Abstract
Objectives
To establish the priorities of primary care providers to improve assessment and treatment of skin sores and sore throats among Aboriginal and Torres Strait Islander people at risk of acute rheumatic fever (ARF) and rheumatic heart disease (RHD).
Design
Modified eDelphi survey, informed by an expert focus group and literature review.
Setting
Primary care services in any one of the five Australian states or territories with a high burden of ARF.
Participants
People working in any primary care role within the last 5 years in jurisdiction with a high burden of ARF.
Results
Nine people participated in the scoping expert focus group which informed identification of an access framework for subsequent literature review. Fifteen broad concepts, comprising 29 strategies and 63 different actions, were identified on this review. These concepts were presented to participants in a two-round eDelphi survey. Twenty-six participants from five jurisdictions participated, 16/26 (62%) completed both survey rounds. Seven strategies were endorsed as high priorities. Most were demand-side strategies with a focus on engaging communities and individuals in accessible, comprehensive, culturally appropriate primary healthcare. Eight strategies were not endorsed as high priority, all of which were supply-side approaches. Qualitative responses highlighted the importance of a comprehensive primary healthcare approach as standard of care rather than disease-specific strategies related to management of skin sores and sore throat.
Conclusion
Primary care staff priorities should inform Australia’s commitments to reduce the burden of RHD. In particular, strategies to support comprehensive Aboriginal and Torres Strait Islander primary care services rather than an exclusive focus on discrete, disease-specific initiatives are needed.
Keywords: primary care, public health, tropical medicine
Strengths and limitations of this study.
This eDelphi study is the first structured approach to understanding what primary care staff think are the biggest priorities for improving primary prevention of acute rheumatic ever.
Two rounds of Delphi responses are used to elucidate consensus priorities of primary care staff.
In addition to quantitative Delphi survey results, a large amount of qualitative data strengthens the study and interpretation of results.
Limitations of the study include a modest number of total participants and the necessary limitation of purposive sampling to include experiential experts.
Introduction
Rheumatic heart disease (RHD) is a consequence of acute rheumatic fever (ARF), stemming from an abnormal immune reaction to untreated group A streptococcal (Strep A) infection. RHD is rare in most high-income countries but persists in low-income and middle-income countries and marginalised First Nations people in high-income settings.1 Aboriginal and Torres Strait Islander people in Australia have a high prevalence of RHD, leading to the greatest disparity in cardiovascular disease burden between Aboriginal and Torres Strait Islander people and non-Indigenous people.2 3 The highest rates of ARF and RHD occur in remote and very remote Aboriginal and Torres Strait Islander communities in Northern Australia.2 These remote communities are socioeconomically deprived, with low household income, high rates of crowded living environments and substantially lower life expectancy than urban and non-Indigenous people in Australia.4 5 These consequences of colonisation drive very high rates of ARF through indirect and direct risk factors.6 Skin infections are endemic in remote communities with almost half of all children having skin infections at any time.7 The primary pathogen of these skin infections is Streptococcus pyogenes (Strep A).8 The incidence of throat infections is less well described, although there are indications that the rate of symptomatic pharyngitis is relatively low in ARF endemic Australian settings.9 10 The high burden of early-life Strep A skin and throat infections is thought to lead to immune priming which increases the risk of developing ARF in childhood.11
There are a number of opportunities to intervene on the causal pathway from Strep A infection to ARF, RHD and subsequent complications.12 One of these opportunities is primary prevention. In the absence of a vaccine, primary prevention of ARF is exclusively antibiotic treatment of Strep A infections to reduce the risk of developing ARF.13 The risk reduction for ARF following Strep A throat infection is well described. Treatment with oral penicillin can reduce the attack rate of ARF following Strep A throat infection by about 70%, increasing to 80% if a single intramuscular injection of benzathine benzylpenicillin is given within 9 days of symptom onset.14 The risk reduction of ARF following skin sores has not been empirically well documented but is biologically plausible and consistent with increasingly nuanced understanding of ARF pathogenesis.15 On this basis, if Strep A infections can be diagnosed and promptly treated with appropriate antibiotics, many episodes of ARF would be preventable.13 14
Over the last decade, Australia’s efforts to reduce the burden of RHD have largely focused on delivering secondary prophylaxis for people who have already had ARF.16 17 An external review of Australia’s Rheumatic Fever Strategy in 2017 identified improving primary prevention of ARF as a priority for ending RHD in Australia; however, there is no consensus on how this can be achieved.16 Research, anecdote and opinions suggest that a wide range of strategies could be effective in improving treatment of sore throat and skin sores. However, potential approaches have not been collated, reviewed or consulted with stakeholders. Clinics seeking to improve primary prevention have little indication of which strategies have a robust evidence base or stakeholder support for prioritisation. The END RHD Centre of Research Excellence (END RHD CRE) was funded in 2014 to help identify an ‘endgame’ for RHD in Australia, including recommendations to strengthen primary prevention of ARF.17
This study, embedded within the END RHD CRE, is intended to give voice to the operational priorities of primary healthcare staff working in Aboriginal and Torres Strait Islander health for improving primary prevention. The aim of the study is to identify which strategies primary healthcare workers believe would be most effective in improving assessment and treatment of sore throat and skin sores in remote Aboriginal and Torres Strait Islander communities. Directly, these consensus findings help inform the RHD Endgame Strategy.17 Indirectly, this study adds to international literature about access to healthcare for Indigenous people by applying a disease-specific lens to an existing framework for analysing access. Finally, it seeks to provide avenues for future research to address knowledge gaps and implementation science to prevent RHD.
Methods
Focus group and theoretical framework
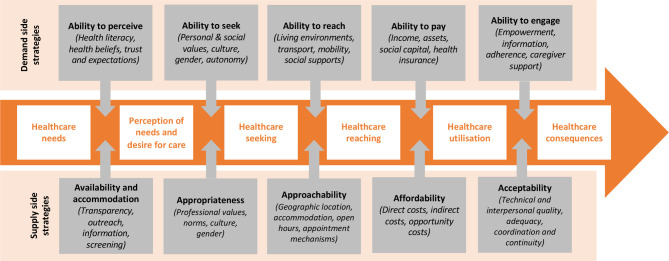
A focus group of END RHD CRE investigators and affiliates was initially convened to inform the scope of this research. The group was asked two questions: (1) ‘What are the priority actions to improve primary prevention of ARF?’ and (2) ‘Which are the three highest priorities?’ Responses were discussed and consensus recommendations were incorporated into a conceptual framework of access to healthcare proposed by Levesque et al which has also been adapted for use in Indigenous primary healthcare settings (figure 1).18 19
Figure 1.
Conceptual framework on access to healthcare (adapted from Levesque et al18).
Literature review
Informed by the focus group findings, a literature review was conducted to identify potential strategies for improving delivery of primary prevention and to sort these according to the Levesque et al’s conceptual framework. A Medline search of peer-reviewed literature from Australia and New Zealand from January 2010 to December 2018 was conducted (search strategy, online supplemental material 1). We focused only on publications from Australia and New Zealand as both countries experience a large burden of ARF and RHD among Indigenous communities, have comparable health systems and some shared challenges in improving access to healthcare. Citation tracking and recommendations from the investigator team were used to identify additional relevant publications. A supplemental grey literature search using Google was conducted to identify operational reports and programme evaluations using adapted search terms [rheumatic fever + (prevention / plan / program / strategy) + (Australia / New Zealand)]. All documents were reviewed for specific strategies to improve assessment and treatment of skin sores and/or sore throats. Strategies were eligible for inclusion if they were an ‘implementable action’, specifically something which clinics or communities could do. Suggestions about research priorities and broad statements about general strategies were not included. Strategies identified in each document were extracted to a Microsoft Excel file by two authors and duplicates removed. Strategies were then sorted into thematic areas of the Levesque et al’s access framework, reviewed by the authorship team and transformed into statements suitable for electronic Delphi (eDelphi) review.
bmjopen-2021-056239supp001.pdf (32.2KB, pdf)
eDelphi study
The Delphi technique is used to identify consensus areas between experts, particularly ‘in scenarios which cannot feasibly or ethically be subject to a randomised controlled trial’.20 The approach involves experts providing feedback on different options over repeated ‘rounds’, with feedback between rounds to move the group towards consensus. eDelphi approaches mirror the process of an in-person Delphi, but maximise opportunities for people to participate from different places and at times most convenient to them. In this study, primary care staff with frontline expertise in service delivery participated in an eDelphi study to identify consensus priorities to improve assessment and treatment of skin sores and sore throat for primary prophylaxis of ARF.
Patient and public involvement
Patient and public stakeholders were not directly involved in this study of health professional preferences. However, patient perspectives were included in the literature review to solicit potential approaches to improving primary prevention.
Three levels of statements were developed from the literature synthesis: concepts (overarching ideas, ‘“what” should be done’), strategies (different approaches to implementing concepts) and actions (‘“how” concepts should be done’). Language in each statement was standardised to maximise applicability for both skin sores and sore throat and throughout Australia. A Research Electronic Data Capture database was built to electronically present concepts, strategies and actions for ranking by participants.21
Potential participants were identified through the professional networks of the investigator team. Participants were eligible if they had worked in any primary care role (including general practitioner, nurse, Aboriginal and Torres Strait Islander health practitioner, environmental health worker, school nurse, administrator, receptionist) within the last 5 years in one of the five states or territories with a high burden of ARF (New South Wales, Queensland, Northern Territory, South Australia, Western Australia). Invitation emails containing a link to Round 1 of the eDelphi were sent to participants, followed by three reminder emails to participate over the following 2 weeks. In Round 1, participants rated each concept on 1–5 Likert scale ranging from low priority to high priority. If the concept was identified as low priority (1–3/5), the participant moved automatically to the next concept. If the concept was identified as high priority (4–5/5), the participant was asked to rank associated strategies and actions on the 1–5 scale. Following each concept, participants were also asked to add other strategies or comments about improving primary prevention as free text entries.
Round 1 responses were extracted and organised in a spreadsheet. Concepts rated as high priority (Likert 4 or 5) by more than 80% of participants were considered to be endorsed. Concepts rated as high priority by 60%–80% of participants were considered equivocal and re-presented to participants in Round 2 alongside feedback from the group, allowing participants to adjust their ranking with a view to forming a consensus opinion. Round 1 concepts that were considered by fewer than 60% of participants to be high priority were excluded. New concepts, strategies or actions identified from free text responses in Round 1 were also coded and presented to participants in Round 2. Participants who completed Round 1 were emailed 4 weeks later to complete Round 2. Concepts rated as high priority (Likert 4 or 5) by more than 80% of participants were considered to be endorsed. All other Round 2 concepts were excluded.
Qualitative data
Free text entries were also thematically analysed, identifying concept-specific feedback and overarching themes about primary prevention priorities.
All authors, two of whom are Aboriginal, contributed to interpretation of results.
Results
Scoping expert focus group
The expert focus group was convened in May 2018 and had nine participants: six researchers, two clinicians and one ‘employed in RHD’ to generate a framework for literature review. Seven participants worked primarily in Australia, one in New Zealand and one in another international setting. There were no Aboriginal or Torres Strait Islander participants. Twenty-seven distinct approaches for improving primary prevention were identified by the focus group (online supplemental material 2). The group identified the three highest priorities as:
bmjopen-2021-056239supp002.pdf (48.1KB, pdf)
Health promotion, awareness and education campaign for skin sores and sore throats targeting health workers, education providers, community members and families.
Augmented approaches that look at new ways to improve identification and management of sore throat: exploring community worker roles, disruptive technologies such as clinical photography and telehealth, point-of-care tests and integration with other health issues, community knowledge and preferences.
Research to understand sore throat burden, how to improve control of skin infections in Aboriginal and Torres Strait Islander communities and Strep A vaccine development.
Literature review
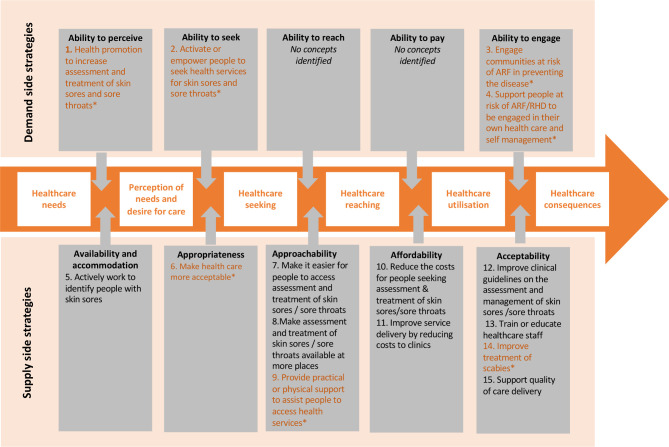
In total, 57 Australasian sources were identified containing suggested approaches to improving assessment and treatment of skin sores or sore throat. Twenty-seven publications were identified from a Medline search with citation review; an additional 30 grey literature documents were identified from the internet Google search. Grey literature was drawn from a broad range of sources, including six ‘Rheumatic Fever Prevention Plans’ developed by District Health Boards in New Zealand and consultative outcomes (including an RHDAustralia colloquium in 201522 and evaluation of the Australia’s Rheumatic Fever Strategy in 201716). From these sources, 15 concepts, comprising 29 strategies and 63 different actions for improving primary prevention of ARF, were developed (online supplemental material 3). The 15 concepts were mapped to the Levesque et al’s access framework (figure 2).
Figure 2.
Concepts for improving primary prevention of acute rheumatic fever (ARF) mapped to the Levesque et al’s framework for access to healthcare. *Strategies subsequently endorsed by the eDelphi process are indicated in orange text. RHD, rheumatic heart disease.
bmjopen-2021-056239supp003.pdf (71.8KB, pdf)
Electronic Delphi
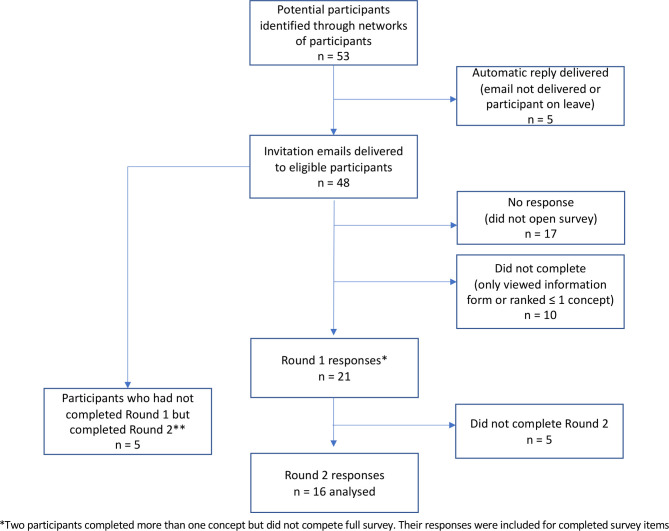
Investigators identified 53 potential participants through their professional networks. Recruitment, response and retention rates are outlined in figure 3; 43% of eligible participants successfully contacted by email participated in Round 1 and 16 (76%) of these people also participated in Round 2.
Figure 3.
Recruitment, response and retention rates in Round 1 and Round 2 of the eDelphi process. *Two participants completed more than one concept but did not complete the full survey. **Invitations to participate in Round 2 of the eDelphi process were inadvertently shared with people who did not participate in Round 1. Five people responded to this invitation and participated in Round 2 who had not participated in Round 1 and these responses were not included in the analysis.
Overall, 26 people completed either Round 1 or Round 2 of the eDelphi process between June and September 2019. Demographic details of participants are presented in table 1. Two participants identified as an Aboriginal or Torres Strait Islander person.
Table 1.
Characteristics of n=26 participants who completed either Round 1 or Round 2 of the eDelphi survey
| n (%) | |
| Professional role | |
| General practitioner | 13 (50) |
| Registered nurse | 3 (12) |
| Aboriginal or Torres Strait Islander health professional | 1 (4) |
| Environmental health worker | 1 (4) |
| Not stated | 8 (31) |
| Jurisdiction | |
| Northern Territory | 12 (46) |
| South Australia | 2 (8) |
| Western Australia | 2 (8) |
| Queensland | 1 (4) |
| New South Wales | 1 (4) |
| Not stated | 8 (31) |
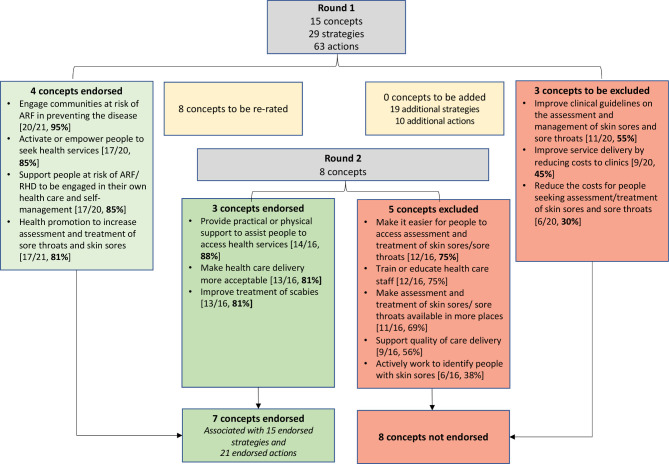
After the two rounds, seven concepts (including 15 strategies and 21 actions) were endorsed as priorities by participants and eight concepts were not endorsed (figure 4 and online supplemental material 4).
Figure 4.
Outcomes of Round 1 and Round 2 of eDelphi process. ARF, acute rheumatic fever; RHD, rheumatic heart disease.
bmjopen-2021-056239supp004.pdf (81.6KB, pdf)
Qualitative data findings
In total, 287 additional free text entries were provided by the participants across two survey rounds. Two passes of qualitative analysis were conducted. The first pass consolidated feedback specific to each concept; this occurred after Round 1 to inform the development of Round 2, and again after Round 2 to explore the evolution of consensus. This concept-specific analysis is presented in online supplemental material 5. A second pass inductive analysis was conducted to identify repeated themes spanning across concepts to develop an understanding of deeper structural determinants of concept-specific responses. Three overarching themes were identified; these themes were well illustrated with specific reference to skin sores (see box 1).
Box 1. Skin sores—an object lesson for qualitative themes.
Skin sores provide a tangible example of how these themes affect access to health services. Participants identified in Theme 1 that the priority for skin sores was prevention rather than treatment: ‘As per previous suggestions re skin sores having access to freely available hot water to wash clothes and bedding on a regular basis (not just when they have scabies) rather than having to buy a power card to wash with hot water’ (ID13). In Theme 2, the importance of culturally responsive care, ideally by Aboriginal and Torres Strait Islander providers, was highlighted in order to work effectively within belief systems about skin sores which included both normalisation and stigmatisation: ‘Need to reduce the shame factor and association with poor hygiene’ (ID23) and ‘“Denormalising” skin sores is very important’ (ID17). Skin sore stigma was also described by healthcare workers, and some participants identified the risk that health promotion activities further contribute to this issue: ‘Health service led efforts are never going to be as effective as community led initiatives to improve treatment uptake and may contribute to stigma associated with skin sores’ (ID13). Others reported that skin sores were considered a low clinical priority in some clinics, potentially contributing to the barriers to access expanded on in Theme 3 (‘Not being sent away from clinics … told not an emergency… come back tomorrow’ (ID21)), though this was not universal.
bmjopen-2021-056239supp005.pdf (86.4KB, pdf)
Theme 1: prevention and environmental health
Although eDelphi statements related to primary prevention of ARF through treatment of skin sores and sore throat, a large number of participants provided comments about how skin sores and sore throat could be better prevented. Some of these comprised opportunities to embed preventative actions within primary care services: ‘Linking primary care services with the ability to refer for services to address the social determinants of health in households with high rates of sore throats or skin sores, for example, access to improved housing, reliable power and water, washing machines etc’ (ID9). However, the majority of qualitative comments implied that eDelphi statements about clinic-based activities to improve primary prevention were of limited value without separate and broader action on environmental determinants of health: ‘Primary prevention ultimately can only be effective in reducing ARF alongside more effective primordial prevention measures’ (ID20).
Theme 2: Aboriginal and Torres Strait Islander health workforce, culture and community
Workforce issues were identified as relevant in almost all concepts. This included inadequate overall numbers of staffing in primary care (limiting access to approachable, timely care and guideline-based, technically acceptable services) and too few Aboriginal and Torres Strait Islander people delivering healthcare, contributing to care which people could not access or engage with: ‘If a health service has a large number of Indigenous staff this will provide much better cultural oversight than giving 'formal' cultural training’ (ID13). By extension, the significance of Aboriginal and Torres Strait Islander ways of knowing, being and doing was addressed in a number of domains. Operationally, this included strong support for the use of materials in Aboriginal and Torres Strait Islander languages for engagement, education and health promotion. Some participants provided more detailed reflections about the importance of using Aboriginal and Torres Strait Islander languages: ‘Most health inequity is due to ongoing colonisation, including loss of languages and culture. Including Aboriginal languages especially on a health topic sends a very strong message’ (ID23). eDelphi statements about approachability and ability to engage in health services also elicited a number of reflections about services which are not culturally responsive nor welcoming for Aboriginal and Torres Strait Islander people attending with skin sores and sore throat: ‘And how to manage culture shock and be aware of own prejudice when treating patients - can be very hard for patients to keep turning up when they feel misrepresented and misunderstood’ (ID19). Community control of health services, incorporation of traditional medicines and community engagement were suggested by some participants as a means to improve culturally responsive care.
Theme 3: permeability and navigability of primary healthcare services
Issues raised in Theme 2 manifest a number of tangible barriers to people accessing care, including long waiting times, limited after-hours services for non-urgent care, inadequate transport and lack of outreach services. Participants identified a number of mitigating strategies, with strong support for increasing outreach care (particularly through schools) and extended clinic opening hours: ‘Provide flexible access options to assessment and treatment. Perhaps option of streamlined skin check clinics, perhaps clinic for adults as well as their children collocated? at school for pickup drop off time walk-in’ (ID16).
Discussion
This study provides insights into primary care worker priorities to improve assessment and treatment of skin sores and sore throat among Aboriginal and Torres Strait Islander people as a core activity for prevention of ARF. It is the first time we are aware of that a primary care approach to inform priorities has been used for primary prevention of ARF, and aligns with the key characteristics of effective Indigenous-led primary care.23 Four of seven endorsed priorities were demand-side domains (ability to perceive, ability to seek and ability to engage in healthcare). These were also the domains with high levels of agreement which were endorsed in Round 1, though agreement varied on specific associated actions. For example, ‘engage communities at risk of ARF in preventing the disease’ was ranked as high priority by 20/21 (95%) respondents to that question, with support for specific actions ranging from 100% (Engage communities by addressing attitudes to skin sores including reducing stigma and denormalising skin sores) to 69% (Engage communities by improving access to local information about the rates of Strep A infection, ARF and RHD). Collectively, endorsed demand-side concepts reflect a provider focus on how services are delivered to drive greater demand for health services, including partnership with communities, empowerment, appropriate health promotion and self-management support. Three of seven endorsed priorities were supply-side strategies (approachability, acceptability and appropriateness). These supply-side issues reflected a similar focus on providing accessible, culturally responsive, primary healthcare services. Conversely, all of the domains which were not endorsed were supply side, including clinic-level activities like healthcare worker training, quality improvement activities and clinical guidelines. ‘Improving treatment of scabies’ was an endorsed supply-side priority, somewhat incongruent with the broader focus on disease-agnostic priorities. This may reflect specific concern about scabies as a risk factor for skin sores or exposure to focused education on the impact of scabies.
Supply-side barriers to access (including navigability and permeability of services24 were identified in qualitative feedback, including waiting times, limited after-hours services and limited outreach capacity. A number of participants reflected on the root cause of these barriers, including an inadequate primary care workforce with too few Aboriginal and Torres Strait Islander people employed and too few employed to their full scope of practice. Navigability barriers have been reported in a number of other primary care studies and tackling these provides an ongoing opportunity to improve service access.19 23 25 26 Outreach services to provide care in schools, in homes and to remote outstations were particularly emphasised in this study. Participants reflected on barriers and enablers to outreach, including the difficulty of delivering treatment outside clinical settings and the potential role of telehealth in supporting outreach workers to communicate with clinic-based staff. Despite these comments, eDelphi concepts including ‘make it easier for people to access assessment and treatment of skin sores and sore throat’ and ‘make assessment and treatment of skin sores and sore throat available in more places’ were not endorsed by the group. This may be because comments on care accessibility may have been perceived as an essential standard of care that did not need re-emphasis. They were dwarfed by feedback on the importance of community, cultural and clinic context in which people seek and receive primary care, including who provides care, how it is governed and how communities participate in decision-making.
Few qualitative responses were specific to the issue of skin sores and sore throat. Rather, they reflected broader determinants of effective primary care for Aboriginal and Torres Strait Islander people. A 2018 systematic review of the characteristics of effective Indigenous primary care identified eight interdependent elements: culture, accessible health services, community participation, continuous quality improvement, culturally appropriate and skilled workforce, flexible approach to care, holistic healthcare, and self-determination and empowerment.23 Each of these elements was clearly identifiable in qualitative responses to this eDelphi.
The prioritisation by primary care staff of how—structurally and culturally—care is delivered for skin sores and sore throat is telling. Culturally and contextually appropriate ways of working in Aboriginal and Torres Strait Islander health are already widely acknowledged to be a major determinant of care quality and outcomes.23 27 However, it is not always clear how these ‘horizontal’ system issues relate to vertical, disease-specific initiatives. Efforts to improve care for specific conditions more commonly focus on tangible supply-side interventions such as clinical guidelines, decision support and staff training. For example, in 10 clinics participating in a stepped wedge study to improve delivery of secondary prophylaxis for people with ARF, action plans developed by clinic staff included far more actions addressing clinical information systems (29 items) than community linkages (4 items) or self-management support (4 items).28 Qualitative evaluation of that study found that limited attention to community linkages and self-management, in addition to contextual factors, contributed to limited gains in secondary prophylaxis adherence.29 This eDelphi parallels these findings, providing more evidence from clinical staff that the context in which disease-specific initiatives are implemented is likely to be the determining factor of success. The participating primary care providers in the current study indicated lack of support for approaches which prioritise clinical supply-side issues over systematic approaches to strengths-based, comprehensive, community-engaged, culturally responsive primary care. A number of participants specifically identified the risks of vertical programmes fragmenting care or services. Overall, supply-side supports (such as clinical guidelines and staff training) are likely to be prerequisites to successful disease management; but time, staffing and cultural constraints identified by primary healthcare staff may make use of these resources prohibitively difficult. Participants identified broader contextual factors as priorities in this study; presumably to potentiate use of existing and emerging resources. Notably, priorities identified by primary care differed from the scoping expert focus group (comprising primarily researchers and RHD content experts) which focused on health promotion, improved clinical approaches to primary care and the need for further research. This highlights that different stakeholders—including lived experience experts, service provision experts and subject matter experts—have varying perspectives and priorities. Understanding and integrating these perspectives into service design is likely to best support improved care delivery.
This study was designed to identify clinic-level strategies in primary care for improving primary prevention (by definition, once Strep A infections have already occurred) and therefore did not include eDelphi statements related to community-level risk reduction strategies. However, this appeared to be an arbitrary distinction for participants; many emphasised that clinical primary prevention strategies alone would be insufficient. Risk factors for Strep A infections, ARF and RHD include household crowding, inadequate access to health hygiene infrastructure and socioeconomic marginalisation.30 In particular, housing and environmental health factors are the major driver of Strep A skin sores in remote Aboriginal and Torres Strait Islander settings.31 Approaches for integrating environmental health into clinical care delivery were suggested by participants, including the need for referral pathways for environmental assessments and services. Efforts to integrate environmental health into comprehensive primary care are increasing in some parts of Australia and warrant ongoing development.32 33 Other participants identified that broader actions addressing the social and environmental drivers of Strep A infection outside the health service are needed, including new housing and infrastructure. Some responses implied a frustration that the greatest outstanding needs for addressing skin sores and sore throat were outside the influence of primary care staff and services.
Skin sores were an important object lesson, illustrating a broad range of clinical and non-clinical issues which participants considered to be priorities. Primary healthcare staff identified complex attitudes influencing community and clinic responses to skin sores, including stigma, normalisation and a strong association with poor hygiene. This resonates with a recently published study on barriers and enablers to skin sore treatment in the Pilbara, which found that shyness, shame, fear of judgement, normalisation and prejudice were significant factors in the decision to seek care.34 Primary healthcare staff in this eDelphi study, and in the Pilbara study, identified health promotion as a priority to increase health seeking for skin sores.34 However, a number of participants discussed the risk of inadvertently increasing stigma if skin sores were associated with poor hygiene in health promotion activities. A strong message from community is to prioritise a strengths-based approach to health promotion.35 This risk is real; stigmatisation associated with health promotion campaigns about sore throat and ARF for Māori and Pacific Islander peoples in New Zealand has been well described.36 Similarly, health promotion about handwashing and healthy living practices may be alienating if people do not have access to functional household infrastructure such as taps and soap.37 Participants identified that culturally relevant, stigma-free health information about skin sores in Aboriginal and Torres Strait Islander languages was a priority. Other qualitative comments made it clear that effective knowledge transfer was predicated on community engagement and access to environmental health supports which would allow people to engage with and act on this information.
This study has a number of limitations. Participants were identified through the professional networks of the investigator team. Therefore, they may not be representative of the primary care workforce or may have been sensitised to issues around ARF and about cultural safety in healthcare. Network-based deliberative sampling is common in Delphi studies.38 Identifying participants through the networks of multiple investigators to approach colleagues in different jurisdictions, roles and professional contacts helps mitigate this risk. The overall number of study participants was modest, though a 43% response rate higher than some comparable eDelphi projects involving primary healthcare in Australia.39 Further, participants were drawn from all five jurisdictions in Australia with ARF/RHD registers and the number of participants is comparable with other eDelphi studies in Aboriginal and Torres Strait Islander health.20 Only two Aboriginal and Torres Strait Islander people participated in this study; consequently, results predominantly reflect perspectives of non-Indigenous remote health staff. It is critically important that findings from this study are considered in conjunction with the perspectives and priorities of Aboriginal and Torres Strait Islander people with lived experience expertise of skin sores, sore throat and at risk of ARF. A number of publications address the experiences of Aboriginal and Torres Strait Islander people with skin sores and address common themes, including that information provided only in English is of limited value and that experiences at the clinic have a major influence on care-seeking behaviour.34 40 41 Most Round 1 respondents (76%) also completed Round 2, indicating reasonable engagement in the process, and the quantity and quality of free text comments indicate that participants were deeply committed and thoughtful with regard to their responses. Detailed qualitative analysis is not a routine part of eDelphi methodology, though qualitative adaptations have been described.38 42 The volume and detail of free text responses to this eDelphi made it possible to use inductive thematic analysis to better understand the rationale for participants endorsing and not endorsing different concepts.
This study suggests that primary care providers perceive that improvements in primary prevention of ARF need to come from broad systems strengthening to achieve excellence in culturally safe primary healthcare. This aligns with what is already known about accessible primary care for Indigenous people and the priorities of Aboriginal and Torres Strait Islander people, including those living with skin sores, sore throat, ARF and RHD.23 34 41 A number of initiatives are underway to map a pathway to end RHD in Australia, including the RHD Roadmap and the RHD Endgame Strategy.43 44 This eDelphi study suggests these efforts should call for culturally responsive, comprehensive primary healthcare for Aboriginal and Torres Strait Islander people which involves whole communities and is readily navigable for people seeking care. These system approaches should be augmented by a small number of disease-specific strategies for tackling Strep A infections.
Conclusions
This eDelphi study demonstrates that primary care staff prioritise demand-side determinants of access to healthcare to improve primary prevention of ARF among Aboriginal and Torres Strait Islander people. In particular, partnership with communities, empowerment, self-management support and approachable care were emphasised. These priorities reflect a focus on how care is delivered in context, rather than technical details of the care itself. Participants largely rejected the idea of vertical, disease-specific strategies to improve primary prevention and consistently identified horizontal, access-strengthening approaches as current priorities. Ultimately, these components are indivisible; guideline and training supports to improve the quality of supply-side primary prevention must be coupled with attention to demand-side drivers which enable people to seek and engage with care. The importance of environmental health strategies and strengthening the Aboriginal and Torres Strait Islander health workforce exemplify that a comprehensive approach to prevention and treatment is also needed for meaningful impact on skin sores and sore throat. Qualitative responses highlighted the importance of a comprehensive primary healthcare approach as standard of care rather than disease-specific strategies related to management of skin sores and sore throat.
Supplementary Material
Acknowledgments
The authors thank Christine Balane for her support to develop the REDCap database used in this project, Stephanie Enkel for extraction of qualitative data and the participants of the focus group and eDelphi.
Footnotes
Twitter: @rosemarywyber, @annapralph, @ashabowen
Contributors: RW, JC and DP conceived the study design. RW, GP and JC developed the formative focus group. RW and CL completed the literature review and extracted the eDelphi statements based on the conceptual framework. All authors (RW, CL, VW, GP, JC, APR, ACB, DP) reviewed the eDelphi statements, and contributed to identification of potential participants and interpretation of results. RW wrote the draft and is guarantor of the study, with contribution from all authors to development of the manuscript text.
Funding: This work was supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship to RW (1151165). APR is supported by an NHMRC Fellowship (1142011). DP is supported by an NHMRC Fellowship (1143904) and a National Heart Foundation Fellowship (101890).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants. Ethics approval for the formative focus group was provided by the Human Ethics Committee of the University of Western Australia (RA/4/20/4489). Ethics approval for the eDelphi survey was provided by the Human Research Ethics Committees of the University of New South Wales (HC180879) and the Aboriginal Health and Medical Research Council of New South Wales (HC180879). Participants gave informed consent to participate in the study before taking part.
References
- 1.Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990-2015. N Engl J Med 2017;377:713–22. 10.1056/NEJMoa1603693 [DOI] [PubMed] [Google Scholar]
- 2.Australian Institute of Health and Welfare . Acute rheumatic fever and rheumatic heart disease in Australia. Canberra: AIHW, 2019. [Google Scholar]
- 3.Australian Institute of Health and Welfare . Australian burden of disease study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. Canberra: AIHW, 2016. [DOI] [PubMed] [Google Scholar]
- 4.ABS . 0 - Census of Population and Housing: Characteristics of Aboriginal and Torres Strait Islander Australians, 2016, 2076. Available: https://www.abs.gov.au/ausstats/abs@.nsf/7d12b0f6763c78caca257061001cc588/392cd9a0e6f7c543ca2583bb000e233d!OpenDocument
- 5.ABS . Aboriginal and Torres Strait Islander life expectancy lowest in remote and very remote areas, 2018. Available: https://www.abs.gov.au/ausstats/abs@.nsf/MediaReleasesByCatalogue/1A6806AB01AB38CDCA25835300141767?OpenDocument [Accessed 16 May 2020].
- 6.Wyber R, Wade V, Anderson A, et al. Rheumatic heart disease in Indigenous young peoples. Lancet Child Adolesc Health 2021;5:437-446. 10.1016/S2352-4642(20)30308-4 [DOI] [PubMed] [Google Scholar]
- 7.Davidson L, Knight J, Bowen AC. Skin infections in Australian Aboriginal children: a narrative review. Med J Aust 2020;212:231–7. 10.5694/mja2.50361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowen AC, Tong SYC, Chatfield MD, et al. The microbiology of impetigo in Indigenous children: associations between Streptococcus pyogenes, Staphylococcus aureus, scabies, and nasal carriage. BMC Infect Dis 2014;14:3854. 10.1186/s12879-014-0727-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDonald M, Brown A, Edwards T, et al. Apparent contrasting rates of pharyngitis and pyoderma in regions where rheumatic heart disease is highly prevalent. Heart Lung Circ 2007;16:254–9. 10.1016/j.hlc.2007.02.087 [DOI] [PubMed] [Google Scholar]
- 10.Ralph AP, Holt DC, Islam S, et al. Potential for molecular testing for group A Streptococcus to improve diagnosis and management in a high-risk population: a prospective study. Open Forum Infect Dis 2019;6:ofz097. 10.1093/ofid/ofz097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raynes JM, Frost HRC, Williamson DA, et al. Serological evidence of immune priming by group A streptococci in patients with acute rheumatic fever. Front Microbiol 2016;7:1119. 10.3389/fmicb.2016.01119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katzenellenbogen JM, Ralph AP, Wyber R, et al. Rheumatic heart disease: infectious disease origin, chronic care approach. BMC Health Serv Res 2017;17:793. 10.1186/s12913-017-2747-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali S, Engel M, Zühlke L, et al. Primary prevention of acute rheumatic fever and rheumatic heart disease. In: Dougherty S, Carapetis J, Zühlke L, et al., eds. Acute rheumatic fever and rheumatic heart disease. Missouri, United States of America: Elsivier, 2020. [Google Scholar]
- 14.Robertson KA, Volmink JA, Mayosi BM. Antibiotics for the primary prevention of acute rheumatic fever: a meta-analysis. BMC Cardiovasc Disord 2005;5:11. 10.1186/1471-2261-5-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watkins D, Baker M, Kumar R. Epidemiology, risk factors, burden and cost of acute rheumatic fever and rheumatic heart disease. In: Dougherty GJ, JR C, Zühlke L, edseds. Acute rheumatic fever and rheumatic heart disease. St Louis, Missouri, 2021. [Google Scholar]
- 16.Health Policy Analysis . Evaluation of the Commonwealth rheumatic fever strategy – final report. Canberra: Commonwealth Department of Health - Primary Healthcare Branch, 2017. [Google Scholar]
- 17.Wyber R, Noonan K, Halkon C, et al. Ending rheumatic heart disease in Australia: the evidence for a new approach. Med J Aust 2020;213(Suppl 10):S3–31. 10.5694/mja2.50853 [DOI] [PubMed] [Google Scholar]
- 18.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013;12:18. 10.1186/1475-9276-12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davy C, Harfield S, McArthur A, et al. Access to primary health care services for Indigenous peoples: a framework synthesis. Int J Equity Health 2016;15:163. 10.1186/s12939-016-0450-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hart LM, Jorm AF, Kanowski LG, et al. Mental health first aid for Indigenous Australians: using Delphi consensus studies to develop guidelines for culturally appropriate responses to mental health problems. BMC Psychiatry 2009;9:47. 10.1186/1471-244X-9-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.RHDAustralia, RHDA Colloquium . Developing a framework to enable a coordinated approach to acute rheumatic feer and rheumatic heart disase throughout Australia, 2015. Available: https://www.rhdaustralia.org.au/system/files/fileuploads/rhda_colloquim_participant_report_final2015.pdf [Accessed 15 Mar 2021].
- 23.Harfield SG, Davy C, McArthur A, et al. Characteristics of Indigenous primary health care service delivery models: a systematic scoping review. Global Health 2018;14:12. 10.1186/s12992-018-0332-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peiris D, Brown A, Cass A. Addressing inequities in access to quality health care for Indigenous people. CMAJ 2008;179:985–6. 10.1503/cmaj.081445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Askew D, Brady J, Brown A. To your door: factors that influence Aboriginal and Torres Strait Islander people seeking care, 2014. [Google Scholar]
- 26.Peiris D, Brown A, Howard M, et al. Building better systems of care for Aboriginal and Torres Strait Islander people: findings from the Kanyini health systems assessment. BMC Health Serv Res 2012;12:369. 10.1186/1472-6963-12-369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laverty M, McDermott DR, Calma T. Embedding cultural safety in Australia's main health care standards. Med J Aust 2017;207:15–16. 10.5694/mja17.00328 [DOI] [PubMed] [Google Scholar]
- 28.Ralph A, de Dassel JL, Kirby A. Improving delivery of secondary prophylaxis for rheumatic heart disase in a high-burden setting: outcomes of a stepped-wedge, community, randomized trial. JAMA 2018;7:e009308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Read C, Mitchell AG, de Dassel JL, et al. Qualitative evaluation of a complex intervention to improve rheumatic heart disease secondary prophylaxis. J Am Heart Assoc 2018;7:e009376. 10.1161/JAHA.118.009376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coffey PM, Ralph AP, Krause VL. The role of social determinants of health in the risk and prevention of group A streptococcal infection, acute rheumatic fever and rheumatic heart disease: a systematic review. PLoS Negl Trop Dis 2018;12:e0006577. 10.1371/journal.pntd.0006577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McMullen C, Eastwood A, Ward J. Environmental attributable fractions in remote Australia: the potential of a new approach for local public health action. Aust N Z J Public Health 2016;40:174–80. 10.1111/1753-6405.12425 [DOI] [PubMed] [Google Scholar]
- 32.Custodio J, Kelly G, Haenga M. Working in partnership with communities at risk: the potential of integrated public health action during an outbreak of APSGN in remote Australia. HealthBulletin 2016;16. [Google Scholar]
- 33.Government of Western Australia Department of Health . Environmental health referrals, 2020. Available: https://ww2.health.wa.gov.au/Articles/A_E/Environmental-health-referrals [Accessed 22 Jun 2020].
- 34.Hendrickx D, Amgarth-Duff I, Bowen AC, et al. Barriers and Enablers of health service utilisation for childhood skin infections in remote Aboriginal communities of Western Australia. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17030808. [Epub ahead of print: 28 01 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Askew DA, Brady K, Mukandi B, et al. Closing the gap between rhetoric and practice in strengths-based approaches to Indigenous public health: a qualitative study. Aust N Z J Public Health 2020;44:102–5. 10.1111/1753-6405.12953 [DOI] [PubMed] [Google Scholar]
- 36.Anderson A, Spray J. Beyond awareness: towards a critically conscious health promotion for rheumatic fever in Aotearoa, New Zealand. Soc Sci Med 2020;247:112798. 10.1016/j.socscimed.2020.112798 [DOI] [PubMed] [Google Scholar]
- 37.McDonald E, Slavin N, Bailie R, et al. No germs on me: a social marketing campaign to promote hand-washing with soap in remote Australian Aboriginal communities. Glob Health Promot 2011;18:62–5. 10.1177/1757975910393577 [DOI] [PubMed] [Google Scholar]
- 38.Niederberger M, Spranger J. Delphi technique in health sciences: a MAP. Front Public Health 2020;8:457. 10.3389/fpubh.2020.00457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heal C, Roberts G. General practice research priority setting in Australia: informing a research agenda to deliver best patient care. Aust J Gen Pract 2019;48:789–95. 10.31128/AJGP-05-19-4928 [DOI] [PubMed] [Google Scholar]
- 40.Bowen A. The SToP (see, treat, prevent) skin sores and scabies trial: a cluster randomised, stepped-wedge trial for skin disease control in remote Western Australia, 2018. Available: http://www.anzctr.org.au/TrialSearch.aspx?searchTxt=12618000520235&isBasic=True [Accessed 17 Jul 2019]. [DOI] [PMC free article] [PubMed]
- 41.Amgarth-Duff I, Hendrickx D, Bowen A, et al. Talking skin: attitudes and practices around skin infections, treatment options, and their clinical management in a remote region in Western Australia. Rural Remote Health 2019;19:5227. 10.22605/RRH5227 [DOI] [PubMed] [Google Scholar]
- 42.Guzys D, Threlkeld G, Dickson-Swift V, et al. Rural and regional community health service boards: perceptions of community health - a Delphi study. Aust J Prim Health 2017;23:543–8. 10.1071/PY16123 [DOI] [PubMed] [Google Scholar]
- 43.COAG Health Council . Council of Australian governments health Council Communique 8 March, 2019. [Google Scholar]
- 44.Wyber R, Katzenellenbogen JM, Pearson G, et al. The rationale for action to end new cases of rheumatic heart disease in Australia. Med J Aust 2017;207:322–3. 10.5694/mja17.00246 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056239supp001.pdf (32.2KB, pdf)
bmjopen-2021-056239supp002.pdf (48.1KB, pdf)
bmjopen-2021-056239supp003.pdf (71.8KB, pdf)
bmjopen-2021-056239supp004.pdf (81.6KB, pdf)
bmjopen-2021-056239supp005.pdf (86.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information.