Abstract
Purpose
Intravesical BCG (bacille Calmette–Guérin) instillation in patients with non-muscle-invasive bladder cancer decreases the risk for tumor recurrence and progression. After one BCG product was discontinued, a chronic global BCG shortage occurred. We focused on identifying a reduced dose of BCG that could maintain efficacy and reduce adverse effects.
Materials and Methods
We conducted a comprehensive literature search of PubMed, Embase, the Cochrane Library, CINAHL, Web of Science, and Scopus to identify randomized controlled trials through April 2021. The odds ratios (ORs) and 95% confidence intervals (CIs) for the low and standard doses in nine studies were compared. A low dose was defined as a low volume of BCG compared with the standard BCG dose (Armand Frappier, 120 mg; Connaught, 81 mg; Danish 1331, 120 mg; modified Danish 1331, 120 mg; Tokyo 172, 80 mg).
Results
The low-dose group experienced aggravated recurrence (OR, 1.45; 95% CI, 1.09–1.94; p=0.01) but similar progression (OR, 1.11; 95% CI, 0.76–1.62; p=0.59), similar cancer-specific survival (OR, 1.02; 95% CI, 0.60–1.75; p=0.93), similar overall survival (OR, 1.09; 95% CI, 0.76–1.56; p=0.65), favorable adverse effects (OR, 0.41; 95% CI, 0.28–0.62; p<0.0001), and favorable withdrawal (OR, 0.42; 95% CI, 0.25–0.71; p=0.001).
Conclusions
Low-dose BCG had more unfavorable outcomes than did standard-dose BCG in terms of recurrence. Tumor progression, cancer-specific survival, and overall survival were similar between the doses. Low-dose BCG improved adverse effects and withdrawal. In the setting of BCG shortage, low-dose BCG may have strong potential as an alternative.
Keywords: Administration, intravesical; Adverse effects; Recurrence; Urinary bladder neoplasms
Graphical Abstract
INTRODUCTION
Non-muscle-invasive bladder cancer (NMIBC), or superficial bladder cancer, constitutes approximately 70% of all bladder cancers [1,2]. Although NMIBC initially appears to be non-life-threatening, 50% to 70% of NMIBC will recur and 10% to 20% of NMIBC will progress to muscle invasion [1,2]. Several trials have explored reducing the recurrence and progression of NMIBC, and intravesical bacille Calmette–Guérin (BCG) has displayed greater efficacy than other chemotherapeutic agents [3]. BCG instillation after transurethral resection was introduced in the mid-1970s and has been established as standard therapy for high-risk tumors (T1 and/or high-grade and/or carcinoma in situ) [4]. Nevertheless, high-risk tumors often exhibit progression and unfavorable outcomes. Although the mechanism remains poorly understood, the immune response is clearly an important component of BCG action [5]. A better understanding of the mechanism of action may improve efficacy of and tolerance to treatment. To date, however, the optimal BCG strategy remains controversial.
BCG adverse effects are one of the main causes of therapy withdrawal. The most common adverse effect is local symptoms. Approximately 63% of patients develop local symptoms, such as cystitis, frequency, and hematuria [6]. The systemic adverse effects of malaise, rash, fever, and sepsis are observed in approximately 31% of patients [6]. Several trials have investigated methods to reduce these adverse effects, such as the addition of antibiotics, anticholinergics, isoniazid, or intravesical lidocaine [7]. Dose reduction of BCG could be a way to reduce the adverse effects.
Unfortunately, Sanofi Pasteur (Lyon, France) halted production of the BCG Connaught strain because of inability to maintain long-term sustainability and a stable supply [8]. Quality testing, validation, and packaging of BCG are time-consuming because of the slow growth of microorganisms; thus, a BCG shortage has begun [8]. There have been no meta-analyses conducted on various study results such as oncologic outcomes and adverse effects of low-dose BCG since the start of the BCG shortage. Considering the BCG shortage, we studied whether a lower dose could maintain efficacy while reducing adverse effects.
EVIDENCE ACQUISITION
1. Ethics statement
This meta-analysis did not require ethical approval because the data were synthesized from previously published studies.
2. Protocol and registration
This systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. This review was registered in the PROSPERO International Prospective Registry of Systematic Reviews (CRD42021247497).
3. Search strategy
A comprehensive literature search was conducted by using several databases (PubMed, Embase, the Cochrane Library, CINAHL, Web of Science, and Scopus). The date was restricted to articles published on or before April 6, 2021; the search was conducted on April 16, 2021. The search specifics were as follows: (“urinary bladder neoplasm”[MeSH] OR “bladder cancer” OR “bladder tumor*” OR “Bladder Neoplasm*”) AND (“BCG Vaccine”[MeSH] OR “Bacillus Calmette Guerin Vaccine” OR BCG OR “low dose”). The search criteria were used to identify all potentially relevant articles. A low dose was defined as a low volume of BCG compared to the BCG standard dose (Armand Frappier, 120 mg; Connaught, 81 mg; Danish 1331, 120 mg; modified Danish 1331, 120 mg; Tokyo 172, 80 mg).
After combining the results, two authors (S.Y.C. and M.S.H.) independently selected the relevant studies. The Kappa value (κ) was assessed for interrater validity. Any conflicts between the two reviewers were resolved through discussion.
4. Eligibility criteria
The inclusion criteria were as follows: 1) the patients had NMIBC; 2) the intervention was intravesical BCG therapy; 3) the comparison was based on the BCG dose; 4) the outcomes were recurrence, progression, cancer-specific survival, overall survival, adverse effects, and withdrawal; and 5) the studies were randomized controlled trials (RCTs). The exclusion criteria were review articles, animal studies, articles not in English, duplicated studies, maintenance treatments, additional treatments, and nonstandard doses of BCG.
5. Data extraction and collection
Two authors (S.Y.C. and M.S.H.) independently reviewed each eligible article and extracted the data. The data included: 1) publication data (name of first author and publication year); 2) population data (sample size of each group and definition of progression or adverse effects); 3) tumor data (tumor stage and grade); 4) treatment data (BCG dose, duration, and strain); and 5) outcome data (recurrence, progression, cancer-specific survival, overall survival, adverse effects, and withdrawal).
6. Assessment of risk of bias
The risk of bias was assessed by two authors independently using the Cochrane Collaboration’s risk of bias tool [9]. Random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other biases were assessed. Any disagreements were resolved through discussion.
7. Statistical analysis
The data analyses were conducted by using Review Manager software (version 5.4; Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The statistical heterogeneity was assessed with I2 statistics: I2>50%, substantial heterogeneity; 20%<I2≤50%, moderate heterogeneity; and I2<20%, low heterogeneity. Odds ratios (ORs) with 95% confidence intervals (CIs) for the forest plot were measured. Meta-regression analyses with a mixed-effects model were also performed to assess the effects of the potential moderators (study year <2000 vs. ≥2000). The interrater reliability was deemed as fair (κ=0.21–0.40), moderate (κ=0.41–0.60), substantial (κ=0.61–0.80), or almost perfect (κ=0.81–1.00). Statistical significance was set at p<0.05, and all reported p-values were from two-sided versions of the respective tests.
EVIDENCE SYNTHESIS
1. Study selection
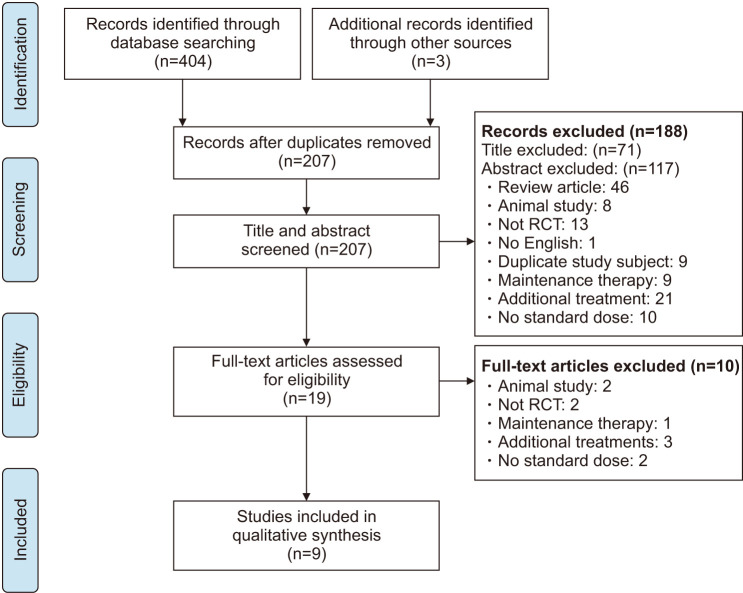
We identified 404 articles through the initial database search and an additional 3 articles through other sources. The number of duplicate publications was 200, leaving 207 records after we removed the duplicates. A total of 188 articles were excluded by reviewing the title and abstract, and 10 articles were excluded after reviewing the full text. Finally, nine articles were included in the meta-analysis (κ=0.88, almost perfect agreement). The selection process is illustrated in the flow diagram in Fig. 1.
Fig. 1. Flow diagram. RCT, randomized controlled trial.
2. Study characteristics
In total, 1,217 patients were included in the nine eligible studies (low dose, n=612 vs. standard dose, n=605; Table 1). The studies were published from 1992 to 2016.
Table 1. Randomized controlled trials included in meta-analysis comparing low-dose BCG with standard-dose BCG.
| Study | Year | No. of patients | Age (y) | Sex (F/M) | Definition of progression | Cystoscopy follow-up | |||
|---|---|---|---|---|---|---|---|---|---|
| Low-dose | Standard dose | Low-dose | Standard-dose | Low-dose | Standard dose | ||||
| Morales et al. [18] | 1992 | 49 | 48 | NA | NA | NA | NA | NA | 4, 12, and 24 weeks and at 6- to 12-month intervals thereafter |
| Yalçinkaya et al. [10] | 1998 | 25 | 25 | 56.28 (37–70) | 55.27 (32–68) | 4/21 | 3/22 | Increase of stage or grade of the papillary tumor | NA |
| Kumar et al. [16] | 2002 | 13 | 13 | 55.9±10.83 | 56.7±12.8 | 2/11 | 1/12 | NA | Every 3 months |
| Martínez‐Piñeiro et al. [11] | 2002 | 248 | 252 | 62.9±11.6 | 64.1±10.3 | 22/226 | 27/225 | Muscle invasion, extravesical extension, metastases | NA |
| Irie et al. [14] | 2003 | 41 | 39 | 62.2±11.2 | 61.6±15.7 | 8/33 | 4/35 | Up-grade or up-stage | Every 3 months for the first 2 years and every 6 months afterward |
| Martínez‐Piñeiro et al. [12] | 2005 | 73 | 82 | 68.3±8.8 | 65.8±11.1 | 7/66 | 5/77 | Muscle-invasive, distant metastases | NA |
| Vijjan et al. [17] | 2006 | 65 | 41 | 59±10.2 | 4/33 (80 mg) | 4/33 (80 mg) | 5/36 | Muscle-invasive disease | Every 3 months |
| 6/22 (40 mg) | 6/22 (40 mg) | ||||||||
| Inamoto et al. [13] | 2013 | 18 | 20 | 71.0±10.8 | 72.7±10.5 | 4/14 | 3/17 | Muscle-invasive disease or distant metastases | Every 3 months |
| Yokomizo et al. [15] | 2016 | 81 | 85 | NA | NA | NA | NA | Muscle-invasive bladder | Every 3 months for the first 2 years and every 6 months after 2 years |
Values are presented as number only, mean (range), or mean±standard deviation.
BCG, bacille Calmette–Guérin; F/M, female/male; NA, not available.
The treatment characteristics are listed in Table 2. The Connaught strain was used in four studies [10,11,12,13]. The Tokyo 172 strain was used in three studies [13,14,15]. Two studies used the Danish 1331 strain [16,17], while one study used the Armand Frappier strain [18]. The standard dose of each strain was 81 mg of Connaught, 80 mg of Tokyo 172, 120 mg of Danish 1331, and 120 mg of Armand Frappier. Most studies provided 6 weekly instillations [10,13,14,16,17,18], although one study used 8 instillations [15] and two studies, 12 instillations [11,12].
Table 2. Inclusion criteria and treatment characteristics.
| Study | Inclusion criteria | BCG dose (mg) | BCG strain | BCG instillation number | |
|---|---|---|---|---|---|
| Low-dose | Standard-dose | ||||
| Morales et al. [18] | Ta, T1, CIS | 60 | 120 | Armand Frappier | 6 |
| Yalçinkaya et al. [10] | Ta, T1 | 54 | 81 | Connaught | 6 |
| Kumar et al. [16] | TaG2-3, T1G1-3 | 40 | 120 | Modified Danish 1331 | 6 |
| Martínez‐Piñeiro et al. [11] | Recurrent Ta, T1, CIS | 27 | 81 | Connaught | 12 |
| Irie et al. [14] | Ta, T1 | 40 | 80 | Tokyo 172 | 6 |
| Martínez‐Piñeiro et al. [12] | T1G3, CIS | 27 | 81 | Connaught | 12 |
| Vijjan et al. [17] | Ta or T1 with >G1, size >1 cm, multiple, recurrent | 40/80 | 120 | Danish 1331 | 6 |
| Inamoto et al. [13] | TaG2-3, T1G1-3 with ≤3 cm | 40 | 81 | Tokyo 172 (low dose) | 6 |
| Connaught (standard dose) | |||||
| Yokomizo et al. [15] | CIS, unresectable Ta or T1 | 40 | 80 | Tokyo 172 | 8 |
BCG, bacille Calmette–Guérin.
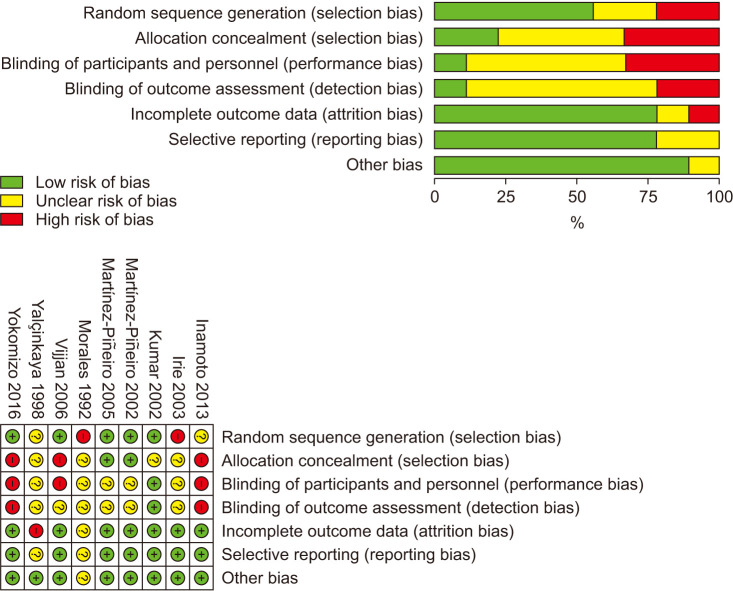
3. Assessment for risk of bias
The results of the assessment of the risk of bias in the included studies are summarized in Fig. 2. Adequate randomization methods and allocation concealment were described in five [11,12,15,16,17] and two studies [11,12], respectively. Blinding of the outcome assessment was performed in one study [16].
Fig. 2. Summary of the risk of bias assessment for included studies.
4. Tumor recurrence
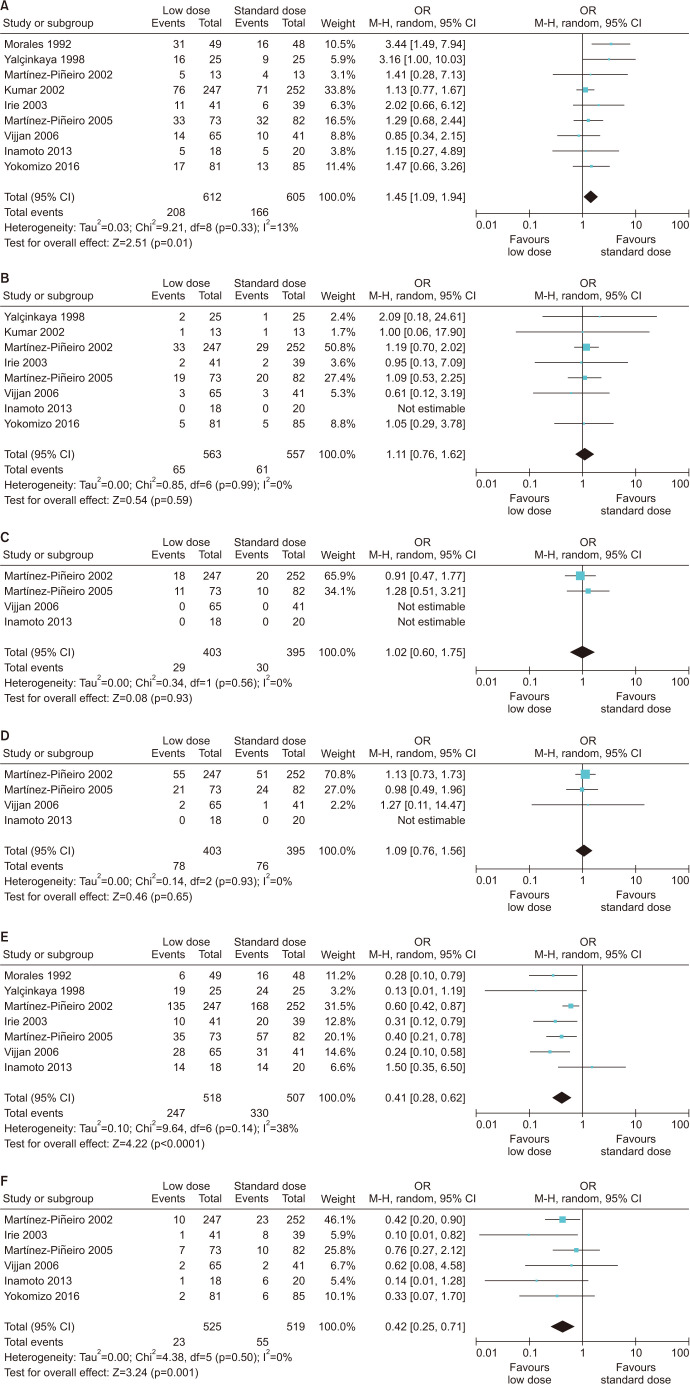
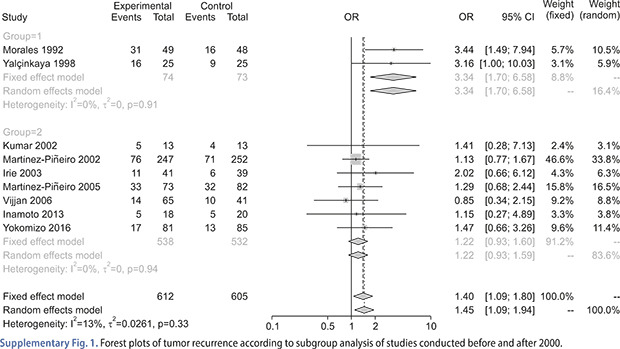
The results of recurrence were described in nine studies [10,11,12,13,14,15,16,17,18]. Among 612 patients in the low-dose group and 605 patients in the standard-dose group, 34.0% and 27.4%, respectively, experienced recurrence during follow-up. Compared with the standard dose, the low-dose group had a poorer recurrence rate (OR, 1.45; 95% CI, 1.09–1.94; p=0.01). There was low heterogeneity (p=0.33, I2=13%; Fig. 3A). The results of the meta-regression analysis indicated that studies conducted before 2000 had greater overall heterogeneity (p<0.01).
Fig. 3. Forest plots of (A) tumor recurrence, (B) tumor progression, (C) cancer-specific survival, (D) overall survival, (E) adverse effects, and (F) withdrawal.
5. Tumor progression
Although eight studies included progression, one study reported no progression events [13]. In the low-dose group, 11.5% of patients experienced progression compared with 11.0% in the standard-dose group. There was no significant difference between the groups (OR, 1.11; 95% CI, 0.76–1.62; p=0.59). There was no interstudy heterogeneity (p=0.99, I2=0%; Fig. 3B).
6. Cancer-specific survival
Although four studies surveyed cancer-specific survival, two studies did not [13,17]. In the low-dose group, 7.2% of patients died of bladder cancer compared with 7.6% in the standard-dose group. There was no significant difference between the groups (OR, 1.02; 95% CI, 0.60–1.75; p=0.93). There was no interstudy heterogeneity (p=0.56, I2=0%; Fig. 3C).
7. Overall survival
Although four studies surveyed overall survival, there was no assessment of overall survival in one study [13]. Among 403 patients in the low-dose group and 395 patients in the standard-dose group, 19.4% and 19.2% died during follow-up, respectively. There was no significant difference between the groups (OR, 1.09; 95% CI, 0.76–1.56; p=0.65) and no interstudy heterogeneity (p=0.93, I2=0%; Fig. 3D).
8. Adverse effects
Among seven studies, three [13,17,18] reported total adverse effects, and four studies [10,11,12,14] reported various adverse effects. Because the addition of various adverse effects could lead to overestimation of the total adverse effects, we selected one major local symptom in four studies [10,11,12,14]. Compared with the standard dose, a low dose could significantly reduce the rate of adverse effects (OR, 0.41; 95% CI, 0.28–0.62; p<0.0001). Moderate heterogeneity was observed (p=0.14, I2=38%; Fig. 3E).
9. Withdrawal
Six studies [11,12,13,14,15,17] reported the results of withdrawal from treatment. Among 525 patients in the low-dose group and 519 patients in the standard-dose group, 4.4% and 10.6% were reported to have withdrawn, respectively. Compared with the standard dose, a low dose could lead to a decrease in withdrawal (OR, 0.42; 95% CI, 0.25–0.71; p=0.001). There was no interstudy heterogeneity (p=0.50, I2=0%; Fig. 3F).
DISCUSSION
In our meta-analysis, treatment with low-dose BCG revealed a higher possibility of recurrence than did treatment with the standard dose. However, there were no significant differences in progression, cancer-specific survival, or overall survival between the two groups. Low-dose BCG revealed favorable outcomes in terms of adverse effects and withdrawal. Over four decades ago, Morales et al. [19] published an innovative study on adjuvant BCG intravesical instillation in NMIBC, and BCG instillation has since been accepted as the standard treatment [4]. In addition, maintenance BCG therapy has been proven to be more beneficial against recurrence than standard induction therapy, and guidelines recommend maintenance therapy [4,20]. Although the requirement for BCG has increased, the shortage of BCG has continued. Therefore, additional countermeasures are required.
Morales et al. [18] conducted an RCT on the potential of BCG dose reduction to reduce adverse effects. They found that the standard dose was favorable for recurrence, but that a low dose resulted in fewer adverse effects [18]. Yalçinkaya et al. [10] reported that low-dose BCG had the same adverse effect profile and a lower success rate for recurrence. However, in other studies, a low dose exhibited no significant recurrence rate compared with the standard dose [11,12,13,14,15,16,17]. According to our meta-regression analysis, the heterogeneity in results on recurrence might be related to the two studies conducted before 2000 by Morales et al. [18] and Yalçinkaya et al. [10]. Except for those two studies, rates of recurrence were similar between the low-dose and standard-dose groups (Supplementary Fig. 1). In the study by Morales et al. [18], the follow-up protocol was monitored more closely, and a different follow-up protocol would be related to the heterogeneity in recurrence. In addition, there was also a significant reduction in adverse effects at low doses in other studies [11,12,14,17]. These results are from studies using induction therapy, and maintenance therapy could have different outcomes. The European Organization for Research and Treatment of Cancer group performed an RCT of 1,355 patients, which revealed no significant differences in toxicity between the low and standard doses [21]. In that study, reducing the length of maintenance failed to prevent recurrence in high-risk patients [21]. As a result, maintenance therapy could suppress recurrence in high-risk patients. However, maintenance therapy requires induction therapy for 6 weeks and additional therapy for 3 weeks at 3, 6, 12, 18, 24, 30, and 36 months; therefore, 27 doses of BCG are required in total [20,21]. Miyake et al. [22] reported that approximately 77% of 2669 high-risk patients received non-maintenance therapy. Sharma et al. [23] reported reduced cost-effectiveness of maintenance therapy after induction therapy. These recent reports discuss the situation of BCG shortage and COVID-2019. The American Urological Association recommended the use of alternative chemotherapy in intermediate-risk patients or low-dose chemotherapy in high-risk patients in the setting of a BCG shortage [24].
An RCT was conducted to investigate reducing the frequency of BCG instillation in high-grade NMIBC [25]. However, the reduced protocol was inferior to the standard protocol in terms of recurrence; therefore, patient recruitment was terminated [25]. Although the frequency of BCG has been determined to a certain degree, the optimal BCG dose has not been established. Each strain has a standard dose for BCG instillation [26]. To date, there has been no definitive superiority among the available strains [26].
Many studies have been conducted to investigate enhancing the efficacy of BCG instillation. First, immune checkpoint inhibitors, which are an established treatment modality for cancer, could be combined with BCG. Wang et al. [27] reported that BCG could upregulate programmed death ligand-1 (PD-L1) on the surface of bladder cancer cells. In a breast cancer mouse model, the combination of BCG and anti-PD-L1 exhibited marked oncolytic effects using immunogenic mechanisms [28]. Second, there have been attempts to keep BCG longer in the bladder. Intravesical drug delivery devices can increase the time of exposure to the drug [29]. Hydrogels, which release drugs continuously, might extend time and efficacy, preventing washout by urination [30]. Third, genetically modified BCG strains could improve the immunotherapeutic effects of BCG. Recombinant BCG can evade the innate immune response of the host and increase the levels of antitumor cytokines [31]. Fourth, studies on increasing the invasion of BCG were conducted. Drug delivery systems such as nanocarriers or liposomes could promote endocytosis and the antitumor effects of BCG [32]. In the case of these upgraded tools, low-dose BCG can be used to reduce adverse effects. BCG has been the major treatment option for intermediate- and high-risk NMIBC for approximately the past 50 years, but the standard dose was provided empirically. Because of the BCG shortage, some patients would not be able to follow the usual protocol. Low-dose BCG could be an alternative strategy for more patients because it results in similar progression, cancer-specific survival, and overall survival and causes lower adverse effects and withdrawal compared with standard doses. High-quality RCTs will confirm the optimal dose.
This study has some limitations. First, the BCG strains varied among the studies. Over the decades, BCG subcultures have evolved genetically [33]. As a vaccine for tuberculosis, there was a concern that the different phenotypes related to the different surface proteins could influence the protective efficacy [34]. Ikeda et al. [35] reported that the Tokyo 172 and Connaught strains exhibited different binding abilities and interactions in an in vivo study. However, another study confirmed that the Tice, Connaught, and Armand Frappier strains have similar binding and antitumor activity [36]. Although several RCTs have been conducted to evaluate differences among the strains, the definitive superiority of any BCG strain has not been proven [37]. Second, the number of BCG instillations differed between the various studies. Different frequencies could have affected the results. However, there are still no definite instillation numbers. Our meta-regression analysis results indicated that studies based on BCG instillation numbers were not significantly different with respect to recurrence (p=0.11; Supplementary Fig. 2) and progression (p=0.72; Supplementary Fig. 3). In addition, since the same instillation number was used for both comparison groups, we believe that the impact on outcome would be minimal. Third, the statistical heterogeneity was moderate in terms of adverse effects and was caused by the use of different assessment criteria and reporting methods in each study.
CONCLUSIONS
In this meta-analysis, low-dose BCG had more unfavorable outcomes than standard BCG, but studies before 2000 were moderators in the recurrence of NMIBC. Tumor progression, cancer-specific survival, and overall survival were similar between the low and standard doses. Low-dose BCG was favorable for adverse effects and withdrawal. In the era of BCG shortage, low-dose BCG could have strong advantages with advanced technology as an alternative option. However, these results should be reinforced by large and well-designed RCTs to improve clinical outcomes.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING: This research was supported by a Chung-Ang University Research Grant in 2021.
- Research conception and design: Se Young Choi and Moon Soo Ha.
- Data acquisition: Jung Hoon Kim and Byung Hoon Chi.
- Statistical analysis: Se Young Choi and Moon Soo Ha.
- Data analysis and interpretation: Jin Wook Kim.
- Drafting of the manuscript: Se Young Choi and Moon Soo Ha.
- Critical revision of the manuscript: In Ho Chang, Tae-Hyoung Kim, and Soon Chul Myung.
- Obtaining funding: Se Young Choi.
- Administrative, technical, or material support: Se Young Choi.
- Supervision: Se Young Choi.
- Approval of the final manuscript: Se Young Choi.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4111/icu.20210340.
Forest plots of tumor recurrence according to subgroup analysis of studies conducted before and after 2000.
Forest plots of tumor recurrence according to subgroup analysis of bacille Calmette–Guérin instillation number.
Forest plots of tumor progression according to subgroup analysis of bacille Calmette–Guérin instillation number.
References
- 1.Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006;49:466–465. doi: 10.1016/j.eururo.2005.12.031. discussion 475-7. [DOI] [PubMed] [Google Scholar]
- 2.Fernandez-Gomez J, Madero R, Solsona E, Unda M, Martinez-Piñeiro L, Gonzalez M, et al. Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with bacillus Calmette-Guerin: the CUETO scoring model. J Urol. 2009;182:2195–2203. doi: 10.1016/j.juro.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Ehdaie B, Sylvester R, Herr HW. Maintenance bacillus Calmette-Guérin treatment of non-muscle-invasive bladder cancer: a critical evaluation of the evidence. Eur Urol. 2013;64:579–585. doi: 10.1016/j.eururo.2013.05.027. [DOI] [PubMed] [Google Scholar]
- 4.Witjes JA, Bruins HM, Cathomas R, Compérat EM, Cowan NC, Gakis G, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol. 2021;79:82–104. doi: 10.1016/j.eururo.2020.03.055. [DOI] [PubMed] [Google Scholar]
- 5.Pettenati C, Ingersoll MA. Mechanisms of BCG immunotherapy and its outlook for bladder cancer. Nat Rev Urol. 2018;15:615–625. doi: 10.1038/s41585-018-0055-4. [DOI] [PubMed] [Google Scholar]
- 6.Brausi M, Oddens J, Sylvester R, Bono A, van de Beek C, van Andel G, et al. Side effects of bacillus Calmette-Guérin (BCG) in the treatment of intermediate- and high-risk Ta, T1 papillary carcinoma of the bladder: results of the EORTC genito-urinary cancers group randomised phase 3 study comparing one-third dose with full dose and 1 year with 3 years of maintenance BCG. Eur Urol. 2014;65:69–76. doi: 10.1016/j.eururo.2013.07.021. [DOI] [PubMed] [Google Scholar]
- 7.Koch GE, Smelser WW, Chang SS. Side effects of intravesical BCG and chemotherapy for bladder cancer: what they are and how to manage them. Urology. 2021;149:11–20. doi: 10.1016/j.urology.2020.10.039. [DOI] [PubMed] [Google Scholar]
- 8.Katz A. Sanofi's halt of BCG production worries bladder cancer patients and urologists [Internet] Cranbury: OncLive; 2016. Dec 02, [cited 2021 May 7]. Available from: https://www.onclive.com/view/sanofis-halt-of-bcg-production-worries-bladder-cancer-patients-and-urologists. [Google Scholar]
- 9.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yalçinkaya F, Kamiş L, Ozteke O, Günlüsoy B, Yigitbaşi O, Ünal S. Prospective randomized comparison of intravesical BCG therapy with standard dose versus low doses in superficial bladder cancer. Int Urol Nephrol. 1998;30:41–44. doi: 10.1007/BF02550276. Erratum in: Int Urol Nephrol 1998;30:following 821. [DOI] [PubMed] [Google Scholar]
- 11.Martínez-Piñei JA, Flores N, Isorna S, Solsona E, Sebastián JL, Pertusa C, et al. Long-term follow-up of a randomized prospective trial comparing a standard 81 mg dose of intravesical bacille Calmette-Guérin with a reduced dose of 27 mg in superficial bladder cancer. BJU Int. 2002;89:671–680. doi: 10.1046/j.1464-410x.2002.02722.x. [DOI] [PubMed] [Google Scholar]
- 12.Martínez-Piñeiro JA, Martínez-Piñeiro L, Solsona E, Rodríguez RH, Gómez JM, Martín MG, et al. Has a 3-fold decreased dose of bacillus Calmette-Guerin the same efficacy against recurrences and progression of T1G3 and Tis bladder tumors than the standard dose? Results of a prospective randomized trial. J Urol. 2005;174(4 Pt 1):1242–1247. doi: 10.1097/01.ju.0000173919.28835.aa. [DOI] [PubMed] [Google Scholar]
- 13.Inamoto T, Ubai T, Nishida T, Fujisue Y, Katsuoka Y, Azuma H. Comparable effect with minimal morbidity of low-dose Tokyo 172 strain compared with regular dose Connaught strain as an intravesical bacillus Calmette-Guérin prophylaxis in nonmuscle invasive bladder cancer: results of a randomized prospective comparison. Urol Ann. 2013;5:7–12. doi: 10.4103/0974-7796.106873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Irie A, Uchida T, Yamashita H, Matsumoto K, Satoh T, Koh H, et al. Sufficient prophylactic efficacy with minor adverse effects by intravesical instillation of low-dose bacillus Calmette-Guérin for superficial bladder cancer recurrence. Int J Urol. 2003;10:183–189. doi: 10.1046/j.0919-8172.2003.00607.x. [DOI] [PubMed] [Google Scholar]
- 15.Yokomizo A, Kanimoto Y, Okamura T, Ozono S, Koga H, Iwamura M, et al. Randomized controlled study of the efficacy, safety and quality of life with low dose bacillus Calmette-Guérin instillation therapy for nonmuscle invasive bladder cancer. J Urol. 2016;195:41–46. doi: 10.1016/j.juro.2015.08.075. [DOI] [PubMed] [Google Scholar]
- 16.Kumar A, Dubey D, Bansal P, Mandhani A, Naik S. Urinary interleukin-8 predicts the response of standard and low dose intravesical bacillus Calmette-Guerin (modified Danish 1331 strain) for superficial bladder cancer. J Urol. 2002;168:2232–2235. doi: 10.1016/S0022-5347(05)64361-3. [DOI] [PubMed] [Google Scholar]
- 17.Vijjan V, Mandhani A, Kapoor R, Dubey D, Srivastava A, Ansari MS, et al. A randomized trial comparing low dose (40 or 80 mg) with standard dose (120 mg) of bacillus Calmette-Guerin for superficial bladder cancer. Indian J Urol. 2006;22:317–321. [Google Scholar]
- 18.Morales A, Nickel JC, Wilson JW. Dose-response of bacillus Calmette-Guerin in the treatment of superficial bladder cancer. J Urol. 1992;147:1256–1258. doi: 10.1016/s0022-5347(17)37532-8. [DOI] [PubMed] [Google Scholar]
- 19.Morales A, Eidinger D, Bruce AW. Intracavitary Bacillus Calmette-Guerin in the treatment of superficial bladder tumors. J Urol. 1976;116:180–183. doi: 10.1016/s0022-5347(17)58737-6. [DOI] [PubMed] [Google Scholar]
- 20.Lamm DL, Blumenstein BA, Crissman JD, Montie JE, Gottesman JE, Lowe BA, et al. Maintenance bacillus Calmette-Guerin immunotherapy for recurrent TA, T1 and carcinoma in situ transitional cell carcinoma of the bladder: a randomized Southwest Oncology Group Study. J Urol. 2000;163:1124–1129. [PubMed] [Google Scholar]
- 21.Oddens J, Brausi M, Sylvester R, Bono A, van de Beek C, van Andel G, et al. Final results of an EORTC-GU cancers group randomized study of maintenance bacillus Calmette-Guérin in intermediate- and high-risk Ta, T1 papillary carcinoma of the urinary bladder: one-third dose versus full dose and 1 year versus 3 years of maintenance. Eur Urol. 2013;63:462–472. doi: 10.1016/j.eururo.2012.10.039. [DOI] [PubMed] [Google Scholar]
- 22.Miyake M, Iida K, Nishimura N, Miyamoto T, Fujimoto K, Tomida R, et al. Non-maintenance intravesical Bacillus Calmette-Guérin induction therapy with eight doses in patients with high- or highest-risk non-muscle invasive bladder cancer: a retrospective non-randomized comparative study. BMC Cancer. 2021;21:266. doi: 10.1186/s12885-021-07966-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma V, Wymer KM, Borah BJ, Saigal CS, Litwin MS, Packiam VT, et al. Cost-effectiveness of maintenance bacillus Calmette-Guérin for intermediate and high risk nonmuscle invasive bladder cancer. J Urol. 2020;204:442–449. doi: 10.1097/JU.0000000000001023. [DOI] [PubMed] [Google Scholar]
- 24.American Urological Association. BCG shortage info [Internet] Linthicum: American Urological Association; 2020. [cited 2021 May 9]. Available from: https://www.auanet.org/about-us/bcg-shortage-info. [Google Scholar]
- 25.Grimm MO, van der Heijden AG, Colombel M, Muilwijk T, Martínez-Piñeiro L, Babjuk MM, et al. Treatment of high-grade non-muscle-invasive bladder carcinoma by standard number and dose of BCG instillations versus reduced number and standard dose of BCG instillations: results of the European Association of Urology Research Foundation randomised phase III clinical trial "NIMBUS". Eur Urol. 2020;78:690–698. doi: 10.1016/j.eururo.2020.04.066. [DOI] [PubMed] [Google Scholar]
- 26.Boehm BE, Cornell JE, Wang H, Mukherjee N, Oppenheimer JS, Svatek RS. Efficacy of bacillus Calmette-Guérin strains for treatment of nonmuscle invasive bladder cancer: a systematic review and network meta-analysis. J Urol. 2017;198:503–510. doi: 10.1016/j.juro.2017.01.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang YH, Cao YW, Yang XC, Niu HT, Sun LJ, Wang XS, et al. Effect of TLR4 and B7-H1 on immune escape of urothelial bladder cancer and its clinical significance. Asian Pac J Cancer Prev. 2014;15:1321–1326. doi: 10.7314/apjcp.2014.15.3.1321. [DOI] [PubMed] [Google Scholar]
- 28.Lu Y, Huang X, Liu X, He Y, Hu Z, Xu W, et al. Remodels the immunosuppressive tumor microenvironment by combination of bacillus Calmette-Guérin and anti-PD-L1 in an orthotopic triple-negative breast cancer mouse model. Onco Targets Ther. 2021;14:2247–2258. doi: 10.2147/OTT.S294129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cima MJ, Lee H, Daniel K, Tanenbaum LM, Mantzavinou A, Spencer KC, et al. Single compartment drug delivery. J Control Release. 2014;190:157–171. doi: 10.1016/j.jconrel.2014.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoon HY, Chang IH, Goo YT, Kim CH, Kang TH, Kim SY, et al. Intravesical delivery of rapamycin via folate-modified liposomes dispersed in thermo-reversible hydrogel. Int J Nanomedicine. 2019;14:6249–6268. doi: 10.2147/IJN.S216432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cho MJ, Kim MJ, Kim K, Choi YW, Lee SJ, Whang YM, et al. The immunotherapeutic effects of recombinant Bacillus Calmette-Guérin resistant to antimicrobial peptides on bladder cancer cells. Biochem Biophys Res Commun. 2019;509:167–174. doi: 10.1016/j.bbrc.2018.12.097. [DOI] [PubMed] [Google Scholar]
- 32.Whang YM, Yoon DH, Hwang GY, Yoon H, Park SI, Choi YW, et al. Liposome-encapsulated bacillus Calmette-Guérin cell wall skeleton enhances antitumor efficiency for bladder cancer in vitro and in vivo via induction of AMP-activated protein kinase. Cancers (Basel) 2020;12:3679. doi: 10.3390/cancers12123679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Behr MA. BCG--different strains, different vaccines? Lancet Infect Dis. 2002;2:86–92. doi: 10.1016/s1473-3099(02)00182-2. [DOI] [PubMed] [Google Scholar]
- 34.Leung AS, Tran V, Wu Z, Yu X, Alexander DC, Gao GF, et al. Novel genome polymorphisms in BCG vaccine strains and impact on efficacy. BMC Genomics. 2008;9:413. doi: 10.1186/1471-2164-9-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ikeda N, Honda I, Yano I, Koyama A, Toida I. Bacillus Calmette–Guerin Tokyo172 substrain for superficial bladder cancer: characterization and antitumor effect. J Urol. 2005;173:1507–1512. doi: 10.1097/01.ju.0000154354.06892.ba. [DOI] [PubMed] [Google Scholar]
- 36.Hudson MA, Ritchey JK, Catalona WJ, Brown EJ, Ratliff TL. Comparison of the fibronectin-binding ability and antitumor efficacy of various mycobacteria. Cancer Res. 1990;50:3843–3847. [PubMed] [Google Scholar]
- 37.D'Andrea D, Gontero P, Shariat SF, Soria F. Intravesical bacillus Calmette-Guérin for bladder cancer: are all the strains equal? Transl Androl Urol. 2019;8:85–93. doi: 10.21037/tau.2018.08.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plots of tumor recurrence according to subgroup analysis of studies conducted before and after 2000.
Forest plots of tumor recurrence according to subgroup analysis of bacille Calmette–Guérin instillation number.
Forest plots of tumor progression according to subgroup analysis of bacille Calmette–Guérin instillation number.