Abstract
Chronic musculoskeletal anterior pelvic pain may originate from a variety of different sources making the diagnosis difficult. Ectopic bone formation on the pubic symphysis is extremely rare and may cause significant disability. Reported herein is the case of a very active patient with symphysis pubis ectopic bone formation causing disability for more than 10 years. Resection of the ectopic bone combined with pubis symphysis fusion led to a successful outcome allowing the patient to return to his previous recreational activities.
Keywords: orthopaedics, surgery, pain, musculoskeletal and joint disorders
Background
Chronic anterior pelvic pain affects 25% of women,1 2%–10% of men2 and may be related to a number of clinical conditions, including sports-related disorders, pregnancy-related pathologies (diastasis/instability), infection, fracture, trauma, arthritis or metastatic disease.3
Chronic pain secondary to ectopic bone formation is exceedingly rare and, unless the pathology and its impact is recognised early, can lead to chronic symptoms causing disability and functional impairment.4 We report a male patient with this entity that resulted in a 10-year disability. To the best of our knowledge, this is the only case in the literature, managed with pelvic fusion, resulting in complete resolution of symptoms and return to full activities. The addition of pelvic fusion to the ectopic bone resection may be a compelling option to be considered in such rare cases eradicating the potential of postoperative chronic instability and recurrence of the ectopic bone.
Case presentation
A man in his late 50s presented to the authors’ institution for pubic symphysis pain evaluation. The pain has been worsening during the past 10 years and was radiating from the symphysis towards the bilateral groin areas and occasionally the thighs. A few years previously, the patient had been quite active with cycling and running; however in recent years, the pain had deteriorated substantially, to the point of making the patient unable to perform any recreational activities, having also significant limitations in his ability to walk and carry out activities of daily living. Of note, there was no history of an acute traumatic event. Previous conservative treatment included physiotherapy and three injections of steroids mixed with local anaesthetic over the period of several years that provided some temporary relief. However, during the past 2 years, the pain had been increasing with further mobility restriction and a negative impact in his mental state. Physical examination demonstrated a slow gait pattern and significant localised tenderness over the pubic symphysis. There was no leg length discrepancy, no muscle wasting, no inguinal hernia and a negative FABER test (no sacroiliac joint pain on provocation testing). The lumbar spine examination was within normal limits, and he was neurovascularly intact symmetrically throughout his bilateral lower extremities.
Investigations
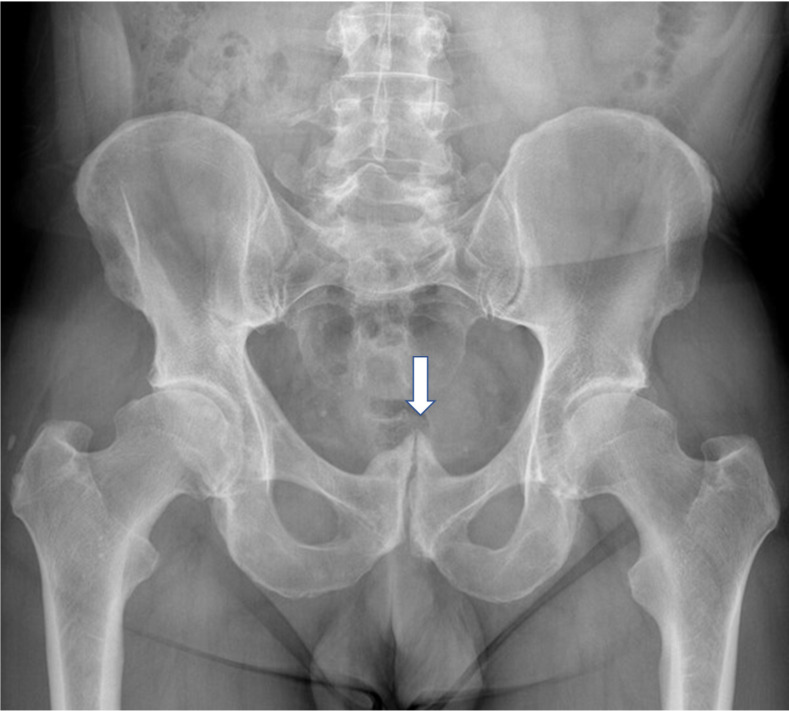
The patient had obtained radiographs of his pelvis when the pain had originally started, but those were negative. Seven years ago, radiographs of the pelvis were repeated and showed a calcification on the upper edge of the pubic symphysis (figure 1). Current repeat radiographs showed interval change with increasing ectopic bone formation and complete bridging over the symphysis (figure 2). Further stress imaging with ‘Flamingo’ views of the pelvis showed no instability present. A pelvic CT scan demonstrated bony hypertrophic degenerative changes with prominent posterosuperior osteophyte, loss of joint space and joint margin irregularity, and its three-dimensional reconstruction is shown in figure 3A–B. An MRI was also obtained that excluded soft tissue pathology but demonstrated inflammation of the rectus abdominis insertion. Of note, there were no signs of sacroiliac joint instability in any of the imaging modalities. Blood results, including infection and rheumatological markers, were within normal limits. Based on the above, a diagnosis of symptomatic heterotopic bone formation with associated degenerative arthritis of the symphysis pubis was established.
Figure 1.
Anteroposterior pelvic radiograph showing the presence of calcifications on the pubic symphysis.
Figure 2.
Anteroposterior pelvic radiograph showing progression to further ectopic bone formation and bridging of the pubic symphysis.
Figure 3.
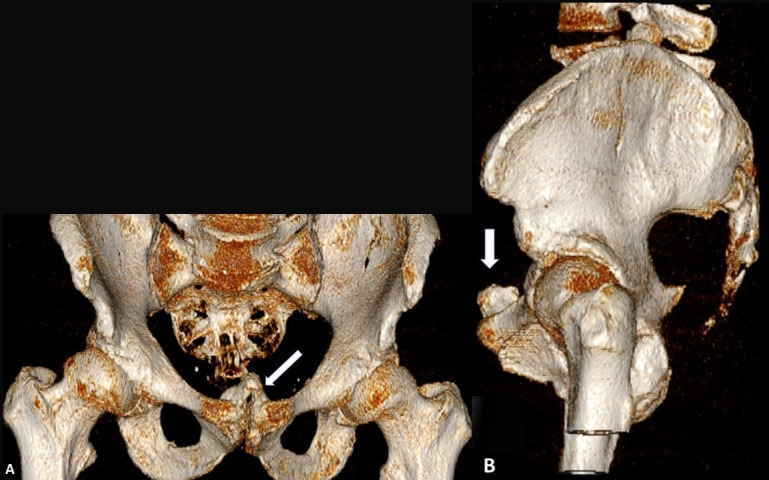
Three-dimensional pelvic CT reconstructions coronal (A) and sagittal (B) views of the pelvis showing ectopic bone formation at the pubic symphysis.
Treatment
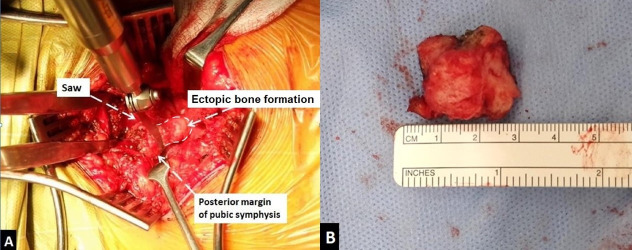
The patient elected to undergo excision of the ectopic bone and pubic symphysis fusion using tricortical iliac crest bone graft and plate, as previously described.5 Briefly, under general anaesthesia, a standard Pfannenstiel incision was made. The rectus muscle at the midline was incised longitudinally and was elevated from its tendinous insertion and retracted laterally allowing adequate exposure and visualisation of the pubis symphysis. The urinary bladder was exposed and protected throughout the procedure. The exostosis was removed using an oscillating saw, and the length of the bone formation removed was 3.0 cm (figure 4A–B). Subsequently, the pubic symphysis cartilage was removed, and a tricortical bone graft taken from the right iliac crest was fashioned in a ‘T’-shape to fill the void created in the pubic symphysis and was compressed down using a 3.5 mm, six-hole Matta plate. At the end of the procedure, the rectus abdominis was repaired with 1/0 Polydioxanone (PDS) suture. The iliac crest defect from the harvested site was reconstructed with a green bone scaffold (synthetic) (Faenza, Italy).
Figure 4.
Intraoperative images showing the bone formation being resected with a saw (A) and the specimen after resection (B).
Postoperative regimen included non-weight bearing for 10 weeks in a wheelchair, thromboprophylaxis (tinzaparin 4.500 IU) treatment for 12 weeks followed by progressive weight bearing and physical therapy. Full weight-bearing was restored at 12 weeks, and at 16 weeks, the patient was allowed to resume all types of physical activity, including jogging, swimming and cycling.
Outcome and follow-up
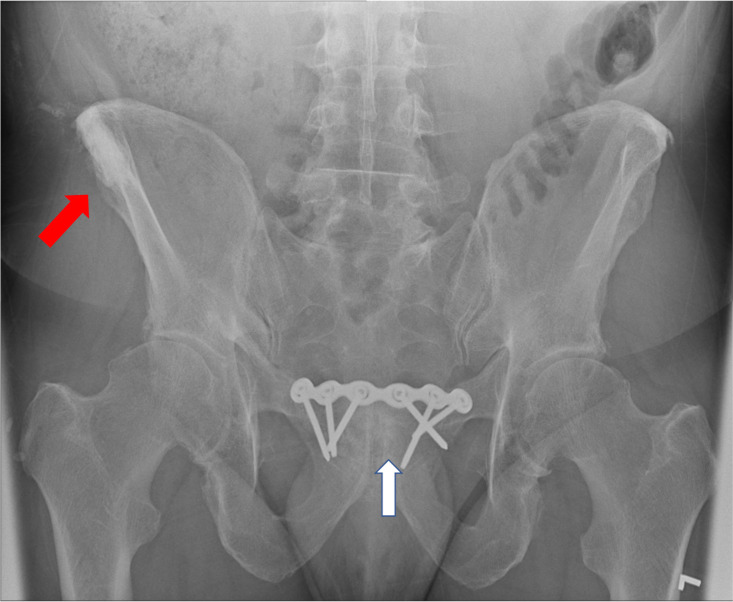
At 12-month follow-up, the patient was pain free, had regained his mobility and had resumed all of his desired recreational activities including cycling, swimming and jogging. His EuroQol index value6 was 0.093 versus 1000 and the EuroQuolVAS was 25/100 versus 90/100 preoperatively and postoperatively (12 month follow-up), respectively. Final imaging demonstrates complete consolidation of the pubic fusion as well as full integration of the Greenbone scaffold to the host (figure 5).
Figure 5.
Outlet view of the pelvis at 12-month follow-up showing fusion of pubic symphysis (white arrow) and full integration of the Greenbone scaffold in the right iliac crest (red arrow).
Discussion
Chronic anterior pelvic pain may constitute a diagnostic challenge to physicians,7 especially given the several potential differential diagnoses, including sports-related disorders, pregnancy-related pathologies (diastasis/instability), arthritis, fracture, infection, trauma and metastatic disease.3
Sports-related disorders occur due to repetitive strain or/and overuse8 9 and may include: sportsman’s hernia, bone articular aseptic inflammation (aka osteitis pubis), myotendinous strain and enthesopathy. This entity may be secondary to pregnancy and labour,10 where mechanical (weight gain, change of gravity centre) and hormonal (relaxin and estrogens) changes may result in permanent pelvic instability/diastasis. Bone-related causes may include: arthritis, fracture (stress/avulsion/insufficiency), infection (osteomyelitis and septic arthritis of the symphysis), metastatic disease (distant or from adjacent organs: prostate, urinary bladder), tumours (most frequently including osteochondromas), diffuse idiopathic skeletal hyperostosis, enthesophytes and ectopic bone formation (aka heterotopic ossification).3 11–15
Bone ectopic formation is a rare, progressive skeletal process, not very well described in the literature. Potential underlying mechanisms may be related to chronic overload including repetitive or excessive traction and compression forces, resulting in joint instability4 16–18 or recurrent microtrauma causing reactive bone formation.18 19 The cellular pattern of this bone formation is different than the fracture healing or normal development pattern.18
All these pathologies can be presented with various chief complaints ranging from low urinary tract symptoms to sexual disturbance.11 19 They may present as urethral compression, bladder pseudotumour or incidentally discovered.20–23 The patient reported herein had no such accompanying symptoms. Initially, he was temporarily relieved by conservative therapy but, for more than 2 years before his operation, was in permanent pain affecting his activities of daily living. Ectopic bone formation was found at the posterosuperior aspect of the symphysis. It can induce chronic pain from mechanical irritation or compression of adjacent soft tissues or bony stress reaction (presence of bone marrow oedema).4 Resection of the exostosis and pubic symphysis fusion using tricortical iliac crest bone graft and plate resulted in solid fusion and a pain-free outcome at 12-month follow-up. The quality of life generic instrument used (EUroQuol) demonstrated vast improvement in all dimensions of assessment.
The existing literature related to this pathology is poor. Hopp et al4 reported the presence of bony exostosis in five cases in young male athletes (soccer and marathon runners), with chronic pain that had failed at least 6 months’ conservative management. The mean length of the spur was 2.2 cm, whereas in our case it was 3 cm, being the longest ever reported. Three of them had pain exacerbation with filling of the bladder, whereas two complained of adductor and/or lower abdominal pain and one of groin pain. In four cases, the bone was posterosuperior where in one was posterior-central. Surgery was performed in four out of the five patients. One patient that had been treated conservatively did not wish to undergo surgery and was lost follow-up. Following removal of the bony exostosis, intraoperative assessment of symphysis pubis instability by using clamps on either side of the superior pubic ramus under fluoroscopy was negative.4 Interestingly, one of their patients presented after having undergone pelvic plating to treat his instability but without fusion and without resection of the spur, and a second surgery was required resect the spur and relieve symptoms. Of note, histological specimens of the ectopic bone resected showed osteocartilaginous tissue with fibrosis.4
In our case, in addition to the resection of the ectopic bone formation, fusion was also carried out to minimise the risk of the patient having ongoing painful stimuli due to the degenerative state of the pubic symphysis joint.
Patient’s perspective.
My symptoms started 10 years ago and have had 3 steroid injections over that period of time. I was suffering from depression as I was not able to do my activities, I did not feel like going out, I was in a dark place and started drinking a lot. I felt stabbing pain during activity which continued for several days before subsiding. I had to stop any impact-related sport activity including running and hill walking which I very much enjoyed in the past. I started taking too much ibuprofen due to the symptoms, however I ended up in the hospital and was subsequently diagnosed with inflammatory bowel syndrome.
After my operation I feel relieved and I am definitely mentally better. I am more positive, and my quality of life is so much better. I am pain free, my mobility is now back to normal and now I can do running again. I am glad that I found someone who knew what to do for me, as I had been wandering around different doctors who could not solve my problem.
Learning points.
Anterior pelvic pain due to musculoskeletal causes is a challenge to diagnose and treat.
Pubic symphysis ectopic bone formation is very rare but may cause significant disability.
Resection of the ectopic bone leads to significant pain relief.
In addition to bone excision, and particularly in cases where degenerative changes of the pubic symphysis exist, fusion may be advocated to minimise the risk of ongoing painful stimuli. Fusion also can maintain pelvic stability and can reduce the chance of new ectopic bone recurrence.
Footnotes
Contributors: NDM: wrote manuscript, literature search. GDC: contributed to the writing of the manuscript. PVG: carried out the surgery and contributed to the final writing of the manuscript and oversaw the entire process
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.Nygaard I, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA 2008;300:1311–6. 10.1001/jama.300.11.1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krieger JN, Ross SO, Riley DE. Chronic prostatitis: epidemiology and role of infection. Urology 2002;60:8–12. 10.1016/S0090-4295(02)02294-X [DOI] [PubMed] [Google Scholar]
- 3.Fitzgerald CM, Plastaras C, Mallinson T. A retrospective study on the efficacy of pubic symphysis corticosteroid injections in the treatment of pubic symphysis pain. Pain Med 2011;12:1831–5. 10.1111/j.1526-4637.2011.01263.x [DOI] [PubMed] [Google Scholar]
- 4.Hopp SJ, Ojodu I, Pohlemann T, et al. Posterior symphyseal spurs – an unusual differential diagnosis in athletes with groin pain. Phys Sportsmed 2015;43:150–4. 10.1080/00913847.2015.1012038 [DOI] [PubMed] [Google Scholar]
- 5.Giannoudis PV, Kanakaris NK. Pubic symphysis fusion. practical procedures in elective orthopaedic surgery. Springer, 2011: 23–8. [Google Scholar]
- 6.Foundation ER . EQ-5D-5L user guide, 2018. Available: https://euroqol.org/publications/user-guides
- 7.Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. J Anat 2010;217:475–87. 10.1111/j.1469-7580.2010.01300.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies AG, Clarke AW, Gilmore J, et al. Review: imaging of groin pain in the athlete. Skeletal Radiol 2010;39:629–44. 10.1007/s00256-009-0768-9 [DOI] [PubMed] [Google Scholar]
- 9.Angoules AG. Osteitis pubis in elite athletes: diagnostic and therapeutic approach. World J Orthop 2015;6:672–9. 10.5312/wjo.v6.i9.672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stolarczyk A, Stępiński P, Sasinowski Łukasz, et al. Peripartum pubic symphysis Diastasis-Practical guidelines. J Clin Med 2021;10:2443. 10.3390/jcm10112443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee W, Amin K, Kieras DM, et al. Osteochondroma of the pubic symphysis involved with aberrantly placed Minisling: a case report. Female Pelvic Med Reconstr Surg 2020;26:e1–3. 10.1097/SPV.0000000000000755 [DOI] [PubMed] [Google Scholar]
- 12.Wang W-Y, Du L-D, Lv W-C, et al. Osteochondroma of the symphysis pubis: a rare cause of bladder outlet obstruction. Am Surg 2010;76:916–8. 10.1177/000313481007600849 [DOI] [PubMed] [Google Scholar]
- 13.Zeitlin SI, Rajfer J, Cochran ST. Extrinsic bladder compression caused by a pubic bone Spur. Urology 1999;54:919–20. 10.1016/S0090-4295(99)00263-0 [DOI] [PubMed] [Google Scholar]
- 14.Cheng CW, Kim SP, Francis JJ, et al. Heterotopic ossification of the inferior pubic ramus. J Am Acad Orthop Surg 2018;26:e246–8. 10.5435/JAAOS-D-17-00101 [DOI] [PubMed] [Google Scholar]
- 15.Dimitrakopoulou A, Schilders E, Bismil Q, et al. An unusual case of enthesophyte formation following an adductor longus rupture in a high-level athlete. Knee Surg Sports Traumatol Arthrosc 2010;18:691–3. 10.1007/s00167-009-1029-0 [DOI] [PubMed] [Google Scholar]
- 16.Krahl H, Pieper HG, Quack G. [Bone hypertrophy as a results of training]. Orthopade 1995;24:441–5. [PubMed] [Google Scholar]
- 17.Chopra A, Robinson P. Imaging athletic groin pain. Radiol Clin North Am 2016;54:865–73. 10.1016/j.rcl.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 18.Benjamin M, Toumi H, Suzuki D, et al. Evidence for a distinctive pattern of bone formation in enthesophytes. Ann Rheum Dis 2009;68:1003–10. 10.1136/ard.2008.091074 [DOI] [PubMed] [Google Scholar]
- 19.Song L-cheng, Xu Q, Li H, et al. Osteochondroma of the pubic symphysis causing hematuria: a case report and literature review. BMC Urol 2021;21:1. 10.1186/s12894-020-00770-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Szopiński TR, Sudoł-Szopińska I, Furmanek MI, et al. Degeneration of the symphysis pubis presenting as a submucosal urinary bladder tumour. Wiitm 2012;1:55–8. 10.5114/wiitm.2011.25622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mnif H, Zrig M, Koubaa M, et al. An unusual complication of pubic exostosis. Orthop Traumatol Surg Res 2009;95:151–3. 10.1016/j.otsr.2009.02.003 [DOI] [PubMed] [Google Scholar]
- 22.Kim SC, Weiser AC, Nadler RB. Resection of a posterior pubic symphyseal protuberance using the electrocautery device. Urology 2000;55:586–7. 10.1016/S0090-4295(99)00559-2 [DOI] [PubMed] [Google Scholar]
- 23.Marshall FF, Hortopan SC, Lakshmanan Y. Partial resection of symphysis: an aid in radical prostatectomy. J Urol 1997;157:578–9. 10.1016/S0022-5347(01)65208-X [DOI] [PubMed] [Google Scholar]