This cohort study assesses the mortality, quality of life, and treatment satisfaction associated with surgical vs nonsurgical interventions for femoral neck or pertrochanteric fractures in older patients.
Key Points
Question
Is nonoperative management of proximal femoral fractures a viable treatment option for selected frail patients with limited life expectancy compared with operative management?
Findings
In this cohort study of 172 frail patients with proximal femoral fractures, 88 opted for nonoperative management and 84 opted for operative management after a shared decision-making process. In patients who chose nonoperative management, the health-related quality of life was not inferior to that in patients who received surgical treatment and treatment was highly satisfactory.
Meaning
Findings from this study suggest that, following shared decision-making, nonoperative management is a viable option for frail institutionalized patients with a proximal femoral fracture at the end of life and that surgery should not be a foregone conclusion for these patients.
Abstract
Importance
Decision-making on management of proximal femoral fractures in frail patients with limited life expectancy is challenging, but surgical overtreatment needs to be prevented. Current literature provides limited insight into the true outcomes of nonoperative management and operative management in this patient population.
Objective
To investigate the outcomes of nonoperative management vs operative management of proximal femoral fractures in institutionalized frail older patients with limited life expectancy.
Design, Setting, and Participants
This multicenter cohort study was conducted between September 1, 2018, and April 25, 2020, with a 6-month follow-up period at 25 hospitals across the Netherlands. Eligible patients were aged 70 years or older, frail, and institutionalized and sustained a femoral neck or pertrochanteric fracture. The term frail implied at least 1 of the following characteristics was present: malnutrition (body mass index [calculated as weight in kilograms divided by height in meters squared] <18.5) or cachexia, severe comorbidities (American Society of Anesthesiologists physical status class of IV or V), or severe mobility issues (Functional Ambulation Category ≤2).
Exposures
Shared decision-making (SDM) followed by nonoperative or operative fracture management.
Main Outcomes and Measures
The primary outcome was the EuroQol 5 Dimension 5 Level (EQ-5D) utility score by proxies and caregivers. Secondary outcome measures were QUALIDEM (a dementia-specific quality-of-life instrument for persons with dementia in residential settings) scores, pain level (assessed by the Pain Assessment Checklist for Seniors With Limited Ability to Communicate), adverse events (Clavien-Dindo classification), mortality, treatment satisfaction (numeric rating scale), and quality of dying (Quality of Dying and Death Questionnaire).
Results
Of the 172 enrolled patients with proximal femoral fractures (median [25th and 75th percentile] age, 88 [85-92] years; 135 women [78%]), 88 opted for nonoperative management and 84 opted for operative management. The EQ-5D utility scores by proxies and caregivers in the nonoperative management group remained within the set 0.15 noninferiority limit of the operative management group (week 1: 0.17 [95% CI, 0.13-0.29] vs 0.26 [95% CI, 0.11-0.23]; week 2: 0.19 [95% CI, 0.10-0.27] vs 0.28 [95% CI, 0.22-0.35]; and week 4: 0.24 [95% CI, 0.15-0.33] vs 0.34 [95% CI, 0.28-0.41]). Adverse events were less frequent in the nonoperative management group vs the operative management group (67 vs 167). The 30-day mortality rate was 83% (n = 73) in the nonoperative management group and 25% (n = 21) in the operative management group, with 26 proxies and caregivers (51%) in the nonoperative management group rating the quality of dying as good-almost perfect. Treatment satisfaction was high in both groups, with a median numeric rating scale score of 8.
Conclusions and Relevance
Results of this study indicated that nonoperative management of proximal femoral fractures (selected through an SDM process) was a viable option for frail institutionalized patients with limited life expectancy, suggesting that surgery should not be a foregone conclusion for this patient population.
Introduction
A proximal femoral fracture is a devastating injury for older individuals. The injury diminishes quality of life (QOL), including health-related quality of life (HRQoL), and is associated with morbidity and mortality.1,2,3 Despite considerable efforts, the mortality rates, which are as high as 55% within 6 months of the injury for institutionalized patients with advanced dementia, have not improved in the past few decades. Proximal femoral fractures therefore are often a prelude to the end of life.4,5,6,7
For life-threatening illnesses, the World Health Organization supports a holistic approach to treating individuals with a limited life expectancy.8 This approach means that, in the case of a proximal femoral fracture, both operative and nonoperative management should be considered. To ensure that the best management strategy is chosen for each individual, the goals of care must be established through a shared decision-making (SDM) process. Improving communication by presenting treatment options with realistic outcomes, eliciting patients’ values, and incorporating these values into a collaborative deliberation may reduce unnecessary surgery with the risk of iatrogenic complications.9,10,11
Although surgery could be performed in the context of palliative care, the nonoperative management option for a subgroup of frail patients with limited life expectancy might also be satisfactory. However, there is limited insight into the true implications of nonoperative management for frail older adults with a proximal femoral fracture.12,13 Consequently, treatment guidelines provide no clear advice on the nonoperative treatment of frail patients with limited life expectancy.14,15 Instead, these guidelines focus mainly on regaining function, but other considerations may be more important to patients at the end of life. In current practice, more than 95% of all proximal femoral fractures are managed surgically.16
The central question remains: is nonoperative management of a proximal femoral fracture a satisfactory alternative for frail patients? In this cohort study, we aimed to investigate the outcomes of nonoperative management vs operative management of proximal femoral fractures in institutionalized frail older patients with limited life expectancy.
Methods
This prospective, multicenter cohort study with a noninferiority hypothesis was conducted at 25 hospitals across the Netherlands. The Medical Research Ethics Committee of VU University Medical Center Amsterdam approved the study. Participants provided written informed consent. The study protocol has been published elsewhere.17 All of the procedures performed were in accordance with the Declaration of Helsinki.18 We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
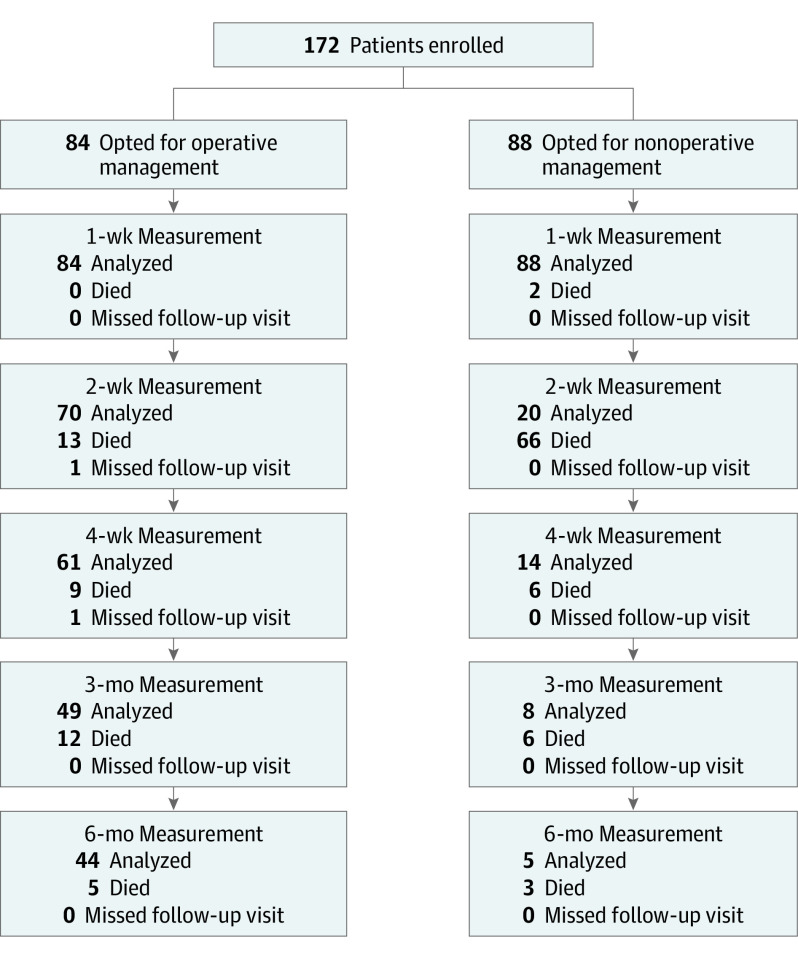
Between September 1, 2018, and April 25, 2020, we enrolled institutionalized frail patients aged 70 years or older with limited life expectancy who had sustained a proximal femoral fracture and were hospitalized in 1 of the 25 participating hospitals. These patients were followed up for 6 months, with planned outcome measurements at 1, 2, and 4 weeks and after 3 and 6 months (Figure 1). The term frail implied that at least 1 of the following characteristics was present: malnutrition, with a body mass index (calculated as weight in kilograms divided by height in meters squared) that was lower than 18.5 or cachexia; severe comorbidities, with an American Society of Anesthesiologists physical status class of IV or V; or severe mobility issues, with a Functional Ambulation Category (FAC) of 2 or lower (with FAC 2 indicating the need for at least [intermittent] manual assistance from 1 person during ambulation, and FAC 0 indicating no functional ambulation abilities).19 The Box provides a complete overview of the inclusion and exclusion criteria.
Figure 1. Flowchart of Participants and Measurements During the Study Period.
Box. Inclusion and Exclusion Criteria.
Inclusion Criteria
Aged 70 y
Femoral neck or pertrochanteric fracture
Nursing home residency before injury
-
Classification as frail with at least 1 of the following
Body mass index <18.5 (calculated as weight in kilograms divided by height in meters squared) or cachexia
Severe comorbidities, with American Society of Anesthesiologists physical status class IV or V
Mobility issues, with Functional Ambulation Category (FAC) 0-2a
Exclusion Criteria
Subtrochanteric fractures
Bilateral proximal femoral fractures
Periprosthetic fractures
Delayed diagnosis by >7 d
Known metastatic disease
Confirmed pathological fracture of proximal femur
Insufficient comprehension of Dutch language by patients or proxies
Participation in another surgical intervention or drug study
A treatment decision was reached using a structured SDM process. With this process, the advantages and disadvantages of both nonoperative management and operative management are discussed by the patient, proxies or relatives, and all relevant health care practitioners. After this deliberation, a joint decision on the treatment is made. Although some form of SDM is used in current practice, it is not specifically mentioned in current guidelines, and no SDM tools are available. In this study, we implemented a more structured SDM approach by providing the health care practitioners in the study a full, unbiased forecast on both nonoperative management and operative management for use as a general guiding tool. Patients received usual care throughout the study period, and no specific recommendations were made by the study team.
The primary outcome was the HRQoL as reported by patient proxies and caregivers (nursing staff) and indicated by the utility scores on the EuroQol 5 Dimension 5 Level (EQ-5D) questionnaire.20,21,22,23,24 The EQ-5D questionnaire was converted into utility scores using the Dutch tariff, and the scores ranged from −0.33 to 1, with lower scores indicating worse HRQoL. Views of proxies or caregivers regarding the patient’s health were established using a vertical visual analog scale, with scores ranging from 0 to 100.
Secondary outcomes were QOL as measured by QUALIDEM (a dementia-specific QOL instrument for persons with dementia in residential settings), which includes 9 domains (care relationship [score range, 0-21], positive affect [score range, 0-18], negative affect [score range, 0-9], restless tense behavior [score range, 0-9], positive self-image [score range, 0-9], social relations [score range, 0-18], social isolation [score range, 0-9], feeling at home [score range, 0-12], and having something to do [score range, 0-6])25; activities of daily living (ADL) dependency, as evaluated with the Katz ADL score (score range: 0-6, with 0 indicating independence and 6 indicating total dependency); level of pain, as assessed using the Pain Assessment Checklist for Seniors With Limited Ability to Communicate, which resulted in a dichotomous outcome of pain or no pain26 and analgesic drug use (daily 1 mg oral equivalent); adverse events, with corresponding Clavien-Dindo classification27; mobility; and mortality. Furthermore, satisfaction of the proxies and caregivers with the chosen treatment was assessed with a numeric rating scale, where 0 was extremely dissatisfied and 10 was extremely satisfied. The quality of dying was assessed by proxies using the Quality of Dying and Death Questionnaire, and the quality may be classified under 3 categories: terrible-poor, intermediate, and good-almost perfect.28,29 A detailed description of the instruments used is included in the study protocol.17 One of us (S.A.I.L.) gathered all of the data. Race and ethnicity data were not collected because this variable is not a relevant factor in the Netherlands where all individuals are insured by law and nursing home stay is funded by the Long-term Care Act; therefore, the decision on operative or nonoperative management was not affected by race and ethnicity or income.
Statistical Analysis
Data were analyzed using SPSS Statistics, version 25.0 (IBM SPSS) on a per-protocol basis. Continuous data were reported as medians (25th and 75th percentile [P25-P75]) or means (95% CI), and categorical data were reported as numbers with percentages. Absolute differences with 95% CI were calculated using MedCalc Statistical Software, version 18.2.1 (MedCalc Software Ltd). For continuous variables, the Hodges-Lehmann risk differences with corresponding 95% CI were calculated. Univariate comparison between groups was performed using a Mann-Whitney test, χ2 test, or Fisher exact test, where applicable. A 2-sided P < .05 was the threshold of statistical significance.
Continuous subjective outcomes (EQ-5D and QUALIDEM scores) that were repeatedly measured over time were compared between treatment groups using linear mixed-effects regression models. These multilevel models included random effects for the intercepts of the model and time coefficient of individual patients. Because the outcome measures were not linearly related with time, the time points were entered as a factor. The models included fixed effects for treatment group, age, sex, and American Society of Anesthesiologists physical status classification. The interaction between treatment group and time was included in the model to test for differences between the groups over time. For each follow-up moment, the estimated marginal mean with 95% CI was computed per treatment group. Descriptive statistical tests were performed only if both groups contained 10 or more participants. Risk factors for mortality were identified using Cox proportional hazards regression analysis.
The sample size calculation indicated a need for 80 participants per treatment group and is detailed in the study protocol.17 For the primary outcome measure, a noninferiority margin of 0.15 points of the 95% CI of the EQ-5D utility score was used, with the null hypothesis that nonoperative management was inferior to operative management.30 As was done in previous studies, the noninferiority limit was based on 50% of the SD of previous EQ-5D data on proximal femoral fractures.30
Results
A total of 172 patients (median [P25-P75] age, 88 [85-92] years; 37 men [22%] and 135 women [78%]) were included in the study, of whom 88 opted for nonoperative management and 84 opted for operative management (Figure 1). No participants were lost to follow-up. Patient and fracture characteristics were statistically similar for both treatment groups (Table 1 and Table 2). A high number of comorbidities and high level of preinjury ADL dependency were found in both nonoperative and operative management groups. Elder care physicians were more often involved in the SDM process for patients in the nonoperative vs operative management group (46 [53%] vs 18 [23%]; P < .001). After choosing nonoperative management, 39 patients (44%) returned to their nursing home residency without hospital admission.
Table 1. Patient Characteristics .
| Characteristic | Nonoperative management group (n = 88) | Operative management group (n = 84) | Absolute or median difference (95% CI), %a | P value | ||
|---|---|---|---|---|---|---|
| Total No. of patients with measurement | No. of patients with measurement (%) | Total No. of patients with measurement | No. of patients with measurement (%) | |||
| Age, median (P25-P75), y | 88 | 88 (84-93) | 84 | 88 (85-91) | 1.0 (−2.0 to 1.0) | .57 |
| Female sex | 88 | 67 (76) | 84 | 68 (81) | 1.0 (−10.8 to 12.9) | .28 |
| Male sex | 88 | 21 (24) | 84 | 16 (19) | ||
| BMI, median (P25-P75) | 68 | 20.4 (18.0-25.2) | 77 | 23.2 (18.4-26.3) | 1.0 (−0.3 to 2.6) | .10 |
| Nursing home resident | 88 | 88 (100) | 84 | 84 (100) | 0 (−4.4 to 4.2) | >.99 |
| CCI, median (P25-P75) | 88 | 3 (2-5) | 84 | 3 (2-5) | 0 (0.0 to 1.0) | .44 |
| ≥4 | 35 (40) | 41 (49) | 9.0 (−5.7 to 23.2) | .28 | ||
| Dementia diagnosis | 88 | 83 (94) | 84 | 75 (89) | 5.0 (−3.7 to 14.1) | .23 |
| Mobility FAC | ||||||
| 0 | 88 | 6 (7) | 84 | 5 (6) | 1.0 (−7.1 to 9.1) | .20 |
| 1 | 13 (15) | 5 (6) | 9.0 (−0.4 to 18.5) | |||
| 2 | 28 (32) | 27 (32) | 0 (−13.7 to 31.8) | |||
| 3 | 13 (15) | 8 (10) | 5.0 (−5.2 to 15.1) | |||
| 4 | 38 (45) | 28 (32) | 13.0 (−1.5 to 26.7) | |||
| 5 | 1 (1) | 0 | 1.0 (−3.5 to 5.9) | |||
| ≤2b | 88 | 47 (53) | 84 | 37 (44) | 9.0 (−5.8 to 23.3) | .23 |
| Mobility | ||||||
| Bedbound | 88 | 0 | 84 | 0 | 0 (−4.2 to 4.4) | .12 |
| Bed-chair transfer | 15 (17) | 10 (12) | 5.0 (−5.8 to 15.6) | |||
| Few steps (AR, <10 m) | 16 (18) | 8 (10) | 8.0 (−2.6 to 18.5) | |||
| Mobile (AR, ≥10 m) | 57 (65) | 66 (78) | 1.03 (−0.5 to 25.8) | |||
| Katz ADL scorec | ||||||
| 0 | 84 | 0 | 82 | 0 | .40 | |
| 1 | 0 | 2 (2) | 2.0 (−2.6 to 7.8) | |||
| 2 | 4 (5) | 4 (4) | 1.0 (−6.3 to 8.4) | |||
| 3 | 13 (16) | 17 (21) | 5.0 (−6.9 to 16.8) | |||
| 4 | 12 (14) | 17 (21) | 7.0 (−4.7 to 18.6) | |||
| 5 | 23 (27 | 18 (22) | 5.0 (−8.1 to 17.8) | |||
| 6 | 32 (38) | 24 (29) | 9.0 (−5.3 to 22.8) | |||
| ASA physical status classd | ||||||
| II | 88 | 4 (5) | 84 | 1 (1) | 4.0 (−1.9 to 10.8) | .41 |
| III | 53 (60) | 54 (64) | 4.0 (−10.4 to 18.1) | |||
| IV | 31 (35) | 29 (35) | 0 (−14.0 to 14.0) | |||
| Prescription drugs, median (P25-P75) | 88 | 6 (4-8) | 84 | 7 (5-9) | 1.0 (0.0 to 2.0) | .05 |
| Hemoglobin level, median (P25-P75), mmol/L | 74 | 7.0 (6.8-8.0) | 84 | 7.6 (7.2-8.3) | 0.4 (0.1 to 0.7) | .004 |
| Creatinine level, median (P25-P75), μmol/L | 73 | 86 (65-104) | 84 | 86 (65-104) | 5.0 (−4.0 to 14.0) | .27 |
Abbreviations: ADL, activities of daily living; AR, action radius; ASA, American Society of Anesthesiologists; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); CCI, Charlson Comorbidity Index; FAC, Functional Ambulation Category; P25-P75, 25th and 27th percentile.
SI conversion factor: To convert mmol/L to g/L, multiply by 10.0.
Absolute difference applied to female sex, male sex, nursing home resident, CCI ≥4, dementia diagnosis, mobility FAC, mobility, Katz ADL score, and ASA status. Median difference was applied to age, BMI, prescription drugs, hemoglobin level, and creatinine level.
Indicates a person who needs at least (intermittent) manual assistance from 1 person during ambulation (FAC 2) or who has no functional ambulation abilities (FAC 0).
Score range: 0-6, with 0 indicating independence and 6 indicating total dependency.
ASA status ranged from class I to V, with V indicating the highest perioperative risk of death.
Table 2. Fracture Characteristics and Management .
| Characteristic | Nonoperative management group (n = 88) | Operative management group (n = 84) | Absolute or median difference (95% CI), %a | P value | ||
|---|---|---|---|---|---|---|
| Total No. of patients with measurement | No. of patients with measurement (%) | Total No. of patients with measurement | No. of patients with measurement (%) | |||
| Fracture type | ||||||
| Femoral neck | 54 | 54 (61) | 45 | 45 (54) | 7.0 (−7.6 to 12.3) | .30 |
| Garden 1-2 | 54 | 13 (24) | 45 | 7 (16) | 8.0 (−8.3 to 23.1) | .33 |
| Garden 3-4 | 54 | 41 (76) | 45 | 38 (84) | 8.0 (−8.3 to 23.1) | NA |
| Pertrochanteric | 34 | 34 (39) | 39 | 39 (46) | 7.0 (−7.6 to 21.3) | NA |
| AO 31-A1 | 34 | 11 (32) | 39 | 14 (36) | 4.0 (−17.3 to 24.5) | .94 |
| AO 31-A2 | 34 | 19 (56) | 39 | 21 (54) | 2.0 (−20.0 to 23.6) | NA |
| AO 31-A3 | 34 | 4 (12) | 39 | 4 (10) | 2.0 (−13.1 to 18.1) | NA |
| Other injuries | 88 | 9 (10) | 84 | 9 (11) | 1.0 (−8.5 to 10.7) | >.99 |
| Attendance for SDMb | ||||||
| Proxy | 87 | 85 (98) | 77 | 71 (92) | 6.0 (−1.0 to 14.4) | .10 |
| Geriatrics | 86 | 57 (66) | 77 | 42 (55) | 11.0 (−3.9 to 25.4) | .13 |
| Trauma surgery | 88 | 56 (66) | 84 | 45 (60) | 6.0 (−8.3 to 20.0) | .44 |
| Elderly care | 87 | 46 (53) | 77 | 18 (23) | 30.0 (15.2 to 42.9) | <.001 |
| Orthopedic surgery | 83 | 20 (24) | 74 | 23 (31) | 7.0 (−6.9 to 20.8) | .33 |
| Emergency medicine | 87 | 3 (3) | 78 | 4 (5) | 2.0 (−4.8 to 9.6) | .71 |
| Anesthesiology | 87 | 1 (1) | 78 | 3 (4) | 3.0 (−2.6 to 10.0) | .35 |
| Cardiology | 87 | 1 (1) | 78 | 1 (1) | 0 (−5.1 to 5.5) | >.99 |
| Palliative care | 87 | 1 (1) | 78 | 0 | 1.0 (−3.8 to 6.0) | >.99 |
| Hospital admission | 88 | 49 (56) | 84 | 84 (100) | 44.0 (33.2 to 54.4) | <.001 |
| Time to surgery, h | ||||||
| <24 | NA | NA | 84 | 43 (51) | NA | NA |
| 24-48 | NA | NA | 84 | 32 (38) | NA | NA |
| >48 | NA | NA | 84 | 9 (11) | NA | NA |
| Anesthesia type | ||||||
| General | NA | NA | 84 | 55 (66) | NA | NA |
| Spinal | NA | NA | 84 | 29 (35) | NA | NA |
| Lead surgeon | ||||||
| Surgeon | NA | NA | 84 | 64 (78) | NA | NA |
| Resident | NA | NA | 84 | 18 (22) | NA | NA |
| Implant | ||||||
| Osteosynthesis | NA | NA | 84 | 7 (8) | NA | NA |
| Intramedullary | NA | NA | 84 | 37 (44) | NA | NA |
| Hemiarthroplasty | NA | NA | 84 | 40 (48) | NA | NA |
| Femoral nerve block | 88 | 14 (16) | 84 | 18 (21) | 5.0 (−6.6 to 16.7) | .35 |
| PENG block | 88 | 1 (1) | 84 | 0 | 1.0 (−3.5 to 5.9) | >.99 |
| Hospital length of stay, median (P25-P75), d | 49 | 2 (2-3) | 84 | 6 (4-7) | 3.0 (2.0 to 4.0) | <.001 |
| Outpatient follow-up | 88 | 2 (2) | 84 | 13 (16) | 15.0 (5.6 to 23.4) | <.001 |
| Follow-up, median (P25-P75), d | 88 | 8 (5-14) | 84 | 176 (31-198) | 131.0 (50 to 169) | <.001 |
Abbreviations: NA, not applicable; P25-P75, 25th and 75th percentile; PENG, pericapsular nerve group; SDM, shared decision-making.
Absolute difference applied to all variables except for hospital length of stay and follow-up (median difference).
Attendance refers to a representative from a hospital department involved in SDM.
In the nonoperative management group, the EQ-5D utility score remained within the set 0.15 noninferiority limit of the 95% CI of the operative management group (week 1: 0.17 [95% CI, 0.13-0.29] vs 0.26 [95% CI, 0.11-0.23]; week 2: 0.19 [95% CI, 0.10-0.27] vs 0.28 [95% CI, 0.22-0.35]; and week 4: 0.24 [95% CI, 0.15-0.33] vs 0.34 [95% CI, 0.28-0.41]) (Figure 2A and B; eTable 1 in Supplement 1). The EQ-5D visual analog scale score for patient health status was significantly lower in the nonoperative management group than in the operative management group according to proxies and caregivers (Figure 2C and D; eTable 1 in Supplement 1). The levels of the problems experienced, according to proxies and caregivers, across the 5 domains of the EQ-5D are shown in eFigure 1 and eTables 2-6 in Supplement 1. In both treatment groups, the levels of problems with self-care (eTable 3 in Supplement 1) and ADL (eTable 4 in Supplement 1) were high. Among the surviving patients in the operative management group, total ADL dependency (Katz ADL score of 6) was found in 25 cases (50%) after 3 months and in 18 cases (41%) after 6 months.
Figure 2. EuroQoL-5 Dimension 5 Level (EQ-5D) Utility Score and Visual Analog Scale (VAS) Score for Patients in the Nonoperative Management (NOM) and Operative Management (OM) Groups, According to Proxies and Caregivers.
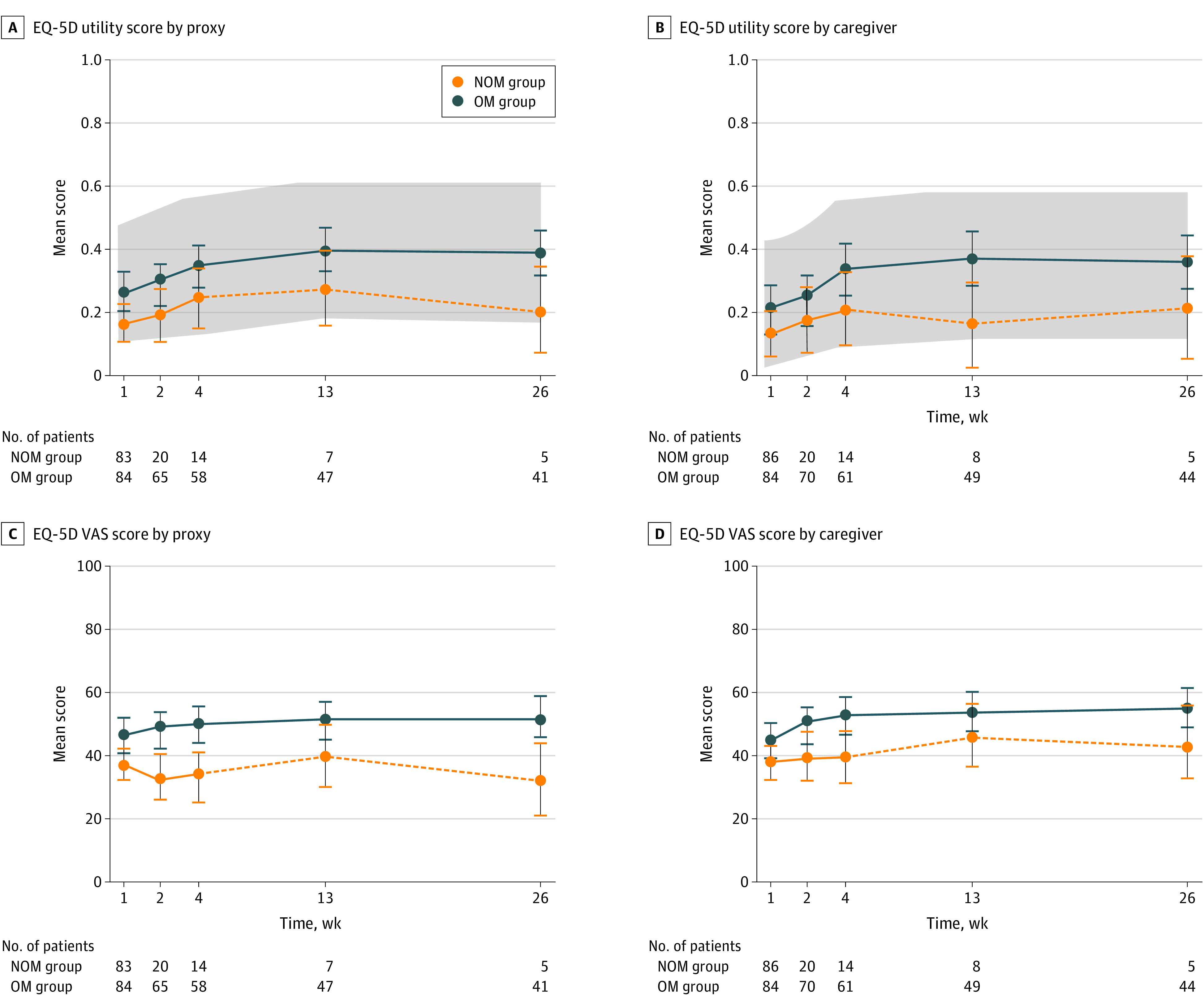
The gray area indicates the 0.15 noninferiority limit of the 95% CI of the utility score in the OM group (the reference group). The dotted line indicates the unadjusted measurements for fewer than 10 patients. Circles represent the mean score and the error bars indicate the 95% CI. The numbers of patients indicate those for whom EQ-5D utility and VAS scores could be ascertained at different follow-up times.
The level of mobility significantly decreased from the preinjury level (eTables 2 and 7 in Supplement 1). In the operative management group, although 66 of 84 patients (79%) were mobile before the injury, only 19 of 66 (29%) regained mobility during the study period. In the nonoperative management group, 78 patients (89%) remained bedbound. The QUALIDEM scores in the 9 domains were similar between the treatment groups without clinically relevant differences (eFigure 2 and eTable 8 in Supplement 1).
The level of pain or discomfort gradually decreased over time, but pain was frequent in the first weeks after the injury in both treatment groups (eFigure 3A and eTables 5 and 9 in Supplement 1). After 1 week, more patients in the nonoperative management group experienced pain compared with those in the operative management group (75 of 85 [88%] vs 56 of 84 [67%]; P = .001) (eFigure 3 in Supplement 1). However, this finding was not the same after 2 weeks (11 [55%] vs 37 [53%]; P > .99). Morphine was administered to almost every patient during the first week after the injury (eFigure 3 and eTable 10 in Supplement 1). The daily administration of morphine in the nonoperative management group was significantly higher than in the operative management group at all points of time (eTable 10 and eFigure 3 in Supplement 1).
In the first 2 weeks after the injury, we observed no statistically significant differences in the daily administered dose of morphine in the nonoperative management group between patients who did and patients who did not experience pain. In the first week, the median (P25-P75) daily morphine dose was 70 (49-95) mg in patients with pain (n = 75) and was 43 (20-113) mg in those without pain (n = 10) (median difference, 22 mg; 95% CI, −49 to 13 mg; P = .15). In the second week, the median (P25-P75) dose was 33 (2-62) mg in patients with pain (n = 11) and 29 (17-53) mg in patients without pain (n = 9) (mean difference, 5 mg; 95% CI, −27 to 22 mg; P = .88). In the operative management group, patients with pain received statistically higher median (P25-P75) doses of analgesia at all points of time compared with patients without pain (week 1: 19 [3-21] mg [n = 28] vs 19 [13-26] mg [n = 56], P = .02; week 2: 4 [0-13] mg [n = 33] vs 13 [3-25] mg [n = 37), P = .03; and week 4: 0 [0-9] mg [n = 44] vs 14 [0-30] mg [n = 17], P = .005).
Adverse events (AEs) were frequent but more frequent in the operative than nonoperative management group (167 vs 67) (Table 3). Significantly more patients in the operative management group vs nonoperative management group experienced at least 1 AE (68 [81%] vs 46 [52%]; P < .001) or multiple AEs (47 [56%] vs 16 [18%]; P < .001). Pressure ulcers were the most common AE in both groups (operative group: 35 [42%]; nonoperative group: 31 [35%]). A third of all patients who opted for operative management developed delirium (27 of 84 [32%]). Most AEs were registered after patients returned to their nursing homes (82% in the nonoperative management group [n = 55] and 62% in the operative management group [n = 103]). Surgery- or fracture-related AEs occurred in 13 patients (15%) in the operative management group. After initially opting for nonoperative management, 2 patients were treated surgically within the index admission because of progressive pain.
Table 3. Adverse Events, Severity, and Consequent Interventions .
| Characteristic | No. (%) | |
|---|---|---|
| Nonoperative management group | Operative management group | |
| All patients | 88 (100) | 84 (100) |
| AEs | ||
| Total No. | 67 (100) | 167 (100) |
| Patients with | ||
| Any AE | 46 (52) | 68 (81) |
| Multiple (≥2) AEs | 16 (18) | 47 (56) |
| Time to AE, d (P25-P75) | 6 (3-16) | 11 (5-32) |
| General AE | ||
| Pressure ulcer | 31 (35) | 35 (42) |
| Multiple pressure ulcers | 4 (5) | 7 (8) |
| Delirium | 10 (11) | 27 (32) |
| Multiple deliria | 0 | 4 (5) |
| Pneumonia | 5 (6) | 20 (24) |
| Multiple pneumonias | 0 | 2 (2) |
| UTI | 5 (6) | 16 (19) |
| Multiple UTIs | 0 | 4 (5) |
| Severe dehydration | 1 (1) | 8 (10) |
| Recurrent severe hydration | 0 | 1 (1) |
| Retention bladder | 0 | 8 (10) |
| Fracture after recurrent fall | 2 (2) | 6 (7) |
| Sepsis of unknown origin | 0 | 2 (2) |
| CVA | 1 (1) | 1 (1) |
| COVID-19 pneumonia | 1 (1) | 1 (1) |
| COPD exacerbation | 1 (1) | 0 |
| Depression | 1 (1) | 0 |
| Phlebitis | 0 | 1 (1) |
| Morphine intoxication | 1 (1) | 0 |
| Oral fungal infection | 0 | 1 (1) |
| Cardiovascular AE | ||
| Heart failure | 3 (3) | 7 (8) |
| Arrhythmia | 0 | 2 (2) |
| Myocardial infarction | 0 | 1 (1) |
| Surgery/fracture-related AE | ||
| Deep wound infection | NA | 4 (5) |
| Hemiarthroplasty dislocation | NA | 2 (2) |
| Superficial wound infection | NA | 1 (1) |
| Progressive paina | 0 | 2 (2) |
| Rebleed | NA | 1 (1) |
| Osteosynthesis malposition | NA | 1 (1) |
| Peroperative respiratory failure | NA | 1 (1) |
| Therapy refractive pain | 0 | 1 (1) |
| Flexion contracture | 1 (1) | 0 |
| Clavien-Dindo grade | ||
| II | 17 (25) | 72 (43) |
| IIIa | 1 (2) | 3 (2) |
| IIIb | 0 | 6 (4) |
| IV | 0 | 1 (1) |
| V | 13 (19) | 27 (16) |
| Interventions AE | ||
| Pharmacological | 28 (42) | 100 (60) |
| Nonpharmacological | 9 (13) | 13 (8) |
| Pharmacological and nonpharmacological | 13 (19) | 30 (18) |
| Invasive | 1 (2) | 10 (6) |
| Expectative, no intervention | 16 (24) | 14 (8) |
| Reoperation | NA | 5 (6) |
| Residence when diagnosed | ||
| Hospital | 12 (18) | 64 (38) |
| Nursing home | 55 (82) | 103 (62) |
| Other undesirable events | ||
| Physical fixation | 2 (2) | 12 (14) |
| Antipsychotic drug use | 29 (33) | 48 (57) |
| Sedative drug use | 65 (75) | 38 (45) |
| Antidepressant drug use | 1 (1) | 1 (1) |
| Antibiotic drug use | 7 (8) | 33 (39) |
| Blood transfusion | 2 (2) | 24 (29) |
| Readmission ED | 0 | 12 (14) |
| Reoperation | NA | 5 (6) |
Abbreviations: AE, adverse event; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; ED, emergency department; NA, not applicable; P25-P75, 25th and 75th percentile; UTI, urinary tract infection.
Patients who initially opted for nonoperative management but eventually underwent surgery because of progressive pain but were grouped in the operative management group because of per-protocol analyses.
In addition, antibiotic therapy (33 [39%] vs 7 [8%]) and blood transfusion (24 [29%] vs 2 [2%]) were frequently required in the operative management group but were less common in the nonoperative management group. All 12 readmissions (14%) in the operative management group were associated with surgery-related AEs or recurrent falls with new traumatic injuries.
The 30-day mortality rate was 83% (n = 73) in the nonoperative management group and 25% (n = 21) in the operative management group. Six months after the injury, 83 patients (94%) in the nonoperative management group and 40 patients (48%) in the operative management group had died (eTable 11 and eFigure 4 in Supplement 1). The median (P25-P75) time to death was 7 (5-12) days in the nonoperative management group and 29 (12-62) days in the operative management group (P < .001). Nonoperative management (odds ratio, 5.3; 95% CI, 3.6-7.8; P < .001) and male sex (odds ratio, 1.53; 95% CI, 1.0-2.4; P = .05) were independent factors in mortality 6 months after the injury (eTable 12 in Supplement 1).
At the end of the follow-up or after a patient’s death, treatment satisfaction according to proxies and health care practitioners was high in both groups, with a median numeric rating scale score of 8 (eTable 13 in Supplement 1). Both proxies and health care practitioners of the patients who died during the study were more satisfied with the choice of nonoperative management than operative management (median [P25-P75] satisfaction, proxies: 8 [8-9] vs 8 [7-8] [P = .001]; health care practitioners: 8 [8-9] vs 7 [5-8] [P < .001]). There was no statistically significant difference in treatment satisfaction between the treatment groups for patients who survived beyond 30 days after the injury. The dying process in both groups was judged as humane (eTable 13 in Supplement 1). The quality of dying was rated as good-almost perfect by 26 proxies (51%) in the nonoperative management group, with only 2 proxies (4%) rating the process as terrible-poor. The quality of dying in the operative management group was scored as intermediate by most proxies (13 [62%]).
Discussion
This study showed that, following SDM in a group of institutionalized frail patients with limited life expectancy who were hospitalized with a proximal femoral fracture, nonoperative management of proximal femoral fractures was a viable treatment option in properly selected patients and not inferior to operative management in terms of HRQoL. Although the short-term mortality in the nonoperative management group was higher than in the operative management group, there was no loss of QOL and HRQoL, and there was high treatment satisfaction and humane quality of dying. The high mortality rate was as expected given that we hypothesized that the frailest patients would opt for nonoperative management and that the explicit choice for nonoperative management would most likely result in an earlier palliative care approach compared with patients who opted for operative management.
When interpreting the results, one should consider that the HRQoL and life expectancy of nursing home residents are low, even without the additional event of a proximal femoral fracture. A previous study reported a mean (SD) EQ-5D utility score of 0.48 (0.09) for the general nursing home population in the Netherlands.31 A proximal femoral fracture further diminishes HRQoL. Among nursing home residents who were surgically treated for their injury, the mean (SD) EQ-5D utility scores at 3 months after the injury decreased from 0.6 (0.2) to 0.35 (0.24) in a Canadian study and 0.43 (0.34) to 0.39 (0.35) in a German study.3,32 The EQ-5D utility scores in the current study were even lower, most likely because of the added criteria of frailty. To our knowledge, no previous study has reported on the HRQoL in this specific group of patients who received nonoperative treatment.
In addition, the mean 1-year mortality after admission to a nursing home is approximately 30% for all age groups and 40% for those 90 years or older.33 Mortality for patients with advanced dementia was even higher at 24% to 37% after 6 months of injury.33,34 These findings further strengthen the assumption that a proximal femoral fracture in frail older patients is merely a symptom of the frail health status and thus often the start of an inevitable cascade breakdown at the end of life regardless of treatment used.
With regard to functional outcomes, the postinjury outcome in this study population was generally poor. Even in the operative management group, only some patients returned to their preinjury level of independence or mobility, and AEs or distressing symptoms were almost always observed. However, satisfactory outcomes after operative management can be achieved, and operative management remains a good treatment option for properly selected patients. Therefore, both operative and nonoperative management should be openly discussed. However, no selection criteria for operative management in this patient population could be identified.
The study results do suggest that pain in the nonoperative management group was undertreated and was a factor in end-of-life care that should be improved. This finding is consistent with previous study results.35
Decision-making on the treatment of proximal femoral fracture in frail patients in the final phase of life not only poses challenges and ethical dilemmas but also requires the consideration of many factors. Surgery in these patients is a decisive fix for an isolated problem (the fracture itself), but it is not an intervention that resolves the complex, multifaceted implications of aging and frailty and is not always beneficial to the patient.11 Therefore, the viability and consideration of a treatment option at the end of life require a multifaceted, comprehensive assessment of all aspects of care and not merely the stand-alone outcomes. To our knowledge, this study is the first to apply this multifaceted approach to both nonoperative and operative management of proximal femoral fractures.
Research suggests that approximately 60% of the proxies of nursing home residents feel that only treatments that promote comfort would best align with their goals of care, which has often meant foregoing life-sustaining treatments.36 Nonoperative management can align with the goals of care in this study population, which was indirectly reflected in the high proportion of patients or proxies who opted for nonoperative management and the high satisfaction with the chosen treatment. Properly discussing treatment options with frail patients who sustain a proximal femoral fracture may presumably be associated with higher rates of nonoperative management. This idea was demonstrated in the study by van der Zwaard et al,37 which found that, by using a comprehensive geriatric assessment followed by an SDM process, patients were 3.6 times more likely to opt for nonoperative management. Furthermore, this idea is reflected in the current study in which elder care physicians were found to be more often involved in the SDM process in patients who opted for nonoperative management. However, this involvement could have been owing to the frailer patients featuring in the nonoperative management group.
We believe this study presents a unique, evidence-based insight into the true outcomes of nonoperative and operative management in this specific frail patient population. Treatment decisions require careful consideration and should not be made hastily. Ultimately, an SDM process that is based on the expectations and goals of care of frail patients with a proximal femoral fracture and at the end of life may prevent surgical overtreatment, but careful patient selection remains pivotal. We believe the results of this study can be used to optimize SDM, to aid realistic expectation management, and to support advance care planning in long-term care facilities for this selected group of patients with proximal femoral fracture.
Limitations
This study has some limitations. First, selection bias is an important factor to consider because patients who opt for nonoperative management may be in worse preinjury condition that may not have been taken into account. The levels of cognitive function and preinjury HRQoL in this patient population were not explored and should be regarded as unmeasured bias because they could play a major role in the treatment decision. Furthermore, type 2 errors in preinjury characteristics could be present because of a relatively low sample size, as was reflected by the absolute differences between both groups. Only a randomized clinical trial would have avoided selection bias through the SDM process but was considered unfeasible and unethical. Second, no preoperative HRQoL questionnaires were administered because of the expected recall bias with the hypothesis that prefracture HRQoL would be overestimated, especially in the nonoperative management group.38 Although this cohort was the largest to date given the number of patients decreasing over time because of mortality, the results of the linear mixed-effects regression model should be interpreted with caution.
Third, no studies have previously evaluated the proxy- and caregiver- reported outcome measures in this population with such a high short-term mortality. However, the results seem valid, not only because of the minimal differences in scores between the proxies and caregivers but also because of the consistency of the results across all instruments. Furthermore, because, to our knowledge, no previous studies have evaluated the EQ-5D utility scores in this population of patients who received nonoperative management, the minimal important change is unknown; therefore, the noninferiority limit was based on 0.5 SD.30 Fourth, given the even-higher-than-expected mortality rate in the nonoperative management group, the validity of the results comparing nonoperative management with operative management was reduced 30 days after the injury. However, the high early mortality rate in the nonoperative management group suggests that, together, health care practitioners or caregivers and patients or proxies can adequately select patients via the SDM process who are good candidates for nonoperative management and for whom this treatment would achieve a high degree of satisfaction.
Conclusions
This cohort study found that, following the SDM process, nonoperative management of proximal femoral fractures is a viable treatment option for institutionalized frail patients with limited life expectancy. A return to preinjury levels of independence or mobility was achieved in some patients who were surgically treated, and a postoperative period without AEs was rare. Surgery in this specific patient population should not be a foregone conclusion.
eTable 1. EQ5D Utility and VAS Scores for Proxies and Caregiver
eFigure 1. EQ-5D Domains With the Levels of Problems per Domain and Point of Time in the Nonoperative and Operative Group
eTable 2. EQ5D Mobility Domain With Levels of Problems per Point of Time
eTable 3. EQ5D Self-Care Domain With Levels of Problems per Point of Time
eTable 4. EQ5D Activities of Daily Life Domain With Levels of Problems per Point of Time
eTable 5. EQ5D Pain/Discomfort Domain With Levels of Problems per Point of Time
eTable 6. EQ5D Activities of Daily Life Domain With Levels of Problems per Point of Time
eTable 7. Mobility Outcomes per Study Arm and Point of Time
eFigure 2. Quality of Life With Regards to the QUALIDEM Scores for the Nine Domains in the Nonoperative and Operative Group
eTable 8. Quality of Life With Regards to the QUALIDEM Scores for the Nine Domains
eFigure 3. Level of Pain and Morphine Administration During the Study Period in the Nonoperative and Operative Group
eTable 9. Pain Based on PACSLAC-D Scores per Point of Time
eTable 10. Morphine Administration per Point of Time
eTable 11. Cumulative Mortality Rates and Cause of Death
eFigure 4. Cox Proportional Hazard Survival Curve
eTable 12. Multivariable Analysis of Survival Risk
eTable 13. Treatment Satisfaction and Quality of Dying and Death
Nonauthor Collaborators
Footnotes
Indicates a person who needs at least (intermittent) manual assistance from 1 person during ambulation (FAC 2) or who has no functional ambulation abilities (FAC 0).
References
- 1.Gjertsen JE, Baste V, Fevang JM, Furnes O, Engesæter LB. Quality of life following hip fractures: results from the Norwegian hip fracture register. BMC Musculoskelet Disord. 2016;17:265. doi: 10.1186/s12891-016-1111-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van de Ree CLP, Landers MJF, Kruithof N, et al. Effect of frailty on quality of life in elderly patients after hip fracture: a longitudinal study. BMJ Open. 2019;9(7):e025941. doi: 10.1136/bmjopen-2018-025941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR. Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: prospective cohort study. J Am Geriatr Soc. 2012;60(7):1268-1273. doi: 10.1111/j.1532-5415.2012.04033.x [DOI] [PubMed] [Google Scholar]
- 4.Panula J, Pihlajamäki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. 2011;12:105. doi: 10.1186/1471-2474-12-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676-685. doi: 10.1016/j.injury.2011.05.017 [DOI] [PubMed] [Google Scholar]
- 6.Morrison RS, Siu AL. Survival in end-stage dementia following acute illness. JAMA. 2000;284(1):47-52. doi: 10.1001/jama.284.1.47 [DOI] [PubMed] [Google Scholar]
- 7.Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop. 2014;85(1):54-59. doi: 10.3109/17453674.2013.878831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Regional Office for Europe . Better palliative care for older people. Accessed January 22, 2021. http://www.euro.who.int/document/E82933.pdf
- 9.Lin JC, Liang WM. Mortality, readmission, and reoperation after hip fracture in nonagenarians. BMC Musculoskelet Disord. 2017;18(1):144. doi: 10.1186/s12891-017-1493-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berry SD, Rothbaum RR, Kiel DP, Lee Y, Mitchell SL. Association of clinical outcomes with surgical repair of hip fracture vs nonsurgical management in nursing home residents with advanced dementia. JAMA Intern Med. 2018;178(6):774-780. doi: 10.1001/jamainternmed.2018.0743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clapp JT, Schwarze ML, Fleisher LA. Surgical overtreatment and shared decision-making—the limits of choice. JAMA Surg. 2022;157(1):5-6. doi: 10.1001/jamasurg.2021.4425 [DOI] [PubMed] [Google Scholar]
- 12.van de Ree CLP, De Jongh MAC, Peeters CMM, de Munter L, Roukema JA, Gosens T. Hip fractures in elderly people: surgery or no surgery? a systematic review and meta-analysis. Geriatr Orthop Surg Rehabil. 2017;8(3):173-180. doi: 10.1177/2151458517713821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loggers SAI, Van Lieshout EMM, Joosse P, Verhofstad MHJ, Willems HC. Prognosis of nonoperative treatment in elderly patients with a hip fracture: a systematic review and meta-analysis. Injury. 2020;51(11):2407-2413. doi: 10.1016/j.injury.2020.08.027 [DOI] [PubMed] [Google Scholar]
- 14.National Institute for Health and Care Excellence . Hip fracture: management. Accessed September 23, 2017. https://www.nice.org.uk/guidance/cg124 [PubMed]
- 15.Federatie Medisch Specialisten . Richtlijn proximale femurfracturen. Accessed September 23, 2017. https://richtlijnendatabase.nl/richtlijn/proximale_femurfracturen/proximale_femurfracturen_-_startpagina.html
- 16.Cram P, Yan L, Bohm E, et al. Trends in operative and nonoperative hip fracture management 1990-2014: a longitudinal analysis of Manitoba administrative data. J Am Geriatr Soc. 2017;65(1):27-34. doi: 10.1111/jgs.14538 [DOI] [PubMed] [Google Scholar]
- 17.Joosse P, Loggers SAI, Van de Ree CLPM, et al. ; FRAIL-HIP Study Group . The value of nonoperative versus operative treatment of frail institutionalized elderly patients with a proximal femoral fracture in the shade of life (FRAIL-HIP); protocol for a multicenter observational cohort study. BMC Geriatr. 2019;19(1):301. doi: 10.1186/s12877-019-1324-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 19.Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired: reliability and meaningfulness. Phys Ther. 1984;64(1):35-40. doi: 10.1093/ptj/64.1.35 [DOI] [PubMed] [Google Scholar]
- 20.Brooks R, Rabin R, de Charro F, eds. The Measurement and Valuation of Health Status Using EQ-5D: A European Perspective. Kluwer Academic Publishers; 2003. [Google Scholar]
- 21.Neugebauer E, Bouillon B, Bullinger M, Wood-Dauphinée S. Quality of life after multiple trauma—summary and recommendations of the consensus conference. Restor Neurol Neurosci. 2002;20(3-4):161-167. [PubMed] [Google Scholar]
- 22.Van Beeck EF, Larsen CF, Lyons RA, Meerding WJ, Mulder S, Essink-Bot ML. Guidelines for the conduction of follow-up studies measuring injury-related disability. J Trauma. 2007;62(2):534-550. doi: 10.1097/TA.0b013e31802e70c7 [DOI] [PubMed] [Google Scholar]
- 23.Tol MCJM, Kuipers JP, Willigenburg NW, Willems HC, Poolman RW. How are you doing in the eyes of your spouse? level of agreement between the self-completed EQ-5D-5L and two proxy perspectives in an orthopaedic population: a randomized agreement study. Health Qual Life Outcomes. 2021;19(1):35. doi: 10.1186/s12955-021-01679-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lamers LM, McDonnell J, Stalmeier PF, Krabbe PF, Busschbach JJ. The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ. 2006;15(10):1121-1132. doi: 10.1002/hec.1124 [DOI] [PubMed] [Google Scholar]
- 25.Ettema TP, Dröes RM, de Lange J, Mellenbergh GJ, Ribbe MW. QUALIDEM: development and evaluation of a dementia specific quality of life instrument—validation. Int J Geriatr Psychiatry. 2007;22(5):424-430. doi: 10.1002/gps.1692 [DOI] [PubMed] [Google Scholar]
- 26.Fuchs-Lacelle S, Hadjistavropoulos T. Development and preliminary validation of the pain assessment checklist for seniors with limited ability to communicate (PACSLAC). Pain Manag Nurs. 2004;5(1):37-49. doi: 10.1016/j.pmn.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 27.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-213. doi: 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Downey L, Curtis JR, Lafferty WE, Herting JR, Engelberg RA. The Quality of Dying and Death Questionnaire (QODD): empirical domains and theoretical perspectives. J Pain Symptom Manage. 2010;39(1):9-22. doi: 10.1016/j.jpainsymman.2009.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gerritsen RT, Hofhuis JGM, Koopmans M, et al. Perception by family members and ICU staff of the quality of dying and death in the ICU: a prospective multicenter study in the Netherlands. Chest. 2013;143(2):357-363. doi: 10.1378/chest.12-0569 [DOI] [PubMed] [Google Scholar]
- 30.Bhandari M, Devereaux PJ, Einhorn TA, et al. ; HEALTH Investigators . Hip fracture evaluation with alternatives of total hip arthroplasty versus hemiarthroplasty (HEALTH): protocol for a multicentre randomised trial. BMJ Open. 2015;5(2):e006263. doi: 10.1136/bmjopen-2014-006263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leontjevas R, Teerenstra S, Smalbrugge M, Koopmans RT, Gerritsen DL. Quality of life assessments in nursing homes revealed a tendency of proxies to moderate patients’ self-reports. J Clin Epidemiol. 2016;80:123-133. doi: 10.1016/j.jclinepi.2016.07.009 [DOI] [PubMed] [Google Scholar]
- 32.Balzer-Geldsetzer M, Buecking B, Ruchholtz S, Kis B, Dodel R, Hessmann P. Association between longitudinal clinical outcomes in patients with hip fracture and their pre-fracture place of residence. Psychogeriatrics. 2020;20(1):11-19. doi: 10.1111/psyg.12450 [DOI] [PubMed] [Google Scholar]
- 33.Reilev M, Lundby C, Jensen J, Larsen SP, Hoffmann H, Pottegård A. Morbidity and mortality among older people admitted to nursing home. Age Ageing. 2019;49(1):67-73. doi: 10.1093/ageing/afz136 [DOI] [PubMed] [Google Scholar]
- 34.van der Steen JT, Mitchell SL, Frijters DH, Kruse RL, Ribbe MW. Prediction of 6-month mortality in nursing home residents with advanced dementia: validity of a risk score. J Am Med Dir Assoc. 2007;8(7):464-468. doi: 10.1016/j.jamda.2007.05.004 [DOI] [PubMed] [Google Scholar]
- 35.Sieber FE, Mears S, Lee H, Gottschalk A. Postoperative opioid consumption and its relationship to cognitive function in older adults with hip fracture. J Am Geriatr Soc. 2011;59(12):2256-2262. doi: 10.1111/j.1532-5415.2011.03729.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mitchell SL, Palmer JA, Volandes AE, Hanson LC, Habtemariam D, Shaffer ML. Level of care preferences among nursing home residents with advanced dementia. J Pain Symptom Manage. 2017;54(3):340-345. doi: 10.1016/j.jpainsymman.2017.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Zwaard BC, Stein CE, Bootsma JEM, van Geffen HJAA, Douw CM, Keijsers CJPW. Fewer patients undergo surgery when adding a comprehensive geriatric assessment in older patients with a hip fracture. Arch Orthop Trauma Surg. 2020;140(4):487-492. doi: 10.1007/s00402-019-03294-5 [DOI] [PubMed] [Google Scholar]
- 38.Scholten AC, Haagsma JA, Steyerberg EW, van Beeck EF, Polinder S. Assessment of pre-injury health-related quality of life: a systematic review. Popul Health Metr. 2017;15(1):10. doi: 10.1186/s12963-017-0127-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. EQ5D Utility and VAS Scores for Proxies and Caregiver
eFigure 1. EQ-5D Domains With the Levels of Problems per Domain and Point of Time in the Nonoperative and Operative Group
eTable 2. EQ5D Mobility Domain With Levels of Problems per Point of Time
eTable 3. EQ5D Self-Care Domain With Levels of Problems per Point of Time
eTable 4. EQ5D Activities of Daily Life Domain With Levels of Problems per Point of Time
eTable 5. EQ5D Pain/Discomfort Domain With Levels of Problems per Point of Time
eTable 6. EQ5D Activities of Daily Life Domain With Levels of Problems per Point of Time
eTable 7. Mobility Outcomes per Study Arm and Point of Time
eFigure 2. Quality of Life With Regards to the QUALIDEM Scores for the Nine Domains in the Nonoperative and Operative Group
eTable 8. Quality of Life With Regards to the QUALIDEM Scores for the Nine Domains
eFigure 3. Level of Pain and Morphine Administration During the Study Period in the Nonoperative and Operative Group
eTable 9. Pain Based on PACSLAC-D Scores per Point of Time
eTable 10. Morphine Administration per Point of Time
eTable 11. Cumulative Mortality Rates and Cause of Death
eFigure 4. Cox Proportional Hazard Survival Curve
eTable 12. Multivariable Analysis of Survival Risk
eTable 13. Treatment Satisfaction and Quality of Dying and Death
Nonauthor Collaborators