Key Points
Question
What were the trends in thyroid cancer incidence, mortality, and disability-adjusted life-years (DALYs) among the 15 pre-2004 European Union countries, the US, Australia, Canada, and Norway (EU15+) between 1990 and 2019?
Findings
This cross-sectional analysis used data extracted from the Global Burden of Disease Study database and identified decreasing trends in thyroid cancer mortality, DALYs, and mortality-to-incidence indexes for most EU15+ countries from 1990 to 2019; however, accompanying increases in thyroid cancer incidences have plateaued in the most recent trends. Australia, Denmark, and the US demonstrated unfavorable increases in both thyroid cancer mortality and DALYs.
Meaning
The trends in the disease burden from thyroid cancer between 1990 and 2019 are favorable for individuals in most EU15+ countries; however, these changes should be frequently observed to ensure they are not affected by differences in practice and risk factor prevalence, especially in countries displaying differential trends.
Abstract
Importance
The global incidence of thyroid cancer has been increasing rapidly, and this increase has had an attendant burden on health systems. However, it is unclear how the burden of this disease differs among the pre-2004 countries of the European Union (Austria, Belgium, Denmark, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden, and the UK), US, Australia, Canada, and Norway (EU15+).
Objective
To assess the trends in mortality, incidence, and disability-adjusted life-years (DALYs) associated with thyroid cancer between 1990 and 2019 in EU15+ nations. Data analysis was conducted from July 11 to October 11, 2021.
Design, Setting, and Participants
Observational cross-sectional analysis of the incidence of thyroid cancer was conducted using data obtained from the Global Burden of Disease Study database. Nineteen countries of the EU15+ were included.
Exposures
Thyroid cancer.
Main Outcomes and Measures
Age-standardized incidence rates (ASIRs), age-standardized mortality rates (ASMRs) and DALYs were extracted for individual EU15+ countries per sex for each of the years from 1990 to 2019, and mortality-to-incidence indexes were computed. Joinpoint regression analysis was used to describe the trends.
Results
Thirteen of 19 countries (68%) showed an average annual percentage change increase in ASIR across the study period (range, 0.2%-2.5%). Joinpoint regression analysis revealed largely plateauing ASIR trends in recent years across most EU15+ nations since 1990. Between 2011 and 2019, the estimated annual percentage change in the US was 0. Australia, Denmark, and the US were the only countries with increasing ASMR trends with positive average annual percentage changes: Australia, 0.6 (95% CI, 0.2-1.0); Denmark, 1.0 (95% CI, 0.8-1.3); and US, 0.4 (95% CI, 0.4-0.5); the remaining 16 countries showed negative trends (range, −0.2 to −2.1). Disability-adjusted life-years decreased in all EU15+ countries except Australia, Denmark, and the US.
Conclusions and Relevance
This cross-sectional analysis found that overall, the burden of thyroid cancer across EU15+ countries appears to be decreasing, evidenced by plateauing incidence rates and reductions in mortality and DALYs over the 30-year study period. However, the US and Australia appear to have increasing ASMR and DALY trends. Ongoing observation is required to monitor how changes in international clinical practice guidelines affect thyroid cancer DALYs and mortality.
This cross-sectional study examines trends among the European Union 15+ countries in the incidence and outcomes of thyroid cancer.
Introduction
Head and neck cancers have the fourth largest global incidence of all cancers.1 The incidence of thyroid cancer, the most common form of head and neck cancer, has increased over the past 50 years.2,3,4,5 The Global Cancer Observatory reported an estimate of 567 233 new cases of thyroid cancer and 41 071 deaths in 2018.1 Across high-income countries, the incidence increased by 19% from 1990 to 20136; this increase poses obvious challenges to health care systems worldwide. Early detection and intervention (active surveillance, surgery, or radioiodine treatment)7,8 improve case fatality but contribute to higher incidences.9
Thyroid cancer also poses a financial burden to health systems. In the US, its societal cost was $1.6 billion in 2013 and is expected to triple by 2030 to exceed $3.5 billion.10 A better understanding of the trends in the disease burden of thyroid cancer may help to inform future health-system planning. The measurement unit disability-adjusted life-year (DALY) has been used to quantify the burden of diseases, injuries, and risk factors on human populations to guide policies toward cost-effective and equitable health care.11,12,13,14
The main objective of this study was to compare the trends in thyroid cancer among the 15 pre-2004 countries of the European Union (Austria, Belgium, Denmark, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden, and the UK), the US, Australia, Canada, and Norway (EU15+). In the context of historically increasing incidence rates, we wanted to observe incidence and its outcomes associated with mortality and DALYs. The EU15+ was originally used to compare UK outcomes with those of high-income countries with similar or higher levels of health expenditure. Therefore, it represents a readily comparable group of 19 countries for observational analyses.15,16 Even though there exist differences in per capita cost expenditure by these countries, studies on Global Burden of Disease (GBD) analysis have shown that health expenditures in these countries are higher than or equal to UK expenditure, making it possible for internal comparison.17,18 We used data obtained from the GBD Study to assess the trends in thyroid cancer mortality, incidence, and DALYs between 1990 and 2019 among these comparable countries.4 Joinpoint regression analysis was used to describe the trend changes in mortality, incidence, and DALY rates and to identify significant trends over the time studied. To our knowledge, no such recent analysis comparing trends in this cohort of countries has been performed.
Methods
Characteristics of the Data Source
This observational analysis of thyroid cancer among EU15+ countries was performed using data from the GBD database. This World Health Organization–commissioned database is an amalgamation of 127 countries’ data sets and registries that provide epidemiological characteristics (eg, incidence, prevalence, mortality, DALYs, years of life lost) for some of the world’s most important health concerns. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Previous publications describe the exact GBD methods in greater detail,14,19 and data from the GBD database have been used to describe trends in the disease burden of type 2 diabetes,20 peripheral arterial disease,16 abdominal aortic aneurysm,21 and lower extremity amputation.22 Data sets used by the GBD researchers include disease registries, insurance data, admission and outpatient encounter data, and systematic reviews among others. For thyroid cancer data, the GBD maps all mortality and incidence data related to the International Statistical Classification of Diseases, 10th Revision (ICD-10) (codes C73-C73.9, D09.3, D09.8, D34-D34.9, D44.0) and the International Classification of Diseases, 9th Revision (ICD-9) (codes 193-193.9, 226-226.9).2,3,23 These data are then combined by bayesian meta-regression with the DisMod-MR 2.19 tool3 that analyzes, adjusts for bias, and produces disease estimates with 95% CIs. The GBD database has different mappings of ICD codes based on incidence or mortality. In brief, generally for incidence of thyroid cancer, the GBD excludes most benign codes, but for mortality it includes many benign codes under the assumption that if a tumor was assigned a benign code but led to death, it was likely misclassified. Based on this method, the GBD database includes D34 (ICD-10) and 226 (ICD-9) codes for thyroid cancer considering that if it led to death, it was likely misclassified instead of being correctly classified using the ICD codes of malignant disease.
Mortality data are collected from vital registration sources, verbal autopsy reports, and surveillance data, and entered into the GBD cause-of-death database. The quality of mortality data from each country is then rated by the GBD authors using a star rating system (0-5 stars) by location year to assist the reader’s comprehension of the reliability of the cause of death data. Ten of 19 EU15+ countries score 5 stars for each location year (representing 85%-100% completeness of mortality data), and the remaining 9 countries score 4 stars (65%-84% completeness of mortality data).
Handling of the GBD Data
We extracted age-standardized incidence rates (ASIRs), age-standardized mortality rates (ASMRs), and DALYs for thyroid cancer from EU15+ countries between 1990 and 2019 using the dedicated GBD Study results tool.24 Age-standardized rates are used to account for the age structures of each country. The method used by the GBD involves calculating a standard population from the United Nations Population Division World Population Prospects 2012 revision.25
We calculated absolute and relative changes in ASIRs, ASMRs, and DALYs from 1990 and 2019 for each sex in each country. We computed mortality-to-incidence indexes by dividing ASMRs by ASIRs for each year (1990 and 2019) for both sexes in all EU15+ countries. Mortality-to-incidence indexes allow for the comparison of disease burden by normalizing mortality to incidence. A DALY incorporates morbidity and mortality figures to calculate the number of years lived with and lost from a disability (ie, a higher DALY represents more good life-years lost due to disability). Disability-adjusted life-years are used by the GBD and World Health Organization to indicate the overall burden of disease on a health system11 and provide a single figure to determine this. However, DALYs have a variety of shortcomings.12,13,26 Years lived with disability scores are based on ratings from an expert panel and therefore DALYs incorporate subjectivity. Moreover, these ratings are based on health states in high-income nations and therefore may not reflect the health states in countries with differential resources. We have used DALYs along with ASIRs, ASMRs, and mortality-to-incidence indexes as measures to facilitate our understanding of the varying temporal disease burden of thyroid cancer across countries. Global and EU mean trends in each parameter assessed are also reported for comparison.
Statistical Analysis
Data analysis was conducted from July 11 to October 11, 2021. Joinpoint Command Line, version 4.9.0.0, was used to apply a joinpoint regression analysis to the incidence, mortality, and DALY data (provided free by the US National Cancer Institute Surveillance Research Program).27 The software observes trends in the data over the time period studied and connects these trends with the simplest model possible on a logarithmic scale, therein producing periods of time during which significant trend changes have been identified. The simplest model has no joinpoints and represents a straight line. As more joinpoints are added, each is tested for significance using a Monte Carlo permutation method. An estimated annual percentage change with 95% CIs for each joinpoint line segment is also computed by the Joinpoint Command Line software and tested for significance based on 95% CIs. Statistical significance was determined by whether the 95% CI was on either side of 1. The result of the analysis is a series of statistically significant joinpoints for each country, with each trend (either positive or negative) represented by a potentially significant estimated annual percentage change. This process is useful for thorough assessment of temporal trends and allows for intercountry comparability. The model also computes an average annual percentage change (AAPC) for each country, which provides a single summary number for the trend over the past 30 years.
Results
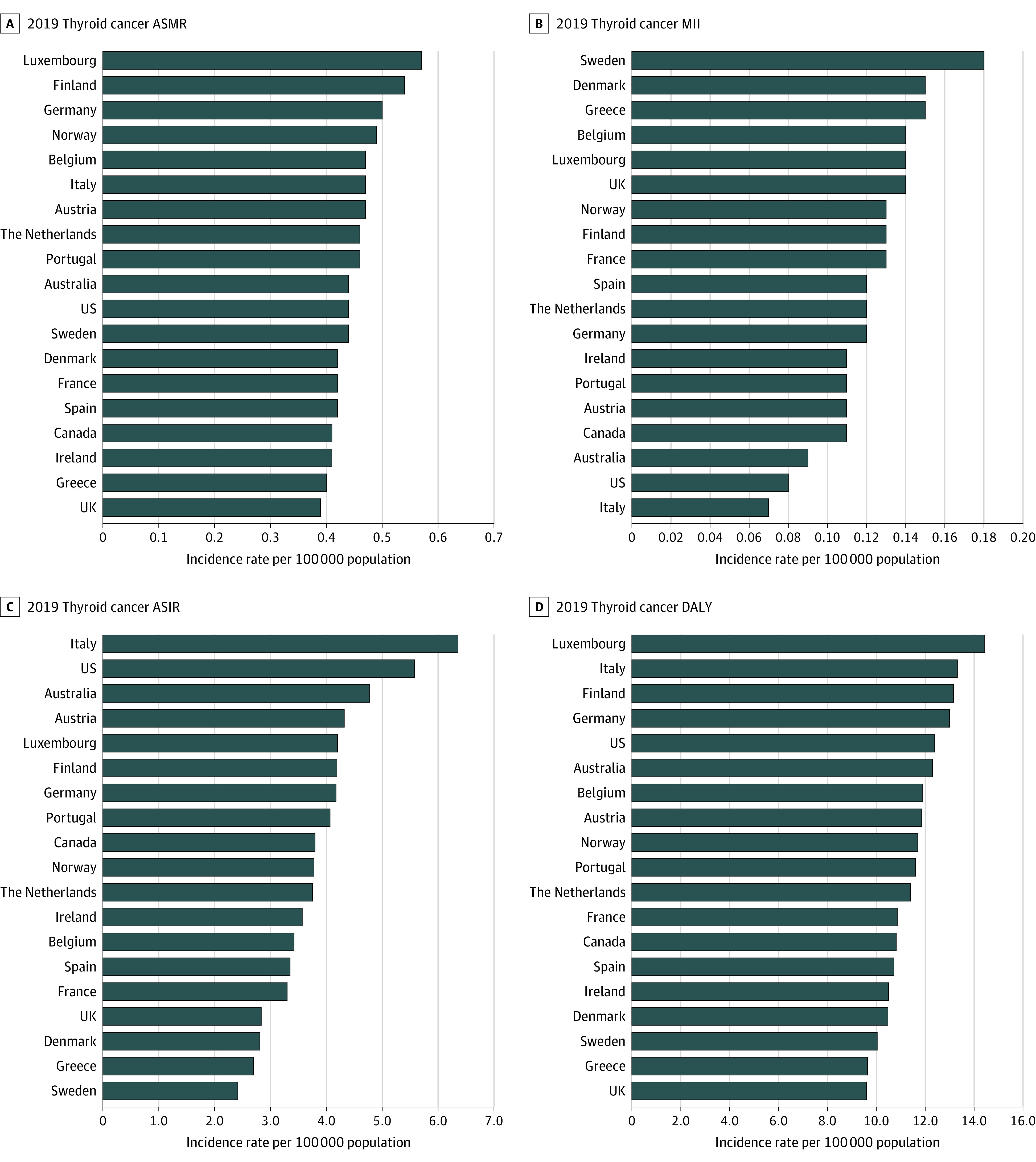
We observed the incidence rates of thyroid cancer in 2019 (Figure 1) as well as yearly changes in thyroid cancer mortality, incidence, mortality-incidence index, and DALYs across the EU15+ countries over the 30-year study period.
Figure 1. Age-Standardized Incidence Rates (ASIRs), Age-Standardized Mortality Rates (ASMRs), Mortality Incidence Index (MII), and Disability-Adjusted Life-years (DALYs) From Thyroid Cancer Across the 19 Countries.
Incidence Trends
Age-standardized incidence rates for EU15+ countries are described in the Table and Figure 2. In 2019, ASIRs were highest in Italy (6.36; 95% CI, 5.07-7.85 per 100 000 population) and second highest in the US (5.59; 95% CI, 4.78-6.53 per 100 000 population). The Table displays trends in ASIRs from 1990 to 2019. Thirteen of 19 countries showed an average annual percentage increase in ASIR across the study period. Australia (2.5; 95% CI, 2.3-2.7 per 100 000 population) and the US (1.2; 95% CI, 1.0-1.3 per 100 000 population) had the highest AAPC of EU15+ countries. Joinpoint regression analysis revealed largely plateauing trends in recent years across the majority of EU15+ nations since 1990 as evidenced by a range of −0.8 to 0.8 per 100 000 in the most recent joinpoint period to 2019 (eTable 1 in the Supplement). Sex-specific trends in ASIR can be found in eTables 2, 3, and 4 in the Supplement. There was a significant decrease in the ASIR of thyroid cancer in women in the US between 2009 and 2019 (−0.4; 95% CI, −0.7 to −0.2 per 100 000 population) (eTable 3 in the Supplement).
Table. 1990 and 2019 Incidence Rates for Thyroid Cancer in the EU15+ Countries.
| Country | Incidence rate, per 100 000 population (95% CI) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASIR | ASMR | MIIs | DALY | |||||||||
| Both sexes | 1990 | 2019 | % Change | 1990 | 2019 | % Change | 1990 | 2019 | % Change | 1990 | 2019 | % Change |
| Global | 2.01 (1.89 to 2.12) | 2.83 (2.55 to 3.06) | 0.289 | 0.59 (0.56 to 0.65) | 0.56 (0.51 to 0.60) | –0.05 | 0.29 (0.29 to 0.30) | 0.20 (0.19 to 0.20) | –0.3 | 15.55 (14.40 to 17.02) | 14.98 (13.55 to 16.13) | –0.03 |
| Australia | 2.46 (2.25 to 2.71) | 4.79 (3.63 to 6.29) | 0.484 | 0.40 (0.37 to 0.43) | 0.44 (0.37 to 0.48) | 0.081 | 0.16 (0.16 to 0.16) | 0.09 (0.07 to 0.10) | –0.4 | 10.60 (9.825 to 11.55) | 12.31 (10.54 to 14.13) | 0.138 |
| Austria | 5.15 (4.52 to 5.71) | 4.32 (3.38 to 5.50) | –0.18 | 0.83 (0.73 to 0.89) | 0.47 (0.40 to 0.52) | –0.76 | 0.16 (0.15 to 0.16) | 0.10 (0.09 to 0.12) | –0.3 | 20.39 (18.03 to 22.19) | 11.88 (10.40 to 13.61) | –0.71 |
| Belgium | 3.61 (3.19 to 3.99) | 3.43 (2.60 to 4.39) | –0.05 | 0.98 (0.88 to 1.06) | 0.47 (0.42 to 0.52) | –1.07 | 0.27 (0.26 to 0.27) | 0.13 (0.11 to 0.16) | –0.4 | 20.88 (18.71 to 22.48) | 11.91 (10.41 to 13.58) | –0.75 |
| Denmark | 1.50 (1.35 to 1.72) | 2.82 (2.14 to 3.69) | 0.465 | 0.33 (0.30 to 0.39) | 0.42 (0.36 to 0.47) | 0.211 | 0.22 (0.22 to 0.22) | 0.15 (0.12 to 0.17) | –0.3 | 8.568 (7.865 to 10.19) | 10.50 (9.065 to 11.91) | 0.184 |
| Finland | 3.13 (2.84 to 3.44) | 4.20 (3.19 to 5.44) | 0.254 | 0.68 (0.63 to 0.73) | 0.53 (0.46 to 0.59) | –0.28 | 0.21 (0.21 to 0.22) | 0.12 (0.10 to 0.14) | –0.4 | 16.36 (15.13 to 17.68) | 13.16 (11.37 to 15.00) | –0.24 |
| France | 3.23 (2.95 to 3.51) | 3.31 (2.49 to 4.30) | 0.023 | 0.75 (0.68 to 0.80) | 0.42 (0.36 to 0.47) | –0.79 | 0.23 (0.22 to 0.23) | 0.12 (0.10 to 0.14) | –0.4 | 17.86 (16.68 to 18.97) | 10.88 (9.513 to 12.44) | –0.64 |
| Germany | 3.97 (2.57 to 4.31) | 4.18 (3.13 to 5.55) | 0.050 | 0.81 (0.73 to 0.86) | 0.50 (0.44 to 0.55) | –0.61 | 0.20 (0.19 to 0.20) | 0.12 (0.09 to 0.14) | –0.4 | 19.93 (17.65 to 21.20) | 13.00 (11.52 to 14.66) | –0.53 |
| Greece | 2.30 (2.08 to 2.50) | 2.70 (2.08 to 3.53) | 0.149 | 0.57 (0.52 to 0.62) | 0.40 (0.36 to 0.43) | –0.43 | 0.25 (0.24 to 0.24) | 0.14 (0.12 to 0.17) | –0.4 | 12.18 (11.21 to 13.09) | 9.661 (8.649 to 10.82) | –0.26 |
| Ireland | 2.56 (2.28 to 2.83) | 3.58 (2.63 to 4.75) | 0.284 | 0.59 (0.53 to 0.64) | 0.41 (0.34 to 0.46) | –0.46 | 0.23 (0.22 to 0.23) | 0.11 (0.09 to 0.13) | –0.5 | 14.35 (13.02 to 15.49) | 10.51 (8.779 to 12.32) | –0.36 |
| Italy | 6.66 (6.04 to 7.20) | 6.36 (5.07 to 7.85) | –0.04 | 0.73 (0.68 to 0.75) | 0.47 (0.41 to 0.51) | –0.54 | 0.10 (0.10 to 0.11) | 0.07 (0.06 to 0.08) | –0.3 | 20.13 (18.17 to 21.54) | 13.32 (11.61 to 15.10) | –0.51 |
| Luxembourg | 4.32 (3.85 to 4.74) | 4.21 (3.36 to 5.30) | –0.02 | 1.03 (0.94 to 1.10) | 0.57 (0.48 to 0.68) | –0.79 | 0.23 (0.23 to 0.24) | 0.13 (0.12 to 0.14) | –0.4 | 24.80 (22.60 to 26.83) | 14.46 (12.16 to 17.60) | –0.71 |
| The Netherlands | 2.57 (2.33 to 2.83) | 3.76 (2.81 to 4.92) | 0.315 | 0.50 (0.45 to 0.53) | 0.46 (0.39 to 0.51) | –0.08 | 0.19 (0.18 to 0.19) | 0.12 (0.10 to 0.13) | –0.3 | 12.11 (10.99 to 13.02) | 11.42 (9.544 to 13.04) | –0.06 |
| Norway | 2.77 (2.56 to 3.02) | 3.78 (3.14 to 4.53) | 0.267 | 0.54 (0.51 to 0.57) | 0.48 (0.43 to 0.52) | –0.11 | 0.19 (0.18 to 0.19) | 0.12 (0.11 to 0.13) | –0.3 | 13.36 (12.72 to 14.24) | 11.71 (10.54 to 12.98) | –0.14 |
| Portugal | 3.73 (3.32 to 4.12) | 4.07 (3.01 to 5.31) | 0.082 | 0.93 (0.83 to 1.01) | 0.45 (0.40 to 0.51) | –1.04 | 0.25 (0.24 to 0.25) | 0.11 (0.09 to 0.13) | –0.5 | 19.79 (18.00 to 21.23) | 11.61 (10.09 to 13.29) | –0.70 |
| Spain | 2.59 (2.31 to 2.81) | 3.36 (2.55 to 4.42) | 0.229 | 0.52 (0.48 to 0.56) | 0.41 (0.35 to 0.46) | –0.26 | 0.20 (0.19 to 0.20) | 0.12 (0.10 to 0.13) | –0.3 | 13.51 (12.21 to 14.41) | 10.73 (9.051 to 12.27) | –0.25 |
| Sweden | 2.16 (1.99 to 2.37) | 2.41 (1.98 to 2.90) | 0.105 | 0.58 (0.53 to 0.62) | 0.43 (0.39 to 0.47) | –0.33 | 0.26 (0.26 to 0.26) | 0.18 (0.16 to 0.19) | –0.3 | 12.77 (11.91 to 13.75) | 10.05 (9.173 to 11.01) | –0.27 |
| UK | 2.17 (2.05 to 2.27) | 2.84 (2.33 to 3.41) | 0.234 | 0.45 (0.42 to 0.47) | 0.38 (0.35 to 0.41) | –0.16 | 0.20 (0.20 to 0.20) | 0.13 (0.12 to 0.15) | –0.3 | 10.92 (10.23 to 11.56) | 9.63 (8.99 to 10.45) | –0.13 |
| Canada | 3.01 (2.72 to 3.31) | 3.81 (2.88 to 4.92) | 0.210 | 0.43 (0.40 to 0.46) | 0.41 (0.36 to 0.45) | –0.05 | 0.14 (0.14 to 0.14) | 0.10 (0.09 to 0.12) | –0.2 | 11.38 (10.54 to 12.29) | 10.83 (9.480 to 12.27) | –0.05 |
| US | 4.06 (3.91 to 4.18) | 5.59 (4.78 to 6.53) | 0.272 | 0.38 (0.36 to 0.40) | 0.43 (0.39 to 0.45) | 0.109 | 0.09 (0.09 to 0.09) | 0.07 (0.06 to 0.08) | –0.1 | 11.02 (10.21 to 11.87) | 12.39 (11.24 to 13.54) | 0.110 |
Abbreviations: ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; DALY, disability-adjusted life-year; EU15+, countries comprising the European Union pre-2004, US, Australia, Canada, and Norway; MIIs, mortality to incidence indexes.
Figure 2. Trends in Age-Standardized Incidence Rate (ASIR) per 100 000 Population for Thyroid Cancer Globally and in EU15+ Countries Between 1990-2019.
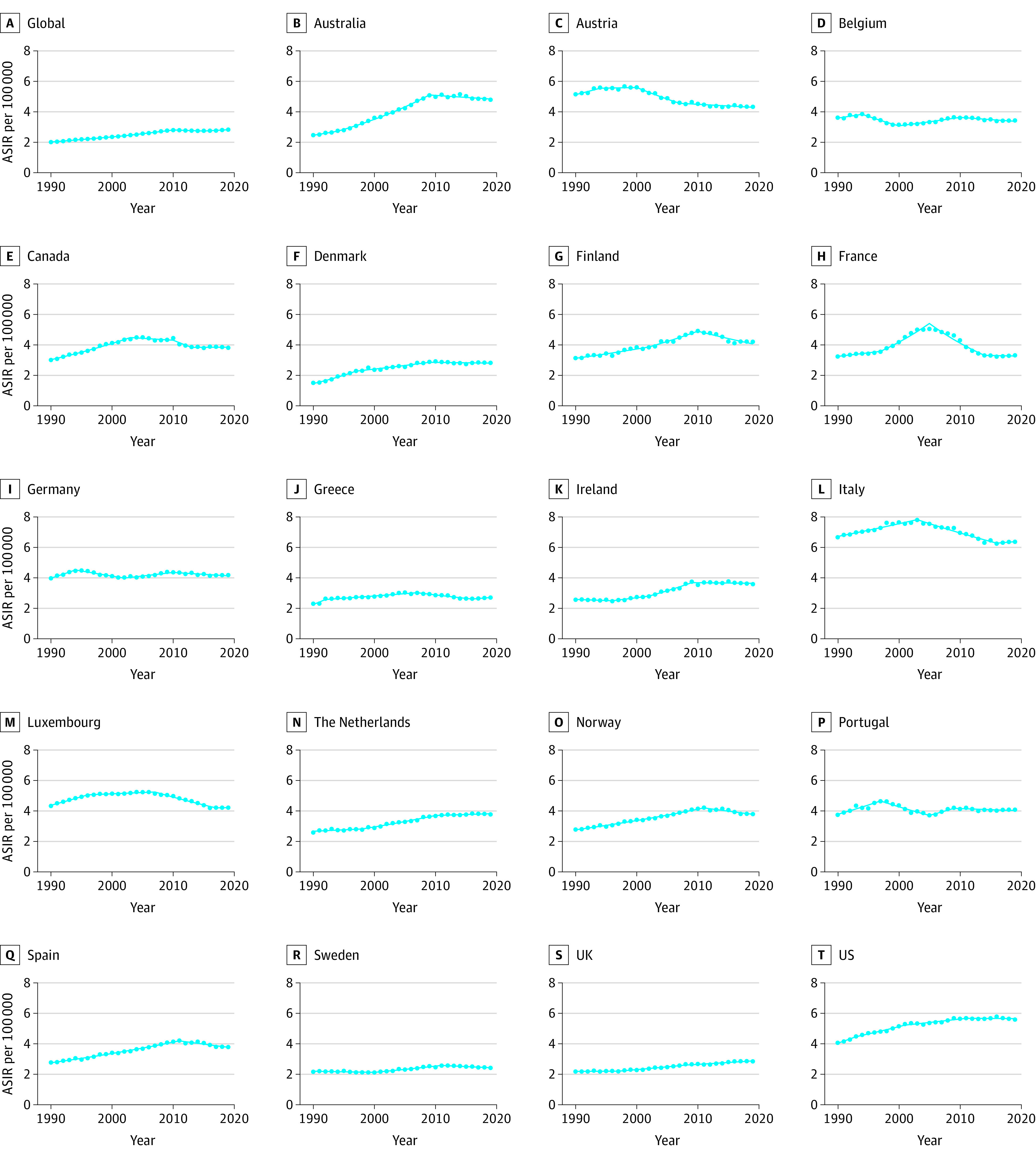
EU15+ indicates the countries of the European Union pre-2004, comprising Austria, Belgium, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden, the UK, as well as the US, Australia, Canada, and Norway.
Mortality Trends
Age-standardized mortality rates for EU15+ countries are also displayed in the Table and Figure 3. In 2019, ASMRs ranged from 0.40 (95% CI, 0.36-0.43 per 100 000 population) in Greece to 0.57 (95% CI, 0.48-0.68 per 100 000 population) in Luxembourg. The ASMR of the US was 0.43 (95% CI, 0.39-0.45 per 100 000 population) in 2019. In 2019, The UK had the lowest ASMR (0.38; 95% CI, 0.35-0.41 per 100 000 population). The data in eTable 5 in the Supplement describe the trends in ASMR over 30 years. Australia, Denmark, and the US were the only countries with positive AAPC changes; the remaining 16 countries had a negative AAPC. In the most recent joinpoint period to 2019, Denmark (−1.5; 95% CI, −2.0 to −1.1 per 100 000 population) and Australia (−1.2; 95% CI, −1.6 to −0.8 per 100 000 population) had reducing ASMR trends; in the US (0.2; 95% CI, 0.1-0.3 per 100 000 population), the trend was increasing. Australia, Denmark, and the US were also the only countries with increasing ASMR trends with positive average annual percentage changes: Australia, 0.6 (95% CI, 0.2-1.0); Denmark, 1.0 (95% CI, 0.8-1.3); and the US, 0.4 (95% CI, 0.4-0.5); the remaining 16 countries showed negative trends (range, −0.2 to −2.1). Sex-specific trends in ASMR can be found in eTables 2, 3, and 6 in the Supplement.
Figure 3. Trends in Age-Standardized Mortality Rate (ASMR) per 100 000 Population for Thyroid Cancer Globally and in EU15+ Countries Between 1990-2019.
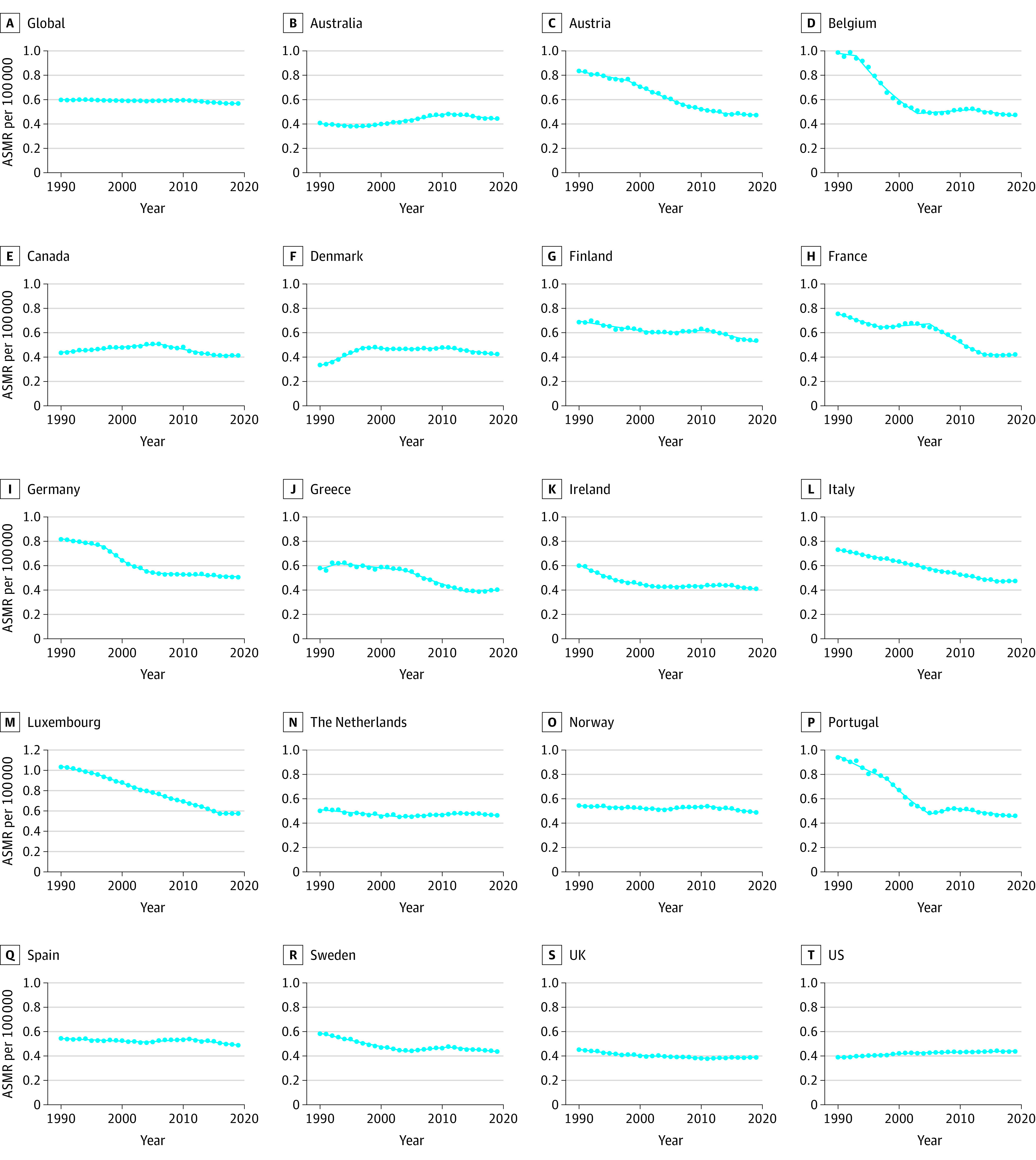
EU15+ indicates the countries of the European Union pre-2004, comprising Austria, Belgium, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden, the UK, as well as the US, Australia, Canada, and Norway.
DALY Trends
Age-standardized DALY rates between 1990 and 2019 are reported in the Table and Figure 4. In 2019, the DALYs of EU15+ nations ranged from 9.63 (95% CI, 8.99-10.45 per 100 000 population) in the UK to 14.46 (95% CI, 12.16-17.60 per 100 000 population) in Luxembourg. eTable 7 in the Supplement reports DALY trends from 1990 to 2019. DALYs decreased in all EU15+ countries except Australia, Denmark, and the US. In the most recent joinpoint period to 2019, a downward DALY trend was seen in Australia (−0.8; 95% CI, −1.1 to −0.6 per 100 000 population) and Denmark (−1.3; 95% CI, −1.7 to −0.9 per 100 000 population). A plateau in DALYs was noted in the US (0.1; 95% CI, 0-0.2 per 100 000 population). Sex-specific trends in DALYs can be found in eTables 2 and 3 in the Supplement.
Figure 4. Trends in Disability-Adjusted Life-years (DALYs) per 100 000 Population for Thyroid Cancer in EU15+ Countries Between 1990-2019.
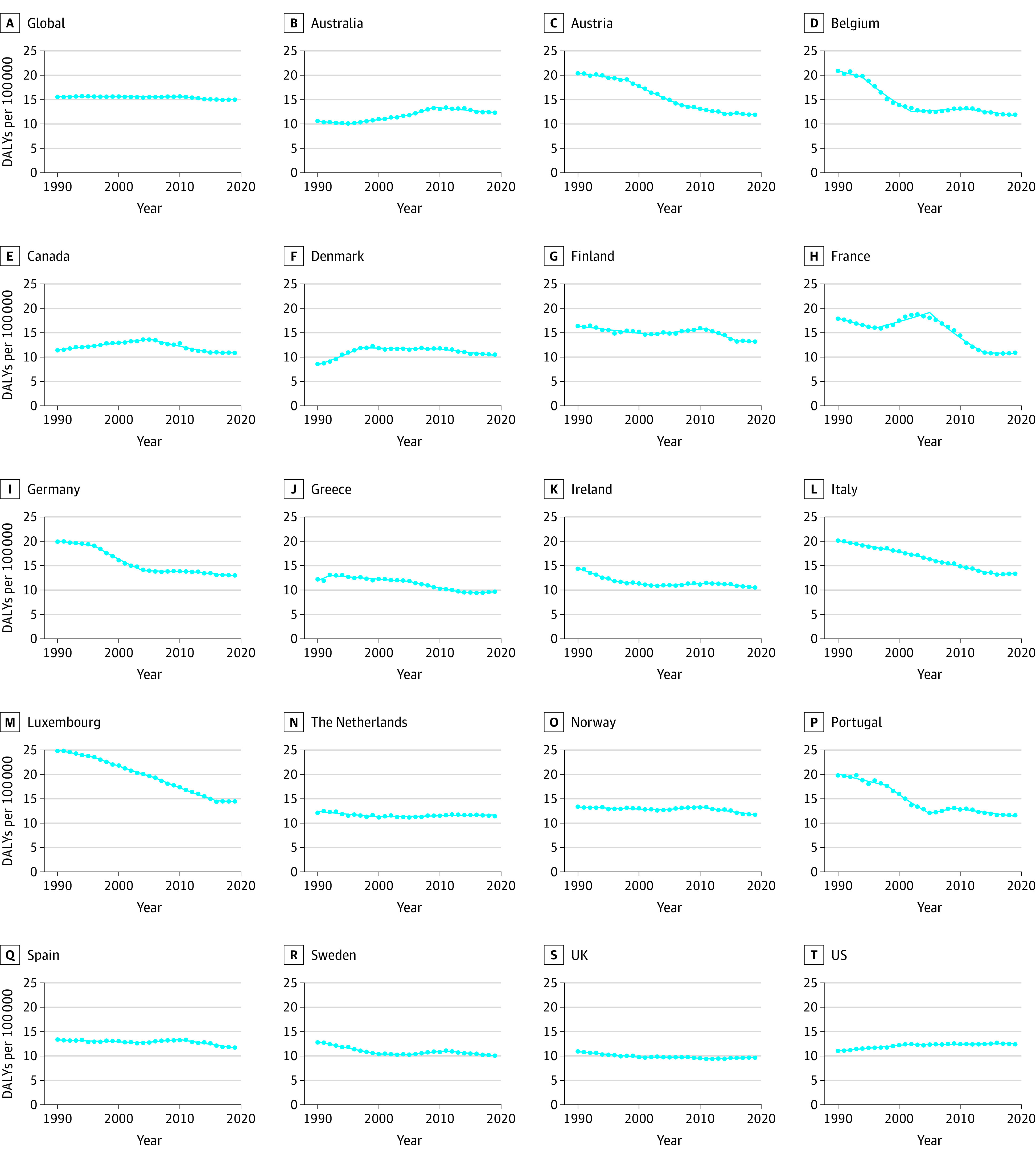
EU15+ indicates the countries of the European Union pre-2004, comprising Austria, Belgium, Finland, France, Germany, Greece, Ireland, Italy, Luxembourg, Netherlands, Portugal, Spain, Sweden, the UK, as well as the US, Australia, Canada, and Norway.
Discussion
To our knowledge, this is the first study to compare 30-year trends in thyroid cancer mortality, incidence, and DALYs across EU15+ countries using data obtained from the GBD Study. Our primary aim was to assess trends in thyroid cancer burden in the EU15+ nations, which have comparable health infrastructure and data availability. We found country-specific variability across all disease burden parameters assessed. However, overall, we identified improvements in thyroid cancer mortality and DALYs, but overall increases in thyroid cancer incidence in EU15+ countries over the past 3 decades.
Our findings of increasing thyroid cancer incidence trends in countries within the EU15+ are consistent with previous reports that used data derived from alternative sources.1,5,9 It has been widely suggested that improvements in diagnostic techniques, such as ultrasonography, computed tomography, and histopathologic testing, are significant contributors to the increasing incidence rates of thyroid cancer28,29,30 because they detect large numbers of slow-growing, subclinical papillary thyroid cancers—1 of 4 thyroid cancer subtypes.5 In South Korea, where there is a screening program for thyroid cancer, Park et al31 found that ASIR increased from 6.4 in 1999 to 40.7 in 2008. This incidence was not proportionally associated with mortality rates. It has therefore been suggested that an increase in the diagnosis of subclinical disease has inflated the data to look more substantial than the clinical reality.9,32
In this study, we found the US and Italy to have the highest ASIR in 2019. The concern for countries with high incidence is the surveillance burden of disease that does not affect mortality. Modeling based on previous estimates predict the societal cost of thyroid cancer in the US to triple by 2030.10 To address the historic increase in thyroid cancer incidence, the American Thyroid Association revised their clinical practice guidelines in 200933 and again in 2015.7 The 2009 clinical practice guidelines recommended less-aggressive diagnostic criteria, especially for ultrasonography-guided fine-needle aspiration, and a more conservative outlook on the management of thyroid cancer was introduced in 2015.7
To our knowledge, the present analysis is the first time that decreasing thyroid cancer incidence rates have been reported in US women, which may reflect the policy changes introduced in the US by the American Thyroid Association. The plateauing of overall thyroid cancer ASIRs seen over recent times in the US is mirrored in the majority of EU15+ nations, reflecting the possible global impact of these American Thyroid Association guidelines.
Overdiagnosis alone is unlikely to account entirely for incidence trends.32 Estimates using the Surveillance, Epidemiology and End Results–9 database suggest comparable increases in incidence between advanced papillary thyroid cancer (3.5% per year) and thyroid cancer overall (3.6% per year).5,9 The mortality rate of advanced papillary thyroid cancer also increased at a greater rate in relation to all thyroid cancers.9 This increase in true disease is attributed to certain environmental risk factors for thyroid cancer associated with a Western lifestyle, which include obesity, food fertilized with nitrates, and smoking.2,34,35
To our knowledge, this is the first study to report trends in DALY figures across EU15+ countries for thyroid cancer that is based on mortality and morbidity data.11 We found improving DALYs across most EU15+ countries, except the US, Denmark, and Australia, suggesting that the years lived with disability and the years of life lost from thyroid cancer are increasing in these 3 countries.
The EU15+ countries with increasing DALYs (US, Australia, and Denmark) were observed to be the only nations to have differential ASMR trends from the rest of the EU15+. In the context of the more-conservative treatment guidelines and a reported increase in true disease,7,9 it is important to closely observe mortality and DALYs over the coming years to ensure optimum thyroid cancer management in these nations. It is essential the balance is struck between avoiding overdiagnosis and incorrectly managing true disease.
Limitations
This study has limitations. The GBD Study collaborators are transparent with regard to the limitations of using the GBD database,23 and these limitations have been previously discussed in detail.15,16 New limitations specific to the present analysis include alterations in data-coding systems and country-specific practice, including a transition from ICD-9 to ICD-10 over the study period. By mapping mortalities to causes of death lists, we attempted to adjust for the different coding systems. Second, variability exists both within and across countries in the accuracy of death certification. Errors in death certification range from 39% to 61% worldwide,36,37,38 and only 39% of deaths globally were registered in 2012. However, the top-performing continents regarding civil registration and vital statistics were Europe, the Americas, and Australasia,39 which augments the reliability of the data presented from EU15+ countries in this study. The GBD uses underregistration corrections and garbage-code distribution algorithms to adjust for underregistration.14,19 Garbage codes relate to deaths denoted to result from poorly defined diagnoses or those that cannot be the single underlying cause of death. Third, data subcategorized by individual thyroid cancer histological subtypes cannot be extracted from the GBD Study results tool; we are mindful that histopathological subtypes as well as stages of thyroid cancer can have differing clinical importance and are managed with different urgency.40 This fact must be considered when interpreting these data. Also, the ICD coding for mortality includes D34 (ICD-10) and 226 (ICD-9) which represent benign diseases, although if they led to death, the cause was likely misclassified instead of ICD codes of malignant disease. For incidence, GBD excludes most benign codes. The incidence rates observed in the US in the present analysis (inclusive of 2019) were markedly lower than those previously reported elsewhere from the World Health Organization and Surveillance, Epidemiology and End Results–9 databases. The latter study found incidence rates for all thyroid histotypes in 2013 to be 7.98 per 100 000.1,5,9 Using the GBD database, we observed the ASIR for thyroid cancer in 2019 to be 5.59 per 100 000. One reason for this difference is that the GBD database uses estimates from a variety of sources to produce its figures. This allows robust estimates of trends in global regions that do not have reliable data sets, like the Surveillance, Epidemiology and End Results–9 database. Although there is a difference in the absolute rates, the GBD database is a valuable resource to identify and compare the trends in thyroid cancer disease burden among nations. In addition, this was an observational analysis and thus there are no causal inferences. As with all observational analyses, there are likely contributory confounders that are not fully accounted for by using sex-specific, age-standardized incidence and mortality rates.
Conclusions
We report overall increases in the burden of thyroid cancer across the majority of EU15+ countries between 1990 and 2019, evidenced by plateaus in incidence rates and reductions in mortality and DALY rates. However, in a number of countries, including the US, there are unfavorable increasing mortality and DALY trends over this time period. Close observation of future time trends in thyroid cancer disease burden should be performed in the context of recent changes in international clinical practice guidelines, which have suggested more conservative diagnostic and management strategies.
eTable 1. Joinpoint Analysis for Thyroid Cancer Age-Standardized Incidence Rates in EU15+ Countries for Years 1990-2019 for Both Sexes
eTable 2. 1990 and 2019 Male Age-Standardized Mortality Rates (ASMRS), Age-Standardized Incidence Rates (ASIRs), Mortality-to-Incidence Indices (MIIs) and Disability-Adjusted Life Years (DALYS), With Associated Percentage Changes, for Thyroid Cancer in the European Union 15+ Countries
eTable 3. 1990 and 2019 Female Age-Standardized Mortality Rates (ASMRS), Age-Standardized Incidence Rates (ASIRs), Mortality-to-Incidence Indices (MIIs) and Disability-Adjusted Life Years (DALYS), With Associated Percentage Changes, for Thyroid Cancer in the European Union 15+ Countries
eTable 4. Joinpoint Analysis for Thyroid Cancer Age-Standardized Incidence Rates in EU15+ Countries for Years 1990-2019 in Males, Females
eTable 5. Joinpoint Analysis for Thyroid Cancer Age-Standardized Mortality Rates in EU15+ Countries for Years 1990-2019 for Both Sexes
eTable 6. Joinpoint Analysis for Thyroid Cancer Age-Standardized Mortality Rates in EU15+ Countries for Years 1990-2019 in Males, Females
eTable 7. Joinpoint Analysis for Thyroid Cancer Age-Standardized DALYs in EU15+ Countries for Years 1990-2019 in Both Sexes
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Kilfoy BA, Zheng T, Holford TR, et al. International patterns and trends in thyroid cancer incidence, 1973-2002. Cancer Causes Control. 2009;20(5):525-531. doi: 10.1007/s10552-008-9260-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-E386. doi: 10.1002/ijc.29210 [DOI] [PubMed] [Google Scholar]
- 4.Fitzmaurice C, Abate D, Abbasi N, et al. ; Global Burden of Disease Cancer Collaboration . Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2019;5(12):1749-1768. doi: 10.1001/jamaoncol.2019.2996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.La Vecchia C, Malvezzi M, Bosetti C, et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer. 2015;136(9):2187-2195. doi: 10.1002/ijc.29251 [DOI] [PubMed] [Google Scholar]
- 6.Fitzmaurice C, Dicker D, Pain A, et al. ; Global Burden of Disease Cancer Collaboration . The global burden of cancer 2013. JAMA Oncol. 2015;1(4):505-527. doi: 10.1001/jamaoncol.2015.0735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133. doi: 10.1089/thy.2015.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells SA Jr, Asa SL, Dralle H, et al. ; American Thyroid Association Guidelines Task Force on Medullary Thyroid Carcinoma . Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015;25(6):567-610. doi: 10.1089/thy.2014.0335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA. 2017;317(13):1338-1348. doi: 10.1001/jama.2017.2719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lubitz CC, Kong CY, McMahon PM, et al. Annual financial impact of well-differentiated thyroid cancer care in the United States. Cancer. 2014;120(9):1345-1352. doi: 10.1002/cncr.28562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . The Global Health Observatory. Metrics: disability-adjusted life year (DALY). Accessed April 23, 2020. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/158
- 12.Murray CJL, Acharya AK. Understanding DALYs (disability-adjusted life years). J Health Econ. 1997;16(6):703-730. doi: 10.1016/S0167-6296(97)00004-0 [DOI] [PubMed] [Google Scholar]
- 13.Devleesschauwer B, Havelaar AH, Maertens de Noordhout C, et al. DALY calculation in practice: a stepwise approach. Int J Public Health. 2014;59(3):571-574. doi: 10.1007/s00038-014-0553-y [DOI] [PubMed] [Google Scholar]
- 14.James SL, Abate D, Abate KH, et al. ; GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salciccioli JD, Marshall DC, Shalhoub J, Maruthappu M, De Carlo G, Chung KF. Respiratory disease mortality in the United Kingdom compared with EU15+ countries in 1985-2015: observational study. BMJ. 2018;363:k4680. doi: 10.1136/bmj.k4680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goodall R, Salciccioli JD, Davies AH, Marshall D, Shalhoub J. Trends in peripheral arterial disease incidence and mortality in EU15+ countries 1990-2017. Eur J Prev Cardiol. 2021;28(11):1201-1213. [DOI] [PubMed] [Google Scholar]
- 17.Murray CJ, Richards MA, Newton JN, et al. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet. 2013;381(9871):997-1020. doi: 10.1016/S0140-6736(13)60355-4 [DOI] [PubMed] [Google Scholar]
- 18.Viner RM, Hargreaves DS, Coffey C, Patton GC, Wolfe I. Deaths in young people aged 0-24 years in the UK compared with the EU15+ countries, 1970-2008: analysis of the WHO Mortality Database. Lancet. 2014;384(9946):880-892. doi: 10.1016/S0140-6736(14)60485-2 [DOI] [PubMed] [Google Scholar]
- 19.Roth GA, Abate D, Abate KH, et al. ; GBD 2017 Causes of Death Collaborators . Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736-1788. doi: 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodall R, Alazawi A, Hughes W, et al. Trends in type 2 diabetes mellitus disease burden in European Union countries between 1990 and 2019. Sci Rep. 2021;11(1):15356. doi: 10.1038/s41598-021-94807-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Balah A, Goodall R, Salciccioli JD, Marshall DC, Shalhoub J. Mortality from abdominal aortic aneurysm: trends in European Union 15+ countries from 1990 to 2017. Br J Surg. 2020;107(11):1459-1467. doi: 10.1002/bjs.11635 [DOI] [PubMed] [Google Scholar]
- 22.Hughes W, Goodall R, Salciccioli JD, Marshall DC, Davies AH, Shalhoub J. Trends in lower extremity amputation incidence in European Union 15+ Countries 1990-2017. Eur J Vasc Endovasc Surg. 2020;60(4):602-612. doi: 10.1016/j.ejvs.2020.05.037 [DOI] [PubMed] [Google Scholar]
- 23.Global Burden of Disease Collaborative Network . Global Burden of Disease Study 2017. (GBD 2017) Causes of death and nonfatal causes mapped to ICD codes. Institute for Health Metrics and Evaluation. Accessed January 23, 2022. http://ghdx.healthdata.org/record/ihme-data/gbd-2017-cause-icd-code-mappings
- 24.Global Health Data Exchange . GBD results tool. Accessed January 23, 2022. http://ghdx.healthdata.org/gbd-results-tool
- 25.United Nations Department of Economic and Social Affairs . World Population Prospects. The 2012. revision highlights and advance tables. Accessed January 23, 2022. https://population.un.org/wpp/Publications/Files/WPP2012_HIGHLIGHTS.pdf
- 26.Anand S, Hanson K. Disability-adjusted life years: a critical review. J Health Econ. 1997;16(6):685-702. doi: 10.1016/S0167-6296(97)00005-2 [DOI] [PubMed] [Google Scholar]
- 27.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351. doi: [DOI] [PubMed] [Google Scholar]
- 28.Baker SR, Bhatti WA. The thyroid cancer epidemic: is it the dark side of the CT revolution? Eur J Radiol. 2006;60(1):67-69. doi: 10.1016/j.ejrad.2006.04.022 [DOI] [PubMed] [Google Scholar]
- 29.Udelsman R, Zhang Y. The epidemic of thyroid cancer in the United States: the role of endocrinologists and ultrasounds. Thyroid. 2014;24(3):472-479. doi: 10.1089/thy.2013.0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295(18):2164-2167. doi: 10.1001/jama.295.18.2164 [DOI] [PubMed] [Google Scholar]
- 31.Park S, Oh C-M, Cho H, et al. Association between screening and the thyroid cancer “epidemic” in South Korea: evidence from a nationwide study. BMJ. 2016;355:i5745. doi: 10.1136/bmj.i5745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim J, Gosnell JE, Roman SA. Geographic influences in the global rise of thyroid cancer. Nat Rev Endocrinol. 2020;16(1):17-29. doi: 10.1038/s41574-019-0263-x [DOI] [PubMed] [Google Scholar]
- 33.Cooper DS, Doherty GM, Haugen BR, et al. ; American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer . Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19(11):1167-1214. doi: 10.1089/thy.2009.0110 [DOI] [PubMed] [Google Scholar]
- 34.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569-578. doi: 10.1016/S0140-6736(08)60269-X [DOI] [PubMed] [Google Scholar]
- 35.Pampel FC. Global patterns and determinants of sex differences in smoking. Int J Comp Sociol. 2006;47(6):466-487. doi: 10.1177/0020715206070267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burger EH, van der Merwe L, Volmink J. Errors in the completion of the death notification form. S Afr Med J. 2007;97(11):1077-1081. [PubMed] [Google Scholar]
- 37.Katsakiori PF, Panagiotopoulou EC, Sakellaropoulos GC, Papazafiropoulou A, Kardara M. Errors in death certificates in a rural area of Greece. Rural Remote Health. 2007;7(4):822. doi: 10.22605/RRH822 [DOI] [PubMed] [Google Scholar]
- 38.Lu TH, Shau WY, Shih TP, Lee MC, Chou MC, Lin CK. Factors associated with errors in death certificate completion: a national study in Taiwan. J Clin Epidemiol. 2001;54(3):232-238. doi: 10.1016/S0895-4356(00)00299-7 [DOI] [PubMed] [Google Scholar]
- 39.Mikkelsen L, Phillips DE, AbouZahr C, et al. A global assessment of civil registration and vital statistics systems: monitoring data quality and progress. Lancet. 2015;386(10001):1395-1406. doi: 10.1016/S0140-6736(15)60171-4 [DOI] [PubMed] [Google Scholar]
- 40.Perros P, Boelaert K, Colley S, et al. ; British Thyroid Association . Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 2014;81(suppl 1):1-122. doi: 10.1111/cen.12515 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Joinpoint Analysis for Thyroid Cancer Age-Standardized Incidence Rates in EU15+ Countries for Years 1990-2019 for Both Sexes
eTable 2. 1990 and 2019 Male Age-Standardized Mortality Rates (ASMRS), Age-Standardized Incidence Rates (ASIRs), Mortality-to-Incidence Indices (MIIs) and Disability-Adjusted Life Years (DALYS), With Associated Percentage Changes, for Thyroid Cancer in the European Union 15+ Countries
eTable 3. 1990 and 2019 Female Age-Standardized Mortality Rates (ASMRS), Age-Standardized Incidence Rates (ASIRs), Mortality-to-Incidence Indices (MIIs) and Disability-Adjusted Life Years (DALYS), With Associated Percentage Changes, for Thyroid Cancer in the European Union 15+ Countries
eTable 4. Joinpoint Analysis for Thyroid Cancer Age-Standardized Incidence Rates in EU15+ Countries for Years 1990-2019 in Males, Females
eTable 5. Joinpoint Analysis for Thyroid Cancer Age-Standardized Mortality Rates in EU15+ Countries for Years 1990-2019 for Both Sexes
eTable 6. Joinpoint Analysis for Thyroid Cancer Age-Standardized Mortality Rates in EU15+ Countries for Years 1990-2019 in Males, Females
eTable 7. Joinpoint Analysis for Thyroid Cancer Age-Standardized DALYs in EU15+ Countries for Years 1990-2019 in Both Sexes


