Abstract
Disparities in the experience of chronic musculoskeletal pain in the United States stem from a confluence of a broad array of factors. Organized within the National Institute on Aging Health Disparity Research Framework, a literature review was completed to evaluate what is known and what is needed to move chronic musculoskeletal pain research forward specific to disproportionately affected populations. Peer-reviewed studies published in English, on human adults, from 2000 to 2019, and conducted in the United States were extracted from PubMed and Web of Science. Articles were reviewed for key words that focused on underrepresented ethnic/race groups with chronic musculoskeletal pain applying health factor terms identified in the NIA Health Disparity Research Framework four levels of analysis: 1) environmental, 2) sociocultural, 3) behavioral, and 4) biological. A total of 52 articles met inclusion criteria. There were limited publications specific to underrepresented ethnic/race groups with chronic musculoskeletal pain across all levels with particular research gaps under sociocultural and biological categories. Current limitations in evidence may be supplemented by a foundation of findings specific to the broader topic of “chronic pain” which provides guidance for future investigations. Study designs including a focus on protective factors and multiple levels of analyses would be particularly meritorious.
Perspective: Chronic musculoskeletal pain unequally burdens underrepresented ethnic/race groups. In order to move research forward and to systematically investigate the complex array of factors contributing toward health disparities, an organized approach is necessary. Applying the NIA Health Disparities Research Framework, an overview of the current state of evidence specific to chronic musculoskeletal pain and underrepresented ethnic/race groups is provided with future directions identified.
Keywords: Health disparities, chronic musculoskeletal pain, aging, ethnicity/race, health factors
Chronic musculoskeletal pain, pain experienced in areas of the body involving muscles, joints, ligaments, and/or tendons; affects 116 million Americans and is a leading cause of disability, loss of work, and loss of participation in life activities.10,33,39,103 A number of factors contribute toward the development and persistence of chronic musculoskeletal pain: biological (co-morbidities and age-related health changes); sociocultural (depression, anxiety, coping patterns, and social support); behavioral (smoking, lack of exercise, and poor-quality diet); and environmental (low education, lack of quality health care, and poverty).19,46,102,105,121,155 The confluence of contributing factors is not equitable, with a number of ethnic/race groups experiencing a greater incidence, prevalence, and severity of chronic musculoskeletal pain compared to non-Hispanic Whites.3,17,29,161,162 The consequences of chronic musculoskeletal pain extend beyond functional limitations and reduced quality of life to include increased psychosocial distress, comorbidities, and greater risk of mortality.18,35,100,104
Health disparities are not unique to pain, as disproportionally affected groups carry a greater disease burden across a wide array of health conditions and outcomes.57,97,106,125 Research efforts across disciplines have provided evidence of a broad array of factors across multiple levels contributing to health disparities among underrepresented ethnic and/or race groups. Factors extend from the macro level (environment and societal influences) to the micro level (individual) with varying influences across the life course.27,31,36,67,88,119,146 Theoretical and conceptual models are evolving to reflect the complex and dynamic array of factors contributing to health disparities and organizational efforts are underway to inform, guide, and fund research efforts moving forward.8,20,50,113
In 2015, the National Institute on Aging (NIA) developed a Health Disparities Research Framework with the goal of providing a structure in which to evaluate health disparity research to promote the health of adults across the life span. The intentions underlying these efforts were to develop an organizational framework to promote an interdisciplinary research focus; evaluate existing research and identify gaps; improve the integration between mechanisms and pathways; and promote the infrastructure to assist in the identification of novel approaches and targets. The NIA Framework was designed to facilitate an “age-related, multidimensional, across the life course” focus comprised of 4 levels of analyses: environmental, sociocultural, behavioral, and biological.77
In order for research specific to disparities in the experience of chronic musculoskeletal pain to move forward, an organized approach is necessary to understand what has been addressed and identify current gaps. Therein lies the intention of this initial literature review. Applying the NIA Health Disparities Research Framework (https://www.nia.nih.gov/research/osp/framework), we evaluate published research specific to identified health factor terms across priority areas within each level of analysis in the area of chronic musculoskeletal pain and underrepresented ethnic/race groups. The goal of this review is to help determine what is known and what is needed to advance research to reduce disparities in chronic musculoskeletal pain and improve health outcomes.
Methods
We conducted a review of the literature with health factor search terms defined by the priority areas listed under each level of analysis (see Table 1) identified in the NIA Health Disparities Research Framework, Fig 1. The search included health factor NIA Framework terms combined with pain-related terms such as “pai” “chronic pai” “musculoskeletal pain,” or “chronic musculoskeletal pain” and one of the following terms “health disparities” or “ethnicity” or “race.” Additionally, based on the productivity of the search term combinations, variations were included such as reducing the number of terms in the search or exploring alternative phrasing associated with the health factor terms (eg, emotional regulation – emotion, emotion dysregulation; physical activity – exercise; occupation – job, work, employment).
Table 1.
Health Factor Search Terms for Each Level of Analysis in the NIA Health Disparities Research Framework
| Environmental | Sociocultural | Behavioral | Biological |
|---|---|---|---|
| Structural Bias | Values | Active Coping | Comorbidities |
| Immigration and/or Documentation | Prejudice | Problem Solving | Cardiovascular |
| Criminalization | Norms | Stress Management | Sympathetic Nervous System |
| Residential Segregation | Traditions | Cognitive Reframing | HPA Axis |
| Urban and/or Rural | Religion | Emotional Regulation | Inflammation |
| Toxins and/or Exposures | Collective Responses | Social Support | Telomere Attrition |
| Education | Institutional Racism | Discrimination | Epigenetic Alteration |
| Income and/or Wealth | Family Stress | Pessimism | Loss of Proteostasis |
| Occupation | Financial Stress | Optimism | Deregulated Nutrient Sensing |
| Limited English | Occupational Stress | Control | Mitochondrial Dysfunction |
| Health Care Access | Residential Stress | Smoking | Cellular Senescence |
| Insurance | Social Mobility | Anger and/or Violence | Cellular Stress Response |
| Quality | Social Network | Alcohol and/or Drug | Stem Cell Exhaustion |
| Literacy | Self-Concepts | Nutrition | Intercellular Communication |
| Numeracy | Stigma | Physical Activity | |
| Bias | |||
| Loneliness | |||
| Stereotypes |
Figure 1.
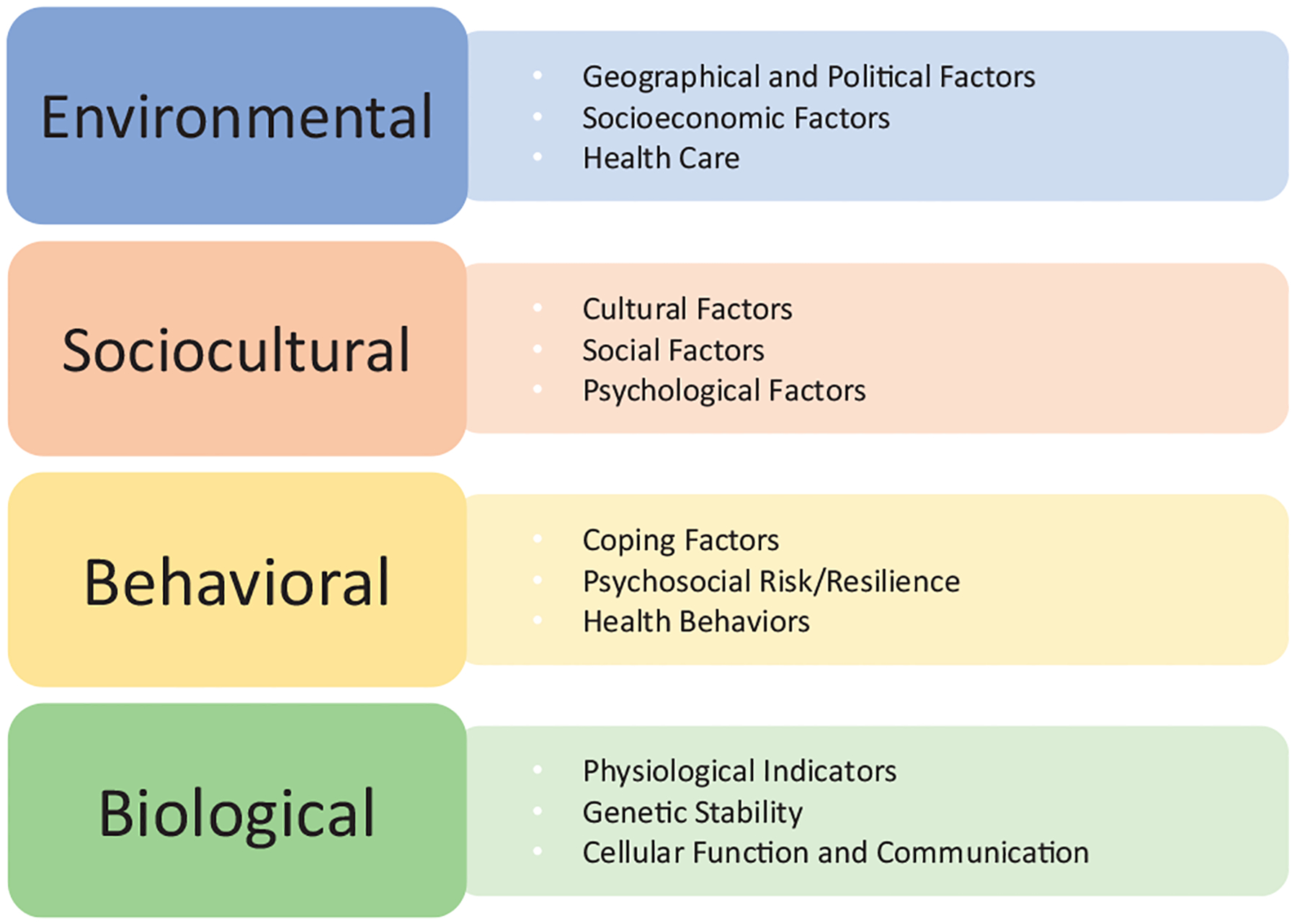
The Levels of Analyses and Priority Focus Areas in the NIA Health Disparities Research Framework.Adapted from the National Institute on Aging Health Disparities Research Framework (Hill et. al, 2015).
Peer-reviewed articles were identified using PubMed, Web of Science, and the reference lists of identified articles. We restricted our search to articles published in English and conducted in the United States between the years 2000 to 2019, on human adults (≥ 18 years old). Inclusion criteria included: 1) studies specific to chronic musculoskeletal pain, chronic musculoskeletal pain conditions (eg, low back pain, osteoarthritis pain, rheumatoid arthritis, fibromyalgia), or associated with chronic musculoskeletal pain conditions; and 2) analyses specific to underrepresented ethnic/race groups. Articles were excluded if they addressed acute or sub-acute musculoskeletal pain lasting less than 3 months, were study protocols, or systematic reviews. Additional exclusion criteria included: pain after stroke, diabetic peripheral neuropathy, post-amputation, cancer-related pain, or chronic pelvic pain. In the first step of data extraction, titles and abstracts were searched by a minimum of 2 coauthors for each level of analysis outlined in the NIA Health Disparities Research Framework: MP and DF – Environmental; SQB, SP, AMM, MP – Sociocultural; EJB, AJJ, LD - Behavioral; and KPR, ELT, AMM – Biological. Full-text articles were reviewed by the level of analysis team (above), to determine inclusion. Final decisions were determined by a consensus of three authors when applicable (AJJ, AMM, and KTS). Due to the broad and overlapping nature of search terms, some articles were applicable to more than one level of analysis. Fifty-two articles (7 articles addressing 2 different levels of analyses) aligned with the above criteria and were included in the review. Included articles are presented in Tables 2–5.
Table 2.
Articles That Met Inclusion Criteria Under the Environmental Level of Analysis
| Author(s) | Year | Study Location | Study Type | Study Population | Health Factor(s) | Outcome Measure(s) |
|---|---|---|---|---|---|---|
| Geographical and Political Factors | ||||||
| No articles met inclusion criteria | ||||||
| Socioeconomic Factors | ||||||
| Gansky et al | 2007 | Berkeley, California, Cincinnati, Ohio | Cross-sectional | n = 1,334 young (21–26 years old) women (684 African American and 650 Caucasian individuals) | Income/wealth | Distribution of widespread pain, tender points and fibromyalgia |
| Thompson et al | 2019 | Birmingham, Alabama Gainesville, Florida | Cross-sectional | n = 191 adults with knee osteoarthritis | Income/wealth | Poverty status, knee pain |
| Health Care | ||||||
| Albert et al | 2008 | United States | Cross-sectional | n = 551 Medicare beneficiaries with osteoarthritis | Health care access | Self-management behaviors |
| Burgess et al | 2008 | United States | Factorial design | n = 382 primary care physicians randomly selected from the American Medical Association Physician Masterfile | Health care quality | Physician’s decision to switch patient to a higher dose or stronger type of opioid in chronic pain patients |
| Burgess et al | 2014 | United States | Retrospective | n = 99,903 veterans with diagnoses of chronic low back, neck, or joint pain selected to participate in the Veterans Affairs Survey of the Healthcare Experiences of Patients in fiscal year 2006 | Health care quality | Prescription of opioids in the year following the first pain diagnosis |
| Burgess et al | 2016 | United States | Retrospective | n = 3,505 Black and n = 46,203 non-Hispanic White patients with diagnoses of chronic musculoskeletal pain who responded to the 2007 Veterans Affairs Survey of Healthcare Experiences of Patients | Health care quality | Pain treatments, pain outcomes |
| Carey et al | 2010 | North Carolina | Cross-sectional | n = 837 respondents (620 White, 183 African American, 34 Latino) with chronic back or neck pain | Health care access | Pain 1–10 scale, Roland-Morris back-specific disability scale, health care utilization, opioid use |
| Dominick et al | 2004 | Durham, North Carolina | Retrospective | n = 3,061 patients with osteoarthritis treated at a federal Veterans Affairs Medical Center between October 1998 and September 1999 | Health care quality | Opioid variables |
| Dominick et al | 2004 | United States | Retrospective cohort | n = 6,038 veterans with osteoarthritis | Health care quality | Non-steroidal anti-inflammatory prescribed, amount and time to discontinuation of index non-steroidal anti-inflammatory |
| Evans et al | 2018 | United States | Retrospective | n = 79,537 women and n = 389,269 men veterans age 18−54 with chronic musculoskeletal pain who received Veteran Affairs-provided care between 2010 and 2013 | Health care quality | Predictors of complementary and integrative health therapies as non-pharmacological approaches for chronic pain |
| Hausmann et al | 2013 | United States | Retrospective Cohort | nnd 253 African American patients) patients who filled opioid prescriptions for non-cancer pain (predominately musculoskeletal) for 90 consecutive days at the Veterans Affairs Pittsburgh Healthcare System pharmacy in fiscal years 2007 and 2008 | Health care quality; Health care access | Opioid monitoring and treatment practices |
| Hausmann et al | 2017 | United States | Retrospective cohort | n = 473,170 White, n = 50,172 African American and n = 16,499 Hispanic veterans age 50 years or older with an osteoarthritis diagnosis from 2001 to 2011 | Health care quality | Total knee arthroplasty |
| Heins et al | 2006 | Mobile, Alabama | Retrospective | n = 868 Emergency Department patients 18 years and older who presented with musculoskeletal pain and were treated by core Emergency Department faculty | Health care access | Prescription of Emergency Department opioids and discharge analgesics |
| Ibrahim et al | 2002 | United States | Cross-sectional | n = 596 elderly, male, African American or White patients with moderate-to-severe symptomatic knee or hip osteoarthritis who were receiving primary care at the Department of Veterans Affairs outpatient clinics | Health care access | Willingness to undergo a total knee arthroplasty |
| Katz et al | 2011 | Boston, Massachusetts | Qualitative study | n = 39 Hispanic and non-Hispanic White patients with chronic back or knee pain | Health care quality | Decision management of their conditions and roles they preferred in medical decision-making |
| Parker et al | 2011 | New York City, New York | Prospective cohort | n = 112 (37 African American, 38 Hispanic, and 37 non-Hispanic White adults) 60-years-old and older with non-cancer pain | Health care quality | Impact of the Arthritis Foundation Self-Help Program |
| Tait et al | 2006 | Missouri | Cross-sectional | n =580 African American and n = 892 White workers’ compensation claimants with occupational low back pain | Health care access; Health care insurance | Disability ratings, diagnosis, surgery, medical costs |
| Taylor et al | 2005 | United States | Retrospective | n = 5,690 patients with degenerative lumbosacral pathologies | Health care access | Lumbosacral pathologies |
Table 5.
Articles that Met Inclusion Criteria Under the Biological Level of Analysis
| Physiological Indicators |
| No articles met inclusion criteria |
| Genetic Stability |
| No articles met inclusion criteria |
| Cellular Function and Communication |
| No articles met inclusion criteria |
Terms used to identify ethnic/race groups in the Results section are consistent with the phrasing used in the original publications. The National Institutes of Health (NIH) requires funded clinical researchers to collect and report data on ethnicity/race.116 A 2-question format in the order of ethnicity first and race second is the suggested data collection approach.81 Current Ethnicity categories are limited to Hispanic or Latino and non-Hispanic or Latino. Race categories include: 1) American Indian or Alaska Native, 2) Asian, 3) Black or African American, 4) Native Hawaiian or Other Pacific Islander, and 5) White. Where applicable, we will incorporate phrasing in line with NIH guidelines (eg, Introduction and Discussion sections).
Results
Environmental Level
The priority areas identified under the Environmental level of analysis in the NIA Health Disparities Research Framework are: 1) geographical and political; 2) socioeconomic; and 3) health care.77 Population-level experiences result in a variety of differential exposures and influence health outcomes. Research on environmental factors, ethnic and/or race groups, and chronic musculoskeletal pain is critical to better understand and address the disparities in outcomes. Our search resulted in 18 articles specific to the Environmental level of analysis (Table 2).
Geographical and political factors are recognized as influencing health outcomes. Health factor terms under this priority area include structural bias, immigration and documentation, criminalization, residential segregation, urban and/or rural residence, and toxin exposure.77 Our search did not reveal studies specific to geographical and political factors and chronic musculoskeletal pain. Further research in the area of geographical and political factors and chronic musculoskeletal pain with consideration for underrepresented ethnic/race groups are needed.
Socioeconomic status (SES) is a second priority focus area under the Environmental level of analysis. Health factors identified under the priority area of SES includes education, income and/or wealth, occupation, and English language proficiency.77 In a study of individuals with knee pain with or at risk for knee osteoarthritis, SES has been shown to interact with ethnic/race groups such that non-Hispanic Black individuals below the federal poverty line reported greater clinical pain compared with non-Hispanic White individuals who were also below the federal poverty line.156 Among young women (ages 22–26 years old), African American individuals reported lower SES and more widespread musculoskeletal pain than their Caucasian counterparts.55 Body pain was also significantly associated with lower subjective SES and worse reported heath in individuals with chronic musculoskeletal pain.55 Low educational attainment, regardless of ethnicity/race is associated with poor outcomes in both radiographic and symptomatic knee osteoarthritis.26,69 Language can also be a significant barrier in forming meaningful physician-patient interactions in accessing care. Findings highlight the importance of considering SES and English literacy when evaluating health disparities in chronic musculoskeletal pain.
Health care factors are the third priority area under the Environmental level of analysis with identified health factor terms to include access, insurance, quality, literacy and numeracy.77 As previously noted, African American individuals report higher levels of clinical pain compared to non-Hispanic White individuals.28,161,162 Findings also suggest disparities in health care treatment such that African American patients generally receive less opioid and non-steroidal anti-inflammatory prescriptions compared to White patients with chronic musculoskeletal pain.24,42,43,74 Further, findings suggest that African American adults undergo increased opioid monitoring and receive fewer referrals to pain specialists compared to Hispanic and non-Hispanic White adults.72 Another study found among black patients who “demanded specific narcotics or exhibited anger” were more likely to receive a higher and/or stronger opioid dose with the opposite treatment pattern found for white patients, a higher and/or stronger opioid dose for those with “non-challenging” verbal behaviors.22 African American persons experiencing chronic musculoskeletal pain are also less likely to receive diagnostic imaging tests and surgical interventions, particularly in individuals with lower education and income levels.71,79,153 Additionally, physician characteristics (eg, gender, ethnicity, resident and/or attending, pain management training) were indicated in a pilot study of treatment plans in individuals with chronic low back and lower extremity pain. Although the sample size was limited, findings indicated male physicians were more likely to prescribe valium and physical therapy with female physicians more likely to prescribe psychological counseling. Additionally, resident status was associated with more condition-related instruction.114 A survey of workers’ compensation claimants with occupational low back pain found that African American workers had higher disability ratings and medical costs following claims.150 Further, researchers have reported ethnic/race group differences in the use of non-pharmacological interventions and self-management strategies for chronic musculoskeletal pain.4,51 Importantly, the Arthritis Foundation Self-Help Program, comprised of 6 weekly small group sessions on exercises, cognitive coping, relaxation and other pain related self-care skills performed at 3 community centers in New York City, found improvements across all outcome measures particularly with reductions in pain intensity and increases in physical activity. However, there was higher attendance and greater positive improvements by Hispanic participants. The Spanish program differed from the English program in that Spanish participants had sessions in Spanish, with time to perform exercises during session and take home instructional CDs not offered in the English program.122 Although findings are inconsistent regarding ethnic/race group differences in health care related factors,23,28 it is evident that health care plays a key role in improving health outcomes in individuals from underrepresented ethnic/race groups with chronic musculoskeletal pain.
Sociocultural Level
The Sociocultural level of analysis in the NIA Health Disparities Research Framework includes the following priority areas: 1) cultural; 2) social; and 3) psychological.77 Six articles were identified from searches for studies that investigated chronic musculoskeletal pain, ethnic/race groups, and factors within the sociocultural level of analysis (Table 3). Although, there were limited references specific to chronic musculoskeletal pain, findings illuminate a direction for future research.
Table 3.
Articles that Met Inclusion Criteria Under the Sociocultural Level of Analysis
| Author(s) | Year | Study Location | Study Type | Study Population | Health Factor(s) | Outcome Measure(s) |
|---|---|---|---|---|---|---|
| Cultural Factors | ||||||
| Katz et al | 2011 | Boston, Massachusetts | Qualitative study | n = 234 Hispanic and non-Hispanic White individuals with chronic back or knee pain from urban medical center | Religion | Areas important in medical decision-making |
| Ibrahim et al | 2004 | Cleveland, Ohio | Qualitative Study | n = 75 African Americans with hip and knee pain | Religion | African American’s perceptions and preferences for care |
| Mingo | 2013 | Tampa, Florida, Atlanta, Georgia | Qualitative Study | n = 198 (85 White individuals, 113 African American individuals) | Values | Willingness to help family member with Osteoarthritis |
| Social Factors | ||||||
| Blake et al | 2002 | New Hyde Park, New York | Cross-sectional | n = 515 Black and n = 455 White Medicare beneficiaries | Social Network | Social network experience with surgery and perceptions of benefit |
| Ibrahim et al | 2002 | United States | Cross-sectional | n = 596 elderly, male, African American and White patients with knee/hip osteoarthritis receiving primary care at the Department of Veterans Affairs clinics | Social Network | Willingness to undergo a total knee arthroplasty |
| McIlvane et al | 2008 | Florida | Cross-sectional | n = 175 African American and White women aged 45–90 | Financial Stress | Arthritis-related stress, discrimination, chronic life and financial stress, and well-being |
| Psychological Factors | ||||||
| No articles met inclusion criteria | ||||||
Cultural factors are the first priority area under the Sociocultural level of analysis with health factors to include values, prejudice, norms, traditions, religion, and collective responses.77 Cultural factors indeed play an important role in influencing health beliefs and health behaviors.2,49,75,90 Unfortunately, the evidence specific to cultural factors, chronic musculoskeletal pain, and ethnic/race groups is limited. In a qualitative study of older adults randomly assigned vignettes describing a family member with chronic pain associated with osteoarthritis found older African American adults reported a more optimistic perspective of the benefits of health care and indicated greater willingness to provide care to the family member compared to White adults.111 In another qualitative study of patients with chronic back or knee pain, Hispanic patients indicated religion and faith to be important factors involved in medical and/or health-related decision-making and were more likely to let their physicians take the lead role in their medical care decisions compared to their non-Hispanic white peers.89 Passive coping skills such as praying and hoping was more prevalent in Hispanic patients than non-Hispanic whites.122 Additionally, African American individuals with chronic knee or hip pain expressed in regards to their care, faith was important however, physician’s ethnicity and/or race or religion was not.80 Further research providing an improved understanding of the relationships between cultural factors and chronic musculoskeletal pain would be beneficial.
Social factors are the second priority area under the Sociocultural level of analysis. Health factor terms in this priority area include family stress, financial stress, occupational stress, residential stress, social mobility, social networks, and institutional racism.77 Social factors are associated with stress and pain25,46,85,94,95,114,120,142 and health disparities.1,40 McIlvane (2007) reported that psychological well-being, as measured by the Center for Epidemiological Studies Depression Scale and the Satisfaction with Life Scale, was significantly impacted by both education and race by education, such that African American women with low education had higher depressive symptoms than African American women with high education, but that these differences were not present in White women. Additionally, African American women with arthritis-related pain reported more religious coping, wishful-thinking, emotional expression, and seeking social support compared to White women with arthritis-related pain, irrespective of education.107 Researchers have also demonstrated the importance of social networks on perceived benefits of arthritis interventions, including surgery. It was shown that Black individuals with hip and knee pain tended to report knowing fewer people for whom surgery was beneficial, and therefore perceived such procedures to be less helpful.16 African American adults who were single with lower education, lower income, and greater unemployment were less familiar with total knee replacement outcomes and were less likely to undergo surgery.79 Although limited, findings highlight the influence of social factors on musculoskeletal pain and the need for further research.
Psychological factors are the third priority area under the Sociocultural level of analysis with health factor terms to include self-concepts, stigma, bias, loneliness and stereotypes.77 These health factors may shape individual health care decisions further influencing inequalities in the experience of chronic musculoskeletal pain. The literature search did not identify studies specific to the identified health factor terms, ethnicity/race, and chronic musculoskeletal pain. Research is needed to appreciate the relevance of psychological factors within the sociocultural level of analysis that impact individual and population health behaviors contributing to health disparities.
Behavioral Level
The Behavioral level of analysis in the NIA Health Disparities Research Framework includes the following 3 priority areas: 1) coping factors; 2) psychosocial risk and/or resilience factors; and 3) health behaviors.77 Psychosocial and behavioral factors are well-recognized as highly relevant to health outcomes.52,134 Similarly, pain-related coping styles, psychosocial factors, and health behaviors have been associated with ethnic/race differences in chronic musculoskeletal pain and related functional limitations.109,119 A total of 34 studies were identified specific to the Behavioral level of analysis (Table 4).
Table 4.
Articles that Met Inclusion Criteria Under the Behavioral Level of Analysis
| Author(s) | Year | Study Location | Study Type | Study Population | Health Factor(s) | Outcome Measure(s) |
|---|---|---|---|---|---|---|
| Coping Factors | ||||||
| Allen et al | 2006 | Durham, North Carolina | Daily diary analysis | n = 36 patients with osteoarthritis (13 non-White, 23 White patients) | Emotional regulation | 30-day diaries of pain and coping |
| Allen et al | 2010 | North Carolina | Interventional | n = 491 African Americans and Caucasian individuals enrolled in telephone-based osteoarthritis self-management | Emotional regulation | Arthritis self-efficacy, affect, and use of emotion-focused coping |
| Allen et al | 2019 | North Carolina | Randomized Control | n = 284 African American individuals with osteoarthritis pain | Cognitive Reframing | Pain, disability, general health, coping, pain catastrophizing, depressive symptoms after pain coping skills training program |
| Booker et al | 2019 | Gainesville, Florida | Cross-sectional | n = 162 non-Hispanic Black and non-Hispanic White older adults with knee pain | Active Coping | Identify ethnic/race group differences on movement evoked pain, physical performance and perceived stress |
| Edwards, RR | 2005 | United States | Cross-sectional | n = 1,800 individuals with chronic musculoskeletal (14.9% African American, 79.2% White, 5.9% Hispanic) | Coping | Pain, emotional distress, pain-related disability, and pain coping |
| Hausmann et al | 2018 | Pittsburgh, Philadelphia, Pennsylvania | Randomized controlled | n = 360 non-Hispanic White, n = 180 non-Hispanic African American patients aged >50, diagnosis of osteoarthritis | Cognitive Reframing | Self-reported pain and functional difficulty in response to positive psychological intervention compared to neutral control intervention. |
| Lumley et al | 2005 | Michigan | Cross-sectional | n =155 patients with rheumatoid arthritis, n =160 migraine headaches, n = 123 systemic lupus | Emotional regulation | Toronto Alexithymia Scale, pain severity, functional disability, symptoms |
| Mcilvane, JM | 2007 | Florida | Cross-sectional | n = 175 individuals (77 African American, 98 White individuals) with arthritis | Active Coping | Arthritis related symptoms, coping and well-being |
| Psychological Risk/Resilience | ||||||
| Bartley et al | 2019 | Gainesville, Florida | Cross-sectional | n = 201 individuals with knee osteoarthritis (105 African American, 96 White) | Optimism | Resilience, clinical pain and functioning performance |
| Edwards, RR | 2008 | United States | Cross-sectional | N > 3,000 from the National Survey of Midlife Development | Discrimination | Perceived discriminatory events and back pain frequency |
| Goodin et al | 2013 | Birmingham, Alabama, Gainesville, Florida | Cross-sectional | n = 130 older adults with knee osteoarthritis; (67 African American, 63 White adults) | Discrimination | Racial discrimination, response to noxious thermal stimuli |
| Groeneveld et al | 2008 | Pittsburgh, Pennsylvania, Philadelphia, Pennsylvania | Cross-sectional | n = 909 male patients with osteoarthritis; (450 African American, 459 White patients) | Social support | Patients expectations of joint replacement |
| Herbert et al | 2017 | Birmingham, Alabama, Gainesville, Florida | Cross-sectional | n = 91 individuals with knee osteoarthritis; (56 African American, 35 White individuals) | Discrimination | Cortisol, pain responses during cold pressor task, racial discrimination |
| Mcilvane, JM | 2007 | Florida | Cross-sectional | n = 175 individuals with arthritis (77 African American, 98 White individuals) | Social Support | Arthritis related symptoms, coping and well-being |
| Mcilvane et al | 2008 | Florida | Cross-sectional | n = 175 African American and White women aged 45–90 | Discrimination | Arthritis-related stress, discrimination, chronic life and financial stress, and well-being |
| Tan et al | 2005 | Texas | Cross-sectional | n = 482 individuals with chronic pain at multiple body sites (128 African American, White individuals) | Control | Pain appraisal, beliefs about pain, ways of coping with pain |
| Health Behaviors | ||||||
| Bessiner et al | 2012 | New York City, NY | Interventional | n = 69 seniors with chronic back pain (24 African American, 25 Hispanic, and 20 non-Hispanic White individuals) | Physical Activity | Impact of self-management program combines cognitive-behavioral strategies and exercise |
| Dodani et al | 2016 | St. Louis, Missouri, Gainesville, Florida, and Jacksonville, Florida | Cross-sectional | n = 6,145 African and Caucasian reporting cocaine use | Alcohol/Drug | Differences in clinical characterizes and musculoskeletal conditions by cocaine use |
| Eberly et al | 2018 | New Mexico | Retrospective | n = 355 new patients with knee osteoarthritis | Alcohol/Drug Smoking | Knee pain scores, psychosocial, sociodemographic, disease and treatment |
| Foley et al | 2015 | North Carolina | Cohort study | n = 1,422 individuals with hip osteoarthritis | Smoking | Pain, stiffness, radiographic features |
| Glover et al | 2012 | Gainesville, Florida | Cross-sectional | n = 94 individuals with symptomatic knee osteoarthritis, 45–71 y old | Nutrition | Vitamin D levels, osteoarthritis pain |
| Goeppinger et al. | 2007 | North Carolina | Randomized Controlled | n = 416 older adults with arthritis (365 African American adults) | Physical Activity | Health care use, health related quality of life health behaviors and arthritis self-efficacy between Arthritis-Self-Help Course and Chronic Disease Self-Management Program |
| Golightly et al | 2005 | North Carolina | Cross-sectional | n = 202 African American and Caucasian veterans with osteoarthritis | Physical Activity | Osteoarthritis symptom severity |
| Jones et al | 2018 | Chicago, Illinois | Interventional | n = 62, 40–75 years old adults with non-traumatic knee pain and BMI > 30 (32 African American, 30 Hispanic/Latino adults), 40–75 years old with nontraumatic knee pain and BMI > 30 | Physical Activity | Efficacy of a community-base, culturally sensitive program to stimulate behavioral changes in activity level |
| Parker et al | 2011 | New York City, New York | Prospective cohort | n = 112 (37 African American, 38 Hispanic, and 37 non-Hispanic White adults) 60-years-old and older with noncancer pain | Physical Activity | Impact of the Arthritis Foundation Self-Help Program |
| Peng et al. | 2018 | United States | Cross sectional | n = 32,060 adult respondents to 2015 National Health Interview Survey | Physical Activity | Association between obesity and low back pain |
| Plotnikoff et al | 2003 | Minnesota | Cross sectional | n = 150 African American, East African, Hispanic & American Indian patients w/musculoskeletal pain, aged 10 to 65 y old | Nutrition | Prevalence of hypovitaminosis D in outpatients with musculoskeletal pain |
| Rundell et al | 2017 | California, Detroit, Boston | Cohort Study | n = 5,239 older adults greater than equal to 65, presenting to primary care for back pain 2011–2013 | Smoking | Disability and pain intensity |
| Shmagel et al | 2018 | United States | Cohort Study | n = 2,548 patients with radiographic knee osteoarthritis recruited between 2006 and 2010 | Nutrition | Magnesium intake and the association with knee pain and function |
| Sibille et al | 2018 | Birmingham, Alabama, Gainesville, Florida | Cross-sectional | n = 167 individuals positive for knee osteoarthritis aged 45–85 y | Nutrition | Clinical and experimental pain, physical and psychosocial functioning, plasma omega 6- omega 3 ratio |
| Song et al | 2013 | Illinois | Cross-sectional | n = 1,142 individuals with radiographic knee osteoarthritis and n = 747 at risk of radiographic knee osteoarthritis | Physical Activity | Aerobic component (≥ 150 moderate-to-vigorous (MV) min/wk in bouts ≥ 10 minutes) of the States Department of Health and Human Services Physical Activity Guidelines |
| Turner et al | 2017 | United States | Cross-sectional | n = 516 Hispanic individuals completed survey; n = 102 Hispanic chronic non-cancer pain | Physical Activity | Exercising and using prescription medications for pain control |
| Wolfe and Michaud | 2007 | United States | Longitudinal observational | n = 12,090 patients with rheumatoid arthritis from the National Data Bank for Rheumatic Diseases | Smoking | Comparing visual analog pain scale and Medical Outcomes Study Short Form-36 Health Survey pain measures |
| Wyatt et al | 2014 | North Carolina | Interventional | n = 117 African American individuals with self-reported arthritis participating in self-directed (n = 68) or group (n = 49) 6-wk WWE program | Physical Activity | Effectiveness of Arthritis foundation’s Walk with Ease Program |
Coping factors are the first priority area under the Behavioral level of analysis and includes the following health factors: active coping, problem solving, stress management, cognitive reframing, and emotional regulation.77 Passive coping patterns are associated with greater psychological distress and pain severity.34,99 Research on coping factors specific to chronic musculoskeletal pain suggest that non-Hispanic Black individuals engage in passive coping strategies such as catastrophizing, emotion-focused coping, praying, and hoping to a greater degree than non-Hispanic White individuals.48,107 Additionally, perceived stress was reported as having a stronger negative impact on pain and function in older non-Hispanic Black individuals compared to non-Hispanic White peers.18 Difficulty with emotional regulation was positively associated with pain severity in African American individuals reporting greater pain and emotional-focused coping and decreased function; however, the relationship was not seen in Caucasian individuals.6,98 A pilot study found no association between total coping score and pain level but did find ethnic and/or race groups differed between total coping score (problem-focused and emotion-focused) and pain level with white participants having a positive correlation and nonwhite participants having a negative correlation.5 Interventions targeting cognitive reframing and stress management may provide strategies for mitigating negative effects associated with stress and health disparities in chronic musculoskeletal pain. Interestingly, however, a 6-week positive psychological skills program was minimally successful for improving pain and functioning in non-Hispanic Black and non-Hispanic White veterans.73 Similarly, a culturally tailored pain coping skills training program for 248 African American adults with hip or knee osteoarthritis did not show improvements in pain intensity although key measures of pain coping and perceived ability to manage pain improved compared to a wait list control group.7 Findings highlight the need to further understand the role of coping factors and how to effectively target clinically-relevant skills in the treatment of chronic musculoskeletal pain in diverse ethnic/race groups.
Psychosocial risk and resilience factors are the second priority area included in the Behavioral level of analysis with social support, discrimination, pessimism, optimism, and control as identified as the relevant health factors.77 A few studies have explored ethnic/race differences across social support factors specific to chronic musculoskeletal pain. Though non-Hispanic Black individuals report seeking more social support than non-Hispanic White peers,107 one study found that non-Hispanic Black adults with severe hip and/or knee osteoarthritis reported a lower quality of social support than non-Hispanic White adults.66 However, in a similar study among non-Hispanic Black and non-Hispanic White individuals with knee pain, no group differences in perceived social support were found.13 Lifetime experience of discrimination was the strongest predictor of back pain in non-Hispanic Black adults, particularly among women explaining 13% of the variance in pain reported.47 Similarly, in women with osteoarthritis, greater levels of everyday discrimination and financial stress explained significantly more variance in depressive symptoms in African American adults relative to White peers.108 In experimentally evoked pain, one study found non-Hispanic Black adults with knee osteoarthritis were more sensitive to heat pain and reported greater perceived racial discrimination than non-Hispanic White peers61; however, discrimination was not associated with pain-induced cortisol reactivity or cold pressor pain ratings among non-Hispanic Black adults.76 Resilience factors are known contributors to pain adaptation.13,62,76 Higher optimism was associated with less movement-evoked pain in non-Hispanic Black individuals with knee pain, but not among non-Hispanic White individuals.13 Another study of perceived control found Black participants reported lower levels of perceived control over their pain compared to non-Hispanic White participants.151 Research in the area of resilience is minimal, indicating a clear need for future investigations. Additionally, a pattern of findings suggest that relationships between psychosocial risk and resilience factors and chronic musculoskeletal pain may differ by ethnic/race groups and warrants further investigation.5,13,18,98,107
Health behaviors are the third priority area under the Behavioral level of analysis which includes the following health factors: smoking, anger and violence, alcohol and/or drugs, nutrition, and physical activity.77 Smoking (current or previous) and race were both significant predictors of persistent back pain among older adults.131 Smoking rates tend to be high among underrepresented ethnic/race groups including African American and Native American individuals with chronic musculoskeletal pain54,84) and is associated with increased pain reporting.46,163 Studies specific to ethnic/race group differences in anger and/or violence and chronic musculoskeletal pain were not found. The role of alcohol or recreational drug use as contributing to health disparities in persons with chronic musculoskeletal pain is also unclear. In a study of patients with chronic knee osteoarthritis pain, Native American and Hispanic individuals reported higher levels of pain compared with non-Hispanic White peers, however, those who reported regular alcohol consumption reported significantly lower pain.46 Unfortunately, rates of alcohol consumption among the different ethnic/race groups were not reported, making it difficult to interpret findings.46 In another study, researchers found that of those reporting cocaine use, African Americans had higher odds of back pain and arthritis compared to Caucasians reporting cocaine use.41 Nutrition is another relevant Behavioral factor. While the research specific to nutrition is limited, findings indicate nutritional deficiencies (eg, vitamin D) may be significant contributors to pain disparities in diverse ethnic/race groups.58,126,133,136
There is robust evidence that physical activity reduces chronic musculoskeletal pain.44,59 Studies have shown educational interventions targeting exercise and behavioral changes decreased pain and improved function across multiple ethnic and/or race groups.15,86,122,167 Further, lower body mass index was associated with lower odds of low back pain across ethnic and/or race groups.124 Despite the recognized benefits of physical activity for chronic musculoskeletal pain, disparities in the ability to meet recommended physical activity guidelines143 likely contribute toward pain outcomes among differing ethnic and/or race groups.60 Environmental and structural factors including accessibility, safety, and finances influence the ability to engage in physical activity.92,102,148,160 Data specific to anger and/or violence and alcohol/drug use are limited and warrant further investigation. Research in the areas of smoking, nutrition and physical activity provide an important foundation to extend research efforts in the identification of factors to target both from an interventional perspective and with integrative investigations across differing levels of analysis.
Biological Level
The Biological level of analysis includes the following priority areas:
1) physiological indicators; 2) genetic stability and 3) cellular function and communication.77 Biological processes play a critical role in the pathogenesis of diseases that lead to health disparities.8,77,87 Ethnic/race groups represent a multilevel social construct rather than a biological construct.169 The biological consequences of social inequalities are often reported as ethnic/race group differences. Including the Biological level of analyses in research studies can help inform understanding of the biological interface of environmental, sociocultural and behavioral determinants of health. A review of the literature on biological factors, health disparities, and chronic musculoskeletal pain unearthed a dearth of research investigation in this area, signaling a critical gap in the understanding of health disparities from a biological perspective (Table 5).
Physiological indicators are the first priority area under the Biological level of analysis and encompass heath factors listed as comorbidities, cardiovascular functioning, sympathetic nervous system, hypothalamic-pituitary-adrenal axis, and inflammation.77 A literature search for research on health factor terms representing physiological indicators, underrepresented ethnic/race groups, and chronic musculoskeletal pain resulted in no studies meeting the inclusion criteria. There are some studies that include physiological indicators outside the identified health factor search terms (eg, Herbert et al, 2017; Table 4) which provide an example of where more multilevel research is needed.
Genetic stability is the second priority area under the Biological level of analysis with health factors to include telomere attrition, epigenetic alteration, and loss of proteostasis, protein-related cellular functioning.77 No studies were found specific to identified health factors, chronic musculoskeletal pain, and ethnic/race group populations. Studies with specific consideration for genetic stability are needed to better understand the biological interface of chronic musculoskeletal pain disparities.
Cellular function and communication are the third priority area under the Biological level of analysis with health factors identified as deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, cellular stress response, stem cell exhaustion, and intercellular communication. Studies specific to cellular function and communication health factors in chronic musculoskeletal pain with consideration for underrepresented ethnic/race groups were not found. Extending research to include factors at different levels of analyses specific to cellular communication and mechanisms of pain may inform understanding of chronic musculoskeletal pain disparities.
Discussion
To better understand what is known and what is needed to advance the science of specific to disparities in the experience of chronic musculoskeletal pain, we applied the NIA’s Health Disparities Research Framework in the evaluation of studies specific to adults with chronic musculoskeletal pain in underrepresented ethnic/race groups. Search criteria resulted in the identification of a total of 52 publications across Environmental, Sociocultural, Behavioral, and Biological levels of analysis. There were limited publications specific to ethnic/race groups with chronic musculoskeletal pain across all levels of analyses with particular gaps in Sociocultural and Biological levels. A summary of what is known and what is needed for each level of analysis follows.
The Environmental level of analysis is organized under 3 priority areas: geographical and political factors, socioeconomic factors, and health care. No studies specific to chronic musculoskeletal pain and geographical and political factors area were found. However, research shows underrepresented ethnic/race group communities have fewer adequately stocked pharmacies,64,128 less access to non-pharmacological pain interventions,32 and that prescription opioid poisoning, that is, opioid abuse, may be more common in rural areas.30 State and local policies often exacerbate health disparities by contributing to inequities by citizen status, ethnicity/race, and other social hierarchies.37 Further, studies specific to evaluating residential segregation, toxin exposure, criminalization, immigration, structural bias, education, income, and occupation would be informative as most studies classify these subtopics broadly into socioeconomic status. Additionally, investigations are needed evaluating language fluency, health literacy, and numeracy as these factors may contribute to a limited understanding of chronic musculoskeletal pain conditions and reduce involvement in and compliance with treatment. While there is a growing recognition of the relevance of Environmental level health factors, there remains a considerable knowledge gap specific to disparities in chronic musculoskeletal pain.9,110
Studies encompassing the Sociocultural level of analysis are minimal. Although the biopsychosocial model of pain is touted as the premier model for understanding and treating pain, sociocultural aspects of chronic musculoskeletal pain have not been adequately investigated. The available evidence indicates that sociocultural factors play a highly influential role in ethnicity/race group chronic musculoskeletal pain disparities. Although not specific to chronic musculoskeletal pain, the relevance of sociocultural factors in influencing behaviors such as seeking medical care, taking medication, health care and pain attitudes, coping strategies, and health outcomes are significant.63,115,127,158,144,149,159,168,119,144 Research within the Sociocultural level of analysis specific to underrepresented ethnic/race groups and chronic musculoskeletal pain are needed.
A number of studies were identified at the Behavioral level of analysis representing the 3 priority areas of coping responses, psychosocial risk and resilience factors, and health behaviors. In regard to risk factors, studies have consistently found that non-Hispanic Black individuals report higher levels of discrimination than non-Hispanic White individuals.47,61,76,105,108 Importantly, in a study of pain-free adults, Losin et al reported that areas of the brain associated with discrimination differ from recognized pain activation areas and were associated with higher experimental pain report in African American participants.96 Research is now needed to understand how experiences of discrimination influence chronic musculoskeletal pain. Additionally, there is a strong body of evidence showing that protective psychosocial and behavioral factors are beneficial in mitigating the negative impact of stress on health and are associated with lower levels of chronic musculoskeletal pain.91,95 However, culturally-tailored interventions have been modestly beneficial. Further investigations are necessary to better understand how the relationships with protective factors may differ by ethnic/race group, identify clinically relevant targets, and how to engage vulnerable populations into implementing and sustaining interventions.12,54,84,112,123,157
Publications specific to the Biological level of analysis as it relates to chronic musculoskeletal pain and health disparities were not found. Chronic musculoskeletal pain is associated with an increased incidence of comorbidities.65,118,132 A few studies considered co-morbidities and ethnicity/race related to chronic musculoskeletal pain conditions.41,71,93,97,101,117,145,165 Importantly, relationships between chronic pain and the hypothalamic-pituitary-adrenal axis and inflammation are well established.38,129,138,139 There are also other physiological indicators warranting inclusion in future health disparities research including brain imaging and allostatic load.130,138,141,154 A recent publication indicated sociodemographic groups with consideration for chronic knee pain stage show differences in gray matter thickness in the temporal lobe area of the brain.152 While there is a growing body of evidence regarding the relationships between chronic musculoskeletal pain and physiological measures, investigations specific to better understanding factors contributing to chronic musculoskeletal pain disparities are needed.
Although ethnic/race group considerations are not included, a number of publications have addressed relationships between measures of psychological stress, chronic pain, resilience, and telomere length.70,85,135,137,140,147 Furthermore, epigenetic changes due to higher levels of childhood stress, racial discrimination, and low-economic status have been purported to contribute toward pain disparities in African American adults compared to non-Hispanic White adults.11 While research specific to genetic stability and chronic musculoskeletal pain are increasing, further investigation on determinants across multiple levels of analyses are needed to better appreciate determinates of chronic musculoskeletal pain disparities in disproportionally affected ethnic/race groups.
Lastly, there is a plethora of investigations on cellular function and communication. Investigations exploring the mechanisms of sensory processing of pain in peripheral neuropathies and peripheral injuries and the role of mitochondria and gap junctions in cellular communication at the basic science level are well explored,14,53,68,82,166 Extending these research efforts to include consideration for disparities in chronic musculoskeletal pain is an area of opportunity.
Limitations and Future Directions
There are a number of limitations to consider in the evaluation of findings. First, completing the review based on the terms from the NIA Health Disparities Research Framework provided the structure specific to levels of analysis, priority focus areas, and health factors. However, a broader array or alternative terms and/or concepts may result in the identification of studies not captured in the current review. The National Institute on Minority Health and Health Disparity Research Framework was published in 2019 which is comprised of components of the NIA Health Disparities Research Framework and the socioecological model which may further inform efforts moving forward.10 Second, the current review was limited to the timeframe, location (United States), and search databases described in the Methods. Additional studies aligning with key criteria may be outside the set parameters. Third, many studies on chronic musculoskeletal pain focused on low back pain and osteoarthritis, additional studies specific to other conditions are needed, for example, fibromyalgia and rheumatoid arthritis. Fourth, there are inconsistent terms to characterize ethnic/race groups, aligning with a consistent approach, such as required NIH repoprted phrasing, will improve comparisons across studies.
The research opportunities for future directions are broad and numerous. First, research incorporating measures across multiple levels of analyses should be prioritized. Second, studies frequently are not powered to compare or stratify by ethnic/race groups. Recruiting based on population representation is not sufficient to provide an evidence-based perspective of factors contributing to chronic musculoskeletal pain disparities.56 Thus, strategies to increase participation of underrepresented groups in studies are needed.56 Third, the benefit of a common language among all facets of research is apparent. Consistent identification of ethnic/race groups and utilizing key pain and functional outcome measures would allow for clearer interpretation of findings and the ability to replicate across studies.45,81,116 Fourth, research focusing on buffering and protective factors would also be beneficial in the identification of clinical targets.21,31,164 Further, considerations for similarities between ethnic and/or race groups is also important and will help identify areas that would promote alignment and collaboration. Fifth, input from stake holders such as practicing physicians, individuals with chronic pain, families, health equity advocates, and individuals with cultural diversity expertise to inform and enhance research efforts is needed. Sixth, the NIA Health Disparities Research Framework provides the infrastructure to extend collaborative efforts between funders and researchers allowing for progress tracking, needs identification, and continual process improvement. Seventh, current efforts are to promote improved research designs to better understand the complex array of factor contributing to health disparities. The long-term goals of these efforts would be to identify and develop clear modifiable targets across all levels of analysis (environmental, sociocultural, behavioral, and biological) to reduce health disparities and promote improved health outcomes for all people. Finally, with the strong and consistent evidence of sociodemographic and environmental factors accounting for disparities in health outcomes, relevant factors need to be addressed in advance of interpreting ethnic/race group differences.
Conclusion
Investigations of environmental, sociocultural, behavioral, and biological health factors contributing to underrepresented ethnic/race group disparities in the experience of chronic musculoskeletal pain are in the early stages of development. Current limitations in evidence specific to “chronic musculoskeletal pain” are supplemented by a foundation of findings in the over-arching areas of “pain” and “chronic pain” which provide guidance for future research efforts.27,78,83 Study designs including a focus on protective factors and combined levels of analysis would be particularly meritorious.
Acknowledgments
Many thanks are extended to the Institutes at the NIH who have funded research to better understand factors contributing to health disparities and for the development of specific goals and directives to support research focused on disproportionately affected populations. Amidst the challenges, the broad range of efforts underway are encouraging and indicate signs of progress. The authors would also like to express our appreciation to Carl V. Hill, Ph.D., M.P.H for his contributions to the review.
This work was supported by the National Institutes of Health NIA R01AG054370 (KTS, AMM, AJJ); and P30AG028740, R21AG059207, U01AG061389 (DF); Integrative and Multidisciplinary Pain and Aging Research Training Program 5T32AG049673 (SP); R33AG056540-04 (MP); NIAMS K23AR07646301 (SQB); NINDS K22NS102334 and NIA 1P30AG059297 (ELT); NHLB K01HL153210-01 and NIA 1P30AG059297 (KPR); and NIA R00AG052642 (EJB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest statement: Authors have no conflicts of interest to declare.
References
- 1.Abdallah CG, Geha P: Chronic pain and chronic stress: Two sides of the same coin? Chronic Stress 1:1–10, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agbemenu K: Acculturation and health behaviors of african immigrants living in the United States: An integrative review. ABNF J 27:67–73, 2016 [PubMed] [Google Scholar]
- 3.Ahn H, Weaver M, Lyon DE, Kim J, Choi E, Staud R, Fillingim RB: Differences in clinical pain and experimental pain sensitivity between Asian Americans and whites with knee osteoarthritis. Clin J Pain 33:174–180, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albert SM, Musa D, Kwoh CK, Hanlon JT, Silverman M: Self-care and professionally guided care in osteoarthritis: Racial differences in a population-based sample. J Aging Health 20:198–216, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allen KD, Golightly YM, Olsen MK: Pilot study of pain and coping among patients with osteoarthritis: A daily diary analysis. J Clin Rheumatol 12:118–123, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Allen KD, Oddone EZ, Coffman CJ, Keefe FJ, Lindquist JH, Bosworth HB: Racial differences in osteoarthritis pain and function: Potential explanatory factors. Osteoarthritis Cartilage 18:160–167, 2010 [DOI] [PubMed] [Google Scholar]
- 7.Allen KD, Somers TJ, Campbell LC, Arbeeva L, Coffman CJ, Cené CW, Oddone EZ, Keefe FJ: Pain coping skills training for African Americans with osteoarthritis: Results of a randomized controlled trial. Pain 160:1297–1307, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D: The National institute on minority health and health disparities research framework. Am J Public Health 109:S16–S20, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andreae MH, White RS, Chen KY, Nair S, Hall C, Shaparin N: The effect of initiatives to overcome language barriers and improve attendance: A cross-sectional analysis of adherence in an inner city chronic pain clinic. Pain Med 18:265–274, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arendt-Nielsen L, Fernández-de-Las-Peñas C, Graven-Nielsen T: Basic aspects of musculoskeletal pain: From acute to chronic pain. J Man Manip Ther 19:186–193, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aroke EN, Joseph PV, Roy A, Overstreet DS, Tollefsbol TO, Vance DE, Goodin BR: Could epigenetics help explain racial disparities in chronic pain? J Pain Res 12:701–710, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barry DT, Glenn CP, Hoff RA, Potenza MN: Pain interference, psychopathology, and general medical conditions among black and white adults in the US general population. J Addict Med 11:98–105, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bartley EJ, Hossain NI, Gravlee CC, Sibille KT, Terry EL, Vaughn IA, Cardoso JS, Booker SQ, Glover TL, Goodin BR, Sotolongo A, Thompson KA, Bulls HW, Staud R, Edberg JC, Bradley LA, Fillingim RB: Race/ethnicity moderates the association between psychosocial resilience and movement-evoked pain in knee osteoarthritis. ACR Open Rheumatol 1:16–25, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basbaum AI, Bautista DM, Scherrer G, Julius D: Cellular and molecular mechanisms of pain. Cell 139:267–284, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beissner K, Parker SJ, Henderson CR Jr., Pal A, Iannone L, Reid MC: A cognitive-behavioral plus exercise intervention for older adults with chronic back pain: Race/ethnicity effect? J Aging Phys Act 20:246–265, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blake VA, Allegrante JP, Robbins L, Mancuso CA, Peterson MG, Esdaile JM, Paget SA, Charlson ME: Racial differences in social network experience and perceptions of benefit of arthritis treatments among New York City Medicare beneficiaries with self-reported hip and knee pain. Arthritis Rheum 47:366–371, 2002 [DOI] [PubMed] [Google Scholar]
- 17.Bolen J, Schieb L, Hootman JM, Helmick CG, Theis K, Murphy LB, Langmaid G: Differences in the prevalence and severity of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis 7:A64, 2010 [PMC free article] [PubMed] [Google Scholar]
- 18.Booker S, Cardoso J, Cruz-Almeida Y, Sibille KT, Terry EL, Powell-Roach KL, Riley JL 3rd, Goodin BR, Bartley EJ, Addison AS, Staud R, Redden D, Bradley L, Fillingim RB: Movement-evoked pain, physical function, and perceived stress: An observational study of ethnic/racial differences in aging non-Hispanic Blacks and non-Hispanic Whites with knee osteoarthritis. Exp Gerontol 124:110622, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Booker SQ, Cousin L, Buck HG: Puttin’ on”: Expectations versus family responses, the lived experience of older African Americans with chronic pain. J Family Nurs 25:533–556, 2019 [DOI] [PubMed] [Google Scholar]
- 20.Borrell LN, Vaughan R: An AJPH supplement toward a unified research approach for minority health and health disparities. Am J Public Health 109:S6–S7, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown DL: African American Resiliency: Examining racial socialization and social support as protective factors. J Black Psychol 34:32–48, 2008 [Google Scholar]
- 22.Burgess DJ, Crowley-Matoka M, Phelan S, Dovidio JF, Kerns R, Roth C, Saha S, van Ryn M: Patient race and physicians’ decisions to prescribe opioids for chronic low back pain. Soc Sci Med 67:1852–1860, 2008 [DOI] [PubMed] [Google Scholar]
- 23.Burgess DJ, Gravely AA, Nelson DB, Bair MJ, Kerns RD, Higgins DM, Farmer MM, Partin MR: Association between pain outcomes and race and opioid treatment: Retrospective cohort study of Veterans. J Rehabil Res Dev 53:13–24, 2016 [DOI] [PubMed] [Google Scholar]
- 24.Burgess DJ, Nelson DB, Gravely AA, Bair MJ, Kerns RD, Higgins DM, van Ryn M, Farmer M, Partin MR: Racial differences in prescription of opioid analgesics for chronic non-cancer pain in a national sample of veterans. J Pain 15:447–455, 2014 [DOI] [PubMed] [Google Scholar]
- 25.Buscemi V, Chang W-J, Liston MB, McAuley JH, Schabrun S: The role of psychosocial stress in the development of chronic musculoskeletal pain disorders: Protocol for a systematic review and meta-analysis. Syst Rev 6:224, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Callahan LF, Shreffler J, Siaton BC, Helmick CG, Schoster B, Schwartz TA, Chen JC, Renner JB, Jordan JM: Limited educational attainment and radiographic and symptomatic knee osteoarthritis: A cross-sectional analysis using data from the Johnston County (North Carolina) Osteoarthritis Project. Arthritis Res Ther 12:R46, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell CM, Edwards RR: Ethnic differences in pain and pain management. Pain Manage 2:219–230, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carey TS, Freburger JK, Holmes GM, Jackman A, Knauer S, Wallace A, Darter J: Race, care seeking, and utilization for chronic back and neck pain: Population perspectives. J Pain 11:343–350, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CDC: Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis–United States, 2002. MMWR Morb Mortal Wkly Rep 54:119–123, 2005 [PubMed] [Google Scholar]
- 30.Cerda M, Gaidus A, Keyes KM, Ponicki W, Martins S, Galea S, Gruenewald P: Prescription opioid poisoning across urban and rural areas: Identifying vulnerable groups and geographic areas. Addiction 112:103–112, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen E, Miller GE: Socioeconomic status and health: Mediating and moderating factors. Ann Rev Clin Psychol 9:723–749, 2013 [DOI] [PubMed] [Google Scholar]
- 32.Cheng T, D’Amico S, Luo M, Lestoquoy AS, Yinusa-Nyahkoon L, Laird LD, Gardiner PM: Health disparities in access to nonpharmacologic therapies in an urban community. J Altern Complement Med 25:48–60, 2019 [DOI] [PubMed] [Google Scholar]
- 33.Cimmino MA, Ferrone C, Cutolo M: Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol 25:173–183, 2011 [DOI] [PubMed] [Google Scholar]
- 34.Covic T, Adamson B, Hough M: The impact of passive coping on rheumatoid arthritis pain. Rheumatology 39:1027–1030, 2000 [DOI] [PubMed] [Google Scholar]
- 35.Cruz-Almeida Y, King CD, Goodin BR, Sibille KT, Glover TL, Riley JL, Sotolongo A, Herbert MS, Schmidt J, Fessler BJ, Redden DT, Staud R, Bradley LA, Fillingim RB: Psychological profiles and pain characteristics of older adults with knee osteoarthritis. Arthritis Care Res (Hoboken) 65:1786–1794, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davidson RJ, McEwen BS: Social influences on neuroplasticity: Stress and interventions to promote well-being. Nat Neurosci 15:689–695, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.De Trinidad Young M-E, Wallace SP: Included, but Deportable: A new public health approach to policies that criminalize and integrate immigrants. Am J Public Health 109:1171–1176, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DeVon HA, Piano MR, Rosenfeld AG, Hoppensteadt DA: The association of pain with protein inflammatory biomarkers: A review of the literature. Nurs Res 63:51–62, 2014 [DOI] [PubMed] [Google Scholar]
- 39.Dieppe P: Chronic musculoskeletal pain. The BMJ 346, 2013. bmj.f3146 [DOI] [PubMed] [Google Scholar]
- 40.Djuric Z, Bird CE, Furumoto-Dawson A, Rauscher GH, Ruffin MTt, Stowe RP, Tucker KL, Masi CM: Biomarkers of psychological stress in health disparities research. Open Bio-mark J 1:7–19, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dodani S, Ruktanonchai CW, Kaeley GS, Vaddiparti K, Striley CW, Cottler LB: Clinical comorbidities among cocaine users screened in the community through healthstreet. Health Behav Policy Rev 3:54–61, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dominick KL, Bosworth HB, Dudley TK, Waters SJ, Campbell LC, Keefe FJ: Patterns of opioid analgesic prescription among patients with osteoarthritis. J Pain Palliat Care Pharmacother 18:31–46, 2004 [PubMed] [Google Scholar]
- 43.Dominick KL, Bosworth HB, Jeffreys AS, Grambow SC, Oddone EZ, Horner RD: Racial/ethnic variations in non-steroidal anti-inflammatory drug (NSAID) use among patients with osteoarthritis. Pharmacoepidemiol Drug Saf 13:683–694, 2004 [DOI] [PubMed] [Google Scholar]
- 44.Dugan SA, Everson-Rose SA, Karavolos K, Sternfeld B, Wesley D, Powell LH: The impact of physical activity level on SF-36 role-physical and bodily pain indices in midlife women. J Phys Act Health 6:33–42, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick CG, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson JP, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J: Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 113:9–19, 2005 [DOI] [PubMed] [Google Scholar]
- 46.Eberly L, Richter D, Comerci G, Ocksrider J, Mercer D, Mlady G, Wascher D, Schenck R: Psychosocial and demographic factors influencing pain scores of patients with knee osteoarthritis. PLoS One 13:e0195075, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Edwards RR: The association of perceived discrimination with low back pain. J Behav Med 31:379–389, 2008 [DOI] [PubMed] [Google Scholar]
- 48.Edwards RR, Moric M, Husfeldt B, Buvanendran A, Ivankovich O: Ethnic similarities and differences in the chronic pain experience: A comparison of african american, Hispanic, and white patients. Pain Med 6:88–98, 2005 [DOI] [PubMed] [Google Scholar]
- 49.Eley NT, Namey E, McKenna K, Johnson AC, Guest G: Beyond the individual: Social and cultural influences on the health-seeking behaviors of African American men. Am J Men’s Health 13:1–11, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Epel ES: The geroscience agenda: Toxic stress, hormetic stress, and the rate of aging. Ageing Res Rev:101167, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Evans EA, Herman PM, Washington DL, Lorenz KA, Yuan A, Upchurch DM, Marshall N, Hamilton AB, Taylor SL: Gender differences in use of complementary and integrative health by U.S. military veterans with chronic musculoskeletal pain. Womens Health Issues 28:379–386, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fink DS, Keyes KM, Cerdá M: Social determinants of population health: A systems sciences approach. Curr Epidemiol Rep 3:98–105, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Flatters SJ: The contribution of mitochondria to sensory processing and pain. Prog Mol Biol Transl Sci 131:119–146, 2015 [DOI] [PubMed] [Google Scholar]
- 54.Foley B, Cleveland RJ, Renner JB, Jordan JM, Nelson AE: Racial differences in associations between baseline patterns of radiographic osteoarthritis and multiple definitions of progression of hip osteoarthritis: The Johnston County Osteoarthritis Project. Arthritis Res Ther 17:366, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gansky SA, Plesh O: Widespread pain and fibromyalgia in a biracial cohort of young women. J Rheumatol 34:810–817, 2007 [PubMed] [Google Scholar]
- 56.George S, Duran N, Norris K: A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health 104:e16–e31, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Glantz NM, Duncan I, Ahmed T, Fan L, Reed BL, Kalirai S, Kerr D: Racial and ethnic disparities in the burden and cost of diabetes for US medicare beneficiaries. Health Equity 3:211–218, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Glover TL, Goodin BR, Horgas AL, Kindler LL, King CD, Sibille KT, Peloquin CA, Riley JL 3rd, Staud R, Bradley LA, Fillingim RB: Vitamin D, race, and experimental pain sensitivity in older adults with knee osteoarthritis. Arthritis Rheum 64:3926–3935, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goeppinger J, Armstrong B, Schwartz T, Ensley D, Brady TJ: Self-management education for persons with arthritis: Managing comorbidity and eliminating health disparities. Arthritis Rheum 57:1081–1088, 2007 [DOI] [PubMed] [Google Scholar]
- 60.Golightly YM, Dominick KL: Racial variations in self-reported osteoarthritis symptom severity among veterans. Aging Clin Exp Res 17:264–269, 2005 [DOI] [PubMed] [Google Scholar]
- 61.Goodin BR, Pham QT, Glover TL, Sotolongo A, King CD, Sibille KT, Herbert MS, Cruz-Almeida Y, Sanden SH, Staud R, Redden DT, Bradley LA, Fillingim RB: Perceived racial discrimination, but not mistrust of medical researchers, predicts the heat pain tolerance of African Americans with symptomatic knee osteoarthritis. Health Psychol 32:1117–1126, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goubert L, Trompetter H: Towards a science and practice of resilience in the face of pain. Eur J Pain 21:1301–1315, 2017 [DOI] [PubMed] [Google Scholar]
- 63.Green CR, Baker TA, Ndao-Brumblay SK: Patient attitudes regarding healthcare utilization and referral: A descriptive comparison in African- and Caucasian Americans with chronic pain. J Natl Med Assoc 96:31–42, 2004 [PMC free article] [PubMed] [Google Scholar]
- 64.Green CR, Ndao-Brumblay SK, West B, Washington T: Differences in prescription opioid analgesic availability: Comparing minority and white pharmacies across michigan. J Pain 6:689–699, 2005 [DOI] [PubMed] [Google Scholar]
- 65.Grimby-Ekman A, Gerdle B, Björk J, Larsson B: Comorbidities, intensity, frequency and duration of pain, daily functioning and health care seeking in local, regional, and widespread pain - A descriptive population-based survey (SwePain). BMC Musculoskelet Disord 16:165, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Groeneveld PW, Kwoh CK, Mor MK, Appelt CJ, Geng M, Gutierrez JC, Wessel DS, Ibrahim SA: Racial differences in expectations of joint replacement surgery outcomes. Arthritis Rheum 59:730–737, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grol-Prokopczyk H: Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain 158:313–322, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hanani M: Intercellular communication in sensory ganglia by purinergic receptors and gap junctions: Implications for chronic pain. Brain Res 1487:183–191, 2012 [DOI] [PubMed] [Google Scholar]
- 69.Hannan MT, Anderson JJ, Pincus T, Felson DT: Educational attainment and osteoarthritis: Differential associations with radiographic changes and symptom reporting. J Clin Epidemiol 45:139–147, 1992 [DOI] [PubMed] [Google Scholar]
- 70.Hassett AL, Epel E, Clauw DJ, Harris RE, Harte SE, Kairys A, Buyske S, Williams DA: Pain is associated with short leukocyte telomere length in women with fibromyalgia. J Pain 13:959–969, 2012 [DOI] [PubMed] [Google Scholar]
- 71.Hausmann LR, Brandt CA, Carroll CM, Fenton BT, Ibrahim SA, Becker WC, Burgess DJ, Wandner LD, Bair MJ, Goulet JL: Racial and ethnic differences in total knee arthroplasty in the Veterans Affairs health care system, 2001–2013. Arthritis Care Res 69:1171–1178, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hausmann LR, Gao S, Lee ES, Kwoh CK: Racial disparities in the monitoring of patients on chronic opioid therapy. Pain 154:46–52, 2013 [DOI] [PubMed] [Google Scholar]
- 73.Hausmann LRM, Youk A, Kwoh CK, Gallagher RM, Weiner DK, Vina ER, Obrosky DS, Mauro GT, McInnes S, Ibrahim SA: Effect of a positive psychological intervention on pain and functional difficulty among adults with osteoarthritis: A randomized clinical trial. JAMA Network Open 1, 2018. e182533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Heins JK, Heins A, Grammas M, Costello M, Huang K, Mishra S: Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs 32:219–224, 2006 [DOI] [PubMed] [Google Scholar]
- 75.Henschke N, Lorenz E, Pokora R, Michaleff ZA, Quartey JNA, Oliveira VC: Understanding cultural influences on back pain and back pain research. Best Pract Res Clin Rheumatol 30:1037–1049, 2016 [DOI] [PubMed] [Google Scholar]
- 76.Herbert MS, Goodin BR, Bulls HW, Sotolongo A, Petrov ME, Edberg JC, Bradley LA, Fillingim RB: Ethnicity, cortisol, and experimental pain responses among persons with symptomatic knee osteoarthritis. Clin J Pain 33:820–826, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hill CV, Pérez-Stable EJ, Anderson NA, Bernard MA: The national institute on aging health disparities research framework. Ethn Dis 25:245–254, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT: The pain experience of hispanic Americans: A critical literature review and conceptual model. J Pain 17:513–528, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK: Differences in expectations of outcome mediate African American/white patient differences in “willingness” to consider joint replacement. Arthritis Rheum 46:2429–2435, 2002 [DOI] [PubMed] [Google Scholar]
- 80.Ibrahim SA, Zhang A, Mercer MB, Baughman M, Kwoh CK: Inner city African-American elderly patients’ perceptions and preferences for the care of chronic knee and hip pain: Findings from focus groups. J Gerontol 59:1318–1322, 2004 [DOI] [PubMed] [Google Scholar]
- 81.Improvement IoMUSoSCoREDfHQ: Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. Washington, DC, National Academies Press, 2009 [PubMed] [Google Scholar]
- 82.Jiang B-C, Cao D-L, Zhang X, Zhang Z-J, He L-N, Li C-H, Zhang W-W, Wu X-B, Berta T, Ji R-R, Gao Y-J: CXCL13 drives spinal astrocyte activation and neuropathic pain via CXCR5. J Clin Invest 126:745–761, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jimenez N, Garroutte E, Kundu A, Morales L, Buchwald D: A review of the experience, epidemiology, and management of pain among American Indian, Alaska Native, and Aboriginal Canadian peoples. J Pain 12:511–522, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Johnson-Jennings MD, Belcourt A, Town M, Walls ML, Walters KL: Racial discrimination’s influence on smoking rates among American Indian Alaska Native two-spirit individuals: Does pain play a role? J Health Care Poor Underserved 25:1667–1678, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Johnson AJ, Terry E, Bartley EJ, Garvan C, Cruz-Almeida Y, Goodin B, Glover TL, Staud R, Bradley LA, Fillingim RB, Sibille KT: Resilience factors may buffer cellular aging in individuals with and without chronic knee pain. Mol Pain 15:1–11, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jones LC, Watkins Y, Alva D: Operation change: A new paradigm addressing behavior change and musculoskeletal health disparities. J Racial Ethn Health Disparities 5:1264–1272, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jones NL, Breen N, Das R, Farhat T, Palmer R: Cross-Cutting Themes to Advance the Science of Minority Health and Health Disparities. Am J Public Health, 109:S21–S24, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, Geronimus AT: Life course approaches to the causes of health disparities. Am J Public Health 109:S48–S55, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Katz JN, Lyons N, Wolff LS, Silverman J, Emrani P, Holt HL, Corbett KL, Escalante A, Losina E: Medical decision-making among Hispanics and non-Hispanic Whites with chronic back and knee pain: A qualitative study. BMC Musculoskelet Disord 12:78, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kawi J, Reyes AT, Arenas RA: Exploring pain management among asian immigrants with chronic pain: Self-management and resilience. J Immigr Minor Health 21:1123–1136, 2019 [DOI] [PubMed] [Google Scholar]
- 91.Keefe FJ, Lumley M, Anderson T, Lynch T, Studts JL, Carson KL: Pain and emotion: New research directions. J Clin Psychol 57:587–607, 2001 [DOI] [PubMed] [Google Scholar]
- 92.Kosma M, Cardinal BJ: Theory-based physical activity beliefs by race and activity levels among older adults. Ethn Health 21:181–195, 2016 [DOI] [PubMed] [Google Scholar]
- 93.Lad SP, Bagley JH, Kenney KT, Ugiliweneza B, Kong M, Bagley CA, Gottfried ON, Isaacs RE, Patil CG, Boakye M: Racial disparities in outcomes of spinal surgery for lumbar stenosis. Spine 38:927–935, 2013 [DOI] [PubMed] [Google Scholar]
- 94.Levine S: The influence of social factors on the response to stress. Psychother Psychosom 60:33–38, 1993 [DOI] [PubMed] [Google Scholar]
- 95.Lopez-Martinez AE, Esteve-Zarazaga R, Ramirez-Maestre C: Perceived social support and coping responses are independent variables explaining pain adjustment among chronic pain patients. J Pain 9:373–379, 2008 [DOI] [PubMed] [Google Scholar]
- 96.Losin EAR, Woo C-W, Medina NA, Andrews-Hanna JR, Eisenbarth H, Wager TD: Neural and sociocultural mediators of ethnic differences in pain. Nat Human Behav 4:517–530, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Louie GH, Ward MM: Socioeconomic and ethnic differences in disease burden and disparities in physical function in older adults. Am J Public Health 101:1322–1329, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lumley MA, Radcliffe AM, Macklem DJ, Mosley-Williams A, Leisen JCC, Huffman JL, D’Souza PJ, Gillis ME, Meyer TM, Kraft CA, Rapport LJ: Alexithymia and pain in three chronic pain samples: Comparing caucasians and African Americans. Pain Med 6:251–261, 2005 [DOI] [PubMed] [Google Scholar]
- 99.Lynn Snow-Turek A, Norris MP, Tan G: Active and passive coping strategies in chronic pain patients. Pain 64:455–462, 1996 [DOI] [PubMed] [Google Scholar]
- 100.Macfarlane GJ, Barnish MS, Jones GT: Persons with chronic widespread pain experience excess mortality: Longitudinal results from UK Biobank and meta-analysis. Ann Rheum Dis 76:1815–1822, 2017 [DOI] [PubMed] [Google Scholar]
- 101.MacFarlane LA, Kim E, Cook NR, Lee I-M, Iversen MD, Katz JN, Costenbader KH: Racial variation in total knee replacement in a diverse nationwide clinical trial. J Clin Rheumatol 24:1–5, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maly A, Vallerand AH: Neighborhood, socioeconomic, and racial influence on chronic pain. Pain Manag Nurs 19:14–22, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.McBeth J, Jones K: Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol 21:403–425, 2007 [DOI] [PubMed] [Google Scholar]
- 104.McBeth J, Silman AJ, Gupta A, Chiu YH, Ray D, Morriss R, Dickens C, King Y, Macfarlane GJ: Moderation of psychosocial risk factors through dysfunction of the hypothalamic-pituitary-adrenal stress axis in the onset of chronic widespread musculoskeletal pain: Findings of a population-based prospective cohort study. Arthritis Rheum 56:360–371, 2007 [DOI] [PubMed] [Google Scholar]
- 105.McClendon J, Essien UR, Youk A, Ibrahim SA, Vina E, Kwoh CK, Hausmann LRM: Cumulative disadvantage and disparities in depression and pain among veterans with osteoarthritis: The role of perceived discrimination. Arthritis Care Res 73:11–17, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.McGrath RP, Snih SA, Markides KS, Faul JD, Vincent BM, Hall OT, Peterson MD: The burden of health conditions across race and ethnicity for aging Americans: Disability-adjusted life years. Medicine 98:e17964, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McIlvane JM: Disentangling the effects of race and SES on arthritis-related symptoms, coping, and well-being in African American and White women. Aging Ment Health 11:556–569, 2007 [DOI] [PubMed] [Google Scholar]
- 108.McIlvane JM, Baker TA, Mingo CA: Racial differences in arthritis-related stress, chronic life stress, and depressive symptoms among women with arthritis: A contextual perspective. J Gerontol B Psychol Sci Soc Sci 63:S320–S327, 2008 [DOI] [PubMed] [Google Scholar]
- 109.Meints SM, Miller MM, Hirsh AT: Differences in pain coping between black and white Americans: A meta-analysis. J Pain 17:642–653, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mickle AM, Garvan C, Service C, Pop R, Marks J, Wu S, Edberg JC, Staud R, Fillingim RB, Bartley EJ, Sibille KT: Relationships between pain, life stress, sociodemographics, and cortisol: Contributions of pain intensity and financial satisfaction. Chronic Stress 4, 2020. 2470547020975758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mingo CA, McIlvane JM, Haley WE, Luong M-LN: Impact of race and diagnostic label on older adults’ emotions, illness beliefs, and willingness to help a family member with osteoarthritis. J Appl Gerontol 34:277–292, 2013 [DOI] [PubMed] [Google Scholar]
- 112.Mitchell MM, Maragh-Bass AC, Nguyen TQ, Isenberg S, Knowlton AR: The role of chronic pain and current substance use in predicting negative social support among disadvantaged persons living with HIV/AIDS. AIDS Care 28:1280–1286, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Myers HF: Ethnicity- and socio-economic status-related stresses in context: An integrative review and conceptual model. J Behav Med 32:9–19, 2009 [DOI] [PubMed] [Google Scholar]
- 114.Nampiaparampil DE, Nampiaparampil JX, Harden RN: Pain and prejudice. Pain Med 10:716–721, 2009 [DOI] [PubMed] [Google Scholar]
- 115.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK: Access to care for chronic pain: Racial and ethnic differences. J Pain 6:301–314, 2005 [DOI] [PubMed] [Google Scholar]
- 116.National Institutes of Health: NIH Policy on Reporting Race and Ethnicity Data: Subjects in Clinical Research. Bethesda, MD, Office of Management and Budget, 2001 [Google Scholar]
- 117.Nosek MA, Hughes RB, Petersen NJ, Taylor HB, Robinson-Whelen S, Byrne M, Morgan R: Secondary conditions in a community-based sample of women with physical disabilities over a 1-year period. Arch Phys Med Rehabil 87:320–327, 2006 [DOI] [PubMed] [Google Scholar]
- 118.Oliveira CB, Maher CG, Franco MR, Kamper SJ, Williams CM, Silva FG, Pinto RZ: Co-occurrence of chronic musculoskeletal pain and cardiovascular diseases: A systematic review with meta-analysis. Pain Med 21:1106–1121, 2020 [DOI] [PubMed] [Google Scholar]
- 119.Orhan C, Van Looveren E, Cagnie B, Mukhtar NB, Lenoir D, Meeus M: Are pain beliefs, cognitions, and behaviors influenced by race, ethnicity, and culture in patients with chronic musculoskeletal pain: A systematic review. Pain Physician 21:541–558, 2018 [PubMed] [Google Scholar]
- 120.Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S: Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry (Edgmont) 4:35–40, 2007 [PMC free article] [PubMed] [Google Scholar]
- 121.Park SJ, Yoon DM, Yoon KB, Moon JA, Kim SH: Factors associated with higher reported pain levels in patients with chronic musculoskeletal pain: A cross-sectional, correlational analysis. PLoS One 11:e0163132, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Parker SJ, Vasquez R, Chen EK, Henderson CR Jr., Pillemer K, Robbins L, Reid MC: A comparison of the arthritis foundation self-help program across three race/ethnicity groups. Ethn Dis 21:444–450, 2011 [PMC free article] [PubMed] [Google Scholar]
- 123.Paulus DJ, Ditre JW, Viana AG, Bakhshaie J, Garza M, Valdivieso J, Ochoa-Perez M, Lemaire C, Zvolensky MJ: Pain and alcohol use among latinos in primary care: Examining rumination as an explanatory factor. Subst Use Misuse 53:686–693, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Peng T, Perez A, Pettee Gabriel K: The association among overweight, obesity, and low back pain in U.S. adults: A cross-sectional study of the 2015 national health interview survey. J Manipulative Physiol Ther 41:294–303, 2018 [DOI] [PubMed] [Google Scholar]
- 125.Peterson K, Anderson J, Boundy E, Ferguson L, McCleery E, Waldrip K: Mortality disparities in racial/ethnic minority groups in the veterans health administration: An evidence review and map. Am J Public Health 108:e1–e11, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Plotnikoff GA, Quigley JM: Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clinic Proceedings 78:1463–1470, 2003 [DOI] [PubMed] [Google Scholar]
- 127.Portenoy RK, Ugarte C, Fuller I, Haas G: Population-based survey of pain in the United States: Differences among white, African American, and Hispanic subjects. J Pain 5:317–328, 2004 [DOI] [PubMed] [Google Scholar]
- 128.Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, Lambert B: ‘Pharmacy deserts’ are prevalent in Chicago’s predominantly minority communities, raising medication access concerns. Health Affairs 33:1958–1965, 2014 [DOI] [PubMed] [Google Scholar]
- 129.Quartana PJ, Finan PH, Page GG, Smith MT: Effects of insomnia disorder and knee osteoarthritis on resting and pain-evoked inflammatory markers. Brain Behav Immun 47:228–237, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rodriquez EJ, Kim EN, Sumner AE, Nápoles AM, Pérez-Stable EJ: Allostatic load: Importance, markers, and score determination in minority and disparity populations. J Urban Health 96:3–11, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rundell SD, Sherman KJ, Heagerty PJ, Mock CN, Dettori NJ, Comstock BA, Avins AL, Nedeljkovic SS, Nerenz DR, Jarvik JG: Predictors of persistent disability and back pain in older adults with a new episode of care for back pain. Pain Med 18:1049–1062, 2017 [DOI] [PubMed] [Google Scholar]
- 132.Ryan CG, McDonough S, Kirwan JP, Leveille S, Martin DJ: An investigation of association between chronic musculoskeletal pain and cardiovascular disease in the Health Survey for England (2008). Eur J Pain 18:740–750, 2014 [DOI] [PubMed] [Google Scholar]
- 133.Shmagel A, Onizuka N, Langsetmo L, Vo T, Foley R, Ensrud K, Valen P: Low magnesium intake is associated with increased knee pain in subjects with radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 26:651–658, 2018 [DOI] [PubMed] [Google Scholar]
- 134.Short SE, Mollborn S: Social determinants and health behaviors: Conceptual frames and empirical advances. Curr Opin Psychol 5:78–84, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sibille KT, Chen H, Bartley EJ, Riley J 3rd, Glover TL, King CD, Zhang H, Cruz-Almeida Y, Goodin BR, Sotolongo A, Petrov ME, Herbert M, Bulls HW, Edberg JC, Staud R, Redden D, Bradley LA, Fillingim RB: Accelerated aging in adults with knee osteoarthritis pain: Consideration for frequency, intensity, time, and total pain sites. Pain Rep 2: e591, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sibille KT, King C, Garrett TJ, Glover TL, Zhang H, Chen H, Reddy D, Goodin BR, Sotolongo A, Petrov ME, Cruz-Almeida Y, Herbert M, Bartley EJ, Edberg JC, Staud R, Redden DT, Bradley LA, Fillingim RB: Omega-6: Omega-3 PUFA ratio, pain, functioning, and distress in adults with knee pain. Clin J Pain 34:182–189, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sibille KT, Langaee T, Burkley B, Gong Y, Glover TL, King C, Riley JL 3rd, Leeuwenburgh C, Staud R, Bradley LA, Fillingim RB: Chronic pain, perceived stress, and cellular aging: An exploratory study. Molecular Pain 8:12, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Sibille KT, McBeth J, Smith D, Wilkie R: Allostatic load and pain severity in older adults: Results from the English Longitudinal Study of Ageing. Exp Gerontol 88:51–58, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sibille KT, Steingrímsdóttir ÓA, Fillingim RB, Stubhaug A, Schirmer H, Chen H, McEwen BS, Nielsen CS: Investigating the burden of chronic pain: An inflammatory and metabolic composite. Pain Res Manag 2016:7657329, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sibille KT, Witek-Janusek L, Mathews HL, Fillingim RB: Telomeres and epigenetics: Potential relevance to chronic pain. Pain 153:1789–1793, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Slade GD, Sanders AE, By K: Role of allostatic load in sociodemographic patterns of pain prevalence in the U.S. population. J Pain 13:666–675, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Smith TO, Dainty JR, Williamson E, Martin KR: Association between musculoskeletal pain with social isolation and loneliness: Analysis of the English Longitudinal Study of Ageing. Br J Pain 13:82–90, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Song J, Hochberg MC, Chang RW, Hootman JM, Manheim LM, Lee J, Semanik PA, Sharma L, Dunlop DD, Osteoarthritis Initiative I: Racial and ethnic differences in physical activity guidelines attainment among people at high risk of or having knee osteoarthritis. Arthritis Care Res 65:195–202, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Stangl AL, Earnshaw VA, Logie CH, van Brakel W, CS L, Barré I, Dovidio JF: The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC medicine 17:31, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Steel N, Clark A, Lang IA, Wallace RB, Melzer D: Racial disparities in receipt of hip and knee joint replacements are not explained by need: The Health and Retirement Study 1998–2004. J Gerontol Series A Biol Sci Med Sci 63:629–634, 2008 [DOI] [PubMed] [Google Scholar]
- 146.Steptoe A, Zaninotto P: Lower socioeconomic status and the acceleration of aging: An outcome-wide analysis. Proceed Nat Acad Sci 117:14911, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Steward AM, Morgan JD, Espinosa JP, Turk DC, Patel KV: Chronic pain and telomere length in community-dwelling adults: Findings from the 1999 to 2002 National Health and Nutrition Examination Survey. J Pain 18:1517–1525, 2017 [DOI] [PubMed] [Google Scholar]
- 148.Stubbs B, Hurley M, Smith T: What are the factors that influence physical activity participation in adults with knee and hip osteoarthritis? A systematic review of physical activity correlates. Clin Rehabil 29:80–94, 2015 [DOI] [PubMed] [Google Scholar]
- 149.Sullivan MJ, Scott W, Trost Z: Perceived injustice: A risk factor for problematic pain outcomes. Clin J Pain 28:484–488, 2012 [DOI] [PubMed] [Google Scholar]
- 150.Tait RC, Chibnall JT, Andresen EM, Hadler NM: Disability determination: Validity with occupational low back pain. J Pain 7:951–957, 2006 [DOI] [PubMed] [Google Scholar]
- 151.Tan G, Jensen MP, Thornby J, Anderson KO: Ethnicity, control appraisal, coping, and adjustment to chronic pain among black and white Americans. Pain Med 6:18–28, 2005 [DOI] [PubMed] [Google Scholar]
- 152.Tanner JJ, Johnson AJ, Terry EL, Cardoso J, Garvan C, Staud R, Deutsch G, Deshpande H, Lai S, Addison A, Redden D, Goodin BR, Price CC, Fillingim RB, Sibille KT: Resilience, pain, and the brain: Relationships differ by sociodemographics. J Neurosci Res, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Taylor BA, Casas-Ganem J, Vaccaro AR, Hilibrand AS, Hanscom BS, Albert TJ: Differences in the work-up and treatment of conditions associated with low back pain by patient gender and ethnic background. Spine (Phila Pa 1976) 30:359–364, 2005 [DOI] [PubMed] [Google Scholar]
- 154.Terry EL, Tanner JJ, Cardoso JS, Sibille KT, Lai S, Deshpande H, Deutsch G, Goodin BR, Bradley LA, Price CC, Fillingim RB: Associations of pain catastrophizing with pain-related brain structure in individuals with or at risk for knee osteoarthritis: Sociodemographic considerations. Brain Imaging Behav, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Thielke SM, Whitson H, Diehr P, O’Hare A, Kearney PM, Chaudhry SI, Zakai NA, Kim D, Sekaran N, Sale JEM, Arnold AM, Chaves P, Newman A: Persistence and remission of musculoskeletal pain in community-dwelling older adults: Results from the cardiovascular health study. J Am Geriatrics Soc 60:1393–1400, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Thompson KA, Terry EL, Sibille KT, Gossett EW, Ross EN, Bartley EJ, Glover TL, Vaughn IA, Cardoso JS, Sotolongo A, Staud R, Hughes LB, Edberg JC, Redden DT, Bradley LA, Fillingim RB, Goodin BR: At the intersection of ethnicity/race and poverty: Knee pain and physical function. J Racial Ethn Health Disparities 6:1131–1143, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Tong ST, Hochheimer CJ, Brooks EM, Sabo RT, Jiang V, Day T, Rozman JS, Kashiri PL, Krist AH: Chronic opioid prescribing in primary care: Factors and perspectives. Ann Fam Med 17:200–206, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Torres CA, Thorn BE, Kapoor S, DeMonte C: An examination of cultural values and pain management in Foreign-Born Spanish-Speaking hispanics seeking care at a Federally Qualified Health Center. Pain Medicine 18:2058–2069, 2017 [DOI] [PubMed] [Google Scholar]
- 159.Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, Reynolds M, Foreman ML, Warren AM: Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabil Psychol 60:213–221, 2015 [DOI] [PubMed] [Google Scholar]
- 160.Turner BJ, Rodriguez N, Valerio MA, Liang Y, Winkler P, Jackson L: Less exercise and more drugs: How a low-income population manages chronic pain. Arch Phys Med Rehabil 98:2111–2117, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vaughn IA, Terry EL, Bartley EJ, Schaefer N, Fillingim RB: Racial-ethnic differences in osteoarthritis pain and disability: A meta-analysis. J Pain 20:629–644, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Vina ER, Ran D, Ashbeck EL, Kwoh CK: Natural history of pain and disability among African–Americans and Whites with or at risk for knee osteoarthritis: A longitudinal study. Osteoarthritis Cartilage 26:471–479, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wolfe F, Michaud K: Assessment of pain in rheumatoid arthritis: Minimal clinically significant difference, predictors, and the effect of anti-tumor necrosis factor therapy. J Rheumatol 34:1674–1683, 2007 [PubMed] [Google Scholar]
- 164.Woodward EN, Walsh JL, Senn TE, Carey MP: Positive social interaction offsets impact of low socioeconomic status on stress. J Natl Med Assoc 110:371–377, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wright AR, Shi XA, Busby-Whitehead J, Jordan JM, Nelson AE: The prevalence of neck and shoulder symptoms and associations with comorbidities and disability: The johnston county osteoarthritis project. Myopain 23:34–44, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wu A, Green CR, Rupenthal ID, Moalem-Taylor G: Role of gap junctions in chronic pain. J Neurosci Res 90:337–345, 2012 [DOI] [PubMed] [Google Scholar]
- 167.Wyatt B, Mingo CA, Waterman MB, White P, Cleveland RJ, Callahan LF: Impact of the Arthritis Foundation’s Walk With Ease Program on arthritis symptoms in African Americans. Prev Chronic Dis 11:E199, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Yakobov E, Scott W, Stanish WD, Tanzer M, Dunbar M, Richardson G, Sullivan MJL: Reductions in perceived injustice are associated with reductions in disability and depressive symptoms after total knee arthroplasty. Clin J Pain 34:415–420, 2018 [DOI] [PubMed] [Google Scholar]
- 169.Yudell M, Roberts D, DeSalle R, Tishkoff S: Taking race out of human genetics. Science (New York, N.Y.) 351:564, 2016 [DOI] [PubMed] [Google Scholar]


