Abstract
Eagle’s syndrome is a rare collection of symptoms that occur secondary to an elongated styloid process or calcified stylohyoid ligament irritating its surrounding structures. Classically, this presents as unilateral throat pain or rarely, as acute neurological symptoms secondary to compression of the internal carotid artery: so called ‘stylocarotid syndrome’. Significant neurological events in teenagers, secondary to Eagle syndrome have not been reported. We discuss the rare case of a teenage boy, diagnosed with right internal carotid artery dissection and middle cerebral artery infarction, with no cause initially identified. Following further admission with a transient neurological episode, he was noted to have elongated styloid processes with the right abutting the site of carotid dissection. He underwent styloidectomy and has since remained symptom free. This case highlights the importance of considering anatomical variants when assessing young patients with neurological symptoms, and the potential morbidity and mortality benefit that early surgical intervention may have.
Keywords: neurological injury, stroke, otolaryngology / ENT, head and neck surgery
Background
Eagle’s syndrome is an unusual and rare group of symptoms that occur secondary to an elongated styloid process with a calcified stylohyoid ligament irritating the surrounding neurovascular and pharyngeal structures. The classical presentation was first fully described by Eagle and features atypical unilateral throat pain associated with a sensation of a foreign body in the throat.1 Patients can also suffer from a persistent sore throat that is referred to the ear and becomes worse on swallowing. Other frequently associated symptoms include neck pain, dysphagia, syncope and tinnitus.2
Eagle later described the less common ‘stylocarotid syndrome’3; wherein compression of the extracranial internal carotid artery (ICA) can result in neurological symptoms, stroke and transient ischaemic attacks. Patients with this syndrome can also experience irritation of the sympathetic chain when rotating their neck, causing pain in the distribution of the carotid artery.2 Although more commonly seen in patients with connective tissue disorders and trauma, ICA dissection with acute ischaemic events secondary to stylocarotid Eagle’s syndrome has been described in a growing number of case reports.4–30 These cases share similar clinical presentations, however, given the rarity of the condition, there is no clear consensus on its definitive management. Resultantly, the phenomenon has been treated successfully with both conservative medical and more invasive surgical management in the form of a styloidectomy.
In this report, we discuss the rare case of a teenage boy who underwent a styloidectomy by our ear, nose and throat (ENT) skull base team after experiencing repeat, acute neurological events, secondary to an ICA dissection and elongated styloid process. Significant neurological events in teenagers, secondary to Eagle syndrome have not been reported before. We review the current literature and discuss our management in relation to previously reported cases of this unusual phenomenon.
Case presentation
A teenage boy, presented to hospital with acute onset left-sided hemiparesis, mild dysarthria and a severe headache after carrying a heavy rucksack. He had been admitted to hospital 18 months prior to this event after experiencing similar symptoms, where a right-sided ICA dissection, mural thrombus and middle cerebral artery (MCA) infarction had been found. He had been treated with acute thrombolysis, 6 months of anticoagulation (warfarin) and subsequent antiplatelet therapy. Despite extensive investigations, no cause for his initial presentation was found.
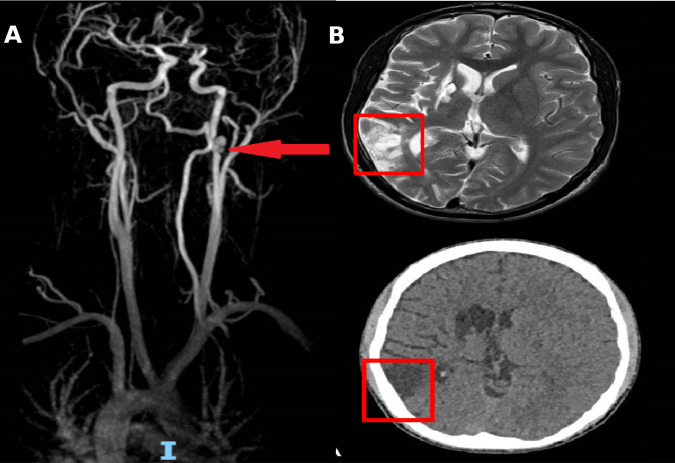
Repeat CT angiography (CTA) noted a reduction in the right MCA calibre, from the M2 segment onwards with a focal dissection of the cervical ICA (figure 1A). When compared with imaging from his previous admission, there had been minimal extension of his ICA dissection. MRI noted mature ischaemia changes in the frontal and temporal lobe, but no acute infarct was seen (figure 1B).
Figure 1.
(A) CT angiography of right carotid. The internal carotid artery dissection is indicated by the red arrow. (B) MRI and CT images of mature middle cerebral artery infarct—indicated by red box.
He underwent acute thrombolysis at his local hospital, and was transferred to our hospital with a view to perform thrombectomy. Before this was achieved, the patients’ symptoms spontaneously resolved. He was reviewed by our ENT team and he was later discharged home with oral-anticoagulation.
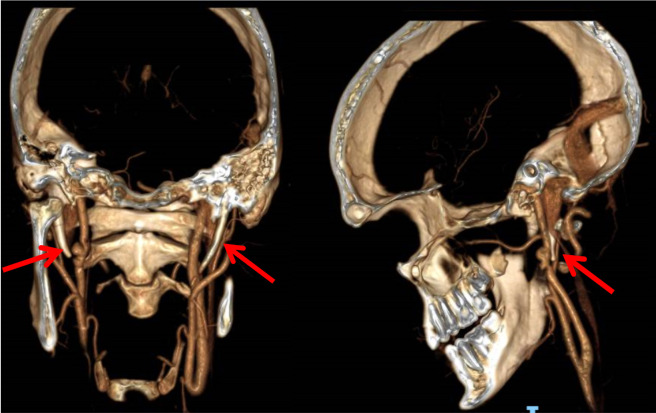
The patient was subsequently discussed at our tertiary skull base multidisciplinary team (MDT) meeting. On further review of imaging, bilateral elongated styloid processes and calcification of the stylohyoid ligament was noticed with the right directly abutting the site of ICA dissection suggesting a diagnosis of Eagle syndrome (figure 2). It was felt that positional compression of the ICA due to this anatomical variant was the likely cause for his current transient neurological event. Furthermore, it is likely that chronic compression by this elongated styloid process prevented a natural resolution of his ICA dissection following his initial presentation.
Figure 2.
CT skull reconstruction. Left—coronal view with bilateral elongated styloid processes. Right—sagittal view showing 34 mm right styloid process in close proximity to Internal carotid artery dissection. Red arrows indication styloid process.
Treatment
Following the diagnosis of Eagle’s Syndrome in a young man with two cerebrovascular events in a short period, our skull base MDT consensus was to perform an elective right styloidectomy. Of note, the ICA dissection was managed medically, with the vascular MDT deciding not to stent in the acute setting due to the transient nature of the neurological episode.
An open approach was used through a right transcervical incision. Careful dissection was made through level II lymph nodes anterior to the sternocleidomastoid. A number of bulky lymph nodes were excised which subsequently revealed benign hyperplasia on histopathological examination. The styloid process was carefully delineated and surrounding neurovascular structures, in particular, the facial nerve, were preserved. The stylohyoid and stylopharyngeus were dissected free before final excision of the styloid process.
The patient had an uneventful inpatient stay and was discharged on day 2 postoperatively with no complications. He was reviewed in the outpatient ENT department 4 weeks after his procedure and had made an excellent recovery with no recurrent episodes of neurological symptoms. He remains on anticoagulation and is under close clinical surveillance by the vascular and stroke teams.
Though currently asymptomatic, due to the patients young age and potential risk of further neurological sequelae, he has been considered for a prophylactic contralateral styloidectomy at a future date.
Discussion
We highlight this unusual case of a young man with recurrent cerebrovascular events, secondary to an elongated styloid process causing ICA compromise.
The styloid process is a long bony prominence that usually measures 20–25 mm, and serves as an important point of attachment for three muscles (stylohyoid, stylopharyngeus, styloglossus muscle) and the stylohyoid ligament.2 Traditionally, a styloid process of >30 mm is thought to be a risk factor for experiencing Eagle’s syndrome, although Eagle found only 4% of patients with abnormal styloid processes noted symptoms.31 In two separate case series, patients with carotid artery dissection were noted to have a significantly increased length of styloid process resulting in a shorter contact distance between the artery and bone,32 33 strongly implicating Eagle’s syndrome as an independent risk factor for carotid artery dissection. In addition to styloid length, Tardivo et al showed that the styloid angulation and its relation to C1 transverse process may also contribute to compression of the ICA and subsequent dissection, demonstrating a multifactorial pathogenesis to symptomatic disease.34
Diagnosis of Eagle’s syndrome is based on clinical findings and cross-sectional imaging. Classically, palpation of the tonsil fossa can demonstrate an elongated styloid process, with resolution of symptoms on injection of local anaesthetic being diagnostic for the condition.35 Plain film radiography can occasionally demonstrate an elongated styloid, but is limited by calcification around the stylohyoid ligament and does not provide information on the adjacent soft tissues. CT scanning is the current imaging modality of choice for diagnosis of Eagle’s syndrome, clearly defining the relationship of the styloid process to the surrounding neurovascular structures.35 Where available, three-dimensional reconstruction of CT images can provide excellent information on the length and angulation of the styloid in relation to the carotid artery.36 Additionally, several previous cases studies have made use of CTA to diagnose aberrant flow and arterial dissection within the carotid vessels secondary to elongated styloid processes.
Surgical intervention for the classical description of Eagle’s syndrome is indicated after failure of medical therapy. Several cases have used styloidectomy to prevent recurrence of stroke symptoms. External approach and intra-oral styloidectomy are the most frequently described surgical techniques.37
The external approach provides the greatest exposure to the deep neck space and therefore facilitates the safest dissection of the styloid process and nearby neurological structures. Theoretically, it poses an increased risk of marginal mandibular nerve injury, however, Ceylan et al, found that in a large case series of 61 patients, only two patients suffered a temporary marginal mandibular nerve weakness with no other reported complications,38 strongly supporting the safety and efficacy of this technique.
Intra-oral styloidectomy avoids the need for an external neck scar and has a shorter operating time, but affords only limited views of the styloid process and has an increased risk of retropharyngeal infection.37 39 Despite this, a number of alternative intraoral resection techniques have been proposed including include a ‘tonsil sparing’ techniques as successfully described by Torres et al in a case series of 10 patients with no post-operative complications.40 Endoscopic41 42 and robotic-assisted transoral43 approaches have also been performed, but are isolated to small cases series and are not common practice.
On review of the literature over the last 20 years, to the best of our knowledge, there has been 34 cases of carotid artery dissection secondary to an elongated styloid process that have been published. The condition is more common in males with a ratio of 2.4:1. The patients were generally fit and well with 23 (68%) having no reported comorbidities. Twenty patients had medical or endovascular management only, and 14 underwent surgical intervention in the form of open approach styloidectomy (9 unilateral, 5 bilateral). Surgery was generally performed on a semi-elective basis, following initial medical or endovascular management. No recurrent clinical characteristics were noted in those selected for surgical intervention, however, there appears to be a trend for surgical management as a definitive treatment choice in recurrent and/or severe ischaemic disease4–30 (online supplemental table 1).
bcr-2021-247954supp001.pdf (230.1KB, pdf)
Excluding our patient, the mean age of cases is 49.3 years old (range 30–80 years old). Our case is the youngest by a considerable margin, demonstrating that ICA dissection due to Eagle’s syndrome can also occur in young patients. ICA dissection is implicated in 2.5% of all patients presenting with a stroke.44 While little epidemiological data are available, case-series have shown ICA dissection to be present on imaging in 8%–20% of patients under 18 years of age presenting with acute neurological symptoms. Often, a history of minor trauma or recent infection are suggested as aetiological factors, however, most commonly ICA dissection occurs spontaneously. In these cases, connective tissue disorders such as Ehlers-Danlos syndrome or Marfans syndrome are commonly implicated.45 Eagle’s syndrome as a contributing factor to ICA dissection in a paediatric population has not been seen.
Importantly, in our case, an elongated styloid process was missed on initial presentation, and was not considered as a possible causative factor for his repeated neurological events. This highlights the importance of considering anatomical variants such as those seen in Eagle’s syndrome in the differential diagnosis for young patients presenting with neurological symptoms. Similarly, young patients are more likely to develop future cerebrovascular events, and therefore definitive surgical management is likely to improve the patient’s morbidity and mortality. As such, we advise that all young patients with recurrent neurological episodes caused by elongated styloid process should undergo definitive surgical management in the form of a styloidectomy.
Learning points.
Although Eagle’s syndrome typically presents with sharp neurological pain in the throat and jaw, a long styloid process can cause carotid artery compression or dissection presenting with recurrent acute neurological symptoms.
Unusual causes of stroke including unusual anatomy and trauma should be considered in young otherwise healthy patients.
Definitive surgical management in the form of an elective styloidectomy is advised in young patients to prevent further cerebrovascular events.
Footnotes
Contributors: SS edited and assisted drafting manuscript. AW edited and assisted drafting manuscript. JV, senior author, operated on patient, reviewed and edited manuscript. PC, senior author, operated on patient, reviewed and edited manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Eagle WW. Elongated styloid process. Arch Otolaryngol 1937;25:584–7. [Google Scholar]
- 2.Fusco DJ, Asteraki S, Spetzler RF. Eagle's syndrome: embryology, anatomy, and clinical management. Acta Neurochir 2012;154:1119–26. 10.1007/s00701-012-1385-2 [DOI] [PubMed] [Google Scholar]
- 3.Eagle WW. Further observations and a new syndrome. Arch Otolaryngol 1948;47:630–40. [DOI] [PubMed] [Google Scholar]
- 4.Zuber M, Meder JF, Mas JL. Carotid artery dissection due to elongated styloid process. Neurology 1999;53:1886–7. 10.1212/WNL.53.8.1886 [DOI] [PubMed] [Google Scholar]
- 5.Soo O-yanY, Chan YL, Wong KS. Carotid artery dissection after prolonged head tilting while holding a newborn baby to sleep. Neurology 2004;62:1647–8. 10.1212/01.wnl.0000123016.81648.b6 [DOI] [PubMed] [Google Scholar]
- 6.Faivre A, Abdelfettah Z, Rodriguez S, et al. Neurological picture. bilateral internal carotid artery dissection due to elongated styloid processes and shaking dancing. J Neurol Neurosurg Psychiatry 2009;80:1154–5. 10.1136/jnnp.2008.159954 [DOI] [PubMed] [Google Scholar]
- 7.Razak A, Short JL, Hussain SI. Carotid artery dissection due to elongated styloid process: a self-stabbing phenomenon. J Neuroimaging 2014;24:298–301. 10.1111/j.1552-6569.2012.00759.x [DOI] [PubMed] [Google Scholar]
- 8.Todo T, Alexander M, Stokol C, et al. Eagle syndrome revisited: cerebrovascular complications. Ann Vasc Surg 2012;26:729.e1–729.e5. 10.1016/j.avsg.2011.12.005 [DOI] [PubMed] [Google Scholar]
- 9.Ohara N, Sakaguchi M, Okazaki S, et al. Internal carotid artery dissection caused by an elongated styloid process: usefulness of transoral ultrasonography. J Stroke Cerebrovasc Dis 2012;21:918.e7–918.e8. 10.1016/j.jstrokecerebrovasdis.2012.05.014 [DOI] [PubMed] [Google Scholar]
- 10.Sveinsson O, Kostulas N, Herrman L. Internal carotid dissection caused by an elongated styloid process (Eagle syndrome). BMJ Case Rep 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamamoto S, Todo K, Kawamoto M, et al. Carotid artery dissection associated with an elongated styloid process. Intern Med 2013;52:1005–6. 10.2169/internalmedicine.52.0024 [DOI] [PubMed] [Google Scholar]
- 12.Ogura T, Mineharu Y, Todo K, et al. Carotid artery dissection caused by an elongated styloid process: three case reports and review of the literature. NMC Case Rep J 2015;2:21–5. 10.2176/nmccrj.2014-0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aydin E, Quilyevh H, Cm C. Eagle syndrome presenting with neurological symptoms. Turk Neurosurg 2016;1. [DOI] [PubMed] [Google Scholar]
- 14.Jo H, Choi EH, Song J. Carotid artery dissection caused by Eagle syndrome precision and future. Medicine 2017;1:173–6. [Google Scholar]
- 15.Subedi R, Dean R, Baronos S, et al. Carotid artery dissection: a rare complication of Eagle syndrome. BMJ Case Rep 2017;2017:bcr2016218184. 10.1136/bcr-2016-218184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hebant B, Guegan-Massardier E, Macaigne V, et al. Ischemic stroke due to internal carotid artery dissection associated with an elongated styloid process (Eagle syndrome). J Neurol Sci 2017;372:466–7. 10.1016/j.jns.2016.10.055 [DOI] [PubMed] [Google Scholar]
- 17.Smoot TW, Taha A, Tarlov N, et al. Eagle syndrome: a case report of stylocarotid syndrome with internal carotid artery dissection. Interv Neuroradiol 2017;23:433–6. 10.1177/1591019917706050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jelodar S, Ghadirian H, Ketabchi M, et al. Bilateral ischemic stroke due to carotid artery compression by abnormally elongated styloid process at both sides: a case report. J Stroke Cerebrovasc Dis 2018;27:e89–91. 10.1016/j.jstrokecerebrovasdis.2017.12.018 [DOI] [PubMed] [Google Scholar]
- 19.Zammit M, Chircop C, Attard V, et al. Eagle’s syndrome: a piercing matter. BMJ Case Rep 2018;11:e226611. 10.1136/bcr-2018-226611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torikoshi S, Yamao Y, Ogino E, et al. A staged therapy for internal carotid artery dissection caused by vascular Eagle syndrome. World Neurosurg 2019;129:133–9. 10.1016/j.wneu.2019.05.208 [DOI] [PubMed] [Google Scholar]
- 21.Galletta K, Granata F, Longo M, et al. An unusual internal carotid artery compression as a possible cause of Eagle syndrome – a novel hypothesis and an innovative surgical technique. Surg Neurol Int 2019;10:174. 10.25259/SNI_317_2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baldino G, Di Girolamo C, De Blasis G, et al. Eagle syndrome and internal carotid artery dissection: description of 5 cases treated in 2 vascular institutions and review of the literature. Eur J Vasc Endovasc Surg 2019;58:e781–2. 10.1016/j.ejvs.2019.09.359 [DOI] [PubMed] [Google Scholar]
- 23.Ikenouchi H, Takagi M, Nishimura A, et al. Bilateral carotid artery dissection due to Eagle syndrome in a patient with vascular Ehlers-Danlos syndrome: a case report. BMC Neurol 2020;20:285. 10.1186/s12883-020-01866-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duarte-Celada WR, Jin D, Neves G, et al. Bilateral carotid dissection due to Eagle syndrome in a young female. eNeurologicalSci 2021;24:100353. 10.1016/j.ensci.2021.100353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horio Y, Fukuda K, Miki K, et al. Dynamic assessment of internal carotid artery and elongated styloid process in a case of bilateral carotid artery dissection. Surg Neurol Int 2020;11:163. 10.25259/SNI_42_2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brassart N, Deforche M, Goutte A, et al. A rare vascular complication of Eagle syndrome highlight by CTA with neck flexion. Radiol Case Rep 2020;15:1408–12. 10.1016/j.radcr.2020.05.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mattioli P, Baldino G, Castaldi A, et al. A peculiar case of internal carotid dissection: "do not forget Eagle's syndrome!". Neurol Sci 2021;42:2527–9. 10.1007/s10072-020-04925-1 [DOI] [PubMed] [Google Scholar]
- 28.Xhaxho S, Vyshka G, Kruja J. Eagle syndrome presenting as a neurological emergency: a case report. Surg Neurol Int 2021;12:257. 10.25259/SNI_362_2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vodopivec I, Klein JP, Prasad S. Bilateral cervical internal carotid artery dissections in Eagle syndrome. Neurol Clin Pract 2013;3:173–4. 10.1212/CPJ.0b013e31828d9fdb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muthusami P, Kesavadas C, Sylaja PN, et al. Implicating the long styloid process in cervical carotid artery dissection. Neuroradiology 2013;55:861–7. 10.1007/s00234-013-1186-1 [DOI] [PubMed] [Google Scholar]
- 31.Eagle WW. Elongated styloid process; symptoms and treatment. AMA Arch Otolaryngol 1958;67:172–6. 10.1001/archotol.1958.00730010178007 [DOI] [PubMed] [Google Scholar]
- 32.Raser JM, Mullen MT, Kasner SE, et al. Cervical carotid artery dissection is associated with styloid process length. Neurology 2011;77:2061–6. 10.1212/WNL.0b013e31823b4729 [DOI] [PubMed] [Google Scholar]
- 33.Montalbetti L, Ferrandi D, Pergami P, et al. Elongated styloid process and Eagle's syndrome. Cephalalgia 1995;15:80–93. 10.1046/j.1468-2982.1995.015002080.x [DOI] [PubMed] [Google Scholar]
- 34.Tardivo V, Castaldi A, Baldino G, et al. Internal carotid artery dissection related to abnormalities of styloid process: is it only a matter of length? Neurol Sci 2022;43:459–65. 10.1007/s10072-021-05350-8 [DOI] [PubMed] [Google Scholar]
- 35.Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol 2001;22:1401–2. [PMC free article] [PubMed] [Google Scholar]
- 36.Huang CC, Tsau YH, Liao YS. Three-Dimensional Reconstruction CT in Diagnosis of Eagle’s Syndrome: a Retrospective Study. Chin J Radiol 2006;31:221–5. [Google Scholar]
- 37.Strauss M, Zohar Y, Laurian N. Elongated styloid process syndrome: intraoral versus external approach for styloid surgery. Laryngoscope 1985;95:976–9. [PubMed] [Google Scholar]
- 38.Ceylan A, Köybaşioğlu A, Celenk F, et al. Surgical treatment of elongated styloid process: experience of 61 cases. Skull Base 2008;18:289–95. 10.1055/s-0028-1086057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chase DC, Zarmen A, Bigelow WC, et al. Eagle's syndrome: a comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol 1986;62:625–9. 10.1016/0030-4220(86)90253-7 [DOI] [PubMed] [Google Scholar]
- 40.Torres AC, Guerrero JS, Silva HC. A modified transoral approach for carotid artery type Eagle syndrome: technique and outcomes. Ann Otol Rhinol Laryngol 2014;123:831–4. 10.1177/0003489414538770 [DOI] [PubMed] [Google Scholar]
- 41.Matsumoto F, Kase K, Kasai M, et al. Endoscopy-assisted transoral resection of the styloid process in Eagle's syndrome. Case report. Head Face Med 2012;8:21. 10.1186/1746-160X-8-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Al Weteid AS, Miloro M. Transoral endoscopic-assisted styloidectomy: how should Eagle syndrome be managed surgically? Int J Oral Maxillofac Surg 2015;44:1181–7. 10.1016/j.ijom.2015.03.021 [DOI] [PubMed] [Google Scholar]
- 43.Kim DH, Lee YH, Cha D, et al. Transoral robotic surgery in Eagle's syndrome: our experience on four patients. Acta Otorhinolaryngol Ital 2017;37:454–7. 10.14639/0392-100X-1502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patel RR, Adam R, Maldjian C, et al. Cervical carotid artery dissection: current review of diagnosis and treatment. Cardiol Rev 2012;20:145–52. 10.1097/CRD.0b013e318247cd15 [DOI] [PubMed] [Google Scholar]
- 45.Kirkham FJ, Prengler M, Hewes DK, et al. Risk factors for arterial ischemic stroke in children. J Child Neurol 2000;15:299–307. 10.1177/088307380001500506 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bcr-2021-247954supp001.pdf (230.1KB, pdf)