Abstract
Background:
Myriad emotion regulation and coping theories have proposed that avoidant/emotion-oriented coping is a cause and consequence of anxiety and depression. However, few studies have investigated potential mechanisms underlying the prospective anxiety-depression disorder relation. The current study examined various coping strategies (i.e., denial, focus on and venting of emotion (FOAVE), and behavioral disengagement) as potential longitudinal mediators between generalized anxiety disorder (GAD) and major depressive disorder (MDD).
Methods:
In a nationally representative sample of adults (N = 3,294), MDD and GAD were assessed at Time 1 (T1) and Time 3 (T3) (Composite International Diagnostic Interview – Short-Form), and avoidant coping strategies (denial, behavioral disengagement, and FOAVE) were measured at Time 2 (T2) (Coping Questionnaire). Assessments occurred over 18 years, each spaced approximately 9 years apart. Structural equation modeling mediation analyses examined whether T1 MDD predicted T3 GAD (and vice versa), and if T2 avoidant coping mediated these relations, above and beyond baseline comorbidity.
Results:
FOAVE mediated the T1 MDD–T3 GAD association, and vice versa. Presence of T1 MDD and GAD predicted more T2 FOAVE, and greater T2 FOAVE forecasted T3 MDD and GAD, accounting for 16–21% of the longitudinal MDD-GAD relations. However, behavioral disengagement and denial did not mediate the prospective MDD-GAD relations. Also, T1 MDD and GAD forecasted greater T2 behavioral disengagement.
Conclusions:
The use of FOAVE, may be a mechanism by which MDD earlier in life may lead to GAD 18 years later, and vice versa. Theoretical and potential clinical implications are discussed.
Keywords: Generalized anxiety disorder, major depressive disorder, denial, venting, longitudinal, behavioral disengagement
Nearly 1 in 6 adults will experience depression at some point in their lives and 29% of people meet criteria for a lifetime anxiety disorder in the United States (Kessler & Wang, 2008). Of these, generalized anxiety disorder (GAD) and major depressive disorder (MDD) are two highly prevalent mental health problems in the U.S. These disorders are characterized by chronic fatigue, irritability, difficulty focusing, and sleep problems. Moreover, GAD and MDD have been related consistently to frequent interpersonal conflicts, poorer relationship quality (Jacobson & Newman, 2016; Shin & Newman, 2019), as well as decreased life satisfaction, educational, and economic attainment (Kessler et al., 2008). Further, elevated GAD and MDD have been associated independently with less personal monthly income on average (Dismuke & Egede, 2010) and lower life satisfaction (Beutel, Glaesmer, Wiltink, Marian, & Brähler, 2010). MDD and GAD can also lead to deleterious effects on physical health by impacting neurocognitive, physiological, cardiorespiratory, and immune systems (Bartek, Zainal, & Newman, 2021; Ottaviani et al., 2016; Zainal & Newman, 2021; Zainal & Newman, in press). Further, a robust GAD-MDD bidirectional association exists, such that GAD predicts future MDD, and vice versa (see meta-analyses by Jacobson & Newman, 2017). Thus, understanding the mechanisms accounting for the GAD-MDD prospective relation is important.
The scar theory proposes that elevated anxiety and depression can reinforce maladaptive habits (e.g., avoidant coping, suboptimal lifestyle choices) across prolonged durations by impacting vulnerability factors over time (Lewinsohn, Steinmetz, Larson, & Franklin, 1981). The idea is that heightened depression and anxiety symptoms could entrench sedentary lifestyles (e.g., physical inactivity, addictive behaviors that trade off short-term momentary pleasure or relief for long-term increased negative affect) (Bonnet et al., 2005), unhelpful beliefs, and construal biases, over long durations (Just, Abramson, & Alloy, 2001). Consequently, scar theory argues that heightened depression and anxiety might chronically result in increased risk of diverse physical illness (Kessler, Ormel, Demler, & Stang, 2003; Stewart, Rand, Muldoon, & Kamarck, 2009), and adversely affect close relationships (Newman & Zainal, 2020; Santini et al., 2020), thereby elevating risk for more future mental health problems. Based on the scar theory, it is thus plausible that avoidant coping strategies, such as excessive focus on and venting of emotion, denial, and behavioral disengagement that were not present prior to the disorders may emerge and persist even as symptoms abate over time.
In support of the scar model, five studies have shown that depression and anxiety disorders predicted future heightened use of avoidant coping strategies. For example, across 3 years, individuals with multiple sclerosis with increased depressive mood displayed significant decrements in active coping styles (Arnett & Randolph, 2006). Moreover, adolescents with elevated levels of depression and anxiety subsequently showed more reliance on disengagement, rumination, and social avoidance (Zimmer-Gembeck, 2015). Consistent with those findings, patients diagnosed with amyotrophic lateral sclerosis who had more symptoms of anxiety and depression utilized less active and positive mood-inducing coping strategies over time (Jakobsson Larsson, Nordin, & Nygren, 2016). Recently, a study showed that a 9-year increase in counts of MDD, GAD, and panic disorder diagnoses predicted larger future 9-year declines in goal persistence and positive appraisal (Zainal & Newman, 2019). All in all, these studies support the idea that over long periods, depression and anxiety disorders render people vulnerable to using avoidant coping mechanisms in the future.
In the past 50 years, myriad coping theories have proposed that avoidant behavioral and maladaptive cognitive patterns predispose individuals to future MDD and GAD. The transactional model of stress and coping posits that avoidant or emotion-oriented coping strategies in response to controllable stressors (i.e., persistent attempts to evade problems or to deal with them indirectly) negatively impact the wellbeing of an individual across time (Lazarus & Folkman, 1984). Relatedly, the learned helplessness theory postulates that risk factors for MDD can include the tendency to avoid responsibilities, assume the worst, lack of initiative, prolonged inactivity, and reduced participation in meaningful pursuits (Maier & Seligman, 2016; Seligman & Ollendick, 1998). The response styles theory posits that rumination exacerbates depression by enhancing negative thinking and impairing problem solving and is correlated with higher levels of general anxiety; rumination is positively related to avoidant coping (Nolen-Hoeksema, et al., 2008). Focus on and venting of emotion is similar to rumination, as both processes involve excessively to attending past events in non-constructive ways. Taken together, theories suggest that avoidant coping strategies (e.g., denial, focus on and venting of emotion, and behavioral disengagement) may present as risk factors of MDD and GAD.
Thus far, seven longitudinal studies have examined whether avoidant coping strategies preceded and predicted anxiety and depression disorders. One study tested if there was a positive relation between avoidant coping and anxiety or depression severity across 12 months among women undergoing fertility treatments (Verhaak et al., 2005); however, this study observed a null relation between avoidant coping and mental health symptoms. Conversely, supporting the stress-coping transactional model, chronically ill patients who used more avoidant coping were at higher risk for developing depression (Rabinowitz & Arnett, 2009). Similarly, avoidant coping was detrimental to the physical and psychological health of undergraduate students (Elliot, Thrash, & Murayama, 2011); however, as this study was conducted over a 15-week period, it might not generalize across adulthood development. Likewise, an 18-month study indicated that increased trait-level passivity was related to a rise in depressive symptoms among breast cancer patients (Avis et al., 2013). Moreover, across four weeks, women with high anxiety sensitivity tended to utilize more avoidant coping mechanisms, including disengagement, denial and suppression of competing activities (Sigmon, Whitcomb-Smith, Rohan, & Kendrew, 2004). Further, lower acceptance toward life events and use of emotion- (vs. problem-) focused coping toward controllable stressors predicted more anxiety symptoms in Western undergraduates over time (Szabo, Ward, & Jose, 2016). In addition, a recent 2-year longitudinal study noted that denial and avoidance was associated with higher future levels of anxiety and depression among dementia caregivers (del-Pino-Casado, Serrano-Ortega, López-Martínez, & Orgeta, 2019). On balance, the findings from these studies suggest that avoidant coping patterns would precede and forecast future depression and anxiety disorders.
So far, two studies have examined avoidant coping mechanisms as mediators of the prospective depression-anxiety relationship. In a four-wave study among children and adolescents, more anxiety symptoms significantly predicted greater depression severity over a decade later, and this anxiety-depression symptom relation was mediated by mid-time-point avoidance patterns (Jacobson & Newman, 2014); however, the construct of avoidance was assessed with a one-item measure, which could yield unstable estimates. The present study built on the prior study by utilizing four-item measures of avoidant coping and recruited a sample of community adults to test if their pattern of findings could generalize across adulthood development. Another study observed that the bidirectional association between depression and anxiety symptoms across one year was either partially or fully mediated by trait rumination in adults (McLaughlin & Nolen-Hoeksema, 2011); despite that, their two-time-point mediation analyses could have yielded biased parameter estimates (Cole & Maxwell, 2003). The current study thus extended prior ones by conducting more rigorous mediation analyses across three waves of measurement (Maxwell & Cole, 2007), and investigating multiple maladaptive coping mechanisms as mediators across a longer timeframe of 18 years. In addition, the present study built on literature by providing analyses at the disorder (vs. symptom) level. This is important as both disorder- and symptom-level information are necessary to guide the development of empirically-supported transdiagnostic treatments and optimize established disorder-specific protocol approaches (Everaert & Joormann, 2019; Spijker, Muntingh, & Batelaan, 2020).
Building on the foregoing theories and existing data, the present study aimed to examine if avoidant coping strategies (i.e., focus on and venting of emotion, behavioral disengagement, denial) would mediate the 18-year relations between MDD and GAD in community adults. Based on theory and literature, we hypothesized that the 18-year bi-directional and positive association between MDD and GAD would be mediated by denial (Hypotheses 1 and 2), focus on and venting of emotion (Hypotheses 3 and 4), and behavioral disengagement (Hypotheses 5 and 6). Specifically, we predicted that elevated baseline MDD and GAD would forecast increased denial, focus on and venting of emotion, and behavioral disengagement 9 years later, above and beyond baseline disorder presence. Moreover, we expected that higher denial, focus on and venting of emotion, and behavioral disengagement would thereby independently predict presence of MDD and GAD following 9 years.
Method
Participants.
This study used the publicly available Midlife Development in the United States (MIDUS) database, and measured data at three different waves, 1995-1996 (Time 1; T1), 2004-2005 (T2), and 2012-2013 (T3) (Brim et al., 2019; Ryff et al., 2017; Ryff et al., 2019). Due to the publicly available nature of this dataset, this study was exempt from Institutional Review Board (IRB) approval. Nonetheless, the original MIDUS investigators received IRB approval from the participating institutions. The 3,294 adults in the sample used for this study participated in all three waves and were able to speak to our research question. At T1, the average age of participants was 45.62 years (range = 20-74, SD = 11.41), 54.61% of participants were female, and 42% were college educated. 89.01% of individuals identified as White, 3.25% African American, and 7.73% Native American, Asian, Pacific Islander or other.
Measures
MDD and GAD were assessed via an in-person semi-structured clinical interview at T1 and T3. Coping strategies were measured using self-report at T2.
Major Depressive Disorder.
The Composite International Diagnostic Interview – Short Form (CIDI-SF) aligned with the Diagnostic and Statistical Manual–Third Edition-Revised (DSM-III-R; Kessler, Andrews, Mroczek, Ustun, & Wittchen, 1998) criteria and was used to diagnose MDD at T1 and T3 . Participants reported on any episodes experienced in the past 12 months. To determine overall severity, we summed depression symptoms from a binary response scale (0 = No and 1 = Yes) across 7-items (e.g., depressed mood, changes in appetite, fatigue, ideation of suicide, sleep disturbances; range = 0-7). For MDD, the specificity (93.9%) and sensitivity (89.6%) of the CIDI-SF were good. The CIDI-SF MDD severity scale also has strong internal consistency (T1 and T3 Cronbach’s α = 0.94 herein) and good retest reliability (Wittchen, 1994).
Generalized Anxiety Disorder.
The DSM-III-R-consistent CIDI-SF was also used to diagnose GAD at T1 and T3. Participants reported the degree to which they experienced symptoms as due to their worries for about half to most days over the past year on a 4-point Likert scale (0 = Never to 3 = Most days) (10-item scale; e.g., restlessness, feeling keyed up, irritability, trouble sleeping, trouble focusing; range = 0-10). For GAD, the CIDI-SF specificity (99.8%) and sensitivity (96.6%) were excellent. Further, the CIDI-SF GAD severity scale has good internal consistency (αs = .80 and .83 at T1 and T3 respectively herein) and strong retest reliability (Abel & Borkovec, 1995; Wittchen, 1994).
Coping Strategies.
Table 1 presents all of the items used to measure coping strategies at T2, assessed with the COPE questionnaire (Carver, Scheier, & Weintraub, 1989). Participants rated items on a four-point Likert scale (1 = not at all; 2 = only a little; 3 = a medium amount; 4 = a lot) assessing trait-level denial, focus on and venting of emotion, and behavioral disengagement. Denial was measured with four items (e.g., “I say to myself ‘This isn’t real’”). The denial scale has good internal consistency (α = 0.76 in this study), strong two-week retest reliability, and good convergent validity and discriminant validity (Carver et al., 1989). Additionally, four items tapped into focus on and venting of emotion (e.g., “I feel a lot of emotional distress and find myself expressing those feelings a lot”). The 4-item focus on and venting of emotion scale has shown good internal consistency (α = 0.82 herein), acceptable two-week retest reliability, and strong construct validity (Carver et al., 1989). Likewise, a four-item scale captured behavioral disengagement (e.g., “I admit to myself that I can’t deal with it and quit trying”). This scale had strong internal consistency (α = 0.72 in this study), good two-week retest reliability, and excellent construct validity (Carver et al., 1989).
Table 1.
Descriptive Data and Correlation Matrix of Study Variables of Interest
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. T2 FOAVE | – | – | – | – | – | – | – |
| 2. T2 Denial | .95*** | – | – | – | – | – | – |
| 3. T2 BD | .92*** | .94*** | – | – | – | – | – |
| 4. T1 MDD | .07*** | .03 | .03 | – | – | – | – |
| 5. T1 GAD | .05*** | .04* | .03 | .29*** | – | – | – |
| 6. T3 MDD | .05*** | .02 | .02 | .28*** | .18*** | – | – |
| 7. T3 GAD | .04* | .03 | .02 | .16*** | .35*** | .34*** | – |
| Mean | 5.30 | 1.99 | 2.82 | 0.69 | 0.14 | 0.60 | 0.13 |
| SD | 2.80 | 2.18 | 2.26 | 1.82 | 0.86 | 1.71 | 0.92 |
| Minimum | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Maximum | 12.00 | 12.00 | 12.00 | 7.00 | 10.00 | 7.00 | 10.00 |
| Skewness | 0.42 | 1.25 | 0.58 | 2.44 | 7.47 | 2.69 | 7.89 |
| Kurtosis | −0.28 | 1.44 | 0.09 | 4.35 | 60.84 | 5.74 | 65.66 |
Note.
p < .001;
p < .01;
p< .05.
BD = behavioral disengagement; FOAVE = focus on and venting of emotion; GAD = generalized anxiety disorder; MDD = major depressive disorder; SD = standard deviation.
Data Analytic Strategy
Longitudinal structural equation modeling analyses were conducted with the Lavaan package using RStudio software (Version 1.3.959). In terms of evaluating the fit of our various models, we utilized the confirmatory fit index (CFI) (Bentler, 1990; McDonald & Marsh, 1990), root mean square error of approximation (RMSEA) (Browne & Cudeck, 1993; Steiger, 1990), and standardized root mean square residual (SRMR) (Hu & Bentler, 1999). As the manifest indicators of the latent variables of coping strategies, MDD, and GAD were ordinal in nature. We performed all analyses with maximum likelihood with robust estimators to maximize power and reduce biases in the parameter estimates (Zhong & Yuan, 2011). Using a series of CFAs, the measurement models were found to have satisfactory to good fit (χ2 = 2.952 – 69.609, p < .770, CFI = 0.968–1.000, RMSEA = 0.000–0.127, SRMR = 0.008–0.034). Additionally, we observed statistically significant standardized factor loadings (all ps < .001) for the indicators of latent T1 MDD (λs = 0.712– 0.953), T1 GAD (λs = 0.558– 0.756), T2 focus on and venting of emotion (λs = 0.686– 0.812), T2 denial (λs = 0.551–0.775), T2 behavioral disengagement (λs = 0.572– 0.685), T3 MDD (λs = 0.712– 0.962), and T3 GAD (λs = 0.606– 0.755).
A product-of-coefficients approach was utilized to conduct mediation analyses of the indirect effects for T1 MDD and T1 GAD predicting T2 avoidant coping (a path), and T2 avoidant coping predicting T3 GAD and T3 MDD severity (b path), beyond the indirect effect (c path). The unstandardized regression coefficients (β) and standard errors were presented, and bootstrapping with 10,000 resampling draws was utilized (Cheung & Lau, 2008). The ratio of the indirect effect (a*b) to the total effect is the mediation effect size, c = a*b + c’, which was expressed in the percentage variance that the T2 avoidant coping mediator accounted for in the bi-directional relation between MDD and GAD across T1 and T3 (Preacher & Kelley, 2011; Wen & Fan, 2015). For a robust analysis, we controlled for baseline symptoms in all of our models (Maxwell & Cole, 2007). In total, 0.1% of the data was missing, and was handled using full information maximum likelihood, the recommended approach (Graham, 2009).
Results
Latent Mediation Analyses
T2 Denial as a Mediator.
First, we tested the hypothesis that the relationship between T1 MDD and T3 GAD (and vice versa) would be mediated by T2 denial. Based on the practical fit indices, this mediation model showed good fit (χ2 (df = 12) = 85.97, p < .001, CFI = .968, RMSEA = .056, SRMR = .032). Supporting Hypothesis 1, higher T1 MDD significantly predicted greater T2 denial (β = 0.102, SE = 0.034, z = 3.026, p = .002), and more T2 denial was significantly related to greater T3 GAD (β = 0.020, SE = 0.010, z = 2.065, p = .039). However, the indirect effect (T1 MDD → T2 denial → T3 GAD) was not statistically significant (β = 0.002, SE = 0.001, z = 1.729, p = .084). Thus, Hypothesis 1 was not supported.
Next, we examined if T2 denial would mediate the T1 GAD–T3 MDD relation. This T1 GAD → T2 denial → T3 MDD mediation model showed acceptable fit (χ2 (df = 12) = 108.02, p < .001, CFI = .971, RMSEA = .052, SRMR = .025). T1 GAD was significantly associated with more T2 denial (β = 0.300, SE = 0.093, z = 3.209, p = .001), but T2 denial did not significantly predict T3 MDD (β = 0.019, SE = 0.015, z = 1.282, p = .200). Simultaneously, the indirect effect (T1 GAD → T2 denial → T3 MDD) was not significant (β = 0.006, SE = 0.005, z = 1.167, p = .243). Therefore, Hypothesis 2 was not supported.
T2 Focus on and Venting of Emotion as a Mediator.
Next, we tested the hypothesis that the association between T1 MDD and T3 GAD (and vice versa) would be mediated by T2 focus on and venting of emotion. This mediation model had good fit (χ2 (df = 12) = 137.18, p < .001, CFI = .974, RMSEA = .061, SRMR = .028). Supporting Hypothesis 3, higher T1 MDD significantly predicted greater T2 focus on and venting of emotion (β = 0.406, SE = 0.046, z = 8.857, p < .001), and more T2 focus on and venting of emotion was significantly related to greater T3 GAD (β = 0.017, SE = 0.005, z = 3.257, p = .001). Additionally, the indirect effect (T1 MDD → T2 focus on and venting of emotion → T3 GAD) was significant (β = 0.007, SE = 0.002, z = 2.996, p = .003). T2 focus on and venting of emotion accounted for 20.59% of the T1 MDD–T3 GAD association. Thus, Hypothesis 3 was supported.
The T1 GAD → T2 focus on and venting of emotion → T3 MDD mediation model displayed acceptable fit (χ2 (df = 12) = 190.71, p < .001, CFI = .961, RMSEA = .072, SRMR = .051). Lending support to Hypothesis 4, T1 GAD was significantly associated with higher T2 focus on and venting of emotion (β = 0.484, SE = 0.097, z = 4.993, p < .001), and greater T2 focus on and venting of emotion significantly predicted higher T3 MDD severity (β = 0.048, SE = 0.010, z = 4.793, p < .001). Also, the indirect effect (T1 GAD → T2 focus on and venting of emotion → T3 MDD) was significant (β = 0.023, SE = 0.007, z = 3.390, p = .001). T2 focus on and venting of emotion explained 16.08% of the T1 GAD-T3 MDD relation. Thus hypothesis 4 was supported. Figures 1 and 2 depict the regression path coefficients, standard errors, factor loadings, item error variances, and T1 MDD-GAD correlation, of the parameter estimates for Hypotheses 3 and 4.
Figure 1. Focus on Emotion and Venting as a Mediator of MDD Predicting GAD 18 Years Later.
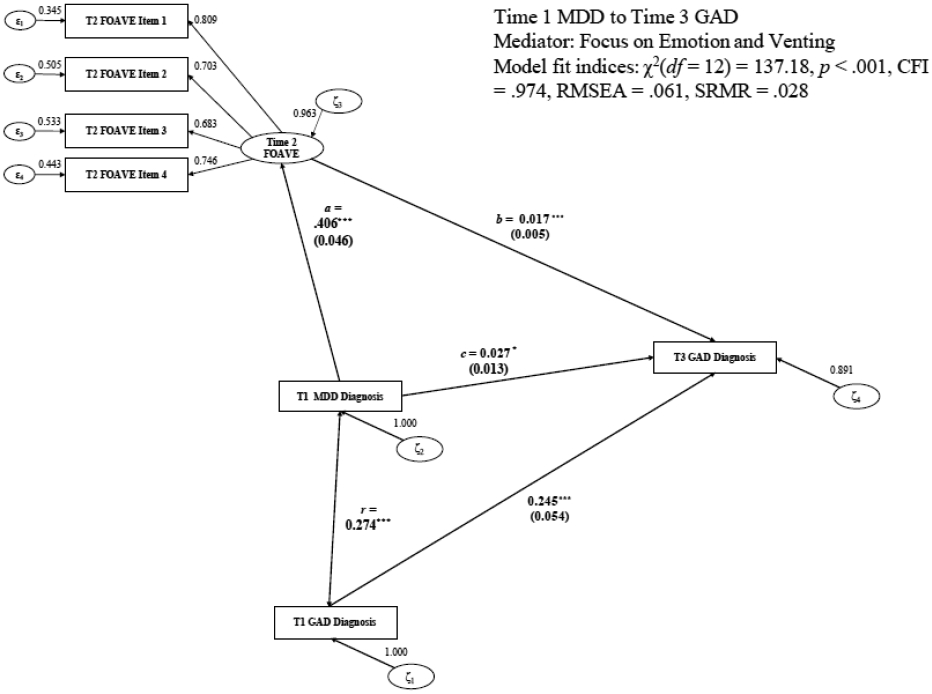
Note. ***p < .001; **p < .01; *p < .05.
MDD = major depressive disorder; GAD = generalized anxiety disorder.
Figure 2. Focus on Emotion and Venting as a Mediator of GAD Predicting MDD 18 Years Later.
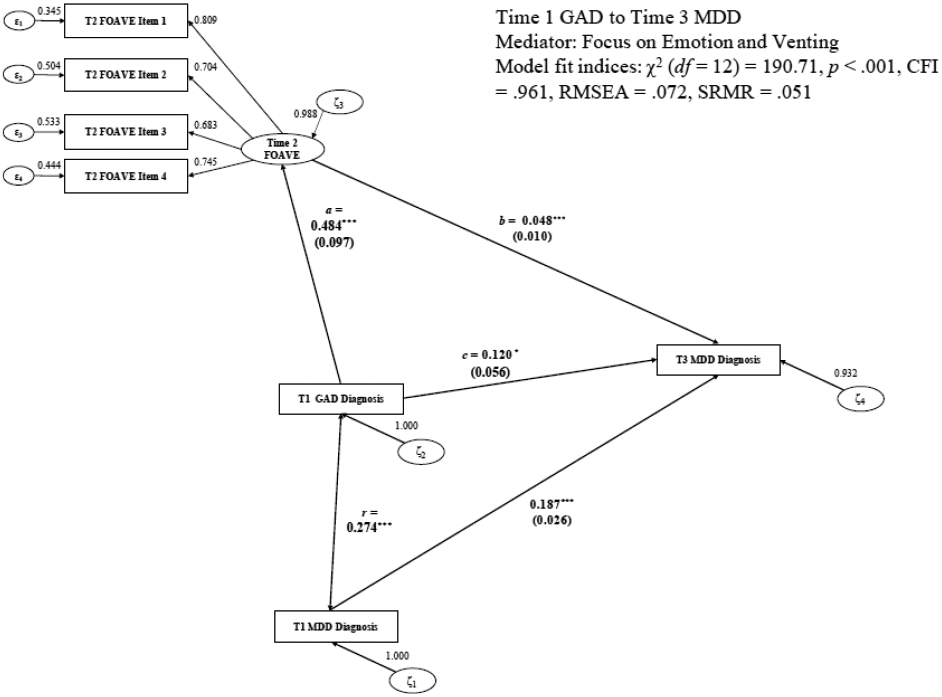
Note. ***p < .001; **p < .01; *p < .05. MDD = major depressive disorder; GAD = generalized anxiety disorder.
T2 Behavioral Disengagement as a mediator.
Following this, we examined the hypothesis that the T1 MDD–T3 GAD association (and vice versa) would be mediated by T2 behavioral disengagement. Based on the practical fit indices, this mediation model showed good fit (χ2 (df = 12) = 22.39, p = .033, CFI = .997, RMSEA = .015, SRMR = .018). T1 MDD significantly predicted more T2 behavioral disengagement (β = 0.127, SE = 0.034, z = 3.753, p < .001), but T2 behavioral disengagement did not significantly relate to T3 GAD (β = 0.014, SE = 0.009, z = 1.574, p = .116). Additionally, the indirect effect (T1 MDD → T2 behavioral disengagement → T3 GAD) was not significant (β = 0.002, SE = 0.001, z = 1.409, p = .159). Therefore, Hypothesis 5 was not supported.
Finally, we tested the hypothesis that behavioral disengagement would mediate the T1 GAD-T3 MDD relation. The T1 GAD → T2 behavioral disengagement → T3 MDD mediation model showed good fit (χ2 (df = 12) = 28.03, p = .005, CFI = .994, RMSEA = .021, SRMR = .020). T1 GAD was significantly associated with higher T2 behavioral disengagement (β = 0.260, SE = 0.081, z = 3.223, p = .001), but T2 behavioral disengagement did not significantly predict T3 MDD (β = 0.027, SE = 0.014, z = 1.895, p = .058). Also, the indirect effect (T1 GAD → T2 behavioral disengagement → T3 MDD) was not significant (β = 0.007, SE = 0.005, z = 1.558, p = .119). Thus, Hypothesis 6 was not supported.
Discussion
Results suggested that focus on and venting of emotion may be a mechanism by which GAD may lead to MDD 18 years later (and vice versa), accounting for 16.08% of the T1 GAD-T3 MDD association, and 20.59% of the T1 MDD-T3 GAD relation. Also, although T1 MDD and T1 GAD predicted higher T2 denial, and greater T2 denial thereby forecasted T3 GAD, denial did not mediate the 18-year bi-directional relations between MDD and GAD. Further, although T1 GAD and T1 MDD preceded and predicted greater T2 behavioral disengagement, T2 behavioral disengagement did not present as a risk factor for T3 MDD and GAD. Overall, our findings partially supported our hypotheses and the transactional model of stress and coping and learned helplessness theories (Lazarus & Folkman, 1984; Swanson, Dougall, & Baum, 2012), furthering the idea that GAD and MDD are linked to maladaptive coping behavior repertoires across long durations. We offer potential accounts for our complex pattern of findings.
Why did greater T1 MDD and GAD render people more vulnerable to higher focus on and venting of emotion, denial, and behavioral disengagement at T2? In general, these findings lend credence to cognitive and behavioral scar theories which propose that experiences of psychopathology can reinforce poor habits, such as chronic rumination, avoidance, passivity, and adoption of limiting mindsets across long durations (Hong, 2007; Zainal & Newman, 2019). Stated differently, prior MDD and GAD might “scar” individuals and render them susceptible to future long term relapses via continual information processing biases, suboptimal lifestyles, dissatisfying social relationships, and associated factors (see empirical review by Burcusa & Iacono, 2007). Relatedly, it is plausible that people with MDD and GAD were inclined to rigidly avoid dealing with their problems instead of confronting them head-on by using a wide repertoire of coping approaches. This construal is aligned with data that whereas healthy controls tend to flexibly and optimally utilize myriad situation-specific coping mechanisms (approach, avoidance, escape), GAD- and MDD-disordered persons tend to rigidly choose avoidant coping approaches (Haskell, Britton, & Servatius, 2020). Denial, focus on and venting of emotion, and behavioral disengagement are also likely to be intrinsically linked to unhelpful self-referential repetitive thinking (i.e., focusing on negative feelings triggered by dwelling on past stressors or worrying excessively) common in MDD and GAD, as demonstrated in diverse samples (Jakobsson Larsson et al., 2016; Liu, Liu, & Yuan, 2020; Michl, McLaughlin, Shepherd, & Nolen-Hoeksema, 2013; Sumner, Griffith, & Mineka, 2010). Consistent with this interpretation, depression and anxiety disorders have been found to be associated with non-constructive repetitive negative thinking over 3 years (Spinhoven, van Hemert, & Penninx, 2018). Also, the finding that GAD predicted more focus on and venting of emotion might be related to pseudo-problem-solving tendencies in habitual worriers (Llera & Newman, 2020; Provencher, Dugas, & Ladouceur, 2004). Upcoming longitudinal studies can test these ideas.
Further, these results indicate that increased focus on and venting of emotion, but not denial or behavioral disengagement, present as a risk factor for future MDD. In addition, the data suggests that denial and focus on and venting of emotion, but not behavioral disengagement, serve as predictors of subsequent GAD. These findings do not come as a surprise. Extensive cross-sectional research has documented strong relations between more frequent passive coping behaviors and elevated depression and anxiety across diverse cultures (e.g., North American, European, Asian samples; Marguerite et al., 2017; Suzuki et al., 2018). Further, focus on and venting of emotion can be viewed as part of cognitive and behavioral deficits repertoire across social and nonsocial domains (Ottenbreit, Dobson, & Quigley, 2014). It may also relate to the tendency to avoid positive emotions as a negatively reinforcing way to experience temporary relief at the cost of prolonged, chronic, and increased negative affect; a feature consistently observed in clinical anxiety and depression (Buhk, Schadegg, Dixon, & Tull, 2020). Similarly, by venting emotions and avoiding addressing problems head-on, individuals tend to prolong stressful events, rather than actively working to find and implement effective, concrete, and actionable solutions to alleviate their mental health symptoms and prevent a downward spiral into anxiety and depression disorders. The excessive use of ruminative brooding akin to focus on and venting of emotion has been shown to be related to increased depression and anxiety in various clinical and community-dwelling adult samples (Lee et al., 2001; Michl et al., 2013; Pollard & Kennedy, 2007). Similar findings have been found in adolescents and children, with maladaptive coping (e.g., avoidance, denial), resulting in later higher levels of psychopathology symptoms (Compas et al., 2017). Future studies can test these speculations by further investigating the impact that focus on and venting of emotion and related problem-solving strategies can have on individuals’ mental health at different life stages.
Several limitations deserve consideration. The sample used in the current study was comprised of predominately White, middle-to-upper income individuals. Future studies may test whether these patterns of findings extend to more diverse cultural and socio-economic backgrounds. Additionally, MDD and GAD were measured in this study using DSM-III-R instead of the latest DSM-5, which future replication efforts should utilize. Unmeasured third variables (e.g., gender differences in problem-solving and coping approaches; Sigmon et al., 2004) should also be considered in upcoming studies. Nonetheless, strengths of this study include its prospective design that allowed for the establishment of temporal precedence and evaluation of participants’ disorder development over a longer time course than previous studies that used cross-sectional designs or shorter durations. Additionally, the present study used psychometrically reliable and valid measures for the purposes of assessing coping behaviors as well as gold standard clinical interviews to determine MDD and GAD diagnoses. Future studies could expand the age range of the sample to investigate the timeline of this relationship from childhood or adolescence to older adulthood. Such endeavors could offer more information on the long-term developmental ramifications of avoidant coping tendencies during youth.
Our findings present with several clinical implications. Interventions used to treat depression and anxiety disorders could target the coping mechanisms we studied, in particular, venting of emotion. By targeting venting, clinicians may be able to relieve both GAD and MDD symptoms more effectively, whereas focusing on remediating behavioral disengagement or denial may only impact symptoms of one or the other. For example, applied relaxation, problem-solving training, and cognitive therapy have been shown to be clinically effective in reducing symptoms of GAD and MDD (Beaudreau, Gould, Mashal, Terri Huh, & Kaci Fairchild, 2019; Kirkham, Seitz, & Choi, 2015; Newman, Zainal, & Hoyer, 2020; Provencher et al., 2004). To this end, clinicians could apply the theories examined herein for persons with MDD and GAD by helping them to utilize active coping (e.g., exercising agency) versus passive coping toward life situations and vulnerabilities largely within their control.
Highlights.
Longitudinal structural equation modeling analyses were performed.
Major depressive disorder (MDD) predicted generalized anxiety disorder (GAD) 18 years later and conversely.
Focus on and venting of emotion (FOAVE) mediated the 18-year MDD-GAD relations.
Behavioral disengagement (BD) and denial did not mediate the 18-year MDD-GAD relations.
Baseline MDD and GAD predicted greater BD and denial 9 years later, but not vice versa.
Acknowledgements
The data used in this publication were made available by the Data Archive on University of Wisconsin - Madison Institute on Aging, 1300 University Avenue, 2245 MSC, Madison, Wisconsin 53706-1532. Since 1995 the Midlife Development in the United States (MIDUS) study has been funded by the following: John D. and Catherine T. MacArthur Foundation Research Network; National Institute on Aging (P01-AG020166); National Institute on Aging (U19-AG051426). The original investigators and funding agency are not responsible for the analyses or interpretations presented here.
Footnotes
Conflict of Interest
My research team, Ms. Zainal, Dr. Newman, and I, do not have any conflicts of interest in regards to the authorship, research, and/or publication of this article, and have enclosed the manuscript and tables in Microsoft word format. All authors are affiliated with PSU.
Statement of Ethics
This study was conducted in compliance with the American Psychological Association (APA) ethical standards in the treatment of human participants and approved by the institutional review board (IRB). Further, this research was conducted was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. Informed consent was obtained from participants as per IRB requirements at Harvard University, Georgetown University, University of California at Los Angeles, and University of Wisconsin. Since this study used a publicly available dataset, it was exempt from IRB approval.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abel JL, & Borkovec TD (1995). Generalizability of DSM-III-R generalized anxiety disorders to proposed DSM-IV criteria and cross-validation of proposed changes. Journal of Anxiety Disorders, 9, 303–315. doi: 10.1016/0887-6185(95)00011-C [DOI] [Google Scholar]
- Arnett PA, & Randolph JJ (2006). Longitudinal course of depression symptoms in multiple sclerosis. Journal of Neurology, Neurosurgery, and Psychiatry, 77, 606–610. doi: 10.1136/jnnp.2004.047712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avis NE, Levine B, Naughton MJ, Case LD, Naftalis E, & Van Zee KJ (2013). Age-related longitudinal changes in depressive symptoms following breast cancer diagnosis and treatment. Breast Cancer Research and Treatment, 139, 199–206. doi: 10.1007/s10549-013-2513-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartek ME, Zainal NH, & Newman MG (2021). Individuals’ marital instability mediates the association of their perceived childhood parental affection predicting adulthood depression across 18 years. Journal of Affective Disorders, 291, 235–242. doi: 10.1016/j.jad.2021.04.091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaudreau SA, Gould CE, Mashal NM, Terri Huh JW, & Kaci Fairchild J (2019). Application of problem solving therapy for late-life anxiety. Cognitive and Behavioral Practice, 26, 381–394. doi: 10.1016/j.cbpra.2018.05.003 [DOI] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. doi: 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Beutel ME, Glaesmer H, Wiltink J, Marian H, & Brähler E (2010). Life satisfaction, anxiety, depression and resilience across the life span of men. Aging Male, 13, 32–39. doi: 10.3109/13685530903296698 [DOI] [PubMed] [Google Scholar]
- Bonnet F, Irving K, Terra J-L, Nony P, Berthezène F, & Moulin P (2005). Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis, 178, 339–344. doi: 10.1016/j.atherosclerosis.2004.08.035 [DOI] [PubMed] [Google Scholar]
- Brim OG, Baltes PB, Bumpass LL, Cleary PD, Featherman DL, Hazzard WR, … Shweder RA (2019). Midlife in the United States (MIDUS 1), 1995-1996: Inter-university Consortium for Political and Social Research [distributor]. [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternate ways of assessing model fit. In Bollen KA & Long JS (Eds.), Testing equation models (pp. 136–162). Newbury Park, CA: Sage. [Google Scholar]
- Buhk AH, Schadegg MJ, Dixon LJ, & Tull MT (2020). Investigating the role of negative and positive emotional avoidance in the relation between generalized anxiety disorder and depression symptom severity. Journal of Contextual Behavioral Science, 16, 103–108. doi: 10.1016/j.jcbs.2020.03.006 [DOI] [Google Scholar]
- Burcusa SL, & Iacono WG (2007). Risk for recurrence in depression. Clinical Psychology Review, 27, 959–985. doi: 10.1016/j.cpr.2007.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, & Weintraub JK (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56, 267–283. doi: 10.1037//0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- Cheung GW, & Lau RS (2008). Testing mediation and suppression effects of latent variables: Bootstrapping with structural equation models. Organizational Research Methods, 11, 296–325. doi: 10.1177/1094428107300343 [DOI] [Google Scholar]
- Cole DA, & Maxwell SE (2003). Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology, 112, 558–577. doi: 10.1037/0021-843x.112.4.558 [DOI] [PubMed] [Google Scholar]
- Compas BE, Jaser SS, Bettis AH, Watson KH, Gruhn MA, Dunbar JP, … Thigpen JC (2017). Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin, 143, 939–991. doi: 10.1037/bul0000110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del-Pino-Casado R, Serrano-Ortega N, López-Martínez C, & Orgeta V (2019). Coping strategies and psychological distress in family carers of frail older people: A longitudinal study. Journal of Affective Disorders, 256, 517–523. doi: 10.1016/j.jad.2019.06.038 [DOI] [PubMed] [Google Scholar]
- Dismuke CE, & Egede LE (2010). Association between major depression, depressive symptoms and personal income in US adults with diabetes. General Hospital Psychiatry, 32, 484–491. doi: 10.1016/j.genhosppsych.2010.06.004 [DOI] [PubMed] [Google Scholar]
- Elliot AJ, Thrash TM, & Murayama K (2011). A longitudinal analysis of self-regulation and well-being: Avoidance personal goals, avoidance coping, stress generation, and subjective well-being. Journal of Personality, 79, 643–674. doi: 10.1111/j.1467-6494.2011.00694.x [DOI] [PubMed] [Google Scholar]
- Everaert J, & Joormann J (2019). Emotion regulation difficulties related to depression and anxiety: A network approach to model relations among symptoms, positive reappraisal, and repetitive negative thinking. Clinical Psychological Science, 7, 1304–1318. doi: 10.1177/2167702619859342 [DOI] [Google Scholar]
- Graham JW (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. doi: 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Haskell AM, Britton PC, & Servatius RJ (2020). Toward an assessment of escape/avoidance coping in depression. Behavioural Brain Research, 381, 112363. doi: 10.1016/j.bbr.2019.112363 [DOI] [PubMed] [Google Scholar]
- Hong RY (2007). Worry and rumination: Differential associations with anxious and depressive symptoms and coping behavior. Behaviour Research and Therapy, 45, 277–290. doi: 10.1016/j.brat.2006.03.006 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jacobson NC, & Newman MG (2014). Avoidance mediates the relationship between anxiety and depression over a decade later. Journal of Anxiety Disorders, 28, 437–445. doi: 10.1016/j.janxdis.2014.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NC, & Newman MG (2017). Anxiety and depression as bidirectional risk factors for one another: A meta-analysis of longitudinal studies. Psychological Bulletin, 143, 1155–1200. doi: 10.1037/bul0000111 [DOI] [PubMed] [Google Scholar]
- Jacobson NC, & Newman MG (2016). Perceptions of close and group relationships mediate the relationship between anxiety and depression over a decade later. Depression and Anxiety, 33, 66–74. doi: 10.1002/da.22402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakobsson Larsson B, Nordin K, & Nygren I (2016). Coping with amyotrophic lateral sclerosis; from diagnosis and during disease progression. Journal of the Neurological Sciences, 361, 235–242. doi: 10.1016/j.jns.2015.12.042 [DOI] [PubMed] [Google Scholar]
- Just N, Abramson LY, & Alloy LB (2001). Remitted depression studies as tests of the cognitive vulnerability hypotheses of depression onset: A critique and conceptual analysis. Clinical Psychology Review, 21, 63–83. doi: 10.1016/S0272-7358(99)00035-5 [DOI] [PubMed] [Google Scholar]
- Kessler RC, & Wang PS (2008). The descriptive epidemiology of commonly occurring mental disorders in the United States. Annual Review of Public Health, 29, 115–129. doi: 10.1146/annurev.publhealth.29.020907.090847 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Demler O, & Stang PE (2003). Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: Results from the National Comorbidity Survey. Journal of Occupational and Environmental Medicine, 45, 1257–1266. doi: 10.1097/01.jom.0000100000.70011.bb [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, & Wittchen H-U (1998). The World Health Organization Composite International Diagnostic Interview short-form (CIDI-SF). International Journal of Methods in Psychiatric Research, 7, 171–185. doi: 10.1002/mpr.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, … Zaslavsky AM (2008). Individual and societal effects of mental disorders on earnings in the United States: Results from the national comorbidity survey replication. American Journal of Psychiatry, 165, 703–711. doi: 10.1176/appi.ajp.2008.08010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham J, Seitz D, & Choi NG (2015). Meta-analysis of problem solving therapy for the treatment of depression in older adults. The American Journal of Geriatric Psychiatry, 23, S129–S130. doi: 10.1016/j.jagp.2014.12.131 [DOI] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal and coping. New York: Springer. [Google Scholar]
- Lee JN, Rigby SA, Burchardt F, Thornton EW, Dougan C, & Young CA (2001). Quality of life issues in motor neurone disease: the development and validation of a coping strategies questionnaire, the MND Coping Scale. Journal of the Neurological Sciences, 191, 79–85. doi: 10.1016/S0022-510X(01)00619-0 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Steinmetz JL, Larson DW, & Franklin J (1981). Depression-related cognitions: Antecedent or consequence? Journal of Abnormal Psychology, 90, 213–219. doi: 10.1037/0021-843X.90.3.213 [DOI] [PubMed] [Google Scholar]
- Liu C, Liu Z, & Yuan G (2020). The longitudinal influence of cyberbullying victimization on depression and posttraumatic stress symptoms: The mediation role of rumination. Archives of Psychiatric Nursing, 34, 206–210. doi: 10.1016/j.apnu.2020.05.002 [DOI] [PubMed] [Google Scholar]
- Llera SJ, & Newman MG (2020). Worry impairs the problem-solving process: Results from an experimental study. Behaviour Research and Therapy, 135, 103759. doi: 10.1016/j.brat.2020.103759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier SF, & Seligman MEP (2016). Learned helplessness at fifty: Insights from neuroscience. Psychological Review, 123, 349–367. doi: 10.1037/rev0000033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marguerite S, Laurent B, Marine A, Tanguy L, Karine B, Pascal A, & Xavier Z (2017). Actor-partner interdependence analysis in depressed patient-caregiver dyads: Influence of emotional intelligence and coping strategies on anxiety and depression. Psychiatry Research, 258, 396–401. doi: 10.1016/j.psychres.2017.08.082 [DOI] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12, 23–44. doi: 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- McDonald RP, & Marsh HW (1990). Choosing a multivariate model: Noncentrality and goodness of fit. Psychological Bulletin, 107, 247–255. doi: 10.1037/0033-2909.107.2.247 [DOI] [Google Scholar]
- McLaughlin KA, & Nolen-Hoeksema S (2011). Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy, 49, 186–193. doi: 10.1016/j.brat.2010.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michl LC, McLaughlin KA, Shepherd K, & Nolen-Hoeksema S (2013). Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology, 122, 339–352. doi: 10.1037/a0031994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, & Zainal NH (2020). The value of maintaining social connections for mental health in older people. The Lancet Public Health, 5, e12–e13. doi: 10.1016/s2468-2667(19)30253-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Zainal NH, & Hoyer J (2020). Cognitive-behavioral therapy (CBT) for generalized anxiety disorder (GAD). In Gerlach AL & Gloster AT (Eds.), Generalized Anxiety Disorder and Worrying (pp. 203–230). NY: John Wiley & Sons. doi: 10.1002/9781119189909.ch10 [DOI] [Google Scholar]
- Ottaviani C, Watson DR, Meeten F, Makovac E, Garfinkel SN, & Critchley HD (2016). Neurobiological substrates of cognitive rigidity and autonomic inflexibility in generalized anxiety disorder. Biological Psychology, 119, 31–41. doi: 10.1016/j.biopsycho.2016.06.009 [DOI] [PubMed] [Google Scholar]
- Ottenbreit ND, Dobson KS, & Quigley L (2014). An examination of avoidance in major depression in comparison to social anxiety disorder. Behaviour Research and Therapy, 56, 82–90. doi: 10.1016/j.brat.2014.03.005 [DOI] [PubMed] [Google Scholar]
- Pollard C, & Kennedy P (2007). A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: A 10-year review. British Journal of Health Psychology, 12, 347–362. doi: 10.1348/135910707X197046 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Kelley K (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16, 93–115. doi: 10.1037/a0022658 [DOI] [PubMed] [Google Scholar]
- Provencher MD, Dugas MJ, & Ladouceur R (2004). Efficacy of problem-solving training and cognitive exposure in the treatment of generalized anxiety disorder: A case replication series. Cognitive and Behavioral Practice, 11, 404–414. doi: 10.1016/S1077-7229(04)80057-9 [DOI] [Google Scholar]
- Rabinowitz AR, & Arnett PA (2009). A longitudinal analysis of cognitive dysfunction, coping, and depression in multiple sclerosis. Neuropsychology, 23, 581–591. doi: 10.1037/a0016064 [DOI] [PubMed] [Google Scholar]
- Ryff C, Almeida DM, Ayanian J, Carr DS, Cleary PD, Coe C, … Williams D (2017). Midlife in the United States (MIDUS 2), 2004-2006: Inter-university Consortium for Political and Social Research [distributor]. [Google Scholar]
- Ryff CD, Almeida DM, Ayanian J, Binkley N, Carr DS, Coe C, … Williams D (2019). Midlife in the United States (MIDUS 3), 2013-2014. Ann Arbor, MI: Inter-university Consortium for Political and Social Research. [Google Scholar]
- Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, … Koushede V (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. The Lancet Public Health, 5, e62–e70. doi: 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- Seligman LD, & Ollendick TH (1998). Comorbidity of anxiety and depression in children and adolescents: An integrative review. Clinical Child and Family Psychology Review, 1, 125–144. doi: 10.1023/a:1021887712873 [DOI] [PubMed] [Google Scholar]
- Shin KE, & Newman MG (2019). Self- and other-perceptions of interpersonal problems: Effects of generalized anxiety, social anxiety, and depression. Journal of Anxiety Disorders, 65, 1–10. doi: 10.1016/j.janxdis.2019.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigmon ST, Whitcomb-Smith SR, Rohan KJ, & Kendrew JJ (2004). The role of anxiety level, coping styles, and cycle phase in menstrual distress. Journal of Anxiety Disorders, 18, 177–191. doi: 10.1016/S0887-6185(02)00243-8 [DOI] [PubMed] [Google Scholar]
- Spijker J, Muntingh A, & Batelaan N (2020). Advice for clinicians on howto treat comorbid anxiety and depression. JAMA Psychiatry, 77, 645–646. doi: 10.1001/jamapsychiatry.2020.0601 [DOI] [PubMed] [Google Scholar]
- Spinhoven P, van Hemert AM, & Penninx BW (2018). Repetitive negative thinking as a predictor of depression and anxiety: A longitudinal cohort study. Journal of Affective Disorders, 241, 216–225. doi: 10.1016/j.jad.2018.08.037 [DOI] [PubMed] [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25, 173–180. doi: 10.1207/s15327906mbr2502_4 [DOI] [PubMed] [Google Scholar]
- Stewart JC, Rand KL, Muldoon MF, & Kamarck TW (2009). A prospective evaluation of the directionality of the depression-inflammation relationship. Brain, Behavior, and Immunity, 23, 936–944. doi: 10.1016/j.bbi.2009.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner JA, Griffith JW, & Mineka S (2010). Overgeneral autobiographical memory as a predictor of the course of depression: A meta-analysis. Behaviour Research and Therapy, 48, 614–625. doi: 10.1016/j.brat.2010.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki M, Furihata R, Konno C, Kaneita Y, Ohida T, & Uchiyama M (2018). Stressful events and coping strategies associated with symptoms of depression: A Japanese general population survey. Journal of Affective Disorders, 238, 482–488. doi: 10.1016/j.jad.2018.06.024 [DOI] [PubMed] [Google Scholar]
- Swanson JN, Dougall AL, & Baum A (2012). Learned helplessness. Encyclopedia of Human Behavior (pp. 525–530). doi: 10.1016/B978-0-12-375000-6.00220-2 [DOI] [Google Scholar]
- Szabo A, Ward C, & Jose PE (2016). Uprooting stress, coping, and anxiety: A longitudinal study of international students. International Journal of Stress Management, 23, 190–208. doi: 10.1037/a0039771 [DOI] [Google Scholar]
- Verhaak CM, Smeenk JMJ, Evers AWM, van Minnen A, Kremer JAM, & Kraaimaat FW (2005). Predicting emotional response to unsuccessful fertility treatment: A prospective study. Journal of Behavioral Medicine, 28, 181–190. doi: 10.1007/s10865-005-3667-0 [DOI] [PubMed] [Google Scholar]
- Wen Z, & Fan X (2015). Monotonicity of effect sizes: Questioning kappa-squared as mediation effect size measure. Psychological Methods, 20, 193–203. doi: 10.1037/met0000029 [DOI] [PubMed] [Google Scholar]
- Wittchen H-U (1994). Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research, 28, 57–84. doi: 10.1016/0022-3956(94)90036-1 [DOI] [PubMed] [Google Scholar]
- Zainal NH, & Newman MG (in press). Depression and worry symptoms predict future executive functioning impairment via inflammation. Psychological Medicine, 1–11. doi: 10.1017/s0033291721000398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainal NH, & Newman MG (2021). Larger increase in trait negative affect is associated with greater future cognitive decline and vice versa across 23 years. Depression and Anxiety, 38, 146–160. doi: 10.1002/da.23093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zainal NH, & Newman MG (2019). Relation between cognitive and behavioral strategies and future change in common mental health problems across 18 years. Journal of Abnormal Psychology, 128, 295–304. doi: 10.1037/abn0000428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong X, & Yuan K-H (2011). Bias and efficiency in structural equation modeling: Maximum likelihood versus robust methods. Multivariate Behavioral Research, 46, 229–265. doi: 10.1080/00273171.2011.558736 [DOI] [PubMed] [Google Scholar]
- Zimmer-Gembeck MJ (2015). Emotional sensitivity before and after coping with rejection: A longitudinal study. Journal ofApplied Developmental Psychology, 41, 28–37. doi: 10.1016/j.appdev.2015.05.001 [DOI] [Google Scholar]


