where there was insufficient food to meet their needs in the previous 12 months) increased by 36% at 1.5 years (OR 1.36, 95% CI 0.93 to 1.97; 827 participants; P = 0.108) and 12% at three years (OR 1.12, 95% CI 0.75 to 1.67; 827 participants; P = 0.585).
3.3.2 Dietary diversity
Four cRCTs (Beegle 2017; Darrouzet Nardi 2016; Marquis 2018; Olney 2016) and three PCS (Alaofe 2019; Doocy 2017; Jodlowski 2016) reported on seven different measures of dietary diversity. Definitions and explanations of dietary diversity measures reported here are provided in Table 12.
Cluster randomised controlled trials
Evidence from four RCTs suggests that income‐generation interventions may improve dietary diversity in children and may result in little or no difference to household dietary diversity (4 cRCTs, 3677 households and 3790 children; low‐certainty evidence; Table 3). Two cRCTs reported a clear effect favouring income‐generation interventions (Darrouzet Nardi 2016; Marquis 2018), one reported an unclear effect favouring the intervention (Olney 2016), and one reported an unclear effect favouring the control group (Beegle 2017) (P = 0.047; Figure 7).
A meta‐analysis of two of these trials, assessing a public works programme in Malawi and an integrated agriculture and nutrition programme including provision of inputs and training, showed that income‐generation interventions make no difference to the HDDSs at three months to two years (SMD 0.02, 95% CI –0.09 to 0.13; 3677 households; I2 = 63%; Analysis 3.2) (Beegle 2017; Olney 2016). Beegle 2017 was at high and Olney 2016 at unclear overall risk of bias. Beegle 2017 measured dietary diversity using the FCS (scale: 0 to 126) and Olney 2016 used the HDDS (scale: 0 to 11); for both, the higher the score, the higher the food diversity. Another meta‐analysis of three of these cRCTs, assessing the implementation of women's groups, agricultural and nutritional training, and community development, showed that children in intervention households were 1.28 times more likely to achieve MDD, compared to children from control households, one to two years after the implementation of the interventions (OR 1.28, 95% CI 1.11 to 1.47; 3790 children; Analysis 3.3) (Darrouzet Nardi 2016; Marquis 2018; Olney 2016). Marquis 2018 was at low overall risk of bias and Darrouzet Nardi 2016 and Olney 2016 were at unclear overall risk of bias.
3.2. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 2: HDDS – RCTs
3.3. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 3: Minimum dietary diversity (MDD) – RCTs
Prospective controlled studies
Two PCS reported a clear effect favouring income‐generation interventions and one study reported an unclear effect potentially favouring income‐generation interventions on dietary diversity (Figure 7). A meta‐analysis of these studies indicated that income‐generation interventions increase the HDDS (MD 0.67, 95% CI 0.29 to 1.05; 1571 households; I2 = 67%; Analysis 3.4) (Alaofe 2019; Doocy 2017; Jodlowski 2016). Doocy 2017 assessed farmer field schools or women's empowerment groups at 3.5 years, Alaofe 2019 assessed the installation of a low‐pressure drip irrigation system, combined with a solar‐powered water pump in each intervention village, and Jodlowski 2016 assessed a livestock transfer with training support. All studies were at high overall risk of bias.
3.4. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 4: HDDS – PCS
Secondary outcomes
3.4 Change in adequacy of dietary intake
Prospective controlled studies
Although one PCS reported two measures of dietary intake adequacy among participants of an intervention where smallholder sugarcane growers were enrolled in a scheme to provide sugarcane to a new factory, the study authors did not report any effect measures (Kennedy 1989).
3.5 Change in anthropometric indicators
Four cRCTs (Darrouzet Nardi 2016; Olney 2016; Osei 2017; Verbowski 2018) and six PCS (Alaofe 2019; Asadullah 2015; Doocy 2017; Katz 2001; Kennedy 1989; Weinhardt 2017) reported nine different anthropometric measures in children and women.
3.5.1 Stunting: height‐for‐age z‐scores < –2SD (chronic undernutrition)
Four cRCTs (Darrouzet Nardi 2016; Osei 2017; Marquis 2018; Verbowski 2018) and two PCS (Doocy 2017; Kennedy 1989) reported on stunting.
Cluster randomised controlled trials
Evidence from two trials indicated that income‐generation interventions probably make little or no difference to wasting (2 trials, 3500 children; moderate‐certainty evidence; Table 3) (Osei 2017; Verbowski 2018). A meta‐analysis of these two studies showed no difference to stunting (OR 1.00, 95% CI 0.84 to 1.19; I2 = 0%; Analysis 3.5).
3.5. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 5: Proportion stunted (HAZ < ‐2 SD) – RCTs
In addition to reporting the proportion of children who are stunted, Marquis 2018, Darrouzet Nardi 2016, and Osei 2017 reported on the effect of income‐generation interventions on mean HAZ. Data from these studies could not be pooled due to high heterogeneity (I2 = 100%; Analysis 3.6). Marquis 2018 was at low overall risk of bias whereas Darrouzet Nardi 2016 and Osei 2017 were at unclear risk. All three studies assessed some form of training on agricultural practices or livestock management but, in all but one (Darrouzet Nardi 2016), nutrition and health education sessions were also provided, with which the most beneficial effects were observed. If this study was removed from the meta‐analysis, heterogeneity reduced to 0%. All three studies reported a clear effect favouring income‐generation interventions at 1 to 2.5 years of follow‐up. In Marquis 2018, the mean HAZ increased by 0.22 SD with the intervention at 12 months (95% CI 0.10 to 0.34; 428 children); the study assessed an integrated package of agricultural inputs and training as well as education in nutrition, health care and child stimulation for participants. In Darrouzet Nardi 2016, it increased by 0.03 SD in the intervention group, which included training for poverty alleviation, citizen empowerment, community development and optimisation of livestock management as means to generate income (95% CI 0.02 to 0.04; 609 children). However, the effect was unclear potentially favouring the intervention at one year. In Osei 2017, which assessed an enhanced homestead food production (EHFP) programme encompassing training in improved gardening and poultry‐rearing practices, among others, it increased by 0.22 SD at 2.5 years (95% CI 0.22 to 0.22; 2569 children) (Table 20).
3.6. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 6: HAZ – RCTs
Prospective controlled studies
Two PCS reported on stunting (Doocy 2017; Kennedy 1989). One study, assessing an income‐generation intervention with women's groups and farmer field schools, reported an unclear effect potentially favouring the control, with an increase in the proportion of stunted children at 3.5 years (MD 1.4, 95% CI –10.7 to 13.6; P = 0.81, 471 children) (Table 21) (Doocy 2017). The other study did report any effect measures (Kennedy 1989).
3.5.2 Wasting: weight‐for‐height z‐scores < –2SD (acute undernutrition)
Three cRCTs (Marquis 2018; Osei 2017; Verbowski 2018) and one PCS (Kennedy 1989) reported on wasting.
Cluster randomised controlled trials
Evidence indicated that income‐generation interventions probably make little or no difference to wasting (2 cRCTs, 3500 children; moderate‐certainty evidence; Table 3). A meta‐analysis of these two cRCTs showed an unclear effect potentially favouring the control, with an increased risk of wasting in children in the intervention group at two years (OR 1.13 95% CI 0.92 to 1.40; I2 = 0%; Analysis 3.7) (Osei 2017; Verbowski 2018).
3.7. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 7: Proportion wasted (WHZ < ‐2 SD) – RCTs
In addition, Marquis 2018 and Osei 2017 reported on the effects of income‐generation interventions on the mean WHZ. Data could not be pooled due to high heterogeneity (I2 = 85%; Analysis 3.8). Marquis 2018 reported a clear effect favouring the control (MD 0.07, 95% CI –0.087 to 0.227; 429 children), and Osei 2017 reported an unclear effect favouring the income‐generation intervention (MD –0.14, 95% CI –0.142 to –0.138; 2603 children) (Table 20).
3.8. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 8: WHZ – RCTs
3.5.3 Underweight
3.5.3.1 Weight‐for‐age z‐scores < –2SD
Three cRCTs (Darrouzet Nardi 2016; Marquis 2018; Osei 2017) and three PCS (Doocy 2017; Kennedy 1989; Weinhardt 2017) reported on weight‐for‐age measures.
Cluster randomised controlled trials
A meta‐analysis of two cRCTs showed that income‐generation interventions make little or no difference to the percentage of children who are underweight in households that receive the intervention compared to households that did not, after two years follow‐up (MD 1.06, 95% CI 0.89 to 1.26; 3808 children; I2 = 4%; Analysis 3.9) (Osei 2017; Verbowski 2018).
3.9. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 9: Percentage underweight – RCTs
In addition, three cRCTs reported on the effect of income‐generation interventions on WAZ (Darrouzet Nardi 2016; Marquis 2018; Osei 2017). Data could not be pooled due to high heterogeneity (I2 = 99%; Analysis 3.10). Two studies reported a clear effect favouring income‐generation interventions and Osei 2017 reported no effect at 2.5 years (MD 0.00, 95% CI –0.00 to 0.00; 2613 children).
3.10. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 10: WAZ – RCTs
Prospective controlled studies
Two studies reported on the effects of income‐generation interventions on the percentage of children who were underweight (Doocy 2017; Weinhardt 2017). A meta‐analysis of these studies showed that these interventions make no difference to the percentage of children who are underweight (OR 0.83, 95% CI 0.61 to 1.12; 909 children; I2 = 16%; Analysis 3.11). No effect measures could be calculated for Kennedy 1989.
3.11. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 11: Percentage underweight – PCS
3.5.3.2 Body mass index
Two cRCTs (Olney 2016; Osei 2017) and three PCS (Alaofe 2019; Asadullah 2015; Kennedy 1989) reported on BMI measures in women.
Cluster randomised controlled trials
Two cRCTs reported a clear effect favouring income‐generation interventions on the proportion of women who were underweight (BMI< 18.5 kg/m2) (Olney 2016; Osei 2017) and one study reported an unclear effect potentially favouring the control (Verbowski 2018) (P = 0.047). Data could not be pooled due to high heterogeneity (I2 = 80%; Analysis 3.12). Heterogeneity seemed to be driven by Verbowski 2018, which was the only study with an aquaculture component in the intervention. All three studies were a variation of the EHFP intervention, so similar in other characteristics.
3.12. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 12: Proportion of women underweight – RCTs
Olney 2016 and Osei 2017 reported a clear effect favouring income‐generation interventions. Olney 2016 reported that the proportion of underweight women in the intervention group was 8.7 pp lower compared to the control group at two years (1297 women; P = 0.01). Osei 2017 reported reduced odds of underweight among women in the intervention group by 39% at two years (OR 0.61, 95% CI 0.46 to 0.82; 2614 mothers) (Table 20). Both studies were at unclear overall risk of bias.
Verbowski 2018 reported an unclear effect potentially favouring the control, with the proportion of underweight women being higher in the intervention group by 3.88 pp (95% CI –4.36 to 12.12; 911 women) (Table 20). This study was at unclear overall risk of bias.
In addition Olney 2016 and Osei 2017 reported on the mean BMI in women. A meta‐analysis of these two cRCTs reported little or no effect on the mean BMI of women from households who received income‐generation interventions, such as integrated agriculture and nutrition programmes or community development programmes, compared to women from households who did not, after two years of follow‐up (MD –0.02, 95% CI –0.28 to 0.25; 2 RCTs, 3911 women; Analysis 3.13).
3.13. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 13: BMI – RCTs
Prospective controlled studies
One PCS reported an unclear effect on the proportion of underweight women in the villages with the intervention, compared to women from villages who did not, after one year of follow‐up (MD –0.22, 95% CI –0.75 to 0.31; 359 women) (Table 21) (Alaofe 2019).
Three studies reported on the effect on mean BMI in women. Effect measures for mean BMI could not be calculated for one PCS (Kennedy 1989). The other two studies reported an unclear effect potentially favouring the intervention (P = 0.063). Asadullah 2015 did not report the variance of effect for mean BMI of women (MD 0.14; P = 0.29). Alaofe 2019 reported an unclear effect on the mean BMI of women, favouring the intervention (the installation of solar‐powered irrigation systems), compared to the mean BMI of women from households in villages where the technology was not available, after one year of follow‐up (difference in differences (DID) 0.43, 95% CI –0.05 to 0.89; 359 women; P < 0.1).
3.5.4 Mid‐upper arm circumference
One PCS reported no difference in the mean MUAC of women who were part of an employment intervention compared to women in the control group, in Nepal at two years; the mean change in the intervention group was –0.20 cm and in the control group was –0.25 cm (718 women; P = 0.67) (Katz 2001).
3.6 Change in biochemical indicators
Two cRCTs reported biochemical indicators, such as haemoglobin levels in women and children (Osei 2017; Verbowski 2018), and one PCS reported iron and vitamin A deficiency in women (Alaofe 2019).
Cluster randomised controlled trials
A meta‐analysis of two cRCTs showed a clear effect on mean haemoglobin levels in children, favouring income‐generation interventions (MD 3.49, 95% CI 3.25 to 3.72; 2 RCTs, 3808 children; Analysis 3.14) (Osei 2017; Verbowski 2018). We could not pool the data for women due to high heterogeneity (I2 = 96%; Analysis 3.15). Osei 2017 reported a clear effect on haemoglobin levels favouring income‐generation interventions at 2.5 years (MD 4.6, 95% CI 4.59 to 4.61; 2614 mothers), whereas Verbowski 2018 reported an unclear effect potentially favouring the control (MD –0.07, 95% CI –1.92 to 1.78; 811 women) (Table 20). Both studies were at unclear overall risk of bias.
3.14. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 14: Haemoglobin concentration (children) – RCTs
3.15. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 15: Haemoglobin concentration (women) – RCTs
Prospective controlled studies
Alaofe 2019 reported unclear effects favouring the intervention (the installation of solar‐powered irrigation systems) for the proportion of women with iron deficiency (MD –0.11, 95% CI –0.94 to 0.72; 68 women; P > 0.05), and favouring the control for the proportion of women with vitamin A deficiency (MD 0.54, 95% CI –0.41 to 1.49; P > 0.05; 60 women) (Table 21).
3.7 Cognitive function and development
None of the studies included in this comparison reported cognitive function and development.
3.8 Change in proportion of anxiety or depression
None of the studies included in this comparison reported proportion of anxiety or depression.
3.9 Morbidity
Cluster randomised controlled trials
Two cRCTs report on morbidity measures, such as the prevalence of anaemia in women and children (Osei 2017; Verbowski 2018). A meta‐analysis of these showed a clear effect favouring income‐generation interventions on the proportion of children with anaemia, after two years of follow‐up (OR 0.73, 95% CI 0.61 to 0.88; 2 RCTs, 3808 children; Analysis 3.16). However, in women, these interventions resulted in an unclear effect favouring the control after follow‐up for two years (OR 1.06, 95% CI 0.82 to 1.38; 2 RCTs, 3696 women; Analysis 3.17).
3.16. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 16: Prevalence of anaemia (children) – RCTs
3.17. Analysis.

Comparison 3: Income generation (IG) versus no intervention, Outcome 17: Prevalence of anaemia (women) – RCTs
Prospective controlled studies
Three PCS reported unclear effects different morbidity measures (Alaofe 2019; Asadullah 2015; Kennedy 1989).
Asadullah 2015 reported an unclear effect potentially favouring the intervention in the proportion of household members reporting serious illness in the previous year, over nine years of the intervention, with this proportion reducing both in the intervention and the control group (3 years: pp –1.72, P > 0.1; 6 years: pp –0.78, P > 0.1; 9 years: pp –0.70, P > 0.1; 4038 households). This study is at high overall risk of bias. Kennedy 1989 reported a higher percentage of time being ill among those in the intervention group (sugarcane growers scheme) at two years; both for children (29.8% with intervention versus 31.2% with control; 1055 children) and for women (23.8 with intervention versus 24.3% with control; 420 women). In terms of the percent of time children were ill with diarrhoea, this was higher in the intervention group at two years (4.6 with intervention versus 4.0% with control; 1055 children). However, the study reported no baseline values or effect measures, which was at unclear overall risk of bias. Alaofe 2019 reported a clear effect favouring income‐generation interventions on the prevalence of anaemia in women from intervention households, compared to control households (at 1 year: MD –1.25, 95% CI –1.83 to –0.67; 126 women; P = 0.05); the effect was unclear favouring the intervention for the prevalence of iron‐deficiency anaemia in women from intervention households compared to control households (at 1 year: MD –0.99, 95% CI –2.39 to 0.41; 546 women; P > 0.05).
3.10 Adverse outcomes (proportion of overweight/obesity)
None of the studies included in this comparison reported proportion of overweight/obesity.
Comparison 4: food prices – food vouchers
Three cRCTs (Fenn 2015; Hidrobo 2014; Ponce 2017) and one RCT (Jensen 2011) reported the effects of food vouchers compared to no intervention. Food vouchers are provided to households or individuals for the purchase of food, which could be specific to particular foods or for any foods, and usually can be redeemed at specific vendors. Hidrobo 2014 provided vouchers to households, to the value of USD 40 per month, that could be redeemed at specific supermarkets in urban areas in Ecuador for nutritionally approved foods within 30 days of receiving the vouchers. Participants in this study also had to attend monthly nutrition sensitisation sessions. Fenn 2015 provided monthly fresh food vouchers with a cash value of 1500 PKR (approximately USD 14), which could be exchanged for specified fresh foods (fruits, vegetables, milk and meat) in nominated shops in Pakistan. Vouchers were distributed at specific distribution points either by mobile banks that travelled to a central location serving some of the participating villages or through central banks that served a number of villages. In Ponce 2017, households in Ecuador received a food voucher of USD 40 monthly. In Jensen 2011, a month's supply of vouchers entitled participants to a price reduction of the local staple food to the value of 750 g per person per day of that staple food. More details on these studies are available in Table 22 and in the Characteristics of included studies table.
16. Food vouchers, subsidies, social support: overview of included studies.
| Study ID (country) | Study design | Overall risk of biasa | Other key details of intervention | Population (sample size at baseline: intervention/ control) | Outcome domains and measures with available data | Timepoint of measurement |
| Comparison 4: food vouchers | ||||||
|
Fenn 2015 (Pakistan) |
cRCT | Low |
Programme name: REFANI Pakistan Intervention description and frequency: 3 intervention groups all disbursed at the same time every month for 6 consecutive months:
Provider: Action Against Hunger field staff Delivery: food vouchers disbursed monthly at distribution points. Verbal messaging from Action Against Hunger field staff at distribution that children should benefit from the transfers. Co‐interventions: WINS programme in all villages provided outpatient treatment for children aged 6 (SD 59) months with SAM, micronutrient supplementation (children, pregnant and lactating women), and behaviour change communication. |
Poor and very poor HHs in agrarian district (food voucher intervention/control: 632/632 HHs) |
Anthropometric indicators:
Biochemical indicators:
Morbidity:
|
6 and 12 months |
|
Jensen 2011 (China) |
RCT | Unclear |
Programme name: N/A Intervention description and frequency: 1‐month supply of vouchers entitling HHs to a price reduction of CNY 0.10, CNY 0.20 or CNY 0.30 (Rmb; 1 Rmb = USD 0.13) off the price of 1 jin (1 jin = 500 g) of the local staple (rice or wheat flour) to the value of 750 g per person per day. Provider: employees of the provincial‐level agencies of the Chinese National Bureau of Statistics. Delivery: printed vouchers redeemed by HHs at local grain shops. Shop owners reimbursed for the cost of the vouchers and given a fixed payment for complying with implementation guidelines. Re‐sale of vouchers or goods purchased with vouchers not permitted. Co‐interventions: NR |
Poor urban HHs (969/324) | Adequacy of dietary intake
|
6–7 months |
|
Hidrobo 2014 (Ecuador) |
cRCT | High |
Programme name: N/A Intervention description and frequency: included a CCT group (see OSIS table comparison 2) and a food voucher group. Value of USD 40 per month per HH, given in denominations of USD 20. Participants were required to attend monthly nutrition sensitisation training sessions by HH members. Provider: World Food Programme (NPO) Delivery: printed serialised vouchers redeemed at central supermarkets in urban centres for a list of nutritionally approved foods, within 30 days of receipt. Co‐interventions: NR |
Poor urban HHs (2087 HHs) | Dietary diversity:
|
7 months |
|
Ponce 2017 (Ecuador) |
cRCT | High |
Programme name: N/A Intervention description and frequency: 2 intervention groups:
Provider: NR Delivery: NR Co‐interventions: NR |
HHs based in 3 provinces in Ecuador (food voucher only group/food voucher + training on health and nutrition/control: 171/401/201 HHs) | Dietary diversity:
|
12 months |
| Comparison 5: food and nutrition subsidies | ||||||
|
Chen 2019 (China) |
cRCT | High |
Programme name: N/A Intervention description and frequency: Schools in 2 intervention groups received a one‐off nutrition subsidy with a monetary equivalent of CNY 225 (USD 33) per enrolled student. Schools could use these for nutrition‐related expenses, e.g. buying food. Schoolmasters received information about the proportion of enrolled students who were anaemic, elective methods for reducing iron‐deficient anaemia, and details about anaemia's relation with school attendance, educational performance, and cognitive development. Schoolmasters in treatment group 1 were given a general policy target of 'malnutrition reduction' and in treatment group 2 a specific policy target of 'anaemia reduction', with a potential monetary bonus tied to a reduction in anaemia prevalence (CNY 150/USD 22 per student whose anaemia status changed). Provider: project team and local government Delivery: CNY 225 (equivalent to USD 33) per student was transferred into the school's bank account. Incentive payment for treatment group 2 was only calculated and transferred after the intervention period. Co‐interventions: NR |
Primary schools in rural areas (nutritional subsidy only/nutritional subsidy + monetary incentive/control: 15/15/29 schools) | Dietary diversity:
Anthropometric indicators:
Biochemical indicators:
Morbidity:
|
6 months |
|
Andaleeb 2016 (India) |
Prospective controlled study | High |
Programme name: PDS Intervention description and frequency: universal access to the PDS. All HHs that possess a ration card were eligible for 25 kg of subsidised rice, whether they are the poorest of the poor, below the poverty line or above the poverty line. Provider: state government Delivery: a ration card was a document issued by the government which entitled an individual/family to purchase from the PDS. Ration cards classified HHs based upon their poverty status and were also used as an identity card to avail many of the other government schemes. Co‐interventions: other government schemes (not specified) |
Rural HHs (3819 HHs) | Adequacy of dietary intake
|
7 years |
|
Chakrabarti 2018 (India) |
Prospective controlled study | High |
Programme name: PDS Intervention description and frequency: subsidising a variety of pulses in different districts as part of the PDS, in addition to the usual subsidising of rice, wheat, sugar and kerosene oil. Provider: state governments (subsiding of pulses) and central Indian government (subsiding of rice, wheat, sugar and kerosene). Delivery: government‐issued ration cards are given to poor HHs enabling them to purchase from the PDS. Co‐interventions: NR |
Rural and urban HHs in selected states (23,558/101,086 HHs) | No relevant outcome measures reported | 5 years |
|
Sturm 2013 (South Africa) |
Prospective controlled study | High |
Programme name: HealthyFood Program Intervention description and frequency: provided a rebate of up to 25% on healthy food purchases in > 400 designated supermarkets across South Africa, for members of the private Discovery Health Insurance and their Vitality programme. Provider: Discovery Health Insurance company in collaboration with Pick n Pay (brand) supermarkets. Delivery: members had specific Discovery credit cards that they use for shopping. Scanner data from pay points available every time the card was swiped when purchasing certain healthy food items at Pick n Pay supermarket. These data were collated monthly. Co‐interventions: NR |
169,485 Discovery Vitality members who shopped at Pick n Pay supermarkets with linkable purchasing data (100,344 activated participants and 69,141 non‐participants, i.e. who were not actively using their benefits.) | Proportion of HH expenditure on food
|
Maximum 28 months (period November 2009 to March 2012) |
| Comparison 6: Social support interventions | ||||||
|
Kusuma 2017b (Indonesia) |
cRCT | Unclear |
Programme name: Generasi Intervention description and frequency: block payments to villages of USD 8500 (2007) and USD 18200 (2009) per village. Provider: government Delivery: trained facilitators advised village management team on allocation of funds (41% villages implemented financial incentives for health worker outreach, 79% villages implemented SFP, and 96% villages implemented financial assistance for mothers) Co‐interventions: NR |
Rural HHs 1481 children aged 24–36 months | Anthropometric indicators:
|
1 year |
|
Brunie 2014 (Mozambique) |
Prospective controlled study | High |
Programme name: VSL or a combination of VSL and Ajuda Mútua. Intervention description and frequency: VSLs are self‐managed and capitalised microfinance programmes where members pool savings and can borrow from the pool and repay with interest. Programmes work in cycles which terminate in paying out the accumulated savings and interest to members proportional to their initial deposit. The Ajuda Mútua rotating labour scheme operates with groups of HHs working together on each family's land or enterprise on a rotational basis. Provider: Save the Children (NGO) Delivery: NR Co‐interventions: SANA (Segurança Alimentar de Nutrição e Agricultura) – food security through nutrition and agriculture multiyear assistance programme targeting aspects of food utilisation. Communities are mobilised to adopt good nutrition practices, and pregnant women and carers are taught to prevent malnutrition in young children. |
Interested HHs in randomised district (VSL: 395; VSL+Ajuda Mútua: 401; control: 480) | Food security:
Dietary diversity:
Anthropometric indicators:
|
3 years |
aOverall risk of bias based on key domains: selection and attrition bias. If any of these were high, overall risk of bias was considered high.
ARI: acute respiratory infection; BMI: body mass index; BMIZ: body mass index‐for‐age z‐score; CCT: conditional cash transfer; CNY: Chinese yuan; cRCT: cluster randomised controlled trial; DDI: Dietary Diversity Index; FCS: Food Consumption Score; HAZ: height‐for‐age z‐score; Hb: haemoglobin; HDDS: Household Dietary Diversity Score; HH: household; IDDS: Individual Dietary Diversity Score; MUAC: mid‐upper arm circumference; N/A: not applicable/available; NPO: non‐profit organisation; NR: not reported; PDS: Public Distribution System; PKR: Pakistani rupee; RCT: randomised controlled trial; RDA: recommended daily allowance; SAM: severe acute malnutrition; SD: standard deviation; SFP: Supplementary Feeding Programme; VSL: village savings and loan; WAZ: weight‐for‐age z‐score; WINS: Women and Children/Infants Improved Nutrition in Sindh; WHZ: weight‐for‐height z‐score.
Hidrobo 2014 and Ponce 2017 reported dietary diversity measures. Fenn 2015 reported anthropometric measures. Jensen 2011 reported adequacy of dietary intake measures. Results from individual studies are reported in Table 23 and the harvest plot is presented in Figure 8.
17. Food vouchers – results of included trials.
| Study ID (risk of bias) | Study design (n) | Food vouchers | No intervention | Effect measure (time point) | Effect direction a | Meta‐analysis | Notes | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | ||||||
| Primary outcomes | |||||||||||
| 4.3 Proportion of HHs who were food secure | |||||||||||
| 4.3.1 Dietary diversity | |||||||||||
| 4.3.1.1 Outcome measure: Food Consumption Score (mean): different scales (out of 112 and 8) | |||||||||||
| Hidrobo 2014 (‐) | cRCT (2087 HHs) | 59.75 | — | — | 59.05 | — | — | Coefficient 9.40, 95% CI 6.6 to 12.2, P < 0.01 (7 months) | ▲ | No. SMD needed as scales are different. SMD could not be calculated due to missing group sizes for Hidrobo – MV to email authors. | SE calculated from CI |
| Ponce 2017 food voucher alone (‐) | cRCT (372 HHs) | 5.96 | NR | 171 HHs | 5.89 | NR | 201 HHs | Coefficient 0.394, SE 0.05, 95% CI 0.296 to 0.492, P < 0.01 (1 year) | ▲ | SE available | |
| Ponce 2017 food voucher + education (‐) | cRCT (602 HHs) | 5.83 | NR | 401 HHs | 5.89 | NR | 201 HHs | Coefficient 0.291, SE 0.081, P < 0.01 (1 year) | ▲ | SE available | |
| Secondary outcomes | |||||||||||
| 4.4 Change in adequacy of dietary intake | |||||||||||
| 4.4.1 Outcome measure: Mineral Sufficiency Index (mean, SD) | |||||||||||
| Jensen 2011 (?) | RCT (1265 HHs) | 1.02 (0.36) | — | 969 | 1.00 (0.34) | — | — | % change –0.061, 95% CI –0.219 to 0.098 (5 months) | ▽ | — | — |
| 4.4.2 Outcome measure: Vitamin Sufficiency Index (mean, SD) | |||||||||||
| Jensen 2011 (?) | RCT (1265 HHs) | 1.2 (0.44) | — | — | 1.17 (0.38) | — | — | % change –0.051, 95% CI –0.218 to 0.116 (5 months) | ▽ | — | — |
| 4.5 Change in anthropometric indicators | |||||||||||
| 4.5.1 Stunting | |||||||||||
| 4.5.1.1 Outcome measure: % stunted (HAZ < –2SD), n (%) | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | 473 (54.9) | NR | 834 children | 437 (51.7) | NR | 809 children | OR 0.41, 95% CI 0.25 to 0.67, P < 0.001 (6 months) | ▲ | — | — |
| Fenn 2015 (+) | cRCT (1633 children) | 473 (54.9) | NR | 818 children | 437 (51.7) | NR | 815 children | OR 0.48, 95% CI 0.31 to 0.73, P = 0.001 (12 months) | ▲ | — | — |
| 4.5.1.2 Outcome measure: % severely stunted (HAZ < –3SD) | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | NR | NR | 834 children | NR | NR | 809 children | OR 0.38, 95% CI 0.23 to 0.63, P < 0.001 (6 months) | ▲ | — | — |
| Fenn 2015 (+) | cRCT (1633 children) | NR | NR | 818 children | NR | NR | 815 children | OR 0.51, 95% CI 0.33 to 0.79, P = 0.003 (12 months) | ▲ | — | — |
| 4.5.1.3 Outcome measure: HAZ, mean (SD) | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | –2.12 (1.69) | NR | 834 children | –1.97 (1.75) | NR | 809 children | Beta‐coefficient 0.27, 95% CI 0.19 to 0.34, P < 0.001 (6 months) | ▲ | — | — |
| Fenn 2015 (+) | cRCT (1633 children) | –2.12 (1.69) | NR | 818 children | –1.97 (1.75) | NR | 815 children | Beta‐coefficient 0.29, 95% CI 0.19 to 0.40, P < 0.001 (12 months) | ▲ | — | — |
| 4.5.2 Wasting | |||||||||||
| 4.5.2.1 Outcome measure: % wasted (WHZ < –2SD), n (%) | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | 165 (19.3) | NR | 834 children | 184 (21.9) | NR | 809 children | OR 1.16, 95% CI 0.67 to 2.01, P = 0.6 (6 months) | ▽ | — | — |
| Fenn 2015 (+) | cRCT (1633 children) | 165 (19.3) | NR | 818 children | 184 (21.9) | NR | 815 children | OR 1.17, 95% CI 0.75 to 1.82, P = 0.5 (12 months) | ▽ | — | — |
| 4.5.2.2 Outcome measure: % severely wasted (WHZ) < –3SD | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | 46 (5.4) | NR | 834 children | 62 (7.4) | NR | 809 children | OR 1.27, 95% CI 0.45 to 3.55, P = 0.66 (6 months) | ▽ | — | — |
| 4.5.2.3 Outcome measure: WHZ, mean (SD) | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | –1.08 (1.14) | NR | 834 children | –1.15 (1.30) | NR | 809 children | Beta‐coefficient 0.16, 95% CI 0.05 to 0.26, P = 0.004 (6 months) | ▲ | — | — |
| Fenn 2015 (+) | cRCT (1633 children) | –1.08 (1.14) | NR | 818 children | –1.15 (1.30) | NR | 815 children | Beta‐coefficient 0.02, 95% CI –0.10 to 0.14, P = 0.79 (12 months) | △ | — | — |
| 4.5.3 Underweight | |||||||||||
| 4.5.3.1 Outcome measure: MUAC, mean (SD) | |||||||||||
| Fenn 2015 (+) | cRCT (1643 children) | 13.8 (1.2) | NR | 834 children | 13.5 (1.2) | NR | 809 children | Beta‐coefficient –0.05, 95% CI –0.14 to 0.04, P = 0.27 (6 months) | — | — | — |
| Fenn 2015 (+) | cRCT (1204 women) | 25.2 (3.2) | NR | 603 mothers | 24.3 (3.2) | NR | 601 mothers | Beta‐coefficient –0.16, 95% CI –0.38 to 0.05, P = 0.14 (6 months) | — | — | — |
| 4.5.3.2 Outcome measure: BMI, mean (SD) | |||||||||||
| Fenn 2015 (+) | cRCT (1204 women) | 20.8 (18.5 ± 24.0) | NR | 603 mothers | 20.0 (18.1 ± 22.7) | NR | 601 mothers | Beta‐coefficient 0.29, 95% CI 0.03 to 0.54, P = 0.03 (6 months) | — | — | — |
aEach triangle represents one study.
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
CI: confidence interval; cRCT: cluster randomised controlled trial; FCS: Food Consumption Score; HAZ: height‐for‐age z‐score; HH: household; MUAC: mid‐upper arm circumference; n: number; NR: not reported; OR: odds ratio; RCT: randomised controlled trial; SD: standard deviation; SE: standard error; SMD: standardised mean difference.
8.
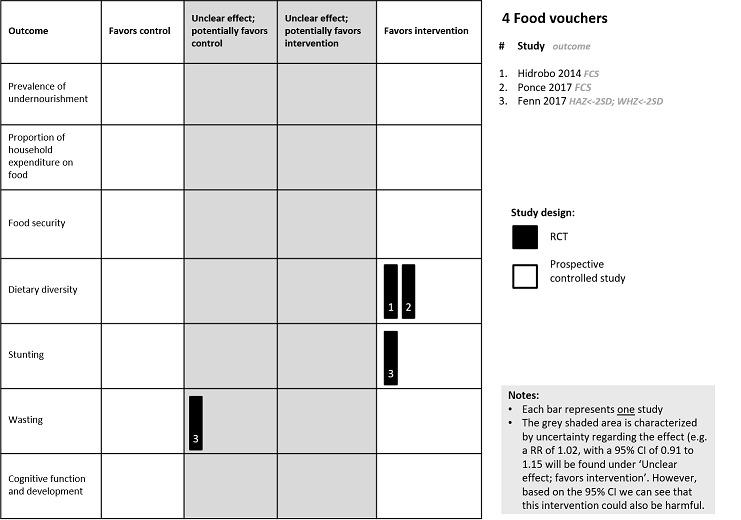
Harvest plot: food vouchers.
Primary outcomes
4.1 Change in the prevalence of undernourishment
None of the included trials reported prevalence of undernourishment.
4.2 Proportion of household expenditure on food
None of the included trials reported household expenditure on food.
4.3 Proportion of households who were food secure
4.3.1 Dietary diversity
Evidence from two trials reported that food vouchers may improve dietary diversity slightly (2 RCT, 2459 households; low‐certainty evidence; Table 4) (Hidrobo 2014; Ponce 2017). Both studies reported clear effects favouring the intervention (P = 0.063; Figure 8).
In Hidrobo 2014, at seven months, among households in the food voucher group the FCS was higher by 9.4 points (out of maximum score of 112) (95% CI 6.6 to 12.2; 2087 households; P < 0.01). Other measures of dietary diversity reported in Hidrobo 2014 also indicate clear effects favouring food vouchers (Table 23). In Ponce 2017, the FCS increased by 0.39 points in the intervention group (95% CI 0.30 to 0.49). Pooled analysis was not possible because numbers per group were not reported for Hidrobo 2014 and thus SMD could not be calculated (Analysis 4.1). Both studies were at high overall risk of bias.
4.1. Analysis.

Comparison 4: Food vouchers vs no intervention, Outcome 1: Food consumption score
Secondary outcomes
4.4 Change in adequacy of dietary intake
Jensen 2011 reported an unclear effect potentially favouring the control on the mineral and vitamin sufficiency indices (Table 23). These indices reflect the mean intake per person relative to the Dietary Reference Intake (DRI). Among households in the intervention group, there was a reduction in the mineral sufficiency index compared to the control group (percentage change –0.06, 95% CI –0.22 to 0.10), and a reduction in the vitamin sufficiency index (percentage change –0.05, 95% CI –0.22 to 0.12) at five months. However, the CIs crossed the null. This study was at low overall risk of bias.
4.5 Change in anthropometric indicators
One cRCT reported on stunting, wasting and underweight (Fenn 2015). This study was at low overall risk of bias.
4.5.1 Stunting: height‐for‐age z‐scores < –2SD
Fenn 2015 reported that food vouchers probably reduce stunting (1 trial; moderate‐certainty evidence; Table 4). At 12 months' follow‐up, the odds of stunting was 52% less in the food voucher group compared to control. This study reported a similar effect on other measures of stunting; it reported a reduction in the proportion of children who are severely stunted (OR 0.51, 95% CI 0.33 to 0.79; 1633 children), and an increase in the mean HAZ at 12 months (MD 0.29, 95% CI 0.19 to 0.40; 1633 children; Table 23).
4.5.2 Wasting: weight‐for‐height z‐scores < –2SD
Fenn 2015 reported that food vouchers may result in little to no difference in wasting (1 trial, 1633 children; low‐certainty evidence; Table 4). At 12 months of follow‐up, it reported an unclear effect potentially favouring the control (Figure 8); the odds of stunting were 17% higher in the food voucher group compared to the control; however, this effect ranged from 25% reduction to an 82% increased odds of stunting. Similar effects are reported for severe wasting at six months (OR 1.27, 95% CI 0.45 to 3.55; 1643 children); however, for mean WHZ they reported unclear effect favouring the food vouchers at 12 months (coefficient 0.02, 95% CI –0.1 to 0.14; 1633 children; Table 23).
4.5.3 Underweight
Fenn 2015 reported two different measures of underweight. In children, it reported an unclear effect on MUAC at six months (MD –0.05, 95% CI –0.14 to 0.04; 1643 children). In mothers, they reported a clear effect on BMI favouring food vouchers (MD 0.29 kg/m2, 95% CI 0.03 to 0.54; 1204 mothers; Table 23).
4.6 Change in biochemical indicators
None of the included trials reported biochemical indicators.
4.7 Cognitive function and development
None of the included trials reported cognitive function and development.
4.8 Change in proportion of anxiety or depression
None of the included trials reported proportion of anxiety or depression.
4.9 Morbidity
None of the included trials reported morbidity.
4.10 Adverse outcomes (proportion of overweight/obesity)
None of the included trials reported proportion of overweight/obesity.
Comparison 5: food prices – food and nutrition subsidies
One cRCT (Chen 2019) and three PCS (Andaleeb 2016; Chakrabarti 2018; Sturm 2013) assessed the effects of food and nutrition subsidies. These interventions aim to address rising food prices by reducing the price of the foods for the consumer, and are usually provided by the government. Chen 2019 assessed the provision of a one‐off nutrition subsidy with a monetary equivalent of CYN 225 (USD 33) per enrolled student to schools in China, which they could use for nutrition‐related expenses (e.g. buying food). Schoolmasters received information about the proportion of enrolled students who were anaemic; elective methods for reducing iron‐deficient anaemia; and details about anaemia's relation with school attendance, educational performance, and cognitive development. Andaleeb 2016 assessed the public distribution system (PDS) in India, in which households with a ration card were eligible for 25 kg of subsidised rice. A ration card was a document issued by the government which entitled an individual/family to purchase from the PDS, and which was also used as an identity card for other government schemes. Chakrabarti 2018 also assessed the PDS in India, but this study subsidised a variety of pulses in different districts as part of the PDS, in addition to the usual subsidising of rice, wheat, sugar and kerosene oil. Sturm 2013 assessed cash rebates on food purchases. It reports on the HealthyFood programme, which provides a rebate between 10% and 25% on healthy food purchases in designated supermarkets in South Africa for members of the Vitality programme of Discovery Health Insurance scheme. More details about this study are available in Table 17 and in the Characteristics of included studies table.
Chen 2019 reported on dietary diversity, anthropometric, biochemical and morbidity measures. Sturm 2013 reported on the proportion of household expenditure on food. Andaleeb 2016 reported on adequacy of dietary intake. Although Chakrabarti 2018 reported food security, dietary diversity and the proportion of household expenditure on food, it did not report any relevant measure under any of these outcome domains.
Further details of these studies are presented in Table 22. Results of included trials are presented in Table 24 and PCS in Table 25. The harvest plot is presented in Figure 9.
18. Food and nutrition subsidies – results of included trials.
| Study ID (risk of bias) | Study design (n) | Food rebate/subsidy | No intervention | Effect measure (timepoint) | Effect direction | Meta‐analysis | ||||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | |||||||
| Primary outcomes | ||||||||||||
| 5.3 Proportion of HHs who were food secure | ||||||||||||
| 5.3.1 Dietary diversity | ||||||||||||
| 5.3.1.1 Outcome measure: DDS for nutrition subsidy only (general target: malnutrition reduction) group vs control (mean, SD) | ||||||||||||
|
Chen 2019 – nutrition subsidy (‐) DDS 0–10 |
cRCT (656 students) | 4.75 (2.17) | 5.21 (2.18) | 219 students | 5.33 (2.32) | 4.82 (2.36) | 437 students | MD 0.956, robust SE 0.255, 95% CI 0.4562 to 1.4558, P < 0.01 (6 months) | ▲ | N/A | ||
| Chen 2019 – nutrition subsidy+monetary incentive (‐) | cRCT | 4.65 (2.20) | 5.32 (2.09) | 210 students | 5.33 (2.32) | 4.82 (2.36) | 437 students | Mean score 1.263, robust SE 0.224, P < 0.01 (6 months) | ▲ | |||
| Secondary outcomes | ||||||||||||
| 5.5 Change in anthropometric indicators | ||||||||||||
| 5.5.1 Outcome measure: BMI‐for‐age z‐score (mean, SD) | ||||||||||||
| Chen 2019 – nutrition subsidy (‐) | cRCT | –0.70 (0.91) | –0.71 (0.95) | 219 students | –0.68 (0.94) | –0.76 (0.97) | 437 students | Mean score 0.080, robust SE 0.058 No significant difference from control (6 months) |
△ | N/A | ||
| Chen 2019 – nutrition subsidy+monetary incentive (‐) | cRCT | –0.63 (0.91) | –0.60 (0.89) | 210 students | –0.68 (0.94) | –0.76 (0.97) | 437 students | Mean score 0.123, robust SE 0.047, P < 0.01 (6 months) | ▲ | |||
| 5.5.2 Outcome measure: proportion underweight (mean, SD) | ||||||||||||
| Chen 2019 – nutrition subsidy (‐) | cRCT | 0.07 (0.25) | 0.07 (0.26) | 219 students | 0.08 (0.26) | 0.11 (0.32) | 437 students | Mean proportion –0.032, robust SE 0.024, 95% CI –0.079 to 0.015 (6 months) | △ | N/A | ||
| Chen 2019 – nutrition subsidy+monetary incentive (‐) | cRCT | 0.06 (0.24) | 0.06 (0.23) | 210 students | 0.08 (0.26) | 0.11 (0.32) | 437 students | Mean proportion –0.041, robust SE 0.022, 95% CI –0.084 to 0.002 (6 months) | △ | |||
| 5.6 Change in biochemical indicators | ||||||||||||
| 5.6.1 Outcome measure: haemoglobin concentration in children in nutrition subsidy only (general target: malnutrition reduction) group vs control (mean, SD) | ||||||||||||
| Chen 2019 – nutrition subsidy (‐) | cRCT | 128.51 (12.63) | 128.11 (15.86) | 219 students | 128.03 (12.95) | 127.93 (14.86) | 437 students | Mean concentration 0.512, robust SE 1.348, 95% CI –2.130 to 3.154 (6 months) | △ | N/A | ||
| Chen 2019 – nutrition subsidy+monetary incentive (‐) | cRCT | 127.84 (12.80) | 130.95 (15.66) | 210 students | 128.03 (12.95) | 127.93 (14.86) | 437 students | Mean concentration 4.490, robust SE 1.241, 95% CI 2.058 to 6.922, P < 0.01 (6 months) | ▲ | |||
| 5.9 Morbidity | ||||||||||||
| 5.9.1 Outcome measure: proportion of anaemic children in nutrition subsidy only (general target: malnutrition reduction) group vs control (mean, SD) | ||||||||||||
| Chen 2019 – nutrition subsidy (‐) | cRCT | 0.18 (0.38) | 0.22 (0.42) | 219 students | 22 (0.42) | 0.23 (0.42) | 437 students | Mean proportion –0.005, robust SE 0.048, 95% CI –0.099 to 0.089, P > 0.01 (6 months) | △ | N/A | ||
| Chen 2019 – nutrition subsidy+monetary incentive (‐) | cRCT | 0.23 (0.42) | 0.16 (0.36) | 210 students | 0.22 (0.42) | 0.23 (0.42) | 437 students | Mean proportion –0.120, robust SE 0.046, 95% CI –0.210 to –0.029, P < 0.01 (6 months) | ▲ | |||
cRCT: cluster randomised controlled trial; DDS: Dietary Diversity Score; MD: mean difference; n: number; N/A: not applicable/available; SD: standard deviation; SE: standard error.
19. Food and nutrition subsidies – results of included prospective controlled studies.
| Study ID (risk of bias) | Study design (n) | Food rebate | No intervention | Effect measure (time point) | Effect directiona | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | ||||
| Primary outcomes | |||||||||
| 5.2 Proportion of HH expenditure on food | |||||||||
| 5.2.1 Outcome measure: ratio of healthy to total food expenditure (mean, SD) | |||||||||
| Sturm 2013 – 10% rebate (‐) | Prospective controlled study (169,485 HHs) | 0.21 (0.11) | — | 67,343 HHs | 0.17 (0.13) | — | 69,141 HHs | Increase by 6.0%, 95% CI 5.3% to 6.8% (3 years) | ▲ |
| Sturm 2013 – 25% rebate (‐) | Prospective controlled study (136,484 HHs) | 0.21 (0.12) | — | — | 0.17 (0.13) | — | — | Increase by 9.3%, 95% CI 8.5% to 10.0% (2 years and 4 months) | ▲ |
| 5.4 Change in adequacy of dietary intake | |||||||||
| 5.4.1 Outcome measure: ratio of current caloric intake to the RDA (multiplied by 100) | |||||||||
| Andaleeb 2016 (‐) | Controlled before‐after study | NR | NR | 1134 HHs | NR | NR | NR | DID estimate 2.55, SE 1.31, 95% CI –0.018 to 5.118, P < 0.1 (7 years) | △ |
| 5.4.2 Outcome measure: ratio of current protein intake to the RDA (multiplied by 100) | |||||||||
| Andaleeb 2016 (‐) | Controlled before‐after study | NR | NR | 1134 HHs | NR | NR | NR | DID estimate 3.75, SE 1.65, 95% CI 0.516 to 6.984, P < 0.05 (7 years) | ▲ |
| 5.4.3 Outcome measure: ratio of current fat intake to the RDA (multiplied by 100) | |||||||||
| Andaleeb 2016 (‐) | Controlled before‐after study | NR | NR | 1134 HHs | NR | NR | NR | DID estimate –0.1, SE 0.00, P > 0.1 (7 years) | ▽ |
aEach triangle represents one study.
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
CI: confidence interval; DID: difference in differences; HH: household; n: number; NR: not reported; RDA: recommended daily allowance; SD: standard deviation; SE: standard error.
9.
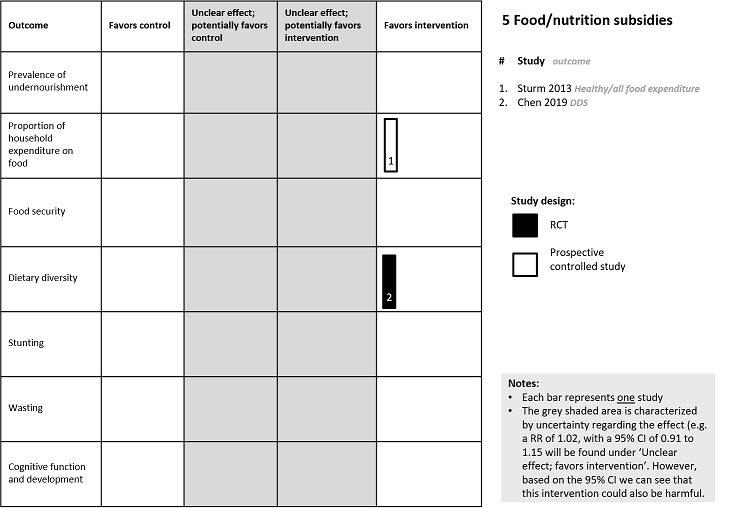
Harvest plot: food and nutrition subsidies.
Primary outcomes
5.1 Change in the prevalence of undernourishment
None of the included studies measured prevalence of undernourishment.
5.2 Proportion of household expenditure on food
Evidence from one study was very uncertain about the effects of food rebates on household expenditure on healthy foods (1 study, 169,485 households; very low‐certainty evidence; Table 5) (Sturm 2013). This study reported clear effects favouring cash rebates on proportion of healthy to total household food expenditure (Figure 9). The study authors reported that food rebates increased the ratio of healthy to total food expenditure: the 10% rebated increased it by 6% at three years (95% CI 5.3 to 6.8; 169,485 households), and the 25% rebate increased it by 9.3% at two years and four months (95% CI 8.5 to 10.0; 136,484 households) (Table 25). This study was at high overall risk of bias due to high risk of selection bias.
5.3 Proportion of households who were food secure
One cRCT reported the effects of nutrition subsidies on dietary diversity (Chen 2019).
5.3.1 Dietary diversity
Evidence from one trial indicated that nutrition subsidies may improve dietary diversity among school children (1 RCT, 656 children; low‐certainty evidence; Table 5) (Chen 2019). This study reported a clear effect favouring nutrition subsidies (Figure 9); at six months, the dietary diversity score of school children in the subsidy group increased 0.956 points more (almost one more food group) more than in the control group (MD 0.96, 95% CI 0.46 to 1.45). This study was at high overall risk of bias.
Secondary outcomes
5.4 Change in adequacy of dietary intake
Andaleeb 2016 reported on the adequacy of dietary intake for energy, protein and fat (Table 25). At seven years, it reported a clear effect favouring food subsidies for the ratio of protein intake to the recommended daily allowance (RDA) (DID 3.75, 95% CI 0.52 to 6.98; n = NR), an unclear effect potentially favouring food subsidies for the ratio of current caloric intake to the RDA (DID 2.55, 95% CI –0.02 to 5.12; n = NR), and unclear effects potentially favouring the control on the ratio of fat intake to the RDA (DID –0.1, SE 0.00; P > 0.1).
5.5 Change in anthropometric indicators
Chen 2019 reported on anthropometric indicators.
5.5.1 Underweight (body mass index z‐score < –2SD)
Chen 2019 reported an unclear effect potentially favouring nutrition subsidies (Table 24). The proportion of underweight children reduced in the schools receiving the nutrition subsidy by 3.2 pp compared to the control schools; however, the CIs crossed the null (MD –0.03, 95% CI –0.08 to 0.02, 656 children). There was a similar effect in mean BMIZ (Table 24). In the group where a monetary incentive was provided if the school achieved the desired targets, the effect was similar for the proportion of children who were underweight, but it clearly favoured nutrition subsidies for BMIZ. This study was at high overall risk of bias.
5.6 Change in biochemical indicators
5.6.1 Haemoglobin
Chen 2019 reported an unclear effect potentially favouring the intervention at six months on the mean concentration of haemoglobin in school children (MD 0.51, 95% CI –2.13 to 3.15; n = 656; Table 24). Adding a monetary incentive resulted in a clear effect favouring nutrition subsidies (MD 4.49, 95% CI 2.06 to 6.92).
5.7 Cognitive function and development
None of the included studies measured cognitive function and development.
5.8 Change in proportion of anxiety or depression
None of the included studies measured anxiety or depression.
5.9 Morbidity
5.9.1 Anaemia
Chen 2019 reported an unclear effect potentially favouring nutrition subsidies on the proportion of school children with anaemia at six months (MD –0.005, 95% CI –0.1 to 0.09). Adding a monetary incentive resulted in a clear effect favouring nutrition subsidies (Table 24). This study was at high overall risk of bias.
5.10 Adverse outcomes (proportion of overweight/obesity)
None of the included studies measured overweight/obesity.
Comparison 6: social support
Two included studies assessed social support interventions. One cRCT in Indonesia randomised subdistricts to receive a community cash grant or to a control group, which were linked to health and education conditionalities (Kusuma 2017b). Two intervention groups were implemented, one with and one without a performance incentive, but the effect of both is reported together. One PCS randomised households either to a VSL group or to a VSL and Ajuda Mutua (AM) group, or to a control group (Brunie 2014). VSLs are self‐managed and capitalised microfinance programmes where members pool savings and can borrow from the pool and repay with interest. AM is a rotating labour scheme, where groups of households work together on each family's land or enterprise on a rotational basis. A combined effect of both groups is reported.
Kusuma 2017b reported effects on anthropometric indicators, and Brunie 2014 reported effects on measures of food security, dietary diversity and anthropometry.
Further details about these studies are presented in Table 22 and in the Characteristics of included studies table. Results from these studies are presented in Table 26 and Table 27, and in the harvest plot in Figure 10.
20. Social support interventions – results of included trials.
| Study ID (risk of bias) | Study design (n) | Village savings/grants | No intervention | Effect measure (time point)a | Effect direction | ||||
| Results at baseline | Results at follow‐up | n | Results at baseline | Results at follow‐up | n | ||||
| Secondary outcomes | |||||||||
| 6.5 Change in anthropometric indicators | |||||||||
| 6.5.1 Stunting | |||||||||
| 6.5.1.1 Outcome measure: proportion stunted (HAZ < –2SD) | |||||||||
| Kusuma 2017b (?) | cRCT (1481 children aged 24–36 months) | — | — | — | — | Mean 0.48 | — | DID 0.034, SE 0.055, 95% CI –0.074 to 0.142, P > 0.05 (2 years) | ▽ |
| 1.1.2 Outcome measure: proportion severely stunted (HAZ < –3SD) | |||||||||
| Kusuma 2017b (?) | cRCT (1481 children aged 24–36 months) | — | — | — | — | Mean 0.29 | — | DID –0.06, SE 0.053, 95% CI –0.164 to 0.044, P > 0.05 (2 years) | △ |
| 6.5.2 Wasting | |||||||||
| 6.5.2.1 Outcome measure: proportion wasted (WHZ < –2SD) | |||||||||
| Kusuma 2017b (?) | cRCT (1481 children aged 24–36 months) | — | — | — | — | Mean 0.19 | — | DID –0.010, SE 0.035, 95% CI –0.079 to 0.059 pp –1.0, 95% CI –7.86 to 5.86, P > 0.05 (2 years) |
△ |
| 6.5.2.2 Outcome measure: proportion severely wasted (WHZ < –3SD) | |||||||||
| Kusuma 2017b (?) | cRCT (1481 children aged 24–36 months) | — | — | — | — | Mean 0.10 | — | DID –0.021, SE 0.025, 95% CI –0.07 to 0.028, P > 0.05 (2 years) | △ |
| 6.5.3 Underweight | |||||||||
| 6.5.3.1 Outcome measure: proportion underweight (WAZ < –2SD) | |||||||||
| Kusuma 2017b (?) | cRCT (1481 children aged 24–36 months) | — | — | — | — | Mean 0.34 | — | Beta –0.020, SE 0.051, 95% CI –0.120 to 0.080, P > 0.05 (2 years) | △ |
| 6.5.3.2 Outcome measure: proportion severely underweight (WAZ < –3SD) | |||||||||
| Kusuma 2017b (?) | cRCT (1481 children aged 24–36 months) | — | — | — | — | Mean 0.12 | — | Beta –0.056, SE 0.034, 95% CI –0.123 to 0.011, P < 0.1 (2 years) | △ |
aEach triangle represents one study.
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
DID: difference in differences; HAZ: height‐for‐age z‐score; n: number; pp: percentage point; SD: standard deviation; SE: standard error; WAZ: weight‐for‐age z‐score; WHZ: weight‐for‐height z‐score.
21. Social support interventions – results of included prospective controlled studies.
| Study ID (risk of bias) | Study design (n) | Village savings/grants | No intervention | Effect measure (time point)a | Combined group effect | Effect direction | Meta‐analysis | ||||
|
Results at baseline |
Results at follow‐up |
n |
Results at baseline |
Results at follow‐up |
n | ||||||
| Primary outcomes | |||||||||||
| 6.3 Proportion of HH who were food secure | |||||||||||
| 6.3.1 Food security | |||||||||||
| 6.3.1.1 Outcome measure: self‐reported months of food sufficiency in previous year (mean, SD) | |||||||||||
| Brunie 2014 – VSL (‐) | Prospective controlled study (851 HHs) | 10.41 | 10.52 | — | 10.58 | 10.21 | — | DID estimate 0.47, 95% CI –0.04 to 0.98, P < 0.1 (3 years) | MD 1.25, 95% CI –0.28 to 2.79 | △ | N/A |
| Brunie 2014 – VSL+AM (‐) | 836 HHs | 9.27 | 11.18 | — | 10.47 | 10.35 | — | DID estimate 2.04, 95% CI 1.53 to 2.55, P < 0.1 (3 years) | ▲ | ||
| 6.3.2 Dietary diversity | |||||||||||
| 6.3.2.1 Outcome measure: HDDS (mean, SD) | |||||||||||
| Brunie 2014 – VSL (‐) | Prospective controlled study (802 HHs) | 4.06 | 5.44 | — | 3.73 | 4.84 | — | DID estimate 0.27, 95% CI –0.16 to 0.70, P > 0.1 (3 years) | MD –0.30, 95% CI –1.46 to 0.87 | △ | N/A |
| Brunie 2014 – VSL+AM (‐) | 813 HHs | 4.2 | 4.56 | — | 3.82 | 5.11 | — | DID estimate −0.92, 95% CI –1.567 to –0.273, P < 0.001 | ▽ | ||
| 6.3.2.2 Outcome measure: IDDS (mean, SD) | |||||||||||
| Brunie 2014 – VSL (‐) | Prospective controlled study (542 children) | 2.51 | 3.43 | — | 2.87 | 2.97 | — | DID estimate 0.81, 95% CI 0.36 to 1.26, P < 0.01 (3 years) | MD 0.52, 95% CI –0.18 to 1.23 | ▲ | N/A |
| Brunie 2014 – VSL+AM (‐) | (579 children) | 2.99 | 3.46 | — | 2.82 | 3.22 | — | DID estimate 0.07, 95% CI –0.7532 to 0.8932, P > 0.01 (3 years) | △ | ||
| Secondary outcomes | |||||||||||
| 6.5 Change in anthropometric indicators | |||||||||||
| 6.5.1 Outcome measure: weight‐for‐age z‐scores (WAZ) | |||||||||||
| Brunie 2014 – VSL (‐) | Prospective controlled study (503 children) | –1.21 | –0.91 | — | –1.25 | –0.83 | — | DID estimate –0.11, 95% CI –0.561 to 0.341, P > 0.1 (3 years) | MD 0.05, 95% CI –0.37 to 0.48 | ▽ | N/A |
| Brunie 2014 – VSL+AM (‐) | (550 children) | –0.96 | –0.93 | — | –1.15 | –0.78 | — | DID estimate 0.34, 95% CI –0.31 to 0.99, P > 0.01 | △ | ||
aEach triangle represents one study.
▲ = Favours the intervention, 95% CI excludes 0; △ = Unclear effect potentially favouring the intervention, 95% CI includes zero; ▼ = Favours the control, 95% CI excludes 0; ▽ = Unclear effect potentially favouring the control, 95% CI includes 0. (+): low overall risk of bias; (?): unclear overall risk of bias; (‐): high overall risk of bias.
AM: Ajuda Mútua; CI: confidence interval; DID: difference in differences; HDDS: Household Dietary Diversity Score; HH: household; IDDS: Individual Dietary Diversity Score; MD: mean difference; n: number; N/A: not applicable/available; SD: standard deviation; VSL: village savings and loan; WAZ: weight‐for‐age z‐score.
10.
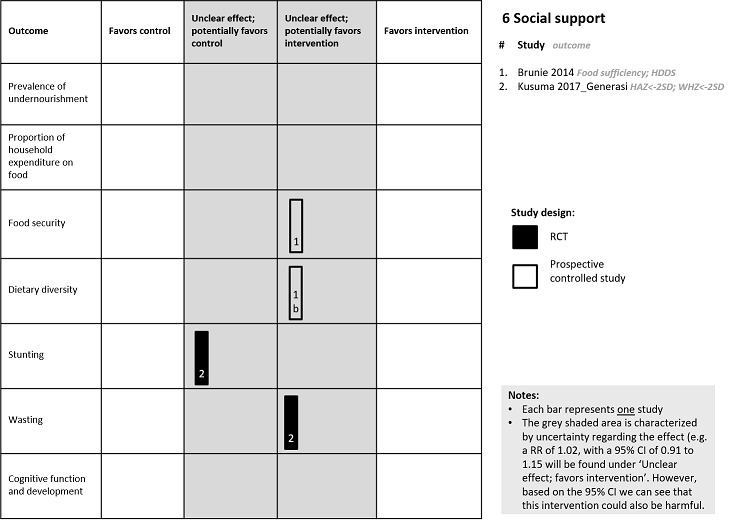
Harvest plot: social support interventions.
Primary outcomes
6.1 Change in the prevalence of undernourishment
None of the included studies measured prevalence of undernourishment.
6.2 Proportion of household expenditure on food
None of the included studies measured household expenditure on food.
6.3 Proportion of households who were food secure
One PCS reported on food security and dietary diversity measures (Brunie 2014).
6.3.1 Food security
The evidence was very uncertain about the effects of VSLs on food security (MD 1.25, 95% CI –0.28 to 2.79; 851 households; very low‐certainty evidence; Table 6; Figure 10). Brunie 2014 reported an unclear effect potentially favouring the VSL intervention on the number of self‐reported months of food sufficiency in the previous year, with an increase by 1.25 months in the intervention group at three years (Table 27).
6.3.2 Dietary diversity
The evidence was very uncertain about the effects of VSLs on dietary diversity (1 study, 802 households; very low‐certainty evidence; Table 6; Figure 10). Brunie 2014 reported an unclear effect on household dietary diversity favouring the control (MD –0.30, 95% CI –1.46 to 0.87; 1615 households) (Table 27).
Brunie 2014 also reported on Individual Dietary Diversity Scores (IDDS) among children: IDDS was slightly higher by 0.81 points (out of 12) in the VSL group (MD 0.52, 95% CI –0.18 to 1.23; 1121 children) (Table 27).
Secondary outcomes
6.4 Change in adequacy of dietary intake
None of the included studies measured adequacy of dietary intake.
6.5 Change in anthropometric indicators
One trial reported on stunting, wasting and underweight measures (Kusuma 2017b). One PCS reported on underweight measures (Brunie 2014).
6.5.1 Stunting (height‐for‐age z‐scores < –2SD)
Community grants may make little or no difference to stunting (1 trial, 1481 children; low‐certainty evidence; Table 6; Figure 10). Kusuma 2017b reported an unclear effect on stunting favouring the control (3.4 pp, 95% CI –7.4 to 14.2; 1481 children aged 24 to 36 months). The effect on severe stunting (HAZ < –3SD) was different: they reported an unclear effect favouring the community cash grants (–6 pp, 95% CI –16.4 to 4.4; 1481 children aged 24 to 36 months; Table 26).
6.5.2 Wasting (weight‐for‐height z‐scores < –2SD)
Community grants probably make little or no difference to wasting (1 RCT, 1481 children; moderate‐certainty evidence; Table 6; Figure 10). Kusuma 2017b reported an unclear effect favouring the intervention at two years (–1.0 pp, 95% CI –7.9 to 5.9). The effect on severe wasting (WHZ < –3SD) was similar (–2.1 pp, 95% CI –7 to 2.8; Table 26).
6.5.3 Underweight: weight‐for‐age z‐scores < –2SD
Randomised controlled trials
Kusuma 2017b reported an unclear effect on stunting favouring community cash grants (–2 pp, 95% CI –11.9 to 7.9; 1481 children). The effect on severe underweight (WAZ < –3SD) was similar (Table 26). This study was at unclear overall risk of bias.
Prospective controlled studies
Brunie 2014 reported an unclear effect on WAZ potentially favouring the VSL intervention (with or without a rotating labour scheme). Among children in the intervention group, the mean WAZ increased slightly by 0.05 SDs compared to the control group at three years (MD 0.05, 95% CI –0.37 to 0.48; 1053 children; Table 27).
6.6 Change in biochemical indicators
None of the included studies measured biochemical indicators.
6.7 Cognitive function and development
None of the included studies measured cognitive function and development.
6.8 Change in proportion of anxiety or depression
None of the included studies measured anxiety or depression.
6.9 Morbidity
None of the included studies measured morbidity.
6.10 Adverse outcomes (proportion of overweight/obesity)
None of the included studies measured proportion of overweight/obesity.
Discussion
Summary of main results
Fifty‐nine studies, addressing six intervention types, met the criteria for inclusion in this review. Some studies evaluated the same programme. None of the studies included assessed the primary outcome of prevalence of undernourishment.
Sixteen cRCTs, two parallel‐group RCTs and three PCS assessed UCTs. Available evidence indicates that UCTs improve food security (six RCTs) and make little or no difference to cognitive function and development (three RCTs) (high‐certainty evidence); UCTs may increase dietary diversity (10 RCTs) and may reduce stunting (four RCTs) (low‐certainty evidence); and that the evidence regarding the effects of UCTs on the proportion of household expenditure on food (five RCTs) and wasting (four RCTs) is very uncertain (very low‐certainty evidence). Regarding adverse outcomes, evidence from one trial indicates that UCTs reduce the proportion of infants who are overweight.
Nine cRCTs and five PCS assessed CCTs. None of these studies reported on food security measures. Available evidence indicates that CCTs result in little to no difference in the proportion of household expenditure on food (two RCTs) and that they slightly improve cognitive function in children (two RCTs) (high‐certainty evidence); that CCTs probably slightly improve dietary diversity (two RCTs) (moderate‐certainty evidence); and that they may make little to no difference to stunting (four RCTs) or wasting (two RCTs) (low‐certainty evidence). Evidence on adverse outcomes (two PCS) shows that CCTs make no different to the proportion of overweight children.
Six cRCTs and 11 PCS assessed income‐generation interventions. None of these studies reported on cognitive function and development, or the proportion of household expenditure on food. Available evidence indicates that income‐generation interventions make little or no difference to stunting (two RCTs) or wasting (two RCTs) (moderate‐certainty evidence); and that they may results in little to no difference to food security (two RCTs) and may improve dietary diversity in children but not for households (four RCTs) (low‐certainty evidence).
Four trials reported on food vouchers. None reported on the proportion of households expenditure on food, food security, or cognitive function and development. Available evidence indicates that food vouchers probably reduce stunting (one RCT) (moderate‐certainty evidence), and that they may improve dietary diversity slightly (two RCTs) and may result in little to no difference in wasting (one RCT) (low‐certainty evidence).
One RCT and three PCS reported the effects offood and nutrition subsidies. None of these studies reported on food security, stunting, wasting, or cognitive function and development. Available evidence indicates that food and nutrition subsidies may improve dietary diversity among school children (one RCT) (low‐certainty evidence), and the evidence is very uncertain about the effects on household expenditure on healthy foods as a proportion of total expenditure on food (very low‐certainty evidence).
One RCT and one PCS reported on the effects of social environment interventions. None of the studies reported on the proportion of household expenditure on food, or on cognitive function and development. Available evidence indicates that community grants probably make little to no difference to wasting (one RCT) (moderate‐certainty evidence) and that they make little or no difference to stunting (one RCT) (low‐certainty evidence); and the evidence is very uncertain about the effects of VSLs on food security (one PCS) and dietary diversity (one PCS) (very low‐certainty evidence).
Overall completeness and applicability of evidence
We considered the differences between the evidence identified and our prespecified eligibility criteria, including relevant gaps identified with the harvest plots regarding outcomes with no data, when assessing the completeness and applicability of the evidence.
Participants in included studies ranged from households to individuals, including adults and children. A few studies specifically targeted women as recipients of the intervention. Most studies targeted poor households, and mostly in rural areas, based on specific criteria to identify poor and vulnerable households. Although we had planned to assess effects within specific disadvantaged subgroups, this was not possible because of unclear reporting about these types of characteristics in the included studies.
Our logic model showed that there is a wide range of interventions that could address access to food. Across all the possible interventions, we included mostly studies aiming to increase buying power, including UCTs, CCTs, and income‐generation interventions. Fewer studies addressed food prices and only two assessed social environment interventions, namely a community cash grant programme, and a VSLs programme. We found no studies assessing infrastructure interventions that aimed to improve physical access to food. Some of the studies we excluded from this review assessed some of these relevant interventions, but they were conducted in high‐income countries. For example, one before‐after study that assessed the implementation of a fruit and vegetable market in low‐income neighbourhoods (Gorham 2015), which addressed lack of infrastructure; a randomised trial that assessed financial incentives to increase fruit and vegetable intake among participants in the USA Food Stamp programme (Olsho 2016), which addresses high food prices. This illustrates, perhaps, a lack of such interventions being implemented in LMIC settings. Regarding the variation in type and intensity of interventions, particularly of CCTs and how the conditions and the enforcement of these components vary across interventions, we were unable to distinguish which specific conditionalities were linked to the outcome based on available data. In these interventions, conditionalities ranged from attending clinic visits, educational sessions and school attendance. For other interventions such as income‐generation interventions, intervention components also varied significantly, and it is difficult to specify which intervention components are associated with the observed outcome.
In majority of studies, the intervention was not compared with another intervention. For some larger studies of government programmes, such as cash transfers, it was common for a delayed control to be used as a comparator. In this case, the control group also received the intervention, but at a later stage, as it would be unethical to randomise communities to no intervention in these types of programmes. One issue with this was that many long‐term outcomes were not eligible for reporting in this review as, by that time, both the intervention and control groups were receiving the intervention.
In terms of outcomes, no included study reported on the primary outcome of prevalence of undernourishment. Prevalence of Undernourishment (PoU) is a national‐level model‐based indicator used to understand access to food in terms of dietary energy inadequacy and can be measured at national or household level (INDDEX Project 2018). It measures the percentage of the population whose dietary energy intake is below the MDER. In line with this, the adequacy of dietary intake at the individual level was also not reported in most studies, and only six studies reported this outcome. Most studies reported on actual energy intake (i.e. calories) or intake of specific nutrients (i.e. grams), without assessing this intake against some measure of adequacy, such as the DRIs. Besides these outcome categories, fewer studies reported on child cognitive function and development compared to other outcomes. We had intended to assess not only if adequacy of dietary intake improved, but also if diet quality increased. Included studies did not report on dietary quality (i.e. whether they were refined and high in saturated fat or healthier foods such as legumes, fruit and vegetables). However, many studies reported on dietary diversity, which is an approximate measure of diet quality. Greater dietary diversity should indicate better overall dietary quality, as it means that foods from more food groups are being consumed. For most outcomes, data were available at two and three years, so there is not much evidence on longer‐term impact of included interventions. Only three studies reported on the adverse outcome of overweight and obesity.
Due to the lack of information in many included studies, we were unable to address our first secondary objective – to identify features of interventions that enable or impair the effective implementation. We believe this warrants a separate study assessing each intervention more in‐depth and using different study designs, such as qualitative studies.
Quality of the evidence
We assessed the certainty of the evidence using the GRADE approach and presented our findings in a 'Summary of findings' table for each comparison. For all comparisons except comparison 6, the 'Summary of findings' tables included only data from RCTs, as there were data from at least one RCT for the key outcomes. The 'Summary of findings' tables for comparisons 5 and 6 include data from RCTs and PCS, as for specific outcomes there were no data from RCTs.
For UCTs, the certainty of the evidence ranged from very low to high across outcomes. Reasons for downgrading included inconsistency due to wide variance of point estimates, imprecision due to wide CIs and due to high overall risk of bias.
For CCTs, the certainty of the evidence ranged from low to high across outcomes. Reasons for downgrading included inconsistency due to wide variation in point estimates, high overall risk of bias and imprecision due to wide CIs.
For income‐generation interventions, the certainty of the evidence ranged from low to moderate across outcomes. Reasons for downgrading included imprecision due to wide CIs, indirectness because the evidence was from a single study, high overall risk of bias and inconsistency due to wide variation in point estimates.
The certainty of the evidence on food voucher interventions ranged from low to moderate across outcomes. Reasons for downgrading included high overall risk of bias, inconsistency as CIs had minimal overlap, indirectness as findings were from one single study and imprecision due to findings ranging from an important harm to important benefit.
The certainty of the evidence on food and nutrition subsidies ranged from very low to low across outcomes. Reasons for downgrading included high overall risk bias and indirectness as the results were from a single study.
For VSLs, the certainty of the evidence ranged from very low to moderate. Reasons for downgrading included indirectness, as the results were from a single study, and imprecision, due to wide CIs.
All but one included study was funded by a for‐profit organisation and 66.1% did not report on potential COI.
Potential biases in the review process
We followed Cochrane Review methodology to prevent potential biases from being introduced into the review process. Nevertheless, potential biases could have been introduced due to the nature of subjective decisions that had to be made while conducting the review and because the protocol was outdated and new methods had emerged since its publication (Durao 2015).
Multiple outcome measures concerning the same outcome category were reported across included studies. Since there is no guidance in the literature on what measures are considered as 'gold standard' for measuring food and nutrition security, we selected the most comprehensive or largest scale measure reported for the same outcome domain in the same study. For example, we reported changes in z‐scores for height or weight but we did not report actual height (in centimetre) or weight (kilogram) measures. We judged changes in z‐scores to be more useful and easier to interpret as they are assessing standardised height and weight attainment adjusted for age and sex. Still, multiplicity of outcome measures made it difficult to include all studies reporting the same outcome domain in meta‐analyses.
We also could not include all studies in meta‐analyses due to incomplete reporting of the required data (e.g. variance measures). Therefore, we made post‐hoc decisions about synthesising the evidence using vote counting based on effect direction, using harvest plots to visually illustrate the results. We used the point estimates and the 95% CI to decide how to categorise the effects of the studies. However, data for these were sometimes not available or could not be calculated, and thus we had to base decisions regarding whether the effect was clear or unclear based on the P value.
As we had not prespecified the outcomes to be assessed using GRADE in the protocol (Durao 2015), we had to make this decision post‐hoc. The author team discussed and agreed through consensus which outcomes we considered best for informing decision‐making. However, it may be that another group could have made different decisions regarding which outcomes to highlight in the 'Summary of findings' tables. All outcomes are, however, reported in the review text and in the tables of individual results. We also had to prioritise outcome measures to report in the review as often there were multiple outcome measures reported in the same study for the same outcome domain. We attempted to prevent introduction of biases by selecting an approach that was independent of the effect measure reported (i.e. prioritising the most comprehensive outcome measure).
Our interpretation of the primary outcome 'proportion of household expenditure on food' was based on Engel's Law "…according to which the household decreases its budget share of food as its income increases". This is the interpretation used in one of the included studies (Brugh 2018). Not all included studies interpreted this outcome in the same way, with some interpreting an increase in this proportion as 'good' while others interpreting a decrease as 'good'. Furthermore, not all studies clearly interpreted their findings. This variability led us to interpret it based on Engel's law. While food expenditure is expected to increase with higher income, the proportion of expenditure on food in relation to other expenditure should decrease. The use of this approach may explain some of the diversity in effect measures observed for this outcome.
Due to our high search yield we were unable to complement the electronic database search with screening reference lists of included studies, reference lists of identified relevant systematic reviews or websites of specific organisations, as planned. Thus, we may have missed some relevant studies. However, since our search was very comprehensive, we believe that the chance of this was small.
One limitation of our review was that the synthesis was unable to draw conclusions about the mean effect size for many outcomes, due to limited availability of suitable data. However, we have tried to calculate all necessary information for meta‐analysis where this was possible.
Agreements and disagreements with other studies or reviews
Other recent reviews on food access tend to focus on individual interventions rather than on a comprehensive review of the evidence base of interventions addressing access to food like ours.
We identified six published reviews among the results of the updated search for this review which addressed access to food or included similar interventions to those included in this review. Three reviews addressed cash transfers (Baird 2014; Hunter 2017; Melo 2016); two reviews evaluated interventions related to the income‐generation category (Bird 2019; Pullar 2018); two reviews focused on interventions addressing food prices (Mizdrak 2015; Alagiyawanna 2015); and one review addressed interventions addressing infrastructure, for which we did not find any studies to include in our review (Hsiao 2019).
Of the reviews addressing cash transfers, two had a different focus to our review: one on the effect of cash transfers on educational outcomes (Baird 2014), and one on use and quality of maternity care services (Hunter 2017). The third review included 10 studies of cash transfer interventions in Latin America and reported a positive association of cash transfers with children's anthropometric status (Melo 2016). However, they also reported that improvements may differ by age and that the included studies, which varied in design, were of questionable methodological quality.
Other systematic reviews on cash transfers had a different focus than that of our review; they assessed the effects of such interventions on improving infant vaccination (Munk 2019), women economic empowerment (Leite 2019), clinical outcomes for pulmonary tuberculosis (Richterman 2018), or social determinants of health (Owusu‐Addo 2018). Of those that had a similar focus, some reported positive effects or no effects. One review of cash transfer programmes including different types of literature assessed the evidence of the impact of cash transfers on a range of individual‐ or household‐level outcomes in 201 included studies, of which 89 reported on health and nutrition outcomes, including the use of health services, dietary diversity and anthropometry (Bastagli 2016). They reported a greater proportion of significant results for dietary diversity than for anthropometric measures, but positive impacts in relation to the cash transfer interventions overall. Another review assessed universal and targeted UCTs and targeted CCTs and reported mostly positive effects of these interventions on birth weight, infant mortality, among other outcomes (Siddiqi 2018). Another review assessed the effects of CCTs on child health in LMICs (Owuso‐Addo 2014), and included 16 studies predominantly from Latin America. The review authors reported that programmes improved nutritional status of children in intervention compared to control groups in terms of, for example, growth in height and weight, decreased chance of being underweight, and improved dietary intake of protein and vegetables. However, some of the programmes did not always find an effect on anthropometric outcomes such as childhood wasting or stunting. Of note, these two reviews included the same studies as this Cochrane Review. Therefore, it is perhaps unsurprising that their findings were similar to ours. In one Cochrane Review of UCTs for reducing poverty and vulnerabilities and its effects on health services use and health outcomes in LMICs, the authors also reported that UCTs had beneficial effects on food security and dietary diversity, with evidence certainty ranging from low to moderate, and uncertain effects on stunting due to very low‐certainty evidence (Pega 2017).
Of the two reviews addressing income‐generation interventions, results were similar, with some potential positive effect on diet intake and diversity. Bird 2019 assessed agriculture interventions on nutrition outcomes in specific countries in South Asia (India, Bangladesh, Nepal, Pakistan and Afghanistan) where agriculture activities are major sources for the livelihoods of large sections of the population. They included six studies assessing interventions of provision of seeds, plants and training, or livestock and training, or both, and reported a positive impact on intermediate outcomes, such as diet quality and diversity, but mixed results regarding impact on nutritional outcomes, such as anthropometry and anaemia. No meta‐analyses were carried out due to high heterogeneity. Pullar 2018 assessed the effects of poverty reduction and development interventions on non‐communicable disease (NCD) prevalence and risk. They included 29 studies, mostly of agricultural interventions, and reported limited methodological quality in included studies and high heterogeneity of outcome measures, similarly to our review. Included studies failed to measure and report on NCD prevalence and risk, but they reported that intensive agricultural interventions were associated with improved calorie, vitamin, fruit and vegetable intake, with the effects being dependent on other factors such as land ownership and infection status. However, the findings had poor generalisability because of small sample sizes and use of convenience samples of population with the highest need.
Both reviews of interventions addressing food prices focused on obesity reduction and not on undernutrition. Alagiyawanna 2015 assessed the effects of fiscal interventions implemented at national or local levels to improve diets and reduce obesity, assessing effects on consumption and health outcomes in adults and children. They included 18 studies, mostly from high‐income countries. Nine of these studies assessed the impact of taxes and these were all were from high‐income countries. They reported that the effects of taxation of soft drinks and its consumption was mixed, as was the effect on BMI among children and adolescents. Existing taxation studies tend to be from high‐income countries, which is likely the reason why we did not find any taxation‐related studies to include in our review, which only focused on LMICs. Regarding subsidies, in high‐income countries, Alagiyawanna 2015 reported positive associations with fruit and vegetable intake, maternal weight gain, increase in mean haemoglobin levels, consumption of healthy foods and height‐for‐age, but no association with BMI, low birthweight or fetal survival. One study in a low‐ to middle‐income country reported a negative association of subsidies with increased obesity. The Mizdrak 2015 review assessed fiscal interventions, but its scope was to specifically assess which personal characteristics influence differential impact of fiscal interventions, as this is considered a barrier to implementation. They included eight studies from high‐income countries, reporting high heterogeneity between studies and population groups concerning the effects of fiscal measures on healthy diets. Although they reported that the evidence pointed towards a differential impact depending on personal characteristics, the data were limited and underpowered to detect effects according to personal characteristics.
Hsiao 2019 assessed the barriers and facilitators of mobile produce markets in the US. This is a category of interventions for which we did not find studies to include in our review (i.e. infrastructure interventions), likely because these types of studies currently tend to be from high‐income countries. They reported a positive association of mobile produce markets and fruit and vegetable intake, but noted that the quality of the evidence was problematic as the studies were found not to be rigorous in their design and had high potential for selection and other types of bias.
An important aspect about this review is that it included interventions addressing upstream factors affecting access to food, that do not only rely on individual agency. This has been globally recognised as the best approach to address over‐ and undernutrition, and cash transfers specifically are high on the agenda of many countries as they address the social determinants of health (Hawkes 2020; Owusu‐Addo 2018). These types of interventions fall under the category of double duty actions that address both under‐ and overnutrition at the same time, especially if complemented by education and behaviour change communication and regular check‐ups as part of the intervention (Hawkes 2020).
Authors' conclusions
Implications for practice.
This review provides policy makers with a comprehensive evidence base, ranging from randomised controlled trials (RCTs) to prospective controlled studies, evaluating the effects of a wide range of community‐level interventions to address access to food in low‐ and middle‐income countries (LMICs).
The body of evidence indicates that unconditional cash transfers (UCTs) can improve food security, income‐generation interventions do not seem to make a difference for food security, but the evidence is unclear for the other interventions. Conditional cash transfers (CCTs), UCTs, those that help generate income, and those that help minimise impact of food prices through food vouchers and subsidies can potentially improve dietary diversity. UCTs and food vouchers may have a potential impact on reducing stunting, but CCTs, income‐generation interventions or social environment interventions do not seem to make a difference on wasting or stunting. CCTs seem to positively impact cognitive function and development but not UCTs. This may be due to the fact that in CCTs, beneficiaries are required to meet specific conditionalities such as attending school, visiting the health clinic regularly for growth monitoring or supplementation. None of the included studies reported on the primary outcome prevalence of undernourishment; in retrospect this was expected given that this is mostly used as a national‐level indicator of food security.
We found no studies reporting specific adverse outcomes. Three studies, one assessing UCTs and two assessing CCTs, reported on increased risk of overweight and obesity, our predefined adverse outcome. The effects on this outcome are unclear and we should thus not discard overweight and obesity as potential harms of these interventions. This is particularly problematic because in LMIC populations, where these interventions are implemented, overweight and obesity are often already a problem. Hawkes 2020 reported that this was the case in cash or food transfers and voucher interventions in Mexico, Egypt and the US where the unintended negative outcomes of these programmes include poorer diet quality and obesity and diabetes‐related NCDs, due to increased intake of foods high in energy, sugar, fat and salt, resulting from the programme itself, or from the income from the programme that enabled people to purchase these types of foods. In some cases, the targeted populations experienced both undernutrition and overnutrition, such as the existence of undernourished children and obese mothers in the same household or community. Thus it is possible that these programmes may exacerbate existing problems. Potential solutions to prevent this could be related to specifying which types of foods can be purchased with interventions such as vouchers, and accompanying health education with transfers.
As these interventions are often implemented at national level, direct implications for practitioners and the community are less clear. Organisations involved in the development and implementation of interventions to improve access to food may be able to better focus their time and resources by optimally designing or choosing programmes which maximise the intended outcome.
Implications for research.
Here, we draw on the EPICOT framework – which stands for Evidence, Population, Intervention, Comparison, Outcomes, and Time stamp (Brown 2006) – to suggest gaps in the evidence base that future research could address. There is enough evidence from RCTs for CCTs and UCTs but not for the other intervention types assessed in this review (i.e. those addressing food prices (e.g. policies, discounts, vouchers and subsidies); addressing infrastructure and transport that affect physical access to food outlets; and those addressing the social environment and providing social support (e.g. social support from family, neighbours or government)).
In general, higher‐quality RCTs and prospective controlled studies are required, particularly concerning methods to minimise the issues with selection and attrition bias.
The multiplicity of outcome measures made analysis for this review challenging. It is thus important for future studies to have a similar set of outcomes that we can usefully compare across studies, and that are most relevant for assessing food and nutrition security at the community or household level. If primary studies measured similar outcomes, it would have likely been possible to pool the majority of results across included studies for this review, resulting in clearer review findings.
None of the included studies clearly and specifically reported on adverse events. Although these types of interventions do not tend to have the same extent of harms as a clinical intervention, for example, it is still important to consider what the potential harms may be. Although overweight or obesity is a potential harm, the studies did not report on this as such.
Most studies reported results from one to two years of the intervention. Longer‐term studies of interventions aimed to improve food access in vulnerable communities or households are required.
What's new
| Date | Event | Description |
|---|---|---|
| 4 August 2020 | New citation required but conclusions have not changed | Project funding added and review altered to Gold Open Access |
History
Protocol first published: Issue 2, 2015 Review first published: Issue 7, 2020
| Date | Event | Description |
|---|---|---|
| 3 August 2020 | Amended | Project funding added and review altered to Gold Open Access |
Acknowledgements
Solange Durão and Anel Schoonees are partly supported by the Research, Evidence and Development Initiative (READ‐It) project. READ‐It (project number 300342‐104) is funded by UK aid from the UK government, however, the views expressed do not necessarily reflect the UK government’s official policies.
Marianne Visser and Amanda Brand are supported by the Research, Evidence and Development Initiative (READ‐It) project. READ‐It (project number 300342‐104) is funded by UK aid from the UK government, however, the views expressed do not necessarily reflect the UK government’s official policies.
Dr Tamara Kredo and Professor Jimmy Volmink from Cochrane South Africa and Professor Paul Garner of the Liverpool School of Tropical Medicine for their contributions to the development of the protocol (Durao 2015).
Joy Oliver, from Cochrane South Africa, for helping develop the initial search strategy and search filter for non‐randomised studies.
Dr Anke Rohwer and Dr Eva Rehfuess for sharing their guidance document on the use of logic models in systematic reviews and health technology assessments of complex interventions (Rohwer 2016).
Patrick Condron, Liaison Librarian at the School of Medicine, University of Melbourne, for refining the search strategy that had been published in the protocol (Durao 2015), which was retrieving an excessive number of results.
Irma Klerings for revising, adapting and implementing the search strategies for this review.
Jenna Patterson, Maryke Wilkinson and Annette Gerritsen for help with screening, data extraction and compiling tables.
Jacob Burns for providing the template for the harvest plots.
Ndi Euphrasia Ebai‐Atuh is gratefully acknowledged as an external referee.
Appendices
Appendix 1. Search strategies for search update in February 2020
| Ovid MEDLINE(R) ALL 1946 to 13 February 2020 | ||
| 14 February 2020 | ||
| # | Searches | Results |
| 1 | *Nutritional Status/ | 24020 |
| 2 | *Diet/ | 75748 |
| 3 | *Body Mass Index/ | 20334 |
| 4 | *Food Supply/ | 8018 |
| 5 | *Nutrition Assessment/ | 7302 |
| 6 | (nutrition* or food? or diet*).ti. | 379668 |
| 7 | ((diet* or food? or nutrition*) adj (status or consumption or diversity)).ab. | 44392 |
| 8 | ((improv* or increas* or enhanc* or influenc*) adj3 (diet* or food? or nutrition*) adj3 (health* or access* or consum*)).ab. | 5207 |
| 9 | or/1‐8 | 453177 |
| 10 | *Social Welfare/ | 5470 |
| 11 | *Community Health Services/ | 19647 |
| 12 | *Public Assistance/ | 1679 |
| 13 | *Financing, Government/ | 8775 |
| 14 | *Government Programs/ | 2776 |
| 15 | *Community Participation/ | 9614 |
| 16 | ((social or economic or welfare or agricultural or labo?r or antipoverty or anti‐poverty) adj (program* or service? or support or intervention*)).ti,ab. | 49542 |
| 17 | ((food? or diet* or nutrition* or vegetable? or fruit? or agricultural) adj (class* or session* or program* or service? or production)).ti,ab. | 15688 |
| 18 | or/10‐17 | 110111 |
| 19 | 9 and 18 | 8935 |
| 20 | ((food or nutrition*) adj (secur* or insecur* or poverty or sufficien* or insufficien*)).mp. | 9377 |
| 21 | ((food or foods or foodstuff* or fruit? or vegetable? or grocer* or nutrition*) adj1 (budget* or shopping or purchas* or expend* or spend* or spent or buy* or acquisition or acquir*)).mp. | 3022 |
| 22 | ((tax or taxes or taxation or subsidy or subsidies or subsidi?ed or voucher* or coupon* or discount* or stamp?) adj2 (food or foods or foodstuff* or grocer* or fruit* or vegetable* or nutrition* or meal or meals)).mp. | 907 |
| 23 | ((cash or in‐kind or price) adj (transfer* or subsidy or subsidies)).mp. | 733 |
| 24 | (food adj (assistance or aid)).mp. | 1570 |
| 25 | Food Assistance/ | 976 |
| 26 | Food/ec [Economics] | 1172 |
| 27 | Diet/ec [Economics] | 987 |
| 28 | or/19‐27 | 23384 |
| 29 | exp animals/ not humans/ | 4673892 |
| 30 | 28 not 29 | 22037 |
| 31 | (Afghan* or Bangladesh* or Benin* or Burkina Faso or Burkinabe or Burundi* or Cambodia* or Central African Republic or Central African* or Chad* or Comoros or Comorian* or Congo* or Eritrea* or Ethiopia* or Gambia* or Ghana* or Guinea‐Bissau* or Haiti* or Kenya* or Kyrgyz Republic or Kyrgyzstani or Lao* or Liberia* or Madagascar or Malagasy or Malawi* or Mali* or Mauritania* or Mozambique or Mozambican or Myanmar* or Burma or Burmese or Nepal* or Niger* or Rwanda* or Sierra Leone* or Solomon Islands or Solomon Islanders or Somali* or Tajikistan* or Tanzania* or Togo* or Uganda* or Zambia* or Zimbabwe*).mp. | 840737 |
| 32 | (Angola* or Armenia* or Belize* or Bhutan* or Bolivia* or Cameroon* or Cape Verd* or China or Chinese or Cote dIvoire or Ivorian or Djibouti or Ecuador* or Egypt* or El Salvador or Salvadoran or Guatemala* or Guyana or Guyanese or Hondura* or India* or Indonesia* or Iraq* or Jordan* or Kiribati or Kosov* or Lesotho or Mosotho or Basotho or Maldiv* or Marshall Islands or Marshallese or Micronesia* or Moldova* or Mongolia* or Morocc* or Nicaragua* or Nigeria* or Pakistan* or Papua New Guinea* or Paraguay* or Philippines or Filipino or Samoa* or Senegal* or Sri Lanka* or Sudan* or Swaziland or Swazi or Syrian Arab Republic or Syria* or Thailand or Thai or Timor Leste or East Timorese or Tonga* or Tunisia* or Turkmen* or Tuvalu* or Ukrain* or Uzbekistan* or Uzbek or Vanuatu or Vietnam* or West Bank or Gaza or Palestinian* or Yemen*).mp. | 920050 |
| 33 | (Albania* or Algeria* or American Samoa or Antigua* or Barbuda* or Argentin* or Azerbaijan* or Belarus* or Bosnia* or Herzegovin* or Botswana or Motswana or Batswana or Brazil* or Bulgaria* or Chile* or Colombia* or Costa Rica* or Cuba* or Dominica* or Dominican Republic or Fiji* or Gabon* or Grenad* or Iran* or Jamaica* or Kazakhstan* or Leban* or Libya* or Lithuania* or Macedonia* or Malaysia* or Mauriti* or Mayotte or Mahoran or Mexic* or Montenegr* or Namibia* or Palau* or Panama* or Peru* or Romania* or Russia* or Serbia* or Seychell* or South Africa* or St Lucia* or Suriname* or Turk* or Uruguay* or Venezuela*).mp. | 625717 |
| 34 | Developing Countries/ | 73775 |
| 35 | (lmic or lmics).mp. | 4361 |
| 36 | ((low income or medium income) adj5 (country or countries or nation or nations or state or states)).mp. | 8741 |
| 37 | (least developed adj (country or countries or nation or nations or state or states)).mp. | 257 |
| 38 | (developing adj (countr* or nation? or state?)).mp. | 125319 |
| 39 | ((united nations or world health organization or world bank or unicef) and ((food or nutrition*) adj3 (program* or project* or fund))).mp. | 340 |
| 40 | or/31‐39 | 2305368 |
| 41 | 30 and 40 | 7034 |
| 42 | (randomized controlled trial or controlled clinical trial).pt. | 589397 |
| 43 | random*.mp. | 1339226 |
| 44 | comparative study.pt. | 1854534 |
| 45 | control groups/ or control group*.mp. or follow‐up studies/ or follow‐up stud*.mp. or follow‐up assessment.mp. or prospective studies/ or prospectiv*.mp. or non‐random*.mp. or nonrandom*.mp. | 1813129 |
| 46 | (before after stud* or (time and series) or retrospective* or longitud* or (controlled and cohort* and stud*)).mp. | 1459595 |
| 47 | "before and after".mp. | 266393 |
| 48 | (controlled before or pre test or pretest or posttest or post test or pre intervention or post intervention).mp. | 43847 |
| 49 | controlled before‐after studies/ or interrupted time series analysis/ | 1253 |
| 50 | or/42‐49 | 5401950 |
| 51 | 41 and 50 | 1621 |
| 52 | limit 51 to yr="1980 ‐Current" | 1615 |
| Cochrane Library | ||
| 14 February 2020 | ||
| ID | Search | Hits |
| #1 | [mh ^"Nutritional Status"[mj]] | 8 |
| #2 | [mh ^diet[mj]] | 15 |
| #3 | [mh ^"Body Mass Index"[mj]] | 5 |
| #4 | [mh ^"Food Supply"[mj]] | 2 |
| #5 | [mh ^"Nutrition Assessment"[mj]] | 1 |
| #6 | (nutrition* or food? or diet*):ti and (intervention* or program* or service*):ti,ab,kw | 15540 |
| #7 | ((diet* or food? or nutrition*) NEXT (status or diversity)):ab,kw | 6376 |
| #8 | ((improv* or increas* or enhanc* or influenc*) NEAR/3 (diet* or food? or nutrition*) NEAR/3 (health* or access* or consum*)):ab | 903 |
| #9 | {or #1‐#8} | 20869 |
| #10 | [mh ^"Social Welfare"[mj]] | 3 |
| #11 | [mh ^"Community Health Services"[mj]] | 6 |
| #12 | [mh ^"Public Assistance"[mj]] | 0 |
| #13 | [mh ^"Financing, Government"[mj]] | 2 |
| #14 | [mh ^"Government Programs"[mj]] | 0 |
| #15 | [mh ^"Community Participation"[mj]] | 4 |
| #16 | ((social or economic or welfare or agricultural or labo?r or antipoverty or poverty) NEXT (program* or service? or support or intervention*)):ti,ab,kw | 8910 |
| #17 | ((food? or diet* or nutrition* or vegetable? or fruit? or agricultural) NEXT (class* or session* or program* or service?)):ti,ab,kw | 1489 |
| #18 | {or #10‐#17} | 10351 |
| #19 | #9 and #18 | 1084 |
| #20 | ((food or nutrition*) NEXT (secur* or insecur* or poverty or sufficien* or insufficien*)):ti,ab,kw | 557 |
| #21 | ((food or foods or foodstuff* or fruit? or vegetable? or grocer* or nutrition*) NEAR/1 (budget* or shopping or purchas* or expend* or spend* or spent or buy* or acquisition or acquir*)):ti,ab,kw | 409 |
| #22 | ((tax or taxes or taxation or subsidy or subsidies or subsidi?ed or voucher* or coupon* or discount* or stamp?) NEAR/2 (food or foods or foodstuff* or grocer* or fruit* or vegetable* or nutrition* or meal or meals)):ti,ab,kw | 143 |
| #23 | ((cash or "in kind" or price) NEXT (transfer* or subsidy or subsidies)):ti,ab,kw | 308 |
| #24 | (food NEXT (assistance or aid)):ti,ab,kw | 161 |
| #25 | [mh ^"Food Assistance"] | 63 |
| #26 | {or #19‐#25} | 2353 |
| #27 | (Afghan* or Bangladesh* or Benin* or "Burkina Faso" or Burkinabe or Burundi* or Cambodia* or "Central African*" or Chad* or Comoros or Comorian* or Congo* or Eritrea* or Ethiopia* or Gambia* or Ghana* or Guinea‐Bissau* or Haiti* or Kenya* or Kyrgyz* or Lao* or Liberia* or Madagascar or Malagasy or Malawi* or Mali* or Mauritania* or Mozambique or Mozambican or Myanmar* or Burma or Burmese or Nepal* or Niger* or Rwanda* or "Sierra Leone*" or "Solomon Island*" or Somali* or Tajikistan* or Tanzania* or Togo* or Uganda* or Zambia* or Zimbabwe*) | 53980 |
| #28 | (Angola* or Armenia* or Belize* or Bhutan* or Bolivia* or Cameroon* or "Cape Verd*" or China or Chinese or "Cote d'Ivoire" or Ivorian or Djibouti or Ecuador* or Egypt* or "El Salvador" or Salvadoran or Guatemala* or Guyana or Guyanese or Hondura* or India* or Indonesia* or Iraq* or Jordan* or Kiribati or Kosov* or Lesotho or Mosotho or Basotho or Maldiv* or "Marshall Islands" or Marshallese or Micronesia* or Moldova* or Mongolia* or Morocc* or Nicaragua* or Nigeria* or Pakistan* or "Papua New Guinea*" or Paraguay* or Philippines or Filipino or Samoa* or Senegal* or "Sri Lanka*" or Sudan* or Swaziland or Swazi or Syrian or Syria* or Thailand or Thai or Timor* or Tonga* or Tunisia* or Turkmen* or Tuvalu* or Ukrain* or Uzbekistan* or Uzbek or Vanuatu or Vietnam* or "West Bank" or Gaza or Palestinian* or Yemen*) | 151389 |
| #29 | (Albania* or Algeria* or Samoa or Antigua* or Barbuda* or Argentin* or Azerbaijan* or Belarus* or Bosnia* or Herzegovin* or Botswana or Motswana or Batswana or Brazil* or Bulgaria* or Chile* or Colombia* or Costa Rica* or Cuba* or Dominica* or "Dominican Republic" or Fiji* or Gabon* or Grenad* or Iran* or Jamaica* or Kazakhstan* or Leban* or Libya* or Lithuania* or Macedonia* or Malaysia* or Mauriti* or Mayotte or Mahoran or Mexic* or Montenegr* or Namibia* or Palau* or Panama* or Peru* or Romania* or Russia* or Serbia* or Seychell* or "South Africa*" or "St Lucia*" or Suriname* or Turk* or Uruguay* or Venezuela*) | 87980 |
| #30 | [mh "developing countries"] | 836 |
| #31 | (lmic or lmics):ti,ab,kw | 351 |
| #32 | (("low income" or "medium income") near/5 (country or countries or nation or nations or state or states)):ti,ab,kw | 875 |
| #33 | ("least developed" next (country or countries or nation or nations or state or states)):ti,ab,kw | 4 |
| #34 | (developing next (country or countries or nation or nations or state or states)):ti,ab,kw | 4015 |
| #35 | ("united nations" or "world health organization" or "world bank" or unicef):ti,ab,kw and ((food or nutrition*) near/3 (program* or project* or fund)):ti,ab,kw | 48 |
| #36 | {or #27‐#35} | 276771 |
| #37 | #26 and #36 with Publication Year from 1980 to 2020, in Trials | 931 |
| Web of Science | ||
| 14 February 2020 | ||
| Set | Results | Search |
| # 1 | 28774 | TS=((food OR nutrition*) NEAR/1 (secur* OR insecur* OR poverty OR sufficien* OR insufficien*)) |
| # 2 | 7900 | TS=((food OR foods OR foodstuff* OR fruit$ OR vegetable$ OR grocer* OR nutrition*) NEAR/1 (budget* OR shopping OR purchas* OR expend* OR spend* OR spent OR buy* OR acquisition OR acquir*)) |
| # 3 | 2186 | TS=((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidi$ed OR voucher* OR coupon* OR discount* OR stamp$) NEAR/2 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition* OR meal OR meals)) |
| # 4 | 3476 | TS=((cash OR "in‐kind" OR price) NEAR/1 (transfer* OR subsidy OR subsidies)) |
| # 5 | 1840 | TS= (food NEAR/1 (assistance OR aid)) |
| # 6 | 1302 | TI=(nutrition* OR food* OR diet*) AND TS=((social OR economic OR welfare OR agricultural OR labo$r OR antipoverty OR anti‐poverty) NEAR/1 (program* OR service* OR support OR intervention*)) |
| # 7 | 920 | TI=("nutrition program*" OR "food program*") |
| # 8 | 43727 | #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 |
| # 9 | 959932 | TS=(afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe*) |
| # 10 | 1680193 | TS=(angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen*) |
| # 11 | 1279195 | TS=(albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela*) |
| # 12 | 3653 | TS=(lmic OR lmics) |
| # 13 | 8152 | TS=(("low income" OR "medium income") NEAR/1 (country OR countries OR nation OR nations OR state OR states)) |
| # 14 | 803 | TS=("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) |
| # 15 | 112430 | TS=("developing countr*" OR "developing nation$" OR "developing state$") |
| # 16 | 290 | TS=(("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund))) |
| # 17 | 3722287 | #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 |
| # 18 | 18310 | #17 AND #8 |
| # 19 | 2489418 | TS=((compar* OR control*) NEAR/10 (study OR trial OR program* OR evaluat* OR assess*)) |
| # 20 | 2076881 | TS=(random* OR "control group*" OR "control subject*") |
| # 21 | 969070 | TS=("follow up" OR "long‐term impact" OR "long‐term effect*" ) |
| # 22 | 902125 | TS=((prospectiv* OR non‐random* OR nonrandom* OR retrospectiv* OR longitud*) NEAR/6 (stud* OR trial* OR evaluat* OR assess*)) |
| # 23 | 176785 | TS=("before after stud*" OR "time series") |
| # 24 | 21621 | TS=((control* OR compar*) NEAR/6 cohort* NEAR/6 (stud* OR trial* OR assess* OR evaluat*)) |
| # 25 | 263527 | TS=("before and after") |
| # 26 | 619042 | TS=("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention" OR baseline) |
| # 27 | 5729458 | #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 |
| # 28 | 3226 | #27 AND #18 |
| # 29 | 2747 | #27 AND #18 Refined by: [excluding] WEB OF SCIENCE CATEGORIES: ( PARASITOLOGY OR VIROLOGY OR ENTOMOLOGY OR REMOTE SENSING OR ZOOLOGY OR MEDICINE RESEARCH EXPERIMENTAL OR ENERGY FUELS OR PLANT SCIENCES OR IMAGING SCIENCE PHOTOGRAPHIC TECHNOLOGY OR GEOGRAPHY PHYSICAL OR SOIL SCIENCE OR EVOLUTIONARY BIOLOGY OR VETERINARY SCIENCES OR HISTORY PHILOSOPHY OF SCIENCE OR OPTICS OR GEOGRAPHY OR SURGERY ) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1980‐2020 |
| Global Health (EBSCO) | |||
| 14 February 2020 | |||
| # | Query | Limiters/Expanders | Results |
| S1 | (DE "food security") OR (DE "food policy") OR (DE "food aid" OR DE "food distribution programs") | Search modes ‐ Boolean/Phrase | 14661 |
| S2 | (food OR nutrition*) W0 (secur* OR insecur* OR poverty OR sufficien* OR insufficien*) | Search modes ‐ Boolean/Phrase | 18939 |
| S3 | (food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) N1 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring) | Search modes ‐ Boolean/Phrase | 5072 |
| S4 | (foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket OR supermarkets OR grocery store OR grocery stores OR food store OR food stores OR food shop OR food shops OR corner store OR corner stores OR cafeteria OR cafeterias OR canteen* OR food outlet*) N2 (access OR accessibility OR cost OR costs OR price OR prices OR pricing) | Search modes ‐ Boolean/Phrase | 896 |
| S5 | (tax OR taxes OR taxation OR subsidy OR subsidies OR subsidi*ed OR voucher* OR coupon* OR discount* OR stamp*) N2 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition* OR meal OR meals) | Search modes ‐ Boolean/Phrase | 1205 |
| S6 | (cash OR in‐kind OR price) W1 (transfer* OR subsidy OR subsidies) | Search modes ‐ Boolean/Phrase | 704 |
| S7 | food W1 (assistance OR aid) | Search modes ‐ Boolean/Phrase | 6607 |
| S8 | TI ( nutrition* OR food* OR diet* ) AND ( (social OR economic OR welfare OR agricultural OR labo#r OR antipoverty OR anti‐poverty OR poverty) N1 (program* OR service* OR support OR intervention*) ) | Search modes ‐ Boolean/Phrase | 2515 |
| S9 | TI (nutrition program* OR food program*) | Search modes ‐ Boolean/Phrase | 2827 |
| S10 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 | Search modes ‐ Boolean/Phrase | 31469 |
| S11 | DE "Developing Countries" OR DE "Least Developed Countries" | Search modes ‐ Boolean/Phrase | 822999 |
| S12 | Afghan* OR Bangladesh* OR Benin* OR Burkina Faso OR Burkinabe OR Burundi* OR Cambodia* OR Central African Republic OR Central African* OR Chad* OR Comoros OR Comorian* OR Congo* OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea‐Bissau* OR Haiti* OR Kenya* OR Kyrgyz Republic OR Kyrgyzstani OR Lao* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Mozambique OR Mozambican OR Myanmar* OR Burma OR Burmese OR Nepal* OR Niger* OR Rwanda* OR Sierra Leone* OR Solomon Islands OR Solomon Islanders OR Somali* OR Tajikistan* OR Tanzania* OR Togo* OR Uganda* OR Zambia* OR Zimbabwe* | Search modes ‐ Boolean/Phrase | 251085 |
| S13 | Angola* OR Armenia* OR Belize* OR Bhutan* OR Bolivia* OR Cameroon* OR Cape Verd* OR China OR Chinese OR Cote dIvoire OR Ivorian OR Djibouti OR Ecuador* OR Egypt* OR El Salvador OR Salvadoran OR Guatemala* OR Guyana OR Guyanese OR Hondura* OR India* OR Indonesia* OR Iraq* OR Jordan* OR Kiribati OR Kosov* OR Lesotho OR Mosotho OR Basotho OR Maldiv* OR Marshall Islands OR Marshallese OR Micronesia* OR Moldova* OR Mongolia* OR Morocc* OR Nicaragua* OR Nigeria* OR Pakistan* OR Papua New Guinea* OR Paraguay* OR Philippines OR Filipino OR Samoa* OR Senegal* OR Sri Lanka* OR Sudan* OR Swaziland OR Swazi OR Syrian Arab Republic OR Syria* OR Thailand OR Thai OR Timor Leste OR East Timorese OR Tonga* OR Tunisia* OR Turkmen* OR Tuvalu* OR Ukrain* OR Uzbekistan* OR Uzbek OR Vanuatu OR Vietnam* OR West Bank OR Gaza OR Palestinian* OR Yemen* | Search modes ‐ Boolean/Phrase | 872351 |
| S14 | Albania* OR Algeria* OR Samoa OR Antigua* OR Barbuda* OR Argentin* OR Azerbaijan* OR Belarus* OR Bosnia* OR Herzegovin* OR Botswana OR Motswana OR Batswana OR Brazil* OR Bulgaria* OR Chile* OR Colombia* OR Costa Rica* OR Cuba* OR Dominica* OR Dominican Republic OR Fiji* OR Gabon* OR Grenad* OR Iran* OR Jamaica* OR Kazakhstan* OR Leban* OR Libya* OR Lithuania* OR Macedonia* OR Malaysia* OR Mauriti* OR Mayotte OR Mahoran OR Mexic* OR Montenegr* OR Namibia* OR Palau* OR Panama* OR Peru* OR Romania* OR Russia* OR Serbia* OR Seychell* OR South Africa* OR St Lucia* OR Suriname* OR Turk* OR Uruguay* OR Venezuela* | Search modes ‐ Boolean/Phrase | 681016 |
| S15 | (lmic OR lmics) | Search modes ‐ Boolean/Phrase | 1967 |
| S16 | (low income OR medium income) N1 (country OR countries OR nation OR nations OR state OR states) | Search modes ‐ Boolean/Phrase | 11661 |
| S17 | least developed countr* OR least developed nation* OR least developed state* | Search modes ‐ Boolean/Phrase | 99060 |
| S18 | developing countr* OR developing nation* OR developing state* | Search modes ‐ Boolean/Phrase | 832983 |
| S19 | (united nations OR world health organization OR world bank OR unicef) AND ((food OR nutrition*) N3 (program* OR project* OR fund)) | Search modes ‐ Boolean/Phrase | 1412 |
| S20 | S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 | Search modes ‐ Boolean/Phrase | 1546628 |
| S21 | S10 AND S20 | Search modes ‐ Boolean/Phrase | 17162 |
| S22 | (DE "clinical trials" OR DE "controls (experimental)") OR (DE "time series") OR DE "program evaluation" | Search modes ‐ Boolean/Phrase | 23578 |
| S23 | (compar* OR control*) N10 (study OR trial OR program* OR evaluat* OR assess*) | Search modes ‐ Boolean/Phrase | 348370 |
| S24 | random* OR control group* OR control subject* | Search modes ‐ Boolean/Phrase | 322654 |
| S25 | "follow up" OR long‐term impact OR long‐term effect* | Search modes ‐ Boolean/Phrase | 120166 |
| S26 | (prospectiv* OR non‐random* OR nonrandom* OR retrospectiv* OR longitud*) N6 (stud* OR trial* OR evaluat* OR assess*) | Search modes ‐ Boolean/Phrase | 150119 |
| S27 | before after stud* OR time series | Search modes ‐ Boolean/Phrase | 10227 |
| S28 | (control* OR compar*) N6 cohort* N6 (stud* OR trial* OR assess* OR evaluat*) | Search modes ‐ Boolean/Phrase | 6599 |
| S29 | "before and after" | Search modes ‐ Boolean/Phrase | 41781 |
| S30 | pre test OR pretest OR posttest OR post test OR pre intervention OR post intervention OR baseline | Search modes ‐ Boolean/Phrase | 106600 |
| S31 | experiment* OR (evaluat* N1 (program* OR impact*)) | Search modes ‐ Boolean/Phrase | 299118 |
| S32 | S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 | Search modes ‐ Boolean/Phrase | 1015368 |
| S33 | S21 AND S32 | Search modes ‐ Boolean/Phrase | 3316 |
| S34 | S33 | Limiters ‐ Publication Year: 1980‐2020 | 3282 |
| Sociological Abstracts (ProQuest) | ||
| 14 February 2020 | ||
| Set | Query | Result |
| S1 | ab((food OR nutrition*) PRE/0 (secur* OR insecur* OR poverty OR sufficien* OR insufficien* OR access*)) OR ti((food OR nutrition*) PRE/0 (secur* OR insecur* OR poverty OR sufficien* OR insufficien* OR access*)) | 2351 |
| S2 | ti((food OR foods OR foodstuff* OR fruit* OR vegetable* OR grocer* OR nutrition*) NEAR/1 (budget* OR shopping OR purchas* OR expend* OR spend* OR spent OR buy* OR acquisition OR acquir*)) OR ab((food OR foods OR foodstuff* OR fruit* OR vegetable* OR grocer* OR nutrition*) NEAR/1 (budget* OR shopping OR purchas* OR expend* OR spend* OR spent OR buy* OR acquisition OR acquir*)) | 736 |
| S3 | ti((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidi*ed OR voucher* OR coupon* OR discount* OR stamp OR stamps) NEAR/2 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition* OR meal OR meals)) OR ab((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidi*ed OR voucher* OR coupon* OR discount* OR stamp OR stamps) NEAR/2 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition* OR meal OR meals)) | 452 |
| S4 | ti((cash OR in‐kind OR price) PRE/0 (transfer* OR subsidy OR subsidies)) OR ab((cash OR in‐kind OR price) PRE/0 (transfer* OR subsidy OR subsidies)) | 611 |
| S5 | ti((food) PRE/0 (assistance OR aid)) OR ab((food) PRE/0 (assistance OR aid)) | 354 |
| S6 | ti(nutrition* OR food* OR diet*) AND ((social OR economic OR welfare OR agricultural OR labor OR labour OR antipoverty OR poverty) NEAR/1 (program* OR service* OR support OR intervention*)) | 773 |
| S7 | ti((nutrition* OR food*) NEAR/1 program*) | 159 |
| S8 | ti((nutrition* OR food*) NEAR/1 program*)MAINSUBJECT.EXACT("Food Stamps") OR MAINSUBJECT.EXACT("Food Security") | 1399 |
| S9 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 | 4732 |
| S10 | (afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) | 474017 |
| S11 | MAINSUBJECT.EXACT("Developing Countries") | 8796 |
| S12 | lmic OR lmics | 179 |
| S13 | (("low income" OR "medium income") PRE/1 (country OR countries OR nation OR nations OR state OR states)) | 1879 |
| S14 | ("least developed" PRE/1 (country OR countries OR nation OR nations OR state OR states)) | 575 |
| S15 | (developing PRE/1 (country OR countries OR nation OR nations OR state OR states)) | 30594 |
| S16 | ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)) | 1133 |
| S17 | 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 | 483676 |
| S18 | 9 AND 17 | 2664 |
| S21 | 18 AND yr(1980‐2029) | 2632 |
| S22 | (SU.EXACT("Cohort Analysis") OR SU.EXACT("Research Subjects") OR SU.EXACT("Time Series Analysis") OR SU.EXACT("Random Samples") OR SU.EXACT("Comparative Analysis") OR SU.EXACT("Longitudinal Studies")) | 14062 |
| S23 | ti(random* OR trial OR study OR evaluation OR controlled OR compar*) | 117165 |
| S24 | "pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention" OR baseline OR "follow up" OR "long‐term impact" OR "long‐term effect*" OR "before after stud*" OR "time series" OR "before and after" OR random* OR ("control group" OR "control groups") OR ("control subject" OR "control subjects") | 111057 |
| S25 | cohort* OR prospectiv* OR retrospectiv* OR longitudinal | 101579 |
| S26 | 22 OR 23 OR 24 OR 25 | 279265 |
| S27 | 21 AND 26 | 746 |
| International Clinical Trials Registry Platform | |
| 14 February 2020 | |
| 98 records for 98 trials found for: | food secur* OR food insecur* OR food access OR food poverty OR food sufficienc* OR food insufficienc* OR nutrition secur* |
Appendix 2. Search strategies for original search (2016)
MEDLINE: Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present
1 (food secur* or food insecur* or food poverty or food sufficien* or food insufficien* or food desert*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
2 ((food or foods or foodstuff* or fruit or fruits or vegetable or vegetables or grocer*) adj5 (budget* or shopping or purchase or purchasing or purchases or expenditure or expenditures or spend or spent or spending or buy or buying or acquisition or acquire or acquiring)).mp.
3 ((foodstuff* or fruit? or vegetable? or grocer* or supermarket? or food store? or food shop? or corner store? or cafeteria? or canteen* or food outlet*) adj5 (access or accessibility or cost or costs or price or prices or pricing)).mp.
4 food system*.mp. and ((fresh or health or healthy or nutrition or nutritional or nutritive or nutrient rich or nutrient dense or adequate or quality or sufficient or insufficient or secure or insecure or safe).mp. or diet/)
5 ((policy or policies) adj5 (food or foods or fruit or fruits or vegetable or vegetables or nutrition or grocer* or meal or meals)).mp.
6 ((council or councils or coalition or coalitions or co‐op or co‐ops or co‐operative*) adj5 (food or foods or fruit or fruits or vegetable or vegetables or nutrition or grocer*)).mp.
7 (access* adj3 food).mp.
8 or/1‐7
9 ((deliver or delivery or deliveries or transport or transportation or distribute or distributes or distribution) adj3 (grocer* or meal or meals or fruit or fruits or vegetable? or food?)).mp.
10 (outreach or service or services or scheme or schemes or program or programs or programme or programmes or policy or policies or project or projects or nutrition or nutritional or home or home‐based or homes or community or communities or neighbor or neighborhood or neighbour or neighbourhood or rural or urban or provide or provision or choice or control).mp.
11 social welfare/
12 9 and 10
13 9 and 11
14 ((public transport or transport service* or transportation service* or transport scheme or travel or travelling or infrastructure or access) adj5 (food store* or food shop* or food retail* or food outlet or supermarket or grocer*)).mp.
15 ((payment or payments or benefit or benefits or money or purchase or purchasing or purchases or buy or buying or welfare or financing or cash or income) adj5 (food? or foodstuff* or grocer* or fruit? or vegetable? or nutrition or nutritional or meal?) adj10 (supplement or supplementation or assist or assistance or extra or aid or support or help)).mp.
16 ((tax or taxes or taxation or subsidy or subsidies or subsidized or subsidised or voucher* or coupon* or discount*) adj5 (food or foods or foodstuff* or grocer* or fruit* or vegetable* or nutrition or nutritional or meal or meals)).mp.
17 ((Cash transfer* or social protection) and (food or foods or foodstuff* or grocer* or fruit* or vegetable* or nutrition or nutritional or meal or meals)).mp.
18 ((community nutrition or public health nutrition or food access) and (project* or program*)).mp.
19 food assistance/
20 Food/ec [Economics]
21 exp Diet/ec [Economics]
22 8 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21
23 exp animals/ not humans/
24 22 not 23
25 (Afghan* or Bangladesh* or Benin* or Burkina Faso or Burkinabe or Burundi* or Cambodia* or Central African Republic or Central African* or Chad* or Comoros or Comorian* or Congo* or Eritrea* or Ethiopia* or Gambia* or Ghana* or Guinea‐Bissau* or Haiti* or Kenya* or Kyrgyz Republic or Kyrgyzstani or Lao* or Liberia* or Madagascar or Malagasy or Malawi* or Mali* or Mauritania* or Mozambique or Mozambican or Myanmar* or Burma or Burmese or Nepal* or Niger* or Rwanda* or Sierra Leone* or Solomon Islands or Solomon Islanders or Somali* or Tajikistan* or Tanzania* or Togo* or Uganda* or Zambia* or Zimbabwe*).mp.
26 (Angola* or Armenia* or Belize* or Bhutan* or Bolivia* or Cameroon* or Cape Verd* or China or Chinese or Cote dIvoire or Ivorian or Djibouti or Ecuador* or Egypt* or El Salvador or Salvadoran or Guatemala* or Guyana or Guyanese or Hondura* or India* or Indonesia* or Iraq* or Jordan* or Kiribati or Kosov* or Lesotho or Mosotho or Basotho or Maldiv* or Marshall Islands or Marshallese or Micronesia* or Moldova* or Mongolia* or Morocc* or Nicaragua* or Nigeria* or Pakistan* or Papua New Guinea* or Paraguay* or Philippines or Filipino or Samoa* or Senegal* or Sri Lanka* or Sudan* or Swaziland or Swazi or Syrian Arab Republic or Syria* or Thailand or Thai or Timor Leste or East Timorese or Tonga* or Tunisia* or Turkmen* or Tuvalu* or Ukrain* or Uzbekistan* or Uzbek or Vanuatu or Vietnam* or West Bank or Gaza or Palestinian* or Yemen*).mp.
27 (Albania* or Algeria* or American Samoa or Antigua* or Barbuda* or Argentin* or Azerbaijan* or Belarus* or Bosnia* or Herzegovin* or Botswana or Motswana or Batswana or Brazil* or Bulgaria* or Chile* or Colombia* or Costa Rica* or Cuba* or Dominica* or Dominican Republic or Fiji* or Gabon* or Grenad* or Iran* or Jamaica* or Kazakhstan* or Leban* or Libya* or Lithuania* or Macedonia* or Malaysia* or Mauriti* or Mayotte or Mahoran or Mexic* or Montenegr* or Namibia* or Palau* or Panama* or Peru* or Romania* or Russia* or Serbia* or Seychell* or South Africa* or St Lucia* or Suriname* or Turk* or Uruguay* or Venezuela*).mp.
28 developing countries/
29 (lmic or lmics).mp.
30 ((low income or medium income) adj5 (country or countries or nation or nations or state or states)).mp.
31 (least developed adj (country or countries or nation or nations or state or states)).mp.
32 (developing adj (country or countries or nation or nations or state or states)).mp.
33 (united nations or world health organization or world bank or unicef or ((food or nutrition*) adj3 (program* or project* or fund))).mp.
34 or/25‐33
35 24 and 34
36 (randomized controlled trial or controlled clinical trial).pt.
37 (randomized or placebo or (random* and trial* and group*)).mp.
38 comparative study.pt.
39 control groups/ or control group*.mp. or follow‐up studies/ or follow‐up stud*.mp. or follow‐up assessment.mp. or prospective studies/ or prospectiv*.mp. or non‐random*.mp. or nonrandom*.mp.
40 (before after stud* or (time and series) or retrospective* or longitud* or (controlled and cohort* and stud*)).mp.
41 "before and after".mp.
42 (controlled before or pre test or pretest or posttest or post test or pre intervention or post intervention).mp.
43 or/36‐42
44 35 and 43
45 limit 44 to yr="1980 ‐Current"
46 remove duplicates from 45
Cochrane Central Register of Controlled Trials: Issue 8 of 12, August 2016
#1 ("food secur*" or "food insecur*" or "food poverty" or "food sufficien*" or "food insufficien*" or "food desert*"):ti,ab,kw
#2 ((food or foods or foodstuff* or fruit or fruits or vegetable or vegetables or grocer*) near/5 (budget* or shopping or purchase or purchasing or purchases or expenditure or expenditures or spend or spent or spending or buy or buying or acquisition or acquire or acquiring)):ti,ab,kw
#3 ((foodstuff* or fruit or fruits or vegetable or vegetables or grocer* or supermarket* or "food store*" or "food shop*" or "corner store*" or cafeteria* or canteen* or "food outlet*") near/5 (access or accessibility or cost or costs or price or prices or pricing)):ti,ab,kw
#4 food system*:ti,ab,kw and ((fresh or health or healthy or nutrition or nutritional or nutritive or "nutrient rich" or "nutrient dense" or adequate or quality or sufficient or insufficient or secure or insecure or safe):ti,ab,kw or diet:kw)
#5 ((policy or policies) near/5 (food or foods or fruit or fruits or vegetable or vegetables or nutrition or grocer* or meal or meals)):ti,ab,kw
#6 ((council or councils or coalition or coalitions or co‐op or co‐ops or co‐operative*) near/5 (food or foods or fruit or fruits or vegetable or vegetables or nutrition or grocer*)):ti,ab,kw
#7 (access* near/3 food):ti,ab,kw
#8 {or #1‐#7}
#9 ((deliver or delivery or deliveries or transport or transportation or distribute or distributes or distribution) near/3 (groceries or meal or meals or fruit or fruits or vegetable or vegetables or food or foods)):ti,ab,kw
#10 (outreach or service or services or scheme or schemes or program or programs or programme or programmes or policy or policies or project or projects or nutrition or nutritional or home or home‐based or homes or community or communities or neighbor or neighborhood or neighbour or neighbourhood or rural or urban or provide or provision or choice or control):ti,ab,kw
#11 social welfare:kw
#12 #9 and (#10 or #11)
#13 (("public transport" or "transport service*" or "transportation service*" or "transport scheme" or travel or travelling or infrastructure or access) near/5 ("food store*" or "food shop*" or "food retail*" or "food outlet" or supermarket or grocer*)):ti,ab,kw
#14 ((payment or payments or benefit or benefits or money or purchase or purchasing or purchases or buy or buying or welfare or financing or cash or income) near/5 (food or foods or foodstuff* or groceries or fruit or fruits or vegetable or vegetables or nutrition or nutritional or meal or meals) near/10 (supplement or supplementation or assist or assistance or extra or aid or support or help)):ti,ab,kw
#15 ((tax or taxes or taxation or subsidy or subsidies or subsidized or subsidised or voucher* or coupon* or discount*) near/5 (food or foods or foodstuff* or grocer* or fruit* or vegetable* or nutrition or nutritional or meal or meals)):ti,ab,kw
#16 (("Cash transfer*" or "social protection") and (food or foods or foodstuff* or grocer* or fruit* or vegetable* or nutrition or nutritional or meal or meals)):ti,ab,kw
#17 (("community nutrition" or "public health nutrition" or "food access") and (project* or program*)):ti,ab,kw
#18 [mh "food assistance"]
#19 [mh ^Food/ec]
#20 [mh Diet/ec]
#21 {or #12‐#20}
#22 #8 or #21
#23 (Afghan* or Bangladesh* or Benin* or "Burkina Faso" or Burkinabe or Burundi* or Cambodia* or "Central African*" or Chad* or Comoros or Comorian* or Congo* or Eritrea* or Ethiopia* or Gambia* or Ghana* or Guinea‐Bissau* or Haiti* or Kenya* or Kyrgyz* or Lao* or Liberia* or Madagascar or Malagasy or Malawi* or Mali* or Mauritania* or Mozambique or Mozambican or Myanmar* or Burma or Burmese or Nepal* or Niger* or Rwanda* or "Sierra Leone*" or "Solomon Island*" or Somali* or Tajikistan* or Tanzania* or Togo* or Uganda* or Zambia* or Zimbabwe*)
#24 (Angola* or Armenia* or Belize* or Bhutan* or Bolivia* or Cameroon* or "Cape Verd*" or China or Chinese or "Cote d'Ivoire" or Ivorian or Djibouti or Ecuador* or Egypt* or "El Salvador" or Salvadoran or Guatemala* or Guyana or Guyanese or Hondura* or India* or Indonesia* or Iraq* or Jordan* or Kiribati or Kosov* or Lesotho or Mosotho or Basotho or Maldiv* or "Marshall Islands" or Marshallese or Micronesia* or Moldova* or Mongolia* or Morocc* or Nicaragua* or Nigeria* or Pakistan* or "Papua New Guinea*" or Paraguay* or Philippines or Filipino or Samoa* or Senegal* or "Sri Lanka*" or Sudan* or Swaziland or Swazi or Syrian or Syria* or Thailand or Thai or Timor* or Tonga* or Tunisia* or Turkmen* or Tuvalu* or Ukrain* or Uzbekistan* or Uzbek or Vanuatu or Vietnam* or "West Bank" or Gaza or Palestinian* or Yemen*)
#25 (Albania* or Algeria* or Samoa or Antigua* or Barbuda* or Argentin* or Azerbaijan* or Belarus* or Bosnia* or Herzegovin* or Botswana or Motswana or Batswana or Brazil* or Bulgaria* or Chile* or Colombia* or Costa Rica* or Cuba* or Dominica* or "Dominican Republic" or Fiji* or Gabon* or Grenad* or Iran* or Jamaica* or Kazakhstan* or Leban* or Libya* or Lithuania* or Macedonia* or Malaysia* or Mauriti* or Mayotte or Mahoran or Mexic* or Montenegr* or Namibia* or Palau* or Panama* or Peru* or Romania* or Russia* or Serbia* or Seychell* or "South Africa*" or "St Lucia*" or Suriname* or Turk* or Uruguay* or Venezuela*)
#26 [mh "developing countries"]
#27 (lmic or lmics):ti,ab,kw
#28 (("low income" or "medium income") near/5 (country or countries or nation or nations or state or states)):ti,ab,kw
#29 ("least developed" next (country or countries or nation or nations or state or states)):ti,ab,kw
#30 (developing next (country or countries or nation or nations or state or states)):ti,ab,kw
#31 ("united nations" or "world health organization" or "world bank" or unicef):ti,ab,kw and ((food or nutrition*) near/3 (program* or project* or fund)):ti,ab,kw
#32 {or #23‐#31}
#33 #22 and #32
#34 #33 in Trials
#35 #34 Publication Year from 1980 to 2016
Embase Session Results (16 Sep 2016)
#1 'food security'/exp OR 'food availability'/exp
#2 'food insecurity'/exp
#3 'food secur*':ab,ti OR 'food insecur*':ab,ti OR 'food poverty':ab,ti OR 'food sufficien*':ab,ti OR 'food insufficien*':ab,ti OR 'food desert*':ab,ti OR (access* NEAR/3 food):ab,ti
#4 ((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)):ab,ti
#5 ((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer* OR supermarket* OR 'food store*' OR 'food shop*' OR 'corner store*' OR cafeteria* OR canteen* OR 'food outlet*') NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)):ab,ti
#6 'agrifood system*':ab,ti OR 'food system*':ab,ti AND (fresh:ab,ti OR health:ab,ti OR healthy:ab,ti OR nutrition:ab,ti OR nutritional:ab,ti OR nutritive:ab,ti OR 'nutrient rich':ab,ti OR 'nutrient dense':ab,ti OR adequate:ab,ti OR quality:ab,ti OR sufficient:ab,ti OR insufficient:ab,ti OR secure:ab,ti OR insecure:ab,ti OR safe:ab,ti OR 'diet'/de)
#7 ((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)):ab,ti
#8 ((council OR councils OR coalition OR coalitions OR 'co op' OR 'co ops' OR 'co operative*') NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)):ab,ti
#9 ((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)):ab,ti
#10 outreach:ab,ti OR service:ab,ti OR services:ab,ti OR scheme:ab,ti OR schemes:ab,ti OR program:ab,ti OR programs:ab,ti OR programme:ab,ti OR programmes:ab,ti OR policy:ab,ti OR policies:ab,ti OR project:ab,ti OR projects:ab,ti OR nutrition:ab,ti OR nutritional:ab,ti OR home:ab,ti OR 'home based':ab,ti OR homes:ab,ti OR community:ab,ti OR communities:ab,ti OR neighbor:ab,ti OR neighborhood:ab,ti OR neighbour:ab,ti OR neighbourhood:ab,ti OR rural:ab,ti OR urban:ab,ti OR provide:ab,ti OR provision:ab,ti OR choice:ab,ti OR control:ab,ti
#11 'social welfare'/exp
#12 #9 AND (#10 OR #11)
#13 (('public transport' OR 'transport service*' OR 'transportation service*' OR 'transport scheme' OR travel OR travelling OR infrastructure OR access) NEAR/5 ('food store*' OR 'food shop*' OR 'food retail*' OR 'food outlet' OR supermarket OR grocer*)):ab,ti
#14 ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)):ab,ti
#15 ((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)):ab,ti
#16 'cash transfer*':ab,ti OR 'social protection':ab,ti AND (food:ab,ti OR foods:ab,ti OR foodstuff*:ab,ti OR grocer*:ab,ti OR fruit*:ab,ti OR vegetable*:ab,ti OR nutrition:ab,ti OR nutritional:ab,ti OR meal:ab,ti OR meals:ab,ti)
#17 'community nutrition':ab,ti OR 'public health nutrition':ab,ti OR 'food access':ab,ti AND (project*:ab,ti OR program*:ab,ti)
#18 'food assistance'/exp
#19 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18
#20 afghan*:de,ab,ti OR bangladesh*:de,ab,ti OR benin*:de,ab,ti OR 'burkina faso':de,ab,ti OR burkinabe:de,ab,ti OR burundi*:de,ab,ti OR cambodia*:de,ab,ti OR 'central african*':de,ab,ti OR chad*:de,ab,ti OR comoros:de,ab,ti OR comorian*:de,ab,ti OR congo*:de,ab,ti OR eritrea*:de,ab,ti OR ethiopia*:de,ab,ti OR gambia*:de,ab,ti OR ghana*:de,ab,ti OR 'guinea bissau*':de,ab,ti OR haiti*:de,ab,ti OR kenya*:de,ab,ti OR kyrgyz*:de,ab,ti OR lao*:de,ab,ti OR liberia*:de,ab,ti OR madagascar:de,ab,ti OR malagasy:de,ab,ti OR malawi*:de,ab,ti OR mali*:de,ab,ti OR mauritania*:de,ab,ti OR mozambique:de,ab,ti OR mozambican:de,ab,ti OR myanmar*:de,ab,ti OR burma:de,ab,ti OR burmese:de,ab,ti OR nepal*:de,ab,ti OR niger*:de,ab,ti OR rwanda*:de,ab,ti OR 'sierra leone*':de,ab,ti OR 'solomon island*':de,ab,ti OR somali*:de,ab,ti OR tajikistan*:de,ab,ti OR tanzania*:de,ab,ti OR togo*:de,ab,ti OR uganda*:de,ab,ti OR zambia*:de,ab,ti OR zimbabwe*:de,ab,ti
#21 angola*:de,ab,ti OR armenia*:de,ab,ti OR belize*:de,ab,ti OR bhutan*:de,ab,ti OR bolivia*:de,ab,ti OR cameroon*:de,ab,ti OR 'cape verd*':de,ab,ti OR china:de,ab,ti OR chinese:de,ab,ti OR (cote NEXT/1 ivoire):de,ab,ti OR ivorian:de,ab,ti OR djibouti:de,ab,ti OR ecuador*:de,ab,ti OR egypt*:de,ab,ti OR 'el salvador':de,ab,ti OR salvadoran:de,ab,ti OR guatemala*:de,ab,ti OR guyana:de,ab,ti OR guyanese:de,ab,ti OR hondura*:de,ab,ti OR india*:de,ab,ti OR indonesia*:de,ab,ti OR iraq*:de,ab,ti OR jordan*:de,ab,ti OR kiribati:de,ab,ti OR kosov*:de,ab,ti OR lesotho:de,ab,ti OR mosotho:de,ab,ti OR basotho:de,ab,ti OR maldiv*:de,ab,ti OR 'marshall islands':de,ab,ti OR marshallese:de,ab,ti OR micronesia*:de,ab,ti OR moldova*:de,ab,ti OR mongolia*:de,ab,ti OR morocc*:de,ab,ti OR nicaragua*:de,ab,ti OR nigeria*:de,ab,ti OR pakistan*:de,ab,ti OR 'papua new guinea*':de,ab,ti OR paraguay*:de,ab,ti OR philippines:de,ab,ti OR filipino:de,ab,ti OR samoa*:de,ab,ti OR senegal*:de,ab,ti OR 'sri lanka*':de,ab,ti OR sudan*:de,ab,ti OR swaziland:de,ab,ti OR swazi:de,ab,ti OR syrian:de,ab,ti OR syria*:de,ab,ti OR thailand:de,ab,ti OR thai:de,ab,ti OR timor*:de,ab,ti OR tonga*:de,ab,ti OR tunisia*:de,ab,ti OR turkmen*:de,ab,ti OR tuvalu*:de,ab,ti OR ukrain*:de,ab,ti OR uzbekistan*:de,ab,ti OR uzbek:de,ab,ti OR vanuatu:de,ab,ti OR vietnam*:de,ab,ti OR 'west bank':de,ab,ti OR gaza:de,ab,ti OR palestinian*:de,ab,ti OR yemen*:de,ab,ti
#22 albania*:de,ab,ti OR algeria*:de,ab,ti OR samoa:de,ab,ti OR antigua*:de,ab,ti OR barbuda*:de,ab,ti OR argentin*:de,ab,ti OR azerbaijan*:de,ab,ti OR belarus*:de,ab,ti OR bosnia*:de,ab,ti OR herzegovin*:de,ab,ti OR botswana:de,ab,ti OR motswana:de,ab,ti OR batswana:de,ab,ti OR brazil*:de,ab,ti OR bulgaria*:de,ab,ti OR chile*:de,ab,ti OR colombia*:de,ab,ti OR costa:de,ab,ti AND rica*:de,ab,ti OR cuba*:de,ab,ti OR dominica*:de,ab,ti OR 'dominican republic':de,ab,ti OR fiji*:de,ab,ti OR gabon*:de,ab,ti OR grenad*:de,ab,ti OR iran*:de,ab,ti OR jamaica*:de,ab,ti OR kazakhstan*:de,ab,ti OR leban*:de,ab,ti OR libya*:de,ab,ti OR lithuania*:de,ab,ti OR macedonia*:de,ab,ti OR malaysia*:de,ab,ti OR mauriti*:de,ab,ti OR mayotte:de,ab,ti OR mahoran:de,ab,ti OR mexic*:de,ab,ti OR montenegr*:de,ab,ti OR namibia*:de,ab,ti OR palau*:de,ab,ti OR panama*:de,ab,ti OR peru*:de,ab,ti OR romania*:de,ab,ti OR russia*:de,ab,ti OR serbia*:de,ab,ti OR seychell*:de,ab,ti OR 'south africa*':de,ab,ti OR 'st lucia*':de,ab,ti OR suriname*:de,ab,ti OR turk*:de,ab,ti OR uruguay*:de,ab,ti OR venezuela*:de,ab,ti
#23 'developing country'/exp
#24 lmic:ab,ti OR lmics:ab,ti
#25 (('low income' OR 'medium income') NEAR/5 (country OR countries OR nation OR nations OR state OR states)):ab,ti
#26 ('least developed' NEXT/1 (country OR countries OR nation OR nations OR state OR states)):ab,ti
#27 (developing NEXT/1 (country OR countries OR nation OR nations OR state OR states)):ab,ti
#28 'united nations':ab,ti OR 'world health organization':ab,ti OR 'world bank':ab,ti OR unicef:ab,ti AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)):ab,ti
#29 #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28
#30 #19 AND #29
#31 'animal'/exp NOT 'human'/exp
#32 #30 NOT #31
#33 [controlled clinical trial]/lim OR [randomized controlled trial]/lim
#34 randomized:de,ab,ti OR placebo:de,ab,ti OR (random*:de,ab,ti AND trial*:de,ab,ti AND group*:de,ab,ti)
#35 random*:de,ab,ti OR placebo:de,ab,ti OR (random*:de,ab,ti AND trial*:de,ab,ti AND group*:de,ab,ti)
#36 'comparative study'/de
#37 'control group'/exp OR 'follow up'/exp OR 'prospective study'/exp OR 'epidemiology'/de OR 'time series analysis'/exp OR 'retrospective study'/exp OR 'longitudinal study'/exp OR 'pretest posttest control group design'/exp
#38 'control group*':ab,ti OR 'follow up':ab,ti OR prospectiv*:ab,ti OR 'non random*':ab,ti OR nonrandom*:ab,ti
#39 'before after stud*':ab,ti OR 'before and after':ab,ti OR 'time series':ab,ti OR retrospective*:ab,ti OR longitud*:ab,ti
#40 controlled:de,ab,ti AND cohort*:de,ab,ti AND stud*:de,ab,ti
#41 'controlled before':ab,ti OR 'pre test':ab,ti OR pretest:ab,ti OR posttest:ab,ti OR 'post test':ab,ti OR 'pre intervention':ab,ti OR 'post intervention':ab,ti
#42 #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41
#43 #32 AND #42
#44 #43 AND [1980‐2016]/py
#45 #44 AND [embase]/lim
| GreenFILE 16 September 2016 | ||
| # | Query | Limiters/Expanders |
| S1 | DE "FOOD consumption" | Search modes ‐ Boolean/Phrase |
| S2 | (food secur* OR food insecur* OR food poverty OR food sufficien* OR food insufficien* OR food desert*) | Search modes ‐ Boolean/Phrase |
| S3 | ((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) N5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) | Search modes ‐ Boolean/Phrase |
| S4 | ((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket OR supermarkets OR grocery store OR grocery stores OR food store OR food stores OR food shop OR food shops OR corner store OR corner stores OR cafeteria OR cafeterias OR canteen* OR food outlet*) N5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) | Search modes ‐ Boolean/Phrase |
| S5 | food system* AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR nutrient rich OR nutrient dense OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe OR diet) | Search modes ‐ Boolean/Phrase |
| S6 | ((policy OR policies) N5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) | Search modes ‐ Boolean/Phrase |
| S7 | ((council OR councils OR coalition OR coalitions OR co‐op OR co‐ops OR co‐operative*) N5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) | Search modes ‐ Boolean/Phrase |
| S8 | (access* N3 food) | Search modes ‐ Find all my search terms |
| S9 | ( ((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) N3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)) ) AND ( (outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR home‐based OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control OR welfare) ) | Search modes ‐ Boolean/Phrase |
| S10 | ((public transport OR transport service* OR transportation service* OR transport scheme OR travel OR travelling OR infrastructure OR access) N5 (food store* OR food shop* OR food retail* OR food outlet OR supermarket OR grocer*)) | Search modes ‐ Boolean/Phrase |
| S11 | ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) N5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) N10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) | Search modes ‐ Boolean/Phrase |
| S12 | ((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) N5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) | Search modes ‐ Boolean/Phrase |
| S13 | ((Cash transfer* OR social protection) AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) | Search modes ‐ Boolean/Phrase |
| S14 | ((community nutrition OR public health nutrition OR food access) AND (project* OR program*)) | Search modes ‐ Boolean/Phrase |
| S15 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 | Search modes ‐ Find all my search terms |
| S16 | (Afghan* OR Bangladesh* OR Benin* OR Burkina Faso OR Burkinabe OR Burundi* OR Cambodia* OR Central African Republic OR Central African* OR Chad* OR Comoros OR Comorian* OR Congo* OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea‐Bissau* OR Haiti* OR Kenya* OR Kyrgyz Republic OR Kyrgyzstani OR Lao* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Mozambique OR Mozambican OR Myanmar* OR Burma OR Burmese OR Nepal* OR Niger* OR Rwanda* OR Sierra Leone* OR Solomon Islands OR Solomon Islanders OR Somali* OR Tajikistan* OR Tanzania* OR Togo* OR Uganda* OR Zambia* OR Zimbabwe*) | Search modes ‐ Boolean/Phrase |
| S17 | (Angola* OR Armenia* OR Belize* OR Bhutan* OR Bolivia* OR Cameroon* OR Cape Verd* OR China OR Chinese OR Cote dIvoire OR Ivorian OR Djibouti OR Ecuador* OR Egypt* OR El Salvador OR Salvadoran OR Guatemala* OR Guyana OR Guyanese OR Hondura* OR India* OR Indonesia* OR Iraq* OR Jordan* OR Kiribati OR Kosov* OR Lesotho OR Mosotho OR Basotho OR Maldiv* OR Marshall Islands OR Marshallese OR Micronesia* OR Moldova* OR Mongolia* OR Morocc* OR Nicaragua* OR Nigeria* OR Pakistan* OR Papua New Guinea* OR Paraguay* OR Philippines OR Filipino OR Samoa* OR Senegal* OR Sri Lanka* OR Sudan* OR Swaziland OR Swazi OR Syrian Arab Republic OR Syria* OR Thailand OR Thai OR Timor Leste OR East Timorese OR Tonga* OR Tunisia* OR Turkmen* OR Tuvalu* OR Ukrain* OR Uzbekistan* OR Uzbek OR Vanuatu OR Vietnam* OR West Bank OR Gaza OR Palestinian* OR Yemen*) | Search modes ‐ Boolean/Phrase |
| S18 | (Albania* OR Algeria* OR American Samoa OR Antigua* OR Barbuda* OR Argentin* OR Azerbaijan* OR Belarus* OR Bosnia* OR Herzegovin* OR Botswana OR Motswana OR Batswana OR Brazil* OR Bulgaria* OR Chile* OR Colombia* OR Costa Rica* OR Cuba* OR Dominica* OR Dominican Republic OR Fiji* OR Gabon* OR Grenad* OR Iran* OR Jamaica* OR Kazakhstan* OR Leban* OR Libya* OR Lithuania* OR Macedonia* OR Malaysia* OR Mauriti* OR Mayotte OR Mahoran OR Mexic* OR Montenegr* OR Namibia* OR Palau* OR Panama* OR Peru* OR Romania* OR Russia* OR Serbia* OR Seychell* OR South Africa* OR St Lucia* OR Suriname* OR Turk* OR Uruguay* OR Venezuela*) | Search modes ‐ Boolean/Phrase |
| S19 | (lmic OR lmics) | Search modes ‐ Find all my search terms |
| S20 | ((low income OR medium income) N5 (country OR countries OR nation OR nations OR state OR states)) | Search modes ‐ Boolean/Phrase |
| S21 | (least developed N1 (country OR countries OR nation OR nations OR state OR states)) | Search modes ‐ Boolean/Phrase |
| S22 | (developing N1 (country OR countries OR nation OR nations OR state OR states)) | Search modes ‐ Boolean/Phrase |
| S23 | (united nations OR world health organization OR world bank OR unicef OR ((food OR nutrition*) N3 (program* OR project* OR fund))) | Search modes ‐ Boolean/Phrase |
| S24 | S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 | Search modes ‐ Find all my search terms |
| S25 | S15 AND S24 | Limiters ‐ Publication Date: 19800101‐20161231 |
| S26 | compar* AND (study OR trial OR program*) | Search modes ‐ Boolean/Phrase |
| S27 | random* OR controlled OR placebo OR control group* | Search modes ‐ Boolean/Phrase |
| S28 | follow up | Search modes ‐ Boolean/Phrase |
| S29 | prospectiv* OR non‐random* OR nonrandom* | Search modes ‐ Boolean/Phrase |
| S30 | before after stud* OR (time AND series) OR retrospectiv* OR longitud* | Search modes ‐ Boolean/Phrase |
| S31 | control* AND cohort* AND study | Search modes ‐ Boolean/Phrase |
| S32 | "before and after" | Search modes ‐ Boolean/Phrase |
| S33 | pre test OR pretest OR posttest OR post test OR pre intervention OR post intervention | Search modes ‐ Boolean/Phrase |
| S34 | S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 | Search modes ‐ Find all my search terms |
| S35 | S25 AND S34 | Search modes ‐ Boolean/Phrase |
| AfricaBib 15 July 2016 | ||
| Field | Search | Mode |
| Title | food security | exact phrase |
| Title | food insecurity | exact phrase |
| Title | food access | whole words |
| Title | food poverty | exact phrase |
| Title | food sufficiency | exact phrase |
| Title | nutrition security | exact phrase |
| Title | food insufficiency | exact phrase |
| Title | healthy food | whole field |
| Title | nutritious food | whole field |
| Subject | food security | whole words |
| Subject | food insecurity | whole words |
| Subject | food access | whole field |
| Subject | food poverty | whole words |
| Subject | food sufficiency | whole words |
| Subject | nutrition security | whole words |
| Subject | food insufficiency | whole words |
| Subject | healthy food | whole field |
| Subject | nutritious food | whole field |
| Abstract | food security | exact phrase |
| Abstract | food insecurity | exact phrase |
| Abstract | healthy food access | whole words |
| Abstract | nutritious food access | whole words |
| Abstract | food poverty | exact phrase |
| Abstract | food sufficiency | exact phrase |
| Abstract | nutrition security | exact phrase |
| Abstract | food insufficiency | exact phrase |
AGRIS (16 September 2016)
(""food security"" OR ""food insecurity"" OR ""food poverty"" OR ""food sufficiency"" OR ""food insufficiency"" OR ""food desert"" OR ""food access"" OR ""nutrition security"" OR ""food purchase"") AND ((random* OR controlled OR placebo OR ""control group"" OR ""follow up"" OR prospectiv* OR non‐random* OR nonrandom* OR ""before and after"" OR ""time series"" OR retrospective* OR longitud* OR ""pre test"" OR pretest OR posttest OR ""post test"" OR ""pre intervention"" OR ""post intervention"") OR (control* AND cohort* AND study)) OR (compar* AND (study OR trial OR program*)) +publicationDate:[1980 TO 2016]
Agricola 16 September 2016
Database Name: Article Citation Database
Search Request: Command = (T000 OR U000) AND ("food supply" OR "food insecurity" OR "food secure" OR "food purchase" OR "food access" OR "food price" OR "food environment" OR "food security" OR "nutrition security" OR "food purchase")
Published after 1979
Search Results: 975 entries.
Subject category codes
Human Nutrition (T000)
Home Economics and Human Ecology (U000)
| Africa‐Wide Information (Ebsco) 17 September 2016 | ||
| # | Query | Limiters/Expanders |
| S1 | (food secur* OR food insecur* OR food poverty OR food sufficien* OR food insufficien* OR food desert* OR nutrition secur*) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S2 | ((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) N5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S3 | ((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer* OR supermarket* OR food store* OR food shop* OR corner store* OR cafeteria* OR canteen* OR food outlet*) N5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S4 | food system* AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR nutrient rich OR nutrient dense OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S5 | ((policy OR policies) N5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S6 | ((council OR councils OR coalition OR coalitions OR co‐op OR co‐ops OR co‐operative*) N5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR grocer*)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S7 | (access* N3 food) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S8 | ( ((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) N3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)) ) AND ( (outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR home‐based OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control OR welfare) ) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S9 | ((public transport OR transport service* OR transportation service* OR transport scheme OR travel OR travelling OR infrastructure OR access) N5 (food store* OR food shop* OR food retail* OR food outlet OR supermarket* OR grocer*)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S10 | ((payment* OR benefit* OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) N5 (food OR foods OR foodstuff* OR grocer* OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) N10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S11 | ((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) N5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S12 | ((Cash transfer* OR social protection) AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S13 | ((community nutrition OR public health nutrition OR food access) AND (project* OR program*)) | Limiters ‐ Data Contributor: AFRICAN HEALTHLINE, .....African Journals Online |
| S14 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 | Limiters ‐ Year Published: 1980‐2015 |
| S15 | compar* AND (study OR trial OR program*) | Search modes ‐ Boolean/Phrase |
| S16 | random* OR controlled OR placebo OR control group* | Search modes ‐ Boolean/Phrase |
| S17 | follow up | Search modes ‐ Boolean/Phrase |
| S18 | prospectiv* OR non‐random* OR nonrandom* | Search modes ‐ Boolean/Phrase |
| S19 | before after stud* OR (time AND series) OR retrospectiv* OR longitud* | Search modes ‐ Boolean/Phrase |
| S20 | control* AND cohort* AND study | Search modes ‐ Boolean/Phrase |
| S21 | "before and after" | Search modes ‐ Boolean/Phrase |
| S22 | pre test OR pretest OR posttest OR post test OR pre intervention OR post intervention | Search modes ‐ Boolean/Phrase |
| S23 | S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 | Search modes ‐ Boolean/Phrase |
| S24 | S14 AND S23 | Search modes ‐ Boolean/Phrase |
Trials Register of Promoting Health Interventions (TRoPHI) 17 September 2016
1 Freetext (All but Authors): "secur*" OR "insecur*" OR "access*" OR "purchas*" OR "expen*" OR "price*" OR "availab*"
2 Focus of the report: healthy eating
3 In which country/countries was the study carried out?: Developing countries
4 1 AND 2 AND 3
5 Freetext (All but Authors): "food security" OR "food insecurity" OR "nutrition security"
6 Freetext (All but Authors): "food" NEAR "access*"
7 4 OR 5 OR 6
WHO Global Index Medicus (17 September 2016)
(ti:((food* OR fruit* OR vegetable* OR nutrition*) AND (secur* OR access* OR supply OR price* OR insecur* OR purchas*))) AND (instance:"ghl") AND ( db:("LILACS" OR "WPRIM" OR "IMSEAR" OR "IMEMR" OR "WHOLIS" OR "BDENF"))
tw:("food security" OR "food insecurity" OR "food poverty" OR "food sufficiency" OR "nutrition security" OR "food insufficiency" OR "food insufficience") AND (instance:"ghl") AND ( db:("LILACS" OR "WPRIM" OR "IMSEAR" OR "IMEMR" OR "WHOLIS" OR "BDENF"))
mh:("Food and Nutrition Security" OR "World Food Programme") AND (instance:"ghl") AND ( db:("LILACS" OR "WPRIM" OR "IMSEAR" OR "IMEMR" OR "WHOLIS" OR "BDENF"))
Web of Science 17 September 2016
# 1 TOPIC: ("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/2 food))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 2 TS=((food* OR fruit* OR vegetable* OR grocer* OR meal OR diet) NEAR/4 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 3 TOPIC: (((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/4 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 4 TS=(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe OR diet))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 5 TOPIC: (((policy OR policies) NEAR/4 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 6 TOPIC: (((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/4 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 7 TOPIC: (((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/2 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 8 TOPIC: ((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/4 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 9 TOPIC: (((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/4 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/9 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 10 TOPIC: (((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/4 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 11 TS=(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 12 TS=(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 13 #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 14 TOPIC: (afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe*)
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 15 TOPIC: (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen*)
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 16 TOPIC: (albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela*)
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 17 TOPIC: (lmic OR lmics)
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 18 TS=((("low income" OR "medium income") AND (country OR countries OR nation OR nations OR state OR states)))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 19 TS=("developing countr*" OR "developing nation*" OR "developing state*")
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 20 TS=("least developed countr*" OR "least developed nation*" OR "least developed state*")
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 21 TS=(("united nations" OR "world health organization" OR "world bank" OR unicef) AND (food OR nutrition*) AND (program* OR project* OR fund))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 22 #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 23 #22 AND #13
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 24 TOPIC: (compar* AND (study OR trial OR program*))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 25 TOPIC: (random* OR controlled OR placebo OR "control group*")
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 26 TOPIC: ("follow up")
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 27 TOPIC: (prospectiv* OR non‐random* OR nonrandom*)
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 28 TOPIC: (("before after stud*" OR "time series" OR retrospectiv* OR longitud*))
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 29 TOPIC: (control* AND cohort* AND study)
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 30 TOPIC: ("before and after")
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 31 TOPIC: ("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention")
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 32 #31 OR #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
# 33 #32 AND #23
Indexes=SCI‐EXPANDED, SSCI, CPCI‐S Timespan=1980‐2016
Refined by: [excluding] WEB OF SCIENCE CATEGORIES: ( PLANT SCIENCES OR ZOOLOGY OR VETERINARY SCIENCES )
# 34 #32 AND #23
Sociological Abstracts (ProQuest)
September 17 2016 15:06
S1 SU.EXACT("Food Security")
S2 ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )
S3 ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )
S4 ab(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) ) OR ti(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) )
S5 ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )
S6 ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )
S7 ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )
S8 ((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND SU.EXACT("Social Welfare")
S9 ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )
S10 ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help))
S11 ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )
S12 ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )
S13 ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) )
S14 SU.EXACT("Food Security") OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) ) OR ti(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND SU.EXACT("Social Welfare") ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))
S15 (afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* )
S16 SU.EXACT("Developing Countries")
S17 lmic OR lmics
S18 (("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states))
S19 ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states))
S20 (developing NEAR/1 (country OR countries OR nation OR nations OR state OR states))
S21 ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund))
S22 ((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR SU.EXACT("Developing Countries") OR (lmic OR lmics) OR (("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)))
S23 (SU.EXACT("Food Security") OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) ) OR ti(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND SU.EXACT("Social Welfare") ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))) AND (((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR SU.EXACT("Developing Countries") OR (lmic OR lmics) OR (("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund))))
S24 (SU.EXACT("Food Security") OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) ) OR ti(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND SU.EXACT("Social Welfare") ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))) AND (((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR SU.EXACT("Developing Countries") OR (lmic OR lmics) OR (("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)))) AND pd(19800101‐20161231)
S25 (compar* AND (study OR trial OR program*)) OR ((random* OR controlled OR placebo OR "control group*") OR ("follow up")) OR ((prospectiv* OR non‐random* OR nonrandom*) OR ("before after stud*" OR (time AND series) OR retrospectiv* OR longitud*)) OR ( (control* AND cohort* AND study) OR ("before and after")) OR ("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention") OR (SU.EXACT("Cohort Analysis") OR SU.EXACT("Research Subjects") OR SU.EXACT("Time Series Analysis") OR SU.EXACT("Random Samples") OR SU.EXACT("Comparative Analysis") OR SU.EXACT("Longitudinal Studies"))
S26 ((SU.EXACT("Food Security") OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) ) OR ti(((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket* OR "grocery store*" OR "food store*" OR "food shop*" OR "corner store*" OR cafeteria* OR canteen* OR "food outlet*") NEAR/5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND SU.EXACT("Social Welfare") ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))) AND (((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR SU.EXACT("Developing Countries") OR (lmic OR lmics) OR (("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR (("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)))) AND pd(19800101‐20161231)) AND ((compar* AND (study OR trial OR program*)) OR ((random* OR controlled OR placebo OR "control group*") OR ("follow up")) OR ((prospectiv* OR non‐random* OR nonrandom*) OR ("before after stud*" OR (time AND series) OR retrospectiv* OR longitud*)) OR ( (control* AND cohort* AND study) OR ("before and after")) OR ("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention") OR (SU.EXACT("Cohort Analysis") OR SU.EXACT("Research Subjects") OR SU.EXACT("Time Series Analysis") OR SU.EXACT("Random Samples") OR SU.EXACT("Comparative Analysis") OR SU.EXACT("Longitudinal Studies")) )
International Bibliography of the Social Sciences (IBSS) (ProQuest)
September 17 2016 16:28
S1 SU.EXACT("Food security") OR SU.EXACT("Food safety") OR SU.EXACT("Food policy") OR SU.EXACT("Food price policy")
S2 ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )
S3 ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )
S4 ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )
S5 ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )
S6 ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )
S7 ((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND (SU.EXACT("Social Welfare") OR SU.EXACT("Social support"))
S8 ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )
S9 ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help))
S10 ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )
S11 ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )
S12 ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) )
S13 (SU.EXACT("Food security") OR SU.EXACT("Food safety") OR SU.EXACT("Food policy") OR SU.EXACT("Food price policy")) OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND (SU.EXACT("Social Welfare") OR SU.EXACT("Social support")) ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))
S14 (afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* )
S15 SU.EXACT("Developing countries") OR SU.EXACT("Less developed countries") OR SU.EXACT("Developing areas")
S16 (lmic OR lmics) OR ((("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) ) OR ((developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)) )
S17 ((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR (SU.EXACT("Developing countries") OR SU.EXACT("Less developed countries") OR SU.EXACT("Developing areas")) OR ((lmic OR lmics) OR ((("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) ) OR ((developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)) ))
S18 ((SU.EXACT("Food security") OR SU.EXACT("Food safety") OR SU.EXACT("Food policy") OR SU.EXACT("Food price policy")) OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND (SU.EXACT("Social Welfare") OR SU.EXACT("Social support")) ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))) AND (((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR (SU.EXACT("Developing countries") OR SU.EXACT("Less developed countries") OR SU.EXACT("Developing areas")) OR ((lmic OR lmics) OR ((("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) ) OR ((developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)) )))
S19 ((SU.EXACT("Food security") OR SU.EXACT("Food safety") OR SU.EXACT("Food policy") OR SU.EXACT("Food price policy")) OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND (SU.EXACT("Social Welfare") OR SU.EXACT("Social support")) ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))) AND (((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR (SU.EXACT("Developing countries") OR SU.EXACT("Less developed countries") OR SU.EXACT("Developing areas")) OR ((lmic OR lmics) OR ((("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) ) OR ((developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)) ))) AND pd(19800101‐20161231)
S20 SU.EXACT("Comparative analysis") OR SU.EXACT("Long‐term analysis") OR SU.EXACT("Time series") OR SU.EXACT("Random sampling") OR SU.EXACT("Control groups") OR SU.EXACT("Cohort analysis")
S21 (compar* AND (study OR trial OR program*)) OR ((random* OR controlled OR placebo OR "control group*") OR ("follow up")) OR ((prospectiv* OR non‐random* OR nonrandom*) OR ("before after stud*" OR (time AND series) OR retrospectiv* OR longitud*)) OR ( (control* AND cohort* AND study) OR ("before and after")) OR ("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention")
S22 (SU.EXACT("Comparative analysis") OR SU.EXACT("Long‐term analysis") OR SU.EXACT("Time series") OR SU.EXACT("Random sampling") OR SU.EXACT("Control groups") OR SU.EXACT("Cohort analysis")) OR ((compar* AND (study OR trial OR program*)) OR ((random* OR controlled OR placebo OR "control group*") OR ("follow up")) OR ((prospectiv* OR non‐random* OR nonrandom*) OR ("before after stud*" OR (time AND series) OR retrospectiv* OR longitud*)) OR ( (control* AND cohort* AND study) OR ("before and after")) OR ("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention") )
S23 (((SU.EXACT("Food security") OR SU.EXACT("Food safety") OR SU.EXACT("Food policy") OR SU.EXACT("Food price policy")) OR (ab("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food)) OR ti("food secur*" OR "food insecur*" OR "food poverty" OR "food sufficien*" OR "food insufficien*" OR "food desert*" OR (access* NEAR/3 food) )) OR (ab(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) ) OR ti(((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) NEAR/5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) )) OR (ab(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) ) OR ti(("agrifood system*" OR "food system*") AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR "nutrient rich" OR "nutrient dense" OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) )) OR (ab(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) ) OR ti(((policy OR policies) NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) )) OR (ab(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) ) OR ti(((council OR councils OR coalition OR coalitions OR "co op" OR "co ops" OR "co operative*") NEAR/5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) )) OR (((ab(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods))) OR ti(((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) NEAR/3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)))) OR (ab(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control) OR ti(outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR "home based" OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control))) AND (SU.EXACT("Social Welfare") OR SU.EXACT("Social support")) ) OR (ab((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) ) OR ti((("public transport" OR "transport service*" OR "transportation service*" OR "transport scheme" OR travel OR travelling OR infrastructure OR access) NEAR/5 ("food store*" OR "food shop*" OR "food retail*" OR "food outlet" OR supermarket OR grocer*)) )) OR ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) NEAR/5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) NEAR/10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) OR (ab(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) ) OR ti(((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) NEAR/5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) )) OR (ab(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) ) OR ti(("cash transfer*" OR "social protection") AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals) )) OR (ab(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ) OR ti(("community nutrition" OR "public health nutrition" OR "food access") AND (project* OR program*) ))) AND (((afghan* OR bangladesh* OR benin* OR "burkina faso" OR burkinabe OR burundi* OR cambodia* OR "central african*" OR chad* OR comoros OR comorian* OR congo* OR eritrea* OR ethiopia* OR gambia* OR ghana* OR "guinea bissau*" OR haiti* OR kenya* OR kyrgyz* OR lao* OR liberia* OR madagascar OR malagasy OR malawi* OR mali* OR mauritania* OR mozambique OR mozambican OR myanmar* OR burma OR burmese OR nepal* OR niger* OR rwanda* OR "sierra leone*" OR "solomon island*" OR somali* OR tajikistan* OR tanzania* OR togo* OR uganda* OR zambia* OR zimbabwe* ) OR (angola* OR armenia* OR belize* OR bhutan* OR bolivia* OR cameroon* OR "cape verd*" OR china OR chinese OR (cote NEAR/1 ivoire) OR ivorian OR djibouti OR ecuador* OR egypt* OR "el salvador" OR salvadoran OR guatemala* OR guyana OR guyanese OR hondura* OR india* OR indonesia* OR iraq* OR jordan* OR kiribati OR kosov* OR lesotho OR mosotho OR basotho OR maldiv* OR "marshall islands" OR marshallese OR micronesia* OR moldova* OR mongolia* OR morocc* OR nicaragua* OR nigeria* OR pakistan* OR "papua new guinea*" OR paraguay* OR philippines OR filipino OR samoa* OR senegal* OR "sri lanka*" OR sudan* OR swaziland OR swazi OR syrian OR syria* OR thailand OR thai OR timor* OR tonga* OR tunisia* OR turkmen* OR tuvalu* OR ukrain* OR uzbekistan* OR uzbek OR vanuatu OR vietnam* OR "west bank" OR gaza OR palestinian* OR yemen* OR albania* OR algeria* OR samoa OR antigua* OR barbuda* OR argentin* OR azerbaijan* OR belarus* OR bosnia* OR herzegovin* OR botswana OR motswana OR batswana OR brazil* OR bulgaria* OR chile* OR colombia* OR costa AND rica* OR cuba* OR dominica* OR "dominican republic" OR fiji* OR gabon* OR grenad* OR iran* OR jamaica* OR kazakhstan* OR leban* OR libya* OR lithuania* OR macedonia* OR malaysia* OR mauriti* OR mayotte OR mahoran OR mexic* OR montenegr* OR namibia* OR palau* OR panama* OR peru* OR romania* OR russia* OR serbia* OR seychell* OR "south africa*" OR "st lucia*" OR suriname* OR turk* OR uruguay* OR venezuela* ) ) OR (SU.EXACT("Developing countries") OR SU.EXACT("Less developed countries") OR SU.EXACT("Developing areas")) OR ((lmic OR lmics) OR ((("low income" OR "medium income") NEAR/5 (country OR countries OR nation OR nations OR state OR states)) OR ("least developed" NEAR/1 (country OR countries OR nation OR nations OR state OR states)) ) OR ((developing NEAR/1 (country OR countries OR nation OR nations OR state OR states)) OR ("united nations" OR "world health organization" OR "world bank" OR unicef) AND ((food OR nutrition*) NEAR/3 (program* OR project* OR fund)) ))) AND pd(19800101‐20161231)) AND ((SU.EXACT("Comparative analysis") OR SU.EXACT("Long‐term analysis") OR SU.EXACT("Time series") OR SU.EXACT("Random sampling") OR SU.EXACT("Control groups") OR SU.EXACT("Cohort analysis")) OR ((compar* AND (study OR trial OR program*)) OR ((random* OR controlled OR placebo OR "control group*") OR ("follow up")) OR ((prospectiv* OR non‐random* OR nonrandom*) OR ("before after stud*" OR (time AND series) OR retrospectiv* OR longitud*)) OR ( (control* AND cohort* AND study) OR ("before and after")) OR ("pre test" OR pretest OR posttest OR "post test" OR "pre intervention" OR "post intervention") ))
| Global Health (Ebsco) 17 September 2016 | ||
| # | Query | Limiters/Expanders |
| S1 | (DE "food security") OR (DE "food policy") OR (DE "food aid" OR DE "food distribution programs") | Search modes ‐ Boolean/Phrase |
| S2 | (food secur* OR food insecur* OR food poverty OR food sufficien* OR food insufficien* OR food desert*) | Search modes ‐ Boolean/Phrase |
| S3 | ((food OR foods OR foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR grocer*) N5 (budget* OR shopping OR purchase OR purchasing OR purchases OR expenditure OR expenditures OR spend OR spent OR spending OR buy OR buying OR acquisition OR acquire OR acquiring)) | Search modes ‐ Boolean/Phrase |
| S4 | ((foodstuff* OR fruit OR fruits OR vegetable OR vegetables OR groceries OR supermarket OR supermarkets OR grocery store OR grocery stores OR food store OR food stores OR food shop OR food shops OR corner store OR corner stores OR cafeteria OR cafeterias OR canteen* OR food outlet*) N5 (access OR accessibility OR cost OR costs OR price OR prices OR pricing)) | Search modes ‐ Boolean/Phrase |
| S5 | food system* AND (fresh OR health OR healthy OR nutrition OR nutritional OR nutritive OR nutrient rich OR nutrient dense OR adequate OR quality OR sufficient OR insufficient OR secure OR insecure OR safe) | Search modes ‐ Boolean/Phrase |
| S6 | ((policy OR policies) N5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries OR meal OR meals)) | Search modes ‐ Boolean/Phrase |
| S7 | ((council OR councils OR coalition OR coalitions OR co‐op OR co‐ops OR co‐operative*) N5 (food OR foods OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR groceries)) | Search modes ‐ Boolean/Phrase |
| S8 | (access* N3 food) | Search modes ‐ Boolean/Phrase |
| S9 | ( ((deliver OR delivery OR deliveries OR transport OR transportation OR distribute OR distributes OR distribution) N3 (groceries OR meal OR meals OR fruit OR fruits OR vegetable OR vegetables OR food OR foods)) ) AND ( (outreach OR service OR services OR scheme OR schemes OR program OR programs OR programme OR programmes OR policy OR policies OR project OR projects OR nutrition OR nutritional OR home OR home‐based OR homes OR community OR communities OR neighbor OR neighborhood OR neighbour OR neighbourhood OR rural OR urban OR provide OR provision OR choice OR control OR welfare) ) | Search modes ‐ Boolean/Phrase |
| S10 | ((public transport OR transport service* OR transportation service* OR transport scheme OR travel OR travelling OR infrastructure OR access) N5 (food store* OR food shop* OR food retail* OR food outlet OR supermarket OR grocer*)) | Search modes ‐ Boolean/Phrase |
| S11 | ((payment OR payments OR benefit OR benefits OR money OR purchase OR purchasing OR purchases OR buy OR buying OR welfare OR financing OR cash OR income) N5 (food OR foods OR foodstuff* OR groceries OR fruit OR fruits OR vegetable OR vegetables OR nutrition OR nutritional OR meal OR meals) N10 (supplement OR supplementation OR assist OR assistance OR extra OR aid OR support OR help)) | Search modes ‐ Boolean/Phrase |
| S12 | ((tax OR taxes OR taxation OR subsidy OR subsidies OR subsidized OR subsidised OR voucher* OR coupon* OR discount*) N5 (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) | Search modes ‐ Boolean/Phrase |
| S13 | ((Cash transfer* OR social protection) AND (food OR foods OR foodstuff* OR grocer* OR fruit* OR vegetable* OR nutrition OR nutritional OR meal OR meals)) | Search modes ‐ Boolean/Phrase |
| S14 | ((community nutrition OR public health nutrition OR food access) AND (project* OR program*)) | Search modes ‐ Boolean/Phrase |
| S15 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 | Search modes ‐ Boolean/Phrase |
| S16 | DE "Developing Countries" OR DE "Least Developed Countries" | Search modes ‐ Boolean/Phrase |
| S17 | (Afghan* OR Bangladesh* OR Benin* OR Burkina Faso OR Burkinabe OR Burundi* OR Cambodia* OR Central African Republic OR Central African* OR Chad* OR Comoros OR Comorian* OR Congo* OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea‐Bissau* OR Haiti* OR Kenya* OR Kyrgyz Republic OR Kyrgyzstani OR Lao* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Mozambique OR Mozambican OR Myanmar* OR Burma OR Burmese OR Nepal* OR Niger* OR Rwanda* OR Sierra Leone* OR Solomon Islands OR Solomon Islanders OR Somali* OR Tajikistan* OR Tanzania* OR Togo* OR Uganda* OR Zambia* OR Zimbabwe*) | Search modes ‐ Boolean/Phrase |
| S18 | (Angola* OR Armenia* OR Belize* OR Bhutan* OR Bolivia* OR Cameroon* OR Cape Verd* OR China OR Chinese OR Cote dIvoire OR Ivorian OR Djibouti OR Ecuador* OR Egypt* OR El Salvador OR Salvadoran OR Guatemala* OR Guyana OR Guyanese OR Hondura* OR India* OR Indonesia* OR Iraq* OR Jordan* OR Kiribati OR Kosov* OR Lesotho OR Mosotho OR Basotho OR Maldiv* OR Marshall Islands OR Marshallese OR Micronesia* OR Moldova* OR Mongolia* OR Morocc* OR Nicaragua* OR Nigeria* OR Pakistan* OR Papua New Guinea* OR Paraguay* OR Philippines OR Filipino OR Samoa* OR Senegal* OR Sri Lanka* OR Sudan* OR Swaziland OR Swazi OR Syrian Arab Republic OR Syria* OR Thailand OR Thai OR Timor Leste OR East Timorese OR Tonga* OR Tunisia* OR Turkmen* OR Tuvalu* OR Ukrain* OR Uzbekistan* OR Uzbek OR Vanuatu OR Vietnam* OR West Bank OR Gaza OR Palestinian* OR Yemen*) | Search modes ‐ Boolean/Phrase |
| S19 | (Albania* OR Algeria* OR American Samoa OR Antigua* OR Barbuda* OR Argentin* OR Azerbaijan* OR Belarus* OR Bosnia* OR Herzegovin* OR Botswana OR Motswana OR Batswana OR Brazil* OR Bulgaria* OR Chile* OR Colombia* OR Costa Rica* OR Cuba* OR Dominica* OR Dominican Republic OR Fiji* OR Gabon* OR Grenad* OR Iran* OR Jamaica* OR Kazakhstan* OR Leban* OR Libya* OR Lithuania* OR Macedonia* OR Malaysia* OR Mauriti* OR Mayotte OR Mahoran OR Mexic* OR Montenegr* OR Namibia* OR Palau* OR Panama* OR Peru* OR Romania* OR Russia* OR Serbia* OR Seychell* OR South Africa* OR St Lucia* OR Suriname* OR Turk* OR Uruguay* OR Venezuela*) | Search modes ‐ Boolean/Phrase |
| S20 | (lmic OR lmics) | Search modes ‐ Boolean/Phrase |
| S21 | ((low income OR medium income) N5 (country OR countries OR nation OR nations OR state OR states)) | Search modes ‐ Boolean/Phrase |
| S22 | (least developed N1 (country OR countries OR nation OR nations OR state OR states)) | Search modes ‐ Boolean/Phrase |
| S23 | (developing N1 (country OR countries OR nation OR nations OR state OR states)) | Search modes ‐ Boolean/Phrase |
| S24 | (united nations OR world health organization OR world bank OR unicef OR ((food OR nutrition*) N3 (program* OR project* OR fund))) | Search modes ‐ Boolean/Phrase |
| S25 | S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 | Search modes ‐ Boolean/Phrase |
| S26 | S15 AND S25 | Search modes ‐ Boolean/Phrase |
| S27 | S26 | Limiters ‐ Publication Year: 1980‐2016 |
| S28 | (DE "clinical trials" OR DE "controls (experimental)") OR (DE "time series") | Search modes ‐ Boolean/Phrase |
| S29 | compar* N6 (study OR trial OR program*) | Search modes ‐ Boolean/Phrase |
| S30 | random* OR controlled OR placebo OR control group* | Search modes ‐ Boolean/Phrase |
| S31 | follow up AND (study OR trial) | Search modes ‐ Boolean/Phrase |
| S32 | prospectiv* OR non‐random* OR nonrandom* | Search modes ‐ Boolean/Phrase |
| S33 | before after stud* OR (time N2 series) OR ((retrospectiv* OR longitud*) AND study) | Search modes ‐ Boolean/Phrase |
| S34 | control* AND cohort* AND study | Search modes ‐ Boolean/Phrase |
| S35 | "before and after" | Search modes ‐ Boolean/Phrase |
| S36 | pre test OR pretest OR posttest OR post test OR pre intervention OR post intervention | Search modes ‐ Boolean/Phrase |
| S37 | S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 | Search modes ‐ Boolean/Phrase |
| S38 | S27 AND S37 | Search modes ‐ Boolean/Phrase |
ClinicalTrials.gov 17 September 2016
78 studies found for "food security" OR "food insecurity" OR "food access" OR "food poverty" OR "food sufficiency" OR "food insufficiency" OR "nutrition security"
International Clinical Trials Registry Platform 17 September 2016
42 records for 42 trials found for: food secur* OR food insecur* OR food access OR food poverty OR food sufficienc* OR food insufficienc* OR nutrition secur*
Appendix 3. Record of communication with authors of included studies
| Study ID | References to other relevant studies | Correspondence required (yes or no, and why) | Further study information requested | Correspondence received (from whom, what, when) | Information used in review |
| Neufeld 2013 | — | Abstract, requested full text | MV emailed author on 10 April 2018 | Received email from Lynnette Neufeld <lneufeld@gainhealth.org> on 12 April 2018, who provided 2 full texts. | Screened 2 full texts provided |
| Shamah‐Levy 2015 | — | Abstract, requested full text | MV emailed author on 10 April 2018 | Received email from Elsa Berenice Gaona Pineda <berenicegp.insp@gmail.com> on 10 April 2018 with full text | Screened 1 full text provided |
| Wood | — | Abstract, requested full text | MRC library requested dissertation requested on 12 April 2018 | No response | None |
| Kusuma 2016 | — | Method of randomisation of village clusters not clear, data from nutrition and food security intervention comparisons required, treatment regimen of control group unclear | AS emailed author about outcomes on 6 February 2018 (follow‐up on 13 February 2018 and 13 March 2018). Authors only nutrition outcomes is whether mothers took supplements therefore review excluded on the basis of no relevant outcomes | No response from dkusuma@mail.harvard.edu | None |
| Murshed E Jahan 2011 | — | Baseline data | MV emailed author on 22 March 2018 | No response from 'k.jahan@cgiar.org'; d.pemsl@cgiar.org | None |
| Skoufias 2013 | — | Additional outcome data, requested study report | MV emailed author on 8 June 2018 | Received email from Emmanuel skoufias <eskoufias@worldbank.org on 8 June 2018 | Need to screen 1 full text in Spanish |
| Asadullah 2015 | — | nrs LTFU unclear and nrs of participants do not match between tables in paper; unclear units of measurement and measure of central tendency; data duplicated for two outcomes | SD emailed author Mohammad N. Asadullah about nrs LTFU and participant numbers on 31 July 18; AB emailed author on two additional email addresses on 7 February 2019 to follow‐up SD queries and additional issues identified in outcome extraction. AB followed up on 18 February 19. | Author responded on 6 March 19 from m.niaz@um.edu.my and endeavoured to provide further information | None yet |
| Asfaw 2014 | — | Mean monthly food consumption expenditure exceeds mean total monthly household consumption expenditure (defined as including all household expenses) | AB emailed author Patrick Ward on 28 January 19 to determine whether mean household food consumption expenditure is not included in mean total monthly household expenditure and, if not the case, why this sub‐category exceeds the category total. AB followed up on 18 February 19. | Author responded on 19 February 19 from patrick.ward@opml.co.uk and endeavoured to provide further information, requested from Aly Visram (co‐author; aly.visram@opml.co.uk) on 28 February 2019 | None yet |
| Weinhardt 2017 | — | yes. Information re clarification of outcome malnutrition in paper and what it means exactly | SD emailed Weinhardt and Alice Yan about clarification of table 3 malnutrition outcome and whether there are separate results for stunting and wasting | No response | — |
| Darrouzet‐Nardi 2016 | — | yes. Information re correct data for HAZ in table 4 of Miller 2014 | SD emailed both Darrouzet‐Nardi and Miller on 25 September 2019 re this issue | No response | — |
| Seidenfeld 2013 | Daidone 2014 | yes. Effect measure and narrative description of result on food security scale discrepant. | SD emailed 14 October 2019 | Response on 18 December 2019, responding to query. | Correct effect direction confirmed and used in the review |
| Nkonya 2019 | — | Yes. | AB emailed 1 April 2020 to clarify study design eligibility. | Yes | Study excluded |
| Hidrobo 2014 | — | Yes | MV emailed 29 April 2020. Request for number of participants analysed per group | No response | — |
| Osei 2017 | — | Yes | MV emailed 30 April 2020. Request for number of participants analysed per group | No response | — |
| Beegle 2017 | — | Yes | MV emailed 30 April 2020. Request for number of participants analysed per group | Yes. Provided required information. | Enabled meta‐analysis to be carried out |
Appendix 4. Sensitivity analysis for outcomes with five or more studies
| Outcome (analysis) | All studies (primary analysis) | Studies at low risk of bias (sensitivity analysis) |
| HAZ (Analysis 1.8) | MD 0.07, 95% CI –0.04 to 0.18 | MD 0.16, 95% CI 0.02 to 0.29 |
| WHZ (Analysis 1.9) | MD –0.02, 95% CI –0.10 to 0.06 | MD 0.02, 95% CI –0.18 to 0.21 |
| HAZ – RCTs (Analysis 2.4) | MD 0.09, 95% CI 0.04 to 0.15 | MD 0.09, 95% CI 0.01 to 0.17 |
| CI: confidence interval; HAZ: height‐for‐age z‐score; MD: mean difference; WHZ: weight‐for‐height z‐score. | ||
Data and analyses
Comparison 1. Unconditional cash transfers (UCT) versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Proportion of household expenditure on food | 3 | Mean Difference (IV, Random, 95% CI) | 4.24 [‐2.88, 11.36] | |
| 1.2 Proportion consuming > 1 meal/day | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.3 Food security scores | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [0.13, 0.23] | |
| 1.4 Dietary Diversity Score including composite food consumption score (FCS) (weighted) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.5 Proportion with minimum dietary diversity | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6 Proportion of food poverty (per capita daily caloric intake < 2122 calories) | 2 | Mean Difference (IV, Random, 95% CI) | ‐4.64 [‐9.34, 0.06] | |
| 1.7 Proportion stunted (height‐for‐age z‐score (HAZ) < ‐2SD) | 2 | Odds Ratio (IV, Random, 95% CI) | 0.62 [0.46, 0.84] | |
| 1.8 HAZ | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.8.1 Change in z‐scores | 6 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.04, 0.18] | |
| 1.8.2 Change in z‐score/month | 1 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.00, 0.00] | |
| 1.9 Weight‐for‐height z‐score (WHZ) | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.9.1 Change in z‐scores | 5 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.10, 0.06] | |
| 1.9.2 Change in z‐scores/month | 1 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.01, 0.00] | |
| 1.10 Weight‐for‐age z‐score (WAZ) | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.43, 0.35] | |
| 1.11 Haemoglobin concentration (g/dL) | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.21, 0.09] | |
| 1.12 Depression score (CES‐D scale) | 3 | Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐1.31, 0.49] | |
| 1.13 Perceived Stress Scale (PSS) | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.26, ‐0.03] |
1.6. Analysis.

Comparison 1: Unconditional cash transfers (UCT) versus no intervention, Outcome 6: Proportion of food poverty (per capita daily caloric intake < 2122 calories)
Comparison 2. Conditional cash transfers (CCT) versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Household Dietary Diversity Score (HDDS) | 2 | Mean Difference (IV, Random, 95% CI) | 0.45 [0.25, 0.65] | |
| 2.2 Proportion stunted (height‐for‐age z‐score (HAZ) < ‐2SD) – RCTs | 3 | Mean Difference (IV, Random, 95% CI) | ‐2.51 [‐7.78, 2.75] | |
| 2.3 Proportion with severe stunting (HAZ < ‐3 SD) – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | ‐3.05 [‐17.63, 11.53] | |
| 2.4 HAZ – RCTs | 5 | Mean Difference (IV, Random, 95% CI) | 0.09 [0.04, 0.15] | |
| 2.5 Proportion stunted (HAZ < ‐2 SD) – PCS | 2 | Mean Difference (IV, Random, 95% CI) | ‐5.63 [‐26.59, 15.34] | |
| 2.6 HAZ – PCS | 3 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.06, 0.12] | |
| 2.7 Proportion wasted (weight‐for‐height z‐score (WHZ) < ‐2 SD) – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | ‐2.50 [‐8.04, 3.04] | |
| 2.8 WHZ – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.11, 0.44] | |
| 2.9 Proportion underweight (weight‐for‐age z‐score (WAZ) < ‐2SD) – RCTs | 3 | Mean Difference (IV, Random, 95% CI) | ‐4.87 [‐8.65, ‐1.09] | |
| 2.10 Proportion severely underweight (WAZ < ‐3 SD) – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐4.73, 2.57] | |
| 2.11 WAZ – RCTs | 3 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.03, 0.11] | |
| 2.12 BMI‐for‐age z‐score – PCS | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.13 Cognitive test scores – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | 0.13 [0.09, 0.18] | |
| 2.14 Proportion reporting being ill in past 4 weeks/parents seeking care for illness past 2 weeks – RCTs | 3 | Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐5.92, 5.35] | |
| 2.15 Overweight (BMI z‐score > 2 SD)_PCS | 2 | Odds Ratio (IV, Random, 95% CI) | 1.00 [0.59, 1.71] |
2.1. Analysis.

Comparison 2: Conditional cash transfers (CCT) versus no intervention, Outcome 1: Household Dietary Diversity Score (HDDS)
Comparison 3. Income generation (IG) versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 HFIAS – PCS | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.2 HDDS – RCTs | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.09, 0.13] | |
| 3.3 Minimum dietary diversity (MDD) – RCTs | 3 | Odds Ratio (IV, Random, 95% CI) | 1.28 [1.11, 1.47] | |
| 3.4 HDDS – PCS | 3 | Mean Difference (IV, Random, 95% CI) | 0.67 [0.29, 1.05] | |
| 3.5 Proportion stunted (HAZ < ‐2 SD) – RCTs | 2 | Odds Ratio (IV, Random, 95% CI) | 1.00 [0.84, 1.19] | |
| 3.6 HAZ – RCTs | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.7 Proportion wasted (WHZ < ‐2 SD) – RCTs | 2 | Odds Ratio (IV, Random, 95% CI) | 1.13 [0.92, 1.40] | |
| 3.8 WHZ – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.25, 0.15] | |
| 3.9 Percentage underweight – RCTs | 2 | Odds Ratio (IV, Random, 95% CI) | 1.06 [0.89, 1.26] | |
| 3.10 WAZ – RCTs | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.11 Percentage underweight – PCS | 2 | Odds Ratio (IV, Random, 95% CI) | 0.83 [0.61, 1.12] | |
| 3.12 Proportion of women underweight – RCTs | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.13 BMI – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.28, 0.25] | |
| 3.14 Haemoglobin concentration (children) – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | 3.49 [3.25, 3.72] | |
| 3.15 Haemoglobin concentration (women) – RCTs | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.16 Prevalence of anaemia (children) – RCTs | 2 | Odds Ratio (IV, Random, 95% CI) | 0.73 [0.61, 0.88] | |
| 3.17 Prevalence of anaemia (women) – RCTs | 2 | Odds Ratio (IV, Random, 95% CI) | 1.06 [0.82, 1.38] |
Comparison 4. Food vouchers vs no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Food consumption score | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aguero 2006.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? NR Randomisation ratio: N/A Recruitment method: for the KIDS survey in 1998, the core people in each HH who participated in the 1993 PSLSD survey, were identified prior to starting fieldwork according to prespecified criteria. Study period: 1998–2004 Sample size justification and outcome used: NR Sampling method: sample of PSLSD survey in 1993 was obtained by a 2‐stage self‐weighting design. In the first stage, clusters were chosen with probability to size of census ESD. In the second stage, all HHs in each chosen cluster were enumerated and a random sample of HHs was then selected. For the KIDS survey in 1998, a subsample of HHs In Kwazulu‐Natal from the 1993 sample was selected (included only African and Indian HHs) and followed up to 2004. Study aim or objective: the KIDS study "… aims to contribute to knowledge in this area by studying the impact of the South African Child Support Grant (CSG), which was first rolled out in 1998." Unit of allocation or exposure: individual children |
|
| Participants |
General description of participants (sex, place of residence, ethnicity): children living in HHs eligible for Child Support Grant Age: NR Occupation: NR Education: NR SES: NR Social capital: NR Nutritional status: NR Morbidities: NR Concomitant/previous care: NR Inclusion criteria: HHs in KwaZulu‐Natal that participated in the 1993 PSLSD survey, and where there is any of the following: a self‐declared head of HH; a spouse/partner of a self‐declared head of HH; lived in a 3‐generation HH where there was a child, child‐in‐law, or niece/nephew of a self‐declared head aged ≥ 30 years and had ≥ 1 child living in the HH. Exclusion criteria: HHs without children or grandchildren residing with core people who participated in the KIDS study. Baseline differences: NR Total number completed and analysed: 720 children (245 children who received CSG during birth to 3 years; 321 children who received CSG after they were aged 3 years; 154 children who applied for CSG support, but had applications rejected or not yet received benefits by the time of the survey) Total number enrolled per relevant group: NR Total number randomised per relevant group: N/A Attrition: overall, 84.1% of the African and Indian HHs surveyed in 1993 in KwaZulu‐Natal (1171 HHs) agreed to take part in the 1998 survey. 71% of the original 1993 sample (988 HHs) took part in the 2004 survey. Description of subgroups measured and reported: children who received low vs high coverage of CSG during birth to 3 years |
|
| Interventions |
Intervention: UCT (Child Support Grant) Food access intervention category: increase buying power Description: CSG implemented in 1998, initially covering children aged ≤ 7 years. Money paid over to the primary carer of the child, with no recording of what the carer used the money for. When the CSG started, it was intended for the 30% poorest children, and was means‐tested (i.e. the income of the primary carer and partner must have been under a specific bracket). In April 2003, the age eligibility was raised to 9 years old and in 2004 to 11 years old. The initial monthly benefit was SAR 100 in 1998 and during the time of the 2004 survey it was SAR 170 (about USD 25 at that time). Duration of intervention period: 6 years (1998–2004) Frequency: monthly payments Number of study contacts: baseline PSLSD survey (July–December 1993); first follow‐up KIDS survey (March–June 1998); second follow‐up KIDS survey (2004) Providers: South African Government Delivery: payments to primary carer of the child/children (98% of primary carers were female). Co‐interventions: NR Resource requirements: NR Economic indicators: NR Control: no intervention (HHs that did not receive the CSG; children "… that received child support grant only after they were 3 years old (321 children); those who had applied for CSG support, but who had their applications rejected or had not yet received benefits by the time of the survey (154 children)") |
|
| Outcomes | Anthropometry: HAZ | |
| Identification |
Sponsorship source: UK DfID and USAID Country: South Africa Setting: urban and non‐urban HHs in the KwaZulu Natal province Authors' names: Jorge M Agüero and Julian May Email: jorge.aguero@ucr.edu Declarations of interest: not declared Study or programme name and acronym: KwaZulu Natal Income Dynamics Study (KIDS), about the South African Child Support grant CSG) Type of record: 2 research reports (on institution web sites) and 1 journal article Trial registration: N/A Protocol availability: no |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | This was a cohort study. |
| Allocation concealment (Selection bias) | High risk | This was a cohort study. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Baseline data (1998 survey) between intervention and control groups were NR. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Baseline data (1998 survey) was collected but details regarding this were NR. |
| Blinding of participants and personnel (Performance bias) | Low risk | There was no blinding, but outcomes were objective (e.g. children anthropometrics) and thus not likely to have been influenced by a lack of blinding. |
| Blinding of outcome assessment (Detection bias) | Low risk | It is not stated whether outcome assessors were blinded; however, outcome measurements were objective (anthropometry) |
| Protection against contamination (Performance bias) | Unclear risk | Unclear whether HHs in the intervention and control groups were from the same community. |
| Incomplete outcome data (Attrition bias) | Unclear risk | The number of HHs with children providing nutrition outcomes at the 1998 and 2004 surveys were NR. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available, and outcomes were not pre‐specified in the Methods section. |
| Other bias | Unclear risk | Misclassification bias: unclear risk as it was unclear whether Child Support Grant data reported by core people from each HH was verified. Measurement bias: low risk as they used trained field workers. |
Ahmed 2019a.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? NR but based on Table 1 reporting baseline data for fewer number of participants than randomised we assume that missing data were excluded. Randomisation ratio: 1:1:1:1:1 (village‐level randomisation) Recruitment method: NR Sample size justification and outcome used: sample size calculations undertaken to assess the number of clusters (villages) and HHs needed to detect changes in both HH‐ and child‐level outcomes. Using data from an earlier study in Bangladesh (Ahmed et al. 2010), setting significance level at 0.05 and statistical power at 0.80, assuming attrition of 10% over duration of intervention, and using outcome‐specific means, SDs and intracluster correlations, a sample based on 50 clusters per treatment and 10 HHs per cluster would provide sufficient statistical power to detect an increase of: 12% in HH per capita total expenditure per month; 7% in HH per capita calorie intake per day; 16% in child HAZ; and 8% in dietary diversity of children aged 12–60 months. Sampling method: same process followed for each region – North and South: in North, 5 upazilas (subdistricts) were selected using simple random sampling from a list of upazilas where in 2010 the proportion of HHs living below Bangladesh's lower poverty line was ≥ 25%. All villages within these 5 upazilas were listed. Villages classified as urban or with < 125 HHs were dropped. Using a random number generator, each village was assigned a random number. Villages were then sorted in ascending numerical order with the first 275 retained. Given that in each region, there were 4 treatment groups and a control group, the first 50 villages were assigned to treatment group 1, the second 50 to treatment group 2, the third 50 villages to treatment group 3, the fourth 50 villages to treatment group 4 and the fifth 50 villages to the control group. The remaining 25 villages were held as a reserve. A complete village census was carried out in each of the 250 selected villages, collecting information on HH demographics, a set of poverty indicators, and whether HHs participated in safety nets and other targeted interventions. Using these data, a list was compiled of HHs that: 1. were considered poor (i.e. based on the poverty indicators collected, they were estimated to have consumption below Bangladesh's lower poverty line); 2. would have ≥ 1 child aged 0–24 months when the intervention began; and 3. were not receiving benefits from other safety net interventions. These HHs were eligible to participate in the study. Using simple random sampling, 10 eligible HHs were selected from each village. The total sample in the North included 250 clusters and 2500 HHs. An identical process was used in the South to select upazilas, villages and HHs. Study aim or objective: to devise and implement 2 × 2‐year RCTs in 2 poor rural areas of Bangladesh with both cash and food treatment groups. Building on the work of Black et al. (2013), the intervention also included 2 treatment groups that aimed to improve maternal knowledge and practices surrounding infant and young child nutrition – through BCC – thus making those treatment groups nutrition‐sensitive. We designed survey instruments to capture impacts at the child level, both for the key outcome measure of child anthropometry and for individual‐level mechanisms that plausibly underlie programme impacts. Using the RCT design, they estimated impacts of each treatment on child height‐for‐age. In the other paper, the authors assessed its implications for economic outcomes. Study period: 24 months: baseline survey was carried out in March–April 2012, the endline survey was conducted in April 2014. Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics Cash only
Control
Cash and food
Cash and BCC
Food only
Overall
Inclusion criteria: subdistrict eligibility: proportion of HHs living below Bangladesh's lower poverty line ≥ 25%." Village eligibility: rural; HH eligibility: list compiled of 1. HHs that: were considered poor (i.e. based on the poverty indicators collected, they were estimated to have consumption below Bangladesh's lower poverty line); 2. would have ≥ 1 child aged 0–24 months when the intervention began and 3. were not receiving benefits from other safety net interventions. Target beneficiary was mother of an 'index child' aged 0–24 months in March 2012, residing in a poor rural HH. Exclusion criteria: village level: villages classified as urban or villages with fewer than 125 HHs were dropped. Pretreatment: outcome and control variables similar across the North and South and similar across treatment groups. Attrition per relevant group: only overall: 4992 HHs interviewed at baseline, 2498 in North and 2494 in South. In North, 2,410 HHs were re‐interviewed at endline, an attrition rate of 3.5%. 78 HHs were not surveyed at endline because they had migrated, another 10 dropped out of study, refused to be interviewed or could not be found. In South, 2438 HHs re‐interviewed at endline, an attrition rate of 2.2%. 49 HHs were not surveyed at endline because they had migrated, another 7 dropped out of study, refused to be interviewed or could not be found. Using probit regressions, there was no evidence that attrition was related to treatment status or HH demographic, occupational or asset characteristics (Ahmed et al. 2016). Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: total number of HHs interviewed in North was 2410 and in South was 2438 at endline. For the outcomes related to children (due to restrictions related to age at baseline, biological children): this led to an estimation sample of 4399 children; 2218 in North and 2181 in South. Note that sample sizes differed per outcome as can be seen in the legends of the tables. Numbers per group NR. Total number enrolled per relevant group: interviewed 4992 HHs at baseline, 2498 in North and 2494 in South. Table 1 presented number of mothers/children per group at baseline, but total was 2275 for North and 2288 for South. North: cash only group: 458; food only group: 454; cash and food group: 458; cash and BCC group: 455; control: 450. South: cash only group: 454; food only group: 462; cash and food group: 446; cash and BCC group: 462; control group: 464 Total number randomised per relevant group: North included 250 clusters and 2500 HHs. Similar in South. |
|
| Interventions |
Intervention characteristics Cash only
Control: no intervention Cash and food
Cash and BCC
Food only
Food and BCC
|
|
| Outcomes | Dietary diversity: FCS; percentage with low FCS (FCS < 35) Adequacy of dietary intake: percentage with per capita daily caloric intake < 2122 calories (food poverty) Anthropometry: WHZ; HAZ Morbidity: % of children with the following symptoms in the previous 2 weeks: fever, cough or cold, diarrhoea |
|
| Identification | Food security | |
| Notes | Dietary diversity | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Authors reported that, "Using a random number generator, each village was assigned a random number." Comment: but this was to sort the villages in ascending numerical order. They did not report how the random sequence for allocation into each trial group was generated. |
| Allocation concealment (Selection bias) | Low risk | Allocation concealment NR; however, this was carried out at village level. |
| Baseline characteristics similar (Selection bias) | Low risk | Outcome and control variables were similar across the North and South and similar across treatment groups. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Outcome and control variables were similar across the North and South and similar across treatment groups. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not possible, but it was unlikely that it influenced the intervention delivered. |
| Blinding of outcome assessment (Detection bias) | Low risk | Core outcomes were anthropometric measures objectively measured, which lack of blinding was unlikely to influence. |
| Protection against contamination (Performance bias) | Low risk | Allocation was by village and it is unlikely that contamination occurred. Authors reported that in some localities the "… same payment point was used for both the cash arm and the cash plus BCC arm,…" and that "… cash beneficiaries were paid in the morning while cash plus BCC beneficiaries were paid in the afternoon to minimize the likelihood of information from the BCC activities spilling over to the cash treatment arm." According to authors, the implementation fidelity was high; therefore, contamination was likely avoided. |
| Incomplete outcome data (Attrition bias) | Low risk | Overall attrition was low; 3.5% in the North and 2.3% in the South, but attrition per treatment group was NR. Reasons for HHs not being surveyed at endline in the North included "… they had migrated, another 10 dropped out of study, refused to be interviewed, or could not be found." and in the South: "49 households were not surveyed at endline because they had migrated, another seven dropped out of study, refused to be interviewed, or could not be found." Authors reported that, "Using probit regressions, we found no evidence that attrition was related to treatment status or household demographic, occupational or asset characteristics (Ahmed et al. 2016)." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol accessed. |
| Other bias | Low risk | Judgement comment: misclassification bias of exposure: low risk. Exposure determined by researchers. Measurement bias: low risk. Incorrect analysis: low risk. Study has taken into account the cluster design. We note that one might be concerned that BCC could lead to social desirability bias affecting the IYCDDS responses – i.e. after 2 years of nutrition training, mothers might respond to questions about child feeding by over‐reporting foods commonly discussed during the group training sessions. The fact that there were differences between what mothers in the North described and what mothers in the South described – e.g. that mothers receiving BCC in the South did not report feeding their children dairy products more frequently than those in the control group – despite their receiving identical BCC gave us some confidence in these results. |
Ahmed 2019b.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? NR but based on Table 1 reporting baseline data for fewer number of participants than randomised we assume that missing data were excluded. Randomisation ratio: 1:1:1:1:1 (village‐level randomisation) Recruitment method: NR Sample size justification and outcome used: sample size calculations undertaken to assess the number of clusters (villages) and HHs needed to detect changes in both HH‐ and child‐level outcomes. Using data from an earlier study in Bangladesh (Ahmed et al. 2010), setting significance level at 0.05 and statistical power at 0.80, assuming attrition of 10% over duration of intervention, and using outcome‐specific means, SDs and intracluster correlations, a sample based on 50 clusters per treatment and 10 HHs per cluster would provide sufficient statistical power to detect an increase of: 12% in HH per capita total expenditure per month; 7% in HH per capita calorie intake per day; 16% in child HAZ; and 8% in dietary diversity of children aged 12–60 months. Sampling method: same process followed for each region – North and South: in North, 5 upazilas (subdistricts) were selected using simple random sampling from a list of upazilas where in 2010 the proportion of HHs living below Bangladesh's lower poverty line was ≥ 25%. All villages within these 5 upazilas were listed. Villages classified as urban or with < 125 HHs were dropped. Using a random number generator, each village was assigned a random number. Villages were then sorted in ascending numerical order with the first 275 retained. Given that in each region, there were 4 treatment groups and a control group, the first 50 villages were assigned to treatment group 1, the second 50 to treatment group 2, the third 50 villages to treatment group 3, the fourth 50 villages to treatment group 4 and the fifth 50 villages to the control group. The remaining 25 villages were held as a reserve. A complete village census was carried out in each of the 250 selected villages, collecting information on HH demographics, a set of poverty indicators, and whether HHs participated in safety nets and other targeted interventions. Using these data, a list was compiled of HHs that: 1. were considered poor (i.e. based on the poverty indicators collected, they were estimated to have consumption below Bangladesh's lower poverty line); 2. would have ≥ 1 child aged 0–24 months when the intervention began; and 3. were not receiving benefits from other safety net interventions. These HHs were eligible to participate in the study. Using simple random sampling, 10 eligible HHs were selected from each village. The total sample in the North included 250 clusters and 2500 HHs. An identical process was used in the South to select upazilas, villages and HHs. Study aim or objective: to devise and implement 2 × 2‐year RCTs in 2 poor rural areas of Bangladesh with both cash and food treatment groups. Building on the work of Black et al. (2013), the intervention also included 2 treatment groups that aimed to improve maternal knowledge and practices surrounding infant and young child nutrition – through BCC – thus making those treatment groups nutrition‐sensitive. We designed survey instruments to capture impacts at the child level, both for the key outcome measure of child anthropometry and for individual‐level mechanisms that plausibly underlie programme impacts. Using the RCT design, they estimated impacts of each treatment on child height‐for‐age. In the other paper, the authors assessed its implications for economic outcomes. Study period: 24 months: baseline survey was carried out in March–April 2012, the endline survey was conducted in April 2014. Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics Cash only
Control
Cash and food
Food only
Food and BCC
Overall
Inclusion criteria: subdistrict eligibility: proportion of HHs living below Bangladesh's lower poverty line ≥ 25%." Village eligibility: rural; HH eligibility: list compiled of 1. HHs that: were considered poor (i.e. based on the poverty indicators collected, they were estimated to have consumption below Bangladesh's lower poverty line); 2. would have ≥ 1 child aged 0–24 months when the intervention began and 3. were not receiving benefits from other safety net interventions. Target beneficiary was mother of an 'index child' aged 0–24 months in March 2012, residing in a poor rural HH. Exclusion criteria: village level: villages classified as urban or villages with fewer than 125 HHs were dropped. Pretreatment: outcome and control variables similar across the North and South and similar across treatment groups. Attrition per relevant group: only overall: 4992 HHs interviewed at baseline, 2498 in North and 2494 in South. In North, 2410 HHs were re‐interviewed at endline, an attrition rate of 3.5%. 78 HHs were not surveyed at endline because they had migrated, another 10 dropped out of study, refused to be interviewed or could not be found. In South, 2438 HHs re‐interviewed at endline, an attrition rate of 2.2%. 49 HHs were not surveyed at endline because they had migrated, another 7 dropped out of study, refused to be interviewed or could not be found. Using probit regressions, there was no evidence that attrition was related to treatment status or HH demographic, occupational or asset characteristics (Ahmed et al. 2016). Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: total number of HHs interviewed in North was 2410 and in South was 2438 at endline. For the outcomes related to children (due to restrictions related to age at baseline, biological children): this led to an estimation sample of 4399 children; 2218 in North and 2181 in South. Note that sample sizes differed per outcome as can be seen in the legends of the tables. Numbers per group NR. Total number enrolled per relevant group: interviewed 4992 HHs at baseline, 2498 in North and 2494 in South. Table 1 presented number of mothers/children per group at baseline, but total was 2275 for North and 2288 for South. North: cash only group: 458; food only group: 454; cash and food group: 458; cash and BCC group: 455; control: 450. South: cash only group: 454; food only group: 462; cash and food group: 446; cash and BCC group: 462; control group: 464 Total number randomised per relevant group: North included 250 clusters and 2500 HHs. Similar in South. |
|
| Interventions |
Intervention characteristics Cash only
Control: no intervention Cash and food
Cash and BCC
Food only
Food and BCC
|
|
| Outcomes | Dietary diversity: FCS; percentage with low FCS (FCS < 35) Adequacy of dietary intake: percentage with per capita daily caloric intake < 2122 calories (food poverty) Anthropometry: WHZ; HAZ Morbidity: % of children with the following symptoms in the previous 2 weeks: fever, cough or cold, diarrhoea |
|
| Identification |
Sponsorship source: funding support provided by the German Ministry for Economic Cooperation and Development, the UK's DfID, PIM, the Swiss Agency for Development and Cooperation, the United Nations Development Programme, and the USAID. Country: Bangladesh Setting: 1. rural areas of the northwest region (the 'North'), where poverty and food insecurity rates were high but where food markets functioned well; and 2. rural areas of the southern region (the 'South'), where food markets existed but were less accessible. Comments: ClinicalTrials.gov (study ID: NCT02237144) Authors' names: Akhter Ahmed. Contact author: John Hoddinott Institution: NR Email: jfh246@cornell.edu Address: NR Declarations of interest: NR Study or programme name and acronym: Transfer Modality Research Initiative (TMRI) Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Quote: "Using a random number generator, each village was assigned a random number." Comment: this was to sort the villages in ascending numerical order. They dis not report how the random sequence for allocation into each trial group was generated. |
| Allocation concealment (Selection bias) | Low risk | Allocation concealment was NR; however, this was carried out at village level. |
| Baseline characteristics similar (Selection bias) | Low risk | Outcome and control variables were similar across the North and South and similar across treatment groups. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Outcome and control variables were similar across the North and South and similar across treatment groups. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not possible but it was unlikely to have influenced the intervention delivered. |
| Blinding of outcome assessment (Detection bias) | Low risk | Core outcomes were anthropometric measures objectively reported, which lack of blinding is unlikely to influence. |
| Protection against contamination (Performance bias) | Low risk | Allocation was by village and it was unlikely that contamination occurred. Authors reported that in some localities the "… same payment point was used for both the cash group and the cash plus BCC arm,…" and that "… cash beneficiaries were paid in the morning while cash plus BCC beneficiaries were paid in the afternoon to minimize the likelihood of information from the BCC activities spilling over to the cash treatment arm." Comment: according to authors, the implementation fidelity was high, therefore, contamination was likely avoided. |
| Incomplete outcome data (Attrition bias) | Low risk | Overall attrition was low; 3.5% in North and 2.3% in South, but attrition per treatment group was NR. Reasons for HHs not being surveyed at endline in the North included "… they had migrated, another 10 dropped out of study, refused to be interviewed, or could not be found." and in the South: "49 households were not surveyed at endline because they had migrated, another seven dropped out of study, refused to be interviewed, or could not be found." Authors reported that "Using probit regressions, we found no evidence that attrition was related to treatment status or household demographic, occupational or asset characteristics (Ahmed et al. 2016)." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol accessed. |
| Other bias | Low risk | Judgement comment: misclassification bias of exposure: low risk. Exposure determined by researchers. Measurement bias: low risk. Incorrect analysis: low risk. Study accounted for the cluster design. We noted that 1 might be concerned that BCC could lead to social desirability bias affecting the IYCDDS responses – i.e. after 2 years of nutrition training, mothers might respond to questions about child feeding by over‐reporting foods commonly discussed during the group training sessions. The fact that there are differences between what mothers in the North described and what mothers in the South described – e.g. that mothers receiving BCC in the South did not report feeding their children dairy products more frequently than those in the control group – despite their receiving identical BCC gave us some confidence in these results. |
Alaofe 2016.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? in 2008, enumerators repeated surveys with each woman in the agricultural groups who had been interviewed the year before, if possible. For the village sample, enumerators returned to previously sampled HHs and interviewed the same respondent, wherever possible. If an original respondent was not present and another woman aged > 18 years in the HH could answer the questions, she was interviewed and this was noted. If a respondent's HH could not be found, a neighbouring HH was substituted and this was noted. Randomisation ratio: N/A Recruitment method: HH surveys conducted for each woman in the women's agricultural groups and for a random representative sample of HHs in each village, with women aged > 18 years as respondents. Surveys conducted following installation of the PVDI systems but before any harvest. Any women who were away from the district at the time of the survey were omitted. Sample size justification and outcome used: NR Sampling method: all HHs of women who were involved in local women's agricultural groups were sampled from 2 intervention villages and 2 matched‐pair control villages (similar in terms of location along the same roads, administrative status and size). A random, representative sample of 30 HHs in each village was also selected from each village. Study aim or objective: to evaluate the impact of SMGs on crop production diversity and dietary diversity in the Kalale district of Northern Benin. Study period: November 2007 to November 2008 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure group (n = 116)
Control group (n = 98)
Overall group characteristics: NR Inclusion criteria: HHs in 4 selected villages in the Kalale district Exclusion criteria: none reported Baseline differences: fewer literate women were in the intervention group than in the control group (P < 0.05). HH size was lower in control WG (mean 5.9 (SD 2.7)) than the intervention WG (mean 7.8 (SD 3.5)) (P = 0.2). Total number completed and analysed: intervention group: WG: n = 56; NWG: n = 60; control group: WG: n = 38; NWG: n = 60. Total number enrolled per relevant group: intervention group: WG: n = 56; NWG: n = 60; control group: WG: n = 38; NWG: n = 60 Total number randomised per relevant group: N/A Attrition: NR Description of subgroups measured and reported: for the intervention and control groups, there were 2 subgroups: HHs with women who participated in a local women's agricultural group (WG) and HHs where no‐one belonged to a women's agricultural group (NWG). |
|
| Interventions |
Intervention/exposure group: income generation through SMGs
Control: no intervention (usual circumstances of hand‐watered irrigation) |
|
| Outcomes | HH food expenditure: proportion of income spent on food; foods purchased in dry season Dietary diversity: variety of fruits and vegetables consumed |
|
| Identification |
Sponsorship source: quote: "We would like to acknowledge the Solar Electric Light Fund (SELF) for implementing the PVDI project, ICRISAT technicians for their extension work with project farmers, and l'Institut de Recherche Empirique en Economie Politique (IREEP, Cotonou, Benin) for their enumeration of the HH surveys. This project was supported by an Environmental Ventures Projects grant from the Woods Institute for the Environment at Stanford University." Country: Benin Setting: Kalale district in northern Benin, which is a rural setting without an electricity grid, no secondary school and "100 km from a paved road;" 85–90% of HHs totally depended on agriculture for livelihoods. Many women's agricultural groups were engaged in small‐scale vegetable production before project implementation; as such, this PVDI project fit within social and cultural norms. Authors' names: Halimatou Alaofe; Jennifer Burney; Douglas Taren Email: halaofe@email.arizona.edu; burney@stanford.edu; taren@email.arizona.edu Declarations of interest: quote: "The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article." Study or programme name and acronym: Solar Market Gardens (SMGs) Type of record: 2 journal articles Trial registration: N/A |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA study. No randomisation of intervention. |
| Allocation concealment (Selection bias) | High risk | CBA study. No random allocation of intervention. |
| Baseline characteristics similar (Selection bias) | Low risk | Although there were some baseline differences between the intervention and control groups, the regression analysis was adjusted for variables such as age, education, local languages, occupation, HH size and consumption expenditures. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Quote: "At baseline, there was no significant difference in the variety of fruits and vegetables produced and consumed between the 4 groups." "… there were no significant differences in food purchases during the dry season between the 4 groups at baseline." |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding not possible, but unlikely that a lack of blinding affected outcomes. |
| Blinding of outcome assessment (Detection bias) | High risk | NR by study authors but outcomes were self‐reported and likely to be influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Allocation by village and contamination was unlikely. |
| Incomplete outcome data (Attrition bias) | Unclear risk | It is NR how many HH from the baseline survey per group were N/A for endpoint survey. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. |
| Other bias | Low risk | Misclassification bias: low risk. Measurement bias: low risk. Structured questionnaire on HH food consumption. Recall period of 1 month during dry season. Seasonality bias: low risk. Follow‐up survey conducted during the same season. |
Alaofe 2019.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? The analytic sample was restricted to HHs or mothers with complete data at baseline and endline for a given indicator. Pregnant women at baseline (n = 3) or endline (n = 8) excluded from analyses. ITT protocol used for analysis as 19 SMG WGs at baseline became SMG NWGs at follow‐up and 2 SMG NWGs became SMG WGs. Randomisation ratio: N/A Recruitment method: villages: before the baseline evaluation, villages in the district of Kalalé were identified for possible inclusion in the SMG. WG HHs: only 1 mother or carer of childbearing age (15–49 years) who had a child aged 6–59 months at time of baseline survey (January–March 2014) was invited to participate. NWG HHs: delegates/leaders of the selected villages were contacted to obtain a complete listing of all NWG HHs with a target mother–child. From that list, a single HH was selected as a starting point, using a random number between 1 and the required number of HHs in village. Sample size justification and outcome used: sample size based on available funds with expectation that it would be able to show differences in agricultural production and changes in food security when scaled up from the original pilot study. Sample size was not based on changes in nutritional status. Sampling method: purposive (villages) and random (control HHs): participating villages needed to have potential water sources (as determined by geophysical survey to map groundwater) to support production during dry season. 16 eligible villages identified. Delegates/leaders of selected villages were contacted to obtain a complete listing of all NWG HHs with a target mother–child. From that list, a single HH was selected as a starting point, using a random number between 1 and the required number of HHs in village. Study aim or objective: to examine the impact of a 1‐year solar‐powered drip irrigation SMG programme in Kalalé district of northern Benin on mothers' nutritional status and micronutrient levels. Study period: January–March 2014 to February–March 2015 Unit of allocation or exposure: cluster: villages (16 eligible villages identified, matched and assigned to 1 of 2 groups) |
|
| Participants |
Baseline characteristics Intervention: WG
Control: WG
Intervention: NWG
Control: NWG
Overall
Inclusion criteria: villages: participating villages needed to have potential water sources (as determined by geophysical survey to map groundwater) to support production during dry season. Control group: similarity along several variables, including pre‐existing local WG, location along the same roads, administrative status and size. HH: women in an agricultural group, each of whom farmed her own 120 m2 plot (SMG WG and control WG); women NOT in an agricultural group (SMG NWG and control NWG). Women: in each investigated HH, only 1 mother or carer of childbearing age (15–49 years) who had a child aged 6–59 months at time of baseline survey (January–March 2014) was invited to participate in the impact evaluation. Exclusion criteria: NR Pretreatment: at baseline, there was no significant difference in HH religion, ethnicity, access to an improved source of water, self‐reported food insecurity, mothers' education level and occupation between SMG and control groups. However, a greater proportion of SMG WG HHs had older mothers, access to latrines, healthcare insecurity and high SES compared with the other 3 groups (P < 0.05). In addition, HH size in SMG NWG was lowest compared with the other 3 groups while the prevalence of access to electricity was greatest (Table 1). Attrition per relevant group: outcome: BMI: intervention group: total 161/415 (38.8%) (WG women 56/187 (30.0%); NWG women 105/228 (46.1%)); control group: total 136/359 (37.9%) (WG women 40/126/(31.7%); NWG women 96/233 (41.2%)). Outcome: HDDS: intervention group: total 111/415 (26.7%) (WG women 39/187 (20.9%); NWG women 72/228 (31.6%)); control group: total 58/359 (16.1%) (WG women 14/126 (11.1%); NWG women 44/233 (18.9%). Outcome: Hb: intervention group: total 111/415 (26.7%) (WG women 39/187 (20.9%); NWG women 72/228 (31.6%)); control group: total 95/359 (26.5%) (WG women 26/126 (20.6%); NWG women 69/233 (29.6%)). Outcome: iron: intervention group: total 148/415 (35.7%) (WG women 62/187 (33.2%); NWG women 86/228 (37.7%)). Control group: total 119/359 (33.1%) (WG women 37/126 (29.4%); NWG women 82/233 (35.1%)). Outcome: Vitamin A: intervention group: total 145/415 (34.9%) (WG women 61/187 (32.6%); NWG women 84/228 (36.8%)); control group: total 119/359 (33.1%) (WG women 37/126 (29.4%); NWG women 82/233 (35.1%)). There was some attrition from baseline to follow‐up (4.3%) that was spread across villages, with no structural differences in terms of who was most likely to dropout. Most common reason was that mothers/carers were working on their land or moved/travelled out of village on day of data collection. In addition, some blood samples were unsuitable for further processing: 5.74% due to haemolysis, 0.47% were specimens without proper requisition slips and 3.23% had insufficient sample quantity. Description of subgroups measured and reported: intervention villages: WG: HHs with women who participated in a local women's agricultural group and NWG: HHs where none of the women belonged to a women's agricultural group. Control villages: WG: HHs with women who participated in a local women's agricultural group and NWG: HHs where none of the women belonged to a women's agricultural group. Total number completed and analysed per relevant group: depended on outcome. SMG WG: BMI, n = 131 (83.44%); HDDS, n = 148 (81.32%); Hb, n = 148 (86.05%); iron, n = 125 (79.625%); vitamin A, n = 126 (79.25%). SMG NWG: BMI, n = 123 (72.35%); HDDS, n = 156 (71.23%); Hb, n = 156 (77.61%); iron, n = 142 (78.45%); vitamin A, n = 144 (81.82%). Control WG: BMI, n = 86 (90.53%); HDDS, n = 112 (90.32%); Hb, n =100 (90.91%); iron, n = 89 (89.90%), vitamin A, n = 89 (78.76%). Control NWG women: BMI, n = 137 (84.05%); HDDS, n = 189 (81.82%); Hb, n = 164 (83.67%); iron, n = 151 (83.43%), vitamin A, n = 151 (75.50%) Total number enrolled per relevant group: total: 771 women (intervention villages: 415 women (184 WG women; 228 NWG women); control villages: 359 women (126 WG women; 233 NWG women) Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention group: WG
Intervention group: NWG
Control group: no intervention |
|
| Outcomes | Dietary diversity: HDDS (0–12); Women's DDS (0–10) Anthropometry: BMI (mothers); prevalence of underweight (mothers) (BMI < 18.5 kg/m2) Biochemical: iron deficiency; vitamin A deficiency Morbidity: anaemia; iron‐deficiency anaemia |
|
| Identification |
Sponsorship source: University of Stanford, the Hellman Fellows Programme at the University of California, San Diego and the University of Arizona. Country: Benin Setting: rural villages in Kalalé district, northern Benin with sufficient groundwater sources to sustain agricultural production during the dry season. Comments: none Author's name: Halimatou Alaofè Institution: NR Email: halaofe@email.arizona.edu Address: NR Declarations of interest: none Study or programme name and acronym: Solar Market Garden (SMG) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | PCS; no randomisation done |
| Allocation concealment (Selection bias) | High risk | Quasi‐experimental design; allocation not concealed. |
| Baseline characteristics similar (Selection bias) | Low risk | Groups were different in many characteristics, but these were adjusted for in the analyses. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Groups were different in outcomes at baseline, but these were adjusted for in the analyses. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding, but no major impact expected on outcome measurement as only some outcomes were subjective. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether the field workers who collected the dietary intake data were blinded; however, dietary recall data were self‐reported and thus at high risk for reporting bias. Local health workers conducted the anthropometric measurements; and, therefore, there was a risk of detection bias. |
| Protection against contamination (Performance bias) | Low risk | SMG systems were only installed in intervention villages, in conjunction with local women's agriculture groups. In their analysis, the study authors reported that there was little evidence of a 'spillover' effect of these systems to NWG HHs in intervention villages, as well as to WG and NWG HHs in control villages. Note: 19 SMG WG at baseline became SMG NWG at follow‐up and 2 SMG NWG became SMG WG. |
| Incomplete outcome data (Attrition bias) | Unclear risk | High percentages of incompleteness of outcome data (e.g. BMI (37.9–38.8%); HDDS (16.1–26.7%); Hb (26.5–26.7%); iron intake (33.1–35.7%) and Vitamin A intake (33.1–34.9%). However, the study authors reported no significant differences in BMI, anaemia, iron deficiency or vitamin A insufficiency between women who dropped out compared to those who were not (data not shown). They do not report whether there were any differences in HDDS between those who dropped out and those who did not. There was some attrition from baseline to follow‐up (4.3%) that was spread across villages, with no structural differences in terms of who was most likely to dropout. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. All the important outcomes in the methods section were reported in the results section. |
| Other bias | High risk | Measurement bias: high risk. Although standardised scores were calculated, dietary data consisted of 2 recalls of 1 day each (at baseline and endline). Seasonality bias: low risk. Baseline and endline surveys conducted during the same season. |
Andaleeb 2016.
| Study characteristics | ||
| Methods |
Study design: CBA How were missing data handled? NR (only available survey data used) Randomisation ratio: N/A Recruitment method: ration cards issued to individuals or families based on their poverty status, and purchased from the PDS. In Odisha state, the KBK region, comprising 8 districts, has universal PDS access; whereas it was a targeted programme in the 22 non‐KBK districts. Sample size justification and outcome used: no sample size calculation. National‐level surveys carried out to be nationally representative of consumer expenditure; conducted by the National Sample Survey Organization. Sampling method: purposive programme placement by government as the decision to make PDS a universal programme in the KBK region based upon its history of poor nutritional outcome. Hence, the selection of districts into the programme was not random. Sample was restricted to rural areas of Odisha since the PDS revival was more effective in rural areas. KBK region – with a universal PDS – was the treatment group while the rest of Odisha was the control group. Non‐KBK districts within the same states were control group. For further robustness checks, samples restricted to the KBK districts and considered HHs without any ration card as the alternative control group, with all other HHs with a ration card (AAY/BPL/APL) as the treatment group. Study aim or objective: to determine the role of consumer food subsidies in improving nutritional intake and diet quality by evaluating the expansion of the government food assistance programme coverage in the hunger prone state of Odisha in India. Study period: about 8 years. 2004–2005 survey was baseline and the 2011–2012 survey was postintervention information Unit of allocation or exposure: cluster: districts 8 KBK districts with universal PDS (treatment) vs 22 non‐KBK districts (control). Alternative: within KBK districts: no ration card (control) vs any ration card (treatment) |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: HHs in the Odisha state of India. Treatment: HHs in 8 KBK districts in the state (alternative: HHs with ration card in KBK districts). Control: HHs in 22 non‐KBK districts in the state (alternative: HHs without a ration card in KBK districts) Exclusion criteria: NR Pretreatment: outcome variables related to macronutrient and calorie sources were all higher for the control group. Poverty levels: We estimate that the MPCE stood at INR 294.95 in the KBK districts as compared to INR 415.32 in the rest of Odisha at 2004–2005 constant prices. Mean HH consumption of rice from PDS: 8.9 kg per month KBK districts, 3.3 non‐KBK districts. Share of monthly rice consumption from PDS to total: 19% KBK, 5.2% non‐KBK. Attrition per relevant group: N/A as they are 2 repeated cross‐sectional HH surveys. Description of subgroups measured and reported: besides KBK vs non‐KBK districts, there are also analyses done comparing ration card vs no ration card HHs in the KBK districts. Total number completed and analysed per relevant group: at follow‐up, 2973 HHs were surveyed and contributed outcome data to the total group. Numbers NR for intervention and control separately. Total number enrolled per relevant group: at baseline, 3819 HHs were surveyed. Numbers NR for intervention and control separately. Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Dietary diversity: contribution of different types of food to caloric intake, e.g. cereals; non‐cereals; pulses; milk; eggs, fish and meat; vegetables and fruits; edible oils; other foods Dietary intake: intake of protein; intake of fat; ratio of nutrient intake to the RDA, multiplied by 100, e.g. caloric; protein; fat |
|
| Identification |
Sponsorship source: System of Promoting Appropriate National Dynamism for Agriculture and Nutrition (SPANDAN) initiative; housed in IGIDR and supported by Bill & Melinda Gates Foundation. Country: India Setting: rural HHs in Odisha, India Author's name: Andaleeb Rahman Email: arahman@iihs.ac.in Declarations of interest: NR Study or programme name and acronym: Public Distribution System (PDS) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA. KBK regions were by definition poorer than non‐KBK regions. |
| Allocation concealment (Selection bias) | High risk | CBA. Intervention was given to the poorest regions of the Odisha state, and control to less‐poor regions. |
| Baseline characteristics similar (Selection bias) | Low risk | Although the HHs in the treatment groups are not comparable based on the fact that the allocation of the districts in the programme is based on the poverty level, this has been taken into account in the analysis. Quote: "The present case is of purposive program placement by the government as the decision of make PDS a universal program in the KBK region was based upon its history of poor nutritional outcome. Hence, the selection of districts into the program (here, PDS) is not random. We do a slew of robustness check to ensure that we control for this later in the paper." "Results from the DID regressions are presented in Table 6. Estimates as reported in column (1) were arrived at by controlling for the district fixed effects but not for the HH characteristics. In the column (2), both district fixed effects and the HH characteristics were controlled for." |
| Baseline outcome measurements similar (Selection bias) | Low risk | Outcome variables related to macronutrient intake and sources of calories were all significantly higher in the control group: calories; protein; fat as well as calories from cereals; non‐cereals; pulses; egg, fish and meat; dairy products; vegetables and fruits and edible oil all P < 0.01. However, PSM was performed to account for the non‐random allocation of the intervention and control: there were no significant group differences for the covariates used to perform the PSM. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants were not blinded to allocation as their subsidy status was determined by their residential district; however, it is unlikely that they would have known that the national survey (from which the data were obtained) would be comparing their nutritional intake with participants receiving another intervention. Implementation of the project by local state government seems totally separate from implementation of the surveys by the respective organisation. |
| Blinding of outcome assessment (Detection bias) | High risk | It is NR whether outcomes were assessed blindly. Outcomes were assessed by self‐reported measures. |
| Protection against contamination (Performance bias) | Low risk | As intervention and control treatments were government‐assigned according to state district, it is unlikely that meaningful contamination could have occurred. Any small spillover effect at the border between the 2 areas would be diluted by the large sample sizes and geographical area. NR, but although it is controlled who could and could not buy the rice (ration card), it did not control who actually used it. |
| Incomplete outcome data (Attrition bias) | High risk | Very little information provided about attrition, but 3819 HHs were surveyed at baseline and 2973 at follow‐up, indicating a 87.8% 'response rate'. According to the supplementary data sheet, difference‐in‐difference estimates were performed on 6722 observations; roughly the sum of available baseline and follow‐up data. Therefore, it would appear that missing values were not adjusted for or imputed. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available and the paper did not follow the usual journal format with a designated Methods section. The aim of the study was to assess unspecified 'nutrient intake indicators' as well as a variety of food items in the diet, according to 6 groups. The latter have all been reported on. |
| Other bias | Low risk | Selection bias was overcome by correction for HH variables. Since we were testing for the significance of a large number of dependent variables, it might lead to higher probability of Type I errors leading to false rejection of the null hypothesis. To control for this bias, we used the summary indices approach of Clingingsmith et al. (2009) and Kling et al. (2004). |
Andersen 2015.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled: authors excluded participants without complete covariate and anthropometric outcome data from the analysis. Randomisation ratio: N/A Recruitment method: Peruvian sample recruited from 20 sampling sites selected to reflect diversity in region, ethnicity and religion; however, authors did not report how recruitment was done. Sample size justification and outcome used: NR Sampling method: within the study sites, children within the eligible age category (6–18 months) were randomly sampled for participation. Study aim or objective: to estimate the association of participation in Peru's Juntos CCT with anthropometry, language development and school achievement among children aged 7–8 years. Study period: initial recruitment of 6‐ to 18‐month‐old children started in 2002 with interim follow‐up data collected in 2006 (children aged 4–6 years) and final follow‐up data collected in 2009 (children aged 7–8 years). Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure group (n = 374)
Control (n = 586)
Overall: NR Inclusion criteria: children from the Peruvian section of the Young Lives study (poorer districts); from mountain regions only; with full Juntos participation data; from the younger cohort (aged 6–18 months at recruitment) of the Young Lives study; full covariate and anthropometric data for the 3 rounds; having had round 2 receptive vocabulary assessments completed before recruitment (if any) into the intervention; full covariate data as well as language development and school achievement outcomes at final follow‐up. Exclusion criteria: none reported Baseline differences: significant differences between intervention recipients and non‐recipients for nearly all covariates at round 1, all of which indicated an increased level of vulnerability and poverty among intervention participants; e.g. more likely to live in rural areas, have a lower wealth index, have a carer who spoke an indigenous language, and have a carer who did not complete primary education. Total number enrolled per relevant group: anthropometric: intervention > 2 years = 179 children; intervention ≤ 2 years = 195 children; controls = 586 children. Language development/school achievement: intervention = 272; controls = 586. Total number randomised per relevant group: N/A Total number completed and analysed per relevant group: anthropometric outcomes: intervention > 2 years: 188; girls 100; boys 88. Intervention ≤ 2 years: 169; girls 84; boys 85. Language development/school achievement: intervention = 243 children, control = 521 children. Attrition per relevant group: intervention (anthropometric outcomes) = 17 children (7/195 exposed for ≤ 2 years and 10/179 exposed for > 2 years); control (anthropometric outcomes) = 29/586 children; intervention (language development/school achievement outcomes) = 29/272 children; control (language development/school achievement) = 65/586 children. No reasons for attrition provided. Description of subgroups measured and reported: intervention group divided into 2 subgroups for anthropometric analysis: intervention for ≤ 2 years and Intervention for > 2 years. Both groups were compared with unexposed controls. Results presented for girls and boys. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Anthropometry: HAZ, stunting, BMI‐for‐age Cognitive function and development: language (TVIP) score, grade attainment Adverse event: overweight |
|
| Identification |
Sponsorship source: Bill Melinda Gates Foundation (Global Health grant OPP10327313), the Eunice Kennedy Shriver National Institute of Child Health and Development (grant R01 HD070993) and Grand Challenges Canada (grant 0072‐03 to the grantee, the Trustees of the University of Pennsylvania). The Young Lives Study was core funded by the UK Aid from the DfID and cofunded from 2010 to 2014 by the Netherlands Ministry of Foreign Affairs. Country: Peru Setting: poor HHs in poor districts Authors' names: Christopher T Andersen; Lia CH Fernald Email: chrisandersen@berkeley.edu; fernald@berkeley.edu Type of record: journal article Declarations of interest: no conflicts of interest. Study or programme name and acronym: Young Lives Study; Juntos conditional cash transfer programme |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Cohort study and no randomisation performed. |
| Allocation concealment (Selection bias) | High risk | Cohort study and no allocation concealment performed. |
| Baseline characteristics similar (Selection bias) | Low risk | Baseline characteristics balanced by PSM. |
| Baseline outcome measurements similar (Selection bias) | High risk | Serious baseline imbalances for overweight, stunting and TVIP score outcomes that were not adjusted for when matching controls to participants. Overweight participants were significantly lower (P < 0.05); and stunting was significantly higher (P < 0.01) for intervention participants. TVIP scores were significantly lower (P < 0.01) among intervention participants. |
| Blinding of participants and personnel (Performance bias) | Low risk | Cohort study and no blinding performed. However, this was unlikely to affect objective outcomes of weight and height. |
| Blinding of outcome assessment (Detection bias) | Low risk | Unclear whether study staff assessing outcomes were aware of Juntos exposure during the assessment procedure; however, outcomes were objective. |
| Protection against contamination (Performance bias) | Unclear risk | Unclear whether control participants may have benefited indirectly from Juntos through eligible HHs in their community (e.g. a control child taking meals at his/her friend's participating home). |
| Incomplete outcome data (Attrition bias) | Low risk | Although children without complete outcomes data were excluded from the analysis, similar proportions were excluded from the control group (n = 29, 4.9%) and from intervention groups (n = 10, 5.5% and n = 7, 3.6%), and outcomes were frequent enough that it was unlikely that the small numbers missing would greatly change the effect observed. In the Young Lives sample less than (quote) "3% of children were completely lost to follow‐up between rounds 1 and 3. Those lost to follow up were more likely to have a caretaker who spoke an indigenous language, but they were similar across all other covariates and baseline outcomes." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. All a priori stated outcomes in the Methods section were reported in the Results section. |
| Other bias | Low risk | None identified. |
Asadullah 2015.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? disaggregated attrition analysis was done to identify significant differential attrition and found none. No mention made of ITT analysis, but the footnote to Table A3 indicated the intervention sample as 2098 and control sample as 1940 HHs, which suggests that only HHs that completed the entire follow‐up (2002–2011) were included in analysis as these numbers + total attrition numbers add up to 5626 participants. Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: NR Sampling method: panel data from 4‐round surveys conducted in the Rangpur, Kurigram and Nilphamari districts in Bangladesh used. Participants recruited from extremely poor, with intervention participants recruited through a first‐order community‐based participatory wealth ranking to identify the lowest 10% of the population for income distribution. Authors did not report how recruitment for the panel data survey was done. Study aim or objective: to determine long‐term effects of phase 1 of the CFPR‐TUP programme, predominantly a one‐off transfer of livestock assets, in terms of changes in food expenditure, HH assets, food security and microfinance participation of very poor women in Bangladesh. Study period: panel data obtained at baseline in 2002, interim follow‐up in 2005 and 2008, and final follow‐up in 2011. Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure group (n = 2098)
Control group (n = 1940)
Overall group (n = 5626): NR Inclusion criteria: ultra‐poor woman who met ≥ 3 of the following 5 criteria: 1. HH dependent upon female domestic/seasonal work, e.g. begging, maid; 2. own < 10 decimals of land; 3. no active male adult member in HH; 4. no productive assets in HH; and 5. children of school age have to take paid work. Exclusion criteria: no women should have any of the 3 exclusion criteria: 1. no adult woman in the HH who is able to work; 2. participating in microfinance and 3. beneficiary of government/NGO development project. Baseline imbalance: HHs in treatment and control groups differed significantly in many baseline characteristics. Intervention group had fewer cash savings, poorer HH conditions, faced more food deficit, had a smaller number of assets, was more likely to be female headed and had fewer years of education of HH head. Male members from intervention HHs were also less likely be in non‐farm self‐employment, and more likely to be day labourers. Female members of intervention HHs were more likely to be day labourers and servants, and less likely to stay home for HH chores. Attrition per relevant group: 1588 (28.2%) HHs lost to attrition over the total survey period. 895/2993 (20%) were intervention HHs and 693/2633 (26%) were control HHs. Attrition over short‐run (2002–2005) and medium‐run (2002–2008) impact times were NR per group, but total attrition was 398 (7.1%) HHs in 2005 and 1067 (19.0%) HHs in 2008. Description of subgroups measured and reported: none reported Total number completed and analysed per relevant group: footnote to Table A3 indicates the intervention sample as 2098 and control sample as 1940 HHs. This suggests that only HHs that completed the entire follow‐up (2002–2011) were included in analysis. Total number enrolled per relevant group: intervention 2993; control 2633 Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention: poverty‐reduction programme with direct one‐off transfer of livestock and livelihood training
Control: no intervention |
|
| Outcomes | Per capita food expenditure (per day) Food security: proportion experiencing food deficit always/somewhat of a food deficit/neither experiencing food deficit nor having surplus/with surplus food Dietary intake: per capita daily energy intake, with intake < 1805 kcal/day below what is required Anthropometry: HAZ; WHZ; BMI (women) Morbidity: HH members seriously ill |
|
| Identification |
Sponsorship source: Research and Evaluation Division (RED) of BRAC Country: Bangladesh Setting: ultra‐poor HHs in poor communities Author's name: M Niaz Asadullah Email: m.niaz@um.edy.my Declarations of interest: yes; no potential conflicts of interest. Study or programme name and acronym: Challenging the Frontiers of Poverty Reduction – Targeting the Ultra Poor (CFPR‐TUP) Type of record: journal article Trial registration: N/A Protocol availability: yes |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA, therefore, no randomisation performed. |
| Allocation concealment (Selection bias) | High risk | CBA, therefore, no allocation concealment. |
| Baseline characteristics similar (Selection bias) | High risk | There were significant differences in characteristics between the groups at baseline. |
| Baseline outcome measurements similar (Selection bias) | High risk | Serious baseline imbalance for ownership of natural and physical assets (all P < 0.01 with the exception of number of goat/sheep owned: P < 0.05); food security (all P < 0.01); per capita food expenditure and income (both P < 0.01); and financial market participation (all P < 0.01 with the exception of size of outstanding lending: P < 0.10; NS). |
| Blinding of participants and personnel (Performance bias) | Low risk | There was no blinding as this was a CBA but this is unlikely to have influenced the performance of the participants. |
| Blinding of outcome assessment (Detection bias) | High risk | There was no blinding. Outcomes were measured with surveys, based on self‐reports from participants. So knowledge of treatment allocation, and perceived benefit or not from this, could have influenced their reporting. |
| Protection against contamination (Performance bias) | Unclear risk | Nothing reported regarding how contamination was prevented. It is also unclear who the control groups were so it is difficult to assess potential contamination. |
| Incomplete outcome data (Attrition bias) | High risk | Attrition was relatively high for the total follow‐up period; with higher attrition in the intervention compared to the control group (31.4% with intervention vs 25.5% with control). Although reasons for attrition were unrelated to treatment, the characteristics of those who were LTFU and those who remained in the study differed significantly, and the characteristics of people who were LTFU in the intervention and control group were also different. |
| Selective outcome reporting (Reporting bias) | Unclear risk | We could access the protocol. In the report of Rabbani et al 2006, some outcomes that are NR in the article were listed such as schooling, purpose of cash borrowing, legal awareness, social inclusion and Eid spending. Note: minor differences in baseline values between Asadullah and Rabbani. |
| Other bias | Low risk | None identified. |
Asfaw 2014.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled: data from HHs that were LTFU were excluded from the analysis (Ward 2010). For the HH spending study, a further 45 HHs were excluded due to very large values for total adjusted expenditure as well as missing values (The Kenya CT‐OVC team 2012). Randomisation ratio: 1:1 Recruitment method: NR Sample size justification and outcome used: NR Sampling method: within 7 districts, 4 locations (clusters) were selected randomly after excluding those with particularly low poverty rates or an inadequate capacity to supply the relevant health and education services, or large existing orphans and vulnerable children support programmes. List of eligible HHs was compiled in the intervention locations according to standard programme operation guidelines. In control districts, programme targeting was 'simulated' in order to identify a sample of HHs that were comparable to eligible HHs in intervention areas. Study aim or objective: 1. to determine if the Kenya CT‐OVC led to an increase in investment in agricultural and non‐agricultural productive assets and activities; increased food consumption obtained from own production; resulted in a shift in adult labour towards own agricultural and non‐agricultural activities and away from casual labour; resulted in heterogeneous impact by gender; and reduced the time children spend at work. 2. to investigate whether the CT‐OVC had changed the preferences of HHs in terms of their consumption behaviour. Study period: 4 years (March–August 2007 to May–July 2011) Unit of allocation or exposure: location within eligible district |
|
| Participants |
Baseline characteristics Overall (n = 1783)
Intervention or exposure group (n = 1265)
Control group (n = 518)
Inclusion criteria: ultra‐poor HHs and contain an OVC (defined as a HH resident aged 0–17 years with ≥ 1 deceased parent, or who was chronically ill, or whose main carer is chronically ill) in selected locations within 4 districts (Nyanza, Nairobi, Garissa, Kwale) Exclusion criteria: NR Baseline imbalance: in Asfaw et al 2014: intervention HHs had significantly older HH heads, more female‐ and elderly‐headed HHs, smaller HH size, lower education of HH head and spouse, fewer number of young and middle‐aged HH members and ill HH heads, and more elderly HH members. Intervention HHs were also less likely to use unprotected water sources, have various HH assets, but more HHs in which agriculture was the main source of income and less in which salaried employment was the main source of income. Intervention communities had more access to a road to the village and less distance to the local market, but a lower share of HHs which could make telephone calls. Intervention individuals were significantly older and more likely to be disabled, unemployed or in casual work; and had lower levels of education. For the HH spending paper (Kenya CT‐OVC 2012): intervention HHs expended significantly more of their monthly budget on tubers. Attrition per relevant group: at 24 months (Asfaw 2014): intervention group: 231/1542 (15%); control group: 184/571 (24.4%). Attrition by district (intervention clusters vs control clusters) Garissa (11.6% vs 31.6%); Homabay (14% vs 21.1%); Kisumu (15% vs 25.3%); Kwale (13.2% vs 16.1%); Migori (16.3% vs 18.7%); Nairobi 16.9% vs 47.6%); Suba (10.9% vs 20.8%) (Ward 2010). Study authors reported that the loss of HHs was partly due to postelection violence. At 48 months (Asfaw 2014): intervention group: 262/1542 (16.9%); control group: 224/755 (29.7%). The HH spending paper reported only total attrition, i.e. 16.9% (387/2294). Further post‐hoc exclusion of 45 HHs due to large values for total adjusted expenditure and missing values leads to a total 'attrition' of 18.8%. Description of subgroups measured and reported: HH size 5 vs ≥ 5; female‐headed vs male‐headed HHs Total number completed and analysed per relevant group: in the HH spending paper (Kenya CT‐OVC 2012) 1907 HHs completed baseline and 2‐year (2009) follow‐up, but only 1862 HHs were analysed due to post‐hoc exclusions. In the food consumption paper (Asfaw et al 2014), 1280 intervention and 531 control HHs completed baseline and 4‐year (2011) follow‐up, but only 1265 intervention and 518 control HHs were included. Total number enrolled per relevant group: intervention group: 1542 HHs; control group: 755 HHs Total number randomised per relevant group: 4 locations within each of 7 districts randomised to either the intervention or control group. Intervention group: 14 locations (clusters); control group: 14 locations (clusters) |
|
| Interventions |
Intervention: UCT
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food: total monthly consumption expenditure (per AE); proportion of HH monthly consumption expenditure on food; total monthly food expenditure (cereals, tubers, meat/fish, dairy, fruit/vegetables, other food, food eaten out) Dietary diversity: DDS; proportion of HHs that consumed individual food groups (e.g. cereal, fruit, etc.) in the preceding 7 days Anthropometry: HAZ; WAZ; WHZ; stunting; underweight; wasting Morbidity: number of children with reported symptoms of upper respiratory illness |
|
| Identification |
Sponsorship source: UK DfID; US National Institute of Mental Health; Eunice Kennedy Shriver National Institute of Child Health and Development Country: Kenya Setting: ultra‐poor HHs in rural areas with high prevalence of HIV/AIDS Authors' names: Solomon Asfaw; Tia Palermo; Patrick Ward Email: solomon.asfaw@fao.org; tiampalermo@gmail.com; patrick.ward@opml.co.uk Declarations of interest: no Study or programme name and acronym: Kenya CT‐OVC (Cash Transfer Programme for Orphans and Vulnerable Children) Type of record: journal articles, operational and impact evaluation report Trial registration: none reported Protocol availability: no |
|
| Notes | Population: AE: children aged < 15 years were considered as 0.75 of an adult; children aged ≥ 15 years were considered a full adult. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Authors mentioned random selection of intervention and control locations within 7 districts, but did not report how the random sequence was generated. |
| Allocation concealment (Selection bias) | Unclear risk | No information provided on how the locations within districts were randomised; or how this randomisation sequence was protected. |
| Baseline characteristics similar (Selection bias) | Low risk | Baseline differences reported between groups. The heads of treatment HHs were older (P ≤ 0.01), more likely to be male (P < 0.05) and to have less education (P < 0.01) than those in control HHs. Intervention HHs also had significantly fewer assets (99% CI). The proportion of control HHs that had agriculture as the main source of income was significantly lower (90% CI). The 24‐month analyses adjusted for baseline HH demographic composition (Kenya CT‐OVC team 2012), whereas the analysis after 4 years used estimated propensity scores to account for these baseline differences (Asfaw 2014). |
| Baseline outcome measurements similar (Selection bias) | Low risk | No baseline non‐equivalence was detected for the HH spending (Kenya CT‐OVC 2012) paper; with the exception of proportion AE monthly expenditure for tubers which was significantly higher in the intervention group (P = 0.005). Outcomes such as HH expenditure on food and proportion of children with underweight or stunting, or both (< –2SD z‐scores) were similar between the groups. There was no baseline non‐equivalence for the HH spending paper; with the exception of proportion AE monthly expenditure for tubers, which was significantly higher in the intervention group (P = 0.005). All outcomes for the food consumption paper were NR for the baseline survey. |
| Blinding of participants and personnel (Performance bias) | Low risk | Given the way in which the intervention was rolled out, it is not possible for participants to be blinded. However, it is unlikely that lack of blinding influenced behaviour of participants and personnel beyond that expected by the intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | There was no blinding. As outcomes were predominantly self‐reported it is likely that the lack of participant blinding would have affected the measurement of outcomes. |
| Protection against contamination (Performance bias) | High risk | Quote: "Taylor et al. (2012) simulated the local economy impact and revealed a minimal inflationary impact and real production value added multipliers of Ksh1.58 [KES] per shilling transferred, which suggests that the programme may have led to spillovers." |
| Incomplete outcome data (Attrition bias) | High risk | High attrition and no ITT analysis performed. Differential attrition between the 2 groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. |
| Other bias | High risk | Misclassification bias: high risk due to self‐report of CCT receipt by HHs. Measurement bias: unlikely. Incorrect analysis: unlikely. Recruitment bias: high risk. Clusters were assigned before recruitment of HHs; which may have lead to a bias in participation, especially for control HHs. Other bias: the introduction of punitive conditionalities in some intervention clusters, but not others, may have lead to bias in attrition or bias in outcome measurement. |
Baird 2013.
| Study characteristics | ||
| Methods |
Study design: cRCT How were missing data handled: for the analysis of the postintervention follow‐up data, the study authors stated: "We conducted all analysis among those who were successfully interviewed in Round 4, which maximises sample size for the estimation of longer‐term impacts." Randomisation ratio: 1:1 Recruitment method: after the random selection of EAs and individuals into the treatment group, the local NGO implemented the cash transfers held meetings in each treatment EA between December 2007 and January 2008 to invite the selected individuals into the programme. At these meetings, the programme beneficiary and her parents/guardians were offered the monthly transfer amounts. This consisted of a transfer to the parents, a transfer directly to the girl and payment of school fees for girls attending secondary school. Transfer amounts to parents were varied randomly across EAs at USD 4, USD 6, USD 8 and USD 10 per month, so that each parent within an EA received the same offer. Within each EA, there was a lottery to determine the transfer amount to the programme beneficiaries, which was USD 1, USD 2, USD 3, USD 4 or USD 5 per month. The lottery was held publicly to ensure that the process was transparent. Secondary school fees were paid in full directly to schools. Sample size justification and outcome used: NR Sampling method: stratified random sampling. Zomba district contains 550 EAs (Zomba city 50; rural traditional authorities 500). 176 EAs were selected from 3 different geographical strata: urban (Zomba city, 29 EAs), near rural (16 km from Zomba city, 119 EAs) and far rural (≥ 16 km from Zomba city, 28 EAs). Of the 50 EAs in Zomba city, 21 were excluded on the basis of advice from local experts who deemed these areas too affluent for the proposed intervention. In each of the 2 rural strata, with the exception of 1 TA that was unsafe for field work, the study EAs were randomly selected. In the 176 sampled EAs, each dwelling was visited to take a census of all never‐married girls aged 13–22 years (sample frame). Girls were grouped according to those enrolled in school at baseline (baseline schoolgirls), or those not enrolled in school at baseline (baseline dropouts). In the cohort of baseline schoolgirls, a subset of eligible girls was randomly selected for the study. The sampling percentages for this cohort differed by geographical stratum and age group and was 14–45% in urban areas and 70–100% in rural areas. All the girls who were not enrolled in school at baseline (baseline dropouts) were sampled to participate in the study This sampling procedure yielded a baseline study sample of 4051 girls of whom 3796 (94%) were enrolled and completed a baseline interview at the end of 2007. Of these, 889 were baseline dropouts and 2907 were baseline schoolgirls. Study aim or objective: to examine whether a cash transfer programme targeted at adolescent girls in Malawi helped empower its recipients in the short‐run, i.e. during and immediately after the 2‐year intervention. Study period: 2007–2012 Unit of allocation or exposure: females aged 13–22 years |
|
| Participants |
Baseline characteristics Overall group (n = 2706): NR Intervention or exposure group (n = 1211)
Control group (n = 1495)
Inclusion criteria: never‐married girls aged 13–22 years enrolled in school at baseline (baseline schoolgirls), and those not enrolled in school at baseline (baseline dropouts) in selected 176 EAs. Exclusion criteria: NR Baseline imbalance: in the girls who attended school at baseline, those in the CCT group were younger than those in the UCT group, and, therefore, also a lower grade attained. Attrition per relevant group: reported at postintervention follow‐up (2 years after intervention): baseline school girls: control group: 10.7%; intervention group: NR. Baseline dropouts: control group: 15.7%; intervention group: NR. Reported at second postintervention follow‐up (4 years after intervention): Baseline school girls: control group: 12.5%; intervention group: NR. Baseline dropouts: control group: 15.7%; intervention group: NR Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: NR Total number enrolled per relevant group: baseline school girls: CCT intervention group: 685 girls from 27 intervention EAs; UCT intervention group: 526 girls from 46 intervention EAs. Control group: 1495 girls from 88 control EAs. Baseline dropouts: CCT intervention group: 436 girls from 88 intervention EAs. Control group: 453 girls from 88 control EAs Total number randomised per relevant group: intervention group: 88 EAs; control group: 88 EAs |
|
| Interventions |
Intervention: CCT and UCT
Control: no intervention |
|
| Outcomes | Dietary diversity: number of times respondents ate protein‐rich food in past 7 days Cognitive function and development: cognitive test scores (Raven's Coloured Progressive Matrices) Anxiety and depression: psychological distress (GHQ‐12 score) |
|
| Identification |
Sponsorship source: Global Development Network, the Bill and Melinda Gates Foundation, NBER Africa Project, World Bank Research Support Budget Grant, 3ie Open Window (Round 2) as well as several trust funds at the World Bank: Knowledge for Change Trust Fund (TF090932), World Development Report 2007 Small Grants Fund (TF055926), Spanish Impact Evaluation Fund (TF092384) and Gender Action Plan Trust Fund (TF092029). Country: Malawi Setting: urban and rural HHs, Zomba district Author's name: Sarah J Baird Email: sbaird@gwu.edu; bozler@worldbank.org; ctmcintosh@ucsd.edu Declarations of interest: yes; no conflicts of interest Study or programme name and acronym: Schooling, Income, and Health Risks study (SIHR) Type of record: journal article, policy research working paper Trial registration: none reported Protocol availability: no |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Clusters (EAs) randomly assigned to intervention or control groups with computer‐generated random numbers. Within intervention group, EAs were randomly assigned to 1 of 2 intervention groups (UCT or CCT groups). Girls in the intervention EAs were allocated to different cash transfers by drawing numbers from an envelope. |
| Allocation concealment (Selection bias) | Low risk | Allocation by EAs at start of study. Codes for randomisation of the EA into trial groups, and for random assignment of different cash transfer amounts, were written by 1 of the study investigators. The programme field manager then studied staff with EA identification numbers and individuals selected. |
| Baseline characteristics similar (Selection bias) | Low risk | For baseline school girls, those in CCT group were younger than those in UCT group, and, therefore, also attained a lower grade. The study authors controlled for this difference in their analysis of programme impacts. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Relevant baseline outcome measurements, e.g. food consumption not presented by study authors. |
| Blinding of participants and personnel (Performance bias) | Low risk | Quote: "study participants were not masked to their assignment, but did not know what the comparison groups were because they were assigned at the enumeration area level." |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether the outcome assessors were blinded but outcomes were self‐reported and likely to be influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | To reduce the possibility of crossover from intervention group to control group, participants were assigned to trial groups on basis of random assignment of EAs that they lived in. |
| Incomplete outcome data (Attrition bias) | Low risk | Loss of clusters: low risk. Study authors stated that none of the EAs had complete LTFU. Attrition rates at second postintervention follow‐up were reported as 15.7% in control group of baseline dropouts. Study authors reported that girls in this group who received CCT and who were from urban areas, were more likely to be LTFU. In baseline school girls, attrition was 12.5%, with no differences in baseline characteristics of those who remained in the study, compared to those LTFU. |
| Selective outcome reporting (Reporting bias) | Low risk | Outcomes reported were in line with those prespecified in the trial registry preanalysis plan. |
| Other bias | Low risk | Misclassification bias: unclear. Recruitment bias (cRCT): low risk. A baseline survey was conducted among all eligible participants in all the EA before randomisation of EA. Measurement bias: low risk. Outcomes reported at baseline and follow‐up included the number of times the respondent ate protein‐rich food in the 7 days prior. Incorrect analysis: unlikely. Seasonality bias: unclear risk. Low risk of seasonality bias for follow‐up during the intervention period; however, it was unclear whether the study authors adjusted for seasonality in the postintervention follow‐up analysis. |
Beegle 2017.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? NR Randomisation ratio: 1:1:1:1:1 (according to table 1) Recruitment method: village headmen together with the village committees select HHs to participate. Specific recruitment methods NR Sample size justification and outcome used: NR Sampling method: sampling for the trial: of 28 districts with the PWP programme, 12 districts randomly sampled, stratified by geographic region. Of these 12 districts, 182 villages (EAs) that had been sampled for the national survey in 2010–2011 AND preselected for PWP were selected. These were then randomised to the treatment groups. Villages in the sampling frame were randomly assigned to 1 of 5 groups. Group 0 was control group of villages that were not included in PWP programme in 2012–2013 Season. Groups 1–4 participated in the PWP in the planting season (cycle 1 of PWP). These 4 groups varied in terms of timing of the second cycle of programme and the schedule of payments in both cycles. At HH level: they choose 10 HHs from the 16 survey HHs in the village to be offered the programme. Sampling for MSFA programme covered all districts of Malawi through a 2‐stage targeting approach. In the first stage, there was pro‐poor geographic targeting and in the second there was a combination of community‐based targeting and self‐selection of beneficiaries. The amount of funds given to a district was proportional to the district's population and to the poverty rates as well as other measures of vulnerability. District officials then targeted a subset of EPAs based on poverty and vulnerability criteria. Traditional authorities in the EPAs then allocated funds to a subset of selected GVH who each oversaw 3–10 villages. The GVH determined how many HHs participated in each village based on available funding; the GVH then worked with the village committees in each village to select participating HHs. Study aim or objective: to determine the impact of these programmes by estimating the effect of Malawi's large‐scale PWP, which operates under the MSAF to improve food security and increase the use of fertiliser and other agricultural inputs. The MASAF PWP has been operational since mid‐1990s and aimed to provide short‐term labour‐intensive activities to poor, able‐bodied HHs for the purpose of enhancing their food security, mainly through increased access to farm inputs during the planting period. Programme was designed to be interlinked with Malawi's large‐scale FISP through the implementation of the PWP in the planting months of the main agricultural season when the FISP distribution also occurs. The premise behind this is that the PWP facilitates poor, credit‐constrained HHs to access subsidised fertiliser. Study period: baseline: 2010–2011 (based on data collected during the national integrated HH survey. Endline: November 2013. Data come from 5 rounds of panel HH survey data. Unit of allocation or exposure: villages allocated to control or intervention. Within villages, HHs were randomly selected. |
|
| Participants |
Baseline characteristics Intervention or exposure: NR Control: NR Overall: NR Inclusion criteria: project: poor, able‐bodies HHs. Exclusion criteria: NR Pretreatment: 2 analysis carried out: for 23 villages included in sample but that had not been included in the national HH survey; and for 159 villages included that had been part of the national HH survey. For the former, analyses are based on round 1 of data collection, when interventions had not started in all but 3 villages but knowledge of PWP implementation existed and could have influenced behaviour. For the latter, they explored the balance between treatment and control villages in terms of pretreatment covariates and outcomes, they used the IHS3 data from 2010–2011. Using the first round of follow‐up data, they found that HHs in the non‐IHS3 sample were better off than the IHS3 sample, with better educated HH heads, smaller HH sizes and fewer children aged < 14. However, there was imbalance in preprogramme food security at both the village and HH levels in the 159 villages for which IHS3 data were available. The IHS sample was well balanced for a range of non food‐security outcomes. Attrition per relevant group: NR Description of subgroups measured and reported: effects by geographic region Total number completed and analysed per relevant group: NR: only total number of observations reported. Total number enrolled per relevant group: 10 HHs in each village offered the programme Total number randomised per relevant group: group 0 (control): 38 communities; group 1 (cycle 1: planting season, cycle 2: harvest season; lump sum): 40 communities; group 2 (cycle 1: planting season, cycle 2: harvest season; split payment): 34 communities; group 3 (cycle 1: planting season, cycle 2: lean season; lump sum): 35 communities; group 4 (cycle 1: planting season, cycle 2: lean season; split payment): 35 communities. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Food security: Food Security Score; Resilience Index; Principal Components Analysis Index Dietary diversity: FCS; number of food groups consumed in the last week for 7 main groups Dietary intake: log per capita food consumption for the last week; per AE calories of the food consumed |
|
| Identification |
Sponsorship source: World Bank Research Committee, Knowledge for Change programme and GLM‐LIC (grant number C2‐RA2‐211). Country: Malawi Setting: poor and able‐bodied HHs in 3 regions of Malawi Author's name: Kathleen Beegle Email: kbeegle@worldbank.org (K Beegle); egalasso@worldbank.org (E Galasso); goldberg@econ.umd.edu (J Goldberg). Declarations of interest: NR Study or programme name and acronym: MASAF PWP (Malawi Social Action Fund's Public Works Programme) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "Villages were randomly assigned (by computer) to one of the four treatment groups or a control condition; households within treatment villages were randomly selected to be offered the program." |
| Allocation concealment (Selection bias) | Low risk | Allocation to treatment group was done at village level. Quote: "Villages were randomly assigned (by computer) to one of the four treatment groups or a control condition; households within treatment villages were randomly selected to be offered the program." |
| Baseline characteristics similar (Selection bias) | High risk | Allocation to treatment group was done at village level. Quote: "Villages were randomly assigned (by computer) to one of the four treatment groups or a control condition; households within treatment villages were randomly selected to be offered the program." |
| Baseline outcome measurements similar (Selection bias) | High risk | Even though randomisation was conducted by computer, there was imbalance in preprogramme food security at both the village and HH levels in the 159 villages for which IHS3 data were available. Unclear how well these were adjusted for in the analyses. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not possible for this type of intervention; however, it was unlikely that lack of blinding would have influenced the delivery of the intended intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | Outcome assessment was not blinded. Data were based on HH surveys, therefore, self‐reported data. Knowledge of intervention allocation could have biased responses. |
| Protection against contamination (Performance bias) | Low risk | Authors only reported contamination in relation to untreated HHs in villages selected to receive the PWP intervention. Allocation was by village and it was unlikely that the control group received the intervention. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Number of villages were reported but not number of HHs and individuals assessed at the start and endline. It was unclear if there was any attrition or not. |
| Selective outcome reporting (Reporting bias) | Unclear risk | 2 outcome measures were omitted due to space constraints. A composite measure was compiled and included. |
| Other bias | Unclear risk | Misclassification bias of exposure: low risk. Treated and control assigned externally. Measurement bias: unclear risk. Authors did not report which tools were used to collect data, who did it and whether they were validated. They only reported and defined the food security outcomes assessed. Incorrect analysis: low risk. Analyses adjusted for clustering. Recruitment bias: low risk. HHs in allocated villages were randomly selected to participate. |
Breisinger 2018.
| Study characteristics | ||
| Methods |
Study design: controlled trial (using regression discontinuity for allocation) How were missing data handled? It is assumed that missing data were excluded. The intended sample for the Takaful and Karama analysis components consisted of 7996 HHs. Of these, 1144 HHs could not be located based on the address data in the registration form. An additional 261 HHs were visited but no HH members could be located, and 70 HHs were not surveyed due to other reasons including declining to participate in the survey, no capable respondent being identified, being part of another HH already in the sample or the registrant having died. Considering only HHs for which there was no error in the location information, the overall response rate was 95.2%. Randomisation ratio: N/A Recruitment method: see sampling methodology. Sampled HHs were visited by an interviewer. Sample size justification and outcome used: outcome used NR. Justification: based on power calculations that the evaluation team conducted to determine the sample size required for the TKP impact evaluation, the study required 8016 HHs spread across 501 clusters (villages), with 16 HHs per cluster. Authors purposefully selected more than the 16 HHs per cluster knowing that there was a risk of being unable to locate all the HHs in the registrant sample. Sampling method: targeting for programme: to avoid inefficient targeting, the programme combined geographical targeting with a PMT mechanism. With respect to the geographical targeting, the programme was first launched in the poorest districts within the poorest governorates in Egypt. The PMT was used to identify the poor within the selected districts, based on selection criteria and a set cutoff score, based on the poverty line derived from Egypt's HH Income, Expenditure and Consumption Survey for 2012–2013. In addition to the PMT, both Takaful and Karama have other categorical selection criteria; Takaful requires that beneficiaries have children and Karama requires that beneficiaries be elderly or disabled (or both), or (added later) orphaned. PMT formula varies by region but the threshold is the same across all regions. Over time, since the programme started and across the 4 enrolment waves, the threshold has been changed. Sampling for the impact evaluation survey: "The sampling strategy for the TKP Impact evaluation was designed to provide a representative sample of Takaful and Karama HHs with Proxy Means Test scores near the thresholds for an RD [regression discontinuity] approach to impact analysis. Stratification for the sample selection was based primarily on region. For the Upper Rural region of Egypt, they stratified by governorate (9 governorates in Upper Rural). As such, they defined 14 strata: 5 for each region excluding Upper Rural and 9 strata for Upper Rural. They sampled VCs within the 14 region‐governorate strata using simple random sampling, where the number of clusters per stratum was proportional to the share of registrants in each stratum, and restricted selection to clusters in which there was a sufficient number of registrants near the threshold. The clusters were defined as Takaful‐only clusters (325) or mixed Takaful and Karama clusters (75). Within each village, 20 HHs were randomly selected for inclusion in the survey if they were within 600 points of the current Takaful threshold score of 4500 or 200 points of the Karama threshold of 7203. On average, they selected 10 eligible and 10 ineligible HHs, and for Takaful HHs, they weighted the probability of selection such that HHs within 200 points of the current threshold of 4500 were 2.5 times more likely, and HHs within 200–400 points of the cutoff were 1.5 times more likely to be selected than those that were 400–600 points from the cutoff. They selected more HHs than the 16 HHs per cluster that the power calculations suggested would be necessary, knowing that there was a risk of not being able to locate all the HHs in the registrant sample. Study aim or objective: objective of programme: Takaful and Karama is a conditional 5 cash transfer programme that seeks to provide income support to poor families with children (under 18 years of age), poor elderly (aged ≥ 65 years) and people with severe disability. Objective of impact evaluation: to provide rigorous evidence on the impacts of the programme on HH consumption, poverty and other measures of well‐being including child education, health and food security, and the prevalence of overweight and obesity in adult women. Study period: approximately 28 months. Programme start: March 2015; impact evaluation survey: 15 July to 30 August 2017. Takaful beneficiaries were in programme for about 11 months on average. Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure: NR Control: NR Overall: NR Inclusion criteria: 1. Eligible governorates: those where the share of Takaful‐eligible HHs (HH eligibility defined as having a PMT score ≤ 4500) in the governorate was ≥ 0.5%. Therefore, governorates that had a very small share of eligible HHs in TKP were excluded, in part to help manage survey costs. The only exception was governorates in the Frontier region, where the share of eligible HHs was < 0.5%. These governorates were kept so that the Frontier region, which may have had different sources of poverty and food insecurity, was represented in the evaluation sample. 2. Eligible VCs for Takaful: those that had ≥ 7 Takaful eligible HHs. 3. Eligible VCs for Karama: those that had ≥ 6 Karama eligible HHs with a PMT score 7000–7400 and had ≥ 1 elderly (aged ≥ 65 years) or disabled member. Exclusion criteria: PMT‐score‐based targeting, if they met 1 of 6 exclusion criteria: owned a car, owned > 1 feddan of land, had a government job or pension, received transfers from abroad or had a formal private sector job with insurance. No children. Pretreatment: Tables A2.1–A2.6 showed that of 20 HH characteristics all but 1 showed a statistically significant difference for beneficiaries vs non‐beneficiaries. Therefore, the HHs on either side of the cutoff were similar and provided valid comparison groups. There were NO baseline data – the above related to (quote): "Finally, we check whether adding some HH characteristics to the specifications affects our impact estimates. Rather than include all of the variables in the PMT score (which would be endogenous and also highly correlated with the PMT score, which is a requirement for inclusion in the generalised IV and RD models), we include a subset of potentially exogenous HH characteristics (such as HH size, education level of the HH head) as controls in the specification." Attrition per relevant group: as there was no baseline and follow‐up of participants in this study, no attrition was reported. Authors reported that since only HHs for which there was no error in the location information were included, the overall response rate was 95.2%. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: total number of HHs surveyed: 6003; beneficiary 2190; non‐beneficiary 3813 Total number enrolled per relevant group: no baseline data. Total number of HHs surveyed: 6003; beneficiary 2190; non‐beneficiary 3813 (however, there was a potential error in the data (numbers in 'details' column of table 3.3.2 do not equal the numbers in 'number of HHs column') Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Dietary diversity: HH DDS (0–12); mother's DDS; child 6‐ to 23‐month DDS; child 24‐ to 59‐month DDS Anthropometry: HAZ; wasted Morbidity: % children aged < 5 years who had diarrhoea in past 4 weeks; % children aged < 5 years who had fever in past 4 weeks Adverse outcomes: overweight |
|
| Identification |
Sponsorship source: UK Foreign and Commonwealth Office (UK FCO) Country: Egypt Setting: poor HHs. Districts: the rollout phases were: first wave launched in the poorest 19 districts of 6 governorates in Upper Egypt (Suhag, Assiut, Luxor, Qena, Aswan and Giza); where poverty rate was ≥ 50%. Through the second wave, the programme expanded to districts where poverty rate was ≥ 30%. In the third wave, the programme was expanded further, covering districts where poverty rate was to ≥ 17.9%. Finally, fourth wave opened registration to all districts (MoSS biannual report, December 2016). Author's name: Clemens Breisinger Email: ifpri@cgiar.org Declarations of interest: NR Study or programme name and acronym: Takaful cash transfer programme and Karama cash transfer programme Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | No randomisation done. Study approximated a controlled trial, which used a regression discontinuity design to define allocation to study groups (i.e. according to a threshold for inclusion in the intervention). |
| Allocation concealment (Selection bias) | High risk | Allocation was not concealed. Study approximated a controlled trial, which used a regression discontinuity design to define allocation to study groups (i.e. according to a threshold for inclusion in the intervention). |
| Baseline characteristics similar (Selection bias) | Unclear risk | Although technically there were no baseline measurements, it was indicated that (quote) "Finally, a key assumption for our estimation strategy is that the households just above and just below the threshold are similar in household characteristics. Annex II Tables A2.1–A2.6 provide evidence that this is indeed the case." |
| Baseline outcome measurements similar (Selection bias) | High risk | No baseline data available. Although HH characteristics not related to the outcomes were the same, this might not be the case for the outcomes itself. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not possible but it is unlikely that lack of blinding caused a deviation in how the intervention was implemented. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear if interviewers were blinded. Blinding was not possible. Outcomes were assessed based on data self‐reported by the participants. Participants were aware whether they had been approved to receive transfers or not, and this may have influenced their responses. |
| Protection against contamination (Performance bias) | Low risk | Assignment was at HH level, based on the PMT score threshold. The threshold varied over time, after the programme started, so different HHs were enrolled over the different enrolment waves, so that some HHs that did not qualify for the intervention in 1 wave could qualify in the subsequent wave. However, the analyses were based on instrumental variables model, which takes into account the different thresholds over time. |
| Incomplete outcome data (Attrition bias) | Low risk | All HHs surveyed were analysed. Quote: "Considering only households for which there was no error in the location information, the overall response rate was 95.2 percent." |
| Selective outcome reporting (Reporting bias) | Unclear risk | Authors mentioned a protocol that was submitted to an ethics review board, but we were unable to access it. |
| Other bias | Low risk | Misclassification bias of the exposure: low risk. Exposure assigned externally and confirmed with administrative data. Measurement bias: low risk. |
Brugh 2018.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel How were missing data handled? 162 HHs (4.6%) LTFU and 70 HHs with missing data were excluded from the analysis. Randomisation ratio: 1:1 Recruitment method: NR Sample size justification and outcome used: evaluation team calculated number of VCs that would need to be visited based on the number of total eligible. HHs in VCs. Additionally, the statistical power of the study was based on having a minimum number of VCs included. There needed to be ≥ 29 VCs included in the study. Sampling method: in the first sampling stage, 2 traditional authorities were randomly selected from each of the 2 study districts. The second sampling stage consisted of randomly selecting 14 VCs within the 2 traditional authorities in Mangochi and 15 VCs from Salima for a total of 29 study VCs. The final sampling stage was at the HH level; in Mangochi VCs, where the number of eligible HHs tended to be high, 125 eligible HHs were randomly selected in each of the 14 study VCs. All eligible HHs were selected for interview in Salima study VCs. Study aim or objective: evaluation of the expansion of the Malawi's Social Cash Transfer Program on HH food insecurity and dietary diversity. Study period: June–September 2013 to November 2014–January 2015 Unit of allocation or exposure: VCs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: HHs in Mangochi and Salima districts that were either ultra‐poor (unable to meet the most basic urgent needs, including food and essential non‐food items, e.g. soap and clothing) or labour‐constrained (HH had no 'fit to work' members or the ratio of 'unfit' to 'fit' > 3; HH members were 'unfit if aged < 18 years or > 64 years, or if they aged 18–64 but had chronic illness, disability or are otherwise unable to work). Beneficiary selection through a community‐based approach with oversight provided by the local District Commissioner's Office and the District Social Welfare Office. Exclusion criteria: NR Pretreatment: no baseline differences. Attrition per relevant group: intervention group: 70 HHs LTFU (4.2%); missing outcome data (2.8%). Control group: 92 HHs LTFU (4.9%); missing outcome data 32 HHs (1.7%). HHs that were LTFU did not differ from HHs that remained in the study (analysis reported by Abdoulayi et al. 2015) Description of subgroups measured and reported: level of HH's transfer share (low vs high: > 30%; 20–30%; 15–20%; ≤ 15%) Total number completed and analysed per relevant group: intervention group: 1561 HHs; control group: 1729 HHs; total 3290 Total number enrolled per relevant group: intervention group: 1678 HHs; control group: 1853 HHs; total: 3511 Total number randomised per relevant group: intervention group: 14 VCs; control group: 15 VCs |
|
| Interventions |
Intervention
Control: no intervention for the duration of the study; implementation of the cash transfers in the control group was delayed until study was completed. |
|
| Outcomes | Proportion of HH expenditure on food Food security: worried not enough food; having > 1 meal per day Dietary diversity: HDDS Adequacy of dietary intake: proportion food energy deficient; depth of hunger |
|
| Identification |
Sponsorship source: The Malawi Social Cash Transfer Program Impact Evaluation was contracted to the University of North Carolina at Chapel Hill and the Center for Social Research at the University of Malawi. The baseline and first follow‐up (midline) were funded by UNICEF, the German Government through KfW, Irish Aid and FAO; the International Initiative for Impact Evaluation (3ie) and the EU provided additional funding for the second follow‐up (endline) survey. The Government of Malawi provided significant in‐kind contributions and support to all 3 rounds. Country: Malawi Setting: ultra‐poor and labour constraint HHs, Mangochi and Salima districts Comments: no trial registry number Authors' names: Kristen Brugh, Gustavo Angeles, Peter Mvula Email: knbrugh@gmail.com; gustavo_angeles@unc.edu; petermvula58@yahoo.com Declarations of interest: NR Study or programme name and acronym: Malawi Social Cash Transfer Program Type of record: journal article, study reports |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Coin tossing was conducted for each TA in each district whereby half of the VCs were allocated to the intervention or control group (baseline report p. 9; Appendix C1). |
| Allocation concealment (Selection bias) | Low risk | VCs in each of selected traditional authorities were selected (from a hat) and an ordered list of clusters was created. At 2 district meetings, the allocation of VCs to the intervention or control was conducted for each TA, according to the ordered list (baseline report page 7, 9, Appendix C1). |
| Baseline characteristics similar (Selection bias) | Low risk | HH baseline characteristics similar in both groups. |
| Baseline outcome measurements similar (Selection bias) | Low risk | HH outcome measurements (e.g. measures of food security and dietary diversity) were similar in both groups at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding of HHs or personnel was not possible; however, performance bias was unlikely as the intervention was implemented by government structures. |
| Blinding of outcome assessment (Detection bias) | High risk | Not stated whether the field teams collecting the outcome data at the end of the study were blinded. However, measurements of HH food security and dietary diversity were self‐reported. |
| Protection against contamination (Performance bias) | Low risk | The geographical location of the VCs selected for the intervention or control groups were in the same district. However, a geographical map of the study villages suggest that the majority of the intervention villages were not close to any of the control villages (see Abdoulayi 2014 Baseline report). |
| Incomplete outcome data (Attrition bias) | Low risk | Low attrition due to LTFU and missing outcome data (intervention group: 117/1678 (7%) vs control group: 124/1853 (6.7%). No evidence of differential attrition between groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. Although the cash transfer programme had several aims, the paper by Burgh reported on the outcome domains of food security and dietary diversity. The study authors described 7 outcomes in their methods (e.g. consuming > 1 meal a day, per capita caloric availability, HDDS) and they provided outcome data for all of these variables. |
| Other bias | Unclear risk | Misclassification of exposure: low risk. Measurement bias: unclear risk. Detailed description of measurements NR. Incorrect analysis: low risk. Effects adjusted for clustering. |
Brunie 2014.
| Study characteristics | ||
| Methods |
Study design: PCS Study grouping: parallel group How were missing data handled? attrition between baseline and endline was 10.1% overall. Missing data were excluded from analyses. 38 HHs declared participating in activities that did not correspond to their group – these observations were excluded from analyses. Randomisation ratio: 2:2:2:2 – VSL only; VSL + AM; AM only; control; authors mentioned factorial randomised design but it was not really randomised. Recruitment method: districts were randomised to 1 of 2 intervention groups or a control group. Intervention HHs declared interest in participating and the control group comprised sample HHs taken from the general population. Sample size justification and outcome used: sample size was calculated based on approximate estimates from past studies on food sufficiency, HDDS, IDDS and WAZ. These calculations indicated that 20 primary sampling units, comprising 14 HHs, per district was sufficient; resulting in 560(?) HHs per group. Sampling method: 2‐stage sampling approach employed. First, 8/18 districts purposefully selected, and each intervention group was allocated 2 districts. Sample of HHs that declared interest in participating in VSL/AM activities was drawn and a sample from general population was drawn for the control group. Then PSUs were selected: in intervention group, PSUs were VSL groups, and in the control group the PSUs were the EAs from the 2007 Census. Second, HHs were selected: eligible HHs within selected PSUs were enumerated and random sample drawn. HH participation was voluntary. PSUs were randomly selected with probability proportionate to size (in terms of number of HHs represented). Study aim or objective: to evaluate the impact of participation in an economic‐strengthening initiative, namely VSL groups, on HH and child nutritional outcomes, with an additional focus on identifying possible gaps and areas for complementary programming. Study period: August 2009–August 2012 Unit of allocation or exposure: provincial districts allocated to intervention groups |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: HHs expressing interest in participating in the activity their district was randomised to. Exclusion criteria: NR. Pretreatment: NR. From baseline characteristics table there seems to be differences across intervention groups regarding annual HH income, education of spouse, age of HH head and number of children aged < 5 years, but whether this was statistically significant was NR. Attrition per relevant group: no attrition per group was reported, but total attrition was 10.1% and an additional 38 (2.7%) HHs did not participate in the intervention their district was randomised to. Description of subgroups measured and reported: no subgroups were measured, but there were 3 intervention groups namely VSL alone, AM alone and VSL + AM. Only VSL alone and VSL + AM were analysed in this study. Total number completed and analysed per relevant group: 395 HHs in the VSL group, 401 in the VSL + AM group and 480 in the control group. Note: check numbers – estimated impact have higher HH numbers Total number enrolled per relevant group: VSL: 395 HHs; VSL + AM: 401 HHs; control: 480 HHs Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Food security: months of food sufficiency Dietary diversity: HDDS, IDDS Anthropometry: WAZ (underweight) |
|
| Identification |
Sponsorship source: US Agency for International Development (USAID) under the terms of associate agreement DFD‐AA‐00‐07‐00251‐00, the Supporting Transformation by Reducing Insecurity and Vulnerability with Economic Strengthening (STRIVE) project. Country: Mozambique Setting: HHs in an area with high prevalence of stunted, wasted and underweight children. Author's name: Diana Rutherford Email: drutherford@fhi360.org Declarations of interest: NR Study or programme name and acronym: village savings and loan (VSL) or a combination of VSL and AM. Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Although the paper described this as a randomised design, there was no randomisation of districts to intervention groups. Quote: "Eight of Nampula's 18 districts were purposefully selected for this study. Two districts were assigned to each intervention and control arms such that, once paired, they formed arms similar with respect to distance from the capital, economic performance, rainfalls, and market activities." CBA design, and randomisation was N/A. |
| Allocation concealment (Selection bias) | High risk | Allocation was not concealed; CBA study. |
| Baseline characteristics similar (Selection bias) | Low risk | Unclear if groups were significantly different at baseline but analyses were adjusted for these characteristics. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Unclear if baseline outcome measurements were significantly different between the intervention and control groups but analyses were adjusted for covariates. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding of participants as this was a cohort study, but it was unlikely that this influenced participant performance. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding of participants as this was a cohort study. While some outcomes were objective measurements, others were self‐reported, which could have been influenced by knowledge of treatment allocation. |
| Protection against contamination (Performance bias) | Unclear risk | No information given on how potential contamination was prevented. As groups were matched inter alia on proximity it is possible that districts may have influenced each other due to relational ties (sending of money to family in a neighbouring district) or migration. |
| Incomplete outcome data (Attrition bias) | Unclear risk | 10% overall LTFU but attrition per group was NR and it was unknown whether attrition was greater in 1 of the groups or if it was equal. Certain observations were excluded from the analyses. These missing data could have influenced the observed effect. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available, but all a priori stated outcomes in the methods section were reported on in the results section. |
| Other bias | Low risk | None identified |
Chakrabarti 2018.
| Study characteristics | ||
| Methods |
Study design: CBA Study grouping: N/A How were missing data handled? NR. Randomisation ratio: N/A Recruitment method: state governments identify families eligible for PDS support and issue ration cards to such HHs. Sample size justification and outcome used: NR Sampling method: the National Sample Survey Organization (NSSO) conducts a survey of 100,000–125,000 HHs representative of the state and national level. Study aim or objective: to examine the impact of subsidies on pulses in select Indian states on HH consumption and protein intake. Study period: 2007 (for Himachal Pradesh, Punjab and Tamil Nadu) or 2008 (Andhra Pradesh) to 2010 Unit of allocation or exposure: states |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: HHs qualifying for PDS subsidies in selected Indian states. Details of eligibility criteria NR. Exclusion criteria: NR Pretreatment: none Attrition per relevant group: total of 4872/23,558 (20.7%) fewer HHs in intervention and 18,917/101,086 (18.7%) fewer HHs in control states were included in the follow‐up survey. Description of subgroups measured and reported: poorest HHs, vegetarian HHs and HHs with different quantities of pulse consumption. Total number completed and analysed per relevant group: 18,686 HHs in intervention and 82,169 HHs in control states. Total number enrolled per relevant group: 23,558 HHs in intervention states and 101,086 HHs in control states. Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | HH expenditure on food (excluding pulses) per month Dietary diversity: amount of different types of food consumed by HH per month Dietary intake: amount of protein from pulses/all foods consumed per HH per day |
|
| Identification |
Sponsorship source: Indian Council of Agricultural Research (ICAR); Swiss Agency for Development and Cooperation. This work was also undertaken as part of the Consultative Group on International Agricultural Research (CGIAR) Research Program on Agriculture for Nutrition and Health (A4NH). Country: India Setting: rural and urban HHs in selected states (Andra Pradesh; Maharashtra) Authors' names: Suman Chakrabarti; D Roy Email: d.roy@cgiar.org Declarations of interest: NR Study or programme name and acronym: Public Distribution System (PDS) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | No randomisation. CBA. |
| Allocation concealment (Selection bias) | High risk | No randomisation. CBA. |
| Baseline characteristics similar (Selection bias) | Low risk | No formal tests of hypotheses were done, but between‐group baseline equivalence appeared to have been attained for baseline characteristics. |
| Baseline outcome measurements similar (Selection bias) | Low risk | No formal tests of hypotheses were done, but between‐group baseline equivalence appeared to have been attained for quantity of pulses, protein from pulses and protein from all foods at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | Although the participants were not blinded, the intervention (introduction of pulses) was implemented as part of a central government programme. The programme was implemented in a similar way in both intervention and control villages. |
| Blinding of outcome assessment (Detection bias) | High risk | Not described by study authors. |
| Protection against contamination (Performance bias) | Low risk | As intervention and control treatments were assigned by state government, it was unlikely that meaningful contamination could have occurred. 2 intervention states in the north (Himachal Pradesh and Punjab) and 2 in the south (Tamil Nadu and Andhra Pradesh) border each other, while Maharashtra (a control state) does not border any of the intervention states; making contamination highly unlikely. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Total attrition was fairly high (13.0%), but comparable between intervention (20.7%) and control (18.7%) groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol was available and the paper did not follow the usual journal format with a designated Methods section. The aim of the study was to assess the effect of pulse subsidy on pulse consumption and protein intake, both of which are reported on. |
| Other bias | Low risk | No other biases identified. |
Chen 2019.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? data from non‐boarding students and from boarding students who did not have Hb concentration, height and weight measurements were excluded from the analysis. Randomisation ratio: 1:1:2 (nutrition subsidy intervention:nutrition subsidy + monetary incentive intervention:control) Recruitment method: in each 1 of 30 townships, with the necessary permission from the Chinese government, schools were chosen if they offered fourth and fifth grade classes and accommodated ≥ 400 students. Once schools were selected, written assent was requested from students and their parents. Written consent was also requested from the students' legal guardians at school (schoolmasters and head teachers). Sample size justification and outcome used: NR Sampling method: 30 townships were randomly selected from 2 provincial‐level administration units, Qinghai Province and Ningxia Autonomous Region. Schools were selected from these townships and all fourth and fifth graders from these schools with assent and consent were included. Study aim or objective: how does the provision of nutrition subsidies translate into observed nutritional and health outcomes? Will policy targets with different levels of specificity, e.g. general ones such as malnutrition prevention and specific ones such as anaemia reduction, lead to different behavioural responses and, thus, nutritional and health outcomes, partly through different incentives attached to these policy targets (since certain incentives are presumably needed to achieve any specific policy target)? Study period: October 2009–May 2010 Unit of allocation or exposure: cluster: elementary schools |
|
| Participants |
Baseline characteristics Nutrition subsidy
Nutrition subsidy + monetary incentive
Control
Overall: NR Inclusion criteria: townships: located in Qinghai Province or Ningxia Autonomous Region. Schools: offering fourth and fifth grade classes; accommodating ≥ 400 students. Children: fourth or fifth grade students; written assent provided; consent from guardians provided; boarding (to be included in analysis). Exclusion criteria: NR Pretreatment: baseline characteristics and outcome variables presented in Table A1 and 2. Table A1: most variables were quite balanced across groups, with minor differences due to sampling errors, suggesting that the random group assignments were done reasonably well. However, due to the modest number (i.e. 59) of project schools, some student or school characteristics may have been balanced across the 3 groups (Appendix A Table A1), even under randomised group assignments. To address this issue, the authors modified the estimating equation. Quote: "Unless otherwise stated, all estimates presented below are obtained after controlling for the full set of covariates reported in Appendix A Table A1." Attrition per relevant group: 61% of boarding students (who were considered in the analysis) were not analysed because they did not have health information collected due to budgetary reasons. Considering the full sample of 6994, attrition was 88%. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: to fully capture the impacts of the treatments, the authors' analysis focused only on the 2199 boarding students in the sample (of 6994 students). Due to budgetary reasons, while dietary information was collected from all (boarding) students, health information was collected only from about half of them: 1020 boarding students had information on Hb concentration level, 952 had height and weight information, and 866 had both sets of information. Thus, the final analytical sample comprised 866 boarding students with information available on all 3 dimensions. Students: 219/582 (38%) for nutrition subsidy; 210/563 (36%) for nutrition subsidy + monetary incentive; 437/1550 (28%) for control group. Total number enrolled per relevant group: total sample 6994. Not clear per group, as only reported on those with Hb and height/weight information. Total number randomised per relevant group: total of 15 schools for nutrition subsidy, 15 for nutrition subsidy + monetary incentive and 29 for control group. |
|
| Interventions |
Intervention characteristics Nutrition subsidy (treatment group 1)
Nutrition subsidy + monetary incentive (treatment group 2)
Control: no intervention |
|
| Outcomes | DDS (0–10) Anthropometry: BMZ; proportion underweight (BMZ < –2SD) Biochemical: Hb concentration Morbidity: proportion anaemic |
|
| Identification |
Sponsorship source: National Natural Science Foundation of China [grant number 71603261]; Humanities and Social Science Fund of the Ministry of Education of China [grant numbers 16YJC880107, 18YJC790010]; The Fundamental Research Funds for the Central Universities [grant number 2019TC110]. Country: China Setting: fourth and fifth graders enrolled in elementary schools in rural Qinghai and Ningxia Authors' names: Qihui Chen; corresponding: Qiran Zhao Email: zhaoqiran@cau.edu.cn Declarations of interest: yes; no conflicts of interest. Study or programme name and acronym: NR Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | No information provided how the random sequence generation is done. Only (quote): "schools were randomly assigned into three groups." |
| Allocation concealment (Selection bias) | Low risk | Unit of allocation was by school; all assignments were done at start of study. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Low for the analysed group, but no data available for the entire group. Quote: "Due to both randomisation plus taking this into account during the analysis. Baseline characteristics and outcome variables presented in Table A1 and 2. Table A1: Most of these variables are quite balanced across groups, with minor differences due to sampling errors, suggesting that the random group assignments were done reasonably well." "However, due to the modest number (i.e., 59) of project schools, some student or school characteristics may not be perfectly balanced across the three groups (Appendix A Table A1), even under randomized group assignments. To address this issue, we modify the estimating equation (1) in two ways." "Unless otherwise stated, all estimates presented below are obtained after controlling for the full set of covariates reported in Appendix A Table A1." |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Low for the analysed group, but no data available for the entire group. Quote: "Due to both randomisation plus taking this into account during the analysis. Baseline characteristics and outcome variables presented in Table A1 and 2. Table A1: Most of these variables are quite balanced across groups, with minor differences due to sampling errors, suggesting that the random group assignments were done reasonably well." "However, due to the modest number (i.e., 59) of project schools, some student or school characteristics may not be perfectly balanced across the three groups (Appendix A Table A1), even under randomized group assignments. To address this issue, we modify the estimating equation (1) in two ways." "Unless otherwise stated, all estimates presented below are obtained after controlling for the full set of covariates reported in Appendix A Table A1." |
| Blinding of participants and personnel (Performance bias) | High risk | Not explicitly reported whether students and school staff were blinded to assignment. Given the integral role of the schoolmaster in administering the intervention and their access to information on anaemia; however, it is not possible that these people could be blinded. The lack of blinding may have resulted in considerable performance bias, specifically in the group of schoolmasters not receiving incentives. |
| Blinding of outcome assessment (Detection bias) | High risk | NR whether the medical professionals who assessed some outcomes were blinded. Most outcomes were objective and not prone to detection bias, but outcomes such as dietary diversity may have been affected by unblinded self‐report from participants. |
| Protection against contamination (Performance bias) | Low risk | Since payment was made into the school account and information was provided to the headmasters, contamination at school level was not expected. Furthermore, only boarders were analysed: boarding arrangement ensures that almost all the food consumed by boarding students came from the intervention. |
| Incomplete outcome data (Attrition bias) | High risk | Very high levels of attrition among students: 363/582 (62%) for nutrition subsidy; 353/563 (64%) for nutrition subsidy + monetary incentive; 1113/1550 (72%) for control group. This is predominantly due to only including boarding students with Hb and anthropometric data, as well as the loss of 1 control cluster. Attrition appears to be differential for the control group versus the intervention groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No study protocol available. |
| Other bias | Unclear risk | Recruitment bias: randomisation of schools occurred after students had been recruited; low risk. Incorrect analysis: adjustment for clustering NR, but robust SEs used; unclear risk. |
Daidone 2014.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? investigated attrition at 24‐month follow‐up by testing for similarities at baseline between 1. treatment and control groups for all non‐missing HHs (differential attrition) and 2. all HHs at baseline and the remaining HHs at the 24‐month follow‐up (overall attrition). Testing these groups on baseline characteristics can assess whether the benefits of randomisation are preserved at follow‐up. There was no significant differential attrition at 24‐month follow‐up, meaning that benefits of randomisation were preserved. There were small differences between study population at baseline and those that remained at 24‐month follow‐up; the remaining HHs were less likely to have experienced a shock, especially flooding or drought at baseline, and they consumed a higher proportion of maize over cassava. The differences from overall attrition were primarily driven by the lower response rate in Kaputa district. Randomisation ratio: about 1:1 Recruitment method: 90/300 CWACs in the 3 districts were randomly selected and ranked through a lottery to be considered in the programme. In second phase, CWAC members and Ministry staff identified all eligible HHs with ≥ 1 child under the age of 3 years living in these 90 randomly selected communities. This resulted in > 100 eligible HHs in each of the CWACs. Sample size justification and outcome used: power analysis completed to ensure study size was able to detect meaningful effects. Sampling method: randomised phase‐in method that included several levels of random selection. First, 90/300 CWACs in the 3 districts were randomly selected and ranked through a lottery to be considered in the programme. In second phase, CWAC members and Ministry staff identified all eligible HHs with ≥ 1 child under the age of 3 years living in these 90 randomly selected communities. This resulted in > 100 eligible HHs in each of the CWACs. After implementing a power analysis to ensure the study was able to detect meaningful effects, 28 HHs were randomly selected for inclusion in the evaluation from each of the 90 communities. This yielded a final study sample of > 2500 HHs. Baseline data collection carried out before CWACs were randomly assigned to treatment and control. Importantly, neither the HHs nor the enumerators knew who would benefit first and who would benefit later. Randomisation was concluded with the flip of a coin and was carried out in public with local officials, Ministry staff and community members. Study aim or objective: CGP has 6 specific objectives: 1. supplement and not replace HH income; 2. increase the number of children enrolled in and attending school; 3. reduce the rate of mortality and morbidity among children aged < 5 years; 4. reduce stunting and wasting among children aged < 5 years; 5. increase the number of HHs owning assets such as livestock and 6. increase the number of HHs that have a second meal a day. Study period: 3‐year RCT; began in December 2010 and ended in 2013. Evaluation occurred at 24‐month follow‐up. Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: any HHs with a child aged < 5 years in 3 districts (Kalabo, Kaputa and Shangombo) that had not participated in a previous cash transfer programme. Exclusion criteria: NR Pretreatment: treatment HHs were slightly larger than the control group. HHs in Kaputa were bigger compared to the other 2 districts. Attrition per relevant group: NR. Overall attrition rate 8.8% (Diadone 2014) and 9% (Seidenfeld 2013). Attrition rate for treatment 8.1%; attrition rate for control 0.9% (Seidenfeld 2013). Description of subgroups measured and reported: subgroup analyses by districts (Kalabo, Kaputa and Shangombo). Total number completed and analysed per relevant group: total 2519 HHs. Calculated based on response rate; intervention 1158 (91.9%); control 1141 (90.6%) Total number enrolled per relevant group: treatment 1260 HHs (7254 individuals); control 1259 HHs (7091 individuals); total 2519 HHs (14,345 individuals) Total number randomised per relevant group: NR |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food: HH monthly expenditure on food and expenditure on individual food groups Food security: proportion people eating > 1 meal/day; proportion not severely food insecure; proportion who ate meat/fish ≥ 5 times in last month HHFIAS Dietary diversity: HDDS (0–12) Anthropometry: WAZ; HAZ; WHZ Cognitive function and development: ECD Index Morbidity: proportion of children aged 0–60 months with ARI; proportion of children aged 0–60 months with diarrhoea |
|
| Identification |
Sponsorship source: From Protection to Production (PtoP) programme, jointly with the UNICEF, is exploring the linkages and strengthening co‐ordination between social protection, agriculture and rural development. The PtoP is funded principally by the UK DfID, the FAO of the UN and the EU. The programme is also part of the Transfer Project, a larger effort together with UNICEF, Save the Children and the University of North Carolina, to support the implementation of impact evaluations of cash transfer programmes in sub‐Saharan Africa. Country: Zambia Setting: communities in the 3 poorest districts of Zambia: Shangombo, Kalabo and Kaputa Comments: both Daidone 2014 and Seidenfeld 2013 used for data extraction. Seidenfeld 2013 was the official programme impact report and more useful in the population and intervention extraction, while Diandone was more useful in the methods extraction. Author's names: Silvio Daidone, David Seidenfeld, Sudhanshu Handa, Benjamin Davis Email: dseidenfeld@air.org; shanda@email.unc.edu; benjamin.davis@fao.org Declarations of interest: NR Study or programme name and acronym: Zambian Child Grant Programme (CGP) Type of record: research report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | The CGP impact evaluation was designed as an RCT using a randomised phase‐in method (Duflo et al 2008) that included several levels of random selection. First, 90/300 CWACs in the 3 districts were randomly selected and ranked through a lottery to be considered in the programme. In second phase CWAC members and Ministry staff identified all eligible HHs with ≥ 1 child aged < 3 years living in these 90 randomly selected communities. |
| Allocation concealment (Selection bias) | Low risk | Allocation at CWAC level at start of study. Importantly, neither HHs nor enumerators knew who would benefit first and who would benefit later. |
| Baseline characteristics similar (Selection bias) | Low risk | Randomisation was successful, as mean characteristics were balanced across groups (Table 2). |
| Baseline outcome measurements similar (Selection bias) | Low risk | At baseline, majority of indicators were not statistically different at the conventional 5% significance level, with 10 exceptions out of 71 (Table 2). 4 indicators had standardised differences > 10, but they were all < 15. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding not done but unlikely to influence behaviour of personnel and participants. |
| Blinding of outcome assessment (Detection bias) | High risk | Neither HHs nor enumerators knew who would benefit first by receiving the case grant (treatment) and who would benefit later by receiving the case grant after the RCT (control) at baseline. However, blinding was not possible. Some outcomes were subjective and could have been influenced by knowledge of intervention allocation. |
| Protection against contamination (Performance bias) | Unclear risk | Possible that increases in treatment HHs agricultural productivity could have had a spillover effect on controls as they resided in the same community. |
| Incomplete outcome data (Attrition bias) | Low risk | Seidenfeld et al (2013) investigated in detail both differential and overall attrition. Differential attrition relates to baseline characteristics between treatment and control HHs that remain at follow‐up. Overall attrition looked at similarities at baseline between the full sample of HHs and the non‐attriters. They found no significant differential attrition after 24 months, meaning that the benefits of randomisation were preserved. The differences in overall attrition were primarily driven by the lower response rate in Kaputa district. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Authors did not refer to a protocol. |
| Other bias | Low risk | None identified. |
Darrouzet Nardi 2016.
| Study characteristics | ||
| Methods |
Study design: cRCT How were missing data handled? NR Randomisation ratio: 1:1 Recruitment method: HHs were identified via 'Village Development Committees,' and all were invited to participate. A parent from each HH provided informed consent. Sample size justification and outcome used: original trial sample size was calculated to detect a difference of > 0.25 in mean WAZ with a power of 87% and a 2‐sided significance level of 0.05. Sampling method: 3 pairs of comparable communities in each district were identified, based on geographic location (including altitude), size, local natural resources, employment opportunities, availability of health care, type of agriculture practiced and other demographic features. Paired communities were randomly assigned to receive Heifer development activities either first (intervention communities) or second (control communities). Study aim or objective: to evaluate the effect of a holistic community‐level nutrition‐sensitive intervention on child dietary diversity and animal source food consumption in rural Nepal. Study period: NR Unit of allocation or exposure: communities |
|
| Participants |
Baseline characteristics Intervention or exposure group:
Control
Overall
Inclusion criteria: all members of each participating HH. Exclusion criteria: children with physical or neurological disabilities that prevented ingestion of a normal diet for age or children with severe intercurrent illnesses at time of survey Pretreatment: animal ownership was greater in control HHs (2.42 (SD 0.13) than in intervention HHs (1.71 (SD 0.12) at baseline (P = 0.0001). Attrition per relevant group: unclear, as the participatory HHs increased over duration of study. Description of subgroups measured and reported: gender; age (6–12 months; > 12 months); season (hungry vs harvest); region for dietary quality outcomes. Total number completed and analysed per relevant group: for growth outcomes at 24 months: intervention group: 305 children aged 6–60 months; control group: 306 children aged 6–60 months. Number of HHs unclear. For dietary outcomes at 24 months: 533 children in total (unclear how many per group). Number of HHs unclear. Total number enrolled per relevant group: intervention group: 201 HHs (including 283 children aged 6–60 months); control group: 214 HHs (including 324 children aged 6–60 months) Total number randomised per relevant group: intervention group: 3 study sites; control group: 3 study sites |
|
| Interventions |
Intervention characteristics Intervention or exposure group: multicomponent agriculture training
Control group: no intervention |
|
| Outcomes | Dietary diversity: HH DDI, child MDD Dietary intake: % children consuming specific foods – oil, dal, milk, meat, eggs, vitamin A rich foods, other Anthropometry: HAZ, WAZ |
|
| Identification |
Sponsorship source: Heifer International Country: Nepal Setting: HHs of communities mainly populated by low‐income subsistence farmers. 2 regions involved: Hills region is conducive to livestock production; Terai region is conducive to crop production. Authors' names: Amelia F Darrouzet‐Nardi; Laurie C Miller Email: adarrouzetnardi@allegheny.edu; lmiller1@tuftsmedicalcenter.org Declarations of interest: yes; no conflicts of interest. Study or programme name and acronym: Heifer International Intervention Type of record: journal articles |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Method of randomisation NR. |
| Allocation concealment (Selection bias) | Unclear risk | NR. |
| Baseline characteristics similar (Selection bias) | Low risk | The mean HH size was larger in 1 control community compared to the intervention community. Animal ownership was greater in 1 control community. The study authors controlled for baseline HH characteristics in their analysis. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Study authors reported no differences in growth parameters or morbidity of children aged 6–60 months between the intervention and control groups at baseline (Miller 2014). DDSs, e.g. DDS, MDD at baseline between the intervention and control groups were NR (Darrouzet‐Nardi 2016). |
| Blinding of participants and personnel (Performance bias) | Low risk | Although blinding was not possible, it was likely that a lack of blinding influenced the children's nutritional outcomes. |
| Blinding of outcome assessment (Detection bias) | High risk | The enumerators who collected baseline data were blinded to the allocation of the intervention but not those collecting data during the subsequent 12 months. Outcomes were based on self‐report, which could have been influenced by participant's knowledge of treatment allocation. |
| Protection against contamination (Performance bias) | Low risk | The intervention and control communities were not adjacent to each other to minimise spillover effects. |
| Incomplete outcome data (Attrition bias) | Unclear risk | NR how many HHs and participants dropped out per group; and it seems that HHs were added after randomisation and initial enrolment. It is also unclear how missing data were handled. No clusters were lost. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: low risk. Single 24‐hour dietary recall at baseline and repeated during follow‐up. Bias between intervention clusters due to level of participation in intervention. Quote: "Villages were randomly assigned to either Group 1 or Group 2, but within villages, HHs could choose their level of participation in the intervention, creating the potential for selection bias." Incorrect analysis: high risk. Study authors did not adjust for clustering in their analysis. Recruitment bias: unclear. Unclear whether HHs were recruited before or after randomisation. |
Doocy 2017.
| Study characteristics | ||
| Methods |
Study design: PCS Study grouping: N/A How were missing data handled? With exception of imputation procedures for child anthropometric data, analysis did not consider interim measures of each indicator because after exploratory analysis, it became clear that inclusion of interim data points did not change results and conclusions, and thus eliminating analysis of interim measures would facilitate the interpretation of findings. Used a multiple imputation approach for anthropometric outcomes, where missing values were replaced by values sampled from a distribution defined by the fit of a linear regression model at a given follow‐up as a function of previous outcomes, as well as of child age and sex. Missing values for maternal age was assigned the mean and education the mode of those variables, so they could be included in the analysis. Randomisation ratio: N/A Recruitment method: at enrolment, a full description of study was read to prospective participants and they had the opportunity to ask questions about participation; those who agreed to participate gave oral consent due to high levels of illiteracy. At each subsequent survey, the respondent was read an abbreviated consent statement and asked to re‐affirm their willingness to participate prior to the interview (Doocy 2018). Study enrolment occurred between August and October 2012 following identification of beneficiaries for each intervention. 1820 beneficiaries and their HHs were enrolled and followed over 3.5 years during February/March 2016; study HHs were followed for the entire period, regardless of whether they graduated or dropped out of intervention. Sample size justification and outcome used: primary outcome measure was reduction in HH food insecurity, and authors conducted calculations for varying levels of reduction, assuming 80% power and a significance level of 0.05. With a minimum sample size of 325 HHs per group (or 1625 HHs in total for the parent study), study was powered to detect a 10% or greater reduction in prevalence of food insecurity indicators within each comparison group compared to baseline levels. Sampling method: The Jenga Jamaa II parent study used a quasi‐experimental matched design in which communities planned to receive 1 intervention (vs multiple interventions) selected for participation so that the effect of individual interventions could be assessed. Authors analysed 2 of the 5 comparison groups recruited for the parent study of Jenga Jamaa II: the FFS intervention group (388 participants) and the control group (324 participants). Participating communities within each territory (Fizi and Uvira) were matched by livelihood zone (mountains, plains or lakeside) and proximity into sets of villages with each type of intervention. The final sample had 13 sets of 3 villages; within each set of villages, 1 village received agricultural interventions, 1 received PM2A, and 1 received WEGs. In each set of villages, intervention groups were formed (i.e. 1 intervention per village) and all beneficiaries in the group were enrolled in the study. In agricultural intervention villages, the entire FFS group of approximately 30 beneficiaries was enrolled in the study. Controls were selected from WEG villages, where each beneficiary was matched with a female neighbour not participating in Jenga Jamaa II interventions, and that woman's HH was enrolled as a control. Villages were assigned to an intervention based on agreement with local leaders and availability programme resources; intervention participants were identified based on programme targeting criteria and community selection processes. Once intervention groups were formed, all group members were invited to participate in the research. In agriculture villages, 1 FFS with approximately 30 participants was enrolled; 1 of 3 farmer‐to‐farmer trainees of each FFS participant was randomly selected to comprise the F2F group. In WEG villages, 1 WEG group of 25 participants was selected. Members of the control group were also selected from WEG villages because the WEG intervention had lower coverage than FFS/farmer‐to‐farmer and PM2A interventions (i.e. there was only 1 WEG group per village compared to multiple PM2A and agricultural intervention groups), which lessened the likelihood of spillover effects on control HHs. Study aim or objective: to examine the changes in agricultural production practices, HH food security and child nutritional status that are associated with participation in FFS programmes. Study derived from a subset of data from the parent study of Jenga Jamaa II which sought to address HH food insecurity and child undernutrition through 1. increasing incomes among farming HHs through FFS and farmer‐to‐farmer training interventions, 2. improving the health and nutritional status of children aged < 5 years through the PM2A, and 3. empowering women via WEGs. Study period: HHs were followed for 3.5 years, from enrolment in autumn of 2012 (baseline) to February or March 2016 (endline). Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics FFSs
Control
WEGs
Overall (all intervention groups; including those irrelevant to the review)
Inclusion criteria: intervention participants identified based on programme targeting criteria and community selection processes. For the control group, enrolled primary carer of children, and 100% were women. No other details. Exclusion criteria: NR Pretreatment: more women in control group (as control group selected was women only – from the village where women empowerment intervention was implemented, whereas the interventions included all FFS beneficiaries (men and women). Intervention group participants were significantly older; control group participants had higher proportion completing any formal education control; group had higher mean number of younger children (aged 0–4 years); higher proportion of farmers in intervention group; mean HH size differed significantly between the groups; smaller for FFS groups and larger for WEG groups; number of income sources (highest in FFS group and lowest in control group). Attrition per relevant group: results included only 82% of participants who were present for both baseline and endline surveys (both conducted in February/March). Village of Kibirizi, which included 1 FFS group, was not included in endline survey (and thus was excluded from the final evaluation) due to security concerns. 1820 HHs were enrolled in study and 1481 (81%) participated in the endline survey; follow‐up ranged from 74% to 90% in different intervention groups and was lowest among the control group: FFS baseline 390; endline participation rate 81%; WEG baseline 325; endline participation rate 90%; control baseline 325; endline participation rate 78%. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: for food security outcomes: intervention group: 317 FFS beneficiaries; control group: 254 non‐FFS participants. For child anthropometric outcomes: intervention group: 265 children of FFS beneficiaries; control group: 206 children of non‐FFS participants. Total number enrolled per relevant group: FFS programme: study enrolled 388 FFS beneficiaries and their HHs in the intervention group and 324 non‐FFS adults and their HHs in the control group. WEG group: 390 HHs. Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics FFSs
Control
WEGs
|
|
| Outcomes | Food security: HFIAS; proportion of HHs improving in a HFIAS category from baseline to endline; proportion of HHs food secure and mildly/moderately/severely food insecure Dietary diversity: HDDS; HHs achieving target dietary diversity Anthropometry: stunting, underweight |
|
| Identification |
Sponsorship source: USAID Office of Food for Peace Cooperative Agreement (AID‐FFP‐A‐11‐00006). Country: Democratic Republic of the Congo Setting: 2 farming villages in South Kivu province in the Congo Author's name: Shannon Doocy Email: doocy1@jhu.edu Declarations of interest: none declared. Study or programme name and acronym: Farmer Field Schools programme, subset of interventions implemented as part of the Jenga Jamaa II project Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | PCS |
| Allocation concealment (Selection bias) | High risk | PCS; therefore, no allocation concealment carried out. |
| Baseline characteristics similar (Selection bias) | Low risk | Some imbalances in gender, age, number of younger children, proportion who were farmers between the intervention and control groups. These characteristics were adjusted for in the analysis and authors also carried out PSM. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Study authors reported differences in food security outcomes at baseline, although the statistical analysis of these outcome variables was not provided. Analyses regarding food security outcomes was adjusted for baseline HDDS values. However, for child anthropometric outcomes, there were no baseline values reported, thus it is unclear whether there were imbalances or not. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding of participants and personnel was done. However, in this type of intervention, it is unlikely that lack of blinding would have affected experience or treatment of participants. |
| Blinding of outcome assessment (Detection bias) | High risk | Although blinding was not possible, interviews were carried out by staff that did not regularly interact with the participants. However, outcomes such as dietary diversity and food insecurity, that are based on respondents recall, may be susceptible to lack of blinding. |
| Protection against contamination (Performance bias) | High risk | Control HHs were sampled from villages that received 1 of the intervention types (WEG), thus the risk for contamination was high. Authors also reported that, "It is also possible that spillover from the intervention areas affected the control areas." |
| Incomplete outcome data (Attrition bias) | High risk | Differential attrition observed between groups: 10% for WEGs, 19% for FFS and 22% for control group. Reasons for missing/excluded data not provided. 1 entire village (Kibirizi) was excluded from the analyses (due to conflicts in the country). For child anthropometric data, missing values were inputted using a multiple imputation approach, where missing values were replaced by values sampled from a distribution defined by the fit of a linear regression model at a given follow‐up as a function of previous outcomes, as well as of child age and sex. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A; however, the primary outcome, namely HH food security (as prespecified in the Methods section of the citation by Doocy 2017), was reported in the text. |
| Other bias | Low risk | Misclassification bias of exposure: low risk. Measurement bias: low risk; scales used were validated and widely used, as was anthropometric measurement; and staff were trained in data collection. Seasonality: low risk; study collected data over different seasons over 3.5 years. Random sequence generation (selection bias). |
Evans 2014.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? Authors carried out both ETT and ITT regressions. However, in ETT analyses, treated HHs were those assigned to the intervention and actually received the intervention, whereas in an ITT analysis 'treated' HHs were those that were assigned to intervention, regardless of whether they actually received it. It appears as data not collected was excluded from the analysis. Randomisation ratio: 1:1; 40 intervention and 40 control communities Recruitment method: HHs were invited to enrol in the pilot. Enrolment of beneficiaries carried out in each community, with the enrolment process lasting 1–3 days, depending on total number of beneficiary HHs in the community. The enrolment team identified who would receive payments in each HH (usually the mother of the children in the HH if present), updated family information, linked children and the elderly with schools and health centres, provided an orientation session about the programme, and provided identity cards. Sample size justification and outcome used: once all communities were assigned into groups, power calculations identified the need to interview a mean of 25 HHs per community. With a total of 80 participating communities (40 treatment and 40 control) and a standardised effect size of 0.20, it was expected to need to interview 20 HHs per community to achieve 80% power. 25 HHs per community were then interviewed since not every HH would have vulnerable children: some few HHs would only have vulnerable elderly people. Calculation assumed 95% CIs for statistical significance and an intracluster correlation of 0.05. Sampling method: pilot study implemented in districts and communities targeted under TASAF I, which targeted the poorest and most vulnerable districts of Tanzania using a rigorous selection process. Regions were ranked using several indicators (poverty level, food insecurity, primary school gross enrolment ratio, access to safe water, access to health facilities, AIDS case rates and road accessibility). Districts were then prioritised within the regions using an index of relative poverty and deprivation constructed using data from Tanzania's 1992 Income and Expenditure Survey. Targeting done using screening forms designed to identify vulnerable children and elderly people based on specific criteria, which were defined by the communities themselves. The CMCs used these poverty indicators to identify the poorest (approximately) half of HHs in the community. Validation of the list of eligible HHs was done by the village assembly, allowing for community validation. They ranked HHs by priority. Random selection of control and treatment communities was done after identification of vulnerable HHs in all 80 communities. Study aim or objective: pilot project aiming to develop operational modalities for the community‐driven delivery of a CCT programme through a social fund operation; and test the effectiveness of the community‐based CCT model and ensure that lessons from the pilot informed government policy on support for vulnerable families. Study period: 31–34 months: January 2010 (when first payments were made) to October 2012 (endline survey). Unit of allocation or exposure: communities (with random selection of HHs within communities allocated to each intervention group) |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: HHs with vulnerable children (1 parent or both parents deceased; abandoned children; having 1 or 2 chronically ill parents (e.g. HIV/AIDS); chronically ill children, despite having 2 parents alive. Vulnerable elderly people defined as: elderly with no carers, poor health, very poor. Communities in the selected 3 districts. Exclusion criteria: none specifically reported. Pretreatment: HHs in treatment communities were less likely to have houses with improved floors or electricity. Control communities had slightly more elderly people, HHs electricity and improved roofs, floors and toilets, children ever in school, children with own textbooks, than treatment communities. Treatment communities had slightly more acres farmed, children than missed school in the previous week and participants that could trust other people on the community, than control communities. Attrition per relevant group: total attrition: 13% at endline. Per group attrition NR. Description of subgroups measured and reported: women vs men (or girls vs boys). Poorest half vs the less poor half of HHs (on an asset index constructed using principal components analysis). HHs in Kibaha vs Bagamoyo vs Chamwino districts. Age groups: all ages, age 0–1 year; 0–2 years; 0–4 years; 0–18 years; 7–14 years; 15–18 years; ≥ 60 years. Total number completed and analysed per relevant group: 13% (n = 325) of the 2500 recruited HHs were LTFU at endline; therefore, 2175 were analysed. Numbers per group NT. Total number enrolled per relevant group: 1764 HHs and 6918 individual beneficiaries in total at baseline. Numbers per group NR. Total number randomised per relevant group: 40 villages in treatment group and 40 villages in control group. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Value of flour/rice purchased Anthropometry: weight; height; MUAC; HAZ; WAZ; WHZ; BMIZ Morbidity: proportion reported being ill in the past 4 weeks; number of days too ill for normal activities in the past 4 weeks |
|
| Identification |
Sponsorship source: Japan Social Development Fund (JSDF); Trust Fund for Environmentally and Socially Sustainable Development (TFESSD); Spanish Impact Evaluation Fund (SIEF), International Initiative for Impact Evaluation (3ie), and the Consultative Group on International Agricultural Research (CGIAR) Research Program on PIM. Country: Tanzania Setting: communities in 3 poorest and most vulnerable districts (Bagamoyo, Chamwino and Kibaha) Author's name: David K Evans Email: devans2@worldbank.org; pubrights@worldbank.org Declarations of interest: NR Study or programme name and acronym: Community‐Based Conditional Cash Transfers in Tanzania Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Authors mentioned that villages were randomly selected for intervention and control groups but did not describe any method of random sequence generation. |
| Allocation concealment (Selection bias) | High risk | No allocation concealment and HH selection was done after villages had been allocated to each intervention group. Unclear how this was done and whether knowledge of the group to which the village had been allocated influenced the process. |
| Baseline characteristics similar (Selection bias) | Low risk | Baseline differences between groups were reported and adjusted for in the difference‐in‐difference analysis. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | NR |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding but this was unlikely to affect participant and personnel behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding and some outcomes were self‐reported or subjective outcomes that could have been influenced by knowledge of treatment allocation. |
| Protection against contamination (Performance bias) | Low risk | Allocation to intervention group by village so there was no risk of contamination. |
| Incomplete outcome data (Attrition bias) | Low risk | Comment: overall, there were no data for 13% of HHs at baseline. Samples varied for different outcomes reported and it seemed that data were excluded from analysis. However, authors indicated that (quote) "Overall, these balanced rates of attrition across treatment and comparison suggest that the impact evaluation results are unlikely to be affected by attrition." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available for this study/report. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unclear. Validated tool NR for measuring food consumption and it was only measured 3 times in an almost 3‐year period, which may be insufficient. Incorrect analysis: high. Authors adjusted for intracluster correlation. |
Fenn 2015.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: N/A How were missing data handled? WHZ data coded as missing if WHZ > +5 or WHZ < –5; HAZ data coded as missing if HAZ > +5 or HAZ < –6. A child's data were excluded from the analysis if the child was deemed to be a different child to the child enrolled at baseline. While checks were in place to ensure that the same child was measured every month, in some cases these were not followed. Used criteria for exclusion a decrease in height or length > 1 cm (measurement error) or an increase > 15 cm (considered the maximum height a child could grow in 6 months). All effect analyses were ITT. Randomisation ratio: 1:1:1:1 Recruitment method: Action Against Hunger provided the initial HH lists, and these were further verified and updated by the study research team. HHs defined as poor and very poor were selected. Field officers then visited identified HHs to share details of study and get informed consent before collecting baseline data. Study participants were enrolled by data collection team and were unaware which intervention they would be getting at enrolment. However, blinding of participants was not possible due to nature of intervention. Data collection team was different to cash and voucher disbursement team. Data collection team was responsible for collection of data and sensitisation of the study recipients to use of cash and vouchers. Data collection team was accompanied by local research mobilisers who facilitated the data collectors (e.g. in locating HHs), and were responsible for delivering key BCC messages. Sample size justification and outcome used: target sample size (about 632 HHs per group) was calculated to measure a detectable difference of prevalence of being wasted of 7% between the intervention and the control groups postintervention. Sample size was powered to detect a 0.19 WHZ difference between the intervention and the control groups. Sample size was reached for the standard cash transfer, food voucher and control groups. However, for the double cash transfer group, the sample size was 600 due to the different funding amounts given for this group, which did not allow for an equivalent number of HHs to be included compared to the other 3 groups. Target sample size was calculated using an estimated ICC of 0.02 for prevalence of being wasted from an Action Against Hunger nutrition survey in Dadu District. ICC for prevalence of being wasted was 0.01 (Fenn 2017). Sampling method: it was not possible to carry out a public randomisation, therefore, randomisation was done by the principal investigator using a random number table to generate the randomisation sequence and then drawing village names from a box. Block randomisation was done, allowing equal distribution of the villages to each group for small (< 40 HHs), medium (40 (SD 85) HHs) and large (> 85 HHs) villages. The investigator had no knowledge of the villages involved and was not involved in the intervention implementation or any data collection. HHs were selected from villages from 3 agricultural areas sharing similar livelihoods, geography and access to the same elements of the standard WINS programme. Action Against Hunger provided the initial HH lists, and these were further verified and updated by the study research team. HHs defined as poor or very poor using eligibility criteria decided by research team with village participation, and based on ownership of cultivated land and number of goats and with ≥ 1 children aged 6±48 months were selected. The study was a closed cohort and followed all children in the same eligible HHs regardless of their baseline anthropometric status. Study aim or objective: to evaluate 3 cash‐based transfer modalities on nutritional outcomes in children aged < 5 years from poor and very poor HHs in Dadu District, Sindh Province, Pakistan. Aimed to 1. compare the nutrition status of children receiving either a seasonal UCTs or a fresh food voucher with those with access to Action Against Hunger care only, after 6 months and 1 year; 2. assess the costs and cost‐effectiveness of the different interventions; 3. understand the factors that determined the ways in which HHs used the different transfers and 4. explore the role of the different processes involved in the study outcomes and how they interact with the context (Fenn 2015). Study period: data for the main impact analysis and findings reported here involved 3 periods: baseline (May–July 2015), 6 months after baseline (December 2015), and 1 year after baseline (June/July 2016). Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics Standard cash transfer
Double cash transfer
Food voucher
Control
Overall: NR Inclusion criteria: HHs selected from villages from 3 agricultural areas sharing similar livelihoods, geography and access to the same elements of the standard WINS programme. HHs defined as poor or very poor using eligibility criteria decided upon by the research team with village participation, and based on ownership of cultivated land and number of goats and with ≥ 1 children aged 6 (SD 48) months were selected. Exclusion criteria: NR Pretreatment: baseline characteristics of clusters and participants between the different intervention and control groups were well balanced for mothers and their children, apart from the proportion of children who had received deworming treatment, which was lower in the control group. There were a few potential imbalances at the HH level and between villages due to the clustered nature of the study design. These included village size, ethnicity, access to safe water and distance to nearest health service. In the control group, there was a higher proportion of HHs of Balochi ethnicity. There also appeared to be differences in the SES and educational status of mothers and fathers (both lower) and a higher number of HHs participating in the BISP in control group (Fenn 2017). Attrition per relevant group: no evaluation clusters LTFU; response rates for HHs were 95.6% and children were 98.3% within clusters at 6 months and for HHs were 95.0% and children were 96.8% at 1 year. 109 (1.6%) children missing (WHZ outliers, excluded children, missing data at either time point): control 31, double cash 32, food voucher 24 standard cash 22. From Figure 1: excluded/missing HH data: control 3.9%; double cash 5.3%; food voucher 4.7%; standard cash: 5.9%; children missing/excluded: control 4.3%; double cash 5.1%; food voucher 5.5%; standard cash 6.2%; mothers BMI outcomes: 1307 (26.9%) mothers with missing data: control 308; double cash 315; food voucher 334; single cash 350. For MUAC, Hb and anaemia, missing data were ≤ 5%. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: at 12 months: control: HH and carer 607; children 815; double cash: HH and carer 568; children 796; food voucher: HH and carer 602; children 818; standard cash: HH and carer 595; children 849. At 6 months: control: HH and carer 601; children 809; double cash: HH and carer 573; children 809; food voucher: HH and carer 603; children 834; standard cash: HH and carer 607; children 874. Total number enrolled per relevant group: cluster allocations: total 114 eligible clusters randomised to: control 28; double cash 24; standard cash 31; food voucher 31. HH allocations: HHs assessed for eligibility 5128. Total HHs eligible to participate 2494. Baseline allocation 2494. HHs to the study groups: control 632; double cash 600; standard cash 632; food voucher 632. Total HH number receiving intervention (after dropped out due to relocation at baseline): control: HH 621; children 852; double cash: HHs 596; children 839; standard cash: HHs 623; children 905; food vouchers: HHs 629; children 866. Total number randomised per relevant group: 114 clusters (villages) randomised to: control 28; double cash 24; food voucher 31; standard cash 31. HH allocations 2494: control 632; double cash 600; food voucher 632; standard cash 632. |
|
| Interventions |
Intervention characteristics Standard cash transfer
Double cash transfer
Food voucher
Control
|
|
| Outcomes | Anthropometry: WHZ; wasting (WHZ ≤ –2SD); severe wasting (WHZ ≤ –3SD); BMI; MUAC; HAZ; stunting (HAZ ≤ –2SD); severe stunting (HAZ ≤ –3SD) Biochemical: Hb Morbidity: prevalence of anaemia; incidence of diarrhoea, ARI and fever/malaria |
|
| Identification |
Sponsorship source: 6 study authors received funding from the DfID (DFiD PO 6433). 2 study authors received funding from the Directorate‐General for European Civil Protection and Humanitarian Aid Operations of the European Union (ECHO/ERC/BUD/2015/91001). The funders had no role in study design, data collection and analysis, decision to publish or preparation of manuscript. Standard cash and food voucher groups were funded by the EU. Double cash group funded by EU Humanitarian Aid and Civil Protection. Country: Pakistan Setting: poor and very poor HHs in Agrarian district Comments: ISRCTN registry ISRCTN10761532 Author's name: Bridget Fenn Email: bridget@ennonline.net Declarations of interest: yes; no competing interests (Fenn 2017). Study or programme name and acronym: REFANI Pakistan Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Randomisation by principal investigator using a random number table to generate randomisation sequence and then drawing village names from a box. Block randomisation was done, allowing equal distribution of the villages to each group for small, medium and large villages. |
| Allocation concealment (Selection bias) | Low risk | Allocation at village level. |
| Baseline characteristics similar (Selection bias) | Low risk | Village‐level characteristics were balanced at baseline but not all HH or child‐level characteristics. However, these were adjusted for in the analyses (child age at baseline, child sex; and for mother's analyses adjusted also for SES and baseline values of the outcome variables). |
| Baseline outcome measurements similar (Selection bias) | Low risk | There were some imbalances but these were adjusted for in the analyses. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding in this type of study is not possible. It is unlikely that lack of blinding would influence participant or personnel behaviour or experience, beyond changes expected due to the intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | Quote: "masking of the interventions to both participants and data collectors was not possible in this setting and for this type of study. Precautions were taken at the start of the study to try to mask the different interventions to participants, e.g., through incorporating buffer zones and training data collectors to keep the information to themselves, but it soon became clear that participants were aware of the other interventions." Comment: some outcomes were self‐reported and could have been susceptible to lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Cash transfers/food vouchers were only distributed to specific HHs, and all HHs in the same village were allocated to the same intervention. Therefore, contamination was unlikely. |
| Incomplete outcome data (Attrition bias) | Low risk | Children were excluded from the analyses if they had outlying data. In general, attrition was low (response rate for HHs was 95.6% and children was 98.3% within clusters at 6 months and for HHs was 95.0% and children was 96.8% at 1 year. For child outcomes, missing data were low (mostly < 5%). For maternal outcomes, only BMI had high missing data (26.9%) but ≤ 5% for other outcomes. No clusters were LTFU. |
| Selective outcome reporting (Reporting bias) | Low risk | All outcomes reported as specified in the protocol. |
| Other bias | Low risk | Misclassification bias of exposure: low risk; allocation by investigators. Measurement bias: low risk; appropriate instruments used and field workers trained in data collection. Incorrect analyses: low risk; clustering was taken into account in analyses. |
Fernald 2011.
| Study characteristics | ||
| Methods |
Study design: cRCT How were missing data handled? missing data excluded from analysis Randomisation ratio: 2:1 (79 parishes in intervention: 39 parishes in control) Recruitment method: NR Sample size justification and outcome used: NR Sampling method: stratified random sampling. Parishes stratified into rural and urban groups and from each group, treatment and comparison parishes were randomly selected. Study aim or objective: to analyse the impact of a programme that transfers cash to women in rural Ecuador on measures of ECD (Paxson 2010). First objective was to use a randomised effectiveness trial in Ecuador to address the question of whether very young children (aged 12–35 months) benefit in terms of health outcomes or language development if their families receive a cash transfer (Fernald 2011; study included a subset of younger children only). Study period: duration of intervention during which participants received transfers was unclear. Rural families in treatment group were eligible for the transfer for 17 months prior to the follow‐up survey. Rural families became eligible for transfer from June 2004, and urban families in November 2006 and follow‐up survey was conducted between September 2005 and January 2006. Unit of allocation or exposure: parishes allocated to intervention and control groups but certain HHs only selected for inclusion in study. |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: primary sample of HHs drawn for this study included only families in the first or second Selben quintiles who had children aged 0–6 at baseline, had no older siblings and had not received the Bono Solidario programme Exclusion criteria: NR Pretreatment: no significant difference between intervention and control parishes. Differences in baseline characteristics between HHs in the treatment and control groups were small and are never significant at conventional levels. This was true for the sample as a whole, as well as for families and children in the poorest quartile of per capita expenditures." Attrition per relevant group: total: 163/2748 children were LTFU (belonging to 77/1642 HHs). Attrition per group NR. Description of subgroups measured and reported: baseline expenditure (bottom quartile, top 3 quartile); age (young vs old); gender (boys vs girls) Total number completed and analysed per relevant group: total completed: 2585 children, 1565 HHs. Total number of children per group NR. Total number parishes analysed: varied per outcome due to missing data. Total number enrolled per relevant group: 77 parishes enrolled: 51 treatment; 26 control. Total enrolled: either 2748 or 2069 children (numbers in table A2 and 2 differed). Total HHs enrolled: 1642; 1388 children in intervention; 681 children in control. Total sample at baseline consisted of 3426 HHs and 5547 children aged < 72 months. Fernald 2011 focused only on children aged < 36 months at follow‐up (included children in urban and rural areas whereas Paxson 2010 only reported results for rural areas). Total number randomised per relevant group: 77 parishes randomised: 51 treatment; 26 control. Total enrolled: either 2748 or 2069 children (numbers in table A2 and 2 differed); 1388 children in intervention; 681 children in control. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Anthropometry: HAZ; height Biochemical: Hb Cognitive function and development: language (TVIP score and IDHC‐B score); long‐term memory; short‐term memory; visual integration Anxiety and depression: mother's depression score (CES‐D); mother's PSS |
|
| Identification |
Sponsorship source: Center for Economic and Policy Studies at Princeton University, the government of Ecuador, and the World Bank Country: Ecuador Setting: rural and urban parishes Author's name: Lia Fernald Email: fernald@berkeley.edu Declarations of interest: NR Study or programme name and acronym: Bono de Desarrollo Humano (BDH) programme Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Study was randomised but authors did not report how random sequence was generated. |
| Allocation concealment (Selection bias) | Low risk | Allocation was at parish level at beginning of study, and all eligible HHs that were in these parishes were either in intervention or control group. For inclusion in study, HHs had to meet specific criteria and then eligible HHs were randomly selected. |
| Baseline characteristics similar (Selection bias) | Low risk | Quote: "there is no evidence of significant differences between treatment and control parishes." "The table shows that differences in baseline characteristics between HHs in the treatment and control groups are small in magnitude and are never significant at conventional levels. This is true for the sample as a whole, as well as for families and children in the poorest quartile of per capita expenditures." |
| Baseline outcome measurements similar (Selection bias) | Low risk | Baseline outcome measurements (HAZ and TVIP score) were similar between children in intervention and control groups. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not possible due to the nature of the intervention, but it is unlikely to have influenced participant or personnel behaviour. |
| Blinding of outcome assessment (Detection bias) | Low risk | Blinding was not possible due to nature of intervention. However, objective outcomes were measured and, thus, it is unlikely that lack of blinding affected outcome assessment. |
| Protection against contamination (Performance bias) | Low risk | Quote: "According to survey response data, there was very little contamination of the intervention: take‐up of the BDH program was 73% for the treatment group and 3% for the comparison group." |
| Incomplete outcome data (Attrition bias) | Unclear risk | The numbers varied per outcome reported which indicates that missing data were excluded from the analysis. Total attrition was reported in 1 table as 163/2748 (5.9%) children; however, the total number of children enrolled/randomised was reported as 2069 in another table. Given the unclear reporting of numbers, it is unclear how much missing data there was and how it differed between the intervention and control groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol was available for this study. |
| Other bias | Low risk | Misclassification bias: unlikely as allocation was not self‐reported. Measurement bias: unlikely; standardised processes and tools used to assess outcomes. Incorrect analysis: SEs were clustered at parish level, therefore, clustering was adjusted for. No other bias identified. |
Ferre 2014.
| Study characteristics | ||
| Methods |
Study design: PCS Study grouping: N/A How were missing data handled? exclusions: the high attrition rate in Narayanganj, while not unusual given the high frequency of in and out migration among the residents of urban slums, was clearly a challenge for any social programme targeted towards the urban slum population. Due to this high attrition rate in Narayanganj, the impact evaluation was restricted to the Jaldhaka sample. Randomisation ratio: N/A Recruitment method: project: following a public information campaign on the project objectives and duration, the targeting and enrolment processes were carried out. Shombhob set up an open registration process where interested HHs with ≥ 1 child aged 0–36 months or at ≥ 1 primary school‐aged child (or both) were invited to apply for selection. Out of the 37,801 families who applied, the poorest 15,952 families were selected based on their PMT scores. The list of eligible beneficiaries was validated by community leaders, and verified by UP chairmen, and the Mayor's office in case of Narayanganj City Corporation. Sample size justification and outcome used: NR, but eligible families were requested to enrol, and this process was completed in April 2012. The final number of enrolled HHs was 14,125. Sampling method: random: 1. random sample of 3000 HHs drawn from the census list (all HHs in the 5 project unions of Jaldhaka) and interviewed. 2. HHs were randomly selected within each of the 4 demographic groups and within each of 2 PMT score groups (below 25th percentile and between 25th and 50th percentiles). (Note: HHs were assigned to the treatment group by a non‐random assignment rule based on the assignment variable. The eligibility for becoming beneficiaries of a programme was solely determined by whether they were below or above the unique cut‐off point.) Study aim or objective: 1. to test the delivery of CCTs to the poorest HHs through local governments to reduce their HH poverty levels; 2. increase school attendance of beneficiary children going to primary school, and 3. improve the nutritional status of beneficiary children aged 0–36 months. Study period: baseline (survey conducted): May/June 2011. Implementation: April 2012–December 2013 (although transfers only provided for 13 months). Follow‐up: May/June 2013. Unit of allocation or exposure: cluster: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: project used PMT scores to determine HH eligibility. Of the 37,801 families who applied for the programme, the poorest 15,952 were selected based on their PMT scores. This meant the cut‐off thresholds for selection was a PMT score of 660 for the 2 rural Upazilas. Eligible families had scores below the treatment cut‐off (treatment group) and ineligible families with had scores above the cut‐off (control group). Exclusion criteria: PMT score above the cut‐off. Pretreatment: most of the differences between the treatment and control HHs were nutrition outcomes. Treatment HHs appeared to be worse off compared to the control HHs in the incidence of stunting, wasting, underweight, knowledge of breastfeeding and dietary diversity. The same is true in terms of HH consumption. However, school attendance (defined as the number of classes missed in the last 2 weeks) and enrolment rates were almost identical. The DiD estimator assumes that the mean change in the control group represents the counterfactual change in the treatment group if there was no treatment. This allows a reliable inference of programme impact by comparing the pre‐ to postintervention change in the outcome of interest for the treated group relative to a control group. Attrition per relevant group: Jaldhaka (rural): 114 Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: Jaldhaka (rural) analysed only. Total 2287; treatment: 700; control: 1587 Total number enrolled per relevant group: 2401: 700 treatment and 1587 control (and 114 that were lost during follow‐up – unclear to which group these belonged). Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food Diet diversity: proportion of children aged ≥ 6 months fed from ≥ 4 food groups Anthropometry: stunting (HAZ < –2SD); wasting (WHZ < –2SD); underweight (WAZ < –2SD) |
|
| Identification |
Sponsorship source: South Asia Food and Nutrition Security Initiative (SAFANSI) and the Rapid Social Response (RSR) MDTF of the World Bank Country: Bangladesh Setting: rural only. Due to the high attrition rate in Narayanganj, the impact evaluation was restricted to the Jaldhaka sample. 10 Unions from 2 rural Upazilas (Jaldhaka and Hatibandha). Authors' names: Céline Ferré and Iffath Sharif Email: isharif@worldbank.org Declarations of interest: quote: "The papers carry the names of the authors and should be cited accordingly. The findings, interpretations, and conclusions expressed in this paper are entirely those of the authors. They do not necessarily represent the views of the International Bank for Reconstruction and Development/World Bank and its affiliated organisations, or those of the Executive Directors of the World Bank or the governments they represent." Study or programme name and acronym: Shombhob project Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Quote: "One way to deal with possible selection bias is to use a Regression Discontinuity Design (RDD) technique that exploits the targeting design itself. RDD is a quasi‐experimental design and makes use of discontinuities generated by program eligibility criteria such that program assignment is based on a cut‐off point of some assignment variable. Households are assigned to the treatment group by a non‐random assignment rule based on the assignment variable. The eligibility for becoming beneficiaries of a program is solely determined by whether they are below or above the unique value of a cut‐off point." |
| Allocation concealment (Selection bias) | High risk | Prospective cohort study |
| Baseline characteristics similar (Selection bias) | Low risk | Table B3 in Annexe II provides descriptive statistics of other HH level characteristics of both groups. The data suggest the groups are quite similar in terms of their observable characteristics, but treatment HHs are slightly bigger despite having the same number of young children (aged 0–3 years). Asset ownership is similar across the 2 groups (land, cattle, tube well, fan, television, bicycle, number of rooms) except for house ownership (slightly higher for the control group). Control houses have fewer children on average (0.74 vs 1.27 for treatment families), leading to slightly smaller HHs (4.5 members on average vs 5 for treatment families). |
| Baseline outcome measurements similar (Selection bias) | Low risk | Treatment HHs appeared worse off compared to control HHs in incidence of stunting, wasting, underweight, knowledge of breastfeeding, dietary diversity and HH consumption. However, this seemed to be addressed in the analysis. Quote: "Instead of computing this double difference in means, we run a set of DiD regressions, allowing controlling for differences in observable characteristics." |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants knew if they received a cash transfer or not. It is unlikely that lack of blinding influenced intervention received. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear if the interviewers were blinded. School enrolment, attendance, nutritional status (stunting, wasting, underweight), semi‐solid food intake and MDD are all objective outcomes. However, knowledge on infant feeding and consumption outcomes were self‐reported outcomes. |
| Protection against contamination (Performance bias) | High risk | If not enrolled for a cash transfer, a HH would not be able to receive it. There may be other bias. Quote: "The results on knowledge however are not able to take into account potential 'spillover effects' since nutrition sessions were delivered via classes held out in the open. In some villages, the growth monitoring was also conducted in courtyards. This modality of conducting the nutrition and growth monitoring sessions allowed non‐beneficiary mothers to have access nutrition‐related knowledge that this analysis is not able to capture." (page 33) |
| Incomplete outcome data (Attrition bias) | Unclear risk | Unclear how the 114 attrition cases were distributed over treatment and control. It is also unclear if the numbers that do not have a certain outcome (which could be because the outcome was not relevant or missing) were distributed evenly over the groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | None identified. |
Gangopadhyay 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group How were missing data handled? Midline survey results indicated that only 4 HHs that received the cash transfer (4%) did not want to continue, so dropped out of the analysis. Missing data were excluded from the analyses. Randomisation ratio: 1:1:1 – bank account and UCT (100 HHs); bank account and no UCT (100 HHs); no bank account or UCT (100 HHs) Recruitment method: study authors collaborated with the Self‐Employment Women's Association to explain the experiment to a 12‐block community of Raghubir Nagar. Awareness campaign ran for 2 weeks (first week of August 2010 to 13 August 2010). It initially targeted groups of 15–20 people, but, because ration shop owners tried to influence people to avoid participation in experiment, group sizes were reduced to 5 or 6 people at a time, to make their participation less noticeable. Sample size justification and outcome used: NR Sampling method: random selection of 350 HHs that had agreed to participate, of which 50 dropped out. These 300 HHs were selected for treatment group and control groups 1 and 2. Random selection of 150 HHs that did not want to participate were selected for control group 3. Study aim or objective: to compare effects of replacing welfare transfers in‐kind with a UCT on food security (measured as food consumption) to determine the impact of the cash transfer and the bank account. Study period: January 2011 to December 2011 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention: bank account + UCT
Control 1: bank account and no cash transfer
Control 2: no bank account + cash transfer
Control 3: random selection of 150 HHs that did not want to participate. Not included in analyses. Overall
Inclusion criteria: community in Delhi that received Government's BPL card (part of PDS programme; in‐kind transfer programme) Exclusion criteria: participants who were not BPL cardholders and lived outside of Raghubir Nagar Pretreatment: groups of self‐selected HHs were similar, such that randomisation apparently resulted in balanced groups (according to Table 3). Per capita expenditure on non‐food items was significantly different between the control groups 1 and 2; which was linked to differences in personal care expenditures between men and women. Attrition per relevant group: attrition in treatment group: 6 (6%); control group 1: 3 (3%); control group 2: 9 (9%); control group 3: 14 (9.3%) Description of subgroups measured and reported: N/A Total number completed and analysed per relevant group: total number completed and analysed in treatment group 94; control group 1: 97; control group 2: 91; control group 3: 136 Total number enrolled per relevant group: total number enrolled to participate 300 HHs. 100 HHs per group (intervention group, control group 1 and control group 2) Total number randomised per relevant group: 100 HHs per group (intervention group, control group 1 and control group 2) |
|
| Interventions |
Intervention characteristics Intervention: bank account and UCT
Control 1: bank account and no cash transfer
Control 2: no bank account or cash transfer Control 3: 150 HHs that did not want to participate, therefore no bank account or cash transfer. Not included in analyses. |
|
| Outcomes | Per capita expenditure on non‐cereal food items (pulses, milk, eggs, fish and meat, fruits and vegetables) Per capita calories consumed from cereals |
|
| Identification |
Sponsorship source: NR Country: India Setting: poor communities in Raghubir Nagar (West Delhi) Author's name: Robert Lensink Email: b.w.lensink@rug.nl Declarations of interest: yes; no potential conflict of interests Study or programme name and acronym: N/A Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Authors mentioned this was an RCT but did not describe how the random sequence was generated. |
| Allocation concealment (Selection bias) | High risk | Unit of allocation were HHs and HHs self‐selected into intervention group. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Although authors stated that characteristics of HHs were similar, percentages were reported with no CIs. |
| Baseline outcome measurements similar (Selection bias) | Low risk | No important differences in outcomes were present at baseline according to author's analyses. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding done, but it was unlikely to have influenced participant's and personnel behaviour during trial. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding was done and outcomes were based on self‐reports, which may have been influenced due to knowledge of treatment allocation. |
| Protection against contamination (Performance bias) | Low risk | Intervention was delivered as planned in intervention and control groups, and no‐one in control group received the intervention, aside from those that chose to be excluded from the study after it started (4 HHs). |
| Incomplete outcome data (Attrition bias) | Low risk | Comment: there was little attrition in all groups. Authors tested whether attrition was random through (quote) "… estimating a logit model that explained attrition using a vector of baseline variables …" and concluded that "… there is little reason to anticipate that our statistical results might be compromised by non‐random attrition biases." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. Outcomes were not explicitly stated in the Methods section of the paper |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: high risk. Measurement of outcomes was through a questionnaire; it was unclear which specific tools were used to ascertain dietary intake and HH expenditure and whether these had been validated. |
Gertler 2000 (PROGRESA).
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? missing data or potentially invalid data were excluded from the analysis (see footnote Table 3; Hoddinott 2003) Randomisation ratio: 60:40 (Gertler 2000) Recruitment method: using door‐to‐door methods to inform HHs about eligibility; PROGESSA achieved a take‐up rate of 97% (Gertler 2000) Sample size justification and outcome used: NR Sampling method: 506 communities randomly sampled from 50,000 eligible PROGRESA communities (matched on initial index level of community poverty) were chosen to participate, with each community randomly assigned to a treatment (n = 320) or control (n = 185) group. Study aim or objective: PROGRESA aimed to improve the nutritional status of poor children in rural Mexico in addition to improving education and health attainments while also reducing consumption poverty. Study period: about 2 years. Summer 1998 to summer 2000 (Gertler 2000). Some studies report < 2 years: from April 1998 (start of benefits) to October 1999 (when control HHs started receiving benefits). Intervention currently ongoing. Unit of allocation or exposure: communities |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: poor HHs within 506 poor communities with schooling and health infrastructure identified by PMT. List of beneficiary HHs presented to a community assembly for review and discussion and list was changed according to established criteria for the selection of beneficiary families (process called densification). No other criteria reported. Exclusion criteria: NR Pretreatment: overall, communities were comparable but this was not the case at HH or individual level. HHs in the intervention group were bigger, had more children but fewer adults aged > 55 years compared to control group (Hoddinott 2003). No difference in illness rates or number of visits to clinics for nutrition monitoring between control and treatment groups (Gertler 2000). Attrition per relevant group: overall attrition varied between papers and there was no report of attrition per group. 3350/12,291 (27%) intervention HHs did not receive the intervention by March 2000. Of these, 2872 HHs were not incorporated into programme; 478 HHs chose not to participate (no official records) or moved out of locality (Skoufias 2005). Attrition per group NR. In total, 221 HHs excluded as reported no food was consumed within the home, and 7165 HHs excluded with caloric availability per person per day < 875 kcal or > 4.768 kcal (Hoddinott 2003). Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: total 16,614 HHs, which excluded 7386 HHs that were excluded because of inadequate data. Number analysed per group NR and also varied depending on report. Total number enrolled per relevant group: 320 communities allocated to intervention and 186 to control groups, out of 506 communities. 24,000 HHs overall in sample at beginning of study (Hoddinott 2003). 97% of HHs enrolled in programme (Gertler 2000). Baseline sample included 112,319 individuals from 18,795 HHs in 506 experimental communities. Approximately, 60% of sample came from treatment areas and 40% from control (Gertler 2000). Total number randomised per relevant group: intervention group: 320 communities; control group: 186 communities |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention (started receiving benefits 2 years later)
|
|
| Outcomes | Total HH expenditure; HH expenditure on food Diet intake: HH caloric availability per month per day – all food/individual food groups Anthropometry: height; HAZ, stunting, BMIZ Biochemical indicators: anaemia Cognitive function and development: cognitive test scores (verbal, cognitive, behavioural) Morbidity: child illness rates |
|
| Identification |
Sponsorship source: Gertler 2000 NR. Gertler 2004 – Mexican government and Mexican Institute of Public Health funded data collection and initial data analysis, US National Institute of Child and Human Development provided research support Country: Mexico Setting: poor rural communities Authors' names: Paul J Gertler; Jere R Behrman; Lia CH Fernald; John Hoddinott; Emmanuel Skoufias Email: Gertler@haas.berkeley.edu; jbehrman@pop.upenn.edu; fernald@berkeley.edu; j.hoddinott@cgiar.org; eskoufias@worldbank.org Declarations of interest: NR Study or programme name and acronym: PROGRESA (Programa de Educacion Salud y Alimentacion)/ Oportunidades (PROGRESA was the original name and currently called Oportunidades) Type of record: IFPRI reports; journal articles |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Random assignment generated without weighting with randomisation commands in STATA version 2.0 (Fernald 2009). |
| Allocation concealment (Selection bias) | Low risk | Allocation done at community level. |
| Baseline characteristics similar (Selection bias) | Low risk | Study authors reported no baseline differences between groups at community level in terms of age, education, income and access to health care, but there were differences at HH level. They adjusted for HH demographic characteristics (e.g. HH size; proportions of children; and age, gender, education, occupation, ethnicity and marital status of the HH head) in their analyses. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Outcome measurements such as food consumption and child's anthropometry NR by study authors at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | Quote: "No sites were told that they would be participating in the programme, and information about timing of programme roll‐out was not made publicly available." Comment: blinding not possible in this type of intervention but researchers aimed to ensure that participants were not aware of the intervention evaluation. Lack of blinding is unlikely to influence participant or personnel behaviour in this type of intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | There was no blinding and outcomes were subjective, which could have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Unclear risk | Intervention communities were randomly selected from a set of rural communities in the same geographic region. In a baseline report, the study authors stated that it would be important to monitor individuals leaving or entering the localities in order to assess contamination bias (Behrman 2005), but no further data were provided in the later study report. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Attrition not clearly reported by study authors. Loss of clusters: NR. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available but outcomes outlined in methods section were reported in results section. |
| Other bias | High risk | Misclassification bias: low risk. Receipt of the programme was verified by examination of PROGRESA records. Measurement bias: unlikely. Incorrect analysis: unclear. Not all papers reported adjusting for clustering. Seasonality bias: unclear. Not controlled for in the analysis. Recruitment bias: high risk. List of beneficiary HHs within a community presented to a community assembly for review and discussion. |
Haushofer 2013.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel How were missing data handled? missing data due to attrition excluded from analysis. Analyses were based on total 1372 HHs, which is the sum of HHs at baseline only. Randomisation ratio: 1:1 (503:505) Recruitment method: after HHs and members identified, in private conversation, members were asked questions about demographics, and informed that they had been chosen to receive a cash transfer of KES 25,200 (USD 404). The recipient was informed that this transfer was unconditional, that they were free to spend it however they chose, and that it was a one‐time transfer and would not be repeated. Sample size justification and outcome used: sample size 500 individuals in each of the treatment, control and pure control group was chosen based on a power calculation, which showed that a sample of 1000 individuals was sufficient to detect effect sizes of 0.2 SD for all treatment vs pure control HHs with 89% power. Different treatment groups within the treatment groups (male vs female recipient, lump‐sum vs monthly, large vs small transfers) could be compared with 60% power (from registry record). Sampling method: purposive sampling of villages and HHs followed by random selection of HHs into treatment or control groups. GiveDirectly selected poor HHs by identifying poor regions of Kenya according to census data. Region chosen was Rarieda, a peninsula in Lake Victoria west of Kisumu in Western Kenya. GiveDirectly identified target villages through a rough estimation of the population of villages and the proportion of HHs lacking a metal roof, which is GiveDirectly's targeting criterion. Identified 126 villages. 63 of these villages were randomly chosen to be treatment villages. Control villages were only surveyed at endline; in these villages, authors sampled 432 HHs referred to as 'pure control' HHs. In treatment villages, second stage of randomisation assigned 50% of HHs to treatment condition, and 50% to control condition. Process resulted in 503 treatment HHs and 505 control HHs in treatment villages at baseline. Note: numbers were different between reports. Study aim or objective: to assess the relative welfare impacts of 3 design features of UCTs: gender of transfer recipient; temporal structure of transfers (monthly vs lump‐sum); and magnitude of transfer. Study period: transfers between June 2011 and January 2013 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: HHs lacking metal roof (indicator of poverty) Exclusion criteria: none reported Pretreatment: results were largely insignificant, suggesting that the treatment and control groups did not differ at baseline. Attrition per relevant group: overall: 68 (6.7%) (940/1008 surveyed at endline). Treatment: 32 (6.4%); LTFU (471/503 surveyed at endline); control: 36 (7.1%); LTFU (469/505 surveyed at endline) Description of subgroups measured and reported: male vs female recipients of transfers; monthly vs lump‐sum transfers; large vs small transfers Total number completed and analysed per relevant group: treatment: 471 HHs; control: 469 HHs Total number enrolled per relevant group: treatment: 503 HHs; control: 505 HHs Total number randomised per relevant group: treatment: 503 HHs; control: 505 HHs |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food: Total monthly HH food expenditure (cereals, tubers, meat/fish, dairy, fruit/vegetables, other food, food eaten out, Food security: FSI (based on weighted mean of measures of food security and hunger based on 17 outcome measures) Anthropometry: MUAC; height; weight Anxiety and depression: psychological well‐being index (standardised weighted mean of 6 psychological and neurobiological measures); log cortisol; CES‐D; Cohen PSS |
|
| Identification |
Sponsorship source: NIH Grant R01AG039297 and Cogito Foundation Grant R‐116/10 to Johannes Haushofer. Country: Kenya Setting: poor rural villages in Kenya Comments: additional documentation: online Appendix. RCT ID (trial registry): AEARCTR‐0000019 (www.socialscienceregistry.org/trials/19) Author's name: Johannes Haushofer Email: joha@mit.edu Declarations of interest: NR either authors. Quote: "Shapiro is a co‐founder and former director of GiveDirectly, Inc. (2009–2012). This paper does not necessarily represent the views of GiveDirectly, Inc" Study or programme name and acronym: N/A Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Randomisation method NR. |
| Allocation concealment (Selection bias) | Unclear risk | Concealment of allocation was not described, and HHs in the same cluster (village) were randomised to either receive the intervention or not. |
| Baseline characteristics similar (Selection bias) | Low risk | Quote: "The only significant difference between treatment and control households appears in income from self‐employment, where treatment households have a $33 PPP [purchasing power parity] lower income relative to the control mean of $85 PPP (39%) at baseline. This difference is significant at the 10% level, but does not survive FWER [familywise error rate] correction for multiple inference" |
| Baseline outcome measurements similar (Selection bias) | Low risk | Quote: "Online Appendix Table 35 shows only minor differences in the estimates of the treatment effects when baseline controls are included; none of the significant results become non significant or vice versa. Thus, baseline covariates do not affect our results strongly." "The only significant difference between treatment and control households appears in income from self‐employment, where treatment household shave a $33 PPP lower income relative to the control mean of $85 PPP (39%) at baseline. This difference is significant at the 10% level, but does not survive FWER correction for multiple inference." |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding. Unlikely to influence behaviour or experience of participants. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding, which may have affected self‐reported outcomes of participants who did not receive the cash transfers. |
| Protection against contamination (Performance bias) | Low risk | Quote: "First, we find no spillovers in consumption. This is surprising, given that we might have expected some informal insurance among households: in effect, the transfer is a temporary lottery gain, and theory predicts that households should have been sharing it with their insurance network." |
| Incomplete outcome data (Attrition bias) | Low risk | Few and balanced missing data – approximately 6% in each group. This was unlikely to introduce bias. |
| Selective outcome reporting (Reporting bias) | Low risk | No study protocol available but all outcomes outlined in registry were reported. |
| Other bias | Unclear risk | Misclassification bias: low. Measurement bias: unclear. Potential bias as information on dietary intake only captured at baseline and after 1 year. Incorrect analysis: unclear. Although there was a cluster randomisation, the analysis used for this review were at HH level and not cluster level. Comparison of intervention and control HHs in villages allocated to intervention group. |
Hidrobo 2014.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel How were missing data handled? Overall attrition 10%. Authors excluded data from HHs LTFU and with missing data but they constructed worse‐case scenarios to assess effects of excluding missing data. Construct worst‐case scenarios by assuming those HHs who select into the sample because of treatment (marginal HHs) were at the very top or very bottom of the outcome distribution. No differences in estimates observed in these analyses. Randomisation ratio: neighbourhoods and clusters randomised into 4 treatment groups using percentages of 20/20 for the control and food groups, and 30/30 for the cash and food voucher groups. 80 neighbourhoods and 145 clusters were randomised. Recruitment method: each HH in the selected neighbourhood was visited, mapped and administered a 1‐page questionnaire with basic demographic and socioeconomic questions. Sample size justification and outcome used: NR Sampling method: Neighbourhoods within urban centres were chosen for the intervention by WFP in consultation with the United Nations High Commissioner for Refugees (UNHCR) as areas that had large numbers of Colombian refugees and relatively high levels of poverty. Each HH was visited, mapped and administered a 1‐page questionnaire that consisted of basic demographic and socioeconomic questions designed to develop a PMT to define programme eligibility. However, based on point scores by nationality, the decision was made to automatically enrol all Colombian and mixed‐nationality HHs. First, neighbourhoods were randomised to either treatment or control group; second, all treatment clusters (geographical units within neighbourhoods) were randomised to cash, food voucher or food transfer. 1 unexpected complication in study design was change in beneficiary criteria implemented during baseline survey data collection. In process of surveying HHs, it was concluded that the targeting for transfers was too broad, resulting in the inclusion of HHs who were relatively well off. This led to a retargeting process where HHs who were relatively well off were dropped from the programme. Since there were not enough HHs in existing neighbourhoods to replace those that had been excluded and still reach programme enrolment targets, the decision was made to expand coverage to additional neighbourhoods on the outer circle of urban areas. These areas were subsequently rerandomised into treatment groups according to the approximate percentage lost. Study aim or objective: to compare the impact and cost‐effectiveness of cash, food vouchers and food transfers on the quantity and quality of food consumed. Objectives were 3‐fold: 1. to improve food consumption by facilitating access to more nutritious foods, 2. to increase the role of women in HH decision‐making related to food consumption and 3. to reduce tensions between Colombian refugees and host Ecuadorian populations. Study period: May 2011 to October 2011 Unit of allocation or exposure: neighbourhoods and clusters (geographical units within neighbourhoods) |
|
| Participants |
Baseline characteristics Control
Food transfer
Cash
Food voucher
Overall: NR Inclusion criteria: HHs residing in the selected neighbourhoods with low SES as measured by the PMT. All Colombian and mixed‐nationality HHs. Exclusion criteria: all HHs who reported receiving the government's social safety net transfer programme, the BDH. Pretreatment: higher proportion of Colombian heads in HHs in control vs cash group (P = 0.01). Larger HH size and number of children aged 6–15 years in HHs in control vs voucher group. Across 132 (22 × 6) difference‐in‐means tests between the treatment and control groups, only 4 were statistically different at the 5% level, which revealed that randomisation was, mostly, effective at balancing baseline characteristics. Attrition per relevant group: overall attrition 11.5% (235 HHs did not complete follow‐up survey and an additional 35 HHs did not have complete food consumption data and were excluded from analysis). Attrition rates: 11% in control group, 8% in food group, 9% in cash group and 11% in voucher group. Description of subgroups measured and reported: N/A Total number completed and analysed per relevant group: conducted analysis on the 2087 HHs that were in the baseline and follow‐up surveys and had complete data on food consumption. Number per group NR. Total number enrolled per relevant group: NR Total number randomised per relevant group: in total, 80 neighbourhoods and 145 clusters were randomised into the 4 intervention groups: control, cash, vouchers and food. Total number of HHs randomised = 2357. Number per group NR. |
|
| Interventions |
Intervention characteristics Food transfer
Cash transfer
Food voucher
Control: no intervention |
|
| Outcomes | Food expenditure per capita per month (log values) Dietary diversity: DDI; HDDS; FCS; proportion with poor food consumption; number of days a HH consumed foods from each individual food group Diet intake: log per capita caloric intake per person per day – total and per food group/item |
|
| Identification |
Sponsorship source: Government of Spain received through the WFP and funding provided by the CGIAR's Policy, Institutions and Markets research programme to IFPRI. Country: Ecuador Setting: poor neighbourhoods within 7 urban centres in the provinces of Carchi and Sucumbíos Author's name: Melissa Hidrobo Email: m.hidrobo@cgiar.org Declarations of interest: NR Study or programme name and acronym: N/A Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Authors stated that neighbourhoods and clusters were randomised to either intervention groups but there was no description of how the random sequence was generated. |
| Allocation concealment (Selection bias) | High risk | The unit of allocation was neighbourhoods. After the baseline survey there was (quote) "a retargeting process where households who were relatively well off were dropped from the programme. Since there were not enough households in existing barrios to replace those that had been excluded and still reach programme enrolment targets, the decision was made to expand coverage to additional barrios on the outer circle of urban areas. These areas were subsequently re‐randomised into treatment groups according to the approximate percentage lost." This rerandomisation of households was done after neighbourhoods had already been allocated to intervention groups, which could have introduced bias. |
| Baseline characteristics similar (Selection bias) | Low risk | Most baseline characteristics were comparable. Quote: "Across 132 (22 × 6) difference‐in‐means tests between the treatment and control groups, only four are statistically different at the 5% level, which reveals that randomisation was, for the most part, effective at balancing baseline characteristics." Although authors did not adjust for baseline characteristics in the analyses, they assessed the robustness of estimations in additional analyses, which provided similar effect measures. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Quote: "… estimate the treatment effect using Analysis of Covariance (ANCOVA) which controls for the lagged outcome variable." |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding of participants and personnel was not done. Knowledge of intervention allocation was unlikely to have affected participants' experience of the intervention. Authors reported that most participants used the interventions as they were supposed to. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding was possible. Outcomes were based on self‐reports from recipients; if they were not satisfied with intervention received, this could have biased their reporting of food consumed. |
| Protection against contamination (Performance bias) | Low risk | Allocation was by neighbourhood and cluster and it was unlikely that interventions were implemented in the wrong group. |
| Incomplete outcome data (Attrition bias) | Low risk | Quote: "Table B.1 in the appendix reveals that across 126 difference in means test for those who attrited, only 3 are significant at the 5% level. Those who left the food and cash arm are significantly younger than those who left the control arm; and those who left the food arm are less likely than the voucher arm to have a dirt floor. However, baseline analysis across treatment and control groups for households that remained in the study (Table 1) reveals that differences in age and dirt floor are not significant; therefore, the bias due to the differential attrition of these variables is likely to be very small." |
| Selective outcome reporting (Reporting bias) | Unclear risk | All relevant outcomes seemed to be reported but no protocol available. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Researchers knew who had been allocated to each group. Measurement bias: unclear. Authors reported different valid measures of food security and dietary diversity; however, this is based on information only measured once at baseline and once at follow‐up, which may not be sufficient for representative sample of food consumption. Incorrect analysis: unlikely. |
Hjelm 2017.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? subsample of HHs with female carers. No systematic difference in treatment group, age, education or marital status between women who responded and those with missing values. Due to their relatively small number, these observations were dropped from the analysis. Randomisation ratio: 1:1 Recruitment method: CWACs were randomly selected from 2 districts by the Zambian Ministry of Community Development Mother and Child Health. Each CWAC identified eligible HHs meeting ≥ 1 inclusion criterion, and 33 HHs were approached from these. Sample size justification and outcome used: reported that a power analysis was conducted to determine a sample size large enough to detect meaningful effects, also among subgroups. Outcomes used in their calculation NR. Sampling method: total sample: 46 CWACs out of approximately 100 CWACs from each district (Luwinga, Serenje districts) were included through a lottery held at Ministry headquarters in June 2010. Thereafter, 33 HHs per CWAC were randomly selected (out of approximately 100 eligible HHs per CWAC), resulting in 3077 HHs (15,630 people). Subsample: 2490 HHs with female carers were included in the secondary analysis of the outcome perceived stress. Study aim or objective: impact evaluation of programme related to changes in 5 primary areas: income, education, health, food security and livelihoods. Study period: December 2011 to December 2014 Unit of allocation or exposure: communities through CWACs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: HHs that are female‐headed and caring for orphans, had a disabled member, were elderly headed (> 60 years) and caring for orphans, or are special cases (cases that are critical, but did not qualify under other categories; e.g. 2 elderly people unable to care for themselves). Exclusion criteria: NR Pretreatment: no differences reported between the groups in the total sample (3077 HHs), or those in the subsample of HHs with female carers (2490 HHs). Attrition per relevant group: overall attrition was 106/3076 (3.4%) HHs. Per‐group attrition was 70/1561 (4.5%) HHs (4.2% in Serenje district and 4.9% in Luwingu district) in the intervention, and 35/1515 (2.3%) (2.3% in Serenje district and 2.4% in Luwingu district) in the control group. Description of subgroups measured and reported: HHs caring for orphans, female‐headed HHs and HHs with adolescents. Total number completed and analysed per relevant group: 2970/3076 (96.6%) HHs overall, with 1490/1561 (95.5%) in intervention group and 1480/1515 (97.7%) in control group. Total number enrolled per relevant group: 3076 HHs; 1561 in intervention group and 1515 in control group. Subsample of HHs with female carers: NR. Total number randomised per relevant group: 3076 HHs in 92 CWACs; 1561 from 46 CWACs in intervention group and 1515 from 46 CWACs in control group. Subsample of HHs with female carers: NR. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention
|
|
| Outcomes | Proportion of per capita expenditure spent on buying food Food security: HFIAS Anxiety/depression: Cohen PSS; CES‐D short form; depression (based on cut‐off value for the CES‐D) |
|
| Identification |
Sponsorship source: consortium of donors including DfID, UNICEF, Irish Aid, and the Government of Finland. Palermo, Handa, and Hjelm received additional funding from the Swedish International Development Cooperation Agency (G41102) to the UNICEF Office of Research – Innocenti for analysis of the data and drafting of the manuscript. Country: Zambia Setting: socially vulnerable HHs in 2 rural districts with extreme poverty (Luwinga, Serenje) Author's name: Lisa Hjelm Email: lhjelm@unicef.org Declarations of interest: no Study or programme name and acronym: Zambia Multiple Category Cash Transfer Program (MCP) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Randomisation by coin toss with local officials, ministry staff and community members present. Randomisation appeared to have occurred by a single coin toss, allocating one half of the list of CWACs to intervention or control – unclear how this may have biased the process. |
| Allocation concealment (Selection bias) | Unclear risk | NR whether the allocation outcome of the randomisation process (a single coin toss) was protected from the person performing the randomisation (the Ministry's permanent secretary) beforehand. |
| Baseline characteristics similar (Selection bias) | Low risk | HH characteristics were similar for both groups at baseline in the total sample, as well as in the subsample of HHs with female carers. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Total group: balanced at baseline with no statistically significant differences for outcome measures. Subsample of HHs with female carers: indices of HH food insecurity were similar at baseline; however, parameters of perceived stress were only measured at the end of the study period. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants and study staff do not appear to have been blinded to assignment, but it is unlikely that this influenced the intervention received. |
| Blinding of outcome assessment (Detection bias) | High risk | Participants did not appear to have been blinded to assignment and were the outcome assessors as outcomes were self‐reported. |
| Protection against contamination (Performance bias) | Low risk | Serenje and Luwingu are both large, geographically discrete districts. In addition, communities were the unit of randomisation. It is unlikely that contamination would present considerable bias. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Missing values were dropped from the analysis, but there was low overall attrition of 3.4% (with 4.5% in the intervention and 2.3% in the control group); with no evidence of selective attrition. Attrition in HHs with female carers, however, was not described. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Outcomes for the overall evaluation were not clearly stated, but all outcomes appeared to have been addressed in the evaluation report. |
| Other bias | Low risk | Recruitment bias, low risk: randomisation followed recruitment and baseline survey. Incorrect analysis, low risk: OLS regression with cluster robust SEs were used to account for the clustered nature of the data. Loss of clusters, low risk: no loss of clusters reported. Seasonality bias, low risk: unlikely as the baseline and follow‐up data were conducted at the same time of the year. |
Hoddinott 2013.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel How were missing data handled? NR Randomisation ratio: NR Recruitment method: phase 1: all HHs in selected villages could voluntarily participate in the PWP and receive cash or food transfers. Study authors reported that the intervention began after a process of sensitisation in all villages. Phase 2: targeted HHs in selected villages continued with unconditional cash or food transfers according to specific criteria. Sample size justification and outcome used: NR Sampling method: phase 1: convenience sample. 79 villages were suitable and could receive either food or cash transfers. Of these, 52 villages were included in final sample since it would have been too complicated/led to tension if proximate villages shared a work site (5670 HHs). Phase 2: 50% of HHs in each village were targeted to receive the same transfer without having to fulfil a work requirement (2786 HHs). Random sample was taken from these HHs for the collection of outcome data such as food security outcomes before the start of the unconditional transfers (2268 HHs). Study aim or objective: to examine the differential impact of food and cash transfers on 5670 HHs eligible for emergency assistance in eastern Niger. Study period: first phase included 3 months of public works (April–June 2011), while second phase provided 3 months of unconditional transfers (July–September 2011) to the most vulnerable HHs during the peak of the lean season. Unit of allocation or exposure: village |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: phase 1: HHs in 52 selected villages in the Mirrah district willing to participate in PWP. Phase 2: the following were targeted to receive unconditional cash or food transfers: HH with: female heads (for Karkara only, female heads with ≥ 5 dependents); children aged 6–23 months; lactating mother and child aged 0–5 months; migrants from Côte d'Ivoire, Libya or Nigeria; with disabled person (for Karkara only); and very vulnerable HHs (as decided in a consultative process with the community). Exclusion criteria: NR Pretreatment: no group differences between HHs targeted to receive unconditional cash or food transfers (during phase 2 of study) in terms of HH composition, age and gender of HH head, and housing characteristics. Attrition per relevant group: intervention group (UCT): 19/1198 (1.6%); comparison group (unconditional food transfers): 40/1070 (3.4%). Study authors stated that these HHs could not be traced. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: NR Total number enrolled per relevant group: phase 2 Intervention group (UCTs): 1198 HHs from 25 VCs; control group (unconditional food transfers): 1070 HHs from 27 VCs. Total number randomised per relevant group: phase 1: intervention group (cash villages): 25 VCs; control group (food villages): 27 VCs |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Dietary diversity: HDDS; FCS; DDI; CDS; consumption of individual food groups | |
| Identification |
Sponsorship source: government of Spain through the WFP Country: Niger Setting: poor rural HHs at high risk of famine. Author's name: John Hoddinott Email: J.Hoddinott@cgiar.org Declarations of interest: NR Study or programme name and acronym: NR Type of record: study report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Method of random sequence generation not described. |
| Allocation concealment (Selection bias) | Unclear risk | Quote: "Randomization was done through a procedure that assured an approximately equal distribution of villages/work sites by zone and size receiving each transfer." Comment: unclear how the procedure was conducted. |
| Baseline characteristics similar (Selection bias) | Low risk | HHs that were targeted to receive UCT (intervention group) or food transfers (control group) were similar in terms of HH composition; age and gender of HH head; and housing characteristics. Although these data were collected retrospectively, it was unlikely to increase the risk. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Since food security outcome data were only collected from HHs after first phase of study it is unknown what the food security status of these HHs was before the start of any intervention. |
| Blinding of participants and personnel (Performance bias) | Low risk | Unclear whether participants or personnel involved with the study (or both), were blinded. However, this is unlikely to influence participant or personnel behaviour beyond that expected by the intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether outcomes were assessed blindly but outcomes were self‐reported and likely to be influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Study authors reported that they excluded proximate villages that would have had to share a worksite. Study villages were, therefore, geographically removed from one another. |
| Incomplete outcome data (Attrition bias) | Low risk | Although attrition was higher in the control group (food transfers; 3.4%) compared to the intervention group (UCT; 1.6%), it was low. Loss of entire clusters were NR. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: low risk. HH food consumption was assessed using standardised methods. Incorrect analysis: low risk. Analysis was adjusted for clustering. Recruitment bias (cRCTs): low risk. Majority of all HHs in villages that were randomised participated in the study (95–98%). |
Huerta 2006 (PROGRESA).
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? missing data excluded Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: a subsample was chosen because a smaller number of children was adequate to assess the expected 2‐year impact on growth (0.8 cm) and anaemia (10 pp reduction). Sample size was calculated according to the original 2‐year intervention design for 1‐tailed tests, assuming a 0.05 significance level and a power of 90%. It was first estimated as a simple random sample, which was further multiplied by a design effect of 1.4 to take into account the complex sample design. Sampling method: nutritional impact substudy was conducted in a random selection of 205/320 communities scheduled to enrol in the programme at the end of 1998 and 142 communities randomly selected from the 186 communities that enrolled 1 year later, in late 1999. The communities for the larger PROGRESA evaluation were randomly selected; more details in Gertler 2000). Study aim or objective: to document the short‐term nutritional impact of a large‐scale, incentive‐based development programme in Mexico (Progresa) (Rivera 2004). To assess whether PROGRESA reduced the major childhood diseases that affect children aged < 5 years: diarrhoea and respiratory infections (Huerta 2006). Study period: August–September 1998 to November–December 2000 (data included a period when both groups were receiving the intervention) Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure: NR Control: NR Overall: NR Inclusion criteria: poor households in rural areas where there is schooling and health infrastructure. Rivera 2004: infants aged 12 months. Huerta 2006: children aged 0–59 months. Gertler 2004: children aged < 3 years at baseline. Exclusion criteria: NR Pretreatment: True baseline data NR. Actual baseline data indicated no baseline differences between children aged ≤ 12 months, between the groups in terms of gender, age and anthropometric status (Rivera 2004). Socioeconomic and morbidity data N/A at baseline. Attrition per relevant group: From baseline to first follow‐up (1999): intervention: 172 children LTFU; control: 132 children LTFU. Description of subgroups measured and reported: Children aged 6 months at baseline or aged 12 months at baseline Total number completed and analysed per relevant group: total: 595 children (however, these are children surveyed in 2000, when control HHs had already been receiving the intervention for 1 year). Intervention: 336 children (2 years of exposure); control: 259 children (1 year of exposure) Total number enrolled per relevant group: 795 children. Exposed group (received intervention): 461 children (aged 12 months) from 175 communities; unexposed group (also termed crossover intervention group): 334 children (aged 12 months) from 107 communities Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention
|
|
| Outcomes | Anthropometry: LAZ or HAZ, WAZ, WLZ Biochemical: Hb Morbidity: anaemia, diarrhoeal disease, respiratory disease |
|
| Identification |
Sponsorship source: CONACYT and the ESRC Research Centre for Analysis of Social Exclusion (CASE) at the London School of Economics; Mexican Ministry of Health. Country: Mexico Setting: poor rural HHs Authors' names: Juan A Rivera; Maria C Huerta Email: jrivera@correo.insp.mx; m.c.huerta@lse.ac.uk Declarations of interest: Mexican Ministry of Health commissioned the evaluation of the nutrition component of the Education, Health and Nutrition Program (Progresa) to a group of investigators of the Instituto Nacional de Salud Publica as independent evaluators. Ministry and its personnel did not participate in design, data collection or analysis. They did not participate in the preparation of manuscript or its authorisation for publication (Rivera 2004). No (Huerta 2006). Study or programme name and acronym: PROGRESA/Oportunidades Type of record: journal articles |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Nested cohort study design within a cRCT; therefore; no randomisation done. |
| Allocation concealment (Selection bias) | High risk | Nested cohort study design within a cRCT; therefore, no allocation concealment done. |
| Baseline characteristics similar (Selection bias) | Low risk | Data at baseline N/A, but some analyses showed that, although sample was balanced at community level, it was not at HH or individual level. However, authors accounted for potential confounders in their analyses. Quote: "In order to isolate the intervention effect from the possible influence of other background variables, we included a set of explanatory variables at the individual, household and community level." |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Data at baseline N/A. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding; however, unlikely that the performance of participants and personnel were influenced by lack of blinding. |
| Blinding of outcome assessment (Detection bias) | High risk | Blinding not done. Health outcomes based on self‐report and could have been influenced by knowledge of treatment allocation. Authors reported evidence from preliminary analysis on biased reporting of these outcomes. |
| Protection against contamination (Performance bias) | High risk | There was contamination for some components of the intervention. Quote: "For ethical reasons, health centres provided supplements to malnourished children irrespective of whether they belonged to a control or a treatment community. Therefore, children in both types of localities could receive this in‐kind benefit" (Huerta 2006). |
| Incomplete outcome data (Attrition bias) | High risk | Very high levels of attrition/missing data after 1 year of the intervention: intervention: 172/461 (37%) children; control: 132/334 children (39%). |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | High risk | Misclassification bias: low risk. Recipients registered as beneficiaries of programme. Measurement bias: high risk. Quote: "One of the limitations of these data is that information on health outcomes may suffer from reporting errors. In preliminary analyses, we found some evidence of reporting errors, specifically for respiratory infections." Incorrect analysis: low risk. Authors adjusted for clustering (this was a nested cohort of a cRCT) |
Jensen 2011.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group How were missing data handled? NR Randomisation ratio: 3:1 (3 intervention levels) Recruitment method: NR Sample size justification and outcome used: NR Sampling method: officially designated urban poor HHs in the Chinese provinces of Hunan and Gansu were randomly selected to participate using lists kept at the local offices of the Ministry of Civil Affairs. Study aim or objective: to determine whether food price subsidies result in improved nutrition in poor Chinese HHs. Study period: April–December 2006 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: officially designated as urban poor (HHs fell below a locally defined poverty threshold (the Di Bao line), typically CNY 100–200 per person per month or USD 0.41–0.82 per person per day, which is below even the World Bank's 'extreme' poverty line of USD 1 per person per day); located in 2 Chinese provinces which provide subsidies for staples goods (rice in Hunan and wheat flour in Gansu). Exclusion criteria: NR Pretreatment: no group differences for the total sample, but in the Hunan subsample the 0.3 subsidy group had higher vitamin and mineral intake compared to control as well as a smaller family size compared to the 0.2 subsidy group. In the Gansu subsample 0.1 and 0.2 subsidy groups both had a smaller family size compared to control, while the 0.3 subsidy group had lower protein per capita compared to control and lower mineral intake compared to the 0.2 subsidy group. Attrition per relevant group: NR. Total attrition between round 1 and 2 was < 1% (11/1300 HHs), and no HHs attrited between round 2 and 3. Description of subgroups measured and reported: baseline characteristics and outcomes were reported for Hunan and Gansu provinces as subgroups of the pooled data. Intervention group split into 3 levels: 0.1, 0.2 and 0.3 subsidy level (corresponding to CNY 0.1, CNY 0.2 and CNY 0.3 reduction per 500 g of staple good). Total number completed and analysed per relevant group: total of 1293 HHs (Hunan 644; Gansu 649) completed baseline surveys: 324 in control group and 324 for subsidy level 0.1, 324 for subsidy level 0.2 and 321 for subsidy level 0.3. 1271 HHs were included in the analysis, but no breakdown by control and intervention levels provided. Total number enrolled per relevant group: 1300 HHs enrolled. 324 HH completed baseline surveys in the control, 324 in subsidy level 0.1, 324 in subsidy level 0.2 and 321 in subsidy level 0.3. Total number randomised per relevant group: NR |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Adequacy of dietary intake: caloric/protein intake per capita Mineral Sufficiency index, Vitamin Sufficiency Index |
|
| Identification |
Sponsorship source: National Institute of Aging, the William F. Milton Fund at Harvard Medical School, the Harvard Kennedy School's Dean's Research Fund, the Center for International Development at Harvard University, and the Hefner China Fund. Country: China Setting: extremely poor HHs in urban areas Authors' names: Robert T Jensen; Nolan H Miller Email: nmiller@illinois.edu; robertjensen@ucla.edu Declarations of interest: NR Study or programme name and acronym: N/A Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | HHs were randomised to control or 3 levels of intervention, but no information provided on how this was achieved. The even distribution of HHs at baseline (324, 324, 324 and 321) indicated that a pseudo‐random technique may have been employed. |
| Allocation concealment (Selection bias) | Unclear risk | No information reported on whether or how the randomisation sequence was protected. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Covariates were balanced across the entire pooled group, but significant differences existed at the province level. In Hunan, 0.3 subsidy HHs had significantly fewer members (t = 0.27; P < 0.05) when compared to 0.2 subsidy HHs; while in Gansu 0.1 and 0.2 subsidy HHs had significantly fewer HH members (0.1: t = 0.24; P < 0.05; 0.2: t = 0.19; P < 0.05) when compared to control. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Overall, for the pooled sample randomisation appears to have achieved balance across the control and 3 treatment groups. Statistically significant differences exist between intervention and control groups at the province level, with 0.3 subsidy HHs in Hunan having significantly higher mineral (t = –0.074; P < 0.05) and vitamin (t = –0.13; P < 0.001) intake; and 0.3 subsidy HHs in Gansu having significantly lower (t = 3.84; P < 0.05) per capita protein consumption. In the latter province, 0.3 subsidy HHs also had a significantly lower mineral intake when compared to 0.2 subsidy HHs (t = 0.058; P < 0.05). |
| Blinding of participants and personnel (Performance bias) | Low risk | Given the nature of the intervention, it is very unlikely that participants could have been blinded to their allocation but this is unlikely to have introduced performance bias. |
| Blinding of outcome assessment (Detection bias) | High risk | As participants were the outcome assessors during the survey and were likely aware of their allocation to control or intervention, it is possible that this knowledge may have influenced the results. |
| Protection against contamination (Performance bias) | Low risk | Quote: "The possibility that the subsidy may attract other non eligible family members to the household is one case where the subsidy as we implemented it may yield different impacts from general subsidy. Our subsidy was assigned to only a subset of households, creating a potential pool of ineligible persons related to an eligible person. In the case of a universal subsidy for which all individuals are eligible, or a subsidy targeted to the poor where there is high correlation in poverty among relatives, we would not expect the same household composition response. While this is a potential threat to the external validity of our study, the fact that we find that no such changes took place makes this concern less important." |
| Incomplete outcome data (Attrition bias) | Low risk | Attrition was very low across the study, with < 1% of HHs (11/1300) being LTFU. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available, but it appeared that all relevant outcomes in the methods section were reported in the results section. |
| Other bias | Low risk | None identified. |
Jodlowski 2016.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? 8 HHs that were missing in some of the survey rounds were excluded in the analyses. The authors stated that they found little evidence to suggest that attrition was systematic or influenced their results. No data provided. Randomisation ratio: N/A Recruitment method: formation of local community groups, followed by submitting an application to Heifer International's Zambia offices for participation in the livestock assistance programme. Sample size justification and outcome used: NR Sampling method: unclear. The authors stated: "The selection of original beneficiaries among the eligible households is known to have been random in 1 community, and is assumed to have been random in other communities where the process was not observed." Study aim or objective: to use unique panel data from the rollout of a Heifer International livestock programme in Zambia to identify the causal effect of livestock ownership on dietary diversity and consumption expenditure. Study period: January 2012 to August 2013 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure group (livestock receipt and training programme):
Control (Prospectives and Pass‐on‐the‐Gift (POG) group – no livestock receipt)
Overall: NR Inclusion criteria: poor HHs from 5 rural communities in Zambia (Kamisenga, Kaunga, Kanyenda, Chembe and Mwanaombe) who were eligible to receive livestock from the Heifer International programme. These HHs were required to participate in training activities and agree to make initial investments in animal facilities at their homes, as well as payments into a community insurance fund. Exclusion criteria: non‐poor HHs in these communities or those not willing to partake in the livestock programme Pretreatment: participants in the POG group were significantly different from those in the originals group with respect to age of head, and amount of land cultivated. Participants in POG group were significantly different from those in the independent group with respect to education of head, weekly expenditure per capita; value of HH and farm assets; amount of cultivated land. Attrition per relevant group: intervention group (original group) 2/105; control group (POG): 8/111; control group (prospective group): 1/67 Description of subgroups measured and reported: types of livestock received by intervention HHs. Dairy cattle (Kamisenga): 73; graft cattle (Kaunga): 40; goat (Kanyenda): 103 Total number completed and analysed per relevant group: intervention group (original group) 103; control group (POG group) 103; prospective group 66 Total number enrolled per relevant group: intervention group (original group) 105; control group (POG group) 111; prospective group 67 Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure group:
Control (POG) group – no livestock receipt
|
|
| Outcomes | Per capita total weekly expenditures on food and non‐food items Dietary diversity: HDDI, probability weighted DDS |
|
| Identification |
Sponsorship source: Elanco Animal Health (USA) and Heifer International Country: Zambia Setting: rural communities in Coppervelt Province of Zambia Author's name: Margaret Jodlowski Email: mcj47@cornell.edu Declarations of interest: no Study or programme name and acronym: Copperbelt Rural Livelihoods Enhancement Support Project (CRLESP) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA study; therefore, randomisation was not done. |
| Allocation concealment (Selection bias) | High risk | CBA study and no randomisation was done. |
| Baseline characteristics similar (Selection bias) | Low risk | The study authors reported a marginally larger mean cultivated land area in the intervention group. However, they stated that 1 HH largely drove this difference and that when this outlier was removed, the difference disappeared (data not shown). |
| Baseline outcome measurements similar (Selection bias) | Low risk | HH DDSs were similar in intervention and control groups at baseline. Regression analyses reported no significant differences in terms of baseline dietary diversity or consumption between HHs receiving different types of livestock, compared to control HHs. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants and personnel were aware of the livestock intervention but this was unlikely to have influenced their behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding and for DDS outcome: (quote) "Food groups are recalled by the family member responsible for food preparation and recorded on the survey instrument." Self‐reported data could have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | High risk | Authors assessed spillover effects to HHs in the control group (POGs) but that were in the same community as the intervention HHs, and found no statistically significant difference in outcomes except for milk consumption, which also increased in POG HHs although not to the same extent as in intervention HHs. |
| Incomplete outcome data (Attrition bias) | Low risk | Overall attrition was low (3.8%; 11/283). |
| Selective outcome reporting (Reporting bias) | Unclear risk | Outcomes reported were in line with those specified in the methods but no protocol available. |
| Other bias | Low risk | None identified |
Kandpal 2016.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? authors reported that ITT analysis was performed; however, what they defined as ITT analysis was NR Randomisation ratio: 1:1 Recruitment method: sample selected in 3 stages (Figure 1). First, provinces in which the programme had not been introduced as of October 2008 were enumerated. Of the 11 provinces available, 3 were excluded because of security concerns. From the remaining 8 provinces, 4 provinces were chosen to span all 3 macro areas of the country (North, Visayas and Mindanao). Next, in each of these 4 provinces, 2 municipalities were randomly chosen to represent the mean poverty level of areas covered by the programme. Within each selected municipality, 130 villages were randomly assigned to treatment and control groups of 65 villages each. Data for the HH assessment form to run the PMT for beneficiary selection were fielded in the 8 RCT municipalities between October 2008 and January 2009. This was followed by the implementation of Pantawid in treated villages, with the first payment of cash grants commencing in April 2009. Data used in this analysis were collected in a follow‐up survey from the 130 villages in October and November 2011, allowing for a programme exposure period of 30–31 months. Sample size justification and outcome used: because this evaluation was a cRCT with treatment assignment at the village level, a power analysis (Supplemental Table 1) was conducted using the 3 main outcomes of interest: monthly per capita HH consumption, school participation by children aged 6–14 years, and health facility visits by children aged 0–5 years. In keeping with the programme's stated objective of improving child health and nutrition, the central research question of the impact evaluation was to estimate the programme effect on child health and education. However, at the time of the power calculations, data on child anthropometric measurements were N/A for the Philippinesat, a decentralised level; as a result, these outcomes were omitted from the power calculations despite their being a central concern of the impact evaluation. The 2007 Family Income and Expenditure Survey and the 2003 National Demographic Health Survey data sets were used as proxies for outcome mean and variance in the comparison population. A modest hypothesised impact ensured an adequately powered study. The power analysis used a 10% increase in HH per capita expenditures, a 7 pp increase in school enrolments in children aged 6–14 years, and a 7 pp increase in health facility visit rate in children aged 0–5 years. Intracluster correlation coefficients were 0.12–0.25, depending on the outcome of interest. These factors combined to suggest an RCT size of 3900 HHs randomly selected from 134 enumeration clusters. Sampling method: eligible poor HHs were identified by the survey conducted by the National Household Targeting System for Poverty Reduction (NHTS‐PR) that used a PMT, which estimated per capita HH income on the basis of observable and easily provided information, including HH size and physical dwelling conditions. HHs with estimated per capita income below the poverty line were classified as poor. From this subset of poor HHs, Pantawid identified eligible HHs as being those with children aged 0–14 years or a pregnant woman at the time of the assessment, or both. Poor and eligible HHs received a combination of health grants and education grants every 2 months of PHP 500–1400 (USD 11–32), depending on number of eligible children in HH. Study aim or objective: to assess the impact of the Pantawid Pamilyang Pilipino Program (or Pantawid Pamilya) on HAZ and stunting of young children aged 6–36 months at the time of follow‐up survey. Study period: baseline data collected October 2008 to January 2009; follow‐up data collected October–November 2011 Unit of allocation or exposure: villages were allocated as clusters |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: category 1 HH: 1418 poor HHs, i.e. HHs whose estimated per capita income fell below the poverty line, and that also had children aged 0–14 years or a pregnant mother (or both) at time of assessment. Exclusion criteria: 3 provinces were excluded because of security concerns Pretreatment: baseline data showed that HH characteristics were not significantly different between the 1418 category 1 treatment and control HHs. Attrition per relevant group: survey data included complete HAZ data on 194/241 treated children aged 36 months and 178/244 control children aged 36 months. Complete weight‐for‐age data collected for 204/241 treated children aged 36 months, and 189/244 control children aged 36 months. Anthropometric z‐scores were calculated on the basis of the WHO growth standard. Scores > 6 SDs above or below the reference mean were dropped from the sample. This trimming resulted in the dropping 10/194 treated children and 11/178 control children from the HAZ regressions, and the dropping of 2/204 treated children and 1/189 control children from the weight‐for‐age regressions. 15% of those eligible in the treatment villages reported that they did not participate; NR for control villages. Description of subgroups measured and reported: N/A Total number completed and analysed per relevant group: intervention group (children aged 6–36 months): 194 had height‐for‐age data, and 204 had weight‐for‐age data; control group (children aged 6–36 months): 178 had height‐for‐age data and 188 had weight‐for‐age data Total number enrolled per relevant group: intervention group: 241 children aged 6–36 months were part of HHs that underwent survey; control group: 244 children aged 6–36 months were part of HHs that underwent survey. Total number randomised per relevant group: sample of 1418 HHs was randomly assigned to 714 treated HHs and 704 control HHs for the impact evaluation. At time of the data collection in 2011, in these 714 treated HHs there were 241 children aged 3 years who could have been exposed to the programme in the first 1000 days of their lives, and 244 children in the same age range from poor HHs in control areas. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Diet diversity: child consumption of eggs/dairy/meat/fish in the past week Anthropometry: WAZ, underweight, severely underweight, HAZ, stunted, severely stunted Morbidity: fever, cough, or diarrhoeal disease in past 2 weeks |
|
| Identification |
Sponsorship source: Consultative Group on International Agricultural Research (CGIAR) Research Program on Policies, Institutions, and Markets Country: Philippines Setting: poor HHs across all 3 macro areas of the country (North, Visayas and Mindanao) Author's name: Eeshani Kandpal Email: ekandpal@worldbank.org Declarations of interest: yes; no conflicts of interest. Study or programme name and acronym: Pantawid Pamilyang Pilipino Program (CCT programme) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Method of randomisation NR. |
| Allocation concealment (Selection bias) | Unclear risk | Allocation concealment NR. |
| Baseline characteristics similar (Selection bias) | Low risk | Reported baseline characteristics were similar across intervention and control groups. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Baseline data for nutritional outcomes NR. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants not blinded, but this was unlikely to have influenced participant behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether data collectors were blinded towards the group allocations, which may or may not have influenced the measurement of outcomes across groups, as some outcomes were self‐reported. |
| Protection against contamination (Performance bias) | High risk | 7% of the control group participated in the intervention (ITT analysis performed), which may or may not have biased the estimated effects of the intervention towards 0. |
| Incomplete outcome data (Attrition bias) | High risk | Missing outcome data excluded from analyses and differed across groups, and reasons for LTFU were NR. For the outcome height‐for‐age, attrition was 47/241 (19.5%) in intervention group and 66/244 (27%) in control group. For the outcome weight‐for‐age, attrition was 37/241 (15.4%) in intervention group and 55/244 (22.5%) in control group. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol or trial registration number NR. While height‐for‐age and weight‐for‐age anthropometrical measurements in children aged 6–36 months were reported; weight‐for‐height (important to indicate wasting) was not. Results for the following outcomes were NR: monthly per capita HH consumption and health facility visits by children aged 0–5 years. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: low risk. Quote: "Several rounds of training were conducted before data collection to ensure data quality, particularly of the anthropometric and dietary intake modules." However, the method for collecting dietary data (e.g. 24‐hour recall, or food frequency questionnaire) was NR. Incorrect analysis: low risk. Quote: "In order to take into consideration regional factors, including province‐specific eligibility cutoffs, and the clustered nature of the sample …, municipality fixed‐effects regressions were included. In addition, all SEs were clustered at the village level." |
Kangmennaang 2017.
| Study characteristics | ||
| Methods |
Study design: PCS Study grouping: N/A How were missing data handled? NR Randomisation ratio: N/A Recruitment method: villages in the Mzimba and Dedza districts were selected in consultation with residents after the project was introduced at awareness meetings. Community representatives generated a list of indicators for different levels of food security with project staff, and these were used as part of selection criteria. Participants were interviewed at baseline and asked to be re‐contacted at follow‐up. Sample size justification and outcome used: NR Sampling method: NR for intervention. Control: random (control HHs with similar characteristics to intervention group were randomly selected from nearby villages) Study aim or objective: to examine the impact of a participatory agroecology development project on family farmers' food security and assets following 2 years of intervention. Study period: about 2 years. Baseline: 2012. Follow‐up survey (1000 HHs) June–September 2014. Unit of allocation or exposure: cluster: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: interest in doing farm experiments, food insecurity (determined at baseline using HFIAS and ability to farm (self‐reported) with further probes as to whether the HH had access to land and labour, and were already cultivating crops. Exclusion criteria: NR Pretreatment: agroecological users and non‐users were similar for HH structure, wife's age, husband's age, educational level of both husband and wife, knowledge of agricultural practices, food security and farm size at the baseline level. Significant differences for wealth, HH size, number of crops grown per field, dry season farming and general HH well‐being (see Table 2): non‐adopters were less wealthy, had a larger HH size, grew a lower number of crops and had a lower general HH well‐being. Attrition per relevant group: total 191/1191 (16%) HHs at follow‐up. Per‐group attrition unclear. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: 429 control, 571 intervention (based on MAFFA member) Total number enrolled per relevant group: 408 control, 793 intervention (based on MAFFA member) Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | HFIAS score | |
| Identification |
Sponsorship source: Global Affairs Canada of the Government of Canada, the Canadian Food Grains Bank, and Presbyterian World Service and Development. Sponsors had no role in study design, data analysis and interpretation, writing report, and decision to submit report for publication. Country: Malawi Setting: smallholder farm HHs Author's name: Joseph Kangmennaang Email: jkangmen@uwaterloo.ca Declarations of interest: yes; no conflicts of interest. Study or programme name and acronym: the Malawi Farmer to Farmer Agroecology project (MAFFA). Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Prospective controlled study. No randomisation carried out. |
| Allocation concealment (Selection bias) | High risk | Prospective controlled study. No randomisation carried out. |
| Baseline characteristics similar (Selection bias) | Low risk | Due to differences in baseline characteristics between MAFFA and non‐MAFFA HHs, study authors applied kernel‐based PSM to reduce the effects of confounding and account for any systematic differences in baseline characteristics to enable them to obtain unbiased estimates of the mean treatment effects on the outcomes (Austin 2011). However, the balancing test after weighting revealed no significant differences between participants and non‐participants (see Table 8). |
| Baseline outcome measurements similar (Selection bias) | Low risk | No significant difference between adopters and non‐adopters for HH food security outcome. Difference for wealth. However, (quote) "Due to differences in baseline characteristics between MAFFA and non‐MAFFA HHs, we applied kernel based propensity score matching to reduce the effects of confounding and account for any systematic differences in the baseline characteristics to enable us to obtain unbiased estimates of the average treatment effects on the outcomes (Austin 2011)." |
| Blinding of participants and personnel (Performance bias) | Low risk | Given the prospective longitudinal design of the study, it was not possible to blind participants or personnel; however, it was unlikely that the outcomes of interest (food security and HH wealth) were prone to performance bias. |
| Blinding of outcome assessment (Detection bias) | High risk | NR whether outcome assessors were blinded. Given the design of the study, participants could not be blinded, and it appeared as though outcomes were self‐reported (participants were interviewed and the HFIAS used to assess food security). |
| Protection against contamination (Performance bias) | Unclear risk | Adopters and non‐adopters coexisted in the same villages, and the nature of the intervention was farmers teaching other farmers about agroecology, making contamination likely. However, given that non‐adopters had to actively opt out of intervention, it is unclear to what extent contamination might have occurred. Despite the total number of HHs was smaller at the time of follow‐up, the number of HHs in the control group (based on MAFFA membership) increased. |
| Incomplete outcome data (Attrition bias) | High risk | Attrition was high (16%) in total group and there was no strategy to account for missing values. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | Unclear risk | Potential of recruitment bias. Although inclusion criteria were mentioned, was not clear from these criteria who was included or excluded from the study: (quote) "interest in doing farm experiments, food insecurity (determined at the baseline using the Household Food Insecurity Access Scale (HFIAS), and ability to farm (self‐reported) with further probes as to whether the HH had access to land and labor, and were already cultivating crops." |
Katz 2001.
| Study characteristics | ||
| Methods |
Study design: Prospective controlled study How were missing data handled? women who were LTFU and did not complete the follow‐up questionnaires were excluded from the analysis. Randomisation ratio: N/A Recruitment method: not described but women applied for employment; therefore, we assumed that job adverts were circulated. Sample size justification and outcome used: NR Sampling method: purposive sampling. Women enrolled had applied for part‐time employment in their own or neighbouring communities. Selection was based on results of a reading and writing test, relevant work experience and an interview. Study aim or objective: to evaluate the impact of providing a small income on the HH food expenditures and nutritional status (MUAC) of women employed part‐time in a health project compared to women not employed. Study period: 2 years: February 1993 to January 1995. Unit of allocation or exposure: individuals (women) |
|
| Participants |
Baseline characteristics Intervention or exposure group:
Control
Overall
Inclusion criteria: employees based on the results of a reading and writing test, relevant work experience and an interview. Exclusion criteria: NR Pretreatment: women who were hired were significantly younger than those who were not (25.2 years vs 28.9 years) (table 1). They were more likely to be literate (98.2% vs 81.7%; OR 10.8, 95% CI 4.9 to 28.2), to have ≥ 10 years of formal schooling (23.2% vs 13.2%; OR 2.0, 95% CI 1.3 to 3.0), and to have HH servants (35.4% vs 21.1%; OR 2.0, 95% CI 1.5 to 2.9). They were less likely to smoke (2.4% vs 12.4%; OR 0.54, 95% CI 0.36 to 0.80) and to spend > 4 hours per week fetching firewood (14.9% vs 24.8%; OR 0.17, 95% CI 0.07 to 0.38). Those who were hired and those who were not hired were comparable with respect to caste, HH size, and ownership of animals and other HH goods such as radios, watches, bicycles and furniture. Group differences assessed using t‐test for continuous data and Chi2 test for categorical data. Attrition per relevant group: intervention (employed): 9/350 (2.6%) (7 no longer employed, 2 on leave of absence); control (not employed): 125/520 (24%) (2 dead, 2 moved to hired group, 85 no longer in area, 36 were not at initial addresses) Description of subgroups measured and reported: no subgroups reported Total number completed and analysed per relevant group: 341 employed and 395 not employed used for all baseline and follow‐up outcomes, except changes in MUAC (data for 335 employed and 383 not employed). Total number enrolled per relevant group: intervention: 350; control: 520 Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure: short‐term part‐time employment for women
Control group: no intervention
|
|
| Outcomes | Proportion of HH expenditure on food: weekly food expenditure (NR), food expenditure for different food groups (NR) Anthropometry: MUAC |
|
| Identification |
Sponsorship source: co‐operative agreement No. DAN 0045‐A‐5094 between the office of Nutrition, US Agency for International Development (USAID), the Center for Human Nutrition (CHN), and the Dana Center for Preventive Ophthalmology (DCPO) at Johns Hopkins University. Country: Nepal Setting: rural area of the Sarlahi District Author's name: Joanne Katz Email: NR Declarations of interest: NR Study or programme name and acronym: N/A Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA; therefore, no randomisation was done. |
| Allocation concealment (Selection bias) | High risk | Selection of study participants based on them getting employed. They had to do a reading and writing test, demonstrate relevant work experience and they were interviewed. |
| Baseline characteristics similar (Selection bias) | Low risk | Quote: "The women who were hired were younger and better educated than those who were not hired, but in other respects the two groups of women were similar. After adjustment for these baseline differences, the change in MUAC was not significantly different between the two groups of women." |
| Baseline outcome measurements similar (Selection bias) | Low risk | Quote: "… after adjustment for baseline differences between the two groups of women, the difference between the two groups was not significant. Among those households buying specific foods, the expenditure on each item was comparable for households of women who were hired and households of women who were not hired (table 3)." |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding carried out but it was unlikely that lack of blinding had an effect on the participant's behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding carried out. It is likely that self‐reports of food purchases and expenditures was influenced by knowledge of allocation. MUAC was unlikely to have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | High risk | Quote: "At follow‐up, 36 of the 395 women who had not been employed by the nutrition project (9.1%) reported that they had been employed in jobs for which they were paid some cash. Among the 341 women who had been employed by the project, 106 (31.1%) reported additional cash employment (the project employment was part‐time). However, the amount of cash payments associated with these additional activities was not determined." |
| Incomplete outcome data (Attrition bias) | High risk | Very different proportion of attrition between the groups: 2.6% for women who were hired compared to 24% among women who were not hired. Missing data were excluded from the analysis and information from those in the control group could have an effect on the outcomes. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. Authors stated in the methods that they would conduct baseline comparisons and conduct an assessment of the impact of employment (changes in expenditure and in MUAC) by fitting a linear regression model that adjusts for baseline differences. There was evidence that authors did these analyses. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unclear. Measurement of MUAC or food expenditure is not very well described. |
Kennedy 1989.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? 462/504 HHs remained at follow‐up. Report relied on a longitudinal analysis, the data presented were based primarily on the cohort sample. Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: NR Sampling method: Sony (The South Nyanza Sugar Factory) provided a list of all farmers in the outgrowers' scheme. From this list, a random sample of sugar farmers, weighted by sublocation, was chosen. Once the sample of sugar farmers was chosen, field staff identified the next nearest non‐sugar farmers who met the same selection criteria. Study aim or objective: to evaluate the effects of cash crop production on agricultural production, income and food consumption, and to assess the impact of cash cropping on the health and nutritional status of preschool children and women. Study period: baseline: June 1984 to March 1985; follow‐up: December 1985 to March 1987 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure group: cash cropping sugarcane
Control group: no intervention
Overall: NR Inclusion criteria: HHs had to have ≥ 1 preschool child; ≥ 1 resident farmer; and own < 20 hectares of land. Exclusion criteria: NR Pretreatment: Sugar farmers have a higher mean nominal income per capita than non‐sugar farmers and higher marketed agricultural income per capita than all other groups. Attrition per relevant group: attrition of the total HHs was 8.3% (42/504) from baseline: no clear attrition present in the sugar farmers subgroup (139 at baseline and 146 at follow‐up); 35.7% (15/42) of new entrants attrited; and 11.3% (26/231) of non‐sugar farmers attrited. Attrition of women was 37.6% (298/793), but 529 new women entered the sample. Attrition of preschool children was 34.9% (409/1171), but 535 new preschool children entered into/were born into the sample. Preschool children from 356 sugar farmer HHs, 90 from new entrant HHs, and 556 from non‐sugar farmer HHs provided anthropometric data at baseline; with 243 sugar farmer HHs, 61 from new entrant HHs and 349 non‐sugar farmer HHs providing data at follow‐up. Description of subgroups measured and reported: 1677 preschool children and 1343 women. Intervention HHs were split into 'sugar farmers' who had completed ≥ 1 harvest at baseline and 'new entrants' who were farming with sugar, but had not completed a harvest (and had consequently not been paid). Total number completed and analysed per relevant group: 146 sugar farmer and 27 new entrant HHs completed the study, along with 205 HHs of non‐sugar farmers. 1024 women and 1297 preschool children completed the study – no per group numbers are available. Total number enrolled per relevant group: 139 sugar farmer and 42 new entrant HHs were enrolled at baseline, as well as 231 HHs of non‐sugar farmers. Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure group: cash cropping sugarcane
Control group: no intervention |
|
| Outcomes | Proportion of HH budget spent on food; food expenditure for different food groups/items; total per capita food expenditure in previous 7 days Adequacy of dietary intake: percentage of HHs with caloric deficiency; caloric adequacy of preschool children Anthropometry: WAZ; underweight; HAZ; stunted; WHZ; wasting; women weight; adult BMI Morbidity: illness of women and children (all‐cause and diarrhoea) |
|
| Identification |
Sponsorship source: IFPRI received support as a constituent of the Consultative Group on International Agricultural Research from a number of donors including Australia, Belgium, Canada, the People's Republic of China, the Ford Foundation, France, the Federal Republic of Germany, India, Italy, Japan, the Netherlands, Norway, the Philippines, the Rockefeller Foundation, Switzerland, the UK, the US, and the World Bank. In addition, a number of other governments and institutions contribute funding to special research projects. Country: Kenya Setting: smallholder farm HHs Author's name: Eileen Kennedy Email: eileen.kennedy@tufts.edu Declarations of interest: NR Study or programme name and acronym: smallholder sugarcane outgrowers' scheme Type of record: research report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Cohort study and there was no randomisation performed. |
| Allocation concealment (Selection bias) | High risk | Cohort study and no allocation concealment was done. |
| Baseline characteristics similar (Selection bias) | Low risk | HHs of sugar farmers had significantly higher (P < 0.05) incomes than non‐sugar farmer HHs, as well as significantly higher (P = 0.05) marketed agricultural income per capita than all other groups. However, the main comparison was between 'new entrants' and 'sugar farmers', between which there were no major differences. |
| Baseline outcome measurements similar (Selection bias) | Low risk | No baseline outcome measurements were significantly different. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants were not blinded, but it was unlikely that the lack of blinding could have resulted in performance bias given the outcomes. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether outcome assessors were blinded to allocation. Outcomes were subjective/self‐reported and could have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | NR, but it was unlikely that the control group received the intervention due to the nature of the intervention. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Attrition was considerable for new entrants and non‐sugar farmers, and no information on differential attrition was provided. It was also difficult to assess the impact of attrition as more HHs were included at follow‐up. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available, but all a priori stated outcomes were reported on. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: high. Some of the outcomes relied on participants having to recall information for several days or weeks. |
Kurdi 2019.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: N/A How were missing data handled? A conservative ITT approach was taken for determining impact estimates. 6 HHs, which had identification matching problems at follow‐up, were dropped entirely from analysis. Randomisation ratio: 1:1. Data for the evaluation came from a HH survey of 2000 HHs with indirect relatives of Social Welfare Fund beneficiaries in the 3 targeted districts in Al Hodeidah, half of which were in communities where indirect relatives were included in the programme (treated) and half of which were in communities where they were not included (control). (Kurdi 2019 policy brief) Recruitment method: programme targeted the poorest and the most vulnerable HHs in the country by restricting recipients to Social Welfare Fund beneficiary HHs in 3 eligible districts in Al Hodeidah governorate: Marawi'ah, Bayt Al Faqiah and Zabid (Kurdi 2019, Introduction – Program description). Beneficiaries were divided into 2 separate priority groups. Women in the pilot districts who were direct family members of Social Welfare Fund beneficiaries were in the first priority group and were automatically included in the Cash for Nutrition programme (received the intervention). Indirect family members, such as daughters‐in‐law, of Social Welfare Fund beneficiaries were added to a second priority list. Because the programme was not large enough to include all of these second priority women, inclusion of these indirect family member beneficiaries was randomised at the community level (Kurdi 2019, Sample and Methodology – Randomization). The primary survey respondent was the woman identified as a second‐priority potential beneficiary by the programme, which meant that all respondents were pregnant or mothers of children aged < 2 at the time of the baseline survey (Kurdi 2019, Sample and Methodology – Survey). Manner in which HHs were approached and invited to participate NR. Sample size justification and outcome used: NR Sampling method: purposive sampling. Programme targeted the poorest and the most vulnerable HHs in the country by restricting recipients to Social Welfare Fund beneficiary HHs (Kurdi 2019, Introduction). Because the pilot programme was limited to 4800 beneficiaries, Social Welfare Fund beneficiaries were divided into 2 separate priority groups. Women in the pilot districts who were direct family members of Social Welfare Fund beneficiaries were in the first priority group and were automatically included in the Cash for Nutrition programme (received intervention). Indirect family members, such as daughters‐in‐law, of Social Welfare Fund beneficiaries were added to a second priority list. Because the programme was not large enough to include all of these second priority women, inclusion of these indirect family member beneficiaries was randomised at the community level (Kurdi 2019, Sample and methodology – Randomization). The cRCT population consisted of the HHs of these women on the 'second priority list.' Study aim or objective: to measure the impact of the Cash for Nutrition programme on eligible HHs; to describe the degree to which HH characteristics, details of programme implementation and the external environment increased or decreased programme impact; and to describe the functioning of the programme and changes in HH welfare in the current conflict environment. Study period: December 2014 to August 2017 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Cash for Nutrition Intervention
Control
Overall: NR Inclusion criteria: for cRCT (not overall Cash for Nutrition programme): residents in 1 of the 3 targeted districts in Al Hodeidah (Marawi'ah, Bayt Al Faqiah or Zabid); mothers of children aged < 2 years and pregnant women; indirect relatives of Social Welfare Fund beneficiaries Exclusion criteria: NR Pretreatment: intervention HHs had a lower Asset Index mean than control HHs; fewer intervention HHs owned TVs and washing machines compared to controls; and more mothers in intervention HHs were illiterate compared to mothers in control HHs. Attrition per relevant group: at baseline, communities that included indirect relatives of Social Welfare Fund beneficiaries were randomly assigned to the intervention (95 communities, 1001 HHs) or control (95 communities, 999 HHs) groups. The randomisation only applied to HHs of INDIRECT relatives of Social Welfare Fund beneficiaries – DIRECT relatives all received the intervention, and were not included in the impact analysis. In the intervention group, 935 HHs in 95 communities were resurveyed at follow‐up (attrition rates: HHs 6.59%, community 0.0%). In the control group, 915 HHs in 93 communities were resurveyed at follow‐up (attrition rates: HHs 8.41%, communities 2.1%). Total HH attrition rate was 7.5%, slightly higher among the treatment sample, but not significantly different between treatment and control (Kurdi 2019, Sample and Methodology – Sample size and attrition). Description of subgroups measured and reported: heterogeneity of impacts for baseline HH wealth, baseline sources of information, women's position in the HH, women's educational level. Total number completed and analysed per relevant group: with replacement HHs at follow‐up: 935/1001 (93.4%) intervention HHs; 915/999 (91.6%) control HHs. Without replacement HHs at follow‐up: 898/1001 (89.7%) intervention HHs; 857/999 (85.8%) control HHs (communities: 95/95 (100.0%) intervention communities; 93/95 (97.9%) control communities). Total number enrolled per relevant group: 1001 women from intervention HHs (in 95 communities) and 999 women from control HHs (in 95 communities). Total number randomised per relevant group: number of HHs randomised (indirect family members of Social Welfare fund beneficiaries): 2000; intervention group: 1001 HHs in 95 communities; control group: 999 HHs in 95 communities |
|
| Interventions |
Intervention characteristics Cash for Nutrition intervention
Control: no intervention
|
|
| Outcomes | Diet diversity: HDDS (0–12) WHZ; HAZ |
|
| Identification |
Sponsorship source: managed by the World Bank and funded by the Nordic Trust Fund. Data collection funded by World Bank and United Nations Development Programme. Country: Yemen Setting: poor and vulnerable HHs in 3 eligible districts in Al Hodeidah governorate: Marawi'ah, Bayt Al Faqiah and Zabid (Kurdi 2019, Introduction). Comments: N/A Author's name: Sikandra Kurdi Institution: N/A Email: s.kurdi@cgiar.org; ifpri@cgiar.org Address: N/A Declarations of interest: NR Study or programme name and acronym: Cash for Nutrition programme Type of record: impact evaluation report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Reported that communities were randomised to either the intervention or control groups, but the method was not specified. |
| Allocation concealment (Selection bias) | High risk | Allocation of communities of HHs to intervention and control groups was done for indirect family members of Social Welfare Fund beneficiaries. However, direct beneficiaries in all the communities all received the intervention. Therefore, it was not possible (and there does not seem to have been attempts made) to conceal group allocation. |
| Baseline characteristics similar (Selection bias) | High risk | Intervention HHs had significantly lower Asset Indices (P = 0.001), and owned significantly fewer televisions (P < 0.01) and washing machines (P = 0.007). Intervention HHs also had a significantly higher percentage of illiterate mothers (P < 0.001). |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | No formal hypotheses to test baseline outcome values reported. |
| Blinding of participants and personnel (Performance bias) | Low risk | Given the nature of the study design, it was unlikely that blinding of participants and training volunteers was possible. Some outcomes, such as health and nutrition behaviour and spending on food, may have been prone to performance bias. It was not clear, however, whether participants and volunteers were aware that the survey was recording their behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | It is NR whether people administering the survey and taking anthropometric measurements were blinded to assignment. It is also unclear whether participants, the outcome assessors for self‐reported measures, were blinded. |
| Protection against contamination (Performance bias) | High risk | The authors reported high levels of contamination. During the survey, 16% of intervention HHs reported not receiving the transfer at baseline and 7% at follow‐up. 23% of control HHs reported receiving the cash transfer at baseline and 24% follow‐up. It is not clear how large the role of contamination was for non‐recipient HHs located close to recipient HHs in the same communities. |
| Incomplete outcome data (Attrition bias) | High risk | Attrition 7.5% overall and fairly balanced across intervention (6.59%) and control groups (8.41%). The use of replacement HHs for those who could not be resurveyed at follow‐up is reported, but it was assumed that these HHs are in addition to those HHs 're surveyed at follow‐up'. However, 2 entire control clusters were lost. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available for review |
| Other bias | Low risk | Incorrect analysis: low risk for SEs for model coefficients clustered at community level; recruitment bias: low risk for recruitment prior to randomisation. |
Kusuma 2017a.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? No missing data reported Randomisation ratio: 1:1 Recruitment method: NR Sample size justification and outcome used: NR Sampling method: First, within each province, the 20% richest districts were excluded for both programmes (based on school transition rates, malnutrition and poverty). Districts who participated in the Kecamatan Development Project (a governmental poverty programme that developed infrastructure and capacity) were eligible for Generasi, from which 20 were selected and stratified by province. In NTT, East Java, and West Java selection was random, in Gorontalo and North Sulawesi all eligible districts were selected. Within the selected districts, subdistricts were not eligible if they had participated in the UPP or where < 30% of the villages (desa) and urban precincts (kelurahan) were considered as rural by the national statistics office. The final screening yielded 300 PNPM Generasi eligible subdistricts. The remaining districts were considered for PKH. The subdistricts that were deemed as 'supply‐side ready' were then randomly assigned to the PKH treatment and control groups. Study aim or objective: Kusuma 2016: to provide evidence on the effects of HH cash transfers (PKH) and community cash transfers (Generasi) on determinants of maternal mortality. Kusuma 2017: to provide evidence on the impact of HH cash transfers (PKH) and community cash transfers (Generasi) on children's food consumption. Study period: from June–August 2007 to October–January 2010 Unit of allocation or exposure: subdistricts |
|
| Participants |
Baseline characteristics Intervention: NR Control
Overall: NR Inclusion criteria: very poor HHs (UCT database) with pregnant/lactating women, children aged 0–15 years in supply‐ready urban subdistricts (based on existing health and education facilities). Exclusion criteria: NR Pretreatment: for PKH there were more girls in the intervention group (P < 0.05). However, the study authors did not report any other differences for a number of maternal, HH and subdistrict characteristics at baseline between the intervention and control groups within each programme. Attrition per relevant group: the PKH children sample can be considered without attrition because it was 1394 at follow‐up out of 1395 at baseline. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: 1394 children, 1376 HHs in total. Total number enrolled per relevant group: Kusuma 2017 used subsets of data from HHs that participated in PKH and Generasi and reported on food consumption for children aged 24–36 months: 1395 HHs at baseline. Total number randomised per relevant group: 360 subdistricts (Intervention group: 180 subdistricts; control group: 180 subdistricts) |
|
| Interventions |
Intervention characteristics
Control characteristics: no intervention |
|
| Outcomes | Anthropometry: underweight (WAZ < –2SD); severe underweight (WAZ < –3SD); wasting (WHZ < –2SD); severe wasting (WHZ < –3SD); stunting (HAZ < –2SD); severe stunting (HAZ < –3SD) | |
| Identification |
Sponsorship source: research fellowship from the Harvard Kennedy School Indonesia Program. Country: Indonesia Setting: urban very poor HHs (PKH) and rural very poor HHs (Generasi) in West Java, East Java, North Sulawesi, Gorontalo, and East Nusa Tenggara provinces Author's name: Dian Kusuma Email: dkusuma@mail.harvard.edu Declarations of interest: none declared. Study or programme name and acronym: Program Keluarga Harapan (PKH) and Generasi. Type of record: journal articles |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Random sequence generation method NR. |
| Allocation concealment (Selection bias) | Unclear risk | Allocation concealment methods NR |
| Baseline characteristics similar (Selection bias) | Low risk | No important differences between groups reported at baseline. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Although food consumption was similar at baseline, growth outcomes at baseline were NR |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding of participants and personnel was not possible but unlikely to influence intervention received. |
| Blinding of outcome assessment (Detection bias) | Low risk | Unclear whether outcome assessors were blinded but key outcomes were objective and unlikely to be influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Allocation was at subdistrict level, which minimised the risk of spillovers. |
| Incomplete outcome data (Attrition bias) | Low risk | No attrition was reported. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Protocol N/A. |
| Other bias | Unclear risk | Misclassification of exposure: low risk. Measurement bias: unclear risk. Incorrect analysis: low risk. analyses adjust for clustering. Recruitment bias: low risk. HHs randomly selected after subdistrict randomisation. |
Kusuma 2017b.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? No missing data reported Randomisation ratio: 1:1:1. Recruitment method: NR Sample size justification and outcome used: NR Sampling method: first, within each province, the 20% richest districts were excluded for both programmes (based on school transition rates, malnutrition and poverty). Districts who participated in the Kecamatan Development Project (a governmental poverty programme that developed infrastructure and capacity) were eligible for Generasi, from which 20 were selected and stratified by province. In NTT, East Java, and West Java selection was random, in Gorontalo and North Sulawesi all eligible districts were selected. Within the selected districts, subdistricts were not eligible if they had participated in the UPP or where < 30% of the villages (desa) and urban precincts (kelurahan) were considered as rural by the national statistics office. The final screening yielded 300 PNPM Generasi eligible subdistricts, which were randomly assigned to incentivised treatment (hereafter referred to as treatment I), non‐incentivised treatment (hereafter treatment II) and the control group. The remaining districts were considered for PKH. The subdistricts that were deemed as 'supply‐side ready' were then randomly assigned to the PKH treatment and control groups. Study aim or objective: Kusuma 2016: to provide evidence on the effects of HH cash transfers (PKH) and community cash transfers (Generasi) on determinants of maternal mortality. Kusuma 2017: to provide evidence on the impact of HH cash transfers (PKH) and community cash transfers (Generasi) on children's food consumption. Study period: from June–August 2007 to October 2009 to January 2010 Unit of allocation or exposure: subdistricts |
|
| Participants |
Baseline characteristics Intervention: NR Control
Overall: NR Inclusion criteria: very poor HHs (UCT database) with pregnant/lactating women, children aged 0–15 years in rural villages. Exclusion criteria: NR Pretreatment: no baseline differences reported. Attrition per relevant group: 2 independent cross‐sectional samples analysed. Overall attrition: 98/4262 (2.3%). Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: 1481 children, 1472 HHs in total (2 cross‐sectional samples; 1 for baseline and 1 at follow‐up). Total number enrolled per relevant group: Kusuma 2017 used subsets of data from HHs that participated in PKH and Generasi and reported on food consumption for children aged 24–36 months: 4262 HHs. Kusuma 2016 used subsets of data from HHs that participated in Generasi and had married women aged 16–49 who had had pregnancies or deliveries within the past 24 months in 2007 and 2009: 4262 women at baseline Total number randomised per relevant group: 300 subdistricts (Intervention group (Versi A – with rewards): 100 subdistricts; intervention group (Versi B – without rewards): 100 subdistricts; control group: 100 subdistricts). Results for Generasi Versi A and B are presented together. |
|
| Interventions |
Intervention characteristics
Control: no intervention |
|
| Outcomes | Anthropometry: underweight (WAZ < –2SD); severe underweight (WAZ < –3SD); wasting (WHZ < –2SD); severe wasting (WHZ < –3SD); stunting (HAZ < -2SD); severe stunting (HAZ < –3SD) | |
| Identification |
Sponsorship source: research fellowship from the Harvard Kennedy School Indonesia Program. Country: Indonesia Setting: urban very poor HHs (PKH) and rural very poor HHs (Generasi) in West Java, East Java, North Sulawesi, Gorontalo, and East Nusa Tenggara provinces Author's name: Dian Kusuma Email: dkusuma@mail.harvard.edu Declarations of interest: none declared. Study or programme name and acronym: Program Keluarga Harapan (PKH) and Generasi. Type of record: journal articles |
|
| Notes | The Generasi programme is reported in the same papers that report PKH programme, a CCT to HHs programme. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Study authors referred to randomisation of subdistricts but did not describe how randomisation sequence was generated. |
| Allocation concealment (Selection bias) | Unclear risk | Allocation concealment NR. |
| Baseline characteristics similar (Selection bias) | Low risk | No important differences reported in terms of maternal, HH and subdistrict characteristics between groups at baseline. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Food consumption in children was similar at baseline; however, important growth outcomes were NR at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding of participants and personnel in these types of studies was not possible, but lack of blinding was unlikely to influence intervention received. |
| Blinding of outcome assessment (Detection bias) | Low risk | Unclear whether outcome assessors were blinded. However, key anthropometric outcomes were objective and thus less susceptible to lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Randomisation was at subdistrict level which reduces spillover effect risk. |
| Incomplete outcome data (Attrition bias) | Low risk | 2 independent cross‐sectional surveys conducted. Response rate was high. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. |
| Other bias | Unclear risk | Misclassification of exposure: low risk. Measurement bias: unclear risk. Incorrect analysis: low risk. analyses adjust for clustering. Recruitment bias: low risk. HHs randomly selected after subdistrict randomisation. |
Leroy 2008 (PROGRESA).
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? children LTFU or with missing data were excluded from the analysis. Randomisation ratio: N/A Recruitment method: mass media advertised the programme and invited families to solicit a socioeconomic screening questionnaire at the enrolment centres. Assessment utilised HH assets, housing quality, years of education and HH composition. Programme staff visited all HHs that appeared eligible to validate the results of the screening questionnaire. Eligible applicants subsequently had to return to the programme office to register. HH enrolment in urban areas started in 2002 and was staged over 2 years. Sample size justification and outcome used: NR Sampling method: For the evaluation sample, 149 manzanas (the smallest administrative unit within an urban area) in 17 of Mexico's 31 states were selected through probabilistic stratified sampling from the pool of localities where Oportunidades would be implemented in 2002. The localities were selected based on density of low‐income HHs. The survey included eligible HH that enrolled and eligible HHs that did not enrol in the programme. Study aim or objective: to evaluate the impact of Mexico's CCT programme, Oportunidades, on the growth of children aged 24 months living in urban areas. Study period: 2 years (baseline: 2002; follow‐up: 2004) Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: poorest HHs in an urban block in urban centres (based on a cut‐off of the national HH Income and Expenditure Survey). None other reported. Exclusion criteria: NR Pretreatment: baseline characteristics did not differ between treatment and comparison HHs. However, the propensity score was substantially higher in intervention HHs (P < 0.05). The score was based on SE variables and likelihood of enrolment. Attrition per relevant group: total: 301/733 (41.1%) children (263 LTFU and 38 with missing data); intervention: 230/574 (40.1%) children (202 LTFU and 28 with missing data); control: 71/159 (44.7%) children (61 LTFU and 10 with missing data). Description of subgroups measured and reported: age of child at baseline: 0–6 months; 6–12 months and 12–24 months. Socioeconomic tertile at baseline: tertile 1, 2 and 3. Total number completed and analysed per relevant group: intervention group (HHs who enrolled in the programme): 344 children; control group (HHs who did not enrol in the programme): 88 children Total number enrolled per relevant group: total: 733 HHs; intervention: 574 children; control: 159 children Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Anthropometry: height; weight; HAZ, WHZ | |
| Identification |
Sponsorship source: National Coordination of the Oportunidades programme of the Mexican secretary of Social Development Country: Mexico Setting: urban poor HHs participating in a national anti‐poverty programme Authors' names: Lynnette M Neufeld; first author: Jef L Leroy Email: neufeld@insp.mx Declarations of interest: no conflicts of interest Study or programme name and acronym: PROGRESA/Oportunidades Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA; no randomisation done. |
| Allocation concealment (Selection bias) | High risk | CBA; no randomisation done. By excluding 26% of all HHs surveyed, this could have introduced other forms of bias in their sample. Study authors did not compare these HHs to included HHs. |
| Baseline characteristics similar (Selection bias) | Low risk | Although intervention HHs had a higher baseline mean propensity score (probability of enrolment in the Oportunidades programme) than those in the control group, the study authors used PSM to compare changes in HHs in both groups during their analysis. |
| Baseline outcome measurements similar (Selection bias) | Low risk | The anthropometric parameters of the children at baseline did not differ. The study authors also adjusted for baseline child anthropometric measurements and maternal height in their analyses. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding not possible but lack of blinding unlikely to influence participant or personnel behaviour. |
| Blinding of outcome assessment (Detection bias) | Low risk | Blinding of outcome assessors NR. However, outcomes of interest (anthropometric measures) were objective and unlikely to have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Eligible HHs were enrolled in the programme and control HHs were eligible HHs that did not enrol in the programme. Therefore, it was not possible for control HHs to receive any programme benefits. |
| Incomplete outcome data (Attrition bias) | High risk | High levels of missing data overall (41%) and in intervention (40.1%) and control (44.7%) groups. Although for most HHs reasons for LTFU were because of moving to another area, this information was only available for some of these HHs (91/263). Furthermore, by excluding 26% of all HHs surveyed this could have introduced other forms of bias in their sample. The study authors did not compare these HHs to included HHs. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | Low risk | Misclassification bias: low risk. The study authors only used data from included HHs that were consistently classified as either intervention or control HHs. Measurement bias: low risk. Incorrect analysis: N/A. Seasonality bias: unknown risk (time of year not stated). |
Lopez Arana 2016.
| Study characteristics | ||
| Methods |
Study design: CBA How were missing data handled? Children's study (secondary analysis): children with missing covariates at baseline as well as children LTFU were excluded from the analysis. Analysis of differential attrition was done for children LTFU (Lopez‐Arana 2016); Women's study (secondary analysis): ITT analysis was according to HH allocation, but women with missing covariates as well as those LTFU were excluded from the analysis. Analysis of differential attrition was done for women LTFU (Forde 2012). Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: NR Sampling method: stratified sample. 57 municipalities were randomly selected from 622 municipalities (with < 100,000 inhabitants) implementing FA (classified into 25 strata based on routine government data on region, health/education structure, population). Intervention municipalities were matched with 65 control municipalities from the same stratum. Of the eligible HHs within each municipality, 100 HHs were randomly sampled. Study aim or objective: to evaluate the impact of the FA programme on under‐ and overnutrition of children as well as the BMI of women from poor HHs in Colombia. Study period: June 2002–2006. Unit of allocation or exposure: municipalities |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: families living in a municipality where the intervention (FA) was implemented were required to 1. hold a Colombian citizen card, 2. have children aged < 18 years and 3. be classified in the lowest level of the official socioeconomic classification in December 1999. Exclusion criteria: none reported for IFS report summary (Attanasio 2005) or children's study (secondary analysis) (Lopez‐Arana 2016). Women's study (secondary analysis): women who were underweight (BMI 18.5 kg/m2) at baseline; women who were pregnant or breastfeeding at any point during the study (Forde 2012). Pretreatment: in the children's study more children in the control group were participating in the Hogares Comunitarios programme. Control HHs were also less likely to have a mother with no education or be in an un urbanised (rural) area. In the women's study women in the treatment group were more likely to be slightly older and participate in community activities. Treatment HHs also had less persons per room, less piped water to the HH, and were less likely to be in an urban location; while control HHs had lower HH wealth. Treatment areas had larger populations, more intervention‐eligible families, slightly higher average HH wealth, and many more banks; while control areas a higher quality of life index, ratio of doctors to population, and proportion of HHs with piped water. Attrition per relevant group: Attanasio 2006: attrition was 6% overall at the first follow‐up. Lopez‐Arana 2016: children's study (secondary analysis): attrition was 39.2% (833/2123) in the intervention group and 41.8% (1138/2722) in the control group, with no differential LTFU reported between the 2 groups. Forde 2012: women's study (secondary analysis): attrition was 38.8% (785/2023) in the intervention group and 38.0% (512/1347) in the control group with no differential LTFU reported between the 2 groups (Chi2 = 0.21, P = 0.64). Description of subgroups measured and reported: women's study (secondary analysis): subgroup analysis excluding women in pre‐exposed areas (26 municipalities). Total number completed and analysed per relevant group: Attanasio 2006: unclear. Forde 2012: women's study (secondary analysis): intervention group: 1238 women from 57 municipalities; control group: 835 women from 65 municipalities. Lopez‐Arana 2016: children's study (secondary analysis): intervention group: 1290 children (aged 7 years) from 31 municipalities; control group: 1584 children (aged 7 years) from 65 municipalities. Total number enrolled per relevant group: Attanasio 2006: intervention group: 6293 HHs from 57 municipalities (2954 TSP HHs from 31 municipalities and 3339 TCP HHs from 26 municipalities); control group: 4424 HHs from 65 municipalities Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention
|
|
| Outcomes | Diet diversity: DDI Anthropometry: HAZ, stunting, BMIZ, thinness Adverse events: overweight, obesity |
|
| Identification |
Sponsorship source: IFS report summary: NR; children's study: (quote) "S. L.‐A. was supported by the European Union Erasmus Mundus Partnerships programme Erasmus‐Colombus (ERACOL) and Fundación para el Futuro de Colombia (COLFUTURO) at Erasmus MC in the Netherlands. M.A. was supported by the European Research Council (ERC) (grant no. 2636840), the National Institute on Ageing (award numbers R01AG040248 and R01AG037398), and the LIFEPATH project funded by the European Union's Horizon2020 research and innovation programme under grant agreement 633666. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript."; women's study: (quote) "IF is funded by a Medical Research Council Fellowship which mandates open access publishing (grant code G0701333). In 2001, a partnership between the Institute of Fiscal Studies (London, a research institute), Econometria (Bogotá, a research institute) and SEI (Bogotá, a company specialising in the design and collection of social surveys) was commissioned by the Colombian Government to evaluate Familias, after open tendering." Country: Colombia Setting: very poor rural and urban HHs Authors' names: Sandra Lopez‐Arana; Ian Forde; Orazia Attanasio Email: o.attanasio@ucl.ac.uk; s.lopezarana@erasmusmc.nl; i.forde@ucl.ac.uk Declarations of interest: Attanasio 2006: No. Forde 2012: Yes. "All authors have completed the Unified Competing Interest form and declare no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work." Lopez‐Arana 2016: Yes. "The authors declare that no conflicts of interest exist." Study or programme name and acronym: Familias en Acción (FA) Type of record: Centre for the Evaluation of Development Policies: Institute for Fiscal Studies report summary; journal articles (Attanasio 2006; Forde 2012; Lopez‐Arana 2016) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Prospective controlled study. No randomisation carried out. |
| Allocation concealment (Selection bias) | High risk | Prospective controlled study. No randomisation carried out. |
| Baseline characteristics similar (Selection bias) | Low risk | Baseline non‐equivalence was detected for a number of pertinent characteristics: children's participation in the Hogares Comunitarios programme (P = 0.01) in the control group; while control children were significantly less likely to have mothers with no education (P = 0.006) or come from rural areas (P = 0.002). Women in the treatment group were older (P < 0.01), while control women came from significantly less wealthy (P < 0.001) HHs which were more likely to be in semi‐urban areas (P < 0.001). However, the study authors adjusted for covariates at the individual, HH and municipality level in the regression analyses. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Study authors stated that the higher level of food consumption in TCP HHs was an early effect of the intervention (26 municipalities who received the intervention before the baseline survey was conducted). The true baseline comparability in terms of food consumption across the intervention municipalities was, therefore, unknown (Attanasio 2006). |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding as this was a CBA. Unclear if this lack of blinding and the awareness of follow‐up surveys would have resulted in a temporary performance bias in terms of the volume and quality of food purchased; which may have affected anthropometric outcomes. |
| Blinding of outcome assessment (Detection bias) | Low risk | Unclear whether the field workers were blinded but outcomes were objective and unlikely to have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Unclear risk | Study authors provided no information on the geographical location of intervention vs control municipalities. |
| Incomplete outcome data (Attrition bias) | High risk | The secondary analysis by Forde 2012 reported high attrition among women (38.8% vs 38%). Women who were LTFU were older (P = 0.01), with lower formal educational attainment (P = 0.01) and greater parity (P < 0.001) compared to those with complete data. The secondary analysis by Lopez‐Arana 2016 also reported high attrition (39.2% vs 41.8%) in children. Children who were LTFU were older (P < 0.0001), less likely to be overweight (P = 0.02) and had lower BMIZ (P = 0.001). |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study protocol N/A. |
| Other bias | Unclear risk | Misclassification bias: high. Information on receipt of cash transfer was self‐reported by HHs. Measurement bias: unlikely. |
Macours 2012.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel How were missing data handled? N/A Randomisation ratio: about 1:1 Recruitment method: municipalities selected for their extreme levels of poverty and because they had been affected by a severe drought in previous year. Sample size justification and outcome used: NR Sampling method: in communities randomly selected to participate in the Atención a Crisis programme, the primary child carer (known as the 'titular'), mainly a woman, was invited to a registration assembly where the programme objectives and various components were explained. At the end of assembly, a lottery took place in each community. Participation in the assemblies and lotteries was close to 100%. Based on lottery, all eligible HHs within each community were assigned to 1 of 3 treatments. Study aim or objective: to analyse the impact of a cash transfer programme on early childhood cognitive development and the extent to which changes in child development could be explained solely by the cash component of the Atención a Crisis programme. Study period: Atención a Crisis pilot programme was implemented between November 2005 and December 2006, Baseline data for the evaluation collected in April–May 2005. A first follow‐up survey collected in July–August 2006, 9 months after the HHs had started receiving payments. A second follow‐up survey, covering the same HHs, was collected between August 2008 and May 2009. Unit of allocation or exposure: HHs, stratified by community |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: baseline data on HH assets and HH composition were then used to define programme eligibility. The eligibility criteria were determined using the proxy means methodology developed for the RPS and based on the national HH data from 2001 (EMNV). Additional discussions with local leaders from each intervention community were conducted to identify possible exclusion or inclusion errors. Based on the discussions with leaders, 3.7% of all the HHs considered were re‐assigned from non‐eligible to eligible, and 3.7% from eligible to non‐eligible. To avoid any possible selection bias resulting from the re‐assignment by the leaders, the results they presented use eligibility by the proxy means as the ITT (without taking into account the reclassification by the community leaders). Exclusion criteria: NR Pretreatment: children aged 0–5 years in the intervention group at baseline were significantly more underweight and received fewer vitamins and deworming drugs in the previous 6 months when compared to those in the control group. Also, in the control compared to the intervention group, HHs had more members aged ≥ 65 years. Attrition per relevant group: attrition over the study period was minimal, < 1.3% in 2006 and 2.4% in 2008. Attrition is uncorrelated with treatment status, and does not differ across treatment packages. The low attrition rates were a result of repeat visits to recover temporary absence and extensive tracking of migrants. Migrant HHs and children were interviewed and tested in their new locations. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: overall: 3326 in 2006 and 4245 in 2008. Numbers of participants per group N/A. Total number enrolled per relevant group: NR Total number randomised per relevant group: NR |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food: % of food in total expenditure; % staple/animal protein/fruit and vegetables in total food expenditure Anthropometry: WAZ; HAZ Anxiety and depression: depression score (CES‐D scale); Cognitive function and development: language test score (TVIP score) Morbidity: number of days ill in bed in past month |
|
| Identification |
Sponsorship source: World Bank support including the Trust Fund for Environmentally and Socially Sustainable Development (TFESSD) made available by the governments of Finland and Norway, the Bank‐Netherlands Partnership Trust Fund Program (BNPP), as well as the Research Committee through a Research Support Budget (RSB) grant. Funding from BASIS was also received under the USAID Agreement No. EDH‐A‐ 00‐06‐0003‐00 awarded to the Assets and Market Access Collaborative Research Support Program. Country: Nicaragua Setting: poor HHs in 6 municipalities of rural Nicaragua Author's name: Karen Macours Email: karen.macours@parisschoolofeconomics.eu Declarations of interest: NR Study or programme name and acronym: Atención a Crisis Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "These households were allocated one of three different packages through a participatory lottery." |
| Allocation concealment (Selection bias) | Low risk | Allocation at community level, and it performed on all units at start of study. |
| Baseline characteristics similar (Selection bias) | Low risk | Some small differences noted at baseline, but regressions were used to adjust for differences between treated and control groups (page 258). |
| Baseline outcome measurements similar (Selection bias) | Low risk | There were significant differences between the groups at baseline (the WHZ was higher in the control group) but these were controlled for in the analysis. |
| Blinding of participants and personnel (Performance bias) | Low risk | It is difficult to blind in these types of interventions, but lack of blinding is unlikely to influence participants or personnel behaviour during a trial of this nature. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether the data collectors were blinded towards the group allocations, which may have influenced the measurement of outcomes across groups as these were self‐reported. |
| Protection against contamination (Performance bias) | Low risk | Geographical communities were the unit of allocation. Therefore, it is unlikely that there was a spillover effect of the intervention. |
| Incomplete outcome data (Attrition bias) | Low risk | Quote: "Attrition over the study period was minimal, less than 1.3 percent in 2006 and 2.4 percent in 2008." |
| Selective outcome reporting (Reporting bias) | Unclear risk | Protocol or trial registration number NR. Specific outcomes were not specified in the article's Methods section. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unclear risk. Unclear how food intake data were collected. Incorrect analysis: low risk. SEs adjusted for clustering at the community level. |
Maluccio 2005.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? 90% (1581) of the stratified random sample was interviewed in the first round. In 2002, just over 90% of these were re‐interviewed. The sample for which there is a complete set of observations (1 in each of the 3 survey rounds) was 1396, smaller than the 1434 shown in the first row of the third column of Table 3. The HHs were about evenly divided between intervention and control groups, indicating that at least the level of attrition was not significantly different between them. Similarly, when the sample was limited to those interviewed in all 3 rounds as a partial control for attrition bias, estimated effects changed only slightly, with no systematic bias. Another partial remedy to control for attrition bias is to estimate a HH fixed‐effects model, particularly if one suspects that unobserved persistent heterogeneity is leading to attrition. However, as with the other robustness checks, when the models were estimated with these controls, the results differed little. The number of HHs was about evenly divided between intervention and control groups, suggesting that attrition was not significantly different between groups. Combining this with the evidence from the robustness checks just described, it was concluded that attrition bias was not driving the results presented. Randomisation ratio: 1:1 Recruitment method: NR Sample size justification and outcome used: 42 HHs were randomly selected in each comarca using a census carried out by RPS 3 months prior to the survey as the sample frame, yielding an initial target sample of 1764 HHs. The sample size calculation was based on assessing the necessary sample sizes for the indicators listed in Appendix B, Table 26. Assuming a random sample, the indicator that required the largest sample size, using a significance level of 5% and a power of 80%, was enrolment for Grades 1–4 (indicator 5 in Appendix B, Table 26). To detect a minimum, statistically significant difference of 8 pps between intervention and control groups, a sample size of 549 students for each group was required. Not all HHs had children in this age group. According to the 2000 RPS population census, 63% of HHs had ≥ 1 child aged 6–12 years. Therefore, to obtain a sample of 549 children (in different HHs), it was necessary to interview 871 HHs in each group (549 divided by 0.63) or 1742 in total. Thus, the study authors arrived at a target sample of 1764 HHs. Sampling method: in the design phase of RPS, rural areas in all 17 departments of Nicaragua were eligible for the programme. In addition, these departments had easy physical access and communication (including being < 1‐day drive from the capital, Managua, where RPS is headquartered), relatively strong institutional capacity and local co‐ordination, and reasonably good coverage of health posts and schools. By purposively targeting, RPS avoided devoting a disproportionate share of its resources during the pilot to increasing the supply of educational and health services. In the next stage of geographic targeting, all 6 (out of 20) municipalities that had the participatory development programme Microplanificación Participativa (Participatory Micro‐planning), run by the national Fondo de Inversión Social de Emergencia (FISE), were chosen. In the last stage of geographic targeting, a marginality index based on information from the 1995 National Population and Housing Census was constructed, and an index score was calculated for all 59 rural census comarcas2 in the selected municipalities. The index was a weighted mean of the following set of poverty indicators (with respective weights in parentheses) known to be highly associated with poverty (Arcia 1999): 1. family size (10%), 2. access to potable water (50%), 3. access to latrines (30%), and 4. illiteracy rates (10%). Higher index scores were associated with more impoverished areas. Recognising that the index could not reliably distinguish between 2 comarcas with similar scores, rather than use the scores directly, the 59 rural comarcas were grouped into 4 priority levels after renormalising the highest index score to 100: a score > 85 was given highest priority (priority 1); 70–85, priority 2; 60–70, priority 3 and below 60, lowest priority. The 42 comarcas with the priority scores 1 and 2 were eligible for the pilot phase's first stage. Comarcas are administrative areas within municipalities that include 1–5 small communities averaging 100 HHs each. Study aim or objective: to determine the impact evaluation of a randomised community‐based intervention, RPS, against a broad range of outcomes related to the programme's primary objectives, including 1. HH (food) expenditures, 2. child schooling and child labour, 3. preventive health care of children aged < 5 years, and 4. nutritional status of children. Study period: baseline: 2000; follow‐up: 2001–2002 Unit of allocation or exposure: randomisation was at the comarca level. Intervention at HH level |
|
| Participants |
Baseline characteristics Intervention or exposure: NR Control: NR Overall
Inclusion criteria: in the design phase of RPS, rural areas in all 17 departments of Nicaragua were eligible for the programme. The focus on rural areas reflects the distribution of poverty in Nicaragua of the 48% of Nicaraguans designated as poor in 1998, 75% resided in rural areas. For the pilot, the Government of Nicaragua selected the departments of Madriz and Matagalpa from the northern part of the Central Region, on the basis of poverty as well as on their capacity to implement the programme. Table 1 of the publication summarises the eligibility requirements and demand and supply‐side benefits of RPS. Exclusion criteria: HH not extremely poor satisfying 1 or both of the following: 1. own a vehicle, truck, pickup truck or jeep; 2. own > 20 manzanas (14.1 hectares) of land. Based on these criteria, 169 HHs (2.9% of HHs living in the intervention areas as reported in the May 2000 RPS census population) were excluded from the programme. In addition to these HHs, 219 (3.8%) HHs were excluded after the orientation assemblies and programme registration for ≥ 1 of the following reasons: 1. HH comprising a single man or woman who was not disabled, 2. HH with significant economic resources or a business, 3. HH that omitted or falsified information during the RPS population census. Finally, 240 (4.2%) HHs did not attend the orientation assembly or chose not to participate. Pretreatment: there were few significant differences between HHs (or individuals) in intervention and control groups at baseline. Differences in baseline 2000 study: RPS mean effect on annual total HH: intervention: NIO 20,903 control; NIO 20,695 in control Attrition per relevant group: 90% (1581) of the stratified random sample was interviewed in the first round (see Table 3 of publication). In a few comarcas, the coverage was 100%, but in 6, it was < 80%. For the follow‐up surveys in October 2001 and October 2002, the target sample was limited to these 1581 first‐round interviews. In 2002, just over 90% of these were re‐interviewed, on a par with surveys of similar magnitude in other developing countries. Again, however, coverage in 6 of the comarcas was substantially worse, with < 80% successfully re‐interviewed (and 1 was 1 of the 6 from above with high first‐round non‐response rate). This attrition was unlikely to have been random. Description of subgroups measured and reported: Grades 1, 2, 3 and 4; extreme poor, poor and non‐poor; children aged 0–3 years, 12–23 months; HHs with children aged 0–5 years; HHs with children aged 7–13 years; Total number completed and analysed per relevant group: total completed interview: 1581 in 2000, 1490 in 2001 and 1434 in 2002. Total completed interview in all 3 rounds: 1396. Total number enrolled per relevant group: total enrolled: 1764 in 2000, 1581 in 2001 and 1581 in 2002. Total number randomised per relevant group: evaluation design was based on a randomised, community‐based intervention with measurements before and after the intervention in both treatment and control communities. One‐half of the 42 comarcas (targeted in the first stage) were randomly selected into the programme. Thus, there are 21 comarcas in the intervention group and 21 in the control group. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food: per capita food expenditure (annual); percentage of HH food expenditure; food expenditure for different food groups/items Anthropometry: underweight (WAZ < –2SD); stunted (HAZ < 2SD); wasted (WHZ < –2SD); HAZ |
|
| Identification |
Sponsorship source: IFPRI Country: Nicaragua Setting: 42 rural comarcas areas in rural departments of Madriz and Matagalpa in the northern part of the Central Region in Nicaragua Authors' names: John A Maluccio and Rafael Flores Email: NR Declarations of interest: NR Study or programme name and acronym: Red de Protección Social (RPS) or 'Social Safety Net' Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Randomisation done through lottery process. Given the geography of the programme area, control and intervention comarcas were at times adjacent to one another. The selection was done at a public event with representatives from the comarcas, the Government of Nicaragua, IADB, IFPRI and the media present. The 42 comarcas were ordered by their marginality index scores and stratified into 7 groups of 6 each. Within each stratum, randomisation was achieved by blindly drawing 1 of 6 coloured balls (3 blue for intervention, 3 white for control) from a box after the name of each comarca was called out. Thus, 3 comarcas from each group were randomly selected for inclusion in the programme, while the other 3 were selected as controls. The survey sample is a stratified random‐sample at the comarca level from all 42 comarcas. The areas represented comprise a relatively poor part of the rural Central Region in Nicaragua, but the sample is not statistically representative of the 6 municipalities (or other areas of Nicaragua, for that matter). 42 HHs were randomly selected in each comarca using a census carried out by RPS 3 months prior to the survey as the sample frame, yielding an initial target sample of 1764 HHs. |
| Allocation concealment (Selection bias) | Low risk | Allocation was at the comarca level at the beginning of the study. Randomisation process was done at a public event with representatives from the comarcas, the Government of Nicaragua, IADB, IFPRI, and the media present. No recruitment was done after randomisation. |
| Baseline characteristics similar (Selection bias) | Low risk | Baseline outcome data are presented. On the whole, there were few significant differences between HHs (or individuals) in intervention and control groups at baseline. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Quote: "… double‐difference estimates of the effects of the program presented later in this report all show differences at baseline for the entire range of outcomes analyzed. In no instance were any of those measures significantly different at baseline." |
| Blinding of participants and personnel (Performance bias) | Low risk | Although authors stated that, "Within each stratum, randomisation was achieved by blindly drawing one of six colored balls (three blue for intervention, three white for control) from a box after the name of each comarca was called out." Unclear who was blinded. |
| Blinding of outcome assessment (Detection bias) | High risk | No information on whether or not the assessments were done blindly but some outcomes were self‐reported which could have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Unclear risk | Although this study had a community cluster randomised design, the clusters in the intervention and control comarcas were at times adjacent to one another. A HH may be a beneficiary while its neighbour is a non‐beneficiary, particularly in a few cases where boundaries such as roads divide 2 comarcas. Seeing the activity and the emphasis placed on the RPS objectives may lead non‐beneficiaries to undertake behaviour they would not have otherwise. |
| Incomplete outcome data (Attrition bias) | Low risk | Quote: "We now document non‐response in the 2000 baseline survey and attrition in the follow‐up surveys. Overall, 90 percent (1,581) of the stratified random sample was interviewed in the first round (see Table 3)." The authors also state that, "Recall that the number of households is about evenly divided between intervention and control groups, suggesting that attrition was not significantly different between intervention and control groups. Combining this with the evidence from the robustness checks just described, we conclude that attrition bias is not driving the results presented here." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol is available |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unlikely. Incorrect analysis: unlikely. Seasonality bias: low. Authors statistically controlled for seasonality. |
Marquis 2018.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? ITT analysis Randomisation ratio: 1:1 Recruitment method: 6 Upper Manya Krobo District subdistricts stratified by population size, 3 subdistricts randomly selected as study site, census of communities completed with GPS location of all HHs, 89 communities organised geographically into 16 clusters, within each cluster, communities randomly chosen to reach target number of eligible HHs per cluster, 39 communities selected as study area. Enrolment and intervention implementation carried out in 2 phases: Phase 1 (2014–2015): all women with infants who lived in selected communities and planned to remain community for duration of project invited to enrol. Phase 2 (2016–2017): age range expanded to target young children < 18 months to include planned sample size – both phases included additional eligibility criteria. All 277 eligible HHs in selected communities of 8 intervention clusters invited to enrol in Phase 1 (2014). At end of Phase 1, new 95 eligible HHs from same communities identified and invited to enrol in Phase 2 (2016). 2 intervention clusters had no new eligible HHs so 6 intervention clusters were active in Phase 2. 34 eligible HHs were not enrolled, 51 were enrolled, baseline data lost due to malfunction. Control cluster communities with no benefit not enrolled a second time and order of including control clusters randomly assigned. To mimic intervention enrolment, 5 control clusters were used in Phase 1 (135 eligible HHs) and 3 control clusters (114 eligible HHs) in Phase 2. Among control clusters, 36 HHs were not enrolled. Sample size justification and outcome used: sample size calculated with an α = 0.05, power = 0.80, effect size d = 0.35, and variance inflation factor = 1.79, resulting in 227 HHs/group. Assuming an LTFU of 10%, the sample size estimate was 250 per treatment group or a total of 500 mother–child pairs. Outcome not mentioned. Sampling method: random as communities within clusters were randomly chosen. Study aim or objective: to determine the effect of a 12‐month intervention (inputs and training for poultry farming and home gardening, and nutrition and health education) on child diet and nutritional status. Study period: phase 1: 12 months; phase 2: 12 months Unit of allocation or exposure: clusters consisting of either 1 distinct community or multiple adjacent small communities. |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: in Phase 1 (2014–2015), all women with infants (aged 0–12 months) who lived in the selected communities and who planned to remain in the community for the duration of the project were invited to enrol in the trial. In Phase 2 (2016–2017), the age range was expanded to target young children aged < 18 months to include the planned sample size. For both phases, additional eligibility criteria for the intervention participants included the timely preparation of a chicken coop that met project specifications and a fenced home garden plot. Exclusion criteria: NR Pretreatment: rate for enrolment with baseline completion was lower among the intervention compared with the control clusters, partly due to a malfunction of the electronic data collection system (77.2% intervention vs 83.5% control; P < 0.01). There were no enrolment phase differences in baseline values for the infant anthropometric indices (data not shown). There were no baseline treatment group differences in child, maternal or HH characteristics Attrition per relevant group: total 14.4%. Total LTFU cases were due to refusal (2), participant moved outside study area (49), and maternal or child death (5). The remaining cases could not be found (16). There was no difference in attrition rate by treatment group (13.9% intervention vs 15.0% control; P = 0.73). Description of subgroups measured and reported: logistic regression models: primary or secondary/above education vs none, married vs not married, middle or high wealth vs low, male vs female, krobo ethnicity vs non‐krobo, mild or moderate or severe food insecurity vs secure. Total number completed and analysed per relevant group: intervention: 247 analysed for endline outcomes; control: 181 analysed for endline outcomes Total number enrolled per relevant group: intervention: 287 mother–infant pairs (194 in phase 1, 93 in phase 2); control: 213 mother–infant pairs (122 phase 1, 91 phase 2) Total number randomised per relevant group: intervention: 372 mother–infant pairs (277 phase 1, 95 phase 2); control: 249 mother–infant pairs (135 phase 1, 114 phase 2) |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Dietary diversity: MDD Anthropometry: HAZ; WAZ; WHZ |
|
| Identification |
Sponsorship source: McGill University, Heifer International, World Vision Canada, Global Affairs Canada, Grant/Award Number: S065653 Country: Ghana Setting: rural: Upper Manya Krobo District of the Eastern Region of Ghana. 86 communities in 3 selected subdistricts + 3 additional. Comments: trial was registered at Clinicaltrials.gov (NCT01985243). Author's name: Grace S Marquis Email: Grace.Marquis@mcgill.ca Declarations of interest: no conflicts of interest. Study or programme name and acronym: Nutrition Links (NL) Type of record: journal article (supplement) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "The 16 clusters were randomly assigned to treatment group (sequential, using random numbers)." |
| Allocation concealment (Selection bias) | Low risk | The 16 clusters were randomly assigned to treatment group (sequential, using random numbers). |
| Baseline characteristics similar (Selection bias) | Low risk | Quote: "There were no baseline treatment group differences in child, maternal, or household characteristics." |
| Baseline outcome measurements similar (Selection bias) | Low risk | There were no enrolment phase differences in baseline values for the infant anthropometric indices (data not shown). Baseline dietary outcome values (egg consumed and minimum diet diversity) were not compared, as phase was associated with child age and diet changed with age. |
| Blinding of participants and personnel (Performance bias) | Low risk | Given the nature of the intervention, it was not possible to mask the treatment assignment; therefore, the project maintained separate field staff for the implementation of the intervention and survey data collection. The clusters were geographically distant enough to avoid direct contamination, i.e. no control community participants received inputs or took part in educational activities planned for intervention participants. |
| Blinding of outcome assessment (Detection bias) | Low risk | Given the nature of the intervention, it was not possible to mask the treatment assignment; therefore, the project maintained separate field staff for the implementation of the intervention and survey data collection. |
| Protection against contamination (Performance bias) | Low risk | 16 clusters were randomly assigned to treatment group. The clusters were geographically distant enough to avoid direct contamination, i.e. no control community participants received inputs or took part in educational activities planned for intervention participant. |
| Incomplete outcome data (Attrition bias) | Low risk | Quote: "There were no significant differences in child, maternal, or household characteristics (see list of variables in Table 1) between those participants who were lost to follow‐up and those who completed the study (data not shown). There was no difference in attrition rate by treatment group (13.9% intervention vs. 15.0% control; P = 0.73)." |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. All relevant outcomes in the methods section were reported in the results section. |
| Other bias | Unclear risk | Quote: "There may have been some selection bias due to enrolment procedures. enrolment, all eligible women were informed of the project requirements including preparation of a chicken coop and a garden plot. Not all participants completed the requirement in time; those who did not received no project inputs. This additional requirement may have led to a group bias in willingness to participate. However, we did not detect any baseline differences by treatment group, and the sensitivity analysis results were consistent with the ITT analysis, suggesting that selection bias was not large enough to affect the results." |
Merttens 2013.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? (quote) "Column 8 shows the number of observations at follow‐up (FU1) which is 2,867 (the sample of households comprising the treatment plus control panel) minus any missing values." Therefore, where there were missing data, the sample size for that outcome was reduced accordingly. Probability of retention was estimated using regression, and weighting of HHs was adjusted by inverse retention probability to adequately represent attrition HHs. Randomisation ratio: 1:1 Recruitment method: evaluation covered the 4 former districts of Mandera, Marsabit, Turkana and Wajir, in 12 randomly selected sublocations in each district. The sublocations that were covered by the evaluation were referred to as the evaluation sublocations. The HSNP applied a staggered roll‐out, with sublocations being brought into the Programme on a month‐by‐month basis. Sample size justification and outcome used: calculated based on the expected sampling error for point estimates, differences and DID for key indicators. These key indicators were not explicitly reported. A sample attrition buffer of 10% was factored in to compensate for the high risk of sample attrition. Sampling method: intervention and control HHs were sampled from HSNP administrative records. From these, 66 HHs were sampled from each sublocation using simple random sampling. In the event of non‐response, a replacement HH which had not yet been drawn was randomly selected from the administrative record. The sequence in which the sampled evaluation sublocations were targeted and surveyed was determined randomly. The evaluation sublocations were selected from a sample frame of all secure sublocations in each district. The evaluation sublocations were sorted within new districts by population density and paired up, with 1 of the pair being control and 1 being treatment. The reason sublocations were sorted (within each new district) by population density before pairing them up was to ensure that similar sublocations were matched to reduce as far as possible significant variations between the characteristics of the control and treatment groups. For both the treatment and control sublocations there were an equal number of CBT, SP and DR sublocations. Study aim or objective: to evaluate the HSNP programme's impact on consumption expenditure and poverty reduction, food security, and increased asset retention and accumulation. Secondary impacts namely uptake of health and education services, stabilised food prices, supplies of key commodities, diversity of livelihood activities, financial savings, vulnerability to shocks, empowerment of women, and well‐being of the young and elderly people were also assessed. Study period: August 2009 to November 2012 Unit of allocation or exposure: sublocations (geographical areas within counties) |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: selected for the HSNP programme (whether currently receiving or on the waiting list), which included: community identification as a HH in need of cash transfer, or HHs with proportion of its members aged < 18 and > 55 years exceeding a prespecified dependency ratio, or individuals aged ≥ 55 years. Exclusion criteria: ineligible for the HSNP programme. Pretreatment: lower proportion of intervention HHs were food insecure in the worst recent food shortage when compared to control HHs. Higher proportions of intervention HHs were receiving food aid when compared to control HHs, and a lower proportion of intervention HHs had children aged < 5 years with moderate stunting. A lower proportion of intervention HHs reported having skipped eating for entire days in the past 30 days. School attendance for all ages and both sexes was higher in intervention HHs. Significantly more control HHs owned livestock when compared to intervention HHs. Attrition per relevant group: follow‐up (November 2011): 9% (137/1571) for intervention and 7% (103/1536) for control HHs. From baseline at second follow‐up (November 2012): 22% (347/1571) for intervention and 21% (324/1536) for control HHs. Description of subgroups measured and reported: NR. Total number completed and analysed per relevant group: for the final impact analysis there were 20 treatment and 20 comparison (control) sublocations, with 1224 intervention HHs and 1212 control group HHs. Total number enrolled per relevant group: total of 1571 intervention and 1536 control HHs at baseline. Total number randomised per relevant group: just over 5000 HHs were randomly selected at baseline (prior to programme roll‐out) for interview on an annual basis in 48 evaluation sublocations (24 treatment and 24 control), also selected at random. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Proportion of HH expenditure on food: proportion of consumption expenditure spent on food; monthly food consumption expenditure per AE Food security: proportion of HHs food insecure in worst recent food shortage period Dietary diversity: HDDS (0–12) Anthropometry: moderate and severe wasting; moderate and severe stunting; moderate and severe underweight Morbidity: proportion of people ill/injured in previous 3 months |
|
| Identification |
Sponsorship source: DfID. Country: Kenya Setting: impoverished rural HHs Author's name: Fred Merttens Email: fred.merttens@opml.co.uk; admin@opml.co.uk Declarations of interest: NR Study or programme name and acronym: Hunger Safety Net Programme (HSNP) Type of record: impact evaluation report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "Forty‐eight programme sub‐locations were then randomly selected from the pool of all programme sub‐locations and then from those each pair were randomly assigned between treatment and control at a public lottery event (bahati na sibu) facilitated by the HSNP Secretariat and attended by officials from the district and the two sub‐locations in question." |
| Allocation concealment (Selection bias) | Low risk | The unit of allocation was 'sublocations', stratified by district. Allocation was performed on all units at the start of the study. |
| Baseline characteristics similar (Selection bias) | High risk | Important differences between the number of children going to school (intervention group: 63.2%; control group: 42.6%), and the number of HHs owning any livestock (intervention group: 61.5%; control group: 85.1%) were present and not adjusted for in analyses. |
| Baseline outcome measurements similar (Selection bias) | High risk | Some outcomes were not equivalent at baseline: intervention HHs were significantly more food secure in the worst recent food shortage and significantly more received food aid (both P = 0.05). Intervention HHs also had significantly fewer moderately stunted children aged < 5 years (P = 0.05) and significantly less reported skipping eating for entire days (P = 0.10). Proportion of children attending school (for all ages and both sexes) was significantly higher for intervention HHs (P = 0.05). The HHs for which the baseline characteristics were reported differed from the HHs that were analysed in the year 2 analysis, so it is unclear whether outcome measurements of those analysed have been similar. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants were not blinded, but this was unlikely to have influenced participant behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether the data collectors were blinded towards the group allocations, which may or may not have influenced the measurement of outcomes across groups. Self‐reported outcomes may have been prone to reporting bias. |
| Protection against contamination (Performance bias) | Low risk | Given the geographical separation between intervention and control sublocations, the risk of contamination was low. Participants were also selected from a list that identified current recipients and waiting list recipients. According to the report itinerant/mobile people were more likely to attrite from the sample, and, therefore, unlikely to contaminate conditions due to their migration. |
| Incomplete outcome data (Attrition bias) | High risk | Quote: "The reduction in the number of sublocations surveyed at follow‐up 2 was the result of decisions made by the programme and its stakeholders, rather than a technical decision by the evaluation team. This reduction in sample size is unfortunate for a number of reasons …" Comment: in the intervention group, 1224/1571 (77.9%) and in the control group 1212/1536 (78.9%) HHs were analysed. Although the percentage attrition per group was similar, the total attrition was > 20%. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol or trial registration reported. All expected outcomes were prespecified in methods section and addressed in results section. |
| Other bias | Unclear risk | Misclassification bias: high risk. Loss of 8 clusters (sublocations) – a programme and stakeholder decision. Measurement bias: incorrect analysis: unclear. It is unclear whether these findings were comparable to individually randomised trials. Low risk of bias due to clustering, as adjustment for clustering was performed. Seasonality bias: high risk. The 8 sublocations that were dropped were scheduled to be surveyed in the end and beginning of the calendar year. Recruitment bias: unclear. Could not be ruled out as it is not explicitly stated whether randomisation, in the form of a public lottery, preceded recruitment. |
Miller 2011.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? Only participants for which there were data for all 3 data collection rounds, were analysed Randomisation ratio: 1:1 Recruitment method: research team attempted to interview all HH heads in the sampling frame by setting up appointments, meeting respondents at their homes or fields, and returning to HHs ≥ 3 times. Sample size justification and outcome used: sample size for this study was determined considering the wide range of expected impacts at the child and HH level. Used the software package R (Version 2.11.1) to perform posthoc power calculations and confirm there was sufficient power to detect statistically significant results at or exceeding the standard 0.80 level for each analysis. Sampling method: 8 village groups were randomly assigned to the intervention or control group. The sampling frame consisted of all cash transfer targeted HHs in these village groups (about 100 villages per village group). Study aim or objective: to examine the impact of the SCTS on food security and diversity at the HH level. Study period: March 2007 to April 2008 Unit of allocation or exposure: village groups |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: ultra poor HHs in selected villages in the Mchinji district (within the lowest economic quintile, having no assets, or consuming only 1 meal and labour constrained) (dependency ratio > 3, or undefined) Exclusion criteria: child‐headed HHs Pretreatment: intervention group had a greater number of HHs with orphans, whereas the control group had a greater number of elderly headed HHs. According to the study authors these differences were due to differences observed during the targeting process. A greater number of HH heads had no schooling in the intervention group, compared to the control group. HH size was higher in the control group. Attrition per relevant group: intervention group: 42/408 (10.3%); control group: 25/411 (6%); most common reason for LTFU was death (7 deaths in intervention group and 16 deaths in control group). Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: number of HHs: intervention group: 366; control group: 386 Total number enrolled per relevant group: number of HHs: intervention group: 385; control group: 411. 17 intervention HHs were found not to be eligible during recruitment. Total number randomised per relevant group: number of village groups: intervention group: 4; control group: 4 |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention for duration of the study; however, after the study (May 2008), the control group also received the intervention.
|
|
| Outcomes | Proportion of HH expenditure on food; proportion of total weekly expenditure on food; weekly HH food expenditure; per capita total weekly expenditures Food security: proportion of HHs reporting not consuming enough food per day/eating ≥ 2 meals per day/reporting hunger after meals/reporting insufficient food for > 8 days/month Dietary diversity: food diversity composite score based on number of food groups consumed in the past week. |
|
| Identification |
Sponsorship source: USAID and UNICEF Country: Malawi Setting: HHs that were ultra‐poor and labour constrained; Mchinji district Author's name: Candace M Miller Email: candace@bu.edu Declarations of interest: yes; none reported. Study or programme name and acronym: Malawi Social Cash Transfer Scheme (SCTS) Type of record: journal article, policy research working paper |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Method to generate random sequence NR. |
| Allocation concealment (Selection bias) | Unclear risk | Allocation concealment NR. |
| Baseline characteristics similar (Selection bias) | Low risk | Some baseline characteristics differed between the groups: intervention group had fewer HH heads with no schooling (P < 0.0001), larger HH size (P < 0.0001), fewer elderly‐only HHs (P < 0.001). The study authors used the DID method to account for these differences in their analysis. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Quote: "… the outcome variables of interest were statistically similar between study households at baseline, so that these groups generally experienced the same level of food insecurity" at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | Participants were not blinded, but this was unlikely to have influenced the participant behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear whether the data collectors were blinded towards the group allocations. Outcomes were self‐reported, which could have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | HHs were monitored by the district to prevent contamination. |
| Incomplete outcome data (Attrition bias) | Low risk | No clusters were lost. In terms of HHs: 42/408 (10.3%) from the intervention group and 25/411 (6.1%) from the control group were not part of the final analysis. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Protocol citation or trial registration number NR. All expected outcomes were reported on in the methods section, and reported on in the results section. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: low risk. Repeated 7‐day dietary recall administered by trained research assistants: (quote) "We trained the team of research assistants (RAs) over 1 week prior to each round of data collection." "Study supervisors checked surveys on a daily basis for consistency and completeness." Incorrect analysis: low risk. Quote: "These villages are homogeneous however; and as was expected, simple OLS regression and regression models that account for village level clustering yielded nearly identical effect sizes and standard errors". Seasonality bias: low risk. Recruitment bias: low risk. The study authors stated that baseline differences between the 1 groups most likely resulted from differences in the prioritisation of either elderly‐only HHs or HHs with orphans in the intervention group during targeting process. However, analyses adjusted for these differences. |
Murshed E Jahan 2011.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? No missing data reported by study authors. Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: NR Sampling method: stratified random sampling. Respondents were selected in such a way that farmers of different wealth ranks were included by means of a participatory wealth ranking exercise undertaken in the study sites. The participants identified land holding as the proxy measure of wealth for ranking the HHs. All HHs were ranked based on their access to different natural resources. Study aim or objective: to assess the farm productivity, profitability, efficiency and HH nutrition of participants in integrated aquaculture‐agriculture training (with and without a small financial grant) and of a group of control farmers. Study period: 3 years; 2002/2003 to 2005/2006 Unit of allocation or exposure: individuals (farmers) |
|
| Participants |
Baseline characteristics Intervention or exposure group:
Control group:
Overall: NR Inclusion criteria: farmers from 4 districts (Mymensingh, Comilla, Magura and Bogra). No other criteria reported. Exclusion criteria: farmers who had previously received training in aquaculture production or integrated aquaculture‐agriculture and those who did not agree to participate were excluded from the pool. Pretreatment: baseline characteristics were not assessed for the control group; table 2 presented characteristics of both groups assessed in 2006, which showed no differences between them. At baseline the table showed that there was no significant difference between different groups of farmers included in the study at the time of selection in terms of farm area, i.e. number of hectares owned (land holding was proxy measure for wealth). Attrition per relevant group: attrition NR. Description of subgroups measured and reported: none Total number completed and analysed per relevant group: intervention (project farmers) 260 (grant farmer: 127; non‐grant farmers: 133); control farmers 126 Total number enrolled per relevant group: intervention (project farmers) 260 (grant farmer: 127; non‐grant farmers: 133); control farmers = 126 Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure group: integrated agriculture‐aquaculture intervention
Control group: no intervention |
|
| Outcomes | Total and per capita HH food consumption – total/for individual foods | |
| Identification |
Sponsorship source: USAID; World Fish Center Country: Bangladesh Setting: small‐scale farms in 4 Bangladesh districts Author's name: Khondker Murshed‐E‐Jahan Email: k.jahan@cgiar.org; d.pemsl@cgiar.org Declarations of interest: NR Study or programme name and acronym: Development of Sustainable Aquaculture Project (DSAP) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA; no randomisation done. |
| Allocation concealment (Selection bias) | High risk | CBA; no allocation concealment done. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Study authors reported similar farm areas and access to social capital for both groups at baseline; however, other baseline characteristics were NR. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | No baseline measurements reported. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding but this was unlikely to have influenced participant or personnel behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | There was no blinding. Measures were based on self‐report, and lack of blinding could have influenced reporting. |
| Protection against contamination (Performance bias) | Unclear risk | Control farmers were selected from the same districts as project farmers but it was not clear what their distance was from project farmers and whether any of these started any integrated aquaculture‐agriculture projects by themselves. |
| Incomplete outcome data (Attrition bias) | Low risk | All farmers completed the study; there were no missing data. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | Unclear risk | Misclassification bias: unlikely. NGO assigned farmers to intervention. Measurement bias: low risk. HHs completed daily food consumption diary. Seasonality bias: low risk. |
Olney 2016.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? analytic sample was restricted to HHs or mothers with complete data at baseline and endline for a given indicator. To address possible attrition bias, attrition weights were calculated and applied to the sample descriptive statistics and impact estimates." Randomisation ratio: approximately 1:1 (initially 25:15:15 for control, intervention led by OWLs, and intervention led by HC members; intervention data were combined as no differences were observed for OWL‐led and HC‐led with regards to outcomes, and to increase statistical power) Recruitment method: HHs were invited to participate. Trained field workers explained the study to eligible HHs, and informed consent was obtained from either the HH head or the mother of the selected child. Sample size justification and outcome used: the study was restricted to 55 villages that met minimum programme eligibility criteria in the 4 departments because of logistics and cost. We estimated a sample size of 30 children per cluster with statistical significance of 0.05, power of 0.80 and an intracluster correlation of 0.02. This sample size provided the ability to detect minimum differences between treatment groups of a change of 0.25 in mean HAZ and WHZ and a 0.3 g/dL change in Hb. The sample also permitted the estimation of changes of 10 pps in the prevalence of wasting, anaemia and diarrhoea and 15 pp in stunting." Sampling method: before the baseline evaluation, villages within 4 'departments' in the province of Gourma were identified for possible inclusion in the EHFP programme; participating villages needed to have water sources to support production during the dry season. 55/181 eligible villages were identified for randomisation and were stratified by commune/department and village size before randomisation into 1 of 3 groups: 1. control group, which received no interventions from HKI (25 control villages), 2. EHFP programme with BCC led by OWLs (15 OWL villages – nutrition and health education done by OWLs), or 3. EHFP programme with BCC led by HC members (15 HC villages – nutrition and health education done by HC members). Within the selected villages, all HHs with a mother who had a child aged 3–12 months at the time of the baseline survey (February–May 2010) were invited to participate in the impact evaluation. Study aim or objective: to assess the impact of the EHFP programme on child nutritional status and health as primary impact measures, as well as on mothers' nutritional status and empowerment as secondary impact measures. Study period: February 2010 to June 2012. Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall
Inclusion criteria: villages located in the 4 selected departments, had access to water in the dry season to enable participation in the agricultural intervention, and met the population size criteria (≤ 4000 inhabitants) (Olney 2015). Mothers with a child aged 3–12 months. Exclusion criteria: NR. Pretreatment: mothers' BMI was lower in the treatment group compared to control, and more underweight mothers (BMI 18.5 kg/m2) were present in the treatment group. Attrition per relevant group: total attrition 16% of the original sample. Attrition: control villages: 19% (113/597) for HHs and 29% (148/510) for mothers; intervention villages: 14% (124/884) for HHs and 22% (173/787) for mothers. Description of subgroups measured and reported: NR. Total number completed and analysed per relevant group: total 1481 completed the endline survey; intervention: 884 HHs (441 in HC group and 443 in OWL group). 376 children (HC group) and 395 children (OWL group) with complete observations. Control: 597 HHs. 511 children with complete observations. Mothers' BMI: control 510, intervention 787; mothers' consumption of individual food groups and mean DDS: control 506, intervention 766; HH consumption of individual food groups and mean DDS: control 596, intervention 880; women's empowerment: control 517, intervention 781. Total number enrolled per relevant group: total: 1767 HHs. Intervention: 15 villages in HC group and 15 villages in OWL group. 514 HHs in HC group and 512 HHs in OWL group. Control: 25 villages, 741 HHs Total number randomised per relevant group: control: 25 villages; intervention: 30 villages (15 OWL villages and 15 HC villages analysed together in Olney 2015). Total group: 1767 HHs with intervention HHs 514 in HC group and 512 in OWL group. Control HHs were 741. |
|
| Interventions |
Intervention characteristics Intervention or exposure group: integrated agriculture and nutrition programme
Control group: no intervention |
|
| Outcomes | Dietary diversity: HDDI, MDD; proportion of mothers consuming individual food groups in past 7 days Dietary intake: energy gap Anthropometry: adult BMI; prevalence of underweight among adults |
|
| Identification |
Sponsorship source: USAID, Office of US Foreign Disaster Assistance through HKI; European Commission/International Fund for Agricultural Development; the Gender, Agriculture and Assets Project, supported by the Bill Melinda Gates Foundation; the CGIAR Research Program on Agriculture for Nutrition and Health led by the IFPRI; and the USDA (AD). Country: Burkina Faso Setting: homesteads in agricultural areas Comments: trial registration: NCT01825226 Author's name: Deanna K Olney Email: d.olney@cgiar.org Declarations of interest: yes; 5 authors had no conflicts of interest. 1 author (A Pedehombga) worked for HKI. Study or programme name and acronym: Helen Keller International (HKI) enhanced‐homestead food production (EHFP) programme Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Stratified randomisation was performed (by commune and village size), but no information provided on how the randomisation sequence was generated. |
| Allocation concealment (Selection bias) | Low risk | Allocation to intervention groups was done at the same time for all clusters/villages. |
| Baseline characteristics similar (Selection bias) | Low risk | All baseline characteristics (with the exception of BMI outcomes) were similar across groups. Many of these were also adjusted for in the analysis. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Prevalence of diarrhoea was lowest in control group, and, for mothers, BMI and prevalence of underweight was lower in control group. However, these were adjusted for in the analysis. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding not possible, but this is unlikely to have influenced participants' or staff's behaviour or experience. |
| Blinding of outcome assessment (Detection bias) | High risk | Unclear who collected outcome data. Some outcomes were based on women's self‐reports, which could have been influenced by lack of blinding, e.g. the self‐reported consumption by food group. |
| Protection against contamination (Performance bias) | Low risk | Allocation was by village and it was unlikely that the control group received the intervention. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Overall attrition was fairly low (16%); however, differential attrition across groups resulted in significantly higher attrition among control HHs and mothers. This problem was addressed by including attrition weights in analyses. Differential attrition also occurred by HH size and composition, the presence of polygamy, female‐headed HHs and female formal education. Furthermore, women with a higher BMI were more likely to attrite resulting in an attenuation of effect size. |
| Selective outcome reporting (Reporting bias) | Low risk | No protocol available. All outcomes in the trial registry reported in publications. Some stated measures such as mothers' health and knowledge of nutrition and hygiene were NR. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unlikely. Incorrect analysis: low risk. Analyses adjusted for clustering, it is unclear whether these findings were comparable with an individually randomised trial. Recruitment bias: high risk. Randomisation was performed before recruitment was done, significant baseline imbalance was present for important outcomes of interest, there was a considerable risk of bias from loss of clusters as 1 intervention cluster attrited before follow‐up. |
Osei 2017.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? Missing or implausible outcome data were reported in the article and were excluded from the analysis involving the respective outcomes variables (Osei 2017). Attrition not relevant as study data were collected through independent cross‐sectional surveys at baseline (2009) and follow‐up (2012). Therefore, data on the impact of the intervention were not gathered from the same individuals in the 2 surveys. Randomisation ratio: 1:1 (subdistrict level) Recruitment method: recruitment to intervention group: not described. 1 woman per group of intervention villages (about 5 or 6) was selected and trained by HKI in improved gardening and poultry‐rearing practices in preparation to host a VMF. Under the guidance of HKI, this woman then trained 20 other beneficiary women on how to establish their home gardens and poultry production (Osei 2017). Sample size justification and outcome used: calculated to detect an assumed difference in the prevalence of stunting and underweight of 10% as well as a difference in wasting of 5% among children in the treatment compared to the control communities. Using a power of 0.80, a 95% CI (2 sided), an assumed design effect of 2 and an upward adjustment of 10% to account for LTFU, 1970 children were considered adequate for each of the pre‐ and post‐treatment surveys. The baseline sample was increased to 2106 to allow enough participants for a substudy, which involved providing micronutrient powders to a subsample of 110 children in the intervention communities for 6 months. The follow‐up sample was also increased to 2614 to allow sufficient participants for disaggregated analysis (Osei 2017) Sampling method: multistage cRCT. The Baitadi district is administratively divided into 12 subdistricts called 'Ilakas', and each 'Ilaka' is further divided into 'village development committees' (VDCs), which consist of several (about 9) villages. (Osei 2015). Assigned Ilakas (instead of villages or HHs) into each of the 2 study groups. Ilakas were paired on several key socioeconomic indicators, and 4 of the generated 6 pairs of Ilakas were selected for inclusion in study using a simple random sampling procedure. The same procedure was followed to assign 1 Ilaka in each pair as the treatment group and the other as the control. Overall, there were 21 VDCs in the treatment Ilaka and 20 in the control Ilakas (Osei 2017). All the VDCs in the EHFP programme communities received the EHFP intervention. To select families for the pre‐ and postsurveys, VDCs were stratified by treatment (21) or control group (20), and 14 VDCs were selected from each using a simple random sampling procedure to participate in the surveys. However, all the VDCs in the EHFP programme communities received the EHFP intervention, regardless of their participation in the surveys. Within each selected VDC, HHs were selected using the probability proportional to size technique, and in each selected HH, a child aged 12–48 months was chosen together with his/her mother for the assessments. If a HH had > 1 eligible child, the youngest child was chosen (Osei 2017). Study aim or objective: to determine the effect of an EHFP programme consisting of home garden, poultry raising and nutrition education implemented over 2.5 years vs control (no intervention) on anthropometry and anaemia among children (aged 12–48 months) and their mothers (Osei 2017). Study period: 2.5 years from 2009 to 2012. The baseline survey was conducted in August 2009, the follow‐up survey in August/September 2012. Unit of allocation or exposure: subdistricts (Ilakas) |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: families with children aged 0–23 months in 1 group of communities received the EHFP intervention (treatment group); in each selected HH, a child aged 12–48 months was chosen together with his/her mother for the assessments. Exclusion criteria: NR Pretreatment: baseline intervention sample had significantly more pregnant women, lower maternal parity, larger family size and a lower proportion of male‐headed HHs than the control, although these characteristics did not differ between the groups at follow‐up. Children in the intervention group were significantly older than those in the control group at follow‐up. Other characteristics that were similar among the study groups at baseline but differed significantly at follow‐up included the proportion of HHs with no monthly cash income and those with some financial debts at the time of the surveys. Both surveys showed significantly fewer mothers with no formal education, mothers who worked outside the home, and proportion of families with married HH heads, in the upper caste and lower tercile of wealth among the treatment compared to the control group. Attrition per relevant group: attrition not relevant as baseline and follow‐up samples were independent. NR. Authors reported data excluded from analysis. Of the 2106 mother–child pairs in the baseline sample, 1 child and 2 mothers missed Hb measurements; 8 children had implausible HAZ and 4 children had implausible WHZ values, and 1 mother had implausible BMI (< 12.0 kg/m2). Therefore, these participants were excluded from the analysis involving these outcomes. In addition, 10.9% of the mothers (intervention: 100; control: 129) were pregnant at baseline and were excluded from maternal BMI and underweight analysis. For the 2614 mother–child pairs assessed at follow‐up, 18 had implausible HAZ and 11 children had implausible WHZ values, and 9.7% mothers (intervention: 125; control: 128) were pregnant. These participants were excluded from the analysis involving the respective outcome variables. Description of subgroups measured and reported: NR. Total number completed and analysed per relevant group: total number varied depending on the outcome being analysed. General numbers at follow‐up: intervention: 1037 families (1037 mothers and 1037 children); control: 1037 families (1037 mothers and 1037 children). Total number enrolled per relevant group: intervention: 4 subdistricts; 21 VDC; 1055 families (1055 mothers and 1055 children); control: 4 subdistricts; 20 VDC; 1051 families (1051 mothers and 1051 children). Total number randomised per relevant group: intervention: 4 subdistricts; 21 VDC; 1055 families (1055 mothers and 1055 children); control: 4 subdistricts; 20 VDC; 1051 families (1051 mothers and 1051 children). |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Food security: HFIAS Anthropometry: WAZ, WHZ, HAZ, stunting, wasting, underweight, BMI and underweight of mothers Biochemical: mean Hb concentration (mother/child) Morbidity: anaemia (mother/child) |
|
| Identification |
Sponsorship source: USAID Country: Nepal Setting: homesteads in Baitadi District, a remote hilly community in the far western region of Nepal. Author's name: Akoto Osei Email: andykofi20@gmail.com; oseia@africa‐union.org Address: Department of Social Affairs, African Union Commission, Room 1216, New Building, PO Box 3243, Addis Ababa, Ethiopia Declarations of interest: no potential conflicts of interest. Study or programme name and acronym: Enhanced Homestead Food Production (EHFP) programme Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Quote: "Simple random sampling procedures' were performed to select both the sub‐district pairs (Ilakas), allocate one sub‐district in each pair to either the intervention and control groups, and to select village development committees from which families were selected for the pre‐and post intervention surveys. However, no information is provided on which 'simple random sampling procedure' was followed. Households that participated in the pre‐ and post intervention surveys were selected using the probability proportional to size technique." |
| Allocation concealment (Selection bias) | Low risk | Allocation of subdistricts to study groups were performed for all units at the start of the study. |
| Baseline characteristics similar (Selection bias) | Low risk | Imbalances at baseline and follow‐up for many variables were present, but these were adjusted for in the analysis. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | At baseline, treatment HHs were less food insecure, had a higher mean WAZ for children, had a lower prevalence of underweight and stunting in children, and a significantly lower adjusted mean BMI compared to the control HHs. Unclear to what extend these were adjusted for in the analysis. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding was possible but it was unlikely this influenced the intervention received. |
| Blinding of outcome assessment (Detection bias) | Low risk | Blinding of participants and personnel was not possible due to the nature of the intervention, but it was unlikely that the outcomes were influenced by the lack of blinding. The primary outcome variables (stunting, underweight, wasting, Hb concentration and anaemia among children and Hb concentration, anaemia and underweight among their mothers) were assessed using objective anthropometric and Hb measurements that were taken at baseline and follow‐up. |
| Protection against contamination (Performance bias) | Unclear risk | Although the randomisation was done at a subdistrict level, which should have minimised contamination, the authors reported an increase in the same activities of the intervention in the control group during the trial. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Unclear how the micronutrient powder intervention provided in the substudy (Osei 2015) might have affected the study outcomes. It is NR if it was adjusted for in the analysis. Attrition not relevant: study data were collected through independent cross‐sectional surveys at baseline (2009) and follow‐up (2012), so data on the impact of the intervention were not gathered from the same individuals in the 2 surveys. Outcome data from both intervention and control groups were excluded from the analysis, but the number of exclusions for Hb measurements, HAZ and WHZ values, maternal BMI were small and the reasons for them reported. Exclusion of maternal BMI and underweight analysis due to pregnancy in both the baseline and follow‐up surveys were balanced across groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | The stated primary outcomes were reported on in the article, and intermediary outcomes are reported in supplemental tables. However, no protocol was available. |
| Other bias | High risk | Measured association might be biased. Study data were collected through independent cross‐sectional surveys and assessments at baseline (2009) and follow‐up (2012), so data on the impact of the intervention were not gathered from the same individuals in the 2 assessment periods. Therefore, the observed changes in outcomes cannot be directly associated with the intervention. |
Pellerano 2014.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel How were missing data handled? HHs that were living elsewhere or unavailable for interview for other reasons were dropped from the study. Analysis was limited to panelled HHs that were observed both at baseline and follow‐up (25% of the original sample not analysed). Randomisation ratio: 1:1 (clusters = EDs) Recruitment method: field workers visited each randomly selected HH, where the head of each HH was interviewed. In case the head of the HH/carer was N/A, any knowledgeable member of the HH aged > 18 years qualified for the interview. Sample size justification and outcome used: NR Sampling method: multistage stratified random cluster sampling. Within 10 community councils, 96 EDs were randomly allocated to the CGP programme or not (primary sampling units) in public lottery events that took place in each ED. EDs that were selected for the programme were paired with EDs that were not (48 pairs). Of these, 40 pairs were randomly selected. Within each selected ED, 2 villages (or clusters) were randomly selected (secondary sampling units). In every cluster, a random sample of 20 HHs (10 eligible and 10 non‐eligible at baseline) were randomly selected and interviewed. Study aim or objective: to assess the direct impact of the CGP on the well‐being of eligible HHs. To assess the indirect impact of the CGP on non‐eligible HHs (data not extracted). Study period: 2 years; September 2011–2013 Unit of allocation or exposure: EDs (HHs within these were then selected based on eligibility criteria). |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: ultra‐poor HHs with any child aged 0–17 years in 10 selected community councils spread across 5 districts. Ultra‐poor HHs were identified by members of their community and by collection of proxy indicators of HH wealth, captured in the National Information System for Social Assistance (NISSA – HHs had to be categorised as NISSA 1 or NISSA 2) Exclusion criteria: NR Pretreatment: baseline differences between HHs in the intervention and control group included number of children aged 0–5 years (P < 0.01), females aged 18–59 years (P < 0.05), and proportion of HHs that borrowed or received support from other family members, friends or neighbours (P < 0.05) (data included eligible and non‐eligible HHs in treatment and control groups – not disaggregated for only eligible HHs). Attrition per relevant group: intervention group: 5% (41/747); control group: (12%; 92/739); main reason for LTFU: moved outside the cluster. Description of subgroups measured and reported: none reported Total number completed and analysed per relevant group: total: 1353 HHs (91%); intervention group: 706 HHs; control group: 647 HHs. Only 75% of children were in both baseline and follow‐up surveys (attrition: 25%) Total number enrolled per relevant group: intervention group: 747 HHs; control group: 739 HHs Total number randomised per relevant group: total: 48 EDs in 5 districts. Intervention: 24 EDs; control: 24 EDs. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Real monthly total consumption expenditure; monthly amount spent on food Food security: proportion of children aged 0–5 and 6–17 years with severe food deprivation (FSI); number of months in which HHs had sufficient/some shortage/extreme shortage food to meet their needs Dietary diversity: DDI; FCS; proportion of HHs with poor/borderline/acceptable food consumption Anthropometry: weight; underweight Morbidity: proportion of children ill in previous month; mean number of days children ill in previous month. Adverse event: overweight |
|
| Identification |
Sponsorship source: Oxford Policy Management (OPM) was contracted by UNICEF to design and undertake an independent evaluation of Round 2 Phase 1 of the CGP pilot. Country: Lesotho Setting: rural HHs Author's name: Luca Pellerano Email: luca.pellerano@opml.co.uk Declarations of interest: NR Study or programme name and acronym: Lesotho Child Grants Programme (CGP) Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Randomisation took place through public lottery events in each community council. |
| Allocation concealment (Selection bias) | Low risk | Allocation was at the ED level, in public lottery events. |
| Baseline characteristics similar (Selection bias) | Low risk | A number of baseline differences reported between HHs in the intervention and control group despite the matching of electoral districts (primary sampling unit), followed by random sampling of clusters (secondary sampling units). These include number of children aged 0–5 years (P < 0.01), women aged 18–59 years (P < 0.05), price of rubber boots in the community (P < 0.05), and proportion of HHs that borrowed or received support from other family members, friends or neighbours (P < 0.05). The study authors used the DID method and adjusted for baseline imbalances in their analyses. |
| Baseline outcome measurements similar (Selection bias) | Low risk | HHs in both groups were similar at baseline in terms of outcome measurements such as HH food consumption, HH food security and expenditure on food. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding possible. This was unlikely to introduce performance bias. |
| Blinding of outcome assessment (Detection bias) | High risk | Outcomes were measured by self‐report in questionnaire. Self‐reported outcomes could have been influenced by knowledge of treatment allocation. |
| Protection against contamination (Performance bias) | Low risk | CGP administrative records indicated that no eligible HHs in control areas received the intervention. |
| Incomplete outcome data (Attrition bias) | Low risk | Differential attrition (12% in control group; 8% in intervention group), mainly due to more HHs in the control group that moved outside their clusters. The study authors adjusted sampling weights for selective non‐response in their analysis by calculating the probability of HHs being retained in the sample on the basis of key HH characteristics at baseline. Loss of clusters (cRCT): low risk. No loss of complete clusters (villages) reported. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No study protocol available. |
| Other bias | Unclear risk | Misclassification bias: low risk. Measurement bias: low risk. Trained fieldworkers. Used a 7‐day dietary recall 8 food groups at baseline and follow‐up. Incorrect analysis: low risk. Estimates adjusted for clustering. Recruitment bias: low risk. Villages (clusters) were sampled before randomisation of electoral districts to the intervention or control group. Seasonality bias: low risk. |
Ponce 2017.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? NR Randomisation ratio: 1:2:1 Recruitment method: NR Sample size justification and outcome used: power estimates as well as sample size were computed using the Optimal Design software, working with a power of 80%, at 5% significance and with a minimum detectable effect of 0.25 (SD). However, it was NR which outcome was used in this calculation. Sampling method: 3 groups of approximately 200 HHs per group were randomly selected in 3 provinces. Study aim or objective: to differentiate the effects of food vouchers and training in health and nutrition on consumption and dietary diversity in Ecuador by using an experimental design. Study period: baseline data collected between September and November 2013, and the intervention lasted 1 year thereafter. Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention T1: food vouchers
Intervention T2: food vouchers + training on health and nutrition
Control: received no intervention
Overall: NR Inclusion criteria: NR Exclusion criteria: NR Pretreatment: except for the first intervention group (T1, food voucher only) that had significantly fewer (P = 0.008) HH members aged 45–64 years when compared to the second intervention group (T2, food voucher + training), there were no significant differences, indicating that the randomisation worked properly. Attrition per relevant group: unclear if 'cases' referred to HHs or individuals (conflicting statements), and, therefore, it is unclear how many HHs/individuals were enrolled in the study and how many completed the study or what data were included in the analyses. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: T1, food voucher only: individuals analysed 336; T2, food voucher + training: individuals analysed 512; control: unclear (from Table 3) Total number enrolled per relevant group: T1, food voucher only: HHs at baseline 171; individuals at baseline 920; T2, food voucher + training: HHs at baseline 401; individuals at baseline 2426; control: HHs at baseline 201; individuals at baseline 997 Total number randomised per relevant group: T1 group (food voucher only): 171 HHs; T2 group (food voucher + training): 401 HHs; control: 201 HHs. |
|
| Interventions |
Intervention characteristics Intervention T1: food vouchers
Intervention T2: food vouchers + training on health and nutrition
Control: no intervention |
|
| Outcomes | Dietary diversity: FCS Dietary intake: per capita energy consumption at HH level in the previous 7 days |
|
| Identification |
Sponsorship source: WFP in Ecuador and the Spanish Ministry of Science and Innovation (grant number HAR2013‐47182‐C2‐1‐P). Country: Ecuador Setting: 3 provinces in Ecuador, 2 from the Sierra region (Carchi and Chimborazo) and 1 from the Coastal region (Santa Elena)." Comments: no protocol or trial registry number reported Author's name: Jesus Ramos‐Martin Institution: N/A Email: jramos@flacso.edu.ec Address: N/A Declarations of interest: none Study or programme name and acronym: N/A Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Quote: "In our study, we randomly assigned households to one of the following groups …" Comment: however, the method of generating the random sequence was NR. |
| Allocation concealment (Selection bias) | Unclear risk | NR in the paper. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Not many baseline characteristics were reported, thus it is not possible to make a fair judgement. e.g. HH income and farming activities are important characteristics for this study's research question but these were NR. |
| Baseline outcome measurements similar (Selection bias) | Low risk | HH energy intake, per capita energy intake and dietary diversity were measured at baseline and there were no meaningful differences between groups. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not done, but it was unlikely that the lack of blinding influenced the participants' performance. |
| Blinding of outcome assessment (Detection bias) | High risk | Blinding of study participants was not possible. Outcomes were self‐reported and could have been influenced by lack of blinding. |
| Protection against contamination (Performance bias) | Unclear risk | Unclear how close HHs that participated in the study, and who were allocated to different intervention/control groups, lived from each other. It is possible that HHs from the intervention groups could have sold, shared or exchanged the extra food they got through the vouchers with other HHs; however, unclear from the manuscript whether this was likely or not. |
| Incomplete outcome data (Attrition bias) | High risk | Unclear how many individuals were analysed at endpoint in the control group, but there appeared to be high attrition in the 2 groups. |
| Selective outcome reporting (Reporting bias) | Unclear risk | Study authors did not mention whether they had an a priori protocol or if they registered their trial prospectively in a trial registry. All relevant outcomes in the methods section were reported in the results section of the manuscript. |
| Other bias | Unclear risk | Risk of misclassification bias: N/A as this was a trial. Risk of measurement bias: unclear, because the method used to collect 'Weekly HH values of food consumption' was NR. Risk of incorrect analysis: low, because outcomes were analysed at the HH level. Risk of recruitment bias: unclear because it is not clear whether recruitment took place before or after randomisation of HHs. |
Porter 2016.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? NR Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: NR Sampling method: used the data set from the Young Lives Ethiopia survey, which offers rich child and HH level panel information for 2 cohorts (born 1994 and 2001), including siblings, which allows study authors to evaluate programme impacts of different age groups from 5 years to 15 years. The Young Lives Ethiopia was a longitudinal cohort study conducted over 3 waves (2002, 2007 and 2009–2010). This data set included HHs selected for the PSNP programme and others that were not; and this was identified through survey questionnaire questions. The PSNP combines geographic and community‐based targeting to identify chronically food‐insecure HHs. Many communities had public meetings to discuss the shortlist for potential beneficiaries of PSNP, which was then approved by the next level of administration. Due to budget constraints, some HHs were short listed, but did not receive the programme. The sample comprised data from 20 sentinel sites chosen in 5 regions. HHs within sites were chosen randomly among those that had children born in the stipulated year. Importantly, PSNP was operating in 15 of these sites with 530/1886 HHs (29.1% of the sample) active beneficiaries of the programme. Study aim or objective: to provide transfers to the food insecure population' and to 'bridge the food gap' (Ministry of Agriculture and Rural Development, 2004). It operates as a safety net, whereby the public works (also known as cash/food for‐work, or workfare) programme operates seasonally, but predictably (and similarly for the direct support, or UCT). Study period: introduced in 2005 and is still ongoing. Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure group: NR Control: NR Overall: NR Inclusion criteria: targeting criteria for PSNP: HHs were food insecure and had been receiving food aid in the past. Exclusion criteria: NR Pretreatment: NR Attrition per relevant group: NR. Overall attrition for the sample was just 5.7% over the 8‐year period. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: total 1606 HHs; intervention: 682 HHs; control: 924 HHs Total number enrolled per relevant group: NR Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure group: PWP + UCTs
Control group: no intervention |
|
| Outcomes | Anthropometry: HAZ; WAZ | |
| Identification |
Sponsorship source: Young Lives is core‐funded from 2001 to 2017 by UK aid from DfID, and co‐funded by IrishAid from 2014 to 2015. Country: Ethiopia Setting: poor rural areas Comments: useful to look at Supplementary Appendix Material Author's name: Catherine Porter Email: catherine.porter@hw.ac.uk Declarations of interest: NR Study or programme name and acronym: Productive Safety Net Program (PSNP), studied using Young Lives Ethiopia cohort dataset Type of record: journal article |
|
| Notes | Results of this study were reported under "income generation" interventions category, as this component comprised 80% of the programme. Results were NR for the 2 groups; only for the overall group participating in the programme. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | Cohort study, therefore, no randomisation. |
| Allocation concealment (Selection bias) | High risk | Cohort study, therefore, no randomisation done. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Baseline assessment NR. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Baseline assessment NR. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding done. This was unlikely to have influenced behaviour or participants or personnel. |
| Blinding of outcome assessment (Detection bias) | Low risk | No blinding done. Outcomes were objective, which are unlikely to have been influenced by knowledge of intervention allocation. |
| Protection against contamination (Performance bias) | Unclear risk | Unclear what the control group was or if they were in the same communities as intervention groups. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Total number of participants and of those analysed are unclear. Overall attrition was low, 5.7%, but we do not know which group these participants belonged to or reasons for attrition. Missing data were excluded from the analysis. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | Unclear risk | Misclassification bias: unclear. Possible as treatment allocation was based on self‐report in multiple cross‐sectional surveys. Measurement bias: unclear. Potential issues regarding anthropometric or dietary intake data. Unclear whether anthropometry was measured or self‐reported, or if there was validation of questionnaire. Incorrect analysis: low risk. |
Renzaho 2017.
| Study characteristics | ||
| Methods |
Study design: controlled prospective study Study grouping: N/A How were missing data handled? to increase the accuracy of the anthropometric indices, implausible values were excluded. Unclear how much data were excluded due to this. No other missing/excluded data reported but according to table 4, data were missing for 10/3000 originally enrolled HHs (7 in intervention group; 3 in control group; both at baseline and follow‐up for each). Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: sample size calculation was primarily to detect meaningful levels of change in the study outcomes compared to the comparison group. Planned to sample only 1 child per HH, hence an equal sample size of 750 HHs at baseline and 750 at follow‐up was obtained in the intervention (1500) as well as the control area (1500). This sample size was adequate to show a 10% effect size for stunting (primary outcome) among children aged < 5 years at 6 years follow‐up (32.9% in the intervention vs 40% in the control) with > 80% power and 5% significance level (2‐sided test), a design effect of 2% and 5% sampling error. The sample size allowed for a 10% non‐response rate. The sample size was adequately powered to detect a 6% effect size in the prevalence of wasting at 6‐year follow‐up and to model associations between outcome and intervention, adjusted for demographics and other variables. Sampling method: the surveys were conducted using a 2‐stage cluster sampling method. The first stage involved identifying clusters (wards) within each district to be included in the study. All wards in each district were listed separately in alphabetical order by VDC. Using the 2011 population census data for each ward (cluster), a cumulative population for all wards was computed. From this cumulative list, the required number of clusters in each district was determined using the probability proportional to size sampling method. In the second stage, HHs within the selected clusters were identified for inclusion in the study. A list of HHs in each selected ward was constructed with the help of the local leaders and UNICEF staff. From the list, a HH was selected using a systematic sampling approach. Only HHs with ≥ 1 child aged < 60 months were eligible for the study. The sampling interval (X) was determined by dividing the total number of HHs in each ward with the expected sample size, and the first HH to be surveyed was randomly selected by choosing a number between 1 and X. For each selected HH, mothers/caretakers of children aged < 5 years volunteered to take part in the surveys, and the interview occurred outside the home, away from other HH members. If the selected HH was not inhabited, or there was no‐one at home, the closest neighbouring HH was used for the survey. Sampled about 30 HHs per cluster in each selected district at baseline, midline and endline surveys. For clusters where the number of HHs was < 25, the selected ward and its adjoining neighbour were merged and treated as a single cluster. In HHs with > 1 child, only 1 child was randomly selected for enumeration. Study aim or objective: to evaluate the effectiveness of the synergetic effect of child sensitive social protection programmes, augmented by a capacity building for social protection and embedded within existing government's TRTs for families on child nutritional status. Study period: 6 years: October–December 2009 (pre) to December 2014–February 2015 (post) Unit of allocation or exposure: district |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: HHs with ≥ 1 child aged < 60 months. Exclusion criteria: NR Pretreatment: total literacy rate was higher in the intervention group than the control group (38.5% with intervention vs 35.5% with control). A larger percentage of HHs in the control group were in the middle class or rich categories (measured by Household Wealth Index) than the intervention group (intervention group: poor 89.1%, middle class 9.7%, rich 1.2% compared with control group: poor 10.1%, middle class 23.9%, rich 65.9%). Imbalances were adjusted for using PSM for the analyses. Attrition per relevant group: none reported. According to table 4 and initial enrolment of 1500 HHs per district: data missing for 2 control HHs at baseline and 1 control HH at follow‐up; and for 7 intervention HHs at baseline. Description of subgroups measured and reported: children's age groups: children aged < 5 years (all, girls, boys); children aged > 24 months; children aged < 24 months. Total number completed and analysed per relevant group: total HHs: baseline 1491; follow‐up 1499; control HHs: baseline 748; follow‐up 749; intervention HHs: baseline 743; follow‐up 750 Total number enrolled per relevant group: 3000 HHs; 1500 in intervention district and 1500 in control district Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Anthropometry: HAZ; WHZ; WAZ; stunting; wasting; underweight | |
| Identification |
Sponsorship source: designed and implemented by UNICEF Nepal. The capacity building for social protection element was partly funded by the Asian Development Bank through Japan Fund for Poverty Reduction. The CCG programme introduced in the Government of Nepal's 2009/2010 budget Country: Nepal Setting: poor communities and HHs in 2 districts in Nepal (Bajhang District and Kalikot District) Comments: the study was approved by the Nepal Health Research Council Ethical Review Board (Approval No. 2071‐12‐18; Reg No. 29/2015). Author's name: Andre MN Renzaho Institution: N/A Email: Andre.Renzaho@westernsydney.edu.au Address: N/A Declarations of interest: yes; no conflict of interest. Study or programme name and acronym: Child Cash Grant (CCG) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | PCS; no randomisation done. |
| Allocation concealment (Selection bias) | High risk | PCS; no randomisation done. |
| Baseline characteristics similar (Selection bias) | Low risk | High variability at baseline for some characteristics such as Household Wealth Index (control wealthier than intervention), ethnicity (control group with slightly higher proportion of people from upper caste group whereas intervention group had more people from more disadvantaged ethnic groups), and education (intervention group had higher schooling than comparison group). However, PSM was used for analysis. |
| Baseline outcome measurements similar (Selection bias) | High risk | Higher proportions of stunting, underweight and wasting in the intervention group at baseline. This was not adjusted for in the analysis. |
| Blinding of participants and personnel (Performance bias) | Low risk | There was no blinding, but the outcomes were unlikely to be influenced by the lack of blinding. |
| Blinding of outcome assessment (Detection bias) | Low risk | No blinding possible. Outcomes were objective and not susceptible to influence due to lack of blinding. |
| Protection against contamination (Performance bias) | Low risk | Allocation at district level and the distance between them acted as a buffer zone, hence minimising the risk of contamination. |
| Incomplete outcome data (Attrition bias) | Low risk | No missing data reported but they excluded anthropometric data that was biologically implausible. According to table 4 of the publication and initial enrolment of 1500 HHs per district: data missing for 2 control HHs at baseline and 1 control follow‐up; and for 7 intervention HHs at baseline. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol mentioned. |
| Other bias | Low risk | Misclassification bias of exposure: low risk; intervention assigned by government. Measurement bias: low risk. |
Schwab 2013.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? Authors reported that data were analysed as ITT. However, due to discrepancies in timing of implementation of the interventions in both groups, with the food group receiving the last instalment 15 days before the endline survey whereas in the cash group the transfer was received 49 days before, some HHs were excluded from the analysis: for outcomes that rely on a recall period including the week before the survey (e.g. days in the last 7 the HH consumed meat), the analysis excluded those HHs that received their transfer in the 8‐day period before the survey. Other data were also excluded. This analysis conducted throughout this report was restricted to 3353 treatment and comparison HHs for whom consistent data from both the baseline and endline surveys exists. In addition, the remaining HHs not considered here had extensive incomplete, missing or unreliable data for key sections. Randomisation ratio: 1:1. The 136 FDPs within the sample area were randomised into equal numbers of cash or food transfers. Recruitment method: NR. Initial meetings with beneficiaries were held in June 2011 before the first transfer of the 2011 cycle was distributed to sensitise beneficiaries to the programme objectives and logistics. A follow‐up meeting for cash beneficiaries was held in November 2011 during the first disbursement of cash transfers. Sample size justification and outcome used: NR. Based on the distribution of clusters in the treatment groups and the required sample sizes, 15 intervention HHs and 11 non‐beneficiary HHs were randomly selected to be interviewed in each FDP. In total, 3536 HHs were included in the baseline sample. Approximate sample size calculations were conducted across countries at the inception of the study and are found in Ahmed et al. (2010). (Note: we were unable to find this reference.) Sampling method: 14 governorates were chosen to implement the ESN based on the classifications of ≥ 10% of the population as severely food insecure, with the end objective of reaching ≥ 75% of this population at the governorate level. The governorates of Hajjah and Ibb were chosen to be the sites of the cash and voucher pilot based on several criteria. These governorates are second‐ and third‐ranked among the 14 governorates implementing the ESN in terms of absolute numbers of food‐insecure people. In addition, Hajjah and Ibb had high percentages of the food‐insecure (Hajjah: 46.3% and Ibb: 44.0%, according to the 2009 CFSS), as well as relative stability and implementation feasibility (WFP‐CO Yemen 2011a). The 136 FDPs within the sample area were randomised into equal numbers of cash or food transfers. Taking into consideration the context of the project area, the study authors stratified the randomisation of clusters at the governorate level due to the distinct socioeconomic and geographic characteristics of Hajjah and Ibb. Based on the distribution of clusters in the treatment groups and the required sample sizes, 15 intervention HHs and 11 non‐beneficiary HHs were randomly selected to be interviewed in each FDP. In total, 3536 HHs were included in the baseline sample. Unclear who the non‐beneficiary HHs were; they were not mentioned elsewhere. Study aim or objective: in order to provide rigorous evidence on the relative impact and cost‐effectiveness of cash and food transfers, the study authors analysed the results of a cRCT of a seasonal safety net programme implemented by the WFP in rural Yemen. The analysis focused on the relative effectiveness of food and cash transfers. The analysis focused primarily on the differential impacts of these transfer types on food security outcomes. Study period: 7 months. Start and end date of study not clearly reported but it started sometime in 2011, with the first cash disbursement in November 2011. Initial meetings with beneficiaries were held in June 2011 before the first transfer of 2011. A follow‐up meeting for cash beneficiaries was held in November 2011 during the first disbursement of cash transfers. Unit of allocation or exposure: clusters; FDPs (villages) |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: both treatment groups, only need‐eligible HHs, as determined by a PMT, received benefits. Authors mentioned criteria for which governorates were selected: governorates are second‐ and third‐ranked among the 14 governorates implementing the ESN in terms of absolute numbers of food‐insecure people. In addition, Hajjah and Ibb have high percentages of food‐insecure people (Hajjah 46.3% and Ibb 44.0%, according to the 2009 CFSS), as well as relative stability and implementation feasibility (WFP‐CO Yemen 2011a). Exclusion criteria: NR Pretreatment: comparing the food and cash treatment groups, the randomisation appeared to function reasonably well. In terms of HH demographics, food HHs appeared relatively more likely to be headed by females and singles, although the education levels of the HH head did not significantly differ. In terms of assets, cash HHs appeared to be slightly more likely to have more telephones and own their plot of land, and they had a Wealth Index Level 0.09 SDs higher than food HHs. These differences were relatively small in magnitude, but significant at the 10% level, implying that controlling for baseline SES in the main analysis would improve the accuracy of estimated treatment effects. Note: the baseline characteristics below were taken from Table 2. (Table 3 could also have been chosen: subsample only. However, text with respect to Table 3 seemed not in line with what is represented in Table 3.) Furthermore, comparisons of means of key outcome variables at baseline were only presented for treatment (food and cash) vs comparison. Attrition per relevant group: data for 183 HHs excluded from analysis (5% of baseline sample): of the 183 HHs in the original sampling frame not included in this analysis, only 26 were omitted due to pure attrition. These 26 HHs had moved away from their location during the baseline survey, and were unable to be interviewed for the endline survey. The majority of these HHs originally resided in the Al‐Wahdah FDP in Hajjah, and were forced to move due to ongoing tribal violence, but these HHs were not included because multiple beneficiaries lived in the same HH. The remaining HHs not considered here had extensive incomplete, missing or unreliable data for key sections. Attrition per group was NR. Furthermore, for outcomes that relied on a recall period including the week before the survey (e.g. days in the last 7 the HH consumed meat), the analysis excluded those HHs that received their transfer in the 8‐day period before the survey. However, they stated that as a whole, the summary statistics did not suggest that selecting the subsample of food HHs who received the transfers > 8 days from survey time introduces discernible bias into the analysis. Description of subgroups measured and reported: dietary diversity in infants and young children: aged 6–23 months and 24–59 months Total number completed and analysed per relevant group: 1581 HHs analysed. Numbers per group NR. Total number enrolled per relevant group: total: 1983 HHs; cash group: 1001 HHs; food group: 982 HHs. Total number in baseline table 1 of publication showed 3355 HHs (this may have included a comparison group that is sometimes mentioned but this was unclear). Total number randomised according to text was 3536. Total number randomised per relevant group: total: 1983 HHs; cash group: 1001 HHs; food group: 982 HHs. Total number in baseline table 1 of publication showed 3355 HHs (this may include a comparison group that is sometimes mentioned but this was unclear). Total number randomised according to text was 3536. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Food expenditure Food security: days in the past week that HHs/adults/children were required to reduce the amount of food consumed at or frequency of meals consumed; months in the previous 6 that HHs had difficulty satisfying their food needs Dietary diversity: HDDS (number of distinct food categories consumed by the HH in the previous 7 days); probability of having a low FCS (< 28.5) |
|
| Identification |
Sponsorship source: government of Spain. Country: Yemen Setting: poor HHs in rural communities in poorest districts in Yemen Author's name: Benjamin Schwab Email: b.schwab@cgiar.org Declarations of interest: NR Study or programme name and acronym: NR Type of record: report |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Unclear risk | Not described how randomisation was conducted other than (quote) "In the intervention under study, 136 village clusters (known as Food Distribution Points) were randomly assigned to receive either food or cash assistance." |
| Allocation concealment (Selection bias) | Low risk | Allocation was at cluster level, by FDP. |
| Baseline characteristics similar (Selection bias) | Unclear risk | There were many disparities in baseline characteristics between the groups. Unclear whether these had been adjusted for in all analyses. Comparing the food and cash treatment groups, the randomisation appeared to function reasonably well. In terms of HH demographics, food HHs appeared relatively more likely to be headed by a females and singles, although the education levels of the HH head did not significantly differ. In terms of assets, cash HHs did appear to be slightly more likely to have more telephones and own their plot of land, and they have a Wealth Index Level 0.09 SDs higher than food HHs. These differences were relatively small in magnitude, but significant at the 10% level, implying that controlling for baseline SES in the main analysis will improve the accuracy of estimated treatment effects. With respect to the subgroup: comparing those included and those excluded within the food treatment group (Table 3), it becomes clear that while the excluded group was slightly more likely to come from Hajjah, differences in other indicators were generally not significant economically and statistically. The lone exception was that the excluded group had higher motor vehicle ownership rates (5% vs 1%), and slightly higher wealth index levels (not statistically significant). As a whole, the summary statistics did not suggest that selecting the subsample of food HHs who received the transfers > 8 days from survey time introduced discernible bias into the analysis. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | Despite the fact that the main analysis was comparing the food and cash transfers, the comparison of baseline outcome measures was only presented for treatment (food and cash) vs comparison (Table 5). The baseline data were not true baseline as the food transfer group had already received the first transfer. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding was possible, but this was unlikely to influence the delivery of the intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | Blinding was not possible. Unclear who the outcome assessors were. Some outcomes were self‐reported and could thus have been influenced by the knowledge of treatment allocation, especially as preferences for cash vs food among participants varied from baseline to endline, with majority preferring cash at endline. |
| Protection against contamination (Performance bias) | Low risk | Communities were randomised. Could only get the relevant intervention when having the correct ID. |
| Incomplete outcome data (Attrition bias) | High risk | 183 HHs were excluded from the analysis (5% of baseline sample). At the HH level, there was high attrition: the number analysed was 1581/1983 at baseline (20%). The numbers missing/excluded per group were not provided. |
| Selective outcome reporting (Reporting bias) | Unclear risk | The paper outlining the methods could not be accessed. Authors did clearly report all the outcomes of interest in the methods section of the report. |
| Other bias | High risk | There might have been bias introduced due to the differences in the timing of the interventions. Quote: "changes in timing of the survey and distribution schedule resulted in the loss of a pure pre‐intervention survey, as the baseline survey occurred after the first food transfer (but before the first cash transfer). Ideally, the disbursement schedules should be identical so that differences in impact can be attributed to difference between the modalities rather than differences in seasonal or other environmental factors influencing budgeting and resource flows within the household, or discrepancies in the period between transfer receipt and survey measurement." Misclassification bias of exposure: low risk. Measurement bias: unclear. It is unclear who collected data and how it was done. Incorrect analysis: low risk. Analyses were adjusted for clustering. Misclassification bias of exposure: low risk. Measurement bias: unclear. Unclear who collected data and how it was done. Incorrect analysis: low risk. Analyses were adjusted for clustering. |
Skoufias 2013.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel How were missing data handled? Missing data were excluded from analysis. Sample of HHs used for the analysis of consumption was what remained after dropping HHs with food consumption < 1 percentile and > 99 percentile of the food distribution in the sample. An additional 802 HHs were excluded from the analysis because of missing or incomplete data (Leroy 2010). Analyses provide an estimate of ITT effect of in‐kind and cash transfers. Randomisation ratio: 1:1:1:1 Recruitment method: NR Sample size justification and outcome used: sample size was calculated so that statistical tests had the power to detect statistically significant and biologically relevant differences in several nutritional and economic variables. Specifically, the calculations of the sample size prior to the baseline survey were based on 60 communities per treatment group, a power of 80%, and a minimum detectable difference in food per capita consumption between each treatment and control group of 17.8%. The final sample consisted of 33 HHs per community and around 52 communities per treatment group (ICC 0.220) (Skoufias 2013). Sampling method: 2‐stage random sampling. A random sample of 208 rural communities was drawn from a pool of communities within 8 of the poorest states in the Southeast region. Within each community, 33 HHs were selected using systematic random sampling. After baseline data collection, the 208 selected communities (6687 HHs) were randomly assigned to 1 of 4 study groups: food basket without education (52 communities, 1657 HHs), food basket with education (52 communities, 1680 HHs), cash transfer with education (53 communities, 1687 communities) or control (51 communities, 1663 HHs). Due to partial contamination of the original evaluation design the analysis pools both in‐kind/food basket groups. Study aim or objective: to examine the impacts of cash and in‐kind transfers on HH welfare as measured by food and total consumption, poverty and labour supply (Skoufias 2008; 2013). To estimate the programme's impact on HH energy and macro‐ and micronutrient consumption and to evaluate whether the cash and in‐kind transfers had a differential effect on these outcomes (LeRoy 2010). Study period: delivery of the PAL benefits began in June 2004 and the mean time of exposure to the availability of the programme transfers was 14 months. Unit of allocation or exposure: communities |
|
| Participants |
Baseline characteristics Intervention (cash transfer)
Control
Overall
Inclusion criteria: HHs eligible for PAL (localities had to meet some requirements such as having a population of < 2500, having a high or very high marginality and being accessible (not > 2.5 km from a road), and close enough (not > 2.5 km) to a DICONSA store (Mexican Government's agency that distributes the supply of food). Exclusion criteria: NR Pretreatment: the occasional significance of some variables indicated that the random assignment did not manage to balance totally the sample across the treatment and control groups, especially with respect to HH consumption (Table A.1). However, DID analysis accounted for this imbalance. In Leroy 2010, baseline nutrient intakes in cash transfer and control groups were similar. Attrition per relevant group: intervention group (cash transfers with education): 195/1687 (11.6%); control group: 279/1663 (16.8%). Total attrition: 864/6687 (13%) HHs. Reasons for attrition not provided, except for 1 cluster (33 HHs) in the control group and another in food basket without education group, that refused to participate in the follow‐up survey. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: full data were thus available for 5823 HHs (food basket without education: 51 communities, 1447 HHs; food basket with education: 52 communities, 1500 HHs; cash transfer with education: 53 communities, 1492 HHs; control: 50 communities, 1384 HHs) (Leroy 2010). Total number enrolled per relevant group: the data use were based on a longitudinal sample of 5851 HHs in 206 poor rural localities from 6 southern Mexican states (Chiapas, Guerrero, Oaxaca, Quintana Roo, Tabasco and Veracruz). Numbers per group NR. Total number randomised per relevant group: after baseline data collection, the 208 selected communities (6687 HHs) were randomly assigned to 1 of 4 study groups: food basket without education (52 communities, 1657 HHs), food basket with education (52 communities, 1680 HHs), cash transfer with education (53 communities, 1687 HHs) or control (51 communities, 1663 HHs) (Leroy 2010). |
|
| Interventions |
Intervention characteristics Intervention (cash transfer)
Control: no intervention |
|
| Outcomes | Dietary diversity: proportion of children with MDD (consumed foods from ≥ 3–6 food groups) Diet intake: consumption of iron‐rich or iron‐fortified foods Anthropometry: BMI |
|
| Identification |
Sponsorship source: Mexican government Country: Mexico Setting: poor rural HHs in Southern states of Mexico Author's name: Emmanuel Skoufias Email: eskoufias@worldbank.org Declarations of interest: no conflicts of interest (Leroy 2010). Study or programme name and acronym: Programa de Apoyo Alimentario (PAL) (food support programme) Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "Localities were randomised into four groups using a simple randomisation algorithm" (Cunha 2014). |
| Allocation concealment (Selection bias) | Low risk | Allocation was at location level (clusters), carried out by the Ministry of Social Development after baseline data collection. |
| Baseline characteristics similar (Selection bias) | Low risk | Although there were some differences between characteristics at baseline, the DID analysis adjusted for these. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Baseline nutrient intakes in both groups were similar (Leroy 2010). Although HH food expenditure was less in the intervention group at baseline (P < 0.1) (Addendum A, Skoufias 2013), the data were analysed with DID methods which adjusts for pre‐existing baseline differences. |
| Blinding of participants and personnel (Performance bias) | Low risk | Blinding was not possible due to the nature of the intervention. This was unlikely to influence behaviour of participants and personnel. |
| Blinding of outcome assessment (Detection bias) | Low risk | Quote: "To avoid potential interviewer bias, field workers were, to the extent possible, unaware of the group assignment." |
| Protection against contamination (Performance bias) | Unclear risk | Allocation was done at the community level; however, there was no information about whether communities in control group received either intervention. Cunha 2014 reported that 1 control HH reported receiving aid. |
| Incomplete outcome data (Attrition bias) | High risk | 11.6% attrition in the intervention group and 16.8% in the control group. 1 cluster lost as 1 community in the control group refused to participate in the follow‐up survey (33 HHs). The study authors reported that HHs excluded from the analyses tended to live in smaller houses than those included (2.48 vs 2.77 rooms; P < 0.05). Nutrient consumption at baseline was higher in excluded HHs, but no details were reported. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No study protocol available. |
| Other bias | Unclear risk | Misclassification bias: unclear risk. Receipt of cash transfers were self‐reported in 1 paper (Cunha 2014), but NR as such in other papers. Measurement bias: low risk. Trained field workers interviewed the homemaker at baseline and follow‐up (semi‐quantitative FFQ questionnaire of 61 food items consumed at home in the 7 days prior). Incorrect analysis: unclear risk. SEs were corrected for clustering of individuals at the village level in Skoufias 2013, but adjusting for clustering NR in Leroy 2010. Recruitment bias: low risk. Participants were recruited after allocation of locations (clusters), but were randomly sampled in each location. Seasonality bias: low risk. The month of data collection was included to adjust for the possible effect of seasonality on consumption. |
Sturm 2013.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? NR. It is unclear how many HHs had incomplete data at follow‐up. Data were analysed as monthly observations for each HH. Randomisation ratio: N/A Recruitment method: N/A Sample size justification and outcome used: NR Sampling method: HHs enrolled in Discovery Vitality used the Discovery visa credit card for purchases at pick n pay supermarkets. Scanner data from Pick n Pay for credit card purchases from November 2009 to March 2012 were linked to 169,485 HHs. Study aim or objective: to examines the effect of a price reduction for healthy food items on HH grocery shopping behaviour among members of South Africa's largest health plan. Study period: 28 months: November 2009 to March 2012 Unit of allocation or exposure: HHs |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: all Vitality members were eligible for the healthy food benefit at no additional cost to them, but they had to activate the benefit online or by telephone. Only purchases made with a Visa credit card issued by Discovery were analysed, as this was the only identifying information for purchases for which there was no rebate. Exclusion criteria: none reported Pretreatment: HHs who became eligible for a rebate during the study period already had a larger proportion of overall food expenditure going towards healthy foods and a smaller proportion towards less desirable foods at baseline (when nobody was eligible for the rebate) than HHs that never participated in the programme. Participants also lived closer to a Pick n Pay supermarket than to a competing supermarket; the opposite was true for non‐participants. The difference between non‐participants and participants was significant for all variables. Attrition per relevant group: NR Description of subgroups measured and reported: effects for all shoppers vs nearby shoppers (those living ≥ 1 km closer to nearest Pick n Pay supermarket relative to nearest Shoprite or Woolworths supermarket) Total number completed and analysed per relevant group: total: 169,485 Discovery visa holders; intervention (HealthyFood benefit): 100,344 (10% rebate); 67,343 (25% rebate); control (non‐participants): 69,141 Total number enrolled per relevant group: total: 169,485. Discovery visa holders; intervention (HealthyFood benefit): 100,344 (10% rebate); 67,343 (25% rebate); control (non‐participants): 69,141 Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control: no intervention |
|
| Outcomes | Proportion of HH expenditure on food: ratio of healthy to total food expenditure for 10% rebate; ratio of healthy to total food expenditure for 25% rebate; ratio of fruit and vegetables to total food expenditure for 10% rebate; ratio of fruit and vegetables to total food expenditure for 25% rebate; ratio of less desirable food to total food expenditure in a HH for 10% rebate; ratio of less desirable food to total food expenditure in a HH for 25% rebate. | |
| Identification |
Sponsorship source: National Cancer Institute (grant R21CA161287); the National Institute of Child Health Human Development (grant R21HD071568); and the Anne and James Rothenberg Dissertation Award, 2011–2012. Country: South Africa Setting: supermarkets Author's name: Roland Sturm Email: sturm@rand.org Declarations of interest: yes; no financial disclosures. Study or programme name and acronym: HealthyFood programme Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA, where participants self‐selected into intervention. |
| Allocation concealment (Selection bias) | High risk | CBA. |
| Baseline characteristics similar (Selection bias) | Unclear risk | Intervention HHs lived closer to a Pick and Pay supermarket than controls. Other sociodemographic characteristics NR. The authors used a DID analysis with matched HHs but, since no characteristics were reported, it was not possible to assess baseline imbalance. |
| Baseline outcome measurements similar (Selection bias) | High risk | Study authors reported that the expenditure on healthy food as a ratio of total expenditure was higher in the intervention HHs than in the controls. |
| Blinding of participants and personnel (Performance bias) | Low risk | Intervention was assessed based on sales data as part of participants' usual grocery shopping behaviour. |
| Blinding of outcome assessment (Detection bias) | Low risk | Outcome was measured using scanner data from supermarkets, therefore, blinding unlikely to influence these outcomes. |
| Protection against contamination (Performance bias) | Low risk | Non‐participants could not have benefited from the intervention (rebates) as they were not registered to receive benefits. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Missing or excluded data among scanner data collected NR. |
| Selective outcome reporting (Reporting bias) | Unclear risk | No protocol available. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Linked with use of Vitality credit card. Measurement bias: unclear. Potential bias due to use of scanner data which may not be representative of total purchasing behaviour. Seasonality bias: unlikely. Seasonality in grocery shopping patterns were controlled for with a set of dichotomous variables for each specific month in a year. |
Tonguet Papucci 2015.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? influence of missing data assessed using a sensitivity analysis using multiple imputation to account for missing values. Children without ≥ 2 measurements or excluded from the analysis. Authors employed ITT analysis. Randomisation ratio: 1:1 (16 control villages and 16 intervention villages) Recruitment method: initial recruitment by approaching a village representative (normally village head and his/her committee) to obtain consent for participation of village following an explanation of aims of research. Individual informed consent then sought from individual HH representatives (usually mothers) following explanation of research aim, sequence of activities and procedures, and risks and benefits of participation. Sample size justification and outcome used: Houngbe: type I error of 5%, a statistical power of 90% and a minimum follow‐up time of 24 months, assuming a 33% reduction in the cumulative incidence of wasting, a coefficient of variation K of 0.25 and an anticipated 25% dropout, 16 clusters with 50 children were required in each study group. Tonguet‐Papucci: to detect a decrease with 33% in the cumulative incidence of wasting assuming a baseline incidence rate of wasting of 0.26 per child‐year with a Type I error of 5%, a statistical power of 90% and a minimum follow‐up of 24 months, assuming a coefficient of variation K of 0.25, 16 clusters of 50 HHs per cluster were necessary per study group. This calculation accounted for an anticipated 25% drop‐out. Sampling method: villages randomly assigned to intervention and control groups during a ceremony to keep the allocation of cash transparent and fair. Representatives of each of 32 villages drew blindly from a bag 1 of the 32 identical papers with 'cash' or 'no cash' written on it. Within villages, HH participation in study was voluntary and based on inclusion criteria. How 32 villages in 3 municipalities were selected was NR. Study aim or objective: Houngbe: "to assess the impact of a cash transfer programme in reducing the incidence of acute malnutrition and morbidity and the prevalence of stunting in children aged 36 months. Study period: June 2013 to October 2015 Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics Intervention or exposure
Control
Overall: NR Inclusion criteria: HHs classified as poor or very poor according to the Household Economy Approach; with ≥ 1 child aged < 1 year at time of inclusion, regardless of nutritional status; children with ≥ 2 follow‐up measurements. Exclusion criteria: NR Pretreatment: overall, baseline characteristics were balanced between groups. Children in intervention group were more likely to be 1 month younger and more wasted than children in the control group. Attrition per relevant group: Houngbe 2017: intervention group: 2.2% (14/644) of children; control group: 2.2% (14/634) of children. Intervention: 14 children LTFU at visit 2 (12 deaths and 2 left study area); excluded from analysis. Additional LTFU: 43 children LTFU between visits 3 and 9 (reasons: 35 deaths; 8 left study area); control: 14 children LTFU at visit 2 (10 deaths, 4 wrongly included); excluded from analysis. Additional LTFU: 28 LTFU between visits 3 and 9 (reasons: 22 deaths; 6 left study area). Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: intervention: 630 children analysed; control: 620 children analysed Total number enrolled per relevant group: Houngbe 2017: intervention: 644 children from 602 HHs; control: 634 children from 583 HHs. Total number randomised per relevant group: total 1278 children from 32 villages randomised; intervention: 644; control: 634. |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control
|
|
| Outcomes | Dietary diversity: DDS; MDD; minimum acceptable diet; proportion consuming iron‐rich or iron‐fortified foods Anthropometry: incidence of wasting; HAZ; WHZ; incidence of stunting; MUAC Morbidity: incidence diarrhoeal disease; incidence ARIs |
|
| Identification |
Sponsorship source: Houngbe et al 2017: Action Against Hunger France and the CDC, European Commission's Humanitarian Aid and Civil Protection department, USAID (through the Technical Operational Performance Support programme) and Foundation Action Against Hunger (France) for research and innovation supported research uptake and the dissemination of results. The cash transfer programme was funded by European Commission's Humanitarian Aid and Civil Protection department. 1 study author supported by the CGIAR Research Program on Agriculture for Nutrition and Health (A4NH), led by the International Food Policy Research Institute. Tonguet‐Papucci: study funded by Actino Contre la Faim – France and the Center for Disease Control. The cash transfer programme was made possible thanks to ECHO funds. The cost‐effectiveness analysis is co‐funded by Action Contre la Faim and the Nutrition Embedding Evaluation Program (NEEP, PATH‐DFID). Country: Burkina Faso Setting: poor and very poor rural HHs in eastern Burkina Faso Comments: registered at clinicaltrials.gov as NCT01866124. Authors' names: F Houngbe; A Tonguet‐Papucci Email: fhoungbe@actioncontrelafaim.org; apapucci@actioncontrelafaim.org Declarations of interest: yes; Houngbe: "J‐FH, LH, and PK, no conflicts of interest. FH, AT‐P, CA, and MA‐A are employed by Action Against Hunger France, which implemented the MAM'Out study." Tonguet‐Papucci: "The authors declare that they have no competing interests." Study or programme name and acronym: Moderate Acute Malnutrition Out (MAM'Out) research project/study Type of record: Houngbe: journal article. Tonguet‐Papucci: study protocol |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "Villages were randomly assigned to the intervention and control groups during a ceremony in order to keep the allocation of cash transparent and fair. Representatives of each of the 32 villages drew blindly from a bag one of the 32 identical papers with "cash" or "no cash" written on it." |
| Allocation concealment (Selection bias) | Low risk | Allocation to intervention groups was by village at the beginning of the study. |
| Baseline characteristics similar (Selection bias) | Low risk | Quote: "Overall, baseline characteristics were balanced between the intervention and the control groups (Table 1)." Comment: intervention group had more young children (aged < 6 years) compared to control group but all analyses adjusted for child's age at baseline. In addition, Houngbe 2017 reported that adjustment had been done for important prognostic covariates. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Children in intervention group were more likely to be wasted. No morbidity outcomes measured at baseline. Analysis adjusted for morbidity status and WHZ at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding possible but this was unlikely to affect participant behaviour. |
| Blinding of outcome assessment (Detection bias) | High risk | Outcome assessors were not blinded to treatment assignment. Morbidity outcomes were recalled by mothers and these could have been influenced by knowledge of treatment allocation. |
| Protection against contamination (Performance bias) | Low risk | Allocation was by village and it was unlikely that control villages received treatment. Given the cluster randomised design of the study combined with poor and very poor participants who likely did not travel to other villages often, the risk of contamination was not judged to be appreciable. |
| Incomplete outcome data (Attrition bias) | Low risk | Attrition was not high: 99/1278 (7.8%) children enrolled LTFU, due to either death or leaving the study area. 57/644 (8.9%) children in intervention group and 42/634 (6.6%) children in control group LTFU from visits 1 to 9. Data from children with < 2 measurements were excluded: 14 (2.2%) children in intervention group (2.2%) and 14 (2.2%) children in control group were excluded. |
| Selective outcome reporting (Reporting bias) | High risk | Some morbidity outcomes reported in the protocol were NR in published paper (oedema and measles). |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unlikely. Incorrect analysis: unclear. Adjusted for clustering. Poisson regression model adjusted for clustering by village, household and child. The payment ('compensations') for the time control participants spent on the study may have resulted in volunteer bias, which may have altered effect sizes. Furthermore, the payment in itself was not meaningfully different from the intervention (though no values were specified) and may have influenced outcomes as well. |
Verbowski 2018.
| Study characteristics | ||
| Methods |
Study design: cRCT Study grouping: parallel group How were missing data handled? In 9 cases, the participant who had been enrolled at baseline was N/A at the time of data collection; so another adult female HH member of the appropriate age completed the 24‐hour recall. When nutrient values were N/A for protein, fat, iron, zinc, calcium, vitamin A, thiamine or riboflavin, values were imputed from USDA food composition equivalents, based on values per 100 g by weight (USDA 2016). Given the high attrition rates, instead of estimating missing data using multiple imputation, study authors employed the direct maximum likelihood method to account for the missing values at 22 months, which uses each respondent's available data to compute the likelihood function. The overall likelihood was the product of 2 factors: 1 computed for those respondents with missing data on some variables and 1 for those with complete data on all variables. Parameter estimation and SEs were derived from maximising the overall likelihood function. Randomisation ratio: 1:1:1 Recruitment method: among the eligible villages (190, which were those not already participating in other development programmes), random selection was used to identify 90 villages to participate in the study. Sample size justification and outcome used: number of clusters and HHs within each cluster was estimated based on the proportion of anaemic women and children, with 80% power and an a priori significant level of 0.025, to account for multiple comparisons. Assuming a 50% prevalence of anaemia and an interclass correlation of 0.05, a sample size of 300 for each group provided 80% power to detect a 15% absolute reduction in the prevalence of anaemia. Sampling method: with randomised villages, purposive sampling was used to identify 10 HHs per village to participate. Half of the participants (5/10 HHs within each cluster) were randomly selected to complete endline dietary assessment. Study aim or objective: to examine the effect of EHFP with or without aquaculture on dietary intake and prevalence of inadequate intake of select nutrients among women and children living in rural Cambodia, compared to controls. Study period: July 2012 to June 2014, a 22‐month period Unit of allocation or exposure: villages |
|
| Participants |
Baseline characteristics EHFP + aquaculture
EHFP
Control
Overall: NR Inclusion criteria: Within each village, 10 HHs were purposefully selected, according to specific criteria: HH home to a woman of childbearing age, considered poor based on local wealth rankings, had access to sufficient land and labour, had Ͱ 1 child aged < 5 years, and the woman was interested in participating in the FoF project. Exclusion criteria: NR Pretreatment: no significant differences between groups (P > 0.05), except for years of education and wealth quintiles were not equally distributed across groups; women on average had completed more years of schooling in the EHFP group than in the EHFP + aquaculture and control groups, and more HHs in the control group were in the bottom Wealth Index quintile as compared with HHs in the EHFP and EHFP + aquaculture groups. Therefore, these were included in the multivariable models as potential confounders. Attrition per relevant group: EHFP + aquaculture group: 7 women and 7 children LTFU; EHFP group: 4 women and 4 children LTFU; control group: 10 women and 10 children LTFU. The overall HH attrition rate was 16.2% (146), which did not differ across groups (P = 0.74), but attrition for women overall was higher (38.6%, 348), mainly due to employment‐related temporary migration. Primary outcome data were available for 179 (control), 185 (EHFP) and 188 (EHFP + aquaculture) women and 232 (control), 255 (EHFP) and 245 (EHFP + aquaculture) children. Venous blood samples were successfully obtained from 88% of the subset of 450 women at 22 months. LTFU for the venous blood draw was higher among women in control group (22.0%, 33) than in the EHFP (6.7%, 10) and EHFP + aquaculture (6.0%, 9) groups. Description of subgroups measured and reported: only a subgroup of participants measured and analysed per group: of the 10 HHs per village, only 5 per group were randomly selected to be assessed for dietary intake outcomes and analysed as such. Of these, further subgroups (43 woman–child pairs for EHFP + aquaculture group; 45 woman–child pairs for EHFP group; 46 woman–child pairs for the control group) were selected to do a repeat dietary intake assessment on a non‐consecutive day. Total number completed and analysed per relevant group: EHFP + aquaculture group: 143 women and 142 children analysed; EHFP group: 146 women and 144 children analysed; control group: 140 women and 135 children analysed. Total number enrolled per relevant group: each group had 30 villages randomly assigned to them, and from each village 10 HHs were enrolled, which provided per group: 300 HHs, 300 women (of which 150 women's venous blood samples were taken), 300 children Total number randomised per relevant group: see above |
|
| Interventions |
Intervention characteristics EHFP + aquaculture
EHFP
Control: no intervention |
|
| Outcomes | Dietary intake: prevalence of inadequacy of food intake in women/children Anthropometry: underweight (mothers/children); stunting Biochemical: Hb concentration (women/children) Morbidity: anaemia (women/children) |
|
| Identification |
Sponsorship source: International Development Research Centre (IDRC, grant number 106928) and Global Affairs Canada (GAC); HKI; University of British Columbia (UBC) Country: Cambodia Setting: villages in the rural Prey Veng Province, 1 of the poorest provinces with 27% of homes classified as poor, and located on the east bank of the Mekong river. Comments: trial registry number: NCT01593423 Authors' names: Susan Barr and Tim Green Email: susan.barr@ubc.ca; tim.green@sahmri.com Declarations of interest: yes; no conflicts of interest Study or programme name and acronym: Fish on Farms (FoF) project using the Enhanced Homestead Food Production (EHFP) programme Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | Low risk | Quote: "Random allocation was done by the study coordinator in Cambodia using a computer generated random number sequence in Excel." |
| Allocation concealment (Selection bias) | Unclear risk | NR |
| Baseline characteristics similar (Selection bias) | Low risk | Baseline characteristics of participants per group were reported and mostly similar, except for it appeared that years of education and wealth quintiles were not equally distributed across groups; women on average had completed more years of schooling in the EHFP group than in the EHFP + aquaculture and control groups, and more HHs in the control group were in the bottom Wealth Index quintile as compared with HHs in the EHFP and EHFP + aquaculture groups. Because these were included in the multivariable models as potential confounders, we judged this domain at low risk of bias. |
| Baseline outcome measurements similar (Selection bias) | Unclear risk | The study authors reported it a limitation of their study, that baseline dietary intake data were not collected. Although most baseline characteristics were similar across groups, the years of education and bottom Wealth Index (which were included in the multivariable models as possible confounders) were not, and it is also not certain that dietary intake data were similar across groups at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | No blinding, but it was unlikely that the performance were influenced by lack of blinding. |
| Blinding of outcome assessment (Detection bias) | High risk | No blinding done. It is possible (but unknown) whether outcome assessors behaved differently when interviewing women from different groups (e.g. prompting women from different groups differently during facilitating the 24‐hour recall). The dietary intake of women and children was self‐reported, thus there was also a possibility that a lack of blinding of participants could have influenced their recall and outcome reporting. |
| Protection against contamination (Performance bias) | Low risk | Allocation was by village and it was unlikely that the control group received the intervention, or that the group with only the EHFP also received the aquaculture. |
| Incomplete outcome data (Attrition bias) | Unclear risk | Quote: "At the end of the study, there were no missed clusters (n = 90). The overall HH attrition rate at 22 months was 16.2% (n = 146) and did not differ across groups (P = 0.74…). Attrition was higher for women only (38.6%; n = 348) than for households …" Comment: because the total attrition was high, study authors used the direct maximum likelihood method to account for the missing values at 22 months. However, no sensitivity analysis was done and we are unclear as to how this method influenced the findings. |
| Selective outcome reporting (Reporting bias) | Low risk | The trial was prospectively registered on a trial registry website (NCT01593423). All important outcomes pre‐specified in this registry entry have reported in either Verbowski 2018, Michaux 2018 or Karakochuk 2015. |
| Other bias | Low risk | Misclassification bias: low risk. Incorrect analysis: low risk as clustering was taken into account adequately during analysis. Recruitment bias: low risk because participants in relevant villages were recruited before randomisation took place. |
Weinhardt 2017.
| Study characteristics | ||
| Methods |
Study design: PCS How were missing data handled? missing data for the analysis of the particular outcome were excluded, but the HH with missing data were retained and all other observations were included. Randomisation ratio: N/A Recruitment method: NR Sample size justification and outcome used: study's statistical power was determined for the primary HIV sexual risk outcome and the primary food security outcome. The sample size was 598 for the control group and 301 for the intervention group. The study authors stated that effect sizes (d) were used in the calculation, but did not report any values. Sampling method: selected HHs in 3 intervention TAs received the intervention, compared with those in 3 non‐intervention TAs (matched for demographics and distance from urban centre. Study aim or objective: to evaluate the impact of a large‐scale multilevel economic and food security intervention on health outcomes and HIV vulnerability in rural Malawi. Study period: 2009–2012 Unit of allocation or exposure: TAs |
|
| Participants |
Baseline characteristics Intervention or exposure group:
Control group:
Overall: NR Inclusion criteria: NR Exclusion criteria: NR Pretreatment: participants in intervention group were older, had smaller HHs and the HHs were less dominated by males. The intervention group and control group had significant differences in income sources (P = 0.025), and practice/applying sustainable agriculture methods. Higher number of HHs with malnourished children in the control group (22%) compared to intervention group (14.8%). Attrition per relevant group: total attrition was 5.7% (34/598) in the intervention group and 12.6% (38/301) in the control group. No differential attrition was detected for the study conditions, or between HHs who attrited and those who did not. Attrition per outcome: for reported HIV testing and self‐reported HIV status there was no additional attrition; for food security there was no additional attrition with the exception of groundnut consumption (0.2% for intervention and 0.4% for control) and HH food security (0.4%, control only); for reduction of amount/number of meals to cope with food shortage additional attrition was 29.4% for intervention and 27.4% for control; and for child anthropometric measurements additional attrition was 25.5% for intervention and 19.0% for control. Description of subgroups measured and reported: NR Total number completed and analysed per relevant group: intervention group (SAFE intervention group): 564 HHs; control group: 263 HHs Total number enrolled per relevant group: intervention group (SAFE intervention group): 598 HHs; control group: 301 HHs Total number randomised per relevant group: N/A |
|
| Interventions |
Intervention characteristics Intervention or exposure
Control group:
|
|
| Outcomes | Food security: mean number of months with less food than necessary to meet needs Dietary intake: self‐reported types of foods consumed in past 3 days Anthropometry: WAZ, HAZ, % malnourished, child BMI |
|
| Identification |
Sponsorship source: National Institutes of Health, Eunice K. Shriver National Institute of Child Health and Human Development grant R01‐HD055868 (2008–2015). Country: Malawi Setting: poor HHs in rural areas Author's name: Lance S Weinhardt Email: weinhardt@uwm.edu; yanf@uwm.edu Declarations of interest: yes; no conflicts of interest. Study or programme name and acronym: Study name: Savings, Agriculture, Governance, and Empowerment for Health (SAGE4‐Health); Programme name: Support to Able‐Bodied Vulnerable Groups to Achieve Food Security (SAFE). Type of record: journal article |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (Selection bias) | High risk | CBA study; no randomisation. |
| Allocation concealment (Selection bias) | High risk | CBA study; no allocation concealment. |
| Baseline characteristics similar (Selection bias) | Low risk | Intervention HHs had significantly older respondents (P = 0.040), and significantly smaller HHs (P = 0.001) and higher likelihood of being male‐headed (P = 0.039). These factors were treated as covariates in the assessment of intervention effects. |
| Baseline outcome measurements similar (Selection bias) | Low risk | Proportion of food insecure HHs was similar between groups at baseline. |
| Blinding of participants and personnel (Performance bias) | Low risk | There was no blinding but outcomes unlikely to be influenced by lack of blinding of participants or personnel administering the intervention. |
| Blinding of outcome assessment (Detection bias) | High risk | Most outcomes were self‐reported and knowledge of treatment allocation, due to lack of blinding, could have influenced outcome assessment. Objective anthropometric measurements were included and unlikely to be influenced by blinding. |
| Protection against contamination (Performance bias) | Low risk | Contamination was assessed and it was found that no control participants received any components of the intervention. |
| Incomplete outcome data (Attrition bias) | High risk | Low attrition overall that was differential (Intervention vs control: 5.7% vs 12.6%), but higher attrition for outcomes such as reduction of number/amount of meals during shortage (33.4% vs 36.5%) and child anthropometric measurements (29.8% vs 29.2%); however these were balanced between the groups. |
| Selective outcome reporting (Reporting bias) | Low risk | Study protocol and methods available. All a priori stated outcomes in the methods sections were reported on in the results section. |
| Other bias | Unclear risk | Misclassification bias: unlikely. Measurement bias: unlikely. Seasonality bias: unclear. Baseline survey conducted during 2009. No details reported in terms of the time period of data collection. The study authors did not specify that the month of data collection was included in their analysis to adjust for the possible effect of seasonality on consumption. |
(?): not clear in report; AAY: Antyodaya Anna Yojana; ADRA: Adventist Development and Relief Agency; AE: adult equivalent; AM: Ajuda Mútua; APL: above poverty line; ARI: acute respiratory infection; BCC: behaviour change communication; BDH: Bono de Desarrollo Humano; BDT: Bangladeshi taka; BLT: unconditional cash transfer program; BMI: body mass index; BMIZ: body mass index‐for‐age z‐score; BPL: below poverty line; BPO: Bangladesh Post Office; BOS: school operational assistance program; CBA: controlled before‐after; CCG: child cash grant; CCT: conditional cash transfer; CDS: Child Diet Score; CES‐D: Center for Epidemiologic Studies Depression Scale; CFPR‐TUP: Challenging the Frontiers of Poverty Reduction – Targeting the Ultra Poor; CFSS: the paper doesn't provide full name ; CGP: Child Grant Programme; CI: confidence interval; CMC: community management committee; CNW: community nutrition worker; CNY: Chinese yuan; COP: Colombian peso; cRCT: cluster randomised controlled trial; CWAC: Community Welfare Assistance Committee; DDI: Dietary Diversity Index; DDS: Dietary Diversity Score; DfID: Department for International Development; ECHO: European Civil Protection and Humanitarian Aid Operations; DID: difference in differences; EHFP: enhanced‐homestead food production; EA: enumeration area; ECD: Early Childhood Development; ED: electoral division; EGP: Egyptian pound; EPA: extension planning area; ESD: enumerator subdistrict; ESDO: Eco‐Social Development Organization; ETB: Ethiopian birr; ETT: effect of treatment on the treated; F2F: farmer to farmer; FA: Familias en Acción; FAO: Food and Agriculture Organization; FCS: Food Consumption Score; FDC: food distribution committee; FDP: food distribution point; FDS: Food Diversity Score; FFS: Farmer Field School; FISP: fertiliser input subsidy programme; FSI: Food Security Index; GD: GiveDirectly; GDP: gross domestic product; GHQ‐12: 12‐item General Health Questionnaire; GPS: Global Positioning System; GVH: group village headmen; HAZ: height‐for‐age z‐score; Hb: haemoglobin; HC: health committee; HDDS: Household Dietary Diversity Score; HH: household; HFAIS: Household Food Insecurity Access Scale; HKI: Helen Keller International; HSNP: Hunger Safety Net Programme; IADB: Inter‐American Development Bank; ICC: intraclass correlation coefficient; IDDS: Individual Dietary Diversity Score; IDR: Indonesian rupiah; IFPRI: International Food Policy Research Institute; IGIDR: Indira Gandhi Institute of Development Research; IHS3: Integrated Household Survey 3; INR: Indian rupees; IQR: interquartile range; ITT: intention to treat; IYCDDS: Infant and Young Child Dietary Diversity Score; KBK: Kalahandi‐Balangir‐Koraput; KES: Kenyan shilling; LGA: local government authority; LPG: liquid petroleum gas; LSL: Lesotho loti; LTFU: loss to follow‐up; MASAF: Malawi Social Action Fund; MDD: minimum dietary diversity; MIS: management information system; MoSS: Ministry of Social Solidarity; MPCE: monthly per capita expenditure; MUAC: mid‐upper arm circumference; MUACZ: mid‐upper arm circumference z‐score; MWK: Malawian kwacha; MXN: Mexican peso; MZN: Mozambican metical; n: number of participants; N/A: not applicable/available; NGO: non‐governmental organisation; NIO: Nicaraguan córdoba; NPO: non‐profit organisation; NPR: Nepalese rupee; NR: not reported; NWG: non‐women's group; OLS: ordinary least squares; OWL: older women leader; PCS: prospective controlled study; PDS: Public Distribution System; PEN: Peruvian sol; PIM: Policies, Institutions and Markets; PHP: Philippine peso; PKH: Program Keluarga Harapan; PKR: Pakistani rupee; PM2A: Preventing Malnutrition in Children under 2 Approach; PMT: Proxy Means Test; POG: Pass‐on‐the‐Gift; pp: percentage point; PPSC: Post and Postal Savings Corporation; PSLSD: Project for Statistics on Living Standards and Development; PSM: propensity score matching; PSNP: Productive Safety Net Program; PSS: Perceived Stress Scale; PVDI: photovoltaic drip irrigation system; PWP: public works programme; RCT: randomised controlled trial; RDA: recommended daily allowance; RPS: Red de Protección Social; SAFE: Support to Able‐Bodied Vulnerable Groups to Achieve Food Security; SAR: South African rand; SCTS: Social Cash Transfer Scheme; SD: standard deviation; SE: standard error; SES: socioeconomic status; SFP: supplementary food programme; SMG: Solar Market Garden; TA: traditional authority; TASAF: Tanzania Social Action Fund; TCP: tratamiento con pago (treatment with payment); TKP: Takaful and Karama Program; TMRI: Transfer Modality Research Initiative; TRT: targeted resource transfer; TSP: tratamiento sin pago: treatment without payment; TVIP: Test de Vocabulario en Imagenes Peabody; UCT: unconditional cash transfer; UMKD: ; UNHCR: United Nations High Commissioner for Refugees; UNICEF: United Nations Children's Fund; UP: Union Parishad; UPP: Urban Poverty Program; USAID: United States Agency for International Development; USDA: United States Department of Agriculture; VC: village cluster; VDC: village development cluster; VMF: village model farm; VSL: village savings and loan; WAZ: weight‐for‐age z‐score; WDDS‐10: Women's Dietary Diversity Score; WEG: Women Empowerment Group; WFP: World Food Program; WFP‐CO: ; WG: women's group; WHO: World Health Organization; WHZ: weight‐for‐height z‐score; WINS: Women and Children/Infants Improved Nutrition in Sindh; WLZ: weight‐for‐length z‐score; XOF: West African CFA franc; YER: Yemeni rial; ZMW: Zambian kwacha.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abubakari 2014 | Wrong study design. |
| ACTRN12611001170910 | Ineligible setting; not LMIC (New Zealand). |
| Aker 2017 | Ineligible setting. |
| Akresh 2016 | Ineligible outcomes. |
| Alderman 2009 | Wrong intervention. |
| Alvarez 2008 | Wrong study design. |
| Amarante 2016 | Wrong study design. |
| Attanasio 2014 | Wrong study design. |
| Attanasio 2014a | Wrong intervention. |
| Ayala 2015 | Ineligible setting; not LMIC. |
| Ayele 2003 | Wrong study design. |
| Barber 2008 | Wrong study design. |
| Bazzi 2012 | Ineligible outcomes. |
| Behrman 2009 | Wrong outcomes. |
| Bezu 2014 | Wrong study design. |
| Bihan 2010 | Ineligible setting; not LMIC. |
| Bleich 2007 | Wrong study design. |
| Braido 2012 | Wrong study design. |
| Broutin 2006 | Wrong study design. |
| Buller 2016 | Wrong outcomes. |
| Cabral 2014 | Wrong study design. |
| Cardenas 2015 | Wrong study design. |
| Cluver 2018 | Ineligible intervention. |
| Cohen 2015 | Wrong patient population. |
| Dammert 2009 | Wrong outcomes. |
| Debela 2015 | Wrong study design. |
| Downs 2017 | Ineligible intervention. |
| ENN 2018 | Ineligible setting. |
| Fenn 2015_Niger | Wrong study design. |
| Fernald 2017 | Wrong intervention. |
| Fortin 2016 | Wrong outcomes. |
| Gelli 2017 | Ineligible intervention. |
| Gertler 2012 | Ineligible outcomes. |
| Gram 2019 | Ineligible outcomes. |
| Grellety 2017 | Ineligible participants. |
| Gutiérrez 2019 | Ineligible outcomes. |
| Haghparast‐Bidgoli 2019 | Ineligible intervention. |
| Haque 2017 | Ineligible outcomes. |
| Hardin Fanning 2014 | Wrong study design. |
| Huey 2019 | Ineligible intervention. |
| Idiaye 2014 | Wrong study design. |
| ISRCTN10323949 | Ineligible intervention. |
| ISRCTN77820875 | Ineligible study design. |
| Issaley 2013 | Wrong study design. |
| Jharendu 2014 | Ineligible outcomes. |
| Kagawa 2017 | Wrong intervention. |
| Kakuhikire 2016 | Wrong study design. |
| Kidoido 2015 | Wrong study design. |
| Kim 2012 | Wrong outcomes. |
| Kimenju 2015 | Wrong study design. |
| Kronebusch 2019 | Ineligible outcomes. |
| KumarGhosh 2011 | Wrong study design. |
| Lopez 2018 | Ineligible outcomes. |
| Loubser 2010 | Wrong study design. |
| Martins 2013 | Wrong study design. |
| Mascie Taylor 2010 | Wrong intervention. |
| NCT02558660 | Not conducted in a LMIC (USA‐based study). |
| NCT02577705 | Ineligible setting; not LMIC. |
| NCT02843178 | Ineligible setting; not LMIC (USA). |
| NCT03311698 | Ineligible intervention. |
| NCT04135625 | Ineligible intervention. |
| NCT04166370 | Ineligible intervention. |
| NCT04171999 | Ineligible participants. |
| Nisbett 2016 | Wrong study design. |
| Nsabuwera 2016 | Wrong study design. |
| Olajide‐Taiwo 2011 | Wrong outcomes. |
| Pasdar 2016 | Wrong study design. |
| Pereko 2017 | Ineligible intervention. |
| Perez Lu 2016 | Wrong study design. |
| Prifti | Ineligible outcomes. |
| Quiñones 2016 | Wrong study design. |
| Ragini 2017 | Ineligible intervention. |
| Rahman 2015 | Wrong outcomes. |
| Ramirez‐Silva 2013 | Wrong study design. |
| Roschnik 2017 | Ineligible intervention. |
| Roy 2019 | Ineligible outcomes. |
| Rutherford 2016 | Wrong study design. |
| Schultz 2001 | Wrong outcomes. |
| Schwab 2019 | Ineligible outcomes. |
| Sinharoy 2017 | Ineligible intervention. |
| Sudfeld 2019 | Ineligible intervention. |
| TorresSalcido 2015 | Wrong study design. |
| Wang 2012 | Wrong study design. |
| Young 2014 | Ineligible outcomes. |
| Zhang 2018 | Ineligible outcomes. |
LMIC: low‐ and middle‐income country.
Characteristics of studies awaiting classification [ordered by study ID]
ACTRN12618001803280.
| Methods | cRCT |
| Participants | Rural households of flood‐prone areas of Bangladesh |
| Interventions | Duck‐rearing intervention |
| Outcomes | Diet diversity |
| Notes | Unclear eligibility from information in trial registry |
ACTRN12618001975280.
| Methods | RCT |
| Participants | Pregnant women |
| Interventions | Unconditional cash transfers and mobile behaviour change communications |
| Outcomes | Changes in the percentage of stunted children (height‐for‐age < –2SD); mean cost per stunted child prevented Changes in the percentage of wasted children; household food security; birthweight |
| Notes | www.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12618001975280 |
Adubra 2017.
| Methods | cRCT |
| Participants | Pregnant women and children aged < 2 years |
| Interventions | Conditional cash transfer and nutritional supplementation |
| Outcomes | Stunting |
| Notes | Conference abstract |
Al‐serhan 2010.
| Methods | Retrospective cohort study Study used a panel data set on 74 Bedouin households in 3 villages in the Northern Badia of Jordan interviewed in 2001 and 2009 |
| Participants | Households in Northern Badia of Jordan |
| Interventions | Households received assistance through the development assistance programmes in the decade before 2006 |
| Outcomes | Factors enabling household to escape poverty |
| Notes | Full‐text could not be accessed |
Antwi 2013.
| Methods | Monitoring and evaluation study A structured questionnaire used to collect and analyse data from the project beneficiaries through face‐to‐face interviews. Livelihood of beneficiaries 'before and after' project was analysed |
| Participants | Unknown |
| Interventions | Distribution of Nguni cattle |
| Outcomes | Critical evaluation of project strategy/design, implementation and determine how well the project objectives had been achieved and the constraints to that effect |
| Notes | Full‐text could not be accessed |
Becquey 2017.
| Methods | cRCT |
| Participants | Children aged 6–12 months |
| Interventions | Enhanced‐Homestead Food Production platform for increasing multiple micronutrient powder knowledge and utilisation and reducing anaemia |
| Outcomes | Anaemia |
| Notes | Conference abstract |
Bezuneh 1989.
| Methods | Unknown |
| Participants | Data collected in 1983–1984 in the Ewalel and Marigat locations of Baringo District, Kenya |
| Interventions | Food‐for‐work |
| Outcomes | Unknown |
| Notes | Full‐text could not be accessed |
Bhandari 2019.
| Methods | Unclear (difference‐in‐difference) |
| Participants | 100 children aged 6–60 months enrolled in each group from households with HIV‐infected adults aged 18–49 years on antiretroviral therapy and with access to surface water and land |
| Interventions | Human‐powered water pump, a microfinance loan to purchase farm commodities, and training in sustainable farming practices and financial management |
| Outcomes | Dietary intake and nutritional status of children living in HIV‐affected households |
| Notes | Conference abstract |
Briaux 2017.
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Cash transfer programme targeting the '1000 days period' |
| Outcomes | Birthweight and growth retardation |
| Notes | Conference abstract |
Deji 2015.
| Methods | Unknown |
| Participants | Rural villages in Nigeria |
| Interventions | Food security sustainability |
| Outcomes | Unknown |
| Notes | Full‐text could not be accessed |
Donato 2017.
| Methods | RCT |
| Participants | Children and mothers in Ethiopia |
| Interventions | Cash transfers and provision of personalised information about quality of child growth |
| Outcomes | Food consumption |
| Notes | Conference abstract |
Gahamanyi 2015a.
| Methods | Unclear |
| Participants | Households in Rwanda |
| Interventions | Vision 2020 Umurenge Programme – Direct Support and Public Works programme |
| Outcomes | Poverty; food security |
| Notes | Conference abstract |
Gauchan 1997.
| Methods | Unknown |
| Participants | Farmers in Nepal's mountainous region |
| Interventions | Fruit tree integration (to increase income) |
| Outcomes | Household income and food security |
| Notes | Full‐text could not be accessed |
Ghattas 2019.
| Methods | Unclear |
| Participants | Women and children in refugee camps in Palestine |
| Interventions | Employment of women through social enterprises to deliver a subsidised healthy daily school meal to elementary school children in Palestinian camps |
| Outcomes | Women's economic, social and food security outcomes |
| Notes | Conference abstract |
Ilham 2011.
| Methods | Secondary time series |
| Participants | Unknown |
| Interventions | Food price support policies |
| Outcomes | Food security |
| Notes | Full‐text could not be accessed |
ISRCTN29521514.
| Methods | Non‐randomised cluster controlled trial |
| Participants | Residents in refugee camps in Mogadishu |
| Interventions | Unconditional cash transfer (concern NGO) |
| Outcomes | Primary outcomes: individual diet diversity scores of children aged 6–59 months, measured during the baseline survey and during end‐line survey after 3 months of intervention; incidence of acute malnutrition in children aged 6–59 months (defined as a MUAC < 12.5 cm or nutritional oedema, or both), measured over 6 months of follow‐up following the start of the intervention Secondary outcomes: prevalence of global acute malnutrition (weight‐for‐height < –2 z‐scores or nutritional oedema, or both) in children aged 6–59 months; mean weight‐for‐height in children aged 6–59 months; household expenditure; Household Dietary Diversity Score (24‐hour recall); Household Food Insecurity Access Scale score (1‐month recall); Coping Strategies Index (7‐day recall); access to water and sanitation; infant and young child feeding practices in children aged < 2 years; 2‐week retrospective morbidity; treatment sought and received; mean maternal MUAC; mean maternal BMI |
| Notes | Potential study for review update |
Kim 2009.
| Methods | Unclear |
| Participants | Underprivileged in Belo Horizonte, Brazil |
| Interventions | Food security programmes of the Secretaria Municipal de Abastecimento in Belo Horizonte |
| Outcomes | Food security |
| Notes | Full‐text could not be accessed |
Kroeun 2019.
| Methods | cRCT |
| Participants | Farmers in Cambodia |
| Interventions | Enhanced Homestead Food Production (EHFP) programme |
| Outcomes | Food security; dietary diversity; food production |
| Notes | Conference abstract |
Lukmanji 2017.
| Methods | Unclear |
| Participants | Rural ultra‐poor households in Bangladesh |
| Interventions | Food and Livelihood Security (FLS) project |
| Outcomes | Food security |
| Notes | Conference abstract |
Marsh 1994.
| Methods | Paper analysed field data collected for a mid‐term evaluation of project impacts; included a control group |
| Participants | Rural areas in northwestern Bangladesh |
| Interventions | Large‐scale home garden project |
| Outcomes | Production and consumption of vitamin‐rich fruits and vegetables; income from garden sales |
| Notes | Full‐text could not be accessed |
Miller 2017.
| Methods | cRCT |
| Participants | Communities in Nepal |
| Interventions | Community development provided by Heifer Nepal, including social capital promotion, livestock/nutrition training |
| Outcomes | Food security; dietary diversity; anthropometry |
| Notes | Conference abstract |
Morris 1999.
| Methods | Quasi‐experimental study |
| Participants | Members Honduran smallholder farmers groups |
| Interventions | 1 year of credit and technical assistance |
| Outcomes | Household food security and nutrition |
| Notes | Full‐text could not be accessed |
Mpiira 2019.
| Methods | cRCT |
| Participants | Villages in Uganda |
| Interventions | Uganda's National Development Plan; 6 intervention groups: agricultural training for the first year; agriculture and health interventions; agricultural credit; a voucher scheme for subsidised inputs; price insurance and health interventions – growth monitoring and promotion in children aged > 2 years, quarterly health and nutrition community forums and conditional food transfers to pregnant women |
| Outcomes | Food security (HFIAS), smallholder family nutrition (prevalence of wasting, underweight and stunting in children aged < 5 years) |
| Notes | Conference abstract |
NCT03336021.
| Methods | Non‐randomised |
| Participants | Farmers in Egypt |
| Interventions | Agribusiness Support and Nutrition Services Projects |
| Outcomes | Food insecurity; nutrition |
| Notes | Unclear eligibility based on available information in the trial register |
NCT03847662.
| Methods | Unclear |
| Participants | Women subsistence farmers in rural Vietnam |
| Interventions | Scaling up small‐scale food processing |
| Outcomes | Food security |
| Notes | Unclear eligibility based on available information in the trial register |
PACTR201804003012418.
| Methods | RCT |
| Participants | Pregnant women |
| Interventions | Enhanced homestead food production (relevant group) |
| Outcomes | Anaemia; dietary diversification; household food security; women empowerment |
| Notes | Unclear eligibility based on available information in the trial register |
Park 2019.
| Methods | cRCT |
| Participants | Mothers |
| Interventions | Food vouchers and behaviour change communication |
| Outcomes | Stunting |
| Notes | Conference abstract |
Pham Van 2004.
| Methods | Unknown |
| Participants | Mothers and children aged < 5 years |
| Interventions | Integrated food security project |
| Outcomes | Child malnutrition (stunting, wasting, low birthweight) |
| Notes | Full‐text could not be accessed |
Raneri 2017.
| Methods | cRCT |
| Participants | Women with children |
| Interventions | Community‐based farmer field school‐like model |
| Outcomes | Dietary diversity |
| Notes | Conference abstract |
Raza 2018.
| Methods | RCT |
| Participants | Poor households |
| Interventions | Targeting the Ultra‐Poor (TUP) is an integrated programme that combines the transfer of income‐generation assets and multifaceted training on entrepreneurship, health‐nutrition and social awareness |
| Outcomes | Nutritional outcomes; food security |
| Notes | Conference abstracts |
Rosas 2017.
| Methods | RCT |
| Participants | Residents of highly and very highly marginalised localities |
| Interventions | National Crusade against Hunger |
| Outcomes | Dietary diversity and nutritional status of children |
| Notes | Conference abstract |
Santoso 2019.
| Methods | RCT |
| Participants | Farmers in Tanzania |
| Interventions | Singida Nutrition and Agroecology Project (SNAP‐Tz) |
| Outcomes | Child's dietary diversity; women empowerment |
| Notes | Conference abstract |
Shamah‐Levy 2003.
| Methods | RCT |
| Participants | Low‐income families in Mexico |
| Interventions | Tortilla subsidy |
| Outcomes | Anthropometry; diet intake |
| Notes | Conference abstract |
Talukder 2017.
| Methods | cRCT |
| Participants | Households in Cambodia |
| Interventions | Aquaculture and enhanced homestead food production |
| Outcomes | Maternal and child anaemia, child anthropometry, household food security, production and income |
| Notes | Conference abstract |
Taren 2017.
| Methods | Unclear |
| Participants | Households with children |
| Interventions | Solar market gardens, a labour‐saving solar power drip irrigation system at the village level |
| Outcomes | Anthropometry measures, haemoglobin |
| Notes | Conference abstract |
Tchale 2000.
| Methods | Data collected as a part of the International Food Policy Research Institute University of Malawi, Bunda College Rural Financial Market Study |
| Participants | Smallholder farmers in Malawi |
| Interventions | Agricultural credit |
| Outcomes | Food security |
| Notes | Full‐text could not be accessed |
Teran Cadima.
| Methods | Unknown |
| Participants | Unknown |
| Interventions | Nutritional interventions in childcare centres |
| Outcomes | Unknown |
| Notes | Full‐text could not be accessed |
Vliegen 2000.
| Methods | Unknown |
| Participants | Unclear (Vietnam) |
| Interventions | Nutrition and household food security project |
| Outcomes | Unknown |
| Notes | Full‐text could not be accessed |
Wood.
| Methods | RCT |
| Participants | Unknown |
| Interventions | Food and cash transfers |
| Outcomes | Children's height‐for‐age and BMI scores |
| Notes | Full‐text could not be accessed |
BMI: body mass index; cRCT: cluster randomised controlled trial; HFIAS: Household Food Insecurity Access Scale; MUAC: mid‐upper arm circumference; NGO: non‐governmental organisation; RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
Green 2016.
| Study name | Scale up of enhanced homestead food production in Cambodia |
| Methods | RCT |
| Participants | Children aged 6–59 months |
| Interventions | Enhanced Homestead Food Production (EHFP) package |
| Outcomes | Primary outcomes
Secondary outcomes:
|
| Starting date | April 2016 |
| Contact information | Tim Green University of British Columbia |
| Notes | Clinicaltrials.gov identifier: NCT02786368 |
Hidrobo 2016.
| Study name | The effect of a cash transfer program on household welfare and child nutritional status in Mali |
| Methods | RCT |
| Participants | Children aged 6 months to 5 years in households part of Jigisemejiri programme |
| Interventions | Cash distribution and behavioural interventions |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | September 2014 |
| Contact information | Dr Melissa Hidrobo m.hidrobo@cgiar.org |
| Notes | Study is recruiting. Clinicaltrials.gov identifier: NCT02858011 |
ISRCTN24757827 2018.
| Study name | Cash for improved nutrition in Somalia |
| Methods | Cluster RCT |
| Participants | Boys and girls aged 0–59 months |
| Interventions | Conditional and unconditional cash transfers, and mHealth intervention |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | 1 January 2019 |
| Contact information | Andrew Seal: Institute for Global Health University College London, UK |
| Notes | Completed 1 January 2020 |
NCT03170986 2017.
| Study name | Multi‐sectoral agricultural intervention to improve nutrition, health, and developmental outcomes of HIV‐infected and affected children in Western Kenya |
| Methods | RCT |
| Participants | Children aged 6–36 months in households participating in parent study, and parents/guardians of eligible children |
| Interventions | Multisectoral agriculture and microfinance Intervention |
| Outcomes | Primary outcome
Secondary outcome
Time frame: 24 months |
| Starting date | June 2016 (completed March 2020) |
| Contact information | Lisa Butler, Associate Research Professor, University of Connecticut, US |
| Notes |
NCT03299218 2017.
| Study name | Effectiveness of SNF, cash and BCC to prevent stunting among children 6–24 months in Rahim Yar Khan, Pakistan |
| Methods | RCT |
| Participants | BISP beneficiary for intervention groups and poverty score between 16.18 and 20.00 according to the BISP approach for control group; living in the catchment area of LHW; have ≥ 1 child aged 6–7 months at time of inclusion and willing and able to provide written informed consent for study |
| Interventions | Cash‐based transfers only; cash‐based transfers, and SBCC; cash‐based transfer and dietary supplement (SNF); cash‐based transfers, SNF and SBCC |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | May 2017 (Completed 31 July 2019) |
| Contact information | Dr Sajid Bashir Soofi, Associate Professor, Aga Khan University |
| Notes |
NCT03455257 2018.
| Study name | Evaluation of a cash transfer program in low‐income families in Guinea‐Bissau |
| Methods | RCT (open label) |
| Participants | Families (defined as groups of individuals who routinely eat together) in 3 regions of Guinea‐Bissau. Identified by developing scale based upon household characteristics and assets per capita. access to services such as water, electricity and sanitation. Families having the lowest income. |
| Interventions | Cash transfer |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | 25 April 2017 (ongoing) |
| Contact information | Ministry of Finance, Guinea‐Bissau |
| Notes |
NCT03518593 2018.
| Study name | Evaluation of NICHE (Nutritional Improvements Through Cash and Health Education) programme activities in Kitui and Machakos, Kenya |
| Methods | RCT (open label) |
| Participants | Pregnant women and children aged ≤ 23 months in households receiving CT‐OVC in Kitui and Machakos counties of Kenya |
| Interventions | Cash transfer and nutritional counselling |
| Outcomes | Stunting |
| Starting date | 1 January 2017 |
| Contact information | Kimetrica LLC |
| Notes |
NCT03590717 2018.
| Study name | Impact evaluation of WFP's Fresh Food Voucher Pilot Programme in Ethiopia |
| Methods | RCT |
| Participants | Households with young children aged 6–17 months at baseline in December 2017 |
| Interventions | Cash transfers, food vouchers; behaviour change communication |
| Outcomes | Primary outcomes
Secondary:
|
| Starting date | 27 June 2018 |
| Contact information | Kalle Hirvonen, Research Fellow, International Food Policy Research Institute |
| Notes |
NCT03741634 2018.
| Study name | Assessing the preliminary effects of a multisectoral agricultural intervention on adolescent girls' health |
| Methods | RCT (open label) |
| Participants | Adult participating in the parent study; currently unmarried adolescent girls aged 13–20 years (preferred target aged 15–19 years); adolescent girl with parent/primary guardian aged > 18 years who resides in the household |
| Interventions | Loan (about USD 175) from a well‐established Kenyan bank used to get a human‐powered water pump, seeds, fertilisers and pesticides, and education in financial management and sustainable farming practices |
| Outcomes | Primary outcomes
|
| Starting date | 5 December 2018 (ongoing) |
| Contact information | Sheri D Weiser, MD, MPH. sheri.weiser@ucsf.edu |
| Notes |
NCT04101487 2019.
| Study name | Cash transfers to increase dietary diversity in Grand Gedeh County, Liberia |
| Methods | RCT (open label) |
| Participants | Participants aged 6–23 months with consenting carers to have monthly visits and to participate in the programme. Carers of any age |
| Interventions | Cash transfers and nutrition education |
| Outcomes | Primary
Secondary
|
| Starting date | 15 October 2019 |
| Contact information | Michelle Niescierenko, Assistant Professor of Pediatrics and Emergency Medicine, Boston Children's Hospital, US |
| Notes |
Wendt 2019.
| Study name | Food and agricultural approaches to reducing malnutrition (FAARM): protocol for a cluster‐randomised controlled trial to evaluate the impact of a Homestead Food Production programme on undernutrition in rural Bangladesh |
| Methods | Cluster RCT |
| Participants | Married women and their children (aged 0–3 years) in 96 rural settlements of Habiganj district in Sylhet division, Bangladesh. |
| Interventions | Homestead Food Production (HFP) programme implemented by Helen Keller International on women's and children's undernutrition: training of women's groups and asset distribution to support year‐round home gardening, poultry rearing, and improved nutrition and hygiene practices |
| Outcomes | Primary outcome
Secondary outcomes
|
| Starting date | 14 March 2015 |
| Contact information | Sabine Gabrysch, Head, Unit of Epidemiology and Biostatistics, Institute of Global Health, Heidelberg University |
| Notes |
BISP: Benazir Income Support Programme; HbA1c: glycated haemoglobin; IYCF: Infant and Young Child Feeding; LHW: Lady Health Worker; MUAC: mid‐upper arm circumference; CT‐OVC: cash transfer for orphans and vulnerable children; RCT: randomised controlled trial; SBCC: social and behaviour change communication; SNF: Dietary supplement; WASH: Water, Sanitation and Hygiene; WFP: World Food Program.
Differences between protocol and review
Although we aimed to follow the methods prespecified in our protocol (Durao 2015), we implemented some necessary changes to methods as we worked on the review. The changes and the reasons for them are detailed below.
We had specified in the protocol that we would include non‐randomised studies including controlled before‐after studies (CBAs) and prospective analytical cohort studies. However, after identification of eligible studies, it was difficult to clearly identify the distinction between these two study designs; in both study designs, observations are made before and after an intervention has been implemented or an exposure has occurred, both in an intervention and a control group. They also have similar issues regarding potential biases due to using non‐randomised methods, such as selection bias. Therefore, we made a pragmatic decision to keep these studies in the same category, namely 'prospective controlled studies'.
A number of databases proposed in the protocol were removed from the initial search in 2016, as they were redundant, the content was not relevant or we did not have access to the databases. They are listed below, with reasons:
Cochrane Public Health Group Specialized Register: included in CENTRAL;
African Index Medicus: included in African Healthline;
CINAHL (via EBSCOhost), PsycINFO: not relevant to the topic;
Food Science and Technology Abstracts, CAB Abstracts: no access.
After the evaluating the 2016 search results regarding number of relevant and eligible articles retrieved by each database, the following databases were omitted from the 2019 update of the search:
Embase (Elsevier);
GreenFILE (EBSCO);
AfricaBib (africabib.org);
AGRIS;
AGRICOLA;
AFRICAN HEALTHLINE, African Journals Online (via Africa‐Wide Information, EBSCO);
Trials Register of Promoting Health Interventions (TRoPHI);
WHO Global Index Medicus;
International Bibliography of the Social Sciences (IBSS) (ProQuest);
ClinicalTrials.gov.
In the protocol, we had planned to also search the top five journals in which the included studies are most frequently published and to contact the authors of included studies and undertake citation tracking of these studies, as well as handsearch reference lists of identified relevant systematic reviews. These additional steps to identify studies were not undertaken. Our search of electronic databases was very comprehensive and already retrieved a very large yield to screen. This made it unfeasible to handsearch individual journals. The electronic database search included grey literature databases and we found many reports from organisations working in this field, that are not from peer‐reviewed journals. Therefore, we considered that the results retrieved from the search conducted was likely to identify all relevant articles.
We had planned that one review author would initially screen the first batch of search results for obviously irrelevant titles, as a way to manage the large number of results expected. This was not done as, after the initial search was revised, the number of records retrieved were manageable for duplicate screening.
We had planned to search the reference lists of the included studies for other relevant studies, and to search for unpublished studies in the grey literature database OpenGREY and on websites of relevant organisations, such as Eldis, International Food Policy Research Institute (IFPRI), World Bank, Global Alliance for Improved Nutrition (GAIN) and Science Development Net. However, given that electronic database searches already included sources of unpublished literature, and given the very high number of search results, we decided not to search these databases. It is important to note that results from the electronic database searching did retrieve reports published by the World Bank and IFPRI, for example, therefore, we believe we have not missed important studies by not carrying out this additional searching of grey literature databases or websites of relevant organisations.
We had planned to contact experts working in various areas related to food security for relevant studies. However, given the number of results retrieved, of both published and unpublished studies, we did not think it was necessary to carry this out. We did contact authors of included studies, who sometimes sent other papers linked to a study identified through the search strategy.
We had planned to meta‐analyse as our main synthesis method. Due to unavailability of relevant data from many studies we had to use other synthesis methods, namely vote counting based on effect direction.
We added a clarification that we also excluded interventions where food was provided in the form of food baskets or in‐kind transfers of food. These types of interventions, according to our logic model, fall under the groups of interventions addressing availability and were, therefore, excluded.
We used a definition (that was not included in the protocol) for overall risk of bias to facilitate decisions for downgrading the evidence during our GRADE assessment. We also selected the key outcomes for the GRADE 'Summary of findings' tables after the protocol was published.
Contributions of authors
SD initiated the review idea with support from BK.
SD drafted the review and all other authors contributed to finalise it. All authors approved the final manuscript.
SD, AS, VR, MV, BS, AB and JO screened records against eligibility criteria and carried out data extraction and risk of bias assessments. YB checked all data extractions and calculations related to outcomes.
SD carried out the initial analyses, YB checked these, and all other authors contributed to the interpretation of the analyses.
SD, AS and MV carried out the GRADE assessment and compiled the 'Summary of findings' tables.
EK helped resolve some disagreements during study selection and reviewed the manuscript.
SD will be responsible for updating the review.
Sources of support
Internal sources
South African Cochrane Centre, South African Medical Research Council, South Africa
External sources
-
Department for International Development, UK
Project number 300342‐104
Declarations of interest
SD: none.
MV: none.
VR: none.
JO: none.
BS: none.
YB: none.
AB: none.
EK: none.
AS: none.
Edited (no change to conclusions)
References
References to studies included in this review
Aguero 2006 {published data only}
- Aguero J, Carter M, Woolard I. The impact of unconditional cash transfers on nutrition: the South African Child Support Grant. Cape Town: Southern Africa Labour and Development; 2006. Research Unit Working Paper Number 06/08.
Ahmed 2019a {published data only}
- Ahmed A, Hoddinott J, Roy S, Sraboni, E. Transfers, nutrition programming, and economic well-being: experimental evidence from Bangladesh. Washington, DC: International Food Policy Research Institute; 2019. IFPRI discussion paper 1879. [DOI: 10.2499/p15738coll2.133450] [DOI]
- Ahmed A, Hoddinott J, Roy S. Food transfers, cash transfers, behavior change communication and child nutrition. Evidence from Bangladesh. Washington, DC: International Food Policy Research Institute; 2019. IFPRI discussion paper 1868. [DOI: 10.2499/p15738coll2.133420] [DOI]
Ahmed 2019b {published data only}
- Ahmed A, Hoddinott J, Roy S, Sraboni, E. Transfers, nutrition programming, and economic well-being: experimental evidence from Bangladesh. Washington, DC: International Food Policy Research Institute; 2019. IFPRI discussion paper 1879. [DOI: 10.2499/p15738coll2.133450] [DOI]
- Ahmed A, Hoddinott J, Roy S. Food transfers, cash transfers, behavior change communication and child nutrition. Evidence from Bangladesh. Washington, DC: International Food Policy Research Institute; 2019. IFPRI discussion paper 1868. [DOI: 10.2499/p15738coll2.133420] [DOI]
Alaofe 2016 {published data only}
- Alaofe H, Burney J, Naylor R, Taren D. Solar-powered drip irrigation impacts on crops production diversity and dietary diversity in Northern Benin. Food and Nutrition Bulletin 2016;37(2):164-75. [DOI: 10.1177/0379572116639710] [DOI] [PubMed] [Google Scholar]
- Burney J, Woltering L, Burke M, Naylor R, Pasternak D. Solar-powered drip irrigation enhances food security in the Sudano–Sahel. Proceedings of the National Academy of Sciences of the United States of America 2010;107(5):1848-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alaofe 2019 {published data only}
- Alaofè H, Burney J, Naylor R, Taren D. The impact of a Solar Market Garden programme on dietary diversity, women's nutritional status and micronutrient levels in Kalalé district of northern Benin. Public Health Nutrition 2019;22(14):2670-81. [DOI: 10.1017/S1368980019001599] [DOI] [PMC free article] [PubMed] [Google Scholar]
Andaleeb 2016 {published data only}
- Andaleeb R. Universal food security program and nutritional intake: evidence from the hunger prone KBK districts in Odisha. Food Policy 2016;63:73-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersen 2015 {published data only}
- Andersen CT, Reynolds SA, Behrman JR, Crookston BT, Dearden KA, Escobal J, et al. Participation in the Juntos conditional cash transfer program in Peru is associated with changes in child anthropometric status but not language development or school achievement. Journal of Nutrition 2015;145(10):2396-405. [DOI: 10.3945/jn.115.213546] [DOI] [PMC free article] [PubMed] [Google Scholar]
Asadullah 2015 {published data only}
- Asadullah MN, Ara J. Evaluating the long-run impact of an innovative anti-poverty programme: evidence using household panel data. Applied Economics 2015;48(2):107-20. [DOI: 10.1080/00036846.2015.1073846] [DOI] [Google Scholar]
- Emran MS, Robano V, Smith SC. Assessing the frontiers of ultra poverty reduction: evidence from challenging the frontiers of poverty reduction/targeting the ultra-poor, an innovative program in Bangladesh. Economic Development and Cultural Change 2014;62(2):339-80. [Google Scholar]
- Haseen F. Change in food and energy consumption among the ultra poor: is the poverty reduction programme making a difference? Asia-Pacific Journal of Clinical Nutrition 2007;16(Suppl 1):58-64. [PubMed] [Google Scholar]
- Jalal CS, Frongillo EA. Effect of poverty reduction program on nutritional status of the extreme poor in Bangladesh. Food and Nutrition Bulletin 2013;34(4):402-11. [DOI] [PubMed] [Google Scholar]
- Rabbani M, Prakash VA, Sulaiman M. Impact assessment of CFPR/TUP: a descriptive analysis based on 2002-2005 panel data. Canada: BRAC Research and Evaluation Division and the Aga Khan Foundation; 2012. CFPR/TUP Working Paper Series No. 12.
Asfaw 2014 {published data only}
- Asfaw S, Davis B, Dewbre J, Handa S, Winters P. Cash transfer programme, productive activities and labour supply: evidence from randomized experiment in Kenya. Journal of Development Studies 2014;50(8):1172-96. [DOI: 10.1080/00220388.2014.919383] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayuku D, Embleton L, Koech J, Atwoli L, Hu L, Ayaya S, et al. The government of Kenya cash transfer for orphaned and vulnerable children: cross-sectional comparison of household and individual characteristics of those with and without. BMC International Health and Human Rights 2014;14(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C, Singh K, Handa S, Halpern C, Pettifor A, Thirumurthy H. Investments in children's health and the Kenyan cash transfer for orphans and vulnerable children: evidence from an unconditional cash transfer scheme. Health Policy and Planning 2017;32:943-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Kenya CT-OVC Evaluation Team. The impact of the Kenya cash transfer program for orphans and vulnerable children on household spending. Journal of Development Effectiveness 2012;4(1):9-37. [Google Scholar]
- Ward P, Hurrell A, Visram A, Riemenschneider N, Pellerano L, O'Brien C, et al. Cash Transfer Programme for Orphans and Vulnerable Children (CT-OVC), Kenya: operational and impact evaluation, 2007–2009. Oxford Policy Management 2010.
Baird 2013 {published data only}
- Baird S, De Hoop J, Özler B. Income shocks and adolescent mental health. Journal of Human Resources 2013;48(2):370-403. [Google Scholar]
- Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. The Quarterly Journal of Economics 2011;126(4):1709-53. [Google Scholar]
- Baird SJ, Chirwa E, De Hoop J, Özler B. Girl power: cash transfers and adolescent welfare. Evidence from a cluster-randomized experiment in Malawi. Cambridge: National Bureau of Economic Research; 2013 September. Working Paper 19479.
- Baird SJ, Garfein RS, McIntosh CT, Özler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet 2012;379(9823):1320-9. [DOI] [PubMed] [Google Scholar]
Beegle 2017 {published data only}
- Beegle K, Galasso E, Goldberg J. Direct and indirect effects of Malawi's public works program on food security. Journal of Development Economics 2017;128:1-23. [DOI: 10.1016/j.jdeveco.2017.04.004] [DOI] [Google Scholar]
Breisinger 2018 {published data only}
- Breisinger C, Gilligan D, ElDidi H, El-Enbaby H, Karachiwalla N, Kassim Y, et al. Impact evaluation study for Egypt's Takaful and Karama cash transfer program. Synthesis report: summary of key findings from the quantitative and qualitative impact evaluation studies. Washington, DC: International Food Policy Research Institute; 2018. Regional program working paper 16.
- Breisinger C, Gilligan D, Karachiwalla N, Kurdi S, El-Enbaby H, Jilani A, et al. Impact evaluation study for Egypt's Takaful and Karama cash transfer program: Part 1: Quantitative report. Washington, DC: International Food Policy Research Institute; 2018 October. Regional programme working paper 14.
Brugh 2018 {published data only}
- Brugh K, Angeles G, Mvula P, Tsoka M, Handa S. Impacts of the Malawi social cash transfer program on household food and nutrition security. Food Policy 2018;76:19-32. [Google Scholar]
Brunie 2014 {published data only}
- Brunie A, Fumagalli L, Martin T, Field S, Rutherford D. Can village savings and loan groups be a potential tool in the malnutrition fight? Mixed method findings from Mozambique. Children and Youth Services Review 2014;47:113-20. [DOI: 10.1016/j.childyouth.2014.07.010] [DOI] [Google Scholar]
Chakrabarti 2018 {published data only}
- Chakrabarti S, Kishore A, Roy D. Effectiveness of food subsidies in raising healthy food consumption: public distribution of pulses in India. American Journal of Agricultural Economics 2018;100(5):1427-49. [DOI: 10.1093/ajae/aay022] [DOI] [Google Scholar]
Chen 2019 {published data only}
- Chen Q, Pei C, Bai Y, Zhao Q. Impacts of nutrition subsidies on diet diversity and nutritional outcomes of primary school students in rural northwestern China - Do policy targets and incentives matter? International Journal of Environmental Research and Public Health 2019;16:2891. [DOI: 10.3390/ijerph16162891] [DOI] [PMC free article] [PubMed] [Google Scholar]
Daidone 2014 {published data only}
- Asfaw S, Carraro A, Davis B, Handa S, Seidenfeld D. Cash transfer programmes, weather shocks and household welfare: evidence from a randomised experiment in Zambia. Journal of Development Effectiveness 2017;9(4):419-42. [Google Scholar]
- Daidone S, Davis B, Dewbre J, González-Flores M, Handa S, Seidenfeld D, et al. Zambia's Child Grant Programme: 24-month impact report on productive activities and labour allocation. Rome: Food and Agriculture Organization of the United Nations; 2014.
- Seidenfeld D, Handa S, Davis B. Zambia's Child Grant Program: 24-month impact report. Washington, DC: American Institutes for Research (AIR); 2013.
Darrouzet Nardi 2016 {published data only}
- Darrouzet-Nardi AF, Miller LC, Joshi N, Mahato S, Lohani M, Rogers BL. Child dietary quality in rural Nepal: effectiveness of a community-level development intervention. Food Policy 2016;61:185-97. [DOI: 10.1016/j.foodpol.2016.03.007] [DOI] [Google Scholar]
Doocy 2017 {published data only}
- Doocy S, Cohen S, Emerson J, Menakuntuala J, Rocha JS. Food security and nutrition outcomes of farmer field schools in eastern Democratic Republic of the Congo. Global Health: Science and Practice 2017;5(4):630-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doocy S, Emerson J, Colantouni E, Strong J, Mansen KA, Caulfield LE, et al. Improving household food security in eastern Democratic Republic of the Congo: a comparative analysis of four interventions. Food Security 2018;10(3):649-60. [Google Scholar]
Evans 2014 {published data only}
- Evans D, Hausladen S, Kosec K, Reese N. Community-based conditional cash transfers in Tanzania: results from a randomized trial. Washington, DC: The World Bank; 2014.
Fenn 2015 {published data only}
- Fenn B, Colbourn T, Dolan C, Pietzsch S, Sangrasi M, Shoham J. Impact evaluation of different cash-based intervention modalities on child and maternal nutritional status in Sindh Province, Pakistan, at 6 mo and at 1 y: a cluster randomised controlled trial. PLoS Medicine 2017;14(5):e1002305-e1002305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenn B, Sangrasi GM, Puett C, Trenouth L, Pietzsch S. The REFANI Pakistan study - a cluster randomised controlled trial of the effectiveness and cost-effectiveness of cash-based transfer programmes on child nutrition status: study protocol. BMC Public Health 2015;15:1044. [DOI: 10.1186/s12889-015-2380-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenn B. A cluster RCT to measure the effectiveness of cash-based interventions on nutrition status in Pakistan. Field Exchange 54. Available at www.ennonline.net/fex/refanirctpakistancash February 2017:61.
- Shwirtz Z, Fenn B, Mioli R, Sangrasi GM, Gallagher M. The REFANI project in Pakistan: adapting research to a multi-sectoral programme for impact measurement. Field Exchange 51. Available at www.ennonline.net/fex/51/refanipakistan January 2016:100.
Fernald 2011 {published data only}
- Fernald LC, Hidrobo M. Effect of Ecuador's cash transfer program (Bono de Desarrollo Humano) on child development in infants and toddlers: a randomized effectiveness trial. Social Science & Medicine 2011;72(9):1437-46. [DOI: 10.1016/j.socscimed.2011.03.005] [DOI] [PubMed] [Google Scholar]
- Paxson C, Schady N. Does money matter? The effects of cash transfers on child development in rural Ecuador. Economic Development and Cultural Change 2010;59(1):187-229. [DOI] [PubMed] [Google Scholar]
Ferre 2014 {published data only}
- Ferré C, Sharif I. Can conditional cash transfers improve education and nutrition outcomes for poor children in Bangladesh? Evidence from a pilot project. World Bank Group; 2014 October. Policy Research Working Paper 7077.
Gangopadhyay 2015 {published data only}
- Gangopadhyay S, Lensink R, Yadav B. Cash or In-kind transfers? Evidence from a randomised controlled trial in Delhi, India. Journal of Developmental Studies 2015;51(6):660-73. [DOI: 10.1080/00220388.2014.997219] [DOI] [Google Scholar]
Gertler 2000 (PROGRESA) {published data only}
- Behrman JR, Hoddinott J. Programme evaluation with unobserved heterogeneity and selective implementation: The Mexican PROGRESA impact on child nutrition. Oxford Bulletin of Economics and Statistics 2005;67(4):547-69. [Google Scholar]
- Fernald LCH, Gertler PJ, Neufeld LM. 10-year effect of Oportunidades, Mexico's conditional cash transfer programme, on child growth, cognition, language, and behaviour: a longitudinal follow-up study. Lancet 2009;374(9706):1997-2005. [DOI: 10.1016/s0140-6736(09)61676-7] [DOI] [PubMed] [Google Scholar]
- Gertler P. Do conditional cash transfers improve child health: evidence from PROGRESA's control randomized experiment. American Economic Review 2004;94(2):336-41. [DOI] [PubMed] [Google Scholar]
- Gertler P. The impact of PROGRESA on health. Final report. Washington, DC: International Food Policy Research Institute; 2000 November. Project paper.
- Hoddinott J, Skoufias E. The impact of PROGRESA on food consumption. Washington, DC: International Food Policy Research Institute; 2003. FCND Discussion Paper No. 150. [DOI] [PubMed]
- Skoufias E. Poverty alleviation and consumption insurance: evidence from PROGRESA in Mexico. Journal of Socio-economics 2007;36(4):630-49. [DOI: 10.1016/j.socec.2006.12.020] [DOI] [Google Scholar]
Haushofer 2013 {published data only}
- Haushofer J, Shapiro J. Household response to income changes: Evidence from an unconditional cash transfer program in Kenya. Massachusetts Institute of Technology; 2013 November.
- Haushofer J, Shapiro J. The short-term impact of unconditional cash transfers to the poor: experimental evidence from Kenya. The Quarterly Journal of Economics 2016;131(4):1973–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hidrobo 2014 {published data only}
- Hidrobo M, Hoddinott J, Peterman A, Margolies A, Moreira V. Cash, food, or vouchers? Evidence from a randomized experiment in northern Ecuador. Journal of Development Economics 2014;107:144-56. [Google Scholar]
Hjelm 2017 {published data only}
- Hjelm L, Handa S, Hoop J, Palermo T. Poverty and perceived stress: evidence from two unconditional cash transfer programs in Zambia. Social Science & Medicine 2017;177:110-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidenfeld D, Handa S, Tembo G. Zambia's Multiple Category Targeting grant: 36-month impact report. American Institutes for Research; Washington, DC 2015.
- Seidenfeld D, Prencipe L, Handa S. Zambia's Multiple Category Cash Transfer Program: baseline report. American Institutes for Research; Washington, DC 2012.
Hoddinott 2013 {published data only}
- Hoddinott J, Sandström S, Upton J. Impact evaluation of cash and food transfers in Zinder, Niger: analytical report. Rome: World Food Programme; 2013 May.
- Hoddinott J, Sandstrom S, Upton J. The impact of cash and food transfers: evidence from a randomized intervention in Niger. American Journal of Agricultural Economics 2018;100(4):1032-49. [Google Scholar]
Huerta 2006 (PROGRESA) {published data only}
- Behrman JR, Hoddinott J. An evaluation of the impact of PROGRESA on preschool child height. Washington, DC: International Food Policy Research Institute; 2001. PROGRESA report.
- Huerta MC. Child health in rural Mexico: has PROGRESA reduced children's morbidity risks? Social Policy & Administration 2006;40(6):652-77. [Google Scholar]
- Rivera JA, Sotres-Alvarez D, Habicht J-P, Shamah T, Villalpando S. Impact of the Mexican program for education, health, and nutrition (PROGRESA) on rates of growth and anemia in infants and young children: a randomized effectiveness study. JAMA 2004;291(21):2563-70. [DOI] [PubMed] [Google Scholar]
Jensen 2011 {published data only}
- Jensen RT, Miller NH. Do consumer price subsidies really improve nutrition? Review of Economics and Statistics 2011;93(4):1205-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jodlowski 2016 {published data only}
- Jodlowski M, Winter-Nelson A, Baylis K, Goldsmith PD. Milk in the data: food security impacts from a livestock field experiment in Zambia. World Development 2016;77:99-114. [DOI: 10.1016/j.worlddev.2015.08.009] [DOI] [Google Scholar]
Kandpal 2016 {published data only}
- Kandpal E, Alderman H, Friedman J, Filmer D, Onishi J, Avalos J. A conditional cash transfer program in the Philippines reduces severe stunting. Journal of Nutrition 2016;146(9):1793-800. [DOI: 10.3945/jn.116.233684] [DOI] [PubMed] [Google Scholar]
Kangmennaang 2017 {published data only}
- Kangmennaang J, Kerr RB, Lupafya E, Dakishoni L, Katundu M, Luginaah I. Impact of a participatory agroecological development project on household wealth and food security in Malawi. Food Security 2017;9(3):561-76. [Google Scholar]
Katz 2001 {published data only}
- Katz J, West KP, Pradhan EK, LeClerq SC, Shakya TR, Khatry SK, et al. Impact of providing a small income on women's nutritional status and household food expenditures in rural Nepal. Food and Nutrition Bulletin 2001;22(1):13-8. [Google Scholar]
Kennedy 1989 {published data only}
- Kennedy E. The effects of sugarcane production on food security, health, and nutrition in Kenya: a longitudinal analysis. Washington, DC: International Food Policy Research Institute; 1989 December. Research report 78.
Kurdi 2019 {published data only}
- Kurdi S, Ghorpade Y, Ibrahim H. The Cash for Nutrition intervention in Yemen: impact evaluation study. Washington, DC: International Food Policy Research Institute; 2019 April. Regional program working paper 19.
Kusuma 2017a {published data only}
- Kusuma D, Cohen J, McConnell M, Berman P. Can cash transfers improve determinants of maternal mortality? Evidence from the household and community programs in Indonesia. Social Science & Medicine 2016;163:10-20. [DOI] [PubMed] [Google Scholar]
- Kusuma D, McConnell M, Berman P, Cohen, J. The impact of household and community cash transfers on children's food consumption in Indonesia. Preventive Medicine 2017;100:152-8. [DOI] [PubMed] [Google Scholar]
Kusuma 2017b {published data only}
- Kusuma D, Cohen J, McConnell M, Berman P. Can cash transfers improve determinants of maternal mortality? Evidence from the household and community programs in Indonesia. Social Science & Medicine 2016;163:10-20. [DOI] [PubMed] [Google Scholar]
- Kusuma D, McConnell M, Berman P, Cohen, J. The impact of household and community cash transfers on children's food consumption in Indonesia. Preventive Medicine 2017;100:152-58. [DOI] [PubMed] [Google Scholar]
Leroy 2008 (PROGRESA) {published data only}
- Leroy JL, García-Guerra A, García R, Dominguez C, Rivera J, Neufeld LM. The Oportunidades program increases the linear growth of children enrolled at young ages in urban Mexico. Journal of Nutrition 2008;138(4):793-8. [DOI] [PubMed] [Google Scholar]
Lopez Arana 2016 {published data only}
- Attanasio O, Gómez LC, Heredia P, Vera-Hernandez M. The short-term impact of a conditional cash subsidy on child health and nutrition in Colombia. Centre for the Evaluation of Development Policies; 2005 December. The Institute for Fiscal Studies report summary: Familias 03.
- Attanasio O, Mesnard A. The impact of a conditional cash transfer programme on consumption in Colombia. Fiscal Studies 2006;27(4):421-42. [Google Scholar]
- Forde I, Chandola T, Garcia S, Marmot MG, Attanasio O. The impact of cash transfers to poor women in Colombia on BMI and obesity: prospective cohort study. International Journal of Obesity 2012;36(9):1209-14. [DOI: 10.1038/ijo.2011.234] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Arana S, Avendano M, Forde I, Van Lenthe FJ, Burdorf, A. Conditional cash transfers and the double burden of malnutrition among children in Colombia: a quasi-experimental study. British Journal of Nutrition 2016;115(10):1780-9. [DOI: 10.1017/S0007114516000714] [DOI] [PubMed] [Google Scholar]
- Lopez-Arana S, Avendano M, Lenthe FJ, Burdorf A. The impact of a conditional cash transfer programme on determinants of child health: evidence from Colombia. Public Health Nutrition 2016;19(14):2629-2642. [DOI: 10.1017/S1368980016000240] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macours 2012 {published data only}
- Macours K, Schady N, Vakis R. Cash transfers, behavioral changes, and cognitive development in early childhood: evidence from a randomized experiment. American Economic Journal. Applied Economics 2012;4(2):247-73. [DOI: 10.1257/app.4.2.247] [DOI] [Google Scholar]
Maluccio 2005 {published data only}
- Maluccio J, Flores R. Impact evaluation of a conditional cash transfer program: The Nicaraguan Red de Protección Social. Washington, DC: International Food Policy Research Institute; 2005. FCND discussion paper.
Marquis 2018 {published data only}
- Marquis GS, Colecraft EK, Kanlisi R, Aidam BA, Atuobi-Yeboah A, Pinto C, et al. An agriculture-nutrition intervention improved children's diet and growth in a randomized trial in Ghana. Maternal & Child Nutrition 2018;14(s3):e12677. [DOI] [PMC free article] [PubMed] [Google Scholar]
Merttens 2013 {published data only}
- Merttens F, Hurrell A, Marzi M, Attah R, Farhat M, Kardan A, et al. Kenya Hunger Safety Net Programme; monitoring and evaluation component: impact evaluation final report: 2009 to 2012. Oxford Policy Management; 2013.
Miller 2011 {published data only}
- Miller CM, Tsoka M, Reichert K. The impact of the Social Cash Transfer Scheme on food security in Malawi. Food Policy 2011;36(2):230-8. [Google Scholar]
- Miller CM. Cash transfers and economic growth: a mixed methods analysis of transfer recipients and business owners in Malawi. Poverty & Public Policy 2011;3(3):1-36. [DOI: 10.2202/1944-2858.1147] [DOI] [Google Scholar]
- Strobbe F, Miller CM. Cash transfers in an epidemic context: the interaction of formal and informal support in rural Malawi. The World Bank; 2011 October. Policy research working paper 5824.
Murshed E Jahan 2011 {published data only}
- Murshed-E-Jahan K, Pemsl DE. The impact of integrated aquaculture–agriculture on small-scale farm sustainability and farmers' livelihoods: experience from Bangladesh. Agricultural Systems 2011;104(5):392-402. [DOI: 10.1016/j.agsy.2011.01.003] [DOI] [Google Scholar]
Olney 2016 {published data only}
- Dillon A, Arsenault J, Olney D. Nutrient production and micronutrient gaps: evidence from agriculture-nutrition randomized control trial. American Journal of Agricultural Economics 2019;101:732-52. [Google Scholar]
- Dillon A, Bliznashka L, Olney D. Experimental evidence on post-program effects and spillovers from an agriculture-nutrition program. Econominc & Human Biology 2020;36:1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olney D, Bilnashka L, Pedehombga A, Dillon A, Ruel M, Heckert J. Women's nutrition and empowerment are improved through participation in an integrated agriculture and nutrition program in Burkina Faso. The FASEB Journal 2015;29(S1):abstract. [DOI: 10.1096/fasebj.29.1_supplement.898.25] [DOI] [Google Scholar]
- Olney DK, Bliznashka L, Pedehombga A, Dillon A, Ruel MT, Heckert J. A 2-year integrated agriculture and nutrition program targeted to mothers of young children in Burkina Faso reduces underweight among mothers and increases their empowerment: a cluster-randomized controlled trial. The Journal of Nutrition 2016;146(5):1109-17. [DOI: 10.3945/jn.115.224261] [DOI] [PubMed] [Google Scholar]
- Olney DK, Pedehombga A, Ruel MT, Dillon A. A 2-year integrated agriculture and nutritionand health behavior change communication program targeted to women in Burkina Faso reduces anemia, wasting, and diarrhea in children 3–12.9 months of age at baseline: a cluster-randomized controlled trial. The Journal of Nutrition 2015;145:1317–24. [DOI] [PubMed] [Google Scholar]
Osei 2017 {published data only}
- Osei A, Pandey P, Nielsen J, Pries A, Spiro D, Davis D, et al. Combining home garden, poultry, and nutrition education program targeted to families with young children improved anemia among children and anemia and underweight among non pregnant women in Nepal. Food and Nutrition Bulletin 2017;38(1):49-64. [DOI] [PubMed] [Google Scholar]
Pellerano 2014 {published data only}
- Pellerano L, Moratti M, Jakobsen M, Bajgar M, Barca V. Child Grants Programme impact evaluation: follow-up report. Oxford: Oxford Policy Management; 2014 April.
Ponce 2017 {published data only}
- Ponce J, Ramos-Martin J. Impact of two policy interventions on dietary diversity in Ecuador. Public Health Nutrition 2017;20(8):1473-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Porter 2016 {published data only}
- Porter C, Goyal R. Social protection for all ages? Impacts of Ethiopia's Productive Safety Net Program on child nutrition. Social Science & Medicine 2016;159:92-9. [DOI: 10.1016/j.socscimed.2016.05.001] [DOI] [PubMed] [Google Scholar]
Renzaho 2017 {published data only}
- Renzaho AMN, Chitekwe S, Chen W, Rijal S, Dhakal T, Dahal P. The synergetic effect of cash transfers for families, child sensitive social protection programs, and capacity building for effective social protection on children's nutritional status in Nepal. International Journal of Environmental Research and Public Health 2017;14(12):1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwab 2013 {published data only}
- Schwab B. In the form of bread? A randomized comparison of cash and food transfers in Yemen. Washington, DC: International Food Policy Research Institute; 2013. Conference paper.
Skoufias 2013 {published data only}
- Avitabile C. Does information improve the health behavior of adults targeted by a conditional transfer program? Journal of Human Resources 2012;47(3):785-825. [Google Scholar]
- Cunha JM. Testing paternalism: cash versus in-kind transfers. American Economic Journal: Applied Economics 2014;6(2):195-230. [DOI: 10.1257/app.6.2.195] [DOI] [Google Scholar]
- Ramirez-Luzuriaga MJ, Unar-Munguia M, Rodriguez-Ramirez S, Rivera JA, Gonzalez de Cosio T. A food transfer program without a formal education component modifies complementary feeding practices in poor rural Mexican communities. The Journal of Nutrition 2016;146(1):107-13. [DOI: 10.3945/jn.115.215962] [DOI] [PubMed] [Google Scholar]
- Skoufias E, Unar M, González-Cossío T. The impacts of cash and in-kind transfers on consumption and labor supply: Experimental evidence from rural Mexico. Washington, DC: International Food Policy Research Institute; 2008 November. Policy research working paper 4778.
- Skoufias E, Unar M, Gonzalez de Cossio T. The poverty impacts of cash and in-kind transfers: experimental evidence from rural Mexico. Journal of Development Effectiveness 2013;5(4):401-29. [Google Scholar]
Sturm 2013 {published data only}
- An R, Sturm R. A cash-back rebate program for healthy food purchases in South Africa: selection and program effects in self-reported diet patterns. American Journal of Health Behavior 2017;41(2):152-62. [DOI] [PubMed] [Google Scholar]
- Sturm R, An, R, Segal D, Patel D. A cash-back rebate program for healthy food purchases in South Africa: results from scanner data. American Journal of Preventive Medicine 2013;44(6):567-72. [DOI: 10.1016/j.amepre.2013.02.011] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tonguet Papucci 2015 {published data only}
- Houngbe F, Tonguet-Papucci A, Altare C, Ait-Aissa M, Huneau J, Huybregts L, et al. Unconditional cash transfers do not prevent children's undernutrition in the Moderate Acute Malnutrition Out (MAM'Out) cluster-randomized controlled trial in rural Burkina Faso. The Journal of Nutrition 2017;147:1410–7. [DOI] [PubMed] [Google Scholar]
- Tonguet-Papucci A, Houngbe F, Huybregts L, Ait-Aissa M, Altare C, Kolsteren P, et al. Unconditional seasonal cash transfer increases intake of high-nutritional-value foods in young Burkinabe children: results of 24-hour dietary recall surveys within the Moderate Acute Malnutrition Out (MAM'Out) randomized controlled trial. The Journal of Nutrition 2017;147(7):1418-25. [DOI] [PubMed] [Google Scholar]
- Tonguet-Papucci A, Houngbe F, Lompo P, Yameogo WME, Huneau J, Ait Aissa M, et al. Beneficiaries' perceptions and reported use of unconditional cash transfers intended to prevent acute malnutrition in children in poor rural communities in Burkina Faso: qualitative results from the MAM'Out randomized controlled trial. BMC Public Health 2017;17:527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonguet-Papucci A, Huybregts L, Ait Aissa M, Huneau JF, Kolsteren P. The MAM'Out project: a randomized controlled trial to assess multiannual and seasonal cash transfers for the prevention of acute malnutrition in children under 36 months in Burkina Faso. BMC Public Health 2015;15:762. [DOI: 10.1186/s12889-015-2060-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verbowski 2018 {published data only}
- Michaux KD, Hou K, Karakochuk CD, Whitfield KC, Ly S, Verbowski V, et al. Effect of enhanced homestead food production on anaemia among Cambodian women and children: a cluster randomized controlled trial. Maternal & Child Nutrition 2019;15(S3):e12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbowski V, Talukder Z, Hou K, Sok Hoing L, Michaux K, Anderson V, et al. Effect of enhanced homestead food production and aquaculture on dietary intakes of women and children in rural Cambodia: a cluster randomized controlled trial. Maternal & Child Nutrition 2018;14(3):e12581. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weinhardt 2017 {published data only}
- Weinhardt LS, Galvao LW, Yan AF, Stevens P, Mwenyekonde TN, Ngui E, et al. Mixed-method quasi-experimental study of outcomes of a large-scale multilevel economic and food security intervention on HIV vulnerability in rural Malawi. AIDS and Behavior 2017;21(3):712-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Abubakari 2014 {published data only}
- Abubakari A, Sadik B Bgaha, Keisan Y. Impact of village savings and loans associations on the nutritional status of under-five children: a case study in the Sissala West district of Upper West Region. Pakistan Journal of Nutrition 2014;13(7):390. [Google Scholar]
ACTRN12611001170910 {published data only}
- ACTRN12611001170910. Spend Study - a randomised controlled trial to examine the effect of providing additional money on food spending among low income households. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=347678 (first submitted 4 November 2011).
Aker 2017 {published data only}
- Aker JC. Comparing cash and voucher transfers in a humanitarian context: evidence from the Democratic Republic of Congo. World Bank Economic Review 2017;31(1):44-70. [Google Scholar]
Akresh 2016 {published data only}
- Akresh R, Walque D, Kazianga H. Alternative cash transfer delivery mechanisms: impacts on routine preventative health clinic visits in Burkina Faso. In: Edwards S, Johnson S, and Weil DN, editors(s). African Successes, Volume II: Human Capital. 1 edition. Cambridge, Massachusetts: National Bureau of Economic Research, 2016. [Google Scholar]
Alderman 2009 {published data only}
- Alderman H, Ndiaye B, Linnemayr S, Ka A, Rokx C, Dieng K, et al. Effectiveness of a community-based intervention to improve nutrition in young children in Senegal: a difference in difference analysis. Public Health Nutrition 2009;12(5):667-73. [DOI: 10.1017/S1368980008002619] [DOI] [PubMed] [Google Scholar]
Alvarez 2008 {published data only}
- Álvarez C, Devoto F, Winters P. Why do beneficiaries leave the safety net in Mexico? A study of the effects of conditionality on dropouts. World Development 2008;36(4):641-58. [DOI: 10.1016/j.worlddev.2007.04.014] [DOI] [Google Scholar]
Amarante 2016 {published data only}
- Amarante V, Manacorda M, Miguel E, Vigorito A. Do cash transfers improve birth outcomes? Evidence from matched vital statistics, and program and social security data. American Economic Journal: Economic Policy 2016;8(2):1-43. [DOI: 10.1257/pol.20140344] [DOI] [Google Scholar]
Attanasio 2014 {published data only}
- Attanasio OP, Lechene V. Efficient responses to targeted cash transfers. Journal of Political Economy 2014;122(1):178-222. [Google Scholar]
Attanasio 2014a {published data only}
- Attanasio OP, Fernández C, Fitzsimons EOA, Grantham-McGregor SM, Meghir C, Rubio-Codina, M. Using the infrastructure of a conditional cash transfer program to deliver a scalable integrated early child development program in Colombia: cluster randomized controlled trial. BMJ 2014;349(Sep 29):g5785. [DOI: 10.1136/bmj.g5785] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayala 2015 {published data only}
- Ayala GX, Baquero B, Pickrel JL, Mayer J, Belch G, Rock CL, et al. A store-based intervention to increase fruit and vegetable consumption: The El Valor de Nuestra Salud cluster randomized controlled trial. Contemporary Clinical Trials 2015;42:228-38. [DOI: 10.1016/j.cct.2015.04.009] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayele 2003 {published data only}
- Ayele Z, Peacock C. Improving access to and consumption of animal source foods in rural households: the experiences of a women-focused goat development program in the highlands of Ethiopia. Journal of Nutrition 2003;133(11):3981S-6S. [DOI] [PubMed] [Google Scholar]
Barber 2008 {published data only}
- Barber SL, Gertler PJ. The impact of Mexico's conditional cash transfer programme, Oportunidades, on birthweight. Tropical Medicine & International Health 2008;13(11):1405-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bazzi 2012 {published data only}
- Bazzi S, Sumarto S, Suryahadi A. Evaluating Indonesia's Unconditional Cash Transfer Program, 2005-6. International Initiative for Impact Evaluation; 2012 March.
Behrman 2009 {published data only}
- Behrman JR, Parker SW, Todd PE. Schooling impacts of conditional cash transfers on young children: evidence from Mexico. Economic Development and Cultural Change 2009;57(3):439-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bezu 2014 {published data only}
- Bezu S, Kassie GT, Shiferaw B, Ricker-Gilbert J. Impact of improved maize adoption on welfare of farm households in Malawi: a panel data analysis. World Development 2014;59:120-31. [DOI: 10.1016/j.worlddev.2014.01.023] [DOI] [Google Scholar]
Bihan 2010 {published data only}
- Bihan H, Castetbon K, Mejean C, Peneau S, Pelabon L Jellouli F, et al. Sociodemographic factors and attitudes toward food affordability and health are associated with fruit and vegetable consumption in a low-income French population. Journal of Nutrition 2010;140(4):823-30. [DOI: 10.3945/jn.109.118273] [DOI] [PubMed] [Google Scholar]
Bleich 2007 {published data only}
- Bleich E, Guerne RZ, Mack S. The FAO special programme for food security: livestock diversification – a case study in Chad. World's Poultry Science Journal 2007;61(1):23-30. [DOI: 10.1079/wps200438] [DOI] [Google Scholar]
Braido 2012 {published data only}
- Braido LHB, Olinto P, Perrone H. Gender bias in intra-household allocation: evidence from an unintentional experiment. Review of Economics and Statistics 2012;94(2):552-65. [Google Scholar]
Broutin 2006 {published data only}
- Broutin C, Bricas N. Agroalimentaire et lutte contre la pauvreté en Afrique subsaharienne. Paris: Editions du Gret; 2007. Etudes et travaux.
Buller 2016 {published data only}
- Buller AM, Hidrobo M, Peterman A, Heise L. The way to a man's heart is through his stomach? a mixed methods study on causal mechanisms through which cash and in-kind food transfers decreased intimate partner violence. BMC Public Health 2016;16:488. [DOI: 10.1186/s12889-016-3129-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cabral 2014 {published data only}
- Cabral CS, Lopes AG, Lopes JM, Vianna RP. Food security, income, and the Bolsa Familia program: a cohort study of municipalities in Paraiba State, Brazil, 2005-2011. Cadernos de Saude Publica / Ministerio da Saude, Fundacao Oswaldo Cruz, Escola Nacional de Saude Publica 2014;30(2):393-402. [DOI: 10.1590/0102-311X00140112] [DOI] [PubMed] [Google Scholar]
Cardenas 2015 {published data only}
- Cardenas MK, Benziger CP, Pillay TD, Miranda J J. The effect of changes in visibility and price on fruit purchasing at a university cafeteria in Lima, Peru. Public Health Nutrition 2015;18(15):2742-9. [DOI: 10.1017/S1368980014002730] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cluver 2018 {published data only}
- Cluver L, Meinck F, Doubt J, Ward C, Lombard C, Shenderovich Y, et al. Cash+Care: parenting support and violence reduction programme associated with reductions in adolescent HIV-risks in South Africa: a cluster randomized trial of a DREAMS and 4Children-implemented programme 'Parenting for Lifelong Health'. Journal of the International AIDS Society 2018;21.
Cohen 2015 {published data only}
- Cohen CR, Steinfeld RL, Weke E, Bukusi EA, Hatcher AM, Shiboski S, et al. Shamba Maisha: pilot agricultural intervention for food security and HIV health outcomes in Kenya: design, methods, baseline results and process evaluation of a cluster-randomized controlled trial. Springerplus 2015;4:122. [DOI: 10.1186/s40064-015-0886-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dammert 2009 {published data only}
- Dammert AC. Heterogeneous impacts of conditional cash transfers: evidence from Nicaragua. Economic Development and Cultural Change 2009;58(1):53-83. [Google Scholar]
Debela 2015 {published data only}
- Debela BL, Shively G, Holden ST. Does Ethiopia's Productive Safety Net Program improve child nutrition? Food Security 2015;7(6):1273-89. [DOI: 10.1007/s12571-015-0499-9] [DOI] [Google Scholar]
Downs 2017 {published data only}
- Downs S, Fanzo J. Developing a voice messaging intervention to improve nutrition in a large scale horticulture intensification project in Senegal. Annals of Nutrition & Metabolism 2017;71:398. [Google Scholar]
ENN 2018 {published data only}
- Emergency Nutrition Network (ENN). Impact evaluation of the Lebanon multipurpose cash assistance programme. Field Exchange 57, March 2018. Available at: www.ennonline.net/fex/57/lebanonmpcashassistanceprog:82.
Fenn 2015_Niger {published data only}
- Fenn B, Noura G, Sibson V, Dolan C, Shoham J. The role of unconditional cash transfers during a nutritional emergency in Maradi region, Niger: a pre-post intervention observational study. Public Health Nutrition 2015;18(2):343-51. [DOI: 10.1017/S1368980014000378] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenn B, Trepel D, Dolan C, Shoham J, Sibson V. Seasonal unconditional cash transfers and wasting in Niger. Annals of Nutrition & Metabolism 2013;63:1002. [Google Scholar]
Fernald 2017 {published data only}
- Fernald LC, Kagawa RM, Knauer HA, Schnaas L, Guerra AG, Neufeld LM. Promoting child development through group-based parent support within a cash transfer program: experimental effects on children's outcomes. Developmental Psychology 2017;53(2):222-36. [DOI: 10.1037/dev0000185] [DOI] [PubMed] [Google Scholar]
Fortin 2016 {published data only}
- Fortin S, Kameli Y, Ouattara A, CastanF, Perenze ML, Kankouan J, et al. Targeting vulnerable households in urban Burkina Faso: effectiveness of geographical criteria but not of proxy-means testing. Health Policy Plan 2016;31(5):573-81. [DOI: 10.1093/heapol/czv104] [DOI] [PubMed] [Google Scholar]
Gelli 2017 {published data only}
- Gelli A, Roschnik N. A cluster randomised control trial of an integrated agriculture-nutrition package to improve children's diets through community based childcare centres in Malawi. Annals of Nutrition & Metabolism 2017;71:685-86. [Google Scholar]
Gertler 2012 {published data only}
- Gertler PJ, Martinez SW, Rubio-Codina M. Investing cash transfers to raise long-term living standards. American Economic Journal. Applied Economics 2012;4(1):164-92. [Google Scholar]
Gram 2019 {published data only}
- Gram L, Morrison J, Saville N, Yadav SS, Shrestha B, Manandhar D, et al. Do participatory learning and action women's groups alone or combined with cash or food transfers expand women's agency in rural Nepal? Journal of Development Studies 2019;55(8):1670-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grellety 2017 {published data only}
- Grellety E, Babakazo P, Bangana A, Mwamba G, Lezama I, Zagre NM, et al. Effects of unconditional cash transfers on the outcome of treatment for severe acute malnutrition (SAM): a cluster-randomised trial in the Democratic Republic of the Congo. BMC Medicine 2017;15(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gutiérrez 2019 {published data only}
- Gutiérrez JP, Shamah-Levy T, Bertozzi SM, Rivera-Dommarco JA. Intergenerational social mobility based on the investments in human capital: evidence of the long-term results of PROSPERA in health. Washington, DC; The World Bank; 2019 September. Policy research working paper no. WPS9001.
Haghparast‐Bidgoli 2019 {published data only}
- Haghparast-Bidgoli H, Skordis J, Harris-Fry H, Krishnan S, O'Hearn M, Kumar A, et al. Protocol for the cost-consequence and equity impact analyses of a cluster randomised controlled trial comparing three variants of a nutrition-sensitive agricultural extension intervention to improve maternal and child dietary diversity and nutritional status in rural Odisha, India (UPAVAN trial). Trials 2019;20:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haque 2017 {published data only}
- Haque A, Dey MM. Impacts of community-based fish culture in seasonal flood plains on income, food security and employment in Bangladesh. Food Security 2017;9(1):25-38. [Google Scholar]
Hardin Fanning 2014 {published data only}
- Hardin-Fanning F, Gokun Y. Gender and age are associated with healthy food purchases via grocery voucher redemption. Rural and Remote Health 2014;14(3):2830. [PMC free article] [PubMed] [Google Scholar]
Huey 2019 {published data only}
- Teo CH, Chin YS, Lim PY, Masrom SAH, Shariff ZM. Impact of a school nutrition program (SNP) in Malaysia. Annals of Nutrition & Metabolism 2019;75(3):1427. [Google Scholar]
Idiaye 2014 {published data only}
- Idiaye CO, Omonona BT. National Special Programme for Food Security (NSPFS) and poverty among farming households in Oyo State, Nigeria. Journal of Emerging Trends in Economics and Management Sciences 2014;5(3):343. [Google Scholar]
ISRCTN10323949 {published data only}
- ISRCTN10323949. Effectiveness of approaches to deliver integrated solutions for optimal child growth and development in Tanzania. www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN10323949 (first posted 3 December 2017).
ISRCTN77820875 {published data only}
- ISRCTN77820875. Cambodia integrated nutrition, hygiene, and sanitation impact evaluation – endline. www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN77820875 (first posted 9 August 2019).
Issaley 2013 {published data only}
- Issaley NA. Le cash transfer à Olléléwa: de la fabrique des" vulnérables" à la gestion locale de l'aide. www.lasdel.net/images/etudes_et_travaux/Le_cash_transfer_a_Ollelewa.pdf 2013.
Jharendu 2014 {published data only}
- Pant J, Barman BK, Murshed-E-Jahan K, Belton B, Beveridge M. Can aquaculture benefit the extreme poor? A case study of landless and socially marginalized Adivasi (ethnic) communities in Bangladesh. Aquaculture 2014;418/419:1-10. [Google Scholar]
Kagawa 2017 {published data only}
- Kagawa RM, Deardorff J, Garcia-Guerra A, Knauer HA, Schnaas L, Neufeld LM, et al. Effects of a parenting program among women who began childbearing as adolescents and young adults. Journal of Adolescent Health 2017;61(5):634-41. [DOI: 10.1016/j.jadohealth.2017.05.023] [DOI] [PubMed] [Google Scholar]
Kakuhikire 2016 {published data only}
- Kakuhikire B, Suquillo D, Atuhumuza E, Mushavi R, Perkins JM, Venkataramani AS, et al. A livelihood intervention to improve economic and psychosocial well-being in rural Uganda: longitudinal pilot study. SAHARA J: Journal of Social Aspects of HIV/AIDS Research Alliance 2016;13(1):162-9. [DOI: 10.1080/17290376.2016.1230072] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kidoido 2015 {published data only}
- Kidoido M, Korir L. Do low-income households in Tanzania derive income and nutrition benefits from dairy innovation and dairy production? Food Security 2015;7(3):681-92. [Google Scholar]
Kim 2012 {published data only}
- Kim K, Hong SA, Yun SH, Ryou HJ, Lee SS, Kim MK. The effect of a healthy school tuck shop program on the access of students to healthy foods. Nutrition Research and Practice 2012;6(2):138-45. [DOI: 10.4162/nrp.2012.6.2.138] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kimenju 2015 {published data only}
- Kimenju SC, Rischke R, Klasen S, Qaim M. Do supermarkets contribute to the obesity pandemic in developing countries? Public Health Nutrition 2015;18(17):3224-33. [DOI: 10.1017/S1368980015000919] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kronebusch 2019 {published data only}
- Kronebusch N, Damon A. The impact of conditional cash transfers on nutrition outcomes: experimental evidence from Mexico. Economics and Human Biology 2019;33:169-80. [DOI] [PubMed] [Google Scholar]
KumarGhosh 2011 {published data only}
- Kumar Ghosh, D. Combating the menace of food insecurity: the experience of West Bengal. Development in Practice 2011;21(4-5):691-704. [Google Scholar]
Lopez 2018 {published data only}
- Lopez BF, Creamer J. Cash, conditions and child development: experimental evidence from a cash transfer in Honduras. Washington, DC; Inter-American Development Bank; 2018 October. IDB working paper series No IDB-WP-952.
Loubser 2010 {published data only}
- Loubser M. HealthyFood™ benefit: impact of financial incentives and rewards on health and purchasing behaviour of members of a private health insurance scheme in South Africa. South African Journal of Clinical Nutrition 2010;23(3):27-29. [Google Scholar]
Martins 2013 {published data only}
- Martins APB. Impacto do Programa Bolsa Família sobre a aquisição de alimentos em famílias brasileiras de baixa renda [PhD Thesis]. Sao Paulo, Brazil: Universidade de São Paulo, 2013. [Google Scholar]
Mascie Taylor 2010 {published data only}
- Mascie-Taylor CG, Marks MK, Goto R, Islam R. Impact of a cash-for-work programme on food consumption and nutrition among women and children facing food insecurity in rural Bangladesh. Bulletin of the World Health Organization 2010;88(11):854-60. [DOI: 10.2471/BLT.10.080994] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02558660 {published data only}
- NCT02558660. Evaluating use of a farmers market incentive program among low-income health center patients. clinicaltrials.gov/ct2/show/NCT02558660 (first posted 24 September 2015).
NCT02577705 {published data only}
- NCT02577705. Building wealth and health network: a microfinance/TANF demonstration project. clinicaltrials.gov/ct2/show/NCT02577705 (first posted 16 October 2015).
NCT02843178 {published data only}
- NCT02843178. Designing food voucher programs to reduce disparities in healthy diets [Coupons for Healthy Intake using Variable Economic Strategies (CHIVES)]. clinicaltrials.gov/ct2/show/NCT02843178 (first posted 25 July 2016).
NCT03311698 {published data only}
- NCT03311698. Homestead agriculture and nutrition project. clinicaltrials.gov/ct2/show/NCT03311698 (first posted 17 October 2017).
NCT04135625 {published data only}
- NCT04135625. Improving nutrition in children under two through increased egg consumption in Burkina Faso. clinicaltrials.gov/ct2/show/NCT04135625 (first posted 22 October 2019).
NCT04166370 {published data only}
- NCT04166370. Bangladesh MSNP: social protection mixed methods study. clinicaltrials.gov/ct2/show/NCT04166370 (first posted 18 November 2019).
NCT04171999 {published data only}
- NCT04171999. CommunityRx-Hunger (CRx-H) [CommunityRx-Hunger: a hospital-based intervention for primary caregivers of children admitted to the hospital]. clinicaltrials.gov/ct2/show/NCT04171999 (first posted 21 November 2019).
Nisbett 2016 {published data only}
- Nisbett N, Longhurst R, Barnett I, Feruglio F, Gordon J, Hoddinott J, et al. Impact evaluation of the DFID programme to accelerate improved nutrition for the extreme poor in Bangladesh. Maximising the Quality of Scaling Up Nutrition (MQSUN); 2016 June.
Nsabuwera 2016 {published data only}
- Nsabuwera V, Hedt-Gauthier B, Khogali M, Edginton M, Hinderaker SG, Nisingizwe MP, et al. Making progress towards food security: evidence from an intervention in three rural districts of Rwanda. Public Health Nutrition 2016;19(7):1296-304. [DOI: 10.1017/S1368980015002207] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olajide‐Taiwo 2011 {published data only}
- Olajide-Taiwo LO. Effect of capacity building on production of safe and profitable leafy vegetables among farmers in Ibadan City of Nigeria. Acta Horticulturae 2011;911:427-32. [Google Scholar]
Pasdar 2016 {published data only}
- Pasdar Y, Rezaei M, Darbandi M, Niazi P, Sharafi K. The effect of eliminating subsidies on food consumption of households in Kermanshah – Iran. International Journal of Pharmacy and Technology 2016;8:11141-50. [Google Scholar]
Pereko 2017 {published data only}
Perez Lu 2016 {published data only}
- Perez-Lu JE, Carcamo C, Nandi A, Kaufman JS. Health effects of 'Juntos', a conditional cash transfer programme in Peru. Maternal & Child Nutrition 2016;22:22. [DOI: 10.1111/mcn.12348] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prifti {published data only}
- Prifti E, Daidone S, Pace N, Davis B. Stuck exchange: Can cash transfers push smallholders out of autarky? Journal of International Trade & Economic Development 2019;29(5):495-509. [DOI: 10.1080/09638199.2019.1702711] [DOI] [Google Scholar]
Quiñones 2016 {published data only}
- Quiñones EJ, Roy S. The impact of conditional cash transfer programs on indigenous households in Latin America: evidence from PROGRESA in Mexico. Washington, DC: International Food Policy Research Institute; 2016. IFPRI discussion paper.
Ragini 2017 {published data only}
- Ragini R. Impact of nutri-garden on food security of rural families in Udaipur District. Annals of Agri-bio Research 2017;22(2):278-80. [Google Scholar]
Rahman 2015 {published data only}
- Rahman AM, Abdel A, Samira M, Fadol IO. The role of Rural Women Schools (RWSs) on increasing income, improving nutrition and food security of rural families, Gezira State, Sudan. Agricultural Science Digest - A Research Journal 2015;35(2):101. [DOI: 10.5958/0976-0547.2015.00036.1] [DOI] [Google Scholar]
Ramirez‐Silva 2013 {published data only}
- Ramirez-Silva I. The Oportunidades program's fortified food supplement, but not improvements in the home diet, increased the intake of key micronutrients in rural Mexican children aged 12-59 months. Journal of Nutrition 2013;143(5):656-63. [DOI] [PubMed] [Google Scholar]
Roschnik 2017 {published data only}
- Roschnik N, Twalibu Al. Lessons learned from designing and implementing an integrated nutrition, livelihood and ECD project in Malawi. Annals of Nutrition & Metabolism 2017;71:63-4. [Google Scholar]
Roy 2019 {published data only}
- Roy S, Hidrobo M, Hoddinott J, Koch B, Ahmed A. Can transfers and behavior change communication reduce intimate partner violence four years post-program? Experimental evidence from Bangladesh. Washington, DC; International Food Policy Research Institute; 2019 September. IFPRI Discussion Paper 01869.
Rutherford 2016 {published data only}
- Rutherford DD, Burke HM, Cheung KK, Field, SH. Impact of an agricultural value chain project on smallholder farmers, households, and children in Liberia. World Development 2016;83:70-83. [DOI: 10.1016/j.worlddev.2016.03.004] [DOI] [Google Scholar]
Schultz 2001 {published data only}
- Schultz TP. School subsidies for the poor: evaluating a Mexican strategy for reducing poverty. Discussion paper 102. core.ac.uk/download/pdf/6289344.pdf.
Schwab 2019 {published data only}
- Schwab B. Comparing the productive effects of cash and food transfers in a crisis setting: evidence from a randomised experiment in Yemen. Journal of Development Studies 2019;55(Suppl 1):29-54. [Google Scholar]
Sinharoy 2017 {published data only}
- Sinharoy SS, Schmidt W-P, Wendt R, Mfura L, Crossett E, Grepin KA, et al. Impact of community health clubs on diarrhoea and anthropometry in western Rwanda: cluster-randomized controlled trial. Lancet Global Health 2017;5:e699-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sudfeld 2019 {published data only}
- Sudfeld CR, Bliznashka L, Ashery G, Yousafzai AK, Masanja H. Effect of a community health worker delivered health, nutrition and responsive stimulation package and conditional cash transfers on child development and growth in rural Tanzania: protocol for a cluster-randomized trial. BMC Public Health 2019;19(1):641. [DOI] [PMC free article] [PubMed] [Google Scholar]
TorresSalcido 2015 {published data only}
- Torres Salcido G, Roble Pensado Leglise M, Smolski A. Food distribution's socio-economic relationships and public policy: Mexico City's municipal public markets. Development in Practice 2015;25(3):293-305. [DOI: 10.1080/09614524.2015.1016481] [DOI] [Google Scholar]
Wang 2012 {published data only}
- Wang R, Shi L. Access to food outlets and children's nutritional intake in urban China: a difference-in-difference analysis. Italian Journal of Pediatrics 2012;38(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2014 {published data only}
- Young JR, O'Reilly RA, Ashley K, Suon S, Leoung IV, Windsor PA, et al. Impacts on rural livelihoods in Cambodia following adoption of best practice health and husbandry interventions by smallholder cattle farmers. Transboundary and Emerging Diseases 2014;61(S1):11-24. [DOI] [PubMed] [Google Scholar]
Zhang 2018 {published data only}
- Zhang Y, Ji M, Zou J, Yuan T, Deng J, Yang L, et al. Effect of a conditional cash transfer program on nutritional knowledge and food practices among caregivers of 3-5-year-old left-behind children in the rural Hunan province. International Journal of Environmental Research and Public Health 2018;15(3):525. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
ACTRN12618001803280 {published data only}
- ACTRN12618001803280. Impact of improved duck rearing on sale and consumption of ducks in rural households of flood-prone areas of Bangladesh [Impact of improved duck rearing on sale and consumption of ducks and dietary diversity of rural households in flood-prone areas of Bangladesh]. www.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12618001803280 (first posted 6 November 2018).
ACTRN12618001975280 {published data only}
- ACTRN12618001975280. Effectiveness of unconditional Cash transfers and mobile behaviour change communications to reduce child under nutrition in rural Bangladesh [A community based cluster randomised controlled trial to determine the effectiveness of unconditional Cash transfers and mobile behaviour change communications to reduce child under nutrition in rural Bangladesh]. apps.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12618001975280 (first posted 7 December 2018).
Adubra 2017 {published data only}
- Adubra L, Fortin S, Kameli Y, Le Port A, Kodjo NE, Savy M, et al. Can conditional cash transfer combined with nutritional supplementation play a role in reducing child stunting in rural Mali? Annals of Nutrition & Metabolism 2017;71:332. [Google Scholar]
Al‐serhan 2010 {published data only}
- Al-serhan M. Addressing poverty and improving livelihoods in Bedouin regions of Jordan [thesis]. Madison: University of Wisconsin, 2010. [Google Scholar]
Antwi 2013 {published data only}
- Antwi MA, Oladele OI. Strategy, operation and effects of the Nguni Cattle Project in the North West Province, South Africa. Asia Life Sciences 2013:91-102. [Google Scholar]
Becquey 2017 {published data only}
- Becquey E, Olney D, Golan J, Praygod G, Veryser S, Smith E, et al. Impacts of using an integrated homestead food production and nutrition program platform to promote utilization of multiple micronutrient powders: a cluster-randomized controlled trial. Annals of Nutrition & Metabolism 2017;71:859. [Google Scholar]
Bezuneh 1989 {published data only}
- Bezuneh M. Farm level impacts of food-for-work in a semi-arid region of Kenya. Eastern Africa Economic Review 5;1:1-8. [Google Scholar]
Bhandari 2019 {published data only}
- Bhandari S, Butler L, Otieno P, Weiser S, Cohen C, Frongillo E. An agricultural and finance intervention improved dietary intake and nutritional status of children living in HIV-affected households in Western Kenya. Current Developments in Nutrition 2019;3(Suppl 1):P10-129-19. [DOI] [PMC free article] [PubMed]
Briaux 2017 {published data only}
- Briaux J, Carles S, Kameli Y, Fortin S, Rollet P, Becquet R, et al. Impact of a cash transfer program targeting the "1000 days period" on low birth weight and growth retardation: a cluster randomized trial in Togo. Annals of Nutrition & Metabolism 2017;71:333-4. [Google Scholar]
Deji 2015 {published data only}
- Deji SA, Onayade AA. A comparative study of food security sustainability among households in selected rural villages of Nigeria. Annals of Nutrition & Metabolism 2015;67:478-9. [Google Scholar]
Donato 2017 {published data only}
- Donato K. Money or knowledge? Behavioral aspects of malnutrition. Annals of Global Health 2017;83(1):78. [Google Scholar]
Gahamanyi 2015a {published data only}
- Gahamanyi V, Kettlewell A. Evaluating graduation: insights from the Vision 2020 Umurenge Programme in Rwanda. IDS Bulletin 2015;46(2):48-63. [Google Scholar]
Gauchan 1997 {published data only}
- Gauchan D. Fruit tree integration: an option to improve household food security in Nepal's mountain region. In: Heidhues F, Fadani A, editors(s). Food Security and Innovations: Successes and Lessons Learned. New York (NY): Peter Lang Publishing Inc, 1997:221-230. [Google Scholar]
Ghattas 2019 {published data only}
- Ghattas H, Jamaluddine Z, Choufani J, Masterson AR, Sahyoun NR. Improvements in economic, social, and food security outcomes of Palestinian refugee women and diet diversity of Palestinian schoolchildren in Lebanon: the Healthy Kitchens, Healthy Children intervention. Lancet 2019;393(Suppl 1):S25. [Google Scholar]
Ilham 2011 {published data only}
- Ilham N. Effectiveness of food price policies on food security. Indonesian Journal of Agriculture 2011;4(1):58-66. [Google Scholar]
ISRCTN29521514 {published data only}
- ISRCTN29521514. Assessing the role of cash transfer programmes in reducing the risk of acute malnutrition in Somalia. www.isrctn.com/ISRCTN29521514 (first applied 19 January 2016).
Kim 2009 {published data only}
- Kim J. A study on the food security of Belo Horizonte, Brazil. Journal of Rural Development 2009;32(4):85-108. [Google Scholar]
Kroeun 2019 {published data only}
- Kroeun H, Cotes G, Sokhoing L, Ngik R, Ridolfi R. Dietary diversity in Cambodian women and children in a cluster randomized control trial of enhanced homestead food production with and without gender components. Annals of Nutrition & Metabolism 2019;75(3):78.
Lukmanji 2017 {published data only}
- Lukmanji Z, Mubarak M, Das L. The assessment of nutritional status of children below five years in households which participated in Food and Livelihood Security (FLS) project in Rajshahi Division-Bangladesh. Annals of Nutrition & Metabolism 2017;71:874. [Google Scholar]
Marsh 1994 {published data only}
- Marsh RR, Talukder A. Effects of the introduction of home gardening on the production and consumption of target, interaction, and control groups: a case study from Bangladesh. Montpellier: Recherches-système en agriculture et développement rural 1994:425-30.
Miller 2017 {published data only}
- Miller L, Joshi N, Lohani M, Rogers B, Mahato S, Neupane S, et al. Greater improvements in child growth and diet quality after a holistic community development intervention than after nutrition training alone. Annals of Nutrition & Metabolism 2017;71:412-3.
Morris 1999 {published data only}
- Morris SS, Banegas JMM. Rural development, household food security, and nutrition in western Honduras [Desarrollo rural, seguridad alimentaria del hogar y nutrición en el oeste de Honduras]. Archivos Latinoamericanos de Nutrición 1999;49(3):244-52. [PubMed] [Google Scholar]
Mpiira 2019 {published data only}
- Mpiira R, Olobo Okello P, Ali Z. A multisectoral approach to eradication of malnutrition in vulnerable groups: a cluster-randomised trial. Lancet Global Health 2019;7:S8. [Google Scholar]
NCT03336021 {published data only}
- NCT03336021. Impact evaluation of agribusiness support and nutrition services projects in Upper Egypt. clinicaltrials.gov/ct2/show/NCT03336021 (first posted 8 November 2017).
NCT03847662 {published data only}
- NCT03847662. Scaling up small-scale food processing to promote food security among women farmers in rural Vietnam. clinicaltrials.gov/ct2/show/NCT03847662 (first posted 20 February 2019).
PACTR201804003012418 {published data only}
- PACTR201804003012418. Randomized controlled trial to study the effect of nutritional intervention from farm to feeding on gestational weight gain, anaemia and child nutrition. www.who.int/trialsearch/Trial2.aspx?TrialID=PACTR201804003012418 (first registered 25 January 2018).
Park 2019 {published data only}
- Park S, Han YE, Kim H. Knowledge, food vouchers, and child nutrition: evidence from a field experiment in Ethiopia. Current Developments in Nutrition 2019;3(Suppl 1):1091.
Pham Van 2004 {published data only}
- Pham Van H. Study on the maternal – children nutritional status improve effects of an integrated food security project. Journal of Vietnamese Medicine 2004;302(9):1-6. [Google Scholar]
Raneri 2017 {published data only}
- Raneri Je, Hoang K, Berti P, Kennedy G, Lachat C. Promotion of local agrobiodiversity improves diets of women and children in North West Vietnam: a cluster RCT. Annals of Nutrition & Metabolism 2017;71:408-9.
Raza 2018 {published data only}
- Raza WA, Van de Poel E, Van Ourti T. Impact and spill-over effects of an asset transfer program on child undernutrition: evidence from a randomized control trial in Bangladesh. Journal of Health Economics 2018;62:105-20. [DOI] [PubMed] [Google Scholar]
Rosas 2017 {published data only}
- Rosas VM, Levy TS, Tapia BM, Gomez-Humaran IM. Impact of the National Crusade Against Hunger (CNCH) on anemia and dietary diversity among Mexican children. In: Special Issue: Experimental Biology 2017 Meeting Abstracts. The FASEB Journal 2017;31(S1):lb585. [Google Scholar]
Santoso 2019 {published data only}
- Santoso M, Kerr RB, Kassim N, Martin H, Mtinda E, Mtei K, et al. Production diversity, men's help with household tasks, & lower women's depression mediate impact of an agriculture intervention on child's dietary diversity in Tanzania. Current Developments in Nutrition 2019;3(Suppl 1):FS01-06-19. [Google Scholar]
Shamah‐Levy 2003 {published data only}
- Shamah Levy T, Avila Curiel A, Cuevas Nasu L, Chavez Villasana A, Avila Arcos MA, Fernandez Mendoza C. The tortilla subsidy in Mexico: a nutritional or economic program? Archivos Latinoamericanos de Nutrición 2003;53(1):5-13. [PubMed] [Google Scholar]
Talukder 2017 {published data only}
- Talukder A, Mundy G, Hou K, Stormer A, Michaux K, McLean J, et al. The role of small scale aquaculture and enhanced homestead food production in improving household food security and nutrition. Annals of Nutrition & Metabolism 2017;71:214-5.
Taren 2017 {published data only}
- Taren D. The impact of solar market gardens on child growth, iron and vitamin a status in the Kalale District of Northern Benin. Annals of Nutrition & Metabolism 2017;71(Supplement 2):1308.
Tchale 2000 {published data only}
- Tchale H, Edriss A. Production and marketing of smallholder tobacco: effect on household food security, nutritional status and intra-household labour allocation in Malawi. UNISWA Research Journal of Agriculture, Science and Technology 2000;4(1):83-92. [Google Scholar]
Teran Cadima {published data only}
- Teran Cadima N. Evaluation of progress and impact of the intervention nutritional in infantils centers integrals of Ministry of Social Security and Public Health in the city of La Paz. n/a.
Vliegen 2000 {published data only}
- Vliegen K. Report on a nutrition and household food security project in Viet Nam. Food, Nutrition and Agriculture 2000;27:40-6. [Google Scholar]
Wood {published data only}
- Wood RP. Transfers for tots: A study of the heterogeneous effects of food and cash assistance on child anthropometry in Uganda [Master thesis]. Chapel Hill: University of North Carolina, 2014. [Google Scholar]
References to ongoing studies
Green 2016 {published data only}
- Green T. Scale up of enhanced homestead food production in Cambodia. University of British Columbia, Helen Keller International and International Development Research Centre (Canada) 2016.
Hidrobo 2016 {published data only}
- Hidrobo M, Roy S, Huybregts L, Gilligan D, Ruel M. The effect of a cash transfer program on household welfare and child nutritional status in Mali. Washington, DC; International Food Policy Research Institute; 2016.
ISRCTN24757827 2018 {published data only}
- ISRCTN24757827. Cash for improved nutrition in Somalia. www.isrctn.com/ISRCTN24757827 (first posted 5 November 2018).
NCT03170986 2017 {published data only}
- NCT03170986. Multi-sectoral agricultural intervention to improve nutrition, health and developmental outcomes of HIV-infected and affected children in Western Kenya. clinicaltrials.gov/show/NCT03170986 (first posted 31 May 2017).
NCT03299218 2017 {published data only}
- NCT03299218. Effectiveness of SNF, Cash and BCC to prevent stunting among children 6-24 months in Rahim Yar Khan, Pakistan [Effectiveness of a programme comprised of SNF, cash-based transfers and BCC to prevent stunting among children 6-24 months in Rahim Yar Khan, Punjab, Pakistan]. clinicaltrials.gov/show/NCT03299218 (first posted 3 October 2017).
NCT03455257 2018 {published data only}
- NCT03455257. Evaluation of a cash transfer program in low-income families in Guinea-Bissau. clinicaltrials.gov/show/NCT03455257 (first posted 6 March 2018).
NCT03518593 2018 {published data only}
- NCT03518593. Evaluation of NICHE programme activities in Kenya [Evaluation of NICHE (Nutritional Improvements through Cash and Health Education) programme activities in Kitui and Machakos, Kenya]. clinicaltrials.gov/show/NCT03518593 (first posted 8 May 2018).
NCT03590717 2018 {published data only}
- NCT03590717. Impact evaluation of WFP's fresh food voucher pilot programme in Ethiopia. clinicaltrials.gov/show/NCT03590717 (first posted 18 July 2018).
NCT03741634 2018 {published data only}
- NCT03741634. Assessing the preliminary effects of a multisectoral agricultural intervention on adolescent girls' health [Shamba Maisha: assessing the preliminary effects of a multisectoral agricultural intervention on the sexual and reproductive health of HIV-affected adolescent girls in Western Kenya]. clinicaltrials.gov/show/NCT03741634 (first posted 15 November 2018).
NCT04101487 2019 {published data only}
- NCT04101487. Cash transfers to increase dietary diversity in Grand Gedeh County, Liberia [A cluster randomized trial to study the effect of cash transfers and nutrition education on dietary diversity among children 6-23 months of age in Grand Gedeh County, Liberia: a pilot study]. clinicaltrials.gov/show/NCT04101487 (first posted 24 September 2019).
Wendt 2019 {published data only}
- Wendt AS, Sparling TM, Waid JL, Mueller AA, Gabrysch S. Food and Agricultural Approaches to Reducing Malnutrition (FAARM): protocol for a cluster-randomised controlled trial to evaluate the impact of a homestead food production programme on undernutrition in rural Bangladesh. BMJ Open 2019;9:e031037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
ACF‐IN 2008
- Action Contre la Faim International Network (ACF-IN). Introduction to food security: intervention principles. www.actionagainsthunger.org/sites/default/files/publications/Introduction_to_food_security_intervention_principles_01.2008.pdf 2008.
Alagiyawanna 2015
- Alagiyawanna A, Townsend N, Mytton O, Scarborough P, Roberts N, Rayner M. Studying the consumption and health outcomes of fiscal interventions (taxes and subsidies) on food and beverages in countries of different income classifications; a systematic review. BMC Public Health 2015;15:887. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arenas 2019
- Arenas DJ, Thomas A, Wang J, DeLisser HM. A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. Journal of General Internal Medicine 2019;34(12):2874-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baird 2014
- Baird S, Ferreira FHG, Ozler B, Woolcock M. Conditional, unconditional and everything in between: a systematic review of the effects of cash transfer programmes on schooling outcomes. Journal of Development Effectiveness 2014;6(1):1-43. [Google Scholar]
Bastagli 2016
- Bastagli F, Hagen-Zanker J, Harman L, Barca V, Sturge G, Schmidt T, et al. Cash transfers: what does the evidence say? A rigorous review of programme impact and of the role of design and implementation features. Overseas Development Institute 2016.
Basu 2013
- Basu S, McKee M, Galea G, Stuckler D. Relationship of soft drink consumption to global overweight, obesity, and diabetes: a cross-national analysis of 75 countries. American Journal of Public Health 2013;103(11):2071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhandari 2003
- Bhandari N, Bahl R, Mazumdar S, Martines J, Black RE, Bhan MK, Infant Feeding Study Group. Effect of community-based promotion of exclusive breastfeeding on diarrhoeal illness and growth: a cluster randomised controlled trial. Lancet 2003;361(9367):1418-23. [DOI: 10.1016/S0140-6736(03)13134-0] [DOI] [PubMed] [Google Scholar]
Bird 2019
- Bird FA, Pradhan A, Bhavani RV, Dangour AD. Interventions in agriculture for nutrition outcomes: a systematic review focused on South Asia. Food Policy 2019;82:39-49. [Google Scholar]
Black 2008
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008;371:243-60. [DOI] [PubMed] [Google Scholar]
Black 2013
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427-51. [DOI] [PubMed] [Google Scholar]
Brown 2006
- Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, et al. How to formulate research recommendations. BMJ 2006;333(7572):804-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns 2010
- Burns C, Kristjansson B, Harris G, Armstrong R, Cummins S, Black A, et al. Community level interventions to improve food security in developed countries. Cochrane Database of Systematic Reviews 2010, Issue 12. Art. No: CD008913. [DOI: 10.1002/14651858.CD008913] [DOI] [Google Scholar]
Carter 2011
- Carter KN, Kruse K, Blakely T, Collings S. The association of food security with psychological distress in New Zealand and any gender differences. Social Science & Medicine 2011;72:1463-71. [DOI] [PubMed] [Google Scholar]
Cole 2011
- Cole SM, Tembo G. The effect of food insecurity on mental health: panel evidence from rural Zambia. Social Science & Medicine 2011;73:1071-9. [DOI] [PubMed] [Google Scholar]
Cotta 2013
- Cotta RMM, Machado JC. Programa Bolsa Família e segurança alimentar e nutricional no Brasil: revisão crítica da literatura. Revista Panamericana de Salud Publica 2013;33(1):54–60. [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Version accessed 27 February 2019. Melbourne, Australia: Veritas Health Innovation.
Dechartres 2013
- Dechartres A, Trinquart L, Boutron I, Ravaud P. Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ 2013;346:f2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JPT, Altman DG, editor(s) In: Cochrane, 2019. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane. 2019. In: Available from www.training.cochrane.org/handbook. [Google Scholar]
Drewnowski 2005
- Drewnowski A. Concept of nutritious food: toward a nutrient density score. American Journal of Clinical Nutrition 2005;82:721-32. [DOI] [PubMed] [Google Scholar]
Ecker 2012
- Ecker O, Breisinger C. The food security system. A new conceptual framework. Washington, DC; International Food Policy Research Institute; 2012. IFPRI discussion paper 01166.
EndNote X8 [Computer program]
- EndNote. Version X8. Philadelphia, PA: Clarivate Analytics, 2016. Available at endnote.com/.
EPOC 2017
- Cochrane Effective Practice and Organisation of Care (EPOC). Suggested risk of bias criteria for EPOC reviews. EPOC Resources for review authors, 2017. epoc.cochrane.org/resources/epoc-resources-review-author 2017.
FAO 2003
- FAO and Sustainable Development Department (SDD). Chapter 2. Food security: concepts and measurement. In: Trade Reforms and Food Security. Conceptualizing the Linkages. Rome: Food and Agriculture Organization of the United Nations, 2003. [Google Scholar]
FAO 2012
- FAO, World Food Programme (WFP) and International Fund for Agricultural Development (IFAD). The State of Food Insecurity in the World 2012. Economic Growth is Necessary but not Sufficient to Accelerate Reduction of Hunger and Malnutrition. Rome: Food and Agriculture Organization, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
FAO 2013
- FAO, IFAD, and WFP. The State of Food Insecurity in the World 2013. The Multiple Dimensions of Food Security. Rome: Food and Agriculture Organization, 2013. [Google Scholar]
FAO 2019
- FAO, IFAD, UNICEF, WFP, and WHO. The State of Food Security and Nutrition in the World 2019. Safeguarding Against Economic Slowdowns and Downturns. Rome: Food and Agriculture Organization, 2019. [Google Scholar]
Garner 2016
- Garner P, Hopewell S, Chandler J, MacLehose H, Akl Elie A, Beyene J, et al. When and how to update systematic reviews: consensus and checklist. BMJ 2016;354:i3507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gittelsohn 2003
- Gittelsohn J, Vastine AE. Sociocultural and household factors impacting on the selection, allocation and consumption of animal source foods: current knowledge and application. Journal of Nutrition 2003;133:4036S-41S. [DOI] [PubMed] [Google Scholar]
Gorham 2015
- Gorham G, Dulin-Keita A, Risica PM, Mello J, Papandonatos G, Nunn A, et al. Effectiveness of Fresh to You, a discount fresh fruit and vegetable market in low-income neighborhoods, on children's fruit and vegetable consumption, Rhode Island 2010-2011. Preventing Chronic Disease 2015;12(10):E176-E. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gross 2000
- Gross R, Schoeneberger H, Pfeifer H, Preuss HA. The four dimensions of food and nutrition security: definitions and concepts. www.fao.org/elearning/course/fa/en/pdf/p-01_rg_concept.pdf 2000.
Guyatt 2010
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction. GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64:383-94. [DOI] [PubMed] [Google Scholar]
Hadley 2006
- Hadley C, Patil CL. Food insecurity in rural Tanzania is associated with maternal anxiety and depression. American Journal of Human Biology 2006;18:359–68. [DOI] [PubMed] [Google Scholar]
Hadley 2008
- Hadley C, Tegegn A, Tessema F, Cowan JA, Asefa M, Galea S. Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: evidence from the Gilgel Gibe growth and development study. Journal of Epidemiology and Community Health 2008;62:980–6. [DOI] [PubMed] [Google Scholar]
Hawkes 2020
- Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet 2020;395(10218):142-55. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC, on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hjelm 2013
- Hjelm L, Dasori W. Ghana Comprehensive Food Security & Vulnerability Analysis, 2012. Rome: World Food Programme, 2013. [Google Scholar]
Hossain 2007
- Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—A growing challenge. New England Journal of Medicine 2007;356(3):213-5. [DOI] [PubMed] [Google Scholar]
Hsiao 2019
- Hsiao BS, Sibeko L, Troy LM. A systematic review of mobile produce markets: facilitators and barriers to use, and associations with reported fruit and vegetable intake. Journal of the Academy of Nutrition and Dietetics 2019;119(1):76. [DOI] [PubMed] [Google Scholar]
Hunter 2017
- Hunter BM, Harrison S, Portela A, Bick D. The effects of cash transfers and vouchers on the use and quality of maternity care services: a systematic review. PLoS ONE 2017;12(3):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
INDDEX Project 2018
- INDDEX Project. Data4Diets: building blocks for diet-related food security analysis. Tufts University, Boston, MA. inddex.nutrition.tufts.edu/data4diets Accessed prior to 27 July 2020.
Leite 2019
- Leite TH, Moraes CL, Marques ES, Caetano R, Braga JU, Reichenheim ME. Women economic empowerment via cash transfer and microcredit programs is enough to decrease intimate partner violence? Evidence from a systematic review. Cadernos de Saude Publica / Ministerio da Saude, Fundacao Oswaldo Cruz, Escola Nacional de Saude Publica 2019;35(9):e00174818. [DOI] [PubMed] [Google Scholar]
Lignani 2011
- Lignani JB, Sichieri R, Burlandy L, Salles-Costa R. Changes in food consumption among the Programa Bolsa Familia participant families in Brazil. Public Health Nutrition 2011;14(5):785-92. [DOI] [PubMed] [Google Scholar]
Liu 2012
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012;379:2151-61. [DOI] [PubMed] [Google Scholar]
MacQueen 2001
- MacQueen KM, McLellan E, Metzger DS, Kegeles S, Strauss RP, Scotti R, et al. What is community? An evidence-based definition for participatory public health. American Journal of Public Health 2001;91(12):1929-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Masset 2011
- Masset E, Haddad L, Cornelius A, Isaza-Castro J. A Systematic Review of Agricultural Interventions that aim to Improve Nutritional Status of Children. London: EPPI-Centre, Social Science Research Unit, Institute of Education, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maynard 2018
- Maynard M, Andrade L, Packull-McCormick S, Perlman CM, Leos-Toro C, Kirkpatrick SI. Food insecurity and mental health among females in high-income countries. International Journal of Environmental Research and Public Health 2018;15:1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKenzie 2019
- McKenzie JE, Brennan SE. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
McLeroy 2003
- McLeroy KR, Norton BA, Kegler MC, Burdine JN, Sumaya CV. Community-based interventions. American Journal of Public Health 2003;93(4):529-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melo 2016
- Melo L, da Costa Uchoa S, Cobucci R, Costa J, Costa A, Gois I, et al. Conditional cash transfer program effects on anthropometric index from children in Latin America: a systematic review. Health 2016;8(7):664-71. [Google Scholar]
Microsoft Excel 2007 [Computer program]
- Microsoft Office Excel. Redmond, WA: Microsoft Corporation, 2007. Available from www.microsoft.com/en-ca/microsoft/excel.
Ministry of Health of Brazil 2014
- Ministry of Health of Brazil. Dietary guidelines for the Brazilian population. 2nd edition. Brasilia: Ministry of Health of Brazil, Secretariat of Health Care, Primary Health Care Department, 2014. [Google Scholar]
Mizdrak 2015
- Mizdrak A, Scarborough P, Waterlander WE, Rayner M. Differential responses to food price changes by personal characteristic: a systematic review of experimental studies. PloS One 2015;10(7):e0130320. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohammadifard 2009
- Mohammadifard N, Kelishadi R, Safavi M, Sarrafzadegan F, Sajadi F, Sadri GH, et al. Effect of a community-based intervention on nutritional behaviour in a developing country setting: the Isfahan Healthy Heart Programme. Public Health Nutrition 2009;12(9):1422-30. [DOI] [PubMed] [Google Scholar]
MOHP 2012
- Ministry of Health and Population (MOHP) Nepal, New ERA, ICF International Inc. Nepal Demographic and Health Survey 2011. Calverton, USA: Kathmandu, Nepal: Ministry of Health and Population, New ERA, and ICF International, 2012. [Google Scholar]
Munk 2019
- Munk C, Portnoy A, Suharlim C, Clarke-Deelder E, Brenzel L, Resch SC, et al. Systematic review of the costs and effectiveness of interventions to increase infant vaccination coverage in low- and middle-income countries. BMC Health Services Research 2019;19(1):741. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ng 2014
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Olsho 2016
- Olsho LEW, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among Supplemental Nutrition Assistance Program participants: a randomized controlled trial of the USDA Healthy Incentives Pilot. American Journal of Clinical Nutrition 2016;104(2):423-35. [DOI] [PubMed] [Google Scholar]
Owuso‐Addo 2014
- Owusu-Addo E, Cross R. The impact of conditional cash transfers on child health in low- and middle-income countries: a systematic review. International Journal of Public Health 2014;59:609-18. [DOI] [PubMed] [Google Scholar]
Owusu‐Addo 2018
- Owusu-Addo E, Renzaho AMN, Smith BJ. The impact of cash transfers on social determinants of health and health inequalities in sub-Saharan Africa: a systematic review. Health Policy Plan 2018;33(5):675-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pega 2017
- Pega F, Liu SY, Walter S, Pabayo R, Saith R, Lhachimi SK. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low- and middle-income countries. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No: CD011135. [DOI: 10.1002/14651858.CD011135.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pennington 2007
- Pennington J, Kandiah J, Nicklas T, Pitman S, Stitzel K. Practice paper of the American dietetic association: nutrient density: meeting nutrient goals within calorie needs. Journal of the American Dietetic Association 2007;107(5):860-9. [DOI] [PubMed] [Google Scholar]
Pinstrup‐Andersen 2009
- Pinstrup-Andersen P. Food security: definition and measurement. Food Security 2009;1:5-7. [Google Scholar]
Popkin 2012
- Popkin BM, Adair LS, Wen Ng S. Now and then: the global nutrition transition: the pandemic of obesity in developing countries. Nutrition Reviews 2012;70(1):3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pullar 2018
- Pullar J, Allen L, Townsend N, Williams J, Foster C, Roberts N, et al. The impact of poverty reduction and development interventions on non-communicable diseases and their behavioural risk factors in low and lower-middle income countries: a systematic review. PloS One 2018;13(2):e0193378-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rank 2003
- Rank MR, Brown GW, Chonbuk HY, Hirschl TA. American poverty as a structural failing: evidence and arguments. Journal of Sociology and Social Welfare 2003;30(4):3-29. [Google Scholar]
Renzaho 2010
- Renzaho AMN, Mellor D. Food security measurement in cultural pluralism: missing the point or conceptual misunderstanding? Nutrition 2010;26:1-9. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richterman 2018
- Richterman A, Steer-Massaro J, Jarolimova J, Luong Nguyen LB, Werdenberg J, Ivers LC. Cash interventions to improve clinical outcomes for pulmonary tuberculosis: systematic review and meta-analysis. Bulletin of the World Health Organization 2018;96(7):471-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rohwer 2016
- Rohwer A, Pfadenhauer L, Burns J, Brereton L, Gerhardus A, Booth A, et al. Logic models help make sense of complexity in systematic reviews and health technology assessments. Journal of Clinical Epidemiology 2016;83:37-47. [DOI: 10.1016/j.jclinepi.2016.06.012.] [DOI] [PubMed] [Google Scholar]
Ruel 2013
- Ruel MT, Alderman H, the Maternal and Child Nutrition Study Group. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? Lancet 2013;382:536-51. [DOI] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Cuello C, Akl EA, Mustafa RE, Meerpohl JJ, Thayer K, et al. GRADE Guidelines: 18. How ROBINS-I and other tools to assess risk of bias in non-randomized studies should be used to rate the certainty of a body of evidence. Journal of Clinical Epidemiology 2019;111:105-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shea 2009
- Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. Journal of Clinical Epidemiology 2009;62(10):1013-20. [DOI] [PubMed] [Google Scholar]
Siddiqi 2018
- Siddiqi A, Rajaram A, Miller SP. Do cash transfer programmes yield better health in the first year of life? A systematic review linking low-income/middle-income and high-income contexts. Archives of Disease in Childhood 2018;103(10):920-6. [DOI] [PubMed] [Google Scholar]
Singh 2017
- Singh S. How to conduct and interpret systematic reviews and meta-analyses. Clinical Translational Gastroenterology 2017;8(5):e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2006
- Smith LC, Alderman H, Aduayom D. Washington, DC; International Food Policy Research Institute. 2006. Food insecurity in Sub-Saharan Africa. New estimates from household expenditure surveys.
SOWC 2019
- UNICEF. New York; UNICEF. The state of the world's children 2019. Children, food and nutrition: growing well in a changing world. 2019.
Sterne 2019
- Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Subramanian 2011
- Subramanian SV, Perkins JM, Özaltin E, Davey Smith G. Weight of nations: a socioeconomic analysis of women in low- to middle-income countries. American Journal of Clinical Nutrition 2011;93(2):413-21. [DOI: 10.3945/ajcn.110.004820] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tugwell 2010
- Tugwell P, Petticrew M, Kristjansson E, Welch V, Ueffing E, Waters E, et al. Assessing equity in systematic reviews: realising the recommendations of the Commission on Social Determinants of Health. BMJ 2010;341:c4739. [DOI] [PubMed] [Google Scholar]
UN 2015
- United Nations. Resolution adopted by the General Assembly on 25 September 2015. Transforming our world: the 2030 Agenda for Sustainable Development. www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_1_E.pdf.
Victora 2008
- Victora CG, Adair LF, Fall C, Hallal P, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2010
- World Health Organization. Chapter 1. Burden: mortality, morbidity and risk factors. Report on Noncommunicable Diseases 2010. Description of the Global Burden of NCDs, their Risk Factors and Determinants 2010.
WHO 2013
- World Health Organization. Food Security. Available at www.who.int/trade/glossary/story028/en/ Accessed prior to 27 July 2020.
World Bank 2020
- World Bank. World Bank country and lending groups. www.datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed prior to 14 July 2020).
References to other published versions of this review
Durao 2015
- Durao S, Schoonees A, Ramokolo V, Oliveira JMD, Kristjansson E. Community-level interventions for improving access to food in low- and middle-income countries. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No: CD011504. [DOI: 10.1002/14651858.CD011504] [DOI] [PMC free article] [PubMed] [Google Scholar]


