Abstract
Prior studies sought to explain the predisposition to suicidal behavior in terms of myopic preference for immediate versus delayed rewards, generating mixed evidence. Data from gambling and bandit tasks, however, suggest that suboptimal decisions in suicidal individuals are explained by inconsistent valuation rather than myopic preferences. We tested these two alternative hypotheses using a delay discounting task in 622 adults (suicide attempters with depression, suicide ideators with depression, nonsuicidal participants with depression, and healthy controls) recruited across three sites through inpatient psychiatric units, mood disorders clinics, primary care, and advertisements. Multi-level models revealed group differences in valuation consistencies in all three samples, with high-lethality suicide attempters exhibiting less consistent valuation than all other groups in Samples 1, 3 and less consistent valuation than the healthy controls or participants with depression in Sample 2. In contrast, group differences in preference for immediate versus delayed rewards were observed only in Sample 1 and were due to the high-lethality suicide attempters displaying a weaker preference for immediate rewards than low-lethality suicide attempters. The findings were robust to confounds such as cognitive functioning and comorbidities. Seemingly impulsive choices in suicidal behavior are explained by inconsistent reward valuation rather than a true preference for immediate rewards. In a suicidal crisis, this inconsistency may result in a misestimation of the value of suicide relative to constructive alternatives and deterrents.
Keywords: suicide, delay discounting, reward, valuation, adults
General Scientific Summary
Is the predisposition to suicidal behavior better explained by an excessive focus on short-term outcomes or by a general failure to consistently estimate the values of available options? We found support for the inconsistent valuation hypothesis in a sample of 324 older adults and replicated this finding in two additional clinical samples of adults that included 298 additional participants. What was previously portrayed as impulsivity in attempted suicide may be more accurately described as inconsistent choice processes that contribute to the appearance of impulsive choice.
Introduction
Transient crises can precipitate suicide attempts, suggesting that people vulnerable to suicidal behavior may overvalue their current experience at the expense of the more remote future (Neuringer & Harris, 1974; Neuringer & Levenson, 1972). Do myopic intertemporal preferences predispose to suicidal behavior? Prior studies have indeed linked a myopic preference for immediate over delayed rewards – known as high delay discounting – to certain forms of suicidal behavior, including less medically serious and poorly planned suicide attempts in late-life depression (Dombrovski et al., 2011), suicide attempts in individuals with addiction (Liu et al., 2012), and suicide attempts among adolescents (Dougherty et al., 2011; Mathias et al., 2011). Yet, other studies found no evidence of myopic preferences in adolescent (Bridge et al., 2015) or adult suicide attempters (Millner et al., 2018). Additionally, published studies on the whole may overstate the magnitude and consistency of group differences due to publication bias (Amlung et al., 2019). Further, the lack of agreement about the features of suicidal behavior (e.g., lethality, planning, recurrence of suicide attempts) associated with myopic preferences suggests either poorly understood clinical heterogeneity, or that traditional metrics of delay discounting do not accurately capture components of decision-making relevant to suicidal behavior.
This ambiguity may stem from the fact that studies of delay discounting in suicidal behavior, and in psychopathology in general, assume that a true consistent preference for immediate reinforcers constitutes a stable pathological trait (Amlung et al., 2019). Instead, evidence from other studies of value-based choice using bandit and gambling paradigms suggests that individuals prone to suicidal behavior may fail to consistently incorporate different attributes of an option into their decisions (Clark et al., 2011; Dombrovski et al., 2013, 2019; Vanyukov et al., 2016). Indeed, rational decision-making involves integrating disparate option attributes – such as magnitude and timing of rewards -– into a single decision variable, expected value (see Table 1 for Key Terms). A person deciding whether a crisis can be resolved by attempting suicide is comparing options with disparate outcomes occurring at varying time points: escape from current suffering, foregoing future joys, impact on others and consequences of a non-fatal suicide attempt vs. alternative futures for competing solutions to the crisis. As discussed earlier, suicide may be myopically preferred to alternatives because it cancels immediate suffering at the expense of the future. However, the valuation of these choices may vary over time as symptoms or environmental stressors fluctuate. We propose an alternative account wherein suicide is not consistently preferred over alternative solutions, but since values of alternatives are constructed in an inconsistent, noisy manner, suicide may sometimes dominate superior alternatives by chance, a kind of a decision accident [cf. Beskow et al., 1994]. Thus, inconsistent valuation may constitute a part of the cognitive diathesis to suicide, a diathesis supported by a large body of prospective cohort and case-control studies (Allen et al., 2019; Bredemeier & Miller, 2015; Cha et al., 2019; Gujral et al., 2014, 2020; Richard-Devantoy et al., 2014; Saffer & Klonsky, 2018). Adjudicating between the competing hypotheses of myopic preference vs. inconsistent valuations would have not only theoretical, but also practical implications. If myopic preferences facilitated suicidal behavior, high-risk individuals who display such preferences could benefit from prospection or working memory training interventions which may reduce discount rates (Bickel et al., 2011; Mellis et al., 2019; Peters & Buchel, 2010). In contrast, if suicidal behavior is better explained by inconsistent valuation, compensatory interventions could focus on consistently reinforcing the value of deterrents or alternative solutions.
Table 1.
Key Terms
| Term | Definition |
|---|---|
| Expected value | The worth of an option as a function of its attributes (in delay discounting, reward magnitude and delay to the receipt of that reward). |
| Hyperbolic discounting | Tendency to discount delayed rewards in inverse proportion to the length of the delay. |
| Discount rates that correspond to the indifference point for a given item consisting of a smaller immediate and a larger delayed reward options (Methods, equation 1). | |
| k subject | Subject-level discount rate that captures individual preferences for smaller, immediate, versus larger, delayed rewards. |
| Valuation consistency, β | A degree to which choices are sensitive to the relative expected values of the available options. This parameter is analogous to the inverse temperature of the softmax choice function (Methods, equation 4). |
An additional reason for inconsistent findings in studies of delay discounting may be statistical. Prior studies examined individual differences in discount rates using two-stage analysis methods similar to that described Kirby, Petry, and Bickel (1999). As we detail below (Methods, Statistical Analysis), two-stage approaches derive subject-level estimates to be used in statistical analyses in stage two by aggregating across multiple choices in stage one. This means that the second stage lacks any information regarding trial-by-trial changes in intertemporal preferences and the precision of these stage one estimates. Thus, this approach does not propagate uncertainty from the within-subject level to the between-subject level and fails to regularize individual estimates by data from the group, yielding unrealistically extreme values in inconsistent subjects (see Young, 2018 for a more in-depth discussion of these issues). We introduce a multi-level modeling (MLM) method intended to overcome these limitations.
To adjudicate between the myopic preference and inconsistent valuation hypotheses, we applied our new MLM approach to the analysis of data from a study of delay discounting in attempted suicide. To ensure that individual differences in discounting were specific to suicidal behavior, we included comparison groups of individuals with depression and with suicidal ideation but without prior suicidal behavior. To test for a dose-response relationship between decision deficits and suicidal behavior, we examined whether discounting parameters would scale with the medical seriousness (lethality) of suicide attempts. A careful characterization enabled us to assess the impact of potential confounds, including age, sex, race, income, and education; global cognitive functioning; possible brain injury from a past suicide attempt; history of substance use and/or anxiety disorders. We replicated our findings in two additional clinical samples: one of younger and one of older adults.
Methods
Samples and their Characteristics
Sample 1 (Reward Learning in Late-Life Suicide study; Pittsburgh, PA).
This sample included 324 participants aged 50-93 (Mage = 65.63, SD = 9.04; 54.0% female) and comprised four groups: 116 suicide attempters with depression (SA+MDD), 76 suicide ideators with depression (SI+MDD), 66 nonsuicidal participants with depression (MDD), and 66 healthy controls (Controls). Suicide attempt was defined as “a potentially self-injurious action with a nonfatal outcome for which there is evidence, either explicit or implicit, that the individual intended to kill himself/herself. The action may or may not result in injuries” (O’Carroll et al., 1996) (p.247). The SA+MDD group was further split into high-lethality (HL SA+MDD) and low-lethality (LL SA+MDD) subgroups. The procedures were approved by the University of Pittsburgh Institutional Review Board (PRO14050627). Recruitment efforts took place via a psychogeriatric inpatient unit, a late-life depression clinic, primary care, and community advertisements. The presence of SA history was verified by a psychiatrist (AYD or KS) who used all available information. The participants with significant discrepancies between the SA-related information in their self-reports, medical records, and collateral information were excluded from the study. The Beck Lethality Scale (BLS) (Beck et al., 1975) was used to determine the medical seriousness of SAs. If a participant had a history of multiple SAs, the data for their highest lethality attempt was used. Sixty-one of the SA+MDD group had at least one high-lethality SA, defined as the BLS score of 4 or greater. The SI+MDD group had SI with a specific plan but no SA history. The MDD group included the participants with no lifetime history of any suicidal or nonsuicidal self-harming thoughts or behaviors. This history was established through clinical interviews, medical record reviews, and Structured Clinical Interview for DSM-IV Axis I Disorders. The Controls had no lifetime history of any SCID-I psychiatric diagnoses. At the time of the study enrollment, all three MDD groups had a SCID-I lifetime diagnosis of unipolar nonpsychotic MDD and a score of 14 or higher on the HRSD. Details are presented in Table 2A.
Table 2A.
Characteristics of Sample 1.
| Controls (n=66) | MDD (n=66) | MDD+SI (n=76) | MDD+LL SA (n=55) |
MDD+HL SA (n=61) |
p | |
|---|---|---|---|---|---|---|
| Age (M, SD) | 69.92 (10.34) | 67.94 (8.56) | 62.75 (8.34) | 62.75 (7.11) | 64.67 (8.18) | <.001 |
| Female (n, %) | 35 (53.0%) | 40 (60.6%) | 33 (43.4%) | 36 (65.6%) | 31 (50.8%) | .101 |
| Caucasian (n, %) | 56 (84.8%) | 55 (83.3%) | 64 (84.2%) | 45 (81.8%) | 57 (93.4%) | .396 |
| Education Years (M, SD) | 15.17 (2.92) | 14.56 (2.78) | 14.84 (2.50) | 13.87 (2.70) | 13.89 (3.37) | .043 |
| Income (Median) | $50,000 to $74,999 | $35,000 to $49,999 | $25,000 to $34,999 | $25,000 to $34,999 | $35,000 to $49,999 | <.001 |
| Substance Use History (n, %) | N/A | 20 (30.3%) | 35 (46.1%) | 33 (60.0%) | 27 (44.3%) | <.001 |
| Any Anxiety History (n, %) | 1a (1.5%) | 39 (59.1%) | 53 (69.7) | 45 (81.8%) | 38 (62.3%) | <.001 |
| MMSE (M, SD) | 27.94 (2.31) | 28.17 (1.78) | 27.77 (2.36) | 27.26 (2.22) | 27.24 (2.23) | .073 |
| Highest Lethality of SA (M, SD) | N/A | N/A | N/A | 2.04 (1.12) | 5.21 (1.28) | <.001 |
Notes.
Participant met diagnostic criteria for Specific Phobia, which was not an exclusion diagnosis for the Controls group. MDD = major depressive disorder. SI = suicidal ideation. SA = suicide attempt. LL = low lethality. HL = high lethality. MMSE = Mini Mental Status Exam
Sample 2 (Neurocognitive Markers of Vulnerability to Suicide Across Life-Cycle study; Pittsburgh, PA).
This sample included 118 participants aged 22-80 (Mage = 59.10, SD = 12.12; 56.20% female) and comprised three groups: 41 participants with a history of suicide attempt and MDD (SA+MDD), 38 participants with MDD (with or without an SI; MDD), and 39 healthy controls (Controls). The SA group was further split into high-lethality (HL SA+MDD) and low-lethality (LL SA+MDD) subgroups. A total of 17 participants in this sample had at least one high-lethality SA. The criteria and procedures used to verify suicide attempt status, ideation severity, suicide intent, medical severity of the attempt, and clinical diagnoses were similar to those in Sample 1. The procedures were approved by the University of Pittsburgh Institutional Review Board (PRO14080281). Recruitment efforts took place via a psychogeriatric inpatient unit, a late-life depression clinic, primary care, and community advertisements. Details are presented in Table 2B.
Table 2B.
Characteristics of Sample 2.
| Controls (n=39) | MDD (n=38) | MDD+LL SA (n=24) |
MDD+HL SA (n=17) |
p | |
|---|---|---|---|---|---|
| Age (M, SD) | 64.21 (9.31) | 60.92 (9.09) | 53.96 (15.58) | 51.18 (12.75) | <.001 |
| Female (n, %) | 26 (66.7%) | 19 (50.0%) | 14 (58.3%) | 7 (41.2%) | .270 |
| Caucasian (n, %) | 36 (92.3%) | 29 (76.3%) | 16 (66.7%) | 15 (88.2%) | .053 |
| Education Years (M, SD) | 15.90 (2.46) | 15.55 (2.58) | 14.17 (2.06) | 14.88 (2.47) | .041 |
| Income (Median) | $50,000 to $74,999 | $25,000 to $34,999 | $25,000 to $34,999 | $25,000 to $34,999 | <.001 |
| Substance Use History (n, %) | N/A | 16 (42.1%) | 12 (50.0%) | 7 (41.2%) | <.001 |
| Any Anxiety History (n, %) | N/A | 14 (36.8%) | 16 (66.7%) | 8 (47.1%) | <.001 |
| MMSE (M, SD) | 29.39 (.86) | 28.76 (.97) | 28.46 (1.38) | 28.88 (1.22) | .007 |
| Highest Lethality of SA (M, SD) | N/A | N/A | 1.75 (1.11) | 6.00 (1.12) | <.001 |
Notes. MDD = major depressive disorder. SI = suicidal ideation. SA = suicide attempt. LL = low lethality. HL = high lethality. MMSE = Mini Mental Status Exam
Sample 3 (Neurocognitive Markers of Vulnerability to Suicide Across Life-Cycle study; Columbus, OH; New York, NY).
This sample combined the participants from two recruitment sites to enable more stable model estimation. It included 180 participants aged 16-74 (Mage = 33.11, SD = 13.00; 66.84% female) and comprised three groups: 64 participants with a history of suicide attempt and MDD (SA+MDD), 57 participants with MDD (with or without an SI; MDD), and 59 healthy controls (Controls). The SA group was further split into high-lethality (HL SA+MDD) and low-lethality (LL SA+MDD) subgroups. A total of 22 participants in this sample had at least one high-lethality SA. The criteria and procedures used to verify suicide attempt status, ideation severity, suicide intent, medical severity of the attempt, and clinical diagnoses were similar to those in Samples 1 and 2. The procedures were approved by the Abigail Wexner Research Institute at Nationwide Children’s Hospital Institutional Review Board or the New York State Psychiatric Institute Institutional Review Board (PRO14080281). Recruitment efforts took place via an adult inpatient unit, a mood disorders clinic, primary care, and community advertisements in both Columbus, OH and New York, NY. Details are presented in Table 2C.
Table 2C.
Characteristics of Sample 3.
| Controls (n=59) | MDD (n=57) | MDD+LL SA (n=42) |
MDD+HL SA (n=22) |
p | |
|---|---|---|---|---|---|
| Age (M, SD) | 34.39 (12.40) | 32.05 (13.43) | 30.81 (12.78) | 36.09 (13.54) | .333 |
| Female (n, %) | 36 (61.0%) | 44 (77.2%) | 28 (66.7%) | 13 (59.1%) | .234 |
| Caucasian (n, %) | 31 (52.5%) | 41 (71.9%) | 17 (40.5%) | 11 (50.0%) | .024 |
| Education Years (M, SD) | 15.57 (2.37) | 14.88 (2.71) | 14.24 (2.30) | 14.23 (2.91) | .040 |
| Income (Median) | $50,000 to $74,999 | $35,000 to $49,999 | $35,000 to $49,999 | $16,000 to $24,999 | .020 |
| Substance Use History (n, %) | N/A | 12 (21.1%) | 14 (33.3%) | 7 (31.8%) | <.001 |
| Any Anxiety History (n, %) | N/A | 42 (73.7%) | 29 (69.0%) | 20 (90.9%) | <.001 |
| MMSE (M, SD) | 29.56 (.82) | 29.40 (.90) | 29.24 (.91) | 29.00 (1.07) | .065 |
| Highest Lethality of SA (M, SD) | N/A | N/A | 1.48 (1.25) | 5.14 (1.32) | <.001 |
Notes. MDD = major depressive disorder. SI = suicidal ideation. SA = suicide attempt. LL = low lethality. HL = high lethality. MMSE = Mini Mental Status Exam
Delay Discounting
Preferences for smaller immediate versus larger delayed rewards were assessed with the Monetary Choice Questionnaire (MCQ) (Kirby et al., 1999), a standard instrument for measuring delay discounting. The MCQ has 27 items asking participants to choose between smaller immediate and larger delayed rewards (e.g., “Would you prefer $25 today, or $60 in 14 days?”). Additional three items had small differences between immediate and delayed rewards to differentiate between the possibility of extremely low discounting (always choosing the later, larger reward) and insensitivity to the attributes of the options. One of the participants’ choices was randomly selected, with the chosen immediate or delayed reward later delivered to the participant via a debit card.
Statistical Analysis
As noted in the Introduction, the two-stage approach to estimating individual discount rates and choice consistencies suffers from several limitations. Specifically, following Kirby, Petry, and Bickel (1999) and assuming hyperbolic discounting (Mazur & Coe, 1987), hyperbolic discount rates at which one is indifferent between the immediate and delayed options for a given prospect or item are calculated as
| (1) |
At stage 1, one’s individual discount rate kindividual most consistent with one’s actual choices is inferred by finding the most probable indifference point , i.e. the most likely point of reversal from delayed choices when to immediate choices when ; when ≥2 values of are equally likely, a geometric mean is taken. At stage 2, point estimates of individual discount rates are entered into analyses of individual differences. Stage 1 also yields an individual estimate of consistency (proportion of choices consistent with the most likely kindividual, but consistency estimates are generally not used in analyses of individual differences. The problem with this approach is that the uncertainty about estimates of kindividual is not propagated from Stage 1 to Stage 2, giving inconsistent subjects undue weight. Further, individual estimates are not regularized by data from the group, yielding unrealistically extreme values in inconsistent subjects. In summary, individual differences in discount rates estimated using two-stage analyses may be partly due to inconsistency. Below, we introduce a method intended to overcome these limitations.
These limitations can be addressed in the multi-level modeling (MLM) framework involving, for delay discounting, logistic regression on item-by-item choices nested within subjects (Young, 2018). Here, we propose and validate a simple regression-based approach to estimating individual differences in discount rates. Assuming hyperbolic discounting, the probability of choosing the delayed reward can be defined as
| (2) |
This choice rule is not easy to adapt for logistic regression. In addition, reward magnitudes and delays are correlated by design in instruments such as Kirby’s MCQ (e.g. r(rewardimmediate,rewarddelayed) = 0.83), and this multi-collinearity complicates estimation and interpretation of coefficients. However, we can infer from equation 1 that value difference is approximately proportional to:
| (3) |
In other words, the more exceeds kindividual, the greater is the value difference favoring the immediate reward. Conveniently, , yielding a linear combination of uncorrelated predictors. The full choice rule adapted for logistic regression is thus:
| (4) |
where β is the individual’s consistency or value sensitivity parameter approximately proportional to Kirby’s consistency and κ is the preference parameter approximately proportional to log (kindividual). This parameterization allows us to estimate valuation consistency (sensitivity) β as the fixed effect of and −βκ, as the subject’s intercept. The logistic sigmoid is a univariate case of the softmax function, and thus β is analogous to the inverse temperature of the softmax choice rule. For the MCQ, assuming a realistic range of , the correlation between the value difference and the log ratio of discount rates is 0.88, approaching 1 near the indifference point, at which the right and left sides of equation 4 are equal by definition and where the most informative choices lie. More importantly for parameter estimation, the correlation between corresponding choice probabilities even before the additional consistency parameter is estimated is 0.93 and approaches 1 once β is added. To ensure that the β and κ parameters accurately recovered true value sensitivities and discount rates of hyperbolic agents, we conducted a simulation study reported below in the results section.
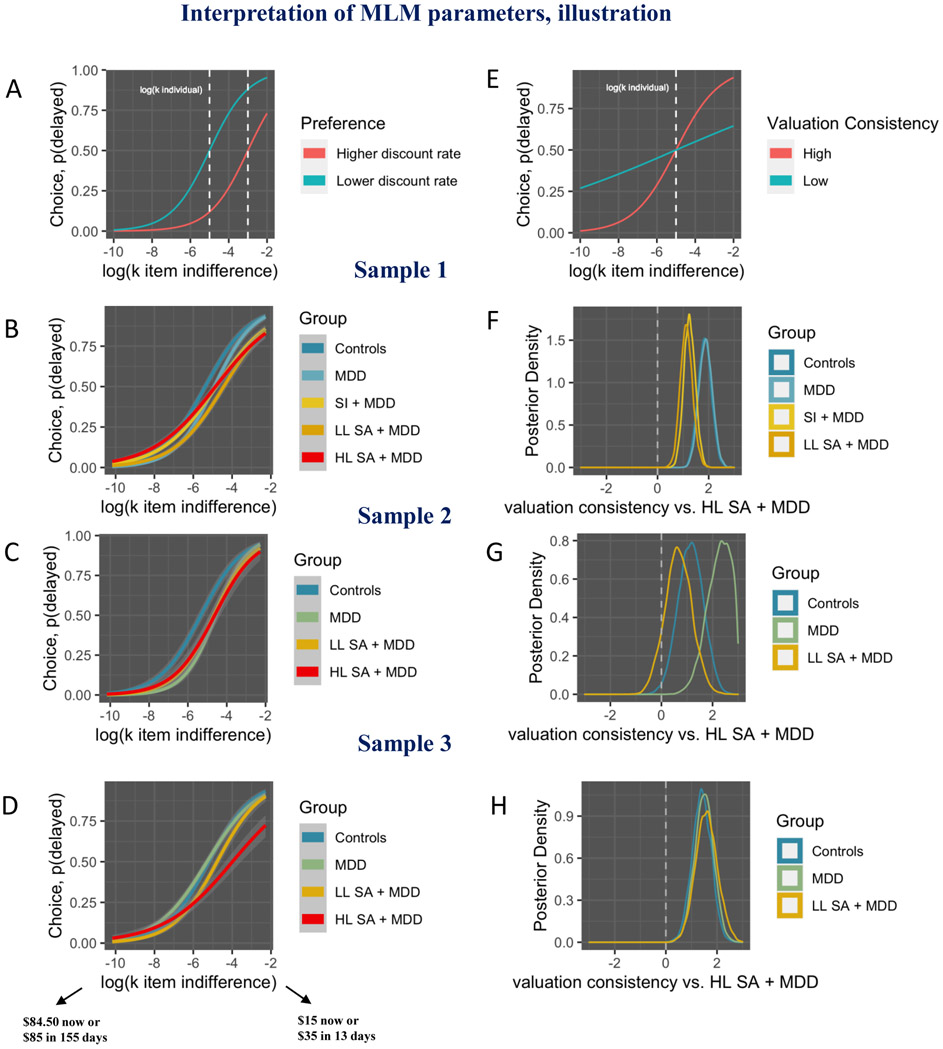
The intuitions behind our method are illustrated in Figure 2. Lower the x-axis correspond to the prospects where only extremely patient individuals choose the delayed option (e.g., $84.50 now or $85 in 155 days), whereas higher values on the x-axis correspond to prospects where even impatient individuals will choose the delayed option (e.g., $15 now or $35 in 13 days). Thus, if the value of a delayed option dominates, implied discount rate is higher. Conversely, if the value of an immediate option dominates, implied discount rate is lower.
Figure 2.
A-E: immediate vs. delayed choice probabilities as a function of item-level discount rates corresponding to the indifference point , log-transformed. Lower on the x-axis correspond to the prospects where only extremely patient individuals choose the delayed option (e.g., $84.50 now or $85 in 155 days), whereas higher values on the x-axis correspond to prospects where even impatient individuals will choose the delayed option (e.g., $15 now or $35 in 13 days). Thus, if the value of a delayed option dominates, implied discount rate is higher. Conversely, if the value of an immediate option dominates, implied discount rate is lower. Probability of choosing the delayed option is on the y-axis (A-E). Psychometric curves for high vs. low MLM preference parameter values, illustration (A). Dashed vertical line illustrates log(kindividual). Psychometric curves (smoothed raw data) sample 1 (B); Psychometric curves (smoothed raw data) sample 2 (C); Psychometric curves (smoothed raw data) sample 3 (D). The inspection of psychometric curves in B-D indicates less consistent valuation (i.e., less steep psychometric curves; conceptually similar to the inverse temperature parameter) in high-lethality suicide attempters, which confirms our multilevel modeling results. Psychometric curves at high versus low valuation consistency, illustration. At high valuation consistency choices are based on the attributes of a given prospect, whereas at low valuation consistency choices are stochastic (E). White dashed vertical lines illustrate log(kindividual).
Posterior parameter distributions from Bayesian multi-level regression models (F-H). Valuation consistency sample 1 (F). Approximate 2-sided ps of all groups, compared to the HL SA + MDD group, are less than 0.001); Valuation consistency sample 2 (G). Approximate 2-sided ps, compared to the HL SA + MDD group: 0.022 in the Controls; less than 0.001 in the MDD group; 0.206 in the LL SA + MDD group; Valuation consistency sample 3 (H). Approximate 2-sided ps of all groups, compared to the HL SA + MDD group, are less than 0.001).
Main Analyses.
We estimated hierarchical logistic regression models using the Bayesian regression R package rstanarm (Goodrich & Gabry, 2020; Muth et al., 2018). This package utilizes Stan through the rstan interface and employs Markov chain Monte Carlo (MCMC) simulation methods to obtain a sample of the posterior distribution of the parameters. Specifically, we used the Hamiltonian Monte Carlo algorithm (Betancourt, 2018) with four chains. We diagnosed chain convergence using the metric and the visual test recommended by Gelman (Gelman et al., 2013). High-lethality suicide attempters were the reference group in all analyses. Fixed effects included , reflecting valuation consistency β of the reference group and the interaction reflecting group differences in valuation consistency. Following equation 4, κ = −intercept/β for each group reflecting that group’s discount rate. Thus, by dividing the main effect of each group (vs. the high-lethality attempters, the reference group) by that group’s β, we estimated the difference in discount rates between groups. We note that this coefficient ratio and its confidence interval could be obtained in the frequentist framework using the delta or Fieller methods (Hirschberg & Lye, 2010), but we employ a precise and easily implemented Bayesian alternative, obtaining the ratio of the samples of the posterior parameter estimates.
Sensitivity Analyses.
Robustness of findings to potential confounds was tested through sensitivity analyses controlling for a) age, sex, race, income, and education; b) global cognitive functioning (assessed via the Mini Mental Status Examination (Folstein et al., 1975); c) possible brain injury from a past suicide attempt; d) comorbid lifetime substance use and/or anxiety. In additional tests of robustness, we also reran the main analyses while excluding all participants who had chosen only immediate or only delayed rewards on the MCQ and those who failed to display monotonic intertemporal preferences.
Results
Model validation: simulation study
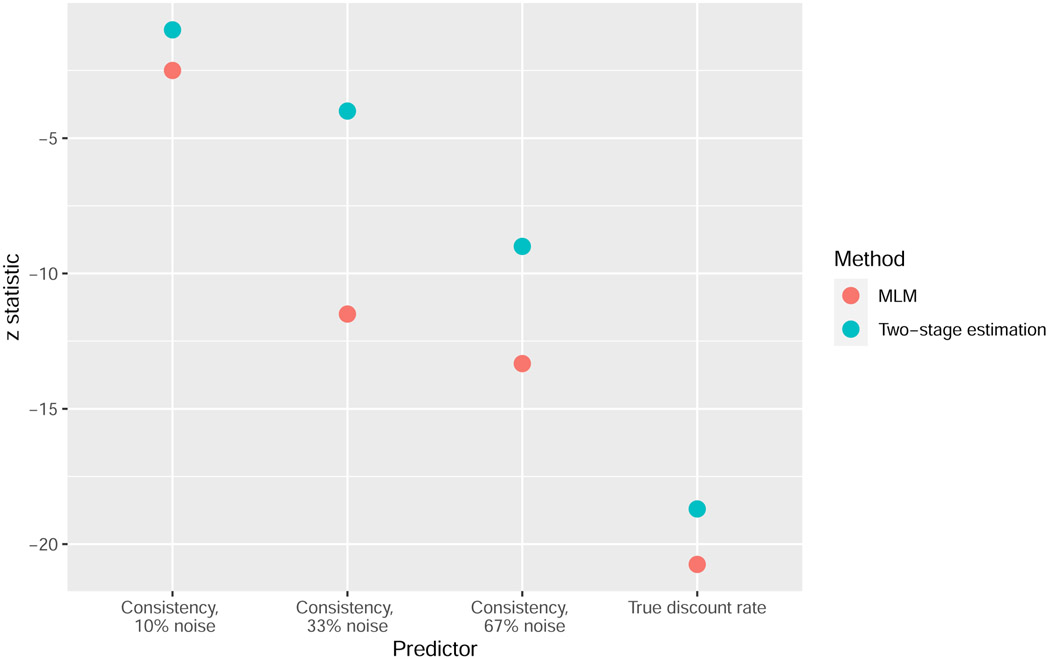
We first validated our multi-level modeling (MLM) approach against a simulated dataset. We compared it with a traditional two-stage approach to estimating subject-level discount rates and choice consistencies (i.e., as described in (Kirby et al., 1999)). We simulated the behavior of 800 pseudo-subjects on the delay discounting task with the true hyperbolic discount rates of - 3.95 (group 1, n = 100) and of −5.64 (group 2, n = 100) with and without the noise injected into the delayed value (noise levels: 0, 0.1, 0.33, 0.67). The two discount rates were based on actual estimated means of the two participant groups from our prior study (i.e., low lethality suicide attempters versus controls; (Dombrovski et al., 2011). To manipulate valuation consistency, we injected noise into delayed, but not immediate option, values since only the computation of delayed option values is cognitively demanding. We then recovered between-group differences in true hyperbolic discount rates and levels of noise via the MLM and using two-stage estimation method (Kirby et al., 1999) and compared the test statistics generated through this recovery. For comparison purposes, mean coefficients from these models were converted into z statistics through division by corresponding standard deviations. As evidenced by greater z values in Figure 1, the MLM method was overall better at recovering between-group differences in “true” hyperbolic discount mean rates and different levels of noise than the two-stage estimation method.
Figure 1.
Comparison of the MLM versus Two-stage estimation approaches towards recovering between-group differences in hyperbolic discount mean rates (True discount rate) and consistency at different levels of noise. Negative z values indicate that (1) the reference group had a higher true hyperbolic discount rate than the group of interest and (2) estimated consistency decreases with increasing noise.
Main Analyses
Our multi-level models aimed to test two competing hypotheses: true preference for smaller immediate rewards versus inconsistent valuation in suicide attempters. With regard to the preference hypothesis, high-lethality suicide attempters displayed a weaker preference for immediate versus delayed rewards only compared to low-lethality suicide attempters and only in Sample 1. Specifically, in this analysis, the effect of prefer now had a probability of 99.10% [pd] of being positive (Median = 0.34, 89% CI[0.10, 0.56], 2-sided p value ≈ 0.02). In contrast, providing stronger support for the inconsistent valuation hypothesis, high-lethality suicide attempters exhibited significantly less consistent valuation than all other comparison groups in Samples 1 and 3. Further, in Sample 2, high-lethality suicide attempters exhibited significantly less consistent valuation than the healthy controls or participants with MDD. Details are presented in Tables 3A-C and Figure 2.
Table 3A.
Preference and Valuation Consistency Sample 1.
| Parameter | Median | 89% CI | pd | ≈ 2-sided p |
|---|---|---|---|---|
| β HL SA+MDD | 2.670*** | [2.458, 2.871] | 1.000 | 0 |
| β Controls (vs. HL SA+MDD) | 1.842*** | [1.415, 2.250] | 1.000 | 0 |
| β MDD (vs. HL SA+MDD) | 1.881*** | [1.474, 2.303] | 1.000 | 0 |
| β SI+MDD (vs. HL SA+MDD) | 1.247*** | [0.892, 1.605] | 1.000 | 0 |
| β LL SA+MDD (vs. HL SA+MDD) | 1.125*** | [0.755, 1.517] | 1.000 | 0 |
| ksubject Controls | 0.015 | [−0, 172, 0.213] | 0.551 | 0.898 |
| ksubject MDD | 0.211 | [0.021, 0.397] | 0.968 | 0.064 |
| ksubject SI+MDD | 0.177 | [−0.036, 0.385] | 0.910 | 0.18 |
| ksubject LL SA+MDD | 0.336* | [0.099, 0.558] | 0.991 | 0.018 |
Note: ksubject: subject-level discount rate (calculated as −group intercept/group β); β: valuation consistency.
p<.05
p<0.01
p<0.001 (two-sided p-value of respectively .05, .01 and .001 corresponds approximately to a pd of 97.5%, 99.5% and 99.95%). Dependent variable: Choice (now versus later). MDD = major depressive disorder. SI = suicidal ideation. SA = suicide attempt. LL = low lethality. HL = high lethality.
Table 3C.
Preference and Valuation Consistency Sample 3.
| Parameter | Median | 89% CI | pd | ≈ 2-sided p |
|---|---|---|---|---|
| β HL SA+MDD | 3.764*** | [3.202, 4.365] | 1.000 | 0 |
| β Controls (vs. HL SA+MDD) | 1.400*** | [0.756, 1.943] | 1.000 | 0 |
| β MDD (vs. HL SA+MDD) | 1.497*** | [0.867, 2.061] | 1.000 | 0 |
| β LL SA+MDD (vs. HL SA+MDD) | 1.586*** | [0.922, 2.293] | 1.000 | 0 |
| β Site Code | −0.805** | [−1.272, −0.331] | 0.997 | 0.006 |
| ksubject Controls | −0.156 | [−0.414, 0.105] | 0.828 | 0.344 |
| ksubject MDD | −0.161 | [−0.398, 0.106] | 0.836 | 0.328 |
| ksubject LL SA+MDD | −0.012 | [−0.267, 0.266] | 0.529 | 0.942 |
Note: ksubject: subject-level discount rate (calculated as −group intercept/group β); β: valuation consistency.
p<.05
p<0.01
p<0.001 (two-sided p-value of respectively .05, .01 and .001 corresponds approximately to a pd of 97.5%, 99.5% and 99.95%). Dependent variable: Choice (now versus later). MDD = major depressive disorder. SI = suicidal ideation. SA = suicide attempt. LL = low lethality. HL = high lethality.
Sensitivity Analyses
Less consistent valuation in high-lethality suicide attempters was not better explained by potential confounds (age, sex, race, income, and education; global cognitive functioning; possible brain injury from a past suicide attempt; history of substance use and/or anxiety; Tables S1-S10). We also ensured that our results are not driven by a handful of unmotivated or poorly performing participants: when excluding all participants who had failed to exhibit monotonic intertemporal preferences or had chosen only immediate or only delayed rewards, high-lethality suicide attempters continued to exhibit less consistent valuation compared to other groups (Tables S11-S13). Further, Tables S14-S16 report the analyses examining whether value sensitivity in suicide attempters varies depending on the degree of attempt planning of their highest lethality suicide attempt. Planning did not have a replicable association with the discounting rate. Further, for completeness, we report subject-level discount rates and consistencies from the traditional two-stage analysis in Table S17. Finally, we present raw task behavior data from all study participants in Figures S1-S3 demonstrating the fit of the logistic sigmoid on hyperbolic value difference to actual choices.
Discussion
We hypothesized that altered intertemporal choice patterns in attempted suicide were due to a failure to consistently integrate the attributes of a prospect (inconsistent valuation), rather than a true preference for immediate over delayed rewards. Indeed, in three samples, the choices of high-lethality suicide attempters were the least sensitive to the overall values of prospects. The relationship between inconsistent valuation and severity of suicidal behavior in three samples and its robustness to confounds such as global cognitive functioning and comorbidities argue for a specific role of this deficit in suicidal behavior.
High discount rates are commonly viewed as a transdiagnostic feature of decision-making in impulsivity and externalizing psychopathology (meta-analysis: Amlung et al., 2019). In counterpoint to this view, our findings suggest that inconsistent valuation rather than a true preference for immediate gratification is part of vulnerability to suicidal behavior. We are not alone in arguing that valuation consistency is a clinically relevant component of decision competence: it has been found to correlate with intelligence (Ripke et al., 2015) and predict relapse in smokers (Grosskopf et al., 2021). Crucially, while earlier observational studies argued that high discount rates reflect cognitive control deficits (meta-analysis: Wesley & Bickel, 2014), recent experimental work indicates that consistency and not discount rate is selectively affected by working memory load (Olschewski, 2018), in line with our finding that consistency scaled with global cognitive function. Our results generally agree with prior findings of suicide attempters (i) performing poorly on gambling tasks requiring one to integrate choice attributes such as magnitude and/or probability into a single value estimate (meta-analysis: Perrain et al., 2021) and (ii) displaying valuation deficits on learning tasks (Dombrovski et al., 2019). What mechanisms may explain inconsistent valuation in people at high risk for suicide? One hypothesis is that it is due to disrupted value comparison in the ventromedial prefrontal cortex (vmPFC) - ventral striatum (VS) paralimbic circuit during intertemporal choice (Kable & Glimcher, 2007, 2010; Lempert et al., 2019), and value-based decision-making in general (Glascher et al., 2012). We have some evidence of disrupted vmPFC value signals in attempted suicide and their association with impulsivity and value-inconsistent choices on a gambling task (Brown et al., 2020; Clark et al., 2011; Dombrovski et al., 2013). Yet, several observations lead us to implicate impaired cognitive control processes in the lateral frontoparietal (LFP) network rather than the vmPFC-VS in inconsistent valuation. The LFP, comprised of the dorsolateral prefrontal (dlPFC) and posterior parietal (PPC) cortices, is recruited during delay discounting, particularly for difficult choices near the indifference point (Laird et al., 2011; McClure et al., 2004; Monterosso et al., 2007; Vanyukov et al., 2016), consistent with the finding that the integration of attributes required for consistent choices is working memory-dependent (Olschewski, 2018). LFP activity mediates the relationship between intelligence and consistency, while vmPFC-VS activity mediates the relationship between intelligence and discount rate (Ripke et al., 2015). Furthermore, we have previously found diminished dlPFC responses to the decreasing value difference favoring larger delayed reward in suicide attempters (Vanyukov et al., 2016). In summary, extant data provide indirect support for the hypothesis that disruptions in LFP cognitive control processes underlie inconsistent valuation in attempted suicide, although neural studies are needed to test this hypothesis directly.
What does the finding of inconsistent valuation tell us about real-life decision-making during a suicidal crisis? A decision to attempt suicide reflects a comparison of values of the options available at different time points. Any choice, including that between suicide versus alternative solutions, involves a process of drifting toward or away from an option depending on the perceived values of these options until a decision threshold is reached (Ratcliff et al., 2016; Ratcliff & McKoon, 2008). The escape account of suicide (Baumeister, 1990) highlights exaggerated and rigid focus on the present aversive state at the expense of one’s personal future during a crisis. During those times, the value of suicide as an option may become misestimated, or may fluctuate wildly. Our findings suggest that it is the noisy (rather than strategic) decision-making that may promote the option of suicide as a solution over the otherwise more rational alternatives. Specifically, failure to consistently integrate the choice attributes uncovered in the present study undermines the consideration of deterrents (e.g., the effects of one’s suicide attempt on family members) and the benefits of alternative solutions. Recent studies using Ecological Momentary Assessment suggest that suicidal thinking not only varies dramatically across and sometimes within a day (Gratch et al., 2021) but that variability is associated with risk for later attempt (Wang et al., 2021). Thus, our findings might help to explain the ultimate decision to attempt suicide (escape) in lieu of other available options such as active problem-solving, getting help, and waiting out the crisis.
The strengths of our study include replication in three clinical samples of different ages, sensitivity analyses to rule out potential confounding variables, and the use of multi-level modeling to capture the stochasticity of individual choices. Careful characterization of suicidal behavior enabled us to examine how the identified deficits were most pronounced in high-lethality suicide attempters. Overall, our findings highlight the importance of considering both consistency and discount rates when describing individual differences in delay discounting and demonstrate the power of multi-level models in estimating these parameters. The main limitation of the present study was its cross-sectional nature, which limits causal inferences. In addition, the lack of response time data precluded us from testing decision process models, such as diffusion decision models. Finally, because the goal of our study was to provide a more robust analysis of intertemporal choice assuming hyperbolic discounting, we do not make any claims about its applicability to alternative discount functions.
Clinically, these findings suggest that interventions that take place during the moments of suicidal ambivalence (i.e., when the values of suicide versus alternative options are close to each other and the individuals drift toward or away from these competing options in order to make a decision) and focus specifically on enhancing deterrents, reinforcing alternative solutions, and deferring the final decision can be particularly effective for suicide prevention. This approach is consistent with a recent call for targeted, individualized (with regard to timing, type, and intensity) interventions for suicide risk (Just-In-Time Adaptive Interventions (Coppersmith et al., 2021). Psychoeducation for patients and family members about impairments in decision competence, such as inconsistent valuation, could also help recruit support and develop compensatory strategies. During such psychoeducation, it is important to convey that decision-making deficits are neurocognitive symptoms rather than character flaws. In our view, compensatory interventions are more likely to succeed than efforts to remediate decision deficits, particularly those resulting from frontoparietal dysfunction. This assertion is corroborated by empirical evidence that the effects of working memory training, for example, are small and do not generalize to other tasks (Soveri et al., 2017) and are thus unlikely to be of significant benefit during real-life crises. In summary, our findings support the decision accident account of suicidal behavior, extending the literature on the neurocognitive diathesis.
Supplementary Material
Table 3B.
Preference and Valuation Consistency Sample 2.
| Parameter | Median | 89% CI | pd | ≈ 2-sided p |
|---|---|---|---|---|
| β HL SA+MDD | 3.907*** | [3.332, 4.530] | 1.000 | 0 |
| β Controls (vs. HL SA+MDD) | 1.147* | [0.382, 1.958] | 0.989 | 0.022 |
| β MDD (vs. HL SA+MDD) | 2.425*** | [1.514, 3.436] | 1.000 | 0 |
| β SA+MDD (vs. HL SA+MDD) | 0.663 | [−0.161, 1.536] | 0.897 | 0.206 |
| ksubject Controls | −0.157 | [−0.446, 0.087] | 0.834 | 0.332 |
| ksubject MDD | 0.254 | [0.031, 0.454] | 0.969 | 0.062 |
| ksubject LL SA+MDD | 0.035 | [−0.290, 0.356] | 0.565 | 0.87 |
Note: ksubject: subject-level discount rate (calculated as −group intercept/group β); β: valuation consistency.
p<.05
p<0.01
p<0.001 (two-sided p-value of respectively .05, .01 and .001 corresponds approximately to a pd of 97.5%, 99.5% and 99.95%). Dependent variable: Choice (now versus later). MDD = major depressive disorder. SI = suicidal ideation. SA = suicide attempt. LL = low lethality. HL = high lethality.
Acknowledgments
The project was supported by the following NIH funding: R01MH100095, R01MH048463, R01MH085651, T32MH019986, T32MH018269.
A pre-print of the manuscript has been posted on PsyArXiv: 10.31234/osf.io/tfp4d. Study procedures were approved by the University of Pittsburgh Institutional Review Board (PRO14050627; PRO14080281) for samples 1 and 2 and by the Abigail Wexner Research Institute at Nationwide Children’s Hospital Institutional Review Board or the New York State Psychiatric Institute Institutional Review Board (PRO14080281) for sample 3.
References
- Allen KJD, Bozzay ML, & Edenbaum ER (2019). Neurocognition and Suicide Risk in Adults. Current Behavioral Neuroscience Reports, 6(4), 151–165. 10.1007/s40473-019-00189-y [DOI] [Google Scholar]
- Amlung M, Marsden E, Holshausen K, Morris V, Patel H, Vedelago L, Naish KR, Reed DD, & McCabe RE (2019). Delay Discounting as a Transdiagnostic Process in Psychiatric Disorders. JAMA Psychiatry. 10.1001/jamapsychiatry.2019.2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF (1990). Suicide as escape from self. Psychological Review, 97(1), 90–113. 10.1037/0033-295X.97.1.90 [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck R, & Kovacs M (1975). Classification of suicidal behaviors: I. Quantifying intent and medical lethality. In The American Journal of Psychiatry (Vol. 132, Issue 3, pp. 285–287). American Psychiatric Assn. 10.1176/ajp.132.3.285 [DOI] [PubMed] [Google Scholar]
- Beskow J, Thorson J, & Öström M (1994). National suicide prevention programme and railway suicide. Social Science & Medicine, 38(3), 447–451. 10.1016/0277-9536(94)90446-4 [DOI] [PubMed] [Google Scholar]
- Betancourt M (2018). A Conceptual Introduction to Hamiltonian Monte Carlo. ArXiv:1701.02434 [Stat]. http://arxiv.org/abs/1701.02434 [Google Scholar]
- Bickel WK, Yi R, Landes RD, Hill PF, & Baxter C (2011). Remember the future: Working memory training decreases delay discounting among stimulant addicts. Biological Psychiatry, 69(3), 260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredemeier K, & Miller IW (2015). Executive function and suicidality: A systematic qualitative review. Clinical Psychology Review, 40, 170–183. 10.1016/j.cpr.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge JA, Reynolds B, McBee-Strayer SM, Sheftall AH, Ackerman J, Stevens J, Mendoza K, Campo JV, & Brent DA (2015). Impulsive Aggression, Delay Discounting, and Adolescent Suicide Attempts: Effects of Current Psychotropic Medication Use and Family History of Suicidal Behavior. Journal of Child and Adolescent Psychopharmacology, 25(2), 114–123. 10.1089/cap.2014.0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown VM, Wilson J, Hallquist MN, Szanto K, & Dombrovski AY (2020). Ventromedial prefrontal value signals and functional connectivity during decision-making in suicidal behavior and impulsivity making in suicidal behavior and impulsivity. Neuropsychopharmacology, 0–1. 10.1038/s41386-020-0632-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha CB, Wilson KM, Tezanos KM, DiVasto KA, & Tolchin GK (2019). Cognition and self-injurious thoughts and behaviors: A systematic review of longitudinal studies. Clinical Psychology Review, 69, 97–111. 10.1016/j.cpr.2018.07.002 [DOI] [PubMed] [Google Scholar]
- Clark L, Dombrovski AY, Siegle GJ, Butters MA, Shollenberger CL, Sahakian BJ, & Szanto K (2011). Impairment in Risk-Sensitive Decision-Making in Older Suicide Attempters With Depression. Psychology and Aging, 26(2), 321–330. 10.1037/a0021646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppersmith DDL, Dempsey W, Kleiman E, Bentley K, Murphy S, & Nock M (2021). Just-in-Time Adaptive Interventions for Suicide Prevention: Promise, Challenges, and Future Directions. PsyArXiv. 10.31234/osf.io/eg9fx [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Hallquist MN, Brown VM, Wilson J, & Szanto K (2019). Value-Based Choice, Contingency Learning, and Suicidal Behavior in Mid- and Late-Life Depression. Biological Psychiatry, 85(6), 506–516. 10.1016/j.biopsych.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Clark L, Reynolds CF, & Siegle GJ (2013). Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry, 70(10), 1020–1030. 10.1001/jamapsychiatry.2013.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Siegle GJ, Wallace ML, Forman SD, Sahakian B, Reynolds CF, & Clark L (2011). Lethal forethought: Delayed reward discounting differentiates high- and low-lethality suicide attempts in old age. Biological Psychiatry, 70(2), 138–144. 10.1016/j.biopsych.2010.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh-richard DM, N, K., Dawes M. a, Hatzis ES, Palmes G, Nouvion SO, Sciences H, Rose AJ, & Rudolph KD (2011). NIH Public Access. Psychiatry: Interpersonal and Biological Processes, 132(1), 98–131. 10.1016/j.psychres.2008.06.011.Impulsivity [DOI] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. 10.3744/snak.2003.40.2.021 [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, & Rubin DB (2013). Bayesian Data Analysis, Third Edition. CRC Press. [Google Scholar]
- Gläscher J, Adolphs R, Damasio H, Bechara A, Rudrauf D, Calamia M, Paul LK, & Tranel D (2012). Lesion mapping of cognitive control and value-based decision making in the prefrontal cortex. Proceedings of the National Academy of Sciences, 109(36), 14681–14686. 10.1073/pnas.1206608109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodrich B, & Gabry J (2020). Rstanarm: Bayesian applied regression modeling via Stan. R package version 2.21.1. http://mc-stan.org/rstanarm/authors.html [Google Scholar]
- Gratch I, Choo T-H, Galfalvy H, Keilp JG, Itzhaky L, Mann JJ, Oquendo MA, & Stanley B (2021). Detecting suicidal thoughts: The power of ecological momentary assessment. Depression and Anxiety, 38(1), 8–16. 10.1002/da.23043 [DOI] [PubMed] [Google Scholar]
- Grosskopf CM, Kroemer NB, Pooseh S, Böhme F, & Smolka MN (2021). Temporal discounting and smoking cessation: Choice consistency predicts nicotine abstinence in treatment-seeking smokers. Psychopharmacology, 238(2), 399–410. 10.1007/s00213-020-05688-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gujral S, Butters MA, Dombrovski AY, & Szanto K (2020). Late-Onset Suicide: A Dementia Prodrome? The American Journal of Geriatric Psychiatry. 10.1016/j.jagp.2020.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gujral S, Dombrovski AY, Butters M, Clark L, Reynolds CF, & Szanto K (2014). Impaired Executive Function in Contemplated and Attempted Suicide in Late Life. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 22(8), 811–819. 10.1016/j.jagp.2013.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschberg J, & Lye J (2010). A Geometric Comparison of the Delta and Fieller Confidence Intervals. The American Statistician, 64(3), 234–241. 10.1198/tast.2010.08130 [DOI] [Google Scholar]
- Kable JW, & Glimcher PW (2007). The neural correlates of subjective value during intertemporal choice. Nature Neuroscience, 10(12), 1625–1633. 10.1038/nn2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kable JW, & Glimcher PW (2010). An “as soon as possible” effect in human intertemporal decision making: Behavioral evidence and neural mechanisms. Journal of Neurophysiology, 103(5), 2513–2531. 10.1152/jn.00177.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, & Bickel WK (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General, 128(1), 78–87. 10.1037/0096-3445.128.1.78 [DOI] [PubMed] [Google Scholar]
- Laird AR, Fox PM, Eickhoff SB, Turner JA, Ray KL, McKay DR, Glahn DC, Beckmann CF, Smith SM, & Fox PT (2011). Behavioral interpretations of intrinsic connectivity networks. Journal of Cognitive Neuroscience, 23(12), 4022–4037. 10.1162/jocn_a_00077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lempert KM, Steinglass JE, Pinto A, Kable JW, & Simpson HB (2019). Can delay discounting deliver on the promise of RDoC? Psychological Medicine, 49(2), 190–199. 10.1017/S0033291718001770 [DOI] [PubMed] [Google Scholar]
- Liu RT, Vassileva J, Gonzalez R, & Martin EM (2012). A comparison of delay discounting among substance abusers. Psychology of Addictive Behaviors, 26(4), 980–985. 10.1037/a0027384.A [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathias CW, Dougherty DM, James LM, Richard DM, Dawes MA, Acheson A, & Hill-Kapturczak N (2011). Intolerance to delayed reward in girls with multiple suicide attempts. Suicide and Life-Threatening Behavior, 41(3), 277–286. 10.1111/j.1943-278X.2011.00027.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazur JE, & Coe D (1987). Tests of Transitivity in Choices Between Fixed and Variable Reinforcer Delays. Journal of the Experimental Analysis of Behavior, 47(3), 287–297. 10.1901/jeab.1987.47-287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure SM, Laibson DI, Loewenstein G, & Cohen JD (2004). Separate neural systems value immediate and delayed monetary rewards. Science, 306(5695), 503–507. 10.1126/science.1100907 [DOI] [PubMed] [Google Scholar]
- Mellis AM, Snider SE, Deshpande HU, LaConte SM, & Bickel WK (2019). Practicing prospection promotes patience: Repeated episodic future thinking cumulatively reduces delay discounting. Drug and Alcohol Dependence, 204, 107507. 10.1016/j.drugalcdep.2019.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner AJ, Lee MD, Hoyt K, Buckholtz JW, Auerbach RP, & Nock MK (2018). Are suicide attempters more impulsive than suicide ideators? General Hospital Psychiatry, April, 0–1. 10.1016/j.genhosppsych.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Monterosso JR, Ainslie G, Xu J, Cordova X, Domier CP, & London ED (2007). Frontoparietal cortical activity of methamphetamine-dependent and comparison subjects performing a delay discounting task. Human Brain Mapping, 28(5), 383–393. 10.1002/hbm.20281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muth C, Oravecz Z, & Gabry J (2018). User-friendly Bayesian regression modeling: A tutorial with rstanarm and shinystan. The Quantitative Methods for Psychology, 14, 99–119. 10.20982/tqmp.14.2.p099 [DOI] [Google Scholar]
- Neuringer C, & Harris RM (1974). The perception of the passage of time among death-involved patients. In Life-Threatening Behavior (Vol. 4, Issue 4, pp. 240–254). Behavioral Publications. [PubMed] [Google Scholar]
- Neuringer C, & Levenson M (1972). Time Perception in Suicidal Individuals. OMEGA - Journal of Death and Dying, 3(3), 181–186. 10.2190/ngcx-hl3w-1gcu-ka76 [DOI] [Google Scholar]
- O’Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, & Silverman MM (1996). Beyond the Tower of Babel: A nomenclature for suicidology. Suicide & Life-Threatening Behavior, 26(3), 237–252. 10.1111/j.1943-278X.1996.tb00609.x [DOI] [PubMed] [Google Scholar]
- Olschewski S (2018). Taxing cognitive capacities reduces choice consistency rather than preference: A model-based test. Journal of Experimental Psychology: General, 147(4), 462. 10.1037/xge0000403 [DOI] [PubMed] [Google Scholar]
- Perrain R, Dardennes R, & Jollant F (2021). Risky decision-making in suicide attempters, and the choice of a violent suicidal means: An updated meta-analysis. Journal of Affective Disorders, 280, 241–249. 10.1016/j.jad.2020.11.052 [DOI] [PubMed] [Google Scholar]
- Peters J, & Buchel C (2010). Episodic future thinking reduces reward delay discounting through an enhancement of prefrontal-mediotemporal interactions. Neuron, 66(1), 138–148. 10.1016/j.neuron.2010.03.026 [DOI] [PubMed] [Google Scholar]
- Ratcliff R, Smith PL, Brown SD, & McKoon G (2016). Diffusion Decision Model: Current Issues and History. Trends in Cognitive Sciences, 20(4), 260–281. 10.1016/j.tics.2016.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratcliff Roger., & McKoon Gail. (2008). Drift Diffusion Decision Model:Theory and data. Neural Computation, 20(4), 873–922. 10.1016/j.biotechadv.2011.08.021.Secreted [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard-Devantoy S, Berlim MT, & Jollant F (2014). A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychological Medicine, 44, 1–11. 10.1017/S0033291713002304 [DOI] [PubMed] [Google Scholar]
- Ripke S, Hübner T, Mennigen E, Müller KU, Li S-C, & Smolka MN (2015). Common Neural Correlates of Intertemporal Choices and Intelligence in Adolescents. Journal of Cognitive Neuroscience, 27(2), 387–399. 10.1162/jocn_a_00698 [DOI] [PubMed] [Google Scholar]
- Saffer BY, & Klonsky ED (2018). Do neurocognitive abilities distinguish suicide attempters from suicide ideators? A systematic review of an emerging research area. Clinical Psychology: Science and Practice, 25(1), e12227. 10.1111/cpsp.12227 [DOI] [Google Scholar]
- Soveri A, Antfolk J, Karlsson L, Salo B, & Laine M (2017). Working memory training revisited: A multi-level meta-analysis of n-back training studies. Psychonomic Bulletin & Review, 24(4), 1077–1096. 10.3758/s13423-016-1217-0 [DOI] [PubMed] [Google Scholar]
- Vanyukov PM, Szanto K, Hallquist MN, Siegle GJ, Reynolds CF, Forman SD, Aizenstein HJ, & Dombrovski AY (2016). Paralimbic and lateral prefrontal encoding of reward value during intertemporal choice in attempted suicide. Psychological Medicine, 46(2), 381–391. 10.1017/S0033291715001890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SB, Coppersmith DDL, Kleiman EM, Bentley KH, Millner AJ, Fortgang R, Mair P, Dempsey W, Huffman JC, & Nock MK (2021). A Pilot Study Using Frequent Inpatient Assessments of Suicidal Thinking to Predict Short-Term Postdischarge Suicidal Behavior. JAMA Network Open, 4(3), e210591. 10.1001/jamanetworkopen.2021.0591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesley MJ, & Bickel WK (2014). Remember the future II: Meta-analyses and functional overlap of working memory and delay discounting. Biological Psychiatry, 75(6), 435–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young ME (2018). Discounting: A practical guide to multilevel analysis of choice data. Journal of the Experimental Analysis of Behavior, 109(2), 293–312. 10.1002/jeab.316 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.