Abstract
Background and Purpose:
Stress contributes to dietary patterns that impede health. Yoga is an integrative stress management approach associated with improved dietary patterns in burgeoning research. Yet, no research has examined change in dietary patterns, body mass index (BMI), and stress during a yoga intervention among stressed adults with poor diet.
Materials and Methods:
Objectively-measured BMI and a battery of self-report questionnaires were collected at 3-month follow-up (NOT 4-month follow-up) during and following a 12-week yoga intervention (N = 78, 71% women, mean BMI = 25.69 kg/m2±4.59) – pre-treatment (T1), mid-treatment (6 weeks; T2), post-treatment (12 weeks; T3), and at 3-month follow-up (24 weeks; T4).
Results:
T1 to T3 fruit and vegetable intake, BMI, and stress significantly declined in the overall sample. Reduction in vegetable intake was no longer significant after accounting for reductions in caloric intake, and reduction in caloric intake remained significant after accounting for reductions in stress.
Conclusion:
Findings may be interpreted as yoga either encouraging or adversely impacting healthy dietary patterns (i.e., minimizing likelihood of future weight gain vs. decreasing vegetable intake and overall caloric intake among individuals who may not need to lose weight, respectively). Continued research is warranted, using causal designs.
Keywords: Diet, gateway effect, stress, yoga
1. Introduction
Fruit and vegetable consumption is independently associated with health through prevention of chronic disease states, reducing inflammation, and promoting wellbeing (1). Widespread deficits in fruit and vegetable intake among adults in the United States (U.S.) are a leading cause of premature mortality (1,2). Research spanning the past two decades suggests that stress may contribute to low fruit and vegetable intake (3,4) as well as dietary preferences for “hyperpalatable” (i.e., high-caloric) foods (5), greater engagement in emotional and comfort-type eating (6), and obesity (5). These eating and dietary preferences may help individuals temporarily cope with the adverse physiological and psychological sequelae of chronic stress. The ‘Comfort Food’ hypothesis and prior research suggests consumption of unhealthy foods may downregulate the hypothalamic–pituitary–adrenal (HPA) axis/sympathetic nervous system (SNS) response to chronic stress (7,8). Substituting healthier coping strategies, such as stress management, exercise, or relaxation training, may interrupt these processes and improve diet/eating behaviors (9–12).
Hatha yoga (henceforth referenced as yoga) is a practice with origins in in ancient Indian philosophy that commonly integrates meditation (dhyana), breathing (pranayama), movement (asana), and relaxation (savasana) in many current international settings (13,14). Yoga may interrupt the effects of stress on poor dietary and eating behaviors. Yoga exerts beneficial and mitigating effects on most of the physiological pathways involved in the HPA/SNS stress response (15) and invokes the relaxation response (16). Indeed, some evidence suggests reductions in stress may improve eating behaviors in yoga practitioners. A recent study in women at risk for obesity-related diseases found heated hatha yoga reduced cortisol reactivity to stress, as well as eating behaviors linked to poor diet (17).
Research moreover associates yoga participation with healthier dietary and eating behaviors. For instance, in the U.S., a population-based cohort study of young adults observed healthier dietary patterns including greater fruit and vegetable intake among yoga practitioners compared to non-practitioners (18), and among adult yoga practitioners, vegetarianism has been indicated up to six times the rate of the general population (19). Similar patterns are consistently observed in other studies with large, nationally-representative samples in the U.S. (20,21) and internationally (22–25). Naturalistic observations of associations between yoga practice and changes in diet over time are less common, although an early retrospective study observed yoga practitioners more likely to consume fruits and vegetables and maintain their weight across four years relative to non-practitioners (26). In the years since, little prospective research has examined the association between yoga practice and changes in dietary patterns, making it difficult to discern whether yoga’s associations with healthy dietary patterns is attributable to factors preceding or extraneous to yoga.
Nascent findings from qualitative and intervention studies support the hypothesis that yoga may improve dietary behaviors over time. Yoga-based interventions with explicit content related to dietary change (e.g., vegetarianism) have observed changes in diet following participation [e.g., 25–27]. However, changes in diet have also been observed during yoga interventions that lack explicit prescription to change dietary behavior, suggesting other mechanisms of action may be implicated. For instance, improved dietary quality was reported by participants in two qualitative studies (30, 32), while a randomized controlled trial comparing yoga to Cognitive-Behavioral Stress Management observed increased fruit and vegetable intake in both groups (31). This finding is consistent with prior work that suggests yoga-related reductions in stress may correspond to improved eating behaviors (17). Indeed, it’s possible that stress reduction during yoga may correspond to increased fruit and vegetable intake.
However, not all research associates yoga with beneficial dietary changes. Pilot research has associated yoga with high rates of orthorexia nervosa (an unhealthy obsession with healthy eating) among Spanish yoga practitioners, particularly among vegetarians (33). Such evidence aligns with pilot findings that increased yoga practice may be associated with greater prevalence of disordered eating behaviors among instructors of body/mind classes and male yoga/Pilates practitioners (34,35). These findings should be understood in the context of the relative emphasis of yoga on mindfulness and embodiment, as mindful yoga has been strongly implicated as protective against poor eating behaviors (36,37). Still, research that examines changes in dietary patterns during yoga would benefit from a nuanced lens that considers the potential for both adaptive as well as maladaptive dietary sequelae related to yoga practice.
In sum, few studies have examined the prospective association between yoga practice and non-prescribed changes in dietary patterns over time, including changes in overall caloric intake. Further, no studies have assessed change in dietary patterns during yoga among stressed adults reporting low intake of fruits/vegetables. Such research is needed to better understand whether yoga may be beneficially or maladaptively associated with dietary changes in this sub-population at heightened risk of chronic diseases.
1.1. The current study
The primary objective of this pilot study was to examine whether participation in a 12-week mindful yoga program was associated with increased fruit/vegetable intake (assessed via dietary screener) among adults reporting low intake levels and a subjective feeling of being “stressed” (38). The secondary objective was to examine whether yoga participation was associated with reductions in Body Mass Index (BMI) and stress. The tertiary objective was to confirm changes in fruit/vegetable intake and examine changes in overall caloric intake using a validated extensive food frequency questionnaire in a subset of participants.
2. Materials and Methods
2.1. Study design
The current study design was a pilot randomized controlled trial (RCT). As a secondary aim reported elsewhere (39), participants were randomized into one of three home practice groups of varied duration. The rationale for this study design was to examine which of three assigned home yoga practice durations would be associated with the greatest improvement in fruit and vegetable intake, perceived stress, and home practice compliance. Using block randomization, participants were randomized with equal allocation ratio into one of three groups in blocks of 6 stratified by gender and site/location (urban and rural). All participants were instructed to practice 6 of 7 days per week, similar to other mindfulness-based interventions (40,41). However, prescribed amounts of home practice varied by randomization group. The high practice group was instructed to practice 40 minutes/day, approximating the duration of home practice typically assigned in other mindfulness-based interventions (40,41). The low practice group was assigned 10 minutes/day (similar to the Headspace app and other popular practice modalities). The “hybrid” or choice group was advised to practice 10 minutes/day three days per week and 40 minutes/day three days per week. As reported elsewhere (39), we hypothesized that the hybrid group would experience greater flexibility and thus report the greatest overall practice minutes and benefit. However, in the present analysis, home practice group assignment did not predict significant differences in examined outcomes – that is, participants in all three groups reported similar changes over time in fruit and vegetable intake, as well as secondary outcomes of BMI and stress reactivity. Thus, the reported analyses collapse across randomization groups, analyzing all participants as one group.
Last, participants were blinded to the primary study objective to examine changes in fruit and vegetable intake, as this may have primed expectancies and confounded our aim to examine implicit (non-prescribed) changes. Instead, participants were informed the primary study outcome was stress. We accounted for participant expectancies by telling participants they would be randomly assigned to either a yoga-based or diet and exercise-based stress management intervention (however, all were allocated to the yoga-based program). Of note, aspects of this study were also published recently in Park and colleagues’ (2020) manuscript, including Time 1 to Time 3 stress reactivity. However, Time 4 was not included in a more sophisticated Linear Mixed Model as done here (42).
2.2. Participants
Participants were recruited via public transit, direct mail, and email advertisements querying, “Feeling stressed?” from two study sites in the Northeastern U.S. – an urban site located at a research hospital in Massachusetts and a rural site located at a large public university in Connecticut. Ads targeted a racially diverse community sample. Participants were required to be 23–67 years of age (elevated stress levels and associated adverse health effects have been reported within this age range) (43,44), to self-report consuming fewer than the 5 servings of fruits and vegetables recommended per day for U.S. adults (38) based on a brief dietary assessment tool for health professionals (45,46), and to self-report feeling “stressed” (yes/no). The lower age threshold was selected to avoid the confound of enrolling undergraduate students who lived in dormitories, and whose food selection choices may have been affected accordingly (47). The higher age threshold was selected based on the yoga intervention and clinical and anecdotal experiences of the interventionists; older adults have different needs and considerations for yoga than do younger populations (48).
All participants were required to be healthy and free from psychiatric or medical conditions known to be associated with altered appetite. All inclusion/exclusion criteria, excepting assessment of psychiatric disorders and BMI, were assessed via web- and study-personnel administered self-report. Exclusion criteria were an exercise regimen of >180 minutes per week (per American College of Sports Medicine guidelines) [49], current diagnosis of psychiatric illness as determined by the Mini-International Neuropsychiatric Interview (MINI) (50) or a prior eating disorder as identified by the Structured Clinical Interview for DSM-IV (SCID) eating disorder module (51), significant previous meditation or yoga experience (defined as ≥12 classes in last 3 years or more than 20 classes in lifetime), medications that altered appetite, and major or chronic medical conditions that would limit the ability to exercise or do yoga, including BMI > 40.
2.3. Procedures
Recruitment initiated April of 2015 with the final follow-up measures collected in October 2016. Screening procedures comprised a web survey, phone screen, and in-person screening appointment where eligible participants provided written informed consent. Final eligibility was determined with the MINI (50), the Eating Disorders module from the SCID (51), and a BMI assessment administered by research assistants trained in procedures for accurate collection of height and weight by graduate students in health psychology and kinesiology (52). Following screening across both sites, 117 volunteers gave informed consent (41 at the rural site), and 84 were randomized (31 at the rural site). The present analysis tests only those participants for whom we have pre-program survey data (N = 78). Participant flow is detailed in Figure 1.
Figure 1.
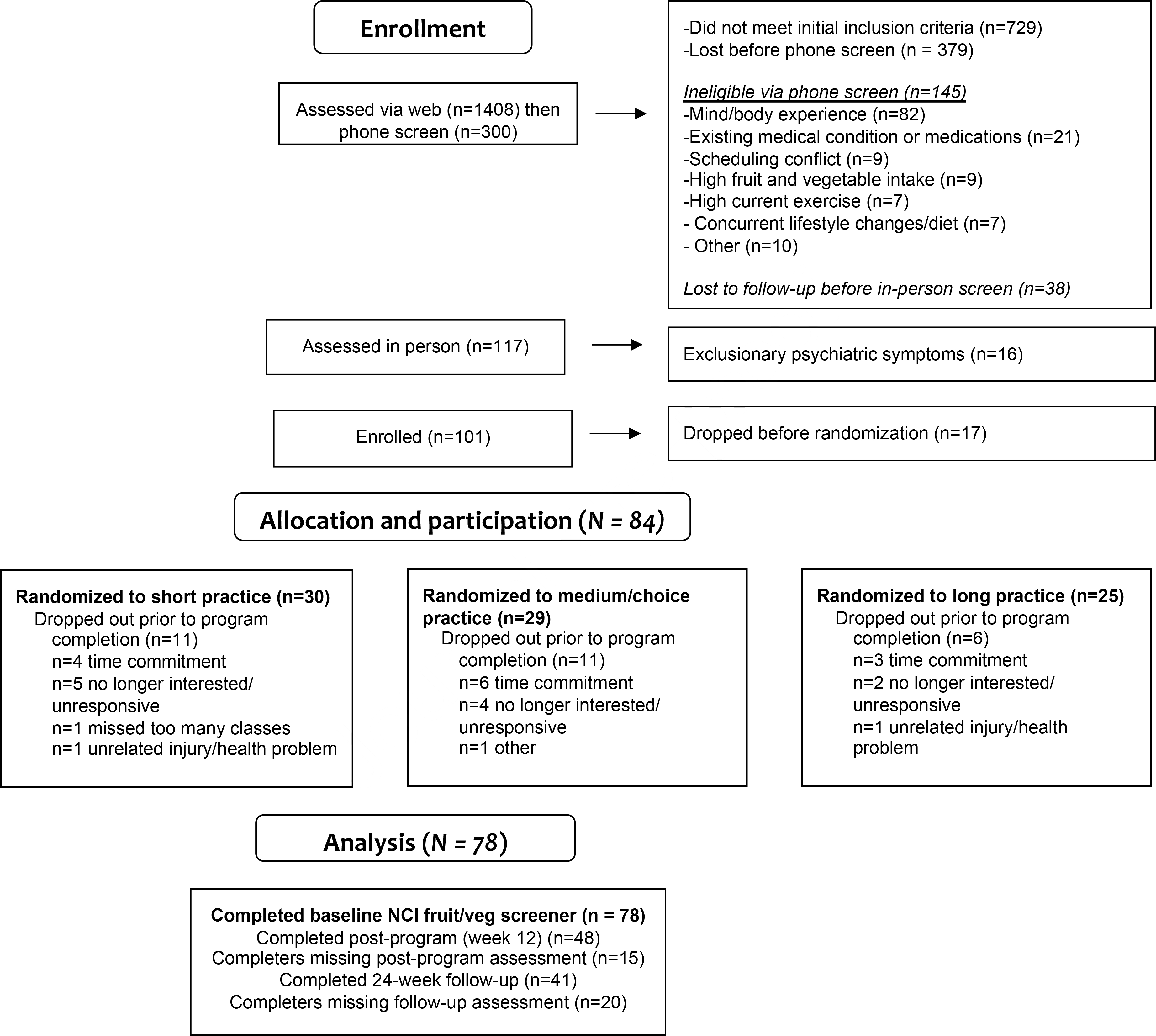
Participant flow (CONSORT diagram); analysis reported for participants collapsed across randomization groups. NCI, National Cancer Institute.
After initial pre-treatment assessment of eligibility (T1), this study included three additional assessment points at 8 weeks (T2; mid-treatment), 12 weeks (T3; post-treatment), and 24 weeks (T4; 3-month follow-up). Data at each time-point were collected via securely-encrypted websites; height and weight were measured on-site to determine BMI. Participants were remunerated up to $100 ($25 per time point) for completing study questionnaires and received the yoga program for free. The study was approved by the Massachusetts General Hospital and University of Connecticut Institutional Review Boards (IRBs).
2.4. Outcome measures
Fruit and Vegetable Screener.
Past-month fruit and vegetable intake was assessed with the National Cancer Institute (NCI) fruit and vegetable screener, a focused assessment listed on the NCI website (53). Scoring algorithms produce a single number of average daily fruit and vegetable intake. This screener has been used in large-scale and intervention studies and has been shown to have reasonable validity (54). This measure was selected as the primary outcome measure for the study.
BMI.
BMI was calculated from height (assessed in stocking feet and measured to the nearest 0.10 cm) and weight (assessed in stocking feet with excessive clothing and materials removed, and measured to the nearest 0.10 kg) with a professional scale (e.g., Health o meter® 597KL, Pelstar, Bridgeville, IL). Follow-up BMI appointments were made at the same time of day to minimize error related to daily fluctuations in weight (52). BMI is weight in kg/height in m2.
Stress.
Stress was assessed with the 7-item stress subscale of the 21-item Depression, Anxiety and Stress Scale (DASS-21) (55). This subscale measures aspects reflective of one’s reactivity under stress (e.g., “I found myself getting agitated”; “I found it hard to wind down”). Items are rated from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time) and summed, then multiplied by 2 to match the full 42-item version. Higher scores indicate higher levels of stress. The DASS has good reliability and validity (55,56). Within this study, Cronbach’s alpha was 0.84.
Food Frequency Questionnaire (FFQ).
Due to limited accuracy in recall related to self-report of diet, it is recommended to use two measures to verify validity of findings (57). The validated Diet History Questionnaire II (DHQ-II) (53,58) was initially administered at both sites to cross-validate findings on prior month’s fruit/vegetable intake in the overall sample, and assess change in caloric intake. However, urban site participants reported the FFQ as a considerable added time burden. Several participants noted they misreported using the skip pattern in order to save time; participants at the rural did not report doing this, nor did they indicate the measure was a time burden upon querying. To ensure validity of study findings and reduce participant burden at the urban site, subsequent study cohorts collected DHQ-II data from the rural site only, and the present analysis reports on rural site participants only. Additional incentives were not provided for completing this measure. The DHQ-II uses national dietary data from the National Health and Nutrition Examination Surveys to generate food list and nutrient/food group database. Reported numbers reflect MyPyramid Equivalents Database (MPED), representing standardized equivalent of total intake servings for a given food group.
2.4. Yoga Intervention
On-site intervention sessions were held in general purpose rooms on a university campus (rural, site one) and at an academic medical center (urban, site two). No mirrors were present. The intervention was modified for use with this population by authors RD and TDB, the latter a certified yoga therapist and both experienced registered yoga teachers with curriculum design experience. Intervention facilitators at both sites were trained, experienced Kripalu yoga instructors, each with over 7 years of teaching experience. There was one lead instructor and one secondary instructor for each site. Instructors were trained in delivery of the yoga protocol by TDB and curriculum co-developer RD, who also served as substitute instructors.
The 12-week Kripalu Yoga intervention comprised two consecutive segments. The first segment was a manualized eight-week intervention designed to serve as an introduction to mindful yoga that was initially created and piloted by the Kripalu Center for Yoga for use in prior research (31,59). The second segment comprised four weeks of 90-minute Kripalu Yoga classes (for intervention structure, see Table 1). In the first segment, each of the eight once-weekly, two-hour sessions initiated with a didactics/discussion on a specific yoga philosophy theme (up to 45 min., including experiential yogic practices). This segment was followed by up to 75 minutes of hatha yoga practice (meditation and breathing exercises [10–15 min.], postures [40–70 min.], and relaxation [8–15 min.]). The second segment initiated the ninth week, and comprised four weeks of 90-minute, once-weekly sessions of hatha yoga practice (no philosophy content). The intervention concluded after twelve weeks and no additional materials were provided between intervention cessation and the follow-up data collection timepoint. A detailed listing of yoga philosophy themes and hatha yoga practices can be viewed in Supplementary Materials.
Table 1.
12-week Kripalu Yoga intervention components, by weekly frequency
| Intervention Component | Week | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| Manualized yoga intervention (1/week, 120 minutes) | x | x | x | x | x | x | x | x | |||||
| Hatha yoga classes (1/week, 90 minutes) | x | x | x | x | |||||||||
| Daily home practice (6 days/week, 10–40 minutes) | x | x | x | x | x | x | x | x | x | x | x | x | |
The trauma-informed Kripalu Yoga intervention integrated yoga practice with yoga philosophy pertinent to self- and affect- regulation to decrease physiological arousal and enhance well-being (60,61). Participants learned how to monitor and modulate momentary mental, emotional, and physiological responses through in-class experiential yoga exercises and practice, and prescribed home yoga training. Yoga philosophy and experiential content included the Kripalu yoga practices of Breathe Relax Feel Watch Allow and Riding the Wave (see Faulds, 2005 for an overview) (61). These mind-body practices share some parallels with the Cognitive-Behavioral Therapy technique, urge surfing (62), and are designed to promote affect regulation and increase distress tolerance. The intervention also taught the principles of witness consciousness (similar to mindfulness) and self-compassion, both cited in Patanjali’s (2003 translation) seminal text, the Yoga Sutras. Sessions emphasized inclusivity of all body shapes and sizes, and adaptations were provided for all postures. Classes emphasized compassionate awareness of present-moment, embodied experience. Because the primary objective of the study was to better understand the effects of yoga on dietary behaviors independent of eating- or weight-related psychoeducation, teachers were explicitly instructed to avoid mention of diet, eating behaviors, body image, or weight loss.
2.5. Statistical Analysis
Data analyses were conducted using SPSS version 25.0. Two-tailed p-values less than 0.05 are considered statistically significant unless otherwise stated. The parent study was conservatively powered (N = 134, accounting for 20% drop-out), based on preliminary data (64). Our enrollment volume fell short and the study was underpowered (N = 78 across both sites with baseline survey data in the present analysis; n = 31 at rural site examining our tertiary objective on food frequency questionnaire, FFQ). All outcome/response variables were positively skewed and log-transformed to approximate normality (65). Primary analyses comprised random intercept linear mixed models (LMM), which uses maximum likelihood methods of parameter estimation, and does not require complete cases assuming the data is missing at random (66). Time was examined as a continuous or categorical predictor and selected as categorical based on graphical examination and AIC/BIC evaluation. Compound symmetry was determined an optimal correlation structure model based on AIC/BIC evaluation. To test whether the yoga intervention improved outcomes within the LMM, baseline (T1) and post-program scores were contrasted (T3), and additional changes at follow-up (T4) were tested by contrasting T3 and T4 scores. Bonferroni adjustments account for multiple contrasts.
Gender and site were included as a covariate in all models for study objectives one and two, as the randomization procedure in the larger study stratified participants by these constructs. Age was also included as a covariate given evidence it may differ by diet, BMI, and stress (67,68). For the tertiary sub-analysis at the rural site (FFQ), age and gender were included as covariates. Last, to probe results further, exploratory analyses were repeated of change in (a) fruit and vegetable intake, adjusting for between- and within-subject changes in calorie intake, (b) caloric intake, adjusting for between- and within-subject changes in stress.
3. Results
3.1. Recruitment and retention
A total of 84 participants were randomized and agreed to proceed with study participation. Of these, the 78 who completed baseline surveys comprise the present analysis. Those attending fewer than 5 intervention sessions (our a priori criterion for having completed the intervention) evidenced no significant variance on baseline demographics or outcome metrics relative to intervention completers (p > .05). No other differences in baseline variables or change scores over time were observed between assessment completers and non-completers at any timepoint (p > .05). Information on study attrition and completion rates are detailed in Figure 1.
3.2. Sample characteristics
Seventy-eight participants (70.5% female, 64.1% White, 87.2% Non-Hispanic) in the overall sample had a mean age of 39.71 (standard deviation [S.D.] = 0.18) and mean (M.) BMI of 25.69 kg/m2 (S.D. = 4.59). At the rural site analyzed for our tertiary objective, thirty-one participants (80.6% female, 77.4% White, 87.1% non-Hispanic) had a mean age of 41.77 (S.D. = 13.78) and mean BMI of 25.55 kg/m2 (S.D. = 5.38).
3.3. Adverse events.
Four adverse events were reported outside of the yoga class setting, three physical (two serious and one not serious), and one psychological. All were determined by the IRB to be unanticipated and unrelated to the research study.
3.4. Study outcomes
Results for contrasts on significant covariates are described in-text. All significant findings held after adjusting for multiple comparisons.
Changes in fruit and vegetable intake (primary objective) and BMI and stress (secondary objective).
Descriptive statistics at each time-point are displayed in Table 2 (for primary and secondary outcomes); Table 3 displays effects of time, covariates, and contrasts of changes from T1 to T3, and T3 to T4 within the linear mixed model, by study outcome.
Table 2.
IQR and medians for NCI dietary screener outcomes (fruit/vegetable intake) and means and SD for BMI and stress, at each time-point in the overall sample. Raw, untransformed data reported for NCI constructs.
| Outcome | T1 |
T2 |
T3 |
T4 |
||||
| IQR (Median) | n | IQR (Median) | n | IQR (Median) | n | IQR (Median) | n | |
|
|
|
|
|
|
||||
| Fruit (Cups) | 1.06 – 3.53 (2.0) | 78 | 0.52 – 2.53 (1.50) | 48 | 0.50 – 3.12 (1.25)** | 41 | 0.50 – 2.13 (1.25) | 39 |
| Vegetables (Cups) | 1.00 – 2.03 (1.52) | 78 | 0.78 – 1.87 (1.31) | 48 | 0.49 – 1.58 (1.10)* | 41 | 0.46 – 1.68 (1.32) | 39 |
|
| ||||||||
| Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | |
|
|
|
|
|
|
||||
| BMI | 25.69 (4.59) | 78 | 25.42 (4.67) | 57 | 25.09 (4.90)* | 52 | 24.10 (4.77)† | 27 |
| Stress | 15.12 (9.37) | 73 | 13.90 (9.71) | 46 | 11.88 (9.22)* | 40 | 10.43 (8.18) | 37 |
p ≤ .025
p ≤ .01
p < .10 refer to results of contrasts between T1 and T3, and T3 and T4, from linear mixed models predicting each outcome from time. IQR, interquartile range; NCI, National Cancer Institute; SD, standard deviation; BMI, body mass index. Bonferonni adjustment applied for multiple comparisons.
Table 3.
Effect of time and post-hoc contrasts from Time 1 - Time 3, and Time 3 - Time 4 within the linear mixed model for NCI dietary screener fruit intake, NCI vegetable intake, BMI, and stress in the overall sample, controlling for age, gender, and study site.
| T1 - T3 contrast |
T3 - T4 contrast |
||||||
|---|---|---|---|---|---|---|---|
| Outcome | Effect | B | SE | t-test | B | SE | t-test |
| NCI Fruit intake (Time) | F(3,137)=3.78 * | −0.47 | 0.18 | t(141) = −2.67** | −0.04 | 0.20 | t(131) = −0.22 |
| Age | F(1,67)=2.38 | ||||||
| Gender | F(1,68)=1.63 | ||||||
| Site | F(1,70)=0.13 | ||||||
| NCI Vegetable intake (Time) | F(3,136)=2.56 † | −0.28 | 0.11 | t(139) = −2.65** | 0.11 | 0.12 | t(132) = 0.96 |
| Age | F(1,72)=1.49 | ||||||
| Gender | F(1,73)=7.52** | ||||||
| Site | F(1,74)=1.24 | ||||||
| BMI (Time) | F(3, 135) = 4.73 ** | −0.02 | 0.01 | t(136) = −2.26* | −0.01 | 0.01 | t(135) = −1.67† |
| Age | F(1,74) = 4.03* | ||||||
| Gender | F(1,74)=3.68† | ||||||
| Site | F(1,75)=0.17 | ||||||
| Stress (Time) | F(3,138) = 3.36 * | −3.27 | 1.42 | t(143) = −2.31* | −0.98 | 1.58 | t(132) = −0.62 |
| Age | F(1,68)=0.24 | ||||||
| Gender | F(1,70)=0.92 | ||||||
| Site | F(1,73)=1.11 | ||||||
p ≤ .025
p ≤ .01
p <.05
p < .10. NCI, National Cancer Institute; BMI, Body Mass Index; B, unstandardized beta coefficient; SE, standard error. Bonferonni adjustment applied for multiple comparisons. Primary outcome variables bolded for emphasis.
Fruit intake decreased significantly over time (p=0.012). Contrasts revealed reductions from T1 to T3 (p=0.008) that were maintained at T4 (p=0.830). There were no effects of age (p=0.128), gender (p=0.206), or site (p=0.720) on fruit intake. Vegetable intake marginally decreased over time (p=0.058), with a significant effect of gender (p=0.008). In the overall sample, contrasts revealed significant reduction in vegetable intake from T1 to T3 (p=0.009), with no further change at T4 (p=0.337). Contrasts by gender showed men reported less vegetable intake than did women (M. 1.08, S.D. 0.67 vs. M. 1.76, S.D. 1.48; t(73)=2.74, p=.008), holding time constant. There were no effects of age (p=0.226) or site (p = 0.269) on vegetable intake.
BMI decreased over time (p=0.004), with a significant effect of age (p=0.048) and a marginal effect of gender (p=0.059). In the overall sample, contrasts revealed significant reductions in BMI from T1 to T3 (p=0.025) that trended towards greater reduction at T4 (p = 0.097). Contrasts by gender showed marginally greater BMI among men compared to women (M. 26.73, S.D. 4.95 vs. M. 24.48, S.D. 4.38; t(74)=−1.92, p=.059), holding time constant. There were no effects of site on BMI (p=.729). Stress decreased over time (p=0.021). Contrasts revealed reductions in stress from T1 to T3 (p=0.023) that were maintained at T4 (p=0.534). There were no effects of age (p=0.625), gender (p=0.340), or site (p=0.295) on stress.
Tertiary objective – Examine DHQ-II fruit, vegetable, and caloric intake among rural site participants.
At pre-treatment, NCI fruit intake was significantly associated with DHQ-II fruit intake (r=0.404, p=0.002), while NCI vegetable intake was similarly associated with DHQ-II vegetable intake (r=0.365, p=0.005).
See Table 4 for descriptive statistics at each time-point and Table 5 for effects of time, covariates, and contrasts of changes in DHQ-II variables from T1 to T3, and T3 to T4. Fruit intake as measured by the DHQ-II did not vary by time (p = 0.862), age (p=0.155), or gender (p=0.167). Vegetable intake as measured by the DHQ-II marginally decreased over time (p = 0.092), with a significant effect of age (p=0.024) but not of gender (p=0.532). Contrasts revealed significant reductions in vegetable intake from T1 to T3 (p = 0.019), with no further change at T4 (p=0.115). We next conducted an exploratory analysis to query whether reductions in vegetable intake were related to overall reduced caloric intake. The initial marginal reduction in vegetable intake over time was not retained (F(3,67) = 1.44, p = 0.240) after controlling for change in calorie intake (between-subject: F(1,29)=50.88, p < 0.001; within-subject: F(1,65) = 11.34, p = 0.001).
Table 4.
IQR and medians for DHQ-II dietary outcomes at each time-point, rural site only. Raw, untransformed data reported.
| Outcome | T1 |
T2 |
T3 |
T4 |
||||
|---|---|---|---|---|---|---|---|---|
| IQR (Median) | n | IQR (Median) | n | IQR (Median) | n | IQR (Median) | n | |
|
|
|
|
|
|||||
| Fruit (Cups) | 0.56 – 1.83 (0.76) | 30 | 0.61 – 2.01 (0.80) | 23 | 0.45 – 1.82 (1.24) | 23 | 0.55 – 0.94 (1.05) | 18 |
| Vegetables (Cups) | 1.18 – 1.62 (1.82) | 30 | 1.07 – 2.06 (1.51) | 23 | 0.69 – 2.15 (1.09)* | 23 | 0.72 – 2.31 (1.58) | 18 |
| Calories (Total) | 1104.73 – 2020.84 (1462.30) | 30 | 857.34 – 1777.36 (1301.25) | 23 | 913.34 – 1672.11 (1136.46)*** | 23 | 766.00 – 1432.64 (1032.12) | 18 |
p ≤ .025
p ≤ .01, p ≤ .001 refer to results of contrasts between T1 and T3, and T3 and T4, from linear mixed models predicting outcomes from time. Bonferonni adjustment applied for multiple comparisons. IQR, Interquartile range; DHQ-II, Dietary History Questionnaire-II. Note: T3 reduction in vegetable intake no longer significant after controlling for between and within subject changes in caloric intake. T3 reduction in calorie intake remained significant after controlling for between and within subject changes in stress.
Table 5.
Effect of time and contrasts (from Time 1 - Time 3, and Time 3 - Time 4), within the linear mixed model for DHQ-II fruit, vegetable, and caloric intake in the rural subsample, controlling for age, gender, and site.
| T1 - T3 contrast |
T3 - T4 contrast |
||||||
|---|---|---|---|---|---|---|---|
| Outcome | Effect | B | SE | t-test | B | SE | t-test |
| DHQ-II Fruit intake (Time) | F(3,64)=0.25 | - | - | - | - | - | - |
| Age | F(1,28)=2.14 | ||||||
| Gender | F(1,27)=2.02 | ||||||
| DHQ-II Vegetable intake (Time) | F(3,65)=2.23 † | −0.40 | 0.17 | t(67) = −2.40* | 0.30 | 0.19 | t(64) = −1.60 |
| Age | F(1,29)=5.70* | ||||||
| Gender | F(1,28)=0.40 | ||||||
| DHQ-II Caloric intake (Time) | F(3,63)=8.02*** | −0.37 | 0.09 | t(64) = −4.29*** | 0.003 | 0.10 | t(61) = 0.03 |
| Age | F(1,26)=4.06† | ||||||
| Gender | F(1,25)=0.03 | ||||||
p ≤ .025
p ≤ .01
p < .10. DHQ-II, Dietary History Questionnaire-II; B, unstandardized beta coefficient; SE, standard error. All analyses control for age, gender, and site. Bonferonni adjustment applied for multiple comparisons. Primary outcome variables bolded for emphasis. Note: T3 reduction in vegetable intake no longer significant after controlling for between and within subject changes in caloric intake, and T3 reduction in calorie intake no longer significant after controlling for between and within subject changes in stress.
Calorie intake as measured by the DHQ-II decreased over time (p<0.001), with a marginal effect of age (p=0.054) and no significant effect of gender (p=0.864). Contrasts revealed significant reductions in caloric intake from T1 to T3 (p < 0.001), maintained at T4 (p = 0.99). We last conducted an exploratory analysis to examine whether reductions in calorie intake on the DHQ-II remained significant after accounting for between- and within-subject reductions in stress. Reductions in calorie intake remained significant (F(3,61)=7.06, p<0.001) after controlling for reductions in stress (between-subject: F(1,23)=0.11, p=0.747; within-subject: F(1,60)=0.03, p=0.864).
4. Discussion
Poor dietary behaviors that undermine U.S. population health via chronic lifestyle diseases have proven resistant to long-term change (38,69–71). Stress is increasingly implicated as a contributor to poor diet (12), with consequent increased interest in stress reduction and relaxation interventions that may improve dietary behavior (12,72). The present study was the first to examine non-prescribed changes in dietary patterns, stress, and BMI during yoga among stressed adults reporting low fruit and vegetable intake, as well as to cross-validate findings on dietary change with an extensive food frequency questionnaire in a subset of participants.
The study’s main findings are trifold. First, contrary to our hypothesis and prior research, fruit and vegetable intake did not increase over the course of the intervention. Instead, fruit and vegetable decreased significantly from T1 to T3 in the overall sample. Second, aligned with our hypotheses, BMI and stress both significantly decreased. Declines in stress were impressive, encouraging, and trended towards further reduction at follow-up. Declines in BMI were statistically significant, though not clinically significant, with an average decrease from 25.69 at T1 to 24.10 kg/m2 at T4 suggesting a gradual decline over time. Third, findings were partially confirmed in the subset of participants at the rural site that utilized a secondary food frequency questionnaire: vegetable intake evidenced significant decline, although fruit intake did not. In exploratory analyses, reduced vegetable intake was fully accounted for following adjustment for between- and within-participant changes in caloric intake over time. That substantive reductions in caloric intake remained significant after accounting for between- and within-person reductions in stress reactivity suggests other mechanisms may underlie the change in dietary behaviors in our sample. It is also possible, however, that our self-report measure of stress fails to capture more objective, biological indices of stress that might better capture stress-related changes in diet.
Study findings could be viewed as potentially beneficial, from the standpoint that reductions in caloric intake may suggest a mechanism through which yoga associates with marginal weight loss and healthy weight and/or greater weight maintenance over time (26,73). Indeed, stressed adults with poor diet are at risk of developing chronic health concerns associated with obesity, and our preliminary findings suggest the possibility that yoga may interrupt this trajectory. Equally, our findings could be viewed as potentially concerning. Adults at the margin of healthy BMI are unlikely to require reduction of their caloric intake to the extent reported in our sample. Indeed, our sample included some individuals with a “normal” BMI (<24.9 kg/m2). This finding of reduced caloric intake may raise questions about the potential of yoga practice to facilitate potentially unhealthful dietary practices – such as orthorexia. Yet, existing research linking yoga to orthorexia or disordered eating patterns has observed this either among teachers or practitioners of yoga/Pilates (failing to differentiate the two practices) (34,35) and Ashtanga yoga (33), a vigorous practice that differs in key ways from the gentle to moderate intensity Kripalu hatha yoga taught in the present intervention. Moreover, it is probable that the reported reductions we witnessed in caloric intake were greatly overestimated and reflected modest, if any, actual reductions, given the DHQ-II’s association with under-reporting up to 46% of actual dietary intake (74–76).
Also potentially concerning were the decreases in fruit and vegetable intake observed in our sample, as greater fruit and vegetable consumption – independent of caloric intake – is an important indicator of health (77). These findings conflict with other intervention studies that report increased fruit and vegetable intake in yoga practitioners (30,31), although ours is the first study to explicitly sample stressed adults with low baseline fruit and vegetable intake. This overall pattern of findings underscores a need for further research investigating the effects of yoga on dietary patterns in stressed adults, as well as eating behavioral patterns such as orthorexia and disordered eating.
Our finding of reduced stress alongside dietary changes underscores the importance of continued research to elucidate mechanisms underlying yoga’s effects on dietary patterns in diverse populations. For instance, the “gateway” or ripple effect hypothesis posits that changes in one health behavior (e.g., yoga) may catalyze changes in other health behaviors (26,78,79). While reduced stress is a strong candidate mechanism of potential yoga-related “gateway effects” on dietary behavior change, we found reduced stress did not account for changes in caloric intake in our sample of stressed adults. Recent qualitative research in a national sample of yoga practitioners also suggests motivations to eat healthier, mindfulness, management of emotional eating, healthy food cravings, and the beneficial influence of the yoga community may contribute to healthier eating behaviors (18), all important targets of future investigation.
Last, national poll data shows rates of stress in the U.S. adult population have remained relatively constant from the period of this study (2014–2016) (80,81) to 2021 (82), despite a temporary increase from April to May 2020 in the early part of the COVID-19 pandemic (83). Increased stress during the pandemic has been tied to worse dietary and eating behaviors as well as weight gain (82), underscoring the adverse effects of stress on behavioral health and the urgent need for approaches to mitigate the impacts of stress on poor eating behaviors. Continued research to elucidate whether yoga improves dietary patterns and potential mechanisms of action is warranted.
4.1. Limitations and future directions
Several limitations should be noted, including the lack of control group, small sample size, and high attrition rates. These factors should be rectified in future research, including the use of more robust incentives to encourage retention, and assessment of whether the observed changes are attributable to yoga or contextual influences and to enhance generalizability, statistical power, and participant retention. The lack of gender and ethno-racial diversity among participants is a considerable limitation that is reflected in much of yoga research, and that has been identified as problematic (84). Historically underrepresented groups (HUG) experience heightened stress due to structural, interpersonal, and intrapersonal discrimination and sequelae that can contribute to poor mental health and health behaviors, resulting in health disparities and health inequity (85,86). Alongside multilevel efforts to dismantle the origins of heightened stress experienced by HUG, studies are needed to better understand the effects of yoga on those often underrepresented in U.S. yoga contexts. Such studies would benefit from community-engaged research to ensure interventions are responsive to community interests and needs, and to address the specific types of stress these groups may experience.
Additionally, stress was a secondary outcome in our study and a foil for the true primary outcome (i.e., fruit and vegetable intake). We thus did not use a validated measure with an established cut-point to enroll those with heightened stress; participants only needed to self-report feeling “stressed”. Those seeking to advance future work in this area would benefit from addressing this limitation, including assessing whether change in stress-related physiological indicators (e.g., cortisol levels) correspond to alterations in diet and eating behaviors during yoga.
The length of online surveys was anecdotally reported by urban site participants to be a burden and may have contributed to study attrition. Interpretation of findings is also cautioned given the well-established limitations of self-report instruments of dietary assessment (57,87,88), confirmed by some inconsistencies observed in our study between the NCI fruit and vegetable screener and the DHQ-II. Food frequency questionnaires are also subject to considerable variability and many factors bias accurate recall. Future research should consider the inclusion of 24-hour dietician-assisted recalls to reduce participant burden and increase confidence and validity of findings. Additionally, research suggests that FFQs and the DHQ-II, used here to cross-validate the NCI screener findings in the larger study, tends to under-estimate caloric intakes as well as most food groups (74,75). Moreover, underreporting has been found greater in the second DHQ-II administration, thought to relate to incremental loss of commitment following multiple instances of completing time-consuming surveys (89). This finding of under-reporting on the DHQ-II is consistent with analyses of other self-reported FFQs that find estimates of true intakes are “implausible” (90). Indeed, as noted, early in the study, several participants at the urban site in our study indicated rushing through the survey due to survey burden, which led to our discontinuing DHQ-II data collection at that site. Although rural site participants analyzed in the present study did not report this to study staff, our findings must be interpreted with caution.
Additionally, the intervention design, comprising an 8-week standardized intervention that integrated theory with yoga practice followed by four weeks of yoga practice only, limits generalizability of our findings to community yoga practitioners, as few participants in community yoga are likely to receive the same extent of yoga philosophy instruction or a manualized yoga intervention. Nonetheless, the findings do align with prior retrospective research that has observed community yoga practice linked with lower BMI over time (26). An additional limitation is that our low available n for BMI at time 4 was due to a staffing turnover at the urban site. Full efforts are recommended to rectify this in future research and examine change in BMI alongside dietary patterns during yoga in stressed adults.
Lastly, the effects of stress on total energy intake vary intra-individually – some people consume less food, not more, under stress (12). Although our sample identified as stressed with poor diet, the study did not explicitly screen for those endorsing increased eating when stressed. Thus theoretically it is possible that reductions in caloric intake were attributable to increases in stress during the yoga intervention. However, our overall pattern of results – characterized by between-person reductions in stress and caloric intake – does not suggest a relationship between heightened stress and decreased caloric consumption. We also excluded those with eating pathology (conditions frequently impacted by stress, which in turn impact eating behavior) because this would have potentially confounded our ability to understand dietary change in a stressed rather than a clinical sample. Future research would benefit from examining the effects of yoga on total energy intake in stressed and clinical samples that explicitly report overeating under conditions of stress, including at the within-person level. Experience sampling methods such as Ecological Momentary Assessment would optimally elucidate the temporality, causality, and mechanisms underlying yoga’s effects on eating behaviors and stress.
5. Conclusion
Our findings present a trend of reduced fruit and/or vegetable intake, as well as reduced caloric intake, BMI, and stress, among stressed adults with poor diet at the margin of healthy/overweight BMI (~25.7) during and following a yoga intervention. Results suggest overall fruit and vegetable intake decreased secondary to decrease in overall caloric intake, while decreased caloric intake appeared unrelated to reduction in stress reactivity. Findings point to the complexity and limitations of using self-report instruments of dietary assessment and stress, and suggest the hypotheses that yoga may either encourage healthy dietary patterns (i.e., minimizing likelihood of future weight gain via reduction in caloric intake and a trend towards BMI reduction) or foster concerning dietary patterns (i.e., decreasing fruit and vegetable intake, as well as caloric intake among a sample with only marginal overweight). Future careful research is needed using longitudinal and controlled designs with objective measures to investigate these patterns with greater rigor.
Study Highlights.
Stress contributes to dietary patterns that impede health
Yoga reduces stress and may therefore improve diet in stressed adults
Reduced fruit/vegetable intake, body mass index, and stress found across 16 weeks
Caloric decrease accounted for the reduced vegetable intake
Yoga either encourages or adversely impacts healthy dietary patterns
Acknowledgments:
We thank the intervention facilitators Sandra Hartnett and David Schouela, as well as research assistants Melanie Klinck, Joan Daniel, Manasi Ravi, Jake Kochin, and Marissa Schneider for their contributions to this study. We thank David Ludwig, MD, PhD and Jean Kristeller, PhD, for their helpful input on study design, and the Kripalu Institute for Extraordinary Living for providing the initial yoga program manual.
Funding:
This work was supported by the National Institutes of Health (NIH; grant numbers R34-AT007197 and R01-AG-048351) and through an NIH Cardiovascular Behavioral and Preventive Medicine Training Grant awarded to the Miriam Hospital, Providence, RI (T32 HL076134).
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health, National Institute of Complementary and Integrative Health (R34-AT007197) and National Heart, Lung, and Blood Institute (T32 HL076134).
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wallace TC, Bailey RL, Blumberg JB, Burton-Freeman B, Chen C y. O, Crowe-White KM, et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit Rev Food Sci Nutr [Internet]. 2020;60(13):2174–211. doi: 10.1080/10408398.2019.1632258 [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, et al. The State of US Health, 1990–2016. JAMA [Internet]. 2018;319(14):1444. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Algren MH, Ekholm O, Nielsen L, Ersbøll AK, Bak CK, Andersen PT. Associations between perceived stress, socioeconomic status, and health-risk behaviour in deprived neighbourhoods in Denmark: A cross-sectional study. BMC Public Health. 2018;18(1):1–12. doi: 10.1186/s12889-018-5170-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papier K, Ahmed F, LEe P, Wiseman J. Stress and dietary behaviour among first-year university students in Australia: Sex differences. Nutrition. 2015;31(2):1–22. doi: 10.1016/j.nut.2014.08.004 [DOI] [PubMed] [Google Scholar]
- 5.Leigh SJ, Lee F, Morris MJ. Hyperpalatability and the generation of obesity: Roles of environment, stress exposure and individual difference. Curr Obes Rep. 2018;7(1):6–18. doi: 10.1007/s13679-018-0292-0 [DOI] [PubMed] [Google Scholar]
- 6.Devonport TJ, Nicholls W, Fullerton C. A systematic review of the association between emotions and eating behaviour in 2 normal and overweight adult populations. J Health Psychol. 2017;24(1):1–31. doi: 10.1177/1359105317697813 [DOI] [PubMed] [Google Scholar]
- 7.Gibson EL. The psychobiology of comfort eating: implications for neuropharmacological interventions. Behav Pharmacol. 2012;23(5–6):442–60. doi: 10.1097/FBP.0b013e328357bd4e [DOI] [PubMed] [Google Scholar]
- 8.Schulte EM, Joyner MA, Schiestl ET, Gearhardt AN. Future directions in “Food Addiction”: Next steps and treatment implications. Curr Addict Reports. 2017;1–7. doi: 10.1007/s40429-017-0140-4 [DOI] [Google Scholar]
- 9.Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica J A. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: A systematic review. Eat Behav. 2014;15(2):197–204. doi: 10.1016/j.eatbeh.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 10.Corsica J, Hood MM, Katterman S, Kleinman B, Ivan I. Development of a novel mindfulness and cognitive behavioral intervention for stress-eating: A comparative pilot study. Eat Behav. 2014;15(4):694–9. doi: 10.1016/j.eatbeh.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 11.Leow S, Jackson B, Alderson J, Guelfi K, Dimmock J. A role for exercise in attenuating unhealthy food consumption in response to stress. Nutrients. 2018;10(2):176. doi: 10.3390/nu10020176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masih T, Dimmock JA, Epel ES, Guelfi KJ. Stress-induced eating and the relaxation response as a potential antidote: A review and hypothesis. Appetite. 2017;118:136–43. doi: 10.1016/j.appet.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 13.Feuerstein G The Yoga Tradition: its History, Literature, Philosophy, and Practice. Prescott, AZ: Hohm Press; 2001. [Google Scholar]
- 14.Askegaard S, Eckhardt GM. Glocal yoga: Re-appropriation in the Indian consumptionscape. Mark Theory. 2012. Mar;12(1):45–60. doi: 10.1177/1470593111424180 [DOI] [Google Scholar]
- 15.Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med. 2010. Jan;16(1):3–12. doi: 10.1089/acm.2009.0044 [DOI] [PubMed] [Google Scholar]
- 16.Melville GW, Chang D, Colagiuri B, Marshall PW, Cheema BS. Fifteen minutes of chair-based yoga postures or guided meditation performed in the office can elicit a relaxation response. Evidence-Based Complement Altern Med. 2012;2012:1–9. doi: 10.1155/2012/501986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hopkins LB, Medina JL, Baird SO, Rosenfield D, Bowers MP, Smits JAJ. Heated Hatha yoga to target cortisol reactivity to stress and affective eating in women at risk for obesity-related illnesses: A Randomized Controlled Trial. J Consult Clin Psychol. 2016;84(6):558–64. doi: 10.1037/ccp0000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Watts AW, Rydell SA, Eisenberg ME, Laska MN, Neumark-Sztainer D. Yoga’s potential for promoting healthy eating and physical activity behaviors among young adults: A mixed-methods study. Int J Behav Nutr Phys Act. 2018;15(1):1–11. doi: 10.1186/s12966-018-0674-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cramer H, Sundberg T, Schumann D, Leach MJ, Lauche R. Differences between vegetarian and omnivorous yoga practitioners—Results of a nationally representative survey of US adult yoga practitioners. Complement Ther Med. 2018;40:48–52. doi: 10.1016/j.ctim.2018.07.012 [DOI] [PubMed] [Google Scholar]
- 20.Ross A, Friedmann E, Bevans M, Thomas S. Frequency of yoga practice predicts health: results of a national survey of yoga practitioners. Evid Based Complement Alternat Med. 2012. Jan;1–10. doi: 10.1155/2012/983258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ross A, Friedmann E, Bevans M, Thomas S. National survey of yoga practitioners: Mental and physical health benefits. Complement Ther Med. 2013. Aug;21(4):313–23. doi: 10.1016/j.ctim.2013.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Penman S, Stevens P, Cohen M, Jackson S. Yoga in Australia: Results of a national survey. Int J Yoga. 2012;5(2):92. doi: 10.4103/0973-6131.98217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cartwright T, Mason H, Porter A, Pilkington K. Yoga practice in the UK: A cross-sectional survey of motivation, health benefits and behaviours. BMJ Open. 2020;10(1). doi: 10.1136/bmjopen-2019-031848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cramer H, Sibbritt D, Park CL, Adams J, Lauche R . Is the practice of yoga or meditation associated with a healthy lifestyle? Results of a national cross-sectional survey of 28,695 Australian women. J Psychosom Res. 2017;101:104–9. doi: 10.1016/j.jpsychores.2017.07.013 [DOI] [PubMed] [Google Scholar]
- 25.Cramer H, Quinker D, Pilkington K, Mason H, Adams J, Dobos G. Associations of yoga practice, health status, and health behavior among yoga practitioners in Germany—Results of a national cross-sectional survey. Complement Ther Med. 2019;42:19–26. doi: 10.1016/j.ctim.2018.10.026 [DOI] [PubMed] [Google Scholar]
- 26.Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-aged men and women. Altern Ther Health Med. 2005;11(4):28–33. Available from: https://pubmed.ncbi.nlm.nih.gov/16053119/ [PubMed] [Google Scholar]
- 27.Manjula S, Saini N, Gupta S. Exploring the effect of yoga and diet counseling on dietery intake of college-going females. Int J Physicol Educ Sport Heal. 2017;4(1):155–60. Available from: https://www.kheljournal.com/archives/2017/vol4issue1/PartC/4-1-17-603.pdf [Google Scholar]
- 28.Braun TD, Park CL, Conboy LA. Psychological well-being, health behaviors, and weight loss among participants in a residential, Kripalu Yoga-based weight loss program. Int J Yoga Therap. 2012;22(1):9–22. doi: 10.17761/ijyt.22.1.y47k2658674t1212 [DOI] [PubMed] [Google Scholar]
- 29.Yadav R, Yadav RK, Khadgawat R, Pandey RM, Upadhyay AD, Mehta N. Randomized Controlled Trial of A 12-Week yoga-based (including diet) lifestyle vs. dietary intervention on cardio-metabolic risk factors and continuous risk score in Indian adults with metabolic syndrome. Behav Med 2020;46(1):9–20. doi: 10.1080/08964289.2018.1538098 [DOI] [PubMed] [Google Scholar]
- 30.Alexander GK, Innes KE, Selfe TK, Brown CJ. “More than I expected”: Perceived benefits of yoga practice among older adults at risk for cardiovascular disease. Complement Ther Med. 2013;21(1):14–28. doi: 10.1016/j.ctim.2012.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley KE, Park CL, Wilson A, Sabo AN, Antoni MH, Braun TD, et al. Improving physical and mental health in frontline mental health care providers: Yoga-Based Stress Management versus Cognitive Behavioral Stress Management. J Workplace Behav Health. 2016;32(1):26–48. doi: 10.1080/15555240.2016.1261254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Braun TD, Uebelacker LA, Ward M, Holzhauer CG, McCallister K, Abrantes AM, “We really need this”: Trauma-informed yoga for Veteran women with a history of military sexual trauma, Compl. Ther. Med 49 (2021) 102729, 10.1016/j.ctim.2021.102729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herranz Valera J, Acuña Ruiz P, Romero Valdespino B, Visioli F. Prevalence of orthorexia nervosa among ashtanga yoga practitioners: a pilot study. Eat Weight Disord. 2014;19(4):469–72. doi: 10.1007/s40519-014-0131-6 [DOI] [PubMed] [Google Scholar]
- 34.Neumark-Sztainer D, Eisenberg ME, Wall M, Loth KA. Yoga and Pilates: associations with body image and disordered-eating behaviors in a population-based sample of young adults. Int J Eat Disord. 2011;44(3):276–80. doi: 10.1002/eat.20858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bratland-Sanda S, Nilsson MP, Sundgot-Borgen J. Disordered eating behavior among group fitness instructors: A health-threatening secret? J Eat Disord [Internet]. 2015;3(1):1–8. Available from: 10.1186/s40337-015-0059-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cox AE, Ullrich-French S, Cook-Cottone C, Tylka TL, Neumark-Sztainer D. Examining the effects of mindfulness-based yoga instruction on positive embodiment and affective responses. Eat Disord. 2020;00(00):1–18. doi: 10.1080/10640266.2020.1738909 [DOI] [PubMed] [Google Scholar]
- 37.Cook-Cottone C, Douglass LL. Yoga communities and eating disorders: Creating safe space for positive embodiment. Int J Yoga Therap. 2017;27(1):87–93. doi: 10.17761/1531-2054-27.1.87 [DOI] [PubMed] [Google Scholar]
- 38.Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. 2015. Available from: https://health.gov/dietaryguidelines/2015-scientific-report/pdfs/scientific-report-of-the-2015-dietary-guidelines-advisory-committee.pdf
- 39.Greenberg J, Braun TD, Schneider ML, Finkelstein-Fox L, Conboy LA, Schifano ED, et al. Is less more? A randomized comparison of home practice time in a mind-body program. Behav Res Ther. 2018;111:52–6. doi: 10.1016/j.brat.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kabat-Zinn J Full Catastrophe Living. New York: Delta Trade Paperbacks; 1990. [Google Scholar]
- 41.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression (2nd ed.). New York, NY, US: Guilford Press; 2013. [Google Scholar]
- 42.Park CL, Finkelstein-Fox L, Sacco SJ, Braun TD, Lazar S. How does yoga reduce stress? A clinical trial testing psychological mechanisms. Stress Heal. 2020;37:116–126. doi: 10.1002/smi.2977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Psychological Association. Stress by Generation. Stressinamerica.org. 2012;19–21. Available from https://www.apa.org/news/press/releases/stress/2012/generations
- 44.Graham JE, Christian LM, Kiecolt-Glaser JK. Stress, age, and immune function: Toward a lifespan approach. J Behav Med. 2006;29(4):389–400. doi: 10.1007/s10865-006-9057-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paxton AE, Strycker L a, Toobert DJ, Ammerman AS, Glasgow RE. Starting the conversation performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med [Internet]. 2011;40(1):67–71. doi: 10.1016/j.amepre.2010.10.009 [DOI] [PubMed] [Google Scholar]
- 46.National Institutes of Health. NHLBI Serving Size Card. 2014. Available from: http://hp2010.nhlbihin.net/portion/servingcard7.pd
- 47.Small M, Bailey-Davis L, Morgan N, Maggs J. Changes in eating and physical activity behaviors across seven semesters of college: Living on or off campus matters. Heal Educ Behav. 2013. Aug;40(4):435–41. doi: 10.1177/1090198112467801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Krucoff C, Carson K, Peterson M, Shipp K, Krucoff M. Teaching yoga to seniors: Essential considerations to enhance safety and reduce risk in a uniquely vulnerable age group. J Altern Complement Med. 2010;16(8):899–905. doi: 10.1089/acm.2009.0501 [DOI] [PubMed] [Google Scholar]
- 49.Haskell WL, Lee I-M, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27 [DOI] [PubMed] [Google Scholar]
- 50.Sheehan D, Lecrubier Y, Sheehan H, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(20):22–33. Available from: https://psycnet.apa.org/record/1998-03251-004 [PubMed] [Google Scholar]
- 51.First MB, Spitzer R, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I disorders—Patient edition (SCID—I/P, version 2.0). New York: New York State Psychiatric Institute; 1995. [Google Scholar]
- 52.Thompson WR, Pescatello LS, Gordon NF, editors. ACSM’s Guidelines for Exercise Testing and Prescription. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 53.Thompson FE, Subar AF, Smith AF, Midthune D, Radimer KL, Kahle LL, et al. Fruit and vegetable assessment: Performance of 2 new short instruments and a food frequency questionnaire. J Am Diet Assoc. 2002;102(12):1764–72. doi: 10.1016/S0002-8223(02)90379-2 [DOI] [PubMed] [Google Scholar]
- 54.Thompson FE, Kipnis V, Subar AF, Krebs-Smith SM, Kahle LL, Midthune D, et al. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am J Clin Nutr. 2000;71(6):1503–10. doi 10.1093/ajcn/71.6.1503 [DOI] [PubMed] [Google Scholar]
- 55.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995. 335–343. [Google Scholar]
- 56.Gloster AT, Rhoades HM, Novy D, Klotsche J, Senior A, Kunik M, et al. Psychometric properties of the Depression Anxiety and Stress Scale-21 in older primary care patients. J Affect Disord. 2008. Oct;110(3):248–59. doi: 10.1016/j.jad.2008.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thompson FE, Subar AF. Dietary assessment methodology. In: Nutrition in the Prevention and Treatment of Disease. Academic Press; 2017. p. 5–48. [Google Scholar]
- 58.Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. Am J Epidemiol. 2001;154(12):1089–99. doi: 10.1093/aje/154.12.1089 [DOI] [PubMed] [Google Scholar]
- 59.Park CL, Riley KE, Braun TD, Jung JY, Suh HG, Pescatello LS, et al. Yoga and Cognitive-Behavioral interventions to reduce stress in incoming college students: A pilot study. J Appl Biobehav Res. 2017;1–25. doi: 10.1111/jabr.12068 [DOI] [Google Scholar]
- 60.Cook-Cottone C, LaVigne M, Guyker W, Travers L, Lemish E, Elenson P. Trauma-Informed Yoga: An embodied, cognitive-relational framework. Int J Complement Altern Med. 2017;9(1):1–10. doi: 10.15406/ijcam.2017.09.00284 [DOI] [Google Scholar]
- 61.Faulds R Kripalu Yoga: A guide to practice on and off the mat. New York, NY: Bantam Dell; 2005. 418 p. [Google Scholar]
- 62.Lloyd A Urge Surfing. In: O’Donohue W, Fisher JE, Hayes SC, editors. Cognitive Behavior Therapy: Applying Emperically Supported Techniques in Your Practice. John Wiley & Sons; 2003. p. 451–5. [Google Scholar]
- 63.Hartranft C. The Yoga-Sutra of Patanjali: A new translation with commentary, Shambhala Publications, Boston, MA, 2003. [Google Scholar]
- 64.Salmoirago-Blotcher E, Morgan L, Fischer D, Carmody J. Mindfulness-Based Stress Reduction and change in health-related behaviors. J Evid Based Complementary Altern Med. 2013;18(4):243–7. doi: 10.1177/2156587213488600 [DOI] [Google Scholar]
- 65.Sedgwick P Log transformation of data. BMJ. 2012;345:1–2. doi: 10.1136/bmj.e6727 [DOI] [Google Scholar]
- 66.Jennrich RI, Schluchter MD. Unbalanced repeated-measures models with structured covariance matrices. Biometrics. 1986;42(4):805–20. doi: 10.2307/2530695 [DOI] [PubMed] [Google Scholar]
- 67.Novais A, Monteiro S, Roque S, Correia-Neves M, Sousa N. How age, sex and genotype shape the stress response. Neurobiol Stress. 2017;6:44–56. doi: 10.1016/j.ynstr.2016.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, Ogden CL. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013–2016. JAMA - J Am Med Assoc. 2018;319(23):2419–29. doi: 10.1001/jama.2018.7270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ogden LG, Stroebele N, Wyatt HR, Catenacci V a, Peters JC, Stuht J, et al. Cluster analysis of the national weight control registry to identify distinct subgroups maintaining successful weight loss. Obesity. 2012;20(10):2039–47. doi: 10.1038/oby.2012.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thomson CA, Ravia J. A systematic review of behavioral interventions to promote intake of fruit and vegetables. J Am Diet Assoc. 2011;111(10):1523–35. doi: 10.1016/j.jada.2011.07.013 [DOI] [PubMed] [Google Scholar]
- 71.Brownell KD. The humbling experience of treating obesity: Should we persist or desist? Behav Res Ther. 2010;48(8):717–9. 10.1016/j.brat.2010.05.018 [DOI] [PubMed] [Google Scholar]
- 72.Xenaki N, Bacopoulou F, Alexandras K, Nicolas NC, George PC, Christina D. Impact of a stress management program on weight loss, mental health and lifestyle in adults with obesity: A randomized controlled trial. J Mol Biochem. 2018;7(2):78–84. [PMC free article] [PubMed] [Google Scholar]
- 73.Lauche R, Langhorst J, Lee MS, Dobos G, Cramer H. A systematic review and meta-analysis on the effects of yoga on weight-related outcomes. Prev Med. 2015;87:213–32. doi: 10.1016/j.ypmed.2016.03.013 [DOI] [PubMed] [Google Scholar]
- 74.Millen AE, Midthune D, Thompson FE, Kipnis V, Subar AF. The National Cancer Institute Diet History Questionnaire: Validation of pyramid food servings. Am J Epidemiol. 2006;163(3):279–88. doi: 10.1093/aje/kwj031 [DOI] [PubMed] [Google Scholar]
- 75.Murtaugh MA, Ma KN, Greene T, Redwood D, Edwards S, Johnson J, et al. Validation of a dietary history questionnaire for American Indian and Alaska native people. Ethn Dis. 2010;20(4):429–36. doi: 10.3402/ijch.v68i2.18319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lissner L, Troiano RP, Midthune D, Heitmann BL, Kipnis V, Subar AF, et al. OPEN about obesity: Recovery biomarkers, dietary reporting errors and BMI. Int J Obes. 2007;31(6):956–61. doi: 10.1038/sj.ijo.0803527 [DOI] [PubMed] [Google Scholar]
- 77.Mozaffarian D, Hao T. Changes in diet and lifestyle and long-term weight gain in women and men. New Engl J. 2011;364(25):2392–404. doi: 10.1056/NEJMoa1014296.Changes [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gorin A, Wing RR, Fava JL, Jakicic JM, Jeffery R, West DS, et al. Weight loss treatment influences untreated spouses and the home environment: Evidence of a ripple effect. Int J Obes. 2008;32(11):1678–84. doi: 10.1038/ijo.2008.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang K, James K a. Yoga, as a transitional platform to more active lifestyle: a 6-month pilot study in the USA. Health Promot Int. 2014;1–7. doi: 10.1093/heapro/dau108 [DOI] [PubMed] [Google Scholar]
- 80.American Psychological Association. Stress in America 2014: Paying with our health. Stress Am Surv. 2015. Available from: http://www.apa.org/news/press/releases/stress/2014/stress-report.pdf [Google Scholar]
- 81.American Psychological Association. Stress in America 2016, Part 1: Coping with change. Stress Am Surv. 2017. Available from: https://www.apa.org/news/press/releases/stress/2016/coping-with-change.pdf [Google Scholar]
- 82.American Psychological Association. Stress in America: One year later, a new wave of pandemic health concerns. Stress Am Surv. 2010. Available from: http://www.apa.org/news/press/releases/stress/national-report.pdf [Google Scholar]
- 83.American Psychological Association. Stress in America 2020: Stress in the time of COVID-19, Volume 1. Stress Am Surv. 2020;1. Available from: https://www.apa.org/news/press/releases/stress/2020/report%0Ahttp://files/461/report.html [Google Scholar]
- 84.Webb JB, Rogers CB, Thomas EV. Realizing Yoga’s all-access pass: A social justice critique of westernized yoga and inclusive embodiment. Eat Disord. 2020;28(4):1–27. doi: 10.1080/10640266.2020.1712636 [DOI] [PubMed] [Google Scholar]
- 85.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21. doi: 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dunkel Schetter C, Schafer P, Lanzi RG, Clark-Kauffman E, Raju TNK, Hillemeier MM. Shedding light on the mechanisms underlying health disparities through community participatory methods: The stress pathway. Perspect Psychol Sci. 2013;8(6):613–33. doi: 10.1177/1745691613506016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kirkpatrick SI, Reedy J, Butler EN, Dodd KW, Subar AF, Thompson FE, et al. Dietary assessment in food environment research: A systematic review. Am J Prev Med. 2014;46(1):94–102. doi: 10.1016/j.amepre.2013.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shim J-S, Oh K, Chang Kim H. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:1–8. doi: 10.4178/epih/e2014009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Subar AF, Kipnis V, Troiano RP, Midthune D, Schoeller DA, Bingham S, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: The OPEN study. Am J Epidemiol. 2003;158(1):1–13. doi: 10.1093/aje/kwg092 [DOI] [PubMed] [Google Scholar]
- 90.Ioannidis JPA. Implausible results in human nutrition research. BMJ. 2013;347:1–2. doi: 10.1136/bmj.f6698 [DOI] [PubMed] [Google Scholar]


